Achieving FAIR Compliance for Viral Sequence Data: A Guide for Researchers and Drug Developers
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on implementing FAIR (Findable, Accessible, Interoperable, and Reusable) principles for viral sequence data.
Achieving FAIR Compliance for Viral Sequence Data: A Guide for Researchers and Drug Developers
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on implementing FAIR (Findable, Accessible, Interoperable, and Reusable) principles for viral sequence data. It covers the foundational importance of FAIR data in accelerating virology research and outbreak response, explores methodological frameworks for data FAIRification, addresses common troubleshooting and optimization challenges, and presents validation strategies through comparative analysis of existing virus databases and regulatory standards. By synthesizing current best practices and future directions, this resource aims to enhance data-driven discovery in viral genomics, therapeutic development, and public health surveillance.
The Critical Role of FAIR Principles in Modern Virology and Pandemic Preparedness
What are the FAIR Principles?
The FAIR principles are a set of guiding rules designed to improve the Findability, Accessibility, Interoperability, and Reusability of digital assets, with particular emphasis on scientific data management and stewardship [1] [2]. Formally published in 2016, these principles were created by a diverse coalition of stakeholders representing academia, industry, funding agencies, and scholarly publishers [2] [3]. A key differentiator of FAIR is its specific emphasis on enhancing machine-actionability—the capacity of computational systems to find, access, interoperate, and reuse data with minimal human intervention [1] [2]. This addresses the critical challenge of managing data given its increasing volume, complexity, and speed of creation [1].
Frequently Asked Questions
Q: Is FAIR data the same as Open data? A: No. FAIR data is focused on making data structured, richly described, and machine-actionable, but not necessarily publicly available. It can be restricted with proper authentication and authorization. Open data is made freely available to anyone without restrictions but may lack the rich metadata and structure required for computational use [3].
Q: What are the primary benefits of implementing FAIR principles for viral research? A: Implementing FAIR principles enables faster time-to-insight by making data easily discoverable, improves data ROI, supports AI and multi-modal analytics, ensures reproducibility and traceability, and enables better collaboration across organizational silos [3]. One study in a health research context concluded that using a FAIR-based solution could save 56.57% of time and significant costs in research execution [4].
Q: We have legacy viral sequence data. Is it feasible to make this FAIR? A: Yes, but it often presents a common challenge due to the high cost and time investment required for transformation. Legacy data may be in fragmented systems and non-standardized formats, requiring retrofitting to meet FAIR standards [3]. A systematic FAIRification workflow can be applied to convert existing data into FAIR-compliant formats [4].
Q: What is a common real-world example of FAIR implementation for pathogen data? A: The GISAID initiative employs FAIR principles by assigning each viral sequence record a unique and persistent identifier (EPI_ISL ID), making data retrievable via standardized protocols, using broadly accepted data formats (FASTA, FASTQ), and maintaining detailed provenance for reusability [5].
Quantitative Impact of FAIR Implementation
The following table summarizes key quantitative findings related to the benefits and costs of FAIR data implementation from recent research:
Table 1: Quantitative Impact of FAIR Principles Implementation
| Metric | Findings | Context / Source |
|---|---|---|
| Time Savings | 56.57% time saved in data management tasks | Health research management using FAIR4Health solution [4] |
| Economic Cost of NOT having FAIR data | €10.2 billion per year (estimated minimum) | European Union economy [4] [6] |
| Potential Additional Innovation Loss | €16 billion per year (estimated) | European Union, due to lack of FAIR data [6] |
| Recommended Investment | 5% of overall research costs should go towards data stewardship | Recommendation from expert analysis [4] |
Experimental Protocol: The FAIRification Workflow
Applying FAIR principles to existing data, a process known as "FAIRification," follows a structured pathway. The workflow below, adapted from the FAIR4Health project, details the methodology for converting health research data, such as viral sequence information, into FAIR-compliant data [4].
Diagram 1: FAIRification workflow for health data.
Step-by-Step Protocol:
- Data Curation and Transformation: Use a Data Curation Tool (DCT) to extract, transform, and load raw healthcare and health research data into a standardized, interoperable format. The FAIR4Health project, for instance, used HL7 FHIR (Fast Healthcare Interoperability Resources) repositories for this purpose [4].
- Privacy Preservation: Process the standardized data through a Data Privacy Tool (DPT) to handle privacy challenges inherent in sensitive health data. This involves applying anonymization and de-identification techniques to comply with ethical and legal requirements while preserving data utility [4].
- Metadata Annotation and Identifier Assignment: Enrich the data with rich, machine-readable metadata. This critical step includes assigning a globally unique and persistent identifier (e.g., a DOI or an accession number like GISAID's EPI_ISL ID) to each dataset [5] [4]. The metadata should use formal, accessible, and broadly applicable languages and vocabularies [1].
- Repository Deposit and Indexing: Register or index the (meta)data in a searchable resource. This could be a general-purpose repository (e.g., Zenodo, FigShare) or a special-purpose repository for viral data (e.g., GISAID, GenBank) to ensure maximum findability [1] [2].
Troubleshooting Common FAIR Implementation Challenges
The following table addresses specific issues researchers might encounter when working towards FAIR compliance for viral sequence data, along with potential solutions.
Table 2: Troubleshooting Guide for FAIR Implementation
| Challenge | Specific Issue | Potential Solution |
|---|---|---|
| Findability | Data and metadata are scattered across platforms and file formats, making them hard to locate [6]. | Solution: Implement a centralized data indexing system. Assign globally unique and persistent identifiers (e.g., DOIs, EPI_ISL IDs) to each dataset and its metadata. Register datasets with global registries like re3data.org [1] [5]. |
| Accessibility | Data access is restricted due to privacy, proprietary concerns, or unclear authentication protocols [6]. | Solution: Use standardized, open communications protocols (like HTTPS). Implement clear authentication and authorization procedures where necessary, and ensure metadata remains accessible even if the data itself is no longer available [1] [5]. |
| Interoperability | Incompatible software systems, tools, and a lack of standardized data models or ontologies impede data integration [6]. | Solution: Use formal, accessible, and shared languages for knowledge representation. Store and exchange data in broadly accepted, machine-readable formats (e.g., CSV, JSON, FASTA, FASTQ). Use community-standardized vocabularies and ontologies for metadata fields [5] [7]. |
| Reusability | Inadequate documentation, incomplete metadata, and unclear licensing affect data quality and reliability, hindering reuse [6]. | Solution: Ensure (meta)data are richly described with a plurality of accurate and relevant attributes. Maintain clear provenance information and state data usage licenses clearly. Adhere to relevant community standards developed with domain experts [1] [5]. |
| Cultural & Resource | Lack of recognition for data sharing, limited incentives, and insufficient infrastructure or technical expertise [6]. | Solution: Advocate for institutional policies that recognize and reward data sharing. Invest in training and secure resources for data stewardship, which is recommended to be ~5% of overall research costs [4] [3]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
This table details key materials, tools, and infrastructure components essential for conducting research and ensuring FAIR compliance of viral sequence data.
Table 3: Research Reagent Solutions for FAIR Viral Sequence Data Management
| Item / Solution | Function in FAIR Compliance |
|---|---|
| Trusted Data Repository (e.g., GISAID, GenBank, Zenodo) | Provides a sustainable infrastructure for depositing, preserving, and providing access to data. Ensures persistent identifiers and indexing, fulfilling Findability and Accessibility principles [5] [2]. |
| Standardized Ontologies & Vocabularies (e.g., SNOMED CT, MeSH) | Provides a formal, accessible, shared language for knowledge representation. Enables semantic interoperability by ensuring metadata uses consistent, FAIR-compliant vocabularies, fulfilling the Interoperability principle [7] [3]. |
| Data Curation Tool (DCT) | Facilitates the extraction, transformation, and loading of raw data into standardized, interoperable formats (e.g., HL7 FHIR). A core component of the FAIRification workflow [4]. |
| Data Privacy Tool (DPT) | Handles the anonymization and de-identification of sensitive health data, allowing for Accessibility and Reusability while complying with ethical and legal requirements [4]. |
| Persistent Identifier Service (e.g., DOI, EPI_ISL ID) | Mints globally unique and persistent identifiers for datasets. This is a foundational requirement for data Findability, Accessibility, and citation [1] [5]. |
| Machine-Readable Metadata Schema | A structured template for capturing rich, machine-actionable metadata. This is critical for making data Findable by computers and Reusable by others by providing essential context [1] [2]. |
In the fields of viral genomics and outbreak response, the vast and growing volume of sequence data presents both an unprecedented opportunity and a significant challenge. The FAIR Guiding Principles—making data Findable, Accessible, Interoperable, and Reusable—provide a critical framework for managing this deluge of information [3]. For researchers, scientists, and drug development professionals, FAIR compliance transforms raw viral sequences into a powerful, collaborative resource that can accelerate scientific discovery and strengthen public health responses to emerging threats [5] [8].
Adhering to FAIR principles ensures that data from arduous field collection and meticulous laboratory work can be fully leveraged by the global community, enabling rapid development of countermeasures, as evidenced during the COVID-19 pandemic [9]. This technical support center is designed to help you navigate the practical implementation of these principles, troubleshoot common issues, and integrate best practices into your research workflow.
Troubleshooting FAIR Compliance: A Guide for Researchers
Frequently Asked Questions (FAQs)
Table: Common FAIR Compliance Challenges and Solutions
| Challenge Category | Specific Issue | Proposed Solution | Key References/Tools |
|---|---|---|---|
| Data Findability | How to ensure my dataset is discoverable after submission? | Insist on repositories that assign globally unique, persistent identifiers (e.g., EPI_ISL ID in GISAID, DOI) and index data with rich, machine-readable metadata [5]. | GISAID, GenBank, DOI Services |
| Data Accessibility | How to share data responsibly before my own publication? | Utilize a "Data Reuse Information (DRI) Tag" linked to your ORCID to signal a request for collaboration prior to reuse, balancing openness with contributor recognition [9]. | ORCID, DRI Tag Framework [9] |
| Data Interoperability | My metadata is not understood by other labs or platforms. | Use controlled, documented vocabularies and community-agreed standards for metadata fields (e.g., host, location, sequencing method). Store data in broadly accepted, machine-readable formats (CSV, TSV, FASTA, FASTQ) [5] [3]. | Public Health Ontologies, CSV/TSV, FASTA/FASTQ |
| Data Reusability | How to guarantee my data can be replicated and reused? | Provide detailed provenance: include origin, submission info, and laboratory methods. Release data under a clear usage license and adhere to community-defined data quality standards [5] [10]. | GISAID Access Agreement, Creative Commons Licenses |
| Ethical Reuse | How to avoid "helicopter research" and ensure fairness to data contributors? | Actively involve originating researchers in new projects, especially when data lacks a formal publication. Adhere to a "code of honour" for reuse that recognizes data generators [9]. | Roadmap for Equitable Reuse [9] |
Experimental Protocols for FAIR Viral Data Submission
Protocol 1: Submitting Viral Sequence Data to a FAIR-Compliant Repository
This protocol outlines the steps for preparing and submitting viral genome sequence data to a repository like GISAID, which exemplifies FAIR principles [5].
- Select a Repository: Choose a recognized, FAIR-aligned repository such as GISAID or GenBank. The choice may be dictated by funder requirements, journal policies, or pathogen-specific community standards.
- Prepare Sequence Data:
- Format: Assemble the consensus genome and save it in a standard format (e.g., FASTA).
- Quality Control: Verify sequence quality, length, and the absence of contamination.
- Compile Rich Metadata: This is critical for interoperability and reuse. Essential metadata includes [5] [10]:
- Unique Identifier: The repository will often assign this (e.g., EPI_ISL ID).
- Temporal & Geographic: Date and location of specimen collection.
- Host Information: Species, age, sex (where applicable and respecting confidentiality).
- Clinical Context: Disease severity, symptoms, comorbidity, travel history.
- Methodological Data: Sequencing technology, assembly protocol, and bioinformatics tools used.
- Submit Data:
- Follow the repository's submission workflow via its web interface or API.
- Adhere to the specific data-sharing agreement, which governs accessibility and reuse terms [5].
- Obtain Persistent Identifier: Upon acceptance, the repository will mint a persistent identifier (e.g., EPI_ISL ID or DOI). Cite this identifier in any related publications to ensure findability and fulfill acknowledgment requirements [5].
Protocol 2: Implementing a Data Reuse Information (DRI) Tag
For data being prepared for public release, this protocol, based on a 2025 roadmap, helps ensure equitable reuse [9].
- Create an ORCID: Ensure all contributing researchers have a unique, persistent digital identifier (ORCID).
- Link ORCID to Dataset: During submission to a repository, associate the dataset with the ORCIDs of the data collectors.
- Define Reuse Expectations: This linkage acts as the DRI Tag, signaling to the community that the data generators should be contacted and considered for collaboration before the data is reused in new projects.
- Communicate Freely Reusable Status: If the data is intended for immediate and unrestricted reuse, the dataset can be submitted without a linked DRI Tag, making this status clear to potential users [9].
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials and Tools for FAIR-Compliant Viral Genomics
| Item/Tool | Function in FAIR Viral Research |
|---|---|
| High-Throughput Sequencer (e.g., Illumina, Oxford Nanopore) | Generates the primary raw genomic data; portable platforms enable real-time, in-field sequencing during outbreaks [11]. |
| Bioinformatics Pipelines (e.g., detectEVE, Serratus) | Processes raw sequence data, performs quality control, assembly, and annotation; open-source tools ensure methodological interoperability and reproducibility [11] [12]. |
| FAIR-Compliant Repositories (e.g., GISAID, NCBI GenBank) | Provides the infrastructure for storing, sharing, and accessing data with persistent identifiers, access controls, and standardized metadata, fulfilling the core FAIR requirements [5] [3]. |
| Controlled Vocabularies & Ontologies (e.g., Public Health Ontologies) | Provides standardized language for metadata fields, ensuring that data from different sources is interoperable and machine-readable [5] [3]. |
| ORCID (Open Researcher and Contributor ID) | A persistent digital identifier for researchers, crucial for unambiguous attribution of data and for implementing the DRI Tag for equitable reuse [9]. |
| AI/ML Tools for Viral Discovery | Machine learning models and platforms (e.g., Serratus) can scan petabase-scale public sequence data to identify novel viruses, predict host ranges, and classify unknown sequences, relying entirely on the availability of FAIR data for training and operation [8] [11]. |
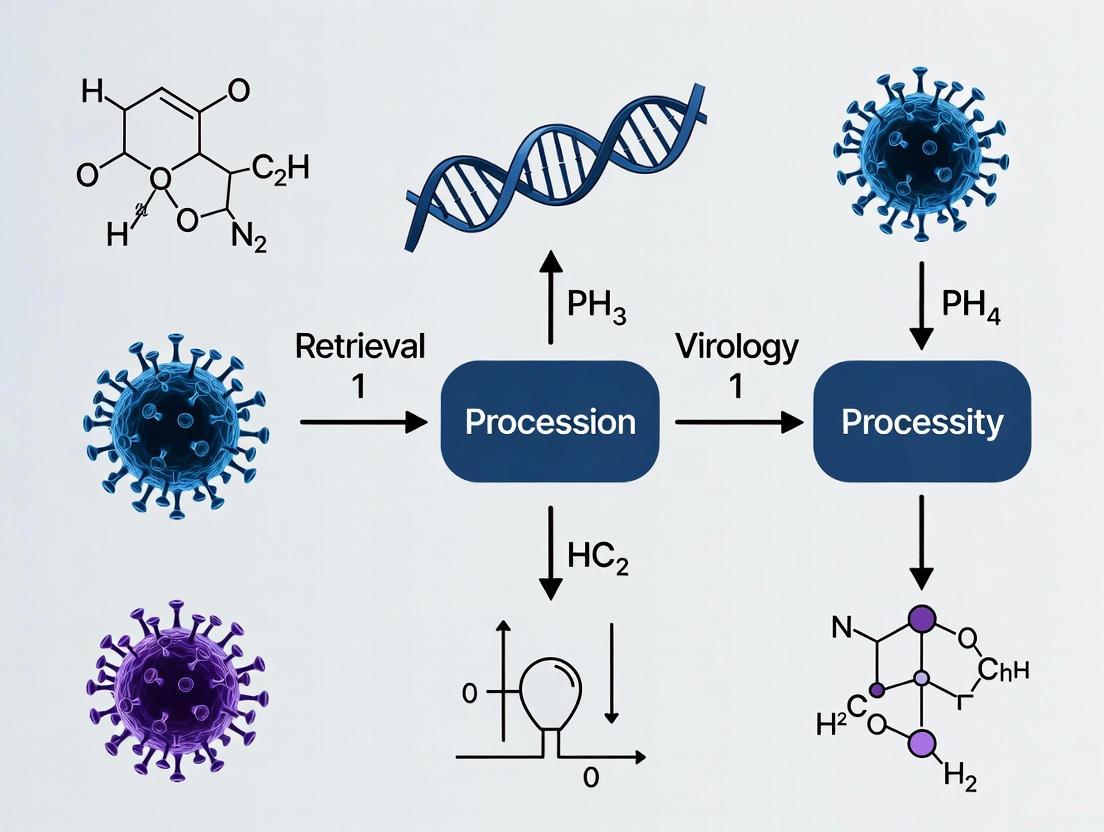
Visualizing the FAIR Data Workflow for Viral Genomics
The following diagram illustrates the logical workflow and interactions between key entities in a FAIR-compliant viral data management system.
FAIR-Compliant Viral Data Lifecycle
Implementing FAIR principles is not merely a technical exercise but a fundamental requirement for maximizing the value of viral sequence data in public health and research. By making data Findable, Accessible, Interoperable, and Reusable, the global scientific community can build a resilient and collaborative ecosystem. This enables faster responses to outbreaks, accelerates drug and vaccine discovery, and ensures that the critical contributions of data generators are recognized and respected. The tools and guidelines provided here offer a practical path toward achieving these essential goals.
Viral sequence databases are critical infrastructures for modern infectious disease research, outbreak response, and drug development. The FAIR principles—Findable, Accessible, Interoperable, and Reusable—provide a framework for evaluating and improving these resources [3]. These principles emphasize machine-actionability, ensuring data is structured not just for human access but for computational systems to process with minimal human intervention [3]. This technical support center addresses common challenges researchers face when working with these databases and provides protocols to ensure their work aligns with FAIR compliance requirements.
The table below summarizes key virus databases and their alignment with FAIR principles.
Table 1: Virus Database Landscape and FAIR Principles Compliance
| Database Name | Primary Content & Coverage | Findability Features | Accessibility Policy | Interoperability Standards | Reusability Provisions |
|---|---|---|---|---|---|
| GISAID | Genetic sequence data from high-impact pathogens (e.g., influenza, SARS-CoV-2) [5] | Unique, persistent EPIISL ID for each sequence; EPISET ID with DOI for collections; indexed in global registries [5] | Free registration with user authentication; data retrievable via HTTPS protocol; metadata remain accessible even if data is withdrawn [5] | Uses standardized formats (CSV, TSV, JSON, FASTA, FASTQ); controlled vocabulary; cross-referencing with publications [5] | Clear access agreement; detailed provenance; data curated to community standards; versioning for updates [5] |
| PalmDB | Database of RNA-dependent RNA polymerase (RdRp) sequences from over 100,000 RNA viruses [13] | Serves as a reference for tools like kallisto to identify viral species in transcriptomic data. | Integrated into open-source software tools (kallisto); enables detection of unexpected or novel viruses in RNA sequence data [13]. | Used with kallisto software for quantifying viral presence in host samples like human lung tissue [13]. | Facilitates the study of viral impact on biological functions and monitoring of emerging diseases [13]. |
| GenBank (NIH) | Annotated collection of all publicly available DNA sequences (Open Data) [3] | Open access: freely available for anyone to access without restrictions [3]. | While open, data is not necessarily FAIR unless properly curated with metadata [3]. |
Troubleshooting Common Database Issues
FAQ 1: My submission to a database was used by another group before I could publish my own analysis. How can I protect my rights?
- Issue: Data generators risk being "scooped" when data is shared rapidly and reused without appropriate attribution or collaboration [9].
- Solution: A new framework proposes the use of a Data Reuse Information (DRI) Tag linked to a researcher's ORCID identifier [9]. When submitting data:
- Provide your ORCID: This unambiguously attributes the dataset to you and signals to potential users that they should contact you before reuse.
- Check for DRI Tags: When reusing data, always check for the presence of a DRI Tag and respect the contributor's guidelines. If the identifier is absent, the data can be considered freely reusable [9].
- FAIR Context: This practice balances the "A" (Accessible) and "R" (Reusable) principles by ensuring accessibility while protecting the authority and rights of data contributors, aligning with ethical data stewardship.
FAQ 2: I found a sequence in a database, but it lacks critical metadata like host information or collection date. How should I proceed?
- Issue: Incomplete metadata severely limits the data's utility for analyses such as transmission dynamics or host tropism.
- Solution:
- Contact the Submitter: Use the contact information provided in the database record, if available.
- Check Linked Publications: Use the database's cross-referencing功能 to find scientific publications that may have used the sequence and contain more context [5].
- Acknowledge the Gap: In your own research, explicitly document this lack of metadata as a limitation.
- FAIR Context: This issue highlights a gap in "F" (Findable) and "R" (Reusable) principles, which require data to be described with rich metadata (R1) to enable reuse [5]. The decision on which metadata to share often remains with the submitter and can be limited by patient confidentiality or resource availability [5].
FAQ 3: I need to integrate genomic sequence data with clinical metadata from a different source. Why is this so difficult?
- Issue: A lack of standardized vocabularies and ontologies across data sources creates interoperability barriers [3].
- Solution:
- Use Controlled Vocabularies: Advocate for and use community-agreed terms for metadata (e.g., for host species, geographic location).
- Leverage Persistent Identifiers: Some databases allow cross-referencing with external clinical datasets using persistent identifiers [5].
- Utilize Interoperable Formats: Work with data exported in standardized, machine-readable formats like CSV, TSV, or JSON [5].
- FAIR Context: This directly addresses the "I" (Interoperable) principle, which requires data to use formal, accessible, and broadly applicable languages for knowledge representation [5] [3].
Experimental Protocol: Submitting Viral Sequence Data to a FAIR-Compliant Repository
This protocol ensures your viral sequence data is submitted in a manner that maximizes its Findability, Accessibility, Interoperability, and Reusability for the global research community.
Table 2: Research Reagent Solutions for Viral Sequencing and Analysis
| Reagent / Material | Function in Viral Research |
|---|---|
| Sample Collection Kit (e.g., nasopharyngeal swab, viral transport media) | Collects and preserves viral material from the host for transport to the laboratory. |
| RNA/DNA Extraction Kit | Isolates and purifies viral genetic material from the patient sample. |
| Reverse Transcription & Amplification Reagents | Converts viral RNA into DNA and amplifies specific genomic regions for sequencing (e.g., via PCR). |
| Next-Generation Sequencing (NGS) Platform | Determines the nucleotide sequence of the amplified viral genome at high throughput. |
| Bioinformatics Tools (e.g., BLAST, Clustal Omega, DeepVariant) | For analyzing sequence data, including assembly, alignment, variant calling, and phylogenetic analysis [14]. |
Procedure:
Pre-Submission: Data and Metadata Collection
- Generate Sequence Data: Use your preferred NGS platform to generate the viral genome sequence. Assemble the raw reads into a consensus sequence.
