Comparative Analysis of Molecular Methods for SARS-CoV-2 Detection: From RT-qPCR and LAMP to NGS and Antigen Tests
This article provides a comprehensive comparative analysis of molecular diagnostic methods for SARS-CoV-2, tailored for researchers, scientists, and drug development professionals.
Comparative Analysis of Molecular Methods for SARS-CoV-2 Detection: From RT-qPCR and LAMP to NGS and Antigen Tests
Abstract
This article provides a comprehensive comparative analysis of molecular diagnostic methods for SARS-CoV-2, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of major testing platforms including RT-qPCR, RT-LAMP, rapid antigen tests, and next-generation sequencing. The scope encompasses methodological applications across clinical and research settings, troubleshooting for optimization, and rigorous validation frameworks according to international standards. By synthesizing recent performance data on sensitivity, specificity, variant detection capability, and operational requirements, this review serves as a critical resource for selecting appropriate methodologies for specific applications from clinical diagnosis to genomic surveillance.
Fundamental Principles and Evolving Landscape of SARS-CoV-2 Molecular Diagnostics
The emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in late 2019 initiated a global health crisis, making accurate and reliable diagnostic testing a cornerstone of pandemic control efforts [1]. SARS-CoV-2 is a positive-sense, single-stranded RNA virus with a genome approximately 30 kilobases in length, encoding both structural and non-structural proteins critical for its replication and pathogenesis [2] [1]. Among molecular diagnostics, reverse transcription quantitative polymerase chain reaction (RT-qPCR) has emerged as the undisputed gold standard for detecting SARS-CoV-2 RNA in clinical specimens due to its superior sensitivity and specificity [3] [1] [4]. This method allows for the direct detection of viral genetic material, enabling identification of infected individuals even during the pre-symptomatic phase.
The reliability of RT-qPCR diagnostics fundamentally depends on the selection of appropriate viral gene targets. The most frequently targeted genes in SARS-CoV-2 detection assays are the envelope (E), nucleocapsid (N), RNA-dependent RNA polymerase (RdRP), and spike (S) genes [3] [1]. Each target offers distinct advantages and limitations concerning conservation, abundance, and specificity, influencing the overall performance of diagnostic assays. This review provides a comprehensive comparative analysis of RT-qPCR methodologies and target gene selection, synthesizing experimental data from multiple studies to guide researchers and clinicians in optimizing SARS-CoV-2 detection strategies.
Comparative Analysis of SARS-CoV-2 Target Genes
The design of effective RT-qPCR assays requires careful consideration of the targeted genomic regions. The ideal target combines high analytical sensitivity with robust specificity for SARS-CoV-2 while remaining conserved across emerging variants. The four primary targets—E, N, RdRP, and S genes—serve different biological functions and exhibit varying degrees of conservation.
The RdRP gene, located within the ORF1ab region, encodes the RNA-dependent RNA polymerase, a critical non-structural protein responsible for viral RNA replication [5] [6]. As an essential component of the replication machinery, this gene is highly conserved among coronaviruses, though specific primer sets can be designed for SARS-CoV-2 specificity [6]. Studies have demonstrated that assays targeting RdRP exhibit some of the highest analytical sensitivities available [6]. The N gene, which encodes the nucleocapsid protein that packages viral RNA, is abundantly expressed during infection, potentially enhancing detection sensitivity [3] [1]. This combination of conservation and abundance makes it a reliable target, though some studies have noted that its sensitivity may be slightly inferior to RdRP in certain assay configurations [7].
The E gene, encoding the small envelope protein, is considered the most sensitive target for detecting SARS-CoV-2 and related beta-coronaviruses [8]. However, this broader reactivity can reduce specificity for SARS-CoV-2 exclusively, potentially leading to cross-reaction with other coronaviruses [3]. Consequently, the E gene often serves as an initial screening target, with positive results requiring confirmation by more specific targets. The S gene, which codes for the spike protein mediating host cell entry, has been particularly affected by mutations in variants of concern, compromising detection in some commercial assays [4]. This susceptibility to genetic drift makes it a less reliable single target but valuable for monitoring specific variants.
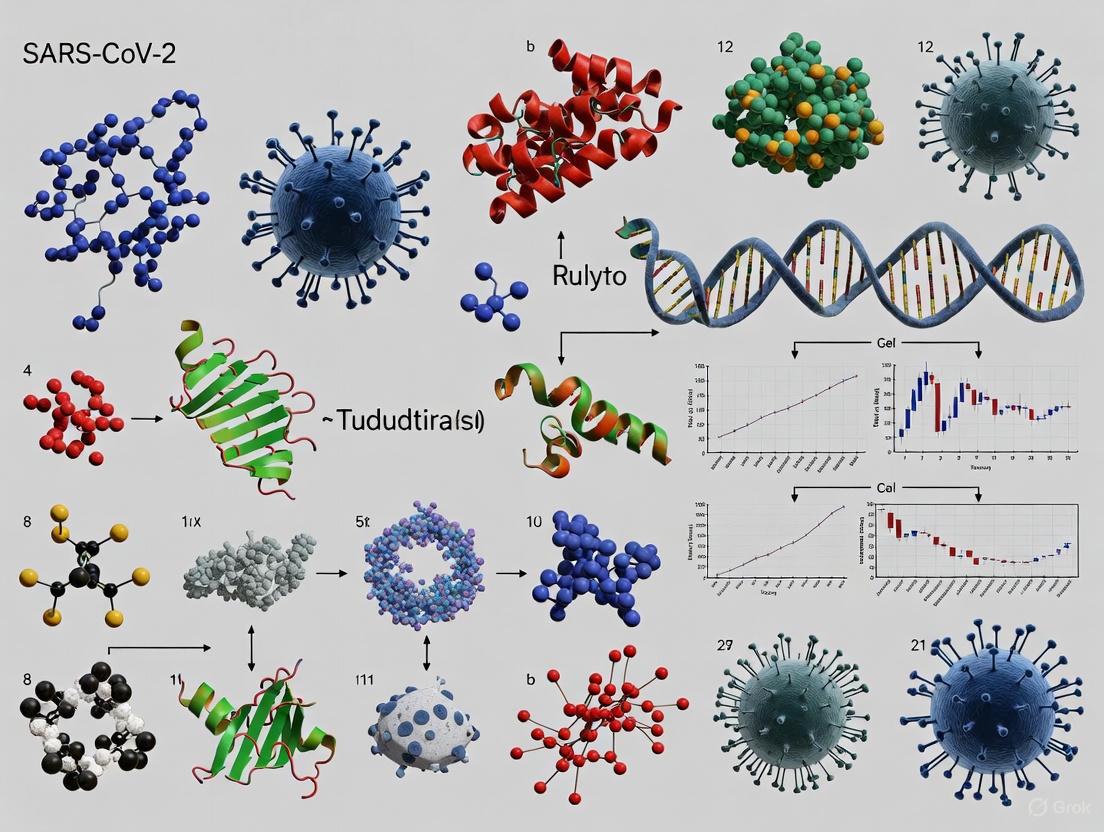
Figure 1: SARS-CoV-2 Target Gene Characteristics. This diagram illustrates the four primary gene targets used in RT-qPCR detection, their genomic classification, and key performance characteristics based on experimental data.
Performance Characteristics of Target Genes
Table 1: Comparison of SARS-CoV-2 RT-qPCR Target Genes
| Target Gene | Sensitivity | Specificity | Conservation | Primary Applications | Key Limitations |
|---|---|---|---|---|---|
| RdRP | High (LOD: 0.81-35.13 copies/μL) [7] [6] | High (SARS-CoV-2 specific) [6] | High (essential replication enzyme) [5] | Primary detection, confirmation [6] | Complex primer design due to conserved regions [6] |
| N | High (LOD: 0.81-20.31 copies/reaction) [7] [6] | High (SARS-CoV-2 specific) [6] | Moderate (subject to variations) [4] | Primary detection, screening [3] | Potential sensitivity reduction in variants [4] |
| E | Very High (excellent sensitivity) [8] | Moderate (cross-reacts with other β-coronaviruses) [3] [8] | Moderate | Initial screening [8] | Requires confirmatory testing with specific targets [8] |
| S | Variable | High (SARS-CoV-2 specific) | Low (frequent mutations in VOCs) [4] | Variant monitoring [4] | Reduced detection in variants due to mutations [4] |
Comparative Performance of Commercial RT-qPCR Kits
Multiple studies have systematically evaluated the performance of commercially available RT-qPCR kits, revealing significant differences in sensitivity, cost, and reliability. These comparative analyses are essential for laboratories to select appropriate testing platforms based on their specific needs and resources.
Analytical Sensitivity and Detection Limits
Independent validation studies have demonstrated substantial variation in the limit of detection (LOD) across different commercial kits. A 2023 comprehensive evaluation of three widely used tests revealed that the Liferiver and TaqPath kits both achieved an LOD of 10 viral RNA copies per reaction, while the Vitassay kit showed a slightly higher LOD of 100 viral RNA copies per reaction [4]. Importantly, this study noted that mean Ct values at low viral concentrations (10 copies/reaction) were significantly lower than the cutoff values declared by manufacturers, highlighting the importance of internal validation rather than relying solely on manufacturer claims [4].
A separate comparison of the BGI and Norgen Biotek systems found that the BGI detection system provided overall superior performance with lower detection limits and lower Ct values, generating comparable results to original clinical diagnostic data [2] [9]. The BGI system effectively identified samples across a wide dynamic range, from 65 copies to 2.1 × 10⁵ copies of viral genome/μl [2]. Meanwhile, the Norgen system, while more cost-effective, accurately detected only samples with clinical Ct values < 33-34, indicating reduced sensitivity for low viral loads [2] [9].
Diagnostic Accuracy and Clinical Performance
Clinical performance evaluations have revealed concerning variability in sensitivity among commercial kits. A study evaluating the AccuPower SARS-CoV-2 Real Time RT-PCR Kit (Bioneer, South Korea) reported a sensitivity of only 78.9% compared to the CDC EUA kit gold standard, with an estimated limit of detection higher than 40,000 viral RNA copies/mL [8]. This poor performance was particularly notable for samples with low to moderate viral loads, potentially missing more than 20% of true positive cases in surveillance programs [8].
In contrast, a 2021 comparison of Sansure Biotech, GeneFinder, and TaqPath kits found no statistically significant differences in their final results (p = 0.107), with all three demonstrating strong positive association and high Cohen's κ coefficient [3]. However, significant differences emerged in average Ct values for ORF1ab and N gene amplification (p < 0.001), with Sansure Biotech showing slightly better diagnostic performance overall [3].
Table 2: Performance Comparison of Commercial SARS-CoV-2 RT-qPCR Kits
| Kit Name | Target Genes | Limit of Detection | Clinical Sensitivity | Advantages | Limitations |
|---|---|---|---|---|---|
| BGI | Orf1ab, Actin (human control) [2] | 65 copies/μl [2] | High (matches clinical diagnosis) [2] | Superior sensitivity, low Ct values [2] | Higher cost, less flexible [2] |
| TaqPath (Thermo Fisher) | ORF1ab, N, S [4] | 10 viral RNA copies/reaction [4] | High [3] [4] | Multi-target design, reliable detection [3] [4] | S gene target dropout in variants [4] |
| Norgen Biotek | N (CDC N1 & N2), RNase P [2] | Detects samples with Ct < 33 [2] | Moderate (78.4% for direct detection) [2] | Significant cost savings [2] | Reduced sensitivity for low viral loads [2] |
| Liferiver | ORF1ab, N, E [4] | 10 viral RNA copies/reaction [4] | High [4] | Reliable performance, internal control [4] | - |
| Sansure Biotech | ORF1ab, N [3] | 200 copies/mL [3] | High (better diagnostic performance) [3] | Good sensitivity, reliable results [3] | - |
| AccuPower (Bioneer) | RdRP, E, IPC [8] | >40,000 copies/mL [8] | Low (78.9%) [8] | - | Poor sensitivity, no RNA quality control [8] |
Advanced Methodologies: Direct Detection and Multiplex Assays
Extraction-Free Direct Detection Methods
Direct RT-qPCR methods that bypass RNA extraction have emerged as promising alternatives to increase testing throughput and reduce costs, particularly during supply chain shortages. These approaches detect viral RNA directly from patient samples without prior nucleic acid purification. Research has demonstrated that simply adding an RNase inhibitor to direct reactions significantly improved detection, without requiring additional treatments like lysis buffers or boiling [2] [9]. The best direct methods detected approximately 10-fold less virus than conventional indirect methods with RNA extraction, but this simplified approach substantially reduced sample handling, assay time, and cost [2] [9].
The BGI system has shown particular utility for direct, extraction-free analysis, providing 78.4% sensitivity compared to standard methods [2] [9]. This approach maintained detection capability while offering significant operational advantages, making it valuable for high-throughput screening scenarios where ultimate sensitivity may be sacrificed for efficiency and resource conservation.
Multiplex RT-qPCR Assay Design
Multiplex RT-qPCR assays that simultaneously detect multiple viral targets alongside human internal controls have demonstrated enhanced diagnostic reliability. One optimized multiplex method targeting viral N, RdRP, and human RP genes achieved 100% positive percent agreement with clinical samples, with LOD values of 1.40 and 0.81 copies/μL for RdRP and N genes, respectively [6]. This approach improves detection probability in patients with low viral loads and incorporates internal controls to prevent false-negative results due to inefficient sampling or PCR inhibition [6].
The design of effective multiplex assays requires careful primer and probe selection to avoid secondary structures such as homo-dimers, hetero-dimers, and hairpins that reduce amplification efficiency [6]. Successful implementations utilize distinct fluorescent dyes for each target (e.g., FAM for RdRP, HEX for N, ROX for RP) and optimized reaction conditions to maintain sensitivity across all targets [6].
Figure 2: RT-qPCR Workflow: Direct vs. Indirect Methods. This diagram compares the standard indirect method requiring RNA extraction with the direct detection approach, highlighting key advantages of each methodology.
Research Reagent Solutions and Experimental Protocols
Essential Research Reagents
Table 3: Key Research Reagent Solutions for SARS-CoV-2 RT-qPCR
| Reagent Category | Specific Examples | Function/Application | Performance Notes |
|---|---|---|---|
| RNA Extraction Kits | Qiagen RNeasy, Invitrogen Purelink, BGI Magnetic Bead, Norgen Biotek Total RNA [2] | Isolation of high-quality viral RNA from clinical specimens | Most procedures performed similarly in comparative studies [2] |
| RT-qPCR Master Mixes | One-step RT-qPCR Master mix (Solis BioDyne) [7], NEB Luna Universal One-Step Kit [2] | Combined reverse transcription and PCR amplification | SYBR green approaches exhibited reduced specificity vs. TaqMan [2] |
| Positive Controls | Synthetic Positive Template (SPT) oligonucleotides [7], Quantitative Synthetic SARS-CoV-2 RNA [4] | Assay validation, sensitivity determination | SPT controls reduce false-positive risk from contamination [7] |
| Internal Controls | RNase P (human gene) [2] [6], MS2 phage [4] | Monitoring RNA extraction efficiency, PCR inhibition | Essential for distinguishing true negatives from assay failures [2] |
| Primer/Probe Sets | CDC N1/N2, Charité/Berlin protocol, custom designs [7] [6] | Target-specific amplification and detection | Multiplex designs require careful optimization to avoid dimer formation [6] |
Detailed Experimental Protocol: Multiplex RT-qPCR Detection
Based on optimized methodologies from recent studies, the following protocol enables reliable detection of SARS-CoV-2 through multiplex RT-qPCR:
Sample Preparation and RNA Extraction:
- Collect nasopharyngeal or oropharyngeal swabs and place in viral transport medium (VTM)
- Extract RNA using approved magnetic bead-based or column-based methods (e.g., Magna Pure Compact, Roche or ELITe InGenius systems) [6]
- Use input volumes of 100-400 μL with elution volumes of 32-100 μL [2] [6]
- Include internal control (e.g., RNase P) to monitor extraction efficiency [2]
Multiplex RT-PCR Reaction Setup:
- Prepare reaction mixture containing:
- Use distinct fluorescent dyes for different targets (FAM for RdRP, HEX for N, ROX for RP) [6]
- Include positive and negative controls in each run [4]
Amplification Conditions:
- Reverse transcription: 15-30 minutes at 45-50°C [3] [6]
- Initial denaturation: 2-3 minutes at 95°C [3]
- 40-45 cycles of:
- Data collection during annealing/extension phase
Result Interpretation:
- Analyze amplification curves and Ct values
- Use predetermined cutoff values (e.g., Ct ≤37-40 for positive result) [2] [4]
- Interpret based on multi-target detection patterns
- Verify internal control amplification to validate negative results
The comparative analysis of RT-qPCR methodologies for SARS-CoV-2 detection reveals a complex landscape where target selection, assay design, and commercial kit choice significantly impact diagnostic performance. The RdRP and N genes emerge as the most reliable targets, offering an optimal balance of sensitivity and specificity, while the E gene serves as a sensitive screening target and the S gene provides utility for variant monitoring. Among commercial platforms, significant variability exists, with BGI and TaqPath systems demonstrating superior sensitivity, while other kits offer cost-effective alternatives with moderate performance compromises.
The emergence of direct detection methods and optimized multiplex assays represents significant advancements, addressing needs for increased throughput and enhanced reliability. These methodologies, combined with careful internal validation of commercial tests, enable laboratories to implement robust SARS-CoV-2 detection pipelines tailored to their specific requirements and resources. As the virus continues to evolve, ongoing evaluation of primer compatibility with emerging variants remains essential for maintaining diagnostic accuracy, reinforcing the need for flexible, multi-target detection strategies in SARS-CoV-2 research and clinical diagnostics.
The COVID-19 pandemic has underscored the critical need for rapid, reliable, and accessible molecular diagnostic methods. Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP) has emerged as a powerful alternative to the gold standard Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR), particularly in resource-limited settings [10]. This guide provides a comparative analysis of these technologies, focusing on their principles, performance characteristics, and implementation requirements to inform researchers, scientists, and drug development professionals in their selection of appropriate molecular methods for SARS-CoV-2 research and diagnostics.
RT-LAMP is a nucleic acid amplification technique that operates at a constant temperature, typically 60-65°C, eliminating the need for thermal cyclers required in PCR-based methods [10]. The technique utilizes a DNA polymerase with high strand displacement activity and specifically designed primer sets to amplify target RNA sequences after an initial reverse transcription step. The amplification products can be detected through various methods including turbidity, colorimetric changes, or fluorescence, often in less than 30 minutes [11] [12].
Principles of RT-LAMP Technology
Molecular Mechanism
The RT-LAMP reaction employs four to six primers that recognize six to eight distinct regions on the target DNA, ensuring high specificity [13]. The core primer set consists of:
- Forward and Backward Outer Primers (F3 and B3): Initiate the reaction
- Forward and Backward Inner Primers (FIP and BIP): Contain complementary sequences that form loop structures for continuous amplification
- Loop Primers (LF and LB): Optional primers that accelerate reaction kinetics by binding to loop regions [14]
This multi-primer system enables a cyclic amplification process involving strand displacement DNA synthesis that generates stem-loop DNA structures with multiple inverted repeats of the target. These structures then serve as templates for subsequent amplification rounds, leading to exponential DNA amplification under isothermal conditions [14].
Detection Methods
Various detection strategies have been developed for RT-LAMP:
Colorimetric Detection: Utilizes pH-sensitive dyes that change color as amplification progresses due to pyrophosphate ion release and subsequent pH drop in the reaction mixture [10] [12].
Turbidity Measurement: Monitors white magnesium pyrophosphate precipitate formation, which increases turbidity proportional to amplified DNA [14].
Fluorescent Detection: Employs intercalating dyes or sequence-specific molecular beacons that fluoresce when bound to double-stranded DNA [15] [11].
Molecular Beacons: Structured oligonucleotide probes with fluorophore and quencher that separate upon binding to specific sequences, increasing fluorescence with high specificity [15].
The following diagram illustrates the core RT-LAMP workflow and detection mechanisms:
Comparative Performance Analysis
Diagnostic Accuracy in Clinical Settings
Multiple clinical studies have validated RT-LAMP performance against RT-qPCR across diverse geographical settings:
Table 1: Diagnostic Performance of RT-LAMP Compared to RT-qPCR
| Study Characteristics | Sensitivity | Specificity | Sample Type | Viral Load Dependency |
|---|---|---|---|---|
| Multicenter study (Cameroon, Ethiopia, Kenya, Nigeria, Italy) [10] | 87% (overall)97% (Ct < 35) | 98% | Pharyngeal swabs | Highly dependent on viral load |
| Japanese hospital study (disease timeline) [16] | 100% (≤9 days after onset)25% (≥10 days after onset) | 100% | Nasopharyngeal swabs | Strong time-dependent performance |
| Iranian clinical evaluation [13] | 93% agreement (saliva)94% agreement (nasopharynx) | 93% agreement (saliva)94% agreement (nasopharynx) | Saliva & nasopharyngeal | Consistent across sample types |
| Indonesian hospital study [12] | 65.5% (overall)73.2% (3-7 days post-onset) | 100% | Saliva | Optimal in early symptomatic phase |
Limit of Detection and Dynamic Range
Analytical sensitivity studies demonstrate RT-LAMP's capability to detect low viral concentrations:
Table 2: Analytical Sensitivity of RT-LAMP Assays
| Study | Limit of Detection (LOD) | Dynamic Range | Target Genes |
|---|---|---|---|
| RT-LAMP-MS assay [11] | 10-1 PFU mL-1 | 103 to 10-1 PFU mL-1 | RdRP gene |
| Japanese clinical evaluation [16] | 6.7 copies/reaction | Not specified | Not specified |
| Indonesian saliva study [12] | 50 copies/μL | Not specified | Not specified |
Experimental Protocols
Standard RT-LAMP Workflow
A typical RT-LAMP protocol for SARS-CoV-2 detection involves these critical steps:
Sample Collection and Processing:
- Collect nasopharyngeal, saliva, or other respiratory specimens [13] [12]
- For saliva: participants should refrain from eating, drinking, or smoking for 1 hour before collection [12]
- Heat inactivation at 65°C for 15 minutes to ensure biosafety [12]
RNA Extraction:
- Use commercial RNA extraction kits (e.g., QIAamp Viral RNA Mini Kit) [16]
- Automated extraction systems (e.g., QIAcube) can standardize the process [16]
- Evaluate RNA purity spectrophotometrically (260/280 ratio ~2.0) [13]
Reaction Setup:
- Prepare 25μL reaction mixture containing:
- Add detection reagents (colorimetric dye, fluorescent probes, or molecular beacons as required) [15]
Amplification and Detection:
- Incubate at 62-65°C for 20-40 minutes [11] [13]
- Monitor amplification in real-time using turbidimetry, fluorescence, or visual color change [15] [12]
- Interpret results: color change from pink to yellow (colorimetric) or increased turbidity/fluorescence indicates positive amplification [12]
The following workflow details the specific steps for molecular beacon-enhanced RT-LAMP:
Research Reagent Solutions
Table 3: Essential Reagents for RT-LAMP Experiments
| Reagent/Component | Function | Implementation Example |
|---|---|---|
| Bst DNA Polymerase | Strand-displacing DNA polymerase for isothermal amplification | Commercial kits (e.g., Loopamp kit, New England Biolabs Bst polymerase) [13] [14] |
| Reverse Transcriptase | Converts RNA template to cDNA | AMV Reverse Transcriptase (200 U/reaction) [14] |
| LAMP Primers | Target-specific amplification | Designed using Primer Explorer V5; 4-6 primers targeting 6-8 regions of SARS-CoV-2 genes (ORF1ab, N, E, RdRP) [13] [14] |
| Molecular Beacons | Sequence-specific detection with fluorophore-quencher pairs | Locked nucleic acid-modified beacons for enhanced temperature stability [15] |
| Reaction Buffer | Optimal enzymatic activity | Contains MgSO₄, betaine, dNTPs, KCl in Tris-HCl buffer [14] |
| Detection Reagents | Visual or fluorescent signal generation | Calcein (colorimetric), SYBR Green (fluorescent), or magnesium pyrophosphate (turbidity) [11] [14] |
Advantages and Limitations in Research Applications
Technical Advantages
RT-LAMP offers several compelling advantages for SARS-CoV-2 research:
Operational Simplicity: Eliminates need for sophisticated thermal cyclers; reactions proceed at constant temperatures (typically 65°C) using simple heating blocks or water baths [10]. This significantly reduces equipment costs and operational complexity compared to RT-qPCR.
Rapid Results: Amplification and detection typically completed within 30-40 minutes, substantially faster than conventional RT-qPCR protocols which often require 1.5-2 hours [11] [12].
Robust Detection Methods: Multiple readout options including colorimetric (visible to naked eye), turbidity, or fluorescence enable flexibility for different laboratory settings [15] [12].
Sample Compatibility: Works effectively with various sample types including saliva, nasopharyngeal swabs, and other respiratory specimens without requiring complex processing [13] [12].
Performance Considerations
Sensitivity Profile: While RT-LAMP demonstrates excellent sensitivity for medium to high viral loads (Ct < 35), its performance decreases with lower viral concentrations, making it particularly suitable for identifying actively infectious individuals [10] [16].
Time-Dependent Sensitivity: Clinical studies show optimal performance during early infection stages (up to 9 days post-symptom onset), with significantly reduced sensitivity during later stages when viral loads decline [16].
Multiplexing Potential: Molecular beacon approaches enable multiplex detection of several targets in single reactions, including simultaneous detection of viral and human control RNA to verify sample integrity [15].
RT-LAMP technology represents a significant advancement in molecular detection methods, offering a balanced combination of speed, accessibility, and reliability. While RT-qPCR remains the gold standard for maximum sensitivity, particularly at low viral concentrations, RT-LAMP provides an excellent alternative for rapid screening, resource-limited settings, and point-of-care applications. The technology's particular strength in identifying cases with higher viral loads makes it exceptionally valuable for public health interventions aimed at curbing transmission. For researchers and drug development professionals, RT-LAMP offers a versatile platform that can be adapted to various experimental needs, from basic viral detection to sophisticated multiplex assays incorporating internal controls and specific probe-based detection systems.
Rapid Antigen Tests (RATs) have become indispensable tools in the management and study of SARS-CoV-2, offering a distinct alternative to molecular methods like reverse transcriptase polymerase chain reaction (RT-PCR). Their value lies in the unique combination of speed, simplicity, and cost-effectiveness, enabling decentralized testing and near-in-time results critical for early isolation and transmission interruption [17] [18]. The core technology underpinning most RATs is the lateral flow immunoassay (LFIA), a platform designed to detect specific viral proteins, or antigens, from patient samples [17].
For researchers and scientists engaged in a comparative analysis of SARS-CoV-2 diagnostic methods, understanding the precise mechanisms, performance boundaries, and technical protocols of RATs is paramount. This guide provides a detailed examination of RATs, placing their performance within the broader context of molecular diagnostics. It summarizes key experimental data, delineates foundational methodologies, and outlines essential research reagents, thereby equipping professionals with the necessary framework for critical evaluation and application of these tests in both clinical and research settings.
Immunoassay Mechanism: The Lateral Flow Assay
The operational principle of most rapid antigen tests is the lateral flow immunoassay (LFIA), a robust technology that leverages antibody-antigen interactions on a nitrocellulose membrane to generate a visual signal [17]. The process is engineered for simplicity and speed, typically yielding results within 10-30 minutes without requiring specialized equipment [18].
