Comparative Viral Infectivity Testing In Vitro: Methods, Applications, and Advancements for Drug Development
In vitro viral infectivity testing is a cornerstone of virology, antiviral drug development, and vaccine efficacy studies.
Comparative Viral Infectivity Testing In Vitro: Methods, Applications, and Advancements for Drug Development
Abstract
In vitro viral infectivity testing is a cornerstone of virology, antiviral drug development, and vaccine efficacy studies. This article provides a comprehensive analysis of the established and emerging methodologies used to quantify and compare viral infectivity. We explore foundational principles, including the critical distinction between detecting viral components and measuring functional infectivity. A detailed comparison of methodological approaches—from traditional plaque and TCID50 assays to modern flow cytometry and label-free technologies—is presented, alongside protocols for critical applications like neutralization testing. The content further addresses common troubleshooting scenarios and optimization strategies to enhance assay robustness and reproducibility. Finally, we discuss validation frameworks per global regulatory standards (ICH Q5A(R2), FDA, EMA, China CDE) and the strategic selection of methods for comparative studies, illustrated with case studies from recent research on SARS-CoV-2, LCMV, and viral vectors for gene therapy.
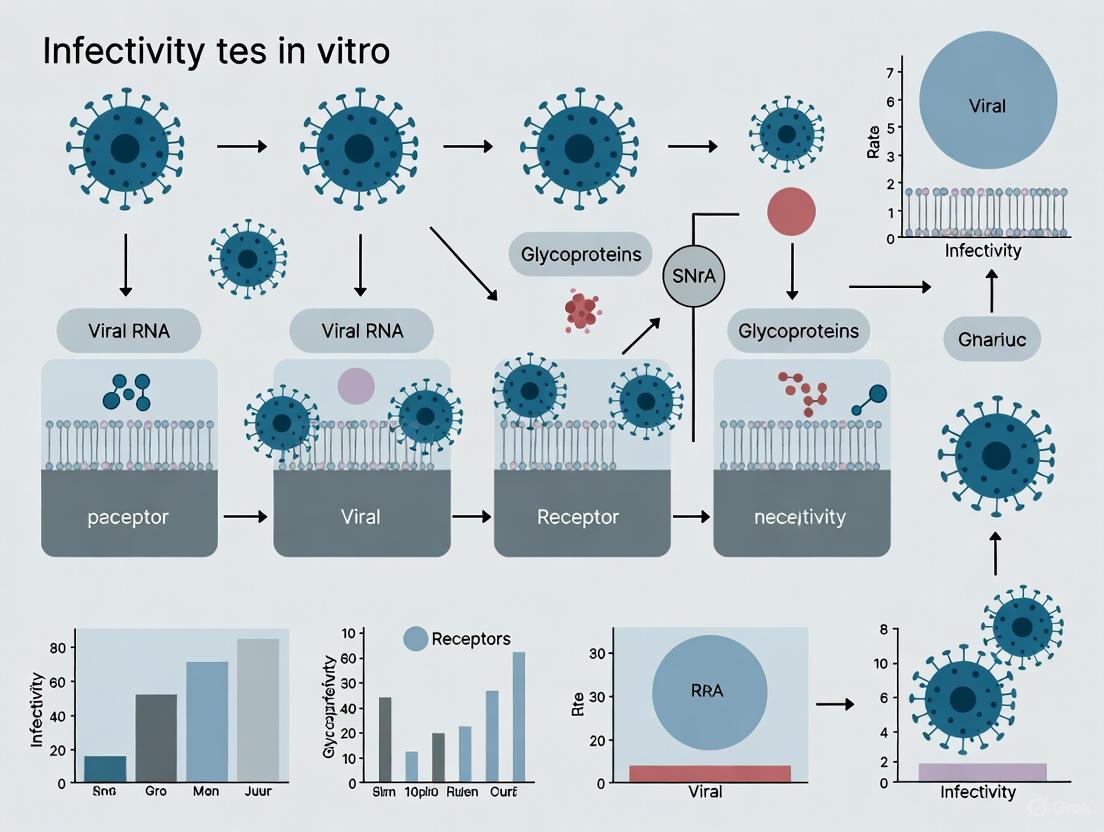
Viral Infectivity Fundamentals: From Viral Lifecycle to Quantitative Measurement
Contents
- Key Concepts and Definitions
- Comparative Methods for Quantifying Viral Infectivity
- Advanced Concepts: Collective Infectious Units
- Experimental Workflows
- Research Reagent Solutions
Key Concepts and Definitions
Viral infectivity is fundamentally defined as the ability of a virus to enter a host cell, replicate within it, and spread to new cells [1]. However, a critical challenge in virology is that not all virus particles are infectious. This distinction separates the mere presence of viral components (like proteins or nucleic acids) from the actual functional capacity to cause an infection. The gold standard for measuring infectivity relies on functional assays that demonstrate a virus's ability to complete its replication cycle in a susceptible cell culture system [2] [3].
A core principle for understanding this distinction is the particle-to-PFU ratio. This ratio compares the total number of physical virus particles in a sample (often determined by methods like electron microscopy or quantitative PCR) to the number of particles capable of forming a plaque—a Plaque-Forming Unit (PFU) [4]. A ratio of 1, as seen in some bacteriophages, indicates that every physical particle is infectious. In contrast, for many animal viruses, this ratio can be much higher.
Table 1: Representative Particle-to-PFU Ratios for Different Viruses
| Virus | Typical Particle-to-PFU Ratio | Implication for Infectivity |
|---|---|---|
| Bacteriophage (e.g., T4) | ~1 [4] | Nearly every viral particle is infectious. |
| Poliovirus | >1000 (can be very high) [4] | A very small fraction of particles initiate a productive infection. |
| Vesicular Stomatitis Virus (VSV) | Varies; aggregation can increase co-infection [5] | Infectivity is influenced by factors like virion aggregation. |
High particle-to-PFU ratios can arise from several factors. Many particles may contain lethal mutations in their genomes or may have been damaged during purification. Furthermore, the infectious cycle is complex, and a particle may fail at any step—from entry and uncoating to genome replication and assembly—preventing the completion of an infectious cycle [4]. This highlights that detecting viral RNA or proteins (e.g., via PCR or ELISA) does not equate to detecting infectious virus, a distinction crucial for diagnostics and public health policies [6].
Comparative Methods for Quantifying Viral Infectivity
Different assays provide varying information about viral infectivity, each with its own advantages and limitations. The following table summarizes key methods used in quantitative comparisons.
Table 2: Key Assays for Quantifying Viral Infectivity and Components
| Assay Name | What is Measured? | Principle | Output Data |
|---|---|---|---|
| Plaque Assay [2] | Infectious Units (PFU/mL) | Serial dilutions of virus are applied to a cell monolayer. After incubation, plaques (clear zones of lysed cells) are counted. | Quantitative titer of infectious virus (PFU/mL). |
| TCID50 Assay [3] | Infectious Dose (Tissue Culture Infectious Dose 50%) | Serial dilutions of virus are applied to cells and observed for cytopathic effect (CPE). The dilution that infects 50% of the cultures is calculated. | Quantitative titer of infectious virus (TCID50/mL). |
| PCR / qRT-PCR [2] | Viral Genome Copies | Amplification of specific viral nucleic acid sequences. Does not distinguish between infectious and non-infectious particles. | Quantitative number of genome copies per volume. |
| ELISA [2] | Viral Antigens | Detection of viral proteins using specific antibodies. Does not distinguish between infectious and non-infectious particles. | Semi-quantitative or quantitative measure of viral protein. |
| Immunofluorescence Assay (IFA) [2] | Viral Proteins in Infected Cells | Fixed cells are stained with fluorescently tagged antibodies against viral antigens and visualized by microscopy. | Qualitative/Quantitative detection of infection in cells. |
| Hemagglutination Assay [2] | Viral Particles Capable of Agglutinating RBCs | Some viruses can bind to and cross-link red blood cells (RBCs). The titer is the highest dilution that causes agglutination. | Quantitative measure of virus particles with functional surface proteins. |
Advanced Concepts: Collective Infectious Units
The traditional model of viral spread involves independent virions. However, growing evidence shows that viruses often spread via collective infectious units, structures that simultaneously deliver multiple viral genomes to a cell [5]. This increases the multiplicity of infection (MOI) independently of viral population density and has profound implications for viral evolution, including the maintenance of genetic diversity and the evolution of social-like interactions such as cooperation and complementation [5].
The main types of collective infectious units include:
- Polyploid Virions: Some virions naturally contain multiple genome copies. Retroviruses are pseudo-diploid, and some paramyxoviruses (e.g., measles) and filoviruses (e.g., Ebola) can package multiple genomes [5] [3].
- Virion Aggregates: Viral particles can form aggregates, often promoted by body fluids like saliva or by non-neutralizing antibodies. These aggregates are transmitted as a single infectious unit, facilitating co-infection [5] [7].
- Virion-Containing Lipid Vesicles: Enteroviruses and other viruses can be released from cells enclosed within lipid microvesicles. These vesicles protect the virions and enable the co-transmission of multiple genomes to a new cell [5] [6].
- Virus-Induced Cell-Cell Structures: Viruses like HIV can induce the formation of virological synapses, which are specialized cell-cell contacts that allow for the direct cell-to-cell transfer of viral progeny, efficiently delivering a high number of virions [5].
Experimental Workflows
A standard workflow for quantifying viral infectivity begins with cell culture, as viruses are obligate intracellular parasites that require living cells to replicate [2]. The following diagram outlines the key steps from generating a virus stock to determining its infectious titer.
Detailed Protocol: Plaque Assay for Infectivity Titer Determination
The plaque assay is a fundamental method for quantifying infectious virus. Below is a generalized protocol that can be adapted for specific viruses.
- Cell Seeding: Seed permissive cells into a multi-well plate (e.g., 6-well or 96-well) to form a confluent monolayer. Allow cells to adhere overnight [2] [3].
- Virus Inoculation:
- Prepare serial log10 dilutions (e.g., 10-1 to 10-8) of the virus stock in an appropriate dilution buffer (e.g., serum-free maintenance medium).
- Remove the growth medium from the cell monolayers and wash with phosphate-buffered saline (PBS).
- Carefully add the virus dilutions to the respective wells. Gently rock the plate to ensure even distribution.
- Incubate the plate at the appropriate temperature (e.g., 37°C for mammalian viruses) for a defined adsorption period (e.g., 1-2 hours), with occasional rocking.
- Overlay and Incubation:
- After adsorption, remove the virus inoculum.
- Overlay the cell monolayer with a semi-solid medium (e.g., carboxymethylcellulose, agarose, or methylcellulose) mixed with maintenance medium. This restricts released virions to infecting only neighboring cells, leading to the formation of discrete plaques.
- Incubate the plates for the required time (typically 2-7 days, depending on the virus) until plaques become visible.
- Plaque Visualization and Counting:
- Plaques can be visualized by various methods:
- Direct Microscopy: Some plaques are visible as clear areas against the confluent cell layer.
- Staining: Fix cells with formaldehyde and stain with crystal violet or neutral red. Live cells take up the stain, while plaques remain clear [2].
- Count plaques in wells that have a countable number (ideally 20-100 plaques). Calculate the viral titer using the formula:
- PFU/mL = (Number of plaques) / (Dilution factor × Volume of inoculum (mL))
- Plaques can be visualized by various methods:
Research Reagent Solutions
Successful viral infectivity testing relies on a suite of specialized reagents and tools. The following table details essential materials and their functions in a research context.
Table 3: Essential Research Reagents and Materials for Viral Infectivity Studies
| Reagent / Material | Function in Viral Infectivity Research |
|---|---|
| Cell Culture Systems (Primary, Immortalized, or Designer Cells) [2] | Provides the necessary living host cells for virus replication. Cell type must express appropriate viral receptors and internal machinery. |
| Maintenance and Growth Media [2] | Supplies nutrients and optimal conditions (pH, osmolarity) to sustain cell health and support viral replication. |
| Semi-Solid Overlay (e.g., Carboxymethylcellulose, Agarose) [2] | Restricts virus diffusion in plaque assays, enabling the formation of discrete, countable plaques. |
| Fixatives and Stains (e.g., Formaldehyde, Crystal Violet) [2] | Used to fix cells and stain the cell monolayer for clear visualization of plaques against a contrasting background. |
| Specific Antibodies (for IFA, ELISA) [2] | Enables detection and localization of viral antigens within infected cells (IFA) or quantification in a sample (ELISA). |
| Fluorescent Tags (e.g., GFP, Alexa Dyes) [2] | Allows direct visualization of viral proteins or tracking of infection progress through live or fixed cell microscopy. |
| Protease (Trypsin) and Collagenase [2] | Enzymes used to dissociate tissues for generating primary cell cultures (collagenase) or to passage adherent cells (trypsin). |
| Centrifugation Equipment (Ultracentrifuges) [2] | Essential for purifying and concentrating virus particles away from cellular debris and media components. |
| PCR/qPCR Reagents and Primers [2] | For highly sensitive detection and quantification of viral genome copies, though it does not indicate infectivity. |
The Viral Lifecycle as a Framework for Infectivity Assays
Viral infectivity assays are fundamental tools in virology, providing critical data on viral replication kinetics, antiviral drug efficacy, and neutralizing antibody responses. The selection of an appropriate infectivity assay is profoundly influenced by the specific stage of the viral lifecycle it targets, from initial entry to the final stages of progeny release and cell death. This guide provides an objective comparison of contemporary viral infectivity assay technologies, evaluating their performance characteristics, experimental requirements, and applications within the framework of the viral lifecycle. We present structured experimental data and detailed protocols to assist researchers in selecting optimal methodologies for their specific investigative needs in antiviral development and basic virology research.
Assay Technology Comparison
Modern viral infectivity assays can be broadly categorized based on their detection principle, throughput, and the specific lifecycle stage they monitor. The following table summarizes the key technologies currently employed in research settings.
Table 1: Comparative Analysis of Viral Infectivity Assay Technologies
| Assay Technology | Lifecycle Stage Targeted | Throughput | Time to Result | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Plaque Assay (PFU) [8] | Late (CPE) | Low | 3-7 days | Direct quantification of infectious units; considered a gold standard | Low throughput; subjective manual counting; lengthy process |
| Endpoint Dilution (TCID₅₀) [9] | Late (CPE) | Medium | 3-7 days | Does not require overlay; can handle viruses that don't form clear plaques | Statistical rather than direct count; lower precision |
| Focus Forming Unit (FFU) [8] | Intermediate (Antigen Expression) | Low | 2-3 days | Detects infected foci before full CPE; uses immunostaining | Requires specific antibodies; additional staining steps |
| AI-Powered Imaging (DVICE) [10] [11] | Late (CPE) / Morphology | High | 1-7 days (real-time possible) | Label-free; high-throughput; objective; virus-specific feature recognition | Requires initial training dataset; model transferability challenges |
| Real-Time Cell Analysis (RTCA) [12] | Late (CPE) / Cell Viability | High | Minutes to Days | Label-free, real-time kinetic data; continuous monitoring | Indirect measure of infectivity; specialized equipment required |
| Luciferase Reporter Assay [13] | Early (Entry/Replication) | High | 1-2 days | Highly sensitive; measures early infection events | Requires engineered reporter viruses; not suitable for clinical isolates |
| Fluorescence Microscopy [12] | Intermediate (Antigen Expression) | Medium | 1-3 days | Direct visualization of infection; can be quantitative | Requires fluorescent tags or antibodies; imaging analysis needed |
Quantitative Performance Data
The quantitative output of an infectivity assay is a critical performance metric. Data from recent studies demonstrate the sensitivity and dynamic range of various methodologies.
Table 2: Experimental Antiviral Efficacy Data from Recent Studies
| Antiviral Compound / Technology | Virus Tested | Assay Type | Key Quantitative Result | Cell Line Used | Reference |
|---|---|---|---|---|---|
| Thymol | Influenza A/H1N1 | Crystal Violet (IC₅₀) | IC₅₀ = 0.022 µg/mL | MDCK | [9] |
| Limonin | Influenza A/H1N1 | Crystal Violet (IC₅₀) | IC₅₀ = 4.25 µg/mL | MDCK | [9] |
| Thymol | SARS-CoV-2 | Crystal Violet (IC₅₀) | IC₅₀ = 0.591 µg/mL | Vero E6 | [9] |
| Limonin | SARS-CoV-2 | Crystal Violet (IC₅₀) | IC₅₀ = 4.04 µg/mL | Vero E6 | [9] |
| GW4064 (FXR agonist) | HEV | Novel in vitro multi-infection | 85-95% reduction in intracellular HEV RNA | dHuH7.5-NTCP | [14] |
| Sofosbuvir | HCV & HEV | Novel in vitro multi-infection | >90% reduction in viral RNAs | dHuH7.5-NTCP | [14] |
| Interferon-α | HCV, HEV, HDV | Novel in vitro multi-infection | 80% reduction in intracellular viral RNAs | dHuH7.5-NTCP | [14] |
| DVICE (AI Model) | SARS-CoV-2, IAV, AdV, etc. | AI-based CPE detection | AUROC = 0.991 ± 0.001 vs. human annotation | Multiple cell lines | [10] [11] |
Experimental Protocols
Automated Plaque Assay Protocol
The automated plaque assay enhances the traditional method by incorporating imaging and analysis to reduce subjectivity. The following workflow visualizes the key stages.
Diagram 1: Automated Plaque Assay Workflow. PFU: Plaque-forming Unit.
Key Steps:
- Cell Seeding: Seed permissive cells (e.g., Vero CCL-81, BHK CCL-10) to form confluent monolayers in multi-well plates (6- to 96-well format) [12] [8].
- Virus Inoculation: Inoculate with 10-fold serial dilutions of virus stock. Adsorb for 1 hour at 37°C with gentle rocking [8].
- Overlay: Replace medium with a semi-solid overlay (e.g., 0.2-0.8% agarose or carboxymethyl cellulose) to restrict viral diffusion and ensure discrete plaque formation [8].
- Incubation: Incubate for 3-7 days (duration is virus-dependent) at 37°C with 5% CO₂ [8].
- Staining and Imaging: Remove overlay, fix cells with ice-cold methanol/acetone (1:1), and stain with 0.1% crystal violet. Alternatively, for focus-forming assays, immunostain with virus-specific antibodies (e.g., 4G2 for orthoflaviviruses) [8]. Image entire wells using an automated imager like the Agilent BioTek Cytation [12].
- Analysis: Use integrated software (e.g., Gen5) to automatically count plaques or foci based on size and contrast, then calculate the titer in PFU/mL or FFU/mL [12] [8].
AI-Powered CPE Detection (DVICE) Protocol
The Detection of Virus-Induced Cytopathic Effect (DVICE) pipeline uses machine learning to automate infection scoring from label-free images.
Diagram 2: AI-Powered CPE Detection Workflow. CPE: Cytopathic Effect, CNN: Convolutional Neural Network.
Key Steps:
- Sample Preparation: Seed ~10,000 permissive cells per well in a 96-well plate. Infect with virus serial dilutions and incubate for up to 7 days to allow CPE manifestation [10] [11].
- Image Acquisition: Acquire transmitted-light microscopy images using a high-throughput microscope (e.g., ImageXpress Micro Confocal) with a 4x objective. One central site per well is typically imaged [10].
- Ground Truth Generation: Fix cells with 4% paraformaldehyde and stain with 0.25% crystal violet. Have multiple human experts independently annotate the infection status of each well to create a ground truth dataset [11].
- Model Training: Train a convolutional neural network (CNN) based on the EfficientNet-B0 architecture using the transmitted-light images and their corresponding labels. The dataset used in the original study comprised 58,619 images (22,873 infected, 35,746 uninfected) across multiple viruses and cell lines [10] [11].
- Validation and Deployment: Validate the model using leave-one-out cross-validation. The published DVICE model achieved an AUROC of 0.991 ± 0.001. Apply the trained model to classify new images and calculate infectivity scores or TCID₅₀ values [11].
Real-Time Cell Analysis (RTCA) Protocol
The xCELLigence RTCA system continuously monitors cell status via electrical impedance, providing real-time, label-free data on CPE development.
Key Steps:
- Cell Seeding and Baseline Monitoring: Seed cells onto specialized E-Plates. Monitor cell index (a measure of impedance) for 12-24 hours to establish a baseline and confirm cell health and appropriate seeding density [12].
- Virus Inoculation and Continuous Monitoring: Inoculate cells with virus. Continue to monitor cell index impedance in real-time. Virus-induced CPE causes cells to detach, resulting in a quantifiable decrease in cell index [12].
- Data Analysis: Analyze the kinetic data to determine the time-point of CPE initiation, the rate of CPE progression, and the final degree of destruction. This data can be used to calculate viral titer or evaluate antiviral compound efficacy [12].
The Scientist's Toolkit
Successful implementation of viral infectivity assays requires specific reagents and instrumentation. The following table details key solutions for setting up these experiments.
Table 3: Essential Research Reagent Solutions for Viral Infectivity Assays
| Item | Function / Application | Examples / Specifications |
|---|---|---|
| Permissive Cell Lines | Support viral replication and CPE development. Critical for assay sensitivity. | Vero CCL-81, Vero E6, BHK CCL-10, MDCK, A549, Huh7 [10] [9] [8] |
| Semi-Solid Overlays | Restrict virus spread to enable plaque formation in plaque assays. | 0.2-0.8% Agarose, Carboxymethyl Cellulose (CMC) [8] |
| Detection Antibodies | Enable immunodetection of viral antigens in FFU assays. | Pan-orthoflavivirus 4G2 monoclonal antibody [8] |
| Vital Stains | Visualize cell viability and plaque formation in endpoint assays. | Crystal Violet (0.1-0.25%), Neutral Red [10] [9] [8] |
| Fixatives | Preserve cell morphology and inactivate virus for safe staining. | Methanol/Acetone (1:1), 4% Paraformaldehyde (PFA) [10] [8] |
| Automated Imaging Systems | Acquire high-throughput, high-content image data for analysis. | Agilent BioTek Cytation series, ImageXpress Micro Confocal (IXM-C) [10] [12] |
| Real-Time Cell Analyzers | Generate label-free, kinetic data on cell health and CPE. | Agilent xCELLigence RTCA systems [12] |
| AI/Image Analysis Software | Automate plaque counting and infection classification. | ViQi AVIA, Gen5 Software, DVICE (EfficientNet-B0 CNN) [10] [11] [12] |
The landscape of viral infectivity testing is evolving from traditional, low-throughput methods toward automated, kinetic, and information-rich platforms. The choice of assay must align with the research question, considering whether the target is early replication events or late-stage cytopathic effects. While plaque and TCID₅₀ assays remain gold standards for direct quantification, AI-powered imaging and real-time impedance technologies offer compelling advantages in throughput, objectivity, and kinetic resolution. The integration of these advanced platforms, supported by robust experimental protocols and reagents, is accelerating the pace of virology research and antiviral discovery.
The accurate quantification of infectious virus particles is a cornerstone of virology, critical for diagnostics, vaccine development, antiviral evaluation, and understanding viral pathogenesis [15]. Among the various techniques available, two cell-based methods stand as fundamental tools for determining the concentration of replication-competent virions: the plaque assay and the 50% tissue culture infectious dose (TCID50) assay. The plaque assay is widely regarded as the gold standard for directly quantifying lytic virions, providing a direct count of infectious units [15] [16]. In contrast, the TCID50 assay employs an endpoint dilution approach to determine the dilution at which 50% of inoculated cell cultures become infected, providing an indirect estimate of infectious titer through statistical calculation [16] [17]. These techniques differ not only in their methodology but also in their underlying mathematical principles, applications, and the interpretation of their results. Understanding the key principles, comparative performance, and appropriate contexts for employing each method is essential for researchers and drug development professionals working in virology and related fields. This guide provides a comprehensive comparison of these fundamental quantification methods, supported by experimental data and detailed protocols to inform their application in contemporary viral research.
Theoretical Foundations and Mathematical Principles
Plaque Assay: Direct Quantification of Infectious Units
The plaque assay operates on the principle that each plaque observed in a cell monolayer represents the infectious activity of a single virion [16]. This one-to-one correspondence makes it a direct measure of infectious virus particles. Technically, the method involves preparing serial dilutions of a virus sample, inoculating susceptible cell monolayers, and then overlaying the cells with a semi-solid medium (such as agarose or carboxymethyl cellulose) that restricts viral spread to neighboring cells, thereby creating discrete zones of infection known as plaques [15] [16]. After an appropriate incubation period, plaques are counted manually or through automated imaging systems. The calculation of the viral titer follows this formula:
IU/ml = Number of plaques / (dilution factor × inoculated volume in ml) [16]
For example, if 32 plaques are counted at the 10⁻³ dilution from an inoculated volume of 0.5 ml, the titer would be calculated as: 32 / (10⁻³ × 0.5) = 6.4 × 10⁵ IU/ml [16]. This direct counting method provides a precise measurement of plaque-forming units (PFU) per milliliter, with the term "infectious units" (IU) often used interchangeably with PFU.
TCID50 Assay: Endpoint Dilution and Statistical Estimation
The TCID50 assay employs a fundamentally different approach based on binary response (presence or absence of infection) across multiple replicate wells at different dilutions to statistically determine the dilution at which 50% of the cultures become infected [16] [17]. Unlike the plaque assay, it does not involve a semi-solid overlay, allowing unconstrained viral spread in liquid medium, with infection typically assessed through visual observation of cytopathic effect (CPE) [15] [17]. The core probabilistic assumption is that at the dilution where only 50% of wells show infection, there is, on average, one infectious particle per well, as this scenario presents a 50% probability of infection occurring [16]. The mathematical foundation relies on the Poisson distribution, which models the probability of a cell culture being infected when a random number of virus particles are distributed across multiple cultures [18].
Two primary statistical methods are used to calculate the TCID50 titer:
Reed-Muench Method: This cumulative approach involves scoring positive and negative wells across dilutions, calculating cumulative sums, determining infection rates, identifying the 50% endpoint, and calculating a proportionate distance to interpolate the exact endpoint [16]. The formula is: Log(TCID50) = log(dilution above 50%) + (-proportionate distance) × log(dilution factor) [16]
Spearman-Kärber Method: This simpler method requires only the total number of positive wells across all dilutions and uses the formula: Log(TCID50) = log(lowest dilution with 100% CPE) + I × [0.5 - (total CPE wells/total replicates)] where I is the log of the dilution factor [16].
Table 1: Comparison of Calculation Methods for TCID50 Assay
| Feature | Reed-Muench Method | Spearman-Kärber Method |
|---|---|---|
| Complexity | More complex, multiple steps | Simpler, fewer calculation steps |
| Data Visualization | Provides clearer infection dynamics across dilutions | Relies on total infected wells |
| Assumption | Fewer assumptions about distribution pattern | Assumes progressive decrease in infected wells with dilution |
| Regulatory Preference | Sometimes preferred for detailed analysis | Often acceptable, depending on specific guidelines |
Mathematical Relationship and Unit Conversion
A critical relationship exists between TCID50 and PFU measurements, derived from Poisson distribution principles. At the 50% infection point (TCID50), the probability of no infection P(0) = 0.5 [18]. According to Poisson distribution:
P(0) = e^(-IU) where IU represents infectious units [18]
Substituting P(0) = 0.5 gives: 0.5 = e^(-IU) Solving for IU: IU = -ln(0.5) ≈ 0.693 [18]
This establishes the fundamental conversion factor: 1 TCID50 ≈ 0.7 PFU or 1 PFU ≈ 1.44 TCID50 [18]
Therefore, to convert a TCID50/ml titer to PFU/ml, multiply by 0.7: PFU/ml = TCID50/ml × 0.7 [18]
This mathematical relationship allows researchers to compare results across studies using different quantification methods and is essential for meta-analyses and standardized reporting in virology.
Comparative Experimental Data and Performance Metrics
Direct Comparative Studies of PFU and TCID50 Assays
Experimental comparisons between PFU and TCID50 assays reveal important differences in their performance characteristics and outputs. A 2022 study systematically compared these methods across several SARS-CoV-2 variants, including the D614G strain (B.1), three Variants of Concern (Alpha, Gamma, Delta), and one Variant of Interest (Mu) [15]. The plaque assay reported viral titers between 0.15 ± 0.01×10⁷ and 1.95 ± 0.09×10⁷ PFU/mL, while the TCID50 assay yielded titers between 0.71 ± 0.01×10⁶ to 4.94 ± 0.80×10⁶ TCID50/mL for the same isolates [15]. The calculated PFU/mL from TCID50 assays differed significantly from directly measured PFU/mL for most variants, with log10 differences of 0.61 for Alpha, 0.59 for Gamma, 0.59 for Delta, and 0.96 for Mu variants (p≤0.0007), though no significant difference was observed for the D614G strain [15]. This variant-dependent discrepancy highlights that the relationship between these assays can be influenced by viral characteristics, possibly due to differences in cell entry mechanisms, replication kinetics, or cell-to-cell spread efficiency among variants.
A separate comparison focusing on filoviruses found that the TCID50 assay appeared to be more sensitive but slightly more variable than plaque assays, with approximately a tenfold difference in the numerical results between the methods [19]. This study also noted that both methods remain useful and practicable in filovirus research, with the comparison providing valuable guidance for standardizing approaches across laboratories [19]. The observed variability in TCID50 assays may stem from its reliance on categorical scoring of CPE rather than direct counting of discrete events, introducing more subjectivity into the measurement process.
Table 2: Experimental Comparison of PFU and TCID50 Titers Across SARS-CoV-2 Variants [15]
| SARS-CoV-2 Variant | Plaque Assay (PFU/mL) | TCID50 Assay (TCID50/mL) | Log10 Difference |
|---|---|---|---|
| D614G (B.1) | Not specified | Not specified | Not significant |
| Alpha (B.1.1.7) | Within study range | Within study range | 0.61 |
| Gamma (P.1) | Within study range | Within study range | 0.59 |
| Delta (B.1.617.2) | Within study range | Within study range | 0.59 |
| Mu (B.1.621) | Within study range | Within study range | 0.96 |
Accuracy, Variability, and Method-Specific Considerations
The precision and reliability of PFU and TCID50 assays have been quantitatively assessed through various studies. Relative errors associated with plaque assays have been estimated at 10–100%, while TCID50 assays have approximately 35% error [17]. This difference in error rates reflects their distinct methodological approaches: the plaque assay's error primarily stems from counting statistics and plaque identification subjectivity, while the TCID50 assay's error derives from the binary scoring system and statistical estimation process.