- Compile Rich Metadata: This is critical for reusability. Collect all relevant information using the database's required controlled vocabulary [5]. Essential metadata includes:
- Virus: Virus name, target gene.
- Host: Host species, health status, anonymity of patient.
- Sample: Sample source (e.g., nasopharyngeal swab), collection date, geographic location.
- Sequencing: Sequencing instrument, assembly method.
- Originating Lab: Lab name, address, responsible scientist.
- Submitting Lab: Lab name, address, submitter name.
Submission: Data Upload and Validation
- Select a FAIR-Compliant Database: Choose an appropriate repository like GISAID for high-impact pathogens [5].
- Register for an Account: Complete the free registration, agreeing to the database's terms of use and access agreement [5].
- Upload Data and Metadata: Use the platform's web interface or API to submit the sequence (in FASTA format) and the associated metadata.
- Validate Your Submission: The database's curation team will perform quality checks on your submission. You may be contacted for clarification or corrections.
Post-Submission: Obtaining Identifier and Citing Data
- Receive Accession Number: Upon successful curation, your data will be assigned a globally unique and persistent identifier (e.g., an EPI_ISL ID in GISAID) [5]. This is the core of Findability.
- Cite the Data in Publications: When publishing, use this accession number in your "Data Availability Statement" to ensure transparency and reproducibility. For a collection of sequences, you may receive an EPI_SET ID with a Digital Object Identifier (DOI) for easier citation [5].
The following diagram outlines the submission and reuse workflow, highlighting key FAIR principles at each stage.
Knowledge Gaps and Future Directions
Despite advances, significant knowledge gaps persist in the landscape of virus databases:
- Equity in Data Sharing: There is a tension between rapid, open data sharing and fairly recognizing the contribution of data generators [9]. The implementation of mechanisms like the DRI Tag is a new development aimed at closing this gap and requires broad community adoption to be effective.
- Metadata Completeness: The variability in the quality and completeness of submitted metadata remains a major hurdle for robust meta-analysis and limits the full reusability of datasets [5].
- Bias in Database Coverage: Genomic databases can be biased towards viruses from certain geographic regions or from hosts of particular economic or medical interest. Initiatives like H3Africa are working to build capacity for genomics research in underrepresented populations and are crucial for creating a truly global atlas of viral diversity [15].
- Integration of FAIR and CARE Principles: While FAIR focuses on data quality and utility, the CARE principles (Collective Benefit, Authority to Control, Responsibility, Ethics) are essential for the ethical handling of data involving Indigenous peoples and other marginalized communities [3]. Future frameworks must integrate both to be both technologically sound and ethically responsible.
Technical Support Center
Troubleshooting Guides
SRA Submission Portal: Common Errors and Solutions
This guide addresses frequent errors encountered during data submission to the Sequence Read Archive (SRA).
| Error / Warning Message | Problem Description | Solution |
|---|---|---|
| Error: Multiple BioSamples cannot have identical attributes [16] | Samples are not distinguishable by at least one controlled attribute; "sample name" or "description" are not considered [16]. | Add distinguishing columns to the attribute sheet (e.g., replicate, salinity, collection time). For biological replicates, add a replicate column [16]. |
| Error: These samples have the same Sample Names and identical attributes [16] | The submission is attempting to create samples that duplicate ones already registered in your account [16]. | On the 'General Info' tab, select Yes for "Did you already register BioSamples?" and use existing sample accessions in your SRA metadata [16]. |
| Warning: You uploaded one or more extra files [16] | Files are present in the upload folder that are not listed in the SRA Metadata table [16]. | Either remove the extra files or update your SRA_metadata spreadsheet to include them. Only files listed in the metadata will be processed [16]. |
| Error: Some files are missing. Upload missing files or fix metadata table. [16] | Files listed in the SRA Metadata table were not found in the submission folder [16]. | Upload the missing files. Check that filenames in your metadata, including extensions, exactly match the uploaded files [16]. |
Error: File <filename> is corrupted [16] |
The file is corrupt, either on your side or due to transfer issues [16]. | Check file integrity (e.g., for gzipped files, use zcat <filename> | tail). Re-upload an uncorrupted version of the file [16]. |
| I uploaded all data files but cannot see any folders when prompted [17] | Files were uploaded directly into the root of the account folder instead of a dedicated subfolder [17]. | Create a subfolder within your account folder and move your files into it. Wait about 15 minutes for file discovery before selecting it [17]. |
Bioinformatic Virus Identification: Tool Selection and Validation
This guide helps troubleshoot issues related to selecting and using bioinformatic tools for identifying viral sequences in metagenomic data.
| Problem Area | Key Challenge | Recommendations & Solutions |
|---|---|---|
| Tool Selection [18] | Performance of virus identification tools is highly variable, with true positive rates from 0–97% and false positive rates from 0–30% [18]. | On real-world data, tools like PPR-Meta, DeepVirFinder, VirSorter2, and VIBRANT show better performance distinguishing viral from microbial contigs [18]. |
| Parameter Adjustment [18] | Using default tool cutoffs may not be optimal for a specific dataset or biome [18]. | Adjust parameter cutoffs before use. Benchmarking indicates that performance improves significantly with adjusted cutoffs [18]. |
| Tool Complementarity [18] | Different tools often identify different subsets of viral sequences [18]. | Employ a multi-tool approach, as most tools find unique viral contigs. This increases the sensitivity of virus detection [18]. |
| Host Association [19] | Incorrectly associating a viral sequence with the sampled species (e.g., the host's diet) rather than the true host [19]. | Perform phylogenetic analysis to validate novel sequences and infer likely hosts. Do not rely solely on the sample source for host assignment [19]. |
| Lack of Phylogenetics [19] | Reporting viruses using only similarity searches (BLAST) or diversity metrics without phylogenetic validation [19]. | Conduct and report phylogenetic analyses. This is central to virus classification and provides a basis for evolutionary and ecological inferences [19]. |
Frequently Asked Questions (FAQs)
Submission and Data Management
Q1: I've registered my BioProject and BioSamples elsewhere. How do I avoid creating duplicates when submitting to SRA? [16] [20] On the "General Info" step of the SRA Submission Wizard, you must select Yes in response to "Did you already register BioSamples for this data set?" This will skip the BioSample creation steps and allow you to use your existing accessions in the SRA metadata [16] [20].
Q2: How do I structure my SRA metadata for multiple experiments or technical replicates? [17]
- Each row in the SRA metadata template represents one Experiment (a unique combination of sample, library, strategy, layout, and instrument model) [17].
- To create multiple experiments (e.g., libraries/replicates) for the same sample, use the same
sample_nameorsample_accessionin multiple rows [17]. - Only one Run is allowed per Experiment. For technical replicates (multiple sequencing runs of the same library), list all file names consecutively in the same row [17].
Q3: What is the recommended way to download SRA data for analysis? [21]
The supported method is to use the prefetch tool from the SRA Toolkit. Avoid using generic tools like ftp or wget, as they can create incomplete files and complicate troubleshooting. prefetch ensures all file dependencies and external reference sequences are correctly downloaded [21].
Q4: My manuscript reviewer needs access to my private submission. How do I provide it? [17] In the Submission Portal's "Manage Data" interface, find your BioProject and press the "Reviewer link" button. This generates a temporary link that provides access to the metadata. Note that this link expires after the data is publicly released [17].
FAIR Principles and Data Compliance
Q5: How does proper SRA submission align with FAIR Data Principles? FAIR Principles provide guidelines to enhance the Findability, Accessibility, Interoperability, and Reuse of digital assets [1]. Submitting to SRA directly supports these principles:
- Findable: Your data is assigned a unique BioProject accession (
PRJNA#) and Run accessions (SRR#), making it indexable and searchable in public databases [17]. - Accessible: Data is retrieved using standardized protocols. While access may be controlled during a publishing embargo, metadata is often accessible, and clear paths to access are provided [5] [3].
- Interoperable: SRA requires data and metadata in specific, standardized formats (e.g., FASTQ, controlled vocabulary for attributes), enabling integration with other datasets and analytical workflows [16] [20].
- Reusable: Rich metadata submitted with your project provides the provenance, context, and experimental detail necessary for others to understand and reuse your data [19] [3].
Q6: What are the common pitfalls in reporting virome-scale metagenomic data that hinder its reusability? [19]
- Insufficient Metadata: Omitting key details like collection date, location, host health status, and sample type limits the ecological context [19].
- Inadequate Methodological Detail: Failing to describe viral enrichment steps, extraction kits, or bioinformatic workflows (e.g., whether all reads were assembled or only those identified as viral) affects reproducibility [19].
- Poor Sequence Characterization: Depositing sequences with no annotation, uninformative names (e.g., "unclassified Riboviria"), or without phylogenetic analysis reduces the utility of public databases [19].
The Scientist's Toolkit: Essential Research Reagents & Solutions
| Item | Function / Application in Virus Discovery |
|---|---|
| SRA Toolkit [21] | A suite of tools, including prefetch and fasterq-dump, to reliably download and access sequencing data from the SRA for local analysis. |
| Kallisto (with translated search) [22] | A tool expanded to perform translated nucleotide-to-amino acid alignment, enabling detection of divergent RNA viruses by targeting conserved RdRP domains. |
| PalmDB [22] | A database of conserved amino acid sequences from the RNA-dependent RNA polymerase (RdRP) used for sensitive identification of RNA viruses beyond reference genomes. |
| VirSorter2 & VIBRANT [18] | Bioinformatic tools that use machine learning and homology searches to identify viral sequences from metagenomic assemblies. |
| BioSample & SRA Metadata Templates [16] [20] | Standardized spreadsheets provided by NCBI to ensure the consistent and complete reporting of sample attributes and sequencing experiment details. |
Experimental Protocols & Workflows
Protocol: Translated Search for RNA Virus Detection in Metagenomic Data
This methodology leverages the highly conserved RNA-dependent RNA polymerase (RdRP) for sensitive virus detection [22].
- Principle: Nucleotide sequencing reads are reverse-translated in all six reading frames and aligned to an amino acid reference database (PalmDB). This method is robust to silent mutations and can detect viruses divergent from those in standard nucleotide reference databases [22].
- Workflow:
- Input: Bulk or single-cell RNA-seq data (FASTQ files).
- Code Execution: The workflow can be executed efficiently on a standard laptop [22].
- Alignment: The six reading frames of the sequencing reads are pseudoaligned to the reverse-translated PalmDB sequences. The best alignment frame is selected for each read [22].
- Output: A list of detected viral sequences with taxonomic assignments.
The following diagram illustrates the core computational process of the translated search.
Protocol: Submitting Data to the Sequence Read Archive (SRA)
A standardized protocol for ensuring your virome data is accessible and FAIR-compliant.
- Prerequisites:
- Submission Steps:
- Login & Initiate: Log in to the SRA Submission Portal and create a new submission to get a temporary
SUB#ID [20]. - General Info: Declare if a BioProject/BioSample already exists to prevent duplicates [16].
- BioSample Attributes: Provide specific and unique metadata for each biological sample. Use the NCBI Taxonomy Browser for accurate organism names [20].
- SRA Metadata: Upload a metadata spreadsheet linking your samples to the data files. Each row defines one sequencing experiment [20].
- File Upload: Pre-upload files to your personal submission folder via FTP/Aspera. Ensure filenames in the metadata match the uploaded files exactly [16] [20].
- Overview & Submit: Review all information and submit. Processing can take over 24 hours [16].
- Login & Initiate: Log in to the SRA Submission Portal and create a new submission to get a temporary
The diagram below outlines the logical sequence of the submission process and its connection to the FAIR principles.
Technical Support Center: Troubleshooting Guides & FAQs
This section addresses common challenges researchers face when working with viral sequence data and implementing FAIR principles, based on documented experiences from the COVID-19 pandemic.
Frequently Asked Questions
Q1: Our clinical data from COVID-19 patients is stored in different hospital systems with different formats. What is the first step to make it FAIR?
A1: The foundational step is to implement a FAIRification process that includes goal definition and project examination [23]. For clinical data, this typically involves:
- Define a clear FAIRification goal: For example, "To make COVID-19 patient cytokine data machine-actionable to enable federated analysis across hospitals." This goal should be specific and avoid simply stating "make data FAIR" [23].
- Conduct a data requirement analysis: Characterize all data types, identifiers, and existing metadata [23].
- Use ontological models: Transform raw, siloed data into machine-actionable digital objects by annotating them with community-developed standards and semantic models, such as those built upon the Observational Medical Outcomes Partnership Common Data Model (OMOP CDM) or core ontological models for common data elements [24] [25]. This creates a virtual warehouse without needing to move data from existing systems.
Q2: We need to share SARS-CoV-2 genomic data quickly, but also ensure contributors get credit. How can FAIR principles help with this?
A2: The GISAID initiative provides a model for this. Its implementation of FAIR principles directly addresses fairness and contributor attribution [5]:
- Findability & Provenance: GISAID assigns a unique, persistent identifier (EPI_ISL ID) to each sequence record, ensuring granular traceability. It also captures rich metadata, including submitting and originating labs [5].
- Reusability: Data are released under a clear access agreement that includes provisions for temporary publishing embargoes, protecting contributors' publication rights while making data available for public health response [5]. This balances rapid sharing with academic credit.
Q3: Our research consortium struggles with semantic interoperability. Different teams use different terms for the same clinical concepts. What is the solution?
A3: This is a common barrier, often categorized as a lack of standardized metadata or ontologies [3]. The solution involves:
- Adopt Controlled Vocabularies: Use community-developed, machine-readable standards like Logical Observation Identifiers Names and Codes (LOINC) for laboratory tests and Systematized Nomenclature of Medicine Clinical Terms (SNOMED-CT) for clinical terms [26].
- Implement a Common Data Model (CDM): Standards like the OMOP CDM ensure both semantic and syntactic interoperability. They allow researchers to write analyses that can be run across multiple, federated databases without sharing raw data directly [25].
- Tooling Support: Use metadata management tools like CEDAR to create templates that enforce the use of controlled vocabularies when capturing metadata [27].
Q4: What are the most critical resource and skill gaps that hinder FAIR implementation in a pandemic?
A4: Systematic identification of barriers shows that the most impactful challenges are often external and related to tooling [25]. The top recommendations to overcome them are:
- Dedicate Expertise: Add a FAIR data steward to the research team. This role possesses the expert knowledge of data, metadata, identifiers, and ontologies that is often lacking [25].
- Provide Accessible Guidance: Create and use accessible step-by-step guides and FAIRification frameworks to provide practical, actionable advice [23] [25].
- Ensure Sustainable Funding: Advocate for proper investments in the implementation and long-term maintenance of FAIR data infrastructure, which is often a high-cost activity [25] [3].
Troubleshooting Common Experimental & Data Workflow Issues
Issue: Inability to integrate genomic data with clinical and imaging data for cross-modal analysis.
- Root Cause: Fragmented data systems and formats; lack of cross-referencing capabilities [28] [3].
- Solution:
- Ensure all datasets are annotated with persistent, globally unique identifiers.
- Implement interoperability technologies like FAIR Data Points (FDPs) to expose metadata in a standardized way [24].
- Use platforms that support cross-referencing, allowing sequences to be linked to external clinical datasets via these identifiers [5].
Issue: Delays in data sharing due to complex and unclear data access procedures and governance.
- Root Cause: Data access regulations are not machine-actionable; governance structures are undefined [28] [25].
- Solution:
- Define and publish a clear Data Usage License or Agreement on the resource website [28].
- Use authentication and authorization protocols that are standardized (e.g., HTTPS) and describe the access procedure clearly in the metadata [5].
- Implement FAIR Data Points that can communicate access restrictions and conditions to machines, enabling automated assessment of data reuse possibilities [24].
Experimental Protocols & Methodologies
This section details specific methodologies cited in the case study for making COVID-19 data FAIR.
Protocol 1: FAIRification of Observational Clinical Data in a Hospital
Objective: To transform siloed, heterogeneous clinical data (e.g., lab measurements, patient observations) into machine-actionable FAIR Digital Objects (FDOs) for secondary use and federated analysis [24].
Workflow Overview:
Detailed Steps:
- Data Acquisition & Initial Storage:
- Collect raw data from source systems (e.g., clinical laboratory information systems, Electronic Health Records - EHRs).
- Transfer data to an Electronic Data Capture (EDC) system like Castor for uniform electronic capture [24].
Data Harmonization:
- Import data from the EDC into a data warehouse system like Opal.
- Perform syntactic transformations and initial annotations using a vocabulary chosen by the user. This makes data syntactically machine-readable and provides researchers a central access point [24].
Semantic Modeling & Interoperability (Key FAIR Step):
- Model Data with Ontologies: Develop or reuse ontological models (e.g., the EJP RD core model for common data elements) to represent data records and metadata. This links the data to a formal, shared knowledge representation [24].
- Map to a Common Data Model: Transform the harmonized data into a community standard like the OMOP CDM. This requires mapping local source terminologies to standard concepts (e.g., LOINC, SNOMED-CT) to achieve semantic interoperability [25].
Metadata Exposure & Findability:
- Deploy a FAIR Data Point (FDP). The FDP is a service that exposes the metadata about the dataset (the "who, what, when, where") in a machine-readable standard [24] [27].
- The FDP metadata must include the persistent identifier of the dataset, access instructions, license information, and the ontologies used.
Access & Reuse:
- The resulting FDOs can now be discovered via the FDP and are prepared for federated querying. Analytical workflows can interact with the FDP and the data it describes to perform "data visiting" without necessarily moving large datasets [24].
Protocol 2: Implementing a Machine-Actionable Data Sharing Platform (GISAID Model)
Objective: To create a data sharing resource for pathogen genomic data that incentivizes rapid sharing by ensuring fairness, transparency, and scientific reproducibility, in alignment with FAIR principles [5].
Workflow Overview:
Detailed Steps:
- Data Submission:
- Submitters (labs) provide genetic sequences and associated metadata using a structured, controlled vocabulary [5].
Curation and Persistent Identification:
- The platform's curation team performs quality checks.
- A globally unique and persistent identifier (EPI_ISL ID) is minted for each sequence and its metadata. This ID enables granular traceability and versioning [5].
Metadata Enrichment:
- The platform automatically annotates sequences with additional context, such as clade and lineage assignments, and nucleotide substitutions.
- Cross-referencing is implemented to link sequences to peer-reviewed studies that use them, enriching provenance [5].
Accessible and Secure Distribution:
- Data are made retrievable via standardized, open protocols (HTTPS) and a web interface.
- User authentication is required, governed by a public access agreement. This balances open access with accountability and ensures transparent use of data [5].
Reuse and Attribution:
- Data are released under a clear license with terms that protect contributors' publication rights (e.g., via temporary embargoes).
- The platform facilitates citation by providing stable identifiers (EPI_ISL ID, DOI) that can be included in data availability statements [5].
Table 1: Distribution and Characteristics of COVID-19 Data-Sharing Resources [28]
| Characteristic | Registries (44 Identified) | Platforms (20 Identified) |
|---|---|---|
| General Focus | Often comorbidity or body-system specific. | Often focus on high-dimensional data (omics, imaging). |
| Typical Data Harmonization | Use shared Case Report Forms (CRFs) for prospective harmonization. | Allow direct upload of diverse datasets; perform retrospective harmonization. |
| FAIR Implementation | Less likely to fully implement FAIR principles compared to omics/platform resources. | More likely to implement FAIR principles, especially for omics data. |
| Geographic Concentration | Concentrated in high-income countries. | Concentrated in high-income countries. |
Table 2: FAIRness Assessment of Shared COVID-19 Research Data [29]
| Assessment Metric | Finding | Context |
|---|---|---|
| Data Sharing Prevalence | Sparse in medical research. | Based on a review of open-access COVID-19-related papers. |
| FAIR Compliance of Shared Data | Often fails to meet FAIR principles. | Shared data often lack required properties like persistent identifiers and machine-readable metadata. |
| Automated FAIR Assessment Feasibility | Challenging for context-specific principles. | Tools struggle to fully assess "Interoperability" and "Reusability," which often require subjective, community-specific evaluation. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools & Platforms for FAIR Viral Research Data
| Tool / Resource | Type | Primary Function in FAIRification |
|---|---|---|
| OMOP CDM [25] | Common Data Model | Provides a standardized schema for observational health data, enabling semantic and syntactic interoperability for analytics. |
| GISAID [5] | Domain-Specific Repository | A trusted platform for sharing pathogen genomic data that implements FAIR principles to incentivize rapid, equitable, and attributable data sharing. |
| FAIR Data Point (FDP) [24] [27] | Metadata Service | A tool to expose and discover metadata about datasets and services, making them findable and defining how they can be accessed and used. |
| CEDAR [27] | Metadata Authoring Tool | Enables the creation of rich, machine-actionable metadata using templates and controlled vocabularies, which is crucial for interoperability. |
| LOINC & SNOMED-CT [26] | Controlled Vocabulary / Ontology | International standard terminologies for identifying health measurements, observations, and documents, essential for semantic interoperability. |
| VODAN-in-a-Box [27] | Implementation Package | A toolset that facilitates the creation of an internet of FAIR data, enabling "data visiting" across distributed sites, such as hospitals. |
Implementing FAIRification Frameworks: Practical Strategies for Viral Data Management
Step-by-Step FAIRification Process for Viral Genomic Data
The FAIRification process transforms existing data to be Findable, Accessible, Interoperable, and Reusable. For viral genomic data, this process is typically divided into three main phases [30].
Table: FAIRification Process Phases
| Phase | Key Steps | Primary Objectives |
|---|---|---|
| Pre-FAIRification | 1. Identify FAIRification Objectives2. Analyse Data3. Analyse Metadata | Define scope, assess current state, and plan the FAIRification project. |
| FAIRification | 4. Define Semantic Model5. Make Data Linkable6. Host FAIR Data | Transform data and metadata into machine-readable, interoperable formats and publish them. |
| Post-FAIRification | 7. Assess FAIR Data | Evaluate outcomes against objectives and ensure sustainability. |
The following diagram illustrates the sequential and iterative nature of this workflow:
Technical Support & Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: How do we initiate the FAIRification process for our SARS-CoV-2 sequencing data? Start by clearly defining your FAIRification objectives in the Pre-FAIRification phase [30]. Determine the primary use cases: is the data for global surveillance (e.g., submission to ENA/GISAID), research (e.g., variant analysis), or both? Focus initially on a critical subset of data elements, such as the consensus sequence and essential metadata (collection date, geographic location) [30] [31]. This scoping makes the initial project manageable.
