Molecular Mechanisms of Viral Pathogenesis: From Viral Entry to Host Response and Therapeutic Intervention
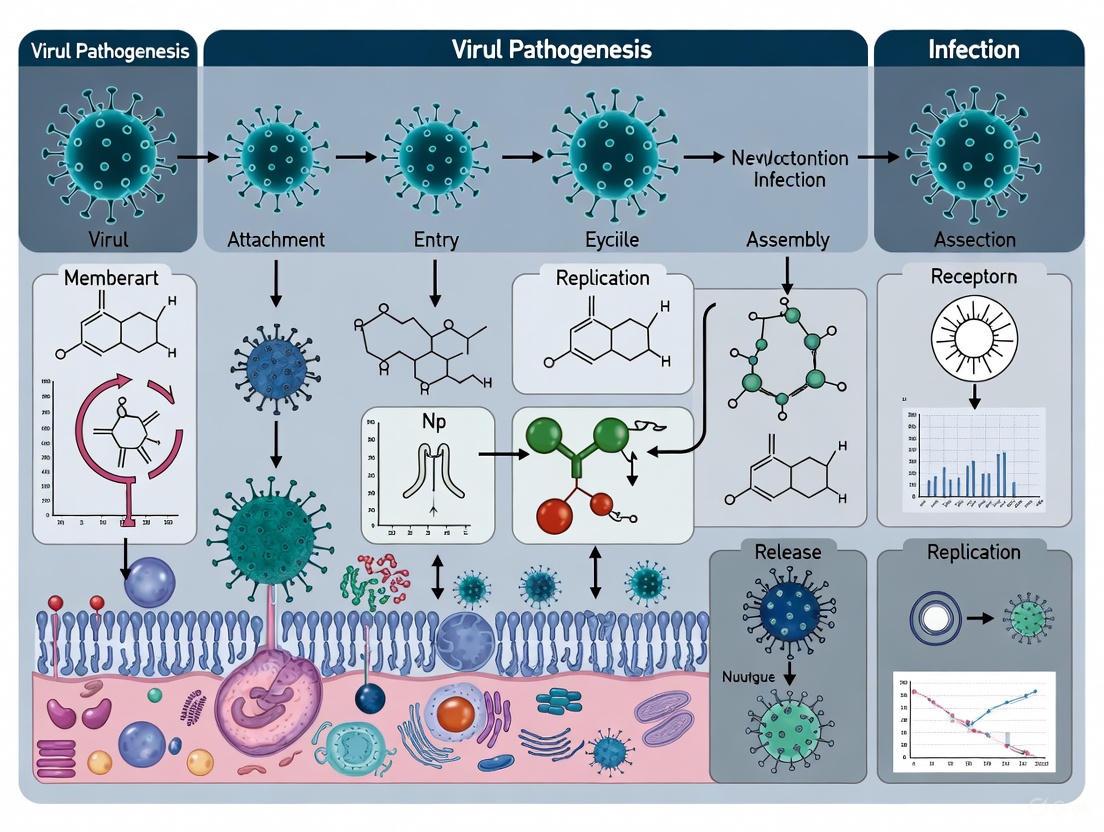
This comprehensive review explores the intricate molecular mechanisms of viral pathogenesis and infection, synthesizing foundational concepts with cutting-edge research and methodological advances.
Molecular Mechanisms of Viral Pathogenesis: From Viral Entry to Host Response and Therapeutic Intervention
Abstract
This comprehensive review explores the intricate molecular mechanisms of viral pathogenesis and infection, synthesizing foundational concepts with cutting-edge research and methodological advances. Tailored for researchers, scientists, and drug development professionals, the article examines viral entry strategies, host-pathogen interactions, immune evasion tactics, and metabolic reprogramming. It critically evaluates contemporary research methodologies, computational approaches, and model systems driving the field forward. The analysis extends to troubleshooting experimental challenges and optimizing therapeutic strategies, while providing validation through comparative analysis of pathogenesis across virus families. By integrating foundational knowledge with translational applications, this review serves as a strategic resource for advancing antiviral drug discovery and novel therapeutic development.
Decoding Viral Invasion: Molecular Entry Portals and Early Host-Pathogen Dynamics
Viral entry into host cells represents the critical first step in infection and a major determinant of pathogenic mechanisms. This process initiates when viral particles attach to specific receptor molecules on the host cell surface, leading to internalization and delivery of the viral genome into the cellular replication machinery [1] [2]. The presence and distribution of these receptor molecules largely dictate viral tropism—the specific tissues and species a virus can infect—making receptor identification fundamental to understanding viral pathogenesis and developing targeted therapeutic interventions [2]. Viruses have evolved to exploit a diverse array of cell surface components as entry receptors, including proteins, carbohydrates, and lipids, with recognition mediated by specialized viral attachment proteins (VAPs) that exhibit precise molecular complementarity to their cognate receptors [3] [1].
The strategic importance of viral entry receptors extends beyond merely anchoring the virus to the cell surface. Receptor binding often triggers essential conformational changes in viral entry proteins that drive subsequent entry steps, including membrane fusion for enveloped viruses or penetration for non-enveloped viruses [4] [1]. Furthermore, some viruses have developed the capacity to utilize multiple receptors either simultaneously or sequentially, engaging initial attachment factors that concentrate virions on the cell surface before transferring to primary entry receptors that mediate internalization [3]. This complex receptor utilization strategy enhances infection efficiency and expands cellular tropism, contributing significantly to the pathogenic potential of many viruses. Consequently, mapping the intricate interplay between viruses and their cellular receptors provides crucial insights into disease mechanisms and reveals vulnerable points in the viral life cycle that can be targeted therapeutically.
Fundamental Principles of Viral Receptor Interactions
Defining Viral Receptors and Attachment Factors
A precise distinction exists between viral attachment factors and true entry receptors, though both participate in the initial stages of cell recognition. Attachment factors are cell surface molecules that promote virus binding but do not directly mediate genome internalization; they function primarily to concentrate virions on the cell surface, thereby facilitating subsequent interactions with bona fide entry receptors [3] [1]. In contrast, entry receptors not only bind viruses with high specificity but also actively promote downstream entry processes such as internalization or conformational activation of viral fusion machinery [3]. For instance, while heparan sulfate proteoglycans often serve as attachment factors for various viruses, proteins like ACE2 for SARS-CoV-2 and CD4 for HIV-1 function as genuine entry receptors by triggering essential structural rearrangements required for membrane fusion and genome delivery [5] [1].
The molecular interactions between viruses and their receptors exhibit several conserved features that optimize infection efficiency. First, viral attachment proteins (VAPs) typically engage receptors through moderate-affinity interactions (0.1–1 μM range for monomeric binding) that, when multiplied across multiple binding sites on a single virion, result in extremely high overall avidity [1]. Second, receptor binding sites on viruses frequently reside within depressed surface regions or "canyons" that may help shield critical interaction motifs from host immune surveillance while still permitting access to receptor molecules [4] [1]. Third, many viruses exploit receptors that perform essential physiological functions and are therefore constitutively expressed on susceptible cell types, ensuring consistent availability for viral exploitation [6]. These strategic interaction principles enable viruses to maintain a delicate balance between entry efficiency and evasion of host defenses.
Structural Basis of Receptor Recognition
Structural studies have revealed remarkable diversity in how viral proteins recognize and bind to their cellular receptors. The spike proteins of coronaviruses, for instance, contain two distinct domains within their S1 subunit—the N-terminal domain (S1-NTD) and C-terminal domain (S1-CTD)—either or both of which can function as receptor-binding domains (RBDs) [6]. This structural arrangement allows different coronaviruses to recognize varied receptors despite sharing overall architectural similarities. For example, while SARS-CoV and HCoV-NL63 both utilize the S1-CTD to bind ACE2, they belong to different genera (β and α, respectively), whereas MERS-CoV, also a β-coronavirus, uses its S1-CTD to bind an entirely different receptor, DPP4 [6].