A study on human herpesvirus 6 (HHV-6) quantification found that a quantitative PCR (qPCR)-based readout of TCID50 demonstrated substantially lower intra-assay variability (9% coefficient of variation) compared to ocular inspection readout of TCID50 (45% CV) [20]. This suggests that alternative detection methods can significantly improve the reliability of TCID50 assays while maintaining comparable absolute values—1 Q-PCR TCID50 equaled 1.41 ocular TCID50 and 1.03 IFA TCID50 values with no statistical significance [20]. This highlights how the choice of detection method (CPE, IFA, or qPCR) can substantially impact the precision of TCID50 assays without fundamentally altering the calculated titer.
Detailed Experimental Protocols
Standard Plaque Assay Protocol
The plaque assay protocol involves multiple critical steps to ensure accurate quantification:
Cell Culture Preparation: Seed susceptible cell monolayers (e.g., Vero E6 cells for SARS-CoV-2) in appropriate culture vessels and incubate until they reach 80-100% confluency [15] [17]. The specific cell line must be permissive to the virus being quantified.
Viral Dilution Preparation: Prepare serial 10-fold dilutions of the virus sample in suitable maintenance medium or buffer, typically covering a range from 10⁻¹ to 10⁻⁸ depending on the expected titer [16].
Inoculation: Remove growth medium from cell monolayers and inoculate with predetermined volumes of each viral dilution, typically in duplicate or triplicate. Include control wells without virus [17].
Adsorption: Allow virus adsorption to cells for a specified period (usually 1-2 hours) at 37°C with occasional gentle rocking to ensure even distribution [17].
Overlay Application: Remove inoculum and carefully add semi-solid overlay medium (e.g., carboxymethyl cellulose or agarose) to restrict viral spread to adjacent cells, enabling plaque formation [15] [16].
Incubation: Incubate cells for an appropriate duration (varies by virus, typically 2-7 days) until visible plaques develop [17].
Plaque Visualization: Remove overlay, fix cells, and stain with crystal violet, neutral red, or immunostaining to visualize and count plaques [15] [16].
Calculation: Count plaques in wells with 10-100 discrete plaques and calculate titer using the formula: IU/ml = (number of plaques) / (dilution factor × volume of inoculum in ml) [16].
Standard TCID50 Assay Protocol
The TCID50 assay protocol follows these essential steps:
Cell Seeding: Seed host cells in 48- or 96-well plates at optimal density (e.g., 7×10⁴ cells/ml for 48-well plates) and incubate until 80-90% confluent [17].
Viral Dilution Series: Prepare serial 1:10 dilutions of virus sample in appropriate medium, typically from 10⁻¹ to 10⁻⁸ or higher [16] [17].
Inoculation: Infect multiple replicate wells per dilution (typically 4-8 replicates) with a fixed volume of each dilution [16] [17]. Include control wells with medium only.
Incubation and Observation: Incubate plates for virus-specific duration (may require 5-20 days for slow-growing viruses) and regularly monitor for cytopathic effect (CPE) [17].
Scoring: Score each well as positive or negative based on CPE presence at predetermined time points [16] [17].
Calculation: Apply Reed-Muench or Spearman-Kärber method to calculate TCID50/ml [16]. For Reed-Muench:
- Calculate cumulative positive and negative wells
- Determine infection rates
- Identify dilutions bracketing 50% infection
- Calculate proportionate distance
- Apply formula: Log(TCID50) = log(dilution above 50%) + (-PD) × log(dilution factor) [16]
Volume Adjustment: Adjust for inoculum volume: TCID50/ml = calculated TCID50 × (1/inoculum volume in ml) [16].
Diagram 1: TCID50 Assay Workflow - This diagram illustrates the sequential steps in a standard TCID50 assay protocol, from cell preparation to final titer determination.
Applications and Method Selection Criteria
Context-Specific Method Applications
The choice between PFU and TCID50 assays depends heavily on the specific research context and viral characteristics:
Plaque Assays are particularly valuable for:
- Vaccine development and evaluation where precise quantification of infectious virus is critical [15]
- Antiviral drug testing that requires accurate measurement of infectious titer reduction [15]
- Purification of viral clones through plaque isolation
- Studies of viral pathogenesis and replication kinetics [15]
- Viruses that form clear, distinct plaques in available cell lines
TCID50 Assays are preferred for:
- Viruses that do not form distinct plaques but still produce observable CPE [17]
- High-throughput applications where 96-well formats offer efficiency advantages
- Situations with limited virus sample availability [17]
- Viruses with long replication cycles where daily monitoring is practical
- Diagnostic virology applications including HIV-1, influenza, and human herpesviruses [17]
Integrated Approach with Molecular Methods
Complementing these traditional infectivity assays, molecular methods like quantitative RT-PCR (qRT-PCR) provide additional layers of information but measure different aspects of viral presence. A key distinction is that qRT-PCR quantifies viral RNA copies rather than infectious particles, which can lead to significant discrepancies as not all viral genomes are packaged into infectious virions [15]. Research on SARS-CoV-2 variants demonstrated varying ratios between PFU and RNA copies across variants: 1:29,800 for D614G, 1:11,700 for Alpha, 1:8,930 for Gamma, 1:12,500 for Delta, and 1:2,950 for Mu [15]. This indicates that the proportion of infectious virions changes depending on the viral variant, with Mu variant reaching higher infectious titers with fewer viral copies [15]. This highlights the importance of selecting quantification methods aligned with the specific research question—whether assessing total viral material (qPCR) or replication-competent virus (PFU/TCID50).
Diagram 2: Method Selection Guide - This decision tree illustrates key considerations when choosing between PFU and TCID50 assays for viral quantification, including common application scenarios for each method.
Essential Research Reagents and Materials
Table 3: Essential Reagents for Viral Quantification Assays
| Reagent/Material | Function | Specific Examples |
|---|---|---|
| Permissive Cell Lines | Provide susceptible host cells for viral replication | Vero E6 cells (SARS-CoV-2) [15], HSB-2 cells (HHV-6) [20] |
| Semi-Solid Overlay Media | Restrict viral spread for plaque formation | Carboxymethyl cellulose, agarose [16] |
| Cell Culture Media | Support cell viability and viral replication | DMEM, RPMI-1640 with serum supplements [15] [20] |
| Staining Reagents | Visualize plaques or infected cells | Crystal violet, neutral red, immunostaining antibodies [16] [20] |
| Fixation Solutions | Preserve cell monolayers for staining | Methanol, acetone-methanol mixtures [20] |
| Dilution Buffers | Prepare serial dilutions of virus samples | Phosphate-buffered saline (PBS), maintenance medium [17] |
| Detection Antibodies | Identify infected cells (IFA readout) | Primary antibodies against viral proteins, fluorescent secondary antibodies [20] |
| qPCR Reagents | Quantify viral genomes (alternative readout) | DNA extraction kits, primers, probes, polymerases [20] |
The plaque assay and TCID50 method represent two fundamental, complementary approaches for quantifying infectious virus, each with distinct advantages, limitations, and appropriate applications. The plaque assay provides direct quantification of infectious units with higher precision and is considered the gold standard for viruses that form clear plaques, making it ideal for vaccine development, antiviral testing, and fundamental virology research. The TCID50 assay offers a statistical estimate of infectious titer through endpoint dilution, providing greater applicability to viruses that don't form plaques and advantages in throughput efficiency. The mathematical relationship between these units (1 TCID50 ≈ 0.7 PFU) enables cross-method comparisons and data integration [18]. Contemporary research increasingly combines these methods with molecular approaches like qPCR to differentiate between infectious and total viral particles, providing a more comprehensive understanding of viral dynamics [15] [20]. Method selection should be guided by viral characteristics, research objectives, and practical constraints, with many laboratories employing both approaches to leverage their complementary strengths in advancing virological research and therapeutic development.
In virology research and vaccine development, the accurate assessment of viral infectivity is foundational. Cell-based infectivity assays, such as plaque assays and the tissue culture infectious dose 50 (TCID₅₀) assay, serve as critical tools for quantifying infectious virus particles, evaluating antiviral therapies, and ensuring vaccine safety and potency [21] [22]. The selection of an appropriate cell line is arguably the most critical variable in these assays, as it directly influences assay sensitivity, specificity, and the kinetics of detectable viral replication. Permissive cell lines support robust viral entry and replication, leading to measurable endpoints like cytopathic effect (CPE), which can be visualized and quantified. The impact of this choice is evident across diverse virus families, from coronaviruses and adenoviruses to more complex viruses like human cytomegalovirus (HCMV) [23] [24] [25]. This guide provides a comparative analysis of cell line performance, supported by experimental data, to inform robust assay design.
Comparative Performance of Cell Lines
The sensitivity of a viral infectivity assay is intrinsically linked to the host cell's susceptibility to infection. Different cell lines express varying levels of viral receptors and host factors necessary for replication, leading to significant differences in assay outcomes. The following sections and tables summarize key experimental findings.
Case Study: SARS-CoV-2 and Adenovirus
Research on SARS-CoV-2 and human adenoviruses highlights how cell line selection can dramatically alter the detection of infectious virus.
Table 1: Comparative Sensitivity of Cell Lines to Different Viruses
| Virus | Cell Lines Compared | Key Findings on Sensitivity | Experimental Context | Source |
|---|---|---|---|---|
| SARS-CoV-2 | Vero E6 vs. Vero E6-TMPRSS2 | Vero E6-TMPRSS2 extended analytical sensitivity by >3 CT values and resulted in faster viral isolation compared to parental Vero E6 cells. | Viral culture from clinical samples | [25] |
| Human Adenoviruses | 293A, A549, others | 293A and A549 were the most sensitive to enteric adenovirus serotypes 40 and 41. 293A detected viral plaques in 7 of 13 primary sewage samples. | Plaque assay in water samples | [23] |
| West Nile Virus (WNV) | Vero, Vero-E6, PER.C6 | Both Vero and Vero-E6 yielded higher viral titers than PER.C6 cells. | Endpoint titration for vaccine safety testing | [21] |
| Human Cytomegalovirus (HCMV) | ARPE-19 (epithelial) | The ARPE-19 epithelial cell line was selected for a potency assay due to the virus's specific reliance on a pentameric glycoprotein complex for epithelial cell entry. | High-throughput relative potency assay (IRVE) | [24] |
For SARS-CoV-2, the presence of the TMPRSS2 protease in modified Vero E6 cells is a critical differentiator, enhancing viral entry and thereby increasing the assay's ability to detect low levels of infectious virus that would be missed in standard Vero E6 cells [25]. Similarly, for adenoviruses, the 293A cell line demonstrated superior performance in environmental monitoring, successfully isolating viruses from complex primary sewage samples where other cell lines might fail [23].
Impact on Infectivity Quantification
The choice of cell line not only affects the binary detection of virus but also the quantitative results of an infectivity assay.
Table 2: Impact of Cell Line on Quantitative Assay Metrics
| Virus | Assay Type | Quantitative Impact | Citation |
|---|---|---|---|
| Various (AdV, HSV, IAV, RV, VACV, SARS-CoV-2) | AI-based CPE detection (DVICE) | The AI model's accuracy (AUROC 0.991) was dependent on training with virus-specific CPE manifestations in specific cell lines (A549, HeLa, Huh7, VeroE6). | [11] |
| SARS-CoV-2 | RT-PCR-based infectivity prediction | A cycle threshold (Ct) cutoff of ≤31 for genomic RNA correlated with positive viral culture in Vero E6-TMPRSS2 cells, defining a rule-out threshold for infectivity. | [25] |
| HCMV | Imaging of Relative Viral Expression (IRVE) | Assay robustness was achieved by optimizing and fixing key cell-related parameters: cell density, serum concentration, and cell passage number. | [24] |
The data show that cell line permissiveness directly influences key quantitative metrics like viral titer and the effective dose (ED₅₀). Furthermore, the manifestation of CPE—a common endpoint in these assays—is highly specific to the virus-cell line pairing, which is a crucial consideration for both manual and automated readouts [11].
Advanced and Automated Methodologies
Traditional infectivity assays are often low-throughput and subjective. Recent advancements leverage automation, label-free imaging, and artificial intelligence (AI) to overcome these limitations, but these technologies still rely fundamentally on well-selected cell lines.
- Real-Time Cell Analysis (RTCA): Systems like the xCELLigence platform use cellular impedance to monitor CPE in real-time without labels. The optimal timepoint for infection and the resulting kinetics are dependent on the cell seeding density and the specific cell line used [22].
- AI-Powered Image Analysis: The DVICE (Detection of Virus-Induced CPE) framework uses convolutional neural networks (CNNs) to identify CPE from transmitted light microscopy images. This method requires training on specific cell lines (e.g., A549 for Adenovirus, Vero E6 for SARS-CoV-2) to learn the unique CPE "fingerprint" for each virus-cell combination [11]. Similarly, the AVIA (Automated Viral Infectivity Assay) platform uses AI on brightfield images to detect early, subtle phenotypic changes in infected cells, a process that is also cell line-dependent [26] [22].
- High-Throughput Fluorescence Imaging: Assays like the Imaging of Relative Viral Expression (IRVE) for HCMV automate the process of counting infected cells via immunostaining (e.g., for the Immediate Early 1 protein) in 384-well plates. This method's success hinges on using a susceptible cell line like ARPE-19 to ensure a strong and specific signal [24].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions as derived from the experimental protocols cited in this guide.
Table 3: Essential Research Reagents for Viral Infectivity Assays
| Reagent / Material | Function in Assay | Example from Literature |
|---|---|---|
| Vero E6 Cells | Standard cell line for isolation of SARS-CoV-2 and other viruses; susceptible to infection. | Used in SARS-CoV-2 culture as the gold standard for viability [27] [25]. |
| Vero E6-TMPRSS2 Cells | Engineered cell line expressing the TMPRSS2 protease; enhances entry of SARS-CoV-2 and increases assay sensitivity. | Critical for isolating SARS-CoV-2 from clinical samples with higher CT values [25]. |
| ARPE-19 Cells | Human retinal pigment epithelial cell line; permissive for HCMV infection due to expression of specific viral entry receptors. | Host cell in the automated IRVE potency assay for HCMV vaccine development [24]. |
| 293A Cells | Human embryonic kidney cell line; highly sensitive to certain adenoviruses, making it suitable for environmental monitoring. | Used for plaque assay detection of adenoviruses in water samples [23]. |
| Subgenomic RNA (sgRNA) Probes | PCR-based detection of viral sgRNA, a marker of active viral replication, used as a surrogate for infectivity. | sgE RNA detection showed high accuracy (98%) in identifying viable SARS-CoV-2 [27]. |
| Crystal Violet (CV) | A histochemical stain used to visualize and count viral plaques by fixing and staining the remaining cell monolayer. | Used as a ground truth staining method for training AI models in the DVICE framework [11]. |
| Anti-IE1 Antibodies | Antibodies targeting the HCMV Immediate Early 1 protein; used in immunostaining to identify infected cells in potency assays. | Key reagent in the IRVE assay for high-throughput counting of HCMV-infected cells [24]. |
Experimental Workflow and Logical Relationships
The diagram below illustrates the core decision-making workflow and the logical relationships between cell line selection, assay execution, and output interpretation in viral infectivity testing.
Detailed Experimental Protocols
To ensure reproducibility, here are detailed methodologies for two key assays cited in this guide.
The Imaging of Relative Viral Expression (IRVE) assay is an automated, high-throughput method for determining the relative potency of a live-attenuated HCMV vaccine.
- Cell Preparation: Seed ARPE-19 cells into 384-well plates using an automated cell culture system. Key parameters like cell density and cell passage number must be optimized and controlled for robustness.
- Infection: Inoculate the cell monolayer with serial dilutions of the HCMV vaccine sample. Include a reference standard on every plate for relative potency calculation.
- Incubation: Incubate the plates for a defined period (e.g., 24-48 hours) to allow for viral entry and early gene expression.
- Immunostaining: Fix the cells and perform immunofluorescence staining using an antibody against the HCMV Immediate Early 1 (IE1) protein. Use a nuclear counterstain to identify all cells.
- Automated Imaging and Analysis: Image the entire plate using a high-throughput microscope. Software is used to count the total number of nuclei and the number of IE1-positive nuclei. The percentage of infected cells is calculated for each dilution.
- Relative Potency Calculation: The half maximal effective dilution (ED₅₀) for both the test sample and the reference standard is determined. Relative potency is reported as the ratio of the reference ED₅₀ to the test sample ED₅₀.
This protocol uses label-free light microscopy and AI to quantify infectivity for a broad panel of viruses.
- Cell Seeding and Infection: Seed permissive cell lines (e.g., A549, Vero E6) in 96-well plates. Inoculate with serial dilutions of virus (e.g., Adenovirus, SARS-CoV-2). Include uninfected control wells.
- Image Acquisition: Incubate plates for up to 7 days. Acquire transmitted light (TL) images daily using a high-throughput microscope (e.g., ImageXpress Micro Confocal).
- Ground Truth Annotation: After imaging, fix the cells and stain with Crystal Violet (CV). Use human expert annotation of the CV-stained plates to define the infection state (positive/negative) for each well. This serves as the "ground truth" for training the AI model.
- AI Model Training: Train a convolutional neural network (CNN), such as EfficientNet-B0, using the TL images as input and the human annotations as labels. The model learns to recognize features associated with CPE.
- Infection Scoring and Titration: Use the trained model to classify the infection state of new TL images. Apply the specific infection (SIN) method to the classification results to calculate TCID₅₀ values, achieving a correlation with human annotation of R² = 0.986.
The selection of a cell line is a foundational decision that governs the sensitivity, accuracy, and applicability of viral infectivity assays. As demonstrated, a one-size-fits-all approach is ineffective; optimal cell lines must be matched to the specific virus based on its entry receptors and replication machinery. The emergence of advanced methodologies like real-time impedance sensing and AI-driven image analysis does not diminish the importance of cell line selection but rather reinforces it, as these technologies are trained on and optimized for specific virus-host systems. For researchers, a rigorous initial evaluation of cell line suitability, informed by comparative data, is essential for developing robust, reproducible, and predictive viral infectivity assays.
Core Conceptual Framework
Virucidal activity and neutralizing activity represent two distinct, critical mechanisms for preventing viral infections in biomedical research and therapeutic development. Virucidal activity refers to the chemical or physical destruction of viral particles in the environment, preventing infection by reducing the concentration of infectious virus on surfaces or in the air. In contrast, neutralizing activity describes the biological mechanism by which antibodies or other substances bind to viruses and block their ability to enter and infect host cells, representing a key immune protection mechanism [28].
The fundamental distinction lies in their mechanisms and applications: virucidal agents act directly on viral structural components through chemical or physical means, while neutralizing agents (particularly antibodies) function through specific molecular interactions that interfere with the viral replication cycle without necessarily destroying the viral particle. Understanding both concepts is essential for developing comprehensive strategies against viral pathogens, from surface disinfection protocols to vaccine efficacy assessment and therapeutic antibody development [28] [29].
Virucidal Activity: Mechanisms and Assessment
Chemical Virucidal Agents and Efficacy
Virucidal disinfectants demonstrate varying efficacy depending on their chemical composition, concentration, and contact time with pathogens. The susceptibility of viruses to these agents is heavily influenced by viral structure, with enveloped viruses generally being more susceptible than non-enveloped viruses due to the vulnerability of their lipid envelopes to disinfectants [29].
Table 1: Virucidal Efficacy of Chemical Disinfectants Against Enveloped Viruses
| Disinfectant Type | Specific Agent | Virus Tested | Effective Concentration | Minimum Contact Time | Log Reduction |
|---|---|---|---|---|---|
| Quaternary Ammonium Compound | Micro-Chem Plus | Nipah Virus | 1:9 dilution | 15 seconds | >4 log₁₀ [30] |
| Quaternary Ammonium Compound | FWD | Nipah Virus | 1:27 dilution | 15 seconds | >4 log₁₀ [30] |
| Alcohol | Medical EtOH | Nipah Virus | 38% ethanol | 15 seconds | >4 log₁₀ [30] |
| Alcohol | Medical EtOH | Nipah Virus | 19% ethanol | 8 minutes | >4 log₁₀ [30] |
| Acidic Alcohol-Based | Proprietary Formulation | Human Norovirus (GII.17) | Product formulation | 30-60 seconds | Complete inactivation [31] |
| Alkaline Alcohol-Based | Proprietary Formulation | Human Norovirus (GII.17) | Product formulation | 60 seconds | No inactivation [31] |
The efficacy of virucidal agents is significantly influenced by their environment. Viruses suspended in solution are typically more easily inactivated than those dried on surfaces, where organic material like blood and saliva may provide protection. Furthermore, as demonstrated in the norovirus study, the pH formulation of alcohol-based disinfectants can dramatically impact their efficacy, with acidic formulations showing superior virucidal activity against nonenveloped viruses compared to alkaline formulations [29] [31].
Standardized Testing Methodologies
The European Committee for Standardization (CEN) has established a rigorous, phased framework for evaluating virucidal activity of chemical disinfectants:
Phase 1 (Suspension Tests): Preliminary tests to determine basic bactericidal, fungicidal, or virucidal activity without regard for specific application areas. These tests cannot be used for product claims [29].
Phase 2/Step 1 (Quantitative Suspension Tests): Quantitative methods where test organisms are exposed to disinfectants at various concentrations, contact times, and temperatures with interfering substances. The standard EN 14476 specifies a requirement of ≥4-log₁₀ reduction (99.99% loss of infectivity) for virucidal claims [29].
Phase 2/Step 2 (Carrier Tests): Methods simulating practical use conditions where microorganisms are applied to carrier surfaces (e.g., stainless steel, glass, PVC) and dried. These tests more accurately reflect real-world conditions, with standards including EN 16777:2018 for surface disinfection and EN 17111:2018 for instrument disinfection [29].
Figure 1: Standardized Virucidal Activity Testing Workflow. The European Committee for Standardization (CEN) three-phase testing methodology progresses from basic screening to simulated practical use conditions [29].
Neutralizing Activity: Mechanisms and Assessment
Antibody-Mediated Neutralization Mechanisms
Neutralizing antibodies (nAbs) represent a crucial component of the adaptive immune response, providing protection against viral infections through multiple mechanisms. The classical definition of neutralization describes it as "the loss of infectivity which ensues when antibody molecule(s) bind to a virus particle, and usually occurs without the involvement of any other agency" [28].
The mechanisms by which antibodies neutralize viruses are diverse and include:
Receptor Binding Interference: nAbs can bind to viral receptor-binding sites or their immediate vicinity, physically blocking attachment to host cell receptors through steric hindrance [28].
Post-Attachment Inhibition: Some nAbs permit initial attachment but prevent subsequent entry steps, such as viral fusion with host cell membranes or uncoating [28].
Conformational Alteration: High-affinity antibody binding can induce disassembly or conformational changes in viral surface proteins, rendering them non-functional for entry [28].
Virion Aggregation: Antibodies with multiple binding sites can cross-link viral particles, forming aggregates that reduce the effective infectious units [28].
It is important to distinguish between in vitro neutralization and in vivo protection. While in vitro assays typically measure direct blocking of viral entry, nAbs can mediate additional antiviral functions in vivo through Fc receptor-dependent mechanisms such as antibody-dependent cellular cytotoxicity (ADCC) and phagocytosis [28].
Neutralization Assay Methodologies
Multiple assay formats have been developed to quantify neutralizing activity, each with distinct advantages and limitations:
Table 2: Comparison of Virus Neutralization Assay Methodologies
| Assay Type | Principle | Biosafety Level | Key Applications | Advantages | Limitations |
|---|---|---|---|---|---|
| Conventional Virus Neutralization Test (cVNT) | Inhibition of authentic virus infection of permissive cells | BSL-3 for live SARS-CoV-2 [32] | Gold standard validation; pathogencity studies [33] | Measures authentic virus neutralization; considers all viral proteins | Requires high containment; longer turnaround time |
| Pseudovirus Neutralization Test (pVNT) | Neutralization of replication-incompetent viral particles pseudotyped with viral glycoproteins | BSL-2 [32] | High-throughput screening; vaccine efficacy studies [32] | Safer; enables study of high-pathogenicity viruses; scalable | Limited to single-cycle infection; may not fully recapitulate authentic virus neutralization |
| Surrogate Virus Neutralization Test (sVNT) | Competitive ELISA measuring antibody blockage of protein-protein interactions | BSL-1 [33] | Population serosurveillance; rapid clinical testing | Rapid; does not require live cells or viruses; high throughput | Measures only binding interference, not functional neutralization in cellular context |
| Inhibition Flow Cytometry VNT (IFVNT) | Flow cytometric detection of infected cells using fluorescent antibodies | BSL-2/3 depending on virus [33] | Detailed cellular infection analysis; monoclonal antibody characterization | Provides single-cell resolution; can quantify infection percentage directly | More complex instrumentation; potentially lower throughput |
Figure 2: Neutralization Assay Selection Framework. Assay choice depends on research objectives, balancing biosafety requirements with biological fidelity needs [33] [32].
The correlation between different neutralization assays has been extensively evaluated. Studies comparing pseudovirus-based neutralization assays (PVNA) with the gold standard micro-neutralization test (MNT) have demonstrated strong correlations, validating PVNA as a reliable tool for assessing anti-SARS-CoV-2 nAbs while offering the practical advantage of BSL-2 containment [32].
Essential Research Reagents and Materials
Successful investigation of virucidal and neutralizing activities requires specific research reagents and biological materials tailored to each methodology:
Table 3: Essential Research Reagents for Viral Inactivation Studies
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Lines | Vero E6, Vero, RAW 264.7, CRFK, Huh7, Caco2, Calu3, HEK293T [30] [33] [31] | Virus propagation; neutralization assays; infectivity quantification | Provide cellular substrate for viral replication and infection detection |
| Reference Viruses | Murine norovirus (MNoV), Feline calicivirus (FCV), Vaccinia virus, Poliovirus, Adenovirus [29] [31] | Surrogate models; virucidal efficacy testing; assay standardization | Serve as representative models for pathogenic viruses requiring high containment |
| Detection Systems | Luciferase reporters, GFP, Horse-radish peroxidase (HRP) [33] [32] | Pseudovirus neutralization assays; surrogate neutralization tests | Enable quantification of infection levels through measurable signals |
| Viral Antigens | Recombinant spike protein, RBD proteins with His-tags [33] | Surrogate neutralization assays; antibody characterization | Provide target antigens for binding and neutralization studies |
| Standardized Disinfectants | Micro-Chem Plus, FWD, Medical EtOH [30] | Virucidal efficacy testing; reference standards | Serve as benchmark compounds for evaluating new virucidal agents |
| Reference Sera/Antibodies | NIBSC reference standards (20/136), WHO international standards [32] | Assay standardization; inter-laboratory comparison | Provide standardized controls for normalizing results across experiments |
Comparative Experimental Data Analysis
Quantitative Comparison of Antiviral Efficacy
Direct comparison of virucidal and neutralizing activities reveals their complementary strengths in viral infection control:
Table 4: Side-by-Side Comparison of Representative Virucidal and Neutralizing Agents
| Parameter | Virucidal Agent (Micro-Chem Plus) | Virucidal Agent (Ethanol) | Neutralizing Antibody Response |
|---|---|---|---|
| Target Pathogen | Nipah virus [30] | Human norovirus GII.17 [31] | SARS-CoV-2 Wuhan-Hu-1 & Variants [32] |
| Effective Concentration | 1:9 dilution (15 sec) [30] | Acidic formulation (30-60 sec) [31] | Serum dilution >1:10 to >1:160 [32] |
| Time to Efficacy | 15 seconds to 1 minute [30] | 30-60 seconds [31] | Days to weeks (immune response development) |
| Log Reduction/ Efficacy | >4 log₁₀ reduction [30] | Complete inactivation [31] | 90% infection inhibition (IC90) [32] |
| Primary Application | Surface decontamination; instrument disinfection [30] | Hand hygiene; surface disinfection [31] | Immune protection assessment; vaccine efficacy [32] |
| Duration of Effect | Immediate but transient | Immediate but transient | Weeks to months (immune memory) [34] |
Methodological Considerations and Limitations
Both virucidal and neutralizing activity assessments present methodological challenges that researchers must consider:
For virucidal testing, a significant limitation is the discrepancy between suspension tests and real-world conditions. The standardized suspension tests (EN 14476) expose viruses to large amounts of disinfectant in homogeneous solutions, making them easier to inactivate compared to viruses dried on surfaces where organic material may provide protection and surface interactions limit disinfectant access [29]. This challenge has been addressed through the development of carrier tests (EN 16777) that more accurately simulate practical conditions.
For neutralization assays, key considerations include the choice between authentic viruses versus pseudovirus systems. While authentic viruses provide the most biologically relevant data, they often require higher biosafety containment (BSL-3 for SARS-CoV-2) [32]. Pseudotyped viruses enable safer BSL-2 work and high-throughput screening but may not fully recapitulate all aspects of authentic virus entry and neutralization, particularly for viruses with complex entry mechanisms [28] [33].
Additionally, the dynamic nature of viral evolution presents challenges for both fields. Emerging SARS-CoV-2 variants of concern (VOCs) such as Delta and Omicron have demonstrated significant capacity to escape neutralizing antibody responses, reducing the efficacy of vaccine-elicited immunity [32]. Similarly, virucidal efficacy must be re-evaluated against emerging variants to ensure continued effectiveness of disinfection protocols.
Virucidal and neutralizing activities represent complementary approaches to viral infection control with distinct mechanisms, applications, and assessment methodologies. Virucidal activity testing provides critical data for environmental decontamination strategies using chemical agents that directly inactivate viral particles, with efficacy dependent on contact time, concentration, and formulation. Neutralizing activity assessment measures biological interference with viral infectivity, primarily through antibody-mediated mechanisms, serving as a key correlate of immune protection for vaccine development and therapeutic antibody evaluation.
The standardized frameworks established by organizations like the European Committee for Standardization (CEN) provide rigorous methodology for virucidal efficacy testing, while the evolving landscape of neutralization assays offers flexible options balancing biological fidelity with practical safety considerations. Researchers must select appropriate methods based on their specific applications, whether developing surface disinfectants, evaluating vaccine efficacy, or characterizing therapeutic antibodies, while acknowledging the limitations inherent in each approach. As viral threats continue to emerge, the complementary insights provided by both virucidal and neutralizing activity assessments will remain essential for comprehensive antiviral strategy development.
