Modern Clinical Virology Diagnostics: Integrating PCR, Serology, and Emerging Technologies for Research and Drug Development
This article provides a comprehensive overview of contemporary viral diagnostic techniques, focusing on the principles, applications, and limitations of polymerase chain reaction (PCR) and serological assays.
Modern Clinical Virology Diagnostics: Integrating PCR, Serology, and Emerging Technologies for Research and Drug Development
Abstract
This article provides a comprehensive overview of contemporary viral diagnostic techniques, focusing on the principles, applications, and limitations of polymerase chain reaction (PCR) and serological assays. Tailored for researchers, scientists, and drug development professionals, it explores the foundational science behind these methods, their practical implementation in clinical and research settings, strategies for optimization and troubleshooting, and their comparative validation. The content synthesizes current literature to address the critical need for accurate pathogen detection, seroprevalence studies, and therapeutic monitoring, while also examining the future trajectory of diagnostic technologies including high-throughput sequencing and their implications for biomedical innovation.
The Pillars of Viral Detection: Understanding PCR and Serology Fundamentals
In the field of clinical virology, the Polymerase Chain Reaction (PCR) has revolutionized the detection and diagnosis of viral pathogens by enabling the exponential amplification of specific viral genetic material from minimal sample input. This core technology allows researchers and clinicians to identify infections with exceptional sensitivity and specificity, even during early stages when viral loads are low or in asymptomatic individuals [1]. Molecular detection techniques, primarily PCR and its advanced derivatives, have become foundational tools for diagnosing diseases such as COVID-19, monitoring treatment efficacy, and conducting public health surveillance [2] [3]. The principle of PCR revolves around the in vitro enzymatic replication of target DNA sequences through repetitive thermal cycling, facilitating the billion-fold amplification of a specific genomic region flanked by primer binding sites, which can then be detected and analyzed [2] [4]. This technical note details the methodological principles, procedural protocols, and key applications of PCR in viral detection, providing a framework for its implementation in research and diagnostic settings.
Fundamental Principles of PCR and Viral Genetic Material Amplification
The core objective of PCR in virology is to selectively amplify a unique sequence within a virus's genome, making detectable what was initially present in quantities too low for direct analysis. The process relies on the complementary base pairing of nucleotides (A-T and G-C for DNA) and a thermostable DNA polymerase to synthesize new DNA strands. Most human viral pathogens, however, are RNA viruses (e.g., SARS-CoV-2, Influenza), which necessitates an initial reverse transcription step to convert viral RNA into complementary DNA (cDNA) before standard PCR amplification can begin [1]. This combined approach is referred to as Reverse Transcription-PCR (RT-PCR).
The amplification process occurs in three fundamental steps that are repeated for 25-45 cycles [4]:
- Denaturation: The double-stranded DNA template is heated to ~95°C, causing the strands to separate.
- Annealing: The temperature is lowered to 50-65°C, allowing short, synthetic oligonucleotide primers to bind (anneal) to their complementary sequences on either side of the target viral gene.
- Extension: The temperature is raised to ~72°C, the optimal temperature for a thermostable DNA polymerase (e.g., Taq polymerase) to extend the primers by adding nucleotides to synthesize new DNA strands.
Each cycle theoretically doubles the amount of the target DNA sequence, leading to an exponential accumulation of the specific amplicon (the amplified product) that can be visualized, quantified, or sequenced [2].
Evolution of PCR Technologies in Viral Detection
Since its inception, PCR technology has diversified significantly, giving rise to advanced formats that enhance quantification, multiplexing, and absolute detection capabilities. The table below summarizes the key PCR methodologies and their relevance to clinical virology.
Table 1: Key PCR Methodologies and Their Applications in Viral Detection
| Technology | Core Principle | Key Advantages | Primary Virology Applications |
|---|---|---|---|
| Traditional PCR | Endpoint detection of amplified DNA via gel electrophoresis. | Simplicity, low cost, equipment accessibility. | Qualitative detection of viral presence; cloning target genes [2]. |
| Nested PCR | Two consecutive amplification rounds with two primer sets. | Enhanced specificity and sensitivity; reduces false positives. | Detection of pathogens with low viral loads [2]. |
| Quantitative Real-Time PCR (qPCR) | Fluorescence-based monitoring of amplification in real-time. | High sensitivity, broad dynamic range, precise quantification of viral load. | Gold standard for diagnosis and monitoring of many viral infections (e.g., HIV, HCV, SARS-CoV-2) [2] [5] [1]. |
| Digital PCR (dPCR) | Partitioning of sample into thousands of individual reactions for absolute quantification. | Absolute quantification without standard curves; superior precision and sensitivity for low-abundance targets; high resistance to inhibitors. | Detection of low-level viremia, viral reservoir monitoring, and quantification of minor variants [6] [2]. |
| Multiplex PCR | Simultaneous amplification of multiple targets in a single reaction using multiple primer pairs. | High throughput, cost efficiency, capacity for co-infection detection and internal controls. | Panels for respiratory viruses (e.g., Influenza, RSV, SARS-CoV-2) and gastrointestinal viruses [2]. |
Performance Comparison: qPCR vs. dPCR
A recent 2025 study directly compared the performance of multiplex dPCR with qPCR for detecting periodontal pathobionts, providing insights applicable to viral load quantification. The findings are summarized in the table below.
Table 2: Comparative Analytical Performance of dPCR versus qPCR [6]
| Performance Parameter | qPCR Performance | dPCR Performance | Implications for Viral Detection |
|---|---|---|---|
| Linearity (R²) | High | >0.99 | Both methods show excellent correlation across a wide range of target concentrations. |
| Intra-assay Precision (CV%) | Lower | Higher (Median CV%: 4.5%) | dPCR provides more reproducible and reliable measurements between technical replicates. |
| Sensitivity at Low Loads | Prone to false negatives at <3 log10Geq/mL | Superior; reliably detects low copy numbers | dPCR is advantageous for detecting early infection or latent viruses with very low viral loads. |
| Accuracy & Agreement | Comparable at medium/high loads | Comparable at medium/high loads | Both methods are reliable for quantifying moderate to high viremia. |
| Quantification Basis | Relative to a standard curve | Absolute via Poisson statistics | dPCR eliminates the need for calibration curves, simplifying workflow and reducing potential variability. |
Experimental Protocols for PCR-Based Viral Detection
Sample Collection and Nucleic Acid Extraction
The accuracy of PCR begins with proper sample collection. For respiratory viruses like SARS-CoV-2, this typically involves a pharyngeal swab [1]. The swab is immediately placed in viral transport media and should be stored at -20°C or colder if processing is delayed. Viral RNA extraction is then performed using commercial kits (e.g., QIAamp DNA Mini kit) or automated extraction systems, which isolate and purify nucleic acids from proteins, inhibitors, and other cellular debris [6] [1]. The purity and concentration of the extracted RNA/DNA should be verified using a spectrophotometer [1].
Reverse Transcription and PCR Amplification
For RNA viruses, the purified RNA is converted to cDNA. A typical reaction uses a reverse transcriptase enzyme (e.g., SuperScript III), dNTPs, and either random hexamers or gene-specific primers [1].
The following protocol details a standard setup for a real-time PCR (qPCR) reaction, which is the workhorse for modern viral diagnostics.
Table 3: Standard qPCR Reaction Setup [4] [1]
| Component | Final Concentration/Amount | Function |
|---|---|---|
| PCR Master Mix (2X) | 10 µL | Contains Taq DNA polymerase, dNTPs, MgCl₂, and optimized buffer. |
| Forward Primer | 0.2 - 0.4 µM | Binds to the complementary sequence on one strand of the target DNA. |
| Reverse Primer | 0.2 - 0.4 µM | Binds to the complementary sequence on the opposite strand. |
| Hydrolysis Probe (e.g., TaqMan) | 0.1 - 0.2 µM | Provides sequence-specific fluorescence signal during amplification. |
| Template DNA/cDNA | 2-5 µL | The sample containing the target viral genetic sequence. |
| Nuclease-free Water | To 20 µL | Adjusts the final reaction volume. |
Thermal Cycling Protocol:
- Initial Denaturation: 95°C for 2-5 minutes (activates polymerase, denatures template).
- Amplification Cycle (Repeat 40-45 times):
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 58-60°C for 30-60 seconds (temperature and duration depend on primer/probe design). Fluorescence is measured at this step.
- Final Hold: 4°C for ∞.
Primer and Probe Design Guidelines
False-positive results can occur with unoptimized primer sets, highlighting the critical need for careful design and validation [1]. The following three-step guideline ensures specificity and sensitivity:
- Target Selection: Select highly conserved and unique regions within the viral genome (e.g., RdRP, N, E, and S genes for SARS-CoV-2) to ensure specificity and avoid cross-reactivity with human or other microbial genomes [1].
- In Silico Validation: Analyze primer and amplicon sequences using software (e.g., Oligo 7, DNASTAR Lasergene) to check for secondary structures, self-dimers, heterodimers, and ensure optimal melting temperatures (Tm) [7] [1].
- Experimental Optimization: Empirically test primer concentrations and annealing temperatures to maximize specific amplification and eliminate spurious primer-dimer artifacts [1].
Advanced Considerations and Troubleshooting
Challenges in Multi-Template PCR
In applications like multiplex PCR or viral metagenomics, simultaneous amplification of multiple targets can lead to skewed abundance data due to sequence-specific differences in amplification efficiency [8]. Recent advances use deep learning models (1D-CNNs) to predict a sequence's amplification efficiency based on its sequence alone, identifying motifs that lead to poor amplification. This allows for the design of better assays and more accurate quantitative results [8].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for PCR-Based Viral Detection
| Reagent / Kit | Function / Application | Example Use Case |
|---|---|---|
| Taq DNA Polymerase | Thermostable enzyme for DNA synthesis during PCR amplification. | Core enzyme in standard and real-time PCR protocols [4]. |
| QIAcuity dPCR Kit (Qiagen) | Reagents and nanoplate for performing digital PCR. | Absolute quantification of viral load with high precision [6]. |
| QIAamp DNA Mini Kit (Qiagen) | Silica-membrane technology for purification of viral DNA/RNA. | Nucleic acid extraction from clinical swab samples [6]. |
| SuperScript III First-Strand Synthesis System | Reverse transcription of RNA into cDNA. | Essential first step for detecting RNA viruses via RT-PCR [1]. |
| Primer/Probe Sets | Sequence-specific oligonucleotides for target binding and detection. | Detection of specific viral genes (e.g., SARS-CoV-2 E-gene) [1]. |
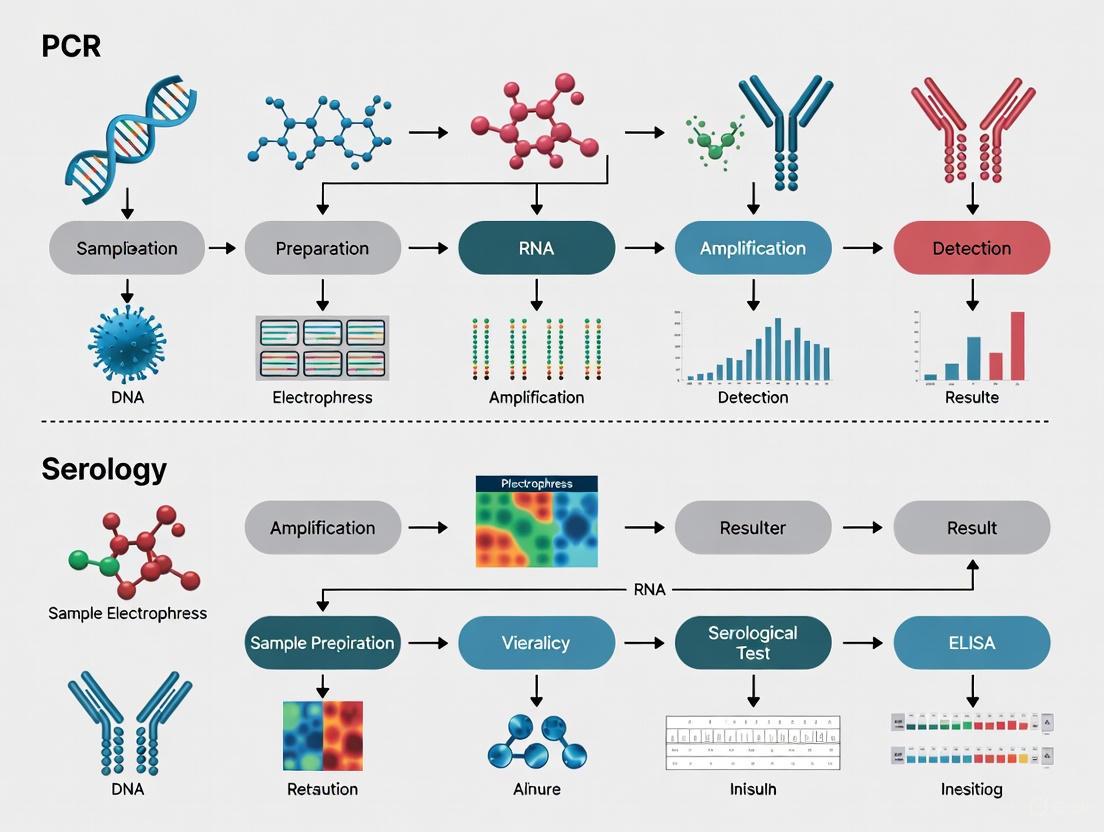
Workflow Diagram: PCR in Viral Detection
The following diagram illustrates the end-to-end workflow for molecular detection of viruses using RT-qPCR, from sample collection to result interpretation.
Diagram 1: Viral Detection via RT-qPCR Workflow. The process begins with sample collection and proceeds through nucleic acid extraction, reverse transcription, and cyclic amplification with fluorescence detection.
PCR and its advanced derivatives constitute the cornerstone of modern molecular virology, providing powerful tools for the sensitive, specific, and rapid detection of viral pathogens. From the quantitative power of qPCR to the absolute precision of dPCR, these techniques enable not only clinical diagnosis but also epidemic surveillance, treatment monitoring, and fundamental viral research. As the field progresses, integration with microfluidics, point-of-care technologies, and artificial intelligence for assay optimization promises to further enhance the speed, accessibility, and accuracy of viral molecular detection, solidifying its role as an indispensable asset in global public health [2] [9] [8].
Serology, the scientific study of blood serum and other bodily fluids, plays a fundamental role in clinical virology by detecting pathogen-specific antibodies that serve as biomarkers of past exposure to viruses, bacteria, or parasites [10]. These immunological methods rely on precise antigen-antibody interactions, where antibodies recognize and bind to unique molecular targets on pathogens called epitopes [11] [12]. The binding occurs through complementary shapes and intermolecular forces including Van der Waals interactions, hydrogen bonds, and electrostatic attractions, with the strength of these forces determining the antibody's affinity [12].
Antibodies exist as one or more copies of a Y-shaped unit composed of four polypeptide chains: two identical heavy chains and two identical light chains [12]. The top of the Y shape contains the variable region (fragment antigen-binding or F(ab) region) that binds specifically to antigens, while the base consists of constant domains forming the fragment crystallizable (Fc) region that mediates immune cell interactions [12]. In mammals, antibodies are divided into five isotypes (IgG, IgM, IgA, IgD, and IgE) based on their heavy chain type, with each isotype exhibiting distinct biological properties, functional locations, and capabilities for dealing with different antigens [12].
Antibody Isotypes in Diagnostic Virology
Structural and Functional Characteristics
The five antibody isotypes demonstrate significant structural and functional diversity critical for their roles in immune defense and diagnostic detection:
Table 1: Structural and Functional Properties of Antibody Isotypes
| Isotype | Heavy Chain | Molecular Weight (kDa) | Structure | Primary Functions and Diagnostic Significance |
|---|---|---|---|---|
| IgG | γ (gamma) | 150 | Monomer | Most abundant serum antibody (~75% of total serum antibodies); provides majority of antibody-based immunity; moderate complement fixer; indicates recent or past infection [12]. |
| IgM | μ (mu) | 900 | Pentamer | First antibody produced in primary immune response; high avidity; eliminates pathogens in early stages before sufficient IgG production; indicates recent/active infection [12]. |
| IgA | α (alpha) | 150-600 | Monomer-tetramer | Predominantly found in mucosal areas (gut, respiratory, urogenital tracts); prevents pathogen colonization; resistant to digestion; secreted in milk [12]. |
| IgD | δ (delta) | 150 | Monomer | Function unclear; works with IgM in B cell development; primarily B-cell bound [12]. |
| IgE | ε (epsilon) | 190 | Monomer | Binds to allergens; triggers histamine release from mast cells; involved in allergic reactions and protection against parasitic worms [12]. |
Temporal Dynamics of Antibody Responses
The diagnostic utility of different antibody isotypes relies heavily on their distinct temporal emergence patterns following infection:
Figure 1: Temporal Sequence of Antibody Responses Following Infection. IgM antibodies appear first, typically within 3-7 days post-infection, serving as markers of recent or active infection. IgG antibodies emerge later (7-14 days), peak around 3-6 weeks, and often persist for months or years, indicating longer-term immunity or past exposure [10] [12].
Application in SARS-CoV-2 Detection: A Case Study
The COVID-19 pandemic highlighted the critical importance of understanding serological responses, with extensive research illuminating the performance characteristics of various antibody detection methods for SARS-CoV-2.
Comparative Performance of Serological Assays
Table 2: Diagnostic Accuracy of SARS-CoV-2 Serological Assays in Clinical Practice
| Assay Type | Target Epitope | Antibody Type | Sensitivity (%) | Specificity (%) | Neutralizing Antibody Sensitivity (%) | Neutralizing Antibody Specificity (%) |
|---|---|---|---|---|---|---|
| Anti-N ECLIA | Nucleocapsid (N) | Pan-Ig | 86.8 | 98.4 | 91.7 | 93.0 |
| Anti-S1 ELISA | S1 spike domain | IgG | 86.2 | 98.2 | 92.7 | 92.0 |
| Anti-S1/S2 CLIA | S1/S2 spike domains | IgG | 84.7 | 97.6 | 90.3 | 97.7 |
| Anti-RBD+LFI | Receptor-binding domain | Pan-Ig | 84.0 | 96.1 | 87.9 | 97.9 |
| Anti-N CLIA | Nucleocapsid (N) | IgG | 81.0 | 98.3 | 84.1 | 100.0 |
| Anti-RBD ELISA | Receptor-binding domain | IgG | 79.2 | 97.2 | 85.8 | 95.9 |
| Anti-N ELISA | Nucleocapsid (N) | IgG | 65.6 | 97.7 | 66.2 | 65.3 |
Data adapted from a prospective cross-sectional study of 2,573 healthcare workers and 1,085 inpatients at a Swiss University Hospital [13].
Comparative Analysis of Detection Methods
Research conducted across university settings in Cameroon demonstrated distinct performance patterns between molecular and serological testing approaches. In a study of 291 participants, the overall COVID-19 PCR-positivity rate was 21.31% (62/291), while overall IgG seropositivity (IgM−/IgG+ and IgM+/IgG+) was 24.4% (71/291) [14]. Notably, 26.92% (7/26) of participants with COVID-19 IgM+/IgG− had negative PCR results versus 73.08% (19/26) with positive PCR, and 17.65% (6/34) with COVID-19 IgM+/IgG+ had negative PCR compared to 82.35% with positive PCR (28/34) [14]. Additionally, 7.22% (14/194) with IgM−/IgG− had positive PCR, highlighting the complex relationship between viral presence and antibody responses [14].
A study of 133 hospitalized COVID-19 patients revealed important performance differences, with IgM antibody tests showing higher positive rates (79.55%, 82.69%, and 72.97% in moderate, severe, and critical cases, respectively) compared to RT-PCR detection (65.91%, 71.15%, and 67.57% in the same groups) [15]. IgG positivity rates were substantially higher across all severity categories (93.18%, 100%, and 97.30% in moderate, severe, and critical cases, respectively) [15].
Significant variability in test performance has been observed across different testing platforms. A comparison of immunochromatography (ICG) rapid test kits and chemiluminescence immunoassay (CLIA) quantitative antibody tests demonstrated substantial discrepancies, with only 2 of 51 staff members who were IgM-positive by rapid testing confirming positive by CLIA, and only 6 of 56 IgG-positive rapid tests confirming by CLIA [16].
Essential Protocols for Serological Detection
Comprehensive Protocol for Antibody Detection in Viral Diagnostics
Principle: This protocol outlines the procedure for detecting virus-specific IgM and IgG antibodies in human serum or plasma samples using enzyme-linked immunosorbent assay (ELISA) methodology, which can be adapted for various viral pathogens.
Materials and Reagents:
- Coating buffer (0.05 M carbonate-bicarbonate buffer, pH 9.6)
- Washing buffer (PBS with 0.05% Tween-20, pH 7.4)
- Blocking buffer (PBS with 1% BSA or 5% non-fat dry milk)
- Viral antigens (recombinant proteins or inactivated virus)
- Test serum samples (heat-inactivated at 56°C for 30 minutes)
- Reference positive and negative control sera
- Anti-human IgM and IgG antibodies conjugated to enzyme (HRP or AP)
- Enzyme substrate (TMB for HRP, pNPP for AP)
- Stop solution (1M H₂SO₄ for TMB, 1M NaOH for pNPP)
Procedure:
- Antigen Coating: Dilute viral antigen in coating buffer to optimal concentration (typically 1-10 μg/mL). Add 100 μL per well to microtiter plate. Incubate overnight at 4°C or 2 hours at 37°C.
Washing: Aspirate liquid from wells and wash three times with washing buffer (300 μL per well). Tap plate dry on absorbent paper between washes.
Blocking: Add 200 μL blocking buffer per well. Incubate for 1-2 hours at 37°C. Wash as in step 2.
Sample Incubation: Dilute test sera in blocking buffer (typically 1:100 to 1:1000). Add 100 μL per well in duplicate. Include positive and negative controls. Incubate 1-2 hours at 37°C. Wash as in step 2.
Conjugate Incubation: Add anti-human IgM (μ-chain specific) or IgG (γ-chain specific) antibody conjugated to enzyme at optimal dilution in blocking buffer. Incubate 1 hour at 37°C. Wash as in step 2.
Substrate Development: Add 100 μL substrate solution per well. Incubate in dark for 10-30 minutes at room temperature.
Reaction Termination: Add 50 μL stop solution per well.
Measurement: Read absorbance at appropriate wavelength (450 nm for TMB, 405 nm for pNPP) using microplate reader.
Interpretation: Calculate cutoff value based on negative control absorbance (typically mean + 3 standard deviations). Samples with absorbance above cutoff are considered positive.
Troubleshooting Notes:
- High background: Increase blocking time or change blocking agent; optimize conjugate dilution; increase wash cycles or washing stringency.
- Low signal: Check reagent expiration; optimize antigen coating concentration; increase sample incubation time or temperature.
- High variation between duplicates: Ensure consistent washing; check pipette calibration; confirm proper sample mixing.
Rapid Lateral Flow Immunoassay Protocol
Principle: This protocol describes the procedure for rapid detection of viral antibodies using immunochromatographic lateral flow devices, suitable for point-of-care testing.
Materials:
- Lateral flow test devices
- Serum, plasma, or whole blood samples
- Sample diluent buffer
- Timer
Procedure:
- Allow test devices and samples to reach room temperature (15-30°C).
- Add specified volume of sample (typically 10-20 μL) to sample well.
- Immediately add specified volume of diluent buffer (typically 2-3 drops).
- Start timer and read results at specified time (typically 10-20 minutes).
- Do not interpret results after maximum reading time (typically 30 minutes).
Interpretation:
- IgM Positive: Control line and IgM test line visible
- IgG Positive: Control line and IgG test line visible
- IgM and IgG Positive: Control line and both test lines visible
- Negative: Only control line visible
- Invalid: Control line not visible, regardless of test lines
Chemiluminescence Immunoassay (CLIA) Protocol
Principle: This automated protocol utilizes chemiluminescent detection for high-sensitivity quantitative measurement of antibody levels.
Materials:
- CLIA analyzer and compatible reagent kits
- Sample diluent
- Calibrators and controls
- Reaction vessels
Procedure:
- Follow manufacturer's instructions for instrument preparation and initialization.
- Load samples, calibrators, and controls into designated positions.
- The automated system performs:
- Sample and reagent dispensing
- Incubation
- Magnetic separation/washing
- Substrate addition
- Luminescence measurement
- Results are calculated automatically based on calibration curve.
- Report quantitative results in standardized units (AU/mL, BAU/mL, or IU/mL).
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Serological Assay Development
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Viral Antigens | Recombinant spike protein (S1, S2, RBD), nucleocapsid protein, inactivated whole virus | Coating antigen for capturing specific antibodies; choice of antigen affects test performance [13] |
| Detection Antibodies | Anti-human IgM (μ-chain specific), anti-human IgG (γ-chain specific), enzyme conjugates (HRP, AP), fluorescent conjugates | Secondary detection; binds to human antibodies of specific isotypes; enzyme conjugates enable colorimetric, chemiluminescent, or fluorescent detection [11] [12] |
| Assay Controls | Known positive and negative serum samples, international reference standards, calibrators | Quality control, standardization, calibration of quantitative assays, determination of cutoff values [13] |
| Signal Generation | TMB (3,3',5,5'-tetramethylbenzidine), pNPP (p-nitrophenyl phosphate), AMPPD (3-(2'-spiroadamantane)-4-methoxy-4-(3''-phosphoryloxy)phenyl-1,2-dioxetane) | Enzyme substrates that generate measurable color (TMB, pNPP) or light (AMPPD) upon enzymatic conversion [11] |
| Carrier Proteins | Bovine serum albumin (BSA), keyhole limpet hemocyanin (KLH) | Used as carrier proteins for haptens; blocking agents to reduce nonspecific binding [12] |
Diagnostic Workflow and Strategic Implementation
The effective implementation of serological testing requires careful consideration of the diagnostic question being addressed and appropriate test selection:
Figure 2: Diagnostic Decision Pathway for Serological Testing. The appropriate testing strategy depends on the clinical or epidemiological question. Molecular methods (PCR) remain superior for detecting active infection, while serological approaches provide valuable information for assessing past exposure, population immunity, and in some cases, complementing molecular testing for active infection diagnosis [14] [10] [13].
Serological testing provides distinct advantages for epidemiological surveillance by capturing both symptomatic and asymptomatic cases irrespective of healthcare-seeking behavior, as antibody profiles maintain a trace of past exposure even after pathogen clearance [10]. This makes serological data particularly valuable for understanding true infection burden, transmission dynamics, and population immunity levels, especially when implemented as part of comprehensive public health surveillance strategies [10].