The receptor recognition process often involves dramatic conformational transitions in viral proteins that are triggered by specific cellular cues. The SARS-CoV-2 spike protein exists in dynamic equilibrium between "closed" and "open" states, with the open state exposing the receptor-binding motif for ACE2 interaction [7]. Notably, emerging variants of concern like Omicron show a shifted equilibrium toward the open conformation, enhancing receptor accessibility and contributing to increased transmissibility [7]. Similarly, enveloped viruses such as influenza and HIV possess fusion glycoproteins that undergo extensive structural rearrangements from metastable pre-fusion states to stable post-fusion configurations, a process typically initiated by receptor binding and/or subsequent environmental triggers like low pH [4] [7]. These structural insights not only elucidate fundamental entry mechanisms but also inform the design of inhibitors targeting specific conformational states.
Table 1: Classification of Major Viral Entry Receptors with Representative Examples
| Receptor Type | Molecular Characteristics | Representative Viruses | Cellular Function of Receptor |
|---|---|---|---|
| IgSF Proteins | Immunoglobulin-like domains | Poliovirus, Rhinovirus, Coxsackievirus | Cell adhesion (ICAM-1, CAR) |
| Enzymes | Metalloproteases, exoproteases | SARS-CoV-2 (ACE2), MERS-CoV (DPP4), HCoV-229E (APN) | Peptide hormone processing, blood pressure regulation |
| Carbohydrates | Sialic acid derivatives | Influenza virus, Coronavirus OC43, Coronavirus HKU1 | Cell surface glycosylation patterns |
| Lipids | Cholesterol, phospholipids | SV40, Rotavirus | Membrane structure components |
| Integrins | Heterodimeric adhesion receptors | Foot-and-mouth disease virus, Echovirus 1 | Cell-matrix adhesion, signaling |
Methodologies for Receptor Identification and Validation
Genetic and Proteomic Approaches
Modern receptor identification relies heavily on genetic screening methods that systematically evaluate gene function across the cellular genome. CRISPR-Cas9 gene editing has emerged as a particularly powerful tool for this purpose, enabling researchers to generate comprehensive knockout libraries where individual genes are inactivated across cell populations [8]. When subjected to viral challenge, cells lacking essential entry receptors survive while susceptible cells perish, allowing subsequent sequencing to identify the protective genetic modifications. This approach was successfully employed to identify the low-density lipoprotein receptor (LDLR) family members LRP1, LRP4, and VLDLR as entry receptors for yellow fever virus, and LRP8 for tick-borne encephalitis virus [8]. The experimental protocol typically involves: (1) generating a CRISPR knockout library in susceptible target cells; (2) infecting cells with the virus of interest at appropriate multiplicity of infection; (3) recovering surviving cells after sufficient time for virus-induced cytopathy; (4) amplifying and sequencing the guide RNAs from surviving cells; and (5) validating candidate genes through individual knockout studies.
Complementing genetic approaches, quantitative proteomics enables systematic mapping of protein-protein interactions during viral entry [3]. Advanced mass spectrometry techniques now allow sensitive detection and quantitation of proteins from limited biological material, making it possible to identify virus-associated host proteins with high confidence. A typical workflow involves: (1) incubating viral particles or viral envelope proteins with cell lysates or membrane preparations; (2) capturing virus-host protein complexes using antibodies against viral proteins; (3) digesting captured proteins into peptides and analyzing by high-resolution mass spectrometry; (4) comparing protein abundances between experimental and control samples to identify specifically bound host proteins; and (5) constructing interaction networks to distinguish primary receptors from secondary binding partners [3]. This approach proved valuable in identifying the complex network of proteins that mediate hepatitis C virus entry, including CD81, SR-BI, claudin-1, and occludin [3].
Functional Validation Strategies
Candidate receptors identified through genetic or proteomic screens require rigorous functional validation to establish their necessity and sufficiency for viral entry. The gold standard validation protocol involves a series of complementary experiments that collectively demonstrate receptor function [8] [1]. First, gene knockout or knockdown experiments determine whether removing the candidate receptor from previously susceptible cells confers resistance to infection. This can be achieved through CRISPR-Cas9-mediated gene disruption, RNA interference, or antibody blockade [8]. Second, heterologous expression studies test whether introducing the candidate receptor into non-susceptible cells renders them permissive to infection, effectively converting them into targets for viral entry [8] [6]. For the yellow fever virus receptors, researchers demonstrated that genetically eliminating LDLR family members from cell surfaces blocked infection, while adding abnormally high numbers of these receptors allowed increased viral entry [8].
Additional validation steps include assessing the direct binding between viral attachment proteins and candidate receptors using techniques like surface plasmon resonance, isothermal titration calorimetry, or co-immunoprecipitation [6] [1]. Furthermore, structural studies of virus-receptor complexes provide the highest resolution evidence for specific molecular interactions, as exemplified by crystal structures of coronavirus spike protein domains complexed with their cognate receptors ACE2, DPP4, or APN [6]. These structural insights not only confirm receptor identity but also reveal the atomic details of binding interfaces, informing the design of targeted entry inhibitors. Together, this multi-faceted validation framework ensures that identified molecules genuinely function as entry receptors rather than merely participating in downstream post-entry processes.
Diagram 1: Comprehensive workflow for viral receptor identification and validation, progressing from initial screening through functional validation to mechanistic characterization.
Diverse Viral Entry Pathways and Mechanisms
Endocytic Mechanisms of Viral Entry
Viruses exploit multiple cellular endocytic pathways to gain entry into host cells, with the specific route determined by virus size, structure, and receptor interactions. Clathrin-mediated endocytosis represents the most well-characterized entry pathway, utilized by both enveloped viruses like influenza and non-enveloped viruses like adenovirus [4] [7]. This process initiates when virus binding to surface receptors triggers recruitment of clathrin proteins to the intracellular membrane face, forming characteristic coated pits that invaginate and pinch off to form virus-containing endosomes [7]. As these endosomal vesicles undergo maturation, they experience a progressive decrease in internal pH, which serves as a critical trigger for conformational changes in viral proteins that facilitate membrane penetration or fusion [4]. The experimental protocol for studying clathrin-dependent entry typically involves: (1) treating cells with pharmacological inhibitors of clathrin function such as chlorpromazine or pitstop; (2) knocking down essential clathrin pathway components using siRNA; (3) visualizing virus co-localization with clathrin light chain using fluorescence microscopy; and (4) monitoring infection kinetics when endosomal acidification is blocked using agents like bafilomycin A1 or ammonium chloride.
Alternative entry pathways provide viruses with additional options for cell invasion. Caveolar entry is preferentially used by certain non-enveloped viruses like SV40 and involves cholesterol-rich membrane microdomains that form distinctive flask-shaped invaginations [4] [7]. Unlike clathrin-mediated endocytosis, caveolar entry maintains a neutral pH environment throughout internalization, delivering viruses to specialized organelles called caveosomes rather than acidic endosomes [7]. Macropinocytosis represents a third major entry mechanism, employed by viruses such as vaccinia virus and Ebola virus, involving actin-mediated ruffling of the plasma membrane that engulfs virions in large fluid-filled vesicles [7]. This pathway is typically studied using inhibitors of actin polymerization (cytochalasin D), Na+/H+ exchangers (EIPA), or Rac1 signaling. The diversity of entry pathways highlights viral adaptability, with some viruses like SARS-CoV-2 capable of utilizing multiple routes—either direct fusion at the plasma membrane when TMPRSS2 is present or endosomal entry via cathepsin L activation when TMPRSS2 is limited [7].