A Practical Guide to Viral Infectivity Assays: From Classic to Cutting-Edge
The plaque assay, developed in the early 1950s by Renato Dulbecco and Marguerite Vogt, remains the gold standard method for quantifying infectious viral titers and neutralizing antibodies in virology research [35] [36]. Despite the emergence of numerous alternative techniques, this foundational method continues to provide the most accurate measurement of replication-competent lytic virions, expressed as plaque-forming units per milliliter (PFU/ml) [37] [36]. Its enduring relevance stems from its unique ability to directly measure viral infectivity rather than simply detecting viral components, making it indispensable for vaccine development, antiviral testing, and serological studies [35] [38]. This guide examines the traditional plaque assay protocol, explores its modern automated counterparts, and provides a critical comparison of their respective capabilities, limitations, and applications in contemporary viral infectivity testing.
Experimental Protocol: Core Methodology
Traditional Plaque Assay Workflow
The fundamental plaque assay protocol involves infecting a confluent cell monolayer with serially diluted virus, restricting viral spread with a semi-solid overlay, and visualizing zones of cell death (plaques) after an incubation period [37] [36]. The standard methodology comprises these essential steps:
Cell Monolayer Preparation: The day before the assay, seed appropriate host cells (e.g., Vero E6, MDCK) into multi-well plates (commonly 6-, 12-, or 24-well format) and incubate until ~90-100% confluency is achieved [37] [39]. Different cell lines are required for different viruses.
Viral Inoculation: Prepare tenfold serial dilutions of viral samples in cell culture media [37] [36]. Rinse cell monolayers with buffer solution, then inoculate with diluted virus sample. Typical inoculation volumes are 500μl for a 12-well plate [39] or 100μl for a 6-well plate [38]. Incubate for 45-90 minutes with periodic rocking to ensure even coverage and prevent monolayer drying [37] [39].
Overlay Application: Following incubation, aspirate viral inoculum and apply a semi-solid overlay medium to restrict viral diffusion. Traditional options include:
- Agarose overlay: Mix 1:1 with 2x plaque media and heated 0.6% agarose for a final concentration of 0.3% [37] [39]
- Carboxymethyl cellulose (CMC): Prepare 2% stock solution and treat similarly to agarose [37]
- Liquid overlays (Avicel): Mix 1:1 with 2x plaque media and 1.2-2.4% microcrystalline cellulose for final concentration of 0.6-1.2% [37]
Incubation and Plaque Development: Incubate plates for 2-14 days depending on viral growth kinetics [37] [36]. Plaque visibility timeframe varies significantly by virus: Vesicular Stomatitis Virus (VSV) may form plaques in 2 days, while slower-growing viruses like some echoviruses require up to 14 days [40].
Fixation and Staining: Fix cells with formaldehyde or similar fixative, then stain with crystal violet (1% in 20% ethanol), Giemsa, or methylene blue to visualize plaques as clear areas against a stained cell monolayer background [37] [36] [39].
Immunoplaque and Focus Forming Modifications
For viruses that do not cause complete cell lysis or require earlier detection, immunostaining modifications enable plaque visualization:
Immunoplaque Assay: Following fixation, permeabilize cells with Triton X-100, then incubate with virus-specific primary antibody (e.g., anti-NP antibody for influenza) [39]. Detect with enzyme-conjugated or fluorescent secondary antibodies and corresponding substrates [39]. This approach is particularly valuable for viruses with non-lytic replication cycles [36].
Fluorescent Focus Assay (FFA): As an alternative to chromogenic detection, use fluorescently-labeled antibodies (e.g., Alexa Fluor 488 conjugates) for visualization by fluorescence microscopy [39]. This method often enables earlier plaque detection with enhanced sensitivity [36].
Data Interpretation and Quantification
PFU/ml Calculation and Statistical Considerations
The fundamental principle of plaque assay quantification assumes that each plaque originates from a single infectious viral particle [36] [40]. The viral titer is calculated using the formula:
PFU/ml = (Number of plaques) / (Dilution factor × Volume of inoculum in ml)
For reliable quantification, aim for plates containing 5-100 distinguishable plaques [37] [36]. Statistical variance approximates 10% for every 100 plaques counted when comparing sample replicates [37]. The dynamic range of accurate quantification depends on plate format and plaque size, with traditional 6-well plates typically accommodating up to 200 distinct plaques [36].
Plaque Morphology Analysis
Plaque characteristics provide valuable insights into viral behavior and pathogenicity [37]. Key morphological features to document include:
- Size variations: May indicate viral subpopulations with different replication kinetics or cytopathic effects [41]
- Clarity and border definition: Sharpness of plaque edges reflects the nature of cell-to-cell spread [37]
- Mixed morphologies: Can suggest genetic heterogeneity or competing viral quasispecies [41]
Technological Evolution: Automation Solutions
Advanced Imaging and Analysis Systems
Recent technological advancements address traditional plaque assay limitations through automation and enhanced imaging:
Lens-free holographic imaging: This label-free approach captures phase information from entire well plates (approximately 30 × 30 mm² area) at ~0.32 gigapixels per hour [38]. Combined with deep learning algorithms, it can detect VSV plaque-forming units in under 20 hours with >90% detection rate at 100% specificity, significantly reducing incubation times [38].
Integrated analysis systems: Commercial systems like the ImmunoSpot Analyzer (CTL) and ScanLab (MicroTechnix) standardize image acquisition and automate plaque counting, mitigating human bias and reducing analysis time from 6-10 minutes to 2-3 minutes per plate [35].
Real-time live-cell imaging: Instruments like IncuCyteS3 provide continuous observation of cellular events without fixation, enabling real-time analysis of neutralizing antibody quantification and viral replication kinetics [35].
High-Throughput Format Adaptations
Transitioning from traditional 6- or 12-well plates to 96-well formats significantly increases throughput. The µPlaque FFA system, for example, increases capacity from 4 samples/plate (24-well) to 16 samples/plate (96-well), enabling processing of 384 samples per run versus 32 with traditional formats [35].
Comparative Analysis: Traditional vs. Modern Approaches
Table 1: Comprehensive Comparison of Plaque Assay Methodologies
| Parameter | Traditional Plaque Assay | Automated Imaging Systems | Lens-free Holography + Deep Learning |
|---|---|---|---|
| Throughput | Low (4 samples/24-well plate) | Medium (16 samples/96-well plate) | High (full well scanning) |
| Assay Duration | 3-10 days [35] | 3-5 days [35] | Significant reduction (e.g., VSV: <20h [38]) |
| Plaque Detection Method | Manual visualization after staining | Software-configured automated counting | Label-free, automated PFU detection |
| Data Integrity | Prone to human bias and variability | Audit trails, user access control [35] | Automated, reproducible quantification |
| Specialized Equipment Needs | Standard tissue culture equipment | Dedicated imaging systems (~$50,000+) | Compact device (<$880 parts cost) [38] |
| Personnel Requirements | Highly trained staff (2 persons) [35] | Reduced staff dependency (1 person) [35] | Minimal staff involvement after setup |
| Dynamic Range | Limited by plate size and countable plaques | Improved through software optimization | 10-fold larger than standard assays [38] |
| Key Limitations | Labor-intensive, subjective counting, long incubation | High initial equipment cost, training requirements | Emerging technology, validation ongoing |
Table 2: Alternative Viral Quantification Methods Comparison
| Method | What It Measures | Throughput | Time to Result | Key Limitations |
|---|---|---|---|---|
| Plaque Assay | Infectious viral particles [36] | Low | 2-14 days [37] [36] | Labor intensive, requires lytic viruses |
| Focus Forming Assay (FFA) | Infectious units (antibody-detected) [36] | Medium | 1-3 days | Requires specific antibodies |
| TCID50 | Infectious dose (binary endpoint) [36] | Medium | 3-7 days | Less precise, statistical calculation |
| qPCR/qRT-PCR | Viral genome copies [37] [36] | High | Hours | Does not distinguish infectious vs. defective particles |
| Flow Cytometry | Viral proteins or infected cells [37] | High | 1-2 days | Complex sample processing, equipment cost |
| ELISA | Viral antigens [36] | High | 1 day | Does not measure infectivity |
| Electron Microscopy | Total viral particles [36] | Very Low | 1-2 days | Expensive, technically challenging |
Limitations and Considerations
Technical and Practical Constraints
Despite its gold standard status, the plaque assay faces several significant limitations:
Throughput Restrictions: Traditional formats process limited samples per run (e.g., 32 samples/run with 24-well plates versus 384 with improved alternatives) [35]
Temporal Constraints: Extended incubation periods (3-10 days depending on virus) delay experimental timelines [35] [36]
Expertise Dependency: Manual counting requires highly trained staff and remains prone to human bias, with operator-to-operator discrepancies affecting reproducibility [35]
Virus-specific Limitations: Some viruses do not form distinct plaques due to size or infection characteristics, requiring alternative approaches [35] [36]
Standardization Challenges: Methodology varies significantly between laboratories regarding cell lines, viral strains, incubation times, overlay types, and titer measurement methods (GMT, PRNT50, ID50), complicating cross-study comparisons [35]
Methodological Vulnerabilities
Common technical issues that compromise assay performance include:
Overlay Problems: Bubbles, lumps, or incomplete coverage from improper agarose handling or cold pipettes [41]
Inadequate Plaque Separation: Too many plaques leading to confluence and uncountable swaths of lysis [36] [41]
Non-viral Artifacts: Toxic components or undissolved agar particles creating false plaques [40]
Cell Monolayer Issues: Gaps in monolayers mistaken for plaques or insufficient confluence limiting infection spread [36]
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Key Research Reagent Solutions for Plaque Assays
| Reagent/Equipment | Function/Purpose | Examples/Specifications |
|---|---|---|
| Cell Lines | Virus-specific host cells for infection | Vero E6, MDCK (CCL-34, CRL-2935, CRL-2936) [39] [38] |
| Overlay Matrix | Restricts viral spread for discrete plaque formation | Agarose (0.3-0.6%), Carboxymethyl Cellulose (2%), Avicel (0.6-1.2%) [37] |
| Staining Solutions | Visualizes plaques against cell monolayer | Crystal violet (1%), Neutral red, Giemsa, MTT [37] |
| Fixation Agents | Preserves cellular architecture | Formaldehyde (10%), Methanol [37] [39] |
| Detection Antibodies | Immunoplaque assay components | Primary (e.g., H16-L10-4R5 for influenza NP), Secondary (enzyme-conjugated or fluorescent) [39] |
| Automated Imaging Systems | Standardizes image acquisition and analysis | ImmunoSpot Analyzer (CTL), ScanLab (MicroTechnix), IncuCyteS3 [35] |
| Multi-well Plates | Assay format and throughput determinant | 6-, 12-, 24-, 96-well formats [35] [36] |
The plaque assay maintains its gold standard status for quantifying infectious virions and neutralizing antibodies despite its recognized limitations. While traditional methodologies provide reliable results, they face challenges in throughput, standardization, and subjectivity. Modern automated systems address many of these limitations through improved imaging, analysis algorithms, and label-free detection methods, significantly reducing incubation times and human error. Researchers should select plaque assay formats based on their specific needs: traditional methods for resource-limited settings, immunoplaque assays for non-lytic viruses, and automated systems for high-throughput applications. As viral research advances toward increasingly complex questions about host-pathogen interactions, co-infections, and therapeutic development [42] [43], the evolution of plaque assay methodologies will continue to balance the technique's foundational principles with the practical demands of contemporary virology research.
In virology research and drug development, accurately quantifying viral infectivity is fundamental for understanding pathogenesis, evaluating antiviral agents, and developing vaccines. Two cornerstone cell-based techniques for determining the quantity of infectious virus in a sample are the plaque assay and the 50% Tissue Culture Infectious Dose (TCID50) assay [16]. While the plaque assay is often considered the gold standard for directly counting replication-competent lytic virions, the TCID50 assay provides a powerful, indirect method based on endpoint dilution [15]. This guide focuses on the TCID50 assay, detailing its workflow and statistical analysis, with a particular emphasis on the Spearman-Karber method. The TCID50 is defined as that dilution of a virus required to infect 50% of a cell monolayer [17]. This assay is especially valuable for viruses that do not form clear plaques in culture but still produce a observable cytopathic effect (CPE) [17]. Its utility spans a plethora of applications in both experimental and diagnostic virology, including work with HIV-1, influenza, and human herpesviruses [17].
Principle and Core Components of the TCID50 Assay
Fundamental Principle
The TCID50 assay operates on a probabilistic assumption. It determines the dilution at which 50% of the inoculated cell cultures exhibit infection, typically marked by CPE [16]. The core principle is that at the dilution where only 50% of the wells show CPE, there is, statistically, only one infectious virus particle present per well. This is because a single particle has a 50% chance of initiating an infection in the well [16]. Unlike the plaque assay, which uses a solid or semi-solid overlay to restrict virus spread and allow the counting of discrete plaques, the TCID50 assay uses a liquid medium, allowing unconstrained cell-free spread of the virus [16] [15]. The readout is not the counting of individual plaques, but a simple scoring of wells as "positive" or "negative" for CPE after a set incubation period.
Key Research Reagent Solutions
The successful execution of a TCID50 assay relies on several essential components. The table below details these key reagents and their functions.
Table 1: Essential Reagents for a TCID50 Assay
| Reagent/Material | Function & Importance |
|---|---|
| Susceptible Cell Line | The host cell that the virus can infect and replicate within, leading to CPE. The cell line must be carefully matched to the virus [17]. Examples include Vero E6 cells for SARS-CoV-2 [9] and MDCK cells for influenza [9]. |
| Virus Sample | The material of unknown infectious titer that is being quantified. The sample is typically serially diluted before inoculation [17]. |
| Growth Medium | Provides nutrients to maintain cell viability throughout the infection period. Often contains a reduced percentage of serum (e.g., 2-5%) during infection [9] [17]. |
| Diluent (e.g., PBS) | A sterile, isotonic solution like Phosphate-Buffered Saline (PBS) used to prepare the serial dilutions of the virus stock [17]. |
| Fixative and Stain (e.g., Crystal Violet) | Used to fix and stain cell monolayers at the endpoint to visualize CPE clearly. Viable cells retain the stain, while areas of CPE appear as clear zones [9]. |
Detailed TCID50 Assay Workflow
The following diagram illustrates the complete step-by-step workflow of the TCID50 assay.
Step-by-Step Protocol
- Cell Seeding: Seed a susceptible cell line (e.g., Vero E6, MDCK) into a 96-well tissue culture plate to achieve a confluent monolayer. A common seeding density is approximately (7 \times 10^4) cells per mL per well, but this should be optimized for the specific cell line and its growth rate [17]. The plate is incubated overnight until cells are 80-90% confluent.
- Virus Dilution Series: Prepare a series of 10-fold dilutions of the virus stock in a suitable diluent like PBS or maintenance medium. For example, to create a (10^{-3}) through (10^{-8}) dilution series, prepare tubes with 1.8 mL of diluent each. Transfer 0.2 mL of the virus stock to the first tube (making a (10^{-1}) dilution). Mix thoroughly and transfer 0.2 mL from this tube to the next, repeating this process through the series [16] [17].
- Cell Inoculation: Carefully remove the growth medium from the cell monolayer. Inoculate multiple wells per dilution (typically 4-8 replicates) with a fixed volume (e.g., 0.1 mL) of each virus dilution [16] [17]. Include several uninfected control wells that receive only diluent.
- Incubation and Monitoring: Incubate the inoculated plates at the appropriate temperature for the virus (e.g., 37°C for many human viruses). The virus is left free to spread in the liquid medium. The plates are monitored daily for the appearance of CPE, which can take from a few days to over a week, depending on the virus [17].
- Endpoint Scoring: After the incubation period, score each well individually. A well is considered "positive" if it shows characteristic CPE (e.g., cell rounding, detachment, syncytia formation) and "negative" if the monolayer appears healthy and intact, similar to the control wells [16] [17]. The results are recorded in a table for statistical analysis.
Statistical Analysis: The Spearman-Karber Method
Calculation Formula and Interpretation
The Spearman-Karber method is a statistical approach for calculating the 50% endpoint. It is known for its relative simplicity and robustness compared to other methods like Reed-Muench [16]. The formula for calculating the log(TCID(_{50})) is:
[ \text{log}(TCID{50}) = L + \left( \frac{d}{2} \right) - d \cdot \Sigma pi ]
Where:
- L = log(_{10}) of the lowest dilution tested (e.g., for a (10^{-1}) dilution, L = -1).
- d = log(_{10}) of the dilution factor (for 10-fold dilutions, d = 1).
- Σ p(_i) = sum of the proportions of positive wells (number of positive wells / total wells at that dilution) from the lowest dilution (i=1) to the highest (i=k).
The following diagram visualizes the logical process and calculation.
Worked Example of Spearman-Karber Calculation
Consider an assay with 8 wells per dilution and an inoculum volume of 0.1 mL. The CPE was scored as follows:
Table 2: Example Data for TCID50 Calculation Using Spearman-Karber Method
| Dilution | Positive Wells / Total | Proportion Positive (pᵢ) |
|---|---|---|
| (10^{-3}) | 8 / 8 | 1.00 |
| (10^{-4}) | 8 / 8 | 1.00 |
| (10^{-5}) | 6 / 8 | 0.75 |
| (10^{-6}) | 2 / 8 | 0.25 |
| (10^{-7}) | 0 / 8 | 0.00 |
Using the formula:
- L = log(_{10})((10^{-3})) = -3
- d = 1
- Σ p(_i) = 1.00 + 1.00 + 0.75 + 0.25 + 0.00 = 3.00
[ \text{log}(TCID_{50}) = -3 + \left( \frac{1}{2} \right) - (1 \times 3.00) = -5.5 ]
Therefore, the TCID({50}) per 0.1 mL is (10^{-5.5}). To express this as TCID({50}) per milliliter: [ TCID_{50}/mL = 10^{5.5} \times 10 = 10^{6.5} \approx 3.16 \times 10^{6} ]
Comparative Analysis with Plaque Assay and Other Methods
Direct Comparison of Performance Metrics
The TCID50 and plaque assays offer different advantages and are suited to different research scenarios. The table below summarizes a direct comparison based on experimental data and established protocols.
Table 3: Performance Comparison of TCID50 vs. Plaque Assay
| Parameter | TCID50 Assay | Plaque Assay |
|---|---|---|
| Principle | Indirect, probabilistic (50% endpoint) [16] | Direct, counting of discrete plaques [16] |
| Readout | Qualitative (Presence/Absence of CPE) [16] [17] | Quantitative (Plaque count) [16] |
| Typical Variability | Higher (∼35% relative error) [17] | Lower (10–100% relative error) [17] |
| Reported Units | TCID(_{50})/mL [16] | Plaque-Forming Units (PFU)/mL [16] |
| Sensitivity | Can be more sensitive for some viruses [19] | Standard sensitivity [19] |
| Key Advantage | Works for viruses that do not form plaques [17]; simpler scoring | Direct visualization and count of infectious units [15] |
| Key Disadvantage | Higher statistical variability; indirect measure [16] [17] | Requires virus to form visible plaques under an overlay [17] |
Experimental Data from Comparative Studies
A 2022 study quantifying SARS-CoV-2 variants provided concrete experimental data highlighting the differences between these assays. The research found that the viral titer obtained by plaque assay (PFU/mL) and the titer calculated from the TCID50 assay differed significantly for some variants, including differences of 0.59 to 0.96 log10 for Alpha, Gamma, Delta, and Mu variants [15]. This underscores that the relationship between PFU and TCID50 is not a fixed constant and can vary depending on the specific virus strain. For the ancestral D614G strain, however, no significant differences were observed, demonstrating that the assays can be comparable under specific conditions [15].
Another study comparing the two assays for filoviruses like Ebola virus found the TCID50 assay to be more sensitive but also slightly more variable. A consistent, approximately tenfold difference was observed in the numerical results between the two enumeration methods [19].
Applications and Protocol Selection in Viral Research
The TCID50 assay is widely used in diverse areas of virology. It is crucial for determining the infectious titer of virus stocks used in experiments, which is essential for standardizing the multiplicity of infection (MOI) across studies [16]. In antiviral drug development, it is employed to evaluate the efficacy of therapeutic candidates by determining the half-maximal inhibitory concentration (IC(_{50})) that reduces viral infection by 50% [9]. Furthermore, it plays a vital role in vaccine development and viral pathogenesis studies [15].
When deciding between the TCID50 and plaque assays, researchers should consider the nature of the virus and the experimental goals. The TCID50 assay is the method of choice when working with viruses that do not form distinct plaques, when a higher throughput is required, or when the available readout is CPE-based [17]. Conversely, the plaque assay is preferable when direct quantification of infectious particles is desired and when the virus forms clear, countable plaques under an overlay [16] [15]. The choice may also be dictated by specific regulatory guidelines or standard operating procedures (SOPs) that mandate one method based on historical usage and validation data [16].
Infectious Focus Assays and Immunostaining Techniques
In the field of virology and antiviral drug development, accurately quantifying infectious viral particles is a cornerstone of research. Among the various techniques available, infectious focus assays have emerged as a critical tool for determining viral titer by counting discrete foci of infection, which are clusters of cells infected by a single viral particle [44]. These assays are frequently combined with immunostaining techniques, which use antibody-based detection to visualize and quantify these infection foci with high specificity and sensitivity [44] [45]. Unlike methods that rely on observable cell death (cytopathic effect), the combination of focus assays with immunostaining allows for the detection of infected cells earlier in the viral life cycle and is applicable to viruses that do not cause clear plaques or cell lysis [44] [46]. This guide provides a comparative analysis of these methodologies, framed within the broader context of comparative viral infectivity testing for in vitro research, offering researchers a data-driven foundation for selecting appropriate protocols for their specific applications.
Core Principles and Techniques
The Basis of Immunostaining
Immunostaining is a foundational technique that utilizes the specific binding of antibodies to target antigens within cells or tissues, allowing for the visualization of specific proteins or pathogens [45]. The core principle involves tagging antibodies with detectable markers, such as fluorescent dyes or enzymes, which reveal the presence and localization of the target antigen when viewed under a microscope [47] [45].
There are two primary methodological approaches:
- Direct Method: A primary antibody, directly conjugated to a detectable marker, binds to the target antigen. This method is faster and involves fewer steps but generally offers lower sensitivity due to the absence of signal amplification [45].
- Indirect Method: An unlabeled primary antibody binds to the antigen, and a labeled secondary antibody, which recognizes the primary antibody, is then applied. This method provides signal amplification because multiple secondary antibodies can bind to a single primary antibody, resulting in enhanced sensitivity [47] [45].
When applied to virus-infected cells, these techniques allow researchers to stain for specific viral antigens, thereby identifying infected cells within a monolayer. The stained foci, each theoretically originating from a single infectious viral particle, are then counted to calculate the virus titer in Focus-Forming Units (FFU) per milliliter [44] [48].
Workflow of an Infectious Focus Assay
The following diagram illustrates the generalized workflow for performing an infectious focus assay with immunostaining, integrating key steps from various protocols [44] [49] [48].
Comparative Assay Performance Data
The selection of an infectivity assay depends on multiple performance metrics. The table below summarizes quantitative data comparing focus assays with other common techniques, based on studies with filoviruses and influenza A virus [44] [46] [50].
Table 1: Quantitative Comparison of Viral Infectivity Assays
| Assay Type | Typical Duration | Sensitivity (Relative to Plaque Assay) | Key Advantage | Primary Limitation | Best Suited For |
|---|---|---|---|---|---|
| Focus Forming Assay (FFA) | 2 days [44] | ~10-fold higher [44] | High specificity for infected cells; quantifies non-lytic viruses [44] [46] | Higher cost of antibodies/dyes [46] | High-throughput screening; non-lytic viruses |
| Plaque Assay (CVMO) | 7+ days [44] | (Benchmark) | Low cost; considered a gold standard [44] [46] | Long turnaround time; subjective counting [44] | Viruses forming clear plaques |
| TCID50 | 7-14 days [44] [49] | ~10-fold lower [44] | Does not require semi-solid overlay [44] | Low reproducibility; subjective endpoint determination [44] | Viruses with irregular/no plaque morphology |
| Digital Focus Assay (dFA) | 1-2 days [46] | Good agreement with plaque assay [46] | Miniaturized volumes; flexible endpoint; automated readout [46] | Requires microfluidic device fabrication [46] | Absolute quantification; limited sample volumes |
A critical metric for any potency assay is its reproducibility. In a comparative study of filovirus assays, the Focus Assay demonstrated a coefficient of variation (CV) of 7.9%, outperforming the Crystal Violet Methylcellulose Overlay (CVMO) Plaque Assay (CV: 18.5%) and the TCID50 assay (CV: 31.3%), highlighting its superior precision and lower operator-dependent variability [44].
Detailed Experimental Protocols
Standard Focus Forming Unit (FFU) Assay for Filoviruses
This protocol is adapted from procedures used to titer filoviruses like Ebola and Marburg [44].
Materials & Reagents:
- Cells: Vero E6 cells (or other susceptible cell line).
- Growth Medium: DMEM supplemented with 10% Fetal Bovine Serum (FBS) and 1% Penicillin/Streptomycin.
- Infection Medium: DMEM supplemented with 2% FBS.
- Fixative: 4% Paraformaldehyde (PFA) in Phosphate Buffered Saline (PBS).
- Permeabilization Buffer: PBS with 0.1% Triton X-100.
- Blocking Buffer: PBS with 1-5% Bovine Serum Albumin (BSA) or serum from the host species of the secondary antibody.
- Antibodies: Primary antibody specific for the target virus (e.g., anti-Ebola virus glycoprotein) and a fluorophore-conjugated secondary antibody.
- Equipment: 96-well or 384-well tissue culture plates, humidified CO2 incubator, fluorescence microscope or high-content imager.
Procedure:
- Cell Seeding: Seed Vero E6 cells in a 96-well plate at 75–90% confluency and incubate overnight.
- Virus Inoculation: Prepare 10-fold serial dilutions of the virus stock in infection medium. Remove the growth medium from the cells and inoculate triplicate wells with each virus dilution. Include control wells with infection medium only. Incubate the plate for 1 hour at 37°C with 5% CO2 on a rocking platform to facilitate even adsorption.
- Post-Inoculation Incubation: Remove the inoculum and carefully replace it with fresh infection medium. Incubate the plate for 24-48 hours (time depends on the virus replication kinetics).
- Immunostaining: a. Fixation: Remove the medium and gently wash the cells with PBS. Add 4% PFA to fix the cells for 30 minutes at room temperature. b. Permeabilization: Remove the PFA, wash with PBS, and add permeabilization buffer for 10-15 minutes. c. Blocking: Remove the permeabilization buffer, wash, and add blocking buffer for 1 hour to reduce non-specific antibody binding. d. Primary Antibody: Dilute the virus-specific primary antibody in blocking buffer. Add to the wells and incubate for 1-2 hours at room temperature or overnight at 4°C. e. Secondary Antibody: Wash the wells thoroughly with PBS to remove unbound primary antibody. Add the fluorophore-conjugated secondary antibody (diluted in blocking buffer) and incubate for 1 hour in the dark.
- Image Acquisition and Analysis: Acquire images using a fluorescence microscope or an automated high-content imager. Count the number of fluorescent foci in wells containing 10-100 foci for accurate counting. Calculate the virus titer using the following formula: Virus Titer (FFU/mL) = (Average number of foci per well) / (Dilution factor × Inoculum volume (mL)) [44] [48].
High-Throughput Automated Potency Assay (IRVE) for HCMV
The Imaging of Relative Viral Expression (IRVE) assay is a high-throughput, automated relative potency assay developed for Human Cytomegalovirus (HCMV) vaccine development [49].
Materials & Reagents:
- Cells: ARPE-19 epithelial cell line.
- Antibodies: Primary antibody against HCMV Immediate Early 1 (IE1) protein and a fluorescently labeled secondary antibody.
- Stain: Hoechst 33342 or DAPI for nuclear counterstaining.
- Equipment: Automated cell culture system, 384-well plates, integrated robotic system for liquid handling, high-content fluorescence microscope.
Procedure:
- Cell Seeding and Infection: Seed ARPE-19 cells into 384-well plates using an automated system. The following day, inoculate the cells with serial dilutions of the HCMV vaccine candidate.
- Incubation: Incubate the plates for a defined period (e.g., 24-48 hours) to allow for the expression of the IE1 viral antigen.
- Automated Immunostaining: Using a robotic liquid handling system, perform the steps of fixation, permeabilization, and blocking. Subsequently, dispense the anti-IE1 primary antibody and the fluorescent secondary antibody.
- Automated Imaging and Analysis: The plates are automatically imaged using a high-content microscope. Software algorithms identify all cell nuclei based on the Hoechst stain and then quantify the number of IE1-positive infected nuclei. The relative potency of the test sample is calculated by comparing its half-maximal effective dilution (ED50) to that of a reference standard [49].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of infectious focus assays relies on a set of well-defined reagents and tools. The following table lists key solutions and their critical functions in the experimental workflow.
Table 2: Essential Research Reagent Solutions for Focus Assays
| Research Reagent | Function in the Assay | Examples & Notes |
|---|---|---|
| Cell Culture Lines | Provide a susceptible host for viral replication. | Vero E6 (filoviruses [44]), ARPE-19 (HCMV [49]), MDCK (influenza [50]). Cell type must be permissive for the virus under study. |
| Specific Antibodies | Core detection reagent for immunostaining; binds viral antigens. | Anti-viral protein antibodies (e.g., anti-nucleoprotein for IAV [51]). Specificity and titer must be validated for the target virus. |
| Fluorophore-Conjugated Secondaries | Enables visualization of primary antibody binding. | Antibodies conjugated to FITC, Cy3, etc. [45]. Choice depends on microscope filters and multiplexing needs. |
| Fixatives | Preserves cellular morphology and immobilizes antigens. | 4% Paraformaldehyde (PFA) is most common [48]. Cross-links proteins, preserving structure. |
| Permeabilization Buffers | Permeabilizes cell membranes to allow antibody access to intracellular antigens. | Detergents like Triton X-100 or Saponin [49]. Critical for staining intracellular viral proteins. |
| Blocking Buffers | Reduces non-specific antibody binding to minimize background signal. | 1-5% BSA or serum [45]. Serum should be from an unrelated species to the antibodies used. |
| Automated Imaging Systems | High-throughput acquisition and quantitative analysis of fluorescent foci. | High-content screening microscopes [49]. Enable automated focusing and multi-well plate scanning. |
Advanced Technological Innovations
The field of viral infectivity testing is evolving with several cutting-edge technologies that address the limitations of traditional assays.