Accurate and timely diagnosis is a cornerstone of effective clinical management and control of viral infections. The reliability of diagnostic results is fundamentally governed by three interconnected biological and immunological phenomena: viral shedding, the diagnostic window period, and seroconversion. Viral shedding refers to the expulsion and release of virus progeny from an infected host, which can occur through various routes such as respiratory droplets, feces, or other bodily fluids [17]. The window period describes the time between infection and the point at which a test can reliably detect the infection [18]. Seroconversion is the specific immune process where an individual develops detectable antibodies in response to an infection or vaccination [19] [20] [18].
Navigating the complex temporal relationships between these three processes is critical for diagnostic accuracy, appropriate patient isolation, and effective treatment initiation. This application note provides a structured overview of these concepts, supported by quantitative data and detailed protocols, to guide researchers and scientists in the field of clinical virology.
Core Concepts and Definitions
Viral Shedding Dynamics
Viral shedding is the process by which infected individuals release viral particles into the environment. The duration and site of shedding are highly variable among different viruses and can profoundly impact epidemiological tracking.
- Prolonged Post-Recovery Shedding: For some pathogens like SARS-CoV-2, viral shedding, particularly from the gastrointestinal tract, can continue for weeks to months after clinical recovery and the cessation of symptoms. This prolonged shedding complicates the interpretation of wastewater-based epidemiology (WBE), as the viral signal in sewage can be dominated by recovered individuals rather than actively infectious cases [17].
- Infectiousness Correlation: In many diseases, the peak of infectiousness often occurs before seroconversion. However, viral shedding can continue after seroconversion, potentially extending the contagious period [19].
Seroconversion and the Immune Response
Seroconversion is a key event in the adaptive immune response, marking the transition from a seronegative to a seropositive status for a specific pathogen.
- Mechanism: When a pathogen enters the body, its antigens activate B cells. These B cells begin producing antibodies, first typically of the Immunoglobulin M (IgM) class, followed by a switch to the more specific and durable Immunoglobulin G (IgG) class [18]. Standard serological tests can only detect these antibodies once their concentration in the serum is sufficiently high to be measured [18].
- Atypical Patterns: While IgM usually appears before IgG, some infections, including COVID-19, can deviate from this pattern, with IgM appearing after IgG, simultaneously, or sometimes not at all [19] [18].
- Clinical Implications: Seroconversion does not automatically equate to sterilizing immunity. The protection conferred by antibodies can be complete, partial, or temporary, depending on the pathogen and the individual's immune response [19] [18].
The Diagnostic Window Period
The window period is a critical concept for diagnostic testing, defined as the interval after infection during which a specific test cannot yet detect markers of the pathogen (either the pathogen itself or the immune response to it) [18].
- Serological Window Period: For antibody tests, the window period is the time between infection and seroconversion, when antibody levels become detectable. During this phase, an infected individual will test negative on an antibody test despite being infected [18].
- Antigen/Nucleic Acid Test Window Period: Antigen and Nucleic Acid Amplification Tests (NAATs), such as PCR, can typically detect an infection earlier because they identify the virus directly, before an antibody response has mounted [21] [22].
- Impact on Diagnosis: The window period is a major source of false-negative results. For HIV, the window period for fourth-generation antigen/antibody tests can be around 14-18 days, meaning individuals can be highly infectious yet test negative during this time [22].
The relationship between viral load, antibody development, and test sensitivity across the timeline of infection is illustrated below.
Quantitative Data and Comparative Analysis
Impact of Season-Specific PCR Panels on Diagnostic Timelines
A 2025 prospective study on emergency department pneumonia diagnostics compared traditional culture methods with season-specific multiplex PCR panels. The quantitative outcomes demonstrate the profound impact of modern molecular techniques on the diagnostic timeline [21].
Table 1: Comparative Diagnostic Performance of Traditional Culture vs. Seasonal PCR Panels for Pneumonia [21]
| Performance Metric | Spring Season | Autumn-Winter Season | Statistical Significance |
|---|---|---|---|
| Median Turnaround Time (Traditional) | 48 hours | 50 hours | - |
| Median Turnaround Time (PCR Panel) | 12 hours | 14 hours | p < 0.001 |
| Time Saved (Median Difference) | 36 hours | 36 hours | 95% CI: -42 to -30 |
| Diagnostic Yield (Traditional) | 61.6% | 56.8% | - |
| Diagnostic Yield (PCR Panel) | 80.6% | 80.0% | p < 0.01 |
| Risk Difference in Yield | +19.0 percentage points | +23.2 percentage points | - |
The data show that PCR panels slashed the time to pathogen identification by approximately three-fourths and significantly increased the likelihood of identifying the causative agent [21].
Seroconversion and Window Periods in Key Viral Infections
The timing of seroconversion and the length of the window period vary significantly by pathogen and the type of assay used.
Table 2: Seroconversion and Diagnostic Window Periods for Selected Viruses
| Virus / Infection | Time to Seroconversion (Typical) | Key Antibody Classes | Notes on Window Period & Diagnostics |
|---|---|---|---|
| SARS-CoV-2 | IgM: Median 5 days post-symptom.\nIgG: Median 14 days post-symptom [18]. | IgM, IgG | Atypical patterns common (IgG before/with IgM). Higher viral load linked to earlier seroconversion [19]. NAAT is gold standard for acute diagnosis. |
| HIV | 2-4 weeks for antibody detection. p24 antigen appears earlier [22]. | IgM, IgG (p24 antigen) | 4th gen Ag/Ab tests shorten window to ~14 days [22]. NAAT (RNA test) is definitive during window period or discordant serology [22]. |
| General Pattern | Days to weeks, depending on pathogen and host. | IgM (acute phase), IgG (long-term) | The "window period" for antibody tests is pre-seroconversion. NAATs can detect infection before seroconversion [18]. |
Experimental Protocols
Protocol: Evaluating a Seasonal Multiplex PCR Panel for Respiratory Pathogens
This protocol is adapted from a 2025 clinical study evaluating rapid PCR panels for pneumonia diagnosis against traditional culture [21].
1. Objective: To assess the performance of season-specific multiplex PCR panels in accelerating pathogen identification and improving antibiotic stewardship in pneumonia patients.
2. Materials and Reagents:
- Sample Type: Lower respiratory tract samples (e.g., sputum, bronchoalveolar lavage).
- Nucleic Acid Extraction Kit: A commercial kit for automated or manual nucleic acid extraction.
- PCR Master Mix: A multiplex RT-PCR master mix suitable for the platform.
- Season-Specific PCR Panel: Two customized panels targeting prevalent seasonal pathogens (see Table 3).
- Platform: A real-time PCR instrument capable of multiplex detection.
- Controls: Positive and negative extraction controls, as well as positive and no-template controls (NTC) for the PCR run.
Table 3: Example Composition of Seasonal PCR Panels [21]
| Pathogen Type | Spring Panel Targets | Autumn-Winter Panel Targets |
|---|---|---|
| Viruses | Influenza A/B, Parainfluenza, Rhinovirus/Enterovirus, Adenovirus | Influenza A/B, Human Metapneumovirus, Rhinovirus/Enterovirus, Seasonal Coronavirus, RSV A/B |
| Bacteria | Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Chlamydia pneumoniae, Legionella pneumophila | Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Mycoplasma pneumoniae, Chlamydia pneumoniae, Legionella pneumophila, Klebsiella pneumoniae |
3. Procedure: 1. Sample Collection and Processing: Collect respiratory samples from enrolled patients using sterile techniques. Homogenize sputum samples if necessary. 2. Nucleic Acid Extraction: Extract total nucleic acids (DNA and RNA) from 200 µL of sample according to the manufacturer's instructions. Elute in a defined volume (e.g., 60-100 µL). 3. PCR Setup: * Thaw all reagents and keep on ice. * Prepare the PCR reaction mix according to the panel's instructions. A typical 25 µL reaction might include: 12.5 µL of 2x Master Mix, 2.5 µL of primer-probe mix, 5 µL of nuclease-free water, and 5 µL of extracted template DNA/RNA. * Load the plate onto the real-time PCR instrument. 4. Amplification: Run the thermocycling protocol as defined by the panel manufacturer. A typical program includes: Reverse transcription (if needed, 10-15 min at 50°C), initial denaturation (2 min at 95°C), followed by 40-45 cycles of denaturation (15 sec at 95°C) and combined annealing/extension (30-60 sec at 60°C). 5. Result Analysis: Analyze the amplification curves. Determine the presence or absence of each pathogen based on the cycle threshold (Ct) value and the pre-defined parameters of the assay.
4. Data Analysis: * Calculate the turnaround time from sample receipt to final report for both the PCR panel and the parallel traditional culture. * Calculate the diagnostic yield (proportion of tests identifying ≥1 pathogen) for both methods. * Compare the appropriateness of empiric antibiotic therapy based on PCR results versus standard care.
Protocol: Navigating Discordant HIV Serology Using a NAAT-Based Algorithm
This protocol is based on a 2025 case series highlighting the importance of NAAT in resolving discordant HIV screening results [22].
1. Objective: To establish a diagnostic algorithm for confirming HIV infection in patients with reactive screening tests but potential serological discordance, minimizing time to diagnosis.
2. Materials and Reagents: * Screening Tests: Fourth-generation HIV antigen/antibody immunoassay (e.g., Elecsys HIV combi PT or HIV Duo). * Rapid Test: Colloidal gold immunochromatographic assay (GICA) for HIV-1/2 antibodies. * Confirmatory Test: Western Blot (WB) or line immunoassay for HIV-1 antibodies. * NAAT Test: Quantitative or qualitative HIV-1 RNA PCR test (e.g., Roche cobas system).
3. Procedure & Decision Algorithm: The following workflow visualizes the steps for resolving discordant HIV test results, which can significantly reduce the diagnostic timeline from 11 days to 5-6 days [22].
4. Key Considerations: * Speed of Diagnosis: As demonstrated in the case series, the algorithm that triggers concurrent NAAT and Western Blot testing (right branch) upon initial serological discordance can reduce the time to definitive diagnosis by more than half compared to a sequential testing algorithm [22]. * Clinical Correlation: Always correlate laboratory findings with clinical presentation, CD4+ T-lymphocyte count, and patient history.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Viral Diagnostics and Serology Research
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| Multiplex PCR Panels | Simultaneous detection of multiple pathogens in a single reaction. | Customized for seasonal pathogens (e.g., respiratory panels for spring vs. winter) [21]. |
| Fourth-Generation HIV Ag/Ab Assay | Screening test that detects both HIV p24 antigen and antibodies, shortening the diagnostic window period. | Elecsys HIV combi PT (single result) or HIV Duo (differentiated results) [22]. |
| NAAT Kit (e.g., RT-PCR) | Gold standard for direct detection of viral RNA/DNA; crucial for confirmation during the window period. | Used for SARS-CoV-2 and HIV-1 RNA detection. Provides definitive diagnosis in serologically discordant cases [21] [22]. |
| Colloidal Gold Immunochromatographic Assay (GICA) | Rapid, point-of-care test for antibody detection. Used for initial retesting in some diagnostic algorithms. | Can yield reactive results even when differentiated immunoassays show non-reactive antibodies, influencing the diagnostic pathway [22]. |
| Western Blot (WB) Kit | Confirmatory test for antibodies. Differentiates specific antibody reactions against individual viral proteins. | Considered a key confirmatory test for HIV in many guidelines, but can be slow. Indeterminate results require NAAT follow-up [22]. |
| ELISA Kit | Detects and quantifies specific antibodies (e.g., IgG, IgM) in serum. Used for seroprevalence studies. | Can be used in combination with pseudotyped viral particle-based entry assays to study seroconversion without live virus [19]. |
The diagnostic timeline of a viral infection is a dynamic interplay of virological and immunological events. Understanding the phases of viral shedding, the constraints of the window period, and the process of seroconversion is non-negotiable for accurate diagnosis and effective public health intervention. The data and protocols presented herein underscore that modern diagnostics, particularly rapid NAAT and sophisticated multiparametric serological assays, are powerful tools for navigating this timeline. Their strategic application, guided by a deep knowledge of the underlying biology, enables researchers and clinicians to shorten diagnostic delays, optimize therapeutic strategies, and ultimately improve patient outcomes. Future advancements will likely focus on integrating these technologies into even faster, point-of-care platforms and leveraging artificial intelligence to better interpret complex diagnostic data within the clinical context.
In clinical virology and infectious disease research, two fundamental diagnostic approaches are employed: direct detection of the pathogen itself and indirect detection of the host's immune response. Direct methods, primarily through polymerase chain reaction (PCR), identify microbial nucleic acids, confirming the presence of the pathogen. Indirect methods, notably serology, detect host-derived antibodies (IgG, IgM, IgA) produced in response to infection. The choice between these methods profoundly impacts diagnostic accuracy, clinical decision-making, and therapeutic intervention, necessitating a clear understanding of their respective principles, applications, and limitations within a research context [23] [24].
Core Principles and Key Distinctions
Direct and indirect testing methods operate on fundamentally different biological principles, which dictates their appropriate application in the diagnostic workflow.
Direct Testing aims to identify the pathogen itself within a host sample. It involves the detection of specific pathogen components, such as microbial DNA, RNA, proteins, or even intact organisms. A primary example is PCR, which amplifies microbial DNA to detectable levels, offering high specificity and confirmation of active infection when the pathogen is present in the sample [23] [25].
Indirect Testing, in contrast, evaluates the host's immune system response to the pathogen. Instead of detecting the microbe, these tests identify antibodies (e.g., IgM, IgG, IgA) produced by the host's adaptive immune system. The presence of specific antibodies indicates exposure to a pathogen at some point, but does not necessarily confirm an active, ongoing infection [23] [24].
The table below summarizes the fundamental characteristics of each approach.
Table 1: Core Characteristics of Direct and Indirect Diagnostic Methods
| Feature | Direct Detection (e.g., PCR) | Indirect Detection (Serology) |
|---|---|---|
| Target Analytic | Pathogen nucleic acids (DNA/RNA), antigens, or whole organism [23] | Host-produced antibodies (IgM, IgG, IgA, etc.) [26] |
| What a Positive Result Confirms | Presence of the pathogen in the sample [23] | An immune response has occurred; indicates exposure [24] |
| Optimal Use Case | Confirming active, ongoing infection [23] [27] | Determining past exposure, immune status, or late-presenting infections [27] [24] |
| Key Advantage | High specificity; definitive evidence of pathogen presence [23] | Can detect infection even if pathogen is not present in the sampled fluid [24] |
| Key Limitation | May miss infection if pathogen load is low or not in sampled compartment [23] | Cannot distinguish between active and past infection; relies on competent host immune response [23] [26] |
The relationship between these diagnostic pathways and the infection timeline is crucial for interpretation. The following diagram outlines the general workflow and logical decision points for applying each method.
Experimental Protocols and Methodologies
Protocol A: Direct Pathogen Detection via Real-Time PCR
Real-time PCR (qPCR) is a gold standard direct detection method that allows for the simultaneous amplification and quantification of target nucleic acids [25]. This protocol is adapted for the detection of viral pathogens from respiratory samples.
Workflow Overview:
- Sample Collection & Nucleic Acid Extraction: Using sterile swabs, collect nasopharyngeal or oropharyngeal samples. Place the swab in viral transport media. Extract DNA/RNA using commercial kits, ensuring purification from inhibitors like hemoglobin or heparin [25].
- Reverse Transcription (if targeting RNA virus): For RNA viruses, synthesize complementary DNA (cDNA) using reverse transcriptase enzyme [25].
- Reaction Setup: Prepare a master mix containing:
- Thermostable DNA polymerase (e.g., Taq polymerase)
- dNTPs
- Sequence-specific forward and reverse primers (20-25 nucleotides long)
- Fluorescent probe (e.g., TaqMan) or intercalating dye
- Magnesium chloride and reaction buffer
- Add extracted template DNA/cDNA.
- Amplification & Detection in Thermal Cycler:
- Initial Denaturation: 95°C for 5 minutes.
- 40-50 Cycles of:
- Denaturation: 95°C for 15-30 seconds.
- Annealing: 55-72°C for 30-60 seconds (primer-specific).
- Extension: 72°C for 30 seconds. Fluorescence is measured at the end of each annealing/extension phase.
- Data Analysis: The quantification cycle (Cq), the cycle number at which fluorescence crosses a predefined threshold, is determined. A positive result is indicated by amplification within a valid Cq range. The Cq value is inversely proportional to the target amount [25].
Protocol B: Indirect Serological Detection via ELISA
Enzyme-Linked Immunosorbent Assay (ELISA) is a widely used serological method to detect and quantify pathogen-specific antibodies in patient serum [28].
Workflow Overview for Indirect IgG ELISA:
- Coating: Coat a microtiter plate with a purified pathogen-specific antigen (e.g., viral spike or nucleocapsid protein). Incubate overnight, then wash and block to prevent non-specific binding.
- Sample Incubation: Add patient serum (diluted appropriately) and control sera to the wells. Pathogen-specific IgG antibodies will bind to the immobilized antigen. Incubate and wash thoroughly.
- Detection Antibody Incubation: Add an enzyme-conjugated secondary antibody (e.g., anti-human IgG conjugated to Horseradish Peroxidase - HRP). This antibody binds to the patient IgG. Incubate and wash.
- Substrate Addition & Signal Detection: Add a chromogenic enzyme substrate (e.g., TMB for HRP). The enzyme converts the substrate, producing a color change.
- Result Interpretation: Stop the reaction and measure the absorbance. The intensity of the color (absorbance) is proportional to the amount of pathogen-specific antibody present in the sample. Results are reported as positive, negative, or equivocal based on comparison to calibrators and controls [28].
Performance Data and Comparative Analysis
The diagnostic performance of serological and molecular methods varies significantly based on the pathogen, infection stage, and assay design. A meta-analysis of COVID-19 serological assays revealed a wide range of accuracy, which can be quantitatively compared using the Diagnostic Odds Ratio (DOR). The DOR represents the odds of a positive test result in an infected individual versus the odds of a positive result in a non-infected individual; a higher DOR indicates better discriminatory power [5].
Table 2: Comparative Diagnostic Accuracy of Serological Assays and Methods
| Assay / Method | Target Antibody & Antigen | Pooled Diagnostic Odds Ratio (DOR) | Key Findings |
|---|---|---|---|
| Elecsys Anti-SARS-CoV-2 (Roche) | Total Antibody / Nucleocapsid (N) | 1,701.56 | Highest overall test accuracy among compared serological assays [5] |
| Elecsys Anti-SARS-CoV-2 N (Roche) | IgG / Nucleocapsid (N) | 1,022.34 | Superior diagnostic efficacy of anti-N antibodies [5] |
| Abbott SARS-CoV-2 IgG | IgG / Nucleocapsid (N) | 542.81 | High DOR for anti-N IgG assays [5] |
| LIAISON SARS-CoV-2 IgG (DiaSorin) | IgG / Spike (S1/S2) | 178.73 | Good performance for anti-spike protein assay [5] |
| Euroimmun Anti-SARS-CoV-2 | IgG / Spike (S1) | 190.45 | Comparable performance to other anti-S1/S2 assays [5] |
| Euroimmun Anti-SARS-CoV-2 | IgA / Spike (S1) | 45.91 | Lower DOR, indicating IgA performs least effectively in this context [5] |
| Serology (IgM) vs PCR for M. pneumoniae | IgM / M. pneumoniae antigen | Not Applicable | 90% (9/10) detection in confirmed cases vs 40% (4/10) for PCR in late-presenting CAP children [27] |
The data underscores that total antibody and anti-nucleocapsid IgG assays generally show superior diagnostic performance among serological tests. Furthermore, a study on Mycoplasma pneumoniae highlights a critical comparative insight: while PCR is a powerful direct tool, serology can demonstrate higher sensitivity in certain clinical scenarios, particularly during later stages of infection when the immune response is fully established but the pathogen may have been cleared from the sampled site [27].
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these diagnostic protocols relies on a suite of specialized reagents and tools.
Table 3: Essential Research Reagents for Diagnostic Development
| Research Reagent | Function / Description | Example Application |
|---|---|---|
| Taq DNA Polymerase | A thermostable enzyme that synthesizes new DNA strands during PCR amplification [25]. | Core component of all PCR-based direct detection assays. |
| Pathogen-Specific Primers & Probes | Short, single-stranded DNA sequences (primers) that bind flanking the target region, and labeled probes for specific detection in qPCR [25]. | Defines the specificity of a PCR assay for a particular virus or bacterial gene. |
| Recombinant Antigen Panels | Purified pathogen-specific proteins (e.g., Spike S1, Nucleocapsid) produced recombinantly [5] [26]. | Used to coat plates in ELISA to capture specific antibodies from patient serum. |
| Enzyme-Conjugated Secondary Antibodies | Antibodies targeting human immunoglobulins (e.g., Anti-human IgG-HRP) for signal amplification in ELISA [28]. | Detects the presence of patient antibodies bound to the antigen in serological assays. |
| Host Response mRNA Signature Panels | Pre-defined sets of host mRNA transcripts (e.g., IRF-9, ITGAM) whose expression changes in response to infection [29]. | Used in novel host-response PCR assays to differentiate infectious from non-infectious etiologies. |
The choice between direct and indirect diagnostic methods is not a matter of superiority, but of context. A comprehensive diagnostic strategy often integrates both approaches to leverage their complementary strengths, as illustrated in the workflow below.
In conclusion, direct PCR-based methods are indispensable for confirming active infection, enabling rapid treatment, and controlling transmission through their high specificity. Indirect serological methods are crucial for understanding the epidemiology of a disease, assessing immune status, and diagnosing infections where the pathogen itself is elusive. The ongoing development of novel host-response biomarkers [29] and improved recombinant antigens [26] promises to further enhance the accuracy and utility of both paradigms. For researchers and clinicians, a nuanced understanding of the principles, protocols, and performance data of both direct and indirect diagnostics is fundamental to advancing clinical virology and improving patient outcomes.
From Bench to Bedside: Application-Specific Methodologies in Research and Clinical Practice
Application Note: Advancing Molecular Diagnostics and Surveillance
The polymerase chain reaction (PCR) remains the cornerstone of modern molecular diagnostics and public health surveillance. Recent advancements have solidified its role in detecting pathogens, quantifying viral loads with precision, and tracking outbreaks in near real-time. The integration of novel buffer systems, digital quantification technologies, and portable platforms is transforming how researchers and clinicians approach infectious disease management.
Advanced Molecular Detection (AMD) represents a powerful integration of next-generation sequencing, bioinformatics, and epidemiological data to drive public health action [30]. This approach is particularly valuable for monitoring pathogen evolution at the human-animal interface, enabling early detection of spillover events and emerging variants [31]. The implementation of software containerization for bioinformatic tools has further enhanced the reproducibility and standardization of genomic workflows across public health laboratories, a critical development during multi-pathogen surveillance periods [30].
For field deployment and outbreak settings, direct PCR methodologies utilizing novel viral-inactivating transport media like DNA/RNA Defend Pro (DRDP) buffer enable rapid, extraction-free testing while maintaining biosafety [32]. This approach simplifies workflows and reduces turnaround times, which is crucial for containing outbreaks of pathogens with high transmission potential.
Table 1: Key PCR Technologies in Modern Infectious Disease Management
| Technology | Primary Application | Key Advantage | Recent Innovation |
|---|---|---|---|
| Digital PCR (dPCR) | Viral load quantification, low-abundance target detection | Absolute quantification without standard curves, high precision | Superior accuracy for high viral loads of influenza A/B and SARS-CoV-2 [33] |
| Direct PCR | Rapid field-based diagnostics, outbreak response | Omits nucleic acid extraction, uses viral-inactivating buffers | DRDP buffer enables extraction-free PCR while maintaining biosafety [32] |
| Whole-Genome Sequencing (WGS) | Pathogen genomics, outbreak tracing, variant surveillance | Comprehensive genetic characterization of pathogens | Optimized multisegment RT-PCR with dual barcoding for high-throughput sequencing [31] |
| Real-Time RT-PCR (qPCR) | Routine diagnostics, broad pathogen detection | Established gold standard, high throughput | Commercial multiplex panels for simultaneous detection of multiple respiratory pathogens [33] |
Experimental Protocol: Direct PCR for Rapid Pathogen Detection in Field Settings
Background and Principles
This protocol describes a streamlined methodology for direct PCR detection of viral pathogens using the DNA/RNA Defend Pro (DRDP) buffer system, which inactivates pathogens upon contact and stabilizes nucleic acids for extraction-free amplification [32]. This approach is particularly valuable for rapid diagnosis during outbreaks of vesiculopustular diseases like mpox, which can resemble herpesviruses (HSV-1, HSV-2, VZV) but require different containment strategies [32].
Materials and Equipment
- Transport Media: DNA/RNA Defend Pro (DRDP) buffer and Universal Transport Medium (UTM) for comparison
- Viral Stocks: HSV-1, HSV-2, and VZV from clinical samples or cultured stocks
- PCR Reagents: Primers and probes specific for target pathogens, PCR master mix
- Equipment: Thermal cycler with real-time detection capability (e.g., Roche LightCycler 480 II)
- Safety Equipment: Biosafety cabinet for initial sample handling
- Consumables: Microcentrifuge tubes, PCR plates, pipette tips
Step-by-Step Procedure
Sample Preparation and Inactivation
- Prepare Serial Dilutions: Create 10-fold serial dilutions (100 to 10-4) of viral stocks in both DRDP buffer and standard UTM [32].
- Safety Note: Samples in DRDP buffer are rendered non-infectious immediately upon contact. UTM samples remain infectious and must be handled in a biosafety cabinet with appropriate precautions [32].
- No Extraction Required: Proceed directly to PCR setup for DRDP samples. For UTM controls, perform thermal lysis at 95°C for 15 minutes followed by a 3-fold dilution to mitigate PCR inhibition [32].
PCR Setup and Thermal Cycling
- Reaction Assembly: Prepare 20 μL PCR reactions containing:
- 15-25% (v/v) of the clinical sample in DRDP buffer
- Primer and probe mixes specific for target pathogens
- PCR master mix
- Magnesium Optimization: For reactions exceeding 25% DRDP content, supplement with 10 mM MgCl₂ to counteract EDTA chelation in the buffer [32].
- Thermal Cycling Conditions:
- Initial denaturation: 95°C for 2 minutes
- 40 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 55°C for 30 seconds with fluorescence acquisition
Data Analysis and Interpretation
- Cycle Quantification (Cq) Analysis: Compare Cq values between DRDP and UTM samples across dilution series.
- Sensitivity Assessment: Determine the limit of detection for each target in both media.
- Inhibition Check: Verify that internal controls amplify efficiently in all reactions.
Diagram 1: Direct PCR workflow for rapid pathogen detection. The process eliminates nucleic acid extraction, significantly reducing processing time while maintaining biosafety through viral inactivation [32].
