Ensuring Reliability: A Comprehensive Guide to Viral Assay Precision and Linearity Validation
This article provides a systematic framework for researchers, scientists, and drug development professionals to validate the precision and linearity of viral assays.
Ensuring Reliability: A Comprehensive Guide to Viral Assay Precision and Linearity Validation
Abstract
This article provides a systematic framework for researchers, scientists, and drug development professionals to validate the precision and linearity of viral assays. Covering foundational principles, methodological applications, troubleshooting strategies, and comparative validation techniques, it synthesizes current best practices from diverse assays including microneutralization, digital PCR, and multiplex serology. The content is designed to guide professionals in developing robust, reliable, and regulatory-compliant viral detection and quantification methods essential for vaccine development, viral load monitoring, and clinical diagnostics.
Core Principles: Understanding Precision and Linearity in Viral Assays
Troubleshooting Guide: Validation Parameters for Viral Assays
Q1: What are the key validation parameters I need to evaluate for a quantitative viral assay, and what do they mean?
For a quantitative viral assay, especially one based on qPCR, you must evaluate a core set of parameters to ensure the reliability, accuracy, and precision of your results. These parameters are critical for supporting preclinical and clinical safety assessments [1]. The definitions below are aligned with standards from organizations like the Clinical Laboratory Standards Institute (CLSI).
- Precision: The closeness of agreement (degree of scatter) between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [2]. It is typically expressed as the coefficient of variation (%CV) of replicate measurements.
- Linearity: The ability of the method to obtain test results that are directly proportional to the concentration (amount) of the analyte in the sample within a given range [2]. For qPCR, the relationship is between the log of the concentration and the threshold cycle (Cq) value.
- Lower Limit of Quantification (LLOQ): The lowest amount of measurand in a sample that can be quantitatively determined with stated acceptable precision and stated acceptable accuracy, under stated experimental conditions [3] [2]. It is the lowest point on your standard curve that can be reliably measured.
- Upper Limit of Quantification (ULOQ): The highest amount of analyte in a sample that can be quantitatively determined with acceptable precision and accuracy. It defines the upper end of the linear range of your assay.
Q2: How do I experimentally determine the LLOQ for my qPCR-based viral assay?
The LLOQ should be determined through a replication experiment involving low-concentration samples. The general procedure, as outlined in regulatory guidance, is as follows [3]:
- Prepare Samples: Create a series of samples at low concentrations, bracketing your presumed LLOQ.
- Multiple Replicates: Analyze a minimum of five replicates per concentration level. A higher number of replicates (e.g., 24 or more) will provide a more robust estimate.
- Calculate Precision and Accuracy: For each concentration level, calculate the %CV (precision) and the relative error from the nominal value (accuracy).
- Define Acceptance Criteria: The LLOQ is the lowest concentration level at which both precision (%CV) and accuracy (relative error) meet your pre-defined acceptance criteria (e.g., ±20-25% for both parameters) [3] [2].
It is critical to note that for qPCR, the conventional approach for calculating LoB and LoD using linear measurements and blank samples is not applicable because negative samples do not produce a Cq value, preventing the calculation of a standard deviation. Therefore, the replication-based method described above is the recommended alternative [3].
Q3: My standard curve shows a correlation coefficient (R²) > 0.99, but my low-concentration quality controls are consistently inaccurate. What could be wrong?
A high R² value alone is not a sufficient indicator of a good assay. This discrepancy often points to an issue with the assay's linear range or the validity of the standard curve at the lower end.
- Potential Cause: The standard curve may appear linear by statistical measure, but the performance at the LLOQ may be inadequate. The LLOQ might have been set too low, or there could be matrix effects or inhibition affecting the low-concentration samples specifically.
- Troubleshooting Steps:
- Re-evaluate LLOQ: Re-perform the LLOQ validation experiment as described in Q2. Ensure that at your claimed LLOQ, both precision and accuracy meet acceptance criteria with the required number of replicates.
- Check for Inhibition: Spike a known low concentration of the target into your sample matrix and compare the recovery to the same concentration in a clean buffer. A significant drop in recovery indicates matrix interference [1].
- Verify Standard Integrity: Ensure that the standard used for the low-concentration points has been properly diluted and has not degraded.
- Inspect Amplification Plots: Manually examine the amplification curves of your low-concentration standards and QCs. Look for abnormal curve shapes or high variability in Cq values, which can indicate issues with amplification efficiency at low target levels.
Q4: How do I establish the linear range and ULOQ for my assay?
The linear range is established by running a standard curve with a minimum of five concentrations that bracket the expected range of your samples, from below the LLOQ to above the ULOQ [2].
- Prepare Standard Curve: A dilution series of the reference standard (e.g., a plasmid with the target sequence or calibrated genomic DNA) is analyzed [1] [4].
- Perform Regression Analysis: The Cq values are plotted against the logarithm of the nominal concentration. A regression analysis is performed on the data points [1].
- Assess Linearity: The linear range is the interval over which the relationship between Cq and log(concentration) is linear. This is assessed by the correlation coefficient and the visual inspection of the standard curve.
- Determine ULOQ: The ULOQ is the highest concentration standard that still falls within the linear range and for which precision and accuracy (like those at the LLOQ) meet the acceptance criteria. Concentrations above the ULOQ may show signal saturation or a significant drop in precision and accuracy.
A well-performing qPCR assay typically has a linear dynamic range spanning several orders of magnitude (e.g., 5-6 logs) with a PCR efficiency between 90% and 110%, which corresponds to a standard curve slope between -3.6 and -3.1 [1].
Q5: How can I improve the precision of my viral load measurements?
Poor precision (high %CV) can stem from multiple sources. A systematic check is required.
- Pipetting Errors: Use calibrated pipettes and ensure technicians are trained. Use master mixes to minimize pipetting steps.
- Reagent Inhomogeneity: Ensure all reagents are thoroughly mixed and aliquoted consistently.
- Inhibition: Co-purified inhibitors from the sample matrix (e.g., heme from blood, components in respiratory fluids) can cause variability. Include an internal positive control (IPC) spiked into each sample to detect inhibition [4].
- Primer/Probe Quality: Ensure primers and probes are of high quality, have high specificity, and are used at optimal concentrations. Probe-based qPCR is generally recommended over dye-based methods for superior specificity in regulated studies [1].
- Instrument Calibration: Ensure the real-time PCR instrument is properly calibrated for the fluorophores you are using.
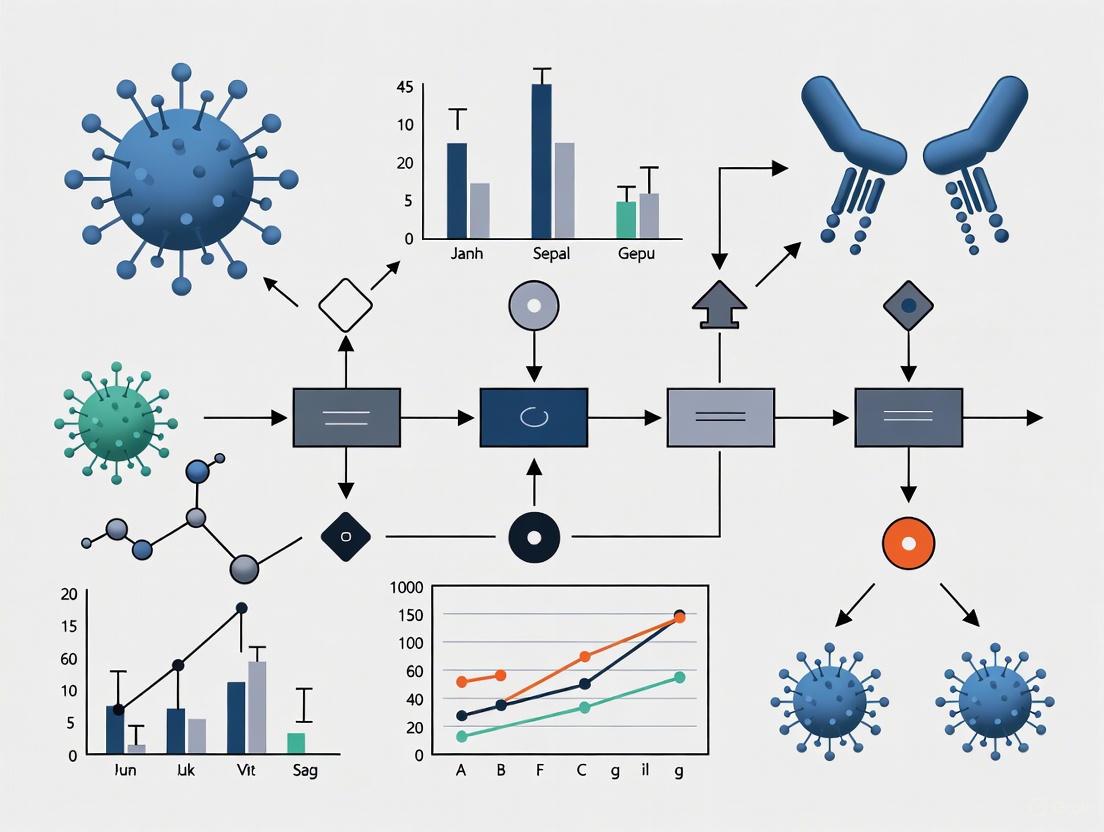
The following workflow can help you systematically diagnose and address precision issues:
The table below summarizes the core validation parameters, their experimental protocols, and typical acceptance criteria for a qPCR-based viral assay.
Table 1: Key Validation Parameters for Viral qPCR Assays
| Parameter | Experimental Protocol | Key Acceptance Criteria |
|---|---|---|
| Precision [2] | Analyze a minimum of five replicates of at least three concentrations (low, medium, high QC levels) within a single run (repeatability) and across different runs/days/analysts (intermediate precision). | CV ≤ 25% (at LLOQ) and ≤ 20% at other levels. Variance in inter-run precision should be comparable to intra-run variance [2]. |
| Linearity [1] [2] | Analyze a standard curve with a minimum of five concentration levels, serially diluted, covering the entire expected range. Plot Cq values vs. log10(concentration). | Correlation coefficient (R²) ≥ 0.99. PCR efficiency (E) between 90%–110% (slope of -3.6 to -3.1) [1]. Visual inspection of residuals. |
| LLOQ [3] [2] | Analyze at least five replicates of several low-concentration samples. The lowest concentration where both precision and accuracy are acceptable is the LLOQ. | Precision (CV) and accuracy (relative error) within ±20-25% [3]. The target should be detected in ≥95% of replicates (for LoD) [3]. |
| ULOQ | The highest standard in the dilution series that still falls within the linear range and meets precision/accuracy criteria. | Precision (CV) and accuracy within ±20-25%. No signal saturation or significant deviation from the standard curve's linear regression. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful validation of a viral assay relies on high-quality, well-characterized reagents. The following table lists essential materials and their functions.
Table 2: Essential Reagents for Viral qPCR Assay Validation
| Reagent / Material | Function | Example / Note |
|---|---|---|
| Reference Standard [1] [4] | A well-quantified material used to construct the standard curve for absolute quantification. | Plasmid DNA, in vitro transcribed RNA, or calibrated genomic DNA (e.g., NIST standard). Should be sequence-verified. |
| Primers & Probe [1] [5] | Sequence-specific oligonucleotides for target amplification and detection. | Probe-based (e.g., TaqMan) is recommended for superior specificity in regulated studies. Primers should be designed to avoid cross-reaction with host DNA [1]. |
| qPCR Master Mix | A pre-mixed solution containing DNA polymerase, dNTPs, buffers, and salts. | Includes a hot-start enzyme to prevent non-specific amplification. May contain uracil-DNA glycosylase (UDG) to prevent carryover contamination [5]. |
| Matrix DNA / gDNA [1] | DNA extracted from naive (untreated) host tissue. | Added to standard and QC samples to mimic the composition of actual test samples and account for potential PCR inhibition. |
| Quality Control (QC) Samples [6] | Samples of known concentration used to monitor assay performance during validation and routine use. | Prepared at low, medium, and high concentrations. Can be diluted reference standard or independently prepared controls [6]. |
| Internal Positive Control (IPC) | A control target spiked into each sample to check for PCR inhibition. | Can be a non-competitive synthetic sequence or a control gene. Abnormal Cq values in the IPC indicate inhibition in the sample [4]. |
The Critical Role of Precision in Viral Load and Neutralization Assays
FAQs and Troubleshooting Guides
What are the key parameters to validate for a precise viral load or neutralization assay?
For both viral load and neutralization assays, rigorous validation is essential. The table below summarizes the core parameters and their performance targets, derived from established laboratory practices and recent publications [7] [8] [9].
| Validation Parameter | Typical Performance Target | Example from Literature |
|---|---|---|
| Linear Range | Correlation coefficient (R²) > 0.99 [7] [9] | HIV-2 assay: 10–1,000,000 copies/mL (R² >0.99) [7] |
| Limit of Detection (LoD) | Consistent detection at the lowest concentration [7] [9] | HIV-1 C subtype SYBR Green assay: 50 copies/mL [9] |
| Precision (Intra-assay) | Low standard deviation (SD) and coefficient of variation (CV) [7] | HIV-2 assay: Intra-run SD of 0.093 at 1.7 log₁₀ copies/mL [7] |
| Precision (Inter-assay) | Consistent results across different runs and operators [7] | HIV-2 assay: Inter-run SD of 0.162 [7] |
| Specificity | No cross-reactivity with related viruses or host material [7] [9] | HIV-2 assay: No cross-reaction with HIV-1, even at high concentrations [7] |
| Robustness | Tolerates minor variations in incubation time, reagent lots, and freeze-thaw cycles [10] | Measles pseudovirus assay: Performance stable despite variations in incubation time and freeze-thaw cycles [10] |
My neutralization assay shows high variability. What are the most common causes and solutions?
High variability often stems from inconsistencies in biological materials or protocol execution. Here are specific issues and their remedies:
- Problem: Inconsistent Cell Culture Health and Passage Number.
- Solution: Standardize cell culture conditions rigorously. Use low-passage cells and ensure consistent viability and confluence at the time of assay setup. The genetic instability of tumor-derived cell lines like HeLa can significantly impact results, so standardizing passage number and culture conditions is critical [11].
- Problem: Unoptimized Critical Reagent Concentrations.
- Solution: Systematically titrate key reagents like virus input and serum incubation time. For example, the smallpox PRNT50 assay was optimized using a virus concentration of 4 × 10² plaque-forming units/mL and a neutralization time of 60 minutes [8]. Record lot numbers for all reagents, as antibody quality can vary considerably between batches [11].
- Problem: Inaccurate Data Interpretation from Incomplete Dilution Series.
- Solution: Implement a robust statistical framework. The CoreTIA framework uses a Bayesian analysis pipeline (Hill-MCMC) to reliably estimate the ND50 (50% neutralization dose) even when dilution series are incomplete, reducing the need for repeat testing and saving sample [12].
How can I improve the efficiency of high-throughput viral load testing without sacrificing accuracy?
Pooled testing is a validated strategy to increase efficiency in populations with low positivity rates, such as routine monitoring of HIV patients on antiretroviral therapy.
- Principle: Specimens are tested in pools. If a pool is negative, all individual specimens in it are reported as negative. Only pools that test positive are reflexed to individual testing [13].
- Efficiency Gain: A study in Cameroon testing pools of three used only 6,797 assays to report results for 12,396 specimens—an efficiency of 0.55 assays per result. This enabled an 80% increase in testing capacity [13].
- Accuracy Consideration: While pooling dilutes individual samples, its impact on clinical accuracy is minimal for viral load monitoring. In the Cameroon study, the limit of detection per specimen increased from <40 copies/mL to <120 copies/mL, but an estimated only 0.01% of unsuppressed specimens (≥1,001 copies/mL) were misclassified as suppressed [13]. This demonstrates robust performance for identifying treatment failure.
My assay fails to detect the target virus or shows weak signal. What should I check?
- Confirm Primer/Probe Specificity: Assays designed for one viral subtype may underperform for others. An HIV-1 viral load assay optimized for Indian subtype C strains demonstrated superior detection of local isolates compared to two commercial kits that failed to amplify 10-13% of samples [9].
- Verify Sample Integrity: While some viral RNAs like HIV-1 are stable at ambient temperature for a limited time [9], establish strict sample handling and storage protocols to prevent degradation.
- Validate Pseudovirus Function: For neutralization assays using pseudotyped viruses, always confirm infectivity in your specific cell line. A measles pseudovirus study showed infectivity was highly dependent on the cell line used, working best in cells expressing the specific receptor SLAM [10].
Why is precise linearity validation critical for viral assays?
Precise linearity ensures that the assay provides a truthful and proportional measurement across the entire range of expected viral concentrations. This is non-negotiable for clinical and research decision-making.
- Accurate Quantification: A linear response (R² > 0.99) allows for confident interpolation of unknown sample concentrations from a standard curve [7] [9].
- Clinical Relevance: In HIV care, a 0.5 log change in viral load is considered clinically significant. Imprecise assays risk misclassifying patient status. One study found that commercial assays underestimated the viral load by >0.5 log in 4-8% of samples compared to a validated test [9].
- Reliable Serostatus Assessment: In measles serology, a robust pseudovirus neutralization assay showed that vaccination induced high geometric mean titers (GMT) that persisted in children, crucial data for informing public health vaccination policies [10].
Experimental Protocols for Key Assays
Protocol: Pseudotyped Virus Neutralization Assay for Measles Antibodies
This high-throughput method allows for the sensitive detection of neutralizing antibodies against multiple circulating measles virus genotypes [10].
Workflow Overview:
Detailed Steps:
Cell Preparation:
- Seed an appropriate cell line (e.g., 293T-SLAM for measles) in a 96-well plate at a density determined during assay optimization [10]. Allow cells to adhere overnight.
Serum-Pseudovirus Incubation:
- Prepare serial dilutions of the test serum samples.
- Mix a fixed volume of each serum dilution with a pre-titered amount of the measles pseudotyped virus (expressing a luciferase reporter).
- Incubate the serum-virus mixtures for a standardized time (e.g., 1 hour) at 37°C to allow neutralization.
Infection:
- Remove the growth medium from the prepared cells.
- Add the serum-virus mixtures to the cells. Include controls: virus-only control (0% neutralization) and cell-only control (100% neutralization/background).
Incubation and Detection:
- Incubate the plates for the determined period (e.g., 24-48 hours).
- After incubation, lyse the cells and quantify the luciferase activity using a luminometer.
Analysis:
- Calculate the percentage neutralization for each serum dilution:
(1 - (Sample Luminescence / Virus-only Control Luminescence)) * 100. - The neutralization titer (NT50) is the serum dilution that inhibits 50% of the luciferase signal. This can be calculated using a sigmoidal dose-response model [10].
- Calculate the percentage neutralization for each serum dilution:
Protocol: Plaque Reduction Neutralization Test (PRNT) for Smallpox Vaccines
The PRNT is a gold-standard method for quantifying neutralizing antibodies against vaccinia virus (VACV) and assessing vaccine immunogenicity [8].
Workflow Overview:
Detailed Steps:
Virus and Cell Preparation:
- Prepare a working stock of vaccinia virus (VACV) at a concentration of 4 × 10² plaque-forming units (PFU)/mL [8].
- Grow a confluent monolayer of susceptible cells (e.g., Vero cells) in a multi-well plate.
Neutralization Reaction:
- Prepare two-fold or four-fold serial dilutions of the test serum.
- Combine equal volumes of each serum dilution with the prepared virus suspension.
- Incubate the mixture at 37°C for 60 minutes to allow neutralization.
Plaque Formation:
- Remove the growth medium from the cell monolayers.
- Inoculate the serum-virus mixtures onto the cells. Include virus control wells (virus without serum).
- Adsorb the virus for a specified time (e.g., 1 hour) at 37°C, with occasional rocking.
- After adsorption, overlay the cells with a semi-solid medium (e.g., 1% carboxymethylcellulose) to prevent viral spread through the liquid medium, ensuring discrete plaque formation.
- Incubate the plates for 3 days at 37°C with 5% CO₂ [8].
Plaque Visualization and Counting:
- After incubation, remove the overlay and stain the cells with crystal violet solution. Live cells will stain, while areas of infection (plaques) will appear as clear zones.
- Count the plaques in each well.
Analysis:
- The PRNT50 is the serum dilution that reduces the number of plaques by 50% compared to the virus control wells. This can be determined by plotting the percentage plaque reduction against the serum dilution and interpolating the 50% endpoint [8].
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Critical Function | Considerations for Precision |
|---|---|---|
| Pseudotyped Viruses [10] | Safe, high-throughput surrogate for wild-type virus in neutralization assays. | Must be titrated to optimal infectious units; receptor specificity must match cell line [10]. |
| Cell Lines with Defined Receptors [10] | Platform for virus infection and neutralization. | Use low-passage, well-characterized stocks (e.g., 293T-SLAM). Cell passage number and health are major sources of variability [11]. |
| International Standard (WHO/NIBSC) [7] | Calibrator to harmonize results across labs and assays. | Essential for traceability and accuracy. The HIV-2 standard was critical for validating the novel assay [7]. |
| Internal Control (IC) RNA [7] | Monitors RNA extraction and amplification efficiency; identifies inhibition. | Should be non-competitive and added at a known concentration before extraction to control for technical variability [7]. |
| Reference Panels [9] | Validate assay performance, sensitivity, and specificity. | Composed of well-characterized samples with known status/titer; used for inter-assay precision testing [9]. |
| Critical Buffers & Additives (e.g., Poly-L-lysine) [12] | Enhance cell adhesion and consistency of monolayer formation. | Standardized coating procedures are necessary for robust and reproducible cell-based assays [12]. |
Establishing Analytical Sensitivity and Specificity for Viral Targets
Troubleshooting Guides
Common Issues in Viral Assay Validation
Problem: Inconsistent results across replicates
- Potential Causes: Inconsistent pipetting technique, inadequate mixing of reagents, or plate stacking during incubation leading to uneven temperature distribution [14].
- Solutions: Calibrate pipettes regularly and ensure tips are properly sealed. Mix all reagents and samples thoroughly before use. Avoid stacking plates during incubations to ensure even heat distribution [14].
Problem: Weak or no signal detection
- Potential Causes: Reagents not equilibrated to assay temperature, omission of protocol steps, or incorrectly stored/expired reagents [15].
- Solutions: Equilibrate all reagents (except enzymes) to room temperature before use. Carefully follow protocol instructions and check expiration dates of all reagents [15].
Problem: Non-linear standard curve
- Potential Causes: Pipetting errors during serial dilution, incorrect calculations, or precipitate formation in wells [15].
- Solutions: Remake standard dilutions with careful pipetting. Check calculations and fitting equations specified in the datasheet. Inspect wells for precipitates or bubbles [15].
Problem: High background noise or false positives
- Potential Causes: Inadequate washing leaving unbound antibody, contamination from cross-reacting substances, or insufficient assay specificity [14] [16].
- Solutions: Ensure complete washing steps between incubations. Validate assay specificity against closely related viral strains. Include appropriate controls to identify contamination [17] [16].
Precision Performance Across Different Assay Platforms
Table: Precision Ranges for Various Viral Detection Assays
| Assay Type | Intra-Assay CV Range | Inter-Assay CV Range | Inter-Operator CV Range | Optimal Response Level |
|---|---|---|---|---|
| Tetramer Assay | 4%-15% [18] [19] | 5%-18% [19] | 5%-20% [19] | >0.25% CD8+ T cells [19] |
| Cytokine Flow Cytometry | 5%-20% [18] [19] | 10%-30% [19] | 15%-35% [19] | >0.25% CD8+ T cells [19] |
| ELISPOT | 10%-133% [18] [19] | 25%-60% [19] | 30%-60% [19] | >30 SFC/2.5×10⁵ PBMC [19] |
| Multiplex PCR | 4%-20% [17] | 10%-25% [17] | 15%-30% [17] | 10-400 copies/μL [17] |
Establishing Acceptance Criteria for Validation Parameters
Table: Recommended Acceptance Criteria for Analytical Method Validation
| Validation Parameter | Recommended Acceptance Criteria | Basis for Criteria |
|---|---|---|
| Specificity | Excellent: ≤5% of tolerance; Acceptable: ≤10% of tolerance [20] | Percentage of specification tolerance consumed by method error [20] |
| Repeatability | Analytical methods: ≤25% of tolerance; Bioassays: ≤50% of tolerance [20] | Control of out-of-specification (OOS) rates [20] |
| Bias/Accuracy | ≤10% of tolerance for both analytical methods and bioassays [20] | Alignment with product specification limits [20] |
| LOD | Excellent: ≤5% of tolerance; Acceptable: ≤10% of tolerance [20] | Risk-based approach relative to product specification [20] |
| LOQ | Excellent: ≤15% of tolerance; Acceptable: ≤20% of tolerance [20] | Risk-based approach relative to product specification [20] |
| Linearity | R² ≥0.85-0.99 depending on assay type [18] [19] | Demonstrated linear response across 80-120% of specification range [20] |
Frequently Asked Questions (FAQs)
Q: What are the key differences between establishing sensitivity for molecular vs. immunological viral assays? Molecular assays (such as PCR) typically define sensitivity as the lowest copy number detected 95-100% of the time, with values ranging from 1.2-1280.8 copies/μL depending on the platform and target [21]. Immunological assays (such as ELISPOT or flow cytometry) express sensitivity relative to cell percentages, with precision highly dependent on response levels (CVs from 4% to 133%) [18] [19]. The fundamental difference lies in the units of measurement and the inherent variability of cellular systems versus nucleic acid detection.