- Digital Focus Assays (dFA): This microfluidic technology discretizes a virus-containing sample into thousands of nanoliter-scale wells [46]. Each well is effectively a separate infection experiment. After incubation, wells are scored as positive or negative for infection based on immunostaining. This digital readout allows for absolute quantification of infectious virus without the need for direct counting of foci, reduces reagent consumption, and eliminates the problem of foci merging that can plague conventional assays [46].
- Virtual Staining with Artificial Intelligence (AI): Emerging AI methodologies, particularly deep neural networks, are being trained to predict the appearance of fluorescent virus infection signals from brightfield or non-specific nuclear stain images [51]. This approach, known as Virus Infection Reporter Virtual Staining (VIRVS), could eventually reduce or eliminate the need for complex immunostaining procedures, saving time, reagents, and reducing potential biases [51].
- Automation and Miniaturization: The integration of robotic systems for cell culture, liquid handling, and immunostaining, as demonstrated in the IRVE assay, significantly increases throughput, improves reproducibility, and enables the screening of large numbers of samples, such as in drug discovery and vaccine development campaigns [49].
Viral infectivity quantification represents a critical step in virology research, vaccine development, and antiviral drug discovery. Traditional methods like plaque assays have served as gold standards for decades but present significant limitations including subjective counting, time-intensive procedures, and limited sensitivity. Within this context, the Semi-Functional Quantitative Flow Cytometry (SFQF) assay has emerged as a powerful alternative that combines the quantitative nature of classical virology with the high-throughput, single-cell resolution of modern flow cytometry. This guide objectively compares the SFQF assay's performance against other established methods, providing researchers with experimental data and protocols to inform their selection of viral quantification approaches.
Experimental Principle and Methodology
Core Concept of SFQF Assay
The SFQF assay is a flow cytometry-based technique designed for the accurate estimation of infectious virus quantity by detecting viral protein expression in infected host cells. Unlike molecular methods that detect viral genetic material (which may represent defective particles), the SFQF assay measures actual viral replication events through immunostaining of intracellular viral proteins, providing a "semi-functional" assessment of viral infectivity. The assay was specifically developed to overcome technical shortcomings in earlier flow cytometric titration methods, including suboptimal parameters such as cell overgrowth, plate scale limitations, and detection threshold issues [52].
Key Research Reagent Solutions
Table 1: Essential Research Reagents for SFQF Assay Implementation
| Reagent/Material | Function in Assay | Specific Example |
|---|---|---|
| Virus-Specific Antibodies | Detection of intracellular viral proteins | LCMV NP-specific VL-4 antibody (clone) [52] |
| Fluorescent Conjugates | Antibody labeling for detection | Alexa Fluor 647 monoclonal antibody labeling kit [52] |
| Cell Lines | Viral propagation and infection platform | Vero cells (for LCMV) [52] |
| Permeabilization Buffers | Enable intracellular antibody access | Fixation/permeabilization solution [52] |
| Flow Cytometry Standards | Quantification calibration | Quantum MESF Kit (for quantitative FCM) [53] |
Detailed SFQF Protocol
The following protocol is adapted from the LCMV detection method optimized for SFQF assay [52]:
Cell Preparation and Plating: Seed Vero cells in appropriate culture vessels (6-well, 12-well, or 24-well plates) at optimized densities to reach 50%-70% confluence after 15 hours of incubation. For 6-well plates, this typically corresponds to 1.5×10^5 cells per well as a low seeding density or 3.0×10^5 cells for high density [52].
Virus Infection: Prepare serial dilutions of viral stock in plain medium. Remove medium from cultured cells and infect with 200μl of viral diluents. Incubate for 1 hour under shaking conditions (intermittent shaking every 15 minutes) to prevent drying and ensure even infection [52].
Post-Infection Incubation: Replace inoculum with fresh complete medium and incubate cells for 24-48 hours at 37°C in a humidified CO₂ incubator to allow viral replication and protein expression.
Cell Harvesting and Fixation: Detach cells using trypsin-EDTA treatment at 37°C for 3 minutes. Wash cells with FACS buffer (supplemented with 2% FBS and 0.1% sodium azide). Treat cells with fixation/permeabilization solution for 20 minutes at room temperature [52].
Intracellular Staining: Wash cells with Perm/Wash buffer, then incubate with fluorophore-conjugated virus-specific primary antibody (e.g., Alexa Fluor 647-conjugated VL-4 antibody for LCMV NP detection) for 35 minutes at room temperature protected from light [52].
Flow Cytometric Analysis: Wash stained cells twice with FACS buffer and analyze using a flow cytometer. Collect a minimum of 10,000 events per sample. Set analysis gates using appropriate isotype controls and uninfected cells [52].
SFQF Assay Workflow
Performance Comparison with Alternative Methods
Quantitative Comparison of Methodologies
Table 2: Comprehensive Method Comparison for Viral Quantification
| Method | Detection Principle | Time to Results | Sensitivity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| SFQF Assay | Viral protein detection via flow cytometry | ~28-52 hours [52] | 7x more sensitive than BHK21 cells for LCMV [52] | Single-cell resolution, high-throughput capability, phenotypic analysis of infected cells [52] | Requires virus-specific antibodies, specialized equipment |
| Plaque Assay | Viral cytopathic effect visualization | 5-7 days [52] [53] | Varies with virus type | Established gold standard, direct quantification of infectious units [52] | Subjective counting, labor-intensive, time-consuming [52] |
| Quantitative PCR | Viral nucleic acid detection | 4-8 hours | High sensitivity for genome detection | Rapid, extremely sensitive | Cannot distinguish infectious from defective particles [52] |
| Endpoint Dilution (TCID₅₀) | Cytopathic effect in serial dilutions | 7-10 days [53] | Moderate | Does not require agar overlay | Statistical rather than direct count, longer duration |
| Quantitative Flow Cytometry (qFCM) | Fluorescence quantification via MESF | 24-48 hours [53] | High with proper standardization | Actual protein quantification, superior to relative fluorescence [53] | Requires standardized beads, more complex calibration [53] |
Experimental Performance Data
In direct comparison studies for LCMV detection, the SFQF assay demonstrated significantly enhanced sensitivity over traditional methods. When comparing cell line susceptibility, Vero cells were approximately 7-times more sensitive to LCMV infection than BHK21 cells at concentrations of 10^3 and 10^4 pfu/ml [52]. The SFQF assay detected viral nucleoprotein in both Vero and BHK21 cells infected with more than 10^3 pfu/ml, with saturation occurring at 10^5 and 10^6 pfu/ml dilutions respectively [52].
The optimization of cell confluence parameters proved critical for assay performance. Researchers established that appropriate monolayer development significantly affects viral detection efficiency, with 50%-70% confluence at the time of infection providing optimal results [52]. Proper plate scaling and cell distribution also influenced viral penetration and detection reliability.
For true quantitative applications, the qFCM approach using Molecules of Equivalent Soluble Fluorochrome (MESF) units has demonstrated a direct relationship (by second-degree polynomial regression) between viral titers and fluorescence intensity, enabling more precise quantification than relative fluorescence measurements alone [53].
Advanced Applications and Integration
Complementary Viromics Approaches
Recent technological advances have demonstrated that flow cytometry-coupled viromics can significantly enhance viral detection sensitivity. When combined with metagenomics, FACS-based sorting identified viral families and annotated contigs that were not detected in bulk samples, with up to 43% of mapped reads exclusively found in FACS-sorted fractions [54]. This approach has proven particularly valuable for detecting rare viral species and improving genome assembly from complex samples [54].
Pathway and Receptor Analysis
The SFQF platform can be integrated with receptor interaction studies to provide mechanistic insights into viral entry. For respiratory syncytial virus (RSV), confocal immunofluorescence and imaging flow cytometry have visualized virus-receptor interactions, demonstrating colocalization of RSV with its receptor nucleolin at the apical surface of polarized cells [55]. Such integration allows simultaneous quantification of infectivity and investigation of entry mechanisms.
Viral Infection and Detection Pathway
Discussion and Research Implications
The development and optimization of SFQF represents a significant advancement in viral quantification methodologies. By leveraging the single-cell resolution and high-throughput capacity of flow cytometry, this approach addresses critical limitations of traditional plaque assays, particularly their subjectivity and prolonged duration [52]. The capability to simultaneously phenotype infected cells provides additional layers of information beyond simple quantification, enabling researchers to investigate viral tropism and host response in heterogeneous cell populations.
The integration of truly quantitative approaches through MESF standardization further enhances the methodology's utility for comparative studies and vaccine potency testing [53]. When combined with emerging techniques such as imaging flow cytometry and FACS-coupled metagenomics, the SFQF platform forms part of an increasingly sophisticated toolbox for viral research [54] [55].
For researchers implementing this technology, careful attention to optimization parameters is essential—including cell line selection, confluence conditions, and antibody validation. The demonstrated 7-fold sensitivity difference between Vero and BHK21 cells for LCMV detection underscores the importance of platform validation for each virus-cell system [52]. With proper optimization, the SFQF assay provides a robust, reproducible, and information-rich alternative to traditional viral quantification methods, particularly suited for high-throughput screening applications and mechanistic studies of viral replication.
Laser Force Cytology (LFC) represents a transformative approach in the field of label-free cellular analysis, offering significant advantages for viral infectivity testing in vitro. This technology leverages the measurement of optical and fluidic forces exerted on single cells as they pass through a laser within a microfluidic channel, capturing up to 24 multivariate parameters per cell in a fraction of a second without the need for antibodies, dyes, or fluorescent labels [56] [57]. For researchers and drug development professionals focused on virology, LFC provides a powerful tool for quantifying viral infectivity, monitoring cytopathic effects (CPE), and conducting neutralization assays with unprecedented speed and precision. Unlike traditional methods that often require days to weeks for results, LFC enables real-time, in-process monitoring of viral infection progression, dramatically accelerating research timelines and process optimization in vaccine development and antiviral therapeutic testing [58] [59].
The core principle of LFC centers on detecting changes in a cell's intrinsic biophysical and biochemical properties, which are altered upon viral infection. As photons from a laser interact with a cell, the resulting optical force provides measurements influenced by the cell's refractive index, size, shape, morphology, and internal structure [57]. Viral infection induces detectable shifts in these properties, creating a unique "cellular fingerprint" that can be quantitatively measured. This allows researchers to monitor infection kinetics, quantify infectious titers, and assess antiviral drug efficacy without the artifacts and delays associated with label-based endpoints. The technology's label-free nature preserves cells in their natural states, reducing measurement bias and ensuring results reflect true cellular physiology during viral infection [56].
Technology Comparison: LFC Versus Traditional Viral Infectivity Assays
Performance Metrics and Capabilities
The following table summarizes how LFC compares with traditional methods across key performance metrics relevant to viral infectivity research:
| Analytical Method | Label/Reagent Free | Time to Result | Throughput | Information Quality | Automation Potential |
|---|---|---|---|---|---|
| Laser Force Cytology (LFC) | Yes [57] | Minutes to hours [56] [59] | High [56] | Multivariate, single-cell data [57] | Full automation possible [56] |
| Plaque Assay | No (requires staining) | 3-14 days [59] | Low | Quantitative but low-resolution | Low |
| TCID₅₀ Assay | No (often requires staining) | 6-8 days [59] | Low | Quantitative but low-resolution | Low |
| Flow Cytometry | No (requires antibodies/fluorophores) | Hours to days [60] | Medium | Multiparametric, but label-dependent | Medium |
| qPCR/ddPCR | No (requires reagents) | Hours [57] | Medium | High (nucleic acid specific) | Medium |
| AI-Based Microscopy (DVICE) | Yes [11] | Hours to days | Medium | Population-level CPE assessment | High |
Advantages of LFC in Viral Research
Elimination of Labeling Artifacts and Workflow Simplification: Traditional infectivity assays like plaque tests and TCID₅₀ require extensive sample processing, staining, and manual interpretation, introducing variability and prolonging time-to-results [59]. Flow cytometry depends on fluorescent labels and antibodies, which can alter cell behavior through non-specific binding or photobleaching, potentially skewing results [56] [60]. LFC's label-free approach bypasses these issues entirely, preserving native cell状态 and eliminating labeling-induced artifacts. This translates to significantly simplified workflows with minimal sample preparation, reducing hands-on time and operator-dependent variability [57] [60].
Superior Data Richness and Sensitivity: LFC captures multiparametric data at the single-cell level, measuring subtle phenotypic changes often undetectable by flow cytometry. For instance, one study demonstrated that while flow cytometry forward and side scatter parameters failed to distinguish macrophages exposed to silica beads, LFC readily detected these changes [57]. This high-resolution capability enables researchers to detect early infection events and subtle cellular responses that precede more obvious cytopathic destruction [58]. The technology's ability to measure optical force index (OFI), deformability, and other intrinsic properties provides a multidimensional view of infection progression unavailable from single-parameter endpoint assays [59].
Experimental Data and Validation in Viral Applications
Quantitative Correlation with Traditional Infectivity Measures
Substantial research has demonstrated strong correlation between LFC measurements and established viral quantification methods, validating its utility for infectivity assessment:
Measles Virus Potency Monitoring: In a seminal study monitoring measles virus production in Vero cells on microcarriers, researchers established a robust correlation between LFC measurements and traditional potency assays. They defined an Infection Metric based on the percentage of cells with an Optical Force Index (OFI) exceeding a threshold of 55 s⁻¹. This metric showed excellent correlation with viral potency per viable cell, with an absolute average log₁₀ difference of just 0.074 between LFC measurements and reference methods [59]. This high degree of correlation, combined with LFC's dramatically faster time-to-result (hours versus days for TCID₅₀), positions LFC as a valuable process analytical technology (PAT) for vaccine manufacturing.
Broad Spectrum Viral Detection: LFC has demonstrated effectiveness across diverse viral families. The technology has been successfully applied to measure infectivity for vesicular stomatitis virus (VSV), adeno-associated virus (AAV), and influenza virus, among others [58]. In AAV transduction studies, LFC achieved a coefficient of variation as low as 14%, highlighting its precision for viral vector characterization [58]. The label-free nature of the assay makes it broadly applicable to different viruses without requiring virus-specific reagents, as it detects the universal cellular responses to infection rather than virus-specific antigens or sequences.
Comparative Experimental Protocol: LFC vs. TCID₅₀ for Viral Quantification
LFC Protocol for Viral Infectivity Measurement:
- Cell Preparation: Culture permissive cells (e.g., Vero cells) to appropriate confluence in standard growth medium [59].
- Viral Infection: Inoculate cells with serial dilutions of viral stock or experimental samples. Include uninfected controls.
- Incubation: Incubate infected cells for a defined period (typically 24-72 hours depending on virus kinetics).
- Sample Harvesting: Gently detach cells using enzymatic or non-enzymatic methods. Stabilize cells in LumaCyte Stabilization Fluid at approximately 750,000 cells/mL [59].
- LFC Analysis: Transfer 200µL aliquots (≈150,000 cells) to a 96-well plate. Analyze using Radiance instrument with automated data acquisition.
- Data Processing: Apply predefined infection metrics (e.g., OFI thresholding) using integrated software. Generate infectivity scores based on established correlation models.
Traditional TCID₅₀ Protocol:
- Cell Seeding: Seed permissive cells in 96-well plates and incubate until confluent monolayers form.
- Viral Inoculation: Inoculate cells with serial dilutions of viral samples (typically 8-10 dilutions with multiple replicates).
- Extended Incubation: Incubate infected cells for 7-14 days to allow for full development of cytopathic effect (CPE).
- Staining and Visualization: Fix cells with paraformaldehyde and stain with crystal violet or other CPE detection dyes [11].
- Manual Scoring: Examine each well microscopically for CPE by trained personnel. Score wells as positive or negative for infection.
- Calculations: Apply statistical methods (e.g., Spearman-Kärber formula) to calculate the 50% infectious dose.
Key Research Reagent Solutions for LFC Viral Infectivity Assays
Implementing LFC for viral infectivity studies requires specific materials and reagents optimized for label-free analysis:
| Reagent/Material | Function in LFC Viral Assays | Application Notes |
|---|---|---|
| LumaCyte Radiance Instrument | Core analysis platform measuring optical & fluidic forces on single cells | Provides 24+ parameters per cell; includes microfluidic cartridge & laser system [56] |
| LumaCyte Stabilization Fluid | Preserves cell state during analysis | Maintains native cell properties without fixation; critical for reproducible OFI measurements [59] |
| Permissive Cell Lines | Host cells for viral infection studies | Vero, A549, Huh7, HEK293 commonly used; must be optimized for specific viruses [11] [59] |
| Microcarriers (for adherent systems) | Support surface for cell growth in bioreactor systems | Enables monitoring of infection in scalable manufacturing-relevant formats [59] |
| 96-Well Plate Autosampler | High-throughput sample processing | Enables automated analysis of multiple samples and conditions [56] |
| Reference Virus Stocks | Assay validation and standardization | Required for establishing correlation models and infection metrics [59] |
Implementation Considerations for Research and Development
Integration with Existing Workflows: Implementing LFC technology requires consideration of several practical aspects. The system is designed for seamless tech transfer, operating with minimal specialized training compared to techniques like flow cytometry that require expert knowledge of antibody panel design and compensation [60]. For viral assay development, researchers must establish virus-specific correlation models between LFC parameters and traditional infectivity measures, a process that requires careful experimental design but yields substantial long-term efficiency gains [59]. The microfluidic format of LFC analysis consumes small sample volumes (typically 200µL), preserving precious experimental materials, while the automated 96-well plate format supports medium-throughput screening applications [56].
Data Analysis and Interpretation: The multivariate data generated by LFC requires specialized analytical approaches. The technology's software typically includes principal component analysis (PCA) and machine learning algorithms to identify infection-specific patterns within the high-dimensional data space [57] [58]. For viral infectivity applications, researchers often define specific infection metrics based on parameters like Optical Force Index (OFI) that show consistent virus-induced changes [59]. These analytical models become more robust with larger training datasets, highlighting the importance of comprehensive assay validation across multiple experimental conditions and biological replicates.
Emerging Alternatives and Future Directions
AI-Powered Microscopy Approaches: Beyond LFC, other label-free technologies are emerging for viral infectivity assessment. The Detection of Virus-Induced Cytopathic Effect (DVICE) platform combines transmitted light microscopy with artificial intelligence (convolutional neural networks) to automatically identify virus-induced CPE [11]. This approach has demonstrated high accuracy across diverse viruses including coronavirus, influenza virus, herpes simplex virus, and adenovirus, achieving an area under the receiver operating characteristic curve (AUROC) of 0.991 [11]. While DVICE monitors population-level changes rather than single-cell biophysical properties, it shares LFC's advantages of being label-free and substantially faster than traditional plaque or TCID₅₀ assays.
Advanced 3D Imaging Flow Cytometry: Light-field flow cytometry represents another technological advancement, enabling high-resolution, volumetric imaging of single cells in flow at rates up to 5,750 cells per second [61]. This approach provides detailed 3D subcellular information with near-diffraction-limited resolution (400-600 nm in all three dimensions), potentially enabling more nuanced analysis of viral infection-induced structural changes [61]. While currently more complex to implement than LFC and not yet widely demonstrated for viral infectivity quantification, this technology illustrates the continuing innovation in label-free cellular analysis.
Laser Force Cytology establishes a new paradigm for viral infectivity testing, addressing critical limitations of traditional methods through its label-free, multiparametric approach and significantly reduced time-to-results. The technology's ability to provide real-time, single-cell resolution data on infection progression makes it particularly valuable for vaccine development, antiviral screening, and bioprocess optimization. While traditional methods like plaque assays and TCID₅₀ remain important gold standards, LFC offers a complementary approach that enhances research efficiency without sacrificing quantitative rigor. As the field advances, integration of LFC with other emerging technologies like AI-powered microscopy and advanced 3D imaging promises to further revolutionize our approach to viral quantification and characterization, ultimately accelerating the development of novel antiviral therapies and vaccines.
Neutralization assays are foundational tools in virology and immunology, providing critical in vitro data on the efficacy of antiviral substances and antibodies. These assays function by measuring the ability of antibodies or compounds to block viral infectivity, thereby "neutralizing" the virus and preventing it from entering and infecting target cells. The data generated is pivotal for vaccine development, therapeutic antibody validation, and antiviral drug screening, forming a cornerstone of preclinical research [62]. In the context of comparative viral infectivity testing, these assays allow researchers to quantitatively compare the potency of different countermeasures against a wide array of viral pathogens and their evolving variants.
The fundamental principle behind these assays is the incubation of serial dilutions of an antiviral agent with a standardized amount of virus. This mixture is then applied to permissive cell cultures. The readout—whether the detection of a cytopathic effect, a luminescence signal, or plaque formation—serves as a proxy for the fraction of virus that remains infectious. Analyzing the dose-response relationship allows for the calculation of key potency metrics, most commonly the half-maximal inhibitory concentration (IC50) or the neutralization titer (NT50, etc.) that reduces viral infection by 50% [63]. The choice of assay type involves a careful balance between biological relevance, practical safety considerations, and throughput requirements, a balance that this guide will explore in detail.
Comparative Analysis of Assay Types
The landscape of neutralization assays is diverse, with each platform offering distinct advantages and limitations. The primary division lies between assays using live, replicating viruses and those using engineered pseudoviruses.
Live Virus Neutralization Assays
Live virus neutralization assays (LVNAs), including Plaque Reduction Neutralization Tests (PRNT), Focus Reduction Neutralization Tests (FRNT), and Microneutralization Assays (MNA), are historically considered the gold standard. They employ authentic, replication-competent viruses to infect cell lines, such as Vero E6 or Calu-3, and quantify neutralization through direct observation of viral replication inhibition [64] [65]. The key advantage of LVNAs is their high biological fidelity, as they recapitulate the entire viral life cycle, including entry, replication, and spread. This makes their readouts highly relevant for predicting in vivo efficacy. However, a significant constraint is the requirement for high-level biosafety containment (e.g., BSL-3 for pathogens like SARS-CoV-2), which limits their accessibility to specialized laboratories. Furthermore, these assays are often lower in throughput and more time-consuming, taking several days to complete due to the need for visual scoring of plaques or cytopathic effects [64] [62].
Pseudotyped Virus Neutralization Assays
Pseudotyped virus neutralization assays (PVNAs) offer a versatile and safer alternative. These assays use engineered surrogate viruses (commonly vesicular stomatitis virus (VSV) or lentiviruses) that are genetically modified to express the surface protein (e.g., the spike protein of SARS-CoV-2) of the target pathogen. They are designed as single-cycle infection systems, often incorporating reporter genes like luciferase or GFP for quantification [64] [65]. The principal benefit of PVNAs is their ability to be handled safely in BSL-2 laboratories, dramatically expanding the number of facilities that can perform this research. Their design also facilitates high-throughput screening and rapid adaptation to newly emerging viral variants by simply swapping the surface protein expression plasmid. A potential limitation is that they do not model the full viral replication cycle, focusing solely on the entry step mediated by the surface protein. This might overlook neutralization mechanisms that target other stages of replication [62].
Table 1: Core Characteristics of Major Neutralization Assay Types
| Assay Type | Virus System | Biosafety Level | Key Readout | Throughput | Key Advantage | Primary Limitation |
|---|---|---|---|---|---|---|
| Plaque/Focus Reduction (PRNT/FRNT) | Live Virus | BSL-3 | Plaque/Focus Count | Low | Gold Standard, Full Virus Lifecycle | Low throughput, Requires BSL-3 |
| Microneutralization (MNA) | Live Virus | BSL-3 | Cytopathic Effect (CPE) | Medium | Visually Simple, Established | Subjective scoring, Requires BSL-3 |
| Pseudotyped Virus (PVNA) | VSV/Lentivirus Pseudotype | BSL-2 | Luminescence/Fluorescence | High | Safe, High-Throughput, Scalable | Models only viral entry |
Concordance Between Assay Platforms
A critical question for the field is the degree of correlation between results from LVNAs and PVNAs. Extensive comparative studies have demonstrated a strong correlation between the two platforms. A large-scale post-hoc analysis of a clinical trial for a bivalent protein vaccine found that PVNAs exhibited over 90% sensitivity and specificity compared to LVNAs, with accuracy rates reaching 98.8% for the Alpha variant and 94.3% for the Delta variant [64] [65]. The Pearson correlation coefficients for neutralization titers between the two assays were remarkably strong: 0.9614 for Alpha, 0.9517 for Beta, and 0.9072 for Delta [65].
However, it is important to note that while the relative fold-changes in neutralization (e.g., against a new variant) are generally consistent, the absolute titer magnitudes can differ. A comprehensive analysis of 18 datasets revealed that PVNAs and assays using animal model sera (e.g., from hamsters or mice) tend to report higher geometric mean titer (GMT) magnitudes than LVNAs using human sera, though the patterns of immunodominance and antigenic mapping remain consistent [66]. This underscores the importance of using homologous assay systems for comparative studies and being cautious when making direct numerical comparisons across different assay platforms.
Experimental Protocols and Workflows
To ensure reproducibility and generate reliable, comparable data, adherence to detailed experimental protocols is essential. Below are standardized methodologies for key assay types.
Live Virus Microneutralization Assay (MNA) Protocol
The following protocol is adapted from studies validating vaccine immunogenicity [64] [65]:
- Serum Inactivation: Heat-inactivate test serum samples at 56°C for 30 minutes to destroy complement proteins and other heat-labile non-specific antiviral factors.
- Serial Dilution: Perform two-fold serial dilutions of the serum in a cell culture-compatible medium (e.g., DMEM) in a separate dilution plate, typically starting from a 1:8 or 1:10 dilution.
- Virus Incubation: Mix an equal volume of live SARS-CoV-2 virus (e.g., 1000 TCID50/well of the target variant) with each serum dilution. Incubate the virus-serum mixtures for 1-2 hours at 37°C under 5% CO2 to allow antibody-virus binding.
- Cell Infection: Transfer the virus-serum mixtures onto sub-confluent monolayers of permissive cells (e.g., Vero E6) prepared in a 96-well plate 24 hours in advance.
- Incubation and Observation: Incubate the infected cell plates for 3-5 days at 37°C with 5% CO2. Monitor the cells daily for the development of a cytopathic effect (CPE).
- Titer Calculation: The microneutralization titer (MN50) is defined as the reciprocal of the highest serum dilution that protects 50% of the wells from CPE. This is typically calculated using a statistical method such as the Reed-Muench method [64].
Pseudotyped Virus Neutralization Assay (PVNA) Protocol
This protocol, utilizing a VSV pseudovirus backbone, is outlined in recent comparative studies [64] [65]:
- Serum Dilution: Prepare three-fold serial dilutions of the test serum in a culture plate, starting from a 1:30 dilution.
- Virus Mixing: Combine a fixed volume of SARS-CoV-2 spike-pseudotyped virus (e.g., 50μL containing 1000 TCID50) with each serum dilution.
- Cell Seeding and Infection: Add the serum-virus mixtures to host cells (e.g., Huh-7 or HEK293T/ACE2 cells) that have been seeded in advance at a density of 2x10^4 cells per well.
- Incubation: Incubate the plates for a set period (e.g., 24-48 hours) to allow a single round of infection.
- Reporter Detection: Lyse the cells and measure the reporter signal (e.g., luciferase activity as Relative Luminescence Units - RLU).
- Titer Calculation: The half-maximal effective concentration (EC50) titer is defined as the reciprocal serum dilution that neutralizes 50% of the pseudovirus activity. This is calculated by comparing the RLU in test wells to the average RLU in virus control wells (100% infection) and cell-only control wells (background), again using a method like Reed-Muench [64].
The following workflow diagram visualizes the parallel steps and key decision points in these two major assay types:
Diagram 1: Comparative Workflow of LVNA and PVNA
Key Applications and Data Interpretation
Neutralization assays are indispensable for several critical applications in antiviral research and public health.
Quantifying Cross-Variant Neutralization
A primary use of these assays is to profile the efficacy of therapeutic antibodies and vaccine-elicited sera against emerging viral variants. Quantitative data is crucial for tracking antigenic drift and informing countermeasure updates. For example, cell culture assays have been used to systematically profile the loss of neutralizing activity of monoclonal antibodies against Omicron sublineages.
Table 2: Comparative IC50 Values of Monoclonal Antibodies Against SARS-CoV-2 Variants (μg/mL) [63]
| SARS-CoV-2 Variant | Casirivimab | Imdevimab | Sotrovimab (S309) |
|---|---|---|---|
| Wuhan | 0.0139 | 0.0125 | 0.1587 |
| Delta | 0.0217 | 0.0290 | 0.0870 |
| Omicron BA.1 | >10 (Inactive) | >10 (Inactive) | 0.9579 |
| Omicron BA.2 | >10 (Inactive) | 1.2525 | 1.3579 |
As illustrated in Table 2, Omicron subvariants BA.1 and BA.2 show a dramatic loss of sensitivity to certain monoclonal antibodies (e.g., Casirivimab and Imdevimab) compared to the ancestral Wuhan strain, while Sotrovimab retained partial activity [63]. In contrast, antiviral drugs like EIDD-1931 (the active form of Molnupiravir) and Nirmatrelvir showed conserved activity across all variants, highlighting their robustness against viral evolution [63].
Assessing Viral Fitness and Immune Evasion
Beyond simple neutralization sensitivity, these assays can be combined to dissect the mechanisms behind the rise of new variants. For instance, by comparing the replication fitness of recombinant viruses in primary human airway epithelium cells with their sensitivity to neutralization by human sera, researchers can determine whether a variant's success is due to better replication or better immune evasion. This approach was key to understanding the succession of BA.2.86 descendants: the JN.1 variant's rise was primarily driven by immune evasion from the L455S mutation, whereas the subsequent KP.2 and KP.3 variants combined this immune evasion with enhanced replication fitness due to additional mutations like F456L and Q493E [67].
