LAMP vs nPCR vs RT-PCR: A Comprehensive Sensitivity Comparison for Molecular Diagnostics
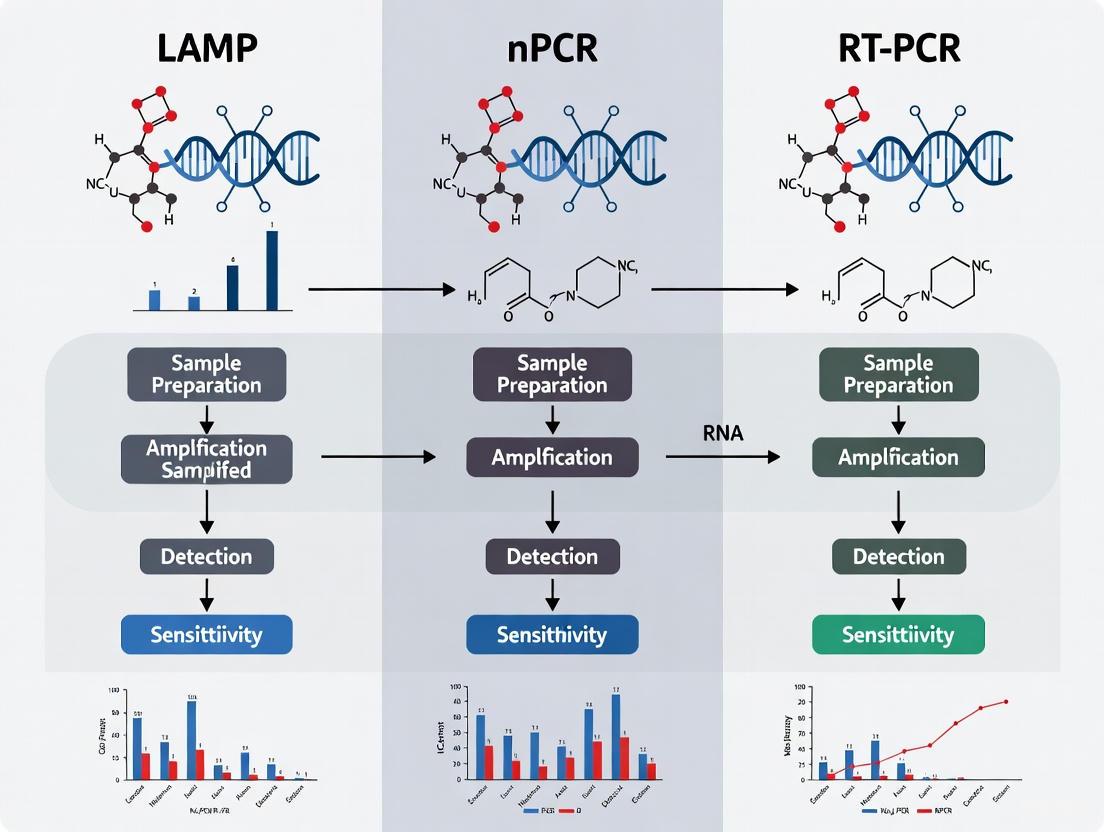
This article provides a systematic comparison of the sensitivity, specificity, and practical application of Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and real-time PCR (RT-PCR) for researchers and drug development...
LAMP vs nPCR vs RT-PCR: A Comprehensive Sensitivity Comparison for Molecular Diagnostics
Abstract
This article provides a systematic comparison of the sensitivity, specificity, and practical application of Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and real-time PCR (RT-PCR) for researchers and drug development professionals. Drawing from recent clinical and analytical studies, we explore the foundational principles of each technique, their methodological workflows in detecting pathogens like SARS-CoV-2, Entamoeba histolytica, and carbapenem-resistant bacteria, and direct head-to-head sensitivity comparisons. The content also covers crucial troubleshooting and optimization strategies to enhance assay performance, and validates findings with clinical data. This resource aims to guide the selection of the most appropriate molecular diagnostic tool for specific research and clinical settings, balancing sensitivity, speed, cost, and operational complexity.
Understanding the Core Technologies: Principles of LAMP, nPCR, and RT-PCR
Loop-mediated isothermal amplification (LAMP) represents a significant advancement in nucleic acid amplification technology, offering a rapid, sensitive, and specific alternative to traditional PCR-based methods. Since its introduction in 2000, LAMP has been incorporated into diagnostic assay development for numerous medically important communicable diseases including Salmonella Typhimurium, pathogenic Leptospira, and toxigenic Vibrio cholerae [1]. This innovative technique has revolutionized molecular biology research and clinical diagnostics by enabling DNA amplification under isothermal conditions, thereby eliminating the need for sophisticated thermal cyclers [2] [1]. The technique employs a DNA polymerase with high strand-displacement activity and utilizes 4-6 primers recognizing 6-8 distinct regions of the target DNA, resulting in highly specific amplification [2] [3]. The exceptional sensitivity, specificity, speed, accuracy, and affordability of LAMP have made it particularly valuable for point-of-care diagnostics and field applications where resources may be limited [4] [3].
Compared to conventional PCR, nested PCR (nPCR), and real-time PCR (qPCR), LAMP demonstrates several distinct advantages in amplification efficiency. A comparative analysis study revealed that LAMP outperformed these PCR methods in terms of limit of detection (LoD) and amplification time [5] [1]. While LAMP detected a single Entamoeba histolytica trophozoite, both qPCR and nPCR recorded LoD of 100 trophozoites, and conventional PCR demonstrated an LoD of 1000 trophozoites [1]. This enhanced sensitivity, coupled with its rapid reaction time and operational simplicity, positions LAMP as a relevant alternative DNA-based amplification platform for sensitive and specific detection of pathogens [5].
Fundamental Principles of LAMP
Core Mechanism and Reaction Dynamics
The fundamental mechanism of LAMP centers on its isothermal amplification process, which occurs at a constant temperature range of 60-65°C, typically around 65°C [3]. This contrasts sharply with conventional PCR that requires thermal cycling between different temperatures. The reaction is initiated by a DNA polymerase with high strand-displacement activity such as Bst-XT WarmStart DNA Polymerase [3]. This enzyme begins synthesis and enables the specially designed primers to form "loop" structures that facilitate subsequent rounds of amplification through extension on the loops and additional annealing of primers.
A key characteristic of the LAMP reaction is the production of very long DNA products (>20 kb) formed from numerous repeats of the short (80–250 bp) target sequence, connected with single-stranded loop regions in long concatemers [2] [3]. These complex structures contain multiple opportunities for initiating synthesis, and the strand displacing Bst DNA Polymerase uses these priming points, resulting in rapid exponential amplification [2]. The amplification efficacy of LAMP beyond exponential has significantly shortened amplification duration compared to PCR-based methods, with reactions often completing within 15-60 minutes depending on optimization [4] [1].
Primer Design Strategy
The exceptional specificity of LAMP stems from its sophisticated primer design strategy that requires recognition of 6-8 distinct regions within the target DNA. A complete LAMP primer set consists of:
- F3 and B3 (Outer Primers): These are the forward and backward outer primers that help initiate the strand displacement process. Their Tm is typically about 59-61°C [2].
- FIP and BIP (Inner Primers): These forward and backward inner primers contain two distinct sequences complementary to the target DNA, which are responsible for forming the loop structures. Their Tm is typically about 64-66°C [2].
- LF and LB (Loop Primers): These optional but recommended loop primers accelerate the reaction by binding to the loop regions formed during amplification, providing additional initiation sites for DNA synthesis [3].
The distance between primer regions follows specific constraints: the distance between 5' end of F2 and B2 is typically 120-160 bp, while the distance between F2 and F3 as well as B2 and B3 is 0-20bp. The distance for loop-forming regions (5' of F2 to 3' of F1, 5' of B2 to 3' of B1) is 0-40bp [2]. This precise arrangement enables the formation of the characteristic "dumbbell" structure that contains multiple opportunities for initiating synthesis, resulting in rapid exponential amplification [2].
Table 1: LAMP Primer Components and Their Functions
| Primer Name | Type | Recognition Regions | Function | Typical Tm (°C) |
|---|---|---|---|---|
| F3 and B3 | Outer Primers | 2 regions | Initiate strand displacement | 59-61°C |
| FIP and BIP | Inner Primers | 4 regions | Form loop structures for auto-cycling | 64-66°C |
| LF and LB | Loop Primers | 2 regions | Accelerate reaction by binding loop regions | ~65°C |
Visualizing the LAMP Mechanism
The following diagram illustrates the fundamental mechanism of LAMP, showing the primer binding sites and the formation of loop structures that enable exponential amplification:
Diagram 1: LAMP primer binding regions and amplification mechanism. Primers recognize 6-8 distinct regions on the target DNA, forming loop structures that enable exponential amplification under isothermal conditions, producing long concatemeric DNA products.
Comparative Performance Analysis
Sensitivity and Detection Limits
Comprehensive studies have demonstrated LAMP's superior sensitivity compared to various PCR methods. In a direct comparison using Entamoeba histolytica DNA derived from faecal samples, LAMP showed significantly better limit of detection (LoD) than conventional PCR, nested PCR, and real-time PCR [5] [1]. The research employed three different post-LAMP analysis methods including agarose gel electrophoresis, nucleic acid lateral flow immunoassay, and calcein-manganese dye techniques, all of which recorded identical LoD of a single E. histolytica trophozoite [1]. This exceptional sensitivity substantially outperformed all PCR methods tested in the same study.
Table 2: Comparison of Detection Limits Between LAMP and PCR Methods
| Method | Limit of Detection | Amplification Time | Equipment Needs | Reference |
|---|---|---|---|---|
| LAMP | 1 trophozoite | 15-60 minutes | Heating block/water bath | [1] |
| Real-time PCR (qPCR) | 100 trophozoites | 60-120 minutes | Thermal cycler with detection system | [1] |
| Nested PCR (nPCR) | 100 trophozoites | 3-4 hours | Thermal cycler | [1] |
| Conventional PCR | 1000 trophozoites | 60-120 minutes | Thermal cycler | [1] |
The high sensitivity of LAMP has been consistently demonstrated across various applications. In plant pathology, a LAMP assay developed for detecting sunflower downy mildew (Plasmopara halstedii) achieved a detection limit of 0.5 pg/μl of pathogen DNA, surpassing the reported lowest detection limit of 3 pg for PCR-based methods [4]. Similarly, in SARS-CoV-2 detection, an optimized RT-LAMP assay demonstrated a limit of detectable template reaching 10 copies of the N gene per 25 μL reaction at isothermal 58℃ within 40 minutes [6]. Another study reported a limit of detection of 6.7 copies/reaction for SARS-CoV-2 RT-LAMP [7].
Speed and Time Efficiency
The amplification efficiency of LAMP significantly reduces reaction times compared to PCR-based methods. While conventional PCR and qPCR typically require 60-120 minutes for amplification alone (excluding analysis time), LAMP reactions are often completed within 15-60 minutes under optimal conditions [4] [1]. This time efficiency is particularly valuable in clinical and field settings where rapid results are critical for decision-making.
In SARS-CoV-2 detection, studies have demonstrated that RT-LAMP can generate results within approximately 1 hour [8]. The rapid turnaround time is attributed to the exponential amplification kinetics of LAMP, which does not require time-consuming thermal cycling. Furthermore, the elimination of post-amplification analysis steps through colorimetric or turbidity-based detection methods can provide results even faster, in some cases within 30-40 minutes [6] [7].
Specificity and Reliability
LAMP demonstrates exceptional specificity due to its requirement for multiple primers recognizing 6-8 distinct regions of the target DNA. This multi-recognition approach significantly reduces the likelihood of non-specific amplification. In one study evaluating LAMP for Entamoeba histolytica detection, the primer set recorded 100% specificity when tested against 3 medically important Entamoeba species and 75 other pathogenic microorganisms [1]. This high specificity is maintained across various applications, from clinical diagnostics to plant pathogen detection [4] [8].
The reliability of LAMP has been validated in numerous clinical studies. For COVID-19 diagnosis, RT-LAMP showed 95.45% accuracy in detecting the p.L858R variant in non-small cell lung cancer patients compared to real-time PCR and next-generation sequencing (NGS) [8]. For SARS-CoV-2 detection, one study reported that up to the 9th day after symptom onset, RT-LAMP had a positivity of 92.8%, with sensitivity and specificity compared with RT-qPCR of 100% [7]. However, the same study noted that after the 10th day after onset, the positivity of RT-LAMP decreased to less than 25%, indicating that diagnostic accuracy may vary depending on the disease stage and viral load [7].
Experimental Protocols and Methodologies
Standard LAMP Reaction Setup
A typical LAMP reaction includes several key components that must be carefully optimized for maximum efficiency. Based on multiple studies, the standard reaction components include:
- Bst DNA Polymerase: 6-12 U (typically 8 U) of strand-displacing DNA polymerase such as Bst 2.0 Warm Start DNA Polymerase [4]
- Primers: F3/B3 (0.1-0.4 μM), FIP/BIP (0.8-3.2 μM), LF/LB (0.2-0.8 μM) [4]
- dNTPs: 1.0-1.6 mM [4]
- Mg²⁺: 6-12 mM (typically 8 mM) [4]
- Reaction Buffer: 20 mM Tris-HCl, 10 mM (NH₄)₂SO₄, 2 mM MgSO₄, 0.1% Tween 20, pH 8.8 at 25°C [4]
- Betaine: Often added to improve reaction efficiency and specificity
- Template DNA: Typically 50 ng or less, depending on application [4]
The reaction is usually performed in a final volume of 25 μL, incubated at a constant temperature of 60-65°C for 15-60 minutes, followed by enzyme inactivation at 80°C for 5 minutes [4].
Optimization Strategies
Successful LAMP implementation requires careful optimization of several reaction parameters. Key optimization areas include:
- Temperature Optimization: Testing temperatures between 60-67°C to determine the optimal amplification temperature for specific primer-template combinations [4]
- Time Course Evaluation: Assessing amplification at different time points (15, 35, 45, 60 minutes) to determine the minimum required amplification time [4]
- Magnesium Concentration: Titrating Mg²⁺ concentrations between 6-12 mM to optimize amplification efficiency [4]
- Primer Ratio Optimization: Balancing inner and outer primer concentrations to maximize amplification yield while minimizing non-specific products [4]
The systematic optimization process typically involves varying one parameter at a time while keeping others constant, then validating the optimized conditions using target and non-target samples to confirm specificity [4].
Detection Methods
LAMP products can be detected through multiple methods, providing flexibility for different laboratory settings and applications:
- Agarose Gel Electrophoresis: Traditional method visualizing the characteristic ladder-like pattern of LAMP amplicons [1]
- Colorimetric Detection: Using dyes such as Neutral Red, Hydroxynaphthol Blue, SYBR Safe, or Thiazole Green that change color in response to amplification [4] [3]
- Turbidity Measurement: Detecting magnesium pyrophosphate precipitate formation as a white precipitate or measuring turbidity changes [3]
- Lateral Flow Dipsticks: Using immunochromatographic strips for rapid visual detection of labeled amplicons [1]
- Real-time Monitoring: Employing intercalating dyes in real-time thermal cyclers to monitor amplification kinetics [4]
The choice of detection method depends on the required sensitivity, available equipment, and intended application, with colorimetric and lateral flow methods being particularly suitable for point-of-care testing.
Research Reagent Solutions
Table 3: Essential Reagents for LAMP Assay Development
| Reagent Category | Specific Examples | Function | Optimization Tips |
|---|---|---|---|
| DNA Polymerase | Bst 2.0 WarmStart DNA Polymerase, Bst-XT WarmStart | Strand-displacing activity for isothermal amplification | Test concentrations 6-12 U/reaction; warm-start versions prevent non-specific initiation |
| Primer Sets | F3/B3, FIP/BIP, LF/LB | Recognize 6-8 distinct target regions for specific amplification | F3/B3: 0.1-0.4 μM; FIP/BIP: 0.8-3.2 μM; LF/LB: 0.2-0.8 μM |
| Detection Dyes | Calcein-manganese, Hydroxynaphthol Blue, SYBR Safe, Neutral Red | Visual detection of amplification through color change | Calcein-manganese: pre- and post-amplestion color change; Hydroxynaphthol Blue: blue to violet |
| Buffer Components | Betaine, MgSO₄, dNTPs, Tween-20 | Enhance reaction efficiency and specificity | Betaine reduces secondary structure; optimize Mg²⁺ at 6-12 mM; dNTPs at 1.0-1.6 mM |
| Sample Preparation Kits | Plant/Fungi DNA Isolation Kits, Viral RNA Extraction Kits | Nucleic acid purification for various sample types | LAMP is robust and tolerant of inhibitors, allowing for crude sample prep |
Applications and Case Studies
Clinical Diagnostics
LAMP has demonstrated significant utility in clinical diagnostics across various diseases. In COVID-19 detection, multiple studies have validated RT-LAMP as a reliable alternative to RT-qPCR, particularly during the acute phase of infection. One study found that until the 9th day after symptom onset, RT-LAMP had the same diagnostic accuracy as RT-qPCR, suggesting its utility as a diagnostic tool in the acute symptomatic phase of COVID-19 [7]. Another study reported 95.45% accuracy of a LAMP test in detecting the p.L858R somatic variant in non-small cell lung cancer patients compared to real-time PCR and NGS [8].
For parasitic infections, LAMP has shown remarkable sensitivity in detecting Entamoeba histolytica from faecal samples, with studies demonstrating detection of a single trophozoite, outperforming all PCR-based methods [1]. The 100% specificity recorded when tested against multiple related species and other microorganisms further supports its clinical utility [1].
Plant Pathology and Agricultural Applications
In agricultural diagnostics, LAMP has proven valuable for detecting plant pathogens with high sensitivity and specificity. The development of a LAMP assay for sunflower downy mildew (Plasmopara halstedii) demonstrated a detection limit of 0.5 pg/μl of pathogen DNA, surpassing conventional PCR methods [4]. The assay provided a cost-effective, field-suitable, and easily analyzable solution with high analytical sensitivity and specificity, making it ideal for use in resource-limited settings [4].
The technique has been successfully applied to detect various other plant pathogens, including barley yellow dwarf virus in cereals, Candidatus phytoplasma vitis, tomato chlorosis virus, and potato ring rot pathogen Clavibacter michiganensis subsp. sepedonicus [4]. The robustness of LAMP and its tolerance to inhibitors reduces the need for extensive DNA purification, further enhancing its suitability for field applications.
Field Deployment and Point-of-Care Testing
The operational characteristics of LAMP make it particularly suitable for field deployment and point-of-care testing scenarios. Its isothermal nature eliminates the need for expensive thermal cyclers, with reactions possible using simple equipment such as water baths or heat blocks [4] [3]. The rapid turnaround time (often under 60 minutes) and multiple detection options, including visual color changes, enable use in settings with limited laboratory infrastructure [3] [7].
Modeling studies evaluating testing strategies during the COVID-19 pandemic identified LAMP as a balanced option between accuracy and practicality. While RT-PCR remained the most accurate diagnostic test, RT-LAMP provided a viable alternative, particularly in resource-limited settings or where rapid screening was prioritized [9] [10]. The combination of reasonable sensitivity, speed, and minimal equipment requirements positions LAMP as a valuable tool for epidemic control and outbreak investigation.
LAMP technology represents a significant advancement in nucleic acid amplification, offering a combination of sensitivity, specificity, speed, and operational simplicity that distinguishes it from traditional PCR-based methods. The fundamental mechanism relying on isothermal amplification with multiple primers recognizing 6-8 distinct regions of the target DNA provides the foundation for its exceptional performance characteristics. Extensive comparative studies have consistently demonstrated that LAMP outperforms conventional PCR, nested PCR, and real-time PCR in terms of detection limit and amplification time while maintaining high specificity.
The versatility of LAMP is evidenced by its successful application across diverse fields including clinical diagnostics, plant pathology, oncology, and infectious disease surveillance. Its robustness, tolerance to inhibitors, and compatibility with various detection methods—from sophisticated real-time instruments to simple colorimetric changes visible to the naked eye—make it particularly valuable for point-of-care testing and resource-limited settings. As molecular diagnostics continue to evolve, LAMP stands as a powerful technique that combines analytical performance with practical implementation, offering researchers and clinicians a reliable alternative to PCR-based methods for a wide range of applications.
Nested PCR (nPCR) is a powerful modification of the conventional polymerase chain reaction that significantly enhances the sensitivity and specificity of nucleic acid detection. This technique employs two successive rounds of amplification with two distinct sets of primers to enable precise detection of low-abundance targets that might otherwise evade standard PCR methods. The fundamental principle involves an initial amplification using outer primers that target a larger DNA fragment, followed by a secondary amplification using inner primers that bind within the first amplification product. This "nested" approach provides a dual verification system that dramatically reduces non-specific amplification while increasing the reliability of results, particularly when working with challenging samples or minimal target material.
Within the molecular diagnostics landscape, nPCR occupies a crucial position between conventional PCR and more recent advancements like real-time PCR and isothermal amplification methods. While newer techniques offer advantages in quantification speed and simplicity, nPCR remains uniquely valuable for applications demanding maximum sensitivity where target DNA is scarce or sample quality is compromised. The technique's robust performance across diverse fields—from clinical pathogen detection to environmental monitoring and forensic analysis—demonstrates its enduring relevance in the researcher's toolkit, particularly when uncompromising detection certainty is required.
Performance Comparison: nPCR Versus Alternative Amplification Methods
Sensitivity and Specificity Profiles Across Platforms
Table 1: Comparative Performance of Nucleic Acid Amplification Techniques for Pathogen Detection
| Method | Target | Sensitivity (%) | Specificity (%) | Detection Limit | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| nPCR | Listeria monocytogenes [11] | 100 | 100 | 3.5 UFC/25 g, 30 copies/reaction | Enhanced sensitivity/specificity, reduced inhibition sensitivity [11] | Contamination risk, longer process |
| SFTS Virus [12] | 100 | 100 | Up to 40 days post-symptom | Detects targets in convalescent phase | ||
| Schistosoma mansoni [13] | 90.06 (snails) | 85.51 (snails) | N/A | Effective for complex samples | ||
| Real-time PCR (qPCR) | Listeria monocytogenes [11] | Equivalent to nPCR | Equivalent to nPCR | 3.5 UFC/25 g, 30 copies/reaction | Faster, quantitative, lower contamination risk | Higher equipment cost |
| SFTS Virus [12] | 94.4 | 100 | Up to 21 days post-symptom | Rapid, quantitative results | Lower detection in convalescent phase | |
| Schistosoma mansoni [13] | 89.79 (overall) | 87.70 (overall) | N/A | Quantification, high throughput | ||
| LAMP | Schistosoma mansoni [13] | Highest among NAATs | Moderate | N/A | Simple, isothermal, rapid | |
| SARS-CoV-2 [14] | 84.13 | 100 | 15 copies/reaction | Equipment simplicity, rapid (≤60 min) [14] [15] | Lower sensitivity vs rRT-PCR [14] | |
| Hypervirulent K. pneumoniae [16] | >95 | >95 | N/A | Visual detection, simple operation |
Analytical Detection Limits and Time-to-Result Comparison
Table 2: Analytical Performance and Operational Characteristics
| Method | Detection Limit | Time to Result | Equipment Requirements | Quantitative Capability |
|---|---|---|---|---|
| nPCR | As low as 30 copies/reaction [11] | 3-6 hours (including gel electrophoresis) | Standard thermal cycler, gel documentation | Qualitative/Semi-quantitative |
| Real-time PCR | As low as 15 copies/reaction [14] | 1-2 hours | Real-time thermal cycler, specialized optics | Fully quantitative |
| LAMP | 100-180 copies/μL [15] | 30-60 minutes [14] [15] | Water bath/heat block, possibly spectrophotometer | Semi-quantitative |
The comparative data reveals nPCR's particular strength in achieving maximum sensitivity and specificity, often reaching 100% for both parameters as demonstrated in detection of Listeria monocytogenes and SFTS virus [11] [12]. This exceptional performance comes at the cost of longer processing time and increased contamination risk due to the need for reaction tube transfer between amplification rounds. Real-time PCR provides an excellent balance of speed and sensitivity with the added advantage of quantification capabilities, while LAMP offers the simplest operational requirements with moderately compromised sensitivity, particularly evident in the SARS-CoV-2 study showing 84.13% sensitivity compared to RT-PCR [14].
Experimental Protocols and Validation Data
nPCR Protocol for Detection ofListeria monocytogenesin Food Samples
This established protocol from the comparative study of nPCR and real-time PCR for detection of Listeria monocytogenes in soft cheese demonstrates the rigorous methodology required for reliable nPCR results [11]:
Sample Preparation and DNA Extraction:
- Artificially contaminate 25g cheese samples with 3.5 to 3,500 CFU/25g of Listeria monocytogenes
- Enrich samples in half-Fraser broth at 30°C for 24h, then transfer to Fraser broth for additional 24h incubation
- Extract DNA using boiling method with PBST (phosphate-buffered saline with 0.05% Tween 20)
- Boil 1mL of culture at 100°C for 12 minutes, centrifuge at 12,000 × g, and use supernatant as PCR template
Primer Design:
- Target: HlyA gene (listeriolysin O) of Listeria monocytogenes
- External primers: HlyA-EF (forward: 5'-CCTGCATATATCTCAAGTGTG-3') and HlyA-ER (reverse: 5'-GGCAAATAGATGGACGATGTG-3') generating 545bp product
- Internal primers: HlyA-IF (forward: 5'-CCGCAAAAGATGAAGTTCAA-3') and HlyA-IR (reverse: 5'-CCCAAGAGATGTTGAATTGAG-3') generating 255bp product
First Round PCR (50μL reaction):
- 10μL DNA template
- 100μM dNTPs, 1.5mM MgCl₂, 1.25U Taq DNA polymerase
- 0.5μM each outer primer (HlyA-EF and HlyA-ER)
- Thermal cycling: 94°C for 5min; 35 cycles of 94°C for 1min, 60°C for 1min, 72°C for 1min; final extension 72°C for 10min
Second Round PCR (25μL reaction):
- 2μL of first-round PCR product as template
- 0.5μM each inner primer (HlyA-IF and HlyA-IR)
- Remaining components identical to first round
- Thermal cycling: Identical to first round
Internal Amplification Control (IAC):
- Synthetic 85bp DNA sequence with terminal regions complementary to HlyA-FI and HlyA-RI primers
- Yields 106bp product when amplified with HlyA-FI and HlyA-RI primers
- Cloned into pGEM-T easy vector to create pGEMT-IAC plasmids
- Included in reactions to identify PCR inhibition and validate negative results [11]
nPCR Protocol for Detection of Severe Fever with Thrombocytopenia Syndrome (SFTS) Virus
This protocol demonstrates nPCR adaptation for viral RNA detection with exceptional sensitivity, maintaining detection capability up to 40 days post-symptom onset [12]:
Target and Primer Design:
- Target: M-segment of SFTS virus genome
- Primer design follows nested principle with external and internal primer sets
- First round amplifies larger fragment, second round targets internal region
Sample Processing and Reverse Transcription:
- Collect blood samples in EDTA tubes
- Extract viral RNA using commercial extraction kits
- Perform reverse transcription using random hexamers or gene-specific primers
Two-Stage Amplification:
- First round: Conventional RT-PCR with external primers
- Second round: Nested PCR using diluted first-round product with internal primers
- Include appropriate negative and positive controls in each run
Detection and Analysis:
- Analyze second-round products by agarose gel electrophoresis
- Confirm positive results by sequencing of amplified products
- Validation against seroconversion and virus isolation confirms clinical accuracy [12]
nPCR Workflow and Technical Considerations
nPCR Workflow Diagram
The nPCR workflow involves sequential amplification steps that collectively enhance specificity and sensitivity. The process begins with sample DNA extraction using methods ranging from simple boiling to commercial kits, depending on sample complexity and purity requirements. The first amplification round employs outer primers that flank the target region, generating an initial amplification product that includes the specific target amid potential non-specific amplification. A critical product dilution step follows, transferring a small aliquot of the first reaction to minimize carryover of primers and byproducts. The second amplification round uses inner primers that bind within the first amplicon, selectively amplifying only the correct target sequence while dramatically reducing background noise. Finally, analysis by gel electrophoresis confirms the presence of the specific-sized amplicon, with the nested approach providing verification that the detected product originates from the intended target.