Membrane Fusion and Penetration Strategies
Following cellular internalization, viruses must breach intracellular membranes to release their genetic material into the replication-competent compartments of the cell. Enveloped viruses accomplish this through membrane fusion, a process mediated by specialized viral fusion proteins that undergo dramatic conformational changes to merge the viral envelope with cellular membranes [4] [7]. These fusion proteins exist in metastable pre-fusion configurations that, when triggered by receptor binding or low pH, refold into extremely stable post-fusion states, releasing substantial free energy that drives membrane merger [7]. Class I fusion proteins (e.g., influenza HA, HIV Env) typically feature central α-helical coiled-coils that thrust the fusion peptide toward the target membrane, while class II fusion proteins (e.g., flavivirus E, alphavirus E1) rearrange from dimeric to trimeric states with fusion loops positioned for membrane insertion [4]. The experimental analysis of viral fusion typically employs: (1) liposome-based fusion assays with fluorescence dequenching; (2) cell-cell fusion assays measuring reporter gene activation; (3) structural studies of pre- and post-fusion conformations; and (4) site-directed mutagenesis of key hydrophobic fusion peptides.
Non-enveloped viruses face the particular challenge of penetrating cellular membranes without the advantage of a lipid envelope, instead employing specialized protein components that disrupt membrane integrity. Some non-enveloped viruses, such as poliovirus, undergo receptor-induced conformational changes that expose hydrophobic domains or myristoyl groups capable of inserting into and disrupting target membranes [4] [1]. Others, including adenoviruses, utilize membrane-lytic peptides that are exposed following partial disassembly of the viral capsid in the endosomal compartment, creating pores through which the viral genome can enter the cytoplasm [1]. The penetration mechanisms of non-enveloped viruses share similarities with those employed by certain protein toxins, such as anthrax toxin, which also form oligomeric pores in target membranes [4]. Studying these penetration events often involves: (1) electron microscopy to visualize membrane disruptions; (2) electrophysiology to detect channel formation; (3) fluorescence assays monitoring release of encapsulated dyes from liposomes; and (4) biochemical analysis of capsid disassembly intermediates.
Table 2: Major Viral Entry Pathways with Key Characteristics and Representative Viruses
| Entry Pathway | Key Features | Cellular Components | Representative Viruses |
|---|---|---|---|
| Clathrin-Mediated Endocytosis | Receptor-mediated, forms coated vesicles, low pH trigger | Clathrin, dynamin, AP2 adaptors | Influenza virus, Adenovirus, Hepatitis C virus |
| Caveolar/Lipid Raft-Mediated | Cholesterol-rich domains, neutral pH, caveosomes | Caveolin-1, cholesterol, dynamin | SV40, Polyomavirus, Echovirus 1 |
| Macropinocytosis | Actin-driven, fluid-phase uptake, receptor-independent | Rac1, Pak1, actin, Na+/H+ exchangers | Vaccinia virus, Ebola virus, Coxsackievirus B |
| Direct Fusion | Plasma membrane fusion, pH-independent | Specific receptors, surface proteases | HIV-1, SARS-CoV-2 (TMPRSS2-dependent) |
| Endosomal Fusion | Acid pH-dependent, cathepsin priming | Early/late endosomes, cathepsins | SARS-CoV-2 (TMPRSS2-low), Influenza virus |
Case Studies in Receptor Utilization
Coronavirus Receptor Recognition Diversity
Coronaviruses exemplify the evolutionary ingenuity of viral receptor utilization, employing diverse entry receptors despite sharing common structural features in their spike glycoproteins. The spike proteins of coronaviruses contain two potentially receptor-binding domains—the N-terminal domain (S1-NTD) and C-terminal domain (S1-CTD)—with different coronaviruses utilizing these domains in various combinations to recognize distinct receptor molecules [6]. This strategic flexibility enables closely related coronaviruses to target different tissues and host species. For instance, SARS-CoV and HCoV-NL63, despite belonging to different genera (β and α, respectively), both utilize ACE2 as their primary receptor through interactions with the S1-CTD [6] [5]. In contrast, MERS-CoV, a β-coronavirus like SARS-CoV, targets DPP4 via its S1-CTD, while HCoV-229E, an α-coronavirus, uses aminopeptidase N (APN) as its receptor [6] [5]. This pattern demonstrates that receptor specificity does not strictly follow phylogenetic relationships, with very different coronavirus S1-CTDs from different genera sometimes recognizing the same receptor, while highly similar S1-CTDs within the same genus can recognize different receptors [6].
Structural biology has been instrumental in elucidating the molecular basis of coronavirus receptor selection. Crystal structures of coronavirus spike domains complexed with their receptors reveal both conserved and divergent strategies for receptor engagement. The SARS-CoV spike protein binds ACE2 through an extended loop that forms a gently concave surface with two ridges, termed the receptor-binding motif (RBM), which makes all contacts with the N-terminal lobe of ACE2 away from its enzymatic active site [6]. Similarly, the MERS-CoV spike engages DPP4 through extensive interactions that also avoid interference with the receptor's enzymatic function [6]. Beyond protein receptors, some coronaviruses utilize carbohydrate receptors, with β-coronaviruses OC43 and HKU1 recognizing 9-O-acetylated sialic acids, while α-coronavirus TGEV and γ-coronavirus IBV use sugar-based receptors recognized through their S1-NTDs [6]. This receptor diversity likely contributes to the expanded host range and tissue tropism observed across the coronavirus family, facilitating cross-species transmission and emergence of novel pathogenic strains like SARS-CoV-2.
Flavivirus Receptor Identification and Decoy Strategies
Recent research on flaviviruses has revealed unexpected insights into receptor usage and inspired innovative therapeutic approaches. Through systematic CRISPR-Cas9 screening, researchers identified members of the low-density lipoprotein receptor (LDLR) family as essential entry receptors for multiple flaviviruses [8]. Specifically, yellow fever virus was found to utilize LRP1, LRP4, and VLDLR for cellular entry, while the closely related tick-borne encephalitis virus employs LRP8 [8]. The distribution of these receptors correlates strongly with disease pathogenesis—LRP1 is highly expressed on liver cells, the primary target of yellow fever virus, while LRP8 is found primarily on nervous system cells, consistent with the neurotropism of tick-borne encephalitis virus [8]. This receptor identification followed a rigorous validation protocol: (1) genetic knockout of LDLR family members in cells rendered them resistant to infection; (2) heterologous expression of these receptors in non-susceptible cells conferred susceptibility; and (3) receptor overexpression enhanced viral entry in a dose-dependent manner.
Building on these receptor discoveries, researchers designed innovative decoy receptor molecules that effectively block viral entry [8]. These decoys consist of the extracellular domain of the identified LDLR family receptors fused to the Fc portion of human immunoglobulin, creating soluble receptor fragments that mimic the viral binding sites on cell surfaces [8]. When administered prophylactically, these decoys potently inhibited infection of human and mouse cells in vitro and protected immunodeficient mice from lethal yellow fever virus challenge [8]. The therapeutic strategy is particularly promising because it targets conserved host proteins rather than rapidly evolving viral components, potentially imposing a significant evolutionary constraint on viral escape mutants—any mutation that avoids decoy binding would likely also reduce affinity for the essential cellular receptor, thereby diminishing infectivity [8]. This decoy approach represents a paradigm shift in antiviral development, moving from direct viral targeting to host factor exploitation, with potential applications against diverse viruses sharing common receptor usage patterns.
Diagram 2: Viral entry process with key intervention points for therapeutic development, including receptor blockers, fusion inhibitors, and the novel decoy receptor strategy.
Experimental Toolkit for Viral Entry Research
Essential Research Reagents and Methodologies
Contemporary viral entry research employs a sophisticated toolkit of reagents and technologies designed to interrogate specific stages of the entry process. CRISPR-Cas9 gene editing systems have become indispensable for genetic screening, enabling comprehensive identification of host factors essential for viral entry [8]. These systems typically utilize lentiviral or retroviral delivery of guide RNA libraries targeting thousands of genes, followed by selection under viral challenge to identify protective knockouts. For proteomic analyses, affinity purification mass spectrometry relies on high-quality antibodies against viral surface proteins to capture virus-host protein complexes from cell lysates, with quantitative comparisons between infected and uninfected samples revealing specific interactions [3]. Advanced imaging techniques, particularly cryo-electron microscopy (cryo-EM) and X-ray crystallography, provide atomic-resolution views of virus-receptor interactions, as demonstrated by the structures of coronavirus spike proteins complexed with their cognate receptors [6] [1].