Neutralizing Antibodies as a Correlate of Protection
A critical application is establishing a link between in vitro neutralization titers and in vivo protection (a "correlate of protection"). A comprehensive analysis of 49 nAb studies and 44 VE studies found that while nAb titers strongly correlate with protection against mild infection, protection against severe disease and death often remains high (>75%) even when nAb titers fall to low or barely detectable levels [68]. This crucial finding indicates that while nAbs are a valuable correlate, they are not a perfect predictor, especially for severe outcomes, and that other immune mechanisms (e.g., T-cells, non-neutralizing antibodies with effector functions) play a vital protective role [68] [62]. This underscores the importance of not relying solely on in vitro neutralization data to predict clinical outcomes.
The Scientist's Toolkit: Key Reagents and Materials
The following table details essential reagents and their functions for establishing and performing robust neutralization assays, particularly for SARS-CoV-2.
Table 3: Essential Research Reagent Solutions for Neutralization Assays
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Permissive Cell Lines | Provide the cellular host for viral infection and replication. | Vero E6 [64] [67], Vero E6/TMPRSS2 [66] [63], Calu-3 [66], Huh-7 [64]. Cell type can influence titer results. |
| Reference Sera & mAbs | Serve as positive controls for assay validation and standardization. | WHO International Standard; Human convalescent serum pools; Defined monoclonal antibodies (e.g., Sotrovimab) [66] [63]. |
| Virus Stocks | The infectious agent used to challenge the neutralizing agents. | Live virus (e.g., WA1/2020 strain, variant-specific isolates) [67] [63]; Spike-pseudotyped viruses (VSV-ΔG or Lentivirus backbones) [64] [65]. |
| Detection Reagents | Enable quantification of the infection readout. | Luciferase substrates for PVNAs [64]; Cell viability dyes; Staining antibodies for FRNT/FFRNT (e.g., anti-spike) [67]. |
| Assay-Specific Kits & Buffers | Provide optimized, standardized reagents for specific steps. | Viral RNA extraction kits [69]; One-Step RT-PCR kits (for nPCR detection) [69]; Cell culture media and supplements. |
Neutralization assays provide an indispensable bridge between in vitro research and in vivo efficacy for antiviral countermeasures. The choice between live virus and pseudotyped assays is not a matter of identifying a single superior option, but rather of selecting the most appropriate tool for the research question at hand, while carefully considering biosafety, throughput, and biological context. As the comparative data shows, different assay formats can yield strongly correlated results, enabling flexible and scalable research pipelines. However, scientists must remain cognizant of the limitations and nuances of their chosen platform, particularly when interpreting absolute titer values or extrapolating results to clinical protection. The ongoing refinement of these assays, coupled with a more integrated understanding of how in vitro neutralization data complements other immunological parameters, will continue to accelerate the development of vaccines and therapeutics against existing and emerging viral threats.
Enhancing Assay Performance: Troubleshooting Common Pitfalls and Optimization Strategies
In vitro viral infectivity testing serves as a cornerstone of virology research, vaccine development, and therapeutic discovery. The reliability of these assays hinges on the meticulous control of cell culture conditions, where subtle variations can significantly alter experimental outcomes. Three critical variables—cell confluence, passage number, and host cell receptors—directly impact cellular physiology, viral entry mechanisms, and ultimately, the accuracy and reproducibility of infectivity data. This guide systematically compares the effects of these variables across different experimental contexts, providing structured data and methodologies to help researchers standardize protocols, minimize variability, and enhance cross-study comparisons in viral research.
Cell Confluence: Effects on Cell Behavior and Viral Studies
Cell confluence refers to the percentage of surface area covered by adherent cells in a culture vessel. It is a critical parameter influencing cellular metabolism, differentiation, and susceptibility to viral infection.
Quantitative Effects of Confluence on Cell Differentiation
Table 1: Effects of High Confluence on Spontaneous Differentiation in Mesenchymal Stem Cells (MSCs)
| Cell Type | Confluence Level | Differentiation Type | Key Upregulated Markers | Effect on Other Lineages | Reference |
|---|---|---|---|---|---|
| Adipose-derived MSCs (ADSCs) | 80% for 7 days | Neurogenic | TUBB3, MAP2, NEFM, NEFH, NEFL, NGF, BDNF, GDNF | No spontaneous adipogenic or osteogenic differentiation | [70] |
| Bone Marrow-derived MSCs (BMSCs) | 80% for 7 days | None | No significant changes observed | No spontaneous adipogenic or osteogenic differentiation | [70] |
Experimental Protocol: Confluence-Initiated Differentiation
Methodology for Assessing Confluence Effects:
- Cell Culture: Human ADSCs at passages 3-5 are cultured in DMEM with 10% FBS until reaching 80% confluence [70].
- Maintenance Phase: Cells are maintained in DMEM supplemented with 1% FBS for 7 days without inducing factors [70].
- Analysis: Differentiated cells are analyzed using RT-qPCR for neurogenic markers (TUBB3, MAP2) and neurotrophins (NGF, BDNF, GDNF), with confirmation via immunofluorescent staining [70].
Confluence Measurement Techniques
Table 2: Methods for Quantifying Cell Confluency
| Method | Principle | Advantages | Limitations | |
|---|---|---|---|---|
| Visual Estimation | Microscopic examination by researcher | Rapid, no specialized equipment | Subjective, high variability (≥10% difference between researchers) | [71] |
| Automated Image Analysis (e.g., EVOS M3000) | Algorithm-based thresholding and edge detection | Objective, consistent, quantitative data | Requires specialized imaging equipment | [71] |
Passage Number: Genetic and Functional Consequences
Passage number represents the number of times cells have been subcultured, reflecting their "age" in culture. High passage numbers can induce genetic instability, phenotypic drift, and altered response to stimuli.
Documented Effects of Passage Number on Cell Characteristics
Table 3: Passage Number Effects Across Different Cell Lines
| Cell Line | Passage Comparison | Observed Changes | Functional Consequences | |
|---|---|---|---|---|
| MIN-6 mouse insulinoma | P18 vs P40 | ~1,000 genes differentially expressed | Altered differentiation state, changes in regulated secretion, adhesion, proliferation | [72] |
| LNCaP prostate cancer | P25 vs P60 | Altered PI3K/Akt pathway regulation | Changes in androgen receptor activity relevant to cancer progression | [72] |
| D1 multipotent bone marrow stromal | P4 to P34 | Fluctuating osteogenic marker expression (peak at P4, P24); increased doubling time after P26 | Variable differentiation capacity; reduced proliferation at high passages | [73] |
| Caco-2 (colonic epithelial) | P22 to P30 (recommended) | Maintained differentiation properties | Consistent model for host-microbe interactions | [74] |
Experimental Protocol: Monitoring Passage Effects
Methodology for Tracking Passage-Dependent Changes:
- Cell Culture: D1 cells are serially passaged from P3 to P34, with samples collected every five passages [73].
- Growth Kinetics: Cell doubling rates are calculated at each passage using a cell counter or automated system like Millipore Sceptor Sensor [73].
- Differentiation Markers: Alkaline phosphatase activity (osteogenic) and triglyceride accumulation (adipogenic) are measured spectrophotometrically and normalized to DNA content (PicoGreen assay) [73].
- Gene Expression: RNA is extracted using Trizol reagent and analyzed via RT-qPCR for markers including ALP, RunX2, osteocalcin (osteogenic), and AP2 (adipogenic) [73].
Best Practices for Passage Number Documentation
- Consistent Tracking: Record passage numbers on all culture vessels and cryovials [75].
- Source Verification: Obtain cells from reputable sources that provide initial passage numbers [72].
- Freezing Strategy: Create low-passage master cell banks early to maintain consistent experimental material [75].
- Defined Limits: Establish laboratory-specific passage number limits based on cell behavior and experimental requirements [75].
Host Cell Receptors: Gatekeepers of Viral Infectivity
Host cell receptors are specific surface molecules that mediate viral attachment and entry, determining tissue tropism and species specificity. Understanding these interactions is fundamental to predicting viral behavior and developing targeted therapies.
Viral Receptors and Their Roles in Infection
Table 4: Host Cell Receptors in Viral Infection Models
| Virus Type | Host Cell Model | Key Receptors/Cofactors | Experimental Significance | |
|---|---|---|---|---|
| HIV-1 | CD4+ T cells, macrophages | Capsid interaction with FG-nucleoporins (Nup153, Nup358) | Critical for nuclear import in non-dividing cells; target for capsid inhibitors like lenacapavir | [76] |
| HIV-1 | CD4+ T cells | CPSF6 and LEDGF/p75 (liquid-liquid phase-separated condensates) | Guides integration to transcriptionally active genomic regions | [76] |
| Salmonella enterica | Differentiated Caco-2 cells | Multiple host receptors identified via cross-linking | Method for discovering unknown host-microbe receptor/ligand pairs | [74] |
| Influenza A virus | MDCK cells | Sialic acid receptors (for entry); viral polymerase targets (for replication) | Model system for anti-influenza drug screening (e.g., thymol, limonin) | [9] |
Experimental Protocol: Identifying Host-Microbe Receptor/Ligand Pairs
Whole Cell Cross-Linking Method for Receptor Discovery:
- Cell Culture: Differentiated Caco-2 cells (passages 22-30) are grown for 14 days post-confluence to ensure complete differentiation [74].
- Bacterial Preparation: Pathogenic or probiotic bacteria are cultured under standard conditions.
- Cross-Linking: Sulfo-SBED reagent (NHS-ester moiety) covalently links proteins within 9-12 Å after photoactivation, creating covalent bonds between interacting host and microbial surface proteins [74].
- Isolation and Identification: Biotinylated complexes are purified using streptavidin affinity capture, followed by mass spectrometry analysis to identify cognate receptor-ligand pairs [74].
- Validation: Putative interactions are confirmed through receptor-blocking antibodies or bacterial ligand deletion mutants in infection assays [74].
Advanced Techniques for Viral Infectivity Assessment
Automated Viral Infectivity Assay (AVIATM):
- Principle: Uses convolutional neural networks (CNNs) and high-throughput brightfield microscopy to quantify infection phenotypes in 96-well plates within hours, without manual sample preparation [26].
- Applications: Validated with HIV, influenza A virus, coronavirus 229E, vaccinia viruses, poliovirus, and adenoviruses [26].
- Advantages: Earlier detection than conventional plaque or TCID50 assays (2-7 days), with precision of ∼10% and comparable or better sensitivity ranges [26].
Integrated Experimental Design: Controlling Multiple Variables
Successful viral infectivity assays require simultaneous management of confluence, passage number, and receptor expression. The following workflow integrates control strategies for these variables.
Comprehensive Experimental Workflow
Research Reagent Solutions for Viral Infectivity Studies
Table 5: Essential Research Reagents and Their Applications
| Reagent/Cell Line | Function in Viral Studies | Key Characteristics | |
|---|---|---|---|
| Caco-2 cells (ATCC HTB-37) | Model for intestinal epithelial infection & host-microbe interactions | Require 14-day post-confluence differentiation; use passages 22-30 | [74] |
| MDCK cells (ATCC CCL-34) | Influenza A virus propagation & infectivity assays | Sensitive to confluence effects; standard for plaque assays | [9] |
| Vero E6 cells (ATCC CRL-1586) | SARS-CoV-2 propagation & antiviral screening | Permissive for coronavirus infection; used in cytotoxicity assays | [9] |
| Sulfo-SBED cross-linker | Identification of host-microbe receptor/ligand pairs | NHS-ester moiety links proteins within 9-12 Å; enables covalent cross-linking | [74] |
| Automated systems (e.g., EVOS M3000) | Objective confluency measurement & analysis | Reduces subjectivity in confluence assessment; integrates imaging and analysis | [71] |
The systematic control of cell culture variables represents a critical frontier in improving the reproducibility and reliability of viral infectivity research. Confluence directly impacts cellular differentiation states and metabolic activity, passage number influences genetic stability and phenotypic consistency, while host cell receptors determine viral tropism and infection efficiency. By implementing the standardized protocols, quantitative assessment methods, and integrated workflows outlined in this guide, researchers can significantly reduce experimental variability. The future of comparative viral studies depends on our ability to recognize these variables as interconnected components of experimental design rather than isolated parameters, ultimately strengthening the translational potential of in vitro findings to clinical applications.
Optimizing Viral Inoculum and Adsorption Conditions
Viral infectivity assays are foundational tools in virology, essential for developing viral vaccines, antiviral therapies, and manufacturing biologicals [26]. These assays measure the concentration of infectious virus particles in a sample, providing critical data for downstream research and development. The precision and efficiency of these assays are paramount, as they influence everything from experimental conclusions to patient dosing in clinical applications [77]. This guide provides a comparative analysis of established and emerging methodologies for optimizing viral inoculation and adsorption, a critical phase where the virus first interacts with host cells. The adsorption phase governs the subsequent fate of the virus, influencing its infectivity, stability, and detectability [78]. We objectively compare the performance of traditional assays against modern, high-throughput alternatives, providing the experimental data and protocols necessary for researchers to select and optimize the most appropriate method for their needs.
Comparative Analysis of Viral Infectivity Assays
The following table summarizes the core characteristics, performance metrics, and optimal use cases for the key infectivity assays discussed in this guide.
Table 1: Comparison of Viral Infectivity Assay Methods
| Assay Method | Principle of Detection | Typical Assay Duration | Key Advantages | Key Limitations & Variability |
|---|---|---|---|---|
| Plaque Assay | Formation of localized lytic zones (plaques) in a cell monolayer under a viscous overlay. | 2-7 days [26] | Considered a gold standard; direct visualization of infectivity; allows for plaque purification. | Low throughput; technically demanding; long incubation; subjective counting; variability ~±0.5 log10 [77]. |
| TCID50 Assay | Endpoint dilution determining the dose at which 50% of inoculated cultures show infection, based on CPE. | 5-10 days [79] | Does not require an overlay; adaptable to many virus-cell systems; statistical robustness. | Lower precision; binary (yes/no) endpoint; long incubation; subjective CPE assessment; variability ~±0.5 log10 [77]. |
| Automated TCID50 | Same as TCID50 but with automated liquid handling and bright-field imaging for CPE analysis. | ~4x faster than manual TCID50 [77] | High standardization; increased throughput and speed; reduced operator-dependent variability. | Requires investment in automation and imaging equipment. |
| Kinetic Infectivity Titer (KIT) Assay | Kinetic imaging of infection-induced morphological changes (e.g., cell rounding) relative to a standard curve. | ~24 hours [77] | Very high throughput (~400 samples/week); high precision (CV < 20%); stability-indicating; results in 24h [77]. | Requires imaging equipment and analysis software; optimization needed for new virus-cell pairs. |
| AI-Based Infectivity Assay | Convolutional Neural Networks (CNNs) trained on infection phenotypes in label-free bright-field images. | Within hours [26] | Rapid results; high sensitivity and precision (~10%); broad-spectrum potential for virus characterization [26]. | Requires significant AI model training and computational resources. |
Detailed Experimental Protocols
Traditional TCID50 Assay Protocol
The TCID50 (Tissue Culture Infectious Dose 50) assay remains a widely used endpoint dilution method for quantifying viral infectivity [79] [77].
- Cell Culture Preparation: Begin by seeding adherent host cells (e.g., Vero E6, MRC-5, A549) into 96-well tissue culture plates. The choice of cell line is critical and must be permissive to the virus under investigation [80] [79]. Grow the cells until they form a confluent, healthy monolayer.
- Viral Inoculum Preparation and Adsorption: Serially dilute the virus sample in a maintenance medium (e.g., DMEM supplemented with 1-2% serum) across a wide range, typically using 10-fold dilutions. Remove the growth medium from the cell plates and inoculate multiple wells (typically 6-12) per dilution with a fixed volume of the viral diluent. Include control wells with maintenance medium only. The adsorption phase is critical: incubate the inoculated plates at 37°C in a 5% CO2 atmosphere for a defined period (usually 1-2 hours) to allow for viral attachment and entry. Gently rocking the plates every 15-20 minutes can enhance adsorption efficiency. After adsorption, remove the inoculum to minimize non-specific cytotoxicity and add fresh maintenance medium.
- Incubation and Endpoint Determination: Incubate the plates for the duration required for the virus to produce a visible cytopathic effect (CPE), which can take 5-10 days [79]. Score each well microscopically for the presence or absence of CPE.
- Titer Calculation: The TCID50/mL titer is calculated using the statistical method of Spearman-Kärber or Reed-Muench [77].
Kinetic Infectivity Titer (KIT) Assay Protocol
The KIT assay is a modern approach that leverages kinetic, label-free imaging to drastically reduce assay time and increase throughput [77].
- Cell Seeding and Preparation: Seed appropriate host cells (e.g., BHK-21 for VSV-GP) in multi-well plates (e.g., 96-well) and culture until a suitable confluence is achieved.
- Viral Inoculation and Adsorption: Infect the cell monolayers with serial dilutions of the virus sample. A reference standard with a known titer should be included on each plate to generate a standard curve. The adsorption conditions (time, temperature, medium composition) should be optimized for the specific virus-cell system. Following adsorption, the inoculum is replaced with fresh medium.
- Kinetic Image Acquisition: Immediately after infection, place the plate in an automated, label-free bright-field imaging plate reader. Acquire images of the entire plate at regular intervals (e.g., every 2-4 hours) for 24-48 hours.
- Image Analysis and Titer Determination: Use image analysis software to quantify infection-induced morphological changes, such as the proportion of rounded cells. The software generates a dose- and time-dependent curve of the percentage of rounded cells. The cumulative kinetic data is then fitted to a model, and the infectious titer of unknown samples is determined by interpolation from the standard curve, yielding results within 24 hours post-infection with high precision (CV < 20%) [77].
Workflow and Pathway Visualizations
High-Throughput Infectivity Assay Workflow
The following diagram illustrates the integrated workflow of a high-throughput infectivity assay, combining automated liquid handling, kinetic imaging, and advanced data analysis.
Virus Adsorption and Coadsorption Modeling
This diagram outlines the logical process of quantifying virus adsorption and coadsorption behavior using advanced spectroscopic techniques and modeling, which is crucial for understanding complex real-world samples.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Viral Infectivity and Adsorption Studies
| Item | Function & Application in Viral Assays |
|---|---|
| Cell Lines (Vero E6, MRC-5, A549, BHK-21, RAW264.7) | Provide a susceptible host system for viral replication. Different lines have varying permissiveness to different viruses, making selection critical [80] [79] [42]. |
| Culture Media & Supplements (DMEM, Fetal Bovine Serum, Antibiotics) | Supports cell health and viability during the assay. Serum concentration is often reduced during viral adsorption and incubation to minimize interference [78] [81]. |
| Viral Transport Medium (VTM) | Preserves viral infectivity during sample storage and transport, typically containing buffered salts, protein stabilizers, and antibiotics [79]. |
| Functionalized Substrates (SiO₂-coated Silver Nanorods, Glass Wool) | Used to study virus-surface interactions or to concentrate viruses from samples. Surface charge and chemistry critically impact adsorption efficiency [78] [82]. |
| Elution Buffers (e.g., Glycine-Beef Extract, High pH) | Used to recover viruses adsorbed to concentration filters; efficiency depends on pH and composition, especially for enveloped viruses [82]. |
| Automated Imaging Systems | Enable high-throughput, kinetic acquisition of label-free bright-field images for assays like KIT, tracking morphological changes in infected cells [77]. |
| Surface-Enhanced Raman Scattering (SERS) Substrates | Enable label-free, sensitive spectroscopic investigation of virus adsorption and coadsorption behavior on surfaces for quantitative modeling [78]. |
The field of viral infectivity testing is evolving from traditional, slow, and labor-intensive methods toward highly automated, rapid, and information-rich assays. While the plaque and TCID50 assays remain foundational for their direct simplicity, modern approaches like the Kinetic Infectivity Titer (KIT) assay and AI-based methods offer transformative advantages in throughput, precision, and speed, which are crucial for pharmaceutical development and advanced research. Furthermore, a deep understanding of viral adsorption, particularly in complex, physiologically relevant matrices like saliva and in the context of mixed infections, is essential for developing accurate diagnostic and sensing platforms [78] [42]. The optimal choice of method depends on the specific research question, required throughput, available resources, and the need for a viable viral isolate.
Overcoming Challenges with Low-Titer or Fastidious Viruses
In virology research and drug development, investigators frequently encounter two significant categories of challenges: viruses that propagate to low concentrations (low titer) and those with demanding growth requirements (fastidious). These characteristics substantially impede research on coronaviruses, human immunodeficiency virus (HIV), and various enteric pathogens, complicating efforts in basic research, vaccine development, and therapeutic discovery. Low-titer viruses yield insufficient material for robust experimentation, while fastidious viruses resist cultivation in standard cell lines or require highly specialized conditions. Successfully overcoming these hurdles necessitates a comprehensive understanding of the factors affecting viral stability and the implementation of advanced, sensitive detection methodologies. This guide objectively compares current approaches and provides the experimental data and protocols necessary for researchers to optimize their work with these challenging pathogens.
Comparative Analysis of Viral Persistence and Assay Sensitivity
Environmental Stability of Coronaviruses
The persistence of viral infectivity on environmental surfaces is a critical factor in transmission risk assessment and procedural planning. Recent research using human beta-coronavirus OC43 as a surrogate for SARS-CoV-2 has quantified its remarkable stability on non-porous stainless steel surfaces under varying conditions [83].
Table 1: Persistence of HCoV-OC43 on Stainless Steel Surfaces
| Mucin Concentration | Absolute Humidity (14.4 g/m³) | Absolute Humidity (3.04 g/m³) |
|---|---|---|
| 3% (High) | Up to 14 days | Remained infectious throughout 22-day test |
| 0.3% (Low) | Up to 3 days | Remained infectious throughout 22-day test |
| 0% (None) | Up to 2 days | Remained infectious throughout 22-day test |
Data adapted from PMC12502581 [83]
The experimental data reveal two crucial findings for researchers: first, the presence of bodily fluids like mucin in artificial saliva dramatically extends viral infectivity, particularly at higher absolute humidity; second, lower absolute humidity conditions (3.04 g/m³ at 18°C/20% RH) can preserve coronavirus infectivity for extended periods exceeding three weeks, regardless of matrix composition [83]. These findings have profound implications for laboratory safety protocols and the handling of potentially contaminated materials.
Comparative Sensitivity of Viral Detection Methods
Accurately detecting infectious virus particles, especially at low concentrations, is fundamental to working with low-titer viruses. Traditional and advanced methods vary significantly in their sensitivity, speed, and ability to distinguish infectious versus non-infectious particles.
Table 2: Comparison of Viral Infectivity Detection Methods
| Method | Principle | Time to Result | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Cell Culture CPE (TCID₅₀) | Microscopic scoring of cytopathic effect in infected cells | 5-14 days | Gold standard for infectivity | Subjective; delayed for slow-growing viruses |
| Integrated Cell Culture qPCR (ICC-qPCR) | Cell culture followed by RT-qPCR to detect replicative virus | 2-7 days | 100x more sensitive than CPE for some coronaviruses; detects replicative virus | More complex workflow |
| Metagenomic NGS (mNGS) | Unbiased sequencing of all nucleic acids in a sample | 3-8 days | Agnostic detection; no pathogen-specific primers needed | High cost; cannot distinguish infectious from non-infectious |
| RT-qPCR Alone | Detection of viral RNA | 1-2 days | Rapid and highly sensitive | Cannot distinguish infectious from non-infectious virus |
Data synthesized from PMC12502581 and PMC7106513 [83] [84]
For human coronavirus OC43, the ICC-RT-qPCR assay demonstrated detection at titers as low as 0.5 TCID₅₀/mL after a 5-day post-infection period, which was both more sensitive and two days faster than CPE-based cell culture alone [83]. Similarly, for other fastidious viruses like human noroviruses that lack reliable cell culture systems, mNGS has proven valuable, identifying novel and unexpected pathogens in clinical samples from patients with central nervous system infections [85].
Experimental Protocols for Enhanced Detection and Culture
ICC-qPCR for Sensitive Detection of Infectious Coronavirus
The Integrated Cell Culture quantitative PCR (ICC-qPCR) protocol combines the infectivity determination of cell culture with the sensitivity of molecular detection.
Protocol:
- Cell Culture Preparation: Grow HRT-18G cell monolayers (ATCC CRL-11663) in 96-well plates to 90-95% confluency using Dulbecco's Modified Eagle Medium (DMEM) supplemented with 3% FBS, 1% penicillin-streptomycin, and 1% sodium pyruvate [83].
- Sample Inoculation: Inoculate cell monolayers with serial dilutions of the viral sample. Include appropriate negative controls.
- Incubation: Incubate inoculated cells at 37°C with 5% CO₂ for 5-7 days to allow viral replication [83].
- Nucleic Acid Extraction: Extract total nucleic acid from the cell culture supernatant.
- RT-qPCR Analysis: Perform reverse transcription quantitative PCR using pathogen-specific primers and probes.
- Interpretation: A positive RT-qPCR signal indicates the presence of replicative virus, confirming infectivity in the original sample.
This method is particularly valuable for detecting low levels of infectious virus that may not produce visible CPE and for confirming negative results in CPE-based assays [83] [84].
Optimized Propagation for Low-Titer Virus Production
Generating sufficient titer of viral vectors for gene therapy or research can be challenging with toxic transgenes. The following troubleshooting protocol addresses common low-titer issues.
Protocol:
- Vector Design Check:
- Verify that the insert size does not exceed the viral vector's carrying capacity.
- Check for high GC content (>70% over >100 bases) and ensure the integrity of inverted terminal repeats (ITRs) in AAV vectors [86].
- Promoter Optimization:
- If the transgene is suspected of being toxic to packaging cells (e.g., pro-apoptotic genes like BAX, NEK1), replace strong promoters with weaker or tissue-specific promoters.
- For an AAV vector carrying the toxic gene Foxn1, switching from a strong to a medium-strength promoter increased total yield from ~10¹¹ vg to ~10¹² vg, comparable to a non-toxic EGFP control [86].
- Packaging System Validation:
- Ensure compatibility between transfer plasmids and packaging plasmids (e.g., 2nd gen transfer plasmids require 2nd gen packaging systems).
- Use healthy, low-passage packaging cells to maximize transfection efficiency [86].
- Harvest Optimization:
- Determine the optimal harvest time point empirically.
- Consider collecting both supernatant and cell pellet, as some viruses are released differentially [86].
Diagram: Troubleshooting Workflow for Low-Titer Viral Vector Production
The Scientist's Toolkit: Essential Research Reagents
Successfully working with low-titer and fastidious viruses requires specific biological materials and reagents optimized for these challenging applications.
Table 3: Essential Research Reagents for Challenging Viruses
| Reagent / Material | Function | Application Example |
|---|---|---|
| HRT-18G Cell Line (ATCC CRL-11663) | Propagation host for human coronaviruses | Significantly improves HCoV-OC43 cultivation and assay sensitivity compared to standard lines [83] |
| Mucin-based Artificial Matrices | Mimics bodily fluid composition for stability studies | Evaluates the protective effect of respiratory secretions on viral persistence on surfaces [83] |
| Broadly Neutralizing Antibodies (e.g., b12) | Probes for studying virus-antibody interactions and escape mutations | Demonstrates that even low titers (IC₅₀ 1:5) can select for HIV-1 escape variants in vivo [87] |
| Species-Specific Pathogen-Free (SPF) Chicken Eggs | Propagation host for influenza and other viruses | Essential for isolating and growing clinical strains that do not adapt readily to cell culture [88] |
| DNase Treatment Reagents | Reduces host background in mNGS samples | Critical for improving the signal-to-noise ratio in metagenomic sequencing from clinical samples [85] |
Overcoming the challenges posed by low-titer and fastidious viruses demands an integrated approach combining optimized culture conditions, highly sensitive detection methodologies, and appropriate biological systems. Key comparative findings indicate that ICC-qPCR offers superior sensitivity over traditional CPE-based methods for detecting infectious virus, while environmental factors like humidity and the presence of organic matter significantly impact viral stability. For viral vector production, strategic promoter selection and vector design are critical for achieving usable titers of toxic transgenes. By implementing these evidence-based protocols and utilizing the appropriate research tools, scientists can significantly advance their research on even the most challenging viral pathogens, thereby accelerating the development of novel vaccines and antiviral therapeutics.
In virology and drug development, the integrity of in vitro research hinges on robust contamination controls. Viral infectivity testing, used to evaluate antiviral drugs and disinfectants, is particularly vulnerable to methodological errors and environmental contamination, which can compromise data validity and lead to erroneous conclusions. This guide provides a comparative analysis of the core techniques and validation controls essential for mitigating these risks, framing them within the context of reproducible viral research. We objectively compare the performance of different aseptic methods and viral quantification assays, supported by experimental data, to establish a framework for reliable scientific outcomes.
Comparative Analysis of Core Aseptic Techniques
Aseptic technique is not a single protocol but a spectrum of practices designed to minimize microbial contamination. The appropriate choice depends on the specific procedure and the associated infection risk to the patient or the experiment. The following table compares the primary techniques used in clinical and laboratory settings.
Table 1: Comparison of Core Aseptic Techniques
| Technique | Key Principle | Typical Applications | Key Performance Differentiators |
|---|---|---|---|
| Surgical Asepsis [89] | Maintains complete sterility of all instruments and surfaces in the field. | Major surgical procedures, insertion of surgical implants or central venous catheters [89]. | Highest level of sterility; requires sterile gowns, gloves, and drapes; all instruments must be sterile. |
| Standard Aseptic Technique (Clean Technique) [89] | Reduces, rather than completely eliminates, the presence of pathogens. | Simple wound dressings, intramuscular injections, venipuncture [89]. | Prioritizes hand hygiene and clean gloves over full sterility; balances infection risk with practicality. |
| Aseptic Non-Touch Technique (ANTT) [90] [89] | Avoids touching any key, sterile "critical sites" (e.g., syringe tips, catheter hubs) with hands or non-sterile equipment. | Intravenous therapy, catheter care, and patient self-administration of home parenteral support [90]. | Focuses on protecting critical parts; can be as effective as sterile techniques with significantly reduced training time and cost [90]. |
Performance Data in Training and Application
A 2025 cohort study directly compared traditional sterile/aseptic technique with Standard-ANTT for training patients and caregivers in managing home parenteral support. The results demonstrate significant practical advantages for ANTT [90]:
- Training Time: The mean time to train individuals to independence was 85 hours for the traditional aseptic technique group, compared to just 8 hours for the Standard-ANTT group—a 66% reduction.