Critical Technical Considerations for Optimizing nPCR
Primer Design Optimization:
- Inner primers must be completely contained within the outer primer amplicon
- Avoid complementarity within and between primer sets to prevent primer-dimer formation
- Maintain similar melting temperatures within each primer pair (±2°C)
- Verify specificity through in silico analysis against relevant databases
Contamination Prevention Strategies:
- Physical separation of pre- and post-amplification work areas
- Use of dedicated equipment and supplies for each amplification stage
- Incorporation of negative controls at both amplification stages
- Implementation of UV irradiation and chemical decontamination protocols
- Consideration of closed-tube systems when possible to minimize aerosol risk
Reaction Optimization Parameters:
- Magnesium concentration titration (typically 1.5-2.5mM)
- Annealing temperature optimization for both primer sets
- Cycle number determination to balance sensitivity and specificity
- Template dilution testing to identify optimal concentration for second round
Essential Research Reagents and Solutions
Table 3: Essential Research Reagent Solutions for nPCR
| Reagent/Solution | Function | Specification Notes |
|---|---|---|
| DNA Polymerase | Catalyzes DNA synthesis | Thermostable (e.g., Taq polymerase); must retain activity through multiple heating cycles |
| dNTP Mix | Building blocks for DNA synthesis | High-purity, neutral pH; typical working concentration 200μM each dNTP |
| Primer Pairs (Outer & Inner) | Target sequence recognition | HPLC-purified; designed with appropriate melting temperatures; minimal self-complementarity |
| Buffer System | Optimal enzyme activity | Typically supplied with enzyme; contains salts, sometimes with enhancers like DMSO or BSA |
| Magnesium Chloride | Cofactor for polymerase | Separate optimization required; typical range 1.5-2.5mM final concentration |
| Template DNA | Target for amplification | Quality and quantity critical; may require purification from inhibitors |
| Nuclease-Free Water | Reaction preparation | Free of nucleases that could degrade primers or templates |
| Agarose | Gel electrophoresis | High-quality, molecular biology grade for product visualization |
| Nucleic Acid Stain | DNA detection | Ethidium bromide, SYBR Safe, or equivalent for visualizing amplified products |
| Internal Amplification Control (IAC) | Inhibition detection | Non-target sequence amplified by same primers; identifies false negatives [11] |
nPCR remains an indispensable technique in the molecular biologist's arsenal when maximum detection sensitivity and specificity are paramount. The two-stage amplification process, while more time-consuming than single-round methods, provides unparalleled verification of target detection through its nested primer design. This approach demonstrates particular value in detecting low-abundance pathogens, working with compromised samples, and applications requiring absolute certainty in results.
The comparative data presented reveals that nPCR consistently achieves exceptional sensitivity and specificity profiles, often matching or exceeding alternative amplification platforms while requiring less sophisticated instrumentation. While real-time PCR offers advantages in quantification speed and reduced contamination risk, and LAMP provides extreme operational simplicity, nPCR maintains its niche for the most challenging detection scenarios. The technique's proven performance across diverse fields—from clinical diagnostics to environmental monitoring—ensures its continued relevance despite the emergence of newer amplification technologies. For researchers and drug development professionals requiring uncompromising detection certainty, nPCR provides a robust, reliable solution validated through decades of laboratory implementation.
This guide details the principles of Real-Time Reverse Transcription Polymerase Chain Reaction (RT-PCR), a cornerstone technology in molecular diagnostics, and objectively compares its performance against two other nucleic acid amplification techniques: Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP) and nested PCR (nPCR).
Core Principles of Real-Time Fluorescence RT-PCR
Real-Time RT-PCR is a highly sensitive technique used to detect and quantify specific RNA sequences. Its core principle involves the reverse transcription of RNA into complementary DNA (cDNA), followed by the simultaneous amplification and detection of the cDNA in real time.
The process relies on fluorescent reporter molecules. As the target sequence amplifies, the fluorescence increases proportionally. The cycle threshold (Ct) value is a critical quantitative parameter, representing the amplification cycle at which the fluorescent signal crosses a predetermined threshold. A lower Ct value indicates a higher starting concentration of the target RNA [17] [18].
The following diagram illustrates the fundamental workflow and detection mechanism.
Performance Comparison: RT-PCR vs. RT-LAMP vs. nPCR
The following tables summarize the direct experimental comparisons and key characteristics of these three techniques.
Table 1: Experimental Performance Comparison from Clinical Studies
| Methodology | Target Pathogen | Reported Sensitivity | Specificity | Key Performance Context |
|---|---|---|---|---|
| RT-PCR | SARS-CoV-2 | Gold Standard [19] [14] | Gold Standard [19] [14] | Used as reference in multiple studies. |
| RT-LAMP | SARS-CoV-2 | 71% (direct swab) to 100% (extracted RNA) [19] [20] | 100% [14] [20] [21] | Sensitivity highly dependent on sample prep; optimal time ~45 min [19]. |
| RT-LAMP | SARS-CoV-2 | 84.1% (overall) [14] | 100% [14] | Sensitivity rises to 98-100% for samples with Ct < 30 [14] [21]. |
| nested PCR | Feline Calicivirus | 31.48% [22] | Not Specified | Higher detection rate vs. conventional PCR (1.85%) in clinical samples [22]. |
Table 2: Characteristic and Workflow Comparison
| Feature | RT-PCR | RT-LAMP | nPCR |
|---|---|---|---|
| Principle | Fluorescence-based amplification with thermal cycling | Isothermal amplification with strand-displacing polymerase | Two rounds of PCR with two primer sets |
| Amplification Temp. | Multiple (Denaturation, Annealing, Extension) [20] | Constant (~60-65°C) [19] [14] | Multiple (Two separate thermal cycling runs) [22] |
| Time to Result | 1 - 2+ hours [19] [20] | ~30 - 60 minutes [19] [14] [21] | Several hours (due to two rounds) [22] |
| Throughput | High (96/384-well formats) | Moderate to High | Low to Moderate |
| Key Advantage | Gold standard sensitivity, robust quantification | Speed, simplicity, potential for point-of-care | High specificity, sensitivity for complex samples |
| Key Limitation | Requires expensive thermal cyclers, skilled personnel [19] | Lower sensitivity with direct samples, primer design complexity [19] | High contamination risk, more complex workflow [22] |
| Quantification | Excellent (Absolute/Robust Relative) [17] | Semi-Quantitative | Qualitative / Semi-Quantitative |
Experimental Protocols and Modeling Data
Detailed RT-LAMP Protocol for SARS-CoV-2 Detection
A typical protocol for detecting SARS-CoV-2, as used in recent studies, is outlined below [14] [21].
- Primer Design: A set of six primers (F3, B3, FIP, BIP, LF, LB) is designed to recognize eight distinct regions of a target gene, such as the ORF8 or ORF1a gene of SARS-CoV-2, ensuring high specificity [19] [14].
- Reaction Setup:
- Amplification: Incubate the reaction at a constant temperature of 63°C for 45-60 minutes in a real-time PCR analyzer or a dry bath [19] [14] [21].
- Result Detection:
- Real-time: Monitor fluorescence (FAM channel) for amplification curves [14].
- Colorimetric: Visually inspect for a color change post-amplification (e.g., from orange to pink with neutral red) [21] [22].
- Post-amplification analysis: Perform melting curve analysis to verify amplification specificity [14].
Detailed nPCR Protocol for Pathogen Detection
A protocol for detecting Feline Calicivirus (FCV) exemplifies the nPCR workflow [22].
- First Round PCR:
- Use an outer primer set to perform a standard PCR reaction, amplifying a larger target region.
- Typical cycling conditions: initial denaturation (e.g., 95°C for 5 min), followed by 30-35 cycles of denaturation, annealing, and extension.
- Second Round (Nested) PCR:
- Use a second set of primers ("nested primers") that bind inside the amplicon generated in the first PCR.
- A small aliquot (e.g., 1-2 µL) of the first PCR product is used as the template for this second reaction.
- Run a second PCR with similar cycling conditions, but for fewer cycles (e.g., 20-25).
- Detection: Analyze the final PCR product using agarose gel electrophoresis to confirm the presence and size of the amplified fragment [22].
Modeling of Testing Strategy Effectiveness
A 2025 modeling study evaluated the effectiveness of different testing strategies for COVID-19 control, considering not just test sensitivity but also turnaround time and frequency [23]. The key findings relevant to this comparison include:
- Daily screening with RT-PCR or RT-LAMP was most effective at reducing transmission risk but incurred the highest costs.
- Symptom-based testing was a more cost-effective alternative. In this context, the turnaround time was found to be a more critical factor for outbreak containment than the raw analytical sensitivity of the assay.
- Antigen tests (with lower sensitivity) were a viable, cost-effective option for symptom-based testing in resource-limited settings, underscoring that the "best" test depends on the public health goal [23].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Nucleic Acid Amplification Assays
| Reagent / Material | Function in the Experiment | Example from Search Results |
|---|---|---|
| Bst DNA/RNA Polymerase | Key enzyme for RT-LAMP; performs reverse transcription and strand-displacement DNA amplification isothermally. | New England Biolabs' WarmStart Bst [14] [20] |
| Fluorescent Probe/Dye | Enables real-time detection of amplification in RT-PCR (hydrolysis probes) or RT-LAMP (intercalating dyes). | FAM-channel dyes [14], SYBR Green [22] |
| Colorimetric Indicator | Allows visual, equipment-free detection of LAMP amplification through pH change or metal ion complexation. | Neutral red [22], phenol red [19] |
| Primer Sets (LAMP) | A set of 4-6 primers recognizing 6-8 target regions, fundamental to LAMP's specificity and efficiency. | Primers targeting SARS-CoV-2 ORF8 or ORF1a [19] [14] |
| Nested Primer Sets | Two pairs of primers for nPCR; the second "nested" set increases specificity and sensitivity by re-amplifying an internal fragment. | Primers for FCV ORF2 gene [22] |
| RNA Extraction Kit | Purifies and isolates high-quality RNA from clinical samples (e.g., swabs, saliva), critical for assay sensitivity. | Magnetic bead-based kits (e.g., MagMax) [17] [24] |
Workflow Comparison and Strategic Selection
The following diagram synthesizes the core workflows of the three techniques, highlighting their procedural differences and key characteristics.
The choice between RT-PCR, RT-LAMP, and nPCR is not a matter of one being universally superior but depends on the specific requirements of the testing scenario.
- RT-PCR remains the gold standard for applications demanding the highest sensitivity and precise quantification, such as clinical diagnostics and viral load monitoring, where resources and technical expertise are available [19] [17].
- RT-LAMP is a powerful alternative for rapid screening, field deployment, and resource-limited settings. Its speed, simplicity, and minimal equipment requirements make it ideal for point-of-care testing, though its performance can vary with sample preparation methods [19] [14] [23].
- nPCR is a highly specific technique useful for detecting low-abundance targets or in complex samples where maximum specificity is needed, despite its longer workflow and high contamination risk [22].
Ultimately, the strategic selection of a molecular diagnostic tool involves a careful balance between the need for sensitivity, speed, cost, ease of use, and the available laboratory infrastructure.
Comparative Analysis of Reaction Conditions and Enzyme Requirements
The evolution of nucleic acid amplification techniques has fundamentally transformed molecular diagnostics and research. Among these methods, Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and Reverse Transcription PCR (RT-PCR) represent significant technological milestones, each with distinct reaction conditions and enzyme requirements that directly influence their application scope and performance characteristics. This guide provides a detailed comparative analysis of these fundamental parameters, drawing upon experimental data and clinical validation studies to offer researchers, scientists, and drug development professionals a clear framework for methodological selection. Understanding the enzymatic dependencies and optimal reaction environments for LAMP, nPCR, and RT-PCR is crucial for designing robust diagnostic assays, particularly in contexts requiring high sensitivity, rapid results, or resource-limited implementation. The following sections will dissect the core components, performance metrics, and practical protocols that define these established amplification platforms.
Fundamental Principles and Core Components
The core distinction between these techniques lies in their amplification mechanics and enzymatic requirements. LAMP is an isothermal amplification method that utilizes a strand-displacing DNA polymerase to synthesize DNA at a constant temperature, typically between 60°C and 65°C [25] [19]. This process employs four to six primers that recognize six to eight distinct regions on the target DNA, creating loop structures that enable self-priming and exponential amplification [25] [26]. In contrast, nPCR and RT-PCR are both thermocycling-based methods that rely on a thermostable DNA polymerase, such as Taq polymerase, which functions through repeated cycles of denaturation, annealing, and extension at varying temperatures [5] [25].
RT-PCR specifically incorporates a reverse transcriptase enzyme to convert RNA into complementary DNA (cDNA) before the amplification process, making it indispensable for RNA virus detection and gene expression analysis [25]. nPCR enhances sensitivity and specificity by performing two consecutive rounds of amplification using two sets of primers, where the product of the first PCR reaction serves as the template for the second round with primers that bind internally to the first amplicon [5] [27].
The following table summarizes the essential reagents and their functions common to these molecular techniques:
Table 1: Key Research Reagent Solutions for Nucleic Acid Amplification
| Reagent | Function | LAMP | nPCR | RT-PCR |
|---|---|---|---|---|
| Bst DNA Polymerase | Strand-displacing enzyme for isothermal amplification | Required | Not Used | Not Used |
| Taq DNA Polymerase | Thermostable enzyme for thermocycling | Not Used | Required | Required |
| Reverse Transcriptase | Converts RNA to cDNA | Required (for RT-LAMP) | Not Used | Required |
| dNTPs | Building blocks for new DNA strands | Required | Required | Required |
| Primers | Bind specific target sequences for amplification | 4-6 primers | 2 sets of 2 primers | 2 primers |
| Buffer System | Maintains optimal pH and reaction conditions | Isothermal buffer | PCR buffer | PCR buffer |
Comparative Performance Data Analysis
Quantitative comparisons across multiple studies consistently reveal distinct performance profiles for each technique. A foundational study comparing LAMP, nPCR, and real-time PCR (qPCR) for detecting Entamoeba histolytica demonstrated striking differences in sensitivity. LAMP achieved a limit of detection (LoD) of a single trophozoite, outperforming both nPCR and qPCR, which recorded LoDs of 100 trophozoites each. Conventional PCR was significantly less sensitive, with an LoD of 1000 trophozoites [5]. This superior sensitivity of LAMP has been consistently documented in plant pathogen detection as well, where it showed a 10-fold improvement over conventional PCR, though it was 100-fold less sensitive than nPCR and 1000-fold less sensitive than qPCR for the specific detection of Alternaria solani [27].
In the context of SARS-CoV-2 detection, the comparative performance is more nuanced. RT-LAMP exhibited a high correlation with RT-qPCR when using extracted RNA, with some studies reporting complete agreement between the two methods [28] [19]. However, this sensitivity can decrease when using direct swab samples without RNA extraction, where RT-LAMP sensitivity relative to RT-qPCR dropped to 71% in one study [19]. The detection limit for SARS-CoV-2 RT-LAMP has been reported at 23.4-42.8 RNA copies for purified RNA, while fewer than 250 copies could not be detected using crude RNA without purification [28].
The following table synthesizes quantitative performance data from empirical studies:
Table 2: Comparative Performance Metrics of Amplification Techniques
| Technique | Limit of Detection (LoD) | Amplification Time | Reaction Temperature | Key Applications |
|---|---|---|---|---|
| LAMP | 1 parasite (E. histolytica) [5]; 23.4-42.8 RNA copies (SARS-CoV-2, purified RNA) [28] | 45-60 min [5] [19] | 60-65°C (constant) [25] [19] | Point-of-care testing, field diagnostics [28] [29] |
| nPCR | 100 parasites (E. histolytica) [5]; 100 fg genomic DNA (A. solani) [27] | 2-3 hours (including two rounds) [5] | 95°C, 50-65°C, 72°C (cycling) | High-sensitivity detection, pathogen differentiation [5] [27] |
| RT-PCR | 100 parasites (E. histolytica) [5]; Varies with protocol | 1.5-3 hours [26] | 95°C, 50-60°C, 72°C (cycling) | Gold standard for RNA virus detection, gene expression analysis [30] [25] |
Detailed Experimental Protocols
RT-LAMP Assay Protocol
The RT-LAMP protocol for SARS-CoV-2 detection, as optimized by Gholami et al., utilizes a primer set targeting the ORF1a gene [19]. The reaction is typically performed in a 25 μL volume containing 12.5 μL of 2× WarmStart Colorimetric LAMP master mix (includes Bst DNA polymerase and reverse transcriptase), 1.6 μM each of FIP and BIP primers, 0.2 μM each of F3 and B3 primers, and 5 μL of extracted RNA template. The mixture is incubated at 65°C for 45 minutes in a thermal cycler or dry block heater, followed by enzyme inactivation at 80°C for 5 minutes. Results can be determined via real-time fluorescence monitoring, agarose gel electrophoresis, or visual color change when using colorimetric master mixes containing pH-sensitive dyes [19] [29]. For dengue virus detection, a similar TURN-RT-LAMP assay employs two primer sets targeting both the 5′- and 3′-UTR regions in a single reaction to enhance sensitivity, achieving >96% in clinical validation [29].
nPCR Assay Protocol
The nPCR protocol for Entamoeba histolytica detection, as described by Foo et al., involves two consecutive amplification rounds [5]. The first round uses external primers in a 25 μL reaction containing standard PCR components: 1× PCR buffer, 1.5-2.0 mM MgCl₂, 200 μM dNTPs, 0.2 μM each primer, 1.25 U Taq DNA polymerase, and 2 μL DNA template. The thermal cycling conditions are: initial denaturation at 95°C for 3 min; 30 cycles of denaturation at 95°C for 30 sec, annealing at 58°C for 30 sec, and extension at 72°C for 1 min; with a final extension at 72°C for 5 min. For the second round, 1 μL of the first PCR product is transferred to a fresh tube containing the same reaction components but with internal primers that bind within the first amplicon. The cycling conditions are identical. Products from both rounds are analyzed by agarose gel electrophoresis [5].
RT-qPCR Assay Protocol
The RT-qPCR protocol for SARS-CoV-2 using the CDC (USA) protocol involves a one-step reaction where reverse transcription and PCR amplification occur in the same tube [30]. A typical 20 μL reaction contains 5 μL of extracted RNA, 10 μL of 2× reaction buffer, 0.4 μL of reverse transcriptase/Taq polymerase mix, 400-500 nM of each primer (targeting N1 and N2 genes), and 125-150 nM of probes. The thermal cycling conditions on a real-time PCR instrument are: reverse transcription at 50°C for 20 min; initial denaturation at 95°C for 3 min; followed by 40-45 cycles of denaturation at 95°C for 15 sec and annealing/extension at 60°C for 1 min. Fluorescence is measured at the end of each cycle, and samples are considered positive if amplification of both N1 and N2 gene fragments occurs at a cycle threshold (Ct) ≤37 [30].
Technical Workflow and Performance Relationships
The following diagrams illustrate the fundamental workflows and performance relationships between these amplification techniques.
Diagram 1: Comparative Workflows of LAMP, nPCR, and RT-PCR
Diagram 2: Performance Attribute Comparison
This comparative analysis elucidates the distinct reaction conditions and enzyme requirements that define LAMP, nPCR, and RT-PCR methodologies. LAMP offers significant advantages in speed, operational simplicity, and cost-effectiveness, requiring only basic equipment while maintaining high sensitivity, making it ideally suited for point-of-care and resource-limited settings [28] [29]. nPCR provides exceptional specificity and sensitivity through its two-stage amplification process, though it demands more time and laboratory infrastructure [5] [27]. RT-PCR remains the gold standard for RNA target quantification with robust performance and widespread validation, albeit with higher equipment requirements and operational complexity [30] [19].
The selection of an appropriate amplification technique ultimately depends on the specific research or diagnostic context, including target type (DNA vs. RNA), required sensitivity and specificity, available resources, and intended application setting. Future advancements in primer design, enzyme engineering, and detection methodologies will continue to refine the performance and accessibility of these foundational molecular tools, further expanding their utility across biomedical research, clinical diagnostics, and public health initiatives.
Key Applications and Historical Development of Each Technique
Molecular diagnostics represent a cornerstone of modern biomedical research and clinical practice, with techniques like reverse transcription PCR (RT-PCR), loop-mediated isothermal amplification (LAMP), and digital PCR (dPCR) enabling sensitive detection and quantification of nucleic acids. The ongoing pursuit of greater sensitivity, specificity, and operational efficiency drives continuous innovation in this field. This guide provides a comprehensive comparison of these three key technologies—RT-PCR, LAMP, and dPCR—focusing on their historical development, key applications, and relative performance characteristics, particularly their analytical sensitivity. For researchers, scientists, and drug development professionals, understanding the technical capabilities and limitations of each method is crucial for selecting the optimal platform for specific diagnostic and research applications, from routine pathogen detection to absolute quantification of rare genetic targets.
Historical Development
The Evolution of PCR and RT-PCR
The invention of the polymerase chain reaction (PCR) by Kary Mullis in 1983 marked a revolutionary advancement in molecular biology [31]. The original process was tedious, requiring fresh polymerase enzyme to be added after each denaturation cycle because the initial enzyme was destroyed by high temperatures [31]. A critical breakthrough came with the utilization of a thermostable DNA polymerase from Thermus aquaticus (Taq polymerase), which could withstand the repeated high-temperature cycles, enabling automation and broader adoption [31]. Early thermal cyclers included both space-domain systems, where samples were moved between different temperature zones, and time-domain systems, where the sample block changed temperature; the latter became more common [31].
The application spectrum of PCR expanded rapidly from its initial use in detecting mutations for sickle cell anemia [31]. The development of multiplex PCR, which allows simultaneous amplification of multiple targets in a single tube, was another significant milestone, first used for detecting deletions in the DMD gene [31]. The integration of reverse transcription (RT) as a preliminary step enabled the amplification and study of RNA targets, giving rise to RT-PCR [32]. The subsequent development of real-time or quantitative PCR (qPCR) in 1993 allowed researchers to monitor amplification kinetics in real-time, transforming PCR from a qualitative to a fully quantitative tool [31]. RT-PCR, particularly in its quantitative form (qRT-PCR), has since become the gold standard for RNA detection and quantification, displacing older techniques like Northern blot [32].
The Emergence of Isothermal Amplification and LAMP
Loop-mediated isothermal amplification (LAMP) was developed by Notomi et al. in 2000 as a novel nucleic acid amplification method that operates at a constant temperature, eliminating the need for thermal cycling [33] [34]. This technique relies on a strand-displacing DNA polymerase and a set of four to six primers that recognize six to eight distinct regions on the target gene, leading to highly specific amplification [33]. The method produces up to 10^9 copies of the target in less than an hour and results can be monitored through turbidity, fluorescence, or colorimetric changes [33]. The isothermal nature of LAMP, typically between 60°C and 65°C, removes the requirement for expensive thermal cyclers, making it particularly suitable for point-of-care testing and resource-limited settings [35] [33]. Continuous improvements in polymerase enzymes, such as the development of Bst 2.0 and Bst 3.0 with enhanced speed, stability, and reverse transcriptase activity, have further advanced LAMP technology [33].
The Advent of Digital PCR
Digital PCR (dPCR) represents a third-generation PCR technology that enables absolute quantification of nucleic acids without the need for standard curves [31] [17]. The core principle involves partitioning a PCR reaction into thousands of individual subsamples, such that each contains either zero or one (or a few) target molecules [31] [17]. After end-point PCR amplification, the number of positive partitions is counted, and using Poisson statistics, the absolute copy number of the target in the original sample is calculated [17]. dPCR platforms are primarily of two types: droplet-based digital PCR (ddPCR), which uses water-in-oil emulsions to create tens of thousands of nanoliter-sized reactions [31], and chip-based digital PCR (cdPCR), which uses microfabricated wells on a silicon chip [31]. This partitioning process makes dPCR exceptionally robust to PCR inhibitors and allows for precise quantification, especially of rare alleles and low-abundance targets [17].
Table 1: Historical Milestones of Molecular Amplification Techniques
| Year | Technique | Key Development | Significance |
|---|---|---|---|
| 1983 | PCR | Invention by Kary Mullis [31] | Enabled targeted DNA amplification |
| 1985 | PCR | First automated system ("Baby Blue") [31] | Reduced manual intervention |
| 1987 | RT-PCR | First used for infectious disease diagnosis [31] | Expanded application to RNA targets |
| 1990s | PCR | Use of Taq polymerase [31] | Enabled full automation of thermal cycling |
| 1993 | qPCR | Real-time kinetic monitoring [31] | Transformed PCR into a quantitative tool |
| 2000 | LAMP | Description by Notomi et al. [33] | Introduced rapid, isothermal amplification |
| 2000s | dPCR | Concept of digital quantification [31] | Enabled absolute quantification without standard curves |
Technique Comparison and Performance Data
Principles and Workflows
The fundamental principles and workflows of RT-PCR, LAMP, and dPCR differ significantly, influencing their application and performance.
RT-PCR/qPCR: This method relies on the reverse transcription of RNA into complementary DNA (cDNA), followed by thermal cycling for amplification. The quantification occurs in real-time using fluorescent chemistries. Two main approaches exist: one-step RT-PCR, where reverse transcription and PCR occur in the same tube, minimizing handling and contamination risk; and two-step RT-PCR, where the reactions are performed separately, offering more flexibility but increased handling [32]. Detection relies on fluorescent signals, with common chemistries including DNA-binding dyes (e.g., SYBR Green) and sequence-specific probes (e.g., TaqMan, molecular beacons) that provide higher specificity [32].
LAMP: This is an isothermal amplification that uses 4-6 primers targeting 6-8 regions of the desired gene. The process involves inner primers (FIP, BIP) and outer primers (F3, B3), which generate complex structures with loop regions that serve as initiation sites for subsequent amplification cycles, leading to the production of long DNA concatemers [33]. The reaction is typically performed at 60-65°C for 15-60 minutes. Results can be monitored in real-time via turbidimetry (measuring magnesium pyrophosphate precipitate), fluorometry (using DNA-intercalating dyes), or colorimetry (using pH-sensitive dyes or metal ion indicators like calcein or hydroxy naphthol blue) for visual, equipment-free detection [33] [36].
dPCR: The workflow begins with a standard PCR mixture, which is partitioned into thousands of nanoscale reactions. Each partition acts as an individual PCR microreactor. After end-point thermal cycling, the partitions are analyzed to determine the fraction that is positive for fluorescence. The absolute concentration of the target molecule is then calculated using Poisson statistics, based on the principle that the number of target molecules per partition follows a Poisson distribution [17]. This method does not require a standard curve and is less affected by inhibitors or amplification efficiency variations [17].
Sensitivity and Performance Comparison
Sensitivity is a critical parameter for comparing molecular diagnostics. Recent studies provide direct comparative data.
A 2025 study on respiratory virus diagnostics during the 2023-2024 "tripledemic" directly compared dPCR and real-time RT-PCR [17]. The results demonstrated that dPCR offered superior accuracy and precision, particularly for samples with high viral loads (Ct ≤ 25) of Influenza A, Influenza B, and SARS-CoV-2, and for medium loads (Ct 25.1-30) of RSV [17]. dPCR showed greater consistency in quantifying intermediate viral levels, highlighting its robustness for precise quantification [17]. However, the authors noted that the routine implementation of dPCR is currently limited by higher costs and reduced automation compared to RT-PCR [17].
For LAMP, a 2025 multi-platform detection system for Human Adenovirus (HAdV) reported a limit of detection (LOD) of 2.5 copies/reaction for colorimetric (calcein) and immunochromatographic (IC) methods, while the fluorescent probe-based LAMP method demonstrated a superior sensitivity of 1 copy/reaction [36]. This fluorescent LAMP assay showed 100% concordance with qPCR when validated on 188 clinical samples (κ = 1.00) and performed reliably in low-viral-load and co-infection cases, with a rapid detection time of ≤20 minutes [36].
Another modeling study on COVID-19 testing strategies concluded that for outbreak control, the turnaround time of testing was a more critical factor than the analytical sensitivity of the assay itself [9]. This finding underscores a key advantage of LAMP and rapid antigen tests, which can provide results much faster than standard RT-PCR, thereby offering a significant public health benefit despite potentially lower sensitivity.
Table 2: Comparative Performance of RT-PCR, LAMP, and dPCR
| Parameter | RT-PCR / qPCR | LAMP | dPCR |
|---|---|---|---|
| Typical Limit of Detection (LOD) | Varies; ~10-100 copies [36] | 1-10 copies/reaction [36] | Single copy detection [17] |
| Quantification Basis | Relative (Ct value vs. standard curve) | End-point or real-time (Time-positive) | Absolute (Poisson statistics) |
| Precision / Reproducibility | High | High | Superior, especially for low targets [17] |
| Tolerance to Inhibitors | Moderate | Moderate (improved with Bst 3.0) [33] | High (due to partitioning) [17] |
| Assay Time (Amplification) | 1 - 2 hours | 15 - 60 minutes [36] | 1.5 - 3 hours (includes partitioning) |
| Throughput | High | Medium to High | Medium |
| Multiplexing Capability | High (with probe-based detection) | Low (challenging in single tube) [33] | Medium (limited by color channels) |
| Key Advantage | Gold standard, quantitative, multiplexable | Rapid, simple, equipment-free options | Absolute quantification, high precision |
Key Applications
RT-PCR and qPCR Applications
As the established gold standard, RT-PCR's applications are vast and foundational. It is indispensable for infectious disease diagnostics, including the detection of SARS-CoV-2, influenza, and RSV [17] [32]. It serves as a critical tool for gene expression analysis in research, allowing for the comparison of mRNA levels across different samples or conditions [32]. Furthermore, it is used in genetic testing for detecting mutations, SNPs, and in cancer research for profiling gene expression and translocations [31].
LAMP Applications
LAMP's speed and simplicity have led to its adoption in diverse fields where rapid, on-site testing is paramount. Its primary application is in infectious disease diagnostics, especially at the point-of-care for pathogens like COVID-19, tuberculosis, and malaria [35] [33]. It is extensively used in food safety testing for the rapid detection of contaminants like Salmonella and Listeria, enabling same-day results and reducing recall risks [35]. In veterinary diagnostics, LAMP allows for swift on-farm identification of diseases such as avian influenza and foot-and-mouth disease [35]. It is also increasingly applied in environmental monitoring for microbial contamination in water sources and in agriculture for detecting plant pathogens, such as those causing pea root rot, directly in the field [35] [34].
Digital PCR Applications
dPCR excels in applications requiring absolute quantification and high precision. It is particularly valuable for detecting rare genetic variants and low-abundance targets, such as circulating tumor DNA (ctDNA) in liquid biopsies for oncology [17]. It is the preferred method for absolute quantification of viral loads without standard curves, providing more precise data for studies on viral dynamics and treatment efficacy [17]. dPCR is also used in gene expression analysis of low-abundance transcripts, copy number variation (CNV) analysis, and quality control of next-generation sequencing (NGS) libraries, where accurate quantification of input material is crucial [31].