Q: How should we determine appropriate sample sizes for validation studies? For precision studies, a minimum of 6 replicates per assay is recommended for intra-assay precision, with 8 assays performed on different days for inter-assay precision [18] [19]. For linearity studies, 7 replicates at each concentration across a dilution series provides sufficient statistical power [21]. These sample sizes allow for reliable calculation of standard deviation and coefficient of variation while accounting for normal experimental variability.
Q: What strategies can improve detection sensitivity in multiplex viral assays? Several approaches can enhance sensitivity: (1) Incorporation of target enrichment steps, such as multiplexed RT-PCR amplification prior to detection [17]; (2) Depletion of host background nucleic acids using ribosomal RNA probes [16]; (3) Optimization of hybridization conditions and signal amplification [17]; (4) Using advanced detection technologies such as electrochemical sensing or high-throughput microscopy [17] [22]. The choice depends on the specific platform and viral targets.
Q: How do we handle validation when reference standards are not available? When formal reference standards are unavailable, the recommended approach includes: (1) Creating in-house standards using characterized viral isolates or synthetic constructs [21]; (2) Using percent recovery calculations relative to theoretical concentrations [20]; (3) Establishing interim specifications based on clinical relevance until formal standards are obtained [20]; (4) Collaborating with other laboratories to harmonize approaches [14].
Q: What criteria define successful linearity in viral assay validation? Linearity success criteria include: (1) R² values ≥0.85-0.99 depending on the assay type [18] [19]; (2) No systematic pattern in residuals from regression analysis [20]; (3) No statistically significant quadratic effect in evaluation of residuals [20]; (4) Demonstration of linear response across at least 80-120% of the product specification range or intended operating range [20].
Experimental Protocols & Workflows
Comprehensive Assay Validation Protocol
Protocol 1: Establishing Analytical Sensitivity and Precision
This protocol provides a standardized approach for determining limit of detection (LOD) and precision parameters for viral assays.
Materials Required:
- Viral standards or isolates with known concentrations [21]
- Appropriate cell lines or matrix for dilution series [21] [19]
- Assay-specific reagents and equipment [17]
- Statistical software for data analysis
Procedure:
- Prepare Standard Dilutions: Create a dilution series spanning the expected detection range. For nucleic acid-based assays, use plasmid DNA with confirmed copy numbers [21]. For cellular assays, use PBMC from characterized donors [19].
Determine LOD: Test 7 replicates at each concentration, using both nuclease-free water and relevant biological matrix as diluents. The LOD is the lowest concentration detected 95-100% of the time [21].
Assess Precision:
Calculate Validation Parameters:
Establish Acceptance: Compare calculated parameters against predefined acceptance criteria (see Table 2) [20].
Viral Assay Validation Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Research Reagent Solutions for Viral Assay Validation
| Reagent/Material | Function in Validation | Application Examples | Critical Storage Parameters |
|---|---|---|---|
| Characterized Viral Standards | Reference material for sensitivity and linearity studies | RRV, UMAV, Influenza isolates for spiking experiments [21] [16] | Temperature varies by virus; aliquot to avoid freeze-thaw cycles |
| Plasmid DNA Controls | Quantitative standards for molecular assays | pCR2.1 vectors with viral inserts for copy number determination [21] | -20°C or -80°C in nuclease-free TE buffer |
| Custom rRNA Depletion Probes | Host background reduction for metatranscriptomics | Mosquito-specific rRNA probes for arbovirus surveillance [16] | -20°C; protect from light and nucleases |
| Multiplex PCR Master Mixes | Simultaneous amplification of multiple viral targets | Influenza Panel (5 types) and Respiratory Panel (14 viruses) [17] | -20°C; multiple freeze-thaw cycles to be avoided |
| Hybridization Buffers & Signal Probes | Target detection in multiplex systems | Ferrocene-labeled probes for electrochemical detection [17] | Temperature varies by formulation; often 4°C protected from light |
| Reference Biological Matrices | Diluent for assessing matrix effects | Characterized PBMC, pooled negative sera, clarified mosquito homogenates [19] [16] | Cryopreservation at -80°C or liquid nitrogen |
| Quality Control Materials | Monitoring assay performance over time | Cryopreserved PBMC with low/medium/high response levels [19] | Consistent cryopreservation protocol; avoid temperature fluctuations |
Statistical Foundations for Assay Validation and Acceptance Criteria
Frequently Asked Questions (FAQs)
FAQ 1: What are the key statistical parameters used to define assay linearity, and what are their typical acceptance criteria?
Linearity confirms that an analytical method produces results proportional to the analyte concentration across a specified range. The evaluation involves several statistical parameters and acceptance criteria, summarized in the table below.
Table 1: Key Statistical Parameters for Linearity Validation
| Parameter | Description | Typical Acceptance Criteria |
|---|---|---|
| Coefficient of Determination (R²) | Measures the proportion of variance in the measured concentration explained by the expected concentration. | R² > 0.995 [23] |
| Slope | The slope of the regression line (on a log scale for bioassays) indicates how measured potency changes relative to expected potency. | A slope of 1.0 indicates perfect proportionality. Confidence Intervals (CI) for the slope should be contained within a pre-defined Equivalence Acceptance Criterion (EAC) [24] [25]. |
| Intercept | The y-intercept of the regression line indicates constant bias. | An intercept of 0 indicates no constant bias. CI for the intercept should be contained within a pre-defined EAC [24] [25]. |
| Residual Plots | Visual assessment of the differences between observed and predicted values. | Residuals should be randomly scattered around zero with no discernible patterns [23]. |
FAQ 2: How do I establish acceptance criteria for assay accuracy and precision?
Accuracy (closeness to the true value) and Precision (closeness of repeated measurements) are fundamental. A modern approach involves setting criteria based on the probability of an Out-Of-Specification (OOS) result.
- Accuracy is expressed as %Relative Bias (%RB) [25].
- Precision is measured as the %Coefficient of Variation (%CV) for intermediate precision [24] [25].
- Setting Criteria: Acceptance criteria are defined for the 90% Confidence Intervals (CIs) of %RB and %CV. These CIs must fall within pre-set limits for the assay to be considered valid [24] [25].
- Total Analytical Error (TAE): The updated USP <1033> guidance suggests using TAE, which statistically combines accuracy and precision into a single acceptance criterion linked to the probability of an OOS result. This provides a more holistic check of assay validity [25].
FAQ 3: What is the difference between validating an FDA-approved test and a laboratory-developed test (LDT)?
The Clinical Laboratory Improvement Amendments (CLIA) regulations mandate different levels of validation depending on the test's origin, particularly for the Reportable Range (linearity) and Analytical Sensitivity (Limit of Detection).
Table 2: Key Validation Requirement Differences: FDA-Approved vs. Laboratory-Developed Tests
| Performance Characteristic | FDA-Approved/Cleared Test | Laboratory-Developed Test |
|---|---|---|
| Reportable Range (Linearity) | Verify using 5-7 concentrations across the stated linear range, with 2 replicates at each concentration [26]. | Establish using 7-9 concentrations across the anticipated range; 2-3 replicates at each concentration [26]. |
| Analytical Sensitivity (LoD) | Not required by CLIA, though CAP requires verification for quantitative assays [26]. | Establish with ~60 data points (e.g., 12 replicates from 5 samples) near the expected detection limit, conducted over 5 days [26]. |
| Precision | Verify per manufacturer's claims, typically testing controls over 20 days [26]. | Establish with a minimum of 3 concentrations tested in duplicate over 20 days [26]. |
| Analytical Specificity | Not required by CLIA [26]. | Must establish by testing for interference from substances like hemolysis, lipemia, and genetically similar organisms [26]. |
Troubleshooting Guides
Problem 1: Poor Linearity (Low R² or Non-Random Residuals)
Potential Causes and Solutions:
- Cause: Inappropriate Concentration Range
- Solution: Ensure the calibration range brackets the expected sample concentrations. A common approach is to prepare at least five concentration standards from 50% to 150% of the target range [23].
- Cause: Matrix Effects
- Cause: Instrument Saturation or Low Signal
- Solution: Verify the analytical method's dynamic range. Detector saturation can flatten responses at high concentrations, while low signals at the range's end can increase variability [23].
Problem 2: Failing Accuracy or Precision Acceptance Criteria
Potential Causes and Solutions:
- Cause: High Imprecision (%CV)
- Cause: High Relative Bias (%RB)
- Solution: Check the calibration standards for accuracy and degradation. Evaluate potential interference from the sample matrix using a recovery study, where a known amount of analyte is spiked into the matrix and the measured value is compared to the expected value [27].
- Cause: Overly Strict Acceptance Criteria
- Solution: Use a statistical performance approach. Simulated data can show the likelihood of meeting all validation criteria for a given level of assay precision (%CV). This helps subject matter experts set realistic, statistically sound acceptance criteria [24].
Experimental Protocols & Workflows
Protocol for a Linearity and Range Experiment
This protocol is adapted from established guidelines for method validation [23] [27].
1. Preparation of Standards:
- Prepare a minimum of five concentration levels over the claimed range of the assay (e.g., 50%, 75%, 100%, 125%, 150% of the target concentration).
- Each concentration should be prepared in triplicate to assess variability.
- Standards should be prepared in the same matrix as the intended samples (e.g., blank serum, buffer) to control for matrix effects.
2. Analysis:
- Analyze all samples in a random run order to prevent systematic bias.
- Follow the established assay procedure meticulously.
3. Data Analysis:
- Plot the measured concentration (or response) against the expected concentration.
- Perform a linear regression analysis to determine the R², slope, and intercept.
- Examine the residual plot (difference between observed and predicted values vs. expected concentration). The residuals should be randomly scattered around zero.
4. Interpretation:
- The linearity is accepted if the R² meets the acceptance criterion (e.g., >0.995), and the confidence intervals for the slope and intercept fall within the pre-defined EAC. The residual plot should show no obvious patterns [24] [23].
Protocol for a Precision Experiment
This protocol follows the principles outlined in validation guides [27] [26].
1. Sample Preparation:
- Select a minimum of two concentrations (high and low) of quality control (QC) samples within the quantitative range.
- These QC samples should be aliquoted and stored appropriately to ensure stability throughout the testing period.
2. Experimental Design:
- Analyze the QC samples in duplicate or triplicate over at least 5 separate operating days.
- This design allows for the calculation of both within-run (repeatability) and between-run (intermediate precision) variation.
3. Data Analysis:
- Calculate the mean, standard deviation (SD), and coefficient of variation (%CV) for the results at each concentration.
- The total imprecision can be calculated by pooling the data from all runs.
4. Interpretation:
- The %CV for repeatability and intermediate precision is compared against pre-defined acceptance criteria. These criteria are often based on the required performance for the assay's intended use [27].
Diagram 1: Assay Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Viral Load Assay Validation
| Item | Function / Application | Example from Literature |
|---|---|---|
| Certified Reference Materials | Provides an analyte of known concentration and quality for calibrating assays, determining accuracy, and establishing the standard curve. | Commercial reference materials from national metrology institutes (e.g., Chinese National Institute of Metrology) were used to validate an RT-ddPCR assay [28]. |
| Inactivated Virus Stocks | Used for specificity testing and as a positive control to ensure the assay detects the intended target without cross-reacting with similar organisms. | Inactivated pathogens (e.g., Parainfluenza virus, Adenovirus) were used to assess the analytical specificity of a multiplex respiratory virus assay [28]. |
| Extraction Kits | Isolate and purify nucleic acids (DNA/RNA) from complex biological matrices (e.g., blood, swabs) for subsequent molecular detection. | The QIAamp DNA Mini Kit was used to extract orthopoxvirus DNA from non-human primate blood in a validated PCR assay [29]. |
| One-Step RT-ddPCR Master Mix | An all-in-one reagent for reverse transcription and digital PCR amplification, enabling absolute quantification of RNA viruses without a standard curve. | The One-Step RT–ddPCR Advanced Kit for Probes was used in an automated high-throughput quadruplex assay for respiratory viruses [28]. |
| Primers & Probes | Specifically designed oligonucleotides that bind to and fluorescently label the target viral gene sequence for detection and quantification. | Primers and probes targeting the matrix protein (M) gene of influenza A and RSV, and the ORF1ab of SARS-CoV-2 were synthesized for a quadruplex assay [28]. |
For researchers and drug development professionals, navigating the regulatory landscape for assay validation is crucial for the success of clinical trials and market approval. Assay validation provides the objective evidence that an analytical method is fit for its intended purpose, ensuring the reliability and reproducibility of data submitted to regulatory agencies. The core principles of validation—including accuracy, precision, specificity, and linearity—are universally acknowledged, yet the implementation guidelines can vary between major regulatory bodies like the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the International Council for Harmonisation (ICH) [30] [31] [27].
Understanding the nuances between these guidelines is particularly critical for advanced applications, such as viral assays in vaccine development or biomarker quantification, where measuring endogenous analytes presents unique challenges that differ from traditional pharmacokinetic studies [30] [32]. This technical support center is designed to help you troubleshoot specific issues and implement validation strategies that meet global regulatory standards.
The table below summarizes the core guidelines and their primary focus from the FDA, EMA, and ICH. This overview helps in understanding the foundational documents for assay validation.
| Regulatory Body | Key Guideline(s) | Primary Focus & Scope |
|---|---|---|
| FDA | 2025 Biomarker Assay Validation Guidance [30] | Clarifies that ICH M10 for drug assays is a starting point, but biomarker assays require different approaches for endogenous analytes [30]. |
| 21 CFR Part 11 [31] | Requirements for electronic records and electronic signatures. | |
| EMA | Annex 11 (EU GMP) [31] | Detailed requirements for computerized systems validation. |
| Guideline on virus safety (EMEA/CHMP/BWP/398498/2005) [33] | Viral safety evaluation of biotechnological investigational medicinal products. | |
| ICH | ICH Q2(R1) [32] | Validation of Analytical Procedures: Text and Methodology. |
| ICH Q5A(R2) [33] | Viral Safety Evaluation of Biotechnology Products. | |
| ICH E6(R3) [34] | Good Clinical Practice (effective January 2025). |
Troubleshooting Common Assay Validation Issues
FAQ: Precision and Linearity
Q: Our viral copy-number assay (ddPCR) is showing high variability (%CV) between replicate measurements. How can we improve precision and demonstrate acceptable linearity?
A: High precision is critical for assays used in potency determination, such as viral titer assays [32]. To troubleshoot precision and linearity:
- Review Your Reference Standard: For viral copy-number assays, consider using a well-qualified hybrid amplicon as a reference control. A synthetic DNA fragment containing the target amplicons (e.g., WPRE and RPP30) can be a robust and reproducible alternative to traditional plasmids or cell lines, improving both precision and accuracy [35].
- Assess the Entire Range: Systematically test the precision across the assay's entire range of quantification. The assay should be tested with "varying amount of input DNA" to establish the upper limit, lower limit, and, crucially, the linearity of the response [35].
- Statistically Evaluate Linearity: Avoid simply comparing point estimates to a pre-specified limit. Use robust statistical methods like the Two One-Sided Tests (TOST) procedure to prove linearity, as older methods may inflate type I error rates and lead to incorrect conclusions [36].
- Document Conditions: Ensure intermediate precision (e.g., between-run, between-day) is thoroughly investigated by varying factors like analyst, equipment, and day, and clearly state these conditions in your validation report [27].
FAQ: Platform Validation for Viral Clearance
Q: We are developing a new monoclonal antibody. For an early-phase clinical trial application, can we use platform validation data for viral clearance instead of product-specific validation?
A: Yes, platform validation is increasingly accepted by global regulators, but specific conditions must be met. The recent China CDE Guideline (Jan 2024), which aligns with FDA and EMA principles, states that platform validation can be used in early-phase trials if [33]:
- The process module is based on sufficient prior data (e.g., validation results from 3-5 related products with similar characteristics and processes).
- Assay methods with the same principles are used.
- Critical process parameters do not exceed the worst-case conditions of the platform.
- For virus filtration, at least one product-specific validation study using parvovirus must be conducted.
The underlying principle, echoed in ICH Q5A(R2), is a comprehensive understanding of the mechanisms of viral clearance for the unit operation and a comparison of the biochemical properties of the products [33].
FAQ: Biomarker Assay Validation
Q: The new 2025 FDA Biomarker Guidance references ICH M10. Does this mean our biomarker ligand-binding assays must now be validated exactly like PK assays?
A: No, this is a common misconception. The 2025 guidance states that the approach for drug assays (ICH M10) should be the starting point, but it explicitly recognizes that biomarker assays require different considerations [30]. The fundamental difference is that biomarker assays measure endogenous analytes, which makes the technical approach distinct from the spike-recovery methods used for drug concentration assays [30].
Your validation must demonstrate suitability for measuring the endogenous analyte. While you will still investigate parameters like accuracy, precision, and parallelism, the technical execution should be adapted. The European Bioanalysis Forum (EBF) emphasizes that biomarker assays benefit more from Context of Use (CoU) principles than a strict PK SOP-driven approach [30].
FAQ: Managing Validation Throughout the Product Lifecycle
Q: How do we maintain a validated state for a commercial product, and what are the key differences between FDA and EMA expectations for ongoing verification?
A: Both agencies view validation as a lifecycle activity, but their emphasis differs. The following table compares their approaches to continued process verification, a concept that also applies to analytical methods.
| Aspect | FDA (Continued Process Verification - CPV) | EMA (Ongoing Process Verification - OPV) |
|---|---|---|
| Focus | Data-driven, real-time statistical process control and trend analysis [37]. | Based on real-time or retrospective data, often incorporated into Annual Product Quality Reviews [37]. |
| Documentation | Does not mandate a Validation Master Plan (VMP) but expects a structured, equivalent document [37]. | Requires a Validation Master Plan (VMP) to outline the scope, responsibilities, and timeline [37]. |
| Batch Requirements | Recommends a minimum of 3 consecutive successful batches for Process Qualification [37]. | Does not mandate a specific number; requires a scientific justification based on risk [37]. |
Essential Experimental Protocols
Protocol for Precision Validation
This protocol is based on established methodologies for immunoassay and viral assay validation [27] [32].
1. Define Experiment Levels: - Repeatability (Intra-assay): Analyze the same sample multiple times (e.g., n=6 or more) in a single run by the same analyst. - Intermediate Precision (Inter-assay): Analyze the same sample over multiple separate runs (e.g., 3-5 days), different analysts, or different equipment.
2. Sample Preparation: Use a minimum of two quality control (QC) samples spanning the dynamic range of your assay (e.g., low, mid, and high concentrations). Use a matrix as close to the study sample as possible.
3. Execution: - For intra-assay precision, run all replicates of the QC samples in one batch. - For intermediate precision, include the QC samples in several different analytical runs.
4. Data Analysis: - Calculate the mean concentration and standard deviation (SD) for each QC level. - Determine the Coefficient of Variation (%CV) as (SD / Mean) * 100. - Compare the %CV to pre-defined acceptance criteria. For a viral plaque assay, for example, intra-assay %CVs of 6.0% to 18.7% have been demonstrated as acceptable [32].
Protocol for Robustness Testing
Robustness is the ability of a method to remain unaffected by small, deliberate variations in method parameters [27].
1. Identify Critical Parameters: List procedural steps that could reasonably vary in a routine laboratory (e.g., incubation time ±5%, temperature ±2°C, reagent concentration ±5%, different analysts).
2. Experimental Design: - Use a set of samples with known concentrations (e.g., low and high QC samples). - Perform the assay while systematically varying one parameter at a time from its nominal value. - Keep all other conditions constant.
3. Data Analysis: - Measure the impact of each variation on the assay result (e.g., reported concentration or % recovery). - If a variation causes a significant change in the result, tighten the control limits for that parameter in your final assay protocol. - The goal is to define acceptable operational ranges (e.g., "incubation time: 30 ± 3 minutes") that ensure reliable performance [27].
Visualizing the Validation Workflow and Regulatory Strategy
Assay Validation and Lifecycle Management Workflow
The following diagram illustrates the key stages in the assay validation lifecycle, from initial design to ongoing verification, integrating requirements from both FDA and EMA.
Platform Validation Strategy for Viral Clearance
This diagram outlines the decision-making process for applying a platform validation approach to viral clearance studies, as per CDE, FDA, and EMA guidelines.
The Scientist's Toolkit: Key Reagents and Materials
The table below lists essential reagents and materials critical for successful viral assay validation, as derived from the cited validation studies.
| Reagent / Material | Function in Validation | Example from Literature |
|---|---|---|
| Reference Standard (Hybrid Amplicon) | Serves as a qualified control for quantifying viral copy number; demonstrates accuracy, precision, and linearity. | A synthetic DNA fragment containing WPRE and RPP30 amplicons for ddPCR VCN assay validation [35]. |
| Cell Line (Vero E6) | Provides the host cell system for viral plaque assays; critical for demonstrating specificity and robustness. | Vero E6 cells from a characterized Working Cell Bank (WCB) used to validate an rVSV-SARS-CoV-2-S vaccine plaque assay [32]. |
| Semisolid Overlay Medium (e.g., Tragacanth Gum) | Restricts viral spread to form discrete, countable plaques in infectivity assays; essential for precision. | Used in the validated plaque assay for BriLife vaccine to ensure plaques were distinguishable for accurate counting [32]. |
| Critical Process Intermediates | Represents the "worst-case" conditions for platform validation of unit operations like viral clearance. | Used to demonstrate that new product parameters do not exceed the validated clearance capability of the platform [33]. |
Practical Implementation: Methodologies for Precision and Linearity Assessment
FAQs: Core Concepts in Precision Validation
Q1: What is the fundamental difference between intra-assay and inter-assay precision?
- Intra-assay precision (also called repeatability) measures the variability between replicate samples (e.g., multiple wells on a plate) processed within a single run of an assay. It assesses the inherent consistency of the assay procedure itself [38] [39].
- Inter-assay precision measures the variability between separate, independent runs of the same assay performed on different days, potentially by different analysts. This evaluates the consistency of the assay over time in a real-world laboratory setting [38] [39].
Q2: What are the typical acceptance criteria for precision in quantitative assays?
For well-controlled, traditional immunoassays like ELISAs, a coefficient of variation (CV) of less than 10% is a common benchmark for both intra-assay and inter-assay precision [38]. However, for more complex biological assays, such as cell-based or viral assays, higher CVs are often accepted. One study on single-cell immune assays reported CVs ranging from 4% to as high as 133%, with variability heavily dependent on the specific assay format and the response level being measured [18] [40]. The table below summarizes precision targets from different assay types.
Table 1: Precision Acceptance Criteria Across Assay Types
| Assay Type | Typical Intra-Assay CV | Typical Inter-Assay CV | Key Influencing Factors |
|---|---|---|---|
| ELISA [38] | <10% | <10% | Matrix effects, reagent stability, pipetting accuracy. |
| ELISPOT [18] [40] | Can exceed 60% at low response levels | Can exceed 60% at low response levels | Cell viability, operator skill, low frequency of responding cells. |
| Cytokine Flow Cytometry (CFC) [18] [40] | ~15% (at 0.25% response) | Varies by day and operator | Gating consistency, instrument performance, antibody lots. |
| PCR-based Viral Assay [29] | Defined by LLOQ and ULOQ | Evaluated via intermediate precision | Extraction efficiency, PCR inhibition, standard curve stability. |
Q3: How do I establish acceptance criteria for a new viral assay validation?