Q2: What are the most common metadata standardization challenges for viral genomic data? The primary challenge is collecting rich, structured metadata necessary for interoperability and reuse [8]. Incomplete metadata (e.g., missing collection date or host information) is a major hurdle. Use public standards like the INSDC (International Nucleotide Sequence Database Collaboration) pathogen package or GA4GH (Global Alliance for Genomics and Health) standards to define your semantic model [31] [32]. This ensures your data can be integrated with other datasets.
Q3: Our data is sensitive. How can we make it FAIR without compromising privacy or equity? Adopt the FAIR+E (Equitable) principles [31]. This involves establishing data ownership where the data is generated and building trust. Technical and governance solutions include:
- Controlled Access: Using Data Access Committees (DACs) as recommended by the GA4GH framework [32].
- Data Anonymization: Implementing techniques to remove personally identifiable information before sharing [33].
- Brokering Model: Submitting data to a trusted national or institutional data hub that can perform curation and controlled brokering to international repositories on your behalf [31].
Q4: How do we make viral sequence data machine-readable and linkable? Transform your sequence data and metadata into a linkable, machine-readable format like the Resource Description Framework (RDF) [30]. This step enables interoperability by allowing machines to automatically discover and link your data to other resources (e.g., linking a viral sequence to a specific variant in a knowledge base). This is crucial for automated analyses and AI applications [8].
Q5: How do we assess if our FAIRification was successful? In the Post-FAIRification phase, re-assess your data using the same FAIR Maturity Indicators (MI) from the initial analysis [30]. Compare the pre- and post-FAIRification scores. The ultimate test is whether the data can be used for its intended objectives, such as being successfully submitted to a designated repository like the EU Covid-19 Data Portal and integrated into analysis platforms like NextStrain [8] [31].
Common Error Scenarios and Resolutions
Table: Troubleshooting Common FAIRification Issues
| Error Scenario | Potential Cause | Resolution Steps |
|---|---|---|
| Data submission to international repository fails. | Inconsistent metadata format or missing mandatory fields. | 1. Validate metadata against the repository's required schema (e.g., INSDC, ENA checklists).2. Use a metadata validation tool provided by the repository or a data brokering platform [31]. |
| Automated tools cannot process the published data. | Data is not truly machine-readable (e.g., stored in PDFs or non-standard formats). | 1. Convert data to a standard, machine-actionable format like RDF or structured CSV with a published schema [1].2. Ensure persistent identifiers (PIDs) are used for all data elements [33]. |
| Data is published but not discovered by other researchers. | Inadequate metadata for discovery; data not indexed in searchable resources. | 1. Enrich metadata with relevant, standardized keywords and ontologies (e.g., Disease Ontology, NCBI Taxonomy).2. Register the dataset in a public repository and a community-specific registry or search portal [1] [34]. |
| Difficulty integrating your data with other datasets for analysis. | Lack of semantic interoperability; use of local or ad-hoc terminologies. | 1. Map your data to community-accepted ontologies and vocabularies in the semantic modeling step [30] [33].2. Use common data models like those provided by GA4GH for genomic data [32]. |
Experimental Protocols & Methodologies
Protocol: Implementing a Data Brokering Model for National Surveillance
The data brokering model, successfully deployed during the COVID-19 pandemic, provides a standardized method for consolidating, curating, and sharing viral genomic data from multiple producers [31].
1. Objective: To establish a centralized national or regional data hub that collects SARS-CoV-2 sequences and associated metadata from multiple sequencing labs, performs quality control and standardization, and brokers the submission to international repositories.
2. Materials and Reagents Table: Research Reagent Solutions for Data Brokering
| Item | Function / Description | Example Solutions |
|---|---|---|
| Central Data Platform | A secure computational environment for receiving, storing, processing, and curating incoming data. | SIB Swiss Institute of Bioinformatics COVID-19 Data Platform [31], CNT (Spanish National Center for Microbiology) platform [31]. |
| Standardized Metadata Sheet | A template (e.g., a CSV or TSV file) with controlled vocabulary to ensure consistent metadata collection from all data providers. | Template based on INSDC pathogen package or GA4GH metadata standards [32]. |
| Curation & Validation Pipelines | Automated workflows (e.g., Galaxy workflows, Snakemake, Nextflow) to check sequence quality, metadata completeness, and format compliance. | Custom scripts, Galaxy Project SARS-CoV-2 analysis workflows [31], FAIRplus validation tools [33]. |
| Submission Connectors | Software tools or APIs that facilitate the automated or semi-automated submission of curated data to international repositories. | Custom API scripts for ENA/GISAID submission, ELIXIR's Data Submission Service [31]. |
3. Step-by-Step Procedure:
- Step 1: Coordination and Agreement. Engage with data-producing labs (e.g., clinical, public health) to establish a common agreement on the data brokering process, data standards, and sharing policies [31].
- Step 2: Data and Metadata Collection. Labs submit raw or consensus sequences alongside a filled standardized metadata sheet to the central data platform.
- Step 3: Centralized Curation. The data brokering team runs automated pipelines to validate file formats, check sequence quality, and ensure metadata completeness. They may also perform additional analyses (e.g., lineage assignment) [31].
- Step 4: Data Anonymization/Pseudonymization. If required, sensitive information is removed or pseudonymized in accordance with the agreed legal and ethical framework [33] [32].
- Step 5: Brokering to Repositories. The curated and anonymized data is submitted on behalf of the producers to international repositories like the European Nucleotide Archive (ENA) and/or GISAID, as per the data providers' preferences [31].
- Step 6: Feedback and Reporting. The data brokering platform provides feedback and tailored reports (e.g., lineage reports) back to the data-producing labs and public health authorities.
The workflow for this protocol is depicted below:
The Scientist's Toolkit
Table: Essential Resources for Viral Genomic Data FAIRification
| Resource Category | Specific Tool / Standard | Role in FAIRification Process |
|---|---|---|
| FAIRification Frameworks | FAIRplus Framework [33]GO-FAIR 3-Point FAIRification Framework [1] | Provides a structured, step-by-step methodology and templates for planning and executing a FAIRification project. |
| Semantic Standards & Ontologies | NCBI TaxonomyDisease Ontology (DOID)Environment Ontology (ENVO)GA4GH Phenopackets [32] | Provides standardized, machine-readable terms for describing data (e.g., virus strain, host, sampling environment), enabling interoperability. |
| Data & Metadata Models | INSDC Pathogen PackageGA4GH Metadata Standards [32] | Defines the structure and required fields for sequence data and associated metadata, ensuring consistency and completeness. |
| Data Repositories & Platforms | European Nucleotide Archive (ENA)GISAIDEU Covid-19 Data Portal [31] | Provides a FAIR-compliant hosting environment with unique identifiers (PIDs), searchable indexes, and standardized access protocols (APIs). |
| Implementation Guides | The FAIR Cookbook [33]Galaxy Project Workflow FAIRification Tutorial [34] | Offers practical, hands-on "recipes" and tutorials for implementing specific FAIRification steps, such as data transformation and workflow annotation. |
Persistent Identifiers (PIDs) for Viral Sequence Data
FAQs on PIDs
Q1: What is a Persistent Identifier and why is it critical for our viral sequence data? A Persistent Identifier (PID) is a long-lasting reference to a digital resource, consisting of a unique identifier and a service that locates the resource over time, even when its physical location changes [35]. For viral sequence data, PIDs are critical because they:
- Establish Provenance: Help verify that the data is what it purports to be [35].
- Ensure Stable Access: Provide a stable link to your data, overcoming the problem of broken links (link rot) common with standard URLs [35] [36].
- Enable Proper Citation: Allow your data to be uniquely cited in publications, giving you credit for your work [37] [36].
Q2: Which PID scheme should I choose for depositing viral sequences? The choice of scheme depends on your repository and specific needs. The table below summarizes the main schemes:
| PID Scheme | Full Name | Key Characteristics | Common Use in Life Sciences |
|---|---|---|---|
| DOI [35] | Digital Object Identifier | A specific type of Handle; very well-established and widely deployed; has a system infrastructure for reliable resolution. | Journal articles, datasets (via DataCite), making research outputs citable [37] [36]. |
| Handle [35] | Handle | A system for unique and persistent identifiers; forms the technical infrastructure for DOIs. | Underpins the DOI system; used in various digital repository applications. |
| ARK [35] | Archival Resource Key | An identifier scheme emphasizing that persistence is a matter of service, not just syntax. | Often used by libraries and archives for digital objects. |
| PURL [35] | Persistent URL | A URL that permanently redirects to the current location of the web resource. | Providing stable links for web resources that may change locations. |
For viral sequence data submitted to major public repositories like the Sequence Read Archive (SRA) or GenBank, a DOI is often assigned or can be requested, making it the de facto standard for data citation [37].
Q3: I have a PID for my dataset, but the link is broken. What should I do? This is a failure of the resolution service. First, check the PID in your web browser. If it fails:
- Contact the PID Provider: If it's a DOI, contact the registration agency (e.g., DataCite or Crossref) or the repository that issued it (e.g., SRA).
- Verify the Metadata: Log in to the provider's service and ensure the URL in the PID's metadata is correct and up-to-date. Persistence requires ongoing maintenance of this link [35].
Troubleshooting Guide: PID Resolution Failure
- Symptom: Clicking a PID (e.g., a DOI link) returns a "404 Not Found" error.
- Diagnosis: The metadata associated with the PID points to an incorrect or outdated URL.
- Solution:
- Identify the issuing organization (e.g., from the DOI prefix).
- Navigate to the resolver service's website (e.g., doi.org for DOIs).
- Use the resolver's lookup tool to check the registered target URL.
- If you are the data owner, update the target URL via the provider's administrative interface.
- If you are a data user, report the broken link to the repository where the data is hosted.
Metadata Registries and Ontology Services
FAQs on Metadata and Ontologies
Q1: What is the role of metadata in making viral data FAIR? Rich, machine-readable metadata is the cornerstone of Findability, Interoperability, and Reusability (the F, I, and R in FAIR) [1] [38]. For viral sequences, it allows both humans and computers to:
- Find data based on specific attributes (e.g., virus species, host, collection date, geographic location) [1].
- Understand the context and methods of the experiment (provenance) [38].
- Integrate datasets from different sources for combined analysis [1].
Q2: How can ontologies help annotate our viral sequencing metadata? Ontologies are machine-processable descriptions of a domain that use standardized, controlled vocabularies [39]. They solve the problem of inconsistent terminology (e.g., "H1N1," "Influenza A virus H1N1," "Influenza A (H1N1)") by providing unique identifiers for each concept. This enables:
- Interoperability: Different datasets using the same ontology terms can be seamlessly integrated and queried [1] [39].
- Advanced Querying: You can query data based on semantic meaning, finding all data related to "influenza virus" even if the specific strain term isn't in the metadata, by leveraging the ontology's hierarchy.
- Semantic Annotation: Tools like the NCBO Annotator can automatically map your free-text metadata to standardized ontological terms [39].
Q3: We want to set up an internal ontology service. Where do we start? You can deploy an open-source service like the EBI Ontology Lookup Service (OLS) in-house [40]. This provides a single point of access to query, browse, and navigate multiple biomedical ontologies, protecting your data and ensuring fast, stable access.
Experimental Protocol: Deploying a Local Ontology Lookup Service (OLS)
This protocol is based on the public OLS deployment guide [40].
Objective: To deploy a local instance of the EBI OLS to manage and serve ontologies for internal data annotation workflows.
Materials and Software:
- Hardware: A Unix-based (Linux/macOS) or Windows server with sufficient memory and storage.
- Software Dependencies:
- Git (v2.17.1 or higher)
- Docker (v18.09.01 or higher) or Docker Desktop for Windows
- A terminal (PowerShell for Windows)
Methodology:
- Install Dependencies: Ensure Git and Docker are installed and running on your system.
- Clone and Configure OLS:
- Edit the
ols-config.yamlfile to load relevant ontologies (see step 3).
- Edit the
- Load Ontologies: In the
ols-config.yamlfile, add ontology metadata. For example, to load the Data Usage Ontology (DUO):- You can download pre-configured metadata for many public ontologies using a command like:
wget -O ols-config.yaml https://www.ebi.ac.uk/ols/api/ols-config?ids=efo,aero[40].
- You can download pre-configured metadata for many public ontologies using a command like:
- Build and Run the Docker Container:
- Access the Service: Your local OLS will be available at
http://localhost:8080.
Troubleshooting:
- Port Conflict: If port 8080 is busy, use a different port (e.g.,
-p 8081:8080). - Ontology Not Loading: Verify the
ontology_purlin the configuration file is correct and accessible. - Permission Denied: On Unix systems, prefix Docker commands with
sudoif your user is not in the docker group.
Visualizing the Technical Infrastructure Workflow
The following diagram illustrates the logical relationships and workflow between PIDs, metadata, and ontology services in a FAIR-compliant viral data pipeline.
FAIR Data Infrastructure Workflow for Viral Sequences
The Scientist's Toolkit: Essential Research Reagents & Digital Solutions
The following table details key digital "reagents" and services essential for implementing FAIR principles for viral sequence data.
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| DataCite DOI [35] [37] | Provides a persistent, citable identifier for research datasets, including viral sequences. | Globally unique, resolvable via https://doi.org, includes rich metadata schema. |
| EBI Ontology Lookup Service (OLS) [40] [39] | A repository and service for browsing, searching, and visualizing biomedical ontologies. | Open-source, can be deployed locally; provides REST API for programmatic access. |
| NCBO Annotator [39] | A web service that maps free-text metadata to standardized terms from ontologies in BioPortal. | Automates metadata annotation; supports semantic enrichment of data descriptions. |
| BioPortal [39] | A comprehensive repository of biomedical ontologies (over 270). | Provides community features like comments and mappings; foundation for the NCBO Resource Index. |
| FAIR Cookbook [40] | A hands-on resource with "recipes" for implementing FAIR principles. | Provides practical, step-by-step guides for technical implementation. |
| Data Reuse Information (DRI) Tag [37] | A machine-readable metadata tag that indicates the data creator's preference for communication before reuse. | Associated with an ORCID; fosters collaboration and equitable data reuse. |
Troubleshooting Guide: Common DDVD Challenges & Solutions
This guide addresses specific issues researchers might encounter during Data-Driven Virus Discovery experiments.
Issue 1: Low Viral Signal in Public Sequencing Data
Question: My analysis of public sequencing data (e.g., from the SRA) returns very few or no viral sequences. What could be the cause?
Answer: Low viral signal can stem from several sources related to data quality and experimental design of the original datasets you are mining.
- Cause: The source biological samples had low viral load, or the sequencing library preparation method was not suitable for viral nucleic acids.
- Solution: Apply read-level quality control and filtering. Focus on data from samples where viruses are more likely to be present (e.g., tissue from diseased organisms, environmental samples). Use sensitive, alignment-free tools designed for low-abundance sequences.
- FAIR Compliance Note: This highlights the need for rich metadata (Accessibility - A2) to understand sample origin and experimental design, aiding in the selection of appropriate datasets [41] [5].
Issue 2: Challenges in Host Assignment
Question: I have identified a novel viral sequence, but I am unsure how to confidently assign its host organism.
Answer: Host assignment is a common challenge in DDVD. Contamination during sample processing or index hopping can mislead assignments.
- Cause: The viral sequence may be a contaminant rather than a true infection of the sampled host.
- Solution: Implement a confidence framework for host assignment. Guidelines include:
- Detect the viral genome in sequencing experiments from at least two independent laboratories.
- Determine a significant portion of the viral genome for accurate phylogenetic placement.
- Require sufficiently deep read coverage to discriminate actively replicating viruses from contaminants [41].
- FAIR Compliance Note: This underscores the importance of Interoperability (I3), where qualified references to host metadata and phylogenetic context are crucial for accurate biological interpretation [5].
Issue 3: Inability to Detect Highly Divergent Viruses
Question: My similarity-based searches are failing to detect viruses that are highly divergent from known references.
Answer: This is a fundamental limitation of sequence-similarity approaches.
- Cause: Standard BLAST and alignment-based methods rely on significant sequence homology, which may be absent for viruses from deeply branching lineages.
- Solution: Employ a combination of protein-profile searches (e.g., HMMER), gene-agnostic methods (e.g., k-mer frequency analysis), and machine learning approaches that can detect remote homology or viral genomic signatures [41].
- FAIR Compliance Note: Effective discovery of divergent viruses depends on the Reusability (R1) of existing data, which must be curated using community-agreed standards to build comprehensive and accurate profile databases [5].
Issue 4: Different Results from Different Recombinant Detection Tools
Question: When analyzing a potential recombinant viral lineage, I get conflicting results from different computational tools.
Answer: Methods for recombination detection use varying statistical frameworks and have different strengths and weaknesses.
- Cause: Tools may differ in their sensitivity to the number of breakpoints, the length of recombined regions, and the level of sequence divergence between parental lineages.
- Solution: Use a consensus approach. Tools like RecombinHunt, which is data-driven and analyzes mutations against a background of known lineage designations, have shown high concordance with expert manual analysis for SARS-CoV-2 and MPXV. Always corroborate findings with phylogenetic analysis [42].
- FAIR Compliance Note: Reproducible identification of recombinants requires that the data are Findable (F1) and Accessible (A1), with unique identifiers and standardized protocols for retrieval, enabling different methods to be applied consistently [5].
Quantitative Data in Data-Driven Virus Discovery
Table 1: Key Metadata for Confident Viral Sequence Annotation in DDVD
| Metadata Field | Importance for DDVD | FAIR Principle Addressed |
|---|---|---|
| Host Organism | Essential for initial host assignment and understanding ecology. | Interoperability (I2) |
| Collection Date & Location | Critical for temporal and spatial tracking of viruses. | Reusability (R1) |
| Isolate Name | Allows grouping of sequences from the same biological sample. | Findability (F1) |
| Sequencing Technology | Informs on potential errors and data quality assessments. | Reusability (R1) |
| Nucleotide Completeness | Indicates whether the sequence is partial or complete, affecting analyses. | Findability (F2) |
Table 2: Common Tools and Resources for DDVD Workflows
| Tool/Resource Name | Primary Function | Application in DDVD |
|---|---|---|
| NCBI SRA | Public repository of raw sequencing data. | The primary source of data for mining; contained over 10.4 million experiments as of mid-2022 [41]. |
| GISAID | Platform for sharing curated pathogen sequences. | Source of well-annotated viral genomes; exemplifies FAIR implementation with EPI_ISL IDs [5]. |
| RecombinHunt | Data-driven recombinant genome identification. | Identifies recombinant viral genomes (e.g., SARS-CoV-2, MPXV) by analyzing mutation profiles against lineage definitions [42]. |
| NCBI Virus | Integrative portal for searching and analyzing viral sequences. | Provides value-added, curated viral sequence data from GenBank and RefSeq with standardized metadata and filtering [43]. |
Experimental Protocol: A Standard DDVD Workflow
Objective: To computationally discover and preliminarily characterize novel viral sequences from public sequencing archives.
- Hypothesis & Target Definition: Define the scope of your discovery effort (e.g., "discover novel RNA viruses in arthropod genomes").
- Data Acquisition:
- Identify and download relevant datasets from archives like the NCBI Sequence Read Archive (SRA) or the Whole Genome Shotgun (WGS) database based on metadata (host, tissue, etc.) [41].
- FAIR Focus: Ensure data is accessed via standardized, open protocols (Accessibility - A1.1) and that datasets are described with rich metadata (Findability - F2) [5].
- Quality Control & Preprocessing:
- Use tools like FastQC and Trimmomatic to assess read quality and remove adapter sequences and low-quality bases.
- Viral Sequence Identification:
- Method A (Similarity-Based): Map reads to a comprehensive viral database using BLAST or aligners like Bowtie2/BWA. Unmapped reads can be de novo assembled, and contigs are then searched against viral databases.
- Method B (Signature-Based): Use tools that identify viral genomic signatures (e.g., VirFinder, VIRALpro) or perform protein-profile searches (e.g., DRAM-v) to detect divergent viruses.
- Characterization & Validation:
- Host Assignment: Cross-reference the sample's metadata. Use phylogenetic analysis to see if the novel virus clusters with known viruses from a specific host [41].
- Genome Completeness: Assess whether the ends of the viral genome are recovered (e.g., check for partial genes, terminal repeats).
- Recombination Check: Apply tools like RecombinHunt or RDP5 to screen for recombinant sequences, which is crucial for correct evolutionary placement [42].
- Data Submission & Sharing:
- Annotate the new viral sequence with all available metadata and submit it to a public database like GenBank or GISAID.
- FAIR Focus: Upon submission, the sequence receives a unique and persistent identifier (Findability - F1), such as an GenBank accession or GISAID EPI_ISL ID, making it findable for the community [5].
Table 3: Key Research Reagent Solutions for DDVD
| Item Name | Function/Description |
|---|---|
| Public Sequence Archives | Foundational data sources for mining. Includes the Sequence Read Archive (SRA), Whole Genome Shotgun (WGS), and Transcriptome Shotgun Assembly (TSA) databases [41]. |
| Viral Reference Databases | Curated collections of known viral sequences (e.g., NCBI Viral Genomes, GISAID, ICTV taxonomy) used for comparison and classification. |
| High-Performance Computing (HPC) | Essential infrastructure for the highly parallelized computation required to process terabytes of sequencing data efficiently [41]. |
| Controlled Vocabulary & Ontologies | Standardized terms (e.g., for host, tissue) that ensure metadata is consistent, machine-readable, and interoperable across different datasets and tools [5] [43]. |
| Pango Lineage Designations | A dynamic nomenclature system for SARS-CoV-2 that provides a curated list of characteristic mutations, serving as a key input for tools like RecombinHunt [42]. |
Workflow Diagram: The DDVD Process
Recombinant Virus Detection Logic
Integrating FAIR Workflows into Pharmaceutical R&D and Drug Validation Processes
Frequently Asked Questions (FAQs)
Foundational FAIR Concepts
Q1: What are the FAIR principles and why are they critical for viral sequence data in pharmaceutical R&D? The FAIR principles (Findable, Accessible, Interoperable, and Reusable) provide a framework for managing scientific research data to maximize its value and reuse [44]. For viral sequence data, these principles are crucial for accelerating responses to emerging threats, as demonstrated during the COVID-19 pandemic when FAIR-formatted virus data enabled large-scale analysis [44]. Implementing FAIR ensures this critical data can be effectively used in drug discovery and validation processes, supporting advanced analyses like machine learning and artificial intelligence [44] [45].
Q2: Is FAIR data the same as open data? No. FAIR data is not necessarily open data [46]. The FAIR principles focus on making data usable by both humans and machines, even under access restrictions [46]. Sensitive viral sequence data can be FAIR-compliant with well-defined access protocols and rich metadata, even if the dataset itself is restricted to authorized researchers [46].
Q3: What are the primary benefits of implementing FAIR workflows for drug development?