Table 3: Key Application Fields for Each Technique
| Application Field | RT-PCR / qPCR | LAMP | dPCR |
|---|---|---|---|
| Clinical Virology | Primary diagnostic tool (Gold Standard) [32] | Rapid point-of-care & screening [35] | Precise viral load monitoring [17] |
| Gene Expression | Standard for relative quantification [32] | Limited application | Absolute quantification of rare transcripts |
| Oncology Research | Mutation detection, expression profiling | Emerging for specific mutations | Rare allele detection (e.g., ctDNA), CNV |
| Food Safety & Veterinary | Used in central labs | Dominant for on-site/field testing [35] | Limited application |
| Environmental Monitoring | Standard lab-based testing | Portable, on-site detection [35] | Limited application |
| Research & NGS | Gene validation, QC | Target verification | Library quantification, QC [31] |
Experimental Protocols and Reagents
Detailed Protocol: Multi-Platform LAMP Assay for HAdV
A 2025 study established a robust multi-platform LAMP system for detecting Human Adenovirus types 3 and 7, providing an excellent example of a modern LAMP workflow [36].
- Primer Design: Primers were designed based on the conserved regions of the Hexon genes of HAdV-3 and HAdV-7, obtained from the NCBI database. A full set of LAMP primers was designed using PrimerExplorer V5, including outer primers (F3, B3), inner primers (FIP, BIP), and loop primers (LF, LB). For different detection platforms, primers were modified: for the immunochromatography (IC) method, the FIP primer was labeled with TAMRA and the LF primer with biotin; for the fluorescent probe method, a dual-labeled probe (HEX at 5' end, BHQ1 quencher at 3' end) was designed [36].
- Nucleic Acid Extraction: Total nucleic acids were extracted from clinical throat swab samples using a commercial nucleic acid extraction kit on an automated platform [36].
- LAMP Reaction Setup: The reaction was performed using a 2× RT-LAMP Premix. The 25 μL reaction mixture contained 12.5 μL of premix, 1 μL of primer mix (final concentrations: 1.6 μM each of FIP and BIP, 0.2 μM each of F3 and B3, 0.4 μM each of LF and LB), 2 μL of template DNA, and nuclease-free water up to the volume. For the fluorescent probe method, the dual-labeled probe was added [36].
- Amplification and Detection: The reaction was incubated at 63°C for 30 minutes. Detection was performed on three platforms:
- Calcein Method: The reaction mix included calcein. A color change from orange to green/yellow under UV light indicated a positive result.
- Immunochromatography (IC) Method: The biotin- and TAMRA-labeled amplicons were applied to a test strip. The appearance of both test and control lines indicated a positive result.
- Fluorescent Probe Method: Real-time fluorescence was monitored on a portable device [36].
Detailed Protocol: Comparative dPCR vs. RT-PCR for Respiratory Viruses
A 2025 study provided a direct comparative protocol for dPCR and real-time RT-PCR [17].
- Sample Collection: Respiratory samples (nasopharyngeal swabs and one BAL) were collected from symptomatic patients and stratified by Ct values into high (Ct ≤25), medium (Ct 25.1–30), and low (Ct >30) viral load categories [17].
- Nucleic Acid Extraction: For both methods, RNA was extracted using automated commercial systems (KingFisher Flex for dPCR; STARlet for RT-PCR) with viral/pathogen nucleic acid kits [17].
- Real-Time RT-PCR Workflow: Extracted RNA was subjected to multiplex real-time RT-PCR using commercial respiratory panel kits targeting specific viral genes (Influenza A, B, RSV, SARS-CoV-2). Amplification and Ct value determination were performed on a standard thermocycler [17].
- Digital PCR Workflow: Extracted RNA was analyzed on a nanowell-based dPCR system (QIAcuity). The reaction mix, including primer-probe sets for the same targets and an internal control, was loaded into nanoplates, partitioning the sample into ~26,000 wells. End-point PCR was performed, and fluorescent signals were analyzed by the instrument's software to provide absolute copy numbers [17].
- Statistical Analysis: Data from both methods were analyzed descriptively. The Kruskal-Wallis test was used to compare the performance of dPCR and RT-PCR across the different viral load categories [17].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents and Kits for Molecular Amplification Techniques
| Reagent / Kit | Function / Description | Example Techniques |
|---|---|---|
| Bst DNA Polymerase | Strand-displacing DNA polymerase for isothermal amplification. Engineered versions (Bst 2.0, Bst 3.0) offer improved speed, stability, and RT activity [33]. | LAMP |
| Taq DNA Polymerase | Thermostable DNA polymerase with 5'-3' polymerase activity; the workhorse enzyme for PCR. | RT-PCR, dPCR |
| Reverse Transcriptase | Enzyme that synthesizes cDNA from an RNA template. | RT-PCR |
| dNTPs | Deoxyribonucleotide triphosphates (dATP, dCTP, dGTP, dTTP); the building blocks for DNA synthesis. | All |
| Primers & Probes | Oligonucleotides designed to specifically hybridize to the target sequence. Probes (TaqMan, Molecular Beacons) provide specificity in qPCR and dPCR [32]. | All |
| DNA Binding Dyes (SYBR Green) | Fluorescent dyes that intercalate into double-stranded DNA, allowing real-time detection of amplification [32]. | qPCR |
| Calcein / HNB Dye | Colorimetric indicators for visual detection of LAMP amplification. Calcein changes from orange to green; HNB changes from violet to sky blue [33] [36]. | LAMP |
| Commercial Premixes | Optimized master mixes containing buffer, enzymes, dNTPs, etc., for specific techniques (e.g., 2× RT-LAMP Premix [36]). | All |
The choice between RT-PCR, LAMP, and dPCR is not a matter of identifying a single superior technology, but rather of selecting the right tool for a specific application, considering the trade-offs between sensitivity, speed, cost, and operational requirements. RT-PCR remains the gold standard for versatile, quantitative analysis in centralized laboratories. LAMP has carved out a critical niche as a rapid, portable, and accessible technology for point-of-care and field-use settings, where speed and simplicity are paramount. dPCR provides the highest level of precision and absolute quantification, making it indispensable for advanced research and clinical applications where detecting rare events or achieving maximum accuracy is necessary. As innovations in polymerase engineering, primer design, and detection chemistries continue, the performance boundaries of all three techniques will expand, further solidifying their collective role in advancing research, public health, and clinical diagnostics.
Methodology in Action: Protocol Design and Pathogen Detection
The accuracy of molecular diagnostic tests for infectious diseases, including SARS-CoV-2, is highly dependent on two critical factors: the sample preparation methodology and the analytical technique employed. The broader thesis of sensitivity comparison between Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and Reverse Transcription-PCR (RT-PCR) research must account for substantial variability introduced during sample collection, processing, and nucleic acid extraction. This guide objectively compares the performance of these molecular techniques across different sample matrices, supported by experimental data and detailed methodologies to inform researchers, scientists, and drug development professionals.
Performance Comparison Across Sample Types
The diagnostic sensitivity of molecular assays varies significantly depending on the sample type and preparation method. The table below summarizes the comparative performance of RT-LAMP and RT-PCR (including real-time quantitative RT-PCR, or RT-qPCR) across different sample types, based on aggregated research findings.
Table 1: Comparative Performance of Molecular Detection Methods Across Sample Types
| Sample Type | Method | Key Performance Findings | Reference |
|---|---|---|---|
| Extracted RNA | RT-LAMP vs. RT-qPCR | Sensitivity comparable to RT-qPCR; 100% specificity reported in multiple studies. [20] [19] | |
| Direct Swabs | RT-LAMP vs. RT-qPCR | Lower sensitivity (71%) for RT-LAMP compared to RT-qPCR; requires optimized protocols. [19] | |
| Nasopharyngeal Swabs | RT-LAMP | Diagnostic sensitivity of 97.4% for samples with Ct ≤33; 100% for high viral loads (Ct ≤25). [37] | |
| Saliva | RT-LAMP vs. RT-qPCR | 93% agreement with RT-qPCR (Cohen’s kappa); viable alternative with simpler collection. [20] | |
| Stool/Feces | RT-LAMP vs. rRT-PCR | Overall diagnostic sensitivity of 62% (Ct ≤40); 100% sensitivity for high viral loads (Ct ≤25). [37] |
Detailed Experimental Protocols
To ensure reproducibility and provide context for the performance data, this section outlines the key experimental methodologies cited in the comparison.
Protocol: SARS-CoV-2 Detection in Extracted RNA via RT-LAMP and RT-qPCR
A 2024 study directly compared one-step real-time RT-PCR and one-step RT-LAMP using 342 clinical samples (nasopharyngeal and saliva). [20]
- Sample Preparation: Nasopharyngeal and saliva samples were collected in Viral Transport Medium (VTM). RNA was extracted using a commercial SARS-CoV-2 RNA extraction kit. The process involved lysis, binding to a filter membrane, washing, and elution in a final volume of 100 µl. RNA purity and quantity were measured via nanodrop. [20]
- One-Step RT-qPCR: Reactions used a 20 µl volume with 5 µl of RNA template and master mix targeting the N gene (HEX channel) and RNase P as an internal control (ROX channel). Cycling conditions were: 50°C for 20 min; 95°C for 3 min; 45 cycles of 95°C for 15s and 55°C for 40s. [20]
- One-Step RT-LAMP: Primers targeted the N gene of SARS-CoV-2. Reactions used a 25 µl mixture containing 5 µl of RNA template, specific primer concentrations (40 pmol internal primers, 20 pmol loop primers, 5 pmol external primers), and Bst DNA/RNA Polymerase. Incubation was performed at 65°C for 45-60 minutes. [20]
Protocol: SARS-CoV-2 Detection in Direct Swab Samples
A 2023 study highlighted the challenge of using direct swabs without RNA extraction for RT-LAMP. [19]
- Sample Preparation: Nasopharyngeal and oropharyngeal swab samples were suspended in VTM. For "direct" assays, these swab samples were used without prior RNA extraction. [19]
- RT-LAMP Assay: The RT-LAMP method utilized a primer set targeting the ORF1a gene. The optimal incubation time was determined to be 45 minutes at 65°C. Results were read using fluorescence, agarose gel electrophoresis, and visual color change. [19]
- Comparison Method: A commercial RT-qPCR kit was used as the reference standard. The study found that while RT-LAMP was highly sensitive with extracted RNA, its sensitivity dropped to 71% when applied to direct swab samples. [19]
Protocol: SARS-CoV-2 Detection in Animal Feces via RT-LAMP
A 2025 study validated a commercial, colorimetric RT-LAMP assay for detecting SARS-CoV-2 in animal feces, a complex sample matrix. [37]
- Sample Type: Clinical fecal samples from various animal species.
- Comparator Assay: Real-time RT-PCR (rRT-PCR).
- RT-LAMP Assay: A pH-based, colorimetric RT-LAMP assay was used. The assay was robust across incubation lengths of 30-45 min and temperatures of 60-70°C.
- Key Findings: The assay showed 100% sensitivity for samples with high viral loads (rRT-PCR Ct ≤ 25) and 62% overall sensitivity (Ct ≤ 40). The limit of detection was determined to be 72 genome copies per reaction. [37]
Workflow and Method Selection
The following diagram illustrates the logical decision-making process for selecting a sample preparation and detection pathway based on research objectives and constraints.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of the described protocols relies on specific reagents and materials. The following table details essential solutions for this field of research.
Table 2: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Example from Protocols |
|---|---|---|
| Viral Transport Medium (VTM) | Preserves virus viability and nucleic acids during sample transport. | Used for collecting and transporting nasopharyngeal and oropharyngeal swabs. [20] [19] |
| Commercial RNA Extraction Kit | Purifies and concentrates viral RNA from complex sample matrices; critical for sensitivity. | Used in all protocols involving extracted RNA to isolate viral RNA from swabs, saliva, or stool. [20] [37] |
| Bst DNA/RNA Polymerase | The strand-displacing polymerase enzyme essential for the isothermal amplification in RT-LAMP. | A key component of the RT-LAMP master mix. [20] |
| LAMP Primers (Sets of 6) | Specifically designed primers (F3, B3, FIP, BIP, LF, LB) that recognize multiple target regions for highly specific amplification. | Designed to target genes such as N or ORF1a of SARS-CoV-2. [20] [38] |
| pH-Sensitive Dye (e.g., Phenol Red) | Allows visual, colorimetric readout of RT-LAMP results; proton release during amplification causes color change. | Enables naked-eye interpretation of results, turning from pink (negative) to yellow (positive). [39] [37] |
The choice between sample preparation methods and molecular diagnostic techniques involves significant trade-offs. RT-qPCR remains the gold standard for sensitivity, particularly for samples with low viral loads or complex matrices like stool. [37] [30] However, RT-LAMP presents a compelling alternative when rapid results, minimal equipment, and cost are primary concerns, especially in settings where high viral load screening is the goal. [9] [20] The key to maximizing sensitivity across all methods lies in the consistent use of robust nucleic acid extraction protocols, particularly when dealing with direct swabs or stool samples where inhibitors are present. Researchers must align their choice of sample preparation and detection methodology with the specific requirements of their diagnostic or research application.
Primer Design Strategies for SARS-CoV-2, Entamoeba histolytica, and Bacterial Resistance Genes
Rapid and precise pathogen detection is a cornerstone of effective public health management, clinical diagnostics, and antimicrobial stewardship. The performance of any molecular diagnostic assay hinges critically on the strategic design of primers that ensure both high sensitivity and specificity. This guide objectively compares the experimental performance of three prominent amplification techniques—Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and Real-Time PCR (RT-PCR or qPCR)—across different pathogen targets. Framed within a broader thesis on sensitivity comparisons, this analysis provides researchers, scientists, and drug development professionals with a structured overview of primer design considerations and supporting experimental data to inform assay selection and development.
Primer Design Fundamentals and Target Selection
Effective primer design begins with the careful selection of a target gene, which must be both unique to the pathogen and functionally critical to avoid genetic drift. For SARS-CoV-2, the primary targets are located in highly conserved regions such as the RNA-dependent RNA polymerase (RdRp) gene within the open reading frame ORF1ab, the Envelope (E) gene, and the Nucleocapsid (N) gene [40]. These regions are preferred for their specificity within the sarbecovirus subgenus. For Entamoeba histolytica, the Serine-rich E. histolytica protein (SREHP) gene is a proven target for designing highly specific primers that can differentiate it from other non-pathogenic Entamoeba species [5] [1]. For bacterial resistance genes, the target depends on the mechanism of resistance, such as beta-lactamase genes (e.g., blaCTX-M, blaNDM), carbapenemases, or vancomycin resistance genes (e.g., vanA, vanB).
A pivotal consideration in viral primer design, especially for RNA viruses like SARS-CoV-2, is the high potential for mutation and recombination. Once virus mutation and recombination occur, it can be difficult to effectively diagnose viral infection with existing primers [40]. Therefore, bioinformatic analysis to confirm target region conservation across a wide array of circulating strains is essential to maintain assay robustness over time.
Comparative Assay Performance: Experimental Data
Direct comparisons of LAMP, nPCR, and RT-PCR reveal distinct differences in sensitivity, speed, and operational complexity. The table below summarizes key experimental findings from the literature for the pathogens in scope.
Table 1: Comparative Performance of LAMP, nPCR, and RT-PCR Assays
| Pathogen / Target Gene | Assay Type | Limit of Detection (LoD) | Amplification Time/Temp | Key Comparative Findings | Source Study |
|---|---|---|---|---|---|
| Entamoeba histolytica (SREHP gene) | LAMP | 1 trophozoite | 60 min / ~63°C | Most sensitive; 100% specificity; visual detection possible. | [5] [1] |
| nPCR | 100 trophozoites | >2 hours / multi-cycling | 100x less sensitive than LAMP. | [5] [1] | |
| RT-PCR (qPCR) | 100 trophozoites | 1-2 hours / multi-cycling | Similar LoD to nPCR; requires costly equipment. | [5] [1] | |
| SARS-CoV-2 (ORF1a gene) | RT-LAMP | Comparable to RT-qPCR (in extracted RNA) | 45 min / ~65°C | Simpler, faster, cost-effective; lower sensitivity (71%) in direct swabs. | [19] |
| RT-qPCR | Gold Standard | 1.5-3 hours / multi-cycling | High sensitivity; requires complex equipment and expert staff. | [40] [19] | |
| Alternaria solani (HK gene) | LAMP | 100 fg (genomic DNA) | 60 min / 63°C | 10x more sensitive than conventional PCR. | [27] |
| nPCR | 10 fg (genomic DNA) | >2 hours / multi-cycling | 100x more sensitive than LAMP. | [27] | |
| RT-PCR (qPCR) | 1 fg (genomic DNA) | 1-2 hours / multi-cycling | Most sensitive; 10x more sensitive than nPCR. | [27] |
The data demonstrates that no single technique is universally superior. The choice depends on the primary requirement: LAMP offers exceptional speed and simplicity for point-of-care applications, nPCR provides high sensitivity for low-target detection in controlled labs, and RT-PCR balances reliable quantification with high throughput.
Detailed Experimental Protocols
- Primer Design: A set of six primers (two outer, two inner, and two loop primers) was designed targeting eight distinct regions of the SREHP gene using software like Primer Explorer V4.
- Reaction Composition: The 25 µL reaction mixture typically contains 1.6 µM each of FIP and BIP primers, 0.2 µM each of F3 and B3 primers, 1.4 mM dNTPs, 0.8 M betaine, 20 mM Tris-HCl (pH 8.8), 10 mM KCl, 10 mM (NH4)2SO4, 8 mM MgSO4, 0.1% Tween 20, and 8 U of Bst DNA polymerase large fragment.
- Amplification Conditions: The reaction is carried out at a constant temperature of 63°C for 60 minutes, followed by an enzyme inactivation step at 80°C for 5 minutes.
- Product Detection: Amplicons can be detected via agarose gel electrophoresis (showing a ladder-like pattern), visual inspection using colorimetric dyes like calcein-manganese (change from orange to green), or a nucleic acid lateral flow immunoassay (LFD).
- Primer Design: Two pairs of primers (outer and inner) are designed to bind sequentially to the histidine kinase (HK) gene.
- First Round PCR: The reaction uses the outer primer pair. A typical 25 µL reaction includes standard PCR components. The thermocycling profile consists of an initial denaturation at 95°C for 3 min, followed by 26 cycles of denaturation (95°C for 1 min), annealing (58°C for 1 min), and extension (72°C for 1 min), with a final extension at 72°C for 5 min.
- Second Round PCR: Approximately 1 µL of the first-round product is used as a template in a new reaction with the inner primer pair. The thermocycling conditions are identical to the first round.
- Product Detection: The final amplicon is analyzed on an agarose gel.
- Primer and Probe Design: Primers and TaqMan probes are designed for conserved regions like ORF1ab, N, or E genes. The probe is dual-labeled with a fluorescent reporter (e.g., FAM) at the 5' end and a quencher (e.g., BHQ1) at the 3' end.
- Reaction Composition: The reaction mix includes sequence-specific primers, the TaqMan probe, dNTPs, MgCl2, a buffer, a reverse transcriptase enzyme, and a hot-start DNA polymerase.
- Amplification and Detection: The one-step RT-qPCR is performed on a real-time PCR instrument. The protocol involves a reverse transcription step (e.g., 50°C for 15 min), initial denaturation (95°C for 5 min), followed by 45 cycles of denaturation (95°C for 15 sec) and annealing/extension (e.g., 60°C for 1 min). Fluorescence is measured at the end of each cycle.
The following workflow diagram illustrates the key steps and decision points in selecting and optimizing a molecular detection assay.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for developing and executing these molecular assays.
Table 2: Essential Reagents and Materials for Molecular Detection Assays
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| Bst DNA Polymerase (Large Fragment) | Isothermal amplification engine for LAMP | Strand-displacing activity; works optimally at 60-65°C; lacks 5'→3' exonuclease activity. |
| Taq DNA Polymerase | PCR amplification for nPCR and RT-qPCR | Thermostable; 5'→3' polymerase activity; used with conventional and real-time PCR. |
| Reverse Transcriptase (e.g., M-MuLV) | Converts RNA to cDNA for RT-based assays | Essential for detecting RNA viruses like SARS-CoV-2 in RT-LAMP and RT-qPCR. |
| dNTP Mix | Building blocks for DNA synthesis | Solution of deoxyadenosine, deoxyguanosine, deoxycytidine, and deoxythymidine triphosphates. |
| SYBR Green or TaqMan Probes | Detection of amplified products in qPCR | SYBR Green binds dsDNA; TaqMan probes provide higher specificity via fluorogenic hydrolysis. |
| Betaine | Additive for LAMP and PCR | Reduces secondary structure in DNA; improves amplification efficiency and specificity. |
| Hot-Start Taq Polymerase | Reduces non-specific amplification in PCR | Enzyme remains inactive until a high-temperature activation step improves assay specificity. |
| Nucleic Acid Lateral Flow Dipstick (LFD) | Visual detection of LAMP and RPA products | Provides a simple, equipment-free readout; often uses biotin- and FITC-labelled primers. |
The strategic design of primers and the selection of an appropriate amplification platform are critical for successful pathogen detection. LAMP, nPCR, and RT-PCR each occupy a unique niche in the molecular diagnostics ecosystem. LAMP is unparalleled for rapid, sensitive, and field-deployable diagnostics. nPCR remains a powerful, highly sensitive laboratory technique for challenging targets where equipment is limited. RT-qPCR is the robust gold standard for quantitative, high-throughput applications in centralized laboratories. The optimal choice is not a function of raw performance alone but must be guided by the specific diagnostic context, including the target pathogen, required sensitivity, available infrastructure, and intended use case. This comparative guide provides a foundation for researchers to make an informed decision.
Loop-mediated isothermal amplification (LAMP) represents a significant advancement in nucleic acid amplification technology, offering a rapid, sensitive, and specific alternative to traditional PCR-based methods in diagnostic and research applications. First described by Notomi et al. in 2000, LAMP utilizes a DNA polymerase with high strand displacement activity and 4-6 specially designed primers that recognize 6-8 distinct regions of the target DNA [41]. This unique priming mechanism enables auto-cycling amplification under isothermal conditions, typically between 60-65°C, eliminating the need for sophisticated thermal cyclers [19]. The method produces long DNA concatemers (>20 kb) consisting of numerous repeats of the target sequence, connected with single-stranded loop regions [41]. These extensive amplification products enable various detection modalities, including real-time fluorescence, colorimetric assessment, turbidity measurement, lateral flow detection, and agarose gel electrophoresis [41].
This protocol focuses specifically on colorimetric detection and turbidity monitoring, two of the most accessible and practical detection methods for LAMP assays. The colorimetric method leverages pH-sensitive dyes that detect the slight acidification of the reaction mixture resulting from amplification, while turbidity monitoring detects the precipitation of magnesium pyrophosphate, a byproduct of DNA synthesis [41]. Both methods enable visual detection without specialized equipment, making LAMP particularly valuable for point-of-care testing, field applications, and resource-limited settings [42] [41]. When properly optimized, LAMP assays can detect target nucleic acids with sensitivity comparable to, and in some cases exceeding, traditional PCR methods [5] [1].
Comparative Performance: LAMP Versus PCR-Based Methods
Extensive comparative studies have demonstrated that LAMP assays frequently outperform conventional PCR in terms of sensitivity while matching the performance of more advanced PCR methods in many applications. The technique's exceptional sensitivity stems from its high amplification efficiency, which allows detection of very low copy numbers of target nucleic acids.
Table 1: Comparison of Detection Limits Between LAMP and PCR Methods Across Various Pathogens
| Pathogen/Application | LAMP Detection Limit | Conventional PCR Detection Limit | nested PCR Detection Limit | Real-time PCR Detection Limit | Citation |
|---|---|---|---|---|---|
| Entamoeba histolytica | 1 trophozoite equivalent | 1,000 trophozoite equivalents | 100 trophozoite equivalents | 100 trophozoite equivalents | [5] [1] |
| Alternaria solani (fungal pathogen) | 10 pg/μL genomic DNA | 100 pg/μL genomic DNA | 1 pg/μL genomic DNA | 0.1 pg/μL genomic DNA | [27] |
| SARS-CoV-2 | 6.7 copies/reaction (RT-LAMP) | Not tested | Not tested | Comparable to RT-LAMP in extracted RNA | [7] [19] |
| Human Cytomegalovirus (hCMV) | 39.09 copies/reaction (95% confidence) | Not tested | Not tested | Established as gold standard | [43] |
| Haemophilus influenzae type b (Hib) | 10 copies of purified DNA | >1,000 copies (conventional PCR) | >1,000 copies (nested PCR) | Not tested | [44] |
The data consistently demonstrate LAMP's superior sensitivity compared to conventional PCR, with 10 to 1000-fold improvements in detection limits across various applications [5] [44] [1]. While nested PCR and real-time PCR may show similar or slightly better sensitivity in some cases [27], LAMP achieves this performance with considerably simpler instrumentation and faster turnaround times. For SARS-CoV-2 detection, multiple studies have confirmed that RT-LAMP provides comparable diagnostic accuracy to RT-qPCR, particularly during the acute symptomatic phase of infection (up to 9 days after symptom onset) [7]. The technique maintains 100% sensitivity and specificity during this period when compared with RT-qPCR as the gold standard [7].
LAMP Primer Design and Mechanism
Primer Design Strategy
The exceptional specificity of LAMP assays derives from the requirement for multiple primers targeting distinct regions of the target DNA. A complete LAMP primer set typically includes:
- F3 and B3 (Outer Primers): These facilitate the initial strand displacement steps.
- FIP and BIP (Inner Primers): These contain complementary sequences that form loop structures and drive the cyclic amplification.
- LF and LB (Loop Primers): These optional but recommended primers accelerate reaction kinetics by binding to loop regions [41].
Primer design represents a critical step in LAMP assay development. The NEB LAMP Primer Design Tool provides specialized software for creating effective primer sets that target 6-8 distinct regions of the desired sequence [41]. For the SARS-CoV-2 N gene, successful primers have been designed with F3 (18nt), B3 (20nt), FIP (F1c=18nt, F2=19nt), BIP (B1c=21nt, B2=20nt), LF (21nt), and LB (20nt) [20]. Similar strategies have been employed for various pathogens, including Entamoeba histolytica targeting the SREHP gene [1] and Alternaria solani targeting the histidine kinase gene [27].
LAMP Mechanism and Amplification Process
The following diagram illustrates the LAMP primer binding mechanism and amplification process:
LAMP amplification initiates when the F3 primer binds to its target and initiates strand displacement DNA synthesis, releasing a single strand that serves as a template for subsequent priming events. The inner primers (FIP and BIP) then bind to their complementary regions on the displaced strand, leading to the formation of loop structures that enable cyclic amplification [41]. The addition of loop primers (LF and LB) can reduce reaction times by approximately half by binding to the loop regions that form during amplification [41]. This process generates long DNA concatemers containing multiple repeats of the target sequence, which form the basis for various detection methods.
Materials and Reagents
Essential Research Reagent Solutions
Table 2: Key Reagents for LAMP Assays
| Reagent/Component | Function/Purpose | Examples/Specifications |
|---|---|---|
| Bst DNA Polymerase | Strand-displacing DNA synthesis | Bst 2.0 WarmStart, Bst-XT WarmStart (NEB) [41] |
| Reaction Buffer | Optimal pH and salt conditions | Typically includes MgSO₄, KCl, (NH₄)₂SO₄, Triton X-100 |
| dNTPs | DNA synthesis building blocks | 1.4 mM final concentration typically recommended |
| Primer Set | Target-specific recognition | F3, B3, FIP, BIP (LF, LB optional but recommended) [41] |
| Colorimetric Dye | Visual pH detection | Phenol red, hydroxynaphthol blue [41] |
| Calcein-Manganese Dye | Alternative visual detection | Fluorescence/color change upon amplification [5] |
| Magnesium Sulfate | Co-factor for polymerase | Concentration optimized for turbidity detection |
| Betaine | Strand separation facilitator | Enhances specificity and efficiency [1] |
For colorimetric LAMP, specialized master mixes such as the WarmStart 2X Colorimetric LAMP Master Mix (NEB) provide pre-optimized conditions with pH-sensitive dyes that change from pink to yellow upon amplification [41]. An updated version including dUTP and UDG is available for carryover prevention between amplification rounds. For turbidity-based detection, the reaction composition remains similar, but the magnesium concentration may be optimized to enhance pyrophosphate precipitation.
Step-by-Step LAMP Protocol
Reaction Setup
Prepare Reaction Mixture:
Positive and Negative Controls:
- Include a known positive control template
- Include a no-template negative control to detect contamination
- For colorimetric detection, a no-amplification control (held at room temperature) helps visualize the color change
Incubation Conditions:
- Incubate reactions at 63-65°C for 30-60 minutes
- For turbidity monitoring, use a real-time turbidimeter with continuous monitoring at 400 nm [44]
- For colorimetric detection, observe color change visually or using a spectrophotometer
Reaction Termination:
- Heat inactivation at 80°C for 5-10 minutes is optional
- For colorimetric reactions, results remain stable for several hours
Detection Methods
Colorimetric Detection
Colorimetric LAMP detection utilizes pH-sensitive dyes that respond to the slight acidification of the reaction mixture during DNA amplification. As dNTPs are incorporated into DNA, the release of pyrophosphate protons gradually lowers the pH [41]. The WarmStart Colorimetric LAMP Master Mix contains a proprietary formulation that changes from pink to yellow upon successful amplification [41]. This color change can be visualized with the naked eye, eliminating the need for specialized equipment. Alternative colorimetric approaches include the use of leuco triphenylmethane dyes such as leuco crystal violet (LCV), which changes from colorless to violet upon contact with double-stranded DNA amplification products [42]. The calcein-manganese complex provides another visual detection method, where the green fluorescence becomes visible after amplification [5].