Expected Results and Performance Characteristics
When optimally implemented, direct PCR with DRDP buffer demonstrates equivalent or superior sensitivity compared to standard UTM processing, with Cq values favoring DRDP at higher viral loads [32]. The method maintains reliable PCR compatibility at reaction volumes containing up to 25% buffer, with magnesium supplementation effectively reversing inhibition at higher concentrations.
Application Note: Digital PCR for Precision Viral Load Quantification
The Evolution of Quantitative PCR
Digital PCR (dPCR) represents a significant advancement in nucleic acid quantification, partitioning samples into thousands of individual reactions to enable absolute quantification without standard curves [33]. This technology has transitioned from a specialized research tool to a clinically relevant platform, particularly valuable for applications requiring high sensitivity and precision [34] [35].
During the 2023-2024 "tripledemic" involving influenza A, influenza B, RSV, and SARS-CoV-2, dPCR demonstrated superior accuracy for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV compared to Real-Time RT-PCR [33]. This precision is crucial for understanding infection dynamics, treatment efficacy, and transmission risk.
Comparative Performance Data
Table 2: Performance Comparison of dPCR vs. Real-Time RT-PCR in Respiratory Virus Detection
| Performance Metric | Digital PCR (dPCR) | Real-Time RT-PCR (qPCR) |
|---|---|---|
| Quantification Method | Absolute quantification without standard curves [33] [35] | Relative quantification requiring standard curves [33] |
| Precision at High Viral Loads | Superior accuracy for influenza A, influenza B, SARS-CoV-2 [33] | Lower precision compared to dPCR [33] |
| Sensitivity for Low Viral Loads | Enhanced detection of low-abundance targets [35] | May miss low viral loads in positive patients [35] |
| Tolerance to Inhibitors | High tolerance to PCR inhibitors [35] | Sensitive to inhibitors in complex matrices [33] |
| Throughput and Cost | Lower throughput, higher cost per sample [33] | High throughput, established cost structure [33] |
| Clinical Utility | Monitoring treatment response, resolving equivocal results [35] | Broad screening, routine diagnostics [33] |
Experimental Protocol: Absolute Quantification of SARS-CoV-2 Viral Load Using Digital PCR
Background and Principles
This protocol details the application of droplet digital PCR (dPCR) for absolute quantification of SARS-CoV-2 viral load in clinical specimens, enabling precise monitoring of infection dynamics and treatment response [35]. The method specifically targets the N (nucleocapsid) and ORF1ab (RNA-dependent RNA polymerase) genes of SARS-CoV-2, which are highly conserved and abundant in the viral genome [35].
Materials and Equipment
- Clinical Specimens: Nasopharyngeal swabs collected in viral transport media
- RNA Extraction Kit: Compatible with KingFisher or similar automated systems
- dPCR System: QIAcuity or equivalent nanowell-based platform [33]
- SARS-CoV-2 Assay: Primers and probes targeting N and ORF1ab genes
- Internal Control: Human or exogenous control to monitor extraction and amplification efficiency
Step-by-Step Procedure
Sample Processing and RNA Extraction
- Nucleic Acid Extraction: Extract RNA from 200 μL of clinical sample using automated systems (e.g., KingFisher Apex) with viral RNA extraction kits following manufacturer protocols [33].
- Quality Assessment: Verify RNA integrity and concentration using spectrophotometric or fluorometric methods.
- Aliquot Storage: Divide extracted RNA into aliquots for parallel testing by dPCR and RT-qPCR if comparative analysis is planned.
dPCR Reaction Setup
- Reaction Assembly: Prepare dPCR reactions according to platform-specific requirements, typically including:
- 1X dPCR master mix
- Primers and probes for SARS-CoV-2 targets (N and ORF1ab)
- Internal control assay
- 2-5 μL of extracted RNA template
- Partitioning: Load reactions into appropriate cartridges or chips for partition generation following manufacturer instructions.
- Sealing and Loading: Ensure proper sealing of partitions before thermal cycling.
Thermal Cycling and Data Analysis
- Amplification Protocol: Perform PCR amplification with platform-optimized cycling conditions:
- Reverse transcription: 50°C for 10-30 minutes
- Enzyme activation: 95°C for 2-10 minutes
- 40-45 cycles of:
- Denaturation: 95°C for 15-30 seconds
- Annealing/Extension: 55-60°C for 30-60 seconds
- Endpoint Reading: Following amplification, analyze each partition for fluorescence signal to determine positive and negative reactions.
- Poisson Statistical Analysis: Apply Poisson statistics to calculate absolute copy numbers of target genes in the original sample, correcting for partition volume and dilution factors [35].
Diagram 2: Digital PCR workflow for absolute viral load quantification. The partitioning enables precise counting of target molecules through Poisson statistical analysis, eliminating the need for standard curves [33] [35].
Expected Results and Interpretation
dPCR typically demonstrates enhanced sensitivity compared to RT-qPCR, particularly for samples with low viral loads or those requiring precise quantification [35]. The method provides absolute quantification of viral load, enabling more accurate monitoring of treatment response and disease progression. When applied to serial samples from hospitalized patients, dPCR can track viral load changes with greater precision than RT-qPCR, offering valuable insights into viral persistence and clearance dynamics [35].
Application Note: Genomic Surveillance and Public Health Implementation
Pathogen Genomics in Public Health
The integration of pathogen genomics into public health surveillance represents a transformative advancement for outbreak investigation and antimicrobial resistance monitoring. Next-generation sequencing (NGS) technologies enable high-resolution strain typing and transmission tracking, providing insights that inform targeted public health interventions [30].
The Next-Generation Sequencing Quality Initiative (NGSQI) addresses laboratory challenges by developing tools and resources for robust quality management systems, helping laboratories navigate complex regulatory environments while implementing NGS effectively [30]. This standardization is critical for ensuring data comparability across public health networks.
Implementation Case Study: Washington State
The Washington State Department of Health successfully piloted a genomic surveillance approach for multidrug-resistant organisms (MDROs) using whole-genome sequencing (WGS) and a genomics-first cluster definition [30]. This methodology identified six distinct carbapenemase-producing organism outbreaks across three species: Pseudomonas aeruginosa, Acinetobacter baumannii, and Klebsiella pneumoniae [30].
The integration of genomic and epidemiologic data proved highly congruent, enabling public health officials to refine linkage hypotheses and address surveillance gaps [30]. This approach demonstrates how genomic data can modernize communicable disease surveillance and enhance outbreak detection precision.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Advanced PCR Applications
| Reagent/Platform | Function | Application Notes |
|---|---|---|
| DNA/RNA Defend Pro (DRDP) Buffer | Viral inactivation and nucleic acid stabilization for direct PCR | Enables extraction-free PCR; contains EDTA requiring magnesium supplementation at high concentrations [32] |
| QIAcuity dPCR System | Nanowell-based digital PCR platform | Partitions samples into ~26,000 reactions; compatible with high-throughput processing [33] |
| LunaScript RT Master Mix | Reverse transcription for whole-genome amplification | Used in optimized influenza WGS protocols with modified cycling conditions [31] |
| Multiplex Primer Panels (Allplex) | Simultaneous detection of multiple respiratory pathogens | Commercial panels for influenza A/B, RSV, SARS-CoV-2 used in tripledemic surveillance [33] |
| Oxford Nanopore Sequencing | Portable, real-time long-read sequencing | Enables rapid genomic surveillance with dual barcoding for high-throughput multiplexing [31] |
| MBTuni Primers | Whole-genome amplification of influenza A virus | Universal primers targeting conserved regions for comprehensive genome coverage [31] |
The evolution of PCR technologies continues to reshape the landscape of infectious disease diagnostics and surveillance. Emerging trends point toward greater integration of artificial intelligence and machine learning for data analysis, interpretation, and predictive modeling [36]. The development of point-of-care QUICK-PCR systems—quick, ubiquitous, integrated, and cost-efficient—represents a promising direction for decentralized testing and rapid pandemic response [37].
The convergence of dPCR with next-generation sequencing creates powerful hybrid workflows that combine precise quantification with comprehensive genetic characterization [34]. These integrated approaches will enhance our ability to detect emerging variants, monitor treatment efficacy, and implement timely public health interventions.
As these technologies mature and become more accessible, they promise to reduce healthcare inequalities by bringing advanced diagnostic capabilities to resource-limited settings. The ongoing standardization of methods and quality control frameworks will ensure that these powerful tools deliver reliable, actionable data for researchers, clinicians, and public health professionals worldwide.
Serology, the study of antibodies in serum, remains a cornerstone of clinical virology, providing critical insights into individual and population-level immune responses. These techniques are indispensable for determining immune status following infection or vaccination, conducting seroprevalence studies to understand disease penetration within communities, and monitoring the effectiveness of vaccine campaigns. While molecular methods like PCR excel at detecting active infections, serological assays offer the unique ability to retrospectively identify past infections and quantify established immunity through antibody detection [38] [39]. This application note details standardized protocols and contemporary data illustrating these three fundamental applications of serological testing in virology.
The COVID-19 pandemic has underscored the vital importance of robust serological monitoring, particularly for informing booster vaccination strategies. A 2025 study demonstrated that providing healthcare workers with their neutralizing antibody status influenced vaccination decisions, with over two-thirds (68.1%) indicating that results would affect their choice to receive a booster dose [40]. This "test-and-boost" approach represents a practical application of immune status determination in public health policy.
Application Note 1: Immune Status Determination
Principle and Significance
Determining immune status involves detecting pathogen-specific antibodies to assess an individual's immunological history and current protection level. The presence of Immunoglobulin G (IgG) typically indicates past infection or vaccination, while Immunoglobulin M (IgM) often suggests recent exposure. Quantitative serology measures antibody titers, providing a correlate of protection against specific pathogens [38]. This application is particularly valuable for managing healthcare workers, immunocompromised patients, and for epidemiological surveillance.
Key Methodologies and Protocols
Table 1: Common Serological Techniques for Immune Status Determination
| Technique | Target | Principle | Time to Result | Applications |
|---|---|---|---|---|
| Enzyme-Linked Immunosorbent Assay (ELISA) | Viral antigens or antibodies | Enzyme-conjugated antibodies produce colorimetric signal | 2-5 hours | High-throughput screening, quantitative antibody measurement |
| Hemagglutination Inhibition (HAI) Assay | Influenza-specific antibodies | Antibodies prevent viral hemagglutination of red blood cells | 4-6 hours | Influenza immunity status, vaccine response evaluation |
| Virus Neutralization Assay (VN) | Neutralizing antibodies | Serum antibodies prevent viral infection of cell cultures | 3-7 days | Gold standard for protective immunity, highly specific |
| Immunofluorescence Assay (IFA) | Viral antigens | Fluorescently-labeled antibodies detect bound serum antibodies | 3-4 hours | Autoimmune testing, confirmatory testing |
| Rapid Diagnostic Tests (RDTs) | Viral antibodies or antigens | Lateral flow immunochromatography | 10-30 minutes | Point-of-care testing, quick screening |
Detailed Protocol: Virus Neutralization Assay for SARS-CoV-2 Neutralizing Antibodies
Principle: This protocol evaluates serum neutralizing capacity by measuring its ability to prevent SARS-CoV-2 infection of susceptible cells in vitro, providing a functional assessment of protective immunity [40].
Materials:
- Vero E6 cells (ATCC CRL-1586)
- SARS-CoV-2 virus isolate (appropriate biosafety level required)
- DMEM culture medium with 2% fetal bovine serum
- 96-well tissue culture plates
- Patient serum samples (heat-inactivated at 56°C for 30 minutes)
- Positive and negative control sera
- Fixation solution (4% formaldehyde)
- Staining solution (crystal violet)
Procedure:
- Seed Vero E6 cells in 96-well plates at 2×10⁴ cells/well and incubate at 37°C with 5% CO₂ until 90% confluent.
- Prepare two-fold serial dilutions of heat-inactivated serum samples in culture medium (starting from 1:8 to 1:1024).
- Mix equal volumes of each serum dilution with 100 TCID₅₀ of SARS-CoV-2 virus and incubate at 37°C for 1 hour.
- Remove growth medium from cell plates and add 100μL of serum-virus mixture to appropriate wells.
- Include virus control wells (virus without serum), cell control wells (medium only), and serum toxicity controls (serum without virus).
- Incubate plates at 37°C with 5% CO₂ for 72 hours.
- Fix cells with 4% formaldehyde for 30 minutes, then stain with 0.1% crystal violet for 15 minutes.
- Wash plates gently with water and air dry.
- The neutralization titer is the highest serum dilution that prevents cytopathic effect in ≥50% of wells.
Interpretation: A neutralizing antibody titer ≥1:32 is considered indicative of protective immunity against SARS-CoV-2, though clinical correlates may vary by variant [40].
Application Note 2: Seroprevalence Studies
Principle and Significance
Seroprevalence studies measure the proportion of a population with specific antibodies against a pathogen, providing crucial data on cumulative infection rates and population immunity levels. These studies help identify the extent of undetected infections, monitor transmission dynamics, and guide public health interventions. The COVID-19 pandemic has highlighted the importance of serial serosurveys for tracking epidemic progression and the impact of control measures [40].
Recent Data and Findings
Table 2: COVID-19 Seroprevalence Study Among Primary Healthcare Workers (2025)
| Parameter | Result | Significance |
|---|---|---|
| Study Population | 474 healthcare workers | Multidisciplinary staff with high exposure risk |
| Neutralizing Antibody Seroprevalence | 99.2% | Near-universal seropositivity in vaccinated cohort |
| Previous COVID-19 Infection | 80.6% | High infection rate despite vaccination |
| Median Time to Infection Post-Vaccination | 163 days | Evidence of waning immunity |
| Preferred Testing Method | 77.0% preferred finger prick | Importance of acceptable sampling methods |
| Influence on Booster Decision | 68.1% | Serological testing impacts vaccination behavior |
This 2025 study demonstrated remarkably high seroprevalence (99.2%) of COVID-19 neutralizing antibodies among fully vaccinated primary care staff, with most participants (79.7%) contracting COVID-19 after vaccination at a median time of 163 days post-vaccination [40]. These findings underscore the value of seroprevalence monitoring in high-risk groups and the necessity for timely boosters.
Detailed Protocol: Population-Level Serosurvey Design
Study Design Considerations:
- Sampling Strategy: Implement stratified random sampling to ensure population representation across age, geographic, and demographic groups.
- Sample Size Calculation: For seroprevalence studies, sample size is typically calculated based on an estimated seroprevalence of 50% (which provides the largest sample size required), with a precision of 5% and 95% confidence interval, yielding a minimum sample of 385 participants [40].
- Ethical Considerations: Obtain institutional review board approval and individual informed consent.
- Data Collection: Standardized questionnaires should capture demographic data, clinical history, vaccination status, and prior infection history.
Laboratory Methodology:
- Sample Collection: Collect serum, plasma, or capillary blood samples. For point-of-care testing, finger prick blood collection increases acceptability [40].
- Testing Algorithm: Employ a two-test algorithm for high accuracy—initial screening by ELISA or rapid test, with positive samples confirmed by a different method (e.g., virus neutralization).
- Quality Control: Include standard reference sera in each assay run to ensure inter-assay comparability.
- Data Analysis: Calculate seroprevalence as the proportion of positive samples with 95% confidence intervals, adjusting for test performance characteristics and sampling design.
Application Note 3: Vaccine Efficacy Monitoring
Principle and Significance
Serological methods are essential for evaluating vaccine immunogenicity and monitoring effectiveness in real-world settings. While randomized controlled trials establish initial efficacy, ongoing serological monitoring detects waning immunity and assesses protection against emerging variants. Vaccine effectiveness (VE) is calculated by comparing disease incidence between vaccinated and unvaccinated populations, with serological correlates providing mechanistic insights [41] [42].
Recent Vaccine Effectiveness Data
Table 3: 2024-2025 COVID-19 Vaccine Effectiveness Estimates
| Outcome | Population | Effectiveness (%) | Time Frame | Data Source |
|---|---|---|---|---|
| ED/UC Visits | Adults ≥18 years | 33% (95% CI: 28-38) | 7-119 days post-vaccination | VISION Network [41] |
| Hospitalization | Immunocompetent adults ≥65 years | 45-46% | 7-119 days post-vaccination | VISION/IVY Networks [41] |
| Hospitalization | Immunocompromised adults ≥65 years | 40% (95% CI: 21-54) | 7-119 days post-vaccination | VISION Network [41] |
| Infection | Adults | 44.7% | 4 weeks post-vaccination | UNC Study [42] |
| Hospitalization/Death | Adults | 57.5% | 4 weeks post-vaccination | UNC Study [42] |
Recent data from the 2024-2025 respiratory season demonstrates that updated COVID-19 vaccines continue to provide substantial protection against severe outcomes, though effectiveness wanes over time. Vaccine effectiveness against hospitalization was 57.5% at 4 weeks post-vaccination but declined to 34.0% by 20 weeks [42]. These findings highlight the importance of serological monitoring to optimize booster timing, particularly for high-risk populations.
Detailed Protocol: Vaccine Effectiveness Study Using Test-Negative Design
Principle: The test-negative design is an efficient method for monitoring vaccine effectiveness in real-world settings by comparing vaccination status between cases (test-positive) and controls (test-negative) with similar healthcare-seeking behavior [41].
Materials and Data Sources:
- Electronic health records from participating healthcare facilities
- State vaccination registries
- Laboratory test results for SARS-CoV-2
- Trained personnel for data abstraction
- Statistical software (e.g., R, SAS, GraphPad Prism)
Procedure:
- Case Ascertainment: Identify patients with COVID-19-like illness who received molecular (RT-PCR) or antigen testing for SARS-CoV-2 within 10 days before or 72 hours after an eligible healthcare encounter.
- Case Definition: Case-patients test positive for SARS-CoV-2; control patients test negative.
- Vaccination Status: Determine 2024-2025 COVID-19 vaccination status from state registries, EHRs, and/or medical claims. Consider patients vaccinated if they received the vaccine ≥7 days before the index date.
- Exclusion Criteria:
- Patients vaccinated <7 days or ≥120 days before the encounter
- Those receiving a 2024-2025 dose <2 months after a previous COVID-19 vaccine
- Immunocompetent persons receiving more than one 2024-2025 dose
- Patients co-infected with influenza or RSV
- Statistical Analysis:
- Use multivariable logistic regression to calculate odds ratios (OR) for vaccination comparing cases to controls
- Calculate vaccine effectiveness as VE = (1 - OR) × 100
- Adjust for potential confounders: age, sex, geographic region, calendar time, and comorbidities
Interpretation: The VISION network analysis found 33% effectiveness against COVID-19-associated ED/UC visits during September 2024-January 2025, supporting the continued benefit of vaccination [41].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Serological Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Antigen Sources | Recombinant spike protein (SARS-CoV-2), Hemagglutinin (influenza), Viral lysates | Capture antigen in ELISA, stimulation antigen in ELISpot |
| Detection Antibodies | Anti-human IgG-Fc HRP, Anti-human IgA-biotin, Anti-human IgM-AP | Secondary detection in immunoassays |
| Assay Kits | cPass SARS-CoV-2 nAb Detection Kit, ELISA kits for specific pathogens | Standardized serological testing |
| Point-of-Care Tests | CoVIm Rapid SARS-CoV-2 nAb Test, lateral flow immunochromatographic assays | Rapid neutralizing antibody detection at point of care |
| Control Sera | WHO international standards, convalescent plasma pools, pre-pandemic sera | Assay calibration and quality control |
| Cell Lines | Vero E6 (SARS-CoV-2), MDCK (influenza) | Virus propagation for neutralization assays |
| Microscopy Reagents | FITC-labeled antibodies, mounting medium with DAPI | Immunofluorescence assays |
Visualizing Serological Workflows and Relationships
Serological Testing Decision Pathway
Vaccine Effectiveness Monitoring Framework
Serological techniques provide indispensable tools for understanding immune responses at both individual and population levels. The protocols and data presented demonstrate how serology informs clinical practice and public health policy through immune status determination, seroprevalence studies, and vaccine effectiveness monitoring. As viral diagnostics continue to evolve, integrating serological data with molecular methods will remain essential for comprehensive disease surveillance and control strategies. The continued development of standardized, high-throughput serological assays will enhance our ability to respond to emerging viral threats and optimize vaccination strategies in future epidemics.
The field of clinical virology diagnostics has been fundamentally transformed by the advent of advanced molecular techniques, with polymerase chain reaction (PCR) methodologies standing at the forefront of this revolution. The COVID-19 pandemic served as a critical catalyst, consolidating molecular techniques as essential tools for epidemiological surveillance and infectious disease control [43]. Among these techniques, quantitative PCR (qPCR) and multiplex PCR assays have emerged as powerful tools that enable researchers and clinicians to detect, identify, and quantify pathogenic nucleic acids with unprecedented sensitivity and specificity.
This application note explores two advanced PCR formats that have become indispensable in modern diagnostic laboratories: multiplex PCR panels for comprehensive syndromic testing and real-time qPCR for precise pathogen quantitation. These methodologies have expanded the diagnostic arsenal beyond traditional serology and viral culture methods, providing rapid, actionable information that directly impacts patient management, infection control, and public health responses to emerging viral threats [44].
Multiplex PCR Assays for Syndromic Testing
Syndromic testing represents a paradigm shift in diagnostic microbiology, allowing for the simultaneous detection of multiple pathogens that cause similar clinical symptoms. This approach is particularly valuable for patients presenting with nonspecific symptoms that could be attributed to numerous infectious agents, enabling clinicians to rapidly narrow down the causative pathogen and initiate appropriate, targeted therapy [45].
Principles and Clinical Utility
Syndromic testing operates on the principle that patients presenting with specific clinical syndromes—such as respiratory infections, gastrointestinal illnesses, or central nervous system infections—may be infected with any of dozens of potential pathogens. Traditional testing methods often require sequential, single-pathogen detection, which consumes valuable time and resources. In contrast, multiplex syndromic panels can detect 10-20 or more pathogens in a single test, significantly reducing the time to diagnosis [45].
The clinical impact of this approach is substantial. Studies have demonstrated that implementation of syndromic testing can enhance antimicrobial stewardship, decrease the risk of resistance development among pathogens, and improve healthcare outcomes by enabling rapid application of directed treatment. Furthermore, these tests save time and resources while enhancing the efficacy of microbiological laboratory processes compared to standard methods [45].
Technological Implementation
Multiplex PCR panels for syndromic testing are typically implemented using automated, closed-system platforms that integrate nucleic acid extraction, amplification, and detection. For example, the Bio-Speedy multiplex qPCR panels (Bioeksen R&D Technologies, Turkey) utilize a robotic nucleic acid isolation system (RINATM-M14) followed by amplification on instruments such as the LightCycler 96 (Roche) [45]. These systems can process multiple sample types, including blood, cerebrospinal fluid, respiratory specimens, and stool samples, with results available within approximately 3 hours for a batch of 10 samples [45].
A key advancement in multiplexing technology is the development of color cycle multiplex amplification (CCMA), which significantly increases the number of detectable DNA targets in a single qPCR reaction using standard instrumentation. In CCMA, the presence of one DNA target species results in a pre-programmed pattern of fluorescence increases across multiple channels, distinguished by cycle thresholds through rationally designed delays in amplification [46]. With just 4 distinct fluorescence colors, CCMA theoretically allows the detection of up to 136 distinct DNA target sequences using fluorescence permutation rather than combination, dramatically expanding multiplexing capabilities [46].
Performance Characteristics
Evaluation of novel multiplex PCR panels has demonstrated robust clinical performance across various specimen types. One comprehensive assessment of four novel multiplex real-time PCR panels reported the following performance characteristics [45]:
Table 1: Clinical Performance of Multiplex Syndromic Panels Across Sample Types
| Sample Type | Relative Sensitivity (%) | Relative Specificity (%) |
|---|---|---|
| Blood | 82 | 94 |
| Blood Culture | 97.1 | 99.3 |
| Stool | 94 | 98 |
| CSF | 96 | 97 |
| Respiratory | 97 | 96 |
The limit of detection (LOD) for these assays typically ranges between 10 and 100 pathogens/mL depending on the target and sample type. No cross-reactivity with potential cross-reacting pathogens has been observed, demonstrating high analytical specificity [45].
Similar performance has been documented with other commercial systems. The BioFire FilmArray Global Fever Panel demonstrated a positive percentage agreement of 85.71% compared to conventional diagnostics for high-consequence infectious diseases, with perfect detection (100%) for certain pathogens including Crimean-Congo hemorrhagic fever virus, dengue virus, Ebola virus, and Marburg virus [47]. For Plasmodium species, the panel achieved 95.65% detection, though it showed limitations for Salmonella enterica serotypes [47].
Workflow and Procedures
The standard workflow for syndromic testing using multiplex PCR panels involves several critical steps from sample collection to result interpretation:
Figure 1: Workflow for multiplex syndromic testing, illustrating the key steps from sample collection to result interpretation.
Detailed Procedural Steps:
Sample Collection and Preparation:
- Collect appropriate specimens (e.g., blood in EDTA tubes, CSF, respiratory specimens, stool) in sterile containers.
- For swab specimens, place in viral transport medium (VTM) or universal transport medium (UTM) containing antibiotics to prevent bacterial contamination [44].
- Process samples within 2-3 hours of collection or store at 4°C for short-term (≤72 hours) or -80°C for long-term storage.
Nucleic Acid Extraction:
- Use automated nucleic acid extraction systems (e.g., RINATM-M14) according to manufacturer's protocols.
- Load samples directly into extraction cartridges; for swabs and stool samples, homogenize in molecular grade water before loading.
- Include negative controls (deionized water) in each extraction run to monitor for contamination.
PCR Reaction Setup:
- Utilize pre-loaded, ready-to-use qPCR strips containing target-specific multiplex qPCR mixtures.
- Combine 5 μL of nucleic acid extract with 15 μL of multiplex qPCR mixture per well.
- Include internal controls targeting human DNA to assess extraction efficiency and PCR inhibition.
Amplification and Detection:
- Perform amplification using a standardized thermocycling protocol (e.g., 90-minute qPCR protocol).
- Monitor fluorescence accumulation in real-time across multiple channels corresponding to different pathogens.
Result Interpretation:
- Analyze amplification curves and cycle threshold (Ct) values for each target.
- Identify detected pathogens based on channel-specific fluorescence signals exceeding predetermined thresholds.
- Report results with appropriate clinical context, considering potential limitations and assay performance characteristics.
Real-Time qPCR for Pathogen Quantitation
While multiplex syndromic panels excel at qualitative pathogen detection, real-time quantitative PCR (qPCR) provides crucial information about pathogen load, which has significant implications for disease monitoring, treatment response assessment, and understanding pathogenesis.