Functional validation of candidate receptors requires additional specialized reagents and assays. Neutralizing antibodies against putative receptors serve both as validation tools and potential therapeutic leads, blocking receptor function to assess infection inhibition [1]. Recombinant soluble receptor fragments find dual use in validation studies and therapeutic development, both as competitive inhibitors and decoy receptors [8] [6]. For studying entry kinetics and pathways, chemical inhibitors targeting specific cellular processes—such as bafilomycin A1 for endosomal acidification, chlorpromazine for clathrin-mediated endocytosis, and EIPA for macropinocytosis—help delineate the precise route of viral internalization [7]. Additionally, reporter virus systems incorporating fluorescent or luminescent markers enable real-time visualization and quantification of entry events in live cells, providing dynamic information about the spatial and temporal progression of infection. Together, this comprehensive experimental toolkit allows researchers to dissect the complex molecular choreography of viral entry with increasing precision.
Table 3: Essential Research Reagents for Viral Entry Studies
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| Gene Editing Systems | CRISPR-Cas9 libraries, RNAi reagents | Genome-wide knockout screens, candidate validation | Off-target effects, delivery efficiency, knockout completeness |
| Proteomic Tools | Co-immunoprecipitation antibodies, crosslinkers, mass spectrometry | Virus-host protein interaction mapping, complex identification | Antibody specificity, interaction stability, false positive rates |
| Structural Biology | Cryo-EM, X-ray crystallography, surface plasmon resonance | Atomic-level receptor binding analysis, conformational changes | Sample purity, conformational heterogeneity, resolution limits |
| Chemical Inhibitors | Bafilomycin A1, chlorpromazine, NH4Cl, EIPA | Entry pathway characterization, kinetic studies | Inhibitor specificity, cellular toxicity, off-target effects |
| Visualization Tools | Fluorescent protein fusions, quantum dots, immunofluorescence | Live-cell entry tracking, co-localization studies | Fluorophore brightness, photostability, labeling efficiency |
Therapeutic Implications and Future Directions
Targeting Viral Entry for Antiviral Development
The precise molecular understanding of viral entry mechanisms has enabled the rational design of innovative antiviral strategies that target specific stages of the entry process. Entry inhibitors represent a growing class of antivirals that block the earliest stages of infection, potentially preventing establishment of viral replication entirely [4] [7]. These include receptor-binding inhibitors like maraviroc (a CCR5 antagonist for HIV-1), fusion inhibitors such as enfuvirtide (HIV-1 gp41 inhibitor), and endosomal acidification blockers [3] [7]. The recently developed decoy receptor molecules against flaviviruses demonstrate a particularly promising approach, leveraging structural insights from virus-receptor complexes to design soluble receptor fragments that effectively compete with cellular receptors for viral binding [8]. This strategy offers potential advantages over traditional antivirals by targeting conserved host structures rather than mutable viral elements, potentially imposing a higher genetic barrier to resistance development [8].
Beyond direct-acting antivirals, viral entry research informs vaccine design by identifying key antigenic sites on viral attachment and fusion proteins [4] [1]. Structural characterization of prefusion conformations of viral glycoproteins has enabled the engineering of stabilized immunogens that elicit potent neutralizing antibodies, as demonstrated by the success of prefusion-stabilized SARS-CoV-2 spike vaccines [7]. Additionally, the identification of broadly neutralizing antibodies against conserved receptor-binding sites or fusion intermediates provides templates for monoclonal antibody therapeutics and vaccine immunogen design [1]. Emerging technologies like artificial intelligence (AI) and machine learning are further accelerating antiviral discovery, with platforms like Model Medicines' AI-driven platform identifying broad-spectrum polymerase inhibitors such as MDL-001 that target conserved viral domains across multiple virus families [9]. These computational approaches analyze vast datasets of viral sequences and structures to predict conserved, druggable pockets that are less prone to mutational escape, potentially yielding therapeutics with broader activity spectra against current and future viral threats [9].
Emerging Technologies and Research Frontiers
The field of viral entry research continues to evolve rapidly, driven by technological advances that enable increasingly sophisticated analyses. Quantitative proteomics methods have reached sensitivities and throughput capabilities that allow comprehensive mapping of dynamic protein interaction networks during viral entry, providing systems-level understanding of the complex host factor requirements [3]. These approaches can detect transient, low-affinity interactions that were previously missed by traditional biochemical methods, revealing previously unappreciated complexity in viral entry pathways. Similarly, single-particle tracking and live-cell imaging techniques now permit real-time visualization of individual virions during the entry process, revealing the dynamic spatial and temporal coordination of entry events with unprecedented resolution [7].
Looking forward, several emerging frontiers promise to further transform our understanding of viral entry mechanisms. Artificial intelligence is increasingly being integrated into the viral entry research pipeline, from target discovery and drug design to clinical trial optimization [9]. At IDWeek 2025, researchers highlighted AI multi-agent systems that can mine pathogen genomes for novel essential targets, generate initial inhibitor scaffolds, and evaluate pharmacological properties in silico before laboratory testing [9]. Additionally, the growing recognition of broad-spectrum antivirals that target conserved host pathways or viral domains represents a paradigm shift from pathogen-specific to pandemic-preparedness approaches [9]. These developments, combined with advanced structural biology techniques and gene editing technologies, are creating an increasingly powerful toolkit for deciphering the intricate molecular mechanisms of viral entry and developing next-generation countermeasures against existing and emerging viral threats.
Viruses, as obligate intracellular parasites, have evolved sophisticated mechanisms to exploit host cell machinery and metabolic pathways to ensure their replication and survival. This process, known as molecular hijacking, represents a fundamental aspect of viral pathogenesis where viruses reprogram cellular processes to create an environment favorable for viral propagation. The host-virus interaction is a perpetual tug-of-war fought at multiple interfaces, from the cell surface to the nucleus [10]. Viruses systematically target master regulator proteins and disrupt critical metabolic processes to alter the host's metabolic environment [11]. This reprogramming provides viruses with more energy for replication and propagation while simultaneously evading host immune defenses. The study of these hijacking mechanisms not only reveals how viruses cause disease but also identifies potential therapeutic targets for antiviral drug development.
The molecular hijacking strategies employed by viruses are remarkably diverse, ranging from direct exploitation of host enzymes and metabolic pathways to sophisticated mimicry of cellular components. Recent research has illuminated how viral RNA structures can hijack or subvert host RNA polymerases, ribosomes, translation-associated enzymes, RNA processing systems, and antiviral immunity proteins [10]. Simultaneously, viruses encode specialized proteins that manipulate host cell structures and signaling networks. Through these multifaceted approaches, viruses effectively reengineer the host cell into a viral replication factory, often while circumventing detection by the immune system. Understanding these mechanisms provides critical insights into viral pathogenesis and reveals novel vulnerabilities that can be targeted therapeutically.
Key Mechanisms of Viral Hijacking
RNA Structure-Mediated Hijacking
Structured RNA elements represent major players at the forefront of virus-host interactions, serving as conduits for viral exploitation of host cellular machinery. Viral RNA structures frequently mimic existing cellular interfaces, functioning as doppelgängers that enable widespread viral mimicry of cellular interactions [10]. These structured elements often amalgamate distinct features from multiple host RNAs to form chimeras that simultaneously target various host systems for viral gains. Through this sophisticated structural mimicry, viral RNAs can hijack host RNA polymerases, ribosomes, translation-associated enzymes, RNA processing systems, modification machinery, transport systems, and antiviral immunity proteins [10].