Acceptance criteria should be fit-for-purpose and based on the assay's intended use. Regulatory guidance suggests moving beyond traditional %CV and instead evaluating precision relative to the product's specification tolerance or design margin [20].
- For repeatability, it is recommended that the standard deviation of repeated measurements consumes ≤25% of the specification tolerance for an analytical method, and ≤50% for a bioassay [20].
- This approach directly links method performance to the risk of out-of-specification (OOS) results, providing a more meaningful basis for setting criteria in drug development [20].
Troubleshooting Guides
High Intra-Assay Variability
Problem: High CV between replicates within the same assay plate.
Possible Causes & Solutions:
- Cause: Inconsistent pipetting technique.
- Solution: Implement regular pipette calibration and user training. Use reverse pipetting for viscous liquids and ensure consistent pre-wetting of tips.
- Cause: Improper plate washing.
- Solution: For ELISA/ELISPOT, ensure thorough and consistent washing. Manually wash with a consistent stream and soak time, or validate the performance of an automated plate washer to prevent clogged needles [39].
- Cause: Edge effects on microplates.
- Solution: Use a thermosealer for plates during incubation to prevent evaporation. If incubating in a humidified chamber, ensure uniform humidity across the plate.
High Inter-Assay Variability
Problem: Results for the same control sample vary significantly between different assay runs.
Possible Causes & Solutions:
- Cause: Lot-to-lot reagent variability.
- Solution: Perform bridging studies when introducing new lots of critical reagents (e.g., antibodies, enzyme conjugates, peptide pools) before using them for sample analysis [39].
- Cause: Inconsistent cell preparation (for cell-based assays).
- Solution: Standardize cell isolation, counting, and cryopreservation protocols meticulously. For ELISpot, use serum-free freezing media and control freezing rates to maintain consistent PBMC viability and functionality across experiments [41].
- Cause: Drift in instrument calibration.
- Solution: Adhere to a strict preventive maintenance and calibration schedule for all critical instrumentation, including plate readers, flow cytometers, and PCR machines [29].
Failure to Meet Linearity Requirements
Problem: Dilutions of a sample do not fall along a linear curve, making accurate quantification impossible.
Possible Causes & Solutions:
- Cause: Matrix interference from sample components.
- Solution: Perform spike-and-recovery experiments in the sample matrix (e.g., serum, plasma). If recovery is outside the 80-120% range, modify the sample diluent or introduce a purification step [38] [39].
- Solution: For PCR-based viral assays, investigate and mitigate PCR inhibitors that may be co-extracted with the target DNA, which can cause non-linear dilution curves [29].
- Cause: Hook effect (prozone effect) in immunoassays.
- Solution: Test samples at multiple dilutions to ensure you are operating within the dynamic range of the assay and not in a region of antigen excess [39].
Experimental Protocols for Precision Validation
Protocol for Determining Intra-Assay Precision
Objective: To quantify the variability within a single assay run.
Materials:
- Quality Control (QC) samples at low, medium, and high concentrations of the analyte.
- All standard assay reagents and equipment.
Method:
- Prepare the QC samples according to your standard procedure.
- For each QC level (low, medium, high), analyze a minimum of n=6 replicates on the same microplate or within the same assay run [18] [40] [38].
- Process the entire plate using your validated assay protocol.
- For each set of replicates, calculate the mean, standard deviation (SD), and coefficient of variation (%CV).
- %CV = (Standard Deviation / Mean) x 100
Acceptance: The %CV for each QC level should meet pre-defined criteria (e.g., <10-15% for ELISA, though higher for cellular assays) [38].
Protocol for Determining Inter-Assay Precision
Objective: To quantify the variability of the assay across different runs over time.
Materials:
- The same batch of QC samples (low, medium, high) as used for intra-assay precision, aliquoted and stored appropriately to ensure stability.
Method:
- Over the course of a validation study, analyze the low, medium, and high QC samples in duplicate or triplicate in a minimum of 3-6 separate assay runs [38] [29].
- These runs should be performed:
- Collate the results for each QC level from all runs.
- For each QC level, calculate the overall mean, SD, and %CV across all runs.
Acceptance: The overall %CV for each QC level should meet pre-defined criteria, demonstrating the assay's robustness over time [38].
Experimental Workflow and Decision Pathway
The following diagram illustrates the logical workflow for establishing and troubleshooting assay precision.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Validation of Viral and Immunoassays
| Reagent / Material | Function in Validation | Critical Considerations |
|---|---|---|
| Reference Standard [38] [39] | Calibrates the assay; used to generate the standard curve for quantification. | Should be traceable to a recognized standard (e.g., NIBSC). Stability and proper storage are critical. |
| Quality Control (QC) Samples [38] [29] | Monitors precision and accuracy across runs. Prepared at low, mid, and high concentrations. | Must be representative of the test samples and stable for the duration of the validation. |
| Validated Antibody Pairs [42] [39] | Core component for specificity in immunoassays (ELISA, ELISPOT). | Requires titration for optimal signal-to-noise. Specificity must be tested against related analytes. |
| Peptide Pools (for T-cell assays) [18] [41] | Stimulate antigen-specific T-cells in functional assays like ELISPOT and CFC. | Purity (>80%), sequence coverage, and solubility (DMSO stock) are key. |
| Cryopreserved PBMCs [18] [41] | Provide a renewable, consistent source of responder cells for cellular immune assays. | Viability post-thaw and consistency in isolation/cryopreservation protocols are paramount. |
| PCR Master Mix & Probes [29] | Enable specific and efficient amplification of viral targets in real-time PCR assays. | Lot-to-lot consistency, resistance to inhibitors, and optimized primer/probe concentrations are vital. |
Quantifying Linear Dynamic Range in Viral Detection Assays
Why Linear Dynamic Range Matters in Viral Detection
In viral detection, the Linear Dynamic Range is the concentration range over which the assay's signal response is directly proportional to the amount of viral analyte present [43]. A broad linear range is crucial for accurately quantifying viruses across diverse clinical scenarios—from early infection with low viral loads to peak replication with high titers. Assays with a narrow range require laborious sample dilutions, increase reagent use, and risk reporting inaccurate quantitative results if samples fall outside the validated range [44] [45]. Properly validating this range ensures that results are both reliable and reproducible, forming a cornerstone of precise viral research and diagnostics.
Core Concepts and Definitions
- Linear Dynamic Range: The range of template concentrations (from the lowest to the highest) over which the assay's measurement signal (e.g., fluorescence) increases in direct proportion to the concentration of the target [43]. Outside this range, saturation occurs at high concentrations and detection fails at low concentrations.
- Linearity (R²): A statistical measure (between 0 and 1) representing how well the data points fit a straight line. Typically, R² ≥ 0.980 is considered acceptable for a qPCR standard curve, indicating a strong linear relationship [43].
- Slope: The slope of the standard curve in qPCR is used to calculate the amplification efficiency. An ideal efficiency (90–110%) corresponds to a slope of approximately -3.32 [43].
The following workflow outlines the key steps for establishing and validating the linear dynamic range of a viral detection assay:
Troubleshooting Guide: Common Problems & Solutions
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High signals/saturated standard curves | Standard reconstituted with incorrect (low) volume; incubation times too long [46]. | Reconstitute standard with correct volume; decrease plate, detection antibody, or substrate incubation times [46]. |
| Sample readings outside range | Analyte concentration is below detection limit or higher than the highest standard point [46]. | Concentrate low-titer samples or dilute high-titer samples; re-analyze [46]. |
| Assay fails unexpectedly after reagent batch change | Different PCR assays show individual sensitivity to minute changes in reaction mixture components, even from the same manufacturer [47]. | Validate new reagent batches with all critical assays; purchase large reagent batches for consistency; have alternative manufacturer protocols ready [47]. |
| Reduced digital PCR (dPCR) efficiency | Sample impurities (salts, alcohols, proteins) or complex template structures (supercoiled plasmids, large DNA) [48]. | Use high-purity nucleic acid kits; for complex structures, employ restriction digestion (ensure enzyme does not cut within amplicon) [48]. |
| Narrow dynamic range in LC-MS/MS | Detector saturation at high analyte concentrations [44] [45]. | Utilize multiple product ions or natural isotopologue transitions to create parallel calibration curves for high and low sensitivity ranges [44] [45]. |
Experimental Protocols for Determining Linear Dynamic Range
Protocol 1: Establishing Linear Dynamic Range for qPCR/qRT-PCR
This protocol is foundational for validating quantitative PCR assays used in viral load monitoring [43] [49].
Preparation of Standard Curve:
Assay Run and Data Collection:
- Amplify the dilution series using the optimized qPCR conditions.
- Record the Ct (threshold cycle) value for each replicate.
Data Analysis:
- Plot the log of the starting template concentration against the mean Ct value for each dilution.
- Perform linear regression analysis on the plot. The assay is considered linear where this relationship forms a straight line.
- Acceptance Criteria: The curve should demonstrate a coefficient of determination (R²) of ≥ 0.990 (or ≥ 0.980, depending on stringency), and the calculated amplification efficiency should be between 90% and 110% [43] [49].
Protocol 2: Expanding Dynamic Range in LC-MS/MS Assays
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) can suffer from detector saturation. This protocol uses a multi-ion strategy to extend the upper limit of quantification [44].
Ion Selection:
Calibration and Validation:
- Establish two separate calibration curves using the two different ions.
- Validate both curves independently, ensuring each meets pre-defined precision (e.g., CV within 20%) and accuracy criteria [44].
- The overall reportable range of the assay becomes the combination of the two curves, effectively expanding the total dynamic range by one or more orders of magnitude [44] [45].
Advanced Applications & Techniques
Digital PCR (dPCR) for Absolute Quantification
dPCR partitions a sample into thousands of individual reactions, allowing for absolute quantification without a standard curve. It is less susceptible to PCR inhibitors and offers high precision for quantifying low-abundance targets [50]. Key considerations for dynamic range in dPCR include:
- Partition Number: The dynamic range is fundamentally limited by the number of partitions. Platforms generating 10 million droplets can achieve a wide dynamic range of up to 6 logs [50].
- Sample Input: To maximize sensitivity for ultra-low targets, the platform must accommodate large nucleic acid inputs (e.g., micrograms of DNA) without inhibition [50].
Expanding Range with Single-Molecule Counting
Innovative imaging techniques are pushing the limits of fluorescence assays. By combining single-molecule counting for low concentrations with calibrated ensemble intensity measurements for high concentrations, researchers can expand the dynamic range to nearly 1,000,000-fold down to femtomolar levels [51]. This is particularly promising for detecting rare cancer biomarkers like circulating miRNAs.
Research Reagent Solutions Toolkit
| Item | Function in Validation | Example/Note |
|---|---|---|
| Armored RNA / Quantified Standards | Provides stable, non-infectious standards for creating serial dilutions to generate the standard curve [49]. | Armored RNA Quant SARS-CoV-2 panel [49]. |
| One-Step RT-PCR Master Mix | A ready-to-use mix containing all core components for reverse transcription and PCR, reducing setup errors and variability [47]. | Batch-to-batch consistency is critical; validate new lots extensively [47]. |
| Hydrolysis Probes (TaqMan) | Provide sequence-specific detection in qPCR and dPCR, crucial for specific viral target quantification [48]. | Use at higher concentrations in dPCR (e.g., 0.25 µM) for better fluorescence [48]. |
| Nucleic Acid Purification Kits | Ensure high-purity template free of contaminants (salts, alcohols, proteins) that can inhibit amplification and skew results [48]. | Essential for reliable dPCR and qPCR performance [48]. |
| Stable Isotope-Labeled (SIL) Peptides | Internal standards for LC-MS/MS assays that account for sample loss during preparation and allow precise quantification [52]. | Used in SISCAPA (Stable Isotope Standards and Capture by Anti-Peptide Antibodies) workflows [52]. |
This technical support center is designed as a resource for researchers and scientists engaged in the development and validation of microneutralization (MN) assays for yellow fever (YF) vaccines. Framed within a broader thesis on viral assay precision and linearity validation, the content below addresses specific, high-priority experimental challenges in the form of detailed troubleshooting guides and frequently asked questions (FAQs). The information synthesizes current standards and data to support robust assay performance for the detection and quantification of YF virus-neutralizing antibodies, a critical component for vaccine licensure.
Troubleshooting Guides
Troubleshooting Common Assay Performance Issues
Table 1: Troubleshooting Guide for Microneutralization Assays
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High intra-assay variability | Inconsistent cell seeding density or viability. | Standardize cell culture protocols; ensure Vero cells are healthy and used at a consistent passage number. Count cells before seeding to ensure uniform density across wells. |
| Poor precision (high %CV) | Inaccurate serial dilution of serum samples; pipetting errors. | Use calibrated pipettes and perform dilutions meticulously. For critical studies, use an automated liquid handler to improve reproducibility [53]. |
| Loss of signal or high background in immunostaining | Improper antibody dilution; incomplete cell fixation or permeabilization. | Titrate all antibodies to determine optimal concentration. Ensure fixation (e.g., with 10% formaldehyde) and permeabilization (e.g., with Triton X-100) steps are performed for the correct duration [54]. |
| Inconsistent neutralization titers between runs | Variation in virus stock titer (TCID₅₀) used between experiments. | Aliquot and titrate virus stocks to determine the exact TCID₅₀ for each batch. Use a consistent, pre-qualified virus dose in every assay run [55] [56]. |
| Failure to meet linearity or accuracy criteria | Serum matrix interference (e.g., from hemolytic, lipemic, or icteric samples). | Validate assay performance using various serum matrices during development. The YF MN assay has demonstrated suitable specificity across such interfering substances [53]. |
Experimental Protocols for Key Validation Experiments
Protocol 1: Assessing Intra-Assay and Intermediate Precision
- Objective: To determine the repeatability (intra-assay precision) and intermediate precision of the microneutralization assay.
- Methodology:
- Prepare a minimum of three replicates of at least two internal quality control (IQC) samples (e.g., a high-titer and a low-titer positive control) within the same assay run to assess intra-assay precision [53].
- Repeat this process across three separate assay runs, performed by different analysts on different days, to assess intermediate precision.
- Calculate the geometric mean titer (GMT) and the percentage geometric coefficient of variation (%GCV) for the results from both the intra-assay and intermediate precision experiments.
- Acceptance Criterion: A validated YF MN assay demonstrated suitable intra-assay precision with a %GCV of 36% and intermediate precision with a %GCV of 54% [53].
Protocol 2: Determining Assay Linearity and Dilutional Accuracy
- Objective: To confirm that serum samples can be accurately diluted without affecting the measured neutralizing antibody titer.
- Methodology:
- Select a high-titer positive human serum sample.
- Perform a series of linear dilutions (e.g., two-fold or three-fold) in negative human serum to maintain a consistent matrix.
- Test each dilution in the MN assay and calculate the observed titer.
- Plot the observed titers against the expected titers and perform linear regression analysis.
- Acceptance Criterion: The assay should demonstrate a linear relationship with an R² value of >0.98 [57]. The back-calculated concentrations for each dilution should fall within predefined limits (e.g., ±2-fold) of the expected value [53].
Protocol 3: Establishing the Lower and Upper Limits of Quantification (LLOQ & ULOQ)
- Objective: To define the range of antibody titers that can be reliably quantified.
- Methodology:
- Prepare serial dilutions of a positive control serum near the expected lower and upper limits of detection.
- Run these samples in multiple replicates (e.g., N=≥24) across several independent assays.
- The LLOQ is the lowest titer where both precision (%GCV) and accuracy (relative to the expected value) meet pre-specified criteria. For the YF MN assay, an LLOQ of 10 (1/dil) was validated with a %GCV of 38% for repeatability [53].
- The ULOQ is the highest titer that can be accurately measured without a prozone effect or signal saturation. The validated YF MN assay reported a ULOQ of 10,240 (1/dil) [53].
Frequently Asked Questions (FAQs)
Q1: What are the key advantages of using a microneutralization assay over the traditional plaque reduction neutralization test (PRNT) for yellow fever vaccine studies?
A1: The MN assay offers several key advantages for high-throughput clinical testing needed for vaccine licensure:
- Higher Throughput: It is performed in a 96-well microtiter plate format, allowing for the simultaneous testing of dozens of samples compared to the more cumbersome 24- or 6-well plate format of the PRNT [53] [56].
- Reduced Labor and Time: The MN assay with an immunostaining readout does not require a solid overlay and can be completed faster than the PRNT, which relies on plaque formation. Furthermore, imaging and analysis can be automated [58] [56].
- Smaller Sample Volume: The assay requires less serum, which is particularly beneficial for pre-clinical studies or pediatric trials where sample volumes are limited [56].
- Objective Readout: While PRNTs can involve subjective plaque counting, the MN assay can use immunostaining and automated imaging for a more quantitative and objective readout of infection foci [58].
Q2: How is the specificity of the yellow fever MN assay confirmed, especially given cross-reactivity concerns with other flaviviruses?
A2: Assay specificity is confirmed by testing sera against other orthoflaviviruses. During the validation of the YF MN assay, its specificity was demonstrated using samples containing antibodies against related viruses such as dengue virus, Japanese encephalitis virus, and Zika virus. The assay successfully distinguished YF-specific neutralizing antibodies, showing minimal cross-reactivity [53].
Q3: What are the critical reagents and their quality controls in a validated YF MN assay?
A3: The reliability of the assay depends on several critical reagents:
- Virus Stock: A well-characterized YF-17D virus stock with a predetermined titer (TCID₅₀/mL). Consistency in the virus working dose is paramount [53].
- Cell Line: Vero cells, which must be maintained under consistent culture conditions and monitored for mycoplasma contamination and passage number [53] [54].
- Internal Quality Controls (IQCs): A panel of controls, including high-titer and low-titer anti-YF positive controls and a negative control. Their valid titer ranges must be established, with over 90% of results falling within a pre-defined ±2-fold range of the geometric mean titer [53].
- Detection Antibodies: For immunostaining, specific primary and conjugated secondary antibodies (e.g., HRP-conjugated) must be titrated for optimal performance [54].
Q4: What short-term stability conditions have been validated for serum samples in this assay?
A4: Validation studies have shown that YF virus-neutralizing antibodies in human serum remain stable under specific short-term conditions. Antibody titers were demonstrated to be stable in serum samples after undergoing up to five freeze-thaw cycles or when stored at 2°C to 8°C for up to 14 days. In these studies, results remained within the two-fold assay variability limit [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for YF Microneutralization Assay
| Reagent/Material | Function in the Assay | Key Considerations |
|---|---|---|
| Vero Cells (ATCC CCL-81) | Host cell line for virus infection and replication. | Monitor for contamination and maintain consistent passage number; check for mycoplasma [53] [54]. |
| YF-17D Virus | Antigen used to challenge serum antibodies in the neutralization. | Use a consistent, pre-titered stock. Aliquots should be stored at ≤-60°C to maintain infectivity [53]. |
| Internal Quality Controls (IQCs) | Monitor precision and accuracy within and across assay runs. | Include high-positive, low-positive, and negative controls. Establish a valid range for positive IQCs (e.g., GMT ±2-fold) [53]. |
| Anti-Yellow Fever Virus Antibodies | Detection of infected cells (for immunostaining readout). | Target viral proteins like the envelope or non-structural proteins. Requires titration to optimize signal-to-noise ratio [53]. |
| Cell Culture Medium (e.g., cDMEM) | Supports cell viability and growth during the assay. | Typically supplemented with fetal bovine serum (FBS) and antibiotics [55] [54]. |
| Fixation Solution (e.g., 10% Formaldehyde) | Preserves cells and inactivates virus after the incubation period. | Essential step before immunostaining; must be performed in a biosafety cabinet [54]. |
| Permeabilization Agent (e.g., Triton X-100) | Allows detection antibodies to enter cells and bind intracellular viral proteins. | Concentration and incubation time must be optimized to avoid destroying cell morphology [54]. |
Workflow and Signaling Pathway Diagrams
YF MN Assay Workflow
Assay Validation & Quality Control Logic
Troubleshooting Guides for Bead-Based Serology Assays
This section addresses common experimental challenges in bead-based multiplex serology and provides evidence-based solutions to ensure precise and linear assay performance.
Table 1: Common Technical Issues and Evidence-Based Solutions
| Problem Category | Specific Issue | Potential Cause | Recommended Solution | Supporting Evidence |
|---|---|---|---|---|
| Assay Performance & Precision | High intra- or inter-assay variability (%CV >25%) | Improper bead aggregation, unstable reagent concentrations, or imprecise pipetting. | Optimize protein and secondary antibody concentrations; validate precision using human serum panels. | Assay precision confirmed with CV ≤20% across runs, days, and analysts using 24 human serum samples [59]. |
| Poor accuracy (recovery outside 80-120%) | Inaccurate standard curve calibration or matrix effects. | Calibrate using WHO International Standards; validate recovery and dilutional linearity. | Back-fitted recoveries of 80-120% achieved using 4-PL regression and WHO standards (e.g., NIBSC 20/136) [59] [60]. | |
| Specificity & Cross-Reactivity | Cross-reactivity between related antigens (e.g., SARS-CoV-2 variants) | Antigenic similarity leading to antibody cross-binding. | Assess specificity with monoclonal antibodies and immunodepletion; use proteins with distinct epitopes. | Specificity of 93-100% demonstrated via inhibition experiments; <10% cross-reactivity observed for most antigens [59] [61]. |
| High background signal | Non-specific antibody binding or suboptimal antigen coupling. | Use mammalian-expressed S proteins over N-based antigens for seasonal CoVs; optimize blocking conditions. | Mammalian-expressed SARS-CoV-1, MERS S proteins reduced background vs. N antigens [59]. | |
| Multiplexing Interference | Signal suppression or enhancement in multiplex vs. singleplex | Bead-to-bead interference or spectral overlap. | Perform singleplex vs. multiplex comparison; ensure no signal interference between bead regions. | Geometric mean ratios of 0.895-1.122 between singleplex and 15-plex formats showed no interference [59]. |
| Dynamic Range & Sensitivity | Narrow dynamic range | Suboptimal antigen coupling efficiency or reference standard preparation. | Characterize international reference standards (e.g., NIBSC 06/142, 10/262) for multiplex suitability; use an equimix. | An equimix of WHO standards provided the best dynamic range for a 7-plex vaccine antigen assay [61]. |
| Low sensitivity for specific antigens | Poor antigen selection or conformation. | Select full-length proteins over short fragments (e.g., full-length N protein over short form). | Full-length SARS-CoV-2 N protein showed superior discrimination over a short form variant [59]. |
Frequently Asked Questions (FAQs)
Q1: How can I validate the precision and linearity of my multiplex serology assay for viral research? A: Validation should follow FDA, EMA, and ICH M10 guidelines. Key steps include:
- Precision: Assess inter-assay and intra-assay precision using a panel of human serum samples (e.g., from vaccinated or infected individuals). The percent coefficient of variation (%CV) should be ≤20% for all antigens [61] [60].
- Linearity & Accuracy: Perform serial dilutions of samples and quality controls. Demonstrate that back-calculated recoveries fall within 80-120% of the expected concentration using a four-parameter logistic (4-PL) regression model [60] [62].
- Standardization: Calibrate the assay using relevant WHO International Standards to report results in standardized units (e.g., BAU/mL for SARS-CoV-2) [59].
Q2: What is the best way to address cross-reactivity when measuring antibodies against highly similar viral variants, such as SARS-CoV-2 mutants? A: A combination of experimental and computational approaches is effective:
- Specificity Testing: Use antigen-specific monoclonal antibodies to verify specific binding to the intended target and minimal cross-reactivity with similar proteins [59].
- Immunodepletion: Pre-incubate serum samples with a specific competitor antigen (e.g., SARS-CoV-2 S protein). A reduction ≥80% in signal for the homologous antigen, with minimal heterologous signal reduction (<10%), confirms specificity [59].
- Antigen Selection: Choose antigen domains with sufficient sequence or structural divergence to maximize discriminatory power.
Q3: We observe inconsistent results between monoplex and multiplex formats. How can I troubleshoot this? A: This indicates potential multiplex interference.
- Systematic Comparison: Measure the same samples (including reference standards and QCs) in both singleplex and multiplex formats.