Fundamental Principles
Real-time qPCR, also known as quantitative PCR, combines the amplification capabilities of traditional PCR with real-time detection, allowing researchers to monitor the accumulation of PCR products as they form [48]. Unlike traditional PCR, which relies on end-point detection, qPCR focuses on the exponential phase of amplification where the precise quantification of initial template concentration is most accurate [48].
The key measurement in qPCR is the cycle threshold (Ct), defined as the PCR cycle at which the sample's fluorescence signal reaches a predetermined threshold above background levels. The Ct value is inversely proportional to the starting quantity of the target nucleic acid, with lower Ct values indicating higher initial template concentrations [48].
Applications in Clinical Virology
In virology, quantitative PCR serves multiple critical functions:
- Viral Load Monitoring: For viruses such as Cytomegalovirus (CMV), Hepatitis B and C, and HIV, quantitative molecular assays assess the severity of infection and monitor response to antiviral therapy [44].
- Disease Progression Assessment: Viral load measurements can correlate with disease severity and help guide clinical management decisions.
- Transmission Risk Assessment: For some pathogens, quantification can inform about transmission potential and inform infection control measures.
The COVID-19 pandemic highlighted the importance of qPCR, with reverse transcription qPCR (RT-qPCR) rapidly adopted as the gold standard method for diagnosing SARS-CoV-2 infection due to its high sensitivity and specificity in detecting viral RNA, even in asymptomatic or pre-symptomatic individuals [43].
Detection Chemistries and Their Applications
Two primary detection chemistries are used in gene expression studies and pathogen detection using real-time PCR:
Table 2: Comparison of qPCR Detection Chemistries
| Chemistry | Principle | Advantages | Limitations | Ideal Applications |
|---|---|---|---|---|
| SYBR Green | Binds nonspecifically to double-stranded DNA | Cost-effective; flexible for different targets | Less specific; prone to primer-dimer artifacts | Initial screening; single-target detection |
| TaqMan Probes | Fluorogenic 5' nuclease chemistry with target-specific probes | High specificity; enables multiplexing | More expensive; requires probe design | Multiplex assays; precise quantification |
TaqMan probe-based assays are particularly valuable for multiplex applications because each assay can be labeled with a unique fluorescent dye, allowing the instrument to discriminate between different targets in the same reaction [48] [49].
Singleplex vs. Multiplex qPCR: Practical Considerations
The decision between singleplex and multiplex qPCR formats depends on several experimental factors:
Table 3: Singleplex vs. Multiplex qPCR Comparison
| Parameter | Singleplex qPCR | Multiplex qPCR |
|---|---|---|
| Reaction Setup | One target per reaction tube/well | Multiple targets per reaction tube/well |
| Design Complexity | Simple; minimal optimization needed | Complex; requires extensive optimization |
| Reagent Consumption | Higher per target analyzed | Lower per target analyzed |
| Sample Requirement | More sample needed for multiple targets | Less sample needed |
| Risk of Interaction | No competition between targets | Targets compete for reagents |
| Data Normalization | Requires separate reference gene reactions | Reference and target genes in same well |
Multiplexing offers significant advantages in throughput and efficiency but presents challenges in assay design and optimization. When multiple targets are amplified in a single reaction, they compete for dNTPs, enzymes, and other reaction components. If one target amplifies more efficiently than others, it may deplete shared reagents, leading to poor amplification of less abundant targets [49]. This can be mitigated by primer-limiting the more abundant target to balance amplification efficiency [49].
Quantitative Analysis Methods
Three primary methods are used for quantification in qPCR experiments:
Comparative CT (ΔΔCT) Method: Used for relative quantitation, this method compares the C_T values of target genes to reference genes across different samples, expressing results as fold-change or fold-difference [48].
Relative Standard Curve Method: Also used for relative quantitation, this approach relies on a standard curve of known concentrations to determine relative quantities of target sequences [48].
Standard Curve Method (Absolute Quantitation): Utilizes a standard curve with known copy numbers to determine the absolute quantity of target nucleic acid in the sample [48].
The selection of appropriate reference genes for normalization is critical in any gene expression study to correct for differences in RNA sampling and avoid misinterpretation of results [48].
Experimental Workflow for Quantitative RT-qPCR
The standard workflow for quantitative RT-qPCR analysis involves multiple critical steps to ensure accurate and reproducible results:
Figure 2: Workflow for quantitative RT-qPCR analysis, highlighting key steps from RNA extraction to data analysis.
Detailed Protocol for Quantitative RT-qPCR:
RNA Extraction:
- Extract high-quality total RNA using silica-membrane columns or magnetic bead-based methods.
- Treat with DNase I to remove genomic DNA contamination.
- Quantify RNA using spectrophotometry (NanoDrop) or fluorometry (Qubit); assess integrity via agarose gel electrophoresis or Bioanalyzer.
- Store RNA at -80°C if not used immediately.
Reverse Transcription:
- Perform reverse transcription using either gene-specific primers, random hexamers, or oligo(dT) primers.
- Use 10 ng-2 μg total RNA in 20 μL reaction volume with reverse transcriptase enzyme and buffer according to manufacturer's instructions.
- Incubate at appropriate temperatures (typically 25°C for 10 minutes, 37-50°C for 30-120 minutes, 85°C for 5 minutes).
- Dilute cDNA 1:5 to 1:10 before use in qPCR reactions.
qPCR Reaction Setup:
- Prepare master mix containing buffer, dNTPs, polymerase, and appropriate detection chemistry (SYBR Green or TaqMan probes).
- For multiplex reactions, ensure dye combinations are compatible with instrument filter sets.
- Include no-template controls (NTC) and positive controls in each run.
- Set up reactions in triplicate to assess technical variability.
- Use reaction volumes of 10-25 μL depending on platform requirements.
Thermal Cycling Conditions:
- Initial denaturation: 95°C for 2-10 minutes
- 40-50 cycles of:
- Denaturation: 95°C for 15-30 seconds
- Annealing/Extension: 60°C for 30-60 seconds (acquire fluorescence)
- For SYBR Green assays: include melt curve analysis (65°C to 95°C, increment 0.5°C) to verify amplification specificity.
Data Analysis:
- Set fluorescence threshold in exponential phase of amplification above background.
- Record Ct values for each reaction.
- Calculate gene expression using ΔΔCt method or standard curve as appropriate.
- Perform statistical analysis on replicate samples.
Essential Research Reagent Solutions
Successful implementation of advanced PCR formats requires careful selection of reagents and materials. The following table outlines key solutions and their applications:
Table 4: Essential Research Reagents for Advanced PCR Applications
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Nucleic Acid Extraction Kits | Qiagen DNA Blood Mini Kit, Pathogen Lysis Tubes | Efficient isolation of high-quality DNA/RNA from clinical samples; critical for sensitive detection [50] [45]. |
| Master Mixes | TaqPath ProAmp Master Mix, SYBR Green Master Mix | Provide optimized buffer, enzymes, and dNTPs for efficient amplification; selection depends on detection chemistry [46] [48]. |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kits | Convert RNA to cDNA for RT-qPCR applications; choice of random hexamers vs. oligo(dT) affects transcript coverage [48]. |
| Predesigned Assays | TaqMan Gene Expression Assays, PCR Arrays | Target-specific primers and probes with validated performance; save time on assay design and optimization [48]. |
| Quantification Standards | gBlocks Gene Fragments, Vector DNAs with target inserts | Create standard curves for absolute quantification; essential for determining copy numbers [45]. |
| Quality Control Reagents | Human DNA-targeted oligonucleotides, Reference genes | Assess extraction efficiency, and PCR inhibition; ensure result reliability through proper normalization [48] [45]. |
Advanced PCR formats, including multiplex assays for syndromic testing and real-time qPCR for quantification, have revolutionized diagnostic approaches in clinical virology. These techniques provide the sensitivity, specificity, and throughput necessary for rapid pathogen identification and quantification, enabling evidence-based clinical decision-making and appropriate therapeutic interventions.
The ongoing development of technologies like color cycle multiplex amplification promises to further expand multiplexing capabilities, while innovations in reagent formulations and instrumentation continue to enhance the precision and accessibility of quantitative PCR. As these methodologies evolve, they will undoubtedly continue to shape the landscape of infectious disease diagnostics, contributing to improved patient outcomes and strengthened public health responses to emerging viral threats.
Automated immunoassays are indispensable in modern clinical virology, providing critical tools for diagnosing infections, monitoring immune status, and guiding therapeutic decisions. These technologies bridge two essential diagnostic paradigms: high-throughput serological screening in centralized laboratories and rapid testing at the point of care (POC). Serological assays primarily detect virus-specific antibodies (IgM and IgG) to identify immune responses to active or past infections, playing a crucial role in determining the etiology of acute viral infections, screening blood products, evaluating immune status for organ transplants, and conducting epidemiological studies [51].
The evolution of immunoassay technologies has transformed virology diagnostics. Traditional methods like complement fixation and hemagglutination inhibition have largely been supplanted by more sensitive and automated techniques, including enzyme-linked immunosorbent assays (ELISA), chemiluminescence immunoassays (CLIA), and digital ELISA [51] [52]. Concurrently, POC testing has advanced significantly, moving from basic test strips to sophisticated molecular platforms that deliver laboratory-quality results in minutes rather than hours [53] [54]. This article examines current automated immunoassay technologies, their applications in clinical virology, and detailed protocols for implementation within a comprehensive viral diagnostic framework.
High-Throughput Automated Immunoassay Platforms
Centralized laboratory testing relies on automated platforms that process hundreds of samples simultaneously with minimal manual intervention. These systems are essential for large-scale serosurveillance, vaccine efficacy studies, and routine clinical diagnostics.
Platform Architecture and Workflow
Modern high-throughput systems integrate liquid handling, incubation, washing, and detection into a single automated workflow. Platforms such as the Tecan Fluent 480 and Freedom EVOlyzer series can process up to twelve 96-well ELISA plates in a single run, handling up to 248 primary tubes with optional pre-dilution capabilities [55]. These systems employ sophisticated scheduling software that dynamically manages resources, allowing continuous loading and simultaneous processing of multiple assays with different protocols [55].
Key technological advancements include Pressure Monitored Pipetting (PMP) and capacitive Liquid Level Detection (cLLD), which ensure accurate liquid transfers and flag potential errors such as tip occlusion or insufficient sample volume [55]. Process security features provide full traceability of samples and pipetting actions, maintaining data integrity for regulatory compliance [55].
Performance Characteristics of Common Immunoassay Types
Table 1: Comparison of Immunoassay Technologies for Serological Diagnosis
| Assay Type | Sensitivity | Reproducibility | Dynamic Range | Multiplexing Capability | Throughput | Common Virology Applications |
|---|---|---|---|---|---|---|
| Western Blot | Qualitative/Semi-quantitative | Low | Low | Singleplex | Low | HIV confirmatory testing, Lyme disease |
| Traditional ELISA | Quantitative (nanomolar-picomolar) | Medium | 2-3 logs | Singleplex | Low-Medium | Viral serology (HIV, Lyme, toxoplasmosis) |
| Bead-Based Immunoassay | Quantitative | High | 3-5 logs | Multiplex | High | Cytokine profiling, vaccine response studies |
| Chemiluminescence Immunoassay (CLIA) | High (picomolar-femtomolar) | High | 3-5 logs | Singleplex/Multiplex | High | Hepatitis, HIV, SARS-CoV-2 serology |
| Digital ELISA | Ultra-high (femtomolar-attomolar) | High | 4-5 logs | Emerging | Medium | Low-abundance biomarker detection |
| Lateral Flow Immunoassay | Semi-quantitative | Medium | Limited | Singleplex | High | Rapid POC testing (influenza, SARS-CoV-2) |
Selection Guidelines for Diagnostic Applications
Assay selection depends on clinical requirements and laboratory infrastructure. For routine serology with abundant targets, traditional ELISA or CLIA provide robust, cost-effective solutions [52]. When analyzing multiple analytes from limited sample volumes, bead-based multiplex assays offer superior efficiency [52]. For detecting low-abundance cytokines or early infection biomarkers, digital ELISA provides the necessary sensitivity [52] [56].
Comparative studies demonstrate that automated ELISA-based methods generally achieve higher relative sensitivity and specificity (85-100% for anti-IF antibodies; 95-100% for anti-PC antibodies) compared to other formats [57]. However, method-specific variations occur due to different antigen sources and detection principles, necess careful validation for each viral pathogen [57].
Point-of-Care Immunoassay Technologies
POC immunoassays deliver rapid results near patients, enabling immediate clinical decisions. These technologies are particularly valuable in emergency departments, primary care settings, and resource-limited environments.
Technology Formats and Principles
Lateral Flow Immunoassays (LFIAs) represent the most widespread POC format, utilizing capillary action to move samples across a membrane containing immobilized capture antibodies [53]. Well-known examples include at-home pregnancy tests and rapid influenza tests. Most LFIAs provide qualitative or semi-quantitative results through visual band interpretation, though recent advances incorporate readers for quantification [53].
Advanced POC Platforms integrate microfluidics and immunoassay cartridges for laboratory-quality quantitative testing. Systems like the Rapi-D with IgLoo reader can measure vitamin D levels from 20μL capillary blood in 15 minutes, demonstrating the potential for rapid quantitative testing outside central laboratories [58]. Modern POC molecular platforms, such as the cobasⓇ Liat system, perform multiplex PCR for respiratory pathogens with high accuracy, significantly reducing turnaround times compared to laboratory testing [54].
Clinical Impact and Performance
POC testing dramatically shortens diagnostic timelines. A recent emergency department study implemented a rapid multiplex POC test for SARS-CoV-2, reducing the median order-to-result turnaround time by more than 11 hours [54]. This acceleration enables faster clinical management decisions, potentially improving patient outcomes.
POC testing also enhances antimicrobial stewardship. Research shows that availability of CLIA-waived molecular influenza testing at POC improves antiviral prescribing practices compared to rapid influenza diagnostic tests (RIDTs) [54]. Similar benefits are anticipated for sexually transmitted infection testing, where current presumptive treatment practices often lead to inappropriate antibiotic use [54].
Table 2: Performance Comparison of POC Testing Modalities
| Parameter | Laboratory Immunoassay | Benchtop POC Analyzer | Lateral Flow POC | Molecular POC |
|---|---|---|---|---|
| Turnaround Time | 2-24 hours | 10-30 minutes | 1-15 minutes | 15-45 minutes |
| Sample Type | Serum, plasma | Whole blood, urine, saliva | Whole blood, urine, nasal swabs | Nasopharyngeal swab, saliva |
| Quantification | Fully quantitative | Quantitative | Qualitative/Semi-quantitative | Quantitative |
| Multiplexing | High | Moderate | Limited | High |
| Throughput | High (hundreds/day) | Medium (tens/day) | High (rapid single tests) | Low-Medium |
| Equipment Cost | High | Medium | Low | High |
| CLIA Waiver Status | Usually not waived | Many systems waived | Most tests waived | Some systems waived |
Integrated Protocols for Virology Diagnostics
High-Throughput Serological Screening for Viral Antibodies
Principle: This protocol utilizes an automated chemiluminescence microparticle immunoassay (CMIA) for detecting virus-specific IgG and IgM antibodies in human serum or plasma. The method employs magnetic particles coated with viral antigens and acridinium-labeled conjugates for sensitive detection [55] [52].
Materials:
- Tecan Fluent 480 platform with HydroFlex washer and MIO incubator [55]
- CMIA reagent kit (viral antigen-coated magnetic particles, conjugate, assay buffer)
- Positive and negative controls, calibrators
- Pre-treatment solution (if required for rheumatoid factor removal)
- 96-well plates or primary sample tubes
Procedure:
- Sample Preparation: Centrifuge blood samples at 1500×g for 10 minutes. Aliquot serum/plasma into sample racks.
- System Setup: Load reagents following the manufacturer's temperature equilibration recommendations. Initialize the Fluent 480 platform and select the assay protocol.
- Automated Processing:
- The system transfers 50μL of sample, calibrators, or controls to designated wells.
- Adds 100μL of viral antigen-coated magnetic particles.
- Incubates for 18 minutes at 37°C with continuous mixing.
- Washes particles three times with wash buffer using the HydroFlex washer.
- Adds 100μL of acridinium-labeled conjugate.
- Incubates for 4 minutes at 37°C.
- Washes particles three times.
- Adds trigger solutions and measures chemiluminescence as relative light units (RLUs).
- Data Analysis: The software calculates antibody concentrations from the calibration curve. Results for IgM antibodies are reported as positive, negative, or equivocal; IgG antibodies may be reported as quantitative values with established reference ranges.
Interpretation: IgM antibodies typically indicate recent infection, while IgG antibodies suggest past exposure or immunity. Seroconversion or a significant (≥4-fold) increase in IgG titers between acute and convalescent samples (collected 2-4 weeks apart) confirms acute infection [51].
Rapid Multiplex POC Testing for Respiratory Viruses
Principle: This protocol describes a rapid molecular POC test for simultaneous detection of influenza A/B and SARS-CoV-2 from nasopharyngeal swabs, using real-time PCR amplification on an integrated cartridge-based system [53] [54].
Materials:
- cobasⓇ Liat system or equivalent POC PCR platform
- Sterile nasopharyngeal swabs
- Transport medium or specific buffer solutions
- Disposable pipettes and personal protective equipment
Procedure:
- Sample Collection: Collect nasopharyngeal specimen using a sterile swab. Immediately place the swab into transport medium.
- Cartridge Loading: Pipette 200μL of the sample transport medium into the sample port of the test cartridge.
- Sample Processing: Insert the cartridge into the Liat analyzer. The system automatically:
- Extracts and purifies nucleic acids
- Performs reverse transcription and PCR amplification
- Detects target sequences in real-time using specific fluorescent probes
- Result Interpretation: The analyzer automatically interprets results and displays them within 20 minutes. Results include detected/not detected for each target and internal control validity indication.
Quality Control: Each cartridge contains internal controls for extraction and amplification. External controls should be run daily according to the laboratory's quality management system.
Troubleshooting: Invalid results may occur due to improper sample collection, cartridge manufacturing defects, or instrument malfunction. Repeat testing with a new sample or cartridge is recommended for invalid results [53].
Research Reagent Solutions
Table 3: Essential Research Reagents for Immunoassay Development
| Reagent/Category | Function | Examples/Sources | Application Notes |
|---|---|---|---|
| Viral Antigens | Capture and detection of specific antibodies | Recombinant proteins, inactivated whole virus, synthetic peptides | Purity and preservation of conformational epitopes critical for assay sensitivity |
| Detection Antibodies | Signal generation for antigen-antibody complexes | Enzyme conjugates (HRP, ALP), fluorescent tags, acridinium labels | Label choice affects sensitivity; enzymes for colorimetry, acridinium for chemiluminescence |
| Solid Phases | Immobilization of capture reagents | Magnetic beads, microplate wells, nitrocellulose membranes | Beads enable automation and multiplexing; membranes used in lateral flow tests |
| Signal Generation Substrates | Produces measurable signal | TMB (colorimetric), luminol (chemiluminescent), ATTO (fluorescent) | Chemiluminescent substrates generally offer highest sensitivity |
| Assay Diluents and Blockers | Reduce non-specific binding | BSA, casein, non-ionic surfactants, animal sera | Optimized blockers essential for reducing background in complex samples |
| Quality Controls | Monitor assay performance | Positive and negative controls, calibrators with known values | Should mimic patient sample matrix and cover clinical decision points |
Workflow Diagrams
Automated immunoassays represent a cornerstone of modern clinical virology, enabling both large-scale serological screening and rapid point-of-care diagnosis. High-throughput systems provide the efficiency, reproducibility, and sensitivity required for population-level testing and sophisticated serological profiling, while POC technologies deliver rapid results that enable immediate clinical decision-making at the patient interface. The continued evolution of these technologies—including enhanced multiplexing capabilities, improved sensitivity through digital detection methods, and greater integration of artificial intelligence for data interpretation—promises to further transform viral diagnostics. As these technologies advance, they will play an increasingly vital role in pandemic preparedness, antimicrobial stewardship, and personalized medicine approaches to infectious disease management.
The polymerase chain reaction (PCR) has evolved from a foundational molecular biology technique into a cornerstone of modern clinical diagnostics. Its unparalleled sensitivity, specificity, and versatility have enabled groundbreaking applications across diverse medical fields. This article explores three transformative domains where PCR technology is driving innovation: oncology diagnostics for cancer stratification, pharmacogenomics for personalized therapeutic guidance, and pathogen discovery for rapid outbreak response. Within clinical virology, PCR complements serological methods by enabling direct pathogen detection during acute infection, while serology provides crucial data on past exposure and immune status. The integration of these methodologies provides a comprehensive diagnostic framework for managing infectious diseases and beyond [59] [43].
The following analysis details the specific applications, experimental protocols, and technical requirements that position PCR as an indispensable tool in contemporary research and clinical practice.
Quantitative Data Analysis
The global market data and technology segmentation presented in the table below underscore the significant economic and scientific impact of molecular diagnostics, with PCR maintaining a dominant position.
Table 1: Global Market Analysis for Molecular Diagnostics in Pharmacogenomics (2025-2035)
| Metric | Value (2025) | Projected Value (2035) | CAGR (2025-2035) | Key Insights |
|---|---|---|---|---|
| Total Market Value | USD 748.5 Million | USD 1,450.5 Million | 6.8% | Market to nearly double in size, driven by personalized medicine. |
| Leading Technology | PCR (38.1% Share) | - | - | PCR remains the most widely adopted platform due to its reliability and cost-effectiveness. |
| Leading Product Type | Kits & Assays (48.1% Share) | - | - | Reflects demand for standardized, ready-to-use clinical solutions. |
| Top Therapeutic Area | Oncology (33.4% Share) | - | - | High complexity of cancer treatment drives demand for pharmacogenomic testing. |
Table 2: Growth Projections for Molecular Diagnostics in Key Geographic Regions
| Country | Projected CAGR (2025-2035) | Primary Growth Drivers |
|---|---|---|
| China | 9.2% | Government-led precision medicine initiatives and major healthcare investments. |
| India | 8.6% | Expanding healthcare infrastructure and rising awareness of personalized medicine. |
| Germany | 7.9% | Integration into clinical practice and comprehensive reimbursement policies. |
| United States | 5.8% | Established precision medicine frameworks and advanced healthcare systems. |
Application Notes & Experimental Protocols
PCR in Oncology Diagnostics
Application Note: In oncology, PCR has moved beyond simple nucleic acid detection to become a critical tool for molecular stratification and precision medicine. Quantitative PCR (qPCR) and digital PCR (dPCR) are extensively used to detect somatic mutations, gene fusions, and expression changes that guide therapy selection [60]. For example, in Non-Small Cell Lung Cancer (NSCLC), multiplexed qPCR panels can simultaneously screen for actionable mutations in genes such as EGFR, KRAS, BRAF, and ALK, delivering results within hours—a critical timeframe for initiating targeted therapies [60]. This approach is particularly valuable for tissue-limited samples like fine-needle aspirates or liquid biopsies, where maximizing data from minimal input is essential. Furthermore, the advent of HER2-low and HER2-ultralow scoring in breast cancer highlights how precise PCR-based quantification can expand patient eligibility for targeted treatments [61] [62].
Protocol: Multiplex qPCR for NSCLC Mutation Profiling from FFPE Tissue
- Objective: To simultaneously detect single-nucleotide variants (SNVs) in EGFR, KRAS, and BRAF from formalin-fixed paraffin-embedded (FFPE) tissue sections.
- Materials:
- Methodology:
- Nucleic Acid Extraction: Extract total nucleic acids from 3-5 sections (5-10 µm thick) of FFPE tissue using a commercial kit. Include a proteinase K digestion step. Quantify and assess purity (A260/A280 ratio ~1.8-2.0).
- Reverse Transcription: For RNA targets, synthesize cDNA using a reverse transcriptase reaction with random hexamers or gene-specific primers.
- qPCR Setup:
- Prepare a reaction mix containing: 1x multiplex master mix, 1x combined primer-probe set, and 2-50 ng of cDNA/DNA template.
- Loading example:
| Sample | Template (cDNA/DNA) | Multiplex Master Mix | Primer-Probe Mix | Nuclease-free Water || :--- | :--- | :--- | :--- | :--- || Patient | 5 µL | 10 µL | 4 µL | 1 µL || No-Template Control (NTC) | 0 µL | 10 µL | 4 µL | 6 µL | - Load samples into a 96-well plate in duplicate.
- Thermal Cycling:
- Cycling conditions:
| Step | Temperature | Time | Cycles | Purpose || :--- | :--- | :--- | :--- | :--- || Enzyme Activation | 95°C | 2 min | 1 | Hot-start polymerase activation || Denaturation | 95°C | 15 sec | | DNA denaturing || Annealing/Extension | 60°C | 60 sec | 40-50 | Primer annealing & amplification |
- Cycling conditions:
- Data Analysis: Analyze amplification curves. Determine the Cq (quantification cycle) value for each target. Use a ΔΔCq method relative to a reference gene for expression analysis, or use allele-specific probes to call mutations based on presence/absence of signal.
PCR in Pharmacogenomics
Application Note: Pharmacogenomics (PGx) leverages PCR to identify genetic polymorphisms in genes governing drug metabolism (e.g., CYP2C19, CYP2D6, TPMT) and response. This enables clinicians to personalize drug selection and dosing to maximize efficacy and minimize adverse events [63]. PCR-based PGx testing is a pillar of the global molecular diagnostics market, with a significant portion focused on oncology to guide the use of chemotherapeutics and targeted agents [63]. The technology's scalability and cost-effectiveness (tests typically cost $50-$200) make it ideal for large-scale population screening and routine clinical implementation [60] [63].
Protocol: Genotyping of CYP2C19 Loss-of-Function Alleles using RT-qPCR
- Objective: To identify the CYP2C192 (c.681G>A) allele from human genomic DNA to guide antiplatelet therapy selection.
- Materials:
- Genomic DNA extracted from whole blood or buccal swabs.
- Allele-specific RT-qPCR assay kit for CYP2C19 *2.
- TaqMan-based genotyping master mix.
- Positive control samples for CYP2C19 *1/ *1, *1/ *2, and *2/ *2 genotypes.
- Methodology:
- DNA Quantification: Normalize all DNA samples to a working concentration of 5-10 ng/µL.
- Reaction Setup:
- For each sample, set up two parallel reactions: one with the VIC-labeled probe for the wild-type allele (1) and one with the FAM-labeled probe for the variant allele (2).