The following diagram illustrates the sequential flow and key components of a typical lateral flow assay for SARS-CoV-2 antigen detection.
Core Components and Signaling Pathway
The signaling pathway within an LFIA involves a cascade of specific biochemical reactions, as shown in the workflow below.
Performance Comparison: Antigen Tests vs. Molecular Methods
A critical component of SARS-CoV-2 research involves the comparative analysis of diagnostic test performance. The table below summarizes the core characteristics of rapid antigen tests against molecular methods like RT-PCR.
Table 1: Comparative Performance: Rapid Antigen Tests vs. Molecular Methods
| Performance Feature | Rapid Antigen Tests (RATs) | Molecular Tests (e.g., RT-PCR, POC NAATs) |
|---|---|---|
| Target Molecule | Viral surface proteins (antigens) [18] | Viral genetic material (RNA) [18] |
| Technology Platform | Lateral Flow Immunoassay (LFIA) [17] | Nucleic Acid Amplification Test (NAAT), including PCR and isothermal amplification [18] |
| Typical Turnaround Time | 10–30 minutes [18] | 15–45 minutes (POC NAATs) to several hours (lab-based) [18] |
| Analytical Sensitivity (LOD) | Moderate; requires higher viral load [19] | High; can detect very low viral copies [20] |
| Clinical Sensitivity (Symptomatic) | ~80-85% (early symptoms) [18]; 90.4% in a recent study [19] | >95% [20] [18] |
| Clinical Specificity | High (>97-99%) [19] [18] | Very High (>99%) [18] |
| Best Use Case | High-prevalence settings, rapid screening, early symptomatic phase [18] | High-stakes diagnosis, low-prevalence settings, asymptomatic detection [18] |
| Cost per Test | Low [18] | Moderate to High [18] |
| Equipment Needs | Minimal to none [18] | Analyzer required [18] |
| Multiplex Capability | Rare [18] | Common (e.g., respiratory panels) [18] |
The Impact of Viral Load on Test Sensitivity
The sensitivity of RATs is not static; it is highly dependent on the viral load present in the patient sample, which is often inversely correlated with RT-PCR Cycle Threshold (Ct) values [19]. One study demonstrated a clear correlation between low Ct values (indicating high viral load) and high RAT sensitivity. The sensitivity was 96.5% for samples with Ct <22, but dropped significantly to 80.5% for Ct 22-26, and only 30.8% for Ct >26 [19]. This performance characteristic underscores a critical limitation of RATs: their significantly reduced ability to detect infections in individuals with low viral loads, which is common in pre-symptomatic, late-stage, or asymptomatic infections [20].
Experimental Protocols for Performance Validation
For researchers validating the performance of rapid antigen tests, the following core experimental protocols provide a framework for generating comparable and reliable data.
Protocol 1: Diagnostic Accuracy Study vs. RT-PCR
This protocol is designed to evaluate the clinical sensitivity and specificity of a RAT against the reference method of RT-PCR.
- 1. Sample Collection: Obtain simultaneous paired oro-nasopharyngeal swabs from a cohort of symptomatic adult patients [19].
- 2. Sample Processing:
- 3. RT-PCR Analysis: Perform RT-PCR testing targeting established SARS-CoV-2 genes (e.g., RdRp, N, E). Record Ct values for all positive samples [19].
- 4. Data Analysis:
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) using RT-PCR results as the reference standard.
- Stratify RT-PCR positive samples by Ct value ranges (e.g., <22, 22-26, >26) and calculate the sensitivity of the RAT for each group [19].
Protocol 2: Limit of Detection (LOD) Determination
This protocol establishes the lowest concentration of the virus that the RAT can reliably detect.
- 1. Sample Preparation: Create serial dilutions of inactivated SARS-CoV- virus or recombinant nucleocapsid protein in a synthetic matrix that mimics nasal fluid [17].
- 2. Test Execution: Apply each dilution to the RAT cartridge. The number of replicates per dilution (e.g., n=20) should be sufficient for statistical analysis [17].
- 3. Data Analysis: The LOD is defined as the lowest virus concentration at which ≥95% of the test replicates produce a positive result [17].
- 4. Correlation with Ct Value: Where possible, correlate the dilution factor with the Ct value obtained from RT-PCR testing of the same material to bridge analytical and clinical sensitivity [19].
The Scientist's Toolkit: Key Research Reagent Solutions
The development and validation of rapid antigen tests rely on a specific set of biological and chemical reagents. The following table details these essential materials and their functions in the research context.
Table 2: Essential Research Reagents for Rapid Antigen Test Development
| Research Reagent | Function and Role in Assay Development |
|---|---|
| Monoclonal Antibodies (mAbs) | Core detection elements; highly specific mAbs target SARS-CoV-2 antigens (e.g., nucleocapsid protein). Different mAbs are used for capture (on test line) and detection (conjugated to labels) [17]. |
| Nucleocapsid (N) Protein | The primary target antigen for most SARS-CoV-2 RATs. Used as a standard (recombinant protein) for assay development, optimization, and calibration [17]. |
| Colloidal Gold Nanoparticles | A common label for conjugation to detection antibodies. Provides a red color at the test line, allowing for visual interpretation of results without instrumentation [17]. |
| Nitrocellulose Membrane | The platform on which the immunoassay occurs. Its porous structure facilitates capillary flow and serves as the solid support for immobilizing capture antibodies at the test and control lines [17]. |
| Viral Transport Medium (VTM) | A solution used to store and transport patient swab samples while maintaining viral integrity. Essential for comparative studies against RT-PCR [19]. |
| Positive Control Swabs | Swabs containing inactivated virus or recombinant antigen at a known concentration. Critical for verifying test performance, lot-to-lot consistency, and operator competency [19]. |
Within the comparative framework of SARS-CoV-2 research methodologies, rapid antigen tests occupy a vital, defined niche. Their immunoassay mechanism, based on lateral flow technology, provides unparalleled speed and operational simplicity, making them powerful tools for mass screening and rapid triage in high-prevalence scenarios [18]. However, this utility is bounded by a well-documented performance characteristic: lower analytical sensitivity compared to molecular methods, leading to a higher likelihood of false-negative results in cases of low viral load [20] [19].
For the research and development community, the future of RATs lies in addressing these limitations. Emerging trends include the integration of digital readers to minimize user interpretation error and enhance signal quantification, the development of multiplex platforms capable of simultaneously differentiating between SARS-CoV-2, influenza, and RSV, and the exploration of novel labels and signal amplification techniques to push sensitivity closer to molecular standards without sacrificing speed [18]. A thorough understanding of the mechanisms, performance data, and experimental protocols detailed in this guide provides the foundational knowledge necessary to drive this innovation forward, ultimately enhancing our diagnostic capabilities against current and future pathogenic threats.
Next-Generation Sequencing (NGS) is the cornerstone of modern genomic surveillance, enabling scientists to track the evolution and spread of SARS-CoV-2 variants. This guide provides a comparative analysis of the primary NGS methods and platforms used in SARS-CoV-2 research, supporting researchers in selecting the optimal approach for their surveillance objectives.
Two primary enrichment methods are used to target the SARS-CoV-2 genome for sequencing: tiling multiplex PCR and sequence hybridization capture [21]. Each method has distinct advantages depending on sample quality and research goals.
- Tiling Multiplex PCR: This approach uses multiple overlapping primer pairs to amplify the entire viral genome into small fragments. It is highly sensitive and efficient for samples with moderate to high viral loads, making it the most common strategy for clinical samples [21] [22]. Common protocols include ARTIC and its derivatives.
- Sequence Hybridization Capture: This method uses biotinylated probes (baits) to hybridize and pull down viral sequences from a pool of nucleic acids. It is particularly useful for samples with low viral load or significant host background, as it is less prone to amplification bias and can handle more diverse sequences [21].
Performance Comparison of NGS Methods and Platforms
The performance of different NGS workflows varies significantly based on the protocol, sequencing technology, and sample quality. The tables below summarize key performance metrics from recent comparative studies.
Table 1: Comparison of Whole Genome Sequencing Protocols for SARS-CoV-2
| Sequencing Protocol | Median Genome Coverage (Ct ≤ 30) | Key Advantages | Noted Limitations |
|---|---|---|---|
| ARTIC (v3 & v4.1) [23] | ~99% (with cell culture variants) | High PCR amplicon yield and genome completeness; accurate lineage calling [23]. | Performance can drop with very low viral titers [23]. |
| Illumina AmpliSeq [22] | 99.8% | Very high genome coverage [22]. | |
| EasySeq (Illumina) [22] | ~99% (included in study) | High proportion of SARS-CoV-2 reads; low hands-on time [22]. | |
| Oxford Nanopore (ONT) [22] | 81.6% | Shortest sequence runtime; low hands-on time; capable of detecting structural variations [22]. | Lower genome coverage compared to other methods [22]. |
| Ion AmpliSeq (Thermo Fisher) [22] | ~99% (included in study) | High genome coverage [22]. | |
| QNome Nanopore [24] | 89.35% (on clinical samples) | Effective for structural variation detection; real-time analysis [24]. | Lower read accuracy and fewer "good" consensus genomes vs. MGI [24]. |
| MGI DNBSEQ [24] | 90.39% (on clinical samples) | High sensitivity for mutation detection [24]. |
Table 2: Cross-Platform Sequencing Performance Metrics
| Performance Parameter | Illumina Systems [22] | Ion Torrent Systems [22] | Oxford Nanopore (ONT) [22] | QNome Nanopore [24] |
|---|---|---|---|---|
| Typical Read Type | Short-read | Short-read | Long-read | Long-read |
| Hands-on Time | Low (EasySeq) to Moderate [22] | Low [22] | ||
| Sequence Runtime | Moderate to Long [22] | Short [22] | ||
| Variant Calling | Accurate for SNVs and small indels [24] | Accurate for SNVs and small indels | Accurate consensus-level sequences [24] [22] | Accurate consensus-level sequences; good for large deletions [24] |
| Error Rate | Low | Low | Higher single-read error rate, but accurate at consensus [24] | Higher single-read error rate [24] |
Experimental Protocols for SARS-CoV-2 Sequencing
Benchmarking of Amplicon-Based Protocols
A 2025 study compared five amplicon-based WGS protocols (ARTIC v3, ARTIC v4.1, QIAseq DIRECT SARS-CoV-2, SNAP, and Midnight) using synthetic SARS-CoV-2 RNA and cell culture-derived variants titrated to represent high, medium, and low viral loads [23].
- Sample Preparation: The study used Twist Synthetic SARS-CoV-2 RNA Control and six cell-cultured SARS-CoV-2 variants (B.1, B.1.1.7, B.1.351, P.1, B.1.617.2, and BA.1). Viral RNA was extracted using a bead-based purification kit and reverse-transcribed to cDNA [23].
- Protocol Evaluation: The protocols were compared based on PCR amplicon yield, genome completeness (percentage of the genome covered at a sufficient depth), and accuracy in lineage calling [23].
- Key Findings: The ARTIC protocols, particularly v4.1, yielded the highest number of amplicons and showed the highest genome completeness across different viral titers. Although the SNAP protocol yielded the fewest amplicons, it showed high genome completeness for the synthetic genome at high titre [23].
Nanopore vs. Short-Read Sequencing
A 2024 study directly compared the performance of the QNome nanopore platform against the short-read MGI platform [24].
- Sample Collection: The study utilized 120 clinical nasopharyngeal swab (NPS) samples with Ct values below 30, alongside synthetic SARS-CoV-2 controls [24].
- Uniform Enrichment and Sequencing: For a fair comparison, RNA from all samples was extracted, reverse-transcribed, and amplified using the ARTIC v4.1 primer set. The resulting amplicons were then split and used for library preparation on both the QNome and MGI platforms [24].
- Analysis Metrics: The platforms were compared on read length, mapping quality, genome coverage, mutation detection sensitivity, and phylogenetic concordance of assigned Pango lineages [24].
Research Reagent Solutions for SARS-CoV-2 Sequencing
Table 3: Essential Research Reagents and Kits for SARS-CoV-2 NGS
| Reagent / Kit Name | Function / Application | Example Use in Protocols |
|---|---|---|
| ARTIC Primer Panels (v3, v4, v4.1) [23] [24] | Tiling multiplex PCR for whole-genome amplification of SARS-CoV-2. | Used for initial cDNA amplification in both ONT and Illumina protocols [23] [24]. |
| Twist Synthetic SARS-CoV-2 RNA Control [23] | A defined synthetic RNA control for benchmarking protocol performance. | Served as a control material in the benchmarking study [23]. |
| iScript Advanced cDNA Synthesis Kit [22] | Reverse transcription of viral RNA into cDNA for subsequent PCR. | Used in the EasySeq RC-PCR protocol [22]. |
| Agenmic SARS-CoV-2 Target Enrichment Kit [24] | A commercial kit for PCR-based enrichment of SARS-CoV-2 genomes. | Used for cDNA synthesis and PCR amplification in the QNome vs. MGI study [24]. |
| AmpliSeq SARS-CoV-2 Panel (Illumina) [22] | A targeted amplicon panel for SARS-CoV-2 sequencing on Illumina systems. | Used for library preparation and sequencing on the Illumina NovaSeq 6000 [22]. |
| Ion AmpliSeq SARS-CoV-2 Insight Assay (Thermo Fisher) [22] | A targeted amplicon panel for SARS-CoV-2 sequencing on Ion Torrent systems. | Used for library preparation and sequencing on Ion Torrent platforms [22]. |
Workflow Visualization of NGS Methods
The following diagram illustrates the two main NGS workflows for SARS-CoV-2, highlighting the key divergences in the enrichment step.
The choice of NGS method for SARS-CoV-2 genomic surveillance involves trade-offs. For most clinical samples with reliable viral loads, tiling multiplex PCR protocols like ARTIC on either short-read (Illumina) or long-read (ONT) platforms offer a robust, sensitive, and cost-effective solution. For challenging samples with very low viral load or high levels of contamination, hybridization capture methods may provide better coverage. The ongoing development of methods like ARTIC-Amp, which adds a rolling circle amplification step to boost yield, shows promise for further enhancing sensitivity for environmental and wastewater surveillance [23].
The rapid and accurate detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been a cornerstone of the global response to the COVID-19 pandemic. While reverse transcription quantitative polymerase chain reaction (RT-qPCR) remains the gold standard for molecular diagnosis, the pandemic has acted as a catalyst for the development of novel diagnostic platforms that offer advantages in speed, portability, and ease of use [25] [26]. Among these, technologies based on Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and other isothermal amplification methods have shown exceptional promise for point-of-care (POC) testing and field deployment. This comparative analysis examines the performance, experimental protocols, and technical characteristics of these emerging platforms within the broader context of molecular methods for SARS-CoV-2 research, providing researchers and drug development professionals with a critical evaluation of the current diagnostic landscape.
The emerging diagnostic platforms for SARS-CoV-2 detection primarily leverage two core principles: CRISPR-Cas systems for specific nucleic acid recognition and isothermal amplification for rapid nucleic acid amplification without specialized thermal cycling equipment.
CRISPR-Cas Systems utilize Cas proteins (e.g., Cas12, Cas13) that, upon recognition of a specific viral RNA sequence through a guide CRISPR RNA (crRNA), exhibit collateral cleavage activity. This activity enables them to degrade reporter molecules, generating a detectable fluorescent or colorimetric signal [25] [27]. The programmable nature of CRISPR-Cas systems allows for high specificity, which is particularly valuable for distinguishing between different SARS-CoV-2 variants [28].
Isothermal Amplification Methods, such as Loop-Mediated Isothermal Amplification (LAMP) and Recombinase Polymerase Amplification (RPA), amplify nucleic acids at a constant temperature. This eliminates the need for thermal cyclers, making them suitable for resource-limited settings [25] [29]. These methods are often coupled with CRISPR-Cas systems to enhance sensitivity or with other detection mechanisms to create integrated diagnostic platforms.
The table below summarizes the key performance metrics of major emerging platforms compared to the reference standard, RT-qPCR.
Table 1: Performance Comparison of SARS-CoV-2 Detection Platforms
| Technology | Principle | Limit of Detection | Time to Result | Clinical Sensitivity | Clinical Specificity |
|---|---|---|---|---|---|
| RT-qPCR | Reverse transcription polymerase chain reaction | 100-1000 copies/μL [26] | 1-4 hours [30] | Gold Standard | Gold Standard |
| CRISPR-Cas (e.g., CALIBURN-v2) | CRISPR-Cas12a with isothermal pre-amplification | ~100-fold improvement vs earlier platforms [28] | ~25 minutes [28] | 94.38%-95.56% [28] | Not specified |
| AND-gated CRISPR-Cas12 | Dual-gene (ORF1ab & N) logic-gated CRISPR | 4.3 aM (~3 copies/μL) [31] | <50 minutes [31] | 100% [31] | 100% [31] |
| RHAM | RNase HII-assisted LAMP amplification | 5×10² copies/mL [29] | 10-25 minutes [29] | 100% [29] | 100% [29] |
| nGQD-SPR Biosensor | Nitrogen-doped graphene quantum dot surface plasmon resonance | 0.01 pg/mL [30] | Real-time (minutes) [30] | Not specified | Not specified |
| Antigen Rapid Tests | Lateral flow immunoassay | Varies by viral load | 15-30 minutes | 71.2% (overall) [32] | 98.9% (overall) [32] |
Experimental Protocols and Workflows
CRISPR-Cas Systems with Isothermal Pre-amplification
A common and effective approach combines the high specificity of CRISPR-Cas systems with the amplification power of isothermal methods. The typical workflow involves sample preparation, nucleic acid amplification, and CRISPR-based detection.
Table 2: Key Steps in a Coupled RT-RPA/CRISPR-Cas12a Assay
| Step | Description | Key Components | Conditions |
|---|---|---|---|
| 1. RNA Extraction | Isolation of viral RNA from nasopharyngeal swabs | TIANamp Virus DNA/RNA Kit [28] | Follow manufacturer's protocol |
| 2. Reverse Transcription Recombinase Polymerase Amplification (RT-RPA) | Isothermal amplification of target RNA | Primer set (e.g., for N gene), rehydration buffer, magnesium acetate [28] | 42°C for 30 minutes [28] |
| 3. CRISPR-Cas Detection | Target-specific cleavage and signal generation | LbCas12a, crRNA, ssDNA fluorescent reporter, NEBuffer [28] | 37°C for 30 minutes [28] |
| 4. Signal Readout | Fluorescence or lateral flow detection | Fluorometer or lateral flow strip | Visual or instrument-based |
Figure 1: CRISPR-Cas Detection Workflow. This diagram illustrates the sequential steps from sample collection to result readout in a typical CRISPR-based diagnostic assay.
Advanced CRISPR Configurations: AND-Gated Logic
To enhance specificity and reduce false positives, researchers have developed sophisticated CRISPR systems that require the presence of multiple viral targets. The AND-gated CRISPR-Cas12 system represents a significant innovation, as it necessitates the simultaneous detection of two distinct SARS-CoV-2 genes (ORF1ab and N) to generate a positive signal [31].
The experimental protocol involves:
- Reverse Transcription Free-Exponential Amplification Reaction (RTF-EXPAR): Viral RNA is converted and amplified into short single-stranded DNA (ssDNA) activators without a separate reverse transcription step. This is performed in two separate tubes, one for each target gene [31].
- CRISPR-Cas12a Activation Logic: The ssDNA activators from each target hybridize with the spacer region of their corresponding crRNA. Only when both activators are present does a stable ternary complex form, activating the trans-cleavage activity of Cas12a [31].
- Signal Generation: Activated Cas12a cleaves a reporter probe (e.g., fluorescent or lateral flow), yielding a detectable signal.
Figure 2: AND-Gated CRISPR-Cas12 Detection Logic. This system requires simultaneous detection of two distinct SARS-CoV-2 genes (ORF1ab and N) to activate the Cas12a enzyme and produce a signal, significantly enhancing specificity.
RNase HII-Assisted Amplification (RHAM)
The RHAM platform integrates LAMP with an RNase HII-mediated fluorescent reporter system to achieve rapid and specific detection in a single reaction [29]. The key differentiator of RHAM is its mechanism for reducing non-specific amplification, a common challenge in LAMP assays.
The experimental process is as follows:
- LAMP Amplification: Primers specific to SARS-CoV-2 targets (Orf1ab and N genes) initiate exponential amplification of the viral RNA at an isothermal temperature (60-65°C) using Bst DNA polymerase [29].
- Hybridization and Cleavage: A ribonucleotide-containing fluorescent probe, labeled with a fluorophore and a quencher, hybridizes specifically with the LAMP amplicon. The RNase HII enzyme recognizes and cleaves the RNA base within the DNA–probe duplex [29].
- Fluorescence Detection: Cleavage separates the fluorophore from the quencher, resulting in a fluorescent signal that can be monitored in real-time. The entire process, from sample to result, can be completed in under 25 minutes, even with unextracted clinical samples [29].
Research Reagent Solutions
Successful implementation of these novel diagnostic platforms relies on a specific set of reagents and materials. The table below details essential components and their functions in a typical CRISPR-based diagnostic assay.
Table 3: Essential Research Reagents for CRISPR-based SARS-CoV-2 Detection
| Reagent/Material | Function | Example Specifications |
|---|---|---|
| Cas Protein | Effector nuclease for target recognition and signal generation | LbCas12a (from Lachnospiraceae bacterium ND2006) [28] |
| crRNA | Guide RNA that confers specificity to the viral target | Designed against SARS-CoV-2 N, Orf1ab, or S genes [28] [31] |
| Isothermal Amplification Mix | Enzymes and reagents for amplifying viral RNA at constant temperature | RT-RPA Kit (e.g., AmpFuture) [28]; LAMP primers and Bst polymerase [29] |
| Fluorescent Reporter | Substrate for detecting collateral cleavage activity | ssDNA probe labeled with FAM (fluorophore) and BHQ1 (quencher) [28] |
| Nuclease-Free Buffers | Optimal reaction environment for enzymatic activity | NEBuffer with optimized Na+, Mg2+, DTT, and BSA concentrations [28] |
| Lateral Flow Strips | Platform for visual, instrument-free readout | Test strips with FAM- and biotin-labeled reporters [31] |
Discussion and Future Perspectives
The emergence of CRISPR-based and other novel detection platforms represents a paradigm shift in molecular diagnostics for infectious diseases. The comparative data clearly demonstrates that these technologies can achieve sensitivity comparable to RT-qPCR while offering significant advantages in speed, portability, and potential for point-of-care use [25] [28] [29]. The integration of isothermal amplification with CRISPR detection has been particularly successful, mitigating the limitations of each method when used alone [25].
The high specificity of CRISPR systems is a critical asset, not only for distinguishing SARS-CoV-2 from other respiratory pathogens but also for detecting specific variants of concern [28]. Innovations such as the AND-gated logic circuit further enhance diagnostic reliability by virtually eliminating false positives through dual-target verification [31]. Furthermore, platforms like RHAM and nGQD-SPR biosensors illustrate how refinements in signal generation and detection can lead to improvements in both speed and accuracy [29] [30].
For the research and drug development community, these platforms offer powerful tools beyond mere diagnosis. The ability to rapidly profile viral loads and characterize variants in near real-time can inform epidemiological models, therapeutic strategies, and vaccine development. Future developments will likely focus on streamlining workflows into single-step reactions, enhancing multiplexing capabilities for simultaneous pathogen detection, and integrating these systems with portable devices and Internet of Medical Things (IoMT) platforms for remote data collection and analysis [28]. As these technologies mature and become more accessible, they are poised to transform not only pandemic response but also routine infectious disease diagnostics.
Application-Specific Method Selection and Implementation Strategies
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR) remains the gold standard for sensitive and reliable detection of RNA viruses such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [9] [33]. The unprecedented diagnostic demands of the COVID-19 pandemic highlighted the critical need for optimized, high-throughput laboratory workflows to enable rapid testing while maintaining analytical accuracy. Efficient diagnostic pipelines are essential not only for patient triaging and clinical decision-making but also for broader public health surveillance efforts [9] [33]. This guide provides a comparative analysis of automated RNA extraction systems, RT-qPCR detection methodologies, and streamlined protocols, presenting objective performance data to inform laboratory setup and reagent selection for molecular testing.
Comparative Analysis of RNA Extraction Systems
The initial step of RNA extraction is a critical determinant for the success of downstream RT-qPCR applications. Automated nucleic acid extraction systems have become indispensable in high-throughput settings, significantly reducing hands-on time and minimizing the risk of cross-contamination compared to manual methods [34] [35].
Performance Comparison of Automated Extraction Platforms
Various automated platforms utilizing magnetic bead-based technology have been developed and validated for SARS-CoV-2 RNA extraction from nasopharyngeal swabs. The following table summarizes the performance characteristics of several tested systems.
Table 1: Comparison of Automated RNA Extraction Systems
| Extraction System / Kit | Technology | Processing Time | Sample Input Volume | Elution Volume | Key Performance Findings |
|---|---|---|---|---|---|
| Standard Kit (MAGABIO PLUS VIRUS DNA/RNA PURIFICATION KIT II) [35] | Magnetic Beads (with Proteinase K) | ~35 minutes | 20-1000 µL | 80 µL | Found to have good efficiency and produced reproducible results; served as a reliable benchmark [35]. |
| Rapid Kit (MAGABIO PLUS VIRUS RNA PURIFICATION KIT II) [35] | Magnetic Beads (without Proteinase K) | ~9 minutes | 10-300 µL | 70 µL | Provided comparable analytical results to the standard kit but with significantly faster turnaround, improving workflow [35]. |
| EZ1 DSP Virus Kit on EZ1 Advanced XL robot [34] | Automated Magnetic Beads | Not Specified | 200 µL [36] | 100 µL [36] | Showed good efficiency and produced more reproducible results than the manual MagMAX method in a forensic evaluation [34]. |
| STARMag 96x4 Viral DNA/RNA Kit on Nimbus IVD platform [9] [36] | Automated Magnetic Beads | ~270 minutes total for extraction and RT-qPCR [36] | 200 µL | 100 µL | Used as the reference standard in clinical diagnostics; demonstrated high sensitivity and reliability [9] [36]. |
Experimental Protocol: RNA Extraction Comparison
A typical protocol for comparing RNA extraction methods, as used in several studies, involves the following steps [35]:
- Sample Collection: Nasopharyngeal swabs are collected from symptomatic individuals and placed in Universal Transport Medium (UTM).
- Sample Processing: A defined volume (e.g., 100-200 µL) of the UTM sample is used for nucleic acid extraction.
- Automated Extraction: Samples are processed on the automated platform according to the manufacturer's instructions. This typically involves lysis, binding of nucleic acids to magnetic silica particles, several wash steps, and final elution in a dedicated buffer.
- Quality Assessment: The concentration and purity of the extracted RNA can be assessed using spectrophotometry (e.g., Nanodrop), measuring absorbance ratios at 260/280 nm and 260/230 nm [35].
- Downstream Analysis: The eluted RNA is immediately used for RT-qPCR or stored at -80°C.
Comparative Analysis of RT-qPCR Detection Methods
Following RNA extraction, the choice of RT-qPCR detection method impacts sensitivity, specificity, cost, and throughput. The main methodologies include TaqMan probe-based assays and SYBR Green-based assays, which can be configured in one-step or two-step formats.
Performance Comparison of Detection Kits and Methods
Multiple RT-qPCR kits and methods have been rigorously evaluated against clinical diagnostic standards. The data below illustrates their comparative performance.