Turbidity Monitoring
Turbidity detection measures the white precipitate of magnesium pyrophosphate that forms as a byproduct of DNA synthesis [44] [41]. Real-time turbidimeters such as the Loopamp Real-time Turbidimeter (LA-200; Eiken Chemical) can monitor this precipitation at 400 nm, providing both quantitative and qualitative assessment of amplification [44]. The turbidity method enables real-time monitoring of reaction progress and can determine amplification kinetics. Studies have demonstrated effective turbidity monitoring for various pathogens, including Haemophilus influenzae type b, with detection limits as low as 10 copies of purified DNA [44].
The following workflow illustrates the complete LAMP process from setup to detection:
Troubleshooting and Optimization
Common Issues and Solutions
- Non-specific Amplification: Redesign primers to improve specificity; optimize Mg²⁺ concentration; include betaine (0.6-1.2 M) to enhance specificity [1]
- Weak or No Amplification: Check primer quality and concentration; optimize reaction temperature (60-67°C range); template quality assessment; increase Bst polymerase concentration
- Inconsistent Color Change: Ensure fresh preparation of colorimetric master mix; check pH of reaction components; include appropriate positive controls
- High Background in Turbidity Measurements: Optimize magnesium concentration; ensure proper mixing of reagents; check for precipitate in negative controls
Sensitivity Optimization
To achieve the maximum sensitivity demonstrated in comparative studies (Table 1), several optimization strategies can be employed:
- Primer Ratios: Systematically vary inner to outer primer ratios (typically 8:1 to 16:1 for inner:outer primers)
- Magnesium Concentration: Titrate MgSO₄ between 4-8 mM for optimal results
- Reaction Time: Extend incubation to 60-90 minutes for low-copy targets
- Template Quality: Implement sample preparation methods that remove inhibitors while preserving target nucleic acids
The LAMP methodology, particularly with colorimetric detection and turbidity monitoring, provides a robust, sensitive, and accessible platform for nucleic acid detection across diverse applications. The technique has been successfully implemented for diagnostic purposes in human medicine [5] [44] [7], plant pathology [27], and food safety testing. Its performance characteristics make it particularly valuable in settings where rapid results, minimal equipment requirements, and high sensitivity are prioritized.
When compared to PCR-based methods, LAMP consistently demonstrates equivalent or superior sensitivity to conventional PCR, with the significant advantages of isothermal amplification and simple detection modalities [5] [1] [27]. While nested PCR and real-time PCR may offer slightly better sensitivity in some applications [27], this advantage must be balanced against their greater complexity, equipment requirements, and time to result. The step-by-step protocol presented here provides researchers with a comprehensive framework for implementing LAMP with colorimetric detection and turbidity monitoring, enabling sensitive nucleic acid detection across diverse research and diagnostic applications.
In molecular diagnostics and research, nucleic acid amplification tests (NAATs) are fundamental tools for detecting pathogens and analyzing genetic material. Nested PCR (nPCR) is a powerful two-step amplification technique that significantly enhances sensitivity and specificity by using two sets of primers in sequential reactions. The first PCR round amplifies the target region with outer primers, followed by a second round using inner primers that bind within the first amplicon. This nested approach provides exceptional detection capability for low-abundance targets but introduces substantial risk of amplicon contamination—where PCR products from previous reactions contaminate subsequent setups, leading to false-positive results [45] [46].
The contamination challenge is particularly acute in two-step workflows because the high concentration of amplification products from the first round can easily aerosolize or transfer during the tube-opening process required for the second round. Even minute quantities of contaminating amplicons can serve as efficient templates in subsequent amplifications, compromising experimental integrity [46]. This article examines contamination prevention strategies specifically for nPCR workflows while contextualizing nPCR performance against alternative amplification methods, including reverse transcription polymerase chain reaction (RT-PCR) and loop-mediated isothermal amplification (LAMP), within a broader sensitivity comparison framework.
Performance Comparison of Amplification Methodologies
Diagnostic Sensitivity and Specificity
The analytical performance of amplification techniques varies significantly based on methodology, target sequence, and implementation context. nPCR traditionally offers superior sensitivity compared to single-round PCR due to its two-stage amplification process, but this comes with increased contamination risk. When compared with isothermal alternatives like LAMP, each method demonstrates distinct advantages depending on the application requirements.
Table 1: Comparative Performance of Nucleic Acid Amplification Techniques
| Method | Theoretical Sensitivity | Clinical Sensitivity (COVID-19) | Specificity | Time to Result | Contamination Risk |
|---|---|---|---|---|---|
| nPCR | Very High (1-10 copies) | Not Fully Characterized for SARS-CoV-2 | High (with proper contamination control) | 2-4 hours | Very High |
| RT-PCR | High (10-100 copies) | Gold Standard | High (>95%) | 1.5-2 hours | Moderate |
| RT-LAMP | High (10-100 copies) | 92.91% (RNA-LAMP, vs. RT-PCR) [47] | 98.33% (RNA-LAMP) [47] | 30-60 minutes | Moderate |
| Direct LAMP | Moderate | 70.92% (vs. RT-PCR) [47] | 99.86% [47] | 30-60 minutes | Lower |
Clinical performance data reveals that RT-LAMP demonstrates excellent diagnostic accuracy during the acute phase of infection. One study found RT-LAMP maintained 100% sensitivity and specificity compared to RT-qPCR until the 9th day after symptom onset, though its sensitivity decreased substantially beyond this point [7]. This positions LAMP as a valuable alternative to nPCR when working with samples containing high viral loads during early infection stages.
Operational Characteristics and Implementation Considerations
Beyond pure sensitivity metrics, operational characteristics significantly influence method selection for specific laboratory environments.
Table 2: Operational Comparison of Amplification Methods
| Parameter | nPCR | RT-PCR | RT-LAMP |
|---|---|---|---|
| Equipment Requirements | Thermal cycler, post-PCR separation | Real-time thermal cycler | Isothermal block, simple heating device |
| Technical Expertise | Advanced (high contamination risk management) | Intermediate | Basic to Intermediate |
| Cost per Test | Moderate | High | Low to Moderate |
| Throughput Capacity | Moderate | High | High |
| Suitability for Point-of-Care | Low | Low | High |
| Resistance to Inhibitors | Moderate (dilution effect in second round) | Moderate | High |
The data indicates that LAMP technology offers significant operational advantages in resource-limited settings or high-throughput scenarios. Its isothermal nature eliminates the need for expensive thermal cyclers, and the rapid turnaround time (30-60 minutes) enhances workflow efficiency [20] [47]. One study noted that "RT-LAMP has been shown to have high sensitivity and specificity, comparable to RT-PCR while being more cost-effective and easier to implement in resource-limited settings" [9] [23].
Contamination Prevention in nPCR Workflows
Understanding Contamination Risks
In nPCR workflows, carry-over contamination represents the most significant challenge, occurring when amplicons from previous reactions are introduced into new reaction mixtures. A typical PCR generates approximately 10⁹ copies of target sequence, and aerosolized droplets can contain as many as 10⁶ amplification products [46]. These contaminants can permeate laboratory environments, contaminating reagents, equipment, and ventilation systems if uncontrolled. The consequences include false positive results, reduced test sensitivity, and compromised research integrity [48] [46] [49].
The two-step nature of nPCR creates multiple vulnerability points:
- Tube opening after the first amplification round
- Reaction transfer between primary and secondary reactions
- Post-amplification analysis of the final product Effective contamination control requires both preventive strategies to avoid contamination incidents and sterilization methods to render any potential contaminants unable to amplify.
Strategic Laboratory Design and Workflow
A foundational approach to preventing nPCR contamination involves physical separation of laboratory areas and establishing unidirectional workflow patterns.
Diagram 1: Unidirectional nPCR Laboratory Workflow
The laboratory should maintain strict physical separation between pre-amplification and post-amplification areas, with dedicated equipment and consumables for each zone [46] [49]. Movement between areas should follow a unidirectional path from clean to contaminated zones, with personnel changing gloves and lab coats when moving between areas. Ideally, technologists who have worked in post-PCR areas should not re-enter pre-PCR areas on the same day [49].
The K-Box Method: A Novel Contamination Prevention System
A sophisticated approach specifically designed for two-step PCR workflows is the K-box method, which incorporates specialized sequence elements into primer design to prevent and identify carry-over contamination [45].
Diagram 2: K-Box Contamination Prevention Mechanism
The K-box architecture incorporates three synergistic sequence elements into first-round amplification primers:
- K1 elements (typically 7 nucleotides) enable suppression of carry-over contamination through sample-specific sequences that must match between first and second-round primers for successful amplification [45].
- K2 elements (typically 3 nucleotides) facilitate detection of possible residual contaminations in subsequent bioinformatics analysis by providing a sample-specific identifier sequence [45].
- S elements (separators, typically 2 nucleotides) prevent amplification bias by creating a mismatch with the template DNA, effectively separating the template-matching part of the primers from their 5' tail [45].
This method establishes a system where each sample receives a unique "set" defined by a specific K/K' combination. Second-round primers containing only K1 elements will only efficiently amplify products from first-round reactions with matching K1 sequences. Contaminating amplicons from non-matching sets cannot amplify, thereby preventing false positives. Experimental validation demonstrated that the K-box method "effectively blocked" spike-in contaminations "even at high rates" [45].
Additional Technical Contamination Control Methods
Enzymatic Decontamination with Uracil-N-Glycosylase (UNG)
The UNG decontamination system incorporates dUTP instead of dTTP during amplification, generating uracil-containing amplicons. Subsequent reactions include UNG enzyme, which hydrolyzes any uracil-containing contaminants from previous reactions before amplification begins. The UNG is then inactivated during the initial high-temperature denaturation step, allowing normal amplification of the natural thymine-containing template [46]. This method is widely incorporated into commercial PCR kits and provides robust contamination control, though it may exhibit reduced activity with G+C-rich targets [46].
Chemical Decontamination Methods
Sodium hypochlorite (bleach) at 5-10% concentration effectively degrades DNA through oxidative damage, preventing reamplification of contaminated materials [46] [49]. Work surfaces should be regularly decontaminated with freshly prepared bleach solutions, followed by ethanol or water rinsing to remove residue [50] [49]. UV irradiation (254-300 nm) can also sterilize reaction setups by inducing thymidine dimers in contaminating DNA, though it exhibits reduced efficacy for short (<300 nucleotides) or G+C-rich templates [46].
Procedural Best Practices for nPCR
Implementing rigorous procedural standards is essential for maintaining nPCR integrity:
- Pipetting technique: Use filter tips or positive displacement pipettes to prevent aerosol contamination; avoid splashing when dispensing liquids; centrifuge tubes before opening to prevent aerosol formation [50] [49].
- Reagent management: Prepare master mix aliquots in a clean environment; use dedicated reagents for pre- and post-amplification areas; avoid repeated freeze-thaw cycles [50].
- Control implementation: Include multiple negative controls (no-template controls, extraction controls) to monitor contamination; use positive controls to verify amplification efficiency [48] [49].
- Personal protective equipment: Wear fresh gloves when working in PCR areas; change gloves frequently, especially when moving between different areas or after handling potentially contaminated materials [49].
Experimental Protocols for Method Comparison
nPCR Contamination Control Validation Protocol
To validate the effectiveness of nPCR contamination control measures, implement the following experimental protocol:
Primer Design: Design outer and inner primer sets following standard nPCR principles. For optimal contamination control, incorporate K-box elements into first-round primers as described in Section 3.3 [45].
Laboratory Setup: Establish physically separated work areas for reagent preparation, sample preparation, first PCR setup, second PCR setup, amplification, and product analysis as shown in Diagram 1.
Reaction Setup:
- First Round: Prepare 25μL reactions containing 1X PCR buffer, 2.5mM MgCl₂, 200μM dNTPs (or dUTP for UNG system), 0.4μM outer primers, 1.25U DNA polymerase, and template DNA.
- Cycling Conditions: Initial denaturation 95°C/2min; 25 cycles of 95°C/30s, 55-60°C/30s, 72°C/1min/kb; final extension 72°C/5min.
- Second Round: Transfer 2μL of first-round product to 23μL reaction containing inner primers (with matching K1 elements if using K-box system).
- Cycling Conditions: Initial denaturation 95°C/2min; 30 cycles of 95°C/30s, 55-60°C/30s, 72°C/1min/kb; final extension 72°C/5min.
Contamination Monitoring: Include no-template controls at a ratio of 1:5 samples in both amplification rounds; use spatial separation of samples and controls in the thermal cycler.
Analysis: Separate amplification products by gel electrophoresis; compare test results with controls to identify contamination events.
LAMP Diagnostic Accuracy Assessment Protocol
For comparative performance assessment between nPCR and LAMP, implement the following protocol based on clinical validation studies:
Sample Collection: Collect nasopharyngeal swabs using flocked sterile plastic swab applicators and place in universal viral transport medium [7].
RNA Extraction: Extract total viral RNA using automated nucleic acid extraction systems (e.g., QIAcube) with commercial kits (e.g., QIAamp Viral RNA Mini Kit) according to manufacturer instructions [7].
LAMP Reaction:
- Prepare 25μL reactions containing 15μL reaction mix (commercial RT-LAMP kit) and 10μL purified RNA.
- Include primer sets targeting SARS-CoV-2 genes (e.g., N gene, ORF1ab).
- Incubate at 62.5°C for 35-40 minutes using a real-time turbidimeter or isothermal instrument.
- Monitor amplification kinetics; interpret results based on time-to-positive threshold or endpoint color change for colorimetric versions [47] [7].
Parallel Testing: Test all samples in parallel with reference RT-PCR method targeting the same genes.
Analysis: Calculate sensitivity, specificity, and concordance metrics compared to reference method; analyze performance based on sample collection timing relative to symptom onset [7].
Research Reagent Solutions for nPCR and LAMP Workflows
Table 3: Essential Research Reagents for Amplification Workflows
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp Viral RNA Mini Kit [7], Bioperfectus Nucleic Acid Extraction Rapid Kit [47] | Isolation and purification of target nucleic acids from clinical samples | Automated systems (e.g., QIAcube) enhance reproducibility; magnetic bead methods suitable for high-throughput |
| Amplification Master Mixes | TaqMan Fast Virus 1-Step Master Mix [7], Warmstart RT-LAMP Mastermix [47] | Provides enzymes, buffers, and dNTPs for efficient amplification | RT-LAMP master mixes often include reverse transcriptase and Bst DNA polymerase for isothermal amplification |
| Contamination Control Additives | Uracil-N-Glycosylase (UNG) [46], K-box modified primers [45] | Prevent false positives by degrading contaminants or requiring sequence matching | UNG requires dUTP substitution in amplification; K-box elements require custom primer design |
| Detection Systems | Loopamp Real-time Turbidimeter [7], Colorimetric LAMP dyes [47] | Enable real-time monitoring or visual interpretation of amplification | Turbidimeters detect magnesium pyrophosphate precipitation; colorimetric dyes detect pH shift |
| Positive Controls | SARS-CoV-2 Positive Control RNA [7], Synthetic template with target sequences [45] | Verify assay performance and efficiency | Should be stored in single-use aliquots to prevent contamination |
nPCR remains a powerful amplification methodology offering exceptional sensitivity for challenging applications, but its implementation requires meticulous attention to contamination control in two-step workflows. The K-box method represents a sophisticated primer-based approach that actively prevents carry-over contamination through sequence-specific amplification requirements. When combined with physical laboratory segregation, UNG incorporation, and rigorous procedural standards, nPCR can deliver highly reliable results despite its inherent contamination risks.
Comparative performance analysis indicates that RT-LAMP provides a viable alternative to nPCR in many scenarios, particularly when rapid results, operational simplicity, and reduced contamination risk are prioritized. While nPCR may still offer superior sensitivity for extremely low-abundance targets, LAMP's combination of competitive sensitivity (92.91% for RNA-LAMP vs. RT-PCR [47]), rapid turnaround (30-60 minutes), and minimal equipment requirements positions it favorably for routine diagnostic applications. The selection between these methodologies should be guided by specific application requirements, available resources, and implementation context, with contamination control remaining a paramount consideration in nPCR workflow design.
Real-time PCR (quantitative Polymerase Chain Reaction) represents the gold standard for gene quantification and detection in molecular diagnostics and research applications. This technology detects amplification of a specific genetic sequence after each PCR cycle, enabling both qualitative and quantitative analysis of genetic material [51]. A typical real-time PCR assay includes a combination of oligonucleotides designed to amplify and detect a specific gene target, often consisting of two PCR primers and a fluorescently labeled probe in the case of TaqMan assays [51]. While RT-PCR maintains its position as the benchmark technology, alternative amplification methods have emerged with distinct operational advantages. Loop-mediated isothermal amplification (LAMP) offers rapid DNA amplification under constant temperature conditions, while nested PCR (nPCR) enhances sensitivity and specificity through two successive amplification rounds with two primer sets [1] [25].
The fundamental principle underlying real-time PCR quantification is the consistent exponential-phase amplification that occurs when all reactants—including primers, DNA polymerase, dNTPs—are in excess, fueling consistent efficiency. This consistency means the initial target gene quantity in the PCR reaction directly determines when amplification signal emerges from the baseline, with greater starting target quantities resulting in earlier signal emergence [51]. Understanding this relationship is crucial for proper interpretation of results across different amplification platforms and for selecting the appropriate technology for specific research or diagnostic applications, particularly when comparing established RT-PCR protocols with emerging isothermal methods like LAMP or enhanced specificity methods like nPCR.
Theoretical Foundations of qPCR Curve Analysis and Ct Values
The Amplification Plot and Its Components
The visualization of real-time PCR data occurs through an amplification plot, which graphs fluorescence intensity (ΔRn) against PCR cycle numbers. This plot reveals four distinct phases of the PCR reaction: the ground phase with minimal fluorescence change, the exponential phase with consistent amplification efficiency, the transition phase where efficiency declines due to limiting reactants, and the plateau phase where amplification ceases [52]. In the initial cycles (typically 5-15), the baseline establishes the background fluorescence level, which appears as a flat line in plots with linear vertical axis scales. During these baseline cycles, target amplification may be occurring but has not accumulated sufficient fluorescent signal to be detectable above background noise [51] [53].
The threshold represents a fluorescent value selected within the exponential phase of amplification, from which Ct values are calculated. This threshold should be positioned sufficiently above the baseline to ensure confidence in amplification curve data while remaining within the exponential phase where reaction efficiency remains constant [51] [53]. The amplification curve itself represents the accumulation of DNA templates throughout the PCR experiment, with the plateau phase representing decreased accumulation rates in later cycles as reaction components become limiting [53].
Understanding Threshold Cycle (Ct) Values
The Ct value (threshold cycle), also known as Cq (quantification cycle), is defined as the intersection between an amplification curve and the threshold line, providing a relative measure of target concentration in the PCR reaction [51] [53]. These values are typically not whole numbers and represent fractional cycle numbers where amplification becomes detectable above background. Critically, Ct values are inversely correlated with initial target quantity—lower Ct values indicate higher starting target concentrations, while higher Ct values indicate lower starting amounts [51].
For qualitative applications, such as pathogen detection, the presence or absence of a Ct value determines target detection, with negative results potentially requiring validation through control genes to rule out technical failures in sample collection, extraction, or inhibition [51]. For quantitative applications, reporting Ct values as final results is not recommended, as they represent abstract, incomplete data points whose quantitative interpretation depends on exponential-phase efficiency. The mathematical complexity of Ct values means standard deviation calculations do not behave like typical standard deviations, making quantities derived from Ct values more appropriate for reporting [51].
Table 1: Components of qPCR Amplification Plots and Their Interpretation
| Component | Description | Interpretation Significance |
|---|---|---|
| Baseline | Fluorescence level during initial cycles (5-15) | Establishes background fluorescence; should appear flat in linear plots |
| Exponential Phase | Phase with constant amplification efficiency | Most valuable for quantification; all reactants are in excess |
| Threshold | Fluorescent value set within exponential phase | Used to calculate Ct values; must be above baseline but within exponential phase |
| Ct Value | Cycle where amplification curve crosses threshold | Inverse indicator of starting target quantity; lower Ct = more target |
| Plateau | Phase where amplification rate decreases | Reaction components become limiting; data has diminished quantitative value |
Comparative Analysis of Nucleic Acid Amplification Techniques
Technical Principles and Operational Requirements
The fundamental distinction between RT-PCR, LAMP, and nPCR technologies lies in their amplification mechanisms and operational requirements. RT-PCR requires thermal cycling between different temperatures (denaturation, annealing, extension) and typically uses two primers, with detection occurring through fluorescent probes or DNA-binding dyes [51] [25]. The method provides real-time monitoring of amplification throughout the process, enabling both detection and quantification. Instrumentation requires sophisticated thermal cyclers with fluorescence detection capabilities, and reaction times typically span 1-2 hours depending on the protocol [51].
LAMP technology operates under isothermal conditions (constant temperature, typically 60-65°C) and employs 4-6 primers recognizing 6-8 distinct regions of the target DNA [1] [20]. The reaction proceeds through auto-cycling strand displacement DNA synthesis, eliminating the need for thermal cycling equipment. Detection methods include turbidity (from magnesium pyrophosphate precipitation), colorimetric changes, or fluorescent dyes, often enabling visual interpretation without specialized equipment [1] [25]. Reaction times are generally rapid, often under 30 minutes, making LAMP particularly suitable for point-of-care applications [20].
Nested PCR enhances specificity and sensitivity through two successive amplification rounds using two primer sets. The first round amplifies a larger target region, while the second round uses primers internal to the first amplicon to generate a smaller product [1]. This approach reduces non-specific amplification but increases contamination risk through amplicon carryover and requires more hands-on time than single-tube reactions. The method typically concludes with endpoint detection through gel electrophoresis, lacking the quantitative capabilities of real-time monitoring [1].
Analytical Sensitivity and Performance Comparison
Direct comparative studies demonstrate significant differences in analytical sensitivity between amplification platforms. A comprehensive analysis comparing LAMP, conventional PCR, nPCR, and real-time PCR for detecting Entamoeba histolytica reported a limit of detection (LoD) of a single trophozoite for LAMP across three different detection methods (agarose gel electrophoresis, nucleic acid lateral flow immunoassay, and calcein-manganese dye techniques) [1]. In contrast, nPCR and real-time PCR both demonstrated LoDs of 100 trophozoites, while conventional PCR showed significantly reduced sensitivity with an LoD of 1000 trophozoites [1].
In SARS-CoV-2 diagnostics, RT-LAMP has demonstrated comparable performance to RT-qPCR in some applications, with one study reporting 93% agreement in saliva samples and 94% agreement in nasopharyngeal samples based on Cohen's kappa coefficient (κ) [20]. However, another prospective study evaluating diagnostic performance in healthcare workers found that RT-qPCR using the CDC (USA) protocol was the most accurate diagnostic test among those evaluated, while RT-LAMP showed the lowest sensitivity among RNA-based molecular tests [30]. This performance variation highlights the context-dependent nature of method selection, where sample type, primer design, and implementation environment significantly impact outcomes.
Table 2: Analytical Performance Comparison of Nucleic Acid Amplification Techniques
| Parameter | RT-qPCR | RT-LAMP | nPCR |
|---|---|---|---|
| Limit of Detection (Entamoeba histolytica) | 100 trophozoites [1] | 1 trophozoite [1] | 100 trophozoites [1] |
| SARS-CoV-2 Agreement with RT-qPCR | Gold standard | 93-94% (saliva/nasopharynx) [20] | Not reported |
| Amplification Time | 1-2 hours [51] | <30 minutes [20] | 2-3 hours [1] |
| Quantification Capability | Excellent | Moderate | Poor |
| Multiplexing Potential | High | Limited | Moderate |
Experimental Protocols for Method Comparison
RT-qPCR Protocol for SARS-CoV-2 Detection
The following protocol outlines the one-step RT-qPCR procedure as implemented in comparative studies evaluating SARS-CoV-2 detection methods [20] [30]:
Reaction Setup:
- Prepare a 20μl reaction mixture containing: 5μl RNA template, 9μl resuspended master mix, 2μl of N/ICON Primer & probe mix (HEX/ROX), and 5μl RNase-free water.
- Utilize commercial kits such as the COVID-19 kit (Pishtaz Teb Co., Iran/ PT. COVID.100) or the GoTaq Probe RT-qPCR System Kit (Promega) with manufacturer-specific primer/probe concentrations.
- For the Charité protocol: Use 400nM primers and 150nM probes targeting the E gene and human RNase P as an internal control.
- For the CDC (USA) protocol: Use 500nM primers and 125nM probes targeting N1 and N2 gene fragments.
Thermal Cycling Conditions:
- Reverse transcription: 50°C for 15-20 minutes
- Initial denaturation: 95°C for 2-3 minutes
- Amplification (45 cycles): Denaturation at 95°C for 15 seconds, Annealing/extension at 55-60°C for 40 seconds with fluorescence acquisition.
Data Analysis:
- For the Charité protocol: Samples are considered positive when amplification of both the E gene and RNase P gene occurs at or below cycle threshold 37 and 35, respectively.
- For the CDC protocol: Samples are positive when both N1 and N2 targets amplify at or below Ct 37.
- Calculate PCR efficiency using serial dilutions: Efficiency (%) = (10^(-1/slope) - 1) × 100 [53] [54].
RT-LAMP Protocol for SARS-CoV-2 Detection
The one-step RT-LAMP protocol provides an isothermal alternative for rapid detection [20]:
Primer Design:
- Design LAMP primers targeting conserved regions of the SARS-CoV-2 N gene (NC_045512.2) using Primer Explorer V5 software.
- Prepare a set of 6 primers: external primers F3 (18nt) and B3 (20nt), internal primers FIP (F1c+F2, 37nt total) and BIP (B1c+B2, 41nt total), and loop primers LF (21nt) and LB (20nt).
- Verify specificity using Primer BLAST against relevant databases.
Reaction Setup:
- Prepare a 25μl reaction mixture containing: 5 pmol each of F3 and B3 primers, 40 pmol each of FIP and BIP primers, 20 pmol each of LF and LB primers, 1μl (8U) of Bst DNA/RNA Polymerase 3.0, and appropriate buffer components.
- Add 5μl of RNA template.
Amplification Conditions:
- Incubate at 65°C for 40 minutes using a heating block or water bath.
- No thermal cycling required.
Detection Methods:
- Visual detection via color change with pH-sensitive dyes or turbidity.
- Fluorescent detection using DNA intercalating dyes.
- Lateral flow dipstick detection for hapten-labeled primers.
nPCR Protocol for Enhanced Specificity
The nested PCR protocol provides a highly specific detection method for challenging targets [1]:
First Round Amplification:
- Prepare a conventional PCR reaction mix with outer primer pair (e.g., Eh-F3-SER and Eh-B3-SER for E. histolytica).
- Thermal cycling: Initial denaturation at 95°C for 5 minutes, followed by 30 cycles of 95°C for 30s, appropriate annealing temperature for 30s, 72°C for 30s, with final extension at 72°C for 5 minutes.
Second Round Amplification:
- Use 1-2μl of first-round product as template.
- Prepare PCR reaction with inner primer pair (e.g., primers adapted from F2 region of Eh-FIP-SER and B2 region of Eh-BIP-SER).
- Use similar thermal cycling conditions as first round but with 25-30 cycles.
Product Analysis:
- Analyze amplified products by agarose gel electrophoresis.
- Visualize using UV transillumination after ethidium bromide staining.
- Confirm product size against molecular weight standards.
Essential Research Reagent Solutions
Successful implementation of amplification technologies requires specific reagent systems optimized for each method:
RT-qPCR Reagents:
- Reverse Transcriptase Enzymes: Moloney Murine Leukemia Virus (M-MLV) or avian myeloblastosis virus (AMV) reverse transcriptases for cDNA synthesis.
- Thermostable DNA Polymerases: Taq polymerase with proofreading capability for high-fidelity amplification.
- Fluorescence Detection Systems: Hydrolysis probes (TaqMan), DNA-binding dyes (SYBR Green), or molecular beacons for real-time monitoring.
- Reference Dyes: Passive reference dyes (ROX) for normalization of fluorescence signals.
RT-LAMP Reagents:
- Bst DNA Polymerase: Strand-displacing DNA polymerase with reverse transcriptase activity for one-step RT-LAMP.
- Betaine: Additive to reduce secondary structure in DNA templates and improve amplification efficiency.
- Metal Ions: Magnesium sulfate (6-8mM) as cofactor for polymerase activity.
- Detection Dyes: Hydroxynaphthol blue, calcein, or SYBR Green for visual or fluorescent detection.
nPCR Reagents:
- High-Fidelity Polymerases: Pfu or similar proofreading enzymes to reduce amplification errors in two-round amplification.
- dNTP Mix: Deoxynucleotide triphosphates at optimized concentrations to balance efficiency and fidelity.
- Buffer Systems: Tris-based buffers with potassium chloride and magnesium chloride optimized for each primer set.