Advanced visualization techniques have revealed complex RNA and ribonucleoprotein structures at virus-host interfaces, providing unprecedented insights into the molecular mechanisms of viral exploitation. These structures frequently have their roots or structural doppelgängers in existing cellular interfaces, suggesting that viruses have evolved to mimic native molecular interactions as an efficient hijacking strategy. The resulting chimeric RNA structures enable viruses to borrow and combine distinct features from several host RNAs, creating multifunctional elements that can simultaneously target multiple host systems. This RNA-level hijacking represents a fundamental strategy across diverse virus families to subvert host cell processes from within the core of cellular machinery.
Viroporins: Pore-Forming Viral Proteins
Viroporins are small hydrophobic transmembrane proteins encoded by viruses that self-oligomerize to form membrane-embedded pores facilitating ion transport. These viral proteins play critical roles in multiple stages of the viral life cycle by modulating ion homeostasis, disrupting host membrane integrity, and orchestrating key stages from viral entry to release [12]. Beyond facilitating viral propagation, viroporins exacerbate pathogenesis by disrupting cellular ion homeostasis and triggering proinflammatory responses through mechanisms such as NLRP3 inflammasome activation [12].
Table 1: Classification and Properties of Characterized Viroporins
| Virus | Viroporin | Classification | Amino Acids | Ion Selectivity | Oligomeric State |
|---|---|---|---|---|---|
| Influenza A virus | M2 | IA/SP type I | 97 | H+, K+, Na+ | 4 |
| SARS-CoV-2 | E | IA/SP type I | 75 | K+, Ca2+ | 2/5 |
| Poliovirus | 2B | IIB/MP type II | 97 | Ca2+ | - |
| Ebola virus | Delta peptide | IA/SP type I | 40-49 | Cl⁻ | - |
| Human astrovirus | XP | IA/SP type I | 112 | - | - |
Viroporins are primarily classified into three structural categories based on their transmembrane domains (TMDs). Type I viroporins contain one TMD and are further subdivided into IA and IB subtypes based on membrane orientation. Type II viroporins possess two TMDs forming a transmembrane helix-turn-helix hairpin structure, with IIA and IIB subtypes distinguished by their terminal orientations. Type III viroporins contain three TMDs [12]. The functional characterization of viroporins typically employs electrophysiological techniques such as patch-clamp and planar lipid bilayers, though these approaches require validation in physiological contexts as heterologous expression systems may produce artifactual results [12].
Metabolic Reprogramming of Host Cells
Viruses fundamentally reprogram host cell metabolism to meet the substantial energy and biosynthetic demands of viral replication. This reprogramming involves targeting master regulator proteins and disrupting important metabolic processes, particularly in metabolic organs [11]. The metabolic alterations induced by viruses promote survival of infected cells while generating abundant energy and building blocks for viral replication and propagation. Viruses achieve this reprogramming through multiple strategies, including releasing molecules like miRNAs, interferons, and adipocytokines that affect both infected cells and distant organs involved in glucose and energy homeostasis [11].
The rewiring of host cell metabolism is particularly evident in the manipulation of central carbon metabolism. Many viruses induce a Warburg-like effect, shifting cells toward aerobic glycolysis even in the presence of oxygen, similar to observations in cancer cells. This glycolytic shift generates ATP rapidly while also providing metabolic intermediates for nucleotide, amino acid, and lipid biosynthesis – all essential components for new virion production. Additionally, viruses commonly enhance glutamine metabolism to replenish TCA cycle intermediates through anaplerosis and boost pentose phosphate pathway flux to generate NADPH for biosynthetic reactions and nucleotide precursors. This comprehensive metabolic restructuring represents a core hijacking strategy essential for efficient viral replication.
Mitochondrial Sabotage for Immune Evasion
Viruses have developed sophisticated mechanisms to sabotage mitochondrial function, particularly to evade host immune responses. Recent research has revealed how Kaposi's sarcoma-associated herpesvirus (KSHV) encodes a viral Bcl-2 protein (vBcl-2) that binds to and activates the host enzyme NM23-H2, recruiting it to mitochondria where it provides GTP to power the mitochondrial fission machinery [13]. This triggers mitochondrial fragmentation at a critical time when these organelles should remain connected, preventing the assembly of the MAVS immune signaling platform that normally triggers Type I interferon responses – the cell's front-line antiviral defense [13].
This mitochondrial sabotage represents a sophisticated immune evasion strategy. By remodeling mitochondrial architecture, the virus destabilizes the entire immune signaling hub rather than merely blocking a single immune protein. In the absence of vBcl-2-induced mitochondrial fragmentation, interferon signaling activates two key antiviral proteins – TRIM22 and MxB – which trap virus particles in the nucleus and prevent their release [13]. Other herpesviruses, including Epstein-Barr virus, encode similar Bcl-2 proteins, suggesting that mitochondrial reshaping represents a conserved strategy across this virus family. This mechanism highlights how viruses can target fundamental cellular organelles to create an environment permissive for viral replication and dissemination.
Experimental Approaches for Studying Viral Hijacking
Structural and Biophysical Characterization
The structural characterization of virus-host interfaces requires sophisticated methodologies to visualize complex molecular interactions. Cryo-electron microscopy (cryo-EM) has emerged as a powerful technique for determining high-resolution structures of viral and host proteins, ribonucleoprotein complexes, and membrane proteins such as viroporins [12]. This technique allows researchers to visualize macromolecular complexes in near-native states, providing insights into the molecular mechanisms of viral exploitation. Complementary to cryo-EM, X-ray crystallography continues to provide atomic-resolution structures of viral proteins in complex with host factors, revealing detailed interaction interfaces that can be targeted therapeutically.
Electrophysiological techniques are essential for characterizing the functional properties of viroporins. Patch-clamp electrophysiology and planar lipid bilayer measurements enable direct assessment of ion channel activity, selectivity, and gating mechanisms [12]. However, these approaches carry inherent limitations as they often require heterologous expression of candidate channels or reconstitution of isolated peptides into artificial membranes, which may not fully recapitulate physiological cellular environments. To address these challenges, researchers are increasingly combining electrophysiological approaches with molecular dynamics simulations and mutational analyses to confirm ion channel activity by perturbing key residues involved in channel gating and ion selectivity [12].
Molecular Imaging of Viral Pathogenesis
Molecular imaging represents a valuable tool for non-invasive study of viral pathogenesis in both clinical and research settings. Unlike traditional microbiological detection methods that provide single timepoint snapshots, molecular imaging enables longitudinal whole-body data collection, allowing pathological changes to be monitored and detected in unexpected body regions [14]. This capability is particularly valuable for understanding systemic viral infections, as demonstrated during the COVID-19 pandemic when what was initially considered a respiratory illness was revealed to cause multi-systemic pathology [14].
Table 2: Molecular Imaging Modalities for Viral Pathogenesis Studies
| Imaging Modality | Probe Types | Spatial Resolution | Key Applications | Advantages |
|---|---|---|---|---|
| PET (Positron Emission Tomography) | Positron-emitting radionuclides (e.g., 18F, 89Zr) | 1-2 mm (clinical); <1 mm (preclinical) | Metabolic imaging, receptor targeting | High sensitivity, quantitative capabilities |
| SPECT (Single Photon Emission Computed Tomography) | Gamma-emitting radionuclides (e.g., 99mTechnetium, 123Iodine) | 1-2 mm (clinical); 0.5-1 mm (preclinical) | Receptor occupancy, perfusion imaging | Multi-isotope imaging, wider availability |
| Magnetic Resonance Spectroscopy (MRS) | Endogenous metabolites (e.g., choline, creatine) | 1-10 mm³ voxels | Metabolic pathway analysis | No ionizing radiation, simultaneous anatomical and metabolic data |
Nuclear imaging techniques, particularly PET and SPECT, offer high detection sensitivity and a growing repertoire of probes for studying viral infections. PET imaging uses positron-emitting isotopes that generate detectable annihilation photons, enabling 3D image reconstruction of functional processes [14]. SPECT relies on probes that undergo gamma decay, releasing photons detectable by gamma cameras. While PET generally offers higher sensitivity and resolution in clinical settings, SPECT provides the advantage of potential multi-isotope imaging to simultaneously monitor multiple biological targets [14]. These imaging modalities are frequently combined with anatomical imaging techniques like CT or MRI to correlate molecular signals with structural changes.