Table 2: Comparison of RT-qPCR Detection Kits and Methods
| Detection System / Method | Chemistry | Target Genes | Reported Sensitivity | Reported Specificity | Key Findings / Limitations |
|---|---|---|---|---|---|
| BGI Real-Time Fluorescent RT-PCR Kit [9] | TaqMan Probe (One-Step) | Not Specified | 100% (vs. clinical diagnosis) [9] | 100% (vs. clinical diagnosis) [9] | Overall superior performance with lower Ct values and higher sensitivity; suitable for direct, extraction-free detection (78.4% sensitivity) [9]. |
| Norgen 2019-nCoV TaqMan RT-PCR Kit [9] | TaqMan Probe (One-Step) | N1, N2 (CDC primers) | Accurately detected samples with clinical Ct < 33 [9] | High | Less sensitive than BGI but offered significant cost savings [9]. |
| Allplex 2019-nCoV Assay (Reference standard) [9] [36] | Multiplex TaqMan Probe (One-Step) | N, RdRp/S, E | High (Clinical Gold Standard) | High (Clinical Gold Standard) | Used as a benchmark in validation studies; demonstrated 100% analytical specificity [9] [36]. |
| Two-Step SYBR Green-based Method [37] | SYBR Green (Two-Step) | S, N | 88% (S gene), 84% (N gene) | 84% | Comparable sensitivity and specificity to one-step methods for samples with Ct ≤ 25; more prone to non-specific amplification [37]. |
| One-Step TaqMan Probe-based Method [37] | TaqMan Probe (One-Step) | RdRp, N | 92% (RdRp gene), 96% (N gene) | 86% | Considered the premier standard test; higher cost but generally more specific than SYBR Green [37]. |
Experimental Protocol: One-Step vs. Two-Step RT-qPCR
The core methodological differences are as follows [37]:
A. One-Step RT-qPCR Protocol: This method combines reverse transcription and PCR amplification in a single reaction tube.
- Reaction Setup: A master mix containing reverse transcriptase, DNA polymerase, dNTPs, buffer, primers, probes (for TaqMan), and the extracted RNA template is prepared.
- Thermal Cycling: The reaction is run on a real-time PCR instrument with a programmed protocol: reverse transcription (e.g., 50°C for 20 min), initial denaturation (e.g., 95°C for 15 min), followed by 40-45 cycles of denaturation (e.g., 95°C for 10 s) and annealing/extension (e.g., 60°C for 15-60 s, with fluorescence acquisition) [37] [36].
B. Two-Step SYBR Green RT-qPCR Protocol: This method separates reverse transcription from the PCR amplification.
- cDNA Synthesis: Extracted RNA is first reverse transcribed into cDNA using a separate kit containing reverse transcriptase, primers, and dNTPs.
- qPCR Setup: A portion of the synthesized cDNA is then added to a qPCR master mix containing DNA polymerase, SYBR Green dye, and gene-specific primers.
- Thermal Cycling: The reaction is run with a standard qPCR cycling protocol (e.g., 95°C for 35 s, followed by 40 cycles of 95°C for 5 s and 60°C for 1 min), followed by a melt curve analysis to verify amplification specificity [37].
Emerging Workflows: Extraction-Free and Direct RT-qPCR
To further increase throughput and circumvent supply chain bottlenecks for RNA extraction kits, extraction-free direct RT-qPCR methods have been developed and validated.
Performance Data and Protocols
The primary direct methods involve using raw sample material with or without a heat inactivation step.
Table 3: Comparison of Extraction-Free Direct RT-qPCR Methods
| Method | Description | Sensitivity vs. Extraction-Based Method | Key Advantages & Limitations |
|---|---|---|---|
| Unheated Extraction-Free (EFh-) [36] | Directly using a diluted UTM sample in the RT-qPCR reaction without any pre-treatment. | 100% [36] | Perfect agreement with standard method; reduces average processing time from ~270 min to ~156 min [36]. |
| Heated Extraction-Free (EFh+) [36] | Sample is heated to 95°C for 3-10 min to lyse cells/virus, then cooled before adding to the RT-qPCR reaction. | 91.8% (false negatives occurred in samples with Ct >30) [36] | Faster than extraction (~163 min total); but heat treatment can reduce sensitivity for low viral loads, increasing Ct values by 4.5-6 cycles [9] [36]. |
| Direct with RNase Inhibitor [9] | Adding an RNase inhibitor directly to the reaction mix without lysis or heating. | Not fully quantified, but detected ~10 fold less virus than indirect methods [9] | Simple approach that reduces sample handling and improves detection over plain direct methods [9]. |
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for establishing robust RT-qPCR workflows for SARS-CoV-2 detection.
Table 4: Key Research Reagent Solutions for RT-qPCR Workflows
| Reagent / Material | Function | Examples & Notes |
|---|---|---|
| Automated RNA Extraction Kits | Purification of viral RNA from clinical samples, removing inhibitors. | Kits based on magnetic silica particles (e.g., Seegene STARMag, Qiagen EZ1, MagMAX, MAGABIO) are standard for automation [9] [33] [35]. |
| One-Step RT-qPCR Master Mix | Enables combined reverse transcription and PCR amplification in a single tube, reducing hands-on time. | Contains reverse transcriptase, thermostable DNA polymerase, dNTPs, and optimized buffer. Kits from BGI, Norgen, and Seegene are commonly used [9] [37]. |
| TaqMan Probes & Primers | Provide high specificity for target detection in multiplex assays by using a fluorescently labeled probe. | Target SARS-CoV-2 genes like N, E, S, and RdRp. CDC-approved N1/N2 primers are widely implemented [9] [33]. |
| SYBR Green Master Mix | A cost-effective fluorescent dye that binds double-stranded DNA, used primarily in two-step methods. | Requires post-amplification melt curve analysis to confirm reaction specificity [9] [37]. |
| Standard Reference Materials | Used to generate standard curves for absolute quantification, ensuring reproducibility and comparability across labs. | Can be plasmid DNA, synthetic RNA (e.g., from CODEX, JRC), or inactivated virus. Choice of standard significantly impacts absolute quantification [38]. |
| Internal Process Controls | Monitor nucleic acid extraction efficiency and detect PCR inhibition in each sample. | A non-competitive control (e.g., mengovirus) spiked into the sample lysis buffer is recommended [38]. |
Workflow Visualization and Data Analysis
High-Throughput RT-qPCR Workflow Diagram
The following diagram illustrates the key decision points and pathways in a high-throughput SARS-CoV-2 testing pipeline, integrating the methods discussed above.
Critical Data Analysis Considerations
For relative quantification of gene expression, the comparative C_T method (2^−ΔΔCt) is widely used [39]. This method relies on the accurate determination of the cycle threshold (Ct), the point at which fluorescence crosses a defined threshold. Key statistical considerations include [40]:
- Data Quality Control: Ensuring high and consistent PCR amplification efficiency for both target and reference genes is critical for valid results.
- Confidence Intervals and P-values: Proper statistical treatment, including confidence intervals and significance testing, is essential to avoid false positive conclusions, especially in clinical applications.
- Standard Curve Validation: For absolute quantification, the choice of standard material (e.g., plasmid DNA vs. synthetic RNA) can significantly impact the reported copy numbers, highlighting the need for harmonization in reporting [38].
The COVID-19 pandemic has underscored the critical need for accurate, rapid, and accessible diagnostic testing, particularly in settings with limited laboratory infrastructure and trained personnel. Molecular diagnostics, especially reverse transcription quantitative polymerase chain reaction (RT-qPCR), remain the gold standard for SARS-CoV-2 detection due to high sensitivity and specificity [16] [41]. However, their reliance on specialized equipment, lengthy processing times, and high costs have driven the development and adoption of alternative diagnostic platforms suitable for point-of-care (POC) and resource-limited environments [16] [42]. Among the most prominent are reverse transcription loop-mediated isothermal amplification (RT-LAMP) and rapid antigen tests (RATs). This guide provides a comparative analysis of these two technologies, focusing on their performance characteristics, operational requirements, and suitability for different testing scenarios within a framework of comparative molecular method analysis.
Fundamental Principles
RT-LAMP is a nucleic acid amplification technique that amplifies target RNA at a constant temperature (typically 60–65°C), eliminating the need for thermal cyclers. It utilizes 4-6 primers targeting 6-8 distinct regions of the viral genome, which confers high specificity. Amplification can be detected in real-time via turbidity or fluorescence, or as an endpoint measurement using colorimetric indicators [41] [43]. Rapid Antigen Tests (RATs) are lateral flow immunoassays that detect the presence of specific viral surface proteins, such as the nucleocapsid protein. They typically provide results within 15-30 minutes by producing a visual band on a test strip when viral antigens are present in the sample above a certain threshold [44] [45].
Comprehensive Performance Metrics
Table 1: Direct Comparison of RT-LAMP and Rapid Antigen Tests
| Performance Parameter | RT-LAMP | Rapid Antigen Test (RAT) |
|---|---|---|
| Detection Target | Viral RNA | Viral Protein (e.g., Nucleocapsid) |
| Assay Time | 30-60 minutes [41] [46] | 15-30 minutes [44] [42] |
| Sensitivity (Overall) | 85.9% - 92.91% [46] [47] | ~67% [44] |
| Specificity (Overall) | 98.33% - 99.5% [46] [47] | ~75% [44] |
| Limit of Detection (LOD) | ~6.7 copies/reaction [16] | ≈ 5.0 × 10² pfu/mL (WHO benchmark) [45] |
| Sensitivity in High Viral Load | ~100% (Ct ≤25) [16] [46] | 100% (Ct ≤20) [44] |
| Sensitivity in Low Viral Load | Decreases after 9-10 days post-symptom onset [16] | 22% (Ct >26) [44] |
| Key Advantage | High sensitivity approaching RT-qPCR, isothermal conditions | Speed, low cost, extreme ease of use |
| Main Limitation | Requires precise primer design and sample prep | Significantly lower sensitivity, especially in asymptomatic cases |
The data reveal a clear performance trade-off. RT-LAMP offers diagnostic accuracy much closer to RT-qPCR, particularly during the acute phase of infection (up to 9 days post-symptom onset), where it demonstrated 100% sensitivity and specificity compared to RT-qPCR [16]. Its performance, however, can depend on the sample processing method, with RNA-extracted samples (RNA-LAMP) showing superior sensitivity (92.91%) compared to direct LAMP protocols (70.92%) [41] [47].
In contrast, RATs provide a speed and convenience advantage but at the cost of significantly lower sensitivity, particularly in patients with lower viral loads. Their sensitivity is highly dependent on viral load, dropping from 100% at Ct values ≤20 to 63% at Ct values 21-25, and as low as 22% at Ct values above 26 [44]. This makes them less effective for detecting pre-symptomatic or asymptomatic infections.
Experimental Protocols and Methodologies
Typical RT-LAMP Workflow
The following diagram illustrates the general workflow for a colorimetric RT-LAMP assay, commonly used for its simplicity and suitability for point-of-care settings.
Diagram 1: Workflow for a colorimetric RT-LAMP assay. The sample preparation step offers two common paths: RNA extraction for higher sensitivity or direct heat inactivation for speed and simplicity.
A standard RT-LAMP protocol, as detailed in [41] and [47], involves the following steps:
- Sample Collection: Nasopharyngeal swabs are collected and placed in a viral transport medium or a specific preservation solution.
- Sample Processing: Two main approaches are used:
- RNA Extraction: Purified viral RNA is extracted using commercial magnetic bead-based kits (e.g., Jiangsu Bioperfectus Technologies nucleic acid extraction kit) to remove inhibitors and increase test sensitivity [41] [47].
- Direct Method: The original sample is heat-inactivated at 95°C for 5 minutes to lyse the virus and inactivate nucleases, then centrifuged. The supernatant is used directly. This method is faster but may yield lower sensitivity [41] [47].
- Amplification Reaction: A 25μL reaction mixture is prepared containing the processed sample and a master mix with primers, DNA polymerase with reverse transcriptase activity, buffers, and dNTPs. For colorimetric detection, a pH-sensitive dye is also included.
- Incubation: The reaction tube is incubated at a constant temperature of 62–65°C for 30–35 minutes in a dry bath or heat block.
- Result Interpretation: A color change from pink to yellow indicates a positive result due to acidification of the reaction mixture. No color change indicates a negative result. Results can be read visually or with a portable spectrophotometer [41] [46].
Typical Rapid Antigen Test Workflow
The following diagram outlines the standard procedure for a typical rapid antigen test, highlighting its simplicity and rapid turnaround.
Diagram 2: Workflow for a typical Rapid Antigen Test (RAT). The process is designed for minimal steps and user-friendly visual interpretation.
A standard RAT protocol, as described in [44] and [47], is as follows:
- Sample Collection: A nasopharyngeal swab is collected from the patient.
- Sample Elution: The swab is inserted into a tube containing a proprietary extraction buffer and rotated vigorously against the tube's inner wall to elute viral proteins.
- Test Application: After waiting approximately one minute, 3-4 drops (around 80μL) of the extracted solution are dispensed into the sample well of the test cassette.
- Lateral Flow and Incubation: The solution migrates across the test strip via capillary action.
- Result Interpretation: Results are read within 15-20 minutes. The appearance of both a control line and a test line indicates a positive result. The appearance of only the control line indicates a negative result. The absence of a control line renders the test invalid [44] [47].
Research Reagent Solutions and Essential Materials
Selecting the appropriate reagents and materials is fundamental to the successful implementation of either diagnostic platform.
Table 2: Essential Research Reagents and Materials
| Item | Function/Description | Example Kits/Catalogs (from search results) |
|---|---|---|
| RT-LAMP Primers/Master Mix | Pre-mixed solutions containing primers, polymerase, buffers, and dNTPs for isothermal amplification. | Loopamp SARS-CoV-2 Detection Kit (Eiken Chemical) [16], Shanghai GeneSc Biotech Kit [41] [47] |
| Viral RNA Extraction Kit | Purifies viral RNA from clinical samples to remove PCR inhibitors and increase assay sensitivity. | QIAamp Viral RNA Mini Kit (Qiagen) [16] [47], Nucleic Acid Extraction Rapid Kit (Magnetic Bead Method) [41] [47] |
| Colorimetric Detection Additive | A pH-sensitive dye that causes a visible color change (e.g., pink to yellow) upon amplification. | Included in commercial RT-LAMP kits like the GeneSc Biotech kit [41] |
| Rapid Antigen Test Cassette | A lateral flow immunoassay device that detects SARS-CoV-2 nucleocapsid protein. | PCL Spit Rapid Antigen Test Kit [44], Panbio COVID-19 Ag Rapid Test [48], BTNX Rapid Response [48] |
| Viral Transport Medium (VTM) | A medium used to preserve virus viability and nucleic acid integrity during swab transport. | BD Universal Viral Transport Medium [16], Universal Transport Media (UTM) [48] |
| Isothermal Heat Block | A device to maintain a constant temperature (60-65°C) required for the RT-LAMP reaction. | Standard dry bath or heat block [41] |
Choosing the Right Tool for the Objective
The choice between RT-LAMP and RATs is not a matter of one being universally superior, but rather of matching the technology to the specific public health or clinical objective, available resources, and stage of infection.
RT-LAMP is the superior choice when the testing goal is high diagnostic accuracy in a decentralized setting. Its performance is closest to RT-qPCR, making it suitable for confirming symptomatic cases in clinics, testing high-risk contacts, and situations where a false negative carries significant risk [42]. It is particularly effective during the early symptomatic phase (first 7-9 days) when the viral load is high [16] [41]. While more complex than RATs, it is far less resource-intensive than lab-based RT-qPCR.
Rapid Antigen Tests are optimal for the purpose of frequent, widespread screening to quickly identify and isolate highly infectious individuals. Their speed, low cost, and simplicity make them ideal for screening programs in schools, workplaces, and before large gatherings [42] [45]. They are most effective in individuals with high viral loads, who are also the most likely to be contagious. Their lower sensitivity is a recognized trade-off for their role in breaking chains of transmission through rapid identification of the most infectious cases [44] [42].
Cost-Effectiveness and Modeling Insights
Mathematical modeling underscores that testing frequency and turnaround time can be more critical than raw test sensitivity for epidemic control [42]. In this context, the low cost and speed of RATs make them highly effective for frequent population screening. One cost-effectiveness analysis of surveillance strategies found that direct testing approaches (similar to how RATs are often deployed) were more cost-effective than complex, pre-screened strategies, with costs per sample tested around €53 for direct household testing [49].
Within the comparative framework of molecular methods for SARS-CoV-2 research and diagnostics, both RT-LAMP and rapid antigen tests have cemented their roles. RT-LAMP serves as a powerful accuracy-oriented POC tool, bridging the gap between lab-based gold standards and field deployment. In contrast, rapid antigen tests are public-health-oriented screening tools, sacrificing some sensitivity for unprecedented speed, scalability, and accessibility. Future research and development will continue to optimize these technologies, but their complementary strengths will remain essential for building resilient and responsive global diagnostic networks.
The COVID-19 pandemic has underscored the critical importance of genomic surveillance in understanding and controlling the spread of viral pathogens. Next-generation sequencing (NGS) technologies have been at the forefront of this effort, enabling researchers to track SARS-CoV-2 transmission routes, monitor the emergence of novel variants, and inform public health responses [50]. Several NGS protocols and platforms have been developed for whole genome sequencing (WGS) of SARS-CoV-2, each with distinct advantages and limitations in terms of cost, throughput, accuracy, and scalability. This guide provides an objective comparison of the leading NGS methodologies and platforms used in SARS-CoV-2 research, supported by experimental data from comparative studies, to assist researchers and public health professionals in selecting appropriate tools for variant surveillance and outbreak investigation.
Table 1: Comparison of SARS-CoV-2 Sequencing Methods
| Method | Best For | Accuracy & Coverage | Cost & Scalability | Key Limitations |
|---|---|---|---|---|
| Amplicon (ARTIC, Midnight) | Population-scale surveillance, low viral load samples [51] | Good genome coverage (>94% with Illumina), sensitive for low Ct samples [51] [52] | Cost-effective, highly scalable, suitable for clinical environments [51] [52] | Primer mismatches with new variants can cause amplicon dropouts [52] |
| Amplicon (Illumina COVIDSeq) | Cost-effective production of consensus sequences [51] | High performance for consensus sequence generation [51] | Most cost-effective among tested methods [51] | Protocol optimized for specific sample types (nasopharyngeal swabs) [51] |
| Hybrid Capture (Twist) | Identifying novel variants, mutation detection across genome [52] | Superior coverage uniformity, better tolerance to mismatches (~10-20%) [52] | Higher cost, more laborious workflow, batch variation [52] | High human host contamination, requires more RNA input [52] |
| Metagenomic Shotgun | Novel pathogen discovery, comprehensive pathogen profiling [50] | Effective when viral abundance is high [51] | No prior knowledge of organisms needed [50] | Lacks sensitivity for low viral load clinical samples [51] |
Table 2: Platform Comparison - GridION vs. MiSeq
| Performance Metric | ONT GridION | Illumina MiSeq | Statistical Significance |
|---|---|---|---|
| Average Genome Coverage | 72.96% [53] | 94.34% [53] | p = 8.1e-16 [53] |
| Genomes Passing QC (>80% coverage) | 27.9% [53] | 89.2% [53] | Significantly different [53] |
| Quality (Good/Mediocre Genomes) | Lower proportion [53] | Higher proportion [53] | p = 0.0028 (good), p = 0.0025 (mediocre) [53] |
| Effect of Ct Score | Strong negative correlation (R = -0.88 to -0.31) [53] | Weak-moderate negative correlation (R = -0.35 to -0.19) [53] | More sensitive to viral load [53] |
| Run Time | ~21 hours [53] | ~36 hours [53] | Faster turnaround [53] |
Experimental Protocols and Workflows
Tiled Amplicon Enrichment (ARTIC and Midnight)
The ARTIC protocol utilizes an reverse transcription step with random hexamers followed by multiplex PCR amplification using two primer pools containing 98 SARS-CoV-2 specific primer pairs that produce amplicons of approximately 400bp in length [51]. The Midnight protocol, a descendant of ARTIC, is designed for long-read sequencing and generates 1200bp amplicons through a similar two-pool approach [52]. Both methods employ tiled amplification strategies that cover the viral genome with overlapping fragments, which are then barcoded and prepared for sequencing on either Illumina or Oxford Nanopore Technologies (ONT) platforms [52].
Hybrid Capture Enrichment (Twist Bioscience)
The Twist hybrid capture protocol involves cDNA synthesis from RNA using random primers, followed by library preparation and target enrichment using biotinylated, single-stranded RNA probes that are complementary to the SARS-CoV-2 genome [52]. The hybridization reaction occurs for 16 hours, after which the target-bound libraries are captured using streptavidin beads, amplified, and purified before sequencing [52]. This method is particularly valuable for detecting novel variants as the baits can tolerate 10-20% sequence mismatch [52].
Comparison of Workflows
The following diagram illustrates the key steps and decision points in selecting and implementing NGS protocols for SARS-CoV-2 sequencing:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for SARS-CoV-2 NGS
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Twist SARS-CoV-2 NGS Assay | Hybrid capture-based target enrichment using biotinylated RNA probes [52] | Tolerates 10-20% sequence mismatch, ideal for novel variant detection [52] |
| ARTIC V3 nCoV-2019 Primers | Tiled amplicon generation with 400bp fragments covering viral genome [51] [52] | Requires updates to address primer mismatches in evolving variants [52] |
| Midnight Primer Panels | Generation of 1200bp amplicons optimized for long-read sequencing [52] | Improved coverage compared to earlier ARTIC versions [52] |
| Illumina COVIDSeq Test | Complete amplicon-based workflow combining ARTIC protocol with Illumina sequencing [51] | Most cost-effective for consensus sequence production [51] |
| MagMAX Viral/Pathogen Nucleic Acid Isolation Kit | RNA extraction from clinical samples [54] | Provides high-quality RNA suitable for sensitive detection [54] |
| QuickExtract RNA Solution | Rapid single-step RNA extraction [54] | Faster processing but may have slightly reduced sensitivity [54] |
Discussion and Technical Considerations
The choice of NGS methodology for SARS-CoV-2 surveillance involves careful consideration of multiple factors, including project objectives, sample characteristics, available resources, and required throughput.
Amplicon-based approaches such as ARTIC and Midnight excel in population-scale surveillance due to their cost-effectiveness and high sensitivity, particularly for samples with low viral loads (higher Ct values) [51]. However, these methods face challenges with primer mismatches when new variants emerge, potentially causing amplicon dropouts that result in incomplete genome coverage [52]. The Illumina COVIDSeq Test, which builds upon the ARTIC protocol, has been identified as the optimal choice for cost-effective, time-efficient production of consensus sequences [51].
Hybrid capture methods like the Twist Bioscience platform offer advantages for detecting novel variants and mutations across the entire genome due to their superior coverage uniformity and greater tolerance to sequence mismatches [52]. The trade-offs include higher costs, more laborious workflows, and increased host contamination [52].
When comparing sequencing platforms, Illumina systems (e.g., MiSeq) demonstrate significantly higher genome coverage and consensus quality compared to Oxford Nanopore technologies (e.g., GridION) [53]. However, Nanopore platforms offer advantages in turnaround time and portability, which can be crucial for rapid response scenarios [53]. The performance of both platforms is influenced by viral load, with Nanopore sequencing showing stronger correlation between Ct values and sequencing success [53].
For comprehensive pathogen detection without prior target knowledge, metagenomic shotgun sequencing provides an unbiased approach, though it requires higher viral loads for effective detection [50] [51].
The optimal selection of NGS protocols and pipelines for SARS-CoV-2 variant surveillance depends on the specific objectives and constraints of the surveillance program. For routine, large-scale monitoring where cost-effectiveness is paramount, amplicon-based methods like Illumina COVIDSeq provide the most practical solution. For research focused on characterizing novel variants with possible primer region mutations, hybrid capture approaches offer better coverage and variant detection capabilities. Platform selection between Illumina and Nanopore technologies involves balancing data quality requirements against the need for rapid turnaround times. As SARS-CoV-2 continues to evolve, the flexibility to adapt these protocols and pipelines will remain essential for effective public health response and ongoing research efforts.
The accurate detection of SARS-CoV-2 is a cornerstone of effective public health response and clinical management during the COVID-19 pandemic. The selection of an appropriate sample type is a critical pre-analytical variable that directly influences the sensitivity, specificity, and overall reliability of diagnostic testing. While nasopharyngeal swabs (NPS) have long been considered the reference standard for respiratory virus detection, the urgent need for scalable testing and mass surveillance has prompted the evaluation of less invasive alternatives, primarily anterior nasal swabs (ANS) and saliva. This comparative guide objectively analyzes the performance characteristics of these three common sample types—nasopharyngeal, anterior nasal, and saliva swabs—within the context of molecular detection of SARS-CoV-2. We provide a synthesized overview of current scientific evidence, including performance metrics and detailed experimental methodologies, to inform researchers, scientists, and drug development professionals in their selection of appropriate sample collection strategies.
Performance Comparison of Sample Types
Extensive independent evaluations have been conducted to compare the real-world performance of different sample types for SARS-CoV-2 detection. The following table summarizes key performance metrics from clinical studies, providing a direct comparison of nasopharyngeal, anterior nasal, and saliva swabs.
Table 1: Performance Comparison of SARS-CoV-2 Sample Types
| Sample Type | Sensitivity (%) | Specificity (%) | Relative Viral Load | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Nasopharyngeal Swab (NPS) | 80.6 (vs. PCR) to 91.2 (viability-corrected) [55] | High (Approaching 100%) [55] | Higher viral loads observed compared to saliva in some studies [56] | Considered the reference standard; high sensitivity [57] | Requires trained healthcare workers; patient discomfort; aerosol-generating [58] [57] |
| Anterior Nasal Swab (ANS) | Lower than NPS; fails to meet WHO sensitivity targets [55] | High [55] | Not specifically quantified in results | Suitable for self-sampling; more comfortable [55] | Lower sensitivity compared to NPS; not suitable for all test protocols [55] |
| Saliva | Variable: 92.1% PPA in one study [58], but lower in others [55] | High [55] | Inconsistent findings: Some report lower than NPS [56], others report higher [58] | Non-invasive; suitable for self-collection; cost-effective; avoids swab shortages [59] [58] | Sensitivity highly variable; potential for PCR inhibition; affected by food/drink intake [55] [56] |
The data reveals a performance trade-off between the reference-standard NPS and the more user-friendly alternatives. The nasopharyngeal swab consistently demonstrates high sensitivity, especially when results are corrected for the presence of viable virus, making it the most reliable sample type for definitive diagnosis [55]. In contrast, independent evaluations of anterior nasal swabs and most saliva-based tests show that they frequently fail to meet the WHO minimum sensitivity criterion of 80% [55]. However, some studies on saliva have reported a higher positivity rate and viral load compared to paired NPS samples, suggesting that performance may be highly dependent on the specific test kit, collection protocol, and patient population [58].
Detailed Experimental Protocols from Cited Studies
To ensure the reproducibility of findings and provide clarity on the generation of comparative data, this section outlines the key methodological approaches from the cited research.
Protocol: High-Capacity Testing Center Evaluation
This study provided a head-to-head comparison of seven different antigen tests using the three sampling methods [55].
- Patient Cohort and Sampling: The study was conducted in a high-capacity testing center during an active outbreak. Participants included both asymptomatic patients with known exposure and mildly symptomatic patients. After obtaining informed consent, trained medical personnel collected a nasopharyngeal swab for qPCR reference testing. Simultaneously, sampling for the rapid antigen tests (RATs) was performed: NPS and ANS were collected by personnel from the contralateral nostril, while saliva tests were performed via self-sampling by patients.