- Accelerated Innovation: Machine-readable, interoperable data enables AI-driven identification of therapeutic targets and biomarker detection [46].
- Enhanced Reproducibility: Clear provenance and standardized annotations allow results to be independently verified, which is essential for regulatory submissions [46].
- Reduced Costs: Eliminating data redundancy and enabling reuse of validated datasets reduces experiment repetition [46].
- Improved Collaboration: Standardized data structures facilitate seamless data exchange across internal teams and with external partners [45].
Implementation & Technical Considerations
Q4: How do I select an appropriate repository for FAIR viral sequence data? A domain repository that supports FAIR principles is ideal. Key selection criteria include [47]:
- Persistent Identifiers: Provides Digital Object Identifiers (DOIs) or similar permanent identifiers for data citation.
- Sustainable Funding: Ensures long-term data preservation and accessibility.
- Transparent Licensing: Clearly defines data reuse terms.
- Community Alignment: Follows domain-specific standards and best practices for viral genomics.
- Certification: Holds certifications like CoreTrustSeal, indicating trustworthy operations.
Tools like the Repository Finder (developed by DataCite) and FAIRsharing.org can help identify suitable repositories [47].
Q5: What are the most common challenges when FAIRifying existing viral sequence data? Organizations often face multiple hurdles [44] [46]:
- Fragmented Legacy Data: Existing data locked in inconsistent formats and siloed systems.
- Non-Standard Metadata: Use of free-text entries and custom labels instead of controlled vocabularies.
- Resource Intensity: Significant upfront investment required for data curation and infrastructure.
- Legal and Ethical Compliance: Navigating data protection regulations (like GDPR) when working with sensitive human data [44].
Q6: What key metadata is essential for making viral sequences reusable? Rich metadata is fundamental to the Reusable principle. For viral sequences, this should encompass [5]:
- Provenance: Detailed information on the origin of the specimen, submitting laboratory, and sequencing methods.
- Host and Context: Data about the host, sample collection date, and geographical location.
- Technical Specifications: Sequencing platform, bioinformatics analysis protocols, and quality metrics.
- Controlled Vocabularies: Use of community-agreed standards for all metadata fields to ensure consistency.
Troubleshooting Guides
Problem 1: Data Cannot Be Found by Colleagues or Automated Systems
Symptoms:
- Datasets cannot be located through internal search systems.
- Unique identifiers for datasets are missing or not persistent.
- Metadata is sparse or uses inconsistent terminology.
Resolution Steps:
- Assign Persistent Identifiers: Ensure each dataset and crucial intermediate data product has a globally unique and persistent identifier, similar to the EPI_ISL ID used by GISAID for viral sequences [5]. This allows granular traceability.
- Enrich with Standardized Metadata: Describe data with rich, machine-readable metadata using controlled vocabularies and ontologies (e.g., EDAM ontology for data analysis) [48]. Avoid free-text descriptions for critical fields.
- Register in Searchable Resources: Register datasets in internal catalogs or public repositories like WorkflowHub or Dockstore, which are indexed by search engines and data registries [5] [48].
Problem 2: Data is Not Interoperable for Cross-Study Analysis
Symptoms:
- Inability to combine viral sequence datasets from different studies or labs.
- Errors when applying analysis workflows to new datasets.
- Significant manual effort required to "map" data before analysis.
Resolution Steps:
- Adopt Standardized Data Formats: Use broadly accepted, machine-readable formats for data and metadata (e.g., FASTA/FASTQ for sequences, CSV/TSV for metadata) [5] [45].
- Implement Controlled Vocabularies: Replace free-text fields with terms from community-agreed ontologies (e.g., BioSharing.org, EDAM) [45] [48]. This ensures semantic consistency.
- Use Formal Language for Knowledge Representation: Structure metadata using formal, accessible languages like JSON-LD, as used in RO-Crate (Research Object Crate), to make data linkable and unambiguous for machines [48].
The following table summarizes the impact of poor interoperability and the solution:
| Symptom | Root Cause | Corrective Action |
|---|---|---|
| Cannot combine datasets from different studies | Inconsistent or missing metadata standards | Implement and enforce use of community-controlled vocabularies and ontologies [46] [45]. |
| Analysis workflows fail on new data | Use of proprietary or inconsistent data formats | Transition to standardized, open file formats (e.g., CSV, FASTA, JSON-LD) [5] [48]. |
| Manual data "wrangling" is required | Data lacks a formal, machine-actionable structure | Adopt a structured metadata specification like RO-Crate to package data and its context [48]. |
Problem 3: Workflows are Not Reproducible
Symptoms:
- Inability to replicate published results using the same data and code.
- Missing or outdated dependencies for analytical workflows.
- Lack of clarity on the specific parameters and environment used.
Resolution Steps:
- Register the Workflow: Publish computational workflows in a dedicated registry like WorkflowHub or Dockstore. These platforms assign unique, persistent identifiers (DOIs) to specific workflow versions, making them citable and findable [48].
- Provide Example Data & Results: Package the workflow with example input data and expected results. This allows users to verify their installation and understand the workflow's function [48]. For sensitive viral data, use synthetic data that mimics the original [48].
- Document Provenance and Environment: Use containerization (e.g., Docker, Singularity) to capture the complete software environment. Clearly document all parameters, software versions, and configuration steps [48].
This table details key resources for implementing FAIR workflows with viral sequence data.
| Resource / Solution | Function in FAIR Workflow | Relevance to Viral Sequence Data |
|---|---|---|
| WorkflowHub [48] | A registry for publishing, discovering, and citing computational workflows. Supports CWL, Nextflow, Snakemake. | Provides a platform to share and gain credit for analysis pipelines used in viral genomics and drug target identification. |
| RO-Crate (Research Object Crate) [48] | A method for packaging workflow source code, data, and metadata into a single, reusable and archivable unit. | Ensures all components of a viral sequence analysis (raw data, tools, parameters, results) are preserved together for full reproducibility. |
| GISAID [5] | A real-world example of a FAIR-aligned platform for sharing pathogen data. Uses unique EPI_ISL IDs and rich metadata. | Serves as a model for how to manage viral sequence data with provenance, access controls, and interoperability. |
| EDAM Ontology [48] | A structured, controlled vocabulary for describing data analysis and management in the life sciences. | Used to richly annotate workflows and their data types, operations, and topics, making them more findable and understandable. |
| Repository Finder Tool [47] | A tool (by DataCite) that uses re3data.org to help researchers find appropriate FAIR-aligned data repositories. | Assists in locating the optimal domain-specific repository for depositing final viral sequence data associated with a publication. |
FAIR Implementation Workflow for Viral Sequence Data
The following diagram outlines a generalized, high-level workflow for making viral sequence data FAIR-compliant within a pharmaceutical R&D setting, incorporating key steps from data generation to reuse.
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What is the key difference in scope between Ph. Eur. 2.6.41 and ICH Q5A(R2) regarding virus spike studies? A1: ICH Q5A(R2) is a broad guideline covering the viral safety of biotechnology products derived from cell lines of human or animal origin. It mandates virus validation studies to demonstrate the capacity of the manufacturing process to clear and/or inactivate viruses. Ph. Eur. 2.6.41 specifically addresses the "Evaluation of the Reduction of Viruses in the Purification Process." It provides more detailed, prescriptive methods for conducting these virus spike studies, including specific calculation methods for reduction factors.
Q2: How do we calculate the overall reduction factor, and what are the acceptance criteria? A2: The overall reduction factor is the sum of the log10 reduction factors (LRF) for individual, orthogonal clearance steps. Each step's LRF is calculated as Log10 (V1 × T1 / V2 × T2), where V1 is the virus load in the starting volume, T1 is the titer of the spiked material, V2 is the volume of the post-step material, and T2 is the titer of the post-step material. Acceptance is not a fixed number but must be sufficient to ensure patient safety, typically demonstrated by a cumulative LRF that exceeds the potential virus load in the source material.
Table 1: Typical Log10 Reduction Factor (LRF) Expectations for Common Purification Steps
| Purification Step | Mechanism of Action | Typical LRF Range | Key Variables Affecting Performance |
|---|---|---|---|
| Low pH Incubation | Viral inactivation | ≥ 4.0 log10 | pH, hold time, temperature, protein concentration |
| Solvent/Detergent | Viral inactivation | ≥ 4.0 log10 | Solvent/detergent type, concentration, time |
| Virus Filtration | Viral removal (size exclusion) | ≥ 4.0 log10 | Filter pore size, product load, fouling |
| Chromatography (AEX) | Viral removal (binding) | 1.0 - 5.0 log10 | Conductivity, pH, resin type, flow rate |
| Chromatography (CEX) | Viral removal (flow-through) | 1.0 - 3.0 log10 | Conductivity, pH, resin capacity |
Q3: Our viral clearance study failed to achieve the target LRF for a chromatography step. What are the primary troubleshooting steps? A3:
- Review Buffer Conditions: Re-evaluate the pH, conductivity, and composition of your equilibration, load, and elution buffers. Small deviations can significantly impact viral binding or flow-through.
- Assess Product Load: High product loading can saturate binding sites, reducing the step's capacity to bind viruses. Perform a study to determine the optimal load density.
- Investigate Flow Dynamics: Ensure consistent flow rates and proper packing of the chromatography column. Channeling or uneven flow can lead to virus breakthrough.
- Re-examine Scale-Down Model: Verify that your small-scale model accurately represents the manufacturing-scale process in all critical parameters (resin lot, contact time, buffer composition).
Q4: How do FAIR Data Principles apply to viral sequence data generated for regulatory submissions? A4: Applying FAIR (Findable, Accessible, Interoperable, Reusable) principles to viral sequence data (e.g., from Next-Generation Sequencing for virus identification) ensures its long-term regulatory value and scientific utility.
- Findable: Data must be assigned a persistent identifier (e.g., DOI) and rich metadata describing the cell line, sequencing method, and analysis pipeline.
- Accessible: Data should be stored in a trusted repository (e.g., NCBI's SRA) with clear access protocols, even if under embargo.
- Interoperable: Data should use standardized formats (e.g., FASTQ, SAM/BAM) and controlled vocabularies (e.g., EDAM Bioimaging, OBI) to allow integration with other datasets.
- Reusable: Data must be thoroughly described with provenance, clear licensing, and meet community standards to enable future re-analysis or regulatory assessments.
Experimental Protocols
Protocol 1: Determination of Log10 Reduction Factor (LRF) for a Virus Inactivation Step (e.g., Low pH)
Objective: To quantify the reduction in viral titer achieved by a low pH hold step.
Materials:
- Product intermediate
- Model virus (e.g., MuLV or X-MuLV)
- Pre-defined inactivation buffer (e.g., citrate, glycine)
- Neutralization buffer
- Cell-based infectivity assay (e.g., TCID50 assay)
Methodology:
- Spike and Inactivate:
- Spike the product intermediate with a high-titer stock of the model virus (e.g., 1:10 to 1:100 v/v ratio).
- Immediately withdraw a pre-inactivation sample (T=0).
- Adjust the spiked material to the target pH (e.g., pH 3.5-3.9) using the inactivation buffer.
- Hold the mixture at the target temperature (e.g., 22-25°C) for the specified time (e.g., 60 minutes).
- Withdraw samples at pre-defined time points (e.g., T=1, 5, 15, 60 minutes).
- Neutralize: Immediately neutralize each time-point sample to a pH compatible with the infectivity assay.
- Titer Determination:
- Perform a serial dilution of each neutralized sample.
- Inoculate the dilutions onto susceptible indicator cells.
- Incubate and monitor for cytopathic effect (CPE).
- Calculate the viral titer for each sample using the Spearman-Kärber or Reed-Muench method.
- Calculation:
- LRF = Log10 (Titer at T=0 / Titer at final time point, e.g., T=60min).
Protocol 2: Next-Generation Sequencing (NGS) for Adventitious Virus Detection
Objective: To identify unknown viral contaminants in a cell culture harvest using a broad-spectrum NGS approach.
Materials:
- Cell culture supernatant or lysate
- Nuclease treatment mix
- Nucleic acid extraction kit (DNA & RNA)
- Reverse transcription and random amplification kit
- NGS library preparation kit
- High-throughput sequencer (e.g., Illumina, MGI)
- Bioinformatics pipeline for viral detection
Methodology:
- Sample Pre-treatment: Treat the sample with nucleases to digest free nucleic acids not protected within a viral capsid.
- Nucleic Acid Extraction: Extract total nucleic acids (DNA and RNA) from the nuclease-treated sample.
- Amplification: Convert RNA to cDNA and amplify both DNA and cDNA using random amplification methods (e.g., SISPA) to ensure unbiased genome representation.
- Library Preparation & Sequencing: Prepare an NGS library from the amplified product and sequence on an appropriate platform to achieve sufficient depth (e.g., >10 million reads).
- Bioinformatic Analysis:
- Quality Control: Trim adapters and filter low-quality reads.
- Host Depletion: Map reads to the host genome (e.g., CHO, HEK293) and remove aligned sequences.
- Viral Identification: Align non-host reads to a comprehensive viral genome database (e.g., NCBI RefSeq Viruses) using tools like BLAST or k-mer based classifiers.
Mandatory Visualizations
Viral Clearance Process Flow
NGS Data for FAIR Compliance
The Scientist's Toolkit
Table 2: Essential Research Reagents for Viral Safety Studies
| Reagent / Material | Function in Viral Safety Evaluation |
|---|---|
| Model Viruses (e.g., X-MuLV, PRV, MVM, Reo-3) | Representative viruses used in spike studies to model potential contaminants and demonstrate clearance capacity. |
| Percellently and Other Bioreactor Materials | Surfaces used in manufacturing; tested for their ability to inactivate viruses upon contact. |
| Virus-Specific Antibodies | Used in immunostaining for TCID50 assays or for neutralizing residual virus in samples. |
| Cell Lines for Infectivity Assays (e.g., Vero, A9, MRC-5) | Indicator cells used to propagate model viruses and quantify infectious titer via CPE or other methods. |
| Nuclease Enzymes (e.g., Benzonase) | Used in NGS sample prep to digest unprotected nucleic acid, enriching for viral sequences within capsids. |
| Total Nucleic Acid Extraction Kits | To simultaneously isolate both DNA and RNA for comprehensive viral detection via NGS. |
| Random Amplification Kits | For unbiased whole-genome amplification of viral nucleic acids prior to NGS library prep. |
| Bioinformatic Viral Databases (e.g., NCBI Virus) | Curated reference databases essential for identifying viral sequences from NGS data. |
Overcoming FAIRification Challenges: Error Management and Strategic Optimization
For researchers working with viral sequence data, achieving compliance with the FAIR (Findable, Accessible, Interoperable, and Reusable) principles is crucial for accelerating pathogen research and pandemic response. However, the FAIRification process—converting existing data into a FAIR-compliant format—presents significant hurdles across financial, technical, legal, and organizational domains. This guide provides troubleshooting advice and methodologies to help scientists, researchers, and drug development professionals navigate these barriers, with a specific focus on the context of viral genomic data.
Troubleshooting Common FAIRification Hurdles
Financial Hurdles
Financial challenges are often the first and most significant barrier, involving costs related to establishing data infrastructure, employing personnel, and ensuring long-term sustainability [44].
- Challenge: High initial investment and unclear return on investment (ROI).
- Troubleshooting: Start with a focused, high-impact project. Instead of attempting to FAIRify all legacy viral sequence data at once, select a specific dataset (e.g., sequences from a particular outbreak) for a pilot project. Demonstrate value by showing how this FAIR data can be reused to accelerate a specific research goal, such as identifying transmission patterns or tracking mutations [44].
- Challenge: Ongoing curation costs and ensuring business continuity.
- Troubleshooting: Develop a long-term data strategy and budget that is integrated into research grant proposals. Funding agencies increasingly expect a commitment to FAIR and open data; therefore, including these costs in funding requests is increasingly viable [44].
Table 1: Financial Hurdles and Required Expertise
| Challenge | Required Expertise |
|---|---|
| Establishing and maintaining physical data structure | IT professionals, Data stewards |
| Data curation costs | Data curators, Domain experts |
| Ensuring business continuity and long-term data strategy | Business lead, Strategy lead |
Technical Hurdles
Technical barriers include the lack of standardized tools and fragmented legacy infrastructure, which can lock data into inaccessible formats [46] [44].
- Challenge: Fragmented legacy systems and inconsistent metadata.
- Troubleshooting: Implement a centralized data platform or integration layer to harmonize data from different sources, such as various sequencing machines or legacy databases. For metadata, adopt community-standard ontologies for viral sequences (e.g., from the INSDC partners: GenBank, ENA, DDBJ) to ensure consistency and machine-actionability [46].
- Challenge: Lack of scalable, automated FAIRification tools.
- Troubleshooting: Utilize open-source toolkits designed for genomic data. For instance, the Nextstrain toolkit provides bioinformatic workflows and visualization apps for phylogenetic analysis of pathogen genomes, which inherently relies on and promotes FAIR data practices [49].
Legal and Ethical Hurdles
Legal challenges are paramount when dealing with viral sequence data that may be linked to patient or geographic information, requiring strict adherence to data protection regulations [44].
- Challenge: Navigating data privacy regulations (e.g., GDPR) while making data accessible.
- Troubleshooting: Conduct a Data Protection Impact Assessment (DPIA) early in the project planning stage. For sensitive data, implement robust security measures like authentication procedures, data encryption, and detailed access logs. Remember, "FAIR" does not necessarily mean "Open"; access can be controlled and provided only to authorized researchers [44].
- Challenge: Managing data ownership and usage licenses.
- Troubleshooting: Clearly document data provenance and define usage rights with standardized licenses. When sharing data via public repositories, use licenses that maximize reuse potential while respecting ethical constraints, such as those recommended by the UNESCO Recommendation on Open Science [50].
Organizational Hurdles
Organizational barriers include a lack of training, unclear data ownership, and the absence of a culture that rewards data stewardship [44].
- Challenge: Lack of a FAIR-minded organizational culture and insufficient training.
- Troubleshooting: Appoint "data champions" within research teams—individuals with both domain expertise (virology, genomics) and data management skills. These champions can advocate for FAIR practices, provide peer training, and bridge the communication gap between researchers and IT professionals [44].
- Challenge: Unclear data governance and ownership.
- Troubleshooting: Establish a clear data governance framework. Define roles and responsibilities, including data owners, stewards, and lifecycle managers. Implement enterprise-wide data stewardship policies that are aligned with broader research and regulatory goals [46].
Frequently Asked Questions (FAQs)
Q1: Our viral sequence data is sensitive. Can it be both FAIR and secure? Yes. The "Accessible" in FAIR means that data should be retrievable by both humans and machines using a standardized protocol, but this can include authentication and authorization. You can have a fully FAIR dataset that is only accessible to researchers who meet specific ethical and data use criteria [46].
Q2: What is the single biggest technical obstacle to making viral sequence data interoperable? The most common obstacle is the lack of standardized metadata and vocabulary misalignment. If one lab describes a host as "human" and another uses "Homo sapiens," or if geographic location is entered in free text, computational tools cannot reliably combine these datasets. The solution is to use controlled vocabularies and ontologies from the start of a project [46] [51].
Q3: How can we justify the high initial cost of FAIRification to our institution's leadership? Frame the ROI in terms of accelerated research and cost avoidance. FAIR data eliminates the need to repeatedly "re-discover" or re-generate existing data. It is also a prerequisite for leveraging advanced analytics, such as AI and machine learning, to identify patterns across vast datasets that would be impossible to analyze manually—a critical capability in tracking fast-evolving viruses [46] [44].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Resources for Viral Sequence Data FAIRification
| Item | Function/Benefit |
|---|---|
| Nextstrain Toolkit | An open-source platform for real-time tracking of pathogen evolution. It provides bioinformatic workflows and visualization apps (like Auspice) that are foundational for working with FAIR viral sequence data [49]. |
| Standardized Ontologies (e.g., INSDC terms, EDAM) | Controlled vocabularies ensure that metadata is consistent and interoperable. Using terms from established resources is critical for making sequence data findable and reusable by others [46]. |
| Data Management Plan (DMP) Tool | A tool to create a comprehensive DMP, which is now required by many funders. A good DMP outlines how data will be made FAIR throughout and after a project [44]. |
| Centralized Data Platform | A platform, such as a consolidated Laboratory Information Management System (LIMS), helps harmonize data from disparate instruments and legacy systems, making it findable and accessible from a single source [46]. |
| Persistent Identifiers (PIDs) like DOIs | Assigning a unique, persistent identifier to your dataset is a core requirement for findability. It ensures the dataset can be permanently cited and linked, even if its web URL changes [46]. |
Experimental Protocol: A Methodology for FAIRifying Viral Sequence Data
The following protocol, adapted from best practices in life sciences and public health projects like Nextstrain, provides a detailed methodology for making viral sequence data FAIR-compliant [49] [44].
Objective: To retrospectively process a collection of viral genome sequences and associated metadata into a FAIR-compliant dataset suitable for shared phylogenetic analysis.
Pre-FAIRification Assessment:
- Data Selection: Prioritize datasets with high reuse potential (e.g., from an ongoing outbreak) and where principal investigator buy-in is strong [44].
- Ethical & Legal Check: Perform a DPIA. Confirm that data sharing is permitted and determine the appropriate access level (open, controlled, restricted). Anonymize any directly identifying personal data linked to sequences [44].
- Resource Evaluation: Ensure the availability of personnel with the required expertise (see Table 1), including a bioinformatician and a domain expert (virologist/epidemiologist).
FAIRification Workflow:
Step-by-Step Procedure:
- Assign Persistent Identifiers: Obtain a Digital Object Identifier (DOI) or similar persistent identifier for the entire dataset. This makes the data Findable.
- Standardize Metadata: Map all metadata fields to a standard schema. For viral sequences, this includes fields like
isolation_host,collection_date, andgeo_loc_countryusing terms from recognized ontologies. This is critical for Interoperability. - Define Access Protocols and License: Choose a trusted repository (e.g., INSDC, GISAID) and upload the data. Clearly state the license (e.g., CC0, CC-BY) under which the data can be Reused. If data is sensitive, configure access controls.
- Document Provenance and Methodology: In a README file, describe how the data was generated (sequencing platform, assembly protocol), who generated it, and any processing steps applied. This documentation is essential for Reusability.
- Deposit in a Trusted Repository: Finalize the deposition in the chosen public repository. The repository will ensure the data remains Accessible over the long term.
Validation: To validate success, attempt to access and use the dataset via its PID from a different computer. A colleague unfamiliar with the project should be able to understand and reuse the data based on the provided metadata and documentation alone.
A technical support guide for ensuring FAIR data compliance in virology research
Frequently Asked Questions
What are the most common types of errors found in virus databases? Virus sequence databases are vital resources, but they are prone to several common error types that can impact downstream analysis. The most prevalent issues include:
- Taxonomic Errors: Misannotation, where a sequence is assigned to the wrong virus species, is a pervasive problem. It is estimated to affect approximately 3.6% of prokaryotic genomes in GenBank and about 1% in its curated RefSeq subset [52]. This often stems from data entry mistakes or incorrect identification by the submitter.