- Loading example per well:
| Component | Volume || :--- | :--- || Genotyping Master Mix (2x) | 5 µL || *CYP2C19* *2 Assay Mix (20x) | 0.5 µL || DNA Template (10 ng/µL) | 2 µL || Nuclease-free Water | 2.5 µL || Total Volume | 10 µL |
- Thermal Cycling:
- Use standard TaqMan genotyping cycling conditions:
| Step | Temperature | Time | Cycles || :--- | :--- | :--- | :--- || Enzyme Activation | 95°C | 10 min | 1 || Denaturation | 95°C | 15 sec | 40 || Annealing/Extension | 60°C | 60 sec | |
- Use standard TaqMan genotyping cycling conditions:
- Genotype Calling: After the run, use the instrument's genotyping software to plot VIC vs. FAM fluorescence. Cluster analysis will clearly separate samples into three groups: homozygous wild-type (1/ *1), heterozygous (1/ 2), and homozygous variant (2/ *2).
PCR in Pathogen Discovery and Virology
Application Note: The COVID-19 pandemic underscored the indispensable role of RT-qPCR as the gold standard for the direct, sensitive, and specific detection of viral pathogens [59] [43]. It remains the benchmark against which newer technologies like CRISPR-based assays and isothermal amplification are measured [59]. Beyond routine diagnosis, PCR is vital for pathogen discovery, enabling the identification and characterization of novel viruses, as demonstrated during the recent Oropouche virus (OROV) outbreak [64]. In the broader context of clinical virology, PCR (detecting current infection) and serology (detecting past infection/immune response) form a complementary diagnostic duo [43].
Protocol: RT-qPCR for Detection of Oropouche Virus (OROV) from Human Serum
- Objective: To detect OROV RNA in human serum samples during an acute febrile illness outbreak.
- Materials:
- Viral RNA extraction kit (e.g., QIAamp Viral RNA Mini Kit).
- One-Step RT-qPCR Master Mix (contains reverse transcriptase, Taq polymerase, dNTPs, buffer).
- Primers and probes specific for the OROV S segment [64].
- RNase-free water.
- Positive control (in vitro transcribed OROV RNA fragment) and negative extraction controls.
- Methodology:
- Viral RNA Extraction: Extract RNA from 140 µL of patient serum using the commercial kit according to the manufacturer's instructions. Elute in 60 µL of elution buffer.
- One-Step RT-qPCR Setup:
- Prepare the following reaction mix on ice:
| Component | Volume per Reaction || :--- | :--- || 2x One-Step RT-qPCR Master Mix | 10 µL || Forward Primer (10 µM) | 0.8 µL || Reverse Primer (10 µM) | 0.8 µL || Probe (5 µM) | 0.4 µL || RNA Template | 5 µL || RNase-free Water | 2 µL || Total Volume | 20 µL |
- Prepare the following reaction mix on ice:
- Thermal Cycling:
- Use the following cycling protocol:
| Step | Temperature | Time | Purpose || :--- | :--- | :--- | :--- || Reverse Transcription | 50°C | 10-15 min | cDNA synthesis || Enzyme Activation | 95°C | 2 min | Polymerase activation || Denaturation | 95°C | 15 sec | |`| Annealing/Extension | 60°C | 60 sec | 45 cycles | Primer annealing & amplification |
- Use the following cycling protocol:
- Result Interpretation: A sample is considered positive if the amplification curve crosses the threshold line within 40 cycles, with a Cq value < 40. The positive control should amplify, and the no-template control (NTC) and negative extraction control should show no amplification.
Visualized Workflows & Pathways
PCR Workflow in Clinical Diagnostics
Diagnostic Strategy in Clinical Virology
The Scientist's Toolkit
The following table lists key reagents and their critical functions for developing and executing robust PCR-based assays in the featured applications.
Table 3: Essential Research Reagent Solutions for PCR-Based Applications
| Reagent/Material | Function & Importance | Application Example |
|---|---|---|
| qPCR Master Mix | Contains DNA polymerase, dNTPs, and optimized buffer. Engineered for high sensitivity, specificity, and resistance to inhibitors found in clinical samples (e.g., from FFPE tissue or plasma) [60]. | Core component for all qPCR assays in oncology, PGx, and virology. |
| Inhibitor-Resistant Polymerase | Specialized enzymes that tolerate common PCR inhibitors (heparin, hemoglobin, etc.), ensuring reliable amplification from challenging clinical matrices [60]. | Essential for direct detection from blood, serum, or extracted nucleic acids. |
| Multiplex Assay Panels | Pre-designed sets of primers and probes for simultaneous detection of multiple targets (mutations, pathogens, alleles) in a single reaction [60]. | NSCLC mutation profiling [60]; Multi-pathogen detection panels [65]. |
| Ambient-Stable Lyophilized Reagents | Master mixes or full assays lyophilized into pellets for storage and transport without cold chain, ideal for decentralized or point-of-care testing [60]. | Rapid deployment in field settings for outbreak response [59]. |
| CRISPR-Cas Enzymes (e.g., Cas12, Cas13) | Used in conjunction with pre-amplification (e.g., RPA) for highly specific nucleic acid detection. Enables development of rapid, lateral-flow readout tests [59] [43]. | Post-amplification detection for SARS-CoV-2, dengue, etc. [59] [65]. |
Enhancing Diagnostic Fidelity: Tackling Technical Challenges and Optimizing Assay Performance
In the field of clinical virology, the polymerase chain reaction (PCR) has revolutionized diagnostic techniques, enabling the rapid and sensitive detection of viral nucleic acids. Multiplex PCR, a variant in which more than one target sequence is amplified in a single reaction using multiple primer pairs, has significantly increased the diagnostic capacity of this technology [66]. It allows laboratories to conserve valuable time, effort, and sample material while comprehensively testing for viral, bacterial, or other infectious agents [66]. However, the development and application of multiplex PCR assays are fraught with technical challenges that can jeopardize their sensitivity and specificity.
This application note addresses three major pitfalls in multiplex PCR: primer dimer formation, PCR inhibition, and amplification bias. These issues are particularly pertinent in clinical virology, where accurate diagnosis directly impacts patient management and public health responses. We provide detailed, evidence-based strategies and protocols to overcome these challenges, ensuring reliable results for researchers, scientists, and drug development professionals.
Understanding the Pitfalls
Primer Dimer Formation
Primer dimers are short, unintended DNA fragments that form when PCR primers anneal to each other instead of to the target DNA template [67] [68]. This occurs primarily through two mechanisms:
- Self-dimerization: A single primer contains regions complementary to itself.
- Cross-dimerization: Two different primers have complementary regions that allow them to bind together [68].
Once formed, these primer-template complexes provide free 3' ends that DNA polymerase can extend, leading to the amplification of nonspecific products. In multiplex assays, the presence of numerous primer pairs exponentially increases the chance of such spurious interactions [66]. Primer dimers consume reaction resources (polymerase, dNTPs, primers) and can be amplified more efficiently than the desired target, thereby reducing the overall yield and sensitivity of the assay [67] [69].
PCR Inhibition
PCR inhibition remains a significant obstacle in clinical diagnostics. Inhibitors can be co-extracted with nucleic acids from clinical specimens (e.g., blood, sputum, swabs) and include substances such as hemoglobin, heparin, urea, and immunoglobulin G. These compounds interfere with the PCR through various mechanisms, including:
- Degradation of nucleic acids.
- Binding to essential divalent cations like Mg²⁺.
- Denaturation of the DNA polymerase enzyme. The presence of inhibitors can lead to reduced amplification efficiency, false-negative results, and an overall decrease in assay robustness.
PCR Bias in Multiplex Assays
In a multiplex reaction, the goal is to amplify all targets with similar efficiency. However, preferential amplification of one target over another is a common phenomenon, leading to biased template-to-product ratios [66]. Two major classes of processes induce this bias:
- PCR Drift: Stochastic fluctuations in reagent interactions during the early cycles, particularly at very low template concentrations [66].
- PCR Selection: An inherent favoritism for amplifying certain templates due to their properties, such as GC content, secondary structures, gene copy number, or the binding efficiency of the primers used [66]. This bias can skew quantification and lead to misinterpretation of results, especially in applications designed to determine viral load or gene expression.
Optimizing Reaction Components and Conditions
Systematic optimization of the PCR reaction is fundamental to overcoming the pitfalls described. The following table summarizes key parameters and their optimization strategies.
Table 1: Optimization Strategies for Multiplex PCR Components and Conditions
| Parameter | Challenge | Optimization Strategy | References |
|---|---|---|---|
| Primer Design | Self-complementarity, cross-homology, primer dimers. | Use software to ensure primers are 18-30 bp, have 40-60% GC content, and similar Tm (within 5°C). Avoid complementary 3' ends. | [66] [70] |
| Primer Concentration | High concentration promotes primer-dimer formation. | Titrate primer concentration (e.g., 0.05-1 μM). A typical starting point is 0.2-0.4 μM per primer. | [66] [71] |
| Annealing Temperature | Low temperature causes non-specific binding and primer dimers. | Perform a gradient PCR to determine the highest possible annealing temperature that maintains efficient amplification. | [70] [68] |
| MgCl₂ Concentration | Suboptimal Mg²⁺ affects enzyme fidelity and primer annealing. | Titrate MgCl₂ concentration (e.g., 1.5 mM to 5.0 mM) to find the optimal level for the specific multiplex assay. | [70] [71] |
| Hot-Start Polymerase | Non-specific extension during reaction setup. | Use hot-start Taq polymerase to inhibit enzyme activity until the first high-temperature denaturation step. | [67] [66] [68] |
| PCR Additives | Secondary structures in GC-rich templates; general instability. | Include additives like DMSO (1-10%), Betaine (0.5 M-2.5 M), or BSA (10-100 μg/mL) to improve specificity and yield. | [66] [70] |
Workflow for Multiplex PCR Assay Optimization
The following diagram illustrates a systematic workflow for developing and optimizing a multiplex PCR assay, integrating the strategies from Table 1 to mitigate common pitfalls.
Advanced Techniques and Protocols
A Detailed Protocol for a 9-Plex PCR Assay
The following protocol is adapted from a study that successfully developed three multiplex systems for simultaneous identification of nine E. coli virulence factors, demonstrating principles directly applicable to clinical virology [72].
Objective: To simultaneously amplify nine target genes in a single reaction tube with high specificity and minimal primer dimer formation.
Materials & Reagents:
- Template DNA: 2 μL of total extracted DNA.
- Primers: 15 pmol of each of the nine forward and reverse primers.
- PCR Master Mix:
- 5.0 μL of 10X Taq DNA polymerase buffer.
- 1.0 μL of 10 mM dNTP mix (final concentration 200 μM).
- 1.0 μL of 50 mM MgCl₂ (final concentration 1 mM).
- 1.0 unit of Taq DNA polymerase (e.g., from Invitrogen).
- Sterile distilled water to a final volume of 50 μL.
Thermal Cycling Conditions:
- Initial Denaturation: 95°C for 5 minutes. (This step is critical for hot-start activation and complete denaturation of the template).
- Amplification (45 cycles):
- Denaturation: 95°C for 30 seconds.
- Annealing: 55°C for 30 seconds. (This temperature was empirically determined via a gradient from 53°C to 58°C).
- Extension: 72°C for 45 seconds.
- Final Extension: 72°C for 5 minutes.
- Hold: 4°C.
Analysis:
- Separate PCR products by agarose gel electrophoresis (2% gel).
- Visualize DNA bands under ultraviolet light.
Key Optimization Steps from the Protocol:
- The primer concentration was tested at 10, 15, and 20 pmol per reaction to find the optimal signal-to-noise ratio.
- A temperature gradient was essential to identify the optimal annealing temperature of 55°C, which balanced specificity and yield for all nine primer pairs.
- The use of a standardized hot-start Taq polymerase was implicit in the protocol to prevent nonspecific amplification during setup [72].
Incorporating Molecular Barcodes to Reduce Artifacts
For high-sensitivity applications such as detecting low-frequency viral variants, incorporating molecular barcodes (or Unique Molecular Identifiers, UMIs) can significantly reduce amplification artifacts and biases [73].
Principle: A short random nucleotide sequence (the barcode) is incorporated into each primer molecule during synthesis. During the reverse transcription or first PCR cycle, each original template molecule is tagged with a unique barcode. All subsequent amplicons derived from that original molecule will share the same barcode.
Application: This allows bioinformatic removal of PCR duplicates, which arise from the preferential amplification of certain molecules and are a major source of quantification bias. Furthermore, it helps distinguish true low-frequency mutations from polymerase errors that occur in later PCR cycles, as a true mutation will be present in all reads sharing the same barcode [73].
Table 2: Research Reagent Solutions for Advanced Multiplex PCR
| Reagent / Solution | Function / Explanation | Example Application | |
|---|---|---|---|
| Hot-Start DNA Polymerase | Remains inactive until a high-temperature step, minimizing primer dimer formation during reaction setup. | Essential for all multiplex PCR to increase specificity. | |
| Self-Avoiding Molecular Recognition Systems (SAMRS) | Modified nucleotides that pair with natural bases but not with each other, drastically reducing primer-primer interactions. | For highly multiplexed assays or SNP detection to avoid primer dimers. | [69] |
| PCR Additives (e.g., Betaine, DMSO) | Destabilize DNA secondary structures, homogenize melting temperatures of heterogenous templates, and prevent enzyme stalling. | Crucial for amplifying GC-rich viral genomes or regions with high secondary structure. | [66] [70] |
| Molecular Barcodes (UMIs) | Short random sequences incorporated into primers to uniquely tag each original template molecule for bioinformatic tracking. | Enables accurate quantification and detection of rare variants in deep sequencing. | [73] |
Mechanism of Hot-Start Polymerase in Preventing Primer Dimers
Hot-start polymerase is a cornerstone technique for minimizing early-stage nonspecific amplification. The following diagram details its mechanism of action compared to a standard polymerase.
The challenges of primer dimer formation, inhibition, and amplification bias are significant but surmountable obstacles in multiplex PCR for clinical virology. A methodical approach that combines meticulous in-silico primer design, empirical optimization of reaction components, and the adoption of advanced techniques such as hot-start enzymes and molecular barcoding is key to developing robust and reliable diagnostic assays. By implementing the detailed protocols and strategies outlined in this application note, researchers and drug development professionals can enhance the accuracy, sensitivity, and specificity of their multiplex PCR assays, thereby strengthening the foundation of modern molecular diagnostics.
Application Note
This document provides detailed protocols and optimized parameters for Polymerase Chain Reaction (PCR) setup, focusing on primer design, hot-start techniques, and reaction additives. These methods are essential for enhancing the specificity, sensitivity, and reliability of PCR assays in clinical virology diagnostics, enabling accurate detection of viral pathogens such as SARS-CoV-2, Cytomegalovirus, HIV, and Hepatitis B and C viruses [74] [75].
Primer Design and Optimization
Careful primer design is the most critical factor for successful PCR, especially for multiplex assays and specific viral detection.
Core Principles for Primer Design
The following parameters should be considered for designing effective primers:
- Length: Optimum length of 18–30 nucleotides [66]
- GC Content: Between 35% and 60% for stable annealing [66]
- Annealing Temperature (Tm): All primers in a reaction should have similar Tm values (within 5°C) [76]
- Specificity: Primers must not display significant homology to non-target sequences or form internal secondary structures [66]
- 3'-End Stability: Avoid complementary 3' ends to prevent primer-dimer formation [77]
Three-Step Optimization Protocol for Viral Targets
Based on SARS-CoV-2 primer development, follow this systematic protocol [1]:
- Target Selection: Choose conserved regions of the viral genome (e.g., RdRP, N, E, and S genes for SARS-CoV-2)
- In Silico Validation: Verify primer and amplicon sequences using bioinformatics tools to ensure specificity
- Experimental Optimization: Optimize primer concentrations and annealing temperatures to eliminate spurious primer dimers
Multiplex PCR Primer Considerations
When designing primers for multiplex PCR to detect multiple pathogens simultaneously:
- Design all primer pairs to have nearly identical optimum annealing temperatures [66]
- Ensure primers do not display significant homology to one another [66]
- Design amplicons to be of distinct sizes that can be resolved by gel electrophoresis [76]
Table 1: Troubleshooting Common Primer-Related Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| No amplification | Primer-template mismatch, poor primer design | Verify primer specificity, redesign primers |
| Multiple bands | Low annealing temperature, nonspecific binding | Increase annealing temperature, use touchdown PCR [76] |
| Primer-dimer formation | 3'-end complementarity | Redesign primers, use hot-start polymerase [78] |
| Preferential amplification in multiplex PCR | Different primer efficiencies | Redesign primers to have similar Tm and GC content [66] |
Hot-Start PCR Techniques
Hot-start PCR methodologies significantly improve assay specificity by preventing nonspecific amplification during reaction setup.
Protocol for Hot-Start PCR Implementation
- Select appropriate hot-start method based on experimental requirements (see Table 2)
- Prepare reaction mix on ice or at room temperature depending on polymerase stability
- Include initial activation step in thermal cycler program (typically 10 minutes at 95°C for antibody-based methods) [79]
- Proceed with standard cycling parameters
Comparison of Hot-Start Technologies
Table 2: Commercial Hot-Start Technologies Comparison
| Technology | Mechanism | Activation | Benefits | Limitations |
|---|---|---|---|---|
| Antibody-based (e.g., Platinum II Taq, DreamTaq Hot Start) | Antibody blocks active site | Short initial denaturation (2-5 min at 95°C) [78] | Full enzyme activity after activation; short activation time [78] | Animal-origin components; higher exogenous proteins [78] |
| Chemical modification (e.g., AmpliTaq Gold) | Covalent modification with chemical groups | Longer activation (10 min at 95°C) [78] | Stringent inhibition; free of animal components [78] | Longer activation time; may affect long targets (>3 kb) [78] |
| Affibody-based (e.g., Phire Hot Start II) | Alpha-helical peptides block active site | Short activation time [78] | Less protein than antibody method; animal-free [78] | Potentially less stringent; limited bench stability [78] |
| Aptamer-based | Oligonucleotides block active site | Short activation time [78] | Animal-free components; short activation [78] | May be less stringent; reversible activation [78] |
Reaction Additives and Enhancers
PCR additives can overcome common challenges such as inhibition from clinical samples and difficult template structures.
Protocol for PCR Enhancer Cocktail (PEC) for Direct Blood Amplification
This protocol enables direct amplification from crude blood samples without DNA purification [79]:
Prepare base reaction mixture containing:
- 1X PCR buffer
- 2 U of inhibitor-resistant Taq polymerase (e.g., OmniTaq or Omni Klentaq)
- 0.2 μM of each primer
- 200 μM dNTP mix
- 2.5-3.5 mM MgCl₂
Add PCR enhancer cocktail containing:
- 0.1-0.5% Nonidet P-40
- 10-20 mM l-carnitine
- 0.5-1 M d-(+)-trehalose
- 0.1-0.5 U/μL heparin (if inhibiting heparinase is not present in polymerase)
Add crude sample (whole blood, plasma, or serum) to constitute 25% of final reaction volume
Perform thermal cycling with initial denaturation at 95°C for 10 minutes, followed by 35-40 cycles of denaturation (95°C for 30s), annealing (primer-specific Tm for 30s), and extension (72°C for 1 min/kb)
Specialized Additives for Challenging Templates
Table 3: PCR Additives and Their Applications
| Additive | Recommended Concentration | Primary Function | Optimal Use Cases |
|---|---|---|---|
| DMSO | 2-10% | Disrupts secondary structure | GC-rich templates (>65% GC) [76] |
| Betaine | 0.5-1.5 M | Equalizes DNA melting temperatures | GC-rich templates, reduces base composition bias [66] |
| BSA | 0.1-0.5 μg/μL | Binds inhibitors | Crude samples, blood, soil [66] |
| Trehalose | 0.5-1 M | Osmoprotectant, stabilizes enzymes | Inhibitor-rich samples, direct PCR [79] |
| l-carnitine | 10-20 mM | Enhances polymerase processivity | Inhibitor-rich samples, direct PCR [79] |
| Glycerol | 5-15% | Destabilizes DNA duplexes | GC-rich templates, enhances specificity [66] |
Integrated Workflow for Clinical Virology Diagnostics
The following workflow diagrams illustrate optimized PCR procedures for clinical virology applications.
PCR Optimization Workflow for Viral Detection
Direct PCR Protocol from Clinical Samples
Research Reagent Solutions
Table 4: Essential Reagents for Optimized PCR in Virology Diagnostics
| Reagent Category | Specific Examples | Function in PCR | Clinical Application |
|---|---|---|---|
| Hot-Start Polymerases | Platinum II Taq, AmpliTaq Gold, Phire Hot Start II | Prevents nonspecific amplification during setup [78] | All viral detection assays |
| Inhibitor-Resistant Enzymes | OmniTaq, Omni Klentaq | Tolerates PCR inhibitors in blood and soil [79] | Direct PCR from blood, tissue |
| PCR Enhancers | GC Solution, Q-Solution, PEC cocktail | Facilitates amplification of difficult templates [79] [76] | GC-rich viruses, direct detection |
| Reverse Transcriptases | SuperScript III | Efficient cDNA synthesis from RNA viruses [1] | RNA virus detection (SARS-CoV-2, HIV, HCV) |
| Fluorescent Detection Reagents | SYBR Green, TaqMan probes | Real-time amplicon detection [80] [75] | Quantitative viral load monitoring |
Quality Control and Validation in Clinical Virology
For regulatory compliance and reliable patient results, implement these quality measures:
- Quantitation Standards: Use WHO International Standards for viral load assays to ensure inter-laboratory consistency [75]
- Controls: Include positive, negative, and internal controls in each run to monitor for contamination and inhibition [74]
- Result Interpretation: Differentiate between limit of detection (LOD) and limit of quantitation (LOQ) for accurate reporting [75]
- Inhibition Monitoring: Use internal control templates to identify samples with PCR inhibitors [75]
Implementing these optimized protocols for primer design, hot-start techniques, and reaction additives will significantly enhance PCR performance in clinical virology diagnostics. The methods described here improve detection sensitivity for low viral loads, increase specificity to reduce false positives, and enable direct amplification from crude clinical samples, ultimately supporting accurate patient diagnosis and treatment monitoring.
Serological tests, which detect pathogen-specific antibodies in blood serum, are indispensable tools in clinical virology for diagnosing past infections, evaluating immune status, and informing public health policy [10] [81]. However, their design and interpretation are fraught with challenges that can compromise diagnostic accuracy. Conventional serological immunoassays, primarily indirect formats like Enzyme-Linked Immunosorbent Assays (ELISA) and Lateral Flow Immunoassays (LFI), are hampered by limitations such as semi-quantitative measurements, lack of universal reference standards, potential cross-reactivity, and difficulties in multiplexing the complete panel of immunoglobulin isotypes and subclasses [82]. These issues become critically important when tests are deployed for population screening, where low disease prevalence magnifies the impact of false positives, or when diagnosing individuals who mount a weak or atypical antibody response [13] [82].
The recent COVID-19 pandemic underscored these vulnerabilities. Early in the pandemic, serological tests with diagnostic specificities as low as 95% were deployed. In a population with a true disease prevalence of 0.1%, such tests would produce overwhelmingly more false positive results than true positives, leading to vastly incorrect estimates of "herd immunity" and potentially undermining public trust in evidence-based medicine [82]. Furthermore, studies consistently identified a subpopulation of PCR-confirmed, symptomatic COVID-19 patients (~5%) who remained seronegative across a wide range of assays and antigens, highlighting a significant gap in our ability to detect all infections [83]. This application note, framed within a broader thesis on clinical virology diagnostics, details these core limitations—cross-reactivity, false positives in low-prevalence settings, and seronegative subpopulations—and provides researchers and drug development professionals with validated experimental protocols and data analysis frameworks to address them.
Quantitative Analysis of Serological Performance
The diagnostic accuracy of serological tests is not an intrinsic property but varies remarkably based on the assay technology, viral antigen target, and the patient population in which it is used [13]. The following tables summarize key performance data from large-scale clinical studies, illustrating the scope of the challenge.
Table 1: Diagnostic Sensitivity of Various Serological Assays for Identifying Previous COVID-19
| Assay Technology | Target Antigen | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| Electrochemiluminescence Immunoassay (ECLIA) | Nucleocapsid (N) | 86.8 | 98.4 |
| Enzyme-Linked Immunosorbent Assay (ELISA) | S1 subunit of Spike | 86.2 | 98.2 |
| Chemiluminescence Immunoassay (CLIA) | S1/S2 subunit of Spike | 84.7 | 97.6 |
| Lateral Flow Immunoassay (LFI) | Receptor-Binding Domain (RBD) | 84.0 | 96.1 |
| Chemiluminescence Immunoassay (CLIA) | Nucleocapsid (N) | 81.0 | 98.3 |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Receptor-Binding Domain (RBD) | 79.2 | 97.2 |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Nucleocapsid (N) | 65.6 | 97.7 |
Source: Adapted from a prospective cross-sectional study of 2,573 healthcare workers and 1,085 inpatients at a Swiss University Hospital [13].
Table 2: Impact of Disease Prevalence on Serological Test Predictive Values
| Prevalence Scenario | Test Specificity | Positive Predictive Value (PPV) | Key Interpretation |
|---|---|---|---|
| High (15%) | 97.7% - 100% | Profoundly impacted [83] | PPV is significantly lower than specificity; many false positives expected in low prevalence. |
| Low (5%) | 97.7% - 100% | Profoundly impacted [83] | |
| Very Low (0.1%) | 95% | <2% | In early pandemic, >98% of positive results would be false positives [82]. |
| Infection Status | Correlation with Neutralizing Antibodies | Sensitivity for Prediction | Key Finding |
| Previous COVID-19 | Anti-S1 ELISA | 92.7% | Sensitivity for predicting neutralizing antibodies is distinct from sensitivity for identifying past infection. |
| Anti-N ECLIA | 91.7% | ||
| Anti-S1/S2 CLIA | 90.3% | ||
| Anti-RBD+LFI | 87.9% |
Source: Compiled from multi-center validation and clinical performance studies [83] [13].
Experimental Protocols for Investigating Limitations
To systematically address serological limitations, researchers must employ rigorous and standardized methodologies. The following protocols are designed for flexibility and can be adapted to various pathogens.
Protocol 1: Evaluating Cross-Reactivity
Objective: To determine the extent to which a serological assay produces false positive results due to antibodies from previous infections with related pathogens or other host factors.
Materials:
- Research Reagent Solutions:
- Panel of Well-Characterized Sera: Includes samples from patients with confirmed infections by related pathogens (e.g., other coronaviruses, influenza, dengue), patients with autoimmune conditions, and pre-pandemic samples [13] [81].
- Reference Standard: A gold-standard reference such as PCR confirmation or viral neutralization assay to define true negative status [13].
- Serological Assays: The test assay(s) under investigation and comparator assays with different antigen targets [13].