- Antigen Testing: Seven RATs were evaluated according to manufacturers' instructions: one using NPS, two using ANS, and four using saliva (three "lollipop" sponge tests and one "spitting" test). Patients provided a history regarding recent eating, drinking, or smoking before saliva collection.
- Reference qPCR and Virus Culture: qPCR was performed on NPS samples within 24 hours, with a cycle threshold (Ct) cutoff of 40. In all cases of discordance between the qPCR and RAT results, virus culture was performed on the original sample using CV-1 cells to confirm the presence of viable virus. This viability testing provided a crucial correction to the PCR-based sensitivity calculations.
Protocol: Longitudinal Saliva and NPS Comparison
This study focused on comparing saliva and NPS in symptomatic, confirmed COVID-19 patients over time [58].
- Study Design and Sample Collection: A paired sample design was used, collecting both NPS and saliva from 152 hospitalized patients on the day of admission (day zero), with follow-up collections on days eight and fifteen. All patients had previously tested positive via RT-PCR 5-7 days prior to admission.
- Molecular Detection and Viral Load Analysis: RNA was extracted from all samples and tested for SARS-CoV-2 using RT-PCR. The cycle threshold (Ct) value was used as a proxy for viral load, with a lower Ct indicating a higher viral load. The authors statistically compared the positivity rates and Ct values between the paired NPS and saliva samples across the different time points to analyze viral shedding dynamics.
Protocol: Viral Load Quantification in Raw Saliva
This study developed and validated an extraction-free RT-qPCR method for saliva and compared it to nasal swabs [59].
- Sample Collection and Processing: Matched anterior nares swab and saliva samples were collected longitudinally from 20 SARS-CoV-2-positive individuals. Saliva was collected raw, without any additives or RNA extraction stabilizers. A combination sample, consisting of a nasal swab immersed in raw saliva, was also tested.
- Extraction-Free RT-qPCR and ddPCR: The CDC RT-qPCR protocol was modified to test raw saliva and the combination sample directly, bypassing the RNA extraction step. The performance of this extraction-free method was benchmarked against digital droplet PCR (ddPCR), a highly precise method for absolute nucleic acid quantification, to confirm the accuracy of viral load measurements.
Research Reagent Solutions
The following table catalogues essential reagents and materials required for conducting similar comparative studies on SARS-CoV-2 sample types, as derived from the experimental protocols.
Table 2: Key Research Reagents and Materials
| Reagent / Material | Function / Application | Example from Studies |
|---|---|---|
| Viral Transport Medium (VTM) | Preserves virus viability during transport of swab samples for culture and PCR [55] [57] | DMEM with 0.5% BSA [55]; Commercial CITOSWAB VTM [56] |
| RNA Extraction Kit | Isolates and purifies viral RNA for downstream molecular detection [59] | QIAamp Viral RNA mini-Kit (Qiagen) [59] |
| RT-qPCR Master Mix | Amplifies and detects specific SARS-CoV-2 RNA targets | CDC 2019-nCoV RT-qPCR Assay (targeting N1, N2) [59]; DBdirect COVID-19 Multiplex qPCR Kit [55] |
| Cell Line for Virus Culture | Determines the presence of replication-competent, viable virus | CV-1 cells (African green monkey kidney fibroblasts) [55] |
| Digital Droplet PCR (ddPCR) Kit | Provides absolute quantification of viral load; used for assay validation [59] | Bio-Rad SARS-CoV-2 ddPCR kit [59] |
| Saliva Collection Device | Standardizes the collection of saliva samples for self-testing | Saliva Collector (Biocomma) [56]; DNA Genotek OM-505 [59]; Saliva Collection Aid (Salimetrics) [59] |
Logical Workflow for Sample Type Selection
The following diagram illustrates the critical decision-making process and logical pathway for selecting an appropriate sample type based on the primary objective of the testing strategy.
The comparative analysis of nasopharyngeal, anterior nasal, and saliva swabs reveals a clear landscape for SARS-CoV-2 detection. The nasopharyngeal swab remains the gold standard for clinical diagnostics where maximum sensitivity is required, supported by its high and consistent performance in detecting infectious virus [55]. Anterior nasal swabs offer a less invasive and more user-friendly alternative suitable for self-testing, but this convenience comes with a demonstrated cost of lower sensitivity. The role of saliva is the most complex; while it holds great promise for scalable, non-invasive surveillance and some studies show exceptional performance [58], its sensitivity is highly variable and can be influenced by collection protocols and individual patient factors [55] [56]. Ultimately, the choice of sample type should be guided by a balanced consideration of the testing objective—whether for high-sensitivity clinical diagnosis or large-scale public health screening—with an understanding of the inherent performance trade-offs involved.
The COVID-19 pandemic has underscored the critical need for diagnostic tools that can rapidly and accurately differentiate between respiratory pathogens with overlapping clinical symptoms. Multiplex assays, which enable the simultaneous detection of multiple pathogens in a single reaction, have emerged as vital technologies for clinical management, infection control, and public health surveillance. Within the broader context of comparative analysis of molecular methods for SARS-CoV-2 research, this guide objectively evaluates the performance of various multiplex platforms, focusing on their application in detecting co-circulating respiratory pathogens such as SARS-CoV-2, influenza viruses, and adenovirus. This comparative analysis provides researchers and clinical laboratory professionals with data-driven insights to inform diagnostic selection and implementation strategies.
Performance Comparison of Multiplex Assays
Commercial Multiplex Molecular Panels
Table 1: Clinical Performance of Commercial Multiplex Respiratory Panels
| Assay Name | Manufacturer | Overall Sensitivity (%) | Overall Specificity (%) | Key Advantages | Notable Limitations |
|---|---|---|---|---|---|
| Anyplex II RV16 [60] | Seegene | 96.6 | 99.8 | Detects 16 viral targets; distinguishes rhinovirus/enterovirus | Does not subtype influenza A; no bacterial targets |
| FilmArray Respiratory 2.1 plus Panel [60] | bioMérieux | 98.2 | 99.0 | Rapid turnaround (45 min); detects 23 targets (19 viral, 4 bacterial) | Lower specificity (88.4%) for rhinovirus/enterovirus |
| QIAstat-Dx Respiratory SARS-CoV-2 Panel [60] | Qiagen | 80.7 | 99.7 | Semi-quantitative Ct values; user-friendly cartridge system | Failed to detect coronaviruses and parainfluenza in significant proportions of positive samples |
A 2024 comparative study of three commercial multiplex molecular assays revealed significant differences in clinical performance. The Seegene Anyplex II RV16 and BioFire FilmArray RP2.1 plus demonstrated high overall sensitivity, at 96.6% and 98.2%, respectively, while the QIAstat-Dx showed inferior sensitivity at 80.7% [60]. The FilmArray panel offers a distinct advantage with its rapid turnaround time of approximately 45 minutes and inclusion of bacterial targets, making it suitable for acute clinical decision-making. However, its lower specificity for rhinovirus/enterovirus (88.4%) requires consideration. Conversely, the QIAstat-Dx platform struggled with detecting coronaviruses and parainfluenza viruses, missing 41.7% and 28.6% of positive specimens, respectively [60].
Novel and Emerging Multiplex Platforms
Table 2: Analytical Performance of Novel Multiplex Assays
| Assay Technology | Target Pathogens | Limit of Detection (LOD) | Turnaround Time | Key Feature |
|---|---|---|---|---|
| QBs-based MF-LFA [61] | SARS-CoV-2, ADV, IAV | 41-120 copies/mL | 20 minutes | 200-1220x more sensitive than colloidal gold LFA |
| FMCA-based Multiplex PCR [62] | SARS-CoV-2, IAV, IBV, RSV, hADV, MP | 4.94-14.03 copies/μL | 1.5 hours | 86.5% cheaper than commercial kits; cost: ~$5/sample |
| Multiplex pVNT [63] | SARS-CoV-2 variants (ancestral & variants) | N/A (Serological) | High-throughput | Measures neutralizing antibodies against multiple variants simultaneously |
Recent technological innovations have focused on improving sensitivity, reducing costs, and increasing throughput. A quantum dot nanobeads-based multiplex fluorescence lateral flow immunoassay (QBs-based MF-LFA) demonstrated exceptional sensitivity for SARS-CoV-2, adenovirus (ADV), and influenza A virus (IAV), with limits of detection of 56, 120, and 41 copies/mL, respectively. This represents a 200 to 1220-fold improvement in sensitivity over traditional colloidal gold-based lateral flow assays while maintaining performance comparable to PCR techniques [61].
A novel laboratory-developed test utilizing fluorescence melting curve analysis (FMCA) for six respiratory pathogens achieved limits of detection between 4.94 and 14.03 copies/μL with high precision (intra- and inter-assay coefficients of variation ≤0.70% and ≤0.50%) [62]. This assay offers significant cost advantages at approximately $5 per sample, which is 86.5% cheaper than commercial multiplex PCR kits, making it particularly suitable for resource-limited settings and large-scale outbreak screening [62].
For serological surveillance, a multiplexed, lentivirus-based pseudovirus neutralization assay (pVNT) enables high-throughput measurement of neutralizing antibodies against multiple SARS-CoV-2 variants simultaneously. This platform shows no significant differences in EC50 titers between single and multiplexed formats, confirming its reliability for assessing vaccine-induced immunity and variant cross-protection [63].
Experimental Protocols and Methodologies
Protocol for QBs-based Multiplex Fluorescence LFA
The QBs-based multiplex fluorescence LFA employs freeze-dried quantum dot nanobeads (QBs) conjugated to detection antibodies, significantly enhancing stability and shelf-life up to 8 months [61].
Key Steps:
- Probe Preparation: Water-soluble carboxylated CdSe/ZnS quantum dot nanobeads (e.g., FM610C, 365 nm excitation/610 nm emission) are conjugated to monoclonal detection antibodies against SARS-CoV-2, ADV, and IAV using EDC/NHS chemistry. The conjugated QBs are then freeze-dried to enhance stability [61].
- Strip Configuration: The lateral flow strip contains three test lines and one control line pre-coated with capture antibodies specific to each target and goat anti-mouse IgG, respectively [61].
- Sample Processing: Clinical samples (nasopharyngeal swabs) are mixed with the reconstituted freeze-dried QB probes and incubated to allow complete antigen-antibody reaction [61].
- Detection: The mixture is applied to the strip, and results are read within 20 minutes using a portable fluorescence reader (e.g., FIC-S1). The fluorescence signal is quantified for each test line, enabling sensitive quantification of the targets [61].
Protocol for FMCA-based Multiplex PCR
The FMCA-based method differentiates pathogens based on the unique melting temperatures (Tm) of hybridization probes, eliminating the need for multiple fluorescent channels and reducing assay cost and complexity [62].
Key Steps:
- Nucleic Acid Extraction: RNA/DNA is co-extracted from nasopharyngeal swabs in viral transport media using an automated system (e.g., Zhuhai Hema Medical Instrument) with an RNA/DNA extraction kit. For frozen samples, a pre-processing step involving centrifugation and resuspension in saline is recommended to remove debris and inhibitors [62].
- Primer and Probe Design: Primers and probes target conserved regions: SARS-CoV-2 (
EandNgenes), IAV (Mgene), IBV (NS1gene), RSV (Mgene), hADV (hexongene), and MP (CARDS toxingene). Probes are modified with tetrahydrofuran (THF) residues at variable positions to minimize the impact of base mismatches and enhance hybridization stability across variants [62]. - Reverse Transcription-Asymmetric PCR: The reaction uses a one-step enzyme mix with unequal primer ratios to favor single-stranded DNA production, improving probe accessibility. Cycling conditions: 50°C for 5 min, 95°C for 30 s, followed by 45 cycles of 95°C for 5 s and 60°C for 13 s [62].
- Melting Curve Analysis: Post-PCR, a melting curve analysis is run from 40°C to 80°C at a rate of 0.06°C/s. Specific melting peaks corresponding to each pathogen are identified, with the
Tmvalue serving as the discriminant [62].
Workflow Visualization: FMCA-based Multiplex PCR
The following diagram illustrates the logical workflow and key principles of the FMCA-based multiplex PCR assay:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Multiplex Assay Development
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| Carboxylated CdSe/ZnS QBs (FM610C) [61] | Fluorescent label for immunoassays; enables ultra-sensitive detection. | Signal generator in QBs-based MF-LFA for detecting SARS-CoV-2, ADV, and IAV. |
| Monoclonal Antibodies (Capture & Detection) [61] | Specific binding to target viral antigens (e.g., SARS-CoV-2 NP). | Immobilized on test lines (capture) or conjugated to QBs (detection) in LFA. |
| EDC/NHS Chemistry Reagents [61] | Activate carboxyl groups on QBs for covalent conjugation to antibodies. | Covalent coupling of detection antibodies to quantum dot nanobeads. |
| THF-Modified DNA Probes [62] | Hybridization probes with abasic sites to tolerate sequence variations. | Probe design in FMCA-based PCR to ensure robust detection of viral variants. |
| Gateway ORFeome Collections [64] | Pre-cloned ORF libraries for high-throughput protein interaction studies. | Screening SARS-CoV-2 - human Protein-Protein Interactions (PPIs) via pooled PPIseq. |
| Lentivirus Pseudovirus Particles [63] | Safe, non-replicating viral particles displaying variant spike proteins. | Multiplexed pseudovirus neutralization assays (pVNTs) for nAb measurement. |
The comparative analysis presented in this guide demonstrates that multiplex assays represent a powerful and diverse toolkit for respiratory pathogen detection. The choice between commercial panels like the FilmArray RP2.1 plus and novel platforms such as the QBs-based MF-LFA or FMCA-based PCR depends on the specific application requirements, including needed turnaround time, required sensitivity, target spectrum, and available budget. The significant advances in sensitivity, cost-effectiveness, and throughput highlighted herein are expanding the accessibility and utility of multiplex diagnostics. These technologies are poised to play an increasingly critical role in clinical diagnostics, therapeutic monitoring, and public health surveillance, ultimately enhancing our preparedness for and response to future respiratory epidemics.
Performance Optimization and Technical Challenges in SARS-CoV-2 Detection
Accurate detection of SARS-CoV-2 is fundamental to controlling transmission and treating COVID-19. However, false-negative results present a persistent challenge, particularly in scenarios involving low viral loads. These false negatives can occur throughout the infection timeline—during the early pre-symptomatic phase, during recovery when viral loads are declining, or due to suboptimal sample collection [65]. The implications are significant for both clinical management and public health, as undetected cases may inadvertently spread the virus. Understanding the technical factors contributing to these diagnostic limitations requires a comparative analysis of available molecular methods. This guide objectively compares the performance of various SARS-CoV-2 detection assays in low viral load conditions, providing researchers and clinicians with evidence-based data to inform test selection and interpretation, ultimately aiming to improve diagnostic accuracy in challenging cases.
Comparative Performance of Molecular Assays
Different diagnostic technologies exhibit varying levels of sensitivity, which directly impacts their false-negative rates, especially near the assays' limits of detection.
False-Negative Rates of Major Commercial Assays
A comprehensive comparative study of five SARS-CoV-2 molecular assays revealed substantial differences in performance. The findings demonstrated that assays incorporating a full nucleic acid extraction step prior to reverse transcription polymerase chain reaction were consistently more sensitive than those that omitted this process [66]. The assessed false-negative rates were as follows:
Table 1: Comparative Performance of SARS-CoV-2 Molecular Assays
| Assay Name | Manufacturer | Sensitivity (%) | False-Negative Rate (%) | Key Characteristics |
|---|---|---|---|---|
| CDC 2019 nCoV RT-PCR | CDC | 100 | 0 | Reference standard in this study [66] |
| Xpert Xpress SARS-CoV-2 | Cepheid | 97.6 | 2.4 | Targets E and N2 genes; LOD: 8.26 copies/mL [67] |
| TIB MOLBIOL/Roche z480 | Roche | 96.5 | 3.5 | Includes nucleic acid extraction [66] |
| Simplexa COVID-19 Direct | DiaSorin | 88.1 | 11.9 | Direct amplification approach [66] |
| ID Now COVID-19 | Abbott | 83.3 | 16.7 | Isothermal amplification technology [66] |
The study noted that most false-negative results occurred specifically in patients with low viral loads, as extrapolated from high cycle threshold (Ct) values [66]. This highlights a critical vulnerability across platforms when viral material is scarce in patient samples.
Discordant Testing Analysis and Real-World Performance
A discordant testing analysis of 100,001 samples found that the false-negative rate in patients with discordant results (initial negative followed by positive within 14 days) was approximately 9.3%, corresponding to a sensitivity of 90.7% in this specific subgroup [68]. This large-scale evaluation identified that most false negatives resulted from low SARS-CoV-2 viral concentrations in samples collected during different stages of infection. The analysis recommended that clinical evaluation should remain paramount and that RT-PCR results should not be the sole factor in excluding COVID-19, particularly when clinical suspicion remains high [68].
Advanced Detection Technologies
Digital Droplet PCR: Enhanced Sensitivity for Low Viral Load Detection
Emerging technologies offer promising alternatives for challenging detection scenarios. Droplet digital PCR (ddPCR) has demonstrated superior sensitivity compared to traditional RT-qPCR, particularly for samples with low viral loads [69]. A blinded comparative study found that while SYBR-Green RT-qPCR failed to diagnose positive samples with low viral loads and TaqMan Probe RT-qPCR produced positive signals only at very late Ct values, ddPCR successfully identified the low viral load sample as positive even at 10-fold diluted concentrations [69].
Table 2: Sensitivity Comparison Between RT-qPCR and ddPCR
| Method | Chemistry | Ability to Detect Low Viral Load | Relative Sensitivity |
|---|---|---|---|
| RT-qPCR | SYBR-Green | Not able to diagnose positive | Lower |
| RT-qPCR | TaqMan Probe | Positive at very late Ct values | Moderate |
| ddPCR | EvaGreen | Positive even at 10-fold dilution | Higher |
| ddPCR | Probe-based | Positive even at 10-fold dilution | Higher |
The partitioning process inherent to ddPCR technology enhances sensitivity by effectively concentrating the target and reducing the impact of inhibitors that might be present in the sample [69]. This makes it particularly valuable for applications requiring high sensitivity, including patient follow-up until complete remission and resolving inconclusive results from standard RT-qPCR testing.
Target Gene Performance in Low Viral Load Scenarios
The choice of viral target gene also influences detection capability in low viral load situations. A comparison of the cobas SARS-CoV-2 test (targeting ORF1a and E genes) with the Xpert Xpress SARS-CoV-2 assay (targeting N2 and E genes) on 24 presumptive positive samples with high Ct values found that the assay targeting the SARS-CoV-2 N2 gene detected more cases with low viral load compared to the assay utilizing the ORF1a region [67]. This observation aligns with other findings that the N gene may persist longer in clinical samples, making it a more reliable target for detecting infections with low viral loads [67].
Experimental Protocols for Sensitivity Assessment
Discordant Testing Analysis Protocol
The false-negative rate assessment protocol involved several methodical steps [68]:
- Sample Collection: Nasopharyngeal, oropharyngeal, deep nasal turbinate swabs, endotracheal aspirates, and bronchoalveolar lavages were collected in appropriate transport media.
- RNA Extraction: Nucleic acid extraction was performed on multiple platforms (QIAamp DSP Viral RNA Mini Kit, EMAG, MagNA Pure 96, and easyMAG).
- Primary Testing: A laboratory-developed RT-PCR test targeting the envelope (E) and RNA-dependent RNA-polymerase (RdRp) genes was used for initial screening.
- Discordant Sample Identification: Patients with an initial negative RT-PCR result followed by a positive result within 14 days were identified.
- Retesting Procedure: Negative samples from discordant specimens were retested using three alternate RT-PCR assays targeting the E gene and N1/N2 regions of the nucleocapsid genes.
- Quality Assessment: All discordant swabs were tested for human ribonuclease P (RNAse P) to assess sample quality.
A sample was considered a false negative if repeat testing yielded a positive result for at least two of three gene targets (E gene, N1, and/or N2) [68].
ddPCR Sensitivity Assessment Protocol
The sensitivity comparison protocol between ddPCR and RT-qPCR included these critical steps [69]:
- Sample Preparation: Blinded RNA samples from negative and positive rhinopharyngeal swabs were used.
- Reverse Transcription: 15 ng of total RNA was reverse transcribed using Superscript II with random hexamer primers.
- RT-qPCR Analysis:
- Serial dilutions of cDNA were prepared (1:1, 1:10, 1:20, 1:50, 1:100)
- Both SYBR-Green and TaqMan probe chemistries were evaluated
- CDC-validated 2019-nCoV_N1 primers and probe were used
- Amplification was performed on the LightCycler 480 System
- ddPCR Analysis:
- Both EvaGreen and probe-based ddPCR were performed
- Reaction mixes were partitioned into nanodroplets using the QX200 system
- The same primer sets as RT-qPCR were used for direct comparison
- Data Analysis: PCR efficiency, melting curve analysis, and expression rates were calculated for RT-qPCR, while absolute quantification was performed for ddPCR.
SARS-CoV-2 Replication Pathway and Detection Interference
The following diagram illustrates the SARS-CoV-2 replication cycle, highlighting key stages where detection can be challenged by low viral loads and where molecular diagnostic methods interact with this process.
SARS-CoV-2 Detection Challenge Points
The diagram highlights how low viral loads particularly impact detection during the uncoating and translation phases, where viral RNA and proteins are present in limited quantities. Molecular tests like RT-qPCR and ddPCR target viral RNA released during uncoating, while antigen tests detect viral proteins produced during translation. In low viral load scenarios, the reduced number of target molecules increases the likelihood of false negatives, with ddPCR demonstrating superior detection capabilities due to its partitioning technology that enhances sensitivity for scarce targets [69].
Essential Research Reagent Solutions
The following table catalogizes key reagents and materials essential for conducting sensitive SARS-CoV-2 detection experiments, particularly those focused on low viral load scenarios.
Table 3: Essential Research Reagents for SARS-CoV-2 Detection Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Universal Transport Media | Preserves specimen integrity during transport | Critical for maintaining RNA stability; alternatives validated due to shortages [65] |
| Nucleic Acid Extraction Kits (QIAamp, EMAG, MagNA Pure) | Isolates viral RNA from clinical samples | Essential for assays requiring extraction; impacts sensitivity [66] [68] |
| 2019-nCoV_N1 Primers/Probes | CDC-validated targets for N gene detection | Provides standardized detection approach; enables cross-study comparisons [69] |
| Reverse Transcriptase Enzymes | Converts viral RNA to cDNA | Essential first step for RT-PCR and ddPCR; choice impacts efficiency [69] |
| ddPCR Supermix (EvaGreen/Probe) | Enables droplet digital PCR reactions | Critical for partitioning technology; EvaGreen provides option without probe design [69] |
| RNAse P Assay Components | Assesses sample quality and collection | Controls for specimen adequacy; distinguishes true negatives from poor samples [68] |
| Positive Control Materials (AccuPlex) | Determines assay limit of detection | Serial dilutions establish analytical sensitivity; various materials used [65] |
These reagents form the foundation of reliable SARS-CoV-2 detection experiments. The selection of appropriate reagents directly impacts assay sensitivity, particularly when working with limited viral material. For instance, the choice between extraction-based versus direct amplification approaches can significantly influence false-negative rates in low viral load scenarios [66].
The comparative analysis of SARS-CoV-2 detection methods reveals significant differences in sensitivity and false-negative rates across platforms, particularly in challenging low viral load scenarios. Traditional RT-PCR assays demonstrate variable performance, with false-negative rates ranging from 2.4% to 16.7% in comparative studies [66]. Emerging technologies like ddPCR show enhanced sensitivity for detecting low viral loads, potentially offering solutions for cases where standard approaches fail [69]. The evidence indicates that target gene selection, nucleic acid extraction methods, and amplification technologies collectively influence detection capabilities. For researchers and clinicians working with SARS-CoV-2, this comparative guidance underscores the importance of matching methodological approaches to specific diagnostic scenarios, particularly when dealing with potentially low viral loads where false negatives would carry significant clinical and public health consequences.
The relentless evolution of SARS-CoV-2 has presented a formidable challenge to molecular diagnostics throughout the COVID-19 pandemic. Variant-driven diagnostic escape occurs when mutations in the viral genome disrupt the binding of primers and probes in real-time reverse transcription PCR (RT-qPCR) assays, potentially leading to false-negative results [70]. This phenomenon, also known as signature erosion, compromises the very tools essential for identifying infected individuals, implementing public health measures, and guiding clinical care [70]. The core of the issue lies in the fact that PCR assays are designed based on the genomic sequence of the pathogen known at a given time. As the virus evolves through sustained transmission, new variants emerge with mutations that may fall within the assay's target regions [70]. The diagnostic community has responded by developing innovative tools for in silico surveillance, such as the PCR Signature Erosion Tool (PSET), and novel wet-lab techniques to empirically test the impact of these mismatches, creating a critical area of comparative research for scientists and assay developers [70].
The Fundamental Impact of Mismatches on PCR Efficiency
The performance of a PCR assay hinges on the specific and efficient binding of primers and probes to their complementary target sequences. The physical parameters governing this interaction are well-established. In general, a 1% base mismatch can reduce the melting temperature (Tm) by 1.0–1.4°C, and single base pair mismatches can affect the Tm by as much as 10°C [70]. This decrease in Tm reduces the annealing rate of the DNA, directly impacting amplification efficiency.
The effect of a mismatch is not uniform; it depends on its position, type, and number. A single mismatch located more than 5 base pairs from the 3' end often has only a moderate effect, whereas mismatches closer to the 3' end can have a severe impact, sometimes completely blocking PCR amplification [70]. Research has shown that single mismatches can instigate a broad variety of effects, ranging from a minor shift of less than 1.5 cycle threshold (Ct) to a severe impact of more than 7.0 Ct [70]. The table below summarizes key factors affecting mismatch impact based on empirical studies.
Table 1: Factors Influencing the Impact of Primer/Probe Mismatches
| Factor | Impact on PCR Assay | Experimental Evidence |
|---|---|---|
| Position from 3' End | Mismatches >5 bp from 3' end are often tolerated; those nearer can cause severe failure [70]. | Single mismatches >5 bp have moderate effect; complete PCR blocking observed with 4 mismatches [70]. |
| Mismatch Type (Base Substitution) | Effects vary widely; A-A, G-A, A-G, C-C mismatches cause severe impact (>7.0 Ct shift) [70]. | A-C, C-A, T-G, G-T mismatches show minor impact (<1.5 Ct shift) [70]. |
| Number of Mismatches | Increased mismatches correlate with decreased efficiency and potential assay failure [70]. | Complete blocking of PCR reaction observed for 4 mismatches in systematic studies [70]. |
| Assay Design Robustness | Well-designed assays can maintain performance despite signature erosion [70]. | Most PCR assays proved extremely robust despite extensive mutation accumulation in SARS-CoV-2 [70]. |
Comparative Analysis of Commercial SARS-CoV-2 PCR Assays
Independent evaluations are crucial for understanding how different commercially available assays perform against evolving variants. A 2022 study compared the analytical and clinical performance of three commercial RT-qPCR kits: the Allplex SARS-CoV-2/FluA/FluB/RSV Assay (Seegene), the Standard M nCoV Real-Time Detection Kit (SD Biosensor), and the U-TOP COVID-19 Detection Kit (Seasun Biomaterials) [71].