Proteomic and Interaction Network Analysis
The systematic mapping of protein-protein interactions (PPIs) between viral and host proteins provides crucial insights into hijacking mechanisms. Human-virus PPIs help elucidate the molecular basis of viral infection and host response, guiding the development of targeted antiviral strategies [15]. These interaction networks are typically represented with nodes representing proteins and edges representing physical interactions, revealing how viral proteins rewire host cellular machinery. Research has demonstrated that viral proteins often interact with highly connected host proteins, suggesting targeting of hub proteins in cellular networks [15].
Advanced technologies for studying interactomes include yeast two-hybrid systems, affinity purification coupled with mass spectrometry, and protein complementation assays. These approaches have revealed that viruses with small genomes, such as HIV, interact extensively with host proteins to compensate for their limited coding capacity [15]. Meanwhile, larger DNA viruses like herpesviruses encode more self-sufficient networks with complex intraviral interactomes. The interfaces of these protein interactions represent critical determinants of binding specificity, with electrostatic and structural properties governing recognition. Mutational analyses of these interfaces have revealed how subtle changes can dramatically alter interaction networks and viral pathogenicity.
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Viral Hijacking Mechanisms
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Structural Biology Tools | AlphaFold, Cryo-EM, Molecular Dynamics Simulations | Viroporin structure determination, RNA-protein complexes | Protein structure prediction, complex visualization |
| Metabolic Assays | Seahorse Analyzer, Stable Isotope Tracers, Mass Spectrometry | Metabolic flux analysis, pathway utilization | Real-time metabolic measurements, pathway mapping |
| Interaction Mapping | Yeast Two-Hybrid, AP-MS, BioID | Host-virus protein interaction networks | Proximity labeling, complex identification |
| Electrophysiology | Patch Clamp, Planar Lipid Bilayers | Viroporin channel characterization | Ion channel activity, selectivity, and gating |
| Molecular Imaging | 18F-FDG, 89Zr-labeled antibodies, Radioactive nucleotides | In vivo tracking of infection, metabolic changes | Non-invasive monitoring, whole-body visualization |
Methodologies for Key Experiments
Viroporin Characterization Workflow
The comprehensive characterization of viroporins requires an integrated multidisciplinary approach. A robust workflow begins with bioinformatic analysis to identify potential viroporin candidates based on sequence features such as hydrophobic domains and propensity for membrane insertion. This is followed by heterologous expression in model systems like Xenopus oocytes or mammalian cell lines for initial functional screening. Electrophysiological characterization using patch-clamp or planar lipid bilayer measurements assesses ion channel activity, selectivity, and gating properties [12]. Structural analysis via cryo-EM or X-ray crystallography provides high-resolution insights into oligomeric states and pore architectures. Crucially, genetic validation through mutational analysis confirms the functional significance of key residues, while cell-based assays establish physiological relevance in the context of viral infection [12].
Metabolic Reprogramming Analysis
Investigating virus-induced metabolic reprogramming requires a combination of metabolomic, fluxomic, and molecular biology techniques. A comprehensive workflow begins with infection of relevant cell culture models followed by metabolite extraction at specific timepoints. Mass spectrometry-based metabolomics enables quantification of metabolite abundance changes across central carbon metabolism, including glycolysis, TCA cycle, pentose phosphate pathway, and nucleotide metabolism [11]. Stable isotope tracing with 13C- or 15N-labeled nutrients (e.g., 13C-glucose, 13C-glutamine) allows determination of metabolic flux through specific pathways. Complementary transcriptional and proteomic analyses identify regulatory changes driving metabolic alterations. Functional validation through pharmacological inhibition or genetic knockdown of key metabolic enzymes confirms the essentiality of specific pathways for viral replication [11].
Mitochondrial Manipulation Assay
The investigation of viral manipulation of mitochondrial dynamics requires specialized methodologies focused on organelle morphology and function. A typical experimental workflow begins with infection of appropriate host cells, followed by fixation and immunostaining of mitochondrial markers (e.g., TOMM20, COX IV) and viral proteins at various timepoints. High-resolution confocal microscopy enables qualitative and quantitative assessment of mitochondrial morphology, distinguishing between fused networks and fragmented puncta [13]. Functional assays measuring mitochondrial membrane potential (using dyes like TMRE or JC-1), ATP production, and reactive oxygen species generation provide insights into bioenergetic alterations. Immunoprecipitation of viral proteins with subsequent mass spectrometry identification reveals interacting host partners, while genetic approaches (siRNA, CRISPR) validate the requirement of specific host factors for viral-mediated mitochondrial fragmentation [13].
The systematic hijacking of host cell machinery and metabolic pathways represents a cornerstone of viral pathogenesis. Through diverse mechanisms including RNA structural mimicry, viroporin-mediated membrane manipulation, metabolic reprogramming, and mitochondrial sabotage, viruses extensively reengineer host cells to support their replication while evading immune detection. The investigation of these processes requires sophisticated methodological approaches spanning structural biology, molecular imaging, interactome mapping, and metabolic analysis. As our understanding of these hijacking mechanisms deepens, new therapeutic vulnerabilities are being revealed that target the essential interfaces between viruses and their host cells. Future research directions will likely focus on developing compounds that disrupt these critical host-virus interactions, potentially leading to broad-spectrum antiviral strategies that are less susceptible to viral resistance.
Viral pathogenesis is defined as the process by which viral infection leads to disease, a complex interplay that extends far beyond simple cell killing to encompass sophisticated mechanisms of host manipulation [16]. At the heart of successful viral colonization lies the critical ability to evade, subvert, or outright disable host immune defenses. This biological arms race has driven the evolution of remarkably diverse immune evasion strategies, which can be broadly categorized into two fundamental approaches: direct interference through viral protein interactions and indirect manipulation through epigenetic silencing of host defense genes. Understanding these tactics is not merely an academic exercise but a pressing necessity for developing next-generation antiviral therapeutics and vaccines. This review synthesizes current research on how viruses employ molecular sabotage at both the protein and epigenetic levels to establish infection, with profound implications for pathogenesis and therapeutic intervention.
The following table summarizes the core immune evasion mechanisms discussed in this review:
Table: Core Categories of Viral Immune Evasion Mechanisms
| Evasion Category | Molecular Mechanism | Representative Viruses | Primary Effect |
|---|---|---|---|
| Direct Protein Interaction | Viral proteins bind and inhibit key immune signaling molecules (e.g., MAVS, STING) | SARS-CoV-2, PRV [17] [18] | Blocks downstream interferon and cytokine production |
| Receptor Modulation | Mutations in surface proteins alter binding interfaces to evade neutralizing antibodies | SARS-CoV-2 (e.g., E484K, T478K) [19] | Reduces antibody neutralization while maintaining host receptor binding |
| Epigenetic Silencing | Recruitment of host epigenetic modifiers (e.g., DNMT1) to immune gene promoters | Tumor viruses via FOXM1 [20], Endogenized giant viruses [21] | Heritable suppression of immune sensor and effector gene expression |
| Decoy & Mimicry | Viral production of cytokine mimics or decoy receptors | KSHV (vIL-6) [22] | Dysregulates host inflammatory responses and cell signaling |
Viral Protein Interactions: Direct Sabotage of Immune Signaling
Viruses deploy a molecular arsenal of proteins that directly target and disrupt the host's immune signaling apparatus. This frontline evasion strategy involves precise protein-protein interactions that intercept critical immune activation pathways at their most vulnerable nodes.