- Infection Outcomes: While not statistically significant in this study's sample size, a lower risk of catheter-related bloodstream infections (CRBSI) was observed. The traditional technique group had three CRBSI episodes, whereas the Standard-ANTT group had zero [90].
This evidence suggests that for specific clinical applications, Standard-ANTT is not only safer and more efficient to teach but may also lead to superior patient outcomes.
Viral Infectivity Testing: Methods & Validation Controls
Accurate quantification of infectious viral particles is fundamental to virology research, from evaluating antiseptics to studying viral pathogenesis. The following section compares common viral quantification methods and the critical validation controls needed to ensure their accuracy.
Comparison of Viral Quantification Methods
Different methods provide different types of data, ranging from direct quantification of infectious units to indirect detection of viral components.
Table 2: Comparison of Key Viral Quantification and Detection Methods
| Method | What It Measures | Key Performance Metrics | Advantages & Limitations |
|---|---|---|---|
| Plaque Assay [2] [91] | Number of infectious viral particles forming plaques (lytic areas) on a cell monolayer. | Plaque-forming units per mL (PFU/mL); considered a gold standard for infectivity. | Advantage: Direct measure of infectious virus. Limitation: Time-consuming (several days), requires cell culture. |
| 50% Tissue Culture Infectious Dose (TCID₅₀) [92] [91] | The dilution at which 50% of inoculated cell cultures show viral cytopathic effect (CPE). | Log10 TCID50/mL; calculated using an endpoint dilution formula. | Advantage: More sensitive than plaque assays; useful for viruses that do not form clear plaques. Limitation: Less precise; requires careful statistical analysis. |
| Quantitative PCR (qPCR) [2] [93] | Concentration of viral genomic material (RNA/DNA). | Cycle threshold (Ct) value; copies/µL. | Advantage: Extremely fast, sensitive, and specific. Limitation: Cannot distinguish between infectious and non-infectious viral particles. |
| Immunofluorescence Assay (IFA) [2] | Presence and location of viral proteins within infected cells. | Visual detection of fluorescently-labeled viral antigens. | Advantage: Confirms active viral replication and provides spatial data. Limitation: Semi-quantitative; requires specific antibodies and expertise. |
Validation Controls for Virucidal Testing
When testing the efficacy of antiseptics and disinfectants (ATS-D), stringent controls are mandatory to attribute any reduction in viral titer to the product's activity and not methodological artifacts. The following workflow and descriptions outline the critical steps and controls involved.
Diagram 1: Workflow for evaluating virucidal activity of chemical agents with key validation controls. A log10 reduction of ≥4 is required for a "virucidal" claim in Europe [92] [91].
- Virus Control: This control determines the initial titer of the virus stock without any disinfectant present. It is essential for calculating the final log10 reduction and for verifying that the neutralization and recovery methods themselves do not unduly reduce the viral titer [92] [91].
- Cytotoxicity Control: The test product or neutralizer residues can be toxic to the cell culture used for virus titration, causing cell death that can be mistaken for viral cytopathic effect (CPE). This control checks for this by adding the neutralized product to cells in the absence of virus [92] [91].
- Neutralization Efficacy Control: It is critical to demonstrate that the neutralization method (e.g., gel filtration, chemical neutralizers) instantly stops the action of the disinfectant at the end of the contact time. Without this, the product could continue to inactivate the virus during the titration step, leading to an overestimation of its potency [92]. Gel-filtration, for instance, works by separating small disinfectant molecules from larger viral particles [92].
Key Experimental Protocol: Quantitative Suspension Test for Virucidal Activity
This protocol, adapted from standardized methods, is used to evaluate the virucidal activity of chemical agents in suspension [92].
Methodology:
- Preparation: Sterilize all components. Prepare Sephadex gel-filtration columns for neutralization. Adjust all reagents and the virus suspension to the test temperature (e.g., 20°C).
- Test Mixture: For each contact time and concentration, combine one part virus suspension with one part interfering substance (e.g., fetal calf serum to simulate organic load) and eight parts of the test disinfectant at 1.25x the desired final concentration [92] [91].
- Contact and Neutralization: After the precise contact time (e.g., 0.5, 1, 5 minutes), immediately stop the reaction by passing the mixture through a Sephadex column or adding a chemical neutralizer.
- Titration: Titrate the recovered virus from the filtrate using an end-point dilution method (TCID₅₀) on susceptible cell monolayers (e.g., L-132 cells for human coronavirus 229E). Include virus control titrations (virus + water instead of disinfectant) for comparison [92].
- Calculation and Interpretation: The virucidal activity is expressed as the log10 reduction in viral titer compared to the virus control. A product is considered efficacious if it achieves a ≥4 log10 reduction (a 99.99% reduction) under dirty (with protein load) and clean conditions, as per European standards [92] [91].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful viral infectivity testing relies on a suite of specialized reagents and materials. The following table details key solutions and their functions in the context of the described protocols.
Table 3: Essential Research Reagents and Materials for Viral Infectivity and Virucidal Assays
| Item | Function/Application | Key Considerations |
|---|---|---|
| Sephadex G-10/G-25 Gel [92] | Gel-filtration matrix for neutralization; separates disinfectant molecules from viral particles. | Choice of Sephadex type depends on the molecular mass of the test disinfectant [92]. |
| Fetal Calf Serum (FCS) [91] | Used as a standardized "interfering substance" or protein load to simulate dirty conditions in disinfectant testing. | A final concentration of 10% FCS is standard to challenge the disinfectant's efficacy under organic load [91]. |
| Cell Cultures (e.g., L-132, standard fibroblast lines) [92] [2] | Host systems for propagating test viruses and performing infectivity titrations (TCID₅₀, plaque assays). | Susceptibility to the target virus is critical. Immortalized cell lines are preferred for ease of culture and reproducibility [2]. |
| Plaque Assay Agar Overlay | Immobilizes viruses to prevent secondary infection, allowing discrete plaque formation for counting. | Concentration must be optimized to be firm enough to restrict diffusion but permit nutrient passage to cells. |
| TaqMan Probes & Master Mix [93] | For specific and sensitive detection of viral genomes via qPCR. Enables multiplex detection of several viruses in one reaction. | Primers and probes must be highly specific to the target virus. Multiplexing requires careful design to ensure no cross-reactivity [93]. |
| Water of Standardized Hardness (WSH) [91] | Diluent for preparing disinfectant solutions to ensure consistency and reproducibility between tests. | The ionic composition of water can significantly influence disinfectant activity, making standardization critical [91]. |
Mitigating contamination in viral research is a multi-faceted endeavor. The choice of aseptic technique, from the highly stringent surgical asepsis to the efficient ANTT, directly impacts procedural safety and training efficacy. For viral infectivity testing, the selection of an appropriate quantification method—whether to measure infectious titer or simply detect presence—must be guided by the research question. Ultimately, the validity of this data rests on a foundation of rigorous validation controls, including virus, cytotoxicity, and neutralization efficacy controls. Adherence to these standardized protocols and controls, as outlined in this guide, ensures the generation of reliable, reproducible, and defensible data that is crucial for advancing both basic virology and applied drug development.
In the field of comparative viral infectivity testing, the accuracy of quantitative results hinges on the rigorous application of normalization strategies. Normalization is defined as the process of returning something to a normal condition or state, and in system-wide -omics analysis, it aims to account for bias or errors—systematic or otherwise—to make samples more comparable [94]. For researchers, scientists, and drug development professionals, selecting the appropriate normalization technique is not merely a statistical formality but a fundamental prerequisite for deriving biologically meaningful conclusions from in vitro experimental data. The central challenge lies in differentiating true biological changes, such as those induced by viral infection or therapeutic intervention, from technical artifacts introduced during experimental processing. This guide provides a comparative analysis of normalization methodologies, enabling virologists to make informed decisions that enhance the robustness and reproducibility of their infectivity assays.
Core Normalization Strategies: A Comparative Framework
Multiple normalization strategies have been developed to address different types of bias that can occur throughout the experimental process. These can be broadly categorized into strategies applied during experimental design and sample handling, and those applied post-acquisition during data analysis [94].
Cellular Normalization Strategies
Before nucleic acid or protein extraction, accurate cellular normalization is crucial. The goal is to ensure that comparisons are made from equivalent biological starting material. The table below compares common cellular normalization techniques used in virology research.
Table 1: Comparison of Cellular Normalization Methods for Viral Infectivity Assays
| Method | Principle | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Cell Counting (Hemocytometer) [94] | Manual estimation of cell number per volume. | Cost-effective; widely applicable to homogenous cell cultures. | Simple, requires no specialized equipment. | Low sampling size; subjective; does not account for viability or cell size variability. |
| Optical Density (OD600) [94] | Measures light scattering proportional to cell number. | Standard for microbial culturing; high-throughput screening. | Rapid and non-destructive. | Bias from fluorescent proteins; estimates cell abundance, not absolute number; ignores viability. |
| Flow Cytometry with Counting Beads [94] | Absolute cell counting using fluorescent beads as an internal standard. | Complex/heterogeneous samples (e.g., co-cultures, PBMCs). | High accuracy; can differentiate cell types. | Requires single-cell suspension; expensive; high technical expertise needed. |
| Proteomic Ruler [94] | Uses MS signal of histone peptides, proportional to DNA mass, to predict protein copies per cell. | Absolute quantification of viral or host proteins in infected cells. | Exploits inherent biological relationship; does not require pre-lysis counting. | Assumes known ploidy; influenced by S-phase subpopulation; less effective for complex tissues. |
| Metabolomic DNA Normalization [94] | Normalizes metabolite levels to genomic DNA copy number. | Metabolomic studies of virus-infected cells. | Accounts for biomass in samples where cell counting is difficult. | Requires known genome size and ploidy; problematic for polyploid systems. |
Data-Driven Normalization for 'Omics' Technologies
Following data acquisition, computational normalization methods are applied to correct for technical variation. In transcriptomics, for instance, the choice of method depends on the technology (e.g., RNA-seq) and the specific biases present.
Table 2: Comparison of Post-Acquisition Data Normalization Methods
| Method | Category | Technical Principle | Impact on Coexpression Accuracy [95] |
|---|---|---|---|
| Counts Per Million (CPM) [95] | Within-Sample | Normalizes for sequencing depth by scaling to a common total count. | Foundational but often insufficient alone for network analysis. |
| Trimmed Mean of M-values (TMM) [95] | Between-Sample | Adjusts counts based on a trimmed mean of log expression ratios, assuming most genes are not differentially expressed. | Highly accurate; produces networks that best recapitulate known functional relationships. |
| Counts adjusted with TMM factors (CTF) [95] | Between-Sample | A variation that directly adjusts counts by TMM size factors without library size correction. | Robust performance, especially accurate for capturing tissue-aware coexpression. |
| Upper Quartile (UQ) [95] | Between-Sample | Uses the upper quartile of counts to calculate size factors, reducing influence of lowly expressed genes. | Good performance, though may be slightly less robust than TMM on heterogeneous datasets. |
| Quantile (QNT) [95] | Between-Sample | Forces the distribution of counts across samples to be identical. | Can be effective but may over-correct in datasets with true global expression differences. |
Experimental Protocols for Viral Infectivity Studies
To ensure reproducibility, detailed protocols for key experiments must be followed. Below is a standardized workflow for a viral infectivity assay incorporating cellular and data normalization.
Protocol: Normalized High-Throughput Viral Infectivity Assay
Objective: To quantitatively compare the infectivity of two viral variants (e.g., Wild-Type vs. Mutant) in a susceptible cell line, with normalization for cellular input and technical variation.
Research Reagent Solutions & Essential Materials: Table 3: Key Research Reagent Solutions for Viral Infectivity Assays
| Item | Function/Application | Example |
|---|---|---|
| Susceptible Cell Line | In vitro model system for viral infection. | Vero E6, A549, Huh-7, or primary cells. |
| Viral Inoculum | The infectious agent being studied. | Wild-type and mutant virus stocks, titered by plaque assay. |
| Cell Dissociation Reagent | Generates single-cell suspension for accurate counting. | Trypsin-EDTA, Accutase. |
| Counting Beads | Internal standard for absolute cell counting via flow cytometry. | Commercial fluorescent bead standards (e.g., CountBright). |
| Lysis Buffer | For downstream nucleic acid or protein extraction. | RLT buffer (Qiagen) for RNA; RIPA buffer for proteins. |
| qRT-PCR Master Mix | For quantification of viral RNA/DNA load. | One-step or two-step SYBR Green or TaqMan kits. |
| SILAC Media Kit [94] | For metabolic labeling enabling precise protein quantification by mass spectrometry. | Media lacking specific amino acids (e.g., Arg, Lys) and their stable isotope-labeled forms. |
Methodology:
Cell Seeding with Cellular Normalization: a. Harvest the susceptible cell line using a standardized dissociation reagent to create a single-cell suspension. b. Perform absolute cell counting using flow cytometry with counting beads to determine the precise cell concentration [94]. c. Seed multiple 96-well plates with an identical number of cells per well (e.g., 1.0 x 10^4). Include control wells for background subtraction (uninfected, no virus).
Viral Infection: a. Dilute viral stocks to the desired Multiplicity of Infection (MOI) using an appropriate dilution buffer. b. Infect triplicate (or more) wells for each viral variant and control. Include a "mock infection" control (dilution buffer only). c. Incubate for a defined period (e.g., 1-2 hours) to allow for viral adsorption, then remove the inoculum and replace with fresh maintenance media.
Sample Harvest and Data Acquisition: a. At designated time points post-infection (e.g., 24, 48, 72 hours), harvest the supernatant and cell lysate from the same well. b. Use the supernatant for plaque assays or RT-qPCR to quantify infectious virion production or viral genome copies. c. Use the cell lysate for Western blotting, RNA-seq, or proteomic analysis to quantify viral and host protein/nucleic acid levels.
Data Normalization and Analysis: a. For qPCR data: Normalize viral genome copies to a validated housekeeping gene (e.g., GAPDH, ACTB) from the cell lysate and to the input cell number determined in step 1b. b. For RNA-seq data: Process raw read counts using a robust workflow. A recommended combination is TPM for within-sample normalization followed by CTF (TMM factor adjustment) for between-sample normalization [95]. This workflow has been benchmarked to accurately recapitulate functional gene relationships. c. For proteomic data (SILAC): Use the incorporated stable isotopes for direct ratio-based quantification, which inherently normalizes for sample handling variations [94]. For label-free data, normalize total signal to the mean of all samples or use a proteomic ruler approach.
Visualization of Experimental and Data Workflows
The following diagrams, created using the specified color palette and contrast rules, illustrate the core workflows for the viral infectivity assay and the corresponding data analysis.
Diagram 1: Integrated experimental and data normalization workflow for viral infectivity assays. The experimental path (yellow) emphasizes precise cellular input, while the data analysis path (green) applies sequential normalization steps.
Diagram 2: A strategic framework linking sources of technical variation to their corresponding normalization countermeasures, culminating in robust quantitative results.
Automation and High-Throughput Adaptations for Screening Applications
The field of viral infectivity testing has been transformed by automation and high-throughput methodologies, shifting from labor-intensive manual assays to rapid, AI-powered platforms. This guide compares the performance of two leading technological approaches—AI-powered label-free microscopy and automated high-throughput flow cytometry—for quantitative viral infectivity testing in vitro.
Comparative Platform Analysis
The following next-generation platforms have demonstrated significant advantages over traditional methods like plaque assays or TCID50.
Table 1: Comparison of Automated Viral Infectivity Assay Platforms
| Platform Name | Core Technology | Throughput | Assay Time | Key Performance Metrics | Viruses Validated With |
|---|---|---|---|---|---|
| AVIATM [26] [96] | Convolutional Neural Networks (CNNs) & High-Throughput Brightfield Microscopy | 96-well plates | Hours (vs. 2-7 days for traditional assays) [26] | Precision of ~10%, sensitivity comparable or better than plaque/TCID50 [26] | HIV, Influenza A, Coronavirus 229E, Vaccinia, Poliovirus, Adenoviruses [26] |
| DVICE [11] | CNN (EfficientNet-B0) & Transmitted Light Microscopy | 96-well plates | Compatible with real-time monitoring over days [11] | AUROC of 0.991 ± 0.001, R² = 0.986 vs. human annotation for TCID50 [11] | SARS-CoV-2, Influenza A, Rhinovirus, Herpes Simplex Virus, Vaccinia, Adenovirus [11] |
| Automated Flow Cytometry [97] | Fully Automated Flow Cytometry | ~50,000 wells per day [97] | Varies by protocol (e.g., 6 days for Treg screen) [97] | Enables robust phenotypic drug discovery; used for diverse drug discovery programs [97] | Primarily used for phenotypic screening in drug discovery, utilizing complex cellular models [97] |
Detailed Experimental Protocols
To ensure reproducibility, below are the detailed core methodologies for the featured platforms.
This protocol outlines the steps for using the DVICE platform for virus infectivity quantification.
- Cell Seeding: Seed 10,000 permissive cells (e.g., A549, HeLa, Huh7, VeroE6) into each well of a 96-well plate.
- Virus Inoculation & Incubation: Inoculate cells with a serial dilution of the virus stock (e.g., Adenovirus, SARS-CoV-2, Influenza A). Incubate the plates for a period sufficient for CPE manifestation, typically up to 7 days.
- Automated Image Acquisition: Acquire transmitted light (TL) images using a high-throughput microscope (e.g., ImageXpress Micro Confocal) with a 4x magnification objective. Automate this process with a plate-loading robot.
- Ground Truth Staining (for model training/validation): After imaging, fix cells with 4% Paraformaldehyde (PFA) for 30 minutes. Stain with 0.25% Crystal Violet (CV).
- Human Expert Annotation: Independently annotate the infection status (infected/uninfected) of the CV-stained wells by at least three human experts to establish the ground truth dataset.
- AI Model Training & Inference: Train a Convolutional Neural Network (CNN), such as EfficientNet-B0, using the TL images as input and the human annotations as labels. Use the trained model to classify new, unlabeled TL images.
This protocol describes a generic workflow for a phenotypic screen, such as for identifying compounds that modulate T-regulatory (Treg) cell differentiation.
- Cell Isolation and Preparation: Isolate primary human cells. For a Treg screen, purify CD4+ T cells from leukapheresis samples using an immunomagnetic isolation kit.
- Plating and Compound Addition: Plate cells in media containing stimulants (e.g., anti-CD3/anti-CD28-coated beads and transforming growth factor β for Treg induction) into 384-well plates. Add the library of screening compounds.
- Incubation: Incubate plates for the required duration (e.g., 6 days for Treg differentiation) at 37°C and 5% CO2.
- Automated Staining: Use an automated online system to perform cell staining. For Tregs, this involves surface staining for markers like CD4 and CD25, followed by intracellular staining for Foxp3 using a fixation/permeabilization buffer set.
- High-Throughput Acquisition: Run samples directly on the automated flow cytometer (e.g., CyAn instrument).
- Data Analysis: Analyze the multi-parametric flow cytometry data to identify hits—compounds that cause a statistically significant shift in the target cell population.
Workflow Visualization
The diagram below illustrates the logical workflow of the AI-powered label-free microscopy assay, from sample preparation to final infectivity score.
AI-Powered Viral Infectivity Workflow
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and reagents are critical for the successful implementation of these automated screening platforms.
Table 2: Essential Research Reagents for Automated Viral Screening
| Item | Function/Application | Example from Protocols |
|---|---|---|
| Cell Lines | Permissive systems for virus propagation and CPE observation. | A549 (lung epithelial), HeLa (cervical cancer), VeroE6 (kidney epithelial), Huh7 (hepatoma) [11]. |
| Staining Antibodies | Enable multiparametric detection of cell surface and intracellular markers in flow cytometry. | Anti-CD4, anti-CD25, anti-Foxp3 for Treg cell screening [97]. |
| Fixation/Permeabilization Buffer | Preserves cells and allows intracellular antibody staining for flow cytometry. | Foxp3 Fix/Perm buffer set [97]. |
| Crystal Violet | Traditional stain used to validate CPE and provide ground truth data for AI model training. | 0.25% solution for staining fixed cells [11]. |
| Paraformaldehyde (PFA) | Cross-linking fixative agent used to preserve cell morphology for endpoint staining. | 4% PFA for fixing cells after live imaging [11]. |
| Serial Dilution of Virus | Fundamental for determining the infectious titer (TCID50) and generating a range of CPE for model training. | Applied to cell cultures after seeding [11]. |
Assay Validation and Comparative Analysis: Ensuring Reliability and Regulatory Compliance
Viral safety is a cornerstone of biopharmaceutical product quality, particularly for biotechnology products derived from cell lines of human or animal origin. The potential for viral contamination presents a significant risk to patient safety, making rigorous viral safety evaluation an essential component of regulatory submissions worldwide. The global regulatory landscape for viral safety has evolved substantially with the recent update to the International Council for Harmonisation (ICH) Q5A(R2) guideline, which provides a science-based framework for assessing and controlling viral contamination risks. This guidance, along with region-specific implementations from the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and China's Center for Drug Evaluation (CDE), establishes a comprehensive approach to viral safety that spans from early clinical development through marketing authorization.
The fundamental principles of viral safety evaluation encompass three main strategies: selecting and testing cell lines and other raw materials for the absence of viral contaminants, testing the product at appropriate manufacturing steps for infectious virus, and assessing the capacity of the production process to clear infectious viruses. This third strategy, termed viral clearance validation, demonstrates that manufacturing processes can effectively remove or inactivate potential viral contaminants. With the advent of "platform processes" commonly used for monoclonal antibodies and other recombinant proteins, regulatory agencies have developed specific approaches to leverage prior knowledge from similar products, reducing development timelines while maintaining safety standards.
Comparative Analysis of Global Regulatory Frameworks
ICH Q5A(R2): The Global Standard
The ICH Q5A(R2) guideline, finalized in January 2024, represents the current international consensus on viral safety evaluation of biotechnology products [98]. This comprehensive document provides a risk-based framework for assessing viral safety, outlining data requirements for marketing applications and reflecting advances in scientific knowledge and regulatory expectations since the original 1998 version. The guideline emphasizes a holistic approach to viral risk mitigation, requiring manufacturers to demonstrate thorough understanding of viral clearance mechanisms and process parameters that impact viral reduction.
A significant advancement in Q5A(R2) is its recognition of platform validation approaches, where prior knowledge from similar processes can be applied to new products. According to the guideline, for any unit operation concerned, there should be a comprehensive understanding of the mechanisms underlying viral clearance to apply a platform validation approach [99]. Additionally, the guideline emphasizes that process parameters impacting viral clearance should be well understood, and health authorities encourage the use of multi-factor orthogonal methods to conduct comprehensive research and analyze relevant factors. The composition of products (or process intermediates) should be compared, including potentially interfering impurities, and any potential interaction with test viruses and subsequent impact on viral clearance should be assessed based on risk.
China CDE Framework
China's Center for Drug Evaluation (CDE) issued the "Guideline on Platform Validation of Viral Clearance in Clinical Trial Applications of Recombinant Proteins (Trial)" in January 2024, representing China's specific implementation of ICH Q5A(R2) principles with some country-specific considerations [99]. This guideline marks a significant step in regulatory harmonization while addressing local requirements. For early-phase clinical trial applications utilizing platform validation for viral clearance, the CDE guideline specifies that acceptance requires meeting several key conditions.
First, the process module must be established based on sufficient cases or multi-factor orthogonal analysis. For monoclonal antibodies, this means a process module can be established based on validation study results of 3-5 other related products with similar characteristics and attributes produced by similar processes [99]. Second, assay methods with the same principles (such as cell-based assays or nucleic acid-based assays) must be used to evaluate viral clearance in the same process module. Third, important process parameters that affect virus removal performance should not exceed the worst-case operating conditions of the corresponding process module. Additionally, when platform validation is applied to virus filtration, at least one product-specific validation study should be conducted using parvovirus as an indicator virus, acknowledging the particular challenge posed by small, non-enveloped viruses.
EMA Requirements
The EMA's approach to viral safety for biotechnological investigational medicinal products is outlined in its scientific guideline "Virus safety evaluation of biotechnological investigational medicinal products" (EMEA/CHMP/BWP/398498/2005) [100]. The EMA positions viral safety requirements within the context of clinical development, stating that validation of virus reduction should be performed before the start of a clinical trial while allowing for certain circumstances where a reduction in virus validation studies may be acceptable [99].
The EMA specifies that virus reduction studies should include both an enveloped virus and a small non-enveloped virus, preferably a parvovirus. The contribution of more than one unit operation for virus reduction should be assessed, with at least two orthogonal steps demonstrating effectiveness. Furthermore, the reproducibility of an effective virus reduction step should be demonstrated by at least two independent experiments [99]. Regarding platform approaches, the EMA outlines general principles for reducing requirements for product-specific viral clearance validation based on prior manufacturer experience with similar products and well-characterized procedures.
A key distinction in the EMA guidance compared to the CDE guidance is that if the manufacturer's rationale for applying a platform validation approach is not entirely convincing, at least a single run with an appropriate virus is needed to confirm that the step is performing as expected [99]. The EMA emphasizes that if process performance differs (e.g., chromatographic profiles differ), then the process step should be fully validated according to ICH Q5A(R2) principles, demonstrating a risk-based approach to platform validation.
FDA Expectations
The FDA has adopted the ICH Q5A(R2) guideline, indicating alignment with global standards for viral safety evaluation [98]. For Investigational New Drug (IND) applications, the FDA generally requires validation data from one batch, testing with at least a murine retrovirus (though now moving toward inclusion of parvovirus), assessment of all relevant operation units (which may total four overall), and duplicate virus assays [99]. This approach ensures comprehensive evaluation of viral clearance capabilities during clinical development.
With the adoption of ICH Q5A(R2), using platform validation for viral clearance in early-phase clinical trial applications is also acceptable in the U.S., creating regulatory convergence with other regions [99]. The FDA's requirements reflect a practical approach to viral safety, recognizing the need for adequate data while allowing for efficient development pathways. The agency's movement toward including parvovirus testing aligns with global recognition of the particular challenges posed by small, non-enveloped viruses in biopharmaceutical manufacturing.
Tabular Comparison of Key Regulatory Requirements
Table 1: Comparative Analysis of Viral Clearance Validation Requirements Across Regulatory Agencies
| Requirement | ICH Q5A(R2) | China CDE | EMA | FDA |
|---|---|---|---|---|
| Platform Validation Basis | Comprehensive understanding of viral clearance mechanisms | 3-5 similar products with comparable attributes | Prior experience with similar products and processes | Consistent with ICH Q5A(R2) principles |
| Minimum Virus Panel | Risk-based approach | Two viruses, two repeats | Enveloped virus and small non-enveloped virus (preferably parvovirus) | At least murine retrovirus, moving to include parvovirus |
| Required Reduction Factor | Not specified (risk-based) | ≥4 logs for each of two operation units | Not specified (risk-based) | Not specified (risk-based) |
| Study Reproducibility | Scientific justification | Two repeats | Two independent experiments | Duplicate virus assays |
| Platform Virus Filtration | Scientific justification | At least one product-specific study with parvovirus | Case-by-case assessment | Consistent with ICH Q5A(R2) |
| Applicable Stage | Marketing application | Early-phase clinical trials | All clinical trial phases | Early-phase clinical trials (IND) |
Table 2: Platform Validation Requirements for Early-Phase Clinical Trials
| Aspect | China CDE | EMA | FDA |
|---|---|---|---|
| Prior Data Requirements | 3-5 similar products for platform establishment | Data from similar products for equivalent processing steps | Consistent with ICH Q5A(R2) |
| Process Parameter Consideration | Must not exceed worst-case conditions of platform | Critical analysis of parameters affecting virus reduction | Evaluation of all relevant operation units |
| Product Comparison | Similar characteristics, attributes, and processes | Comparison of biochemical properties and process parameters | Assessment of product and process similarity |
| Modular Approach | Process module based on orthogonal analysis | Evaluation of specific viral reduction steps | Assessment of unit operations |
| Confirmatory Studies | Required for virus filtration (parvovirus) | Required if rationale not convincing | Generally required for parvovirus |
Experimental Protocols for Viral Clearance Studies
Standardized Viral Clearance Study Methodology
Viral clearance validation studies follow standardized methodologies to ensure consistent and reproducible results across different products and manufacturing platforms. These studies typically use scaled-down models of manufacturing unit operations that accurately represent the full-scale process while allowing for safe handling of infectious viruses. The validation approach involves challenging these scaled-down models with high-titer virus stocks and measuring the log reduction value (LRV) achieved by each unit operation.
The core methodology begins with establishing a representative scaled-down model that has been qualified to match the performance of the manufacturing-scale process. This involves demonstrating that critical process parameters (e.g., flow rates, residence times, buffer compositions, load densities) are maintained within validated ranges. The model is then challenged with a virus preparation, and the amount of infectious virus in the pre- and post-processing samples is quantified using appropriate cell-based infectivity assays. The LRV is calculated as log10 (virus load in pre-processing sample / virus load in post-processing sample), providing a quantitative measure of viral clearance capability.
Orthogonal Viral Clearance Mechanisms
Effective viral clearance strategies employ multiple orthogonal mechanisms to ensure robust viral safety. Orthogonality refers to the use of different viral clearance mechanisms (e.g., inactivation, separation based on size, separation based on charge) to address the diverse physicochemical properties of potential viral contaminants. A typical viral clearance study evaluates several unit operations with different mechanisms of action to provide a layered defense against viral contamination.
The most common orthogonal steps include low-pH viral inactivation (effective against enveloped viruses), virus filtration (effective against both enveloped and non-enveloped viruses based on size exclusion), and chromatographic separations (which can remove viruses based on charge, hydrophobicity, or affinity interactions). Each of these unit operations employs distinct physical or chemical principles to achieve viral reduction, ensuring that if one mechanism is less effective for a particular virus, other mechanisms will provide complementary clearance. Regulatory agencies typically require demonstration of at least two robust orthogonal steps with significant viral reduction capabilities.