The study found that all three assays demonstrated comparable overall clinical performance, with sensitivities ranging from 98.88% to 100% and specificities from 99.38% to 100% [71]. However, the sensitivity of individual target genes within the assays was more variable. For instance, in the Allplex and U-TOP kits, the S and ORF1ab genes were the most sensitive targets, whereas for the Standard M kit, the RdRp gene showed higher sensitivity than the E gene [71]. This highlights that performance is influenced more by the specific primer and probe design than the choice of target gene alone.
Table 2: Comparative Performance of Commercial SARS-CoV-2 RT-qPCR Assays
| Assay Name | Target Genes | Limit of Detection (Copies/mL) | Clinical Sensitivity | Clinical Specificity | Impact of B.1.351 (Beta) Variant |
|---|---|---|---|---|---|
| Allplex SARS-CoV-2/FluA/FluB/RSV | S, RdRp, N | 650 - 1300 | 98.88% | 100% | No prominent Ct shift or target dropout [71]. |
| Standard M nCoV | E, RdRp | 650 - 1300 | 100% | 99.38% | No prominent Ct shift or target dropout [71]. |
| U-TOP COVID-19 | ORF1ab, N, S, E | 650 - 1300 | 100% | 100% | No prominent Ct shift or target dropout [71]. |
The study also specifically tested these assays against the B.1.351 (Beta) variant of concern. Reassuringly, the mean differences in Ct values between the wild-type and B.1.351 RNA controls were within 1.0 for each target across all assays, and no prominent Ct value shifts or target dropouts were observed [71]. This suggests that the primer-probe sets in these particular kits were not critically affected by the mutations present in the Beta variant.
Experimental Protocols for Evaluating Mismatch Effects
To systematically evaluate the impact of mismatches, robust experimental methodologies are required. The following protocol, adapted from a 2025 study, details the process for in vitro testing of in silico predictions [70].
Assay and Template Selection
- Assay Selection: Select multiple PCR assays (e.g., 16 assays as in the foundational study) that target different regions of the SARS-CoV-2 genome and for which in silico analysis predicts signature erosion due to circulating variants [70].
- Template Generation: Generate synthetic DNA or RNA templates that correspond to both the wild-type sequence and variant sequences. These templates should encompass the natural permutations of mutations found in the primer and probe binding sites. Over 200 such templates can be used to cover a wide range of mismatch scenarios [70].
PCR Amplification and Data Collection
- Amplification Run: Perform RT-qPCR reactions using the selected assays and the synthetic templates. Reactions should include a range of template concentrations (e.g., tenfold serial dilutions) to assess amplification efficiency [70] [72].
- Data Capture: For each reaction, record key metrics, including:
- Cycle Threshold (Ct) Value: The cycle at which the fluorescent signal crosses the threshold.
- Amplification Efficiency: Calculated from the standard curve generated using serial dilutions.
- Y-Intercept: Reflects the theoretical Ct value at one viral RNA copy per reaction, indicating sensitivity [72].
- Change in Melting Temperature (ΔTm): If applicable, measure the shift in Tm due to mismatches [70].
Data Analysis
- Efficiency and Sensitivity Calculation: Plot the log of the template concentration against the Ct value to generate a standard curve. The slope of the line is used to calculate PCR efficiency (E) using the formula: ( E = (10^{-1/slope} - 1) \times 100\% ). A slope of -3.32 corresponds to 100% efficiency [72].
- Impact Assessment: Compare the efficiency, Ct value shifts, and y-intercept values between the wild-type and mismatch-containing templates. A significant increase in Ct value or drop in efficiency indicates a negative impact of the mismatch [70] [72].
This experimental workflow is depicted in the following diagram.
Case Studies and Data-Driven Evidence
The Charité RdRp Assay: A Documented Sensitivity Failure
A pivotal 2020 study in Nature Microbiology provided a clear example of how a single mismatch can critically impact diagnostic sensitivity. The study compared nine primer-probe sets from four major assays (China CDC, US CDC, Charité, and HKU) [72]. The RdRp-SARSr (Charité) confirmatory primer-probe set exhibited markedly lower sensitivity, with Ct values 6–10 cycles higher than other sets, meaning it required significantly more cycles to detect the virus [72]. The authors identified a mismatch in the reverse primer to the circulating SARS-CoV-2 strains as the likely cause. This flaw resulted in a 0–50% detection rate at low viral concentrations (1–10 copies/μL), whereas other sets achieved 100% detection at 100 copies/μL [72]. This case underscores the critical importance of rigorous empirical validation and continuous monitoring of assay performance.
General Assay Robustness and the PANDAA Solution
Contrasting with the Charité case, a large-scale 2025 wet-lab study testing 16 assays with over 200 synthetic templates found that the majority of PCR assays proved to be extremely robust, performing well despite the accumulation of mutations in SARS-CoV-2 [70]. This resilience suggests that many well-designed assays can tolerate a degree of signature erosion without complete failure.
To proactively address the challenge of variability, innovative approaches that violate conventional design principles have emerged. The Pan-Degenerate Amplification and Adaptation (PANDAA) assay is one such breakthrough [73]. PANDAA uses ultra-degenerate primers with 3' termini that intentionally overlap the probe-binding site. During the initial PCR cycles, these primers adapt the target through site-directed mutagenesis, replacing sequence variation within the probe-binding site and creating a homogeneous amplicon population [73]. This elegant method allows for the detection of single-nucleotide variations even in highly variable genomic regions, as demonstrated in its application for HIV drug resistance mutation testing [73].
The following diagram illustrates the core mechanism of the PANDAA technology.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers developing or evaluating SARS-CoV-2 molecular assays to address diagnostic escape, a core set of reagents and tools is essential. The following table details key components of this research toolkit.
Table 3: Essential Research Reagents and Materials for Assay Development and Evaluation
| Tool/Reagent | Function/Description | Example Use Case |
|---|---|---|
| Synthetic RNA/DNA Templates | Controlled templates representing wild-type and variant sequences with specific mutations in primer/probe regions [70]. | Empirical testing of mismatch impact on assay efficiency and sensitivity [70] [72]. |
| TaqMan Probes with MGB-NFQ | Hydrolysis probes with a 5' reporter dye, a 3' non-fluorescent quencher (NFQ), and a Minor Groove Binder (MGB) that increases Tm [74]. | Enhances allelic discrimination and assay sensitivity; shorter, more specific probes [74]. |
| Locked Nucleic Acids (LNAs) | Modified nucleotides that act as molecular anchors, increasing primer affinity and countering thermodynamic instability from mismatches [73]. | Incorporated into primers (e.g., in PANDAA) to stabilize binding to variable targets [73]. |
| RNA Transcript Standards | In vitro transcribed RNA of defined length and concentration from key genomic regions (e.g., N, RdRp, E) [72]. | Used as positive controls, for assay validation, and to generate standard curves for quantifying viral load [72]. |
| PCR Signature Erosion Tool (PSET) | An in silico application to monitor the performance of diagnostic tests against a database of pathogen genomic sequences [70]. | Proactive surveillance of circulating variants to predict potential assay failures before they become widespread [70]. |
The ongoing battle between pathogen evolution and diagnostic accuracy makes the study of variant-driven diagnostic escape a critical pursuit. Evidence shows that the impact of primer-probe mismatches is not always catastrophic; many well-designed assays demonstrate remarkable robustness [70]. However, documented failures, such as with the Charité RdRp assay, highlight the real-world consequences of signature erosion and the non-negotiable need for continuous performance monitoring [72]. The future of resilient molecular diagnostics lies in a multi-faceted strategy: leveraging in silico surveillance tools like PSET for early warning, employing rigorous wet-lab validation protocols with synthetic templates, and embracing next-generation assay technologies like PANDAA that are engineered from the outset to tolerate genetic diversity [70] [73]. For researchers and drug development professionals, a deep understanding of these principles and tools is essential for developing reliable diagnostics that can withstand the pressure of viral evolution both in the current pandemic and in future public health emergencies.
The reliability of SARS-CoV-2 diagnostic and research data is fundamentally rooted in the pre-analytical phases of sample management. Variations in transport media and storage conditions can significantly alter viral RNA integrity, directly impacting the sensitivity and accuracy of subsequent molecular analyses [75] [76]. This guide provides a comparative analysis of these critical variables, framing them within a broader evaluation of molecular methods for SARS-CoV-2 research. For scientists, researchers, and drug development professionals, understanding these factors is essential for ensuring data validity, enabling cross-study comparisons, and developing robust diagnostic protocols [77] [13].
Critical Foundations in Sample Collection
The journey of a biospecimen from collection to analysis is fraught with potential pitfalls that can compromise its quality. Adherence to fundamental principles of sample collection is the first and most crucial step in ensuring the integrity of downstream molecular applications.
Core Principles for Sample Integrity
Several non-negotiable practices underpin successful sample collection and handling. Comprehensive documentation is paramount; a sample submission form must be fully completed with all relevant case details, including date of collection, suspected diseases, and animal or patient identification [75]. Accurate labeling is equally critical; labels must withstand extreme conditions, including multiple freeze-thaw cycles and long-term storage in liquid nitrogen (-196°C) without detaching, cracking, or fading [75]. Furthermore, aseptic technique is vital to avoid contamination from non-sterile containers, faecal material, or water, which can lead to haemolysis or false results [75]. Finally, rapid transport with secure, leak-proof packaging using absorbent materials is mandatory to protect both the sample and the personnel handling it [75].
Sample Type Considerations
The choice of sample type influences the optimal collection and storage approach. For SARS-CoV-2, nasopharyngeal swabs and saliva samples are most common, but the principles extend to other sample types used in broader research contexts [13].
- From Live Subjects/Animals: Key samples include whole blood (with EDTA or heparin as anticoagulants), paired serum samples, faeces, and various swabs (e.g., nasopharyngeal, oropharyngeal) [75]. For blood, the tube must be gently inverted several times to mix the anticoagulant thoroughly without causing haemolysis [75].
- From Deceased Subjects/Necropsy: Ideal samples include tissues like liver, spleen, kidney, lung, lymph node, and brain. These should be preserved both on ice or in virus transport medium (VTM) for molecular work and in 10% buffered formalin for histopathology [75].
Comparative Analysis of Transport Media
Transport media serve to preserve pathogen viability and nucleic acid integrity from the moment of collection until laboratory processing. The choice of medium can profoundly affect the stability of the SARS-CoV-2 RNA target.
Virus Transport Media (VTM) and Alternatives
Virus Transport Media (VTM) is the standard for virological samples, including swabs and tissue specimens. Its formulation is designed to mimic the host environment, typically containing a pH buffer, proteins to stabilize the virus, and a cocktail of antibiotics to prevent bacterial and fungal overgrowth [75]. A critical technical consideration is the sample-to-medium proportion, which should be maintained between 1:5 to 1:10 for optimal preservation [75]. The use of dry swabs without transport medium is strongly discouraged for virological examination, as the virus may rapidly degrade without the stabilizing components of the medium [75].
While VTM is the gold standard for transport, other mediums are used for specific testing modalities. For instance, saline solutions can be used for certain rapid tests, but they lack the stabilizers and nutrients needed for long-term viral RNA integrity. Lysis buffers, which contain detergents to break open the viral envelope and stabilize the released nucleic acids, are increasingly used in molecular applications, especially for point-of-care or direct amplification protocols [77].
Impact of Medium on Assay Performance
The choice of transport medium directly influences the performance of molecular diagnostic assays. A 2024 study comparing one-step real-time PCR (RT-qPCR) and one-step RT-LAMP for SARS-CoV-2 detection highlights the practical implications of sample type and medium [13]. In this study, all samples—nasopharyngeal, saliva, and urine—were placed in 2 ml of fresh VTM and maintained in a cold chain during transfer to the laboratory, where they were stored at -70°C prior to RNA extraction [13]. This standardized use of VTM was crucial for ensuring the reliability of the subsequent comparative analysis.
The table below summarizes key characteristics of transport media and their implications.
Table 1: Comparison of Transport Media Characteristics
| Media Type | Key Components | Primary Function | Suitable Sample Types | Key Considerations |
|---|---|---|---|---|
| Virus Transport Media (VTM) | pH buffer, protein stabilizer, antibiotics | Preserve viral integrity and nucleic acids | Nasopharyngeal swabs, oropharyngeal swabs, tissues | Sample-to-medium ratio (1:5 to 1:10) is critical [75] |
| Universal Transport Media (UTM) | Similar to VTM, with broader spectrum | Preserve a wider range of pathogens (viral, bacterial) | Similar to VTM | Often used interchangeably with VTM for SARS-CoV-2 |
| Lysis Buffer | Detergents, chaotropic salts | Lyse virus and stabilize released nucleic acids | Swabs, saliva | Suitable for direct-to-PCR workflows; may not be for culture |
Impact of Storage Conditions on Sample Integrity
Temperature is one of the most critical factors affecting the stability of SARS-CoV-2 RNA in stored samples. Implementing a rigorous temperature management protocol is non-negotiable for preserving sample utility for future research and re-testing.
Temperature Guidelines for Biospecimens
Different sample types and components have specific temperature tolerances. Exceeding these ranges can lead to degradation of viral RNA and biomolecules, rendering the sample useless for sensitive molecular assays.
Table 2: Recommended Storage Conditions for Different Sample Types
| Sample Type | Short-Term Storage (up to 1 week) | Long-Term Storage | Critical Handling Notes |
|---|---|---|---|
| Serum | Refrigerated (2 – 6°C) [75] | Frozen (≤ -20°C) [75] | Avoid repeated freeze-thaw cycles. |
| Swabs in VTM | Refrigerated (2 – 6°C) [75] | Frozen (≤ -70°C) [75] | Storage at -20°C is not sufficient for long-term integrity. |
| Tissue Samples | Refrigerated (2 – 6°C) [75] | Frozen (≤ -70°C) [75] | For RNA work, snap-freezing in liquid nitrogen is ideal. |
| Whole Blood | Refrigerated (2 – 6°C) [75] | Do not freeze. [75] | Freezing causes haemolysis, which compromises serum/plasma. |
The Role of Temperature Monitoring
Equipment designed for sample storage must ensure optimum temperature conditions and have sufficient capacity [75]. Regular temperature monitoring is essential for all types of storage equipment, from refrigerators to ultra-low temperature freezers and liquid nitrogen tanks [75]. The use of continuous monitoring systems with alarms is a best practice in biorepositories to prevent catastrophic loss of samples due to equipment failure.
For long-term biobanking, the stability of biomarkers is a primary concern. Samples should be aliquoted into multiple small vials to avoid repeated freeze-thaw cycles, and each person's specimen should be stored in at least two different physical locations to mitigate the risk of loss from freezer failure [78]. A careful record of sample disbursement, potentially using a barcode system, is also critical for tracking which specimens have been thawed and refrozen, as this can influence future analytical results [78].
Comparative Performance of Molecular Detection Methods
The ultimate test of sample quality is its performance in molecular assays. The integrity of viral RNA, preserved through appropriate transport and storage, directly determines the sensitivity and reliability of different diagnostic platforms.
Experimental Comparison: RT-qPCR vs. RT-LAMP
A 2024 study provides a robust, head-to-head comparison of two key molecular methods: one-step real-time PCR (RT-qPCR) and one-step Reverse Transcriptase Loop-Mediated Isothermal Amplification (RT-LAMP) [13]. The study utilized 342 clinical samples (nasopharyngeal and saliva) stored in VTM and at -70°C, ensuring sample integrity.
The RT-qPCR assay targeted the SARS-CoV-2 N gene and a human internal control (RNase P) using the FAM and ROX fluorescent channels, respectively. The thermal cycling protocol involved reverse transcription at 50°C for 20 minutes, initial denaturation at 95°C for 3 minutes, followed by 45 cycles of 95°C for 15s and 55°C for 40s [13].
In parallel, the one-step RT-LAMP assay was designed to target the N gene with a set of six primers (F3, B3, FIP, BIP, LF, LB). The reaction was conducted at 40°C for 36 minutes (with the first six minutes for reverse transcription) using Bst DNA/RNA Polymerase [13]. The study's findings are summarized below.
Table 3: Performance Comparison of RT-qPCR and RT-LAMP from a 2024 Study
| * | Parameter | RT-qPCR (TaqMan One-Step) | RT-LAMP (One-Step) |
|---|---|---|---|
| Target Gene | N gene & RNase P (internal control) [13] | N gene (NC_045512.2) [13] | |
| Run Temperature | Multiple temperatures (50°C, 95°C, 55°C) [13] | Isothermal (40°C) [13] | |
| Run Time | ~90 minutes [13] | 36 minutes [13] | |
| Limit of Detection | Varies by kit; generally high | 555 RNA copies/mL [77] or 1x101 dilution [13] | |
| Sensitivity | Reference method | 95% [77] | |
| Specificity | Reference method | 100% [77] [13] | |
| Agreement (Kappa, κ) | Reference method | 93-94% (compared to RT-qPCR) [13] | |
| Key Advantage | High sensitivity, gold standard | Simplicity, speed, cost-effectiveness, suitable for point-of-care [13] |
Other Molecular Platforms
Beyond RT-qPCR and RT-LAMP, other platforms have been validated for SARS-CoV-2 detection. A 2020 study compared the RealStar SARS-CoV-2 RT-PCR, ePlex SARS-CoV-2, and the CDC COVID-19 RT-PCR tests, finding comparable analytical performance among them [79]. Furthermore, the SARS-CoV-2 Isothermal Molecular Assay (SIMA), the first molecular diagnostic developed in Nigeria for SARS-CoV-2, uses recombinase amplification coupled with fluorescent detection. SIMA runs at 40°C for 36 minutes, has a detection limit of 555 RNA copies/mL, and reported a sensitivity of 95% and specificity of 100% [77]. This underscores the global effort to create adaptable diagnostics and confirms that isothermal methods like LAMP and recombinase amplification are viable alternatives to PCR, particularly in resource-constrained settings.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting research on SARS-CoV-2, from sample collection to molecular analysis.
Table 4: Essential Research Reagents and Materials for SARS-CoV-2 Sample Processing
| * | Item | Function/Description | Example Use Case |
|---|---|---|---|
| Virus Transport Media (VTM) | Preserves viral integrity during transport; contains antibiotics and stabilizers. [75] | Collection and transport of nasopharyngeal swabs. | |
| EDTA Tubes (Lavender-top) | Anticoagulant for whole blood collection via calcium chelation. [75] [78] | Collecting blood for DNA extraction or plasma analysis. | |
| Heparin Tubes (Green-top) | Anticoagulant; an alternative to EDTA for some applications. [75] [78] | Collecting whole blood for various molecular assays. | |
| Serum Tubes (Red-top) | Tubes without additives for serum collection. [75] | Collecting blood for serology and mineral analysis. | |
| Bst DNA/RNA Polymerase | Key enzyme for RT-LAMP reactions; enables isothermal amplification. [13] | One-step RT-LAMP assay for SARS-CoV-2 detection. | |
| LAMP Primers | A set of 6 primers targeting 8 distinct regions of a gene for high specificity. [13] | Amplifying the SARS-CoV-2 N gene in RT-LAMP assays. | |
| Proteinase K | Enzyme that degrades proteins and inactivates nucleases. [13] | Lysing samples during RNA extraction. | |
| RNA Extraction Kit | Silica-membrane based system to purify viral RNA from samples. [13] | Isolating RNA from nasopharyngeal swabs in VTM. |
Visualizing Molecular Workflows
The following diagrams illustrate the key experimental workflows for the two primary molecular methods discussed, highlighting the procedural and logistical relationships.
RT-qPCR Diagnostic Workflow
RT-LAMP Diagnostic Workflow
The comparative analysis of molecular methods for SARS-CoV-2 research unequivocally demonstrates that the analytical result is only as reliable as the sample process that precedes it. Transport media, storage temperature, and handling protocols are not mere logistical details but are foundational to data integrity. While RT-qPCR remains the gold standard for sensitivity, isothermal methods like RT-LAMP and SIMA offer compelling advantages in speed, cost, and simplicity, making them increasingly viable for point-of-care and resource-limited settings [77] [13]. The choice of diagnostic platform must therefore be made in concert with a rigorous sample management policy. For the scientific community, adherence to standardized protocols for sample collection, processing, and storage is the indispensable prerequisite for generating valid, reproducible, and comparable data in the ongoing fight against COVID-19 and future pandemic threats.
In the field of molecular biology, particularly in SARS-CoV-2 research, the reliability of data from techniques like RT-qPCR and RNA-Seq is fundamentally dependent on the quality of the isolated RNA. Inefficient extraction or the presence of inhibitory substances can lead to false negatives or inaccurate quantification, compromising research conclusions and diagnostic outcomes [80]. For professionals in research and drug development, establishing robust quality control metrics is not optional but a necessity for generating valid, reproducible data. This guide provides a comparative analysis of methods and metrics for monitoring RNA extraction efficiency and detecting inhibition, framing them within the critical context of SARS-CoV-2 molecular research.
Core Metrics and Definitions
RNA Extraction Efficiency
RNA extraction efficiency measures the effectiveness of the RNA isolation process in recovering the total RNA present in a original sample. It is critical for ensuring that the subsequent analysis reflects the true biological condition, especially for low-abundance targets. Low extraction efficiency can disproportionately affect the detection of scarce transcripts, leading to biased data [81].
PCR Inhibition
PCR inhibition occurs when substances co-extracted with the nucleic acids interfere with the enzymatic reactions of reverse transcription or polymerase chain reaction. These inhibitors can cause reduced sensitivity (false negatives) or inaccurate quantification in RT-qPCR assays. Common inhibitors include polyphenolic compounds from plants, polysaccharides, and various components in complex matrices like feces or wastewater [82] [81].
Methods for Assessing Extraction Efficiency
Process Control Viruses
The use of an exogenous process control virus is considered a best practice for precisely quantifying RNA extraction efficiency. The control virus is added to the sample lysate at a known concentration before the extraction begins. By measuring the amount of control RNA recovered after extraction, the efficiency of the entire process can be calculated.
MS2 Phage-Like Particles (MS2 PLP) have been developed as an ideal process control for the detection of enteric RNA viruses. They are non-infectious, genetically distinct from native pathogens to prevent cross-reactivity, and share similar morphological and physiochemical properties with target viruses, ensuring they undergo similar extraction dynamics [83]. One study packaged a unique, non-naturally occurring RNA sequence into MS2 capsids, creating a highly specific and stable control [83].
Mengovirus (MC0) and Murine Norovirus (MNV) are also utilized as process controls. A study on detecting foodborne viruses used these viruses as controls to compare two RNA extraction methods. The recovery rates of these controls were used to directly quantify extraction efficiency [81].
Calculation of Extraction Efficiency
The extraction efficiency is typically calculated as a percentage recovery using the following formula:
% Recovery = (Quantity of Control RNA Measured Post-Extraction / Known Quantity of Control RNA Added Pre-Extraction) × 100
Experimental data from viral recovery studies illustrates how this metric is used to evaluate different extraction methods. For example, an optimised direct lysis method for foodborne viruses demonstrated a mean recovery of 44 ± 38% for MNV, significantly outperforming a modified ISO 15216 standard method, which recovered only 5 ± 11% [81].
Methods for Detecting PCR Inhibition
External RNA Controls
The use of external RNA controls involves adding a known quantity of control RNA to the purified RNA sample after the extraction process, just before the RT-qPCR reaction. Significant suppression of the control's amplification signal compared to its performance in a clean background (e.g., water) indicates the presence of inhibitors in the RNA eluate [83].
Internal Amplification Controls (IAC)
An IAC is a non-target nucleic acid sequence co-amplified in the same reaction tube as the target of interest. Inhibition is detected if the amplification of the IAC is delayed or suppressed. The European Committee for Standardization mandates the use of such controls in diagnostic assays to monitor for RT-qPCR inhibition [83].
Assessment of Inhibition
Inhibition is often identified by a significant increase in the quantification cycle value of a control compared to its expected value. The degree of inhibition can be quantified. One study on foodborne viruses reported inhibition of RT-qPCR amplification using a percentage metric, with their new direct lysis method showing significantly lower inhibition (5 ± 10% to 13 ± 14%) for various viral targets compared to the older method (34 ± 36% to 48 ± 40%) [81].
Comparative Data from Experimental Studies
Comparison of RNA Extraction Kits from Bacterial Cultures
A 2015 study directly compared three total RNA extraction methods for Pseudomonas aeruginosa and evaluated their performance for total RNA sequencing.
Table 1: Comparison of Total RNA Extraction Kits for Bacteria
| Extraction Method | Reported RNA Yield | RNA Integrity (RIN) | Small RNA Content | gDNA Contamination |
|---|---|---|---|---|
| Phenol-free kit (Amresco) | Highest | 9.85 ± 0.3 | Good | Minimal post-DNase treatment |
| RNeasy Mini Kit (Qiagen) | Moderate | Good | Trace amounts | Required DNase treatment |
| TRI Reagent (MRC) | Lowest | Not Specified | Enriched | Required DNase treatment |
The study concluded that the Phenol-free kit yielded the highest quality RNA with excellent integrity and a good representation of both large and small RNAs, making it ideal for comprehensive transcriptome studies [84].
Comparison of Viral RNA Recovery and Inhibition
Research comparing methods for viral RNA extraction from complex matrices like fruits and vegetables provides clear data on efficiency and inhibition.
Table 2: Comparison of Viral RNA Extraction Methods from Food Matrices
| Extraction Method | Mean MC0 Recovery | Mean MNV Recovery | Reported RT-qPCR Inhibition |
|---|---|---|---|
| Optimised Direct Lysis (Method A) | 36 ± 31% | 44 ± 38% | 5 ± 10% to 13 ± 14% |
| Modified ISO 15216 (Method B) | 9 ± 16% | 5 ± 11% | 34 ± 36% to 48 ± 40% |
The optimised method, which incorporated a larger lysis buffer volume and additives like pectinase and an inhibitor removal kit, demonstrated superior recovery and significantly lower inhibition [81].
Comparison of Cell Lysis and RNA Extraction from Fungi
A 2019 study compared different cell lysis methods and commercial kits for extracting RNA from the yeast Candida albicans, which has a tough cell wall.
Table 3: Comparison of Cell Lysis and RNA Extraction Methods for Yeast
| Method | Cell Lysis Efficiency | Relative RNA Yield | Key Findings |
|---|---|---|---|
| Lyticase Treatment | 95% | Not the highest | Effective, but outperformed by physical methods. |
| Bead Beating (Horizontal, in RiboPure Buffer) | 100% | Highest | Most effective lysis and highest yield. |
| Bead Beating (Vertical, in RiboPure Buffer) | 83% | Lower than horizontal | Orientation significantly impacts efficiency. |
| RiboPure Yeast Kit (Ambion) | N/A | Highest | Outperformed easyMAG and RNeasy Mini kits. |
The study established that a physical lysis method (horizontal bead beating) was more efficient than an enzymatic one (lyticase), and that the choice of commercial kit significantly impacted the final RNA yield [85].
Essential Research Reagent Solutions
The following reagents and kits are fundamental for implementing the quality control strategies discussed in this guide.