Methodology:
- Sample Panel Assembly: Compile a minimum of 200 retrospective serum/plasma samples from individuals with no history of infection with the target pathogen (as confirmed by PCR). This panel should be enriched with samples from individuals with known exposures to antigenically similar pathogens [83] [81].
- Blinded Testing: Process all samples using the test assay according to the manufacturer's instructions or established in-house protocol. The operator should be blinded to the clinical and exposure status of the samples.
- Data Analysis: Calculate the assay's specificity as (Number of True Negatives / Total Number of Negative Samples) × 100. Manually inspect and retest any samples yielding false positive results to investigate patterns, such as association with a specific related pathogen [13].
Protocol 2: Assessing Impact in Low-Prevalence Populations
Objective: To model the real-world clinical utility of a serological test when deployed for screening populations with a low prior probability of infection.
Materials:
- Research Reagent Solutions:
- Prevalence Simulation Software: Statistical software (e.g., R, SAS) or calculators capable of computing Bayesian statistics (Positive Predictive Value, PPV; Negative Predictive Value, NPV).
- Validation Cohort: A dataset or sample collection with known true positive and true negative status, used to establish the test's true sensitivity and specificity [13] [83].
Methodology:
- Define Test Parameters: Precisely determine the test's sensitivity and specificity through a controlled validation study against a reference standard, as outlined in Protocol 1 and using data from studies like those in Table 1 [13].
- Prevalence Modeling: Use the following formulas to calculate PPV and NPV across a spectrum of prevalence settings (0.1% to 20%):
- ( PPV = \frac{Sensitivity \times Prevalence}{(Sensitivity \times Prevalence) + ((1 - Specificity) \times (1 - Prevalence))} )
- ( NPV = \frac{Specificity \times (1 - Prevalence)}{(Specificity \times (1 - Prevalence)) + ((1 - Sensitivity) \times Prevalence)} )
- Interpretation and Reporting: Graph PPV against prevalence. Clearly report the minimum prevalence required for the test to achieve a PPV of >90% or another clinically relevant threshold [82].
Protocol 3: Characterizing Seronegative Subpopulations
Objective: To identify and investigate the immunological and clinical characteristics of infected individuals who fail to seroconvert.
Materials:
- Research Reagent Solutions:
- Clinical Cohort: Paired samples (longitudinal if possible) from patients with confirmed active infection (via PCR or antigen test) who subsequently test negative by serology [83].
- Multiplex Serology Panels: Assays that can detect multiple antibody isotypes (IgG, IgM, IgA) and subclasses (e.g., IgG1-4) against a range of viral antigens (e.g., Spike, Nucleocapsid, RBD) [13] [82].
- Cellular Immunity Assays: Kits for evaluating T-cell responses (e.g., IFN-γ ELISpot, activation-induced marker assays).
Methodology:
- Case Identification: From a cohort of PCR-positive individuals, identify those who test negative ("non-responders") across multiple serological assays and time points post-onset of symptoms [83].
- Deep Immunophenotyping:
- Test residual samples from seronegative patients with more sensitive or alternative platforms (e.g., immunoaffinity proteomics, phage display immunoassays) [82].
- Evaluate for the presence of antigen-specific T-cell responses to confirm immunological exposure despite seronegativity.
- Correlative Analysis: Analyze demographic (age, sex), clinical (disease severity, comorbidities), and immunological data to identify factors associated with seronegative status [83].
Visualizing Experimental Strategy and Analysis
The following diagrams outline the core experimental workflows and decision-making processes for the protocols described above.
Experimental Strategy for Serological Validation
Analysis Pathway for Seronegative Cases
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their specific functions in the described experimental protocols.
Table 3: Key Research Reagents for Serological Validation Studies
| Research Reagent | Critical Function & Rationale |
|---|---|
| Well-Characterized Serum Panels | Serves as the ground truth for determining assay specificity and cross-reactivity. Must include samples from individuals infected with related pathogens and pre-pandemic controls [13] [81]. |
| Reference Standard (e.g., PCR, Viral Neutralization) | Provides definitive classification of true positive and true negative infection status, against which the index serological test is validated [13]. |
| Multiplex Serology Assays | Enables simultaneous detection of antibody isotypes (IgG, IgM, IgA) and subclasses against multiple antigen targets, providing a detailed humoral immune profile and increasing the chance of detecting low-level responses [13] [82]. |
| Cellular Immunity Assay Kits (e.g., ELISpot) | Confirms pathogen exposure in seronegative individuals by measuring T-cell memory responses, which are independent of antibody production [83]. |
| Statistical Analysis Software | Calculates performance metrics (sensitivity, specificity, PPV, NPV) and models test performance across different epidemiological scenarios [83] [82]. |
Discussion and Concluding Remarks
The limitations of serological testing—cross-reactivity, poor PPV in low-prevalence settings, and seronegative subpopulations—are not merely theoretical but have direct, profound implications for clinical management and public health policy. The data show that performance varies significantly between assays, meaning that "serology" cannot be treated as a monolith [13]. The finding that approximately 5% of infected individuals are seronegative underscores that even highly sensitive tests will miss a clinically relevant minority, potentially impacting individual patient care and population-level immunity estimates [83].
Future directions in serological diagnostics must focus on next-generation technologies. Immunoaffinity proteomics, which couples affinity enrichment with mass spectrometric detection, offers a promising path forward by enabling multiplexed, quantitative measurement of specific immunoglobulin isotypes and subclasses against numerous antigens simultaneously, potentially minimizing cross-reactivity through superior resolution [82]. Furthermore, a comprehensive diagnostic strategy should not rely on serology alone. Integrating serological data with PCR-based molecular tests for active infection and assays for cell-mediated immunity provides a more complete picture of an individual's infectious status and immunological history, ensuring that both humoral and cellular responses are accounted for in research and clinical decision-making [83] [84]. By adopting the rigorous experimental frameworks and validation protocols outlined here, researchers and drug developers can significantly advance the accuracy and utility of serological diagnostics.
In clinical virology, the accurate detection of pathogens is paramount for patient management, infection control, and public health responses. The diagnostic efficacy of modern laboratory techniques, primarily polymerase chain reaction (PCR) and serology, is not merely a function of assay precision but is profoundly influenced by pre-analytical variables, most critically the timing of sample collection and the selection of appropriate specimen types. The fundamental relationship between the pathogen's life cycle and the host's immune response dictates a dynamic diagnostic window. Nucleic acid-based methods like PCR typically detect the presence of the pathogen during the acute phase of infection, while serological assays identify the host's antibody response, which matures days to weeks later [85]. Misalignment between sample collection and these biological timelines can significantly reduce diagnostic yield, leading to false negatives and impeding clinical decision-making. This application note, framed within a broader thesis on clinical virology diagnostics, synthesizes current research to provide detailed protocols and data-driven recommendations for optimizing sample timing and selection to maximize the sensitivity and specificity of both PCR and serological assays for researchers, scientists, and drug development professionals.
The Diagnostic Windows of PCR and Serology
The efficacy of a diagnostic test is intrinsically linked to the pathophysiology of the infection. The journey of a pathogen within a host follows a predictable sequence: an initial incubation period with replicating pathogen, followed by an immune response. This sequence creates two primary, and often sequential, diagnostic windows.
The PCR Window: Detecting the Pathogen
PCR and other nucleic acid amplification tests are designed to detect the genetic material of the pathogen. Consequently, they are most effective during the acute phase of infection, when the pathogen is actively replicating and present in bodily fluids and tissues. The sensitivity of PCR is therefore highest from the onset of symptoms through the initial days of illness. However, this sensitivity is not static and can be influenced by the timing of sample collection relative to symptom onset and the type of specimen collected [86]. For instance, the compartmentalization of the pathogen can change over time; while blood may be the optimal sample early on, other specimens like urine or respiratory secretions may become more relevant later in the infection course.
The Serology Window: Detecting the Immune Response
Serological assays detect immunoglobulins (IgM, IgA, and IgG) produced by the host in response to the infection. These antibodies take time to develop to detectable levels. IgM antibodies are typically the first to appear, often within the first week after symptom onset, indicating a recent or current infection. IgG antibodies appear later, usually after 10-14 days, and are associated with longer-term immunity and past infection [85] [87]. Therefore, serology is most valuable for retrospective diagnosis, epidemiological studies, and determining immune status. Collecting a sample too early, before seroconversion, will result in a false negative.
Table 1: Optimal Diagnostic Windows for Key Pathogens
| Pathogen | Optimal Sample Timing for PCR | Optimal Sample Timing for Serology (IgG) | Preferred PCR Sample Type(s) |
|---|---|---|---|
| SARS-CoV-2 | Within first week of symptoms [85] | >10-14 days post-symptom onset [87] | Nasopharyngeal swab, saliva [85] |
| Leptospira spp. | Blood: 0-7 days; Urine: >4 days post-symptoms [86] | >10 days for MAT [86] | Blood, Urine [86] |
| Mycoplasma pneumoniae | Early after symptom onset, prior to antibiotics [27] | Late presentation (>2 weeks) [27] | Respiratory secretions |
Quantitative Impact of Timing on Test Sensitivity
The relationship between test sensitivity and the timing of sample collection is quantifiable and critical for diagnostic accuracy. Clinical studies consistently demonstrate that deviations from optimal sampling windows directly reduce the probability of a true positive result.
A landmark study on leptospirosis diagnosis quantitatively illustrated this phenomenon. The research analyzed the sensitivity of blood and urine PCR tests in relation to the number of days since symptom onset. The findings were striking: the overall sensitivity of urine PCR was significantly higher than that of blood PCR (84% vs. 70%). Furthermore, the sensitivity of blood PCR demonstrated a statistically significant decrease over time (adjusted Odds Ratio 0.56 per day, 95% CI [0.44–0.73]). The predicted probability of a positive urine PCR surpassed that of a positive blood PCR as early as four days after symptom onset. This study underscores the necessity of considering not just the test type, but also the sample type and timing in the diagnostic workflow [86].
Similarly, a study on Mycoplasma pneumoniae in children with community-acquired pneumonia revealed a stark contrast in sensitivity between PCR and serology based on timing. In confirmed cases, serology (IgM) was positive in 90% of patients, while PCR was positive in only 40%. This highlights that for patients presenting later in their illness, serology is the more sensitive tool. The authors concluded that "clinicians could consider real-time PCR testing if the patient presents early after onset of symptoms and prior to the use of empirical antibiotics and serology should be the test of choice at late presentations" [27].
For SARS-CoV-2, the performance of serological assays is also highly time-dependent. One evaluation found that the sensitivity of IgG assays was lower (70.8% to 80%) within the first two weeks from the onset of symptoms, rising to over 80% thereafter. In contrast, IgM assays consistently showed low sensitivity (47.6% to 54.6%), making them a less reliable marker for acute infection [87].
Table 2: Impact of Timing on Test Sensitivity: Leptospirosis PCR Example
| Days Post-Symptom Onset | Predicted Probability of Positive Blood PCR (%) | Predicted Probability of Positive Urine PCR (%) |
|---|---|---|
| Day 3 | ~78% | ~75% |
| Day 4 | ~70% | ~80% |
| Day 5 | ~60% | ~84% |
| Day 6 | ~50% | ~87% |
| Day 7 | ~40% | ~89% |
Data derived from [86]
Experimental Protocols for Diagnostic Optimization
Protocol 1: Combined PCR and Serology Testing for Acute Respiratory Infections
This protocol is designed to maximize diagnostic yield for pathogens like SARS-CoV-2 and Mycoplasma pneumoniae by leveraging both molecular and serological techniques in a timed manner.
1. Sample Collection (Day 0-7 of Illness):
- PCR Sample: Collect a nasopharyngeal swab or saliva sample. Place the swab immediately into viral transport medium and store at 4°C for processing within 72 hours or at -80°C for longer storage.
- Acute Serology Sample: Collect 5-10 mL of whole blood into a serum separator tube. Allow it to clot for 30 minutes at room temperature, then centrifuge at 1000-2000 RCF for 10 minutes. Aliquot the serum into sterile cryovials. This is the "acute" serum sample.
2. Nucleic Acid Extraction and PCR:
- Extract viral RNA/DNA from 200 µL of the sample using a commercial silica-membrane-based extraction kit.
- Perform RT-qPCR or qPCR using a validated assay. Target at least two conserved genomic regions (e.g., ORF1ab and N protein for SARS-CoV-2) [85]. Include positive and negative controls in each run.
3. Serology Testing (on Acute Sample and Convalescent Sample):
- Assay Format: Use a high-throughput chemiluminescence immunoassay (CLIA) or enzyme-linked immunosorbent assay (ELISA) per manufacturer's instructions.
- Procedure:
4. Convalescent Sample Collection (Day 14-21):
- If the initial PCR and acute serology are negative but clinical suspicion remains, collect a second ("convalescent") serum sample as in Step 1.
5. Interpretation:
- Positive PCR: Confirms active infection.
- Seroconversion: A four-fold or greater increase in IgG titer between acute and convalescent samples confirms recent infection.
- Single Positive IgG: In the convalescent sample, indicates past infection.
Protocol 2: Optimized Paired Blood and Urine PCR for Systemic Infections
This protocol, derived from leptospirosis research, is applicable to systemic infections where pathogen compartmentalization occurs.
1. Sample Collection (First Clinical Consultation):
- Blood for PCR: Collect 5-10 mL of whole blood into an EDTA tube. Separate plasma by centrifugation at 2000 RCF for 10 minutes within 2 hours of collection. Aliquot and store at -80°C.
- Urine for PCR: Collect 2-10 mL of mid-stream urine. Process immediately by centrifuging at 12,000 rpm for 30 minutes. Discard 1.5 mL of supernatant and resuspend the pellet in the remaining 0.5 mL [86].
2. Nucleic Acid Extraction:
- Plasma: Extract nucleic acids from 200 µL of plasma using an automated or manual extraction system.
- Urine: Use the same extraction protocol as for plasma, applying it to the resuspended pellet.
3. Real-time PCR Amplification:
- Use an in-house or commercial real-time PCR assay targeting conserved, pathogen-specific genes.
- Reaction Mix: Prepare a master mix containing a DNA polymerase, dNTPs, primers, and dual-labeled probes (e.g., FAM/TAMRA) for the target and an internal control.
- Amplification: Run for 45 cycles on a real-time thermocycler. A sample is considered positive if the cycle threshold (Ct) value is below a validated limit [86].
4. Data Analysis:
- Analyze the sensitivity of blood vs. urine PCR based on the day of collection post-symptom onset. A multivariate logistic regression model can be used to identify factors associated with PCR sensitivity [86].
Optimized PCR Sampling Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential reagents and materials required for implementing the PCR and serology protocols described, based on cited literature and standard laboratory practices.
Table 3: Essential Research Reagents for Diagnostic Optimization
| Reagent/Material | Function/Application | Example Specifications & Notes |
|---|---|---|
| Viral Transport Medium | Preserves viability of viral pathogens in swab samples during transport. | Should contain antibiotics and antifungals to prevent microbial overgrowth. |
| Silica-Membrane Nucleic Acid Extraction Kit | Isolation of high-purity DNA/RNA from clinical samples (plasma, urine, swabs). | Compatible with automated systems (e.g., MagNA Pure 96). Must include carrier RNA for optimal RNA recovery. |
| Real-time PCR Master Mix | Amplification and detection of target nucleic acid sequences. | Should include DNA polymerase, dNTPs, buffer, and be compatible with multiplexing (e.g., Applied Biosystems Master Mix) [86]. |
| Primers & Probes | Specific detection of pathogen target genes. | Target conserved regions (e.g., 16S RNA, lipL32 for Leptospira; ORF1ab, N for SARS-CoV-2). Probes are typically FAM/TAMRA labeled [86] [85]. |
| Serum Separator Tube (SST) | Collection and separation of serum from whole blood for serological testing. | Standard 5-10 mL draw tubes. |
| Chemiluminescence Immunoassay (CLIA) Kit | Quantitative detection of pathogen-specific immunoglobulins (IgG, IgM) in serum/plasma. | Includes coated magnetic beads, calibrators, conjugates, and substrates. Kits are often platform-specific (e.g., for LIAISON XL or iFlash analyzers) [87]. |
| Coating Buffer | Immobilization of capture antibody or antigen to solid phase (ELISA). | 50 mM sodium bicarbonate, pH 9.6 [88]. |
| Blocking Buffer | Reduces nonspecific binding to minimize background signal. | 1% BSA or 10% host serum in TBS/TBST; or commercial protein-free blockers [88]. |
| Wash Buffer | Removes unbound reagents between assay steps. | PBS or TBS with 0.05% Tween-20 (PBST/TBST) [88]. |
| Enzyme Substrate | Generates a detectable signal (colorimetric, chemiluminescent) for quantification. | TMB (colorimetric) for HRP; pNpp for Alkaline Phosphatase [88]. |
Diagnostic Pathway Selection
Data-Driven Decisions: Analytical Validation, Comparative Performance, and Integrated Testing Strategies
Within clinical virology, the accurate detection of infectious pathogens is the cornerstone of effective patient management and public health response. Diagnostic tests, however, are not infallible. Their performance and the clinical utility of their results are governed by a set of critical metrics: sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). This application note provides a detailed framework for researchers and scientists to understand, calculate, and apply these metrics in the evaluation of virological diagnostic techniques, with a particular focus on molecular (PCR) and serological assays. We include standardized protocols for test evaluation, synthesize performance data from recent studies on SARS-CoV-2 diagnostics, and provide visual guides for test selection and result interpretation. A clear understanding of these metrics is essential for making informed decisions in both clinical practice and drug development.
The evaluation of any diagnostic test begins with a comparison against a reference method, known as the gold standard, which is the best available method for diagnosing a particular disease [89]. The results of this comparison are typically summarized in a 2x2 contingency table, which forms the basis for all subsequent calculations of test performance [89].
Table 1: Fundamental 2x2 Contingency Table for Diagnostic Test Evaluation
| Gold Standard Positive | Gold Standard Negative | |
|---|---|---|
| Test Positive | True Positive (TP) | False Positive (FP) |
| Test Negative | False Negative (FN) | True Negative (TN) |
From this table, the core metrics of test validity are derived:
Sensitivity is the ability of a test to correctly identify individuals who have the disease. It is calculated as TP / (TP + FN) and represents the probability of a positive test result when the disease is present [89] [90]. A highly sensitive test is optimal for ruling out disease, a concept often remembered by the mnemonic "SnNOUT" [89].
Specificity is the ability of a test to correctly identify individuals who do not have the disease. It is calculated as TN / (TN + FP) and represents the probability of a negative test result when the disease is absent [89] [90]. A highly specific test is optimal for ruling in disease, summarized by the mnemonic "SpPIN" [89].
It is crucial to recognize that sensitivity and specificity are generally inversely related. Adjusting a test's cutoff point to increase sensitivity (e.g., to catch more true cases) will typically decrease its specificity (leading to more false positives), and vice versa [89].
While sensitivity and specificity describe the intrinsic performance of a test, Predictive Values describe the clinical utility of a test result in a specific population.
Positive Predictive Value (PPV) is the probability that a patient with a positive test result actually has the disease. It is calculated as TP / (TP + FP) [89] [90].
Negative Predictive Value (NPV) is the probability that a patient with a negative test result truly does not have the disease. It is calculated as TN / (TN + FN) [89] [90].
Unlike sensitivity and specificity, PPV and NPV are directly influenced by the prevalence of the disease in the population being tested. As prevalence increases, PPV increases and NPV decreases. Conversely, as prevalence falls, PPV decreases and NPV increases [89]. This has profound implications for screening programs in low-prevalence settings, where even tests with excellent sensitivity and specificity can yield a high number of false positives.
Experimental Protocols for Test Evaluation
Protocol: Establishing Sensitivity and Specificity of a Serological Assay
This protocol outlines the steps for evaluating a new SARS-CoV-2 IgG ELISA, adaptable to other viral serological assays.
1. Specimen Collection and Panel Assembly:
- Positive Cohort: Collect serum/plasma from a minimum of 100 individuals with RT-PCR-confirmed SARS-CoV-2 infection. Ensure samples span a range of days post-symptom onset (e.g., 0-5, 6-10, 11-15, 16-20, >20 days) to evaluate time-dependent sensitivity [91] [92].
- Negative Cohort: Collect a minimum of 100 pre-pandemic serum/plasma samples or samples from individuals confirmed to be negative for SARS-CoV-2 by RT-PCR and potentially positive for other respiratory viruses (e.g., seasonal coronaviruses, influenza) to assess cross-reactivity and specificity [91] [92].
2. Gold Standard Testing:
- For the positive cohort, the gold standard is a positive RT-PCR test for SARS-CoV-2.
- For the negative cohort, the gold standard is the confirmed absence of SARS-CoV-2 infection, as defined above.
3. Running the Index Test:
- Perform the new ELISA test according to the manufacturer's instructions on all samples in both cohorts. Ensure technicians are blinded to the gold standard results.
4. Data Analysis:
- Construct a 2x2 table comparing the new ELISA results against the gold standard.
- Calculate Sensitivity: (TP / [TP + FN]) * 100.
- Calculate Specificity: (TN / [TN + FP]) * 100.
5. Determining a Positive Threshold:
- Analyze the distribution of signal-to-cutoff (S/CO) values or optical density (OD) readings. Establish a threshold that optimizes both sensitivity and specificity. Note that classifying weak positive bands as negative can increase specificity but at the cost of decreased sensitivity [92].
Protocol: Quantitative RT-PCR for Viral Load Monitoring
This protocol details the use of qRT-PCR for the quantitative monitoring of viral loads, critical for managing infections like CMV in transplant patients or HIV.
1. Sample Preparation:
- Extract nucleic acids from clinical samples (e.g., plasma, respiratory swabs) using an automated, reproducible system. To control for extraction efficiency and amplification inhibition, incorporate a universal internal control (e.g., a non-human seal herpesvirus, PhHV) into each sample prior to extraction [93].
2. Reaction Setup:
- Prepare a master mix containing reverse transcriptase, Taq polymerase, dNTPs, buffer, and sequence-specific primers and probes.
- Utilize a competitive real-time PCR strategy with an internal quantitation standard that uses the same primer sequence as the target for the most accurate quantitation [75].
- Include a standard curve with known concentrations of the target (traceable to an international standard, e.g., WHO International Standard) in each run to allow for absolute quantification.
3. Amplification and Detection:
- Run the plate on a real-time PCR instrument with cycling conditions optimized for the assay. The cycle threshold (CT), the cycle at which the fluorescence signal exceeds the background, is recorded for each sample and standard.
4. Data Analysis and Reporting:
- The CT value is inversely proportional to the viral copy number. Compare the CT of the sample to the standard curve to calculate the viral load in International Units per milliliter (IU/mL) [75].
- Understand the critical difference between the Lower Limit of Detection (LOD), the lowest viral level at which ≥95% of samples are detected, and the Lower Limit of Quantification (LLOQ), the lowest viral level that can be accurately measured. Report results as "detectable but below the LOQ" when appropriate [75].
Data Presentation and Analysis
Performance of SARS-CoV-2 Diagnostic Assays
Table 2: Performance Characteristics of SARS-CoV-2 Serological Assays (Head-to-Head Evaluation)
| Assay Type | Target | Sensitivity (>20 days post-symptom onset) | Specificity | Key Findings |
|---|---|---|---|---|
| Lateral Flow (LFA) Assays [92] | IgM/IgG | Wide variation; 4 tests achieved >80% | 84.3% - 100% | Specificity improved by setting a higher positivity threshold (from avg. 94.2% to 98.1%), but sensitivity decreased. |
| ELISA [92] | IgG | >80% (for top-performing tests) | >95% (for top-performing tests) | Demonstrated higher agreement with other tests than some LFAs. |
| In-house ELISA [94] | IgA, IgG, IgM (Spike protein) | Suitable sensitivity reported | Suitable specificity reported | Combining immunoglobulin classes and viral antigens improves predictive values. |
Table 3: Comparison of Molecular Assays for SARS-CoV-2 RNA Detection
| Assay Method | Principle | Time to Result | Analytical Sensitivity | Best Use Case |
|---|---|---|---|---|
| rRT-PCR [95] | Target amplification with fluorescent probe detection | ~45 min - 5 h | Varies by kit; can have reduced sensitivity (54%) late in infection (>10-14 days) | Gold standard for acute diagnosis; widely available. |
| ddPCR [95] | Absolute quantification via microdroplet partitioning | Several hours | Superior for low viral load samples; can detect virus when rRT-PCR Ct >34 | Confirming inconclusive rRT-PCR results; monitoring clearance in immunocompromised. |
| Loop-mediated Isothermal Amplification (LAMP) [95] | Isothermal amplification with multiple primers | ~1 hour | Slightly lower than rRT-PCR but suitable for rapid screening | Point-of-care testing; resource-limited settings. |
The Impact of Prevalence on Predictive Values
The following diagram illustrates the critical relationship between disease prevalence and the clinical interpretation of test results.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Virology Diagnostic Research
| Reagent / Solution | Function | Example / Note |
|---|---|---|
| International Standard | Provides a common reference for quantifying viral nucleic acids, enabling assay standardization and inter-laboratory comparison. | First WHO International Standard for SARS-CoV-2 RNA [75]. |
| Universal Internal Control | Monitors nucleic acid extraction efficiency and detects PCR inhibition; co-extracted and co-amplified with patient sample. | Phocid herpesvirus (PhHV) [93]. |
| Primer/Probe Sets | Target-specific sequences for nucleic acid amplification tests. Must be validated for sensitivity and specificity against circulating variants. | CDC N1, N2, N3; Charité E gene assay [95]. |
| Recombinant Antigens | Used as capture antigens in serological assays (ELISA, LFA) to detect virus-specific antibodies. | Full-length spike glycoprotein or nucleocapsid (N) protein of SARS-CoV-2 [94]. |
| Calibrators and Controls | Used to generate a standard curve (quantitative assays) and ensure test run validity. Should be matrix-matched to patient samples. | Commercial panels or in-house preparations traceable to international standards. |
Case Study: Application in SARS-CoV-2 Serology
The COVID-19 pandemic highlighted the practical challenges in deploying serological tests. Initial evaluations of 12 serology assays (10 LFAs and 2 ELISAs) revealed a wide range of performance. The percent of RT-PCR-positive individuals who seroconverted (test sensitivity) increased with time, peaking more than 20 days after symptom onset [92]. This finding directly informed the IDSA guideline recommendation against using serologic testing to diagnose acute SARS-CoV-2 infection within the first two weeks after symptom onset [96].
Furthermore, with high global seroprevalence due to vaccination and past infection, the positive predictive value of a single positive antibody test for diagnosing recent infection is now very low. This has led to the guideline recommendation to use assays that target the nucleocapsid (N) protein, rather than the spike (S) protein, when seeking evidence of prior natural infection in vaccinated populations, as vaccines typically induce anti-spike antibodies only [96].