- Sequence Contamination: This is one of the most recognized database issues. Systematic evaluations have identified over 2 million contaminated sequences in GenBank and over 100,000 in RefSeq [52].
- Incomplete or Inaccurate Metadata: Missing or incorrect metadata, such as the host, collection date, or geographic location, severely limits data reusability. This includes "unspecific taxonomic labelling," where a sequence is accurately assigned to a high-level taxon (e.g., a genus) but not to the most specific leaf (e.g., species or strain) [52] [53].
- Sequence Content Errors: These include issues like incorrect sequence orientation and chimeric sequences, which can lead to false interpretations during sequence alignment and analysis [54].
How can a misannotated sequence in a database affect my research on viral pathogenesis? Taxonomic misannotation can have significant downstream consequences. It can lead to:
- False Positive Detections: Incorrectly identifying the presence of a pathogen in a sample.
- False Negative Detections: Failing to detect a pathogen that is present.
- Imprecise Classifications: Hindering the ability to track the spread and evolution of specific viral strains, which is crucial for understanding pathogenesis and developing targeted treatments [52]. Relying on misannotated data can compromise the validity of transmission maps and evolutionary studies [55].
I need to submit my viral sequences to a repository. What can I do to prevent these errors? Preventing errors at the point of submission is the most effective strategy. When preparing your data, ensure you have the following information ready, as required by major repositories like NCBI GenBank [56]:
- Complete Source Metadata: This includes the scientific name of the virus, precise geographic location, host information, collection date (DD-Mon-YYYY), isolate/strain designation, and sample isolation source (e.g., nasal swab).
- Accurate Annotation: For most viruses, you will need to provide annotation of genes and coding regions. Tools like BankIt or tbl2asn can assist with this.
- Use of Controlled Vocabularies: Whenever possible, use standard naming conventions and ontologies (e.g., from the NCBI Taxonomy Browser) to describe your data. This enhances interoperability and reduces ambiguity [55].
What should I do if I discover a potential error in a public virus database? The process for correcting errors depends on the database. For NCBI databases, GenBank records are owned by the data submitter and cannot be directly modified by NCBI. The NCBI team flags suspicious submissions for review, but the correction process often involves contacting the original submitter [52]. Reporting the error to the database maintainers is a critical step to initiate a review. For databases with a stronger curation model, such as GISAID, errors can be addressed through their dedicated curation processes, which include versioning to reflect updates [5].
Troubleshooting Guides
Guide 1: Identifying and Mitigating Taxonomic Labelling Errors
Objective: To provide a methodology for detecting and correcting inaccurate or unspecific taxonomic labels in viral sequence data.
Background: Taxonomic errors can arise from submission mistakes or limitations in identification techniques. This protocol leverages sequence comparison and gold-standard references to identify anomalies [52].
Table: Common Taxonomic Errors and Mitigations
| Error Type | Description | Potential Impact | Mitigation Strategy |
|---|---|---|---|
| Misannotation | Sequence is assigned to an incorrect species. | False positive/negative detections; skewed evolutionary models. | Compare against type material or a gold-standard database using Average Nucleotide Identity (ANI) [52]. |
| Unspecific Labelling | Sequence is annotated to a high-level taxon (e.g., genus) but not to the species or strain level. | Limits utility for strain-level tracking and precise diagnostics. | Annotate to the deepest node possible; use tools that leverage homology and coverage for finer classification [52]. |
| Legacy Exception | Related but distinct species (e.g., E. coli and Shigella) are grouped due to historical classification. | Misidentification of clinically relevant pathogens. | Be aware of these exceptions and use specialized databases or assays that differentiate them [52]. |
Experimental Protocol: Using ANI for Taxonomic Validation
- Compile a Gold-Standard Set: Gather reference sequences from a trusted, curated source. The ICTV Virus Metadata Resource (VMR) is an excellent starting point, as it provides exemplar viruses for each species [57]. The FDA-ARGOS project also provides verified genomes [52].
- Calculate Average Nucleotide Identity: For your query sequence and the gold-standard references, compute the ANI using tools such as FastANI or PYANI.
- Identify Outliers: Species typically have an ANI demarcation of 95–96%. Sequences falling significantly below this threshold when compared to their assigned species group should be flagged for further review [52].
- Manual Curation: Investigate flagged sequences. Check the original publication (if available) and associated metadata. The sequence may require reclassification or, in severe cases, exclusion from your analytical dataset.
The following diagram illustrates the logical workflow for identifying and mitigating taxonomic errors.
Guide 2: Managing Sequencing Errors and Ambiguities in Downstream Analysis
Objective: To evaluate and apply robust strategies for handling base call ambiguities in next-generation sequencing (NGS) data used for viral analysis.
Background: Sequencing technologies have inherent error rates, resulting in ambiguous base calls (e.g., denoted as 'N'). The chosen strategy for handling these ambiguities can significantly impact diagnostic and prognostic predictions, such as HIV-1 co-receptor tropism determination [58].
Table: Comparison of Error Handling Strategies for NGS Data
| Strategy | Method | Pros | Cons | Best For |
|---|---|---|---|---|
| Neglection | Remove all sequences containing ambiguous bases from the analysis. | Simple; performs well with random, low-frequency errors [58]. | Can introduce bias if errors are systematic; loses data. | Data with very low and random error rates (e.g., Illumina MiSeq) [58]. |
| Worst-Case Assumption | Assume the ambiguity resolves to the nucleotide with the most negative clinical implication (e.g., drug resistance). | Ensures a conservative, safety-first approach. | Can be overly pessimistic, leading to incorrect therapy exclusion; performed worst in comparative studies [58]. | Not generally recommended as a primary strategy. |
| Deconvolution with Majority Vote | Generate all possible sequences from the ambiguities, run analysis on all, and take the consensus result. | Maximizes data usage; robust against systematic errors. | Computationally expensive with multiple ambiguities (complexity: 4^k) [58]. | Data with a high fraction of ambiguous reads or suspected systematic errors [58]. |
Experimental Protocol: Selecting an Error Handling Strategy
- Profile Your Data: Calculate the percentage of reads in your dataset that contain one or more ambiguous bases.
- Assess Error Distribution: Determine if the ambiguities are randomly distributed or clustered in specific genomic regions (e.g., homopolymer tracts). Position-specific errors can indicate systematic issues [58].
- Choose and Apply a Strategy:
- For datasets with <1% ambiguities that are randomly distributed, the Neglection strategy is often optimal.
- For datasets with >1% ambiguities or evidence of systematic errors, use Deconvolution with Majority Vote. For computational feasibility, you may need to set a limit on the number of ambiguous positions (k) per read that will be deconvoluted.
- Validate and Report: Compare the outcomes of different strategies if possible. Always clearly report which error handling strategy was used in your methods section to ensure reproducibility.
Guide 3: Ensuring Metadata Integrity for FAIR Compliance
Objective: To establish a checklist for creating and validating viral sequence metadata to ensure it is Findable, Accessible, Interoperable, and Reusable (FAIR).
Background: Metadata integrity is a fundamental determinant of research credibility. Incomplete or incorrect metadata renders data unusable for reuse and integration, breaking the FAIR data cycle [55] [53].
Experimental Protocol: A Metadata Quality Control Workflow
- Use a Predefined Checklist: Before submission, validate your metadata against a required checklist. For example, NCBI virus submissions require [56]:
- Virus scientific name
- Geographic location (e.g., USA: Bethesda, MD)
- Host (e.g., Homo sapiens)
- Collection date (DD-Mon-YYYY)
- Isolate source (e.g., nasal swab)
- Isolate/strain name
- Adopt Controlled Vocabularies and Ontologies: Instead of free text, use standardized terms from community resources. This is critical for Interoperability [5] [55].
- NCBI Taxonomy Browser: For virus and host names.
- Ontology Lookup Service (OLS): For terms related to diseases (e.g., IDO, DOID), experimental factors (EFO), and sample types [55].
- Ensure Provenance is Transparent: Document the who, where, when, and how of data generation. Key provenance fields include the originating lab, collecting institution, sample processing methods, and ethical compliance [55].
- Automate Checks: For large-scale projects, manual checks are insufficient [53]. Implement automated scripts or use available software tools to validate metadata against the required schema and vocabulary before submission.
The Scientist's Toolkit
Table: Essential Resources for Viral Database Curation and FAIR Compliance
| Resource Name | Function | Relevance to Error Management |
|---|---|---|
| NCBI Taxonomy Browser | Provides the standard taxonomic nomenclature for naming viruses and hosts. | Mitigates taxonomic misannotation by providing a single source of truth for organism names [56] [55]. |
| ICTV VMR (Virus Metadata Resource) | A downloadable spreadsheet of exemplar viruses for each species. | Serves as a gold-standard reference for validating virus sequence taxonomy and nomenclature [57]. |
| BankIt / tbl2asn | NCBI's web-based and command-line submission tools for viral genomes. | Guides submitters through a structured process, ensuring required metadata is provided to minimize submission errors [56]. |
| Ontology Lookup Service (OLS) | A central repository for searching and exploring biomedical ontologies. | Enables the use of controlled vocabularies, ensuring metadata is interoperable and machine-actionable [55]. |
| FastANI | A tool for fast alignment-free computation of whole-genome Average Nucleotide Identity. | Used to detect taxonomic misannotation by comparing genome sequences against reference sets [52]. |
FAQs: Core Legal Frameworks and Data Sharing
1. What is the fundamental difference between HIPAA and GDPR in the context of viral research?
The most apparent difference is their scope and application. HIPAA is a U.S. law that applies specifically to "covered entities" (healthcare providers, health plans, clearinghouses) and their "business associates" handling Protected Health Information (PHI) [59]. GDPR, in contrast, is a broader European regulation that applies to any organization worldwide that processes the personal data of individuals in the EU, regardless of its location or industry [59] [60]. In viral research, HIPAA may govern patient data from U.S. clinics, while GDPR applies if the research involves data from any EU-based individual.
2. How do consent requirements differ under HIPAA and GDPR for using patient data in research?
This is a key area of divergence, as shown in the table below [59] [60].
| Feature | HIPAA | GDPR |
|---|---|---|
| Consent for Care | Permits some PHI disclosure without patient consent for treatment, payment, and healthcare operations [59]. | Requires explicit consent for the processing of personal health data, which is classified as a special category [60]. |
| Legal Basis for Processing | Relies on permissions for specific activities within the healthcare system [59]. | Consent must be freely given, specific, informed, and unambiguous. Other legal bases for processing may also apply under Article 9 [60]. |
3. A research colleague in the EU has offered to share viral sequence data with our US-based lab. The data includes some patient demographic information. What are our key compliance considerations?
This scenario triggers several key questions to ensure compliance:
- Is the data sufficiently anonymized? Both HIPAA and GDPR have standards for de-identification. Under GDPR, even demographic information can be personal data. You must assess if the data can be linked back to an identifiable person.
- What is the legal basis for transfer? The transfer of personal data from the EU to the US requires a valid legal mechanism under GDPR, such as an adequacy decision or appropriate safeguards like Standard Contractual Clauses (SCCs).
- What does the informed consent say? Review the original consent forms from the data subjects (the patients). The planned research use must be compatible with the purposes for which consent was originally given.
- Are you a joint controller? Determine if your lab and the EU lab are independent data controllers or joint controllers under GDPR, as this defines your respective responsibilities.
4. A patient involved in our long-term viral study has asked for their data to be deleted, exercising their "right to be forgotten." How should we handle this?
Your response depends on the governing regulation[s citation:1]:
- Under GDPR, the individual generally has the right to erasure. Unless a specific legal exception applies (e.g., for compliance with a legal obligation or for reasons of public interest in the area of public health), you must delete the personal data upon request.
- Under HIPAA, the right to be forgotten does not exist. Patients have a right to an accounting of disclosures, but covered entities are generally required to maintain medical records and other PHI for a period defined by law (often six years). You cannot alter or delete these records upon patient request.
If your research is subject to GDPR, you must comply with the erasure request unless an exemption is valid. You should document the request and the legal basis for your decision, whether you comply or deny it.
5. We've experienced a small breach involving the potential exposure of pseudonymized viral sequence data linked to a clinical dataset. What are our notification obligations?
The breach notification rules have critical differences in timing and scope [59] [60]:
| Aspect | HIPAA | GDPR |
|---|---|---|
| Reporting Deadline | Notifications must be sent within 60 days of discovery if the breach affects 500 or more individuals [59]. | The supervisory authority must be notified within 72 hours of becoming aware of the breach [59] [60]. |
| Scope of Application | Applies specifically to breaches of unsecured Protected Health Information (PHI) [59]. | Applies to all personal data breaches, which includes pseudonymized data that can be re-identified [59]. |
Troubleshooting Guides: Common Compliance Challenges
Challenge: Combining viral sequence data from clinical labs, research databases, and public knowledge bases for federated analysis. Data is often in different formats with underspecified semantics, creating non-interoperable "silos" [24].
Diagnosis: Your data infrastructure lacks a unified ontological model to make data machine-actionable, hindering Findability and Interoperability.
Solution: Implement a FAIRification workflow using Semantic Web technologies [24].
Experimental Protocol: FAIRification of Observational Patient Data
- Assessment: Evaluate the FAIR status of existing data in hospital or lab systems. Often, data is structured but not in a globally machine-readable way [24].
- Modeling: Develop or reuse existing ontological models (e.g., from the European Joint Programme on Rare Diseases for common data elements) to represent data and metadata [24].
- Annotation: Map dataset variables to terms in public, formal ontologies. This provides the standardized vocabulary needed for Interoperability.
- Deployment: Use a FAIR Data Point (FDP) to expose the structured metadata. The FDP makes datasets findable and provides access instructions, acting as a gateway for machines [24].
- Federated Querying: With data described by ontologies and accessible via FDPs, you can use applications to perform federated queries across your local data and other FAIR data sources worldwide [24].
Problem 2: Determining the Correct Legal Basis for Processing Data
Challenge: A researcher is unsure when to rely on consent versus other lawful bases for processing personal data under GDPR for a public health research project.
Diagnosis: Misunderstanding that consent is the only, or always the preferred, legal basis for processing. This can lead to non-compliance if consent is not properly managed or if a more appropriate basis exists.
Solution: Follow a structured decision flowchart to identify the correct legal basis. For scientific research, public interest or legitimate interests may be more appropriate than consent, especially if the research requires long-term data retention or if seeking consent is impracticable.
Experimental Protocol: Legal Basis Selection Workflow
- Define Purpose: Clearly articulate the purpose of the data processing for the viral research project.
- Check for Consent: Is the data subject's consent already obtained, and is it specific, informed, and unambiguous for this purpose? If yes, and it is feasible to allow withdrawal, consent may be suitable.
- Evaluate Alternatives: If consent is not appropriate or hard to maintain, assess other bases:
- Public Interest: Does the processing perform a task in the public interest or in the exercise of official authority? This is highly relevant for public health research [24].
- Legitimate Interests: Does the processing for research outweigh the data subject's fundamental rights and freedoms? A balancing test is required.
- Document Rationale: Thoroughly document the chosen legal basis and the justification for it in your research data management plan.
Problem 3: Managing the "Right to be Forgotten" vs. Data Integrity for Research
Challenge: Reconciling a data subject's GDPR right to erasure with the need to maintain data integrity and reproducibility for longitudinal viral studies.
Diagnosis: A direct conflict exists between an individual's rights and scientific record-keeping requirements.
Solution: Implement a technical and procedural segmentation of data.
Experimental Protocol: Data Segmentation for Erasure Requests
- Data Classification: At the data collection stage, clearly separate and tag:
- Core Identifiers: Data that directly identifies a person (e.g., name, address, full phone number).
- Pseudonymized Research Data: The key research data (e.g., viral sequences, lab values) linked to a persistent, internal study ID.
- Secure Linking: Maintain a secure "linking table" that maps the core identifiers to the internal study ID. Access to this table must be highly restricted.
- Upon Erasure Request:
- Delete Core Identifiers: Permanently remove the individual's core identifiers from the linking table. This severs the link between the person and the research data, effectively fulfilling the erasure request from a functional perspective.
- Retain Research Data: The pseudonymized research data can be retained for scientific integrity, as it is no longer considered "personal data" under GDPR after the link is broken, provided the risk of re-identification is negligible.
| Tool / Resource | Function in Compliance & FAIRification |
|---|---|
| FAIR Data Point (FDP) [24] | A middleware application that acts as a metadata catalog. It exposes the metadata of your datasets in a standardized, machine-readable way, making them Findable and explaining how they can be Accessed. |
| F-UJI Automated FAIR Assessment Tool [61] [62] | An open-source tool that programmatically assesses the FAIRness of a research dataset using its persistent identifier (like a DOI). It provides a score for each metric, helping you evaluate and improve your data practices. |
| Ontologies (e.g., EDAM, OBI, SNOMED CT) [24] | Formal, machine-readable representations of knowledge in a specific domain. Using ontologies to annotate your data is the primary technical method for achieving Interoperability, ensuring that your data's meaning is clear to both humans and machines. |
| FAIR-Aware Tool [61] | A guided tool that helps researchers self-assess their knowledge of the FAIR principles before they upload data to a repository. It raises awareness and prepares researchers for the practical steps of making data FAIR. |
| Digital Object Identifier (DOI) [5] [63] | A persistent identifier that makes a dataset Findable and citable. It ensures the data can be located even if its web URL changes. Services like the Open Science Framework (OSF) can mint DOIs for your datasets. |
| Standard Contractual Clauses (SCCs) | Standardized data protection clauses adopted by the European Commission for transferring personal data from the EU to third countries. They are a key legal tool for ensuring lawful Accessibility in international research collaborations. |
For researchers handling viral sequence data, complying with the FAIR Guiding Principles (Findable, Accessible, Interoperable, and Reusable) is crucial for accelerating responses to emerging pathogens and facilitating robust scientific discovery [3]. However, significant resource and skills gaps often hinder effective implementation. This technical support guide addresses common experimental and data management challenges faced by scientists, providing practical troubleshooting advice to bridge these competency gaps. By establishing Data Champions—volunteers who support their research communities with data management guidance and training—and implementing structured learning pathways, organizations can build sustainable FAIR capabilities tailored to viral research needs [64].
FAIR Principles: Core Concepts and Relevance to Viral Data
The FAIR principles, formally introduced in 2016, provide a framework to enhance data reusability for both humans and computational systems [3] [65]. While often discussed alongside open data, FAIR compliance does not necessarily mean data must be publicly available; rather, it focuses on making data machine-actionable and well-structured, which is particularly important for sensitive viral sequence information that may have access restrictions [3] [46].
FAIR vs. CARE Principles for Viral Sequence Data
When working with viral genomic data, especially that associated with human hosts, it's important to recognize that FAIR principles sometimes need to be considered alongside other frameworks:
| Principle Type | Primary Focus | Key Considerations for Viral Data |
|---|---|---|
| FAIR Principles | Data quality and technical usability [3] | Machine-actionability, metadata richness, interoperability between platforms |
| CARE Principles | Data ethics and rights of Indigenous peoples [3] | Collective benefit, authority to control, responsibility, ethical use |
Common Experimental Challenges and Troubleshooting Guides
Data Fragmentation and Integration Issues
Problem: Viral sequence data is scattered across multiple platforms, databases, and file formats, making it difficult to locate and integrate for comprehensive analysis.
Troubleshooting Guide:
- Root Cause: Legacy systems, inconsistent data export formats, and lack of standardized data models
- Immediate Action: Implement a centralized cataloging system using persistent identifiers (e.g., DOI, EPI_ISL IDs for GISAID) for all viral sequences [5]
- Long-term Solution: Adopt a FAIR-compliant Laboratory Information Management System (LIMS) that uses standardized data models and APIs for integration [6] [46]
- Validation Method: Use automated FAIR assessment tools like F-UJI or FAIR Evaluator to identify interoperability gaps [65]
Metadata Inconsistencies in Viral Sequencing
Problem: Inadequate or inconsistent metadata documentation affects data quality, reliability, and the ability to reproduce findings.
Troubleshooting Guide:
- Root Cause: Use of free-text entries, custom labels, and non-standard terminology across labs
- Immediate Action: Adopt community-agreed standards for metadata (e.g., GISAID's controlled vocabulary for pathogen attributes) [5]
- Long-term Solution: Implement automated metadata annotation tools and establish dedicated data curation roles within the research team
- Validation Method: Regular metadata quality checks using semantic validation tools to ensure compliance with standardized ontologies
Data Access and Governance Challenges
Problem: Balancing data accessibility with security, privacy, and intellectual property concerns, especially for pre-publication viral sequence data.
Troubleshooting Guide:
- Root Cause: Unclear data ownership, governance gaps, and ethical concerns about data sharing
- Immediate Action: Develop transparent data access agreements that specify authentication protocols and usage terms [5]
- Long-term Solution: Establish cross-functional governance committees with representatives from science, ethics, legal, and IT departments
- Validation Method: Regular audits of access logs and compliance with data security protocols
Essential Research Reagent Solutions for FAIR Viral Data Management
Implementing FAIR principles requires both technical infrastructure and human expertise. The following table outlines key resources for establishing FAIR-compliant viral data workflows:
| Resource Category | Specific Solutions | Function in FAIR Implementation |
|---|---|---|
| Data Management Platforms | FAIR-compliant LIMS (e.g., Labbit) [6], GISAID platform [5], GARDIAN [65] | Provides structured environments for managing data with persistent identifiers and standardized metadata |
| Assessment Tools | F-UJI [65], FAIR Evaluator [65], FAIRshake [65] | Automates evaluation of FAIR compliance through standardized metrics and provides improvement guidance |
| Standardized Ontologies | WHO pathogen nomenclature [5], GA4GH standards [32], ASM (Allotrope Simple Model) [46] | Ensures semantic interoperability using community-agreed vocabularies for viral attributes and experimental conditions |
| Training Resources | FAIR Training Program [66], OpenAIRE FAIR RDM Bootcamp [67], Data Champion networks [64] | Builds institutional capacity through expert-led workshops, real-world case studies, and peer support systems |
Data Champion Program Implementation Framework
Data Champions are volunteers who support research communities by sharing information, tools, and best practices for research data management [64]. The following workflow outlines the key stages for establishing an effective Data Champion program:
Key Implementation Steps:
Program Scope Definition: Identify specific FAIR implementation challenges within your organization that Data Champions will address, focusing on viral sequence data management pain points
Champion Recruitment: Engage volunteers from diverse roles including wet-lab researchers, bioinformaticians, data managers, and principal investigators [64]
Structured Training: Provide specialized training on FAIR principles, metadata standards, and domain-specific tools through programs like the FAIR Training Program [66] or OpenAIRE Bootcamp [67]
Support Infrastructure: Establish regular forums, networking opportunities, and ongoing mentorship to maintain Champion engagement and knowledge sharing [64]
Community Integration: Deploy Champions within research groups and departments to provide localized support and serve as liaisons to central research data management teams
Program Sustainability: Implement recognition mechanisms, career development opportunities, and regular evaluation to ensure long-term program viability
FAIR Training Program Curriculum Development
Structured training is essential for building FAIR competency. The following table outlines a progressive learning path based on established FAIR training initiatives:
| Training Level | Core Content | Practical Skills Development |
|---|---|---|
| Foundational (The Why) | Value proposition of FAIR data, benefits for viral research, case studies from pathogen data infrastructures [66] | Understanding GDPR and ethical considerations, identifying FAIR implementation benefits for specific research contexts |
| Intermediate (The What) | FAIR principles deep dive, FAIR project management, interactive exercises like the (Un)FAIR game [66] | Evaluating existing datasets for FAIR compliance, developing FAIRification plans for viral sequence data |
| Advanced (The How) | Semantic modeling, querying FAIR data with SPARQL, legal and ethical considerations, integration with European Health Data Space [66] | Implementing FAIRification pipelines, applying automated assessment tools, modeling complex viral data for machine-actionability |
Experimental Protocol: FAIRness Assessment for Viral Sequence Data
Objective
To systematically evaluate the FAIR compliance of viral sequence datasets using established assessment tools and metrics.