Table 4: Key Research Reagents for RNA QC
| Reagent/Kits | Primary Function | Example Use Case |
|---|---|---|
| Process Control Viruses (e.g., MS2 PLP, Mengovirus) | Quantify RNA extraction efficiency | Added to sample lysate pre-extraction to calculate % recovery [83] [81]. |
| External RNA Controls | Detect PCR inhibition | Added to purified RNA pre-RT-qPCR to check for suppression of amplification [83]. |
| DNase I (RNase-free) | Remove genomic DNA contamination | Essential pre-treatment for RNA-seq applications; requires validation of removal [84]. |
| Inhibitor Removal Kits | Minimize co-purification of PCR inhibitors | Used in complex matrices (e.g., food, feces) to improve RT-qPCR accuracy [81]. |
| RNA Stabilization Reagents (e.g., RNAlater) | Preserve RNA integrity in samples | Stabilizes transcriptomic profiles but may affect cell lysis efficiency [85]. |
| Silica-Based Nucleic Acid Binding | Purify and concentrate nucleic acids | Core technology in many kits; efficient for removing contaminants [82]. |
Experimental Workflow for Quality Control
The following diagram illustrates a comprehensive experimental workflow that integrates the quality control metrics discussed for a reliable RNA analysis pipeline.
The rigorous assessment of RNA extraction efficiency and PCR inhibition is a cornerstone of robust molecular research, including SARS-CoV-2 studies. As the comparative data shows, the choice of extraction methodology—from lysis to purification—profoundly impacts both the quantity and quality of the isolated RNA, and consequently, the reliability of downstream data. The consistent use of process controls like MS2 PLP and systematic checks for inhibition are non-negotiable practices for generating high-quality, reproducible results. For the scientific community, adhering to these quality control metrics is essential for advancing accurate diagnostics, therapeutic development, and a deeper understanding of viral pathogenesis.
Cycle Threshold (Ct) Value Interpretation and Correlation with Viral Infectivity
The Cycle Threshold (Ct) value is a semi-quantitative output generated by real-time reverse transcription polymerase chain reaction (RT-PCR), the gold standard method for diagnosing SARS-CoV-2 infection. This value represents the number of amplification cycles required for the target viral nucleic acid to exceed a threshold detection level, with lower Ct values indicating higher viral RNA concentrations in the original sample [86] [87]. While RT-PCR tests are typically reported qualitatively (positive/negative), the Ct value provides valuable indirect information about viral load, which has been extensively investigated for its potential correlations with patient infectivity and clinical outcomes [88]. Understanding the technical nuances, limitations, and appropriate interpretations of Ct values is crucial for researchers and clinicians utilizing molecular methods in SARS-CoV-2 research and patient management.
The fundamental relationship between Ct values and viral RNA concentration stems from the exponential nature of PCR amplification. Under ideal conditions, the viral cDNA doubles with each amplification cycle, meaning a difference of 3.3 cycles typically corresponds to an approximately 10-fold difference in the initial viral RNA concentration [86]. This inverse relationship makes Ct values a potentially useful proxy for viral load when interpreted within appropriate technical and clinical contexts. However, significant standardization challenges exist due to variations in laboratory methodologies, equipment, and reagent combinations across testing facilities [86] [89].
Technical Foundations and Methodological Variability
RT-PCR Assay Design and Implementation
SARS-CoV-2 RT-PCR assays target specific viral genes, most commonly the envelope (E), nucleocapsid (N), and RNA-dependent RNA polymerase (RdRp) genes [86] [9]. The testing process involves three critical analytical steps: viral RNA isolation from patient samples, conversion of RNA to complementary DNA (cDNA) via reverse transcription, and amplification of target viral genes [86]. These steps can be performed in a single-tube (one-step reaction) or split into separate procedures (two-step reaction), with variations in methodology contributing to inter-assay variability [86].
The analytical performance of different RT-PCR systems varies significantly. Comparative studies have demonstrated that the BGI RT-qPCR detection system provides superior sensitivity with lower detection limits and lower Ct values compared to other systems like the Norgen Biotek kit, though at higher cost [9]. Similarly, SYBR green-based detection methods have shown reduced specificity compared to TaqMan-based systems [9]. These performance differences directly impact Ct value measurements and complicate cross-study comparisons, highlighting the necessity of methodological transparency in research publications.
Factors Contributing to Ct Value Variability
Multiple pre-analytical and analytical factors contribute significant variability to Ct value measurements, limiting their direct comparability across different experimental setups:
- Sample Type and Quality: Ct values differ substantially between upper respiratory tract samples (nasopharyngeal, mid-turbinate, anterior nasal swabs), lower respiratory tract samples, and extra-pulmonary samples like stool and serum [86]. Poor sample collection technique or improper storage can degrade RNA quality, artificially elevating Ct values [90].
- RNA Extraction Methods: Different RNA extraction kits (e.g., Qiagen RNeasy, Invitrogen Purelink, BGI Magnetic Bead, Norgen Biotek) exhibit variations in extraction efficiency, impacting downstream Ct values [9].
- Platform and Reagent Variations: A study analyzing external quality assessment challenges found that quantitative results could deviate by more than ±4 cycles (up to 18 cycles in extreme cases) when using different combinations of extraction platforms/reagents and RT-PCR platforms/reagents [89].
- Target Gene Selection: Amplification efficiency varies between different viral gene targets (E, N, RdRp, ORF1ab), leading to different Ct values for the same patient sample [88].
Table 1: Factors Contributing to Ct Value Variability in SARS-CoV-2 RT-PCR
| Factor Category | Specific Examples | Impact on Ct Value |
|---|---|---|
| Pre-analytical | Sample type (NP swab vs. saliva) | Varies by viral shedding patterns [86] |
| Sample collection quality | Poor technique → Higher Ct [90] | |
| Time from symptom onset | Early/late infection → Lower/Higher Ct [87] | |
| Analytical | RNA extraction method | Varies by kit efficiency [9] |
| PCR instrumentation | Platform-specific differences [86] | |
| Target gene (N, E, RdRP) | Gene-specific amplification efficiency [88] | |
| Reaction chemistry (Taqman vs. SYBR) | Detection chemistry sensitivity [9] | |
| Biological | SARS-CoV-2 variant | Altered replication dynamics [91] |
| Host immune status | Vaccination/prior infection effects [86] |
Correlation Between Ct Values and Viral Infectivity
Viral Culture as a Surrogate for Infectivity
Viral culture remains the primary method for assessing infectious potential in research settings. Multiple studies have investigated the relationship between Ct values and the ability to isolate replication-competent virus, with consistent findings that lower Ct values (indicating higher viral RNA levels) correlate with higher rates of successful viral culture [89] [88]. However, the critical finding from recent research is that no absolute Ct value threshold reliably discriminates between infectious and non-infectious samples across different experimental conditions.
Evidence challenging simplistic Ct value thresholds for infectivity includes a study demonstrating infectious SARS-CoV-2 virus isolation from a clinical sample with a Ct value of 33 [89]. Another study found that 25% of samples with Ct values higher than 30 still yielded positive viral cultures [89]. Even more strikingly, research by Singanayagam and colleagues showed that culturable virus could be recovered more than 10 days after symptom onset despite Ct values >35 [89]. These findings collectively indicate that while probability of infectivity decreases with increasing Ct values, viable virus may be present even at high Ct values in some circumstances.
Temporal Dynamics of Infectivity
The relationship between Ct values and infectivity varies significantly throughout the infection course. During early infection, viral RNA levels typically peak around symptom onset, with corresponding low Ct values [86]. Infectious virus is most reliably recovered during this pre-symptomatic and early symptomatic phase. As the immune response develops, Ct values generally increase (viral RNA decreases), and the ability to culture virus declines, though the timing of this transition shows considerable inter-individual variation [89].
The duration of infectiousness is influenced by multiple factors beyond Ct values alone. Patients with severe disease or immunocompromised status may remain infectious for longer periods [86]. Additionally, emerging variants of concern may exhibit different relationships between Ct values and infectivity due to altered viral kinetics, though comprehensive comparative data for newer variants remains limited [89].
Table 2: Correlation Between Ct Values and Viral Culture Positivity in Research Studies
| Study Reference | Key Findings on Ct Value and Infectivity | Implications |
|---|---|---|
| Michel Drancourt et al. [89] | Isolated infectious virus from sample with Ct=33 | Challenged assumption that high Ct values indicate non-infectivity |
| Aron et al. [89] | 25% culture positivity (2/8 samples) with Ct>30 | Demonstrated viable virus present in high-Ct samples |
| Singanayagam et al. [89] | Culturable virus shed >10 days post-symptom with Ct>35 | Extended infectious period despite high Ct values |
| Systematic Review [88] | Lower Ct values associated with higher viral culture positivity | Established correlation trend but without definitive threshold |
Comparative Analysis of Molecular Methods
RT-PCR Versus Alternative Detection Methods
The performance characteristics of RT-PCR with Ct value interpretation differ significantly from alternative SARS-CoV-2 detection methods, particularly rapid antigen tests (RATs). While RT-PCR amplifies viral RNA to enable detection, RATs detect viral proteins without amplification, resulting in fundamentally different sensitivity profiles.
Analyses comparing these methodologies have revealed that RATs are frequently negative in PCR-positive samples with Ct values above 24-28 [89]. One comprehensive evaluation of 1,259,559 respiratory samples found that antigen tests could have missed 52.6-64.2% of SARS-CoV-2 infections detected by PCR, predominantly cases with higher Ct values [89]. This sensitivity gap highlights the complementary roles of these tests: RATs effectively identify individuals with high viral loads (low Ct values) who are likely highly infectious, while RT-PCR can detect lower viral loads (high Ct values) that may represent early infection, resolving infection, or non-infectious viral RNA persistence.
Standardization Initiatives and Method Harmonization
Significant efforts are underway to address the methodological variability in Ct value measurement. The lack of standardized protocols, reagents, and reporting frameworks currently limits the clinical utility of Ct values beyond individual research studies [86] [89]. International quality control programs and standardized reference materials would enable more meaningful comparisons across laboratories and studies.
The development of direct, extraction-free RT-PCR methods represents an important advancement for high-throughput testing, though with some sensitivity trade-offs. Studies have demonstrated that simply adding an RNase inhibitor can improve direct detection without complex sample processing [9]. Optimized direct methods typically detect approximately 10-fold less virus than conventional methods with RNA extraction, but offer reduced sample handling, cost, and processing time [9].
Research Reagents and Experimental Workflows
Essential Research Reagent Solutions
Table 3: Key Research Reagents for SARS-CoV-2 Ct Value Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| RNA Extraction Kits | Qiagen RNeasy, Invitrogen Purelink, BGI Magnetic Bead, Norgen Biotek Total RNA Purification Kit | Viral RNA isolation from clinical specimens [9] |
| RT-PCR Detection Kits | BGI Real-Time Fluorescent RT-PCR Kit, Norgen Biotek TaqMan RT-PCR Kit, Seegene Allplex Assay | Target amplification and detection [9] |
| One-Step RT-qPCR Master Mixes | NEB Luna Universal One-Step Kit | SYBR green-based detection [9] |
| Positive Controls | Twist Bioscience synthetic RNA standards | Assay validation and standardization [9] |
| Universal Transport Media | Thermo Fisher Scientific sample buffer | Sample preservation and storage [91] |
Experimental Workflow for Ct Value Studies
The following workflow diagram illustrates a standardized approach for research investigating the relationship between Ct values and viral infectivity:
Experimental Workflow for Ct-Infectivity Studies
This standardized methodology enables reproducible investigation of correlations between molecular detection (Ct values) and infectious potential (viral culture), controlling for key technical variables that significantly impact results.
Ct values from SARS-CoV-2 RT-PCR tests provide valuable semi-quantitative information about viral RNA concentration in clinical samples, but their interpretation requires careful consideration of methodological and biological contexts. While lower Ct values generally correlate with higher probabilities of culturable virus and potential infectivity, no universal Ct value threshold can definitively discriminate infectious from non-infectious individuals across different experimental and clinical settings. The substantial variability introduced by differences in sample processing, amplification methods, and temporal infection dynamics limits the direct comparability of Ct values between laboratories.
Future research directions should focus on standardizing reporting methods, establishing laboratory-specific validation of Ct value thresholds for specific applications, and investigating variant-specific relationships between viral RNA levels and infectivity. Until such standardization is achieved, Ct values remain primarily research tools rather than definitive clinical indicators of individual infectivity status. Researchers should prioritize methodological transparency and laboratory-specific validation when incorporating Ct value interpretations into study designs and conclusions.
Validation Frameworks and Comparative Performance Metrics Across Platforms
Accurate and reliable molecular diagnostic assays for detecting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are fundamental to epidemiology studies and infection-control measures [92]. The limit of detection (LoD) is a critical parameter defining the lowest concentration of viral target that an assay can detect with high confidence (typically ≥95% of repeat measurements) [93]. It serves as a primary indicator of analytical sensitivity, directly influencing clinical performance by determining the ability to identify infected individuals, particularly those with low viral loads [93]. This guide provides a comparative analysis of the LoDs of various SARS-CoV-2 detection methods, presenting objective performance data and detailed experimental protocols to inform researchers, scientists, and drug development professionals in their methodological selections.
Comparative LoD Performance of SARS-CoV-2 Detection Methods
The following table summarizes the LoD values for different SARS-CoV-2 detection platforms as reported in recent scientific literature. These values are crucial for understanding the baseline sensitivity of each method.
Table 1: Comparison of LoD Values for SARS-CoV-2 Detection Methods
| Detection Method | Specific Platform/Assay | Reported LoD | Reference |
|---|---|---|---|
| Sample-to-Answer PCR | BioFire Respiratory Panel 2.1 (RP2.1) | Not specified in results | [92] |
| Sample-to-Answer PCR | cobas Liat SARS-CoV-2 and Influenza A/B | Not specified in results | [92] |
| Sample-to-Answer PCR | Cepheid Xpert Xpress SARS-CoV-2/Flu/RSV | Not specified in results | [92] |
| Automated RT-PCR | NeuMoDx SARS-CoV-2 Assay | 150 copies/mL | [94] |
| Digital PCR (dPCR) | QX200 Droplet dPCR | Similar copy numbers to LOAA; specific LoD not quantified in results | [95] |
| Digital Real-time PCR | LOAA (digital real-time PCR) | Higher sensitivity and precision for low copy numbers vs. QX200 | [95] |
| RT-qPCR Kit | Maccura Kit | 450 copies/mL | [96] |
| RT-qPCR Kit | Sansure Kit | 200 copies/mL | [96] |
| rRT-PCR | Assays targeting E gene | 3.6 copies per 25 μL reaction | [97] |
| rRT-PCR | Assays targeting RdRP gene | 3.9 copies per 25 μL reaction | [97] |
| RT-LAMP | One-Step RT-LAMP (N gene target) | Sensitivity reported at dilution of 1 x 10¹; specific LoD not given | [13] |
The relationship between a method's LoD and its clinical sensitivity—the ability to correctly identify infected individuals—is quantifiable. One study modeling this relationship found that viral loads in patients are relatively evenly distributed across logarithmic bins. This model predicts that for every 10-fold increase in LoD, clinical sensitivity decreases by approximately 13% [93]. This underscores why LoD is a vital metric for diagnostic efficacy.
Detailed Experimental Protocols for LoD Determination
To ensure reproducibility and provide clarity on how the aforementioned LoDs are derived, this section outlines the standard experimental methodologies used in the cited studies.
LoD Determination for RT-PCR and Related assays
The LoD for PCR-based methods is typically established using serial dilutions of standardized reference materials.
- Reference Materials: Studies commonly use commercially available SARS-CoV-2 RNA controls, such as the AMPLIRUN SARS-CoV-2 RNA controls (Vircell) [92] or the SeraCare AccuPlex SARS-CoV-2 Reference Material Kit, which consists of replication-incompetent, enveloped virus particles with cloned SARS-CoV-2 targets quantified by digital droplet PCR [93].
- Experimental Procedure: A serial dilution panel of the reference material is prepared in a matrix that mimics clinical transport media. Each dilution level is tested with a high number of replicates (e.g., 1–10 or more) [92] [93].
- Data Analysis: The LoD is statistically determined as the lowest concentration at which ≥95% of the replicate tests return a positive result [93]. For instance, in the validation of the Abbott RealTime SARS-CoV-2 assay, testing a fine dilution series in replicates of 10 revealed an LoD of approximately 50 copies/mL, even though the manufacturer's stated LoD was 100 copies/mL [93].
LoD Determination for Isothermal Amplification (RT-LAMP)
The protocol for determining the LoD of RT-LAMP assays follows principles similar to RT-PCR but with isothermal amplification conditions.
- Primer Design: A set of six primers (F3, B3, FIP, BIP, LF, LB) is designed to recognize eight distinct regions on a conserved target gene, such as the N gene of SARS-CoV-2, using specialized software like Primer Explorer V5 [13].
- Reaction Setup: The One-Step RT-LAMP reaction is performed in a single tube. A typical 25 μL reaction mixture includes the designed primers, Bst DNA/RNA Polymerase (an enzyme with reverse transcriptase and strand-displacement DNA polymerase activities), and the RNA template [13].
- Amplification and Detection: The reaction is incubated at a constant temperature (often 60–65°C) for a short duration (e.g., 30-60 minutes). Amplification can be detected in real-time using intercalating dyes that fluoresce upon binding to double-stranded DNA products [13].
- Sensitivity Analysis: The analytical sensitivity (LoD) is determined by testing a dilution series of a known positive sample or synthetic RNA and establishing the last dilution that consistently yields a positive amplification signal [13].
Visualizing Molecular Detection Pathways and Workflows
The following diagram illustrates the general workflow and decision-making process for selecting and performing key molecular detection methods for SARS-CoV-2, from sample collection to result interpretation.
Figure 1: A generalized workflow for the primary molecular methods used in SARS-CoV-2 detection, highlighting the key technological branches from sample to result.
Essential Research Reagent Solutions
The successful implementation of SARS-CoV-2 detection methods relies on a suite of critical reagents and materials. The table below details key components, their functions, and examples from the literature.
Table 2: Key Research Reagents for SARS-CoV-2 Molecular Detection
| Reagent/Material | Function | Examples & Notes |
|---|---|---|
| Reference RNA Standards | Quantified viral RNA used for assay calibration, LoD determination, and quality control. Provides a universal benchmark for comparing different assays. | SeraCare AccuPlex SARS-CoV-2 Reference Material [93], AMPLIRUN SARS-CoV-2 RNA controls (Vircell) [92]. |
| Primers & Probes | Short, specific nucleotide sequences that bind to target genes (e.g., E, N, RdRP, ORF1ab) to initiate amplification and enable detection. | Designed to target conserved regions; multiplex assays (e.g., BioFire RP2.1) use multiple primers to detect various pathogens simultaneously [92] [97]. |
| Enzyme Mixes | Enzymatic master mixes that perform reverse transcription (RNA to cDNA) and nucleic acid amplification (e.g., PCR, isothermal). | Mixes often include reverse transcriptase, Taq polymerase, and sometimes UDG enzyme to prevent contamination [96]. Bst DNA/RNA Polymerase is specific for RT-LAMP [13]. |
| Nucleic Acid Extraction Kits | Kits to isolate and purify viral RNA from clinical samples (e.g., swabs in transport media), removing inhibitors that can affect amplification. | Considered a critical step; automated systems (e.g., SSNP-9600A) are often used for high-throughput processing [96]. |
| Internal Controls | Non-target nucleic acids added to or co-extracted with the sample to monitor the efficiency of RNA extraction and amplification, identifying false negatives. | Exogenous (e.g., RNA pseudovirus in Maccura kit) or endogenous (e.g., human RNase P in Sansure kit) controls [96]. |
The landscape of SARS-CoV-2 detection methods reveals a clear trade-off between analytical sensitivity, represented by the LoD, and factors such as throughput, speed, and operational complexity. rRT-PCR remains the gold standard, with some assays boasting LoDs as low as 3.6 copies per reaction [97]. However, digital PCR platforms are emerging as powerful tools offering superior sensitivity and precision for absolute quantification, especially at low viral loads [95]. Meanwhile, isothermal methods like RT-LAMP present a compelling alternative for rapid, field-deployable diagnostics without sacrificing substantial sensitivity, as evidenced by their high agreement (93-94%) with RT-qPCR results [13]. The selection of an appropriate method must be guided by the specific research or diagnostic context, with the understanding that the LoD is a fundamental determinant of an assay's ability to detect early, resolving, or asymptomatic infections, thereby directly impacting the effectiveness of public health interventions and clinical management.
The accurate detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been a cornerstone of the global response to the COVID-19 pandemic. For researchers, scientists, and drug development professionals, understanding the comparative performance of available diagnostic tests is crucial for interpreting data, designing clinical studies, and developing effective therapeutic interventions. The landscape of SARS-CoV-2 diagnostics is dominated by two primary methodologies: nucleic acid amplification tests (NAATs), such as reverse transcription polymerase chain reaction (RT-PCR), which detect viral RNA; and rapid antigen tests, which detect viral proteins. Each method possesses distinct performance characteristics, advantages, and limitations that vary significantly across different patient populations and testing scenarios. This guide provides an objective, data-driven comparison of these diagnostic alternatives, framing the analysis within the broader context of comparative molecular method analysis in SARS-CoV-2 research. By synthesizing experimental data from recent clinical studies, we aim to elucidate the clinical performance—specifically sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV)—of these tests across diverse patient populations and provide detailed methodologies for the key experiments cited.
Comparative Performance of SARS-CoV-2 Testing Modalities
The performance of SARS-CoV-2 diagnostic tests is not absolute but is significantly influenced by factors including viral load, symptom status, timing of testing, and circulating viral variants. The tables below summarize the performance metrics of antigen tests compared to NAATs (primarily RT-PCR) across different patient populations and conditions, as reported in recent studies.
Table 1: Overall Diagnostic Performance of Antigen Tests Versus RT-PCR
| Study Population & Test Type | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Sample Size (n) | Citation |
|---|---|---|---|---|---|---|
| General patient population (Lateral Flow Ag Test) | 59.4 | 99.0 | 64.8 | 98.7 | 3,110 | [98] |
| Symptomatic patients (Lateral Flow Ag Test) | 66.7 | 98.9 | 85.0 | 99.0 | 249 | [98] |
| Asymptomatic patients (Lateral Flow Ag Test) | 47.6 | 97.0 | 44.4 | 91.9 | 2,589 | [98] |
| Hospitalized patients (Standard Q Ag Test) | 95.0 | 97.0 | Not Reported | Not Reported | 200 | [99] |
| Fluorescence Immunoassay (FIA) | 80.3 | 96.8 | 91.6 | 91.9 | 268 | [100] |
| Lateral Flow Immunoassay (LFIA) | 76.5 | 97.3 | 90.5 | 92.6 | 268 | [100] |
| Saliva-based Rapid Antigen Test (RAK) | 67.0 | 75.0 | 86.4 | 50.0 | 320 | [44] |
Table 2: Impact of Viral Load (Cycle Threshold Values) on Antigen Test Sensitivity
| Cycle Threshold (Ct) Value Range | Viral Load Correlation | Antigen Test Sensitivity (%) | Study / Test Type |
|---|---|---|---|
| Ct ≤ 20 | High | 100 | [44] |
| Ct ≤ 25 | High | 100 | [100] |
| Ct 21 - 25 | Intermediate | 63 | [44] |
| Ct > 30 | Low | 22 - 31.8 | [44] [98] |
| Ct > 30 | Low | 27.3 (LFIA), 31.8 (FIA) | [100] |
Table 3: Performance in Specific Subgroups and Against Variants
| Patient Subgroup / Variant | Test Type | Key Performance Finding | Citation |
|---|---|---|---|
| Symptomatic (within 5 days of onset) | Antigen (BD Veritor) | Positive Percent Agreement (PPA): 83.3% | [101] |
| Asymptomatic / Symptoms after 5 days | Antigen (BD Veritor) | Positive Percent Agreement (PPA): 18.2% | [101] |
| Omicron Variant | FIA & LFIA | Sensitivity: 100% | [100] |
| Alpha Variant | FIA & LFIA | Sensitivity: 78.9% (FIA), 69.2% (LFIA) | [100] |
| Delta Variant | FIA & LFIA | Sensitivity: 72.2% (FIA), 83.3% (LFIA) | [100] |
The data demonstrates a consistent theme: antigen tests exhibit high specificity but variable sensitivity. Their performance is strongly correlated with viral load, making them highly sensitive in patients with high viral loads (low Ct values) but substantially less reliable in individuals with lower viral loads. Furthermore, antigen tests perform better in symptomatic individuals compared to asymptomatic carriers, and their efficacy can vary depending on the SARS-CoV-2 variant.
Experimental Protocols for Key Assays
To critically appraise the performance data, a clear understanding of the underlying experimental methodologies is essential. Below are detailed protocols for the key assays referenced in the comparative data.
Real-Time Reverse Transcription Polymerase Chain Reaction (RT-PCR)
RT-PCR remains the gold standard for SARS-CoV-2 detection due to its high sensitivity and specificity [98]. The following protocol is representative of the methodologies used in the cited studies.
- Sample Collection and Transport: Nasopharyngeal or oropharyngeal swabs are collected from patients using sterile flocked swabs. The swab is immediately placed into a tube containing viral transport media (VTM) to preserve viral RNA. The sample is transported to the laboratory under refrigerated conditions and typically stored at -80°C if not processed immediately [44] [99].
- RNA Extraction: Viral RNA is extracted from the VTM sample using commercial nucleic acid extraction kits, such as the GF-1 Viral Nucleic Acid Extraction Kit or the DAAN kit. This process purifies and concentrates the RNA, which is critical for assay sensitivity. Automated extraction systems are often employed for consistency and throughput [44] [99].
- PCR Amplification and Detection: The extracted RNA is mixed with a master mix containing reverse transcriptase, DNA polymerase, specific primers, and fluorescence-labeled probes. The Bosphore Novel Coronavirus (2019-nCoV) Detection Kit is one example. The reaction is run on a real-time thermal cycler (e.g., Anatolia Montania 4896). The protocol involves:
- Reverse Transcription: 50°C for 20 minutes to convert viral RNA into complementary DNA (cDNA).
- Enzyme Activation: 95°C for 10 minutes to activate the Taq polymerase.
- Amplification: 40 cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 30 seconds (fluorescence is measured at this step).
- Result Interpretation: The cycle threshold (Ct) value, which represents the number of cycles required for the fluorescence signal to exceed a background threshold, is determined. Samples with Ct values below a predefined cutoff (e.g., <36 or <37) are considered positive. The target genes detected typically include the E, N, and RdRp genes [44] [99].
Rapid Antigen Test (Lateral Flow Immunoassay)
Rapid antigen tests are designed for point-of-care use and provide results in minutes. The following protocol details the process for a typical lateral flow device, such as the Standard Q COVID-19 Ag Test [99].
- Sample Collection: A nasopharyngeal or nasal swab is collected from the patient.
- Sample Preparation: The swab is inserted into a tube containing a specific extraction buffer. The swab is rotated and pressed against the tube walls to elute the viral antigens into the solution. A filter nozzle cap is often pressed onto the tube to facilitate droplet application.
- Test Execution: Three drops of the extracted sample are applied to the sample well (S) of the test device. The device contains a nitrocellulose membrane pre-coated with two lines: a test line (T) coated with mouse monoclonal anti-SARS-CoV-2 nucleocapsid (N) antibody, and a control line (C) coated with control antibodies.
- Immunochromatography and Result Readout: The liquid sample migrates along the strip via capillary action. If the SARS-CoV-2 N antigen is present, it binds to the antibody conjugated to colored particles and is captured at the T line, forming a visible band. The appearance of both the C and T lines within the specified time (e.g., 15-30 minutes) indicates a positive result. The appearance of only the C line indicates a negative result. The test is invalid if the C line does not appear [99].