Diagram: Viral Clearance Validation Workflow
Viral Clearance Study Methodology
The Scientist's Toolkit: Essential Research Reagents and Materials
Critical Reagents for Viral Clearance Studies
Table 3: Essential Research Reagents for Viral Clearance Validation
| Reagent/Material | Function | Specific Examples | Regulatory Considerations |
|---|---|---|---|
| Virus Panels | Challenge agents for clearance studies | Murine leukemia virus (MuLV), Minute virus of mice (MVM), Pseudorabies virus (PRV) | Must include enveloped and small non-enveloped viruses; representative of potential contaminants |
| Cell Lines | Virus propagation and infectivity assays | Vero cells, MDBK cells, A9 cells | Well-characterized banks; demonstrated susceptibility to target viruses |
| Culture Media | Virus propagation and sample dilution | DMEM, MEM, RPMI-1640 with appropriate supplements | Must support virus growth without cytotoxicity in assays |
| Scale-Down Models | Representative manufacturing unit operations | Chromatography columns, membrane filters, incubation systems | Must be qualified against manufacturing scale for critical parameters |
| Detection Reagents | Virus quantification in samples | Stains for plaque assays, ELISA reagents, PCR master mixes | Validated for sensitivity, specificity, and quantitative range |
| Reference Standards | Assay qualification and validation | Virus stocks with known titer, positive control materials | Fully characterized and traceable to reference standards |
Quality Considerations for Research Materials
The quality and characterization of research reagents used in viral clearance studies are critical for generating reliable and regulatory-acceptable data. Virus stocks must be thoroughly characterized for titer, identity, purity, and stability, with documentation of preparation methods and storage conditions. Cell lines used in infectivity assays should come from well-characterized cell banks and demonstrate consistent susceptibility to the target viruses throughout the study period.
For scale-down models, comprehensive qualification protocols must demonstrate that the scaled-down system accurately represents the full-scale manufacturing process for all parameters relevant to viral clearance. This includes matching critical performance attributes such as step yields, product quality attributes, and operational parameters. Additionally, all analytical methods used for virus detection and quantification must be properly validated for accuracy, precision, specificity, and robustness, with defined limits of detection and quantification.
The comparative analysis of ICH Q5A(R2), FDA, EMA, and China CDE guidelines reveals a significant harmonization in regulatory expectations for viral safety evaluation of biotechnology products. The adoption of ICH Q5A(R2) by major regulatory regions establishes a common scientific framework based on risk assessment and mitigation principles. This convergence is particularly evident in the acceptance of platform validation approaches for viral clearance, which allows manufacturers to leverage prior knowledge from similar processes while maintaining appropriate safety standards.
Despite this harmonization, region-specific nuances remain, particularly in the implementation of platform approaches during early clinical development. The China CDE's specific requirement for 3-5 similar products to establish a platform and mandatory parvovirus testing for virus filtration steps demonstrates how global principles are adapted to local regulatory contexts. Similarly, the EMA's emphasis on a convincing scientific rationale for platform approaches and the FDA's movement toward including parvovirus in early-phase submissions reflect regional regulatory experiences and perspectives.
Looking forward, the continued evolution of viral safety guidelines will likely address emerging challenges such as novel modality types (e.g., gene therapies, cell therapies), advanced analytical methods, and the application of quality by design principles to viral clearance validation. The scientific and regulatory communities are increasingly focusing on risk-based approaches that prioritize resources based on the specific risks presented by different products, processes, and potential viral contaminants. This evolution, coupled with ongoing international collaboration, will further strengthen the global framework for ensuring the viral safety of biopharmaceutical products while supporting efficient development pathways.
Platform Validation Strategies for Viral Clearance in Biologics Development
In the development of biologics, viral safety is a critical regulatory requirement to prevent viral contamination in products derived from human or animal cell lines. Platform validation is an advanced approach that leverages prior knowledge and experience with a specific manufacturing platform to streamline the viral clearance validation process for new biologic entities. This strategy is grounded in the principle that when multiple products are manufactured using a well-characterized, consistent process with a common backbone—such as the same host cell line, similar purification steps, and comparable critical process parameters—the viral clearance data from one or more representative products can be reliably applied to new products within the same platform [101] [99] [102].
The concept gained significant regulatory traction following its inclusion in the updated ICH Q5A(R2) guideline and has been successfully implemented for various biologics, including monoclonal antibodies and recombinant proteins [101] [99]. This approach is particularly valuable for accelerating the development of early-phase clinical trial materials while maintaining a high standard of product safety. By utilizing platform validation, manufacturers can potentially reduce the number of product-specific viral clearance studies required, thereby optimizing resources, shortening development timelines, and reducing costs without compromising patient safety [101] [99] [102].
Regulatory Landscape and Comparative Requirements
Global regulatory agencies have recognized the value of platform validation approaches and have worked toward harmonizing expectations, though region-specific nuances remain.
Table 1: Comparative Regulatory Requirements for Platform Viral Clearance Validation
| Regulatory Agency | Minimum Product Basis for Platform | Virus Panel Expectations | Key Documentation Requirements |
|---|---|---|---|
| China NMPA (CDE) | Data from 3-5 related products with similar characteristics and attributes [99] | Product-specific validation for parvovirus filtration required [99] | Comparison of biochemical properties; justification of parameter ranges [99] |
| EMA | Prior experience with specific downstream steps; comparable effectiveness across products [99] | Enveloped virus and small non-enveloped virus (preferably parvovirus) [99] | Critical analysis of manufacturing step; composition of product intermediate [99] |
| FDA | Adherence to ICH Q5A(R2) principles; sufficient prior knowledge [99] | Murine retrovirus (moving toward inclusion of parvovirus) [99] | Demonstration of comparable clearance across platform; robustness data [99] |
| ICH Q5A(R2) | Comprehensive understanding of mechanisms underlying viral clearance [99] | Virus panel representative of potential contaminants [101] | Assessment of potential interactions with test virus based on risk [99] |
The fundamental regulatory principle across regions emphasizes that platform approaches must be based on a comprehensive understanding of the viral clearance mechanisms for each unit operation and the critical process parameters that affect clearance efficiency [99]. Regulators require demonstration that the new product and process intermediates have comparable biochemical properties to those within the established platform, and that any potential differences that might impact viral clearance have been adequately addressed through risk assessment [101] [99].
Core Viral Clearance Methodologies and Unit Operations
Biologics manufacturing processes typically incorporate multiple orthogonal unit operations that contribute to viral clearance through different mechanisms, providing a layered safety approach.
Inactivation Methods
Low-pH treatment is a robust and widely used method for inactivating enveloped viruses. Typically conducted at pH 3.0–3.6 following affinity chromatography, this method achieves >4.0 log₁₀ reduction for enveloped viruses by disrupting their lipid envelopes [103]. The effectiveness depends on precise control of pH, contact time, and temperature [103].
Solvent/detergent (S/D) treatment is another robust method specifically targeting enveloped viruses. Using reagents such as 0.3% tri(n-butyl) phosphate (TNBP) and 0.2% sodium cholate, S/D treatment disrupts the viral lipid envelope, preventing viral binding and replication [103]. This method is highly effective and considered robust across different manufacturing conditions [103].
Removal Methods
Virus retentive filtration employs membranes with specific pore sizes (typically 20 nm or larger) to physically remove viruses based on size exclusion. This method is particularly effective for small non-enveloped viruses like parvoviruses and is often considered a dedicated viral clearance step [103] [99]. Performance depends on filter chemistry, load conditions, and pressure parameters [103].
Chromatography operations can remove viruses through various mechanisms including binding to resin surfaces, degradation, or sequestration. While not typically considered robust clearance methods, some chromatography steps (particularly anion-exchange) can provide 2-3 log₁₀ reduction or more when optimized [103]. Effectiveness varies significantly with buffer conditions, flow rates, and product characteristics [103].
Table 2: Performance Characteristics of Viral Clearance Unit Operations
| Unit Operation | Primary Mechanism | Virus Susceptibility | Typical Reduction (log₁₀) | Robustness |
|---|---|---|---|---|
| Low-pH Treatment | Envelope disruption | Enveloped viruses (e.g., MuLV, PRV) | >4.0 | High [103] |
| Solvent/Detergent | Envelope solubilization | Enveloped viruses (e.g., HIV, HCV) | >4.0 | High [103] |
| Virus Filtration | Size exclusion | All viruses larger than pore size | >4.0 | High [103] |
| Anion-Exchange Chromatography | Binding/adsorption | Enveloped and some non-enveloped | 2-5 (varies) | Moderate [103] |
| Affinity Chromatography | Multiple mechanisms | Variable depending on virus | 1-4 (varies) | Low to Moderate [103] |
Experimental Design and Protocol Considerations
Scale-Down Model Qualification
Viral clearance studies are performed using scaled-down models that accurately represent manufacturing-scale processes. According to regulatory requirements, these models must demonstrate comparable performance to full-scale operations through rigorous qualification [103]. The qualification process involves demonstrating that the scaled-down model accurately mimics the full-scale process in terms of buffers, linear flow rates, contact times, and other critical parameters. Additionally, the product and impurity profiles must reflect those observed at manufacturing scale to ensure the validity of generated viral clearance data [103].
Virus Panel Selection and Study Design
The selection of an appropriate virus panel is critical for meaningful viral clearance assessment. Regulatory guidelines recommend using viruses with diverse characteristics, including size, genome type, envelope structure, and resistance to physical and chemical challenges [103] [99]. A typical panel includes:
- Murine leukemia virus (MuLV) as a model for retroviruses
- Parvovirus (e.g., MVM or PPV) as a model for small, hardy viruses
- Additional viruses representing potential contaminants based on cell line history [103] [99]
For each unit operation assessed, viruses are independently spiked into the preprocessed intermediate material, and the process step is performed. Viral titers in preprocessed and postprocessed samples are compared to calculate log reduction values [103].
Diagram 1: Viral clearance study workflow. The process begins with qualification of scaled-down models that accurately represent manufacturing conditions, followed by careful virus panel selection, experimental execution, and quantitative analysis of reduction factors.
Platform Validation Implementation Strategy
Establishing Platform Boundaries
Successful implementation of platform validation requires careful definition of platform boundaries based on product and process similarity. Manufacturers must demonstrate that new products fall within the established platform based on multiple criteria:
- Similar biochemical properties of products and process intermediates
- Identical or highly similar purification methods and unit operations
- Comparable critical process parameters and operating ranges [99] [102]
The manufacturing process upstream to the viral clearance step should follow a similar strategy, and any potential impact of product-specific components on viral clearance must be thoroughly evaluated [99].
Risk Management in Platform Approaches
A science-based risk management approach is essential for successful platform validation implementation. This involves:
- Identifying high-risk process parameters that may affect viral clearance
- Defining appropriate control strategies to ensure consistent viral clearance performance
- Conducting comparative analysis of viral clearance performance across multiple products within the platform [101]
When applying platform knowledge to a new product, regulatory agencies typically expect the use of worst-case data (the product demonstrating the lowest reduction value within the platform) unless product-specific data are generated [99].
Diagram 2: Platform validation implementation. This strategic approach involves systematic assessment of product and process similarity, definition of critical parameters, thorough risk assessment, and justification of the platform approach before implementation with appropriate controls.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Viral Clearance Studies
| Reagent/Material | Function in Viral Clearance Studies | Application Notes |
|---|---|---|
| Model Viruses | Challenge agents to assess clearance capacity of unit operations | Panel should represent potential contaminants; include enveloped and non-enveloped species [103] |
| Cell Cultures | Host systems for virus propagation and titer determination | Must support robust virus growth; appropriate for plaque assays or TCID₅₀ [103] |
| Chromatography Resins | Purification matrices that may contribute to viral clearance | Performance affected by ligand chemistry, flow rates, buffer conditions [103] |
| Virus Filters | Dedicated removal step based on size exclusion | Pore size rating critical (typically 20 nm); performance depends on load conditions [103] [99] |
| Detection Assays | Quantify viral titers pre- and post-processing | Include plaque assays, TCID₅₀, or qPCR; must be validated for accuracy [103] |
Platform validation strategies for viral clearance represent a scientifically rigorous and resource-efficient approach to ensuring viral safety of biologics. By leveraging prior knowledge from well-characterized manufacturing platforms, developers can accelerate product development while maintaining appropriate safety standards. Successful implementation requires comprehensive understanding of viral clearance mechanisms, careful definition of platform boundaries, and thorough risk assessment. The alignment among major regulatory agencies on fundamental principles facilitates global development strategies, though attention to region-specific requirements remains important. As platform approaches continue to evolve with increasing industry experience, they will likely play an expanding role in the efficient development of safe biologic therapeutics.
Within the framework of comparative viral infectivity testing for in vitro research, the selection of an appropriate diagnostic methodology is paramount for accurate SARS-CoV-2 detection. Quantitative reverse transcription-polymerase chain reaction (RT-qPCR) is the established gold standard, but nested PCR (nPCR) and loop-mediated isothermal amplification (LAMP) represent critical alternatives with distinct operational profiles. nPCR, through its two-step amplification process, offers enhanced specificity, while LAMP provides a rapid, isothermal amplification suitable for point-of-care settings. This guide objectively compares the performance of nPCR and LAMP for SARS-CoV-2 detection, presenting synthesized experimental data to aid researchers, scientists, and drug development professionals in selecting the optimal method for their specific diagnostic and research applications. The comparison is grounded in published experimental evidence, focusing on key performance metrics such as sensitivity, specificity, limit of detection, and logistical requirements.
Performance Comparison: nPCR vs. LAMP
A direct, side-by-side clinical comparison of nPCR and LAMP for SARS-CoV-2 is less common in the literature, as RT-qPCR is more frequently used as the reference standard. However, performance data from independent studies and a meta-analysis provide a clear basis for comparison. The following table summarizes the key performance characteristics of nPCR and LAMP based on available evidence.
Table 1: Performance comparison of nPCR and LAMP for SARS-CoV-2 detection
| Performance Metric | nPCR | LAMP |
|---|---|---|
| Pooled Sensitivity | Not fully aggregated for SARS-CoV-2, but generally considered very high [104] | 83.3% (95% CI 76.9–88.2) [104] |
| Pooled Specificity | Not fully aggregated for SARS-CoV-2, but generally considered very high [104] | 96.3% (95% CI 93.8–97.8) [104] |
| Limit of Detection (LoD) | Varies by primer-probe set; some can detect down to 5-50 copies per reaction [105] | ~2.2-6.7 copies per reaction [106] [107] |
| Time-to-Result | Several hours (includes two amplification rounds) | 35-60 minutes (isothermal amplification) [106] [108] |
| Sample Type (Example) | Nasopharyngeal swabs (RNA extracted) | Nasopharyngeal swabs, saliva (raw or extracted RNA) [106] [109] |
| Key Advantage | High specificity due to dual amplification | Speed, simplicity, and potential for point-of-care use |
| Main Disadvantage | Time-consuming, higher risk of cross-contamination | Sensitivity can decrease later in infection (post-day 9) [106] |
It is important to note that LAMP's performance is highly dependent on the stage of infection. One study found that up to the 9th day after symptom onset, RT-LAMP had a positivity of 92.8% and a sensitivity and specificity of 100% compared to RT-qPCR. However, after the 10th day, its positivity dropped to less than 25% [106]. This suggests LAMP is an excellent alternative to PCR during the acute symptomatic phase.
Table 2: Impact of sample type and processing on LAMP performance
| Sample Processing Method | Sensitivity | Specificity | Remarks |
|---|---|---|---|
| Purified RNA from Saliva | 95.2% (95% CI 76.1–99.8) [109] | 90.5% (95% CI 69.6–98.8) [109] | Requires RNA extraction, increasing time and cost |
| Raw Saliva (No Purification) | 81.8% (95% CI 59.7–94.8) [109] | 90.9% (95% CI 70.8–98.8) [109] | Faster, less expensive; suitable for mass screening |
Experimental Protocols
To ensure reproducibility and provide a clear technical overview for professionals, this section outlines standard experimental protocols for nPCR and LAMP assays as described in the literature.
nPCR Protocol for SARS-CoV-2 Detection
While a specific nPCR protocol for SARS-CoV-2 was not detailed in the search results, the methodology is well-established and can be inferred from general nPCR principles and a protocol for malaria detection [110]. The process involves two consecutive amplification rounds using outer and inner primer sets.
Workflow Overview:
Detailed Procedure:
- RNA Extraction: Total viral RNA is extracted from nasopharyngeal swab samples placed in viral transport medium using a commercial kit (e.g., QIAamp Viral RNA Mini Kit) on an automated nucleic acid extraction device (e.g., QIAcube). RNA is eluted in 60 μL of buffer and can be stored at -80°C [106].
- Reverse Transcription: This step is integrated into the subsequent PCR reaction using a one-step RT-PCR kit.
- First PCR Round (Outer Primers):
- Reaction Mix: The mixture includes universal outer primers (e.g., targeting a conserved region of the SARS-CoV-2 genome), dNTPs, MgCl₂, reaction buffer, and a DNA polymerase (e.g., AmpliTaq Gold).
- Cycling Conditions: An initial denaturation/activation step (e.g., 94°C for 10 min) is followed by 35-40 cycles of denaturation (e.g., 92°C for 30 s), annealing (e.g., 60°C for 1.5 min), and extension (e.g., 72°C for 1 min), with a final extension at 72°C for 5 min [110].
- Second PCR Round (Inner Primers):
- Template Preparation: The product from the first PCR is diluted 40-fold in sterile nuclease-free water.
- Reaction Mix: The diluted product is added to a new reaction mixture containing inner, species-specific primers.
- Cycling Conditions: The thermal cycling is repeated for 20-25 cycles with parameters similar to the first round.
- Detection: The final amplified product is visualized using gel electrophoresis (e.g., 2.5% agarose gel stained with ethidium bromide) and examined for bands of the expected size [110].
RT-LAMP Protocol for SARS-CoV-2 Detection
The following protocol is adapted from studies that successfully detected SARS-CoV-2 in nasopharyngeal and saliva samples [106] [109].
Workflow Overview:
Detailed Procedure:
- Sample Preparation (Two Pathways):
- Path A (With RNA Extraction): Extract RNA as described in the nPCR protocol. Use 2-10 μL of purified RNA as template [106] [109].
- Path B (Without RNA Extraction): For raw saliva, mix the sample with a lysis buffer (e.g., TCEP/EDTA/NaOH) and inactivate at 95°C for 5 minutes. Centrifuge, and use the supernatant directly as template [109].
- LAMP Reaction Setup:
- Reagents: Use a commercial LAMP kit (e.g., WarmStart Colorimetric LAMP 2× Master Mix) or prepare a master mix containing Bst DNA polymerase, dNTPs, reaction buffer (with MgSO₄ and betaine), and primer sets.
- Primers: A typical reaction uses a set of 6 primers (F3, B3, FIP, BIP, LF, LB) targeting specific SARS-CoV-2 genes (e.g., ORF1a, Gene E, N gene) at optimized concentrations (e.g., 40 pmol each of FIP and BIP, 20 pmol each of LF and LB, 10 pmol each of F3 and B3) [109].
- Assembly: In a single tube, combine 15 μL of reaction mix with 10 μL of template RNA or raw sample lysate, for a total reaction volume of 25 μL [106].
- Amplification:
- Incubate the reaction tube at a constant temperature of 62.5°C for 35-40 minutes in a thermal block, real-time turbidimeter, or water bath [106].
- Detection:
- Real-time: Monitor amplification in real-time using a turbidimeter that measures magnesium pyrophosphate precipitation.
- Endpoint: Visualize results by adding colorimetric dyes (e.g., phenol red) that change color (e.g., from pink to yellow) in response to acidification, or under UV light if using intercalating fluorescent dyes [106] [109].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and their functions essential for conducting nPCR and LAMP assays for SARS-CoV-2 detection, based on the protocols cited in this guide.
Table 3: Essential research reagents for nPCR and LAMP assays
| Reagent / Kit | Function | Example Product / Component |
|---|---|---|
| RNA Extraction Kit | Purifies viral RNA from clinical samples, removing inhibitors. | QIAamp Viral RNA Mini Kit [106] |
| One-Step RT-qPCR Kit | Integrates reverse transcription and PCR amplification in a single tube. | TaqMan Fast Virus 1-Step Master Mix [106] |
| LAMP Master Mix | Provides the core enzymes and buffers for isothermal amplification. | WarmStart Colorimetric LAMP Master Mix [109] |
| Bst DNA Polymerase | Strand-displacing DNA polymerase essential for LAMP amplification. | Bst DNA/RNA Polymerase 3.0 [111] |
| LAMP Primers | A set of 4-6 primers that bind to 6-8 distinct regions of the target gene for highly specific amplification. | Primers for ORF1a, Gene E, or N gene [109] [108] |
| Nuclease-Free Water | A critical solvent free of RNases and DNases to prevent degradation of templates and reagents. | N/A |
| Positive Control RNA | Validates assay performance and serves as a quantitative standard. | SARS-CoV-2 RNA transcript standards [105] |
nPCR and LAMP are both powerful molecular techniques for SARS-CoV-2 detection, yet they serve different purposes within the research and diagnostic landscape. nPCR remains a valuable tool for confirmatory testing in well-equipped laboratories due to its high specificity. In contrast, LAMP offers a compelling combination of speed, simplicity, and high sensitivity—especially during the early stages of infection—making it ideally suited for rapid screening, field deployment, and point-of-care applications. The choice between these methods should be guided by the specific requirements of the research question, including the need for throughput, turnaround time, available infrastructure, and the stage of infection being studied.
In the field of virology, accurate quantification of infectious virus particles is a cornerstone of research, playing a critical role in vaccine development, antiviral drug testing, and fundamental studies of host-pathogen interactions. For the Lymphocytic Choriomeningitis Virus (LCMV), a prototypic arenavirus and a widely used model for studying acute and chronic viral infections, the plaque assay has been the historical standard for virus titration [112]. However, technical limitations inherent to this method have spurred the development of more advanced techniques, including the Semi-Functional Quantitative Flow Cytometry (SFQF) assay [52]. This guide provides an objective, data-driven comparison of these two methods, framing their capabilities within the broader context of viral infectivity testing for research and drug development.
Methodological Principles and Protocols
Understanding the fundamental procedures of each assay is essential for appreciating their comparative advantages and limitations.
Plaque Assay Protocol
The plaque assay is a classical virological technique that quantifies infectious virus based on its ability to form visible lytic areas (plaques) in a cell monolayer.
- Cell Seeding: Vero cells are seeded into 6-well plates and grown to 90-95% confluence [52] [113].
- Virus Infection: The cell monolayer is infected with serially diluted viral samples (e.g., 200 µl) and incubated for approximately 1 hour to allow for viral adsorption. The plate is shaken periodically to ensure even distribution and prevent drying [52].
- Agar Overlay: After adsorption, the medium is removed and the cells are overlaid with a semi-solid medium (e.g., agarose mixed with 199 medium) to confine viral spread to adjacent cells [52] [113].
- Incubation and Staining: Plates are incubated for 4 days. Then, a second overlay containing a vital dye, such as 1% neutral red, is added and incubated for an additional 18 hours. The dye is taken up by living cells, making the unstained plaques clearly visible against the colored monolayer [52].
- Quantification: Plaques are counted visually, and the virus titer is calculated in Plaque-Forming Units (PFU) per milliliter, taking into account the dilution factor [52] [112].
Semi-Functional Quantitative Flow Cytometry (SFQF) Assay Protocol
The SFQF assay is a flow cytometry-based method that directly detects intracellular viral antigen as a marker of infection.
- Cell Seeding and Infection: Vero cells are seeded in an appropriate plate format and infected with serial dilutions of the viral sample. A key differentiator is the infection period, which is typically 48 hours to allow for sufficient viral protein expression [112] [114].
- Cell Harvesting and Fixation: After incubation, cells are detached using trypsin-EDTA and washed [52].
- Cell Staining: Cells are fixed and permeabilized. They are then stained intracellularly with a fluorescently-conjugated antibody specific for the LCMV nucleoprotein (NP), such as the VL-4 clone. An isotype control is used to gate for non-specific background signal [52] [112].
- Flow Cytometry Analysis: The stained cells are analyzed by flow cytometry. The percentage of NP-positive cells is determined for each virus dilution [52] [112].
- Titer Calculation: A standard curve is generated by plotting the percentage of NP-positive cells against known virus concentrations (in PFU/ml). The titer of an unknown sample can then be extrapolated from this curve [112].
The following diagram illustrates the core workflow and fundamental difference in readout between the two assays.
Critical Comparative Data
The following table summarizes the key performance metrics of the SFQF and Plaque assays, based on experimental data.
Table 1: Quantitative Comparison of SFQF Assay vs. Plaque Assay
| Performance Metric | Plaque Assay | SFQF Assay (48h) | SFQF Assay (72h) | Experimental Context |
|---|---|---|---|---|
| Total Assay Time | ~5-6 days [52] [112] | 3 days [112] | 4 days | In vitro infection of Vero cells [112] [114] |
| Limit of Detection (LOD) | 50 PFU/ml [114] | 15 PFU/ml [114] | 1 PFU/ml [114] | Dilution series of LCMV-Arm stock [114] |
| Sensitivity (vs. Plaque) | (Baseline) | ~19-fold increase [112] [114] | ~77-fold increase [114] | Comparison of ID(_{50}) values [114] |
| Practical Limit of Quantification | 200 PFU/ml [114] | 62 PFU/ml [114] | 2 PFU/ml [114] | +/−10× SD of uninfected samples [114] |
| Sample Volume | Up to 500 µl, often requiring pre-dilution [112] | Requires smaller volumes, avoids need for high dilution [112] | Same as 48h SFQF | Assay setup and serial dilution [112] |
| Objectivity | Subjective (visual counting of heterogeneous plaques) [112] | Objective (digital counting of fluorescent cells) [52] [112] | Same as 48h SFQF | Data acquisition and analysis [52] [112] |
| Key Advantage | Directly measures infectious virus; established gold standard. | Speed, sensitivity, and objectivity. Amenable to high-throughput. [112] | Maximum sensitivity for low-titer samples. |
Beyond the metrics in the table, a significant functional advantage of the SFQF assay is its ability to reveal the presence of infectious virus in samples from models of acute and chronic infection that were determined to be negative by the plaque assay [112]. Furthermore, the SFQF assay can be adapted to study infection in specific primary cell populations and for high-throughput diagnostic platforms [112].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of either assay relies on the use of specific, high-quality reagents.
Table 2: Key Research Reagent Solutions for LCMV Titration
| Reagent / Material | Function in Assay | Critical Notes |
|---|---|---|
| Vero Cells | Host cell line for LCMV propagation and infection. | Preferred over BHK-21 due to ~7x higher sensitivity to LCMV infection and better monolayer arrangement [52]. |
| Anti-LCMV NP Antibody (VL-4 clone) | Primary antibody for intracellular detection of viral nucleoprotein in SFQF assay. | Conjugation to a fluorophore (e.g., Alexa Fluor 647) is required. Specificity must be confirmed with an isotype control [52] [112]. |
| Fixation/Permeabilization Buffer | Prepares cells for intracellular antibody staining in SFQF assay. | Chemically treats cells to allow the fluorescent antibody to enter and bind to the intracellular NP antigen [52]. |
| Agarose Overlay | Confines viral spread to adjacent cells in the plaque assay. | Creates a semi-solid matrix that restricts virus to two-dimensional diffusion, enabling plaque formation [52] [113]. |
| Neutral Red Stain | Vital dye for visualizing living cells in plaque assay. | Living cells take up the dye, causing plaques (areas of dead cells) to appear as clear, unstained zones against a colored monolayer [52]. |
This comparative analysis demonstrates that the SFQF assay presents a formidable alternative to the traditional plaque assay for quantifying LCMV. Its principal advantages are accelerated turnaround time, significantly enhanced sensitivity, and superior objectivity. These attributes make it particularly suitable for applications requiring rapid results or the detection of low levels of virus, such as in studies of chronic infection or during high-throughput screening of antiviral compounds [52] [112].
However, the plaque assay remains the "gold standard" that provides a direct functional measure of infectious virus capable of cell-to-cell spread and plaque formation. The choice between methods should be guided by the specific research question. For many contemporary applications, the SFQF assay offers a more powerful and efficient tool, advancing the capabilities of in vitro viral infectivity testing. Its development underscores a broader trend in virology toward leveraging flow cytometry and intracellular staining to gain faster, more precise, and more granular quantitative data on viral infection.
Adeno-associated virus (AAV) vectors have emerged as a leading platform for in vivo gene therapy due to their favorable safety profile, sustained transgene expression, and ability to transduce both dividing and non-dividing cells [115] [116]. A critical factor influencing the efficacy of AAV-based treatments is the selection of serotype, as naturally occurring and engineered AAV variants exhibit distinct infectivity, tissue tropism, and immunogenicity profiles [117] [118]. Pre-existing neutralizing antibodies (NAbs) in human populations pose a significant barrier to successful gene delivery, as they can bind to the viral capsid and prevent transduction of target cells [119] [120]. This comparative case study objectively analyzes the infectivity and neutralization profiles of prominent AAV serotypes, with a specific focus on the highly homologous AAV5 and the novel caprine-derived AAV Go.1. The data and methodologies presented herein are framed within the broader context of comparative viral infectivity testing for in vitro research, providing drug development professionals with critical insights for vector selection and preclinical assessment.
Comparative Analysis of AAV Serotype Properties
Fundamental Characteristics of Common AAV Serotypes
The functional diversity of AAV serotypes is largely dictated by differences in their capsid proteins, which influence receptor binding, cellular entry, and subsequent immune recognition [117] [116]. Table 1 summarizes the primary receptors, coreceptors, and documented tissue tropisms for several clinically relevant serotypes.
Table 1: Receptor Usage and Tissue Tropism of Select AAV Serotypes
| Serotype | Primary Receptor | Coreceptor(s) | Documented Tissue Tropism in Humans |
|---|---|---|---|
| AAV1 | N-linked sialic acid [117] | AAVR [117] | CNS, retina, pancreas, skeletal muscle [115] |
| AAV2 | Heparan Sulfate Proteoglycan (HSPG) [117] | FGFR1, LamR, αVβ5/α5β1 integrins, CD9 [117] | Retina [115] |
| AAV5 | N-linked sialic acid [117] | PDGFR [115] | CNS, retina, kidney, pancreas, liver [115] |
| AAV6 | Heparan Sulfate Proteoglycan, N-linked sialic acid [115] | EGFR [115] | Skeletal muscle [115] |
| AAV8 | Unknown [115] | LamR [115] | CNS, heart, liver, retina [115] |
| AAV9 | terminal N-linked galactose [115] | putative integrin, LamR [115] | CNS, heart [115] |
Global Seroprevalence of Neutralizing Antibodies
The prevalence of pre-existing NAbs varies significantly across different AAV serotypes and geographical regions, directly impacting the potential patient population eligible for treatment. A large-scale study measuring NAb activity against six clinically relevant serotypes across 10 countries revealed a distinct seroprevalence hierarchy: NAb prevalence was generally highest for AAV1 and lowest for AAV5 [120]. Furthermore, the study found considerable variability across countries and identified that co-prevalence was most frequent between AAV1 and AAV6, and less frequent between AAV5 and other AAVs [120]. This unique immunogenicity clustering, which differs from traditional phylogenetic classifications, suggests that AAV5 and, by extension, its close variants may offer an advantage in evading pre-existing humoral immunity.