Materials and Equipment
- Viral sequence dataset with associated metadata
- Computer with internet access
- FAIR assessment tool (e.g., F-UJI, FAIR Evaluator, or FAIRshake) [65]
- Spreadsheet software for documenting results
Methodology
Preparation Phase:
- Select a representative viral sequence dataset from your research
- Document current metadata practices and storage locations
- Identify relevant persistent identifiers associated with the dataset
Assessment Phase:
- Run the selected dataset through at least two different FAIR assessment tools [65]
- Record scores for each FAIR principle (Findable, Accessible, Interoperable, Reusable)
- Document specific metrics where compliance is not achieved
Analysis Phase:
- Compare results across assessment tools to identify consistent gaps
- Prioritize improvement areas based on impact and effort required
- Develop a FAIRification plan addressing the identified gaps
Validation Phase:
- Implement the FAIRification plan
- Reassess the dataset using the same tools
- Document improvements in FAIR compliance scores
Expected Outcomes
- Quantitative FAIR assessment scores for each principle
- Specific, actionable recommendations for improving FAIR compliance
- Documentation of implementation challenges and solutions
Interpretation Guidelines
- Recognize that different assessment tools may produce varying scores due to different metric implementations and interpretations [65]
- Focus on trend analysis rather than absolute scores when measuring improvement over time
- Consider both technical compliance and practical usability when evaluating results
Addressing the resource and skills gap in FAIR implementation requires a multifaceted approach combining technical infrastructure, specialized training, and community engagement. By establishing Data Champion networks and implementing structured training programs, research organizations can create sustainable pathways for building FAIR competency specifically tailored to viral sequence data management. The troubleshooting guides and experimental protocols provided here offer practical starting points for researchers facing common FAIR implementation challenges, enabling more effective data sharing and collaboration in virology research.
Frequently Asked Questions (FAQs) on Data Sharing and FAIR Compliance
FAQ 1: What are the FAIR Principles and why are they critical for viral sequence data? The FAIR Principles are a set of guiding principles to make data Findable, Accessible, Interoperable, and Reusable [28] [5]. For viral genomics, adherence to these principles is not merely a best practice but a cornerstone of rapid pandemic response and effective research. They enable scientists to quickly locate and utilize genomic data, integrate diverse datasets for powerful meta-analyses, and reproduce scientific findings, thereby accelerating the development of diagnostics, therapeutics, and vaccines [28].
FAQ 2: How can a Cost-Benefit Analysis (CBA) be applied to data set prioritization? A Cost-Benefit Analysis provides a systematic, data-driven framework to evaluate the financial and scientific viability of investing in the curation and sharing of a specific data set [68] [69]. The core process involves identifying and quantifying all associated costs and benefits to calculate a net benefit or a benefit-cost ratio. This helps organizations allocate limited resources to the data projects that promise the highest return on investment and the greatest scientific impact [70].
FAQ 3: What are the main data governance models for viral sequence databases? Two primary models have emerged:
- Regulated Access Model (e.g., GISAID): Provides free access to data while implementing constraints on usage to ensure equity and attribution for data contributors. Users must authenticate and agree to terms of use, which fosters participation from groups often concerned about exploitation [71].
- Unrestricted Access Model (e.g., INSDC, which includes GenBank): Advocates for completely free and unrestricted access to all data, permitting immediate availability and use by anyone, including commercial entities, without licensing barriers [71].
FAQ 4: What are common categories for viral genome completeness? Viral genome sequences are often categorized by their level of completeness, which is crucial for assessing their utility for different research applications [72]. The standards range from a Standard Draft to a Finished genome.
FAQ 5: What are the key cost categories in a CBA for data sharing? When conducting a CBA, it is essential to account for a comprehensive range of costs [68] [69]:
- Direct Costs: Expenses directly tied to data production and management (e.g., sequencing reagents, data storage hardware, dedicated bioinformatician salaries).
- Indirect Costs: Fixed overhead expenses (e.g., utilities, rent for server rooms, general IT infrastructure).
- Intangible Costs: Difficult-to-quantify costs such as the time spent by researchers on data curation instead of experimental work, or potential delays in research publication.
- Opportunity Costs: The value of the next-best alternative foregone, such as other research projects that cannot be pursued due to resources allocated to data sharing.
Troubleshooting Guides for Common Data Workflow Issues
Guide 1: Troubleshooting High Variability in Viral Sequence Data Quality
Problem: Submitted viral genome data exhibits inconsistent quality, high error rates, or poor assembly continuity, reducing its reusability and FAIRness.
Investigation & Resolution:
- Step 1: Verify Input Material Quality
- Action: Check the quality and quantity of the input nucleic acid. Use a fluorometer for accurate quantification and a Bioanalyzer or TapeStation to assess degradation.
- Rationale: Low-quality or low-quantity starting material is a primary cause of poor sequencing coverage and incomplete genomes [73].
Step 2: Review Sequencing Methodology and Coverage
- Action: Confirm that the sequencing technology and protocol are appropriate for the viral genome. Ensure average coverage depth is sufficient (e.g., >100x for a "Coding Complete" genome) [72].
- Rationale: Different technologies have different error profiles and read lengths. Insufficient coverage prevents the confident resolution of a consensus sequence.
Step 3: Execute a Systematic Troubleshooting Plan
- Action: Adopt a structured approach: 1) Identify the specific problem (e.g., high error rates in homopolymer regions), 2) Research potential solutions (e.g., optimizing library preparation protocols), 3) Create a detailed plan, 4) Implement the plan while meticulously documenting all steps, and 5) Validate the solution by reproducing the improved results [74].
Guide 2: Resolving Issues with FAIR Principle Implementation
Problem: Your viral data repository or platform is not effectively supporting the Findability or Reusability of its data holdings.
Investigation & Resolution:
- Step 1: Audit Findability Features
- Action: Ensure every data record is assigned a globally unique and persistent identifier (e.g., an accession number like GISAID's EPIISLID) [5]. Check that metadata is rich and described using a controlled, searchable vocabulary.
- Rationale: Without a persistent identifier and rich metadata, data cannot be reliably found by humans or machines, which is the foundation of the FAIR principles [28] [5].
- Step 2: Enhance Reusability through Provenance and Licensing
- Action: Clearly document the provenance of the data, including specimen origin, laboratory methods, and any data processing steps. Apply a clear, accessible usage license that specifies how the data can be reused [5].
- Rationale: Reusability depends heavily on the clarity of its licensing terms and the completeness of its background context, allowing others to understand and trust the data for their own research [28].
Data Presentation: Structured Tables
Table 1: Cost-Benefit Analysis of Data Governance Models
This table compares the two primary governance models for viral genomic data.
| Feature | Regulated Access Model (e.g., GISAID) | Unrestricted Access Model (e.g., INSDC) |
|---|---|---|
| Primary Goal | Incentivize rapid data sharing with equity and attribution [5] [71] | Promote completely open and immediate data access [71] |
| Key Economic Benefit | Higher participation from diverse, global contributors, enriching data diversity [71] | Fosters complex data linkages and unrestricted innovation [71] |
| Key Economic Cost | Requires infrastructure for authentication and enforcement of terms; potential for slower data integration [71] | May disincentivize data submission from some groups due to fears of lack of attribution [71] |
| FAIR Alignment | High, with strong focus on persistent identifiers, rich metadata, and clear reuse licenses [5] | High, with a focus on open, free protocols and universal implementability [28] |
Table 2: Viral Genome Quality Standards and Recommended Use Cases
This table outlines genome quality categories and their suitability for different research applications [72].
| Category | Contigs per Segment | Open Reading Frames | Estimated Genome Covered | Recommended for Downstream Applications |
|---|---|---|---|---|
| Standard Draft | >1 for some segments | Incomplete | ≥50% | Preliminary epidemiological screening |
| High Quality (HQ) | 1 | Incomplete | ~80-90% | Basic phylogenetic analysis |
| Coding Complete (CC) | 1 | Complete | ~90-99% | Molecular epidemiology; Description of novel viruses |
| Complete | 1 | Complete | 100% | Vaccine design; Reference genome creation |
| Finished | 1 | Complete | 100% + population data | Deep evolutionary studies; Pathogenesis research |
Experimental Protocols
Protocol 1: Achieving a "Coding Complete" Viral Genome via High-Throughput Sequencing
I. Objective: To generate a single contiguous sequence per viral genomic segment with all protein-coding regions complete, suitable for most molecular epidemiology and characterization studies [72].
II. Materials and Equipment
- Research Reagent Solutions:
- Nucleic Acid Extraction Kit: For isolating high-quality viral RNA/DNA.
- Reverse Transcription Kit: If sequencing an RNA virus.
- Library Preparation Kit: Compatible with your chosen sequencing platform (e.g., Illumina, Nanopore).
- Conserved PCR Primers: Designed to target the ends of genomic segments to close terminal gaps.
III. Methodology
- Sample Preparation & Sequencing:
- Extract viral nucleic acid, ensuring minimal host contamination.
- Prepare a sequencing library according to the manufacturer's protocol. For high coverage, aim for a depth of >100x [72].
- Sequence the library on an appropriate high-throughput platform.
Genome Assembly & Validation:
- Perform de novo assembly of the sequencing reads to generate contigs.
- Map the contigs to a reference genome to determine their order and orientation.
- Assess the assembly. If gaps remain at the ends of segments, use conserved PCR primers and Sanger sequencing to close them and complete the Open Reading Frames.
Quality Control:
- Verify that the final consensus sequence is a single contig per segment.
- Annotate all major Open Reading Frames to confirm they are complete and uninterrupted.
Protocol 2: Cost-Benefit Analysis for Data Set Prioritization
I. Objective: To quantitatively evaluate and prioritize candidate data sets for investment in FAIR-compliant curation and sharing.
II. Materials and Equipment
- Spreadsheet software or specialized project management tools.
- Historical data on past project costs and outcomes.
- Input from stakeholders across relevant domains.
- Establish the Framework: Define the goals and scope of the analysis. Decide on a common metric (e.g., monetary value, a scoring system) for comparison.
Identify Costs and Benefits:
- Costs: List all projected costs, including direct (e.g., personnel time for curation, cloud storage fees), indirect (e.g., infrastructure overhead), intangible (e.g., training time), and opportunity costs.
- Benefits: List all anticipated benefits, including direct (e.g., potential grant income enabled, cost savings from avoiding redundant experiments), indirect (e.g., increased citation impact), and intangible benefits (e.g., enhanced institutional reputation).
Assign Monetary Values: Assign a dollar value to each cost and benefit. This is straightforward for direct items but requires estimation or modeling for indirect and intangible items.
Calculate and Compare:
- Net Benefit = Total Benefits - Total Costs.
- Benefit-Cost Ratio (BCR) = Total Benefits / Total Costs.
- A positive net benefit or a BCR greater than 1 indicates a financially justifiable project.
Workflow Visualizations
Diagram 1: FAIR Data Prioritization Workflow
Diagram 2: Viral Genome Quality Pipeline
The Scientist's Toolkit: Key Research Reagents
| Item | Function in Viral Genomics |
|---|---|
| Nucleic Acid Extraction Kit | Isolates viral RNA or DNA from clinical or environmental samples, which is the critical first step for any sequencing project. |
| Reverse Transcription Kit | Converts viral RNA into complementary DNA (cDNA), a necessary process for sequencing RNA viruses like SARS-CoV-2 or influenza. |
| High-Throughput Sequencer | Platforms (e.g., Illumina, Oxford Nanopore) that generate massive amounts of sequence data in parallel, enabling rapid whole-genome sequencing. |
| Conserved PCR Primers | Used to amplify and sequence the ends of viral genomes, a key technique for achieving "Coding Complete" or "Complete" genome status [72]. |
| Bioinformatics Software | Tools for genome assembly, variant calling, and phylogenetic analysis, essential for transforming raw sequence data into biological insights. |
Benchmarking Success: Evaluating FAIR Compliance and Database Performance
The FAIR Guiding Principles—Findable, Accessible, Interoperable, and Reusable—establish a framework for optimizing the management and stewardship of scientific data, with emphasis on machine-actionability to handle increasing data volume and complexity [1]. In virology, these principles are critically applied to virus databases, which serve as central hubs connecting viral genomic sequences with essential metadata such as host taxonomy, geographical location, and gene annotations [54]. The COVID-19 pandemic underscored the vital importance of FAIR-compliant data sharing, enabling rapid global collaboration on vaccine development, treatment, and viral evolution surveillance through platforms like GISAID and the EU Covid-19 Data Portal [31].
Assessing the FAIRness of these databases ensures that valuable pathogen data can be effectively located, accessed, integrated with other datasets, and reused for both research and public health responses. This technical support center provides a structured framework, practical metrics, and troubleshooting guidance for researchers evaluating virus database compliance with FAIR principles.
FAIR Metrics and Assessment Framework
Core FAIR Metrics for Virus Databases
Table 1: Core FAIR Metrics for Virus Database Assessment
| FAIR Principle | Key Metric | Assessment Question | Scoring (0-1) |
|---|---|---|---|
| Findable | Unique Identifier | Does each data record have a globally unique and persistent identifier? | 1 = Yes, 0 = No |
| Rich Metadata | Are data described with a rich set of searchable metadata? | 1 = Extensive, 0.5 = Basic, 0 = None | |
| Searchable Index | Are (meta)data registered in a searchable resource or catalog? | 1 = Yes, 0 = No | |
| Accessible | Standard Protocol | Are (meta)data retrievable via standardized, open communication protocol? | 1 = Yes (e.g., HTTPS), 0 = No |
| Authentication Clarity | Is authentication and authorization procedure clearly defined? | 1 = Clear & free, 0.5 = Restricted, 0 = Unclear | |
| Metadata Persistence | Are metadata accessible even when data is no longer available? | 1 = Yes, 0 = No | |
| Interoperable | Formal Language | Do (meta)data use a formal, accessible, shared language? | 1 = Yes (e.g., RDF, JSON), 0 = No |
| FAIR Vocabularies | Are standardized, documented vocabularies used? | 1 = Yes, 0.5 = Partial, 0 = No | |
| Qualified References | Does metadata include qualified references to other metadata? | 1 = Yes, 0.5 = Partial, 0 = No | |
| Reusable | Usage License | Is there a clear, accessible data usage license? | 1 = Yes, 0 = No |
| Data Provenance | Is detailed provenance information provided? | 1 = Yes, 0.5 = Partial, 0 = No | |
| Community Standards | Do data meet domain-relevant community standards? | 1 = Yes, 0.5 = Partial, 0 = No |
The metrics in Table 1 are derived from the universal FAIR guidelines and adapted for the specific context of virology data [75] [1]. For example, GISAID implements these through unique persistent identifiers (EPI_ISL ID), standardized metadata fields, and data exchange in broadly accepted formats like FASTA, CSV, and JSON [5].
FAIRness Assessment Methodology
The following workflow outlines the systematic process for evaluating virus database FAIRness:
Figure 1: FAIRness Assessment Workflow. This diagram illustrates the systematic process for evaluating virus database compliance with FAIR principles.
Experimental Protocol: FAIRshake-Based Assessment
The FAIRshake toolkit provides a standardized methodology for manual and automated FAIRness evaluation [75]. The following steps outline the assessment procedure:
- Database Registration: Create a FAIRshake project to bundle thematically relevant digital resources. Project descriptions must contain minimal information for identification and indexing.
- Rubric Selection: Associate the target virus database with an appropriate FAIR rubric—a collection of FAIR metrics relevant to virology data. FAIRshake provides existing rubrics or allows creation of custom ones.
- Manual Assessment: For each metric in the rubric, answer the corresponding question based on database inspection. Example: "Does the database assign globally unique and persistent identifiers to each sequence record?" (Yes/Partially/No).
- Automated Checks: Where possible, link metric concepts to executable code for automated evaluation. This may include checking for machine-readable metadata via RDF extraction using tools like Extruct.
- Scoring and Visualization: FAIRshake quantifies manual and automated metric answers to a value between 0 and 1, then calculates a composite FAIR score. Results are visualized using the FAIR insignia—a compact grid of colored squares representing the FAIR score.
- Documentation: Compile assessment results, including scores for each metric, overall composite score, and identified areas for improvement.
Troubleshooting Common FAIR Assessment Challenges
Frequently Asked Questions (FAQs)
FAQ 1: What is the difference between FAIR and Open Data? FAIR data focuses on making data machine-readable and reusable under well-defined conditions, which may include necessary restrictions. Open Data emphasizes making data freely available to everyone without restrictions. A virus database can be FAIR without being fully open, especially when handling sensitive patient information or during outbreaks where temporary embargoes protect contributors' publication rights [76].
FAQ 2: How can we assess databases that use authentication and access controls without violating terms? The "Accessible" principle does not prohibit authentication. Assessment should verify that: 1) The authentication process is clearly explained; 2) Access conditions are transparent; 3) The protocol is standard and free (e.g., HTTPS); 4) Metadata remains accessible even if data is restricted. GISAID demonstrates this by requiring free user registration while maintaining transparent access agreements [5].
FAQ 3: How do we handle databases with inconsistent metadata quality across records? This is a common challenge. The assessment should: 1) Sample multiple records to gauge consistency; 2) Check if the database provides a curated subset of high-quality data; 3) Evaluate whether metadata fields use controlled vocabularies to minimize inconsistency; 4) Score "Rich Metadata" metrics based on the percentage of records with complete, structured metadata [54].
FAQ 4: What are the specific interoperability challenges for viral sequence data? Key challenges include: 1) Taxonomic classification conflicts for entities like Endogenous Viral Elements (EVEs), which can be classified as both host and virus; 2) Integration of diverse data types (genomic, clinical, epidemiological); 3) Use of non-standardized vocabularies for critical fields like host species or geographic location. Solutions involve adopting community-agreed standards and semantic frameworks [12].
Advanced Implementation: FAIR+E and Equity
Beyond core FAIR principles, the FAIR+E framework introduces an Equitable dimension, emphasizing trust-building and inclusive design [31]. This is particularly relevant for global pathogen surveillance. Implementation strategies include:
- Establishing data ownership where data is generated, especially in underrepresented regions.
- Creating a distributed network of Pathogen Data Platforms that perform data brokering, ensuring high-quality, standardized data without centralizing sensitive information.
- Developing an International One Health Pathogens Portal connecting human, animal, and environmental data following FAIR+E principles.
The VODAN (Virus Outbreak Data Network) Implementation Network exemplifies this approach by installing local FAIR Data Points in participating countries, allowing data to be "visited" by virtual machines for analysis without the underlying data leaving the source institution, thus accommodating privacy and legal constraints [77].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Research Reagents for FAIRness Assessment
| Tool/Resource Name | Type | Primary Function in FAIR Assessment |
|---|---|---|
| FAIRshake Toolkit | Web Application/API | Enables manual and automated FAIR assessments using customizable rubrics and metrics; visualizes results with FAIR insignia [75]. |
| FAIRsharing | Database Catalog | Provides a curated, searchable registry of standards, databases, and policies to identify relevant community standards for interoperability [54] [75]. |
| RDF (Resource Description Framework) | Data Format | Serves as a key globally accepted framework for machine-readable data and knowledge representation, enabling automated metadata extraction [75]. |
| detectEVE | Bioinformatics Tool | Open-source pipeline for identifying Endogenous Viral Elements; addresses specialized interoperability challenges in viral genomics [12]. |
| FAIR Data Point | Software Application | A FAIR data repository with "docking" capabilities; enables federated, privacy-preserving data access as implemented in VODAN [77]. |
| DataSeer | AI Tool | Helps identify and verify research data and compliance with journal data policies; useful for pre-submission checks [12]. |
| Extruct | Software Library | Extracts structured metadata from webpages; supports automated checking for machine-readable metadata [75]. |
Implementing a rigorous FAIRness assessment framework for virus databases is fundamental for advancing virology research and pandemic preparedness. By applying standardized metrics, following systematic assessment protocols, and utilizing specialized tools, researchers can critically evaluate data resources, identify areas for improvement, and ultimately contribute to a more robust, interoperable, and equitable global data ecosystem for pathogen surveillance. The framework outlined here provides both the theoretical foundation and practical guidance needed to ensure that vital viral sequence data is not only available but truly Findable, Accessible, Interoperable, and Reusable for the global research community.
This technical support center is designed within the context of advanced research on viral sequence data and its compliance with the FAIR (Findable, Accessible, Interoperable, Reusable) principles. For researchers, scientists, and drug development professionals, navigating the landscape of virus databases is crucial for outbreak monitoring, evolutionary studies, and therapeutic design. The following guides and FAQs address common experimental hurdles related to database content, functionality, and data quality, providing targeted troubleshooting strategies.
FAQs: Navigating Virus Database Content and Functionality
FAQ 1: How do I choose a virus database that is both comprehensive and FAIR-compliant?
Selecting the right database requires balancing scope, data quality, and adherence to modern data stewardship principles. A database might be comprehensive but lack the curation needed for reliable analysis.
Troubleshooting Guide:
- Issue: Uncertainty about database features and FAIR compliance.
- Explanation: Virus databases vary significantly in their specialization, data types, and aims. Some are broad repositories, while others focus on specific viruses, epidemiology, or protein structures. Their compliance with FAIR principles directly impacts how easily you can find, access, and reuse data in an automated way [78].
- Solution:
- Define Your Need: Determine if you need genomic sequences, protein structures, or specific metadata.
- Consult Comparative Reviews: Refer to recent scholarly articles that evaluate active virus databases based on their content, functionality, and FAIR adherence [78].
- Check for FAIR Indicators: Look for databases that provide persistent unique identifiers (e.g., EPI_ISL IDs in GISAID), use standardized data formats (FASTA, CSV, JSON), and have clear data usage licenses [5].