Table 3: Essential Research Reagents for Nucleic Acid Amplification Techniques
| Reagent Category | Specific Examples | Function | Technology Application |
|---|---|---|---|
| Polymerase Enzymes | Taq polymerase, Bst polymerase | DNA amplification with thermal stability or strand displacement | All methods |
| Reverse Transcriptase | M-MLV RT, Bst RT variant | RNA to cDNA conversion | RT-qPCR, RT-LAMP |
| Fluorescent Detection | SYBR Green, TaqMan probes | Real-time monitoring of amplification | RT-qPCR |
| Colorimetric Detection | Hydroxynaphthol blue, calcein | Visual detection of amplification | LAMP |
| Primer Systems | Target-specific primers (2-6 per assay) | Specific target recognition | Method-dependent |
| Buffer Components | Betaine, magnesium sulfate, dNTPs | Optimization of reaction conditions | All methods |
Data Analysis and Interpretation Methods
Efficiency Calculation and Validation
PCR efficiency represents a critical parameter determining the accuracy of quantitative results, calculated as the ratio of amplified target DNA molecules at the end of the PCR cycle divided by the number of DNA molecules present at the beginning of PCR [53]. Acceptable efficiency ranges between 85-110%, with deviations potentially indicating issues with template quality, reaction inhibitors, or suboptimal reaction conditions [53].
The standard method for efficiency calculation utilizes serial dilution samples:
- Prepare serial dilutions of known DNA template (e.g., 1/10, 1/100, 1/1000, 1/10000)
- Perform qPCR with technical replicates for each dilution
- Calculate average Ct values for each dilution
- Plot log(10) dilution factor against Ct values
- Determine slope from linear regression
- Calculate efficiency: Efficiency (%) = (10^(-1/slope) - 1) × 100 [53]
Advanced analysis platforms like LinRegPCR implement automated baseline estimation that is user-independent and does not use ground phase measurements, instead employing an iterative approach that determines a baseline value leaving the most data points on a straight line in a log(fluorescence) versus cycle number plot [52]. This method calculates PCR efficiency from the exponential phase of individual reactions rather than standard curves, resulting in improved reproducibility [52].
Quantitative Analysis Methods
For relative quantification, the 2^(-ΔΔCt) method (Livak method) provides a straightforward approach when amplification efficiencies of target and reference genes are approximately equal (90-100%) [51] [53]. This method involves:
- Normalizing target gene Ct values to reference genes: ΔCt = Ct(target) - Ct(reference)
- Comparing experimental and control conditions: ΔΔCt = ΔCt(treatment) - ΔCt(control)
- Calculating expression ratio: Relative Quantity = 2^(-ΔΔCt) [51]
When amplification efficiencies differ between target and reference genes, the Pfaffl method offers a more appropriate alternative by incorporating actual efficiency values into the calculation [53]. For absolute quantification, standard curves with known template concentrations enable copy number determination, essential for applications like viral load testing [53].
Specialized software tools facilitate comprehensive qPCR data analysis:
- LinRegPCR: Provides visualization and analysis of amplification and melting curves, implementing efficiency correction and outlier detection [52]
- qPCRtools: An R package for efficiency calculation, gene expression analysis using multiple methods (2^(-ΔΔCt), standard curve, RqPCR), and statistical analysis [54]
- Commercial Instrument Software: Manufacturer-specific applications for initial data processing and quality assessment
Workflow Visualization and Procedural Integration
The following workflow diagram illustrates the procedural steps and decision points in qPCR data analysis, highlighting critical validation checkpoints:
qPCR Data Analysis Decision Workflow
This workflow outlines the systematic process for analyzing qPCR data, beginning with raw fluorescence data and proceeding through essential processing steps including baseline correction, exponential phase identification, and threshold setting to calculate Ct values [51] [52]. Critical validation checkpoints include efficiency assessment, where reactions outside the 85-110% range should be considered invalid [53], and application-specific method selection for qualitative detection or quantitative analysis [51]. The final interpretation integrates all quality control metrics to ensure result reliability.
The comparative analysis of RT-PCR, LAMP, and nPCR technologies reveals distinct advantages and limitations defining their appropriate application contexts. RT-PCR maintains its position as the gold standard for quantitative gene expression analysis, offering robust quantification, high sensitivity, and extensive validation across diverse applications [51] [30]. The technology's requirement for sophisticated instrumentation and trained personnel, coupled with longer turnaround times, may limit utility in point-of-care or resource-limited settings [9].
LAMP technology demonstrates exceptional potential for rapid diagnostics and field applications, with simplified operational requirements, rapid reaction times, and sensitivity potentially exceeding conventional PCR in some applications [1] [20]. The method's limitations in multiplexing capacity and quantitative accuracy position it as complementary rather than replacement technology for RT-PCR in research settings requiring precise quantification [30].
Nested PCR provides enhanced specificity for challenging targets but suffers from increased contamination risk and limited quantitative capability [1]. The method finds particular utility in detection of low-abundance targets or organisms with complex genetic relationships where specificity is paramount.
Strategic method selection requires careful consideration of research objectives, resource constraints, and required performance parameters. RT-PCR remains the optimal choice for quantitative gene expression studies, while LAMP offers compelling advantages for rapid screening applications, and nPCR provides maximal specificity for detection of low-abundance targets. Understanding the fundamental principles, performance characteristics, and analytical requirements of each platform enables researchers to implement appropriate technologies matching their specific research needs and experimental constraints.
Enhancing Performance: Optimization and Troubleshooting for Maximum Sensitivity
Loop-mediated isothermal amplification (LAMP) has emerged as a powerful molecular diagnostic tool, particularly valuable for point-of-care testing and resource-limited settings. Its performance, however, is critically dependent on the precise optimization of key reaction parameters. This guide provides a comprehensive comparison of LAMP against nested PCR (nPCR) and real-time PCR (RT-PCR), with a specific focus on the experimental optimization of primer concentration, betaine, and magnesium sulfate. Supported by quantitative data and detailed protocols, we demonstrate how systematic optimization of these parameters enhances LAMP sensitivity, making it superior to traditional PCR methods in many diagnostic applications.
Loop-mediated isothermal amplification (LAMP) is a rapid nucleic acid amplification technique that operates at a constant temperature, eliminating the need for thermal cycling equipment required by conventional PCR methods [6]. Since its introduction in 2000, LAMP has gained significant traction in diagnostic applications for infectious diseases, food safety, and environmental monitoring due to its simplicity, speed, and high sensitivity [55]. The technique employs 4-6 primers targeting 6-8 distinct regions of the target DNA, providing exceptional specificity [56]. The reaction proceeds at isothermal conditions (typically 60-65°C) through a strand displacement mechanism, generating amplification yields of up to 10^9 copies within 30-60 minutes [57].
When evaluating diagnostic techniques, sensitivity and specificity are paramount. A 2021 meta-analysis of 23 studies comparing LAMP with PCR and cultivation methods for detecting foodborne pathogens reported pooled sensitivities of 96.6% for LAMP versus 95.6% for PCR, and specificities of 97.6% for LAMP versus 98.7% for PCR, demonstrating comparable performance between the molecular techniques [56]. However, LAMP's distinctive advantage lies in its operational simplicity and robustness to inhibitors commonly found in complex sample matrices [57].
The efficacy of LAMP is profoundly influenced by reaction components, particularly primer concentration, betaine as a destabilizing agent, and magnesium sulfate as a cofactor for both the Bst polymerase and pyrophosphate detection. This guide provides a systematic comparison of optimized LAMP against nPCR and RT-PCR, with detailed experimental data and protocols to assist researchers in implementing this powerful technique.
Comparative Performance: LAMP vs. nPCR vs. RT-PCR
Analytical Sensitivity and Detection Limits
Multiple studies have demonstrated that LAMP frequently outperforms both conventional PCR and nPCR in terms of analytical sensitivity. A comprehensive comparison study targeting the Serine-rich Entamoeba histolytica protein (SREHP) gene reported striking differences in limit of detection (LoD) between the amplification methods.
Table 1: Comparison of Detection Limits for LAMP, nPCR, and qPCR
| Amplification Method | Limit of Detection (LoD) | Amplification Time | Equipment Requirements |
|---|---|---|---|
| LAMP | 1 trophozoite | 30-60 minutes | Isothermal block |
| nPCR | 100 trophozoites | >2 hours | Thermal cycler |
| qPCR | 100 trophozoites | 1-2 hours | Real-time thermal cycler |
| Conventional PCR | 1000 trophozoites | 1-2 hours | Thermal cycler |
Data adapted from a comparative study evaluating Entamoeba histolytica detection [55].
As evidenced in Table 1, LAMP demonstrated a 100-fold greater sensitivity than nPCR and qPCR, detecting a single trophozoite compared to 100 trophozoites for the other methods [55]. This enhanced sensitivity makes LAMP particularly valuable for applications where target abundance is low, such as in early infection diagnosis or environmental monitoring with low pathogen concentrations.
Diagnostic Sensitivity and Specificity in Clinical Applications
The performance of molecular diagnostics is routinely evaluated through clinical sensitivity and specificity metrics. A meta-analysis encompassing 23 studies on foodborne pathogen detection provides robust comparative data:
Table 2: Diagnostic Performance of LAMP vs. PCR for Pathogen Detection
| Performance Metric | LAMP (95% CI) | PCR (95% CI) |
|---|---|---|
| Sensitivity | 96.6% (95.0-97.7%) | 95.6% (91.5-97.8%) |
| Specificity | 97.6% (92.6-99.3%) | 98.7% (96.5-99.5%) |
| Positive Likelihood Ratio | 40.2 | 73.5 |
| Negative Likelihood Ratio | 0.035 | 0.045 |
Data derived from meta-analysis of foodborne pathogen detection methods [56].
While both methods demonstrate excellent diagnostic characteristics, LAMP shows marginally higher sensitivity (96.6% vs. 95.6%), while PCR has slightly superior specificity (98.7% vs. 97.6%) [56]. The clinical significance of these differences depends on the specific application, with LAMP's higher sensitivity being advantageous for screening purposes where false negatives carry substantial consequences.
Tolerance to Amplification Inhibitors
A critical advantage of LAMP in point-of-care applications is its relative tolerance to common amplification inhibitors present in complex biological samples. A systematic evaluation of seven common PCR inhibitors revealed that LAMP generally withstands higher concentrations of these substances:
Table 3: Comparison of LAMP vs. PCR Tolerance to Common Inhibitors
| Inhibitor | Source | Effect on LAMP | Comparative Tolerance |
|---|---|---|---|
| Hematin | Blood components | Fluorescence quenching at high concentrations; reduces amplification products | Comparable or higher |
| Humic Acid | Soil, organic matter | Reduces total amplification products produced | Higher in LAMP |
| Tannic Acid | Plants, food | Fluorescence quenching; reduces amplification products | Higher in LAMP |
| Urea | Urine, feces | Delays amplification but doesn't prevent it | Higher in LAMP |
| Bile Salts | Intestinal contents | Delays onset of amplification | Higher in LAMP |
| IgG | Blood, serum | Delays onset of amplification | Higher in LAMP |
Data summarized from inhibitor evaluation study [57].
The study demonstrated that inhibitors generally delayed the onset of LAMP amplification or quenched fluorescence at similar or higher concentrations compared to PCR, but endpoint detection of LAMP amplicons was often unaffected [57]. This robustness to inhibitors makes LAMP particularly valuable for direct detection from complex samples without extensive nucleic acid purification.
Critical Reaction Components: Experimental Optimization
Primer Concentration Optimization
Primer design and concentration are fundamental to successful LAMP amplification. Unlike PCR, which typically uses two primers, LAMP employs 4-6 primers (F3, B3, FIP, BIP, and optionally LF, LB) recognizing 6-8 distinct regions of the target sequence [56]. This multi-primer system contributes to LAMP's high specificity but also increases the complexity of optimization.
A systematic optimization study for SARS-CoV-2 detection demonstrated that primer concentration significantly impacts time to reaction (TTR). Through design of experiments (DoE) methodology, researchers found that higher primer concentrations (up to the maximum tested) minimized TTR values, with lower concentrations causing increased reaction times [58]. The optimal primer concentrations were determined as 8 μM for outer primers (F3/B3) and 48 μM for inner primers (FIP/BIP) in a Clostridium perfringens detection assay [59].
For SARS-CoV-2 RT-LAMP targeting the N gene, the optimal reaction conditions included:
- 5 pmol each of F3 and B3 external primers
- 40 pmol each of FIP and BIP internal primers
- 20 pmol each of LF and LB loop primers [20]
This asymmetric primer distribution reflects the different roles of primer classes, with inner primers driving the strand displacement amplification and loop primers accelerating reaction kinetics.
Betaine Concentration Effects
Betaine (N,N,N-trimethylglycine) is a crucial additive in LAMP reactions that enhances amplification efficiency by reducing DNA secondary structure formation and stabilizing DNA polymerases. Betaine functions by disrupting base stacking while maintaining base pairing, effectively reducing the melting temperature of DNA without compromising polymerase activity.
In the optimized SARS-CoV-2 colorimetric RT-LAMP assay, betaine concentration was systematically evaluated at different levels, with 400 mM identified as optimal [58]. This concentration provided the best balance between amplification speed and specificity, with lower concentrations reducing amplification efficiency and higher concentrations potentially inhibiting the reaction.
The mechanism of betaine's effect involves equalizing the contribution of AT and GC base pairs to DNA duplex stability, which is particularly beneficial for amplifying GC-rich targets where secondary structures can impede polymerase progression. This property makes betaine especially valuable in LAMP applications where multiple primer binding events must occur simultaneously for efficient amplification.
Magnesium Sulfate Optimization
Magnesium sulfate serves dual critical functions in LAMP reactions: as an essential cofactor for Bst DNA polymerase activity and as a precipitating agent for visual detection. Magnesium ions (Mg²⁺) form complexes with pyrophosphate (PPi), a byproduct of DNA synthesis, generating insoluble magnesium pyrophosphate that increases turbidity for visual detection [60].
Through DoE optimization, 8 mM magnesium sulfate was identified as the optimal concentration for SARS-CoV-2 RT-LAMP [58]. This concentration supported robust polymerase activity while generating sufficient turbidity for detection. The study also revealed that magnesium sulfate concentration exhibited complex interactions with other components:
- Higher concentrations (>8 mM) increased non-specific amplification
- Lower concentrations (<8 mM) reduced amplification efficiency and detection sensitivity
- Magnesium sulfate concentration showed significant interaction effects with betaine and polymerase concentration
For Morganella morganii detection, an optimized LAMP assay utilized the magnesium-pyrophosphate turbidity for endpoint detection measured at 550 nm, demonstrating the utility of this byproduct for quantitative applications [60].
Experimental Protocols for Optimization
DoE Optimization Protocol for Colorimetric RT-LAMP
A comprehensive protocol for optimizing colorimetric RT-LAMP was developed for SARS-CoV-2 detection [58]:
Reaction Setup:
- Prepare a master mix containing:
- 1× isothermal amplification buffer (20 mM Tris-HCl, 10 mM (NH₄)₂SO₄, 50 mM KCl, 2 mM MgSO₄, 0.1% Tween 20)
- 1× primer concentration (as determined optimal)
- 8 mM MgSO₄
- 400 mM betaine
- 1.4 mM dNTPs each
- 0.4 U/μL Bst 2.0 WarmStart DNA polymerase
- 100 μM bromothymol blue pH indicator
- 1.2 mM KOH (for optimal starting pH)
- 8 U M-MLV reverse transcriptase (for RT-LAMP)
Add RNA/DNA template (5-10 μL per 25 μL reaction)
Overlay with mineral oil to prevent evaporation (critical when using heating blocks without lids)
Incubate at 63-67°C for 30-60 minutes
Visualize results by color change from blue to yellow (positive) or remaining blue (negative)
Quality Control Measures:
- Include a pipetting quality control system using dye combinations in the sample solution
- Run no-template controls to monitor contamination
- Use positive controls with known copy number
This optimized protocol achieved a sensitivity of 5 copies per μL, tenfold more sensitive than commercial WarmStart Colorimetric Master Mix [58].
Comparative Sensitivity Evaluation Protocol
To objectively compare LAMP sensitivity with nPCR and RT-PCR, the following protocol was employed [55]:
Sample Preparation:
- Extract DNA from serially diluted Entamoeba histolytica trophozoites (10^0 to 10^5 trophozoites)
- Use identical DNA extracts for all three amplification methods
- Maintain consistent template volume across all reactions
LAMP Assay Conditions:
- Primers: SREHP gene-specific LAMP primers (concentrations not specified)
- Enzyme: Bst DNA polymerase (concentration not specified)
- Temperature: 65°C for 45 minutes
- Detection: Agarose gel electrophoresis, nucleic acid lateral flow immunoassay, and calcein-manganese dye
nPCR Assay Conditions:
- Primary PCR: 30 cycles with outer primers
- Secondary PCR: 30 cycles with inner primers
- Enzyme: Recombinant Taq DNA polymerase
- Detection: Agarose gel electrophoresis
qPCR Assay Conditions:
- Master mix: QuantiFast SYBR Green PCR Kit
- Cycling: Standard qPCR conditions with 40 cycles
- Instrument: CFX96 Touch Real-Time PCR Detection System
Evaluation:
- Determine limit of detection for each method using serial dilutions
- Assess specificity against related microorganisms
- Compare amplification time and hands-on time
This protocol confirmed LAMP's superior sensitivity with detection of a single trophozoite compared to 100 trophozoites for nPCR and qPCR [55].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents for LAMP Optimization and Implementation
| Reagent/Solution | Function | Exemplary Application |
|---|---|---|
| Bst 2.0 WarmStart DNA Polymerase | Strand-displacing DNA polymerase with hot-start capability | SARS-CoV-2 detection [58] |
| Betaine | Destabilizes DNA secondary structures, equalizes AT/GC contribution to TM | Morganella morganii detection [60] |
| Magnesium Sulfate | Essential polymerase cofactor; forms visible precipitate with pyrophosphate | Colorimetric detection [58] |
| dNTP Mixture | Nucleotide substrates for DNA synthesis | Standard component in all LAMP reactions |
| Primer Sets (F3, B3, FIP, BIP, LF, LB) | Recognizes multiple target regions for highly specific amplification | Clostridium perfringens detection [59] |
| pH Indicator Dyes | Visual detection of proton release during amplification | Bromothymol blue in SARS-CoV-2 RT-LAMP [58] |
| Dimethyl Sulfoxide (DMSO) | Resolves secondary structures in GC-rich targets | Morganella morganii detection [60] |
| Guanidine Hydrochloride | Denaturing agent that can enhance amplification efficiency | SARS-CoV-2 RT-LAMP optimization [58] |
The optimization of LAMP reaction components—particularly primer concentration, betaine, and magnesium sulfate—is essential for achieving maximum analytical sensitivity and specificity. The experimental data presented demonstrates that properly optimized LAMP assays can surpass the sensitivity of both nPCR and RT-PCR while offering advantages in speed, simplicity, and tolerance to inhibitors. The systematic optimization protocols and comparative performance data provided in this guide equip researchers with the necessary tools to implement robust LAMP assays across diverse applications, from clinical diagnostics to environmental monitoring. As molecular diagnostics continue to evolve toward point-of-care applications, the optimized LAMP technique represents a powerful alternative to traditional PCR-based methods, particularly in settings where resources are limited or rapid results are critical.
Nested PCR (nPCR) stands as a powerful molecular technique that significantly enhances the sensitivity and specificity of conventional polymerase chain reaction (PCR) assays. This two-stage amplification method employs two sets of primers in sequential reactions to amplify a specific DNA or RNA target, making it particularly valuable for detecting low-abundance pathogens, analyzing genetic mutations, and conducting research where target material is limited [61]. The technique's exceptional sensitivity, often 100-1000 times greater than conventional PCR, has established it as a gold standard in many diagnostic and research applications, including the detection of severe fever with thrombocytopenia syndrome virus (SFTSV) and various fungal pathogens [27] [1].
However, the enhanced sensitivity of nPCR comes with significant technical challenges, primarily contamination control and primer dimer formation. The requirement for physical transfer of first-round amplification products to a second reaction tube dramatically increases the risk of carryover contamination, which can lead to false-positive results and compromised data integrity [1]. Additionally, the use of multiple primer pairs elevates the probability of primer-dimer artifacts, which compete with the target amplification and reduce reaction efficiency [62]. This comprehensive analysis examines these critical challenges while comparing nPCR performance against emerging isothermal amplification technologies, particularly loop-mediated isothermal amplification (LAMP), to provide researchers with strategic approaches for optimizing molecular diagnostic assays.
Understanding nPCR Fundamentals and Technical Challenges
The nPCR Amplification Process
The nPCR technique employs a two-stage amplification process to achieve exceptional specificity and sensitivity. The initial amplification round uses an outer primer pair to generate a primary amplicon, which then serves as the template for a second amplification with inner primers that bind within the first amplicon sequence. This sequential targeting mechanism ensures that only the specific intended product undergoes exponential amplification, significantly reducing non-specific background signals [1]. The process involves carefully optimized thermal cycling parameters for both rounds, with the second round typically utilizing a reduced cycle count to minimize polymerase-induced errors while maintaining high yields.
The fundamental advantage of this approach lies in its verification mechanism. For a product to be amplified in the second round, it must contain binding sites for both the outer and inner primer sets, providing a dual-check system that dramatically increases amplification specificity. This makes nPCR particularly valuable when working with complex samples or when detecting targets with very low initial concentrations, such as in early-stage infections or when analyzing minimal residual disease in oncology applications [61].
Contamination Control in nPCR Workflows
The open-tube transfer step between amplification rounds represents the most significant contamination risk in nPCR protocols. Even microscopic aerosols generated during pipetting can contain sufficient amplicon copies to contaminate subsequent reactions, leading to false-positive results that undermine assay reliability. Research demonstrates that even a single contaminating DNA molecule can amplify exponentially, producing detectable signals that mimic true positive samples [1].
Table 1: Contamination Prevention Strategies for nPCR
| Strategy | Implementation | Efficacy |
|---|---|---|
| Physical Separation | Dedicated rooms/areas for pre- and post-amplification work | Reduces contamination risk by >90% when strictly implemented |
| Uracil-N-Glycosylase (UNG) System | Incorporation of dUTP in first-round products followed by UNG treatment | Effectively degrades >99% of carryover amplicons |
| Closed-Tube Systems | Single-tube nested approaches with physical separation of reagents | Eliminates open-tube transfer but requires specialized formulations |
| Environmental Controls | Regular decontamination (UV irradiation, DNA degradation solutions) | Essential maintenance but variable efficacy depending on implementation |
| Workflow Discipline | Unidirectional workflow with dedicated equipment and supplies | Foundation of all contamination control; requires strict adherence |
Implementing a rigorous contamination control protocol is essential for reliable nPCR results. The most effective approach involves physical separation of pre-amplification and post-amplification work areas, with dedicated equipment, reagents, and personal protective equipment for each zone [1]. The incorporation of uracil-N-glycosylase (UNG) controls, which utilize dUTP incorporation in first-round products followed by enzymatic degradation of carryover contaminants, provides an additional layer of protection. When combined with meticulous laboratory practices and appropriate negative controls, these strategies can effectively mitigate the contamination risks inherent to nPCR methodologies.
Primer Dimer Formation and Impact
Primer dimer artifacts represent another significant challenge in nPCR optimization. These structures form when primers hybridize to each other rather than to the target template, creating short, amplifiable products that compete for reaction components and reduce amplification efficiency. The problem is exacerbated in nPCR due to the presence of multiple primer pairs, increasing the statistical probability of complementary sequences interacting unfavorably [62].
The thermodynamic mechanisms driving primer dimer formation involve transient complementary base pairing, particularly at the 3' ends of oligonucleotides, where even a few complementary nucleotides can initiate polymerase extension. These artifacts are not merely theoretical concerns; studies demonstrate that primer dimers can reduce detection sensitivity by 10-100 fold in extreme cases, particularly when targeting low-abundance sequences where reaction components are limiting [62]. The impact is especially pronounced in quantitative applications, where primer dimers can generate false amplification curves that interfere with accurate quantification of the true target.
Figure 1: nPCR Amplification Pathways: Optimal vs. Problematic Outcomes. The diagram contrasts specific target amplification (left) with common artifacts including primer dimers, amplicon contamination, and hairpin structures (right) that compromise assay performance.
Comparative Performance Analysis of Nucleic Acid Amplification Techniques
Sensitivity and Detection Limits
The exceptional sensitivity of nPCR has been extensively documented across multiple applications. In pathogen detection, nPCR consistently demonstrates 10-1000-fold greater sensitivity compared to conventional PCR, enabling identification of low-level infections that would otherwise escape detection [27] [1]. This enhanced detection capability proves particularly valuable in clinical scenarios where early diagnosis significantly impacts patient outcomes, such as in the detection of SFTS virus during the convalescent phase, where nPCR maintained positive detection up to 40 days post-symptom onset while other methods showed rapidly declining sensitivity [61].
Table 2: Sensitivity Comparison of Amplification Techniques
| Technique | Theoretical Detection Limit | Experimental Evidence | Application Context |
|---|---|---|---|
| nPCR | 10-100 copies | 100-fold more sensitive than conventional PCR; detected 1 log lower than qPCR in convalescent samples [61] | SFTSV detection in human blood; Entamoeba histolytica in stool samples [1] [61] |
| LAMP | 1-100 copies | 10-fold more sensitive than conventional PCR; equivalent to nPCR for E. histolytica detection [1] | SARS-CoV-2 in nasopharyngeal samples; Alternaria solani in plant tissue [27] [63] |
| Conventional PCR | 100-1000 copies | Lower detection limit compared to nPCR and LAMP [1] | General pathogen detection with moderate sensitivity requirements |
| qPCR | 10-100 copies | More sensitive than LAMP for SARS-CoV-2 detection (96% vs 92% sensitivity) [64] | Absolute quantification of viral load; gene expression analysis |
When comparing nPCR to other amplification methods, the sensitivity advantage over conventional PCR is consistent and substantial. However, in comparison with LAMP, the performance appears more application-dependent. For Entamoeba histolytica detection, research demonstrated that LAMP achieved a detection limit of a single trophozoite, outperforming nPCR which detected 100 trophozoites [1]. Conversely, for viral detection in clinical samples, nPCR frequently demonstrates superior sensitivity, particularly in later stages of infection when viral loads decline [61]. This suggests that optimal technique selection must consider both the specific target and the sample matrix.
Specificity and Amplification Efficiency
The two-stage amplification process of nPCR provides exceptional specificity by requiring successful binding of two separate primer pairs to generate a detectable signal. This dual verification mechanism significantly reduces false-positive results from non-specific amplification, making it particularly valuable when working with closely related species or complex background samples [1]. The specificity advantage is most pronounced when compared to single-round amplification methods, where primer mismatch represents a more significant concern.
LAMP achieves its specificity through a different mechanism, employing 4-6 primers targeting 6-8 distinct regions of the target sequence. This multi-target approach provides theoretical specificity advantages, though in practice, the technique faces different challenges. The large number of primers increases the probability of primer-dimer interactions and self-amplifying hairpin structures, particularly in the elongated FIP and BIP primers (typically 40-45 bases) [62]. Studies demonstrate that minor modifications to eliminate these structures can dramatically improve LAMP performance, highlighting the critical importance of primer design in achieving optimal specificity for both techniques.
Operational Considerations and Practical Implementation
Beyond pure performance metrics, practical implementation factors significantly influence technique selection for diagnostic applications. The nPCR method requires precise thermal cycling with two separate amplification programs, extending the total hands-on and amplification time. The essential transfer step between reactions not only introduces contamination risk but also increases operator time requirements [1]. Additionally, nPCR typically requires post-amplification processing, such as gel electrophoresis, for result visualization, further extending the time to result.
In contrast, LAMP operates at a single isothermal temperature (typically 60-65°C), eliminating the need for sophisticated thermal cyclers and reducing power requirements [27]. The technique's compatibility with simple visualization methods, including colorimetric changes, turbidity measurement, or fluorescent dyes, enables rapid result interpretation without extensive post-processing [63]. This operational simplicity makes LAMP particularly suitable for resource-limited settings or point-of-care applications where equipment access and technical expertise may be constrained.
Figure 2: Comparative Workflows: nPCR vs. LAMP. The nPCR process requires multiple steps with a critical contamination risk point during product transfer, while LAMP employs a simplified isothermal amplification with minimal transfer steps.
Primer Design Optimization Strategies
nPCR Primer Design Considerations
Effective nPCR primer design requires careful attention to multiple parameters to ensure successful two-stage amplification while minimizing artifact formation. The outer and inner primer sets must be designed to work in concert, with the inner primers positioned completely within the region flanked by the outer primers to ensure specific nested amplification. Key design considerations include maintaining appropriate melting temperature (Tm) consistency within each primer set (typically within 2°C), avoiding regions of secondary structure, and ensuring primer lengths of 18-25 nucleotides for optimal binding efficiency [1].
Computational tools play an essential role in modern primer design for nPCR. Software such as Primer Premier and OligoAnalyzer enables comprehensive evaluation of potential primer-dimer interactions, hairpin formation, and cross-homology with non-target sequences. Specific attention should be paid to the 3' ends of all primers, as even limited complementarity (≥3 bases) can initiate polymerase extension and primer-dimer artifacts [62]. Empirical validation through controlled experiments remains essential, as computational predictions cannot fully capture the complexity of enzymatic amplification in specific reaction conditions.
LAMP Primer Design Complexities
LAMP primer design presents distinct challenges due to the requirement for 4-6 primers targeting 6-8 regions within a relatively short DNA segment (typically 120-180 bp). The FIP and BIP primers are particularly problematic, as their length (40-45 bases) predisposes them to stable hairpin formation that can sequester primers in inactive conformations or create self-amplifying structures [62]. Research demonstrates that even hairpins with complementarity one or two bases away from the 3' end can still self-amplify, generating non-specific background signals that reduce assay reliability.