SARS-CoV-2: Master of Interferon Interdiction
SARS-CoV-2 exemplifies sophisticated interferon (IFN) pathway evasion. The virus delays the induction of type I and III interferons (IFN-I and IFN-III) at the initial infection site, while paradoxically causing systemic IFN-I priming in distal organs [18]. This dysregulation is a key contributor to COVID-19 severity. The primary cellular defense against RNA viruses like SARS-CoV-2 is the MDA5-mediated recognition of viral double-stranded RNA (dsRNA) structures, which triggers a signaling cascade through the mitochondrial antiviral-signaling protein (MAVS), leading to the activation of transcription factors IRF3 and NF-κB and the production of IFN-I/III [18]. SARS-CoV-2 thwarts this through multiple non-structural proteins (Nsps) and accessory proteins that:
- Block MDA5 Activation: Viral proteins prevent the recognition of dsRNA replication intermediates by MDA5.
- Interfere with MAVS Signaling: Key viral proteins disrupt the critical relay between RNA sensing and downstream transcription.
- Inhibit IRF3 Nuclear Translocation: Even if sensing occurs, the final step of interferon gene activation is often blocked.
This multi-layered interference creates a critical delay in the antiviral response, allowing the virus to establish a foothold and replicate unchecked during the earliest stages of infection [18].
Spike Protein Mutations: Balancing Affinity and Evasion
Beyond innate immune sabotage, viral surface proteins continuously evolve to evade adaptive immunity. The SARS-CoV-2 spike protein receptor-binding domain (RBD) is a hotspot for mutations that fine-tune the trade-off between ACE2 receptor affinity and antibody escape [19]. For instance:
- T478K: This prevalent mutation in Delta and Omicron variants enhances ACE2 binding through structural rigidification and salt bridge formation (e.g., K478-D30), favoring increased transmissibility [19].
- E484K: This mutation, a hallmark of Beta and Gamma variants, balances antibody evasion (e.g., against LY-CoV555) with receptor stabilization via compensatory interactions (e.g., K484-D38) [19].
- F490S and G496S: These mutations act as stealth adaptations, subtly destabilizing the ACE2 interface or introducing metastability without fully disrupting binding, thereby facilitating immune evasion [19].
Table: Functional Impact of Key SARS-CoV-2 Spike Mutations
| Mutation | Variant Association | Impact on ACE2 Binding | Immune Evasion Mechanism |
|---|---|---|---|
| T478K | Delta, Omicron | Enhanced | Electrostatic complementarity and salt bridge formation |
| E484K | Beta, Gamma | Stabilized | Disruption of antibody-binding sites (e.g., LY-CoV555) |
| T478A | Laboratory study | Weakened | Polarity loss and interface relaxation |
| T478E | Laboratory study | Weakened | Electrostatic repulsion at binding interface |
| F490S | Circulating variants | Subtly destabilized | Disruption of hydrophobic interactions with ACE2's K353 |
| G496S | Circulating variants | Subtly destabilized | Introduction of metastability at the RBD-ACE2 interface |
Herpesvirus Strategies: Broad-Spectrum Signaling Disruption
Other viruses employ similar direct interference tactics. The Pseudorabies virus (PRV), an alphaherpesvirus, establishes persistent latent infections by effectively evading the host's antiviral innate immune response through sophisticated strategies that disrupt immune signaling pathways [17]. Similarly, Kaposi's sarcoma-associated herpesvirus (KSHV/HHV-8) encodes viral proteins like latency-associated nuclear antigen (LANA) and viral interleukin-6 (vIL-6) that manipulate host cell survival pathways, including PI3-K signaling and Rho GTPase regulation, to drive oncogenesis while evading immune detection [22].
Epigenetic Silencing: The Stealth Approach to Immune Evasion
Beyond direct protein interactions, viruses have co-opted the host's epigenetic machinery to achieve long-term, heritable suppression of antiviral defense genes. This stealth approach represents a more profound and sustained form of immune subversion.
FOXM1-Mediated Silencing of the DNA Sensing Pathway
A paradigm of viral-induced epigenetic silencing has been elucidated in virological research, particularly in the context of viral oncogenesis. The transcription factor FOXM1, often dysregulated by viruses, creates an immune-suppressive environment by epigenetically silencing the cytosolic DNA-sensing pathway [20]. The mechanism is a multi-step process:
- FOXM1 recruits a DNMT1-UHRF1 complex to the promoter of the STING gene.
- This complex deposits repressive DNA methylation marks, effectively silencing STING expression.
- Silenced STING prevents the activation of the unfolded protein response protein CHOP, which is required to activate the expression of the stress ligand ULBP1.
- The lack of ULBP1 on the cell surface blocks the NKG2D-NKG2DL interaction, which is critical for priming natural killer (NK)- and T cell-mediated cytotoxicity [20].
This elegant epigenetic sabotage allows virus-infected or transformed cells to evade detection and destruction by the innate and adaptive immune system. Cancer patients with higher FOXM1 and DNMT1, and lower STING and ULBP1, experience worse survival and poor response to immunotherapy, underscoring the clinical significance of this pathway [20].
Diagram Title: FOXM1 Epigenetic Silencing of Immune Sensing
Host-Directed Silencing of Endogenized Viral Elements
The host also leverages epigenetic mechanisms defensively to silence endogenized viral DNA. Studies in Acanthamoeba, a protist model for giant virus interactions, reveal that newly acquired viral integrations are disproportionately found in sub-telomeric regions and are hypermethylated and highly condensed [21]. This host-induced heterochromatic silencing suppresses the expression of recently acquired viral DNA, preventing potential toxicity or genome instability. The trajectory of viral sequences follows a clear path: (i) integration of viral DNA, (ii) epigenetic suppression via methylation and condensation, and (iii) long-term deterioration of viral genomes by point mutation and mobile element colonization [21]. This demonstrates that epigenetic silencing is a universal strategy in the host-virus arms race, employed by both parties for survival advantage.
Experimental Methodologies for Deconstructing Immune Evasion
Unraveling these complex evasion tactics requires a robust and multidisciplinary experimental toolkit. The following section outlines key protocols and reagents essential for probing both protein-level and epigenetic evasion mechanisms.
Molecular Dynamics (MD) Simulations for Protein Interaction Analysis
Objective: To assess the biophysical impacts of viral protein mutations on host receptor binding and antibody evasion at atomic-level resolution [19].
Protocol:
- Protein Structure Preparation: Obtain structural coordinates of host receptors (e.g., ACE2, PDB ID: 1R42) and viral proteins (e.g., SARS-CoV-2 Spike RBD, PDB ID: 6M0J) from the Protein Data Bank. Introduce desired mutations into the viral protein using molecular visualization software like PyMOL [19].
- System Setup: Solvate the protein-protein complex in a water box (e.g., TIP3P water model) and add physiological ion concentrations (e.g., 150 mM NaCl) to mimic the cellular environment.
- Energy Minimization and Equilibration: Use molecular mechanics force fields (e.g., AMBER, CHARMM) to minimize the system's energy and gradually equilibrate it under specified temperature and pressure conditions (e.g., NPT ensemble at 310 K).
- Production MD Run: Perform extensive, nanosecond-to-microsecond timescale simulations to sample the conformational dynamics of the complex. Trajectories are analyzed for:
- Binding Free Energy: Calculate using methods like Molecular Mechanics/Generalized Born Surface Area (MM/GBSA) to quantify interaction strength.
- Salt Bridge & H-bond Analysis: Monitor formation, breakage, and stability of key electrostatic interactions.
- Root Mean Square Fluctuation (RMSF): Measure per-residue flexibility to identify mutations that cause rigidification or relaxation of the binding interface.
- Validation: Correlate in silico findings with in vivo viral fitness and neutralization assays from animal models or clinical isolates [19].
Mapping Epigenetic Landscapes via scRNA-seq and Methylation Analysis
Objective: To identify viral-mediated epigenetic reprogramming of host immune genes and its functional consequences on the tumor immune microenvironment (TIME) [20].
Protocol:
- Perturbation and Model Systems: Use CRISPR-Cas9 or shRNA to knockout/down candidate viral or host factors (e.g., FOXM1) in relevant cell lines (e.g., triple-negative breast cancer models like E0771 or MDA-MB-231). Establish syngeneic tumors in immunocompetent mice [20].