Experimental Protocol: Database Selection Workflow The following protocol outlines a systematic approach for selecting an appropriate virus database for your research project.
- Diagram Title: Virus Database Selection Workflow
FAQ 2: Why are my sequences not being classified or are being misclassified in my metagenomic analysis?
This is a frequent issue in metagenomic studies and is often rooted in problems with the reference database itself, rather than your samples or primary analysis tools.
- Troubleshooting Guide:
- Issue: Sequences are excluded from analysis or assigned incorrect taxonomic labels.
- Explanation: Reference databases can contain several common errors:
- Taxonomic Mislabeling: Sequences are assigned to the wrong species. An estimated 3.6% of prokaryotic genomes in GenBank are affected, and this extends to viral sequences [52].
- Sequence Contamination: Databases contain sequences with adapter contamination or host DNA, leading to false positives [52].
- Inappropriate Filtering: Your analysis pipeline may be filtering out sequences that deviate from an expected molecular clock or fail other quality thresholds [79].
- Solution:
- Investigate Filtering Logs: Check your workflow's log files (e.g.,
filtered_log.tsvin Nextstrain) to see why sequences were removed [79]. - Use Curated Subsets: Prefer curated database subsets like RefSeq over the full GenBank where possible, as they have fewer errors [52].
- Validate Findings: For critical results, manually validate classifications by checking sequence alignment quality and consulting multiple databases.
- Investigate Filtering Logs: Check your workflow's log files (e.g.,
FAQ 3: What does FAIR compliance mean for a virus database, and how is it implemented?
FAIR principles provide a framework for enhancing the reuse of digital assets by both humans and machines.
- Troubleshooting Guide:
- Issue: Lack of understanding of how FAIR principles translate to practical database features.
- Explanation: FAIR stands for Findable, Accessible, Interoperable, and Reusable. It is a set of guiding principles for scientific data management and stewardship [5].
- Solution: Look for these concrete implementations:
- Findable: Data is assigned a globally unique and persistent identifier (e.g., a DOI or an accession number like GISAID's EPI_ISL ID) [5].
- Accessible: Data is retrievable using a standardized, open protocol (e.g., HTTPS) with clear authentication and authorization rules [5].
- Interoperable: Data uses formal, accessible, and broadly applicable languages and vocabularies (e.g., CSV, TSV, FASTA) [5].
- Reusable: Data is released with a clear usage license and is richly described with multiple, relevant metadata attributes [5].
Troubleshooting Guides for Common Experimental Issues
Guide 1: Mitigating Reference Database Errors in Viral Metagenomics
Errors in reference sequence databases are a major source of irreproducibility in metagenomic studies. The following table summarizes common issues and their mitigation strategies [52].
- Experimental Protocol: A Tiered Mitigation Strategy
- Awareness: Acknowledge that no database is perfect. Assume that errors like contamination and taxonomic mislabeling are present.
- Curation: Implement a pre-processing step to clean your custom database. Use tools designed to detect contaminants and taxonomically mislabeled sequences.
- Validation: Perform negative control analyses. Process samples that should not contain your virus of interest to identify false-positive detections stemming from database errors.
- Selection: For clinical or high-stakes research, use databases that have been validated across thousands of samples and have undergone manual curation.
Table 1: Common Virus Database Issues and Mitigation Strategies
| Issue | Description & Impact | Mitigation Strategy |
|---|---|---|
| Taxonomic Mislabeling | Sequence is incorrectly assigned to a species; causes false positive/negative detections [52]. | Use curated subsets (e.g., RefSeq); cluster sequences by Average Nucleotide Identity (ANI) to find outliers [52]. |
| Sequence Contamination | Presence of adapter, vector, or host DNA in sequences; leads to false assignments [52]. | Employ bioinformatic contamination-screening tools; use databases that perform routine contamination checks [52]. |
| Insufficient Metadata | Lack of rich, standardized metadata (host, location, date); limits reuse and epidemiological analysis [78]. | Choose databases that enforce community metadata standards; be cautious when reusing data with sparse metadata [78]. |
| Non-FAIR Compliance | Data is hard to find, access, or reuse computationally; hinders collaboration and automated analysis [78]. | Select databases that mint persistent identifiers, use standard formats, and have clear data licenses [5]. |
Guide 2: Resolving Data Accessibility and Equitable Reuse Concerns
The scientific community is grappling with how to balance open data access with fair recognition for data creators.
- Troubleshooting Guide:
- Issue: Uncertainty about the ethics and etiquette of reusing public sequence data, especially when it preempts the original researcher's publication.
- Explanation: Historical agreements like the Fort Lauderdale Agreement advocated for immediate, unrestricted data release. However, the volume of data today means data creators may not have time to publish their findings before others reuse their publicly deposited data [37] [9].
- Solution:
- Look for a DRI Tag: A new initiative proposes a machine-readable Data Reuse Information (DRI) tag linked to an ORCID. This tag signals the data creator's preference to be contacted before reuse [37] [9].
- Communicate: If a DRI tag is present, reach out to the data creator to discuss collaboration or appropriate acknowledgment.
- Cite Generously: Always cite the original database and any primary publications associated with the data you use.
Table 2: Key Resources for Viral Database Research and Analysis
| Item | Function & Application |
|---|---|
| FAIRsharing / re3data.org | Catalogs of databases that provide metadata and evaluations, helping researchers find suitable virus databases [78]. |
| Data Reuse Information (DRI) Tag | A machine-readable tag in a dataset that indicates the data creator's preference for communication prior to reuse, facilitating equitable collaboration [37]. |
| Persistent Identifier (e.g., DOI, EPI_ISL ID) | A globally unique and permanent identifier for a dataset or record, ensuring traceability, versioning, and scientific reproducibility [5]. |
| Curated Database Subsets (e.g., RefSeq) | Higher-quality subsets of larger databases that have undergone additional review to reduce errors like taxonomic mislabeling and contamination [52]. |
| Quality Control Tools (e.g., FastQC) | Software used to assess the quality of raw sequencing data before alignment, helping to identify issues like adapter contamination or low-quality reads [80]. |
Technical Support Center
Troubleshooting Guides
Guide 1: Troubleshooting RWE Study Design for Regulatory Submission
Problem: Inadequate study design leads to FDA rejection of Real-World Evidence (RWE) for a new indication.
- Symptoms: FDA requests additional data, regulatory decision delayed, RWE deemed insufficient for effectiveness claim.
- Root Cause: Misalignment between real-world data (RWD) sources, study methodology, and regulatory standards for providing substantial evidence [81] [82].
Solution:
- Define Regulatory Objective: Precisely specify the regulatory question (e.g., new indication, post-approval study requirement) [81] [83].
- Assess Data Fitness: Evaluate RWD sources (e.g., electronic health records, registries) for relevance, reliability, and ability to address the objective [81]. For viral sequence data, ensure compliance with FAIR principles—Findable, Accessible, Interoperable, Reusable—by using unique identifiers and rich metadata [5].
- Select Robust Design: Choose a study design (e.g., retrospective cohort, externally controlled trial) that minimizes bias and confounding [82].
- Engage FDA Early: Consult with the FDA's Office of Therapeutic Products for feedback on clinical trial design and safety monitoring plans [84].
Guide 2: Resolving FAIR Compliance Issues in Viral Sequence Data
Problem: Viral sequence data and associated metadata are not fully FAIR-compliant, hindering interoperability and reuse for RWE generation.
- Symptoms: Difficulty integrating datasets, metadata inconsistencies across sources, inability to track data provenance.
- Root Cause: Lack of standardized data formats, controlled vocabularies, or clear data licensing [5] [3].
Solution:
- Assign Persistent Identifiers: Mint a globally unique, persistent identifier (e.g., a DOI or accession number like an EPIISLID) for each sequence and dataset [5].
- Use Rich Metadata: Describe data with rich, machine-readable metadata using community-standardized fields and ontologies [5].
- Employ Standard Formats: Share data in broadly accepted, machine-readable formats (e.g., FASTA, FASTQ, CSV, JSON) [5].
- Document Provenance & Licensing: Clearly document data origin, processing steps, and usage rights to ensure reproducibility and proper reuse [5] [3].
Frequently Asked Questions (FAQs)
FAQ 1: What is the difference between Real-World Data (RWD) and Real-World Evidence (RWE) according to the FDA?
- Answer: The FDA defines Real-World Data (RWD) as "data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources," such as electronic health records, medical claims data, and disease registries [81]. Real-World Evidence (RWE) is "the clinical evidence about the usage and potential benefits or risks of a medical product derived from analysis of RWD" [81]. In essence, RWD is the raw data, while RWE is the clinical evidence generated from its analysis.
FAQ 2: For what specific regulatory decisions has the FDA used RWE for biological products?
- Answer: The FDA has used RWE to support various regulatory decisions for biological products, including new drug approvals, labeling changes, and post-market safety assessments. The table below summarizes key examples [82]:
| Product (Biological) | Regulatory Action | RWE Use & Data Source |
|---|---|---|
| Actemra (Tocilizumab) | Approval for a new indication | Primary efficacy endpoint (28-day mortality) assessed using RWD from national death records within a randomized controlled trial [82]. |
| Orencia (Abatacept) | Approval for a new indication | Pivotal evidence from a non-interventional study using data from the CIBMTR registry (an international registry of patients receiving cellular therapies) [82]. |
| Prolia (Denosumab) | Boxed Warning & Labeling Change | Safety assessment via a retrospective cohort study using Medicare claims data, which identified an increased risk of severe hypocalcemia [82]. |
| Entyvio (Vedolizumab) | Labeling Change | Postmarket safety evaluation using a descriptive study from the Sentinel System [82]. |
FAQ 3: How can natural history study data be used in the development of regenerative medicine therapies?
- Answer: For regenerative medicine therapies, such as those with an RMAT (Regenerative Medicine Advanced Therapy) designation, the FDA encourages the use of natural history data. This data can provide the basis for a historical control group in clinical trials, but only if the control and treatment populations are adequately matched in terms of demographics, disease state, concurrent treatments, and other relevant factors [84].
FAQ 4: My RWE study uses viral sequence data. How do FAIR principles support regulatory submission?
- Answer: Adhering to FAIR principles directly enhances the reliability and acceptability of your RWE study for regulatory review by ensuring:
- Findability: Unique identifiers (e.g., EPIISLID) allow FDA reviewers to precisely locate and reference the specific sequences used in your analysis [5].
- Interoperability: Standardized data formats and vocabularies allow the viral sequence data to be integrated with clinical outcome datasets (e.g., from EHRs), which is critical for generating robust RWE [5] [3].
- Reusability: Clear provenance and metadata ensure the analysis is reproducible, a cornerstone of scientific rigor and regulatory assessment [5] [3].
Structured Data and Protocols
The following table provides a detailed breakdown of RWE study methodologies from recent FDA regulatory actions, serving as a reference for designing your own protocols [82].
| Product / Identifier | Study Design | Data Sources | Role of RWE in Regulatory Decision |
|---|---|---|---|
| Voxzogo (Vosoritide) NDA 214938 | Externally controlled trial | Achondroplasia Natural History (AchNH) study (a multicenter US registry) | Served as confirmatory evidence. External control groups were built from patient-level data from the natural history registry [82]. |
| Nulibry (Fosdenopterin) NDA 214018 | Single-arm trial with external controls | Medical records from 15 countries (for both expanded access program patients and natural history controls) | Served as an adequate and well-controlled study generating substantial evidence of effectiveness. RWD was used in both treatment and control arms [82]. |
| Prograf (Tacrolimus) NDA 050708 | Non-interventional study | Scientific Registry of Transplant Recipients (SRTR) disease registry | Served as an adequate and well-controlled study generating substantial evidence of effectiveness for lung transplant patients [82]. |
Experimental Protocol: Generating RWE from a Disease Registry
This protocol outlines the methodology for using a disease registry to generate RWE for a regulatory submission, based on successful FDA cases [82].
1. Objective Definition: Clearly state the regulatory question (e.g., "To compare the overall survival at one-year post-treatment in patients receiving Drug A versus a matched historical control group").
2. Registry Selection & Data Extraction:
- Selection: Identify a fit-for-purpose registry (e.g., CIBMTR, SRTR) with relevant, reliable, and longitudinal data [82].
- FAIR Compliance Check: Verify the registry data uses persistent identifiers, controlled vocabularies, and provides rich metadata for interoperability [5].
- Extraction: Define and extract a cohort from the registry, including patient demographics, treatment history, clinical outcomes, and relevant covariates.
3. Study Population & Matching:
- Treatment Arm: If applicable, pool data from interventional trials with data from expanded access programs [82].
- Control Arm: Construct an external control arm from the registry's natural history data.
- Matching: Use statistical methods (e.g., propensity score matching) to ensure the control group is adequately matched to the treatment group for key prognostic factors [84].
4. Outcome Assessment: Define and assess primary and secondary endpoints (e.g., overall survival, graft failure) from the registry data [82].
5. Data Analysis & Validation:
- Analysis: Employ appropriate statistical models to compare outcomes between groups, adjusting for residual confounding.
- Sensitivity Analyses: Conduct multiple analyses to test the robustness of the findings against different assumptions and potential biases.
The Scientist's Toolkit
Research Reagent Solutions for RWE Generation
This table lists key "reagents" – data sources and methodological tools – essential for constructing robust RWE studies.
| Item | Function / Application |
|---|---|
| Electronic Health Records (EHRs) | Source of detailed, patient-level clinical data including diagnoses, treatments, and outcomes for longitudinal studies [81]. |
| Disease Registries | Curated data sources focused on specific diseases or conditions, often used to create external control arms or study natural history [82]. |
| Medical Claims Data | Provides information on diagnoses, procedures, and prescriptions, useful for large-scale safety and utilization studies [81]. |
| Sentinel System | The FDA's national electronic system for monitoring the safety of approved medical products, used for post-market safety assessments and labeling changes [82]. |
| FAIR-Compliant Sequence Databases (e.g., GISAID) | Platforms that provide viral sequence data with unique identifiers and rich metadata, enabling interoperable and reproducible research integrated with clinical data [5]. |
| Propensity Score Matching | A statistical method used to create comparable treatment and control groups in observational studies, reducing selection bias. |
| Digital Health Technologies (DHTs) | Tools such as wearables and sensors, encouraged by the FDA for collecting real-world safety information in clinical trials [84]. |
Workflow Diagrams
RWE Study Validation Pathway for Regulatory Submission
FAIR Principles Implementation for Viral Sequence Data
For researchers managing viral sequence data, ensuring the database's long-term viability and community trust is paramount. The FAIR principles—making data Findable, Accessible, Interoperable, and Reusable—provide a critical framework for achieving these goals [3]. This technical support center addresses common operational challenges, offering practical methodologies to maintain FAIR compliance, which is intrinsically linked to both the functional longevity of the data resource and the sustained trust of the global research community [85] [5]. A database designed for longevity reduces the frequent need for replacement and associated resource consumption, embodying a commitment to sustained utility and minimal environmental burden [86].
Troubleshooting Common FAIR Compliance Challenges
Findability Issues
- Problem: Users report inability to locate specific sequence datasets using the platform's search function.
- Diagnosis: This often stems from incomplete or non-standardized metadata, which prevents effective indexing. Findability requires data to be easy to find for both humans and computers, assisted by rich metadata and persistent identifiers [5] [3].
- Solution:
- Implement Persistent Identifiers: Assign a globally unique and persistent identifier (e.g., an EPI_ISL ID or DOI) to each sequence record and to curated collections [5].
- Enforce Metadata Standards: Utilize a controlled, documented vocabulary for metadata fields. Implement automated quality checks to ensure submissions are complete and legible [5].
- Registry Indexing: Ensure datasets are registered with global data search engines and repositories like re3data.org to enhance discoverability [5].
Accessibility Problems
- Problem: Data retrieval is slow, or users face unclear authentication barriers.
- Diagnosis: Accessibility issues can arise from non-standard protocols or poorly defined authentication procedures. Data should be retrievable via standardized, open communications protocols like HTTPS, with clear access rules [5] [3].
- Solution:
- Standardize Protocols: Provide data access through open, free, and universally implementable protocols (e.g., HTTPS) via web interfaces and API endpoints [5].
- Clarify Access Tiers: Maintain a transparent access agreement. Differentiate between:
- Open Access: Publicly available metadata and sequences.
- Controlled Access: Data requiring user authentication and agreement to terms to ensure transparent and fair use, protecting contributor rights [5].
- Persistent Metadata: Ensure that basic metadata remain accessible and traceable via their identifier, even if the underlying sequence data is temporarily embargoed or withdrawn [5].
Interoperability Failures
- Problem: Downloaded data cannot be integrated into standard bioinformatics workflows or combined with data from other sources.
- Diagnosis: This is typically caused by the use of proprietary or inconsistent data formats. Interoperability requires data to be machine-readable and use formal, accessible languages for knowledge representation [5] [3].
- Solution:
- Adopt Standard Formats: Offer data exports in broadly accepted, machine-readable formats such as FASTA, FASTQ, CSV, TSV, and JSON [5].
- Utilize Common Vocabularies: Adopt community-sanctioned ontologies for metadata (e.g., for host, collection location, assay). GISAID, for instance, works with domain experts to establish these standards [5].
- Enable Cross-Referencing: Implement systems that allow data to be linked to external resources, such as publications (via DOIs) or clinical datasets, using persistent identifiers [5].
Reusability Limitations
- Problem: Downloaded datasets lack sufficient provenance or context to be replicated or reused in a new study.
- Diagnosis: Reusability is compromised by missing data provenance, unclear licensing, or inadequate documentation. Reusable data must be richly described with accurate and relevant attributes and have a clear license [5] [3].
- Solution:
- Document Provenance Meticulously: Capture and display critical information about the data's origin, including submitting and originating lab, author contributions, and sequencing methods [5].
- Define Clear Usage Licenses: Release data under a clear, accessible license agreement that specifies how the data can be used, often including provisions for temporary embargoes to protect contributors' publication rights [5].
- Provide Rich Context: Annotate sequences with community-agreed data and metadata standards, such as clade and lineage annotations, and quality parameters, often through a combination of automated and human curation [5].
Frequently Asked Questions (FAQs)
Q1: What is the concrete difference between "open data" and "FAIR data"?
- A: Open data focuses on being free to access without restrictions, but it may lack the structure and metadata for computational use. FAIR data is focused on machine-actionability; it can be either open or controlled-access, but it must be structured with rich metadata to be Findable, Accessible, Interoperable, and Reusable by computers. Not all open data is FAIR, and not all FAIR data is open [3].
Q2: How do we measure and build "Community Trust" in a data platform?
- A: Community Trust is a multi-dimensional asset earned through competencies and values. It can be measured using frameworks like the Community Trust Index, which assesses factors like transparency, accountability, and fairness [87]. Building trust involves:
- Demonstrating Competence: Reliable platform performance and high-quality, curated data.
- Upholding Values: Transparent governance, equitable data access policies, and fair recognition of data contributors [87] [88]. A Community Data Trust model, where a community collectively governs data for the common good, is a formal structure for achieving this [88].
- A: Community Trust is a multi-dimensional asset earned through competencies and values. It can be measured using frameworks like the Community Trust Index, which assesses factors like transparency, accountability, and fairness [87]. Building trust involves:
Q3: Our legacy genomic data doesn't meet current FAIR standards. What is the most efficient way to make it FAIR?
- A: Retrofitting legacy data is a common challenge. A recommended methodology is:
- Inventory and Prioritize: Identify high-value datasets for FAIRification.
- Map Metadata: Profile existing metadata and map them to current controlled vocabularies and ontologies.
- Assign PIDs: Mint persistent identifiers (e.g., DOIs) for these datasets.
- Implement a Programmatic Pipeline: Use scalable data processing frameworks (e.g., TileDB, specialized ETL scripts) to transform and standardize data formats in bulk, rather than manual conversion [3].
- A: Retrofitting legacy data is a common challenge. A recommended methodology is:
Q4: Are there specific security concerns with portable sequencing that affect data integrity at the point of acquisition?
- A: Yes. Portable sequencers that rely on external hosts (e.g., laptops) for basecalling broaden the attack surface. Threats include:
- Loss of Confidentiality: Eavesdropping on data transmitted between sequencer and host.
- Loss of Integrity: A compromised host could manipulate basecalling to alter the genomic sequence output.
- Loss of Availability: Denial-of-Service attacks could disrupt sequencing runs [89].
- Mitigation: Employ a zero-trust security approach, verifying every access request, even from within the network. Ensure all data transmissions between devices are encrypted [89].
- A: Yes. Portable sequencers that rely on external hosts (e.g., laptops) for basecalling broaden the attack surface. Threats include:
Quantitative Data on FAIR and Longevity
Table 1: Impact of FAIR Data Implementation on Research Outcomes
| Metric | Pre-FAIR Implementation | Post-FAIR Implementation | Source / Context |
|---|---|---|---|
| Time to Insight | Manual, weeks-long data discovery and formatting | Automated discovery; analysis time reduced to days | Enables faster time-to-insight [3] |
| Data ROI | Data often siloed and underused | Maximizes value of existing data assets; reduces duplication | Improves data ROI and reduces infrastructure waste [3] |
| Reproducibility | Difficult to trace data provenance and methods | Embedded metadata and provenance simplify replication | Ensures reproducibility and traceability [3] |
| Collaboration Efficiency | Hindered by fragmented systems and formats | Standardized formats enable cross-team/silo collaboration | Enables better team collaboration across silos [3] |
Table 2: Community Trust Factors and Measurement
| Trust Factor | Low-Trust Indicator | High-Trust Indicator | Measurement Tool |
|---|---|---|---|
| Network Trust | Reluctance to share data based on negative past experiences | Willingness to contribute data based on mutual respect and transparency | Community Trust Index [87] |
| Transparency | Opaque data usage and governance policies | Clear, accessible, and fair data access agreements | Community Trust Index [87] [5] |
| Competence | Frequent platform downtime or data errors | High platform reliability and data quality | Community Trust Index [87] |
| Reciprocity | Contributors do not receive recognition or benefit | Contributors receive acknowledgment and value from the collective resource | Social Network Analysis [90] |
Experimental Protocol: Implementing a FAIR Compliance Check
Objective: To systematically audit a viral sequence dataset for compliance with FAIR principles.
Materials:
- The viral sequence dataset (e.g., in FASTQ, FASTA format).
- Associated metadata file (e.g., CSV, TSV).
- Access to a persistent identifier resolver (e.g., a DOI lookup service).
- Metadata validation tools (e.g., community-specific schema validators).
Methodology:
- Findability Check:
- Verify that the dataset has been assigned a globally unique and persistent identifier (e.g., DOI, Accession Number).
- Check that the metadata is rich and uses controlled vocabularies where possible (e.g., for species, location).
- Confirm the dataset is indexed in a searchable resource (e.g., the host database's search engine, external registries).
- Accessibility Check:
- Test that the data can be retrieved using its identifier via a standardized protocol (e.g., HTTPS).
- Review the authentication and authorization process—is it clear, free, and universally implementable?