- Quantify Interference: Calculate the geometric mean ratio (GMR) of IgG measurements between the two formats. A GMR between 0.9 and 1.1 suggests no significant interference, as demonstrated in a 15-plex SARS-CoV-2 assay [59].
- Bead Compatibility: Ensure that spectrally unique beads are used and that there is no physical or chemical interference between the different bead sets during the assay procedure.
Q4: How many antigens can I reliably multiplex in a single assay? A: The upper limit depends on the technology. For fluorescent bead-based platforms (Luminex), 50-500-plex assays are theoretically possible, but most validated diagnostic and research assays multiplex 5-20 antigens to maintain robustness, sensitivity, and specificity [59] [61] [63]. Newer technologies using mass spectrometric detection with isotopically barcoded beads can scale to thousands of targets, but these are primarily for research [64].
Experimental Protocols for Key Applications
Protocol 1: Coupling Antigens to Magnetic Beads
This is a core methodology for developing a custom multiplex assay [61] [60].
- Materials: Spectrally unique magnetic carboxylated microspheres (Luminex), purified antigen, 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDAC), Sulfo-NHS, coupling buffer (e.g., PBS, pH 7.4).
- Procedure:
- Bead Activation: Resuspend magnetic beads and transfer 1.25 x 10^6 beads per antigen to a clean tube. Wash beads twice with activation buffer. Resuspend beads in activation buffer containing EDAC and Sulfo-NHS to form stable amine-reactive intermediates. Incubate for 30 minutes on a rotator at room temperature, protected from light.
- Antigen Coupling: Wash activated beads twice with coupling buffer. Resuspend beads in coupling buffer containing the purified antigen at an optimized concentration (e.g., 5 µg of protein per 1.25 x 10^6 beads [59]). Incubate for 2 hours on a rotator at room temperature, protected from light.
- Blocking and Storage: Block the remaining active sites by adding a blocking buffer (e.g., 1% BSA) and incubating for 30 minutes. Wash the coupled beads twice with storage buffer (e.g., PBS with 0.05% ProClin-300 and 1% BSA). Resuspend in storage buffer and count. Store at 4°C protected from light.
Protocol 2: Validating Assay Specificity via Immunodepletion
This protocol confirms that signals are antigen-specific [59].
- Materials: Reference standard or high-titer serum sample, specific competitor antigen (e.g., SARS-CoV-2 S protein), heterologous control antigen (e.g., OC43 S protein), assay diluent.
- Procedure:
- Pre-incubation: Aliquot the reference standard. Incubate one aliquot with a specific competitor antigen, another with a heterologous control antigen, and a third with only assay diluent (control). Perform this pre-incubation for 2 hours at room temperature.
- Run Multiplex Assay: Analyze all three aliquots in your standard multiplex assay procedure.
- Calculate % Inhibition: For each antigen, calculate the percentage signal reduction (in MFI or concentration) in the competitor condition compared to the control condition.
- % Depletion = [1 - (MFIwithcompetitor / MFI_control)] x 100
- Interpretation: Specific binding is demonstrated by ≥80% signal reduction when depleted with the homologous antigen and minimal reduction (<10%) when depleted with the heterologous control.
Research Reagent Solutions
Table 2: Essential Materials for Bead-Based Multiplex Serology
| Reagent / Material | Function in the Assay | Examples & Key Specifications |
|---|---|---|
| Spectrally Unique Beads | Solid-phase support for antigen coupling; enables multiplexing via internal fluorescence coding. | Magnetic carboxylated microspheres (Luminex xMAP) [61] [60]. |
| Purified Antigens | Targets for capturing antigen-specific antibodies from the serum sample. | Recombinant proteins (e.g., SARS-CoV-2 S, N, RBD; Pertussis PT, FHA), viral lysates, toxoids (Diphtheria, Tetanus) [59] [61]. |
| International Reference Standards | Calibrates the assay to report standardized, comparable units; critical for validation. | WHO International Standards from NIBSC (e.g., 20/136 for anti-SARS-CoV-2 IgG, 06/142 for Pertussis) [59] [60]. |
| Detection Antibody | Detects bound human antibodies; conjugated for signal generation. | R-Phycoerythrin (R-PE) conjugated anti-human IgG [60] [62]. |
| Coupling Chemistry Reagents | Covalently links antigens to the carboxylated bead surface. | EDAC (or EDC) and Sulfo-NHS for carbodiimide chemistry [61] [60]. |
Digital PCR (dPCR) represents a transformative advancement in nucleic acid quantification, enabling absolute quantification without standard curves by combining sample partitioning, end-point PCR, and Poisson statistical analysis. This methodology fundamentally differs from quantitative PCR (qPCR) by physically segregating a sample into thousands of individual partitions, each functioning as an independent micro-reactor [65] [66]. Following amplification, partitions are analyzed as positive or negative for the target, and the original template concentration is calculated directly from the ratio of positive to total partitions using Poisson statistics [65] [67]. This approach provides unparalleled precision for validating viral assay linearity, particularly for low-abundance targets and complex sample matrices encountered in viral persistence and therapy development research [68] [69].
The elimination of standard curves removes a significant source of variability and bias, allowing direct comparison of results across laboratories and over time [65] [66]. For viral research, this translates to more reliable quantification of latent reservoirs, low-level viremia, and vector copy numbers—critical parameters for assessing therapeutic efficacy in conditions like HIV, hepatitis B, and gene therapies [68] [69] [70].
Key Experimental Applications in Viral Research
Ultra-Sensitive Hepatitis B Virus (HBV) Detection
Research Objective: To develop and validate a high-sensitivity droplet digital PCR (ddPCR) assay for detecting low-level residual viremia in chronic hepatitis B patients, which is crucial for monitoring antiviral therapy efficacy [68].
Experimental Protocol:
- Platform: QX200 ddPCR System (Bio-Rad)
- Sample Input: 200 µL of serum
- Assay Design: Primers and probe target a highly conserved region in the HBV X gene
- Thermocycling Conditions: Standard ddPCR protocol with endpoint fluorescence reading
- Validation: Using AcroMetrix HBV Panel and patient samples to determine sensitivity, specificity, linearity, and precision
Results and Performance Metrics: The assay demonstrated exceptional sensitivity with a lower limit of detection of 1.6 IU/mL and lower limit of quantification of 9.4 IU/mL using probit regression [68]. The validation showed excellent specificity (96.2%), linearity (R² = 0.988, p < 0.001), and minimal variability (intra-run CV: 0.69%; inter-run CV: 4.54%) [68].
Table 1: Performance Metrics of HBV ddPCR Assay
| Parameter | Result | Significance |
|---|---|---|
| Lower Limit of Detection | 1.6 IU/mL | Enables detection of minimal residual viremia |
| Lower Limit of Quantification | 9.4 IU/mL | Reliable quantification at very low concentrations |
| Specificity | 96.2% | Minimal false positives in clinical samples |
| Linearity (R²) | 0.988 | Excellent correlation across measurable range |
| Intra-run CV | 0.69% | Exceptional run-to-run reproducibility |
HIV Reservoir Quantification in Treated Patients
Research Objective: To establish a duplex digital PCR assay for accurate quantification of total HIV DNA in people with HIV (PWH) on antiretroviral therapy, serving as a surrogate marker for viral reservoir size [69].
Experimental Protocol:
- Platform: Absolute Q dPCR system (microfluidic chamber array)
- Assay Design: Duplex targeting HIV LTR region and human RPP30 reference gene
- PCR Conditions: 40 cycles of: 10s at 96°C (denaturation), 50s at 60°C (annealing/extension)
- Primer/Probe Concentration: 900 nM primers, 250 nM probes
- Sample Types: CD4+ T cells and PBMCs from ART-treated and ART-naïve PWH
Results and Performance Metrics: The assay showed good linearity (R² = 0.977, p < 0.0001) across a range of 78 to 5,000 HIV DNA copies/10⁶ cells [69]. The lower limit of detection with 95% confidence was 79.7 HIV copies/10⁶ cells. Precision varied by target concentration: CV was 8.7% at high concentration (1,250 copies/10⁶ cells) and 26.9% at low concentration (150 copies/10⁶ cells) [69]. The assay successfully quantified HIV reservoir in all patient samples, showing significant differences between ART-treated and ART-naïve individuals (p < 0.0001) [69].
Viral Copy Number (VCN) Assessment for Gene Therapy
Research Objective: To qualify and validate a duplex ddPCR assay for quantifying viral copy number in virus-modified cell therapy products using an innovative hybrid amplicon approach [70].
Experimental Protocol:
- Reference Material: Synthetic DNA fragment containing WPRE (viral) and RPP30 (reference) amplicons connected by HindIII restriction site
- Methodology: Duplex ddPCR simultaneously quantifying viral and reference genes
- Validation Parameters: Range, precision, bias, robustness with varying input DNA
- Application: Determining transduction efficiency and cellular kinetics of therapy products
Results and Performance Metrics: The hybrid amplicon approach provided a reliable reference standard that demonstrated comparable performance to traditional cell reference standards while being faster to develop [70]. This method enabled determination of upper and lower limits of quantification, linearity, precision (CV), and accuracy (% recovery) under various conditions that might introduce variability in traditional VCN assays [70].
Technical Support Center: Troubleshooting Guides and FAQs
Digital PCR Troubleshooting Guide
Table 2: Common dPCR Issues and Solutions
| Problem | Possible Cause | Solution |
|---|---|---|
| No positive partitions | Incorrect threshold setting | Manually adjust threshold in analysis software [71] |
| Template concentration too low | Verify template quality and concentration; increase input volume [72] | |
| PCR inhibition | Further purify template; use alcohol precipitation or cleanup kits [72] [73] | |
| High background noise | Suboptimal primer/probe concentrations | Optimize concentrations for clear cluster separation [73] |
| Non-specific amplification | Increase annealing temperature; verify primer specificity [72] | |
| Poor partition separation | Inadequate droplet generation | Check droplet generator performance; ensure proper oil and sample consistency [65] |
| Inconsistent results between runs | Variable partition volume | Use reference material to normalize volume variations [70] |
| Pipetting inaccuracies | Use calibrated pipettes and techniques for reproducible volumes [70] |
Frequently Asked Questions (FAQs)
Q: What is the key advantage of dPCR over quantitative PCR (qPCR) for viral assays? A: The primary advantage is absolute quantification without standard curves. dPCR provides results in discrete copy numbers per volume, leading to higher precision and lower limits of detection, making it superior for rare target detection in viral reservoir monitoring [65] [66].
Q: How does Poisson distribution relate to dPCR accuracy? A: Poisson statistics account for the random distribution of template molecules into partitions. This model calculates the probability that partitions received zero, one, or multiple target copies, enabling highly accurate back-calculation of the true starting concentration [65] [67].
Q: Why is dPCR more resistant to PCR inhibitors than qPCR? A: Inhibitors are distributed across all partitions, effectively diluting their concentration within any single partition. Additionally, dPCR uses endpoint detection rather than amplification kinetics, so even slightly inhibited reactions that reach threshold are counted as positive [65] [66] [73].
Q: What is the "digital range" and why is it important? A: The digital range refers to the optimal template concentration where some partitions contain template and others do not. If samples are too concentrated, most partitions will be positive, violating Poisson assumptions and compromising accuracy [71].
Q: Can dPCR be used for multiplex detection? A: Yes, dPCR offers excellent multiplexing capabilities. Recent studies have successfully developed pentaplex (5-plex) reference gene panels and duplex viral assays with clear discrimination between targets [74] [69].
Essential Research Reagent Solutions
Table 3: Key Reagents for Viral dPCR Assays
| Reagent/Item | Function | Application Example |
|---|---|---|
| Hybrid Amplicon Standards | Linked viral and reference amplicons provide internal control for both targets simultaneously | WPRE-RPP30 hybrid for VCN assays [70] |
| Restriction Enzymes (HindIII) | Digest genomic DNA to reduce fragment size and improve partitioning efficiency | HindIII digestion of human genomic DNA before dPCR [74] |
| Droplet Generation Oil | Creates stable water-in-oil emulsion for partition formation | Bio-Rad QX200 Droplet Generator Oil [65] |
| Digital PCR Supermix | Optimized buffer containing polymerase, dNTPs, and stabilizers for partition PCR | ddPCR Supermix for Probes (Bio-Rad) [73] |
| Nuclease-Free Water | Diluent for standards and samples to prevent enzymatic degradation | Template dilution for serial dilution series [73] |
Experimental Workflow and Signaling Pathways
Digital PCR Workflow for Viral Assays
Digital PCR represents a paradigm shift in viral quantification, offering absolute quantification capabilities that are transforming how researchers measure viral persistence, reservoir dynamics, and therapeutic outcomes. The technology's independence from standard curves, enhanced sensitivity for rare targets, and superior resistance to inhibitors make it particularly valuable for monitoring low-level viremia in treated patients and quantifying viral vector copy numbers in gene therapy products [68] [69] [70].
As viral assay precision requirements continue to tighten in both clinical research and therapeutic development, dPCR provides the methodological rigor needed to detect subtle changes in viral load that may predict treatment success or failure. The troubleshooting guidelines and experimental protocols outlined in this technical resource provide researchers with practical tools to implement this powerful technology in their viral precision medicine programs, ultimately contributing to more accurate viral monitoring and improved therapeutic outcomes.
Optimization Strategies: Enhancing Assay Performance and Reliability
Addressing Variance in Cell-Based Neutralization Assays
Frequently Asked Questions (FAQs)
Q1: What are the primary sources of variance in cell-based neutralization assays, and how can they be controlled?
Variance in these assays stems from three main areas: biological, reagent, and procedural. Biological variance includes factors like cell passage number and confluency [10] [75]. Reagent variance involves inconsistencies in virus stocks and critical reagents [76]. Procedural variance arises from inconsistencies in incubation times, cell seeding densities, and data analysis methods [10]. Control these by implementing strict reagent qualification, using standardized cell banking protocols, and rigorously validating all assay steps [76] [75].
Q2: How do I determine the correct cut point for my neutralization assay, and what if my negative controls fall outside the expected range?
The cut point is statistically determined to distinguish a positive response from a negative one. It is typically established using data from a minimum of 25-30 individual, disease-negative sera samples [76]. If your negative controls consistently fall outside the expected range during an experiment, it indicates a potential shift in the assay baseline. You should investigate matrix effects, check reagent integrity (especially new lots of virus or cells), and re-qualify critical reagents. Do not proceed with sample analysis until the assay is re-validated and a stable baseline is re-established [76].
Q3: My pseudotyped virus neutralization assay (PVNA) results don't correlate well with the live virus gold standard. What could be wrong?
A weak correlation often points to issues with the pseudovirus preparation or assay conditions. Key troubleshooting steps include verifying that your pseudovirus accurately represents the native virus's entry mechanisms and cell tropism [77]. Re-validate your assay against the gold standard using a robust set of samples; a strong correlation (e.g., Pearson CORR >0.90) is achievable with proper optimization [77]. Also, ensure that the cell line used is appropriate and expresses the necessary receptors for both assay formats [10] [78].
Q4: What acceptance criteria should I use for precision and accuracy during assay validation?
For precision, the %CV between replicate wells should generally be ≤ 25%, though slightly higher may be acceptable for some bioassays [76]. For accuracy (bias), it is recommended that the result be ≤ 10% of the specification tolerance [20]. These parameters should be established during validation to ensure the assay is "fit-for-purpose" and that its error does not unduly impact the interpretation of product quality or biological response [20].
Troubleshooting Guides
High Background Signal or Poor Signal-to-Noise Ratio
| Symptom | Potential Cause | Solution |
|---|---|---|
| High signal in negative/control wells [76] | Non-specific binding of antibodies or serum components. | Pre-absorb serum with relevant cell debris or use a blocking agent. |
| Inadequate washing steps. | Optimize wash buffer composition, volume, and number of cycles. | |
| Suboptimal cell health leading to non-specific uptake. | Check cell viability before assay; ensure cells are not over-confluent [79]. | |
| Excessive variability between replicates [76] | Inconsistent cell seeding. | Standardize cell counting and seeding protocols; use automated dispensers. |
| Pipetting errors during serial dilution. | Use calibrated pipettes and perform dilutions in a consistent manner. |
Low Dynamic Range or Poor Assay Sensitivity
| Symptom | Potential Cause | Solution |
|---|---|---|
| Inability to distinguish between high and low titer samples [76] | Incorrect virus challenge dose. | Titrate the virus to find the dose that gives optimal signal (e.g., 40-120 plaques/well in PRNT) [75]. |
| Suboptimal reading time point. | Perform a kinetic experiment to determine the ideal time for measurement. | |
| Reporter signal saturation. | Dilute the detection reagent or reduce the incubation time. | |
| High false-negative rate [10] | Loss of assay sensitivity. | Re-qualify the positive control antibody; check for loss of reagent activity. |
| Drug or matrix interference [76]. | Increase sample dilution (MRD) or introduce a sample purification step. |
Poor Reproducibility Between Assay Runs
| Symptom | Potential Cause | Solution |
|---|---|---|
| Control titers drifting over time [76] | Reagent degradation or lot-to-lot variation. | Create large, qualified reagent master banks (viruses, cells, antibodies). |
| Changes in cell line characteristics. | Use low-passage cells and establish a new working bank regularly [75]. | |
| Inconsistent IC50/NT50 values [10] | Inaccurate curve fitting. | Use a consistent, appropriate model (e.g., 4-parameter logistic) for all analyses. |
| Variations in incubation temperature or time. | Strictly control and monitor environmental conditions in incubators and work areas. |
Experimental Protocols & Validation Data
1. Cell Preparation:
- Seed Huh-7 cells (or other suitable cell line like 293T-SLAM) in a 96-well tissue culture plate at a density of (2 \times 10^4) cells per well.
- Incubate at 37°C, 5% CO₂ until ~90-95% confluent (typically 24 hours).
2. Serum-Virus Incubation:
- Prepare serial dilutions (e.g., 3-fold) of heat-inactivated test serum samples in a separate dilution plate.
- Mix a fixed volume of diluted serum with an equal volume of measles pseudotyped virus (optimized to ~1000 TCID₅₀/well).
- Incubate the serum-virus mixture for 1 hour at 37°C to allow for neutralization.
3. Infection:
- Transfer the neutralization mixture onto the pre-seeded Huh-7 cell monolayer.
- Incubate the plate for 48-72 hours at 37°C, 5% CO₂.
4. Detection:
- Lyse cells and add a luciferase substrate.
- Measure luminescence (Relative Luminescence Units, RLU) using a microplate luminometer.
- The amount of neutralized pseudovirus is determined by the reduction of RLU relative to the virus control wells (set as 100% infection).
5. Data Analysis:
- The half-maximal neutralization titer (NT₅₀) is defined as the reciprocal of the serum dilution that neutralizes 50% of the pseudovirus infection.
- Calculate NT₅₀ using a statistical method such as the Reed-Muench method [10] [77].
1. Cell and Plate Preparation:
- Seed Vero cells in 24-well tissue culture plates at (4 \times 10^5) cells per well.
- Incubate for three days at 37°C, 5% CO₂ until a confluent monolayer is formed.
2. Serum-Virus Neutralization:
- Perform 2-fold serial dilutions of heat-inactivated test serum, starting from 1:5.
- Mix a constant, pre-determined dose of live dengue virus (aiming for 40-120 plaques/well in virus control wells) with the diluted serum.
- Incubate the mixture for 90 minutes at 37°C.
3. Plaque Assay:
- Inoculate the serum-virus mixture onto the Vero cell monolayers.
- After adsorption, remove the inoculum and overlay the cells with a semi-solid medium (e.g., carboxymethylcellulose) to restrict virus spread.
- Incubate for 4-6 days, depending on the virus growth kinetics.
4. Plaque Visualization and Counting:
- Fix and stain the cells. Typically, cells are immunostained using serotype-specific primary antibodies and an enzyme-conjugated secondary antibody to visualize plaques.
- Count the number of plaques in each well.
5. Data Analysis:
- The PRNT₅₀ titer is the reciprocal of the highest serum dilution that reduces the number of plaques by 50% compared to the virus control wells.
- Calculate using the Reed-Muench method or non-linear regression.
Table 1. Performance characteristics of a validated Pseudotyped Virus Neutralization Assay (PVNA) for Measles. [10]
| Parameter | Validation Result | Comment |
|---|---|---|
| Precision | High intra- and inter-assay reproducibility | Validated across multiple genotypes. |
| Linearity | Demonstrated across a wide range of dilutions | Assessed via linear regression of studentized residuals [20]. |
| Specificity | No cross-reactivity with unrelated viruses | Confirmed using specific controls [10]. |
| Correlation with Gold Standard | Strong correlation with live-virus PRNT | Correlation coefficient (r) > 0.9 in SARS-CoV-2 studies [77]. |
| Robustness | Stable performance under varied conditions (incubation time, freeze-thaw cycles) | Incubation time varied from 0.5 to 1.5 hours; pseudovirus withstood 1-3 freeze-thaw cycles [10]. |
Table 2. Comparative analysis of Pseudotyped Virus (PVNA) vs. Live Virus Neutralization Assay (LVNA) for SARS-CoV-2. [77]
| Variant | Sensitivity (%) | Specificity (%) | Accuracy (%) | Pearson Correlation (vs. LVNA) |
|---|---|---|---|---|
| Alpha (B.1.1.7) | > 90 | > 90 | 98.8 | 0.9614 |
| Beta (B.1.351) | > 90 | > 90 | 99.1 | 0.9517 |
| Delta (B.1.617.2) | > 90 | > 90 | 94.3 | 0.9072 |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3. Essential materials and reagents for cell-based neutralization assays. [10] [79] [75]
| Reagent / Material | Function / Purpose | Examples & Considerations |
|---|---|---|
| Cell Lines | Provides the substrate for viral infection and replication. | Vero E6 (for flaviviruses, SARS-CoV-2 LVNA) [75], Huh-7 or 293T-SLAM (for measles PVNA) [10], A549-ACE2 (for SARS-CoV-2 binding assays) [78]. Must be properly authenticated and tested for susceptibility. |
| Virus Stocks | The challenge agent for the assay. | Live virus (for LVNA, requires BSL-3 for pathogens like SARS-CoV-2) [77]. Pseudotyped virus (e.g., VSV-ΔG based, for PVNA; safe for BSL-2) [10] [77]. Must be titrated and used at a consistent, pre-defined dose. |
| Detection System | Quantifies the infection endpoint. | Plaque immunostaining (for PRNT, using specific primary and secondary antibodies) [75]. Luciferase reporter (for PVNA, measured via luminescence) [10] [77]. High-content imaging (for cell-binding assays, using fluorescent antibodies) [78]. |
| Controls | Monitors assay performance and validates results. | Positive Control: High-titer serum or neutralizing antibody [76]. Negative Control: Pre-immune or naive serum [76]. Virus Control: Virus-only wells (set as 100% infection). Cell Control: Cell-only wells (background signal). |
| Assay Platform | The physical format for conducting the assay. | 96-well or 384-well microtiter plates for medium to high-throughput. 24-well plates are traditional for plaque assays [75]. The choice impacts scalability and reagent usage. |
Methodologies for Key Validation Experiments
Assessing Assay Linearity and Range
Linearity evaluates whether the assay produces results that are directly proportional to the concentration of the analyte (e.g., antibody) within a given range [20]. The recommended methodology is:
- Prepare a series of dilutions of a positive control sample, covering the expected range of the assay (e.g., from below the lower limit of quantitation to above the upper limit of quantitation).
- Run these samples in the assay.
- Plot the measured signal (e.g., NT₅₀, % neutralization) against the expected value or dilution factor.
- Perform a linear regression analysis and, crucially, plot the studentized residuals. The assay is considered linear within the range where the studentized residuals fall within ±1.96, indicating no significant systematic deviation from the linear model [20].
Establishing Cut Points
The cut point is a critical value that determines the sample's positivity. The statistical approach is recommended [76]:
- Run the assay using a minimum of 25-30 individual, appropriate negative control samples (e.g., from naive donors).
- Calculate the mean and standard deviation of the neutralization titers or signals from these samples.
- The preliminary cut point is often set at the mean + 1.645 * standard deviation (for a 5% false positive rate in a one-tailed test).
- Adjust the cut point if needed based on additional validation data to control the desired false positive rate.