Thermodynamic analysis using the nearest-neighbor model provides valuable insights for optimizing LAMP primer specificity. Studies indicate that evaluating the stability of potential secondary structures, with particular attention to the free energy (ΔG) of dimerization and hairpin formation, enables identification of problematic primers before experimental validation [62]. Minor modifications to "bump" priming sites based on these thermodynamic predictions can dramatically reduce non-specific background amplification while maintaining target sensitivity. This approach has proven successful in improving previously published primer sets for dengue virus and yellow fever virus detection, highlighting the universal importance of rigorous primer design regardless of the specific application.
Research Reagent Solutions for Amplification Assays
Table 3: Essential Reagents for Nucleic Acid Amplification Techniques
| Reagent Category | Specific Examples | Function & Importance | Technique Application |
|---|---|---|---|
| DNA Polymerases | Taq DNA polymerase (thermostable), Bst 2.0 polymerase (strand-displacing) | Catalyzes DNA synthesis; thermostability essential for PCR; strand displacement activity critical for LAMP [1] [63] | Universal requirement |
| Reverse Transcriptases | AMV Reverse Transcriptase, M-MLV RT | Converts RNA to cDNA for detection of RNA viruses and gene expression analysis [62] | RT-nPCR, RT-LAMP |
| Primer Design Tools | Primer Explorer V4, Primer Premier 5, mFold tool | Enables design and validation of specific primer sets; critical for avoiding dimerization and secondary structures [27] [62] | Universal requirement |
| Visualization Methods | SYBR Green, phenol red, calcein-manganese, lateral flow dipsticks | Enables detection of amplification products through fluorescence, color change, or immunochromatography [1] [63] | Post-amplification detection |
| Contamination Control | Uracil-N-Glycosylase (UNG), dUTP incorporation | Degrades carryover amplicons from previous reactions; critical for nPCR contamination prevention [1] | Primarily nPCR |
Strategic Implementation and Future Directions
The selection between nPCR and LAMP technologies depends heavily on the specific application requirements and operational context. nPCR remains the technique of choice for applications demanding ultra-sensitive detection, particularly in clinical diagnostics where maximum sensitivity is paramount, such as in detection of SFTSV during the convalescent phase or identification of low-abundance pathogens in complex sample matrices [61]. The well-established protocols, extensive validation history, and widespread institutional familiarity with PCR-based methods further support its continued use in reference laboratories with appropriate contamination control infrastructure.
LAMP technology offers compelling advantages for rapid screening applications, point-of-care testing, and resource-limited settings. The minimal equipment requirements, rapid time-to-result (often 30-60 minutes), and tolerance to inhibitory substances present in crude samples make it ideal for field deployment [27] [63]. The closed-tube format of many LAMP assays significantly reduces contamination risk compared to nPCR, supporting more reliable implementation in settings with less controlled environments. As primer design tools and reaction formulations continue to improve, LAMP is positioned to address an expanding range of diagnostic applications where speed, simplicity, and cost-effectiveness are prioritized.
Future developments in both technologies will likely focus on addressing their respective limitations. For nPCR, innovations in single-tube nested approaches and improved contamination control methods will enhance reliability and broaden implementation. LAMP development will continue to refine primer design algorithms and reaction conditions to minimize non-specific amplification while expanding the repertoire of robust detection methodologies. Both techniques will play complementary roles in the molecular diagnostic landscape, with selection guided by the specific sensitivity requirements, operational constraints, and implementation environment of each application.
Quantitative Reverse Transcription Polymerase Chain Reaction (RT-PCR) remains a cornerstone technique in molecular diagnostics and life science research, valued for its sensitivity and specificity. However, inherent challenges in quantification accuracy, efficiency, and data linearity persist, driving continuous optimization efforts. This guide objectively compares RT-PCR performance against emerging methodologies—Reverse Transcription Loop-Mediated Isothermal Amplification (RT-LAMP) and nested PCR (nPCR)—within a broader thesis on diagnostic sensitivity. The evaluation focuses on technical parameters crucial for researchers, scientists, and drug development professionals, including detection limits, quantitative linearity, and practical implementation in clinical and research settings. Recent studies highlight the critical importance of these optimizations, as variability in amplification efficiency and standard curve implementation can significantly impact result reproducibility and reliability [65] [66] [67].
Performance Comparison of Molecular Amplification Techniques
Table 1: Key Performance Characteristics of Amplification Techniques
| Parameter | RT-PCR | nPCR | RT-LAMP |
|---|---|---|---|
| Theoretical Principle | Fluorescence-based real-time monitoring of amplification; relies on standard curves for quantification [65] | Two consecutive amplification rounds using two primer sets; final product visualized via gel electrophoresis [22] | Isothermal amplification using 4-6 primers; visual detection via turbidity or color change [68] [22] |
| Typical Assay Time | 1.5 - 2 hours [9] | 3 - 4 hours (including gel analysis) [22] | 60 - 70 minutes [68] [22] |
| Detection Limit (Copies/Reaction) | 2 - 10 (for SARS-CoV-2) [69] | Higher sensitivity than conventional PCR [22] | 6.7 (for SARS-CoV-2) [68] |
| Quantification Capability | Excellent (absolute/relative) [67] | No (endpoint detection) | Limited (semi-quantitative) |
| Throughput | High (multiplexing possible) [69] | Low | Moderate |
| Equipment Needs | Thermocycler with fluorescence detector [9] | Standard thermocycler, gel doc system [22] | Water bath/block heater [22] |
| Susceptibility to Inhibitors | Moderate (can be mitigated with sample cleanup) [17] | Lower (second round reduces inhibitor impact) [22] | Low (robust amplification) |
Experimental Evidence and Sensitivity Data
Table 2: Summary of Experimental Findings from Clinical and Analytical Studies
| Study Context | RT-PCR Performance | nPCR Performance | RT-LAMP Performance | Key Finding |
|---|---|---|---|---|
| SARS-CoV-2 Detection (Symptomatic Phase) | Gold standard; high sensitivity [68] | Not assessed | 100% sensitivity vs. RT-PCR up to day 9; sensitivity drops significantly after day 10 [68] | RT-LAMP is equivalent to RT-PCR in acute phase but not for late infection. |
| Feline Calicivirus (FCV) Detection (Clinical Samples, n=54) | 1.85% positivity (1/54 samples) [22] | 31.48% positivity (17/54 samples) [22] | 31.48% positivity (17/54 samples) [22] | nPCR and RT-LAMP showed significantly higher clinical sensitivity than conventional PCR. |
| SARS-CoV-2 Multiplex Assay | LoD: 10 copies/reaction (for E and N genes) [69] | Not assessed | Not assessed | Optimized single-tube multiplex RT-PCR maintains high sensitivity. |
| Malaria Species Detection (HRM vs. Sequencing) | High-resolution melting (HRM) analysis post-PCR showed 100% agreement with sequencing for species identification [70] | Not assessed | Not assessed | PCR/HRM is a reliable closed-tube method for species differentiation. |
Optimization Strategies for RT-PCR Efficiency and Linearity
Addressing Amplification Efficiency and Variability
A primary source of inaccuracy in RT-PCR stems from ignoring the amplification efficiency (E), which is the fold-increase in amplicon per cycle [67]. An ideal reaction has an efficiency of 2 (100%), meaning the product doubles every cycle. However, efficiency can vary significantly between assays and even between samples within the same run due to factors like reagent quality, sample purity, and primer design [65] [67]. The common use of the 2−ΔΔCT method relies on the assumption of perfect, uniform efficiency, which often introduces bias [66] [67]. For rigorous quantification, efficiency-corrected analysis is recommended, which uses the actual efficiency value calculated from standard curves [67].
The implementation of standard curves themselves is a critical optimization point. A study evaluating inter-assay variability for virus detection found that while standard curves had acceptable efficiencies (>90%), their parameters (slope, y-intercept) showed notable variability between runs [65]. For instance, the SARS-CoV-2 N2 gene exhibited a CV of 4.38-4.99% and an average efficiency of 90.97% across 30 experiments [65]. This evidence strongly supports the practice of including a standard curve in every qPCR run to obtain reliable, reproducible quantitative results, rather than relying on a historical "master" curve [65].
Advanced Data Analysis and Multiplexing
Advanced statistical approaches like Analysis of Covariance (ANCOVA) offer greater robustness and statistical power compared to the 2−ΔΔCT method. ANCOVA models are less affected by variations in amplification efficiency and provide a more flexible framework for complex experimental designs [66]. Furthermore, adherence to the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) and FAIR (Findable, Accessible, Interoperable, Reproducible) data principles is crucial for rigor and reproducibility. This includes sharing raw fluorescence data and analysis scripts to ensure transparency [66].
Multiplex RT-PCR, which detects multiple targets in a single reaction, presents both an optimization challenge and opportunity. Key considerations include:
- Primer/Probe Design: In silico evaluation against relevant sequence databases is essential to ensure 100% identity with all target variants [69].
- Concentration Titration: Primer and probe concentrations must be empirically optimized to balance signal intensity and minimize cross-talk [69].
- Validation: A successfully optimized multiplex assay should show no significant difference in Cq values and fluorescence units compared to its singleplex counterparts, maintaining a low limit of detection (e.g., 10 copies/reaction) [69].
Figure 1: Optimized qPCR Data Analysis Workflow. This workflow emphasizes the critical steps of proper baseline correction and efficiency determination from a standard curve to arrive at reliable, efficiency-corrected quantitative results [66] [67].
Essential Research Reagent Solutions
Table 3: Key Reagents and Their Functions in Optimized RT-PCR
| Reagent / Kit Component | Critical Function | Optimization Consideration |
|---|---|---|
| One-Step RT-qPCR Enzyme Mix | Integrates reverse transcription and DNA amplification; essential for workflow efficiency and minimizing sample handling [69]. | Choose mixes validated for multiplexing. High processivity and inhibitor tolerance are key. |
| Sequence-Specific Primers & Probes | Dictates assay specificity and sensitivity. Dual-labeled probes (e.g., TaqMan) enable real-time, specific detection [69]. | In silico specificity analysis and empirical concentration titration are mandatory, especially for multiplex assays [69]. |
| Synthetic RNA Standards | Provides known-concentration material for generating standard curves, enabling absolute quantification and efficiency calculation [65]. | Aliquot to avoid freeze-thaw cycles. Use the same matrix as the sample to control for extraction efficiency [65]. |
| Nucleic Acid Extraction Kit | Determines the quality, purity, and final yield of the template RNA/DNA. Critical for removing PCR inhibitors. | Manual (e.g., silica-column) vs. automated (e.g., magnetic bead) platforms should be chosen based on throughput and reproducibility needs. |
| Internal Control (e.g., RNAse P) | Distinguishes true target negatives from amplification failures due to inhibitors or poor RNA quality [69]. | Must be added prior to nucleic acid extraction to control for the entire process. |
The optimization of RT-PCR is a multi-faceted endeavor central to achieving reliable quantitative data. While emerging techniques like RT-LAMP offer compelling advantages in speed and simplicity for specific applications like acute-phase infection diagnosis, and nPCR provides superior sensitivity for endpoint detection, RT-PCR remains the gold standard for robust quantification. The key to unlocking its full potential lies in rigorous optimization strategies: implementing per-run standard curves, adopting efficiency-corrected data analysis methods like ANCOVA, and carefully designing multiplex assays. By systematically addressing these elements, researchers can significantly enhance the efficiency, linearity, and overall reliability of their RT-PCR assays, ensuring the generation of high-quality data for both research and diagnostic applications.
The selection of an appropriate detection method is a critical step in the design and implementation of molecular diagnostics. Following nucleic acid amplification techniques such as Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and real-time PCR (RT-PCR), researchers must choose from several detection platforms to visualize and interpret results. Each method offers distinct advantages and limitations in terms of sensitivity, specificity, cost, time requirements, and suitability for point-of-care applications. This guide provides an objective comparison of three primary detection methodologies—gel electrophoresis, lateral flow assays (LFA), and colorimetric dyes—within the context of post-amplification analysis for infectious disease diagnostics, particularly focusing on their integration with LAMP, nPCR, and RT-PCR platforms.
The evaluation framework for these detection methods centers on several key performance parameters. Analytical sensitivity refers to the lowest concentration of the target analyte that can be reliably detected, while specificity indicates the method's ability to distinguish the target from non-target analytes. Operational characteristics such as turnaround time, cost per test, and equipment requirements determine practical implementation feasibility. Readout simplicity affects the need for specialized interpretation skills and the potential for deployment in resource-limited settings. Understanding these parameters helps researchers select the optimal detection method based on their specific diagnostic requirements and operational constraints.
The table below summarizes the key characteristics of the three detection methods evaluated in this guide:
Table 1: Performance Comparison of Detection Methods for Molecular Assays
| Detection Method | Optimal Sensitivity (LoD) | Time to Result | Equipment Needs | Cost per Test | Quantification Capability | Ease of Use |
|---|---|---|---|---|---|---|
| Gel Electrophoresis | 1 E. histolytica trophozoite (with LAMP) [1] | 45-90 min (post-amplification) | Electrophoresis chamber, UV transilluminator | Low | No (endpoint detection) | Moderate (technical skill required) |
| Lateral Flow Assay | 0.62 fM (for nucleic acids with enhanced LFA) [71] | 15-30 min (post-amplification) | Minimal (optional readers for quantification) | Low to Moderate | Semi-quantitative with readers | High (minimal training required) |
| Colorimetric Dyes | 1 E. histolytica trophozoite (with LAMP) [1] | 45 min (including amplification) | None (visual detection) | Very Low | No (qualitative) | Very High |
Detailed Methodological Analysis
Gel Electrophoresis
Gel electrophoresis represents a foundational technique in molecular biology for separating and visualizing nucleic acids based on their size and charge. The method employs an electric field to migrate DNA fragments through an agarose or polyacrylamide matrix, with intercalating dyes such as ethidium bromide or SYBR Safe enabling visualization under ultraviolet light.
Experimental Protocol for Post-Amplification Analysis:
- Prepare a 1.5-2% agarose gel by dissolving agarose powder in TBE or TAE buffer
- Add intercalating dye at a concentration of 0.5 µg/mL to the molten agarose before casting
- Load 5-10 µL of amplified product mixed with DNA loading dye into wells
- Conduct electrophoresis at 80-100V for 30-45 minutes in an appropriate running buffer
- Visualize DNA bands using a UV transilluminator or blue light imaging system
- Compare band sizes against a DNA ladder for product verification
In comparative studies, gel electrophoresis coupled with LAMP demonstrated exceptional sensitivity, detecting DNA equivalent to a single Entamoeba histolytica trophozoite, outperforming both nPCR and qPCR which showed limits of detection of 100 trophozoites and 1000 trophozoites, respectively [1]. This method provides robust verification of amplification product size, which is particularly valuable for assay validation and troubleshooting. However, the requirement for specialized equipment, potential exposure to mutagenic dyes, and the time-intensive nature (typically adding 45-90 minutes to the workflow) represent significant limitations for high-throughput or point-of-care applications.
Lateral Flow Assays
Lateral flow assays have emerged as a prominent platform for rapid, point-of-care detection of nucleic acids, particularly when integrated with isothermal amplification methods like LAMP. These paper-based devices leverage capillary action to facilitate the movement of liquid samples through a membrane, where specific biorecognition elements interact with target analytes to produce visual signals.
Experimental Protocol for Nucleic Acid Detection:
- Design hapten-labeled primers (e.g., biotin and fluorescein) during amplification
- Apply amplified product to the sample pad of the lateral flow strip
- Allow capillary flow for 5-15 minutes to develop results
- Interpret visually by observing colored test lines or using dedicated readers
Advanced LFA systems have incorporated innovative signal tracers such as methylene blue, which enables dual-modality detection through both colorimetric and electrochemical readouts. The MebiQue-LFA platform demonstrated remarkable sensitivity, achieving detection limits of 0.62 fM and 43 fM (~100 copies/µL) in buffer and diluted blood, respectively [71]. This approach separates biorecognition and sensing events, effectively minimizing biofouling—a common challenge in biosensors—without requiring specialized coatings. Modern multiplex LFAs can simultaneously detect multiple targets through various strategies, including the use of multiple detection labels, different nanomaterials, and signal amplification methods like hybridization chain reaction [72]. The primary advantages of LFAs include rapid results (typically 15-30 minutes), minimal equipment requirements, and excellent suitability for resource-limited settings, though they may require primer modifications and have historically exhibited lower sensitivity for direct sample detection without amplification.
Colorimetric Dyes
Colorimetric detection methods offer the simplest approach for visualizing amplification results through visible color changes, eliminating the need for specialized equipment. These systems typically employ pH-sensitive dyes or metal-ion indicator complexes that undergo distinct color transitions in the presence of amplification byproducts.
Experimental Protocol for Colorimetric LAMP Detection:
- Add colorimetric dye (e.g., calcein-manganese or phenol red) to the LAMP reaction mixture prior to amplification
- Conduct amplification at 60-65°C for 30-60 minutes
- Observe color change directly without opening tubes to prevent contamination
- Calcein-manganese systems change from orange to green, while pH-sensitive dyes shift from pink to yellow
Research has demonstrated that colorimetric LAMP detection can achieve sensitivity equivalent to 1 Entamoeba histolytica trophozoite, matching the performance of gel electrophoresis and surpassing conventional PCR methods [1]. The optimal incubation time for RT-LAMP assays with colorimetric readout is approximately 45 minutes, significantly faster than traditional RT-qPCR protocols [19]. A significant advantage of closed-tube colorimetric methods is the substantially reduced risk of amplicon contamination, as visualization occurs without opening reaction vessels. However, these methods provide strictly qualitative yes/no results without quantification capability and may be susceptible to subjective interpretation of color changes, particularly with weakly positive samples.
Sensitivity Comparison Across Amplification Platforms
The integration of detection methods with various amplification technologies significantly impacts overall assay performance. The following table compares the limits of detection achieved by different amplification and detection combinations:
Table 2: Sensitivity Comparison of Detection Methods with Different Amplification Techniques
| Amplification Method | Detection Method | Limit of Detection | Application Context |
|---|---|---|---|
| LAMP | Gel Electrophoresis | 1 trophozoite | Entamoeba histolytica detection [1] |
| LAMP | Colorimetric (Calcein-Mn) | 1 trophozoite | Entamoeba histolytica detection [1] |
| LAMP | Lateral Flow Immunoassay | 1 trophozoite | Entamoeba histolytica detection [1] |
| nPCR | Gel Electrophoresis | 100 trophozoites | Entamoeba histolytica detection [1] |
| RT-qPCR | Fluorescence Detection | 100 trophozoites | Entamoeba histolytica detection [1] |
| Conventional PCR | Gel Electrophoresis | 1000 trophozoites | Entamoeba histolytica detection [1] |
| RT-LAMP | Colorimetric | Comparable to RT-qPCR with extracted RNA | SARS-CoV-2 detection [19] |
| RT-LAMP | Colorimetric | 71% sensitivity with direct swab samples | SARS-CoV-2 detection [19] |
Experimental Protocols for Sensitivity Comparison
To ensure reproducible comparison of detection methods, standardized experimental protocols are essential. The following section outlines validated methodologies for evaluating detection platform performance with different amplification techniques.
LAMP Detection Comparison Protocol
Objective: Compare the sensitivity of gel electrophoresis, lateral flow immunoassay, and colorimetric dye techniques for detecting LAMP amplicons.
Sample Preparation:
- Extract DNA from serial dilutions of Entamoeba histolytica trophozoites (1 to 1000 trophozoites)
- Use SREHP gene-specific LAMP primers (F3, B3, FIP, B3, LF, LB)
- Perform LAMP amplification at 65°C for 45-60 minutes
Detection Procedures:
- Gel Electrophoresis: Analyze 5µL of product on 2% agarose gel, visualize with intercalating dye
- Lateral Flow: Use hapten-labeled primers (biotin/fluorescein), apply to LFD strips, interpret at 5-10 minutes
- Colorimetric: Include calcein-manganese dye in reaction mix, observe color change from orange to green
Validation: This protocol confirmed equivalent sensitivity (1 trophozoite) across all three detection methods, outperforming nPCR and qPCR which detected 100 and 1000 trophozoites, respectively [1].
RT-LAMP vs RT-qPCR Direct Comparison
Objective: Evaluate RT-LAMP with colorimetric readout against reference RT-qPCR for SARS-CoV-2 detection.
Sample Processing:
- Collect nasopharyngeal and oropharyngeal swab samples in viral transport medium
- Extract RNA using commercial kits or use direct swab samples with lysis buffer
- For direct swab methods, heat samples at 95°C for 2 minutes in lysis buffer
Amplification Conditions:
- RT-LAMP: Optimize primer set targeting ORF1a gene, incubate at 65°C for 45 minutes
- RT-qPCR: Use commercial kit with recommended cycling conditions
Analysis: Compare sensitivity and specificity between methods using extracted RNA and direct swab samples. This protocol demonstrated 100% agreement between RT-LAMP and RT-qPCR with extracted RNA, but reduced sensitivity (71%) for RT-LAMP with direct swab samples [19].
Research Reagent Solutions
The table below outlines essential reagents and their functions for implementing the detection methods discussed in this guide:
Table 3: Key Research Reagents for Detection Method Implementation
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Bst DNA Polymerase | Isothermal amplification enzyme | LAMP reactions [1] |
| Hapten-labeled Primers | Primer modification for LFA detection | Biotin/fluorescein tags for lateral flow strips [1] |
| Calcein-Manganese Dye | Colorimetric indicator for LAMP | Visual detection of amplification [1] |
| Agarose | Matrix for nucleic acid separation | Gel electrophoresis [1] |
| Nucleic Acid Intercalators | DNA staining for visualization | Ethidium bromide, SYBR Safe [1] |
| Lateral Flow Strips | Solid-phase detection platform | Nucleic acid lateral flow immunoassay [1] |
| Methylene Blue Tracer | Dual-modality signal tracer | Colorimetric and electrochemical LFA [71] |
| Gold Nanoparticles | Colorimetric labels for LFA | Visual signal generation [72] |
Workflow Diagrams
Diagram 1: Workflow for Detection Method Selection and Implementation
Diagram 2: Sensitivity Comparison and Application Context for Detection Methods
The selection of an appropriate detection method requires careful consideration of the specific application context and performance requirements. Gel electrophoresis remains the gold standard for research validation due to its robust product verification capabilities, though it demands specialized equipment and technical expertise. Lateral flow assays offer an optimal balance of sensitivity, speed, and ease of use for point-of-care applications, particularly with recent advancements in signal amplification strategies. Colorimetric dyes provide the simplest implementation with minimal equipment requirements, making them ideal for resource-limited settings, though they lack quantification capabilities.
For maximum sensitivity in diagnostic applications, LAMP coupled with any of the three detection methods outperforms both nPCR and RT-qPCR platforms, demonstrating the potential of isothermal amplification technologies to revolutionize infectious disease diagnostics. Researchers should consider the full ecosystem of requirements—including sensitivity thresholds, equipment availability, operator skill, and intended use setting—when selecting the optimal detection method for their specific application.
Incorporating Internal Controls and Managing Inhibitors in Complex Samples
Robust molecular diagnostics in complex biological samples hinge on two critical pillars: the effective use of internal controls to monitor assay performance and strategic management of inhibitory substances that compromise amplification efficiency. While numerous nucleic acid amplification techniques exist, their performance varies significantly when confronted with challenging sample matrices such as stool, respiratory secretions, and other clinical specimens containing PCR inhibitors. This guide objectively compares how Loop-Mediated Isothermal Amplification (LAMP), nested PCR (nPCR), and Reverse Transcription-PCR (RT-PCR) address these critical challenges, providing researchers with experimental data to inform their methodological selections for drug development and clinical diagnostics.
The fundamental challenge stems from the composition of complex samples, which often contain substances that inhibit polymerase activity or sequester nucleic acids. Stool samples contain bile salts, complex polysaccharides, and hemoglobin derivatives [1], while respiratory samples may contain mucus, blood, and inflammatory cells [20] [19]. These inhibitors disproportionately affect different amplification methods, necessitating tailored approaches for internal control implementation and inhibition management across platforms.
Performance Comparison of Amplification Techniques
Analytical Sensitivity and Robustness Against Inhibition
Table 1: Comparative Performance of LAMP, nPCR, and RT-PCR in Complex Samples
| Parameter | LAMP | nPCR | RT-PCR |
|---|---|---|---|
| Limit of Detection (LoD) in Complex Samples | 1 trophozoite in stool samples [1] | 100 trophozoites in stool samples [1] | 100 trophozoites in stool samples [1] |
| Inhibition Resistance | Moderate to high; works in direct swab samples but with reduced sensitivity [19] | Low; highly susceptible due to two amplification rounds [1] | Moderate; requires RNA extraction for optimal performance [20] [19] |
| Internal Control Options | Co-amplification with sample DNA, colorimetric controls with pH-sensitive dyes [39] | External controls only due to primer competition in nested rounds [1] | Exogenous spike-in controls, endogenous human gene targets (e.g., RNase P) [20] [39] |
| Optimal Sample Processing | Partial purification recommended for direct samples [19] | Extensive purification required [1] | RNA extraction essential for reliable results [20] [19] |
| False Positive Risk | Moderate (primarily from amplicon contamination) [19] | High (from first-round amplicon contamination) [1] | Low (closed-tube systems) [73] |
| Diagnostic Specificity | 100% (when optimized) [39] | 100% (when contamination controlled) [1] | 100% (with proper primer design) [39] |
Key Experimental Findings
Experimental data from comparative studies reveals significant performance differences. In one comprehensive analysis using Entamoeba histolytica-spiked stool samples, LAMP demonstrated a Limit of Detection (LoD) of a single trophozoite, outperforming nPCR and qPCR which both achieved LoDs of 100 trophozoites, and conventional PCR with an LoD of 1000 trophozoites [1]. This superior sensitivity in complex matrices highlights LAMP's robustness against inhibitors naturally present in stool samples.
For SARS-CoV-2 detection, RT-LAMP showed comparable sensitivity to RT-qPCR when using extracted RNA but exhibited reduced sensitivity (71%) with direct swab samples without RNA extraction [19]. This performance reduction underscores the impact of inhibitors in direct samples and emphasizes the necessity of sample processing, even for inhibitor-resistant platforms. Notably, colorimetric RT-LAMP demonstrated 100% specificity when tested against numerous respiratory viruses and healthy controls [39].
Experimental Protocols for Inhibition Management
LAMP Protocol for Complex Samples
Sample Preparation: For stool samples, the Qiagen QIAamp DNA Stool Mini Kit provided effective inhibition management in E. histolytica detection [1]. For respiratory samples, preliminary processing with proteinase K treatment improved detection rates.
Reaction Composition:
- 5 pmol each of F3 and B3 primers
- 40 pmol each of FIP and BIP primers
- 20 pmol each of LF and LB loop primers
- 8U Bst DNA/RNA Polymerase 3.0 (New England Biolabs)
- Betaine (0.8 M final concentration) to facilitate strand separation
- Colorimetric dye (phenol red or hydroxynaphthol blue) for pH-based detection [39]
Amplification Conditions:
- Isothermal amplification at 56-65°C for 30-70 minutes [20] [22] [39]
- No initial denaturation step required
- Visual detection under UV light for fluorescent dyes or visible light for colorimetric changes
Internal Control Implementation:
- Separate primer set for endogenous control gene amplified in parallel
- Color change validation: pink (negative), yellow (positive), orange (indeterminate) [39]
nPCR Protocol with Inhibition Controls
Sample Processing:
- Nucleic acid extraction using NucleoSpin Tissue DNA Extraction kit [1]
- Additional purification steps recommended for inhibitor-heavy samples
First Round PCR:
- Outer primers Eh-F3-SER and Eh-B3-SER
- Recombinant Taq DNA polymerase (Thermo Fisher)
- 30-35 cycles to prevent excessive amplicon accumulation
Second Round PCR:
- Inner primers targeting F2 and B2 regions
- Transfer of minimal first-round product (1-5%) to prevent carryover inhibition
- Strict physical separation of first and second round amplification areas
Contamination Prevention:
- Uracil-DNA Glycosylase (UNG) treatment to degrade carryover amplicons
- Dedicated equipment for first and second round amplifications [1]
RT-PCR Protocol with Internal Controls
RNA Extraction:
- Biorexfars SARS-CoV-2 RNA Extraction Kit or equivalent [20]
- Incorporation of exogenous RNA control during lysis step to monitor extraction efficiency
Reaction Setup:
- 5 µl RNA template in 20 µl reaction volume
- TaqMan One-Step RT-qPCR master mix
- Multiplex detection: HEX channel (target gene), ROX channel (RNase P internal control) [20]
Amplification Parameters:
- Reverse transcription: 50°C for 20 minutes
- Initial denaturation: 95°C for 3 minutes
- 45 cycles of: 95°C for 15s, 55°C for 40s with fluorescence measurement [20]
Inhibition Detection:
- RNase P amplification with expected Ct <33 indicates sufficient RNA quality and absence of inhibitors [39]
- Spike-in controls to monitor extraction and amplification efficiency
Visualizing Methodological Workflows and Performance Relationships
Sample Processing and Amplification Workflow
Sample Processing and Inhibition Management Workflow
Performance Relationship Between Viral Load and Detection
Detection Performance Versus Viral Load and Inhibition
Research Reagent Solutions for Inhibition Management
Table 2: Essential Reagents for Managing Inhibitors in Complex Samples
| Reagent Category | Specific Products | Function in Inhibition Management |
|---|---|---|
| DNA Polymerases | Bst DNA/RNA Polymerase 3.0 (NEB) [20] [1] | Isothermal amplification with enhanced inhibitor resistance |
| Recombinant Taq DNA Polymerase (Thermo Fisher) [1] | Standard PCR with moderate inhibitor tolerance | |
| Extraction Kits | Qiagen QIAamp DNA Stool Mini Kit [1] | Optimized for inhibitor removal from complex matrices |
| Biorexfars SARS-CoV-2 RNA Extraction Kit [20] | Specialized for viral RNA with internal control capability | |
| Amplification Enhancers | Betaine [1] | Reduces secondary structure and improves amplification efficiency |
| Bovine Serum Albumin (BSA) [1] | Binds inhibitors and increases polymerase stability | |
| Detection Reagents | Phenol Red [39] | pH-based colorimetric detection for LAMP |
| Calcein-Manganese Dye [1] | Fluorescent detection for LAMP amplification | |
| SYBR Green I Mastermix [73] | Intercalating dye for RT-qPCR detection | |
| Internal Controls | RNase P Primers/Probes [20] [39] | Endogenous human RNA control for nucleic acid extraction |
| Exogenous RNA Spikes | Process control for extraction and amplification efficiency |
The selection of appropriate molecular amplification methods for complex samples requires careful consideration of inhibition management and internal control strategies. LAMP technology offers superior sensitivity in heavily inhibited samples like stool and provides flexible colorimetric detection options, though it requires careful interpretation of intermediate results [39]. nPCR, while sensitive, demonstrates high susceptibility to inhibition and carries significant contamination risks [1]. RT-PCR remains the gold standard for quantitative results and reliable internal control implementation but demands extensive sample processing [19] [39].