Pseudotyped Virus Neutralization Assay (PVNA)
While not a diagnostic test, the PVNA is a critical research tool for evaluating vaccine-induced immune responses and therapeutic antibodies in a biosafe environment. This assay was used in studies comparing its correlation with live virus neutralization assays [102].
- Pseudovirus Production: A vesicular stomatitis virus (VSV) backbone, in which the native glycoprotein gene has been deleted and replaced with a reporter gene (e.g., firefly luciferase), is used. This vector is then coated with the SARS-CoV-2 spike protein to create the pseudovirus.
- Serum Incubation and Neutralization: Serum samples from vaccinated or infected individuals are serially diluted (e.g., three-fold starting at 1:30). The diluted serum is mixed with a standardized amount of pseudovirus (e.g., 1000 TCID50/well) and incubated for a set period (e.g., 1 hour at 37°C) to allow neutralizing antibodies, if present, to bind to the pseudovirus.
- Cell Infection: The serum-virus mixture is added to a monolayer of susceptible cells, such as Huh7 cells (2 × 10^4 cells/well). The pseudoviruses that are not neutralized will enter the cells.
- Detection and Quantification: After an incubation period (e.g., 24-48 hours), the cells are lysed, and a luciferase substrate is added. The level of infection is quantified by measuring the relative luminescence units (RLU) using a microplate luminometer. The half-maximal effective concentration (EC50) titer is calculated as the reciprocal of the serum dilution that neutralizes 50% of the pseudovirus activity, often using the Reed-Muench method [102].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the logical workflow of the diagnostic tests and the conceptual process of the neutralization assay, highlighting the key steps and decision points.
SARS-CoV-2 Diagnostic Testing Pathway
Pseudotyped Virus Neutralization Assay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
The experiments and diagnostics discussed rely on a suite of specialized reagents and materials. The following table details key solutions and their functions in SARS-CoV-2 research.
Table 4: Essential Research Reagents and Materials
| Research Reagent / Material | Primary Function / Description | Example Use Case | Citation |
|---|---|---|---|
| Viral Transport Media (VTM) | A solution designed to preserve the viability of viruses and viral RNA during swab transport from collection site to laboratory. | Preservation of nasopharyngeal swab samples for RT-PCR analysis. | [44] [99] |
| Monoclonal Anti-SARS-CoV-2 Antibodies | Antibodies specifically targeting viral proteins (e.g., Nucleocapsid-N). Often conjugated to colored or fluorescent particles. | Detection agent in the test line of lateral flow rapid antigen tests. | [99] |
| Pseudotyped Virus Systems | Engineered, non-replicating viral particles bearing the SARS-CoV-2 spike protein and a reporter gene (e.g., luciferase). | Safe, BSL-2 level evaluation of neutralizing antibodies in PVNAs. | [102] |
| Primers & Probes for RT-PCR | Short, specific nucleic acid sequences designed to bind and amplify target genes of SARS-CoV-2 (e.g., N, E, RdRp genes). | Specific detection and amplification of viral RNA in diagnostic RT-PCR tests. | [44] [103] |
| Vero E6 / Vero E6/TMPRSS2 Cells | Cell lines derived from monkey kidney epithelium that are highly susceptible to SARS-CoV-2 infection. | Cell culture for propagating live SARS-CoV-2 virus for LVNAs and research. | [102] [103] |
| Huh7 Cells | A human hepatocyte-derived cell line commonly used in virology research. | Target cells for infection in pseudotyped virus neutralization assays (PVNAs). | [102] |
| Reporter Assay Substrates (e.g., Luciferin) | Chemical compounds that produce light when cleaved by a reporter enzyme like luciferase. | Quantifying pseudovirus infection in PVNAs by measuring luminescence (RLU). | [102] |
The objective comparison of SARS-CoV-2 testing methodologies reveals a clear trade-off between the high analytical sensitivity of molecular methods like RT-PCR and the operational speed and accessibility of antigen tests. The choice between these alternatives in a research or clinical development context must be guided by the specific use case. RT-PCR remains the indispensable gold standard for confirmatory diagnosis and for detecting early or low-level infections. In contrast, antigen tests, while less sensitive, offer a pragmatic tool for rapid screening and identifying individuals with high viral loads who are likely to be contagious. For research into immune responses, pseudotyped virus neutralization assays provide a safe and correlative surrogate for live virus assays. A comprehensive understanding of the performance characteristics, experimental protocols, and reagent systems underlying these tests is fundamental for generating robust, interpretable, and translatable scientific data in the ongoing fight against SARS-CoV-2.
The continuous evolution of SARS-CoV-2 has resulted in the emergence of numerous viral variants characterized by distinct genetic mutations that can alter viral characteristics, including transmissibility, disease severity, and crucially, detection efficacy. Molecular detection methods form the cornerstone of COVID-19 diagnostics, yet their performance can vary significantly when confronted with different variants. Variants of Concern (VOCs) such as Alpha (B.1.1.7), Delta (B.1.617.2), and Omicron (B.1.1.529) lineages have presented unique challenges for diagnostic platforms due to their specific genetic profiles [104] [105] [106]. The World Health Organization (WHO) classifies these variants based on their assessed potential for expansion, replacement of prior variants, ability to cause new waves with increased circulation, and the need for adjustments to public health actions [107].
Understanding how diagnostic tests perform against these variants is paramount for researchers and public health officials working to control the pandemic. Mutations in the SARS-CoV-2 genome, particularly in the spike protein, have raised concerns about potential diagnostic escape, where tests may exhibit reduced sensitivity or even false-negative results [106]. This comparative analysis examines the performance of major molecular detection methods against key SARS-CoV-2 variants, providing experimental data and methodological protocols to inform research and clinical laboratory practices in the context of ongoing viral evolution.
Comparative Performance Data of Detection Methods
The performance of SARS-CoV-2 detection methods varies considerably across different variants, influenced by the specific mutations in each variant and the technical principles of each assay. The following tables summarize key experimental findings regarding how different variants affect test performance.
Table 1: Comparative Performance of SARS-CoV-2 Detection Methods Across Variants
| Detection Method | Variant | Sensitivity | Specificity | Key Performance Notes | Study Details |
|---|---|---|---|---|---|
| RT-PCR | Alpha | High | High | Maintains reliable detection despite variant mutations [104]. | Multi-target molecular tests. |
| Delta | High | High | Effective detection; some single-target assays potentially affected. | ||
| Omicron | High | High | Most multi-target tests effective; specific S-gene dropout observed. | ||
| Ag-RDT (FIA) | Alpha | 78.85% | High | Reduced sensitivity compared to Omicron [100]. | 268 sample study, vs. RT-PCR. |
| Delta | 72.22% | High | Lower sensitivity than for Omicron variant. | 268 sample study, vs. RT-PCR. | |
| Omicron | 100% (High VL) | High | 100% sensitivity at low Ct values (<25) [100]. | 268 sample study, vs. RT-PCR. | |
| Ag-RDT (LFIA) | Alpha | 69.23% | High | Lowest sensitivity among tested variants [100]. | 268 sample study, vs. RT-PCR. |
| Delta | 83.33% | High | Higher sensitivity than FIA for this variant. | 268 sample study, vs. RT-PCR. | |
| Omicron | 100% (High VL) | High | 100% sensitivity at low Ct values (<25) [100]. | 268 sample study, vs. RT-PCR. | |
| Machine Learning (Symptom-Based) | Multiple | 95.2% (Accuracy) | High | Successful variant mapping via symptom profiles [108]. | Stacked Ensemble Model. |
Table 2: Impact of Viral Load on Antigen Test Sensitivity Across Variants
| Variant | Ag-RDT (FIA) Sensitivity at Ct<25 | Ag-RDT (LFIA) Sensitivity at Ct<25 | Ag-RDT (FIA) Sensitivity at Ct>30 | Ag-RDT (LFIA) Sensitivity at Ct>30 |
|---|---|---|---|---|
| All Variants | 100% | 100% | 31.82% | 27.27% |
| Context | High viral load | High viral load | Low viral load | Low viral load |
The data reveal that RT-PCR maintains robust performance across Alpha, Delta, and Omicron variants, particularly when utilizing multi-target approaches [104]. In contrast, Antigen-based Rapid Diagnostic Tests (Ag-RDTs) show more variable performance, with sensitivity highly dependent on both the specific variant and viral load. The Fluorescence Immunoassay (FIA) format generally outperformed the Lateral Flow Immunoassay (LFIA) for Alpha variant detection, while the reverse was true for the Delta variant in one study [100]. Notably, both Ag-RDT formats demonstrated 100% sensitivity for Omicron detection when viral loads were high (Ct <25), suggesting their particular utility during peak infectiousness periods regardless of variant [100].
An alternative approach using machine learning to detect variants based on symptom profiles rather than genetic code has shown remarkable promise, achieving 95.2% accuracy using a stacked ensemble model [108]. This method represents a novel paradigm in variant detection, potentially offering a cost-effective supplement to traditional laboratory methods.
Experimental Protocols for Variant Detection
Genomic Sequencing for Variant Identification
Purpose: To identify specific SARS-CoV-2 variants through whole genome sequencing and analysis of mutations. This protocol is considered the gold standard for variant characterization and is used by programs like the National SARS-CoV-2 Strain Surveillance (NS3) [109].
Methodology:
- Sample Collection: Collect nasopharyngeal or oropharyngeal swab specimens in viral transport media.
- RNA Extraction: Purify viral RNA using commercial nucleic acid extraction kits. Quantify and assess RNA quality.
- Library Preparation: Perform reverse transcription to generate cDNA. Amplify the entire SARS-CoV-2 genome using multiplex PCR with tiling primers covering the ~30kb genome.
- Sequencing: Prepare sequencing libraries with dual indices to allow for multiplexing. Sequence on a high-throughput platform (e.g., Illumina MiSeq/NextSeq).
- Bioinformatic Analysis:
- Quality Control: Assess sequence quality using tools like FastQC.
- Alignment: Map reads to the SARS-CoV-2 reference genome (NC_045512.2) using aligners like BWA or Bowtie2.
- Variant Calling: Identify mutations (SNPs, indels) using variant callers like iVar or LoFreq.
- Lineage Assignment: Classify the sequence into a Pango lineage (e.g., B.1.1.7, B.1.617.2, B.1.1.529) using the Pangolin tool [109].
- Phylogenetic Analysis: Construct phylogenetic trees to contextualize the sequence within the global diversity of SARS-CoV-2.
Applications: This method is used by public health agencies worldwide for national surveillance to track the emergence and prevalence of variants, as depicted in the genomic surveillance workflow below.
Comparative Evaluation of RT-PCR and Antigen Tests
Purpose: To directly compare the diagnostic performance of RT-PCR and Antigen-based Rapid Diagnostic Tests (Ag-RDTs) against different SARS-CoV-2 variants, assessing sensitivity, specificity, and variant-dependent performance.
Methodology [100]:
- Sample Collection: Prospectively collect respiratory samples (e.g., nasopharyngeal swabs) from suspected COVID-19 cases.
- Simultaneous Testing: Split each sample for parallel testing:
- RT-PCR: Extract RNA and perform RT-PCR using approved assays. Record Cycle Threshold (Ct) values as a proxy for viral load.
- Ag-RDT Testing: Test aliquots of the sample transport media using both Fluorescence Immunoassay (FIA) and Lateral Flow Immunoassay (LFIA) formats according to manufacturer instructions. Perform tests blinded to RT-PCR results.
- Variant Identification: For positive samples, determine the infecting variant using a PCR-based method targeting variant-specific mutations or through full genomic sequencing.
- Data Analysis:
- Calculate sensitivity, specificity, Positive Predictive Value (PPV), and Negative Predictive Value (NPV) for each Ag-RDT against RT-PCR as the reference standard.
- Stratify results by SARS-CoV-2 variant (Alpha, Delta, Omicron) and by viral load (using Ct value thresholds, e.g., <25, 25-30, >30).
- Assess agreement between tests using Cohen's Kappa statistic.
Key Findings: This methodology revealed that while both Ag-RDT formats showed high sensitivity for Omicron, their performance against Alpha and Delta variants differed significantly between the FIA and LFIA platforms [100]. The study also confirmed that sensitivity for all variants dropped considerably at Ct values >30, highlighting the critical impact of viral load.
Machine Learning for Variant Detection via Symptom Profiles
Purpose: To accurately map a patient's symptoms to the corresponding SARS-CoV-2 variant and predict mortality risk in severe cases, providing an alternative to genetic sequencing.
Methodology [108]:
- Data Collection and Curation: Compile a comprehensive dataset containing demographic information, clinical symptoms, and confirmed variant lineage from patient records. Key symptoms for analysis may include fever, headache, sore throat, runny nose, cough, and loss of smell.
- Data Pre-processing:
- Handle missing data using appropriate imputation techniques.
- Encode categorical variables and normalize numerical features.
- Split data into training and testing sets (e.g., 80:20 ratio).
- Model Selection and Training:
- Train multiple machine learning algorithms, including Random Forest and XGBoost, using the training dataset.
- Employ a stacked ensemble approach that combines the predictions of multiple base models to improve overall accuracy and robustness.
- Model Evaluation:
- Evaluate performance on the held-out test set using metrics including accuracy, precision, recall, and F1-score.
- Generate confusion matrices to visualize classification performance for each variant.
Key Findings: This novel approach demonstrated that symptom profiles can be mapped to specific variants with high accuracy (95.2%) using an ensemble model, suggesting that clinical presentation can serve as a valuable proxy for variant identification when genomic sequencing is not readily available [108]. The workflow for this method is distinct from genetic-based approaches.
The Scientist's Toolkit: Key Research Reagents and Materials
Successful variant detection and characterization rely on a suite of specialized research reagents and materials. The following table details essential components for the experimental protocols described in this guide.
Table 3: Essential Research Reagents for SARS-CoV-2 Variant Detection
| Reagent/Material | Specific Function | Application Context |
|---|---|---|
| Viral Transport Media (VTM) | Preserves viral integrity during sample transport and storage. | Sample collection for all downstream analyses (sequencing, RT-PCR, Ag-RDT). |
| Nucleic Acid Extraction Kits | Isolate and purify viral RNA from clinical samples. | Essential pre-step for RT-PCR and genomic sequencing. |
| Multiplex PCR Primers | Amplify specific regions or the entire SARS-CoV-2 genome. | Genomic sequencing (tiling primers) and multi-target RT-PCR assays. |
| dNTPs and Reverse Transcriptase | Synthesize complementary DNA (cDNA) from viral RNA templates. | First-step in RT-PCR and library prep for sequencing. |
| Sequence-Specific Probes & Dyes | Enable fluorescent detection of amplified genetic targets. | Real-time RT-PCR for diagnostic detection and viral load quantification. |
| Ag-RDT Test Kits (FIA & LFIA) | Detect viral nucleocapsid or spike protein antigens. | Rapid diagnostic testing; performance varies by variant [100]. |
| Next-Generation Sequencing Library Prep Kits | Prepare amplified DNA for sequencing on high-throughput platforms. | Whole genome sequencing for variant identification and surveillance [109]. |
| Bioinformatic Software (e.g., Pangolin) | Assign phylogenetic lineage based on genetic sequence data. | Final classification step in genomic sequencing [109]. |
The performance of SARS-CoV-2 detection methods is inherently linked to the genetic evolution of the virus. While molecular methods like RT-PCR remain the gold standard for sensitivity and reliability across variants, the emergence of Alpha, Delta, and Omicron has highlighted specific diagnostic considerations. Antigen tests, while faster and more accessible, show variable performance dependent on both variant type and viral load, a critical factor for their application. Innovative approaches, such as machine learning models using symptom profiles, demonstrate promising alternatives for variant mapping where genomic surveillance is constrained. For researchers and public health professionals, a layered strategy that combines these methods, informed by continuous genomic surveillance, is essential for accurate variant detection and effective pandemic response.
The global pandemic underscored the critical role of accurate and reliable in vitro diagnostic (IVD) tests, placing a spotlight on the regulatory frameworks that govern their development and use. For researchers and developers navigating the complex field of molecular diagnostics, particularly for pathogens like SARS-CoV-2, understanding the distinctions and intersections between major regulatory pathways is essential. This guide provides a comparative analysis of three cornerstone frameworks: the In Vitro Diagnostic Regulation (IVDR) for the European market, the Emergency Use Authorization (EUA) pathway from the U.S. Food and Drug Administration, and the international quality standard ISO 15189 for medical laboratories. These frameworks, though differing in geographic scope and legal standing, collectively shape the development, validation, and implementation of laboratory tests worldwide. This analysis is framed within the context of SARS-CoV-2 molecular method research, using published comparative performance data to illustrate the practical implications of these regulations on test quality, market access, and clinical utility.
The following table summarizes the core characteristics, objectives, and applicability of the ISO 15189, EUA, and IVDR frameworks, highlighting their distinct roles in the diagnostics ecosystem.
Table 1: Core Characteristics of Key Diagnostic Regulatory Frameworks
| Feature | ISO 15189:2022 | U.S. Emergency Use Authorization (EUA) | EU IVDR (2017/746) |
|---|---|---|---|
| Nature & Scope | International standard for quality management and competence of medical laboratories [110] [111] | U.S. regulatory authorization for unapproved medical products during a public health emergency [112] | Binding EU regulation for the safety and performance of in vitro diagnostic medical devices [113] [114] |
| Primary Focus | Quality of the total testing process (pre-, intra-, and post-analytical phases) and laboratory competence [110] | Rapid market access for critical tests during an emergency, balancing speed with sufficient evidence [112] | High standards of clinical evidence, safety, and performance for all IVDs placed on the EU market [113] [115] |
| Legal Status | Voluntary standard (unless mandated nationally; supports IVDR compliance) [110] [111] | Conditional authorization under U.S. Federal Food, Drug, and Cosmetic Act [112] | Legally binding regulation in all EU member states [114] |
| Applicability | Medical laboratories (organization-level accreditation) | Manufacturers and specific diagnostic products | Manufacturers placing devices on the EU market; also affects health institutions using in-house devices (LDTs) [113] [114] |
| Risk Classification | Not applicable (focus is on processes) | Not a formal classification system | Four-tier risk-based system (A-D, with D being highest risk) [113] [114] |
The relationships and primary focuses of these frameworks in the context of a laboratory's operations and product lifecycle can be visualized below.
The EU IVDR (2017/746): A New Paradigm
Core Principles and Classification
The IVDR replaced the previous Directive (IVDD) to establish a more robust, transparent, and sustainable regulatory framework within the EU [113] [114]. Its key objectives are to enhance clinical safety and create fair market access by aligning legislation with technical advances and changes in medical science [114]. A fundamental change introduced by the IVDR is a risk-based classification system with four classes (A-D), which determines the conformity assessment route [113]. This has significantly increased the proportion of IVDs requiring certification by a Notified Body from an estimated 15% under the IVDD to 70-90% under the IVDR [113]. SARS-CoV-2 assays, for instance, are classified as high-risk Class D devices [114].
Performance Evaluation and Evidence Requirements
Under the IVDR, manufacturers must establish rigorous performance evaluation procedures, described in Chapter VI and supporting annexes of the regulation [115]. This evaluation is an ongoing process, not just a pre-market requirement, and consists of three core elements [115]:
- Scientific Validity: Demonstrating that the analyte (e.g., a viral gene target) is clinically associated with the condition (e.g., COVID-19).
- Analytical Performance: Proving the device correctly detects or measures the analyte in the laboratory (e.g., through precision, sensitivity, and LoD studies).
- Clinical Performance: Demonstrating the device performs effectively in real-world clinical settings to detect the intended clinical condition (e.g., diagnostic sensitivity and specificity).
The data for this evaluation must be compiled into a Performance Evaluation Report (PER), which must include the device description, the assessments of scientific validity, analytical and clinical performance, a state-of-the-art comparison, and plans for post-market surveillance (PMS) or post-market performance follow-up (PMPF) [115].
Implications for In-House Devices (LDTs)
The IVDR explicitly addresses in-house devices (also called Laboratory Developed Tests, LDTs) manufactured and used within health institutions. Its introduction places specific constraints on their use, requiring laboratories to [113] [110] [114]:
- Implement an appropriate quality management system, inclusive of ISO 15189.
- Justify the use of the in-house device by documenting why an equivalent CE-marked device on the market cannot be used.
- Ensure the devices are not transferred to another legal entity or manufactured on an industrial scale.
- Comply with the General Safety and Performance Requirements (GSPRs) outlined in Annex I of the IVDR.
ISO 15189: Quality and Competence in Medical Laboratories
Scope and Objectives
ISO 15189 is an international standard that specifies requirements for quality management and competence in medical laboratories [110] [111]. Its primary objective is to improve the quality and safety of patient care by ensuring the reliability of laboratory results, protecting patient data, and fostering continuous improvement [110]. Unlike a product-focused regulation, ISO 15189 applies to the total testing process, encompassing pre-analytical, analytical, and post-analytical phases within the laboratory organization itself [110].
Synergy with IVDR for In-House Devices
For laboratories developing and using in-house IVDs under the IVDR, ISO 15189 plays a crucial role. The IVDR's health institution exemption (Article 5.5) mandates that laboratories must operate under "appropriate quality management systems," and specifically references compliance with EN ISO 15189 [110] [114] [111]. However, it is critical to note that ISO 15189 alone is not sufficient for full IVDR compliance for in-house device manufacturing [110]. While ISO 15189 covers the laboratory's overall QMS, it does not fully address the device manufacturing process as required by Annex I of the IVDR. Therefore, laboratories must extend their QMS to include procedures for device development, manufacturing, and change control, often drawing from standards like ISO 13485 [110].
Emergency Use Authorization (EUA): A U.S. Pathway for Crises
Purpose and Context
The Emergency Use Authorization is a mechanism used by the U.S. FDA to facilitate the availability and use of medical countermeasures, including diagnostic tests, during a public health emergency [112]. The EUA pathway was heavily utilized during the COVID-19 pandemic to rapidly authorize hundreds of SARS-CoV-2 assays [112]. Its primary goal is to speed up market access for critical tests while maintaining a baseline of evidence for safety and performance.
Evidence and Performance Considerations
While specific EUA requirements may be adapted to the emergency context, they still demand substantial evidence. For SARS-CoV-2 molecular assays, the FDA provided guidance that analytical sensitivity/LoD should be established as the level that gives a 95% detection rate in at least 20 replicates [112]. This focus on foundational analytical performance allows for rapid deployment, though it may result in a wider variability of performance characteristics between authorized tests compared to the more standardized and comprehensive evidence required under the IVDR [112].
Comparative Analysis of SARS-CoV-2 Molecular Assays Under Different Frameworks
Published studies directly comparing the performance of various SARS-CoV-2 molecular assays provide valuable insights into the practical outcomes of these regulatory frameworks. The following table summarizes experimental data from performance comparisons.
Table 2: Performance Comparison of Selected SARS-CoV-2 Molecular Assays
| Assay Name (Platform/Type) | Regulatory Status in Study | Target Genes | Positive Percent Agreement (PPA) | Key Performance Notes | Citation |
|---|---|---|---|---|---|
| Aptima SARS-CoV-2 (Panther, TMA) | Not Specified | ORF1ab | 100.0% | Excellent PPA; does not provide Ct values; fully automated. | [116] |
| In-house LDT-Fusion (Panther Fusion, RT-PCR) | Laboratory Developed Test | RdRP | 100.0% | Excellent PPA; requires manual sample setup. | [116] |
| R-GENE (easyMAG/RT-PCR) | Not Specified | N, RdRP, E | 98.2% | Good PPA; required 2nd PCR for confirmation in ~17% of initial runs. | [116] |
| CDC N1 Kit (RT-PCR) | EUA | N | High Sensitivity | Ranked among the most sensitive assays in a 12-assay comparison. | [117] |
| CDC N2 Kit (RT-PCR) | EUA | N | 100% Sensitivity | Most sensitive assay in a 12-assay comparison. | [117] |
| NIID N2 (RT-PCR) | RUO (Approved in Japan) | N | 100% Sensitivity | Performance equivalent to CDC N2 kit. | [117] |
Experimental Protocol Insights
The methodologies from these comparative studies highlight the rigorous validation required. In one study, researchers extracted RNA from 155 characterized clinical samples (nasopharyngeal swabs, oropharyngeal swabs, and sputum) and tested them in parallel on 12 different molecular assays [117]. True-positive status was defined as a positive result for more than one assay and one genetic locus. Performance was assessed based on sensitivity and specificity against this consensus result [117]. Another study compared two fully automated, random-access systems (Aptima and LDT-Fusion) against a more manual system (R-GENE), evaluating not just concordance but also practical workflow metrics like hands-on time and turnaround time, which are crucial for laboratory efficiency [116].
Essential Research Reagent Solutions
The development and validation of diagnostic tests under any regulatory framework rely on a core set of reagents and tools. The following table details key materials used in the featured SARS-CoV-2 experiments.
Table 3: Key Research Reagents and Materials for Molecular Test Development
| Item | Function in Experimental Context | Example from Search Results |
|---|---|---|
| RNA Extraction Kits | Purification of viral nucleic acid from clinical specimen matrices for downstream amplification. | QIAamp Viral RNA Mini Kit [117] |
| Nucleic Acid Stabilizers | Preserve RNA integrity in clinical specimens during transport and storage before testing. | DNA/RNA Shield [117] |
| RT-PCR Master Mixes | Provide essential enzymes and buffers for the reverse transcription and PCR amplification steps. | TaqPath 1-Step RT-qPCR Master Mix [117] |
| Primer/Probe Sets | Specifically target and detect unique sequences of the pathogen (e.g., SARS-CoV-2 N, RdRP, E genes). | CDC N1, N2 assays; Charité E assay; NIID N2 assay [117] |
| Internal/Extraction Controls | Monitor the efficiency of nucleic acid extraction and rule out PCR inhibition, ensuring test validity. | RNase P (CDC), EAV (Roche), MS2 phage (Thermo Fisher) [117] |
| Positive Control Material | Heat-inactivated virus or synthetic controls used for assay validation, LOD determination, and QC. | SARS-CoV-2 strain (ATCC VR-1986HK) [117] |
The role of these reagents within a typical molecular test development and validation workflow is summarized in the following diagram.
The regulatory standards of ISO 15189, EUA, and IVDR represent different yet interconnected approaches to ensuring diagnostic quality and safety. ISO 15189 provides the foundational quality framework for the laboratory organization. The U.S. EUA pathway offers a pragmatic, agile response during crises, prioritizing speed while requiring foundational evidence. The EU IVDR establishes a comprehensive, rigorous, and ongoing lifecycle-based system for IVDs in the European market, with a strong emphasis on clinical evidence and post-market surveillance. For developers and researchers, the choice and navigation of these pathways depend on the target market, intended use of the test, and the stage of the product lifecycle. A successful global strategy requires an understanding of their unique requirements, as well as the robust experimental validation and documentation practices they collectively demand.
The global response to the COVID-19 pandemic has underscored the critical importance of diagnostic testing, not just for clinical case management but also for public health surveillance and research continuity. For scientists and drug development professionals, selecting an appropriate SARS-CoV-2 detection method involves careful consideration of operational parameters that directly impact research efficiency, reproducibility, and cost-effectiveness. Molecular diagnostics have emerged as the gold standard for SARS-CoV-2 detection in research settings, enabling everything from basic virological studies to therapeutic development. However, these methods vary significantly in their operational characteristics, creating a complex landscape for researchers designing studies or establishing laboratory protocols.