- Confirm that metadata remains accessible even if data is deprecated.
- Interoperability Check:
- Validate that the data and metadata are in a formal, accessible, and widely used language (e.g., CSV, JSON).
- Check that the metadata vocabularies follow FAIR principles themselves.
- Look for the presence of qualified references to other data (e.g., links to publications via DOI).
- Reusability Check:
- Verify that the dataset is richly described with multiple relevant attributes.
- Check that provenance is thoroughly documented (who, when, how the data was generated).
- Confirm that a clear license or usage terms are provided.
Workflow and Relationship Visualizations
FAIR Data Implementation Workflow
Community Trust and Data Longevity Relationship
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item / Solution | Function | Example / Standard |
|---|---|---|
| Persistent Identifier Service | Provides a globally unique, permanent identifier for a dataset to ensure findability and citability. | DOI, EPI_ISL ID [5] |
| Metadata Schema Validator | Checks that submitted metadata conforms to community-agreed standards and controlled vocabularies. | GISAID curation tools, ISA framework [5] |
| Controlled Vocabulary / Ontology | Provides standardized terms for metadata fields (e.g., specimen type, host) to ensure interoperability. | NCBI Taxonomy, EDAM Ontology, GISAID pathogen-specific terms [5] [3] |
| Data Repository Platform | A platform that supports the storage, management, and publication of data with FAIR principles embedded. | GISAID, TileDB, Zenodo [5] [3] |
| Zero-Trust Security Framework | A security model that requires verification for every access request, critical for portable sequencing data integrity. | As outlined in Nature Communications for portable sequencers [89] |
FAQs on FAIR Data Impact and Troubleshooting
This section addresses common questions about the tangible benefits and common challenges of implementing FAIR principles in viral sequence data research.
Q1: What are the quantifiable benefits of implementing FAIR data principles? Adopting FAIR data principles directly enhances research efficiency and economic performance. Implementing FAIR data can lead to significant cost savings; the lack of FAIR data is estimated to cost the European economy €10.2 billion annually, with potential further losses of €16 billion each year [6]. For research teams, FAIR data minimizes the time and work associated with transferring data between systems, reduces manual processing errors, and dramatically speeds up data handling [6]. These efficiencies streamline research processes, allowing scientists to spend less time gathering data and more time analyzing and interpreting results, which accelerates the pace of discovery [91].
Q2: What are the most common barriers to achieving FAIR compliance for viral sequence data? A systematic study identified the following as the most impactful barriers to FAIRification, many of which are highly relevant to sequence data management [92]:
- External barriers, such as organizational policy preventing the use of required software.
- Tooling challenges, including a lack of necessary software and databases.
- Technical hurdles, like a lack of guidelines and tooling for implementation.
- Resource limitations, including a lack of sustainable funding for implementation and long-term use.
- Expertise gaps, where teams lack specific knowledge on data, metadata, identifiers, and ontologies.
Q3: How can we balance open data access with fairness to data generators? This is a critical issue in genomics. A proposed solution is the use of a "Data Reuse Information (DRI) Tag" for datasets, linked to a researcher's ORCID identifier [93]. This tag unambiguously attributes the contribution and signals to others that they should make contact before reusing the data. This practice ensures that researchers who collect data are recognized and included in new projects, protecting their contribution while maintaining the principle of open access that is vital for rapid progress, as evidenced during the COVID-19 pandemic [93].
Q4: How do FAIR principles apply to research software used for analyzing viral sequences? Research software, including algorithms, scripts, and computational workflows, is fundamental to research and should also be made FAIR. The FAIR for Research Software (FAIR4RS) principles adapt the core concepts for software, requiring it to be [94]:
- Findable: Assigned a globally unique and persistent identifier and described with rich metadata.
- Accessible: Retrievable via standardized, open protocols.
- Interoperable: Able to read, write, and exchange data using community standards and including qualified references to other objects.
- Reusable: Clearly licensed, associated with detailed provenance, and meeting domain-relevant community standards.
Q5: Our team is new to FAIR. What is the first step we should take? The most important recommendation is to begin FAIRification early in a project and to engage a data steward [92] [95]. A data steward brings specialized knowledge in data governance, quality, and lifecycle management, which is invaluable for navigating the technical and organizational requirements of FAIR compliance [95]. Furthermore, incorporating FAIR considerations at the beginning of a project makes it easier to organize, document, and share data later, reducing the risk of data loss or inaccessibility [95].
Quantitative Impact of FAIR Data Implementation
The following table summarizes key metrics that demonstrate the impact of FAIR data on research efficiency and the costs associated with non-compliance.
| Metric Area | Key Finding | Context / Scope |
|---|---|---|
| Economic Impact | €10.2 billion annual cost | Estimated losses in the European economy due to a lack of FAIR data [6]. |
| Research Efficiency | 80% of scientists have spent effort to make their data more FAIR | Survey of researchers indicating widespread recognition of the principles' value and personal investment in implementation [92]. |
| Collaborative Potential | 45 unique barriers identified to FAIR implementation | A systematic study highlighting the complexity of the FAIRification process and the need for targeted resources [92]. |
Experimental Protocol: The FAIRification Workflow for Viral Sequence Data
This protocol outlines a systematic methodology for making viral sequence data FAIR-compliant, based on community best practices and the "Three-point FAIRification Framework" [1] [95].
1. Pre-Experimental Planning and Metadata Standardization
- Action: Before data generation, select and apply domain-specific metadata standards (e.g., from the Genomic Standards Consortium) and controlled vocabularies (e.g., EDAM Ontology, NCBI Taxonomy) to describe all aspects of the project [8] [95].
- Rationale: Using standardized metadata ensures data is described consistently, making it discoverable and interpretable by both humans and machines. This step is crucial for interoperability, allowing different systems and researchers to seamlessly integrate data [95].
2. Data Generation and Unique Identification
- Action: During the experiment, assign a unique and persistent identifier (PID), such as a Digital Object Identifier (DOI), to the dataset and its major components [6] [1]. For viral sequences, this also involves depositing data in public repositories like INSDC members (GenBank, ENA, DDBJ) which provide accessions.
- Rationale: Persistent identifiers are the cornerstone of findability. They ensure that data can be permanently located and cited, extending the data's longevity and utility beyond its original purpose [8].
3. Data Publication and Access Provision
- Action: Post-experiment, publish the data and its rich metadata in a trusted, searchable repository. Define and apply a clear usage license (e.g., Creative Commons) and describe the access protocol, which may include authentication and authorization for sensitive data [92] [95].
- Rationale: Explicit licensing facilitates legal reuse. Registering data in a searchable resource makes it findable, while a clear access protocol ensures it is accessible, even if under controlled conditions [1].
The workflow below visualizes this FAIRification process and its cyclical nature, emphasizing that reuse generates new data, continuing the FAIR cycle.
Troubleshooting Guide: Common FAIR Implementation Challenges
This guide addresses specific issues you might encounter during the FAIRification of viral sequence data and provides recommended solutions.
| Problem | Possible Cause | Solution | Reference |
|---|---|---|---|
| Data Fragmentation: Data is scattered across platforms and formats. | Non-standardized metadata; inconsistent data organization. | Utilize a FAIR-compliant Laboratory Information Management System (LIMS) and establish standard operating procedures for data organization from the project's start. | [6] |
| Limited Data Accessibility due to privacy concerns. | Misconception that FAIR equals "open data"; GDPR/compliance complexities. | Implement a federated analysis model where algorithms are sent to the data, or use a metadata-rich access portal that describes the authentication/authorization process required to access controlled data. | [92] |
| Interoperability Issues when integrating with other datasets. | Use of local, non-standardized file formats and vocabularies. | Adopt community-standard data models (e.g., OMOP CDM) and use formal, accessible languages and vocabularies for all data and metadata. | [92] [94] |
| Inadequate Documentation affecting data reusability. | Lack of detailed provenance and relevant attributes. | Assign a data steward to the team to ensure metadata includes detailed provenance, a clear license, and a plurality of accurate attributes. | [92] [95] |
| Unfair data reuse before original publishers can benefit. | Traditional 24-hour data release policies without attribution mechanisms. | Implement a "Data Reuse Information (DRI) Tag" linked to your ORCID to request collaboration and ensure attribution when your data is reused. | [93] |
The Scientist's Toolkit: Essential Reagents for FAIR Viral Data Research
The following table details key solutions and resources essential for conducting FAIR-compliant research on viral sequences.
| Item / Solution | Function in FAIR Viral Research |
|---|---|
| FAIR-Compliant LIMS (e.g., Labbit) | A Laboratory Information Management System built on FAIR principles to ensure effortless data integration, improved consistency, and flexible querying from the start of a project [6]. |
| Persistent Identifier Services (e.g., DOI, SWHID) | Provides a globally unique and permanent identifier for your dataset, software, or other digital objects, making them findable and citable over the long term [94]. |
| Data Reuse Information (DRI) Tag | A tag linked to a researcher's ORCID that is attached to a dataset to ensure fair attribution and encourage collaboration before data reuse [93]. |
| Common Data Models (e.g., OMOP CDM) | A standardized data model that ensures semantic and syntactic interoperability, allowing data from different sources to be harmonized and analyzed together [92]. |
| Trusted Data Repositories (e.g., INSDC, Zenodo) | A searchable resource that stores data and metadata, provides persistent identifiers, and ensures long-term preservation and accessibility [8] [94]. |
Protocol for Equitable Data Reuse in Viral Genomics
This protocol, derived from an international consortium's roadmap, establishes a fair process for reusing publicly shared viral sequence data [93].
1. Check for a Data Reuse Information (DRI) Tag
- Before reusing a public dataset, check its metadata for a DRI Tag linked to the data contributor's ORCID identifier.
2. Interpret the Tag and Act Accordingly
- If a DRI Tag is present: This is a signal to contact the data contributor(s) before reusing the data. Initiate a dialogue to discuss potential collaboration and ensure their contribution is recognized.
- If a DRI Tag is absent: The data can be considered freely reusable without an obligation to contact the contributor, following the repository's specified license.
3. Acknowledge and Collaborate
- When reusing data, ensure the original contributors are fairly acknowledged. If the reuse leads to a publication, involve them as collaborators or cite their data publication appropriately.
The logic for this equitable reuse protocol is summarized in the following diagram:
Conclusion
The implementation of FAIR principles for viral sequence data represents a fundamental shift toward more efficient, collaborative, and impactful virology research. By establishing robust foundational frameworks, applying systematic methodological approaches, proactively addressing implementation challenges, and rigorously validating outcomes through comparative assessment, the scientific community can unlock the full potential of viral genomic data. Future progress will depend on sustained investment in technical infrastructure, development of specialized data standards, cultivation of FAIR-literate organizational cultures, and closer alignment between data management practices and regulatory requirements. As viral threats continue to evolve, FAIR-compliant data ecosystems will be crucial for accelerating therapeutic discovery, enhancing surveillance capabilities, and ultimately safeguarding global health against emerging pathogens.
References
- 1. FAIR Principles [https://www.go-fair.org/fair-principles/]
- 2. The FAIR Guiding Principles for scientific data ... [https://www.nature.com/articles/sdata201618]
- 3. FAIR data principles: What you need to know [https://tiledb.com/blog/fair-data-principles-explained]
- 4. FAIR principles to improve the impact on health research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10189186/]
- 5. FAIR Principles [https://gisaid.org/help/fair-principles/]
- 6. Applying FAIR Principles to Lab Data: Six Challenges You ... [https://bioit.semaphoresolutions.com/applying-fair-principles-to-lab-data/]
- 7. FAIR data principles - National Library of Medicine [https://www.nlm.nih.gov/oet/ed/cde/tutorial/02-200.html]
- 8. A practical guide to FAIR data management in the age of multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788310/]
- 9. Fair Rules for Sharing Sequence Data [https://www.uni-due.de/2025-09-26-fair-use-of-public-secencing-data-nature-microbiology]
- 10. Framework to Track and Correlate Viral Genome Sequences ... [https://www.ncbi.nlm.nih.gov/books/NBK562769/]
- 11. An Update on RNA Virus Discovery: Current Challenges and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300815/]
- 12. Good practices for FAIR data management [https://www.rug.nl/library/open-access/blog/good-practices-for-fair-data-management-an-interview-with-sebastian-lequime-on-fair-challenges-in?lang=en]
- 13. A New Tool to Detect Viruses in Sequence Data [https://www.bbe.caltech.edu/news/a-new-tool-to-detect-viruses-in-sequence-data]
- 14. Top 10 Bioinformatics Tools in 2025: Features, Pros, Cons ... [https://www.cotocus.com/blog/top-10-bioinformatics-tools-in-2025-features-pros-cons-comparison/]
- 15. The 2025 Bioinformatics Toolkit: From Sample Prep to AI- ... [https://blog.omni-inc.com/blog/the-2025-bioinformatics-toolkit-from-sample-prep-to-ai-driven-analysis]
- 16. Troubleshooting SRA submission in the SRA ... - NCBI [https://www.ncbi.nlm.nih.gov/sra/docs/submitspfiles]
- 17. Frequently asked questions - NCBI - NIH [https://www.ncbi.nlm.nih.gov/sra/docs/submitquestions]
- 18. Benchmarking bioinformatic virus identification tools using ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03236-4]
- 19. Improving the reporting of metagenomic virome-scale data [https://www.nature.com/articles/s42003-024-07212-3]
- 20. Making Submission in SRA Submission Portal - NCBI - NIH [https://www.ncbi.nlm.nih.gov/sra/docs/submitportal/]
- 21. HowTo: Access SRA Data · ncbi/sra-tools Wiki [https://github.com/ncbi/sra-tools/wiki/HowTo:-Access-SRA-Data]
- 22. Efficient and accurate detection of viral sequences at single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10760059/]
- 23. FAIR in action - a flexible framework to guide FAIRification [https://www.nature.com/articles/s41597-023-02167-2]
- 24. Applying the FAIR principles to data in a hospital: challenges ... [https://jbiomedsem.biomedcentral.com/articles/10.1186/s13326-022-00263-7]
- 25. Implementing Findable, Accessible, Interoperable, Reusable ... [https://mental.jmir.org/2024/1/e59113]
- 26. Interoperability: COVID-19 as an Impetus for Change - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7929044/]
- 27. First steps towards data FAIRification in COVID-19 research [https://www.zonmw.nl/en/article/first-steps-towards-data-fairification-covid-19-research]
- 28. FAIR, ethical, and coordinated data sharing for COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10552001/]
- 29. COVID-19-related research data availability and quality ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0313991]
- 30. FAIRification Workflow - FAIR Toolkit - Pistoia Alliance [https://fairtoolkit.pistoiaalliance.org/methods/fairification-workflow/]
- 31. FAIR+E pathogen data for surveillance and research [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1289945/full]
- 32. Framework for responsible sharing of genomic and health- ... [https://www.ga4gh.org/framework/]
- 33. A framework for FAIRification processes [https://fairplus.github.io/the-fair-cookbook/content/recipes/introduction/fairification-process.html]
- 34. Annotate, prepare tests and publish Galaxy workflows in ... [https://training.galaxyproject.org/training-material/topics/galaxy-interface/tutorials/workflow-fairification/tutorial.html]
- 35. Persistent identifiers - Digital Preservation Handbook [https://www.dpconline.org/handbook/technical-solutions-and-tools/persistent-identifiers]
- 36. Persistent identifiers: the building blocks of the research ... [https://insights.uksg.org/articles/10.1629/uksg.457]
- 37. A roadmap for equitable reuse of public microbiome data [https://www.nature.com/articles/s41564-025-02116-2]
- 38. FAIR principles for Research - Data Management for Research [https://guides.library.cmu.edu/researchdatamanagement/FAIR_principles]
- 39. The National Center for Biomedical Ontology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3277625/]
- 40. 6.3. Deploying the EBI OLS [https://fairplus.github.io/the-fair-cookbook/content/recipes/infrastructure/vocabularies/UC3_R13_local_ontology_services.html]
- 41. Opportunities and Challenges of Data-Driven Virus Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC9406072/]
- 42. Data-driven recombination detection in viral genomes [https://www.nature.com/articles/s41467-024-47464-5]
- 43. NCBI Virus Help Documentation - NIH [https://www.ncbi.nlm.nih.gov/labs/virus/vssi/docs/help/]
- 44. Selection of data sets for FAIRification in drug discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9236643/]
- 45. A Guide to the FAIR Principles in Biopharma [https://frontlinegenomics.com/a-guide-to-the-fair-principles-in-biopharma/]
- 46. FAIR Data Principles: Benefits, Challenges & FAQs [https://zontal.io/fair-data-principles/]
- 47. ENABLING FAIR DATA – FAQS [https://copdess.org/enabling-fair-data-project/enabling-fair-data-faqs/]
- 48. Ten quick tips for building FAIR workflows - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10538699/]
- 49. Nextstrain [https://nextstrain.org/]
- 50. Towards a FAIRer World: Implementing the UNESCO ... [https://www.ouvrirlascience.fr/towards-a-fairer-world-implementing-the-unesco-recommendation-on-open-science-to-address-global-challenges-2/]
- 51. Perceptual and technical barriers in sharing and formatting ... [https://www.sciencedirect.com/science/article/pii/S2666979X25001016]
- 52. Ten common issues with reference sequence databases ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2024.1278228/full]
- 53. Metadata integrity in bioinformatics: Bridging the gap ... [https://www.sciencedirect.com/science/article/pii/S2001037023003616]
- 54. A Comprehensive Review of Current Virus Databases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10537806/]
- 55. Data description: FAIR data [https://www.infectious-diseases-toolkit.org/data-description/fair-data]
- 56. Submit Sequences | NCBI Virus - NIH [https://www.ncbi.nlm.nih.gov/labs/virus/vssi/docs/submit/]
- 57. Virus Metadata Resource (VMR) [https://ictv.global/vmr]
- 58. Comparative analyses of error handling strategies for next- ... [https://www.nature.com/articles/s41598-020-62675-8]
- 59. HIPAA vs. GDPR Compliance: What's the Difference? | Blog [https://www.onetrust.com/blog/hipaa-vs-gdpr-compliance/]
- 60. GDPR vs HIPAA - What are the differences and how to ... [https://www.iubenda.com/en/help/22623-gdpr-vs-hipaa]
- 61. FAIR assessment tools [https://fair-impact.eu/fair-assessment-tools]
- 62. An automated solution for measuring the progress toward ... [https://www.sciencedirect.com/science/article/pii/S2666389921002324]
- 63. Making Your Research Data FAIR with OSF: A Practical ... [https://www.cos.io/blog/making-research-data-fair]
- 64. Data Champions | Research Data Management [https://www.data.cam.ac.uk/data-champions]
- 65. The FAIR Assessment Conundrum: Reflections on Tools and ... [https://datascience.codata.org/articles/10.5334/dsj-2024-033]
- 66. FAIR Training Program 2025 - 2027 Part 1 opens registration [https://erdera.org/news/fair-training-program-2025-2027-part-1-opens-registration/]
- 67. Empowering the next generation of Data Stewards: Join ... [http://www.openaire.eu/community/blogs/empowering-the-next-generation-of-data-stewards-join-the-fair-rdm-bootcamp]
- 68. Cost-Benefit Analysis: A Quick Guide with Examples and ... [https://www.projectmanager.com/blog/cost-benefit-analysis-for-projects-a-step-by-step-guide]
- 69. What Is Cost-Benefit Analysis? 4 Step Process - HBS Online [https://online.hbs.edu/blog/post/cost-benefit-analysis]
- 70. Cost-Benefit Analysis test - Requirements Prioritization ... [https://trustedinstitute.com/concept/pmi-pba/requirements-prioritization-techniques/cost-benefit-analysis/]
- 71. Unrestricted Versus Regulated Open Data Governance [https://datascience.codata.org/articles/10.5334/dsj-2024-029]
- 72. Standards for Sequencing Viral Genomes in the Era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4068259/]
- 73. Viral genome sequencing methods: benefits and pitfalls ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11346438/]
- 74. 5 Steps to Follow for Troubleshooting Experiments [https://blog.edvotek.com/2022/06/21/5-steps-to-follow-for-troubleshooting-experiments/]
- 75. FAIRshake: Toolkit to Evaluate the FAIRness of Research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7316196/]
- 76. Understanding FAIR vs Open Data in Life Sciences [https://ranchobiosciences.com/2025/01/unlocking-data-potential-understanding-fair-vs-open-data-in-life-sciences/]
- 77. Virus Outbreak Data Network (VODAN) [https://www.go-fair.org/implementation-networks/overview/vodan/]
- 78. A Comprehensive Review of Current Virus Databases [https://www.mdpi.com/1999-4915/15/9/1834]
- 79. Troubleshoot common issues — SARS-CoV-2 Workflow ... [https://docs.nextstrain.org/projects/ncov/en/latest/reference/troubleshoot.html]
- 80. Troubleshooting Your First NGS Dataset [https://genomebeans.com/blog/troubleshooting-your-first-ngs-dataset-how-genomebeans-simplifies-it]
- 81. Real-World Evidence [https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence]
- 82. FDA use of Real-World Evidence in Regulatory Decision ... [https://www.fda.gov/science-research/real-world-evidence/fda-use-real-world-evidence-regulatory-decision-making]
- 83. CBER and CDER Real-World Evidence (RWE) [https://www.fda.gov/science-research/real-world-evidence/center-biologics-evaluation-and-research-center-drug-evaluation-and-research-real-world-evidence]
- 84. FDA Publishes New Draft Guidance on Regenerative ... [https://www.hklaw.com/en/insights/publications/2025/10/fda-publishes-new-draft-guidance-on-regenerative-medicine-therapies]
- 85. Survival of the greenest: environmental sustainability and ... [https://www.frontiersin.org/journals/organizational-psychology/articles/10.3389/forgp.2025.1521537/full]
- 86. Project Longevity → Area [https://lifestyle.sustainability-directory.com/area/project-longevity/]
- 87. Community Trust Index [https://trust.communityengagementhub.org/]
- 88. Community Data Trust → Term [https://lifestyle.sustainability-directory.com/term/community-data-trust/]
- 89. Toward security-aware portable sequencing [https://www.nature.com/articles/s41467-025-66024-z]
- 90. Evaluating households' community participation: Does ... [https://www.frontiersin.org/journals/environmental-science/articles/10.3389/fenvs.2022.951262/full]
- 91. FAIR Data: Transforming the life sciences industry with ... [https://www.ontoforce.com/whitepaper/transforming-the-life-sciences-industry-with-fair-data]
- 92. Implementing Findable, Accessible, Interoperable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11683739/]
- 93. Fair Rules for Sharing Sequence Data [https://www.rna-seqblog.com/fair-rules-for-sharing-sequence-data/]
- 94. Introducing the FAIR Principles for research software [https://www.nature.com/articles/s41597-022-01710-x]
- 95. A Guide to the FAIR Principles [https://www.openscience.eu/article/infrastructure/guide-fair-principles]