For researchers working with complex samples, the optimal approach involves matching the amplification methodology to sample type, required sensitivity, and available infrastructure. Implementation of appropriate internal controls remains non-negotiable across all platforms, as they provide critical quality assurance for diagnostic results and drug development applications. As molecular diagnostics advance, hybrid approaches that combine the robustness of LAMP with the quantification capabilities of PCR may offer the most promising path forward for challenging sample matrices.
Head-to-Head Validation: Sensitivity, Specificity, and Clinical Concordance
This guide provides a direct, data-driven comparison of the Limits of Detection (LoD) for four prominent DNA-based amplification methods: Loop-mediated isothermal amplification (LAMP), conventional PCR (cPCR), nested PCR (nPCR), and real-time PCR (qPCR). The synthesis of current research consistently demonstrates that LAMP exhibits a superior analytical sensitivity, often detecting target DNA at concentrations 10 to 1000 times lower than other PCR-based techniques. This performance, combined with its isothermal nature and rapid turnaround, positions LAMP as a highly relevant alternative for pathogen detection in both clinical and resource-limited settings.
Defining Limit of Detection (LoD)
The Limit of Detection (LoD) is a fundamental metric of analytical sensitivity, defined as the lowest concentration of an analyte that can be reliably distinguished from a blank sample with a high degree of confidence (typically 95%) [74] [75]. It is distinct from the Limit of Blank (LoB), which is the highest apparent signal from a blank sample, and the Limit of Quantitation (LoQ), which is the lowest concentration that can be measured with acceptable precision and accuracy [74]. In molecular diagnostics, a lower LoD translates to an enhanced ability to identify infections with low pathogen loads, such as during the early stages of disease or with parasites that cause low-level parasitemia [76].
Direct LoD Comparison: LAMP vs. PCR Methods
A critical study provides a direct, head-to-head comparison of these four amplification technologies, all targeting the same Serine-rich Entamoeba histolytica protein (SREHP) gene on DNA extracted from spiked stool samples [55]. The results offer a clear hierarchy of analytical sensitivity.
Table 1: Direct LoD Comparison for Detection of Entamoeba histolytica [55]
| Amplification Method | Limit of Detection (LoD) in Trophozoites | Relative Sensitivity |
|---|---|---|
| LAMP (with various detection methods) | 1 | Highest |
| qPCR (Real-time PCR) | 100 | 100x less sensitive than LAMP |
| nPCR (Nested PCR) | 100 | 100x less sensitive than LAMP |
| cPCR (Conventional PCR) | 1000 | 1000x less sensitive than LAMP |
This trend is corroborated by numerous other studies across different pathogens and sample matrices, confirming that LAMP consistently achieves a lower or comparable LoD to the most sensitive PCR variants.
- In Feline Calicivirus (FCV) Detection: A colorimetric RT-LAMP assay demonstrated a LoD of 14.3 × 10¹ copies/µL and detected significantly more positive clinical samples (31.48%) than conventional PCR (1.85%), performing on par with nested PCR [22].
- In Plant Pathogen Detection: For the fungus Diaporthe aspalathi, LAMP was 100 times more sensitive than conventional PCR and 10 times more sensitive than qPCR, achieving a LoD of 0.01 ng/µL [77].
- In Toxoplasma gondii Detection: LAMP successfully detected down to 5 oocysts in both mussel tissue and hemolymph, demonstrating its effectiveness in complex food matrices [78].
Detailed Experimental Protocols
To ensure an equitable comparison, the referenced primary study [55] established a standardized protocol where all assays were developed to bind the same location on the SREHP gene.
Sample Preparation and DNA Extraction
- Biological Model: The study used Entamoeba histolytica trophozoites (strain HM-1:IMSS).
- Sample Matrix: Stool samples were artificially spiked with a known number of trophozoites.
- DNA Extraction: DNA was isolated from the spiked stool samples using the QIAamp DNA Stool Mini Kit (Qiagen). DNA from other related pathogens (E. dispar, E. moshkovskii) and 75 other pathogenic microorganisms was also extracted to serve as negative controls for specificity testing [55].
Primer Design and Optimization
- LAMP Primers: A set of six specific primers (two outer, two inner, and two loop primers) were designed to recognize eight distinct regions of the SREHP gene. This complex primer design is a key factor in the high specificity of LAMP [55].
- PCR Primers: The same SREHP gene sequence was used to design primers for cPCR, nPCR, and qPCR, ensuring a direct comparison of amplification efficiency without bias from target sequence variation [55].
Amplification Reaction Conditions
Table 2: Key Reaction Components and Conditions [55]
| Method | Polymerase Enzyme | Key Reagents | Thermal Profile | Amplification Time |
|---|---|---|---|---|
| LAMP | Bst DNA polymerase | Betaine, MgSO₄ | Isothermal (60-65°C) | ~60 minutes |
| cPCR / nPCR | Recombinant Taq DNA Polymerase | dNTPs, primers | 25-40 cycles of denaturation, annealing, extension | >90 minutes |
| qPCR | Not specified | QuantiFast SYBR Green PCR Kit | 40-45 cycles of denaturation, annealing, extension | >90 minutes |
Post-Amplification Analysis and LoD Determination
The LoD was determined by testing serial dilutions of DNA extracted from a known number of trophozoites. The LoD was defined as the lowest concentration where amplification was consistently detected.
- LAMP Detection: The study compared three post-amplification detection methods, all of which recorded the same LoD of 1 trophozoite:
- Agarose Gel Electrophoresis: Visualizing the characteristic ladder-like pattern of LAMP products.
- Nucleic Acid Lateral Flow Immunoassay (LFD): Using a dipstick for biotin- and FITC-labelled amplicons.
- Calcein-Manganese Dye: A visual detection where a color change from orange to green indicates a positive reaction [55].
- PCR Detection: All PCR methods (cPCR, nPCR, qPCR) relied on standard analysis: agarose gel electrophoresis for cPCR and nPCR, and cycle threshold (Ct) analysis for qPCR [55].
Visual Workflow of LoD Comparison Experiment
The following diagram illustrates the logical flow of the direct comparison experiment that generated the core LoD data.
The Scientist's Toolkit: Key Research Reagents
The following table details essential reagents and their critical functions in establishing and running these sensitive molecular assays.
Table 3: Essential Research Reagents for Molecular Detection Assays [55]
| Reagent / Kit | Function in the Assay |
|---|---|
| QIAamp DNA Stool Mini Kit (Qiagen) | Efficient extraction of inhibitor-free DNA from complex biological matrices like stool, critical for accurate downstream amplification. |
| Bst DNA Polymerase (Large Fragment) | The core enzyme for LAMP; possesses strand-displacement activity enabling isothermal amplification without a thermal cycler. |
| Recombinant Taq DNA Polymerase | The standard thermostable enzyme for PCR, used in both conventional and nested PCR protocols. |
| QuantiFast SYBR Green PCR Kit (Qiagen) | Contains all optimized components (polymerase, buffer, SYBR Green dye) for sensitive real-time qPCR detection. |
| Calcein-Manganese Dye | A visual indicator for LAMP; a positive reaction causes a color change from orange to green visible under natural light. |
| Betaine | An additive in LAMP reactions that helps equalize the stability of DNA bases and prevents secondary structure formation, improving amplification efficiency. |
| Nucleic Acid Lateral Flow Immunoassay (LFD) Components | Provides a rapid, equipment-free method for visual detection of labelled LAMP or PCR amplicons at the point-of-care. |
The empirical data presented in this guide unequivocally demonstrates the superior analytical sensitivity of LAMP. Its ability to detect a single trophozoite of E. histolytica, outperforming even advanced PCR methods, makes it a powerful tool for diagnosing low-level infections [55]. When combined with its operational advantages—isothermal conditions, speed, and compatibility with simple, visual detection methods—LAMP emerges as a transformative technology. It is particularly suited for enhancing diagnostic capabilities in public health surveillance, field diagnostics, and resource-constrained laboratory environments, without compromising on sensitivity or specificity.
The COVID-19 pandemic has underscored the critical need for rapid, accurate, and accessible diagnostic testing to control disease transmission. Reverse Transcription-Polymerase Chain Reaction (RT-PCR) remains the gold standard for SARS-CoV-2 detection due to its high sensitivity and specificity [9]. However, the need for simpler and faster alternatives has propelled the development of methods like Loop-Mediated Isothermal Amplification (LAMP), a rapid molecular technique that can be deployed in resource-limited settings [14] [79]. This guide provides an objective comparison of the clinical sensitivity and specificity of RT-LAMP and RT-PCR, synthesizing current research data to inform researchers, scientists, and drug development professionals. Understanding the performance characteristics of these assays is crucial for selecting appropriate diagnostic tools based on specific testing scenarios, resource availability, and public health objectives.
Performance Comparison: RT-LAMP vs. RT-PCR
Extensive clinical validation studies have directly compared the performance of RT-LAMP and RT-PCR for SARS-CoV-2 detection. The following tables summarize key performance metrics and factors influencing them.
Table 1: Overall Clinical Performance Metrics of RT-LAMP vs. RT-PCR
| Assay Type | Sensitivity (%) | Specificity (%) | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Reference Standard |
|---|---|---|---|---|---|
| Real-time RT-LAMP (targeting orf8) | 84.13 (95% CI: 71.56–98.27) | 100 (95% CI: 78.38–100) | 100 (95% CI: 85.06–100) | 70.87 (95% CI: 55.55–89.11) | rRT-PCR [14] |
| One-Step RT-LAMP (targeting N gene) | 92.98 - 98.25 (Fluorometric) | 90.91 - 100 (Fluorometric) | Not Reported | Not Reported | RT-qPCR [79] |
| RT-qPCR (Gold Standard) | High (Approaching 100%) | High (Approaching 100%) | High | High | N/A |
Table 2: Impact of Sample Type and Viral Load on RT-LAMP Sensitivity
| Factor | Impact on RT-LAMP Sensitivity | Supporting Data |
|---|---|---|
| Viral Load | Sensitivity is significantly higher in samples with high viral load. | Sensitivity reaches 98-100% for samples with RT-PCR Ct values < 30 [14] [79]. |
| Sample Type (Extracted RNA) | High sensitivity comparable to RT-PCR. | One study reported 100% sensitivity for detecting SARS-CoV-2 in extracted RNA samples [19]. |
| Sample Type (Direct Swab) | Lower sensitivity compared to using extracted RNA. | One study reported sensitivity as low as 71% for direct swab samples without RNA extraction [19]. |
The data demonstrates that while RT-LAMP specificity is consistently high and often matches that of RT-PCR, its sensitivity is highly dependent on viral load and sample processing methods. RT-LAMP performs excellently in patients with high viral loads, typically present during the peak of infection.
Experimental Protocols for RT-LAMP
To ensure reproducibility and understand the basis of the performance data, below are detailed methodologies for key RT-LAMP experiments cited in this guide.
Protocol 1: Real-time RT-LAMP with Melting Curve Analysis
This protocol, adapted from a 2025 study, describes a fluorescent RT-LAMP assay performed in a real-time thermal cycler [14].
- Primer Set: A pre-designed set of six primers (F3, B3, FIP, BIP, LF, LB) targeting the SARS-CoV-2 orf8 gene.
- Reaction Setup:
- Master Mix: 12.5 µL of 2X LAMP Master Mix (e.g., WarmStart from New England Biolabs).
- Primers: 2.5 µL of a 10X primer mix.
- Detection Dye: 0.5 µL of a 50X fluorescence dye (e.g., FAM channel).
- Template: 5 µL of extracted RNA.
- Nuclease-Free Water: 4.5 µL to reach a final volume of 20 µL.
- Amplification Conditions:
- Temperature: 63 °C
- Time: 45 minutes
- Detection: Fluorescence acquisition every minute for 45 cycles on a real-time PCR detector (e.g., Bio-Rad CFX96).
- Post-Amplification Analysis:
- A melting curve analysis is performed immediately after amplification by heating from 63 °C to 95 °C. A characteristic peak on the melting curve verifies amplification specificity [14].
Protocol 2: One-Step RT-LAMP for Saliva and Nasopharyngeal Samples
This protocol, from a 2024 study, validates a one-step RT-LAMP assay for different sample types [20].
- Primer Design: Six primers (F3, B3, FIP, BIP, LF, LB) are designed to target the N gene of SARS-CoV-2 using Primer Explorer V5 software. Specificity is confirmed via Primer-BLAST.
- Reaction Setup:
- Reaction Volume: 25 µL
- Primers: 5 pmol each of F3/B3, 40 pmol each of FIP/BIP, 20 pmol each of LF/LB.
- Enzyme: 8 U of Bst DNA/RNA Polymerase 3.0 (New England Biolabs).
- Template: Extracted RNA from nasopharyngeal or saliva samples.
- Amplification and Readout:
The following workflow diagram visualizes the key steps and decision points in a typical RT-LAMP assay.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of RT-LAMP relies on a specific set of reagents and instruments. The table below details essential materials and their functions based on the cited protocols.
Table 3: Essential Reagents and Kits for SARS-CoV-2 RT-LAMP Assays
| Item | Function / Application | Example Brands / Types |
|---|---|---|
| Bst DNA/RNA Polymerase | The strand-displacing polymerase essential for isothermal amplification. | Bst 3.0 (New England Biolabs) [20] |
| LAMP Master Mix | Pre-mixed solution containing Bst polymerase, buffers, and dNTPs. | WarmStart Colorimetric or Fluorescent LAMP Master Mix (NEB) [14] [79] |
| Primer Sets | Specifically designed oligonucleotides that bind multiple regions of the target gene. | Custom designs for ORF1a, N, orf8 genes [14] [19] [20] |
| Fluorescence Dye | Intercalating dye for real-time fluorescence detection in thermal cyclers. | FAM channel dyes [14] |
| RNA Extraction Kit | For purifying viral RNA from clinical samples (swabs, saliva). | Viral RNA kits (e.g., Biorexfars, Qiagen) [80] [20] |
| Real-Time Thermal Cycler | Equipment for precise temperature control and real-time fluorescence monitoring. | CFX96 (Bio-Rad) [14] |
| Heating Block / Water Bath | Simple, low-cost alternative for constant temperature incubation. | Any device capable of maintaining 63°C [79] |
Both RT-LAMP and RT-PCR are highly specific for SARS-CoV-2 detection. The primary distinction lies in sensitivity, which for RT-LAMP is exceptionally high in high-viral-load samples but diminishes with lower viral loads and in direct swab protocols. The choice between assays should be guided by context: RT-PCR remains the unrivaled gold standard for confirmatory diagnostics where maximum sensitivity is required. In contrast, RT-LAMP offers a powerful, cost-effective alternative for rapid screening, point-of-care testing, and resource-limited environments, particularly when the goal is to identify individuals with high viral load who are most likely to be contagious [9].
In molecular biology and diagnostic fields, the time required to obtain a result is a critical parameter that can significantly impact research outcomes, clinical decision-making, and public health responses. Traditional polymerase chain reaction (PCR) methods have established the gold standard for nucleic acid detection due to their high sensitivity and specificity, but they inherently require multiple temperature cycles that extend processing times. In contrast, loop-mediated isothermal amplification (LAMP) has emerged as a rapid alternative that maintains high accuracy while dramatically reducing time-to-result. This comparison guide objectively analyzes the performance characteristics of these two technologies, with particular focus on their temporal efficiency within the broader context of sensitivity comparisons between LAMP, nested PCR (nPCR), and real-time PCR (RT-PCR) research. For researchers, scientists, and drug development professionals, understanding these trade-offs is essential for selecting the appropriate methodology for specific applications, whether in laboratory research, clinical diagnostics, or field-based testing.
Fundamental Technological Differences: Thermal Cycling vs. Isothermal Amplification
The profound difference in time-to-result between LAMP and PCR protocols stems from their fundamental operating principles. PCR relies on thermal cycling—typically 30-45 repeated cycles of denaturation (95°C), annealing (50-65°C), and extension (72°C)—which requires sophisticated instrumentation and creates inherent time delays during temperature transitions [81]. Each cycle must reach the precise target temperature before proceeding, with the entire process often taking 1.5 hours or more, particularly when incorporating reverse transcription for RNA targets or real-time fluorescent measurements [81].
In contrast, LAMP employs a strand-displacing DNA polymerase (such as Bst DNA polymerase) that operates at a constant temperature between 60-65°C, eliminating time-consuming temperature cycles [56] [82]. This polymerase displaces strands during synthesis, allowing amplification without an initial denaturation step. The reaction utilizes 4-6 primers recognizing 6-8 distinct regions of the target DNA, creating loop structures that facilitate subsequent rounds of amplification [82] [81]. This multi-primer design contributes to both the speed and exceptional specificity of the reaction. The amplification products are long concatemers (>20 kb) containing numerous repeats of the target sequence connected with single-stranded loop regions [82]. The following diagram illustrates the streamlined LAMP workflow compared to traditional PCR:
Direct Time-to-Result Comparison: Experimental Evidence
Multiple studies have directly compared the time efficiency of LAMP and PCR-based methods across various applications. The consistent finding is that LAMP significantly reduces time-to-result while maintaining high sensitivity and specificity.
Table 1: Time-to-Result Comparison Across Various Applications
| Application | LAMP Method & Time | PCR Method & Time | Time Reduction | Reference |
|---|---|---|---|---|
| SARS-CoV-2 Detection | RT-LAMP: 35-70 min [7] [20] | RT-qPCR: ~90 min [20] | ~40-60% faster | PMC ID: 8056478 |
| Fungal Pathogen Detection | LAMP: 60 min [27] | Conventional PCR: >2 hours [27] | ~50% faster | Frontiers in Microbiology, 2018 |
| Feline Calicivirus Detection | Colorimetric RT-LAMP: 70 min [22] | Conventional PCR + electrophoresis: >2 hours [22] | ~40% faster | Animals Journal, 2024 |
| Foodborne Bacteria Detection | LAMP: <60 min [56] | PCR: >90 min [56] | ~33% faster | Iranian Journal of Public Health, 2021 |
The time advantage of LAMP becomes particularly pronounced when considering the complete workflow, including detection. PCR typically requires additional post-amplification processing such as gel electrophoresis, which can add 30-60 minutes to the total time-to-result. In contrast, LAMP products can be detected in real-time through turbidity measurements or visual color changes using colorimetric indicators, enabling "yes/no" answers immediately after amplification [81]. This eliminates the need for post-amplification processing and further reduces the total analysis time.
Sensitivity and Specificity in the Context of Speed
While time-to-result represents a significant advantage for LAMP, its utility in research and diagnostics depends on maintaining acceptable sensitivity and specificity compared to established PCR methods. A 2021 meta-analysis comparing LAMP and PCR for detecting foodborne bacteria provides valuable insights, reporting LAMP sensitivity of 96.6% (95% CI: 95.0–97.7) versus PCR sensitivity of 95.6% (95% CI: 91.5–97.8), and LAMP specificity of 97.6% (95% CI: 92.6–99.3) versus PCR specificity of 98.7% (95% CI: 96.5–99.5) [56]. These results demonstrate that LAMP maintains competitive performance metrics while offering faster results.
The high specificity of LAMP stems from its use of 4-6 primers that must recognize 6-8 distinct regions within the target sequence, making amplification highly specific to the target organism [56]. This multi-primer approach provides an intrinsic specificity advantage over conventional PCR, which typically uses only two primers. However, it's important to note that sensitivity can be time-dependent. A study on SARS-CoV-2 detection found that RT-LAMP maintained 100% sensitivity and specificity compared to RT-qPCR up to 9 days after symptom onset, but sensitivity decreased to less than 25% after the 10th day, when viral loads typically decline [7]. This highlights how the diagnostic accuracy of both methods is influenced by factors beyond the technology itself, including disease progression and viral load.
Table 2: Sensitivity Comparison Across Molecular Detection Methods
| Detection Method | Target | Sensitivity | Specificity | Reference |
|---|---|---|---|---|
| LAMP | Alternaria solani | 10× more sensitive than conventional PCR [27] | Higher specificity than qPCR [27] | Frontiers in Microbiology, 2018 |
| nPCR | Feline calicivirus | 100× more sensitive than conventional PCR [22] | Higher than conventional PCR [22] | Animals Journal, 2024 |
| RT-LAMP | SARS-CoV-2 | 100% during early infection (<9 days) [7] | 100% during early infection (<9 days) [7] | International Journal of Infectious Diseases, 2021 |
| RT-qPCR | SARS-CoV-2 | Gold standard | Gold standard | PMC ID: 8056478 |
| One-Step RT-LAMP | SARS-CoV-2 | Detection at 1×10¹ dilution [20] | 100% specificity [20] | BMC Infectious Diseases, 2024 |
Detailed Experimental Protocols for Comparative Studies
SARS-CoV-2 Detection Protocol (RT-LAMP vs. RT-qPCR)
A 2021 study provides a direct comparison between RT-LAMP and RT-qPCR for SARS-CoV-2 detection [7]. The experimental protocol involved collecting 124 nasopharyngeal swab samples from 24 COVID-19 patients. RNA was extracted using the QIAamp Viral RNA Mini Kit on a QIAcube automated nucleic acid extraction device. For RT-LAMP, reactions were performed using the Loopamp SARS-CoV-2 Detection kit with a 25μL reaction volume containing 10μL of purified RNA, incubated at 62.5°C for 35 minutes in a Loopamp Real-time Turbidimeter. For RT-qPCR, one-step reactions were performed on a QuantStudio 1 Real-Time PCR System using TaqMan Fast Virus 1-Step Master Mix with 45 cycles of amplification. Samples were categorized by days from symptom onset (Group 1: ≤9 days; Group 2: 10-19 days; Group 3: 20-29 days; Group 4: ≥30 days) and tested with both methods. Results showed 100% concordance between RT-LAMP and RT-qPCR during the first 9 days after symptom onset, demonstrating equivalent diagnostic accuracy in the acute phase with significantly faster time-to-result for LAMP [7].
Plant Pathogen Detection Protocol (LAMP vs. PCR vs. nPCR vs. qPCR)
A comprehensive 2018 study compared LAMP with multiple PCR-based methods for detecting the fungal pathogen Alternaria solani [27]. DNA was extracted from mycelia using a commercial kit. LAMP reactions were optimized at 63°C for 60 minutes using specifically designed primers targeting the histidine kinase gene. Conventional PCR was performed with an initial denaturation at 95°C for 3 minutes, followed by 26 cycles of denaturation (95°C for 1 minute), annealing (58°C for 1 minute), and extension (72°C for 1 minute). Nested PCR involved two rounds of amplification using the conventional PCR protocol. qPCR was conducted with appropriate fluorescent probes. Sensitivity testing with serial dilutions of genomic DNA found LAMP to be 10-fold more sensitive than conventional PCR, though nested PCR was 100-fold more sensitive than LAMP, and qPCR was the most sensitive overall (10-fold more sensitive than nested PCR) [27]. Despite not having the absolute highest sensitivity, LAMP provided the best balance of speed, sensitivity, and procedural simplicity.
Research Reagent Solutions for LAMP and PCR Assays
Selecting appropriate reagents is crucial for implementing either LAMP or PCR methodologies. The following table outlines essential reagents and their functions for both techniques:
Table 3: Essential Research Reagents for Nucleic Acid Amplification
| Reagent Category | Specific Examples | Function & Importance | Compatibility |
|---|---|---|---|
| DNA Polymerase | Bst DNA Polymerase (NEB #M0374) [81], Bst-XT WarmStart DNA Polymerase [82] | Strand-displacing activity essential for LAMP; enables isothermal amplification | LAMP only |
| DNA Polymerase | Taq DNA Polymerase | Thermostable polymerase for PCR; lacks strand-displacement activity | PCR only |
| Master Mix | WarmStart 2X Colorimetric LAMP Master Mix [82] | Optimized buffer/dNTPs with visual detection; includes UDG for carryover prevention | LAMP only |
| Reverse Transcriptase | WarmStart RTx [81] | Reverse transcription for RNA targets; optimized for use in LAMP reactions | Primarily LAMP |
| Detection Reagents | Intercalating dyes (SYBR Green), Magnesium pyrophosphate, pH-sensitive dyes (phenol red) [82] [81] | Enable real-time or endpoint detection of amplification products | Both (with different applications) |
| Primer Design Tools | NEB LAMP Primer Design Tool [82], Primer Explorer V5 [20] | Design 4-6 primers recognizing 6-8 distinct regions for LAMP; critical for assay success | LAMP primarily |
Application-Specific Considerations and Decision Framework
The choice between LAMP and PCR methodologies depends heavily on the specific application requirements, available resources, and performance priorities. LAMP excels in field applications, point-of-care testing, and resource-limited settings due to its minimal equipment requirements, rapid results, and tolerance to inhibitors [81]. Its robust performance with crude sample preparations (such as leaf punches or saliva) enables applications where DNA extraction may be challenging [81]. Additionally, the visual detection capabilities of LAMP using colorimetric indicators make it particularly valuable for screening applications where a simple "yes/no" answer is sufficient.
In contrast, PCR-based methods remain essential for applications requiring precise quantification, such as gene expression analysis, or when the highest possible sensitivity is required, as in detection of low-abundance targets [81]. Quantitative PCR (qPCR) provides real-time monitoring of amplification and precise quantification of starting nucleic acid concentration, capabilities that LAMP lacks. Furthermore, PCR remains the preferred method for applications requiring subsequent manipulation of amplification products, such as cloning or sequencing, as LAMP generates complex concatemers that are not suitable for most downstream applications [82] [81].
The following decision diagram illustrates the process for selecting the appropriate molecular detection method based on application requirements:
The comparative analysis of time-to-result between LAMP assays and PCR protocols reveals a consistent pattern: LAMP provides significantly faster results (typically 30-70 minutes) compared to multi-hour PCR protocols while maintaining competitive sensitivity and specificity. This time advantage stems from fundamental methodological differences—specifically, LAMP's isothermal amplification using strand-displacing DNA polymerase versus PCR's thermal cycling requirement. For applications where speed, portability, and operational simplicity are prioritized over precise quantification, LAMP represents a superior alternative. This makes it particularly valuable for point-of-care diagnostics, field surveillance, and high-throughput screening applications. However, PCR-based methods maintain important advantages for quantitative applications, situations requiring the utmost sensitivity, and protocols involving downstream manipulation of amplified products. The decision framework presented enables researchers to select the optimal technology based on their specific requirements, ensuring appropriate methodological alignment with application needs. As both technologies continue to evolve, further reductions in time-to-result while maintaining or improving accuracy will remain a critical focus in molecular diagnostics development.
Entamoeba histolytica is a parasitic protozoan and the causative agent of amebiasis, a significant global health problem that causes an estimated 40-50 million cases of dysentery and liver abscess annually, resulting in up to 100,000 deaths worldwide each year [83] [84]. The accurate diagnosis of this pathogen presents a substantial challenge for clinicians and microbiologists because E. histolytica is morphologically identical to other non-pathogenic Entamoeba species, including E. dispar and E. moshkovskii, when examined by conventional microscopy [84]. This diagnostic limitation has profound clinical implications, as it can lead to either unnecessary treatment of individuals infected with non-pathogenic species or dangerous delays in treating invasive amebiasis.
Traditional microscopy, while widely available, suffers from critically limited sensitivity (under 60% for intestinal infection) and cannot differentiate between pathogenic and non-pathogenic Entamoeba species [85] [83]. Although antigen detection assays offer improved specificity, they face limitations including potential cross-reactions and reduced effectiveness with preserved stool samples [86]. Molecular methods have emerged as the gold standard for accurate detection and differentiation of Entamoeba species, with polymerase chain reaction (PCR) technologies now approved by the World Health Organization for this purpose [84]. Among these molecular techniques, significant performance differences exist between conventional PCR, nested PCR (nPCR), real-time PCR (qPCR), and the relatively newer loop-mediated isothermal amplification (LAMP) technology.
This case study provides a comprehensive comparative analysis of these four DNA-based amplification methods for detecting E. histolytica, with particular emphasis on their analytical sensitivity, specificity, and practical applicability in both research and clinical settings.