This comparative analysis examines three principal molecular detection platforms—conventional RT-qPCR, isothermal amplification methods (including RT-LAMP and recombinase-based assays), and integrated next-generation detection systems (NGDS). We evaluate these technologies through the critical lenses of cost, turnaround time, and technical expertise required, providing a structured framework to guide research method selection. The analysis synthesizes experimental data from recent, peer-reviewed studies to deliver an evidence-based comparison for the scientific community.
Molecular diagnostics for SARS-CoV-2 primarily target specific viral genes such as Nucleocapsid (N), Envelope (E), Spike (S), or RNA-dependent RNA polymerase (RdRp) through amplification-based detection. The platforms discussed herein represent the most widely adopted technologies in research laboratories, each with distinct operational profiles.
Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) remains the most established methodology, involving RNA extraction followed by reverse transcription and amplification with thermal cycling. Its widespread use provides extensive comparative data and established protocols [9] [118].
Isothermal Amplification Methods such as Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP) and recombinase-based assays perform amplification at a constant temperature, eliminating the need for sophisticated thermal cyclers. These methods have gained attention for their potential application in point-of-care testing and resource-limited settings [77] [13].
Next-Generation Detection Systems (NGDS) such as the Cepheid GeneXpert and BioFire FilmArray integrate sample preparation, amplification, and detection into automated, cartridge-based platforms. These systems minimize hands-on time but often at higher per-test costs [119].
Comparative Performance Data
Quantitative Operational Comparison
Table 1: Comprehensive Comparison of SARS-CoV-2 Molecular Detection Methods
| Parameter | Conventional RT-qPCR | Isothermal Methods (RT-LAMP) | Next-Generation Systems (NGDS) |
|---|---|---|---|
| Total Turnaround Time | 60-240 minutes [9] [118] | 36-60 minutes [77] [13] | 20-45 minutes [119] |
| Hands-on Time | 60-90 minutes [118] | 30-45 minutes [13] | <2 minutes [119] |
| Detection Limit | 10-100 copies/reaction [9] | 100-1000 copies/mL [77] [13] | Varies by system [119] |
| Sensitivity | 98.9-100% [118] | 93-95% [77] [13] | Platform-dependent [119] |
| Specificity | 98.8-100% [118] | 100% [77] [13] | Platform-dependent [119] |
| Equipment Cost | High ($15,000-$50,000) | Low ($1,000-$5,000) | Very High ($30,000-$70,000) |
| Cost per Test | $15-$40 [9] | $5-$15 [13] | $30-$100 [119] |
| RNA Extraction Required | Yes [9] [118] | Optional [13] | Integrated in system |
| Technical Expertise | Advanced | Moderate | Minimal |
Direct Method Comparison Studies
A comprehensive 2022 study comparing next-generation detection systems revealed notable performance differences between platforms. The Cepheid GeneXpert system demonstrated superior sensitivity for detecting SARS-CoV-2 in nasopharyngeal swabs in viral transport media (VTM) and saline compared to the BioFire FilmArray 2.0 system. Conversely, the BioFire system showed statistically significant higher sensitivity for saliva specimens, highlighting how method performance varies substantially by sample matrix [119].
In a 2024 evaluation comparing one-step real-time PCR and one-step RT-LAMP methods researchers analyzed 342 clinical samples and found strong agreement between the two methods (93-94% based on Cohen's kappa coefficient, p < 0.001). The RT-LAMP method demonstrated 100% specificity and sensitivity at a dilution of 1 × 10¹, supporting its reliability as a diagnostic tool despite its simpler operational requirements [13].
Detailed Experimental Protocols
Conventional RT-qPCR Methodology
The following protocol is adapted from the laboratory-developed test (LDT) used at Helsinki University Hospital Laboratory (HUSLAB) and represents a robust, widely-adopted approach for SARS-CoV-2 detection [118]:
Sample Inactivation and Lysis:
- Combine 250μL of patient specimen with 250μL of MagNA Pure Lysis/Binding Buffer
- Incubate mixture for minimum of 10 minutes at room temperature in a biosafety cabinet
Nucleic Acid Extraction:
- Extract nucleic acids from 450μL of specimen lysate using MagNA Pure Viral NA SV 2.0 Kit
- Utilize MagNA Pure 96 instrument for automated extraction
- Elute in 50μL of elution buffer
RT-PCR Reaction Setup:
- Prepare 25μL reactions containing:
- 5μL of extracted RNA template
- 600nM forward primer (CACATTGGCACCCGCAATC)
- 800nM reverse primer (GAGGAACGAGAAGAGGCTTG)
- 200nM probe (FAM-ACTTCCTCAAGGAACAACATTGCCA-BBQ)
- SuperScript III Platinum One-Step qRT-PCR Kit components
- Perform amplification on Stratagene Mx3005p PCR instrument with cycling conditions:
- 1 cycle: 55°C for 20 minutes (reverse transcription)
- 1 cycle: 95°C for 15 minutes (initial denaturation)
- 45 cycles: 94°C for 15 seconds, 58°C for 40 seconds (amplification)
This protocol specifically targets the SARS-CoV-2 N gene, which was selected for its superior sensitivity compared to other targets like RdRP based on dilution series experiments [118].
RT-LAMP Protocol for SARS-CoV-2 Detection
The following one-step RT-LAMP protocol is adapted from a 2024 study that demonstrated high sensitivity and specificity for SARS-CoV-2 detection [13]:
Primer Design:
- Design LAMP primers targeting the N gene (NC_045512.2) using Primer Explorer V5 software
- Prepare a set of 6 primers recognizing 8 distinct regions on the target sequence:
- External primers: F3 (18nt) and B3 (20nt)
- Internal primers: FIP (F1c [18nt] + F2 [19nt]) and BIP (B1c [21nt] + B2 [20nt])
- Loop primers: LF (21nt) and LB (20nt)
- Verify specificity using Primer BLAST against SARS-CoV-2 database
RT-LAMP Reaction:
- Prepare 25μL reaction mixture containing:
- 5pmol each of F3 and B3 external primers
- 40pmol each of FIP and BIP internal primers
- 20pmol each of LF and LB loop primers
- 8U (1μL) of Bst DNA/RNA Polymerase 3.0
- Add 5μL of RNA template (extracted or direct sample)
- Incubate reaction at 63°C for 30-60 minutes
- Visualize results via colorimetric change or fluorescent detection
This methodology enables direct detection from patient samples without RNA extraction, significantly reducing both hands-on time and total turnaround time compared to conventional RT-qPCR [13].
Operational Workflow Visualization
Diagram 1: SARS-CoV-2 Detection Workflow Comparison. This diagram illustrates the procedural steps and approximate time requirements for three molecular detection platforms, color-coded by technical expertise level: Red (Advanced), Green (Moderate), and Blue (Minimal).
Technical Expertise Requirements Hierarchy
Diagram 2: Technical Expertise Requirements Hierarchy. This diagram categorizes the specific technical skills required for each detection platform, illustrating the progressive reduction in specialized knowledge needed from conventional methods to fully automated systems.
Research Reagent Solutions
Table 2: Essential Research Reagents for SARS-CoV-2 Molecular Detection
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Viral Transport Media (VTM) | Preserves specimen integrity during transport and storage | Used for nasopharyngeal swab collection [119] [118] |
| Lysis/Binding Buffer | Inactivates virus and releases RNA for extraction | MagNA Pure Lysis/Binding Buffer [118] |
| RNA Extraction Kits | Isolates and purifies viral RNA from clinical samples | Qiagen RNeasy, Invitrogen Purelink, Norgen Biotek, BGI kits [9] |
| One-Step RT-qPCR Master Mix | Contains reverse transcriptase and DNA polymerase for amplification | SuperScript III Platinum One-Step, NEB Luna kits [13] [118] |
| Primer/Probe Sets | Sequence-specific oligonucleotides for target detection | CDC N1/N2, WHO-recommended E/RdRP/N gene targets [9] [118] |
| Bst DNA/RNA Polymerase | Enzyme for isothermal amplification with reverse transcription capability | Key component in RT-LAMP reactions [13] |
| LAMP Primers | Specialized primer sets recognizing multiple target regions | Designed for N gene detection [13] |
| Positive Controls | Synthetic RNA or inactivated virus for assay validation | Twist Bioscience synthetic RNA standards [9] |
The operational considerations for SARS-CoV-2 molecular detection methods present researchers with clear trade-offs between cost, turnaround time, and technical expertise requirements. Conventional RT-qPCR remains the sensitivity benchmark with well-established protocols but demands significant expertise and time investment. Isothermal methods like RT-LAMP offer compelling advantages in speed and operational simplicity with minimal sensitivity compromise, making them ideal for resource-limited settings or rapid screening applications. Next-generation systems provide the simplest operational workflow but at substantially higher cost.
Research program needs should drive method selection: large-scale studies requiring high throughput may benefit from automated NGDS despite higher costs; field studies or projects with limited budgets may prefer isothermal methods; and basic science investigations requiring maximum sensitivity may continue to utilize conventional RT-qPCR. As these technologies continue to evolve, ongoing assessment of these operational parameters will remain essential for efficient research planning and execution in SARS-CoV-2 and related infectious disease research.
Conclusion
The comparative analysis reveals that no single molecular method universally outperforms others across all applications. RT-qPCR remains the gold standard for diagnostic sensitivity, while RT-LAMP offers compelling advantages for rapid, decentralized testing. Rapid antigen tests provide valuable screening utility in high viral load scenarios but show sensitivity limitations at Ct values >25. Next-generation sequencing is indispensable for variant surveillance and requires robust validation under ISO15189 standards. Future directions should focus on developing adaptable diagnostic platforms capable of responding to emerging variants, integrating point-of-care molecular testing into public health infrastructure, and establishing universal validation frameworks for novel methodologies. The lessons from SARS-CoV-2 diagnostics will be crucial for pandemic preparedness against future emerging pathogens, emphasizing the need for flexible, scalable testing strategies that combine reliability with accessibility.
References
- 1. COVID-19 Diagnosis: A Comprehensive Review of the RT-qPCR Method for Detection of SARS-CoV-2 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9221722/]
- 2. Comparison of SARS-CoV-2 indirect and direct RT-qPCR detection methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8127261/]
- 3. and Sensitivity Evaluation of Three Different Commercial... Comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC8309997/]
- 4. Commercially available SARS-CoV-2 RT-qPCR diagnostic tests need obligatory internal validation | Scientific Reports [https://www.nature.com/articles/s41598-023-34220-w]
- 5. Construction and validation of a cell based reporter assay for identifying inhibitors of SARS coronavirus 2 RNA dependent RNA polymerase activity | Scientific Reports [https://www.nature.com/articles/s41598-025-03813-y]
- 6. Multiplex real-time RT - PCR method for the diagnosis of... [https://www.nature.com/articles/s41598-022-06977-z?error=cookies_not_supported&code=9e6327c7-fdba-4926-af30-65a56dcf2338]
- 7. Positive control synthesis method for COVID-19 diagnosis by one-step real-time RT-PCR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7550048/]
- 8. Poor sensitivity of "AccuPower SARS - CoV - 2 real time RT - PCR kit..." [https://virologyj.biomedcentral.com/articles/10.1186/s12985-020-01445-4]
- 9. Comparison of SARS-CoV-2 indirect and direct RT-qPCR detection methods | Virology Journal | Full Text [https://virologyj.biomedcentral.com/articles/10.1186/s12985-021-01574-4]
- 10. Diagnostic performance of a colorimetric RT -LAMP for the identification of SARS-CoV-2: A multicenter prospective clinical evaluation in sub-Saharan Africa - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8401528/]
- 11. Enhanced Point-of-Care SARS - CoV - 2 Detection: Integrating RT - LAMP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274610/]
- 12. Detection of SARS-CoV-2 using RT-LAMP in saliva specimens | IJGM [https://www.dovepress.com/the-performance-of-severe-acute-respiratory-syndrome-coronavirus-2-sar-peer-reviewed-fulltext-article-IJGM]
- 13. Evaluation and comparison of one-step real-time PCR and one-step... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09574-9]
- 14. Rapid Detection of SARS - CoV - 2 Using Reverse... | medRxiv [https://www.medrxiv.org/content/10.1101/2020.03.02.20030130v1.full]
- 15. Detection of SARS - CoV - 2 RNA using RT - LAMP and molecular beacons [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02387-y]
- 16. Diagnostic accuracy of LAMP over the course of... versus PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC8056478/]
- 17. Point-of-care COVID-19 diagnostics powered by lateral flow assay - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8487324/]
- 18. . Antigen : Benefits, Limitations, and Practical... vs Molecular [https://www.physiciansofficeresource.com/articles/point-of-care-testing/antigen-vs-molecular/]
- 19. The Journal of Kırıkkale University Faculty of Medicine » Submission »... [https://dergipark.org.tr/en/pub/kutfd/issue/94274/1702068]
- 20. : less haste, more speed please Antigen testing vs PCR [https://www.cepheid.com/en-US/insights/insight-hub/respiratory-health/2025/09/antigen-testing-vs-pcr-less-haste-more-speed-please.html]
- 21. Catching SARS - CoV - 2 by Sequence Hybridization: a Comparative ... [https://pubmed.ncbi.nlm.nih.gov/34342536/]
- 22. A comparison of five Illumina, Ion Torrent, and nanopore sequencing... [https://link.springer.com/article/10.1007/s10096-023-04590-0]
- 23. Frontiers | A Benchmark of methods for SARS - CoV - 2 whole genome... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1516791/full]
- 24. Analytical Performance of a Novel Nanopore Sequencing for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11621993/]
- 25. Diagnostics of COVID-19 Based on CRISPR –Cas Coupled to... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9222122/]
- 26. Next-Generation Sequencing (NGS) in COVID-19: A Tool for SARS-CoV-2 Diagnosis, Monitoring New Strains and Phylodynamic Modeling in Molecular Epidemiology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8929009/]
- 27. Harnessing CRISPR-Cas to Combat COVID-19: From Diagnostics to Therapeutics [https://www.mdpi.com/2075-1729/11/11/1210]
- 28. Frontiers | Internet of medical things-enabled CRISPR diagnostics for rapid detection of SARS-CoV-2 variants of concern [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1070940/full]
- 29. Rapid and accurate detection of SARS - CoV - 2 using the RHAM... [https://www.nature.com/articles/s41598-023-49733-7?error=cookies_not_supported&code=bd387089-7d4b-4690-9f84-ac12203202c5]
- 30. Enhanced detection of SARS-CoV-2 spike protein using nitrogen-doped graphene quantum dot-based SPR biosensors | npj Biosensing [https://www.nature.com/articles/s44328-025-00046-x]
- 31. Sensitive Detection of SARS-CoV-2 Using a Programmable AND-Logic-Gated CRISPR-Cas12 System Based on RTF-EXPAR - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0925400525014078]
- 32. Accuracy of novel antigen rapid diagnostics for SARS - CoV - 2 : A living... [https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003735]
- 33. Development and Validation of Two RT-qPCR Diagnostic Assays for ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC8813189]
- 34. Forensic evaluation of two nucleic acid extraction systems and validation of a RT-qPCR protocol for identification of SARS-CoV-2 in post-mortem nasopharyngeal swabs - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0379073821000955]
- 35. Comparison of Two RNA Extraction Methods for the Molecular Detection of SARS-CoV-2 from Nasopharyngeal Swab Samples - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9317615/]
- 36. Evaluation of extraction-free RT-qPCR methods for SARS-CoV-2 diagnostics | Archives of Virology [https://link.springer.com/article/10.1007/s00705-021-05165-0]
- 37. Diagnostic power of one-step and two-step RT-qPCR methods to SARS‑CoV‑2 detection | BMC Infectious Diseases | Full Text [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-022-07478-0]
- 38. The effects of RT - qPCR standards on reproducibility and comparability... [https://www.nature.com/articles/s41598-024-77155-6?error=cookies_not_supported&code=5ae3fbbc-1bc2-4f32-b755-e9bfc7cec2ab]
- 39. Analyzing real-time PCR data by the comparative CT method | Nature Protocols [https://www.nature.com/articles/nprot.2008.73]
- 40. Statistical analysis of real-time PCR data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1395339/]
- 41. A diagnostic accuracy study comparing RNA LAMP , direct LAMP , and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9813509/]
- 42. Modeling the effectiveness of RT-PCR, RT-LAMP, and antigen testing strategies for COVID-19 control | BMC Infectious Diseases | Full Text [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11793-7]
- 43. between Comparison -qPCR and RT Methods for a LAMP ... Rapid [https://www.intechopen.com/chapters/1130226]
- 44. of Comparison with RT-PCR for COVID-19... Rapid Antigen Test [https://romj.org/2024-0210]
- 45. of detection in different matrices of 19 commercially available... Limit [https://www.nature.com/articles/s41598-021-97489-9?error=cookies_not_supported&code=f6bffbd9-3a37-4591-90af-0cd77697bc65]
- 46. of rapid and connected salivary Performances - RT diagnostic... LAMP [https://www.nature.com/articles/s41598-022-04826-7?error=cookies_not_supported&code=18352475-5458-4da6-8661-1f5d70bf22c8]
- 47. Frontiers | A diagnostic accuracy study comparing RNA LAMP , direct... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1063414/full]
- 48. Post-market surveillance of six COVID-19 point-of-care tests using pre-Omicron and Omicron SARS-CoV-2 variants - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11218491/]
- 49. Cost and cost-effectiveness of four different SARS-CoV-2 active surveillance strategies: evidence from a randomised control trial in Germany | The European Journal of Health Economics [https://link.springer.com/article/10.1007/s10198-022-01561-8]
- 50. Coronavirus Sequencing | NGS for COVID-19... [https://www.illumina.com/areas-of-interest/microbiology/public-health-surveillance/coronavirus-sequencing.html]
- 51. Evaluation of next approaches for... generation sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10643093/]
- 52. of Comparison - SARS - CoV whole genome 2 using tiled... sequencing [https://www.nature.com/articles/s41598-023-33168-1?error=cookies_not_supported&code=89a38e42-df47-4b99-9e65-0af11428df14]
- 53. of Comparison - SARS - CoV using the ONT GridION and... 2 sequencing [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-022-08541-5]
- 54. Mass molecular testing for COVID19 using NGS -based technology and... [https://www.nature.com/articles/s41598-021-86498-3?error=cookies_not_supported&code=71bce97a-d895-4ed3-851b-8c6f812bcd09]
- 55. of Seven Performance - SARS - CoV Self-Tests Based on 2 ... Saliva [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466378/]
- 56. of Performance and saliva in detecting Delta... nasopharyngeal swab [https://pmc.ncbi.nlm.nih.gov/articles/PMC9348014/]
- 57. COVID-19: molecular diagnostics overview | Journal of Molecular Medicine [https://link.springer.com/article/10.1007/s00109-020-01931-w]
- 58. is superior over Saliva for detecting... nasopharyngeal swab [https://www.nature.com/articles/s41598-021-02097-2?error=cookies_not_supported&code=9d7ce3ac-8562-41a8-b5a1-d5da1704afc9]
- 59. SARS-Cov-2 Viral Load in Nasal Swab and Raw Saliva Samples from COVID-19 Patients [https://www.fortunejournals.com/articles/sarscov2-viral-load-in-nasal-swab-and-raw-saliva-samples-from-covid19-patients.html]
- 60. Performance comparison of three commercial multiplex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369576/]
- 61. Frontiers | Simultaneously ultrasensitive and differential detection of... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1540676/full]
- 62. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 63. Optimisation of a multiplexed , high throughput assay to measure... [https://pubmed.ncbi.nlm.nih.gov/39557342/]
- 64. Pooled PPIseq: Screening the SARS - CoV - 2 and human... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0299440]
- 65. and Reinfections: the Challenges of... false Negatives [https://asm.org/articles/2020/april/false-negatives-and-reinfections-the-challenges-of]
- 66. A Comparison of Five SARS - CoV - 2 Assays With Clinical... Molecular [https://pubmed.ncbi.nlm.nih.gov/33015712/]
- 67. the performance of Comparing commercial assays for detection of... two [https://jlpm.amegroups.org/article/view/6366/html]
- 68. rate of COVID-19 PCR testing: a discordant testing... false negative [https://virologyj.biomedcentral.com/articles/10.1186/s12985-021-01489-0]
- 69. International Journal of Molecular Medicine [https://www.spandidos-publications.com/10.3892/ijmm.2020.4673]
- 70. Frontiers | Reality check: testing the in silico predictions of false... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1524025/full]
- 71. of three Comparison assays for... molecular diagnostic [https://pmc.ncbi.nlm.nih.gov/articles/PMC8842162/]
- 72. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT–qPCR primer–probe sets | Nature Microbiology [https://www.nature.com/articles/s41564-020-0761-6]
- 73. PANDAA intentionally violates conventional qPCR design to enable... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7892852/]
- 74. TaqMan Primers and Probes ... | Thermo Fisher Scientific - DE [https://www.thermofisher.com/de/de/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/taqman-primers-and-probes-support/taqman-primers-and-probes-support-getting-started.html]
- 75. , Sample III.ppt collection Storage [https://www.slideshare.net/slideshow/sample-collection-storage-iiippt/264116042]
- 76. , Sample and collection processing storage [https://pubmed.ncbi.nlm.nih.gov/9354922/]
- 77. characteristics of the Performance - SARS - CoV Isothermal... | medRxiv 2 [https://www.medrxiv.org/content/10.1101/2025.03.29.25324880v1]
- 78. , Sample and Collection - SlideServe Processing Storage [https://www.slideserve.com/aparicio/sample-collection-processing-and-storage-powerpoint-ppt-presentation]
- 79. the analytical Comparing of three... performance [https://pubmed.ncbi.nlm.nih.gov/32361285/]
- 80. Molecular and Serological Tests for COVID-19. A Comparative Review of SARS-CoV-2 Coronavirus Laboratory and Point-of-Care Diagnostics [https://www.mdpi.com/2075-4418/10/6/434]
- 81. An Optimised Direct Lysis Method for Viral RNA and... Extraction [https://pubmed.ncbi.nlm.nih.gov/32651775/]
- 82. of Three Conventional Comparison Methods for the... Extraction [https://scialert.net/fulltext/?doi=ajps.2007.102.107]
- 83. Frontiers | Preparation of MS2 Phage-Like Particles and Their Use As... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2016.01911/full]
- 84. of small and large RNAs in bacteria for excellent... Efficient extraction [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-015-1726-3]
- 85. of the Comparison of different cell lysis methods and... efficiency [https://link.springer.com/article/10.1186/s12866-019-1473-z]
- 86. Laboratory Considerations for Reporting Cycle in... Threshold Value [https://pmc.ncbi.nlm.nih.gov/articles/PMC9562486/]
- 87. RT-PCR CT : Everything You Need To Know - Homage Malaysia Value [https://www.homage.com.my/resources/covid-19-ct-value/]
- 88. A Systematic Review of the Clinical Utility of Cycle ... Threshold Values [https://link.springer.com/article/10.1007/s40121-020-00324-3]
- 89. - SARS - CoV , 2 - CT , and Infectivity—Conclusions to Be Drawn... Values [https://pmc.ncbi.nlm.nih.gov/articles/PMC8402774/]
- 90. What’s a PCR test cycle and why it matters – Full Fact threshold [https://fullfact.org/health/cycle-threshold-values/]
- 91. Frontiers | Pilot study: a descriptive-retrospective analysis of SARS-CoV-2 variants distribution and phylogenesis in the Phlegraean area [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1536953/full]
- 92. Clinical Comparison of Three Sample-to-Answer Systems for... [https://www.dovepress.com/clinical-comparison-of-three-sample-to-answer-systems-for-detecting-sa-peer-reviewed-fulltext-article-IDR]
- 93. The Limit Matters: The Case for Benchmarking of ... Detection Severe [https://pmc.ncbi.nlm.nih.gov/articles/PMC7929140/]
- 94. Comparison of the clinical sensitivity and specificity of two commercial RNA SARS-CoV-2 assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8863925/]
- 95. Comparison of two digital PCR methods for EGFR DNA and SARS-CoV-2 RNA quantification - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8206622/]
- 96. Comparison of the performance of two real-time fluorescent quantitative PCR kits for the detection of SARS-CoV-2 nucleic acid: a study based on large real clinical samples | Virology Journal | Full Text [https://virologyj.biomedcentral.com/articles/10.1186/s12985-022-01922-y]
- 97. COVID-19 Diagnostic Methods and Detection Techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8409760/]
- 98. of antigen testing for Performance of COVID-19: a direct... diagnosis [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06524-7]
- 99. of the Comparison of a Rapid Antigen Test... Diagnostic Performance [https://www.dovepress.com/comparison-of-the-diagnostic-performance-of-a-rapid-antigen-test-with--peer-reviewed-fulltext-article-IDR]
- 100. evaluation of RT-PCR and antigen-based rapid... Comparative [https://pubmed.ncbi.nlm.nih.gov/38683014/]
- 101. of Comparison - SARS - CoV test 2 by sample type and... performance [https://www.news-medical.net/news/20220210/Comparison-of-SARS-CoV-2-test-performance-by-sample-type-and-modality-in-close-contacts-of-SARS-CoV-2-cases.aspx]
- 102. Frontiers | Comparative analysis of neutralization assays performed ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1650083/full]
- 103. Evaluation of a Fully Automated Molecular Performance ... Diagnostic [https://www.mdpi.com/2075-4418/15/14/1791]
- 104. SARS-CoV-2 Alpha - Wikipedia variant [https://en.wikipedia.org/wiki/SARS-CoV-2_Alpha_variant]
- 105. How Dangerous Is the Delta (B.1.617.2)? Variant [https://asm.org/articles/2021/july/how-dangerous-is-the-delta-variant-b-1-617-2]
- 106. Is Omicron worse than Delta ? [https://www.drugs.com/medical-answers/omicron-worse-delta-3564030/]
- 107. - COVID | WHO 19 - variants dashboard COVID 19 [https://data.who.int/dashboards/covid19/variants]
- 108. SARS-CoV-2 virus variant detection and mortality prediction through symptom analysis using machine learning - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0952197623019279]
- 109. Variants and Genomic Surveillance | COVID-19 | CDC [https://www.cdc.gov/covid/php/variants/variants-and-genomic-surveillance.html]
- 110. ISO 15189 for medical laboratories [https://blog.johner-institute.com/regulatory-affairs/iso-15189-medical-laboratories/]
- 111. EN ISO 15189 and its Role in the IVD Regulation [https://www.bdbiosciences.com/en-eu/learn/science-thought-leadership/blogs/medical-laboratories-quality-management-system-requirements]
- 112. Authorized SARS-CoV-2 molecular methods show wide ... [https://www.sciencedirect.com/science/article/abs/pii/S0732889322002449]
- 113. The New EU Regulation on In Vitro Diagnostic Medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8061679/]
- 114. In Vitro Diagnostic Regulation (IVDR)—Frequently Asked ... [https://www.thermofisher.com/us/en/home/clinical/ivdr/faqs.html]
- 115. IVDR Performance Evaluation: 2025 Compliance Guide [https://lfhregulatory.co.uk/performance-evaluation-under-ivdr-2025/]
- 116. Comparison of performance between three SARS‐CoV‐2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9088664/]
- 117. Comparison of 12 Molecular Detection Assays for Severe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7699162/]
- 118. Comparison of two commercial platforms and a laboratory developed test for detection of SARS-CoV-2 RNA | medRxiv [https://www.medrxiv.org/content/10.1101/2020.07.03.20144758v1.full]
- 119. of next generation diagnostic systems (NGDS) for the... Comparison [https://pubmed.ncbi.nlm.nih.gov/35174538/]