The workflow for appropriate test selection and interpretation, guided by these metrics and clinical context, is summarized below.
In the field of clinical virology, the accurate and timely detection of respiratory pathogens is a cornerstone of effective patient management, infection control, and public health surveillance. The diagnostic landscape is dominated by two principal methodological approaches: serology assays, which detect host-derived antibodies against viral infections, and nucleic acid amplification tests (NAATs), notably polymerase chain reaction (PCR) platforms, which detect viral genetic material. Each approach possesses distinct advantages and operational characteristics, making them suitable for different clinical and research scenarios. This application note provides a structured, data-driven comparison of the performance of commercially available serological assays and PCR platforms, with a focus on respiratory viruses such as SARS-CoV-2, influenza, and RSV. It further delineates detailed experimental protocols to guide researchers and drug development professionals in the selection, validation, and implementation of these critical diagnostic tools.
Comparative Performance Data
Performance Metrics of Commercial Serology Assays
The diagnostic accuracy of serology assays varies significantly based on the target antigen, immunoglobulin class, and detection technology. The table below summarizes the pooled diagnostic odds ratios (DOR) for various commercial assays, as revealed by a large-scale meta-analysis [5]. A higher DOR generally indicates better overall test performance.
Table 1: Diagnostic Performance of Selected Commercial Serology Assays
| Assay Name | Manufacturer | Target Antigen | Antibody Type | Detection Method | Pooled Diagnostic Odds Ratio (DOR) |
|---|---|---|---|---|---|
| Elecsys Anti-SARS-CoV-2 | Roche | Nucleocapsid (N) | Total Antibody | ECLIA | 1022.34 |
| Elecsys Anti-SARS-CoV-2 | Roche | Not Specified | Total Antibody | ECLIA | 1701.56 |
| Abbott SARS-CoV-2 IgG | Abbott | Nucleocapsid (N) | IgG | CMIA | 542.81 |
| LIAISON SARS-CoV-2 S1/S2 IgG | DiaSorin | S1/S2 | IgG | CLIA | 178.73 |
| Euroimmun Anti-SARS-CoV-2 | EUROIMMUN | S1 | IgG | ELISA | 190.45 |
| Euroimmun Anti-SARS-CoV-2 | EUROIMMUN | Nucleocapsid (N) | IgG | ELISA | 82.63 |
| Euroimmun Anti-SARS-CoV-2 | EUROIMMUN | Not Specified | IgA | ELISA | 45.91 |
Key Observations:
- Total antibody assays (e.g., Roche Elecsys) demonstrated the highest diagnostic accuracy, followed by IgG-specific assays [5].
- Assays targeting the nucleocapsid (N) antigen generally showed superior diagnostic efficacy compared to those targeting the spike (S) protein, with a pooled DOR of 604.29 for anti-N total/IgG versus 119.88 for anti-S1 IgG [5].
- Electrochemiluminescence immunoassay (ECLIA) and chemiluminescent microparticle immunoassay (CMIA) methods exhibited superior performance compared to enzyme-linked immunosorbent assay (ELISA) and other chemiluminescence immunoassay (CLIA) methods [5].
- Independent validation studies highlight that performance can improve significantly over time, with one evaluation noting a marked increase in sensitivity for the GOLD ELISA COVID-19 IgG + IgM assay 15-21 days post-symptom onset [97].
Performance Metrics of PCR Platforms
PCR platforms offer direct detection of viral pathogens. The critical performance differentiators include turnaround time, sensitivity, and the ability to quantify viral load.
Table 2: Operational and Performance Characteristics of PCR Platforms
| Platform / Technology | Pathogens Detected | Turnaround Time | Key Performance Findings | Reference |
|---|---|---|---|---|
| Seasonal Multiplex PCR Panel | Pathogens vary by season (e.g., Influenza, RSV, S. pneumoniae) | ~12-14 hours (vs. 48-50 hours for culture) | • 80.6% diagnostic yield (vs. 61.6% for culture)• Reduced antibiotic changes by 13.7% in winter | [21] |
| AMDI Fast PCR Mini Respiratory Panel | SARS-CoV-2, Influenza A/B, RSV | < 10 minutes | • Overall Percent Agreement with comparator: 97.2% - 99.7%• 72% of discrepant results associated with low viral load | [98] |
| Digital PCR (dPCR) vs Real-Time RT-PCR | Influenza A/B, RSV, SARS-CoV-2 | Similar to RT-PCR (processing time) | • Superior accuracy for high viral loads (Influenza A/B, SARS-CoV-2)• Greater consistency for medium viral loads (RSV)• Absolute quantification without standard curves | [33] |
| QIAcuity ndPCR vs QX200 ddPCR | Synthetic targets, Paramecium DNA | N/A (Platform Comparison) | • High precision and linearity for both platforms• ndPCR LOD: 0.39 copies/µL; ddPCR LOD: 0.17 copies/µL• Restriction enzyme choice impacts precision, especially for ddPCR | [99] |
Key Observations:
- Turnaround time for PCR results has been drastically reduced with newer point-of-care systems, such as the AMDI Fast PCR, which delivers results in under 10 minutes without sacrificing clinical accuracy [98].
- Digital PCR (dPCR) platforms provide absolute quantification of viral load and demonstrate superior accuracy and consistency compared to real-time RT-PCR, particularly for medium to high viral loads, though they currently face limitations in cost and automation [33].
- Seasonally-tailored PCR panels can significantly improve diagnostic yield and antibiotic stewardship compared to traditional, season-agnostic culture methods [21].
Experimental Protocols
Protocol for a Multicenter Clinical Evaluation of a Rapid POC PCR Test
The following protocol is adapted from a multicenter study comparing the AMDI Fast PCR Mini Respiratory Panel to the Cepheid Xpert Xpress CoV-2/Flu/RSV plus test [98].
Objective: To evaluate the clinical agreement of a rapid point-of-care PCR test for simultaneous detection of SARS-CoV-2, Influenza A, Influenza B, and RSV.
Materials:
- Anterior nasal swab (ANS) collection kits.
- Proprietary AMDI Sample Buffer and Universal Viral Transport Media (UVT).
- AMDI Fast PCR Instrument and single-use test discs.
- Comparator platform (e.g., Cepheid Xpert Xpress system).
- Freezer (-70°C or below) and dry ice for sample storage and shipment.
Procedure:
- Participant Enrollment and Sample Collection:
- Prospectively enroll eligible participants presenting with symptoms of upper respiratory infection.
- Collect two ANS specimens from each participant. The order of collection (AMDI buffer vs. UVT) should be alternated consecutively to minimize bias.
- For low-prevalence pathogens, the sample size may be augmented with archived, characterized samples.
Testing with Index Method:
- Test the ANS sample collected in AMDI Sample Buffer immediately at the point-of-care using the Fast PCR MRP test.
- Load the sample onto the test disc and insert it into the Fast PCR Instrument.
- The integrated system automates sample processing, RT-PCR, and cloud-based data analysis. Record the results.
Testing with Comparator Method:
- Store the paired ANS sample in UVT at -70°C or below.
- Ship frozen samples on dry ice to a central testing facility.
- Thaw samples and test them using the comparator PCR platform according to the manufacturer's instructions.
Data Analysis:
- Calculate overall, positive, and negative percent agreement between the index and comparator tests.
- Analyze discrepant results, stratifying them by the viral load (e.g., cycle threshold values) of the sample.
Protocol for a Meta-Analysis of Serological Assay Performance
This protocol outlines the methodology for an indirect comparison of the diagnostic accuracy of multiple commercial serological assays [5].
Objective: To compare the diagnostic accuracy of seven commercial serological assays for SARS-CoV-2 using meta-analysis and indirect comparison techniques.
Materials:
- Search databases (e.g., Cochrane Library, PubMed, Embase, Web of Science).
- Data extraction forms.
- Statistical software (e.g., R with
netmeta,rjags, andgemtcpackages).
Procedure:
- Systematic Literature Review:
- Execute a comprehensive search of electronic databases for studies published within a specified timeframe.
- Apply pre-defined inclusion and exclusion criteria.
- Include studies that use RT-PCR as the reference standard and provide sufficient data to construct 2x2 contingency tables.
Data Extraction and Quality Assessment:
- Two independent reviewers should extract data: first author, publication year, assay method, target antigen, antibody type, and numbers of true positives, true negatives, false positives, and false negatives.
- Assess the quality of included studies using a validated tool such as the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2).
Statistical Analysis:
- Perform meta-analysis to calculate pooled sensitivity, specificity, and diagnostic odds ratio (DOR) for each assay.
- Conduct an adjusted indirect comparison using a network meta-analysis approach to calculate the relative diagnostic odds ratio (RDOR) between different assays.
- Construct summary receiver operating characteristic (SROC) curves and calculate the area under the curve (AUC) for each assay.
- Assess publication bias using Deek's test.
Visualized Workflows and Signaling Pathways
Diagnostic Pathway for Respiratory Infections
The following diagram illustrates the logical decision flow for selecting and interpreting diagnostic tests for respiratory viral infections, integrating both PCR and serology.
Serology Assay Workflow: ECLIA
The diagram below details the key steps and signaling mechanism of an Electrochemiluminescence Immunoassay (ECLIA), a high-performance method used in platforms like the Roche Elecsys system.
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogues essential materials and reagents referenced in the featured studies, providing researchers with a foundational list for experimental setup.
Table 3: Essential Research Reagents and Materials
| Item | Function / Application | Example Use Case / Note |
|---|---|---|
| Anterior Nasal Swab (ANS) | Collection of patient specimen for nucleic acid or antigen testing. | Used in PCR evaluations for respiratory viruses; sample collection order should be alternated to minimize bias [98]. |
| Universal Transport Media (UTM) | Preserves viral integrity for transport and storage prior to testing. | Used for comparator sample storage in PCR validation studies; requires freezing at -70°C [98]. |
| Recombinant Nucleocapsid (N) Protein | Target antigen for serological assays. | Key component in high-performance assays (e.g., Roche Elecsys, Abbott IgG); highly immunogenic [5] [100]. |
| Recombinant Spike (S1/S1-RBD) Protein | Target antigen for serological assays. | Used in assays like BioMérieux VidasIII; important for detecting vaccine-induced immunity [100]. |
| Ruthenium Complex Label | Electrochemiluminescent label for detection in ECLIA. | Upon voltage application, it emits light measured by the instrument (e.g., Roche Elecsys) [5]. |
| Restriction Enzymes (e.g., HaeIII) | Enzymatic digestion of DNA to improve accessibility for PCR. | Critical for dPCR analysis of organisms with high gene copy numbers; choice of enzyme impacts precision [99]. |
| WHO International Standard | Reference material for standardizing antibody unit measurements. | Allows for conversion of arbitrary units (AU) to Binding Antibody Units (BAU) for cross-assay comparison [101]. |
| Proprietary Sample Buffer | Specific medium for stabilizing sample for a particular platform. | Optimized for use with specific POC systems (e.g., AMDI Fast PCR) to ensure test performance [98]. |
In the evolving landscape of clinical virology and bacteriology, the limitations of relying on a single diagnostic methodology have become increasingly apparent. No single test is universally optimal across all stages of infection, particularly for pathogens with complex, multi-phase infection cycles. This application note articulates a robust diagnostic framework that synergistically combines Polymerase Chain Reaction (PCR) and serological testing to generate comprehensive patient profiles. The integrated approach detailed herein addresses the critical challenge of temporal diagnostic sensitivity, wherein the detectability of a pathogen or its associated biomarkers shifts significantly throughout the course of infection [102] [103]. By leveraging the respective strengths of molecular and immunological detection methods, researchers and clinicians can achieve a more accurate, definitive diagnosis, which is paramount for both effective patient management and advanced research, including drug and vaccine development.
This protocol is framed within a broader thesis on advancing diagnostic techniques in clinical virology. It provides detailed methodologies, performance data, and practical tools for implementing a combined testing strategy, using Anaplasmosis and SARS-CoV-2 as primary exemplars of its application.
The Diagnostic Synergy Principle
The synergy between PCR and serology is fundamentally rooted in the temporal dynamics of infection. During the initial viremic or bacteremic phase, the pathogenic nucleic acid is present and replicating, making it a prime target for PCR-based detection. Conversely, the host's adaptive immune response, characterized by the production of specific antibodies, matures and becomes detectable days to weeks later, forming the basis of serological assays [102] [103].
Pathogen-Specific Justification:
- Anaplasmosis: For Anaplasma phagocytophilum, PCR demonstrates high sensitivity (70-100%) in the first week of symptom onset, while serology is often negative, with a sensitivity of only 15-40%. This relationship inverts in subsequent weeks, with PCR sensitivity dropping below 50% and serological sensitivity rising above 90% after 4 weeks [103]. This pattern strongly supports a testing algorithm where PCR is the primary tool for acute diagnosis, and paired serology confirms the diagnosis convalescently if initial PCR is negative.
- SARS-CoV-2: Similarly, evaluations of SARS-CoV-2 serological tests have shown that the sensitivity of Rapid Lateral Flow (RLF) tests for IgG can be variable and decline over time, while ELISA-based total antibody tests maintain a sensitivity of ≥80% beyond six months post-diagnosis [104]. This underscores the utility of serology for understanding past exposures and population-level immunity, while PCR remains the gold standard for diagnosing active infection.
A combined approach mitigates the risk of false negatives that can occur when using either method in isolation at an inappropriate clinical timepoint. This is crucial for diseases like Anaplasmosis, which can present with non-specific symptoms such as fever, headache, and myalgia, and can be misdiagnosed as other conditions, including COVID-19 [105].
Performance Data & Comparative Analysis
The following tables summarize the quantitative performance characteristics of PCR and serology for the diagnosis of Anaplasmosis and SARS-CoV-2, providing a clear, data-driven rationale for a synergistic testing protocol.
Table 1: Performance Characteristics of Anaplasma phagocytophilum Diagnostic Tests Over Time
| Time Post-Symptom Onset | PCR Sensitivity (%) | Serology (IFA) Sensitivity (%) | Recommended Primary Test |
|---|---|---|---|
| Week 1 (Acute) | 70 - 100 | 15 - 40 | PCR |
| Week 2 | 50 - 100 | 40 - 90 | PCR |
| > Week 2 to 12 weeks | < 50 | > 90 (peaks at ~4 weeks) | Paired Serology |
Source: Adapted from Public Health Ontario Laboratory testing information [103].
Table 2: Evaluation of Selected SARS-CoV-2 Serological Assays
| Assay Type | Test Name | Specificity (%) | Sensitivity at ≥14 Days Post-Diagnosis | Key Performance Note |
|---|---|---|---|---|
| Rapid Lateral Flow (RLF) | PANBIO COVID-19 IgG/IgM | ≥ 95 | Variable (e.g., <80% in 2021, >80% in 2022) | IgG detection capacity decreased with time. |
| Rapid Lateral Flow (RLF) | LABNOVATION COVID-19 IgG/IgM | ≥ 95 | Variable across years | Performance fluctuated with circulating variants. |
| ELISA | PLATELIA SARS-CoV-2 Total Ab | 91 | Constantly ≥80% across 2020-2022 | Sensitivity remained >80% >6 months post-diagnosis. |
Source: Adapted from a comparative evaluation of SARS-CoV-2 serological tests [104].
Experimental Protocols
This section provides detailed, actionable methodologies for implementing the combined PCR and Serology approach.
Protocol 1: Combined PCR and Serology Algorithm for Anaplasmosis
This protocol outlines a definitive testing strategy for suspected Anaplasmosis, as recommended by public health laboratories [103].
I. Specimen Collection & Handling
- For PCR Testing (Acute Phase):
- Preferred Sample: Whole blood (5 mL) collected in EDTA tubes. Do not centrifuge. Heparin is to be avoided [103].
- Alternative Sample: Serum (1.0 mL) separated using Serum Separator Tubes (SST).
- Timing: Collect within the first 2 weeks of symptom onset, ideally before antibiotic initiation. However, do not withhold treatment if clinically indicated.
- For Serology Testing (Convalescent Phase):
- Sample: Serum (1.0 mL) separated using SST.
- Timing:
- Acute Serum: Within 2 weeks of symptom onset.
- Convalescent Serum: 2 to 12 weeks after symptom onset.
II. Testing Algorithm & Methodology
- Acute Phase Testing: Upon receipt of a specimen from a patient with suspected acute Anaplasmosis, perform a real-time PCR assay targeting the msp2 gene of A. phagocytophilum [103].
- Interpretation & Next Steps:
- PCR Positive: Report as "Anaplasma phagocytophilum DNA detected." Clinical correlation is required. This confirms active infection.
- PCR Negative: If clinical suspicion remains high and the sample was collected within the convalescent window (2-12 weeks), proceed to paired serology.
- Convalescent Phase Testing (Paired Serology):
- Method: Indirect Immunofluorescence Assay (IFA) for the semi-quantitation of IgG antibodies.
- Interpretation: A four-fold or greater increase in IFA titer between the acute and convalescent serum samples is considered confirmatory for recent infection [103].
Diagram 1: Anaplasmosis testing algorithm.
Protocol 2: SARS-CoV-2 Combined Diagnostic & Serosurveillance Strategy
This protocol leverages PCR for active infection diagnosis and serology for understanding immune response and epidemiology.
I. Active Infection Diagnosis via PCR
- Method: Real-time Reverse Transcription PCR (RT-PCR) targeting specific genes of SARS-CoV-2 (e.g., N, E, RdRp).
- Sample: Nasopharyngeal or oropharyngeal swab in viral transport media.
- Application: The definitive test for diagnosing current COVID-19 infection, crucial for patient isolation and treatment decisions [105] [106].
II. Immune Response & Sero-epidemiology via Serology
- Method 1 - Rapid Lateral Flow (RLF): Useful for rapid, point-of-care screening of IgG/IgM. However, as performance can be variable and decline over time, results should be interpreted with caution for epidemiological conclusions [104].
- Method 2 - Enzyme-Linked Immunosorbent Assay (ELISA): A more robust, high-throughput platform for detecting total antibodies or specific isotypes (e.g., IgG). ELISA is recommended for sero-epidemiological surveys due to its consistent, high sensitivity over longer periods [104].
Key Consideration: Serological tests for SARS-CoV-2 must be selected and evaluated based on the specific goals of the study (e.g., recent infection vs. long-term immunity), as their performance is not uniform and can be affected by the timing of sample collection and the emergence of viral variants [104].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for executing the experimental protocols described in this application note.
Table 3: Essential Research Reagents for Combined Diagnostic Profiling
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| EDTA Blood Collection Tubes | Prevents coagulation for PCR; preserves nucleic acid integrity for pathogen detection. | Preferred over heparin for Anaplasma PCR [103]. |
| Serum Separator Tubes (SST) | Facilitates clean serum separation for both PCR and serology testing. | Essential for collecting serum samples for convalescent serology [103]. |
| Primers & Probes for msp2 gene | Targets for real-time PCR amplification and detection of A. phagocytophilum DNA. | Core component of a laboratory-developed test (LDT) for Anaplasma [103]. |
| IFA Kit (A. phagocytophilum antigen slides) | Substrate for detecting patient IgG antibodies via immunofluorescence. | A commercial IFA kit is used for the semi-quantitation of antibodies [103]. |
| SARS-CoV-2 RT-PCR Kit | For the reverse transcription and amplification of viral RNA from patient swabs. | Typically includes primers/probes, enzyme mix, and controls [106]. |
| SARS-CoV-2 ELISA Kit | High-throughput quantitation of anti-SARS-CoV-2 antibodies in serum/plasma. | The PLATELIA SARS-CoV-2 total Ab test is an example [104]. |
| CRISPR/Cas13a Reagents | Components for developing highly sensitive, rapid, isothermal nucleic acid detection assays. | Includes LwaCas13a protein, specific crRNA, and reporter probes (e.g., poly-U) [107]. |
| RT-RPA / RPA Kits | Isothermal nucleic acid amplification for use with CRISPR-based detection or rapid PCR alternatives. | Enables amplification without sophisticated thermocyclers, suitable for field use [107]. |
Advanced & Emerging Methodologies
The field of molecular diagnostics is rapidly advancing beyond conventional PCR and ELISA. Integrating these novel technologies can further enhance diagnostic synergy.
- Digital CRISPR/Cas Assays: The combination of CRISPR (e.g., Cas13a, Cas12a) with isothermal pre-amplification and digital droplet partitioning represents a paradigm shift. This approach, as developed for Severe Fever with Thrombocytopenia Syndrome Virus (SFTSV), allows for absolute quantification of viral nucleic acids with exceptional sensitivity and specificity, potentially at the point-of-care [107]. Moving from a two-step to an optimized one-pot reaction system improves stability and repeatability, making it a powerful tool for both clinical and field settings.
- Artificial Intelligence (AI) and Machine Learning (ML): AI and ML are revolutionizing pattern recognition in diagnostics. Convolutional Neural Networks (CNNs) can analyze histopathological slides or radiological images (e.g., chest X-rays) to detect signs of viral infection [108]. Furthermore, ML algorithms can predict outbreak trends by integrating diverse data sources, such as healthcare records and search queries, and can optimize the analysis of complex genomic data to identify emerging viral strains more swiftly than traditional methods [108] [109].
The strategic integration of PCR and serology provides a powerful, synergistic framework for overcoming the inherent limitations of individual diagnostic tests. The protocols and data presented for Anaplasmosis and SARS-CoV-2 demonstrate that a temporally-informed, combined testing algorithm is essential for achieving a comprehensive diagnostic profile, from acute infection through convalescence. This approach is critical not only for accurate patient diagnosis and management but also for robust epidemiological surveillance and advanced research, including therapeutic and vaccine development.
The future of clinical diagnostics lies in the continued refinement of this synergy, incorporating emerging technologies like quantitative CRISPR-based assays and AI-driven analytics to create even more sensitive, rapid, and accessible testing solutions for a wide range of pathogens.
In clinical virology and epidemiological research, accurately estimating the true course of an epidemic is fundamental to public health response. While polymerase chain reaction (PCR) testing provides a real-time snapshot of viral circulation, it does not directly quantify cumulative population exposure. This application note details a methodology for calibrating nucleic acid (PCR) test data with antibody (IgG) seroprevalence to generate refined epidemiological insights, using SARS-CoV-2 as a case study. This calibration is crucial for transforming routine diagnostic data into a reliable assessment of infection dynamics and population immunity, thereby informing both scientific understanding and public health policy.
Background and Significance
PCR testing detects the presence of viral genetic material at a single point in time, indicating current infection. In contrast, the detection of virus-specific IgG antibodies in the blood reflects the immune system's memory of past infections, typically becoming detectable approximately 2-4 weeks after infection and persisting for months to years [110]. The relationship between these two measures is foundational to sero-epidemiology: the IgG-positive fraction at a given time should be proportional to the accumulated PCR-positive incidence from preceding weeks [110]. However, this relationship is confounded by factors including variations in test accuracy, the timing of antibody seroconversion, and the fact that not all PCR-positive individuals progress to full seroconversion [110] [111]. Calibrating PCR data with IgG serology effectively converts a signal of acute viral detection into a measure of cumulative infections, providing a more robust dataset for modeling epidemic trajectories and population immunity.
Experimental Protocol for PCR-IgG Calibration
The following protocol is adapted from a population-level study conducted in Germany, which utilized large-scale datasets from authority-accredited laboratories [110] [112].
Materials and Equipment
Table 1: Key Research Reagent Solutions and Essential Materials
| Item Name | Type/Function | Specific Example/Application |
|---|---|---|
| Nasopharyngeal Swab & UTM | Sample collection for PCR; preserves viral RNA. | Flocked swabs in Universal Transport Media (e.g., Copan Viral Specimen Collection Kit) [113]. |
| RT-PCR Assays | Detects SARS-CoV-2 RNA; the gold standard for active infection. | Assays targeting viral genes (e.g., RdRp, N); performance varies with cycle threshold (Ct) [110]. |
| Serological IgG Assays | Detects SARS-CoV-2 specific IgG antibodies; indicates past infection. | Electrochemiluminescence immunoassay (ECLIA, e.g., Elecsys Anti-SARS-CoV-2) or Chemiluminescent Microparticle Immunoassay (CMIA, e.g., Abbott SARS-CoV-2 IgG) [111] [5]. |
| Automated Nucleic Acid Extractor | Standardizes RNA extraction from patient samples. | EasyMAG instrument (BioMérieux) using the NUCLISENS (Boom) method [113]. |
Step-by-Step Procedure
Data Collection:
- Gather week-resolved, population-level data for the pathogen of interest.
- PCR Data: Collect the weekly count of individuals testing PCR-positive and the total number of PCR tests administered. The output is the weekly PCR-positive fraction (Positive Count / Total Tests) [110].
- IgG Serology Data: Collect the weekly count of individuals testing positive for pathogen-specific IgG antibodies and the total number of IgG tests conducted. The output is the weekly IgG-positive fraction (Positive Count / Total Tests) [110]. Ensure the IgG assays used have known high diagnostic accuracy, as measured by a high Diagnostic Odds Ratio (DOR) [111] [5].
Data Pre-processing:
- Align the PCR and IgG datasets by calendar week.
- Calculate the cumulative sum of the PCR-positive fractions up to each week. This creates a new time series representing the total "signal" of PCR positivity over time.
Model Fitting (Calibration):
- The core of the calibration involves fitting the cumulative PCR data to the observed IgG data using a phenomenological model.
- The model is defined by the equation:
IgG_estimated(t) = α * Cumulative_PCR(t - δ)where:IgG_estimated(t)is the model's estimate of the IgG-positive fraction at timet.αis the scaling parameter to be fitted. This parameter represents the proportion of PCR-positive individuals who subsequently seroconvert to IgG-positive.Cumulative_PCR(t - δ)is the cumulative sum of PCR-positive fractions up to timet - δ.δis the time-shift parameter to be fitted, accounting for the delay between a positive PCR test and the development of detectable IgG antibodies [110] [112].
- Use a non-linear least-squares fitting algorithm to find the values of
αandδthat minimize the difference between theIgG_estimated(t)time series and the empirically observedIgG_positive(t)time series.
Validation and Extrapolation:
- Validate the fitted model by comparing its estimates with independent sources of seroprevalence data, if available (e.g., national serosurveys) [110] [112].
- The fitted model, specifically the parameter
α, can be used to estimate the true number of infected individuals in the population from the raw PCR-positive counts. For instance, a finding thatα = 0.14implies that for every 100 PCR-positive tests, only 14 individuals became infected and seroconverted, suggesting a large number of non-infectious or transient detections [110].
Key Data and Findings
The application of this protocol to SARS-CoV-2 data from Germany yielded critical quantitative insights into the pandemic's trajectory.