Comparative Performance Analysis
Side-by-Side Methodology Comparison
Table 1: Key Characteristics of DNA Amplification Methods for E. histolytica Detection
| Method | Target Gene | Amplification Conditions | Detection Method | Equipment Needs |
|---|---|---|---|---|
| LAMP | SREHP or rRNA genes | Isothermal (63°C, 60-120 min) | Gel electrophoresis, lateral flow, calcein-manganese dye | Heating block/water bath, UV light (for dye) |
| Conventional PCR | SREHP | Thermal cycling (30-40 cycles) | Gel electrophoresis | Thermal cycler, electrophoresis system |
| nPCR | SREHP | Two rounds of thermal cycling | Gel electrophoresis | Thermal cycler, electrophoresis system |
| qPCR | SREHP | Thermal cycling (40-50 cycles) | Fluorescence detection in real-time | Real-time PCR instrument |
Analytical Sensitivity and Detection Limits
A rigorous comparative analysis study conducted in 2020 provides compelling evidence for LAMP's superior sensitivity in detecting E. histolytica. This comprehensive investigation designed all primer sets to bind to the same location of the Serine-rich E. histolytica protein (SREHP) gene, ensuring an equitable comparison across platforms [1]. When evaluated using DNA extracted from stool samples spiked with known quantities of E. histolytica trophozoites, the results demonstrated striking differences in detection limits.
Table 2: Direct Comparison of Detection Limits for E. histolytica Amplification Methods
| Method | Limit of Detection (Trophozoites) | Amplification Time | Post-Amplification Analysis Required |
|---|---|---|---|
| LAMP | 1 | 60-120 minutes | Yes (multiple options available) |
| nPCR | 100 | >4 hours | Yes (gel electrophoresis) |
| qPCR | 100 | 2-3 hours | No |
| Conventional PCR | 1000 | 2-3 hours | Yes (gel electrophoresis) |
The exceptional sensitivity of LAMP, capable of detecting a single trophozoite, was consistently demonstrated across three different post-amplification detection methods: agarose gel electrophoresis, nucleic acid lateral flow immunoassay, and calcein-manganese dye techniques [1]. This remarkable sensitivity represents a 100-fold improvement over both nPCR and qPCR, and a 1000-fold improvement over conventional PCR. Earlier studies have corroborated these findings, with a 2009 report also establishing a detection limit of 1 parasite per reaction for LAMP targeting the small-subunit ribosomal DNA of E. histolytica [83].
Assay Specificity and Diagnostic Performance
The specificity of molecular diagnostic tests is equally crucial as sensitivity, particularly for distinguishing E. histolytica from morphologically similar species. The 2020 comparative study reported that the SREHP gene-specific LAMP primers demonstrated 100% specificity when evaluated against three medically important Entamoeba species and 75 other pathogenic microorganisms [1] [5]. This exceptional specificity ensures reliable differentiation between true E. histolytica infections and colonization by non-pathogenic Entamoeba species.
When deployed in field conditions with clinical samples, LAMP has maintained its robust performance characteristics. An evaluation of 130 clinical fecal samples found that LAMP detected E. histolytica with equal effectiveness to conventional nested PCR, while offering the advantages of rapid results and simpler equipment requirements [83]. The diagnostic accuracy of molecular methods substantially surpasses that of traditional techniques, with PCR-based methods consistently demonstrating superior sensitivity and specificity compared to antigen detection assays and microscopy [86] [84].
Experimental Protocols and Methodologies
LAMP Assay Protocol
The LAMP methodology for E. histolytica detection employs a sophisticated primer design system recognizing six to eight distinct regions of the target DNA, which contributes to its exceptional specificity and efficiency.
Primer Design: Primers are typically designed from highly specific gene targets such as the SREHP gene (GenBank accession numbers: M80910.1, M34438.1, XM_643162.2) or the small-subunit ribosomal DNA (X64142) [1] [83]. A standard LAMP primer set includes:
- F3 and B3: Outer primers that initiate the reaction
- FIP and BIP: Inner primers that form loop structures
- LF and LB (optional): Loop primers that accelerate amplification
Reaction Composition:
- 1.6 μM each inner primers (FIP and BIP)
- 0.2 μM each outer primers (F3 and B3)
- 1× reaction buffer [20 mM Tris-HCl (pH 8.8), 10 mM KCl, 8 mM MgSO₄, 10 mM (NH₄)₂SO₄, 0.1% Tween 20]
- 0.8 M betaine (added to facilitate strand separation)
- 1.4 mM of each deoxynucleoside triphosphate
- 5 μl extracted DNA template
- 1 μl Bst DNA polymerase (with strand displacement activity)
Amplification Conditions:
- Isothermal amplification at 63°C for 60-120 minutes
- Reaction termination at 90°C for 1-2 minutes
Detection Methods:
- Calcein-manganese dye: Visual color change from orange to green under ambient light
- Agarose gel electrophoresis: Characteristic ladder-like band pattern
- Lateral flow immunoassay: Using hapten-labeled primers for dipstick detection
- Turbidity: Monitoring magnesium pyrophosphate precipitate formation
Figure 1: LAMP Experimental Workflow for E. histolytica Detection
PCR-Based Method Protocols
Conventional PCR:
- Primers: Adapted from F2 region of Eh-FIP-SER (forward) and B2 region of Eh-BIP-SER (reverse) generating a 175 bp amplicon [1]
- Thermal cycling: 30-40 cycles of denaturation (92-95°C), annealing (50-60°C), and extension (72°C)
- Detection: Agarose gel electrophoresis with ethidium bromide or SYBR Safe staining
Nested PCR:
- Primary PCR: Outer primers Eh-F3-SER and Eh-B3-SER generating a 223 bp product [1]
- Secondary PCR: Uses primary PCR product as template with inner primers
- Advantage: Enhanced sensitivity and specificity through two amplification rounds
- Disadvantage: High contamination risk and longer processing time
Real-Time PCR (qPCR):
- Chemistry: SYBR Green or TaqMan probe-based detection
- Targets: Small subunit rRNA gene or SREHP gene
- Thermal cycling: 40-50 cycles with continuous fluorescence monitoring
- Advantage: Quantification capability and reduced contamination risk
- Disadvantage: Higher equipment costs and maintenance requirements
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for E. histolytica Molecular Detection
| Reagent/Chemical | Function | Application Notes |
|---|---|---|
| Bst DNA Polymerase | Isothermal amplification with strand displacement activity | Essential for LAMP; does not require thermal denaturation |
| Betaine | Reduces DNA secondary structure; enhances specificity | Critical for LAMP reaction efficiency |
| Calcein-Manganese Dye | Visual detection of amplification | Color change from orange to green indicates positive reaction |
| Primer Sets (SREHP-specific) | Target recognition and amplification | SREHP gene provides high specificity for E. histolytica |
| Lateral Flow Dipsticks | Immunoassay-based amplicon detection | Enables visual detection without specialized equipment |
| Guanidine Thiocyanate | DNA preservation and extraction | Maintains DNA integrity in stool samples |
Discussion: Implications for Research and Clinical Practice
The accumulated evidence demonstrates that LAMP technology offers significant advantages for E. histolytica detection, particularly in settings where resources, equipment, or technical expertise may be limited. The 100-fold higher sensitivity of LAMP compared to nPCR and qPCR translates to practical benefits in both clinical diagnostics and research applications [1]. This enhanced detection capability is particularly valuable for identifying low-level infections, monitoring treatment efficacy, and conducting epidemiological studies in endemic areas.
The isothermal nature of LAMP amplification eliminates the requirement for sophisticated thermal cycling equipment, substantially reducing both initial capital investment and ongoing maintenance costs [83] [86]. Furthermore, the availability of multiple detection formats, including visual color change methods, enables flexible implementation across diverse laboratory settings—from well-equipped reference facilities to basic field laboratories.
While qPCR offers the advantage of real-time quantification and faster amplification times (typically 30-40 minutes for qPCR versus 60-120 minutes for LAMP), it requires significantly more expensive instrumentation and may demonstrate slightly lower sensitivity according to comparative studies [1]. Recent advancements in qPCR methodology, including the use of droplet digital PCR (ddPCR) for optimizing primer-probe sets and establishing accurate cut-off values, continue to refine this technology [87]. However, the persistent challenges of false-positive reactions in stool specimens, as identified in recent studies, highlight the need for careful validation of any molecular diagnostic approach [87].
For clinical laboratories, the choice between these methodologies involves careful consideration of multiple factors, including testing volume, available resources, technical expertise, and intended application. LAMP presents a particularly compelling option for rapid screening, outbreak investigations, and point-of-care testing scenarios where equipment limitations preclude the use of PCR-based methods.
This comprehensive comparison establishes LAMP as a superior molecular platform for E. histolytica detection when analytical sensitivity is the primary consideration. With a demonstrated limit of detection of a single trophozoite—surpassing nPCR and qPCR by two orders of magnitude—coupled with minimal equipment requirements and flexible detection options, LAMP technology represents a transformative advancement in parasitic disease diagnostics [1] [5]. The method's 100% specificity against numerous related pathogens further reinforces its diagnostic utility [1].
For researchers and clinicians working in both resource-limited and well-equipped settings, LAMP offers a robust, reliable, and accessible alternative to PCR-based methods. Its implementation can enhance diagnostic accuracy, facilitate early detection of invasive amebiasis, and support public health interventions through improved epidemiological monitoring. As molecular technologies continue to evolve, LAMP stands as a particularly promising tool for advancing the global fight against amebiasis and other neglected tropical diseases.
Equipment and Cost-Benefit Analysis for Resource-Limited and High-Throughput Settings
Molecular diagnostics are cornerstone technologies in clinical research, pathogen detection, and drug development. The selection of an appropriate amplification platform directly influences the accuracy, speed, and cost-effectiveness of experimental and diagnostic outcomes. Within the context of a broader thesis on sensitivity comparison of Loop-Mediated Isothermal Amplification (LAMP) versus nested PCR (nPCR) and Reverse Transcription-PCR (RT-PCR), this guide provides an objective comparison of these technologies. We focus specifically on their performance characteristics, equipment requirements, and cost-benefit profiles tailored for both resource-limited and high-throughput settings. By synthesizing recent experimental data, this analysis aims to equip researchers, scientists, and drug development professionals with the evidence needed to make informed platform selections for their specific applications.
Performance Comparison: Sensitivity, Specificity, and Speed
The analytical sensitivity, specificity, and turnaround time are primary determinants when selecting a molecular amplification method. A direct comparative analysis study provides crucial experimental data for objective evaluation.
Table 1: Comparative Analytical Performance of LAMP, nPCR, and qPCR
| Method | Limit of Detection (LoD) | Amplification Time | Specificity | Key Findings |
|---|---|---|---|---|
| LAMP | 1 trophozoite [1] | 30-60 min [88] [20] [89] | 100% [1] | Outperformed all PCR variants in sensitivity and speed [1]. |
| nPCR | 100 trophozoites [1] | 2-4 hours (including post-PCR analysis) [1] | High (but susceptible to amplicon contamination) [1] | Two-step procedure increases risk of cross-contamination [1]. |
| qPCR/RT-qPCR | 100 trophozoites [1] | 60-120 min [19] | High [9] [19] | Considered the gold standard for SARS-CoV-2 detection; allows for quantification [88] [19]. |
The data demonstrates that LAMP can provide superior sensitivity and significantly faster results than traditional PCR-based methods. This makes it a powerful tool for applications where rapid detection of low pathogen load is critical. Furthermore, the simplicity of the readout—often a visual color change—reduces reliance on complex instrumentation [1] [89]. However, RT-qPCR remains the validated gold standard in many clinical contexts and provides the added advantage of quantitative results [88] [19].
Cost-Benefit and Operational Analysis
Beyond pure performance, the economic and operational feasibility of implementing a technology is a key consideration, especially in resource-constrained environments.
Table 2: Operational and Cost-Benefit Analysis of Testing Platforms
| Parameter | LAMP | RT-qPCR | nPCR |
|---|---|---|---|
| Equipment Cost | Low (water bath, heat block, portable incubator) [89] | High (expensive thermocycler) [20] [19] | Moderate to High (thermocycler) |
| Assay Cost per Reaction | Low-cost [20] [89] | Higher cost [20] | Moderate |
| Technical Skill Required | Low [89] | High (requires trained personnel) [19] | High (high contamination risk) [1] |
| Turnaround Time | 15-45 min [20] [89] | Several hours (including extraction) [20] [19] | 2-4 hours [1] |
| Throughput | Suitable for field and point-of-care use [89] [29] | High-throughput in centralized labs [9] | Lower due to complex, multi-step process [1] |
| Key Cost-Benefit Insight | Most cost-effective for rapid, on-site screening [9] [23] [89] | High cost justified for gold-standard, quantitative results in central labs [19] | Less cost-effective due to longer time and high contamination risk [1] |
Stochastic modeling of COVID-19 testing strategies confirms that while daily screening with RT-PCR is highly effective, it incurs higher costs. Symptom-based testing with rapid methods like LAMP or antigen tests offers a more cost-effective alternative for outbreak control, particularly in settings with limited resources [9] [23].
Equipment and Infrastructure Requirements
The core equipment needed for each method directly impacts its portability, setup cost, and suitability for different settings.
Research Reagent Solutions and Essential Materials
Table 3: Key Reagent Solutions and Equipment for Molecular Amplification
| Item | Function/Description | LAMP | nPCR | RT-qPCR |
|---|---|---|---|---|
| Bst DNA Polymerase | Enzyme with strand displacement activity for isothermal amplification. | Required [1] | Not Used | Not Used |
| Taq DNA Polymerase | Thermostable enzyme for PCR amplification. | Not Used | Required [1] | Required |
| Reverse Transcriptase | Enzyme for synthesizing cDNA from RNA templates. | Required (for RT-LAMP) [20] | Required (for RT-nPCR) | Required [20] |
| Primers | Oligonucleotides that bind to the target sequence. | 4-6 primers per target [88] [20] | 2 sets of primers per target [1] | 1 primer pair, often with a probe [88] |
| Colorimetric Dye | Allows visual detection of amplification (e.g., calcein, phenol red). | Often Used [1] [89] | Not Typically Used | Not Used |
| Intercalating Dye / Probe | For fluorescence-based detection. | Optional (e.g., EvaGreen) [89] | Ethidium Bromide (post-run) | Required (e.g., SYBR Green, TaqMan) [20] |
| Thermal Cycler | Instrument for precise temperature cycling. | Not Required | Required [1] | Required [19] |
| Isothermal Incubator | Maintains a constant temperature (60-65°C). | Required (simple heat block or water bath) [89] | Not Required | Not Required |
Experimental Protocols and Workflow
The experimental workflow, from sample to result, varies significantly between these methods, impacting their application.
Detailed Protocol: RT-LAMP Assay
A typical protocol for detecting RNA viruses (e.g., SARS-CoV-2) via RT-LAMP is as follows [20] [89]:
- Reaction Setup: Prepare a 25 µL reaction mixture containing:
- 12.5 µL of 2x LAMP master mix (e.g., WarmStart LAMP Kit).
- Primers: 1.6 µM each of FIP and BIP, 0.2 µM each of F3 and B3, and 0.4 µM each of LF and LB.
- 1 µL of Bst DNA/RNA Polymerase (8 U/µL).
- 3-5 µL of extracted RNA template or direct sample.
- Amplification: Incubate the reaction tube at a constant temperature of 60-65°C for 15-45 minutes. This can be performed in a thermos with hot water, a heat block, or a portable incubator [89].
- Result Detection: Visually inspect for a color change if a colorimetric dye (e.g., phenol red) is used. Alternatively, use a portable fluorescence reader or a simple DIY device with a blue LED and an orange filter to detect fluorescence under a dark field [89].
Detailed Protocol: nPCR Assay
A standard nPCR protocol for DNA targets involves two successive rounds of amplification [1]:
- First Round PCR:
- Prepare a reaction mix with recombinant Taq DNA polymerase, outer primer set (e.g., Eh-F3-SER and Eh-B3-SER), dNTPs, buffer, and DNA template.
- Run in a thermal cycler with an initial denaturation (95°C for 3-5 min), followed by 25-35 cycles of denaturation (95°C for 15-30s), annealing (primer-specific temperature for 30s), and extension (72°C for 30-60s), with a final extension at 72°C for 5 min.
- Second Round PCR:
- Use 1-2 µL of the first-round PCR product as a template in a new reaction mixture containing the inner, nested primer set (e.g., primers from the F2 and B2 regions).
- Repeat the thermal cycling profile as in the first round.
- Result Detection: Analyze the final PCR product by agarose gel electrophoresis, which requires additional time and equipment [1].
Workflow Visualization
The following diagram summarizes and compares the key steps involved in each method, highlighting differences in complexity and time investment.
The choice between LAMP, nPCR, and RT-qPCR is not a matter of identifying a universally superior technology, but rather of selecting the right tool for the specific research or diagnostic context.
- For Resource-Limited and Point-of-Care Settings: LAMP is the unequivocal leader. Its minimal equipment requirements, low per-test cost, rapid turnaround, and high sensitivity make it ideal for field deployment, remote clinics, and rapid screening programs [9] [89] [29]. The ability to use direct samples or simple extraction methods further enhances its utility in these environments.
- For High-Throughput Centralized Laboratories: RT-qPCR remains the gold standard for applications requiring high precision and quantification. Its scalability, automation potential, and quantitative output justify the higher equipment and operational costs in well-funded clinical or research labs [9] [19].
- Nested PCR's Niche: Given its procedural complexity, longer turnaround time, and high contamination risk, nPCR is increasingly being superseded by qPCR and LAMP. Its use may be justified in specific research applications where maximizing sensitivity for a particular DNA target is paramount and no alternative primers for qPCR or LAMP are available.
In summary, the ongoing research into LAMP technology is steadily expanding its applications and reliability. For a broad range of qualitative detection needs, particularly where speed, cost, and portability are critical, LAMP presents a powerful and often superior alternative to conventional PCR-based methods.
Conclusion
The comparative analysis reveals that LAMP, nPCR, and RT-PCR each occupy a distinct niche in molecular diagnostics. LAMP excels as a rapid, highly sensitive point-of-care test, with studies showing it can outperform conventional PCR and match RT-PCR sensitivity in the early phases of infections like COVID-19, while demonstrating a 100-fold greater sensitivity than nPCR for detecting Entamoeba histolytica. nPCR offers exceptional specificity and sensitivity for complex samples but is hampered by a longer turnaround time and high contamination risk. RT-PCR remains the gold standard for quantification, offering robust performance but requiring sophisticated equipment. The choice of technique is not one of superiority but of context. Future directions point toward integrated systems combining LAMP's speed with melting curve analysis for multiplexing, and the development of lyophilized, equipment-free LAMP kits to democratize advanced molecular diagnostics in field and primary care settings, ultimately accelerating drug development and personalized medicine.
References
- 1. a comparative analysis study of LAMP, conventional PCR ... [https://bmcbiotechnol.biomedcentral.com/articles/10.1186/s12896-020-00629-8]
- 2. LAMP Primer Design Tool [https://primerdigital.com/tools/lamp.html]
- 3. Loop-Mediated Isothermal Amplification [https://www.neb.com/en-us/applications/dna-amplification-pcr-and-qpcr/isothermal-amplification/loop-mediated-isothermal-amplification-lamp?srsltid=AfmBOoqWX8mhmyTUI5p2APj7pk3Q3wqhtXXWDHWV5E57MLrKmiZDmiar]
- 4. Optimization of loop-mediated isothermal amplification ... [https://www.nature.com/articles/s41598-024-72228-y]
- 5. A Comparative Analysis Study of LAMP, Conventional PCR ... [https://pubmed.ncbi.nlm.nih.gov/32571286/]
- 6. Optimization of loop-mediated isothermal amplification (LAMP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8757654/]
- 7. Diagnostic accuracy of LAMP versus PCR over the course of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8056478/]
- 8. A rapid Loop-Mediated Isothermal Amplification (LAMP) ... [https://www.sciencedirect.com/science/article/pii/S3050632825000058]
- 9. Modeling the effectiveness of RT-PCR, RT-LAMP, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535133/]
- 10. Comparison of diagnostic performance of RT-qPCR ... [https://www.sciencedirect.com/science/article/pii/S1876034123001648]
- 11. Comparison of real-time PCR and nested PCR based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11153442/]
- 12. Comparison of RT-PCR, RT-nested PCRs, and real-time ... [https://www.nature.com/articles/s41598-021-96066-4]
- 13. Nucleic acid amplification techniques for the detection of ... [https://www.sciencedirect.com/science/article/pii/S1201971221006949]
- 14. An alternative real-time fluorescence reverse transcription ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204207/]
- 15. rapid detection of viruses in surface water and wastewater [https://pubs.rsc.org/en/content/articlehtml/2025/ew/d5ew00092k]
- 16. Sensitive and specific LAMP and multiplex qRT-PCR ... [https://www.sciencedirect.com/science/article/pii/S0732889325000070]
- 17. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 18. Comparative Analysis of RT-PCR and a Colloidal Gold ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154499/]
- 19. Comparison of RT-LAMP and RT-qPCR assays for ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093423001969]
- 20. Evaluation and comparison of one-step real-time PCR and ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09574-9]
- 21. An alternative colorimetric RT-LAMP assay for the rapid ... [https://jidc.org/index.php/journal/article/view/39288391]
- 22. Comparison of PCR, Nested PCR, and RT-LAMP for Rapid ... [https://www.mdpi.com/2076-2615/14/16/2432]
- 23. Modeling the effectiveness of RT-PCR, RT-LAMP, and antigen ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11793-7]
- 24. Performance Comparison and Clinical Evaluation of Three ... [https://brieflands.com/articles/jjm-156608]
- 25. of Comparison with Other... | MyBioSource Learning Center PCR [https://www.mybiosource.com/learn/comparison-of-pcr-with-other-nucleic-acid-amplification-techniques/]
- 26. Quantitative mRNA expression measurement at home [https://www.nature.com/articles/s41598-023-49651-8]
- 27. Frontiers | Comparative Evaluation of the LAMP Assay and... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.02089/full]
- 28. Comparison of RT-PCR, RT-LAMP, and Antigen ... [https://pubmed.ncbi.nlm.nih.gov/34588370/]
- 29. Development and Validation of a Combined RT-LAMP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898505/]
- 30. Comparison of diagnostic performance of RT-qPCR, RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10170900/]
- 31. PCR past, present and future - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7439763/]
- 32. Reverse transcription polymerase chain reaction [https://en.wikipedia.org/wiki/Reverse_transcription_polymerase_chain_reaction]
- 33. Advancements and applications of loop-mediated ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1406632/full]
- 34. Loop mediated isothermal amplification (LAMP) as a rapid ... [https://www.nature.com/articles/s41598-025-18738-9]
- 35. LAMP Reagents in the Real World: 5 Uses You'll Actually ... [https://www.linkedin.com/pulse/lamp-reagents-real-world-5-uses-youll-actually-vw6ec/]
- 36. Development and validation of a multi-platform LAMP system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619727/]
- 37. Evaluation of RT-LAMP for SARS-CoV-2 Detection in ... [https://www.mdpi.com/1999-4915/17/6/783]
- 38. Diagnostic utility and validation of a newly developed real ... [https://www.sciencedirect.com/science/article/pii/S2667038022000205]
- 39. Colorimetric RT-LAMP SARS-CoV-2 diagnostic sensitivity ... [https://www.nature.com/articles/s41598-021-88506-y]
- 40. Primer design for quantitative real-time PCR for the emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7330846/]
- 41. Loop-Mediated Isothermal Amplification [https://www.neb.com/en-us/applications/dna-amplification-pcr-and-qpcr/isothermal-amplification/loop-mediated-isothermal-amplification-lamp?srsltid=AfmBOoogEeYQmZO-a7QQqpqtKQjv-gvp_jC2GC6W_M_aDSjlt-W41JoP]
- 42. Method for colorimetric of double-stranded nucleic acid... detection [https://pubmed.ncbi.nlm.nih.gov/25575759/]
- 43. Determination of limit of detection (LOD) for loop-mediated ... [https://www.sciencedirect.com/science/article/abs/pii/S0732889324003924]
- 44. Loop-Mediated Isothermal Amplification Assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3187296/]
- 45. A new method to prevent carry-over contaminations in two ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4787772/]
- 46. Preventing PCR Amplification Carryover Contamination in ... [https://www.annclinlabsci.org/content/34/4/389.long]
- 47. A diagnostic accuracy study comparing RNA LAMP, direct ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1063414/full]
- 48. How to prevent PCR contamination [https://www.minipcr.com/how-to-prevent-pcr-contamination/]
- 49. 6 Ways to Minimize Contamination during PCR [https://www.labclinics.com/2019/07/22/six-ways-to-minimize-contamination-during-pcr/?lang=en]
- 50. Optimizing PCR Workflows: 4 Strategies for Lab Managers [https://www.labmanager.com/optimizing-pcr-workflows-4-strategies-for-lab-managers-33688]
- 51. Understanding Ct Values in Real-Time PCR [https://www.thermofisher.com/blog/behindthebench/understanding-ct-values/]
- 52. Web-based LinRegPCR: application for the visualization and ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-021-04306-1]
- 53. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOooqERXbgcZ_ShBgxMjRUZlpuVboyj-RRFxl02csT2sCre_q4O46]
- 54. An R package for qPCR data processing and visualization [https://pmc.ncbi.nlm.nih.gov/articles/PMC9513427/]
- 55. Loop-mediated isothermal amplification (LAMP) reaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7310076/]
- 56. The Sensitivity and Specificity of Loop-Mediated Isothermal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8826321/]
- 57. Evaluation of molecular inhibitors of loop-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10928092/]
- 58. Development of an optimized colorimetric RT-LAMP for ... [https://www.nature.com/articles/s41598-022-25872-1]
- 59. Optimization of a loop-mediated isothermal amplification ... [https://www.sciencedirect.com/science/article/pii/S1056617124001119]
- 60. Development and evaluation of an improved quantitative ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914018308440]
- 61. of Comparison - RT , RT-nested PCRs, and real-time PCR for... PCR [https://www.nature.com/articles/s41598-021-96066-4?error=cookies_not_supported&code=9497fcd0-0dab-43e6-9165-078f24362741]
- 62. Impact of Primer Dimers and Self-Amplifying Hairpins on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5922443/]
- 63. A molecular test based on RT-LAMP for rapid, sensitive ... [https://www.nature.com/articles/s41598-021-95799-6]
- 64. The screening value of RT-LAMP and RT-PCR in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8629515/]
- 65. The Impact of the Variability of RT-qPCR Standard Curves ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12029521/]
- 66. Analyzing qPCR data: Better practices to facilitate rigor and ... [https://www.sciencedirect.com/science/article/pii/S2405580825004431]
- 67. Analysis of qPCR Data: From PCR Efficiency to Absolute ... [https://www.preprints.org/manuscript/202510.2485]
- 68. Diagnostic accuracy of LAMP versus PCR over the course ... [https://www.sciencedirect.com/science/article/pii/S1201971221003295]
- 69. Development and Optimization of a Multiplex Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10948217/]
- 70. Optimization of the real-time PCR platform method using ... [https://www.nature.com/articles/s41598-025-16972-9]
- 71. Methylene blue as a new signal tracer for nucleic acid ... [https://www.nature.com/articles/s41598-025-19701-4]
- 72. Beyond Traditional Lateral Flow Assays: Enhancing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853705/]
- 73. Experimental validation of novel and conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC167648/]
- 74. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 75. Limit of Detection | National Exposure Report [https://www.cdc.gov/environmental-exposure-report/php/about-the-data/limit-of-detection.html]
- 76. Diagnostic Methods for Non-Falciparum Malaria - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8248680/]
- 77. Comparative Evaluation of PCR-Based, LAMP and RPA- ... [https://www.mdpi.com/1422-0067/25/11/5773]
- 78. Comparative evaluation of loop-mediated isothermal ... [https://www.sciencedirect.com/science/article/abs/pii/S0014489419303376]
- 79. Standardization and performance of SARS-CoV-2 RT- ... [https://pubmed.ncbi.nlm.nih.gov/40956555/]
- 80. Performance of novel digital real-time PCR for detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403756/]
- 81. Getting started with loop-mediated isothermal amplification ... [https://www.neb.com/en-us/nebinspired-blog/getting-started-with-loop-mediated-isothermal-amplification?srsltid=AfmBOorxp1giovFTmOhxwNOM5nZtuz37K7OYCOL0EXLuw8nwXf7_L2Nl]
- 82. Loop-Mediated Isothermal Amplification [https://www.neb.com/en-us/applications/dna-amplification-pcr-and-qpcr/isothermal-amplification/loop-mediated-isothermal-amplification-lamp?srsltid=AfmBOoqeKO4-EZGKMIhsIhPBEJs2eP_oNayLyJWl0H4-FDQVcO9yzaFB]
- 83. Development of Loop-Mediated Isothermal Amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2691116/]
- 84. Real-time PCR assay in differentiating Entamoeba histolytica ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3765902/]
- 85. Entamoeba histolytica (Amebiasis) – Microscopy, Antigen, ... [https://www.publichealthontario.ca/en/Laboratory-Services/Test-Information-Index/Amebiasis-PCR]
- 86. Detection of Entamoeba histolytica by Recombinase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4559702/]
- 87. Optimization of TaqMan-based quantitative PCR diagnosis ... [https://pubmed.ncbi.nlm.nih.gov/40472050/]
- 88. Effectivity of RT‐PCR to the RT‐LAMP - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9015626/]
- 89. Rapid On-Site Detection of SARS-CoV-2 Using RT-LAMP ... [https://www.mdpi.com/2079-6374/13/7/724]