Experimental Workflow and Validation Logic
Neutralization Assay Workflow
Assay Validation and Troubleshooting Logic
Normalization Methods to Reduce Inter-Assay Variability
FAQs and Troubleshooting Guides
Core Concepts
What is inter-assay variability, and why is it a problem in viral load assays?
Inter-assay variability refers to the plate-to-plate or run-to-run inconsistency that can occur when the same samples are tested on different occasions. In the context of viral load assays, high inter-assay variability can lead to unreliable quantitation of viral particles, making it difficult to accurately monitor disease progression or treatment efficacy in patients. This variability can be caused by differences in technicians, equipment, reagent lots, or laboratory conditions across different runs [27].
How does normalization help reduce inter-assay variability?
Normalization uses a standard reference material analyzed in every assay run to correct for run-to-run technical variation. By establishing a fixed reference range for this standard plasma, you can create an internal quality control (IQC). Results from test samples can then be normalized against this standard, or experimental runs where the standard falls outside its pre-defined acceptance range can be excluded. This process significantly improves assay precision and ensures the production of accurate and reproducible data [80].
Methodologies and Protocols
What are the primary normalization methods used to improve assay precision?
The two primary normalization approaches involve using a standard reference plasma. The table below summarizes these core methodologies.
| Method | Description | Key Application |
|---|---|---|
| Result Normalization [80] | Test results from a sample are normalized using the concurrently run values from a standard reference plasma. | Correcting for technical variation by reporting values relative to a standard. |
| Run Acceptance Criteria [80] | A pre-defined acceptance range is established for the standard plasma. Experimental results are only valid if the standard's value falls within this range. | Ensuring that only data from technically sound assay runs are accepted and reported. |
Can you provide a protocol for establishing and using a reference standard?
The following workflow details the steps for implementing a reference standard to control inter-assay variability.
Detailed Protocol Steps:
- Select a Standard Plasma: Obtain a consistent and well-characterized standard plasma, such as the NIBSC reference plasma (TGT-RP) used in thrombin generation assays [80].
- Characterize the Standard: Run the standard plasma in a large number of independent experiments (e.g., 153 runs) under specific assay conditions (e.g., with 1 pM or 5 pM tissue factor, with or without thrombomodulin) [80].
- Calculate the Acceptance Range: For each parameter (e.g., Thrombin Peak, ETP), calculate the mean and standard deviation (SD) of the results from the standard plasma. The acceptance range is typically defined as the mean ± 2 SD [80].
- Routine Use as IQC: In every subsequent assay run, include this standard plasma.
- Apply Acceptance Criteria: If the value for the standard plasma falls within the pre-established acceptance range, the run is considered valid. If it falls outside the range, the results for that entire run should be rejected or the cause of the deviation investigated [80].
- (Optional) Normalize Data: To further reduce variability, raw data from test samples can be normalized using the value of the standard plasma from the same run [80].
Data Analysis and Interpretation
How do I calculate inter-assay CV to monitor variability over time?
The inter-assay Coefficient of Variation (CV) is calculated from the mean values of control samples (high and low) run on multiple plates. It is a key metric for monitoring plate-to-plate consistency [81]. The process is summarized in the table below.
| Step | Action | Example (High Control) |
|---|---|---|
| 1 | Run high and low controls on multiple plates (e.g., 10 plates). | - |
| 2 | Calculate the mean value for the control on each plate. | Plate 1 Mean: 1.090 µg/dL |
| 3 | Calculate the overall Mean of these plate means. | Mean of Means: 1.005 |
| 4 | Calculate the Standard Deviation (SD) of the plate means. | SD of Means: 0.051 |
| 5 | Calculate the % CV for the control: (SD of Means / Mean of Means) * 100. | % CV: (0.051 / 1.005) * 100 = 5.1% |
| 6 | The final inter-assay CV is the average of the high and low control % CVs. | Inter-assay CV = (5.1% + 6.3%) / 2 = 5.7% |
Example data derived from [81]
What are the recommended acceptance criteria for CVs?
For immunoassays, a general guideline is that inter-assay % CV should be less than 15% and intra-assay % CV should be less than 10% [81] [82]. However, these are general benchmarks, and criteria should be established based on the assay's intended use and the biological variation of the analyte.
Troubleshooting High Variability
My inter-assay CV is consistently high. What are the common causes and solutions?
High inter-assay CV indicates poor consistency between runs. The following diagram and table outline common culprits and corrective actions.
Common Causes and Solutions for High Inter-Assay CV:
| Category | Specific Issue | Corrective Action |
|---|---|---|
| Technical Error [83] [82] | Inconsistent pipetting | Practice proper technique; pre-wet tips; calibrate pipettes regularly [81] [82]. |
| Inconsistent incubation | Ensure stable incubation temperature; cover plates to prevent evaporation; use consistent timers [82]. | |
| Inconsistent sample handling | Standardize freeze-thaw protocols; ensure uniform sample preparation across runs [82]. | |
| Reagent & Plate [83] [82] | Reagent lot variation | Use large, uniform reagent lots for long-term studies; qualify new lots before use. |
| Inconsistent washing | Optimize and standardize wash volume and number of cycles across all runs [82]. | |
| Instrumentation [82] | Uncalibrated equipment | Perform regular calibration and maintenance of plate washers, readers, and automated pipettes [82]. |
What should I do if my normalization fails to improve data consistency?
If normalization does not resolve variability issues, consider these steps:
- Verify the Standard: Ensure the reference standard is stable and has been properly characterized. Using a standard plasma with an established reference range has been shown to significantly improve precision more than normalization alone [80].
- Check for Systematic Bias: Investigate if there is a systematic bias in your method that normalization cannot correct. Re-evaluate the method's precision (repeatability and intermediate precision) as part of a full or partial validation [27].
- Review Acceptance Criteria: Ensure the acceptance range for your internal quality control is appropriately set. An overly wide range will not catch problematic runs [80] [20].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and their functions for implementing effective normalization and variability control.
| Reagent / Material | Function in Variability Reduction |
|---|---|
| Standard Reference Plasma [80] | Serves as an internal quality control (IQC) to monitor run-to-run performance and allows for data normalization. |
| Control Samples (High & Low) [81] | Used to calculate the inter-assay CV, providing a quantitative measure of plate-to-plate consistency. |
| Calibrator RNA/DNA [84] | In amplification-based viral assays (e.g., NASBA), an internal calibrator is added to correct for extraction and amplification efficiency variances. |
| Optimized Blocking Buffers [83] | Reduces non-specific binding and background noise, which decreases well-to-well and plate-to-plate variation. |
| Consistent Reagent Lots | Using a single, large lot of critical reagents (antibodies, enzymes) for a study minimizes a major source of inter-assay variability. |
Optimizing Primer/Probe Concentrations and Thermal Cycling Conditions
FAQ: Why is optimizing primer and probe concentrations important for my viral assay?
Optimal primer and probe concentrations are fundamental to achieving a sensitive, specific, and efficient qPCR assay. Using suboptimal concentrations can lead to higher variability between replicates, decreased sensitivity, and non-specific amplification like primer-dimer formation, which can compromise your data reliability [85]. Research has demonstrated that varying primer concentrations can have a greater effect on assay performance than varying probe concentrations [85]. Proper optimization ensures your assay is robust enough for the precise linearity validation required in viral research.
FAQ: How do I optimize primer concentrations using a primer matrix?
A primer optimization matrix is a key tool for establishing robust assay conditions, especially when multiple assays need to run under identical thermal cycling conditions.
Detailed Methodology:
- Design your primers and probe following best practices (e.g., using tools like Primer-BLAST for specificity) [86].
- Prepare a matrix of reactions that test different combinations of forward and reverse primer concentrations. A common approach is to test three concentrations (e.g., 100 nM, 200 nM, and 300 nM) in all possible combinations [85].
- Run the qPCR reactions using a standardized template and your standard thermal cycling protocol.
- Analyze the results based on the following criteria to select the optimal combination:
- Low Cq value: Indicates high sensitivity and early detection.
- Low standard deviation between replicates: Ensures assay precision and reproducibility.
- High signal-to-noise ratio: Confirms robust fluorescence intensity.
- Minimal primer-dimer: Checked via melt curve analysis or gel electrophoresis to ensure specificity [85].
The table below summarizes typical outcomes from a primer matrix experiment:
Table 1: Primer Concentration Optimization Matrix Outcomes
| Forward Primer (nM) | Reverse Primer (nM) | Cq Value | Specificity (Melt Curve) | Recommended? |
|---|---|---|---|---|
| 100 | 100 | High | Specific | No |
| 100 | 200 | Medium | Specific | Possible |
| 100 | 300 | Medium | Specific | Possible |
| 200 | 100 | Medium | Specific | Possible |
| 200 | 200 | Medium | Specific | Yes (Default) |
| 200 | 300 | Low | Specific | Yes (Optimal) |
| 300 | 100 | Low | Specific | Possible |
| 300 | 200 | Low | Specific | Yes (Optimal) |
| 300 | 300 | Low | Primer-dimer | No |
Note: The "optimal" combination is often asymmetric (different concentrations for forward and reverse primers), which was the case for 65% of optimized assays in one study [85].
FAQ: What is the process for probe concentration optimization?
After identifying the best primer concentrations, you can further refine the assay by optimizing the probe concentration.
Detailed Methodology:
- Using the optimal primer concentration combination, run a set of qPCR reactions that test at least two different probe concentrations (e.g., 100 nM and 200 nM) [85].
- Compare the Cq values and signal intensity (signal-to-noise ratio) between the different probe concentrations.
- Select the lower probe concentration unless the higher concentration provides a significantly lower Cq value or a substantial improvement in signal intensity [85]. In practice, most assays (around 78%) perform optimally with a probe concentration of 100 nM [85].
FAQ: How do I optimize thermal cycling conditions for speed and specificity?
Thermal profile optimization is critical for efficient and rapid detection, which is especially valuable in viral diagnostics and high-throughput screening. The goal is to find the shortest times and most accurate temperatures that still allow for specific and efficient amplification.
Detailed Methodology:
- Annealing Temperature Optimization: If your thermocycler allows, perform a temperature gradient experiment to determine the optimal annealing temperature for your primer-probe set. This is the temperature that yields the lowest Cq value and highest fluorescence amplitude without non-specific amplification.
- Time Reduction: Test shorter durations for the annealing/extension step. The time must be long enough for the polymerase to synthesize the amplicon but can often be significantly shortened. For example, one study optimized a SARS-CoV-2 assay by reducing the 60-second annealing/extension step to 30 seconds without losing performance [87].
- Protocol Modification: Consider a two-stage cycling protocol for increased specificity. The optimized SARS-CoV-2 protocol used 8 initial cycles without fluorescence measurement, followed by 32 cycles with measurement, which reduced total reaction time by 40 minutes and improved the accuracy of the results [87].
Table 2: Example Thermal Cycling Protocol Optimization for Viral Detection
| Parameter | Standard Protocol | Optimized Protocol | Impact of Change |
|---|---|---|---|
| Reverse Transcription | 55°C for 10 min | 55°C for 4 min | Faster time-to-result [87] |
| Enzyme Activation | 95°C for 2 min | 95°C for 1 min | Faster time-to-result [87] |
| Cycling (Denaturation) | 95°C for 10 s | 95°C for 5 s | Faster time-to-result [87] |
| Cycling (Annealing/Extension) | 60°C for 60 s | 60°C for 30 s | Faster time-to-result; improved specificity [87] |
| Total Reaction Time | ~100 minutes | ~60 minutes | 40% reduction in run time [87] |
Experimental Workflow for Full Assay Optimization
The following diagram illustrates the stepwise workflow for systematically optimizing a qRT-PCR assay, from initial preparation to final validation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for qPCR Optimization
| Reagent / Kit | Function in Optimization |
|---|---|
| PCR Optimization Kits (e.g., buffers A-H) [86] | Contains a range of pre-formulated buffer chemistries to find the optimal salt and additive conditions for your specific primer-probe set and template. |
| Hot Start DNA Polymerase | Reduces non-specific amplification and primer-dimer formation by inhibiting polymerase activity until the high-temperature denaturation step. |
| One-Step RT-qPCR Master Mix | A pre-mixed solution containing reverse transcriptase, DNA polymerase, dNTPs, and optimized salts. Simplifies reaction setup and reduces pipetting variability during optimization [88]. |
| Inhibitor-Resistant Master Mix | Essential for analyzing complex sample types like blood or crude lysates, as it maintains robust amplification efficiency in the presence of common PCR inhibitors [88]. |
| Universal ProbeLibrary (UPL) [85] | A set of short, hydrolyzed probes that can be used to design assays for many targets, often requiring only primer optimization. |
| DNase I (RNase-free) | Critical for removing contaminating genomic DNA from RNA samples to ensure that amplification is derived from the RNA target (e.g., viral RNA) [89]. |
| RNase Inhibitor | Protects precious RNA templates from degradation during reverse transcription and PCR setup, which is vital for maintaining assay sensitivity [86]. |
Should you require further assistance with a specific optimization challenge, consult the MIQE guidelines for comprehensive best practices [43].
In viral assay precision and linearity validation research, the accuracy of results is paramount. A significant challenge in achieving this accuracy is managing preanalytical errors, which account for as much as 70% of all errors in laboratory medicine diagnostic testing [90]. Among the most common preanalytical interferences are those caused by hemolytic, lipemic, and icteric sample matrices. These endogenous substances can interfere with assay components or cause physiological changes to the serum or plasma, leading to erroneous results. This guide provides researchers and drug development professionals with targeted troubleshooting and FAQs to identify, understand, and resolve these interferences, thereby ensuring the reliability of data in critical viral assay studies.
Understanding the Interferences
Hemolysis
What is hemolysis and how does it affect lab tests? Hemolysis is defined by the release of hemoglobin and intracellular components from erythrocytes into serum or plasma. While it can be characteristic of a pathology like hemolytic anemia, it is most often a result of in vitro disruption of red blood cells during sample collection, transportation, or storage [90].
Interference occurs through two primary mechanisms:
- Release of Intracellular Components: This falsely elevates serum/plasma concentrations of analytes such as potassium and lactate dehydrogenase, while diluting others like sodium [90].
- Spectral Interference: Hemoglobin absorbs light at 340–400 nm and 540–580 nm wavelengths, which can prevent the accurate photometric measurement of analytes in specific assays [90].
Lipemia
What is lipemia and how does it affect lab results? Lipemia is an endogenous interference defined by an elevation of lipids in serum or plasma, making the sample appear cloudy [91] [90]. It is most often caused by inadequate time between a patient's last meal and blood sampling, or by parenteral administration of synthetic lipid emulsions [91].
Lipemia interferes through several mechanisms:
- Spectral Interference: Lipoprotein particles can scatter and absorb light, particularly at lower wavelengths. Methods using 340 nm, such as NAD(P)H-based reactions (e.g., for ALT, AST, glucose), are strongly affected [91].
- Volume Displacement Effect (VDE): Lipids alter the ratio of aqueous to non-aqueous components in serum. For analytes dissolved in the aqueous phase, this results in a spuriously low concentration. This is a particular problem for measuring electrolytes by indirect ion-selective electrode (ISE), which involves a dilutional step [91] [90].
- Physical and Chemical Interference: Lipoproteins can interfere with antigen-antibody reactions in immunoassays, causing either falsely elevated or decreased results. They can also cause abnormalities in electrophoretic methods [91].
Icterus
What is icterus and how does it interfere with lab tests? Icterus is an endogenous interference defined by an elevation of bilirubin. It is visually identified by a yellow-green coloration of serum/plasma and is detected photometrically at an absorbance of 480 nm and 505 nm [90]. Interference is caused either by spectral interference or by reactivity with assay reagents. It is important to note that both conjugated and unconjugated bilirubin can cause different levels of interference, and the amount of each type can vary significantly between specimens [90].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our laboratory frequently receives hemolyzed samples from the clinical unit. What are the most effective strategies to prevent this? A: Prevention is key for hemolysis, as there is no way to analyze a hemolyzed sample after the fact [90]. Focus on:
- Specimen Collection: Communicate with phlebotomists and nursing personnel about correct blood draw technique. Factors such as tourniquet time, fill volume, needle size, and gentle specimen mixing are critical. Venipuncture has been shown to reduce hemolysis by as much as 84 percent compared to draws via intravenous catheters (IV) [90].
- Sample Transportation: Pneumatic tube systems (PTS) expose specimens to damaging g-forces. Mitigation strategies include padding carriers with foam, reducing transport speeds, using tubes with clotting additives, and using thermally insulated courier lockboxes for outpatient samples [90].
Q2: How can I resolve interference caused by a lipemic sample in my viral neutralization assay? A: Unlike other interferences, lipemia can often be removed from the sample.
- Ultracentrifugation: This is the most effective method. High g-forces separate the lipids from the serum/plasma, resulting in an interference-free specimen [90]. The resulting clear infranatant can then be used for analysis.
- Alternative Measurement Techniques: For electrolyte measurement, using direct ion-selective electrodes (e.g., on blood gas analyzers) avoids the volume displacement effect because this technique does not require a dilutional step [90].
- Sample Dilution: In some cases, dilution can reduce the interference below the threshold, but this must be validated for the specific assay as it may affect the lower limit of quantitation [90].
Q3: Are manufacturer-provided lipemia interference thresholds reliable? A: You should critically evaluate manufacturer thresholds. Most manufacturers use an intravenous lipid emulsion called Intralipid to simulate lipemia. Several studies have shown that Intralipid does not replicate the diversity of lipids found in vivo, and consequently, Intralipid-derived thresholds are often set too high to accurately detect lipemic interference in patient samples [90]. It is recommended that clinical laboratories verify these thresholds using their own methodologies.
Q4: What is the best approach for dealing with an icteric sample? A: Unlike lipids, bilirubin cannot be easily removed from serum/plasma.
- Dilution: The primary method for resolving icteric interference is to dilute the sample to reduce the bilirubin concentration below the interference threshold [90].
- Validation is Crucial: This approach requires a validated dilutional protocol for the assay. Furthermore, dilution may not be feasible for assays with a high lower limit of quantitation (LLOQ) [90]. Laboratories should always validate manufacturer-set thresholds for icteric interference, as these can vary between instruments and assays [90].
Quantitative Interference Thresholds
The following table summarizes the characteristic visual and photometric features of the three interferences. Note that interference thresholds are assay- and analyzer-dependent; these values should be verified internally.
Table 1: Characteristic Features and Measurement of Common Interferences
| Interference Type | Visual Indicator | Primary Photometric Absorbance (nm) | Common Affected Analytes |
|---|---|---|---|
| Hemolysis | Reddish hue in serum/plasma [90] | 340-400, 540-580 [90] | Potassium (↑), Lactate Dehydrogenase (↑), Sodium (↓) [90] |
| Lipemia | Cloudy, milky, pale-yellow appearance [91] [90] | Turbidity measured at 570, 660 [90]; strongest interference at lower wavelengths (e.g., 340) [91] | Electrolyes (↓ by VDE), Bilirubin (variable), Photometric assays at low wavelengths [91] [90] |
| Icterus | Yellow-green coloration [90] | 480, 505 [90] | Assays susceptible to spectral overlap or chemical reactivity with bilirubin [90] |
Experimental Protocols for Interference Testing
A critical component of viral assay validation is assessing the assay's susceptibility to these interferences. The following protocol is adapted from validation approaches for immunoassays and cellular immune response tests [92] [93].
Protocol for Determining Lipemic Interference in a Viral Neutralization Assay
1. Principle: This experiment evaluates the effect of lipemia on the accuracy of a viral neutralization assay by spiking patient samples with a known lipid emulsion (e.g., Intralipid) at various concentrations and comparing the results to an unspiked control.
2. Materials:
- Test serum samples (pooled, known positive and negative for neutralizing antibodies)
- Lipid emulsion (e.g., Intralipid)
- Viral neutralization assay reagents (cells, virus, detection antibodies)
- Standard laboratory equipment (pipettes, incubator, centrifuge, spectrophotometer)
3. Procedure: a. Prepare Lipemic Samples: Spike the test serum samples with increasing volumes of the lipid emulsion to create a series of samples with known, graded levels of lipemia (turbidity). The highest concentration should exceed the level expected in typical patient samples. b. Measure Lipemic Index: Determine the lipemic index (or triglyceride concentration) for each spiked sample and the unspiked control using a clinical chemistry analyzer [91]. c. Run Neutralization Assay: Perform the viral neutralization assay (e.g., microneutralization assay as described in [92]) on all samples (spiked and unspiked) in the same run to avoid inter-assay variability. d. Calculate Neutralization Titer: Determine the neutralizing antibody titer for each sample.
4. Data Analysis:
- Compare the neutralizing antibody titer of each lipemic sample to the titer of the unspiked control.
- Calculate the percentage bias:
[(Titer_lipemic - Titer_control) / Titer_control] * 100. - The interference threshold is defined as the lipemic index at which the bias exceeds a pre-defined acceptance criterion (e.g., ±10% or based on biological variation) [91].
Workflow for Systematic Interference Investigation
The logical flow for designing and executing an interference study is outlined in the following diagram.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials used in managing and studying sample interferences.
Table 2: Essential Reagents and Materials for Interference Management
| Item | Function/Application | Example Use Case |
|---|---|---|
| Intralipid | A synthetic lipid emulsion used to simulate lipemic conditions in validation studies [91] [90]. | Spiking into normal serum to create lipemic quality control materials or to determine interference thresholds for an assay [90]. |
| Lympholyte-Mammal | Density gradient medium for the isolation of peripheral blood mononuclear cells (PBMCs) from whole blood [93]. | Preparing high-quality PBMCs for cellular immune response assays (e.g., IFN-γ ELISpot) from potentially hemolyzed or lipemic blood samples [93]. |
| CryoStor CS10 | Serum-free, GMP-compatible cryopreservation medium [93]. | Preserving the viability and functionality of isolated PBMCs for later batch analysis in viral assay studies [93]. |
| IFN-γ ELISpot Kit | A standardized kit for enumerating antigen-specific T-cells by detecting secreted interferon-gamma [93]. | Monitoring cellular immune responses to viral vectors or vaccines; validation should include testing with hemolytic, lipemic, and icteric PBMC samples [92] [93]. |
| Peptide Pools (e.g., JPT) | Overlapping peptides spanning viral antigens (e.g., CMV, AAV capsid) used to stimulate T-cells [93]. | Investigating T-cell responses in ELISpot or other cellular assays to determine if interference affects cell function rather than just readout [93]. |
Establishing Robust Internal Quality Control Systems
FAQs: Fundamentals of Internal Quality Control
Q1: What is the primary purpose of an Internal Quality Control (IQC) in viral assays? The primary purpose of an IQC is to monitor the accuracy and precision of an assay during routine use, ensuring that results are reliable. It acts as a real-time check for each run, detecting errors arising from reagent degradation, operator variability, or instrument malfunction. In viral assays, this is crucial for distinguishing true negative results from assay failure [94].
Q2: How does a process control differ from a positive control? A positive control confirms that the assay can detect the target pathogen when it is present. A process control (or internal control) confirms that the entire sample processing and analysis procedure has worked correctly, even when the target pathogen is absent. For example, targeting a human gene like RNase P in a respiratory sample verifies that human cells were properly collected, nucleic acid was successfully extracted, and amplification was not inhibited [94] [95].
Q3: What are the key parameters to validate for an IQC system? Key validation parameters include precision (repeatability and reproducibility), accuracy, the limit of detection (LoD), robustness, and specificity. These parameters provide objective evidence that the IQC is fit for its purpose and can reliably detect deviations in assay performance [27] [32].
Q4: Our qPCR results are inconsistent. Could this be due to poor QC? Yes, inconsistent results often highlight QC issues. Common causes and solutions include:
- Inhibitors in Sample: Add an internal process control (e.g., RNase P) to detect inhibition. Re-extract or dilute the sample if the control fails [94] [96].
- Reagent Degradation: Use a positive control with a known, stable concentration to monitor reagent performance. A shift in the control's quantification cycle (Cq) can indicate loss of potency.
- Pipetting Inaccuracy: Implement a digital PCR-based QC, which is less sensitive to volumetric errors, to validate your pipetting accuracy and reaction setup [70].