Table 2: Key Quantitative Findings from PCR-IgG Calibration Study
| Parameter | Finding | Epidemiological Interpretation |
|---|---|---|
| Scaling Parameter (α) | 0.14 (14%) | Only 14% of individuals with a positive PCR test were estimated to have developed a full infection leading to IgG seroconversion [110] [112]. |
| Infected Population (Est.) | ~25% by end of 2020 | Based on the model, a quarter of the German population was estimated to have been infected by the end of 2020, far exceeding official case counts [110]. |
| IgG Seroprevalence | ~92% by end of 2021 | The model's extrapolation aligned with an independent national serosurvey, validating its long-term predictive power [110] [112]. |
| PCR to Infection Ratio | 1:10 | A literature-based parameter used for cross-validation, meaning one positive PCR test corresponded to approximately 10 actual infections in the population [110]. |
Table 3: Diagnostic Accuracy of Select Serological Assays (Meta-Analysis) [111] [5]
| Serological Assay | Target | Method | Pooled Diagnostic Odds Ratio (DOR) |
|---|---|---|---|
| Elecsys Anti-SARS-CoV-2 | Total Antibody | ECLIA | 1701.56 |
| Elecsys Anti-SARS-CoV-2 N | IgG (Nucleocapsid) | ECLIA | 1022.34 |
| Abbott SARS-CoV-2 IgG | IgG | CMIA | 542.81 |
| LIAISON SARS-CoV-2 S1/S2 IgG | IgG (S1/S2) | CLIA | 178.73 |
| Euroimmun Anti-SARS-CoV-2 S1-IgG | IgG (Spike) | ELISA | 190.45 |
Conceptual and Experimental Workflows
The following diagrams illustrate the logical relationship between diagnostic data and the experimental workflow for calibration.
Diagram 1: Logical framework for calibrating PCR and IgG data. The core process involves transforming the cumulative PCR signal and fitting it to observed IgG data to derive the calibration parameters α and δ.
Diagram 2: End-to-end experimental workflow for the PCR-IgG calibration protocol, from sample collection to model validation.
Discussion
The calibration protocol demonstrates that a significant discrepancy can exist between the number of positive PCR tests and the number of true infections leading to seroconversion. The finding that only 14% of PCR-positive individuals in Germany developed IgG antibodies underscores the limitations of relying solely on PCR data for epidemiological inference [110]. Factors contributing to this discrepancy may include the detection of non-infectious viral fragments, especially at high cycle thresholds (Ct), and the robust ability of the mucosal immune system (e.g., via IgA) to clear the virus before a systemic IgG response is mounted [110].
This methodology provides a powerful tool for reconstructing the true infection time course and for assessing population immunity, which is vital for planning public health interventions. The principles outlined here for SARS-CoV-2 are readily applicable to the study of other infectious diseases, enabling researchers to extract deeper insights from routine diagnostic data.
High-Throughput Sequencing (HTS), commonly referred to as Next-Generation Sequencing (NGS), represents a paradigm shift in clinical virology diagnostics. Unlike traditional methods like PCR and serology that require prior knowledge of the target pathogen, NGS enables comprehensive, unbiased detection of known and novel viruses through massively parallel sequencing of nucleic acids in clinical samples [114]. This capability is particularly valuable for investigating unexplained infections, characterizing emerging viral threats, and detecting mixed viral infections that conventional methods might miss.
The technology's impact is amplified by its rapidly declining cost and increasing speed; where the first human genome required 13 years and nearly $3 billion to complete, a full genome can now be sequenced in hours for under $1,000 [114]. This transformative potential positions NGS not merely as a complementary tool but as a future gold standard in viral diagnostics, capable of integrating genomic information directly into clinical decision-making and therapeutic development.
Comparative Diagnostic Performance: NGS Versus Conventional Techniques
Detection Sensitivity and Pathogen Identification
Multiple clinical studies demonstrate the superior detection capabilities of NGS-based approaches compared to Conventional Microbiological Tests (CMTs), which include culture, microscopy, and targeted PCR.
Table 1: Comparative Performance of NGS vs. Conventional Methods in Pulmonary Infections
| Parameter | Targeted NGS (tNGS) | Conventional Microbiological Tests (CMTs) | Statistical Significance |
|---|---|---|---|
| Positive Detection Rate | 99.5% (204/205 specimens) | 35.6% (73/205 specimens) | P < 0.0001 [115] |
| Number of Pathogens Identified | 56 putative pathogens | 20 pathogens | Significantly higher [115] |
| Polybial Detection | Proportion of ≥2 species significantly higher | Lower proportion of polybial infections | χ² = 337.283, P < 0.001 [116] |
| Overall Positivity Rate | 92.6% | 25.2% | χ² = 378.272, P < 0.001 [116] |
A separate study on spinal infections further highlighted methodological differences, showing that tissue-based NGS (90.48% positive rate) significantly outperformed blood-based NGS (42.86% positive rate), underscoring the importance of appropriate sample selection in viral diagnostics [117].
Analytical Sensitivity in Controlled Environments
In vaccine safety testing, a multi-laboratory study evaluated the sensitivity of short-read HTS for detecting adventitious viruses spiked into a high-titer adenovirus background. All seven participating laboratories consistently detected five distinct viruses (Epstein-Barr virus, feline leukemia virus, respiratory syncytial virus, mammalian orthoreovirus type 1, and porcine circovirus type 1) at concentrations of 10^4 genome copies/mL using both targeted and non-targeted bioinformatic analyses [118]. Some laboratories achieved even greater sensitivity, detecting certain viruses at concentrations as low as 10^2 genome copies/mL, demonstrating the method's robustness for ensuring biological product safety [118].
Experimental Protocols for Viral Detection Using NGS
Targeted NGS (tNGS) for Pulmonary Pathogen Detection
Protocol Application: This protocol is adapted from a clinical study on pulmonary infections using bronchoalveolar lavage fluid (BALF) specimens [115].
Sample Preparation:
- Sample Collection: Collect BALF via bronchoscopy from the target lung segment using sterile saline injection (60-120 mL total) with a minimum 40% recovery rate.
- Sample Processing: Transfer viscous sample precipitates to a grinding tube. Add lysis buffer and disrupt using a shock crusher.
- Nucleic Acid Extraction: Perform automated nucleic acid extraction using a magnetic bead-based pathogen DNA/RNA kit on an automated extraction instrument.
Library Preparation and Sequencing:
- cDNA Synthesis and Library Prep: Use a respiratory multi-pathogen targeted sequencing kit. Synthesize cDNA followed by target region PCR amplification.
- Library Purification: Purify PCR products using magnetic beads and amplify libraries for sequencing.
- Quality Control: Assess DNA library concentration using a fluorometer. Require Q30 ≥ 75%, minimum raw reads ≥ 50k, and internal reference gene amplification reads ≥ 200.
- Sequencing: Perform sequencing on a desktop sequencer using appropriate sequencing kits.
Bioinformatic Analysis:
- Quality Filtering: Process raw data using the fastp program for basic quality control and filtering.
- Pathogen Identification: Map filtered reads against a tNGS-specific database containing 198 pathogens and 15 drug resistance genes using alignment software.
- Result Interpretation: Classify microorganisms as pathogenic, conditionally pathogenic, or colonizing based on pathogenicity within specific sample types, requiring comprehensive clinical assessment for final determination.
Figure 1: Targeted NGS (tNGS) workflow for pathogen detection in bronchoalveolar lavage fluid, demonstrating the integrated process from sample collection to clinical interpretation [115].
Metagenomic NGS (mNGS) for Comprehensive Virus Detection
Protocol Application: This protocol is adapted from studies on spinal infection diagnostics and virus spiking studies for vaccine safety [117] [118].
Sample Processing:
- Sample Collection: Obtain tissue through percutaneous needle biopsy or surgical debridement, or blood samples collected in appropriate containers.
- DNA Extraction: Extract DNA using a commercial micro DNA kit. Precisely quantify extracted DNA using a fluorometer to ensure sufficient input material.
Library Preparation:
- DNA Fragmentation: Fragment DNA to appropriate sizes for sequencing platform.
- End Repair and Adapter Ligation: Repair fragment ends and ligate sequencing adapters.
- Library Amplification: Amplify adapter-ligated fragments using PCR.
- Quality Assessment: Validate library quality and quantity prior to sequencing.
Sequencing and Analysis:
- Sequencing: Convert libraries into DNA nanoballs and load onto a high-throughput sequencing platform.
- Host Sequence Removal: Align sequencing reads to human reference genome (hg19) and remove matching sequences.
- Microbial Identification: Classify non-host reads by alignment to comprehensive microbial genome databases.
- Variant Calling and Reporting: Identify pathogenic variants and generate clinical reports.
Key Application Areas in Clinical Virology and Drug Development
Pathogen Identification and Resistance Prediction
In pulmonary infections, tNGS demonstrates significant clinical utility by identifying putative pathogens in 99.5% of BALF specimens compared to 35.6% with CMTs [115]. This enhanced detection directly impacts treatment decisions, with tNGS results guiding therapy adjustments in 17.2% (35/203) of patients [115]. Furthermore, tNGS shows potential for predicting drug resistance through detection of resistance genes, demonstrating 40% concordance with phenotypic drug sensitivity for carbapenem-resistant organisms and 80% for methicillin-resistant Staphylococcus aureus [115]. However, inconsistencies between resistance genotypes and phenotypes highlight the need for further refinement before standalone clinical implementation [116].
Vaccine Safety and Adventitious Virus Detection
NGS plays a critical role in biologics manufacturing by detecting adventitious viruses in vaccine products. The technology's sensitivity enables identification of viral contaminants in high-titer virus preparations, ensuring product safety [118]. This application is particularly valuable since NGS can detect novel or unexpected viruses that conventional methods might miss, addressing a key limitation in current safety testing paradigms.
Outbreak Investigation and Transmission Tracking
The ability of NGS to generate whole viral genome sequences enables precise tracking of transmission chains and identification of outbreak sources. Real-time genomics facilitates infection control measures by providing high-resolution data on pathogen evolution and spread [119]. Phylogenetic analysis of viral sequences can identify transmission patterns and inform intervention strategies, making NGS invaluable for public health responses to viral outbreaks [119].
Essential Research Reagent Solutions for NGS in Virology
Table 2: Key Research Reagent Solutions for NGS-Based Viral Detection
| Reagent Category | Specific Examples | Function in Workflow |
|---|---|---|
| Nucleic Acid Extraction Kits | Magnetic Pathogen DNA/RNA Kit [115], TIANamp Micro DNA Kit [117] | Automated extraction of high-quality nucleic acids from clinical samples |
| Target Enrichment Solutions | Respiratory multi-pathogen targeted sequencing kit [115], Hybridization capture kits [120] | Enrichment of viral sequences through probe-based or PCR-based methods |
| Library Preparation Kits | Commercial library prep kits compatible with Illumina, BGI, or other platforms [117] | Fragment end repair, adapter ligation, and library amplification for sequencing |
| Sequencing Reagents | Platform-specific sequencing kits (e.g., BGISEQ, Illumina) [117] | Provide enzymes, buffers, and nucleotides for the sequencing reaction |
| Bioinformatic Tools | Bowtie 2 [115], BWA [117], fastp [115], Reference Viral Databases (RVDB) [118] | Quality control, sequence alignment, variant calling, and phylogenetic analysis |
Integrated Workflow for Viral Diagnostics Using NGS
Figure 2: Decision workflow for selecting appropriate NGS methodology in clinical virology, showing pathways for both metagenomic and targeted approaches based on clinical presentation [115] [117] [120].
While NGS demonstrates clear advantages over traditional diagnostic methods, several challenges remain before it can become the gold standard in clinical virology. The technology requires specialized instrumentation, bioinformatics expertise, and standardized protocols for consistent implementation across clinical laboratories [119] [120]. Additionally, the interpretation of complex genomic data and integration with clinical findings necessitates multidisciplinary collaboration between virologists, clinicians, and bioinformaticians.
Future development should focus on automating workflows, standardizing bioinformatic pipelines, and establishing robust quality control metrics to ensure reproducible results across laboratories. As sequencing costs continue to decline and analytical methods improve, NGS is poised to become an increasingly accessible and indispensable tool for viral diagnosis, outbreak investigation, and therapeutic development, ultimately fulfilling its potential as the new gold standard in clinical virology.
Conclusion
The landscape of clinical virology diagnostics is firmly anchored by the complementary strengths of PCR and serology. PCR remains the cornerstone for acute-phase detection and quantification of active infection, while serology is indispensable for understanding immune response, past exposure, and population-level immunity. Future directions point toward greater integration of these modalities, increased automation, and the rise of high-throughput sequencing, which promises unprecedented breadth in pathogen identification. For researchers and drug developers, these evolving technologies are critical for accelerating therapeutic discovery, conducting robust clinical trials, and implementing effective public health interventions. The continuous refinement of diagnostic accuracy, speed, and accessibility will be paramount in addressing both existing and emerging viral threats.
References
- 1. Optimization of primer sets and detection protocols for ... [https://www.nature.com/articles/s12276-020-0452-7]
- 2. A comprehensive review of methodological and ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975025002058]
- 3. Clinical Virology | Laboratory Medicine [https://medicine.yale.edu/labmed/clinical-service/virology/]
- 4. Standard PCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/pcr/standard-pcr?srsltid=AfmBOoq6s9lJ0ej9QQw-OkomCWluDSaBarXaChBTaHaOmHR2QnehMQw3]
- 5. An Indirect Comparison of Diagnostic Accuracy for Seven ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418076/]
- 6. Digital PCR outperforms quantitative real-time PCR for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288185/]
- 7. Protocol to Mine Unknown Flanking DNA Using PER-PCR ... [https://en.bio-protocol.org/en/bpdetail?id=5188&type=0]
- 8. Predicting sequence-specific amplification efficiency in ... [https://www.nature.com/articles/s41467-025-64221-4]
- 9. Molecular point-of-care testing technologies: Current status ... [https://www.sciencedirect.com/science/article/pii/S2950160125000063]
- 10. Serology as a Tool to Assess Infectious Disease Landscapes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9323579/]
- 11. Immunological Detection and Characterization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122539/]
- 12. Antibody basics guide [https://www.abcam.com/en-us/technical-resources/guides/antibody-basics/antibody-basics]
- 13. Serological testing for SARS‐CoV‐2 antibodies in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9303219/]
- 14. Comparative Performance of Serological (IgM/IgG) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9966400/]
- 15. The comparative superiority of IgM-IgG antibody test to real ... [https://www.medrxiv.org/content/10.1101/2020.03.28.20045765v1]
- 16. The difference between IgM and IgG antibody prevalence ... [https://www.sciencedirect.com/science/article/pii/S1567576920338285]
- 17. Post-recovery viral shedding shapes wastewater-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098667/]
- 18. Seroconversion [https://en.wikipedia.org/wiki/Seroconversion]
- 19. What is Seroconversion? [https://www.news-medical.net/health/What-is-Seroconversion.aspx]
- 20. Seroconversion | Research Starters [https://www.ebsco.com/research-starters/health-and-medicine/seroconversion]
- 21. Rapid, season-specific PCR testing versus traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318422/]
- 22. High sensitivity of HIV antibody screening tests may lead to ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1562946/full]
- 23. Direct vs. Indirect Testing: How to Catch a Stealth Infection [https://www.restorativemedcenter.com/blogs/direct-vs-indirect-testing-for-infections-cracking-the-case-of-the-missing-microbes]
- 24. Direct vs. Indirect Testing for Tick-Borne Diseases [https://igenex.com/tick-talk/direct-vs-indirect-testing-for-tick-borne-diseases/]
- 25. Polymerase Chain Reaction (PCR) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK589663/]
- 26. Surpassing the natural limits of serological diagnostic tests [https://www.sciencedirect.com/science/article/pii/S2949928324000476]
- 27. Evaluation of real-time PCR with serology for diagnosis ... [https://www.sciencedirect.com/science/article/pii/S2213398422001269]
- 28. Trend in serological and molecular diagnostic methods for ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-024-02055-4]
- 29. Novel Host Response-Based Diagnostics to Differentiate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000761/]
- 30. Volume 31, Supplement—April 2025 - Emerging Infectious ... [https://wwwnc.cdc.gov/eid/articles/issue/31/13/table-of-contents]
- 31. Optimized high-throughput whole-genome sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465963/]
- 32. Direct PCR for Rapid and Safe Pathogen Detection [https://www.mdpi.com/2813-9038/2/3/12]
- 33. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 34. Digital PCR Breaks Into the Mainstream in 2025 - Vocal Media [https://vocal.media/feast/digital-pcr-breaks-into-the-mainstream-in-2025]
- 35. The potential application of digital PCR in detecting ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093425000448]
- 36. Artificial intelligence and machine learning in infectious ... [https://www.sciencedirect.com/science/article/pii/S0026265X25031509]
- 37. Towards practical point-of-care quick, ubiquitous ... [https://www.nature.com/articles/s41378-025-01057-4]
- 38. Serological Techniques (Chapter 50) - Clinical and ... [https://www.cambridge.org/core/books/clinical-and-diagnostic-virology/serological-techniques/8263E52AF31DE4B3E9629CE2161E1F74/core-reader]
- 39. The future of diagnostic virology - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7162382/]
- 40. Seroprevalence of COVID-19 neutralizing antibodies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12573950/]
- 41. Interim Estimates of 2024–2025 COVID-19 Vaccine ... [https://www.cdc.gov/mmwr/volumes/74/wr/mm7406a1.htm]
- 42. New 2025 data shows COVID-19 vaccines provide ... [https://sph.unc.edu/sph-news/new-2025-data-shows-covid-19-vaccines-provide-effective-durable-protection/]
- 43. Molecular Diagnostics in the Post-COVID-19 Era [https://irispublishers.com/ajmi/fulltext/molecular-diagnostics-in-the-post-covid-19.ID.000513.php]
- 44. Virology review 2025 - Margie Morgan, PhD | PPTX [https://www.slideshare.net/slideshow/virology-review-2025-margie-morgan-phd/276984185]
- 45. Syndromic Testing—The Evaluation of Four Novel ... [https://www.mdpi.com/2075-4418/15/10/1228]
- 46. Advancing quantitative PCR with color cycle multiplex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11417387/]
- 47. Comparative Evaluation of a multiplex PCR panel for high ... [https://www.sciencedirect.com/science/article/pii/S1201971225003698]
- 48. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 49. Multiplex vs. Singleplex qPCR: What Do I Need To Know? [https://www.thermofisher.com/blog/behindthebench/multiplex-vs-singleplex-qpcr-what-do-i-need-to-know/]
- 50. Comparison of Multiplex PCR Hybridization-based and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5224703/]
- 51. Diagnostic Techniques: Serological and Molecular Approaches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7157465/]
- 52. Types Of Immunoassay - And When To Use Them [https://www.quanterix.com/immunoassay-technologies-past-present-and-future/]
- 53. Point-of-Care Testing - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK592387/]
- 54. Why point-of-care testing is vital to medical diagnostics [https://diagnostics.roche.com/us/en/article-listing/why-point-of-care-testing-is-vital-to-medical-diagnostics.html]
- 55. Integrated immunoassay solutions [https://lifesciences.tecan.com/integrated-immunoassay-solutions]
- 56. New Immunoassay Tools: From Samples to Results Faster [https://www.criver.com/eureka/new-immunoassay-tools-samples-results-faster]
- 57. Comparison of different immunoassays for the detection ... [https://www.sciencedirect.com/science/article/pii/S0022175920301617]
- 58. Comparative Analysis of a Rapid Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388426/]
- 59. Next-Generation Nucleic Acid-Based Diagnostics for Viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388196/]
- 60. qPCR in Early Cancer Detection: Why It Still Leads the Pack [https://www.meridianbioscience.com/lifescience-blog/why-qpcr-still-leads-in-oncology/]
- 61. 2025: The future of cancer diagnostics in the pathology lab [https://diagnostics.roche.com/us/en/article-listing/2025-the-future-of-cancer-diagnostics-in-the-pathology-lab.html]
- 62. Advances in Diagnostics, Immunotherapy, Precision ... [https://www.asco.org/about-asco/press-center/news-releases/advances-diagnostics-immunotherapy-precision-medicine-2025-asco-annual-meeting-press-program]
- 63. Molecular Diagnostics In Pharmacogenomics Market [https://www.futuremarketinsights.com/reports/molecular-diagnostics-in-pharmacogenomics-market]
- 64. Protocol for detection of Oropouche viruses from human ... [https://www.sciencedirect.com/science/article/pii/S2666166725002114]
- 65. Next Generation Diagnostics for Rapid Detection of Viruses ... [https://www.longdom.org/open-access/next-generation-diagnostics-for-rapid-detection-of-viruses-and-fungi-1102913.html]
- 66. Multiplex PCR: Optimization and Application in Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC88949/]
- 67. PCR Optimization: Strategies To Minimize Primer Dimer [https://genemod.net/blog/pcr-optimization]
- 68. Troubleshooting primer dimer in PCR [https://www.minipcr.com/primer-dimer-pcr/]
- 69. Eliminating primer dimers and improving SNP detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7200914/]
- 70. Polymerase Chain Reaction: Basic Protocol Plus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846334/]
- 71. PCR Basic Troubleshooting Guide [https://www.creative-biogene.com/blog/pcr-basic-troubleshooting-guide]
- 72. Optimization and application of multiplex PCR [https://bio-protocol.org/exchange/minidetail?id=4871670&type=30]
- 73. Reducing amplification artifacts in high multiplex amplicon ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-015-1806-8]
- 74. Molecular Diagnostic (PCR) Testing [https://depts.washington.edu/uwviro/clinical-testing/]
- 75. Clinical Applications of Quantitative Real-Time PCR in Virology [https://pmc.ncbi.nlm.nih.gov/articles/PMC7148891/]
- 76. PCR Methods - Top Ten Strategies [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-methods.html]
- 77. Guidelines for Polymerase Chain Reaction (PCR) [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/introduction/guidelines-for-pcr]
- 78. How is Hot-Start Technology Beneficial For Your PCR [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/hot-start-technology-benefits-PCR.html]
- 79. Direct DNA Amplification from Crude Clinical Samples ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2871721/]
- 80. Real-time PCR in virology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC101343/]
- 81. Humoral Responses and Serological Assays in SARS-CoV ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.610688/full]
- 82. Redefining serological diagnostics with immunoaffinity ... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-023-09431-y]
- 83. Multi-center nationwide comparison of seven serology ... [https://www.sciencedirect.com/science/article/pii/S2589537020303953]
- 84. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 85. The Main Molecular and Serological Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7823618/]
- 86. Urine PCR testing as an effective method for early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584711/]
- 87. Recent Advances in the Evaluation of Serological Assays ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2020.620222/full]
- 88. Immunoassay Methods - Assay Guidance Manual - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92434/]
- 89. Understanding and using sensitivity, specificity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2636062/]
- 90. Sensitivity and Specificity Fundamentals [https://www.beckmancoulter.com/en/blog/diagnostics/sensitivity-and-specificity-fundamentals]
- 91. Test performance evaluation of SARS-CoV-2 serological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7740072/]
- 92. Evaluation of SARS-CoV-2 serology assays reveals a ... [https://www.nature.com/articles/s41587-020-0659-0]
- 93. Molecular and diagnostic clinical virology in real time - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7129573/]
- 94. Performance evaluation of serological assays to determine ... [https://www.sciencedirect.com/science/article/pii/S1386653220303310]
- 95. Applications of laboratory findings in the prevention ... [https://www.nature.com/articles/s41392-021-00731-z]
- 96. IDSA Guidelines on the Diagnosis of COVID-19: Serologic ... [https://www.idsociety.org/practice-guideline/covid-19-guideline-serology/]
- 97. Assessing the performance of commercial serological tests ... [https://www.sciencedirect.com/science/article/pii/S2772707624000547]
- 98. Multicenter Clinical Comparison of the 10 Minute AMDI™ ... [https://www.medrxiv.org/content/10.1101/2025.11.04.25339522v1.full]
- 99. Comparing the precision of two digital PCR applications for ... [https://www.nature.com/articles/s41598-025-13143-8]
- 100. Analytic comparison between three high-throughput ... [https://www.nature.com/articles/s41598-021-91235-x]
- 101. Comparison of six COVID-19 serology assays for detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12282051/]
- 102. Comparison of PCR and Serology Assays for Early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC262519/]
- 103. Anaplasma – PCR and Serology | Santé publique Ontario [https://www.publichealthontario.ca/fr/laboratory-services/test-information-index/anaplasma-pcr-serology]
- 104. Comparative evaluation of SARS-CoV-2 serological tests ... [https://www.sciencedirect.com/science/article/pii/S2667038023000352]
- 105. Human Granulocytic Anaplasmosis as a COVID-19 Mimicker [https://pmc.ncbi.nlm.nih.gov/articles/PMC8765683/]
- 106. Polymerase Chain Reaction Testing: Selected Indications [https://es.aetna.com/cpb/medical/data/600_699/0650.html]
- 107. Development and characterization of a digital CRISPR ... [https://www.sciencedirect.com/science/article/abs/pii/S092540052300504X]
- 108. Transforming clinical virology with AI, machine learning and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10533451/]
- 109. Multidisciplinary approaches to combat emerging viruses [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1387623/full]
- 110. A calibration of nucleic acid (PCR) by antibody (IgG) tests ... [https://www.frontiersin.org/journals/epidemiology/articles/10.3389/fepid.2025.1592629/full]
- 111. An Indirect Comparison of Diagnostic Accuracy for Seven ... [https://pubmed.ncbi.nlm.nih.gov/40923344/]
- 112. A calibration of nucleic acid (PCR) by antibody (IgG) tests ... [https://pubmed.ncbi.nlm.nih.gov/41158834/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1piP1Xotxtp-HYn_RK90yc7u-9qUoAV30MLQwddB9kAlCglEeQ&fc=None&ff=20251029123319&v=2.18.0.post22+67771e2]
- 113. Nasal biomarker testing to rule out viral respiratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216728/]
- 114. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 115. Application of targeted next-generation sequencing for ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1590881/full]
- 116. Comparison of targeted next-generation sequencing and ... [https://www.sciencedirect.com/science/article/pii/S0732889324003596]
- 117. The Comparison of Diagnostic Performance Between Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12432008/]
- 118. Virus detection by short read high throughput sequencing ... [https://www.nature.com/articles/s41541-025-01104-1]
- 119. Genomics and Clinical Virology 2025 — 20250302 [https://coursesandconferences.wellcomeconnectingscience.org/event/genomics-and-clinical-virology-2025-20250302/]
- 120. NGS Approaches in Clinical Diagnostics: From Workflow to ... [https://www.mdpi.com/1422-0067/26/19/9597]