Case Study: AAV5 vs. AAV Go.1
Rationale for Comparison
AAV Go.1, a caprine-derived AAV variant, shares 95% genome sequence identity and 94% capsid protein homology with the well-characterized AAV5 serotype [119]. Despite this high genetic similarity, 42 amino acid differences are localized on the exterior surface of the capsid, a region critical for host cell interaction and antibody recognition [119]. This makes the AAV5/AAV Go.1 pair an ideal model system for a comparative case study, as it allows for the isolation of capsid surface variations as the primary variable influencing infectivity and neutralization profiles.
Quantitative Comparison of Infectivity and Immune Evasion
Recent original research directly compared the performance of recombinant AAV (rAAV) Go.1 and rAAV5 in vitro and in vivo. Key quantitative findings from this comparative study are summarized in Table 2 below.
Table 2: Direct Comparative Data for AAV5 and AAV Go.1
| Parameter | AAV5 | AAV Go.1 | Experimental Context |
|---|---|---|---|
| Packaging Efficiency | Baseline | Significantly higher [119] | Using AAV2-rep gene in production system [119] |
| Transduction Efficiency | Baseline | Markedly higher [119] | In vitro (cell lines) and in vivo (mouse models) [119] |
| Resistance to Mouse NAbs | Baseline | 100-fold higher resistance [119] | In vitro neutralization assay using sera from rAAV5-immunized mice [119] |
| Resistance to Human NAbs | More pronounced inhibitory effect | Less pronounced inhibitory effect, 4-fold increase in resistance [119] | Study with sera from 20 healthy human volunteers [119] |
The data indicate that the minor capsid variations in AAV Go.1 confer not only enhanced production and transduction characteristics but also a superior capacity to evade neutralizing antibodies from both animal models and humans [119]. This suggests that AAV Go.1 is a promising candidate for clinical applications where pre-existing immunity to common AAV serotypes is a concern.
Experimental Protocols for In Vitro Comparison
To ensure reproducibility and provide a framework for similar comparative studies, this section outlines the key experimental protocols used to generate the data discussed in the case study.
Vector Construction and Production
The foundational step involves generating the recombinant viral vectors for testing.
- Plasmid Construction: The rAAV Go.1 was engineered by cloning the AAV Go.1 capsid coding region into a plasmid backbone containing the AAV2 Rep gene (pAAV-RC2/5), creating the plasmid pAAV-RC2/Go.1 [119]. This "pseudotyping" approach, using the well-characterized AAV2 Rep protein, can improve packaging efficiency and allows for standardized production across different capsids.
- Virus Production: The rAAV virions were produced in HEK293 cells using the traditional triple-plasmid transfection method [119]. This co-transfection involves:
- The transgene plasmid (e.g., containing a luciferase-EGFP reporter cassette flanked by ITRs).
- The packaging plasmid (pAAV-RC2/Go.1 or pAAV-RC2/5).
- A helper plasmid providing adenoviral functions essential for AAV replication [119].
- Virus Titration: The physical titer of the produced viral vectors (e.g., genome copies per mL) must be accurately determined using methods like quantitative PCR (qPCR) or droplet digital PCR (ddPCR) to ensure equivalent dosing in subsequent functional assays.
In Vitro Transduction and Neutralization Assays
These assays are core to evaluating the functional performance of the serotypes.
In Vitro Transduction Assay:
- Seed target cells (e.g., HEK293T, HeLa) in culture plates.
- Transduce cells at a specific multiplicity of infection (MOI) with rAAV vectors carrying a reporter gene (e.g., luciferase, GFP).
- After an appropriate incubation period (e.g., 48-72 hours), quantify transduction efficiency by measuring reporter signal (e.g., luminescence for luciferase, fluorescence for GFP) and normalize to total protein content or cell number [119].
In Vitro Neutralization Assay:
- Pre-incubate a fixed titer of rAAV vectors with serial dilutions of heat-inactivated test sera (e.g., from immunized mice or human volunteers) for a set time (e.g., 1 hour at 37°C).
- Add the virus-antibody mixture to pre-seeded cells.
- After incubation, measure the reporter signal as in the transduction assay.
- The neutralization titer (e.g., NT50) is defined as the serum dilution that inhibits transduction by 50% compared to a no-serum control [119].
Diagram 1: In vitro neutralization assay workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful in vitro infectivity and neutralization profiling requires a suite of specialized reagents and tools. The following table lists essential materials and their functions for researchers designing such studies.
Table 3: Essential Research Reagents for AAV Infectivity & Neutralization Studies
| Research Reagent / Material | Function in Experimental Protocol |
|---|---|
| Packaging Plasmids (e.g., pAAV-RC2/5) | Provides AAV serotype-specific Cap genes and AAV2 Rep genes in trans for vector production [119]. |
| Helper Plasmid | Supplies essential adenoviral genes (E2A, E4, VA RNA) required for AAV replication in the production system [119] [121]. |
| ITR-flanked Transgene Plasmid | Carries the therapeutic or reporter gene (e.g., Luciferase, GFP) flanked by AAV2 ITRs; serves as the "payload" packaged into the virion [119] [116]. |
| HEK293 Cells | Standard adherent cell line used for rAAV production via triple-plasmid transfection and for in vitro transduction assays [119]. |
| Fetal Bovine Serum (FBS) | Critical component of cell culture media, providing nutrients and growth factors for maintaining HEK293 and other cell lines. |
| qPCR/ddPCR Reagents & System | Used for the precise titration of viral genome copies (vg/mL) to ensure accurate and reproducible dosing in functional assays [119]. |
| Luciferase Assay Kit | Provides the substrate and buffer for detecting and quantifying luminescence output from cells transduced with luciferase-reporting rAAVs. |
| Anti-AAV Neutralizing Antibody Standards | Used as positive controls in neutralization assays to validate experimental system performance and for assay calibration. |
Visualizing Key Findings and Mechanisms
The comparative data between AAV5 and AAV Go.1 can be synthesized into a conceptual model illustrating the core findings of this case study.
Diagram 2: Comparative transduction and neutralization model. AAV Go.1 shows enhanced transduction and reduced NAb binding affinity compared to AAV5.
This comparative case study demonstrates that minor sequence variations in AAV capsids can profoundly impact key functional properties, including production efficiency, infectivity, and, most critically, susceptibility to neutralization. The direct comparison between AAV5 and the highly homologous AAV Go.1 provides a clear example of how capsid surface residues dictate interactions with host cell receptors and the immune system. The data robustly indicate that AAV Go.1 possesses superior transduction efficiency and a significant advantage in evading pre-existing NAbs in both animal models and human sera [119]. These findings underscore the importance of rigorous in vitro profiling of serotype variants as a critical step in the selection and development of the next generation of AAV-based gene therapies. For researchers and drug developers, this work highlights the potential of exploring novel or engineered serotypes to overcome the major challenge of pre-existing immunity and to develop more effective and accessible treatments.
Statistical Methods for Comparing Assay Sensitivity, Specificity, and Dynamic Range
In the field of virology, accurately quantifying virus infectivity and characterizing biological targets are fundamental to drug discovery, vaccine development, and clinical diagnostics. The reliability of this research hinges on the analytical performance of the assays employed, specifically their sensitivity, specificity, and dynamic range. These parameters determine an assay's ability to correctly identify true positives, exclude false positives, and measure responses across a wide spectrum of concentrations or expression levels. This guide objectively compares the performance of established and emerging methodologies, from traditional viral titrations to advanced artificial intelligence (AI)-powered and immunohistochemistry (IHC) assays, providing researchers with a framework for selecting the optimal tools for their investigative needs.
Comparative Assay Performance Data
The following tables summarize the key performance metrics and characteristics of various assay types relevant to viral and biomarker research.
Table 1: Performance Metrics for Viral Infectivity and Biomarker Assays
| Assay Method | Key Performance Metrics | Optimal Applications & Contexts |
|---|---|---|
| Plaque/Endpoint Dilution Assays [122] [13] | Statistical variability due to stochastic virus-cell interactions at low concentrations; requires probabilistic models (e.g., Poisson distribution) for accurate titer estimation [123] [13]. | Virus quantification (VQA); determining TCID₅₀ or PFU; foundational research requiring direct infectivity readouts [11] [13]. |
| AI-Powered CPE Detection (DVICE) [11] | AUROC: 0.991 ± 0.001; achieves human-level accuracy (R² = 0.986 vs. human annotation) for infection classification; enables label-free, real-time monitoring [11]. | High-throughput drug screening; automated virus titer determination (TCID₅₀); serum neutralization assays [11]. |
| Standard HER2 IHC Assay (Predicate) [124] [125] | Sensitivity: 85.7%; Specificity: 100% (for HER2 3+ detection). Poor dynamic range for HER2-low scores [124] [125]. | Differentiating HER2-positive (overexpressing) tumors for Trastuzumab eligibility in breast cancer [124] [125]. |
| Enhanced HER2 IHC with Image Analysis [124] [125] | Achieves a six-fold improvement in accurate HER2-low detection (p = 0.0017) compared to standard predicate assays [124] [125]. | Identifying HER2-low and ultra-low breast cancer subtypes for T-Dxd (Trastuzumab deruxtecan) therapy [124] [125]. |
Table 2: Statistical and Technical Considerations for Assay Design
| Factor | Description | Impact on Assay Performance |
|---|---|---|
| Sample Size & Power [122] | The number of experimental units (e.g., replicates) in a study. Power is the probability of detecting a true statistically significant difference [122]. | Inadequate sample size reduces power, leading to false negatives. For example, with only 3 animals/group, a perfect treatment effect remains statistically insignificant (p=0.1) [122]. |
| Dynamic Range [124] | The range of analyte concentrations over which an assay provides accurate measurements. | Standard HER2 assays (threshold: 30,000-60,000 molecules/cell) are reliable for high overexpression but fail to accurately classify low-expression subtypes, missing critical therapeutic targets [124]. |
| Analytic Sensitivity [124] | The lowest amount of an analyte that an assay can reliably detect. | Enhanced analytical sensitivity in IHC assays, combined with image analysis, is critical for expanding dynamic range and accurately detecting low-expression targets like HER2-low [124]. |
| Statistical Multiplicity of Infection (SMOI) [13] | A probabilistic model for the distribution of viral infections per host cell, accounting for randomness in infection events. | Provides a more accurate framework for interpreting data from virus quantification assays (e.g., plaque assays) and infectivity assays, especially at high or low viral particle concentrations [13]. |
Detailed Experimental Protocols
AI-Powered Automated Framework for Virus Infectivity (DVICE)
This protocol outlines the procedure for using label-free light microscopy and artificial intelligence to quantify virus-induced cytopathic effects (CPE), as described in the DVICE pipeline [11].
- Cell Seeding and Infection: Seed 10,000 permissive cells (e.g., A549, HeLa, Huh7, VeroE6) into each well of a 96-well plate. Inoculate the cells with a serial dilution of the virus stock (e.g., Adenovirus, SARS-CoV-2, Influenza). Include uninfected control wells. Incubate the plates for a period sufficient for CPE manifestation (e.g., up to 7 days) [11].
- Image Acquisition: Acquire transmitted light (TL) images of the live cells using a high-throughput microscope (e.g., ImageXpress Micro Confocal) with a 4x magnification objective. One central site per well is typically imaged [11].
- Ground Truth Annotation (for training): Following imaging, fix cells with 4% paraformaldehyde (PFA) and stain with 0.25% Crystal Violet (CV). The infection state of each CV-stained well is then independently annotated by multiple human experts to create a ground truth dataset for AI training [11].
- AI Model Training and Classification: Train a Convolutional Neural Network (CNN), such as EfficientNet-B0, using the TL images as input and the expert annotations as the ground truth. The trained model can then classify new TL images of infected cells as "infected" or "uninfected" with high accuracy, and can be used to calculate TCID₅₀ values [11].
HER2-Low Testing Comparative Study (CASI-01)
This protocol summarizes the methodology from the CASI-01 study, which compared HER2 testing assays across 54 laboratories [124] [125].
- Sample Preparation and Assay Setup: Utilize tissue samples with known HER2 expression levels, including those with HER2 overexpression (3+), HER2-low (1+ or ultra-low), and HER2-negative status. Process samples according to standard IHC protocols [124] [125].
- Comparative Testing: Test each sample using both the conventional FDA-cleared HER2 IHC assay ("predicate") and higher-sensitivity IHC assays. Perform testing across multiple participating laboratories to assess inter-laboratory variability [124] [125].
- Validation and Readout: Validate HER2 3+ scores against HER2 gene amplification status determined by in situ hybridization (ISH). For HER2-low accuracy, use newly introduced HER2 reference standards. Perform readouts using both traditional pathologist assessment and automated image analysis software [124] [125].
- Data Analysis: Calculate sensitivity and specificity for HER2-overexpression detection. Evaluate the dynamic range of each assay for accurately scoring HER2-low cases. Statistically compare the performance of predicate assays versus enhanced-sensitivity assays with image analysis [124] [125].
Experimental Workflow and Statistical Analysis Diagrams
The following diagrams illustrate the core workflows and statistical relationships for the key methodologies discussed.
Diagram 1: AI-Powered Viral Infectivity Assay Workflow
Diagram 2: Statistical Framework for Assay Comparison
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for Featured Assays
| Item | Function / Application |
|---|---|
| Permissive Cell Lines (e.g., A549, VeroE6, HeLa, Huh7) [11] | Provide the host cellular system required for viral replication and the manifestation of virus-induced cytopathic effects (CPE) in infectivity assays. |
| Crystal Violet Stain [11] | A standard histological dye used to fix and stain cell monolayers after infection, providing a "ground truth" readout for training AI models in assays like DVICE. |
| High-Throughput Microscope (e.g., ImageXpress Micro Confocal) [11] | Automates the acquisition of transmitted light images from multi-well plates, enabling large-scale, label-free data collection for AI-based analysis. |
| Convolutional Neural Network (CNN) Software (e.g., EfficientNet-B0) [11] | The AI engine that learns to identify patterns associated with CPE from microscopy images, automating and standardizing infection scoring. |
| HER2 IHC Assay Kits (Predicate & High-Sensitivity) [124] [125] | Contain the specific antibodies and reagents needed to visualize and quantify HER2 protein expression levels in formalin-fixed, paraffin-embedded (FFPE) tissue sections. |
| Automated Image Analysis Software (e.g., Visiopharm) [124] | Provides an objective, quantitative method for scoring HER2 expression, overcoming limitations of subjective pathologist readout and improving dynamic range for HER2-low detection. |
| HER2 Reference Standards [124] | Newly introduced calibrated materials that allow laboratories to validate and standardize the analytical sensitivity and accuracy of their HER2 IHC tests, particularly for low expression levels. |
Conclusion
Comparative viral infectivity testing in vitro remains an indispensable, yet rapidly evolving, discipline. This analysis underscores that no single method is universally superior; the choice of assay must be guided by the specific research question, the virus under investigation, and the required balance between throughput, sensitivity, and functional insight. The integration of foundational principles with robust methodological execution and systematic validation is paramount for generating reliable, reproducible data. Future directions will be shaped by the increased adoption of label-free, high-content technologies like Laser Force Cytology, the application of sophisticated computational models for data analysis, and the ongoing harmonization of global regulatory standards. As novel viruses emerge and advanced therapeutics like viral vectors and oncolytic viruses progress, the continued refinement of these comparative infectivity platforms will be critical for accelerating drug discovery and ensuring product safety.
References
- 1. and meaning | Collins English Dictionary VIRAL INFECTIVITY definition [https://www.collinsdictionary.com/dictionary/english/viral-infectivity]
- 2. Methods to Study Viruses - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7149989/]
- 3. Virus Assays [https://www.bmglabtech.com/en/blog/virus-assays/]
- 4. Are all virus particles infectious? [https://virology.ws/2011/01/21/are-all-virus-particles-infectious/]
- 5. Collective infectious units in viruses - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5837019/]
- 6. sciencedirect.com/topics/medicine-and-dentistry/ virus - infectivity [https://www.sciencedirect.com/topics/medicine-and-dentistry/virus-infectivity]
- 7. Quantitative comparisons & data interpretation : GRE ... [https://archive.org/details/quantitativecomp0000unse]
- 8. Standardization of Quantitative Plaque-Based Viral Assays ... [https://www.mdpi.com/1999-4915/17/10/1355]
- 9. In vitro antiviral activities of thymol and Limonin against ... [https://www.nature.com/articles/s41598-025-06967-x]
- 10. A versatile automated pipeline for quantifying virus infectivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11180103/]
- 11. A versatile automated pipeline for quantifying virus ... [https://www.nature.com/articles/s41467-024-49444-1]
- 12. Viral Infectivity Assays [https://www.agilent.com/about/tektalk/en/viral-infectivity-assays.html?srsltid=AfmBOoqjuPHaLGExF171o9EgkT39kZVAkBiB8kuaL__mHxkl2fe-NErC]
- 13. The Effects of Statistical Multiplicity of Infection on Virus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6026352/]
- 14. A novel in vitro system for simultaneous infections with ... [https://pubmed.ncbi.nlm.nih.gov/40242313/]
- 15. Comparison among plaque assay, tissue culture infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10132340/]
- 16. Virology through numbers: Plaque and TCID50 assays [https://virologyresearchservices.com/2024/07/15/virology-through-numbers-plaque-and-tcid50-assays/]
- 17. Viral Titering-TCID50 Assay Protocol [https://www.creative-biogene.com/support/Viral-Titering-TCID50-Assay-Protocol.html]
- 18. Virology through numbers: Converting TCID50 to IU [https://virologyresearchservices.com/2024/07/15/virology-through-numbers-converting-tcid50-to-iu/]
- 19. Comparison of the plaque assay and 50% tissue culture ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093413002024]
- 20. Development and validation of a Q-PCR based TCID50 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3546908/]
- 21. A sensitive cell-based assay for the detection of residual ... [https://www.sciencedirect.com/science/article/abs/pii/S0264410X0700789X]
- 22. Viral Infectivity Assays [https://www.agilent.com/about/tektalk/en/viral-infectivity-assays.html?srsltid=AfmBOoqJoT6Eaxu59T5QQA4TXWhOqSwDO_EN1Bdz8nj4-hu-yl0qqksd]
- 23. Evaluation of four cell lines for assay of infectious ... [https://pubmed.ncbi.nlm.nih.gov/19590132/]
- 24. A High-Throughput and Robust Relative Potency Assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12197749/]
- 25. Predicting infectivity: comparing four PCR‐based assays to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8819313/]
- 26. A rapid, high-throughput, viral infectivity assay using ... [https://www.sciencedirect.com/science/article/pii/S2472630323000456]
- 27. Viral viability markers of SARS-CoV-2: a comparison of cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502786/]
- 28. Antiviral neutralizing antibodies: from in vitro to in vivo activity [https://pmc.ncbi.nlm.nih.gov/articles/PMC10108814/]
- 29. Evaluating the Virucidal Activity of Disinfectants According ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8063834/]
- 30. Evaluation and comparison of three virucidal agents on ... [https://www.nature.com/articles/s41598-022-15228-0]
- 31. In Vitro Differential Virucidal Efficacy of Alcohol-Based ... [https://www.mdpi.com/2076-2607/13/2/368]
- 32. Comparative analysis of the neutralizing activity against ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.981693/full]
- 33. Comparative assessment of four virus neutralization ... [https://www.sciencedirect.com/science/article/abs/pii/S0003269725000983]
- 34. Comparing neutralizing antibody activity over time between ... [https://www.nature.com/articles/s41598-025-18673-9]
- 35. Evolution of the PRNT: Merging tradition and innovation to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243916/]
- 36. Measuring infectious virus: the plaque assay [https://virologyresearchservices.com/2022/08/10/the-plaque-assay/]
- 37. Viral Concentration Determination Through Plaque Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC4255882/]
- 38. Rapid and stain-free quantification of viral plaque via lens ... [https://www.nature.com/articles/s41551-023-01057-7]
- 39. Immunoplaque Assay (Influenza Virus) [https://en.bio-protocol.org/en/bpdetail?id=959&type=0]
- 40. Plaque Assay - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/plaque-assay]
- 41. Plaque Assay: Illustrations of Poor Technique and Plating ... [https://asm.org/image-gallery/plaque-assay-illustrations-of-poor-technique-and]
- 42. Viral-bacterial co-infections screen in vitro reveals ... [https://www.nature.com/articles/s41467-024-52905-2]
- 43. In vitro modeling of influenza infection in the respiratory ... [https://www.sciencedirect.com/science/article/abs/pii/S1879625725000021]
- 44. Automation of Infectious for Determination of Filovirus... Focus Assay [https://pmc.ncbi.nlm.nih.gov/articles/PMC7826780/]
- 45. Brief guide to immunostaining - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11699723/]
- 46. Microfluidic digital focus assays for the quantification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11796355/]
- 47. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467]
- 48. and Multiplicity of Infectious ... Focus Assays Infection [https://bio-protocol.org/en/bpdetail?id=1295&type=0]
- 49. A High-Throughput and Robust Relative Potency Assay ... [https://www.mdpi.com/2076-393X/13/6/626]
- 50. Advances in Diagnostic Techniques for Influenza Virus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12197469/]
- 51. A Benchmark for Virus Infection Reporter Virtual Staining in ... [https://www.nature.com/articles/s41597-025-05194-3]
- 52. Semi-Functional Quantitative Flow Cytometry Assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5662780/]
- 53. Quantitative Flow Cytometry to Measure Viral Production ... [https://www.mdpi.com/2076-3417/8/10/1734]
- 54. A comparative study of flow cytometry‐sorted communities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10989988/]
- 55. Imaging Flow Cytometry and Confocal ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2021.749039/full]
- 56. Real-Time, Label-Free Single-Cell Analysis in Cell Therapy [https://www.bioprocessintl.com/sponsored-content/enabling-real-time-label-free-analysis-of-single-cells-a-discussion-on-analytical-needs-in-cell-therapy-manufacturing]
- 57. Label-Free Cellular & Multivariate Analysis Technology [https://www.lumacyte.com/single-cell-analysis-technology/]
- 58. Label-Free Cell Analysis with Laser Force Cytology [https://www.genengnews.com/topics/translational-medicine/label-free-cell-analysis-with-laser-force-cytology/]
- 59. Rapid In-Process Measurement of Live Virus Vaccine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9608199/]
- 60. Beyond Flow Cytometry: How Laser Force Cytology™ is ... [https://www.lumacyte.com/uncategorized/beyond-flow-cytometry-how-laser-force-cytology-is-transforming-cellular-analytics/]
- 61. Light-field flow cytometry for high-resolution, volumetric ... [https://www.nature.com/articles/s41467-024-46250-7]
- 62. Antiviral neutralizing antibodies: from in vitro to in vivo activity [https://www.nature.com/articles/s41577-023-00858-w]
- 63. Different efficacies of neutralizing antibodies and antiviral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9251960/]
- 64. Comparative analysis of neutralization assays performed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502732/]
- 65. Comparative analysis of neutralization assays performed ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1650083/full]
- 66. Comparative Analysis of SARS-CoV-2 Neutralization Titers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362660/]
- 67. Comparative analysis of replication and immune evasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12153290/]
- 68. Comparative duration of neutralizing responses and ... [https://www.nature.com/articles/s41467-025-60024-9]
- 69. A Comparative Analysis of Molecular Biological Methods ... [https://www.mdpi.com/2076-2607/12/1/180]
- 70. Comparison of the Confluence-Initiated Neurogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8615071/]
- 71. How to Measure Cell Confluency [https://www.thermofisher.com/blog/life-in-the-lab/how-to-measure-cell-confluency/]
- 72. Passage Number Effects in Cell Lines [https://www.atcc.org/resources/technical-documents/passage-number-effects-in-cell-lines]
- 73. The effect of cell passage number on osteogenic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4960171/]
- 74. Whole Cell Cross-Linking to Discover Host–Microbe ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.01585/full]
- 75. Cell Passage Number: An Easy Explanation for Biologists [https://bitesizebio.com/13685/cell-culture-passage-number-explained/]
- 76. CROI 2025: Summary of Basic Science Research in HIV - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12324712/]
- 77. High-Throughput Determination of Infectious Virus Titers by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11311753/]
- 78. Quantitative Analysis of Virus Adsorption and Co ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415823/]
- 79. Role of Cell Culture for Virus Detection in the Age of Technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC1797634/]
- 80. In vitro comparison of viral replication and cytopathology ... [https://pubmed.ncbi.nlm.nih.gov/39130731/]
- 81. In Vitro Antiviral Activity of the Fungal Metabolite 6-Pentyl-α ... [https://www.mdpi.com/2306-7381/12/7/634]
- 82. Glass Wool Concentration Optimization for the Detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7090506/]
- 83. Infectivity duration of HCoV-OC43, a surrogate for SARS-CoV ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502581/]
- 84. Methods to detect infectious human enteric viruses in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7106513/]
- 85. Seven-year performance of a clinical metagenomic next- ... [https://www.nature.com/articles/s41591-024-03275-1]
- 86. Slipping under Titer: Why Is My Viral Titer So Low? [https://en.vectorbuilder.com/resources/vector-academy/troubleshooting/low-viral-titer.html]
- 87. EFFECTIVE, LOW TITER, ANTIBODY PROTECTION ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4334439/]
- 88. Virology Culture Guide [https://www.atcc.org/resources/culture-guides/virology-culture-guide]
- 89. What Is Aseptic Technique? 2025 Guide to Infection Control [https://learntastic.com/blog/what-is-aseptic-technique]
- 90. Comparison of traditional aseptic technique versus ... [https://pubmed.ncbi.nlm.nih.gov/40345650/]
- 91. Guideline for testing chemical disinfectants regarding their ... [https://link.springer.com/article/10.1007/s00103-020-03115-w]
- 92. Evaluation of Antiseptic Antiviral Activity of Chemical Agents [https://pmc.ncbi.nlm.nih.gov/articles/PMC7162257/]
- 93. Rapid diagnosis of viral infections and application to infection ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11823-4]
- 94. What is Normalization? The Strategies Employed in Top- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6789750/]
- 95. Robust normalization and transformation techniques for ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02568-9]
- 96. A rapid, high-throughput, viral infectivity assay using ... [https://pubmed.ncbi.nlm.nih.gov/37451651/]
- 97. A Fully Automated High-Throughput Flow Cytometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6055113/]
- 98. Q5A(R2) Viral Safety Evaluation of Biotechnology Products ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q5ar2-viral-safety-evaluation-biotechnology-products-derived-cell-lines-human-or-animal-origin]
- 99. New China CDE guidance on platform validation of viral ... [https://www.parexel.com/insights/blog/new-china-cde-guidance-on-platform-validation-of-viral-clearance-aligns-with-fda-and-ema]
- 100. Virus safety evaluation of biotechnological investigational ... [https://www.ema.europa.eu/en/virus-safety-evaluation-biotechnological-investigational-medicinal-products-scientific-guideline]
- 101. Risk management for viral clearance: A case study on ... [https://pubmed.ncbi.nlm.nih.gov/39137462/]
- 102. Platform Technology in Global Vaccine Regulation [https://www.mdpi.com/2076-393X/12/12/1436]
- 103. Fundamental Strategies for Viral Clearance Part 2 [https://www.bioprocessintl.com/viral-clearance/fundamental-strategies-for-viral-clearance-part-2-technical-approaches]
- 104. Diagnostic performances of common nucleic acid tests for ... [https://www.sciencedirect.com/science/article/pii/S2666524721002147]
- 105. Analytical sensitivity and efficiency comparisons of SARS ... [https://www.nature.com/articles/s41564-020-0761-6]
- 106. Diagnostic accuracy of LAMP versus PCR over the course of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8056478/]
- 107. LAMP-Seq enables sensitive, multiplexed COVID-19 ... [https://www.nature.com/articles/s41587-021-00966-9]
- 108. Evaluation and comparison of one-step real-time PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11232332/]
- 109. Accuracy of a raw saliva-based COVID-19 RT-LAMP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10391658/]
- 110. Comparative Diagnosis of Malaria Infections by Microscopy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2912576/]
- 111. Evaluation and comparison of one-step real-time PCR and ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09574-9]
- 112. Accelerated and Improved Quantification of Lymphocytic ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0037337]
- 113. Chronic LCMV infection regulates the effector T cell ... [https://www.nature.com/articles/s12276-023-00991-5]
- 114. Accelerated and Improved Quantification of Lymphocytic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3355137/]
- 115. AAV-Based Gene Therapy: Opportunities, Risks, and Scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428605/]
- 116. Adeno-Associated Virus Vectors: Principles, Practices, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11861813/]
- 117. Various AAV Serotypes and Their Applications in Gene Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000783/]
- 118. Advances in AAV capsid engineering: Integrating rational ... [https://www.sciencedirect.com/science/article/pii/S1525001625002655]
- 119. Distinct infectivity and neutralization antibody responses in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1554449/full]
- 120. Global seroprevalence of neutralizing antibodies against ... [https://www.sciencedirect.com/science/article/pii/S2329050124000895]
- 121. In vivo applications and toxicities of AAV-based gene ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03893-z]
- 122. Basic Statistical Considerations in Virological Experiments [https://pmc.ncbi.nlm.nih.gov/articles/PMC538531/]
- 123. Statistical evaluations of viral clearance studies for ... [https://www.sciencedirect.com/science/article/abs/pii/S1045105612001170]
- 124. New standards in HER2-low testing: the CASI-01 ... [https://pubmed.ncbi.nlm.nih.gov/40945049/]
- 125. New Findings Show Standard HER2 Assays Miss Key ... [https://www.pharmacytimes.com/view/new-findings-show-standard-her2-assays-miss-key-her2-low-cases]