Q5: How can we establish an IQC for a digital PCR-based viral copy number assay? For droplet digital PCR (ddPCR), traditional single-gene reference materials can be unreliable. A robust approach is to use a synthetic hybrid amplicon that links the viral target amplicon (e.g., WPRE) to a reference gene amplicon (e.g., RPP30). This linked control ensures that both targets are amplified with equal efficiency, providing a true one-to-one ratio that validates the accuracy of the partitioning, PCR, and analysis steps [70].
Troubleshooting Guides
Problem: Erratic Recovery of Internal Control
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| Delayed or absent amplification of the process control (e.g., RNase P) in both positive and negative samples. | PCR Inhibition: Carryover of inhibitors from the sample matrix. | Dilute the extracted nucleic acid and re-amplify. Use an internal process control to monitor for inhibition in every sample [94]. |
| Inefficient Nucleic Acid Extraction: Lysis or binding failure during extraction. | Include a control of known concentration to validate the extraction kit and procedure [96]. | |
| Consistently low signal across all samples and controls. | Degraded QC Material: The stock solution of the internal control is degraded. | Prepare a new aliquot of the control material and re-test. |
| Faulty Reagent in Master Mix: The enzyme or buffers in the PCR master mix are inactive. | Test a new batch or lot of master mix. |
Problem: Poor Assay Precision and High Variability
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| High %CV in replicate samples or controls. | Inconsistent Pipetting: Especially critical when making serial dilutions for qPCR or neutralization assays. | Regularly calibrate pipettes; train operators on proper technique; use digital PCR for absolute quantification, which is less sensitive to volumetric variation [70]. |
| Cell Culture Variability: In cell-based assays (e.g., plaque, neutralization), cell passage number or confluence varies. | Control cell culture conditions strictly; use cells within a validated passage range (e.g., passages 5-19) [32] [97]. | |
| Drift in control values over time. | Reagent Lot Change: A new lot of a key reagent has different performance. | Re-validate critical assay performance parameters when introducing a new reagent lot [27]. |
Experimental Protocols for Core Validation Experiments
Protocol: Precision and Linearity Validation for a Viral Load Assay
This protocol is used to establish the repeatability and linearity of a quantitative viral assay, such as qRT-PCR or ddPCR.
1. Methodology:
- Sample Preparation: Create a linear dilution series of the target virus or a synthetic control (e.g., hybrid amplicon) in the appropriate matrix (e.g., saline, negative serum). The series should span the entire claimed dynamic range of the assay [70].
- Testing: Analyze each dilution level with a minimum of five replicates within a single run (for repeatability) and over at least three separate runs on different days (for intermediate precision) [27].
- Data Analysis:
- Calculate the mean, standard deviation (SD), and percentage coefficient of variation (%CV) for the measured concentration at each dilution level.
- Plot the measured values against the expected values and perform regression analysis.
- Evaluate linearity using statistical methods like the two one-sided tests (TOST) procedure to prove that the average deviation from linearity (ADL) falls within a pre-defined acceptable limit [36].
2. Validation Parameters & Acceptance Criteria:
| Parameter | Measurement | Acceptance Criteria |
|---|---|---|
| Repeatability | Intra-assay %CV | Typically ≤ 25-30% for cell-based assays; ≤ 10% for molecular assays [97] [95]. |
| Intermediate Precision | Inter-assay %CV | Typically ≤ 25-30% for cell-based assays; ≤ 15% for molecular assays [97]. |
| Linearity | R² value from regression | R² ≥ 0.98 is generally acceptable, but should be justified for the assay context [36]. |
Protocol: Incorporating a Process Control to Enhance Sensitivity
This protocol details how to integrate a human gene target to monitor sample quality and avoid false negatives.
1. Methodology:
- Assay Design: Design a multiplex assay that simultaneously detects the viral target (e.g., SARS-CoV-2 E gene) and a human process control gene (e.g., RNase P) [94] [95].
- Sample Processing: Extract nucleic acids from clinical samples (e.g., nasopharyngeal swabs) and run the multiplex assay.
- Data Interpretation:
- A valid test requires successful amplification of the RNase P control.
- Samples negative for the viral target but positive for RNase P are classified as true negatives.
- Samples negative for both targets are considered inconclusive/invalid, as this indicates poor sample collection or the presence of inhibitors.
2. Validation Data: As demonstrated in the ViraLite HIV test, incorporating RNase P as a process control allowed the identification of 17 inconclusive samples that would have been misclassified as negative. This increased the assay's clinical sensitivity from 66.66% to 93.33% while maintaining 100% specificity [94].
Workflow and System Diagrams
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Quality Control | Example & Notes |
|---|---|---|
| Synthetic Hybrid Amplicon | A linked DNA fragment used to validate duplex ddPCR assays. Provides a 1:1 ratio of target and reference genes to check partitioning and reaction efficiency [70]. | WPRE-RPP30 amplicon connected by a HindIII site for Viral Copy Number (VCN) assays. |
| Process Control Gene | A naturally occurring target in samples used to monitor nucleic acid extraction and check for PCR inhibition. | RNase P: A human gene used as an internal control in tests from nasopharyngeal swabs [94] [95]. |
| Reference Viral Strains | Well-characterized viruses used as positive controls and for assessing assay specificity and cross-reactivity. | WHO Influenza Strains: (e.g., A/Thailand/8/2022) are essential for validating neutralization and detection assays against current strains [98]. |
| Plaque Assay Components | Cell-based system for quantifying infectious virus titer, a key potency measure for live viral vaccines. | Vero E6 Cells & Overlay Medium: Critical for the validated plaque assay used to titer the BriLife SARS-CoV-2 vaccine [32]. |
| Digital PCR (ddPCR) | A technology for absolute quantification of viral load without a standard curve. Superior for detecting small fold-changes and validating assay precision [70]. | QX200 ddPCR System (Bio-Rad). Used with hybrid amplicons for robust VCN assay validation. |
Validation Frameworks: Comparative Analysis and Regulatory Compliance
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: When validating a new high-sensitivity ddPCR assay, my results for low viral load samples are inconsistent. What could be the cause? Inconsistent results near the detection limit often relate to sample input volume and reaction partitioning. For a ddPCR Hepatitis B virus DNA assay, ensure you use at least 200 μL of serum for the RNA extraction step to concentrate the target and achieve a lower limit of detection of 1.6 IU/mL. Low-concentration inconsistency can also be due to improper droplet generation; verify that the droplet generator is functioning correctly and that no droplets have merged or ruptured [68].
Q2: My new multiplex respiratory virus assay shows high background in one fluorescence channel. How can I resolve this? High background in a specific channel of a multiplex assay, such as a quadruplex RT-ddPCR, typically indicates fluorescent probe interference. Ensure that the probe concentrations for each target in the mix are optimized and balanced; a common starting point is 0.8 μL of probe mix per 20 μL reaction. Also, confirm that the spectral properties of the probes are compatible and that there is no cross-talk between the channels on your detection platform [28].
Q3: I am transitioning from an ELISA to a multiplex bead array. What is the key factor in ensuring the new assay's accuracy? The most critical factor is using a validated antibody pair. Multiplex immunoassays rely on highly specific antibody-antigen interactions for each analyte measured concurrently. Unlike singleplex ELISA, cross-reactivity between antibodies in a multiplex setting can lead to inaccurate results. Always run a parallelism experiment to ensure the new multiplex assay behaves similarly to your gold standard ELISA when measuring serially diluted real-world samples [99].
Q4: In my colorimetric viral titration assay, the signal is saturated even at low viral doses. What should I do? Signal saturation usually means the cell monolayer's metabolic activity is being measured outside the assay's linear range. For a tetrazolium-based (MTS) assay, you must first establish a calibration curve that correlates formazan absorbance with viral dose. If saturated, reduce the incubation time with the virus or with the MTS reagent. Alternatively, reduce the number of cells seeded per well in the 96-well plate to bring the measurement back into the linear regime [100].
Troubleshooting Common Assay Validation Issues
Problem: Poor Linearity in a New Digital PCR Assay
- Potential Cause: The dynamic range of digital PCR is constrained by the number of partitions. Poor linearity often occurs at high target concentrations where partitions become saturated.
- Solution: Dilute the sample and re-run the assay. For absolute quantification, ensure the sample concentration falls within the linear range established during validation, which for a modern ddPCR system can be from single copies per microliter to tens of thousands [28] [68].
Problem: Low Analytical Specificity in a Multiplex Assay
- Potential Cause: Primer or probe cross-reactivity with non-target sequences or between targets in the multiplex reaction.
- Solution: Perform rigorous in silico specificity checks (e.g., BLAST) during design. Experimentally, test the assay against a panel of closely related pathogens or analytes to identify and eliminate cross-reactive components. The quadruplex RT-ddPCR for respiratory viruses, for instance, was validated against other common pathogens like parainfluenza and adenovirus to ensure specificity [28].
Problem: High Intra-Assay Variation in a Cell-Based Neutralization Assay
- Potential Cause: Inconsistent cell seeding density or viability across the assay plate.
- Solution: Standardize the cell culture protocol. Ensure cells are passaged at a consistent confluence and are seeded at an optimized, uniform density. Using an automated cell counter and a calibrated multichannel pipette can significantly improve reproducibility. In the validated YF MN assay, precise cell culture was critical for achieving an intermediate precision of 54% [92].
Problem: Significant Discrepancy Between New Immunoassay and Gold Standard MS Results
- Potential Cause: Immunoassays are susceptible to cross-reactivity with structurally similar compounds or metabolites, leading to false positives.
- Solution: Always run a confirmation test using a gold standard method like LC-MS/MS for a subset of samples, especially those near the cut-off value. Calculate the measurement uncertainty for the immunoassay to understand its performance boundaries. A study on drugs of abuse screening found that performance between different immunoassays (CEDIA, EMIT II Plus) varied significantly, reinforcing the need for confirmation [101].
Quantitative Data from Comparative Studies
The tables below summarize key performance metrics from recent validation studies, providing a benchmark for new assay development.
Table 1: Analytical Performance of New Viral Detection Assays
| Assay Name | Target | Linear Range | Limit of Detection (LOD) | Key Advantage vs. Gold Standard |
|---|---|---|---|---|
| AHQR–ddPCR [28] | IFA, IFB, RSV, SARS-CoV-2 | Wide linear range demonstrated | 0.65–0.78 copies/μL | Absolute quantification without standard curve; higher sensitivity than RT-PCR. |
| HBV ddPCR [68] | Hepatitis B Virus DNA | ( R = 0.994 ), ( R^2 = 0.988 ) | 1.6 IU/mL | Higher sensitivity with lower serum input (200 μL) than real-time PCR. |
| YF MN Assay [92] | Yellow Fever Virus Neutralizing Antibodies | LLOQ: 10 (1/dil) to ULOQ: 10,240 (1/dil) | LLOQ: 10 (1/dil) | Higher throughput and objective readout vs. Plaque Reduction Neutralization Test (PRNT). |
Table 2: Performance Comparison of Immunoassay Platforms for Drugs of Abuse Screening [101]
| Immunoassay Platform | Best For | Performance Note |
|---|---|---|
| EMIT II Plus | Cannabinoids, Amphetamine, Ecstasy, Opiates | Showed better performance for these drug classes compared to CEDIA and DRI assays. |
| CEDIA | Cocaine, Methadone, Heroin, Benzodiazepines | No discrepancy with EMIT II Plus for these drug classes. Second-generation assay superior for Buprenorphine. |
| DRI | Oxycodone | No discrepancy with Immunalysis EIA for Oxycodone. |
| EIA (Immunalysis) | Fentanyl | The Ark EIA method performed slightly better than the DRI method. |
Detailed Experimental Protocols
Protocol 1: Automated High-Throughput Quadruplex RT-ddPCR for Respiratory Viruses
This protocol is for the simultaneous detection and absolute quantification of Influenza A, Influenza B, RSV, and SARS-CoV-2 RNA on the QX ONE Droplet Digital PCR System [28].
- RNA Extraction: Extract viral RNA from 300 μL of sample (e.g., nasopharyngeal swab in transport medium) using an automated nucleic acid extraction system (e.g., EX3600). Elute the purified RNA in 50 μL of elution buffer. Store at -80°C if not used immediately.
- Reaction Mix Preparation: Prepare the PCR master mix on ice in a 1.5 mL microcentrifuge tube. For a single 20 μL reaction, combine:
- 5 μL of RNA template
- 5 μL of One-Step RT–ddPCR Advanced Supermix
- 2 μL of Reverse Transcriptase (20 U/μL)
- 1 μL of Dithiothreitol (DTT, 15 mM)
- 4.8 μL of primer mix (containing all forward and reverse primers)
- 0.8 μL of probe mix (containing all fluorescently-labeled probes)
- 1.4 μL of Nuclease-Free Water
- Droplet Generation: Pipette the entire 20 μL reaction mix into the sample well of a DG8 Cartridge. Carefully add 70 μL of Droplet Generation Oil to the oil well. Place the cartridge into the Droplet Generator. The instrument will automatically generate thousands of nanoliter-sized droplets.
- PCR Amplification: Transfer the emulsified samples to a 96-well PCR plate. Seal the plate with a foil heat seal. Perform reverse transcription and PCR amplification on a thermal cycler using the following protocol:
- Reverse Transcription: 25°C for 3 min, 48°C for 20 min.
- Enzyme Activation: 95°C for 5 min.
- Amplification (45 cycles): 95°C for 15 s (denaturation), 55°C for 30 s (annealing/extension).
- Enzyme Deactivation: 98°C for 10 min.
- Hold: 25°C forever. (Use a ramp rate of 2°C/s for all steps).
- Droplet Reading and Analysis: Place the PCR plate into the QX ONE Droplet Reader. The instrument will automatically read the fluorescence in each droplet from four independent fluorescence channels. Use the system's software to analyze the data and apply Poisson statistics to determine the absolute concentration (copies/μL) of each viral target in the original reaction.
Protocol 2: Colorimetric High-Throughput Screening (HTS) Viral Titer Assay
This protocol uses a tetrazolium salt (MTS) to measure virus-induced cytopathic effect (CPE) as a surrogate for viral titration, providing results much faster than traditional TCID50 or plaque assays [100].
- Cell Seeding: Seed a permissive cell line (e.g., Vero cells) in a 96-well plate at a consistent, optimized density (e.g., 1x10^4 cells/well in 100 μL growth medium). Incubate the plate for 24 hours at 37°C with 5% CO2 to form a semiconfluent monolayer.
- Virus Inoculation: Remove the growth medium from the cells. Add 100 μL of the viral suspension (or negative control medium) to the test wells. For a full titration, a dilution series may be required, but the assay can be used without dilution within its predetermined linear range. Incubate the plate for a virus-specific period (e.g., 48-72 hours) until CPE is evident in the positive control wells under a microscope.
- MTS Reagent Application: Prepare a homogeneous mixture of MTS reagent and culture medium according to the manufacturer's instructions. Carefully remove the supernatant from the 96-well plate to eliminate detached dead cells. Add 120 μL of the MTS-medium mixture to each well.
- Formazan Development: Incubate the plate for 1-4 hours at 37°C with 5% CO2. Metabolically active living cells will convert the MTS reagent into a brown-colored formazan product.
- Absorbance Measurement: Measure the absorbance of each well at a wavelength of 490 nm using a multi-well plate reader.
- Data Analysis: Calculate the percentage of cell viability for each test condition using the formula:
Cell Viability (%) = [(A_tested - A_MTS) / (A_CTRL100% - A_MTS)] * 100Where:A_tested= Absorbance of the virus-infected well.A_MTS= Absorbance of the background control (MTS-medium with no cells).A_CTRL100%= Absorbance of the negative control (mock-infected, 100% viable cells). The viral titer is then determined by comparing the cell viability to a pre-established calibration curve that correlates viability with known viral doses (e.g., TCID50/mL).
Experimental Workflow Visualization
Assay Validation Workflow
HTS Colorimetric Viral Titer Assay
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Advanced Assay Development
| Item | Function / Application | Example from Literature |
|---|---|---|
| QX ONE Droplet Digital PCR System | Automated, high-throughput absolute quantification of nucleic acids; enables multiplexing with 4-color detection. | Used for the AHQR–ddPCR assay for respiratory viruses [28]. |
| One-Step RT–ddPCR Advanced Kit | Integrated reverse transcription and digital PCR chemistry for direct RNA target detection and quantification. | Core reagent for the quadruplex respiratory virus assay [28]. |
| Automated Nucleic Acid Extractor | Standardizes and streamlines the purification of nucleic acids from complex samples, reducing manual error. | EX3600 system used for RNA extraction in clinical sample validation [28]. |
| Tetrazolium Salt (MTS Reagent) | Colorimetric indicator of cellular metabolic activity; used to quantify cell viability in viral infection assays. | Core of the high-throughput viral titer screening assay [100]. |
| Validated Antibody Pairs | Essential for developing specific and accurate multiplex immunoassays (e.g., bead-based arrays). | Noted as a critical requirement for multiplex immunoassays to ensure specificity for each analyte [99]. |
| Reference Materials | Calibrators with known analyte concentrations, critical for determining the accuracy and linearity of a new assay. | Commercial reference materials (e.g., from CNIM) used for analytical validation of the AHQR–ddPCR assay [28]. |
Setting Statistical Acceptance Criteria for Precision and Linearity
Troubleshooting Guides
Guide 1: Addressing High Variation in Replicate Measurements (Precision)
Problem: The coefficient of variation (%CV) from repeatability or intermediate precision experiments consistently exceeds your pre-defined acceptance criteria.
Investigation & Solutions:
Step 1: Check for Technical Replication Errors.
- Action: Review laboratory procedures for consistency in pipetting, reagent preparation, incubation times, and equipment calibration across all analysts and test runs.
- Rationale: Minor technical inconsistencies are a major source of inflated %CV in cell-based assays [97].
Step 2: Inter-Analyst Comparison.
- Action: Implement a study where two analysts perform the assay in parallel on the same samples and also re-count or re-analyze each other's plates [102] [103].
- Rationale: This evaluates operator-dependent variability. High agreement between analysts, confirmed by statistical methods like intraclass correlation, indicates the protocol is robust. Disagreement points to a need for standardized training [102] [103].
Step 3: Evaluate Cell Culture and Reagent Stability.
- Action: Ensure consistent passage number and health of cell lines (e.g., Vero E6). Use freshly prepared or properly aliquoted and stored reagents to avoid freeze-thaw cycles that can degrade components [102] [97].
- Rationale: Biological components like cells and viruses are intrinsic sources of variation; their stable quality is foundational for assay precision [102].
When to Consider Re-defining Criteria: If the investigation reveals the high %CV is an inherent property of the biological system (e.g., a cell-based neutralization assay), and all procedural issues have been mitigated, compare your data to field-accepted norms. For viral assays, a %CV of ≤30% is often deemed acceptable [102] [103] [97].
Guide 2: Failure to Meet Linearity Acceptance Criteria
Problem: The assay's linear regression analysis fails to meet criteria for the coefficient of determination (R²), slope, or intercept over the intended range.
Investigation & Solutions:
Step 1: Verify Antigen/Virus Titration.
- Action: Re-titrate the critical reagent (e.g., virus, recombinant protein) to ensure the amount used in the linearity assessment falls within the dynamic, linear range of the detection method [104].
- Rationale: Using too much or too little antigen can cause a plateau or loss of signal, compressing the range and distorting linearity [104].
Step 2: Assess Sample Dilution Series.
- Action: Confirm that serial dilutions are performed accurately and that the sample matrix does not cause non-linear effects at the extremes of the range (e.g., very high or low concentrations) [102].
- Rationale: Matrix effects can interfere with the assay's ability to detect a proportional signal. A sufficient number of data points across the range (e.g., 5 points as used in USP <1033>) improves the reliability of the linearity assessment [24].
Step 3: Re-evaluate the Assayed Range.
- Action: The assay may be linear over a narrower range than initially selected. Analyze a subset of the data to determine if a shorter range meets the R², slope, and intercept criteria [24].
- Rationale: It is preferable to validate a smaller, linear range than to force a linear model onto a non-linear relationship.
Frequently Asked Questions (FAQs)
FAQ 1: What is an acceptable %CV for a viral neutralization or plaque assay? For cell-based bioassays, such as filovirus plaque assays or SARS-CoV-2 microneutralization assays, a %CV of ≤30% is generally considered an acceptable level of variation for precision (repeatability and intermediate precision) [102] [103] [97].
FAQ 2: What statistical approach should I use to set acceptance criteria for linearity and accuracy? A recommended method is to use confidence interval (CI) comparisons. Following USP <1033>, you calculate two-sided 90% CIs for parameters like slope, intercept, and %relative bias. Equivalence is concluded only if the entire CI falls within a pre-defined Equivalence Acceptance Criteria (EAC) interval [24]. This method directly relates these parameters to the assay's %CV.
FAQ 3: How can I improve the reproducibility of my assay across multiple laboratories? The use of a common calibrator or standard serum to normalize results has been proven to significantly improve inter-laboratory agreement. This practice helps correct for systematic variability between different reagent batches, equipment, and operators [104].
FAQ 4: What is the difference between biological and technical replicates, and why does it matter?
- Technical Replicates: Multiple measurements taken from the same biological sample (e.g., running the same extracted RNA sample in three PCR wells). They measure the variability of the assay procedure itself.
- Biological Replicates: Measurements taken from different, independent biological samples (e.g., cells or serum from different animals or donors). They measure the true biological variability in the system [105]. For validation, both are important, but biological replicates are essential for defining the overall precision of the assay in a real-world context.
Experimental Protocols for Validation
Protocol 1: Assessing Assay Precision (Repeatability & Intermediate Precision)
This protocol evaluates the closeness of agreement between results under defined conditions.
- Sample Preparation: Prepare a minimum of three Quality Control (QC) samples at low, medium, and high concentrations within the assay's dynamic range [102].
- Repeatability (Intra-assay Precision):
- Intermediate Precision (Inter-assay Precision):
- Acceptance Criteria: The calculated %CV for all QC levels should be less than or equal to a pre-defined limit (e.g., ≤30% for viral titers) [102] [103].
Protocol 2: Establishing Assay Linearity
This protocol validates that the assay produces results that are directly proportional to the analyte concentration.
- Sample Series: Prepare a dilution series of the analyte (e.g., virus, recombinant protein) that spans the entire claimed range of the assay. A minimum of 5 concentrations is recommended [24].
- Assay Execution: Test each concentration in the series with an appropriate number of replicates (e.g., n=3-8) within a single run to minimize inter-assay variability [24] [102].
- Data Analysis:
- Plot the measured response (e.g., PFU/mL, spot count, OD) against the expected concentration or dilution factor.
- Perform linear regression analysis to determine the coefficient of determination (R²), slope, and y-intercept.
- Statistical Acceptance: Apply confidence intervals to the regression parameters. For example, conclude linearity if the 90% CI for the slope contains 1 and the CI for the intercept contains 0, or if these CIs fall entirely within your EAC [24]. A high R² (e.g., >0.98) may also be a criterion.
Table 1: Examples of Statistical Acceptance Criteria from Viral Assay Validations
| Assay Type | Validation Parameter | Reported Acceptance Criteria | Source / Context |
|---|---|---|---|
| Filovirus Plaque Assay | Precision (%CV) | ≤30% | [102] [103] |
| Filovirus Plaque Assay | Accuracy (%Relative Bias) | ±0.5 log₁₀ PFU/mL | [102] [103] |
| IFN-γ ELISpot | Precision (Intra-/Inter-assay %CV) | Specific to validated cut point & LOD | [41] |
| Multiplex RT-PCR | Precision (Intra-/Inter-assay Variation) | Maximum variation of 4.41% | [106] |
| Bioassay (General) | Linearity (Slope) | 90% CI for slope contained within EAC* | [24] |
| Bioassay (General) | Linearity (Intercept) | 90% CI for intercept contained within EAC* | [24] |
EAC: Equivalence Acceptance Criteria, determined a priori by subject matter experts [24].
Research Reagent Solutions
Table 2: Key Reagents for Viral Assay Validation
| Reagent / Material | Function in Validation | Example from Literature |
|---|---|---|
| Vero E6 Cells | Cell monolayer for viral infection and plaque formation in neutralization and plaque assays. | Used in SARS-CoV-2 microneutralization and filovirus plaque assays [102] [97]. |
| Quality Control (QC) Samples | Materials with known or assigned potency to assess precision and accuracy across multiple runs. | High, medium, and low titer QC samples prepared from virus stocks [102]. |
| Reverse Genetics (RG) Viruses | Engineered viruses with mismatched HA to avoid interference when measuring NA-specific antibodies in ELLA-NI. | Used in neuraminidase inhibition assay validation to ensure specificity [104]. |
| Recombinant Proteins (e.g., rNA) | Defined source of antigen to avoid interference from antibodies against other viral components. | Recombinant Neuraminidase (rNA) used as an alternative antigen source in ELLA-NI [104]. |
| Peptide Pools | Collections of overlapping peptides spanning a viral protein, used to stimulate antigen-specific T-cells in ELISpot assays. | Used to detect T-cell responses to AAV5 capsid and transgene products [41]. |
Assay Validation and Troubleshooting Workflows
Assay Validation and Troubleshooting Workflows
Statistical Design Informs Power Analysis
Comprehensive Validation of Multiplex Viral Detection Panels
Performance Benchmarks and Validation Data
Successful validation of a multiplex viral panel requires demonstrating robust performance across key analytical metrics. The following table summarizes typical performance characteristics from recent studies and commercial panels.
Table 1: Key Performance Metrics for Multiplex Viral Detection Panels
| Validation Parameter | Representative Performance Data | Source/Context |
|---|---|---|
| Analytical Sensitivity (LoD) | SARS-CoV-2: 29.3 IU/mL; Influenza A: 179.9 cp/mL; Range: 9.4 cp/mL (hCoV-NL63) to 21,419 cp/mL (HPIV-2) [107] | Laboratory-developed 16-plex respiratory panel [107] |
| Clinical Concordance | 80% concordance with clinical diagnostics; 100% for bacterial/yeast targets; 85.9% for viral targets [108] [109] | Multiplex metagenomic sequencing vs. routine diagnostics [108] |
| Coverage & Comprehensiveness | >1M unique probes targeting 3,153 viral genomes; >99.8% coverage at 1x depth [110] | Twist Bioscience Comprehensive Viral Research Panel [110] |
| Precision (Inter-run Variability) | Standard differentials ranging between 0.13-0.74 Ct for all targets over 3 days [107] | Laboratory-developed 16-plex respiratory panel [107] |
| Cross-Reactivity | Successful multiplex capture of 4 different virus types (ssRNA, dsDNA, ssDNA, dsRNA) in co-infection assay [110] | Comprehensive Viral Research Panel performance data [110] |
Troubleshooting Common Experimental Issues
Frequently Asked Questions (FAQs)
Q1: My multiplex PCR shows no amplification or low yield for all targets. What should I check?
- Solution: This indicates a fundamental reaction failure. First, verify all PCR components were added (buffer, template, polymerase) [111]. Check the dNTP solution, as it is sensitive to freeze-thaw cycles, especially in multiplex PCR [111]. Increase template amount, adjust primer concentration, or add more polymerase/MgCl₂ [112] [111]. Using adjuvants like BSA (0.1-0.8 µg/µL final concentration) or DMSO/glycerol (5% v/v) can also improve yield [111].
Q2: I am getting non-specific amplification (smearing or multiple bands) in my multiplex reaction. How can I resolve this?
- Solution: Non-specific products often result from suboptimal primer binding. Gradually increase the annealing temperature [111]. Decrease the amount of template, primer, or enzyme [111]. If the non-specific products are long, increase the buffer concentration (1.2-2x), but keep MgCl₂ concentration constant. If they are short, decrease the buffer concentration to 0.7-0.9x [111]. Redesigning primers to avoid repetitive sequences or cross-hybridization is also recommended [113] [111].
Q3: One or a few specific targets in my multiplex are weak or invisible, while others amplify well. How can I balance amplification?
- Solution: This is a classic problem of preferential amplification. The most effective solution is to re-balance primer concentrations—increase the amount of primer for the "weak" loci while simultaneously decreasing the amount for the "strong" loci [111] [114]. Check for primer-primer interactions that might be inhibiting the weak loci [111]. For weak short products, decrease denaturing, annealing, and extension times. For weak long products, increase these times and the extension temperature [111].
Q4: My test was working but now I get false negatives. What could have changed?
- Solution: False negatives can arise from several factors. Check reagent integrity, especially dNTPs which are sensitive to freeze-thaw cycles [111]. Test for inhibitors in the template or reaction [112]. A major cause is target secondary structure inhibiting primer binding; sophisticated tools that solve coupled equilibria are needed to predict this [113]. Also, check for primer-dimers or primer-amplicon interactions that deplete reagents [113]. Finally, sequence variation in the target can lead to detection failure if the panel's mismatch tolerance is exceeded [110] [113].
Q5: How do I interpret a positive result for a common cold virus in a patient with severe symptoms?
- Solution: A positive result does not automatically indicate the detected virus is the causative agent. Asymptomatic viral detection is common—one study found ~50% of viral detection episodes were asymptomatic, particularly for rhinovirus and bocavirus [115]. Correlate the result with the patient's clinical presentation. The positive result could be incidental, and the true cause might be a different pathogen (viral or bacterial) not on the panel [115]. For immunocompromised patients, consider that viruses causing mild illness in healthy hosts can be severe and prolonged [115].
Advanced Troubleshooting Guide
Table 2: Advanced Troubleshooting for Multiplex Viral Panels
| Problem Phenomenon | Root Cause | Corrective Action |
|---|---|---|
| False Positives | Primer cross-hybridization; contaminating nucleic acids; amplicon carryover [113] [116]. | Redesign primers for greater specificity; implement strict physical separation of pre- and post-PCR areas; use uracil-DNA glycosylase (UDG) carryover prevention [116]. |
| Uneven Coverage | Highly divergent viral sequences; variable GC content; secondary structure in template DNA [110] [113]. | Use long probes with high mismatch tolerance (e.g., Twist's 10% variation tolerance) [110]; apply algorithms like CATCH to manage sequence diversity [110]. |
| Inconsistent Results Between Runs | Enzyme lot variability; thermal cycler calibration drift; reagent degradation [112]. | Standardize reagents using master mixes; perform regular instrument calibration; include internal controls in every run [112] [107]. |
| Failure to Detect Novel Strains | Overly specific primer/probe design; high sequence variation in target regions [110] [108]. | Implement panels designed for viral discovery that use exhaustive tiling across viral genomes [110]; employ metagenomic sequencing for unbiased detection [108]. |
Detailed Experimental Protocols
Protocol 1: Analytical Sensitivity and Limit of Detection (LoD) Validation
Principle: Determine the lowest concentration of viral target that can be reliably detected by the panel in ≥95% of replicates [107].
Step-by-Step Workflow:
- Sample Preparation: Obtain quantified reference standards for each viral target. Serially dilute standards in a matrix that mimics the clinical sample (e.g., viral transport medium for respiratory samples, artificial CSF for CNS infections).
- Testing Replicates: Test a minimum of 20 replicates per target at each dilution level around the expected LoD. Include negative controls.
- Data Analysis: Calculate the proportion of positive results at each concentration. Use statistical models (e.g., probit analysis) to determine the concentration at which the detection rate is ≥95%.
- Verification: Confirm the LoD by testing an additional 20 replicates at the determined concentration.
Figure 1: LoD Validation Workflow
Protocol 2: Clinical Concordance Studies
Principle: Establish agreement between the new multiplex panel and established reference methods (e.g., singleplex PCR, culture) using well-characterized clinical specimens [109] [107].
Step-by-Step Workflow:
- Sample Selection: Procume residual, anonymized clinical specimens that have previously been tested by the reference method. Include samples with positive results for each target and negative samples.
- Blinded Testing: Test all samples with the novel multiplex panel in a blinded manner.
- Data Comparison: Compare results against the reference method. Calculate positive percent agreement (PPA), negative percent agreement (NPA), and overall agreement with 95% confidence intervals.
- Discordant Analysis: Re-test discrepant results using an alternative method (e.g., sequencing) to assign the true result.
Figure 2: Clinical Concordance Study Design
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Multiplex Panel Validation
| Reagent / Material | Function in Validation | Technical Notes |
|---|---|---|
| International Reference Standards | Provides quantifiable, standardized material for determining analytical sensitivity (LoD) and linearity [107]. | Use WHO International Standards or FDA reference panels when available. Essential for cross-platform comparisons. |
| Clinical Specimens (Characterized) | Serves as the gold matrix for establishing clinical sensitivity and specificity versus reference methods [109]. | Include a range of sample types (e.g., nasopharyngeal, CSF) and storage conditions relevant to intended use. |
| Sequence-Independent, Single-Primer Amplification (SISPA) Kits | Enables unbiased amplification of nucleic acids in metagenomic studies for comprehensive viral detection [108]. | Critical for detecting novel or unexpected viruses not covered by targeted panels. |
| Multiplex PCR Master Mix | Provides optimized buffer, enzyme, and dNTP concentrations for simultaneous amplification of multiple targets [112] [107]. | Reduces optimization time; often includes additives to minimize primer-dimer formation and enhance yield. |
| Internal Control Targets | Monitors sample extraction efficiency, detects PCR inhibition, and verifies reaction validity [109] [107]. | Must be non-competitive with viral targets and added at a constant level to all clinical samples. |
| Bioinformatics Analysis Pipeline (e.g., Centrifuge, One Codex) | Performs taxonomic classification of sequencing reads, generates reports, and enables data visualization [110] [108]. | Cloud-based platforms (e.g., One Codex) can simplify analysis and generate publication-ready figures [110]. |
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our validation shows poor precision (high %CV) at low viral concentrations. What could be the cause and how can we address this?
A: High %CV at low concentrations is common and often relates to the assay's Lower Limit of Quantitation (LLOQ). First, ensure your target concentration is above the validated LLOQ. For the pan-orthopox PCR assay, the LLOQ was established at 50 genome copies/5 μL sample [29]. If precision remains poor, consider:
- Sample Processing: Increase sample input volume or concentrate nucleic acid extracts
- Reaction Optimization: Verify primer/probe efficiency and optimize master mix components
- Statistical Treatment: Apply appropriate data transformation; logit transformation is often used for proportion-type data like sensitivity and specificity to meet statistical assumptions [117]
Q2: How do we handle discrepant results between our new ddPCR assay and the reference RT-PCR method?
A: Discrepancies, particularly with weakly positive samples, are expected when implementing more sensitive methods. The AHQR–ddPCR assay demonstrated better diagnostic sensitivity compared to RT–PCR, especially in detecting weakly positive samples that RT–PCR might miss [28]. To resolve:
- Retest: Re-extract and retest the original sample
- Alternative Method: Use a third validated method or sequencing for confirmation
- Clinical Correlation: Review patient symptoms and sample collection timing
- Statistical Analysis: Calculate positive/negative percent agreement rather than simple percent concordance
Q3: Our linearity evaluation failed despite good R² values. What alternative statistical approaches should we consider?
A: R² alone is insufficient for linearity validation. Current statistical methods recommended by CLSI guideline EP6-A may inflate type I error rates due to ignored sampling error [36]. Instead, implement:
- Residuals Analysis: Plot studentized residuals to detect systematic patterns
- TOST Procedure: Use the Two One-Sided Test to prove linearity as an alternative hypothesis
- Corrected Kroll's Method: Addresses inappropriate hypothesis formulation in average deviation from linearity (ADL) assessment [36]
- Acceptance Criteria: Establish linearity as ≤25% of tolerance for analytical methods [20]
Q4: How do we establish proper acceptance criteria for method validation parameters?
A: Acceptance criteria should be risk-based and relative to the assay's intended use:
- For Precision: Repeatability should be ≤25% of tolerance (USL-LSL) for analytical methods, ≤50% for bioassays [20]
- For Accuracy/Bias: ≤10% of tolerance for both analytical methods and bioassays [20]
- For LOD/LOQ: LOD should be ≤5-10% of tolerance; LOQ should be ≤15-20% of tolerance [20]
- Clinical Parameters: For diagnostic sensitivity and specificity, use bivariate models that account for within-study and between-study variations [117]
Q5: We're observing significant titer discrepancies between our lab and a collaborator's when testing identical virus stocks. What factors should we investigate?
A: Viral titer discrepancies arise from methodological differences and handling variables [118]:
- Titration Methods: Compare fundamental approaches (e.g., p24 ELISA vs. qPCR for lentivirus)
- Primer/Probe Design: For AAV titration, primers targeting ITRs vs. internal regions yield different values
- Cell Line Selection: Ensure cell lines are efficiently infected by the virus being tested
- Sample Handling: Enveloped viruses quickly lose infectivity with improper storage; avoid repeated freeze-thaw cycles
- Reagent Sensitivity: Verify detection equipment sensitivity for identifying single virus integration events
Troubleshooting Common Validation Challenges
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Poor reproducibility between runs | Inconsistent sample processing, reagent lot variation, operator technique | Standardize protocols, use single reagent lots, implement rigorous training, calculate intermediate precision [92] |
| Reduced sensitivity in clinical samples | PCR inhibitors co-extracted from sample matrix, suboptimal extraction efficiency | Add purification steps, use inhibition-resistant polymerases, incorporate internal controls, evaluate different extraction methods [29] |
| Non-linear standard curve | Probe degradation, improper standard preparation, instrument calibration issues | Freshly prepare standards, verify instrument performance, check reagent stability [20] |
| Specificity failures | Cross-reactivity with related pathogens, non-specific amplification | Redesign primers/probes, optimize annealing temperature, test against closely related organisms [28] |
| Inaccurate quantification | Improper standard curve fitting, matrix effects, sub-optimal regression model | Use weighted regression, validate against reference materials, account for matrix effects in calculations [119] |
Performance Metrics of Viral Detection Assays
Table 1: Comparative Analytical Sensitivity of Molecular Assays
| Assay | Target | Limit of Detection | Linear Range | Reference |
|---|---|---|---|---|
| AHQR–ddPCR | IFA, IFB, RSV, SARS-CoV-2 | 0.65–0.78 copies/μL | Not specified | [28] |
| Pan-orthopox PCR | Orthopoxviruses | 2.5 GC/5μL | 50 - 5×10⁷ GC/5μL | [29] |
| Microneutralization | Yellow fever antibodies | LLOQ: 10 (1/dil) | Up to 10,240 (1/dil) | [92] |
| Pseudotyped virus neutralization | Measles antibodies | Established via cut-off value | Demonstrates wide linear range | [10] |
Table 2: Precision Performance Across Validation Studies
| Assay Type | Intra-assay Precision (%CV) | Inter-assay Precision (%CV) | Context | Reference |
|---|---|---|---|---|
| YF Microneutralization | 36% | 54% | Upper limit of quantitation | [92] |
| YF Microneutralization | 38% | 41% | Lower limit of quantitation | [92] |
| Pseudotyped MV Neutralization | Demonstrates high precision | Comparable to gold standard | Correlation with live virus neutralization | [10] |
Table 3: Diagnostic Accuracy Parameters
| Parameter | Definition | Calculation | Application Context |
|---|---|---|---|
| Sensitivity | True positive rate | TP/(TP+FN) | Ability to correctly identify positive samples [120] |
| Specificity | True negative rate | TN/(TN+FP) | Ability to correctly identify negative samples [120] |
| Diagnostic Odds Ratio (DOR) | Overall diagnostic performance | (TP×TN)/(FP×FN) | Single indicator of test performance [117] |
Experimental Protocols and Workflows
Protocol 1: Automated Quadruplex RT–ddPCR Assay
Principle: Based on the AHQR–ddPCR assay for simultaneous detection of IFA, IFB, RSV, and SARS-CoV-2 using the QX ONE platform [28]
Workflow:
- RNA Extraction
- Input: 300 μL sample
- Method: EX3600 Automatic Nucleic Acid Extraction System
- Elution: 50 μL volume
- Storage: -80°C until analysis
Reaction Setup
- Platform: QX ONE Droplet Digital PCR System
- Reaction Volume: 20 μL
- Components:
- 5 μL RNA template
- 5 μL supermix
- 2 μL reverse transcriptase (20 U/μL)
- 1 μL DTT (15 mM)
- 4.8 μL primer mix
- 0.8 μL probe mix
- 1.4 μL nuclease-free water
Thermal Cycling
- Reverse Transcription: 25°C for 3 min, 48°C for 20 min
- Enzyme Activation: 95°C for 5 min
- Amplification: 45 cycles of 95°C for 15 s and 55°C for 30 s
- Final Steps: 98°C for 10 min, 25°C for 1 min
- Ramp Rate: 2°C/s throughout
- Heated Lid: 105°C
Analysis
- Automated quantification via QX ONE software
- Absolute quantification without standard curves
- Multiplex detection via four-color fluorescence channels
Figure 1: Experimental Workflow for Clinical Sample Correlation
Protocol 2: Diagnostic Accuracy Statistical Analysis
Principle: Bivariate model for simultaneous analysis of sensitivity and specificity [117]
Implementation using R:
Key Considerations:
- Use logit transformation for proportion-type data
- Bivariate and HSROC models account for within-study and between-study variation
- Forest plots visualize individual study effects and confidence intervals
- SROC curves summarize overall test performance
Research Reagent Solutions
Table 4: Essential Reagents for Viral Assay Validation
| Reagent/Category | Specific Examples | Function/Application | Validation Parameters |
|---|---|---|---|
| Reference Materials | CNIM reference materials (IFA: NIM-RM4054, IFB: NIM-RM4056) [28] | Analytical validation with known concentrations | Accuracy, linearity, precision |
| Nucleic Acid Extraction | QIAamp DNA Mini Kit (Qiagen) [29] | Purification of viral nucleic acids from clinical matrices | Yield, purity, inhibitor removal |
| Amplification Master Mix | One-Step RT–ddPCR Advanced Kit for Probes (Bio-Rad) [28] | Reverse transcription and amplification | Efficiency, sensitivity, specificity |
| Primers/Probes | MGB probe technology [29] | Target-specific detection | Specificity, cross-reactivity testing |
| Positive Controls | Cloned HA gene insert (Variola Bangladesh) [29] | Standard curve generation | LOD, LOQ, linear range |
| Cell Lines | Vero cells [92], 293T variants [10] | Virus propagation and neutralization assays | Specificity, robustness |
Figure 2: Essential Research Reagent Categories
Advanced Statistical Approaches for Validation
Linearity Evaluation Methodology
Current Limitations:
- CLSI EP6-A method ignores sampling error of point estimates [36]
- Kroll's ADL procedure uses inappropriate hypothesis formulation [36]
- R² values alone are insufficient for linearity claims
Recommended Procedures:
- Two One-Sided Test (TOST)
- Formulate linearity as alternative hypothesis
- Adequately controls Type I error rates
- Provides sufficient statistical power
Residuals Analysis
- Plot studentized residuals from regression line
- Identify systematic patterns indicating non-linearity
- Establish linear range where residuals remain within ±1.96 limits [20]
Acceptance Criteria
- Method range should be ≤120% of upper specification limit
- Demonstrate linearity, accuracy, and repeatability across range
- Evaluate relative to product specification tolerance [20]
Diagnostic Accuracy Statistical Models
Model Selection Guide:
- Moses-Littenberg SROC: Simple linear regression approach; limited heterogeneity assessment [117]
- Bivariate Model: Binomial distribution for within-study variation; bivariate normal distribution for between-study variation [117]
- HSROC Model: Logistic regression with hierarchical distribution; equivalent to bivariate model without covariates [117]
Practical Implementation:
- Use bivariate model as default for sensitivity/specificity analysis
- Report both summary statistics and SROC curves
- Account for correlation between sensitivity and specificity
- Calculate diagnostic odds ratios for overall test performance
Documentation and Reporting for Regulatory Submissions
Frequently Asked Questions (FAQs)
What are the key regulatory submission types for new drugs and biologics in the US and EU? The primary regulatory submissions for market approval are the New Drug Application (NDA) for pharmaceutical drugs and the Biologics License Application (BLA) for biologics with the US FDA. In the European Union, the equivalent is the Marketing Authorization Application (MAA), submitted to the EMA [121] [122]. For clinical trials, an Investigational New Drug (IND) application is submitted to the FDA, while a Clinical Trial Application (CTA) is used in the EU [121] [122].
What is the required format for submitting applications to agencies like the FDA and EMA? Regulatory submissions must be compiled in the Electronic Common Technical Document (eCTD) format. This standardized structure ensures that data is presented in a consistent, reviewer-friendly manner, helping to accelerate the review process [121] [122].
Why is a validated plaque assay critical for a viral vaccine submission? A validated plaque assay is a direct measure of the potency (the concentration of infectious virus) of a live-attenuated viral vaccine, such as the rVSV-SARS-CoV-2-S vaccine [32]. Regulatory authorities require extensive validation data to ensure the assay is specific, accurate, precise, and robust, as this data directly supports the dosage and efficacy claims of the product [32].
Our ddPCR viral copy number assay is showing high variability. What are the key parameters to check? High variability in a duplex droplet digital PCR (ddPCR) assay, such as one targeting WPRE and RPP30, often stems from issues with precision and robustness. You should systematically evaluate the following parameters [35]:
- Precision: Calculate the coefficient of variation (CV) for both intra-run and inter-run replicates.
- Accuracy/Bias: Determine the percent recovery (% recovery) to assess bias.
- Robustness: Test the assay under varying conditions that could impact performance (e.g., different input DNA amounts, reagent lots, or operator skill levels).
How can I improve the sensitivity of our HBV DNA detection assay for monitoring residual viremia? Transitioning from a real-time PCR to a droplet digital PCR (ddPCR) platform can significantly enhance sensitivity. A recently developed and validated ddPCR assay for serum HBV DNA achieved a lower limit of detection of 1.6 IU/mL and a lower limit of quantification of 9.4 IU/mL, using only 200 μL of serum. This high sensitivity is crucial for detecting low-level residual viremia in patients on antiviral therapy [68].
Troubleshooting Guides
Guide 1: Troubleshooting a New Viral Titer Assay (Colorimetric MTS)
Problem: The colorimetric MTS assay for viral titer shows inconsistent results and poor linearity.
This high-throughput screening method indirectly quantifies infectious viruses by measuring the metabolic activity of infected cells. Inconsistency can arise from multiple factors in the protocol [100].
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Incorrect cell seeding density | Check cell confluency under a microscope before infection. Seeding density must be consistent and optimal for the specific cell line. | Optimize and standardize the number of cells seeded per well. For Vero E6 cells in a 6-well plaque assay, 700,000 cells per well is an example [32]. |
| Suboptimal timing of infection | The incubation period for the virus to infect cells must be determined empirically for each virus-cell pair. | Review literature for standard infection times for your virus. Conduct a time-course experiment to establish the ideal infection incubation period [100]. |
| Improper MTS reagent handling | Ensure the MTS reagent is fresh and has been stored correctly. | Follow the manufacturer's instructions precisely. For homogeneity, remove the supernatant after infection and add a fresh mix of culture medium and MTS reagent [100]. |
| Inadequate controls | Confirm that your plate includes all necessary controls for data normalization. | Always include [100]:- Background control (well with only MTS-medium, no cells).- Positive control (wells with cells treated with a high viral dose or cytotoxic compound to indicate 0% viability).- Negative control (wells with mock-infected cells to indicate 100% viability). |
Guide 2: Troubleshooting a Validated Plaque Assay
Problem: Our previously validated plaque assay for a vaccine now yields counts outside the acceptable range (10-80 PFU/well).
Deviations in a validated assay often point to changes in a critical reagent or a shift in a key procedural step [32].
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Cell passage number is too high | Check the records for the cell passage number used in the assay. | Use cells within the validated passage range (e.g., passages 5-19 for Vero E6 cells). Create a new Working Cell Bank if the current cells are beyond the validated passage number [32]. |
| Degradation of the overlay medium | Check the preparation and storage of the immobilizing overlay, such as tragacanth gum. | Prepare the overlay medium fresh according to the validated protocol. Ensure it forms a proper semigel to restrict viral spread and form distinct plaques [32]. |
| Inaccurate serial dilution | Review the technique of the personnel performing the dilutions. | Train staff on proper serial dilution techniques. Use calibrated pipettes and fresh dilution tubes for each step to ensure accuracy [32]. |
| Deviation in incubation time or temperature | Monitor incubators with independent data loggers to verify consistent 37°C and 5% CO₂ conditions. | Calibrate incubators regularly and establish procedures to minimize door openings that cause temperature and CO₂ fluctuations [32]. |
Essential Experimental Protocols
Protocol 1: Plaque Assay for Determining Viral Titer
Application: Quantifying the concentration of infectious virus (in PFU/mL) for a viral vaccine or vector, such as the rVSV-SARS-CoV-2-S vaccine [32].
Workflow:
Detailed Methodology:
- Cell Seeding: Seed Vero E6 cells (or a relevant permissive cell line) at a density of 700,000 cells per well in 6-well tissue culture plates. Incubate for 24 hours at 37°C with 5% CO₂ to form a confluent monolayer [32].
- Viral Dilution: Prepare tenfold serial dilutions of the viral sample in a suitable medium like Minimal Essential Medium (MEM). Further dilute the sample to a target concentration that will yield 15, 30, and 60 PFU per well in a final volume of 0.2 mL [32].
- Inoculation: Aspirate the growth medium from the cell monolayers. Inoculate each well in six replicates with 0.2 mL of the final virus dilutions [32].
- Adsorption: Incubate the plates for 1 hour at 37°C with 5% CO₂ to allow for viral adsorption. Gently rock the plates every 15 minutes [32].
- Overlay: Aspirate the viral inoculum. Overlay the cell monolayer with 3 mL of a tragacanth gum-based medium (e.g., MEM with 0.4% tragacanth, 2% FBS) to restrict secondary infection and plaque formation [32].
- Incubation: Incubate the plates for 72 hours (or virus-specific duration) at 37°C with 5% CO₂.
- Staining and Counting: Aspirate the overlay medium. Stain the cells with 1 mL of 0.1% crystal violet solution for at least 30 minutes to visualize plaques. Rinse off the excess stain and count the clear plaques. Calculate the titer using the formula: PFU/mL = (Mean PFU/well) × (Dilution Factor) × 5 [32].
Protocol 2: Validation of a Duplex Droplet Digital PCR (ddPCR) Assay
Application: Qualification and validation of a viral copy number (VCN) assay, such as for a virus-modified cell therapy product, using a hybrid amplicon as a reference standard [35].
Workflow:
Detailed Methodology:
- Reference Standard: Use a synthetic hybrid DNA amplicon (e.g., connecting WPRE and RPP30 with a restriction site) as a reference control instead of traditional plasmids or cell lines [35].
- Range and Linearity: Test a wide range of input DNA quantities to establish the upper and lower limits of quantification (ULOQ, LLOQ) and demonstrate a linear relationship between expected and measured concentrations [35].
- Precision: Perform multiple replicates (intra-run) and repeat the assay over different days (inter-run). Calculate the Coefficient of Variation (CV) for both, aiming for a low percentage (e.g., mean intra-run CV of 0.69%) [35] [68].
- Accuracy/Bias: Compare the measured concentration from the ddPCR assay to the known concentration of the reference standard. Calculate the percent recovery (% Recovery) [35].
- Robustness: Deliberately introduce small, controlled variations in the assay conditions (e.g., annealing temperature, reagent volumes) to ensure the assay's performance remains consistent [35].
Quantitative Data for Assay Validation
Table 1: Performance Characteristics of a Validated ddPCR Assay for HBV DNA [68]
| Validation Parameter | Result | Method of Calculation |
|---|---|---|
| Lower Limit of Detection (LLOD) | 1.6 IU/mL | Probit Regression |
| Lower Limit of Quantification (LLOQ) | 9.4 IU/mL | Probit Regression |
| Linearity | R = 0.994, R² = 0.988 | Linear Regression |
| Specificity | 96.2% | |
| Intra-run Precision | Mean CV: 0.69% | Coefficient of Variation |
| Inter-run Precision | Mean CV: 4.54% | Coefficient of Variation |
Table 2: Acceptance Criteria for a Validated Plaque Assay [32]
| Validation Parameter | Sample | Result (Mean Deviation) | Precision (Mean %CV) |
|---|---|---|---|
| Accuracy | DP_Low | 0.01 log₁₀ | 18.7% |
| Accuracy | DP_High | 0.02 log₁₀ | 12.0% |
| Accuracy | QC Sample | 0.09 log₁₀ | 6.0% |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Viral Assay Development and Validation
| Reagent / Material | Function in the Assay |
|---|---|
| Hybrid Amplicon Standard (e.g., WPRE-RPP30) [35] | A synthetic DNA fragment used as a reference material to qualify and validate duplex ddPCR assays for viral copy number, serving as an alternative to plasmid or cell line standards. |
| Tragacanth Gum Overlay [32] | A viscous solution used in plaque assays to restrict virus propagation to neighboring cells, enabling the formation of discrete, countable plaques. |
| Vero E6 Cells [32] | A specific cell line derived from African green monkey kidney cells, widely used as a permissive host for propagating viruses and for assays like plaque formation. |
| Tetrazolium Reagent (MTS) [100] | A compound used in colorimetric assays to measure cellular metabolic activity. It is reduced to a colored formazan product in viable cells, allowing indirect quantification of virus-induced cell death. |
| Droplet Digital PCR (ddPCR) System [35] [68] | A platform that partitions a PCR reaction into thousands of nanodroplets, allowing for absolute quantification of nucleic acid targets without a standard curve, ideal for detecting low-level viremia. |
Conclusion
The validation of precision and linearity forms the critical foundation for reliable viral assays in both research and clinical applications. By implementing systematic validation frameworks that address foundational principles, methodological applications, troubleshooting strategies, and comparative analysis, researchers can ensure their assays generate accurate, reproducible data meeting regulatory standards. Future directions include increased adoption of digital PCR for absolute quantification, development of standardized multiplex platforms for comprehensive pathogen detection, and enhanced computational approaches for managing complex validation data. Robust validation directly impacts vaccine development, therapeutic monitoring, and public health responses by ensuring the reliability of viral detection and quantification across diverse applications and settings.
References
- 1. qPCR and qRT-PCR analysis: Regulatory points to consider when conducting biodistribution and vector shedding studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7786041/]
- 2. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 3. Methods to determine limit of detection and limit of quantification in quantitative real-time PCR (qPCR) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 4. 为马科动物疱疹病毒2诊断的呼吸道液体 定 方法的开发和 量 PCR 检 测 验 证 [https://www.jove.com/cn/t/53672/development-validation-quantitative-pcr-method-for-equid-herpesvirus]
- 5. CN104988242A - Pcr ... - Google Patents [https://patents.google.com/patent/CN104988242A/zh]
- 6. 实时 定 BCR-ABL (P210... 量 PCR 检 测 [https://pmc.ncbi.nlm.nih.gov/articles/PMC7342103/]
- 7. for Clinical Use of a Novel HIV-2 Plasma RNA Validation ... Viral Load [https://pmc.ncbi.nlm.nih.gov/articles/PMC3444162/]
- 8. Plaque reduction neutralization test for smallpox vaccines: Laboratory... [https://pubmed.ncbi.nlm.nih.gov/39672372/]
- 9. A robust HIV-1 viral detection load optimized for Indian sub type... assay [https://biolres.biomedcentral.com/articles/10.1186/0717-6287-47-22]
- 10. Evaluation of Measles Vaccine Immunogenicity and Durability Using... [https://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2025.224]
- 11. Standardizing experimental protocols - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0958166908000773]
- 12. Frontiers | CoreTIA: a modular, statistically robust transduction... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1623848/full]
- 13. Implementation of pooled testing to increase access to routine viral load monitoring for people living with HIV on antiretroviral therapy | Scientific Reports [https://www.nature.com/articles/s41598-025-92709-y]
- 14. Troubleshooting Immunoassays - Ansh Labs [https://www.anshlabs.com/resources/immunoassay-troubleshooting/]
- 15. Troubleshooting | BioAssay Systems [https://bioassaysys.com/troubleshooting/]
- 16. and Sensitivity of metatranscriptomics as an arbovirus... specificity [https://www.nature.com/articles/s41598-019-55741-3?error=cookies_not_supported&code=f36f207a-7f2d-4781-ac22-ed18724aaef0]
- 17. Development of high-throughput liquid chips for respiratory virus ... [https://pubmed.ncbi.nlm.nih.gov/24697109/]
- 18. Precision and linearity targets for validation of an IFNgamma ELISPOT, cytokine flow cytometry, and tetramer assay using CMV peptides - PubMed [https://pubmed.ncbi.nlm.nih.gov/18366814/]
- 19. Precision and linearity targets for validation of an IFNγ ELISPOT, cytokine flow cytometry, and tetramer assay using CMV peptides - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2275721/]
- 20. Establishing Acceptance Criteria for Analytical Methods | BioPharm International [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 21. Comparison between Singleplex... | PLOS One Analytical Sensitivity [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0143164]
- 22. A rapid, high-throughput, viral infectivity assay using automated brightfield microscopy with machine learning - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2472630323000456]
- 23. Ensuring Linearity in Method Validation - A Step-by-Step Guide [https://altabrisagroup.com/linearity-in-method-validation/]
- 24. Statistical Assessments of Bioassay Validation Acceptance Criteria [https://www.bioprocessintl.com/assays/statistical-assessments-of-bioassay-validation-acceptance-criteria]
- 25. USP 1033: Top 3 Highlights from New Draft Guidances - Quantics... [https://www.quantics.co.uk/blog/usp-1033-top-3-highlights-from-new-draft-guidances/]
- 26. Validation of Laboratory-Developed Molecular Assays for Infectious Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2901657/]
- 27. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 28. Frontiers | Development and validation of an automated and... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1529336/full]
- 29. of a pan-orthopox real-time PCR Validation for the detection... assay [https://virologyj.biomedcentral.com/articles/10.1186/s12985-017-0880-8]
- 30. The 2025 Biomarker Guidance: Understanding the Evolution from... FDA [https://www.linkedin.com/pulse/2025-fda-biomarker-guidance-understanding-lxoke]
- 31. Latest FDA & EU Guidelines Every Pharma Validation Professional... [https://pharmaconnections.in/latest-fda-eu-guidelines-every-pharma-validation-professional-should-know-in-2025/]
- 32. Development and Validation of a Plaque Assay to Determine the Titer of a Recombinant Live-Attenuated Viral Vaccine for SARS-CoV-2 [https://www.mdpi.com/2076-393X/12/4/374]
- 33. New China CDE guidance on platform validation of viral ... :: Parexel [https://www.parexel.com/insights/blog/new-china-cde-guidance-on-platform-validation-of-viral-clearance-aligns-with-fda-and-ema]
- 34. Guidelines and Regulations Resource Center - ACRP [https://acrpnet.org/insights/guidelines-and-regulations]
- 35. A method to validate viral copy-number assay involving a hybrid amplicon and duplex droplet digital PCR - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2329050125000786]
- 36. On statistical evaluation of the linearity in assay validation - PubMed [https://pubmed.ncbi.nlm.nih.gov/18607801/]
- 37. vs FDA Expectations on Process EMA | Pharmaguideline Validation [https://www.pharmaguideline.com/2025/07/ema-vs-fda-expectations-on-process-validation.html]
- 38. ELISA Kit Validation and Quality Testing | Thermo Fisher Scientific - IN [https://www.thermofisher.com/in/en/home/life-science/antibodies/immunoassays/elisa-kits/elisa-kit-validation-quality-testing.html]
- 39. ELISA Assay : Best Practices, Methods, and Key Insights Validation [https://www.nebiolab.com/elisa-assay-validation-guide/]
- 40. and Precision targets for linearity of an IFNγ ELISPOT... validation [https://bmcimmunol.biomedcentral.com/articles/10.1186/1471-2172-9-9]
- 41. of an IFN-gamma ELISpot Validation to measure cellular... assay [https://www.nature.com/articles/s41434-020-00214-w?error=cookies_not_supported]
- 42. A Novel Surface Plasmon Resonance Imaging (SPRi) Biosensor for the Determination of Bovine Interleukin-10: Development, Validation, and Application in Biological Fluids [https://www.mdpi.com/1422-0067/26/21/10395]
- 43. Quantitative PCR validation for research scientists: Part 1 of 2 - VIROLOGY RESEARCH SERVICES [https://virologyresearchservices.com/2023/01/13/quantitative-pcr-validation-part-1-of-2/]
- 44. Expanding the linear dynamic range in quantitative high performance liquid chromatography/tandem mass spectrometry by the use of multiple product ions - PubMed [https://pubmed.ncbi.nlm.nih.gov/11400204/]
- 45. Expanding the linear dynamic range for multiple reaction monitoring in quantitative liquid chromatography-tandem mass spectrometry utilizing natural isotopologue transitions - PubMed [https://pubmed.ncbi.nlm.nih.gov/22099684/]
- 46. ELISA Troubleshooting Guide | Sino Biological [https://www.sinobiological.com/category/elisa-troubleshooting]
- 47. Pitfalls in PCR troubleshooting: Expect the unexpected? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4822207/]
- 48. dPCR assay development | Digital PCR troubleshooting - Qiagen [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-guide/setup-and-troubleshooting]
- 49. Analytical validation of quantitative SARS-CoV-2 subgenomic and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10309597/]
- 50. Ultrasensitive detection and quantification of viral nucleic acids with... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8563494/]
- 51. Expanding the Dynamic Range of Fluorescence Assays through Single-Molecule Counting and Intensity Calibration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6462413/]
- 52. Rapid and sensitive detection of SARS-CoV-2 infection using... [https://elifesciences.org/articles/70843]
- 53. The development and validation of a microneutralization for... assay [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960057/]
- 54. An In Vitro Microneutralization Assay for SARS‐CoV‐2 Serology and Drug Screening - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7361222/]
- 55. An In Vitro Microneutralization Assay for Influenza Virus Serology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9298957/]
- 56. Assay of the month: The microneutralization assay - VIROLOGY RESEARCH SERVICES [https://virologyresearchservices.com/2019/04/30/assay-of-the-month-the-microneutralization-assay/]
- 57. The mathematics of qRT-PCR in virology - VIROLOGY RESEARCH SERVICES [https://virologyresearchservices.com/2025/01/13/the-mathematics-of-qrt-pcr-in-virology/]
- 58. Micro-Focus Reduction Neutralization Tests (mFRNT) for... | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-0716-4458-4_17]
- 59. Development, Validation, and Utilization of a Luminex- Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10100979/]
- 60. Multiplexed bead-based assay for the simultaneous quantification of human serum IgG antibodies to tetanus, diphtheria, pertussis toxin, filamentous hemagglutinin, and pertactin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10278353/]
- 61. Frontiers | Quantitative bead–based multiplex assay for simultaneous determination of IgG concentrations of pertussis toxin, filamentous hemagglutinin, pertactin, diphtheria, tetanus, Haemophilus influenzae b, and hepatitis B in human serum samples [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1587567/full]
- 62. Frontiers | Multiplexed bead-based assay for the simultaneous quantification of human serum IgG antibodies to tetanus, diphtheria, pertussis toxin, filamentous hemagglutinin, and pertactin [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1190404/full]
- 63. Development of a Bead-Based Multiplex Assay for the Analysis of the Serological Response against the Six Pathogens HAV, HBV, HCV, CMV, T. gondii, and H. pylori | MDPI [https://www.mdpi.com/2571-5135/6/4/14]
- 64. High-throughput multiplexed serology ... | Nature Biomedical Engineering [https://www.nature.com/articles/s41551-025-01349-0?error=cookies_not_supported]
- 65. Droplet Digital : PCR and Applications in Molecular... Advantages [https://www.labx.com/resources/droplet-digital-pcr-advantages-and-applications-in-molecular-diagnostics/5581]
- 66. vs. Real-Time Digital : Understanding the Key... | Lab Manager PCR PCR [https://www.labmanager.com/digital-pcr-vs-real-time-pcr-understanding-the-key-differences-33665]
- 67. dPCR for Beginners - QIAGEN [https://www.qiagen.com/us/applications/digital-pcr/beginners]
- 68. Development and Validation of a High-Sensitivity Droplet Digital PCR Assay for Serum Hepatitis B Virus DNA Detection - PubMed [https://pubmed.ncbi.nlm.nih.gov/40087905/]
- 69. Duplex digital PCR assay on microfluidic chamber arrays for total HIV DNA reservoir quantification in persons with HIV | Scientific Reports [https://www.nature.com/articles/s41598-025-17392-5]
- 70. A method to validate viral copy-number assay involving a hybrid amplicon and duplex droplet digital PCR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229726/]
- 71. Support— Digital | Thermo Fisher Scientific - CN PCR Troubleshooting [https://www.thermofisher.cn/cn/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/digital-pcr-support/digital-pcr-support-troubleshooting.html]
- 72. neb.com/en/tools-and-resources/ troubleshooting - guides / pcr ... [https://www.neb.com/en/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide]
- 73. In-House Validation of Four Duplex Droplet Digital PCR Assays to Quantify GM Soybean Events [https://www.mdpi.com/2304-8158/13/24/4011]
- 74. Multiplexed Digital PCR Reference Gene Measurement for Genomic and Cell-Free DNA Analysis | MDPI [https://www.mdpi.com/2073-4409/14/19/1544]
- 75. Optimization and Validation of a Plaque Reduction Neutralization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3752766/]
- 76. Antibody Validation Testing and Reporting Harmonization Neutralizing [https://link.springer.com/article/10.1208/s12248-023-00830-5]
- 77. Comparative analysis of neutralization performed using live... assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502732/]
- 78. - Cell highlights differences in antibody based ... assay neutralizing [https://www.news-medical.net/news/20220628/Cell-based-assay-highlights-differences-in-antibody-neutralizing-capacity-for-SARS-CoV-2-variants.aspx]
- 79. The Assay Guidance Manual: A Guide for In Vitro and In Vivo Assays in Early Drug Discovery [https://www.promega.com/resources/pubhub/tpub_191-the-assay-guidance-manual/]
- 80. Establishing a reference range for thrombin generation using... [https://pubmed.ncbi.nlm.nih.gov/25956288/]
- 81. Calculating Inter- and Intra-Assay Coefficients of Variability – Salimetrics [https://salimetrics.com/calculating-inter-and-intra-assay-coefficients-of-variability/]
- 82. %CV in ELISA: How to Reduce Them and Why They’re Important - Enzo [https://www.enzolifesciences.com/science-center/technotes/2018/january/cv-in-elisa-how-to-reduce-them-and-why-they-re-important/]
- 83. Factors affecting the accuracy and... | MyBioSource Learning Center [https://www.mybiosource.com/learn/factors-affecting-the-accuracy-and-reliability-of-elisa-results/]
- 84. Stochastic processes defining sensitivity and variability of internally calibrated quantitative NASBA-based viral load assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC140086/]
- 85. Validation of a primer optimisation matrix to improve the performance... [https://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-2-112]
- 86. How to Optimize - RT using the qPCR Kit PCR Optimization [https://ita.promega.com/en/resources/pubhub/2017/rt-qpcr-using-the-pcr-optimization-kit/]
- 87. of the Optimization temperature profile is... | Research Square qPCR [https://www.researchsquare.com/article/rs-891318/v1]
- 88. 5 Questions to Ask When Your RT-qPCR Isn’t Working - Promega Connections [https://www.promegaconnections.com/5-questions-to-ask-when-your-rt-qpcr-isnt-working/]
- 89. Two-Step Versus One-Step RNA-to-CT™ 2-Step and One-Step RNA-to-CT™ 1-Step: Validity, Sensitivity, and Efficiency - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2700466/]
- 90. , Hemolysis , and Icterus ... | Today's Clinical Lab Lipemia Interference [https://www.clinicallab.com/hemolysis-icterus-and-lipemia-interference-new-approaches-to-old-foes-26664]
- 91. : causes, Lipemia mechanisms, detection and... interference [https://pmc.ncbi.nlm.nih.gov/articles/PMC3936974/]
- 92. The development and validation of a microneutralization assay for the... [https://pubmed.ncbi.nlm.nih.gov/40035587/]
- 93. of an IFN-gamma ELISpot Validation to measure cellular... assay [https://www.nature.com/articles/s41434-020-00214-w?error=cookies_not_supported&code=95aee66d-6451-4ad9-a23c-8e0a39dcab3f]
- 94. ViraLite: An Ultracompact HIV Viral Load Self-Testing System with... [https://pubmed.ncbi.nlm.nih.gov/40236396/]
- 95. Development and clinical validation of a novel multiplex PCR test for detection of respiratory pathogens via fluorescence melting curve analysis | Scientific Reports [https://www.nature.com/articles/s41598-025-16434-2]
- 96. Guide to Quality Sequencing - CD Genomics Control for Viral [https://www.cd-genomics.com/resource/quality-control-for-viral-sequencing.html]
- 97. Optimization and evaluation of a live virus SARS-CoV-2 neutralization assay | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0272298]
- 98. 2024-2025 WHO-Recommended Influenza Strains: Now Available at VRS - VIROLOGY RESEARCH SERVICES [https://virologyresearchservices.com/2025/03/06/2024-2025-who-recommended-influenza-strains-now-available-at-vrs/]
- 99. Multiplex Immunoassays vs Techniques Gold Standard Assay [https://www.news-medical.net/whitepaper/20170926/Multiplex-Immunoassays-vs-Gold-Standard-Assay-Techniques.aspx]
- 100. Development of high-throughput screening viral titration assay: Proof of concept through two surrogate viruses of human pathogens - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417078/]
- 101. of several immunoassays used in drugs of abuse... Comparison [https://pubmed.ncbi.nlm.nih.gov/31730939/]
- 102. of the Filovirus Plaque Validation for Use in Preclinical Studies... Assay [https://pmc.ncbi.nlm.nih.gov/articles/PMC4848606/]
- 103. Validation of the Filovirus Plaque Assay for Use in Preclinical Studies [https://pubmed.ncbi.nlm.nih.gov/27110807/]
- 104. Frontiers | Validation of a Harmonized Enzyme-Linked-Lectin- Assay ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.909297/full]
- 105. Statistical relevance—relevant statistics, part I - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4682647/]
- 106. and utilization of an internally controlled multiplex Real-time... Validation [https://virologyj.biomedcentral.com/articles/10.1186/s12985-015-0316-2]
- 107. Analytical and clinical validation of a novel, laboratory-developed... [https://pubmed.ncbi.nlm.nih.gov/38820916/]
- 108. Multiplex metagenomic sequencing for rapid viral pathogen identification and surveillance in clinical specimens | BMC Infectious Diseases | Full Text [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11952-w]
- 109. Performance Evaluation of Multiplex Molecular Syndromic Panel vs. Singleplex PCR for Diagnosis of Acute Central Nervous System Infections [https://www.mdpi.com/2076-2607/13/4/892]
- 110. Comprehensive Viral Research Panel - Twist Bioscience [https://www.twistbioscience.com/products/ngs/fixed-panels/comprehensive-viral-research-panel]
- 111. PCR Troubleshooting [https://diyhpl.us/~bryan/irc/protocol-online/protocol-cache/Trblesht.html]
- 112. Sample Preparation Troubleshooting in Issues Multiplex PCR [https://www.linkedin.com/advice/0/how-do-you-troubleshoot-sample-preparation-issues]
- 113. The Four Most Common Problems in Multiplex ... | DNA Software pcr [https://www.dnasoftware.com/common-problems-in-multiplex-panel-design/]
- 114. - Molecular Biology Multiplex PCR troubleshooting [https://www.protocol-online.org/biology-forums/posts/6655.html]
- 115. Making Sense of Respiratory Viral Panel Results | ASM.org [https://asm.org/articles/2020/march/making-sense-of-respiratory-viral-panel-results]
- 116. Respiratory Viral Nucleic Acid Assay - Class II... | FDA Panel Multiplex [https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/respiratory-viral-panel-multiplex-nucleic-acid-assay-class-ii-special-controls-guidance-industry-and]
- 117. test accuracy: application and practice using R software Diagnostic [https://www.e-epih.org/journal/view.php?number=1022]
- 118. Troubleshooting Viral Titrations | VectorBuilder [https://en.vectorbuilder.com/resources/faq/titer-discrepancies.html]
- 119. Key aspects of analytical method validation and linearity evaluation - PubMed [https://pubmed.ncbi.nlm.nih.gov/18929516/]
- 120. Testing Accuracy: Diagnostic , Sensitivity , Predictive... Specificity [https://pubmed.ncbi.nlm.nih.gov/32491423/]
- 121. The Ultimate Guide to Regulatory Submissions [https://pharmuni.com/2025/06/02/the-ultimate-guide-to-regulatory-submissions/]
- 122. A Guide to Regulatory in the US (FDA) & EU (EMA) Submissions [https://kivo.io/news/a-regulatory-submissions-guide-for-the-us-fda-eu-ema]