- Single-Cell RNA Sequencing (scRNA-seq):
- Tissue Processing: Create single-cell suspensions from harvested control and knockout tumors.
- Library Preparation & Sequencing: Use platforms like 10x Genomics to generate barcoded scRNA-seq libraries. Sequence to an appropriate depth (e.g., 50,000 reads/cell).
- Bioinformatic Analysis: Perform unsupervised clustering and cell population annotation using known markers (e.g., Cd3e for T cells, Ncr1 for NK cells). Conduct gene set enrichment analysis (GSEA) to identify differentially activated pathways [20].
- DNA Methylation Analysis:
- DNA Extraction & Bisulfite Treatment: Treat genomic DNA from cells with bisulfite, which converts unmethylated cytosines to uracils.
- Targeted Sequencing: Perform bisulfite sequencing (e.g., Whole Genome Bisulfite Sequencing or targeted approaches) on promoters of genes of interest (e.g., STING).
- Analysis: Map sequencing reads and calculate methylation percentages at individual CpG sites. Compare profiles between control and experimental groups.
- Functional Immune Assays: Validate findings using flow cytometry to quantify immune cell infiltration (CD45+, CD8+ T cells, Tregs) and surface expression of stress ligands (e.g., ULBP1). Use cytotoxicity assays to measure NK and T cell killing capacity [20].
The Scientist's Toolkit: Essential Research Reagents
A comprehensive investigation of immune evasion requires a carefully selected set of reagents and model systems, as detailed below.
Table: Key Research Reagent Solutions for Immune Evasion Studies
| Reagent / Material | Specific Example | Function in Investigation |
|---|---|---|
| CRISPR-Cas9 System | sgRNAs targeting FOXM1 [20] | Gene knockout to validate the functional role of a host factor in immune evasion. |
| Stable Cell Lines | FOXM1-knockout E0771 or MDA-MB-231 cells [20] | Provide a consistent in vitro and in vivo model for studying the loss-of-function effects. |
| Syngeneic Mouse Models | Immunocompetent C57BL/6J mice [20] | Enable the study of immune evasion in a context of a fully functional immune system. |
| Flow Cytometry Antibodies | Anti-CD45, CD8, CD4, FOXP3, CD11b, CD11c, MHC-II [20] | Phenotype and quantify immune cell populations infiltrating the tumor or infected tissue. |
| scRNA-seq Platform | 10x Genomics Chromium [20] | Unbiased profiling of the transcriptome of every cell in a complex tissue sample (TIME). |
| Protein Structural Data | PDB IDs: 6M0J (SARS-CoV-2 RBD), 1R42 (ACE2) [19] | Starting points for molecular dynamics simulations and structural analysis of protein interactions. |
| Molecular Dynamics Software | AMBER, CHARMM, GROMACS [19] | Simulate the physical movements of atoms and molecules to study dynamic protein behavior. |
The intricate interplay between viral protein interactions and epigenetic silencing represents a cornerstone of modern viral pathogenesis research. Direct protein interference allows for rapid, potent shutdown of specific immune pathways, while epigenetic reprogramming offers a stealthier, more sustained strategy for immune avoidance. The convergence of these tactics—observed in diverse viruses from SARS-CoV-2 to KSHV—highlights their fundamental importance to viral fitness and persistence.
Future research must focus on the dynamic intersection of these fields. Key questions remain: How do initial protein interactions trigger long-term epigenetic changes? Can the repressive epigenetic marks laid down by viruses be therapeutically erased? The answers will hinge on integrated methodologies that combine structural biology, omics technologies, and immunology. The experimental frameworks and tools outlined herein provide a roadmap for this work. By continuing to deconstruct these evasion tactics, researchers can identify novel vulnerabilities, paving the way for host-directed therapies that bolster innate immune recognition and break the cycle of viral persistence and pathogenesis.
Viral tropism is defined as the ability of a virus to infect and replicate within specific cell types, tissues, or host species while encountering restrictions in others [23]. This fundamental property shapes viral pathogenesis, determining the clinical manifestations of disease, the efficiency of transmission, and the potential for cross-species spread. The molecular basis of tropism involves a complex interplay between viral surface proteins and host cell factors, which govern every step of the viral life cycle from initial attachment to progeny release. Understanding these determinants is crucial for predicting disease outcomes, developing targeted antiviral therapies, and designing effective vaccines.
Within the broader context of viral pathogenesis research, elucidating tropism mechanisms provides a framework for explaining why respiratory viruses predominantly cause cough and shortness of breath, why enteric viruses lead to gastrointestinal symptoms, and why neurotropic viruses can cause encephalitis and long-term neurological sequelae [24] [25]. Furthermore, variations in tropism can explain differences in transmission dynamics and pathogenicity between related viruses, as exemplified by the distinct clinical manifestations of SARS-CoV and SARS-CoV-2 despite their genetic similarity [24]. This guide examines the molecular mechanisms underlying tissue-specific viral pathogenesis, current methodologies for tropism investigation, and the implications for therapeutic development.
Molecular Mechanisms of Viral Entry and Cellular Invasion
Initial Attachment and Receptor Interactions
The first critical determinant of cellular tropism is viral attachment to host cell surfaces. This process is mediated through specific interactions between viral surface proteins and host cell receptors:
- Animal viruses typically utilize plasma membrane receptors for cell entry, with different virus families employing distinct receptor types. For example, SARS-CoV-2 primarily engages the angiotensin-converting enzyme 2 (ACE2) receptor through its Spike protein, initiating the entry process [26].
- Plant viruses face the unique challenge of the plant cell wall, which acts as a physical barrier restricting diffusion of macromolecules larger than 60 kDa. These viruses bypass this barrier by exploiting mechanical damage or vector organisms to introduce viral particles directly into plant tissues [23].
Beyond primary receptor binding, many viruses require co-receptors or attachment factors that enhance binding efficiency or trigger conformational changes necessary for entry. Proteolytic priming of viral surface proteins by host proteases represents another critical tropism determinant, as the distribution of these activating enzymes varies across tissues [26].
Intracellular Trafficking and Membrane Fusion
Following attachment, viruses employ diverse entry mechanisms to penetrate cellular membranes and deliver their genetic material into the host cell cytoplasm:
- Direct membrane fusion at the cell surface is utilized by some viruses, such as SARS-CoV-2 when primed by plasma membrane proteases like TMPRSS2.
- Receptor-mediated endocytosis pathways are hijacked by many viruses, with subsequent fusion events occurring within endosomal compartments. These pathways often depend on endo-lysosomal proteases (e.g., cathepsins) that further process viral proteins to activate fusion potential.
- Viroporin activity facilitates the release of viral genomes from endocytic compartments into the cytoplasm. These small, hydrophobic viral proteins oligomerize to form membrane-embedded pores that modulate ion homeostasis and disrupt host membrane integrity [12].
Table 1: Classification and Properties of Characterized Viroporins
| Virus | Viroporin | Classification | Amino Acids | Ion Selectivity | Oligomeric State |
|---|---|---|---|---|---|
| Influenza A virus | M2 | IA/SP type I | 97 | H+, K+, Na+ | 4 |
| SARS-CoV-1 | E | IA/SP type I | 76 | K+, Ca2+ | 5 |
| SARS-CoV-2 | E | IA/SP type I | 75 | K+, Ca2+ | 2/5 |
| Poliovirus | 2B | IIB/MP type II | 97 | Ca2+ | - |
| Ebola virus | Delta peptide | IA/SP type I | 40-49 | Cl⁻ | - |
Host and Viral Determinants of Tissue Specificity
Host Factors Governing Tropism
Cellular susceptibility to viral infection is governed by the constellation of host factors that either facilitate or restrict the viral life cycle:
- Entry factor expression patterns directly determine which tissues can be initially infected. CRISPR activation screens have identified numerous membrane proteins beyond the canonical ACE2 receptor that can modulate SARS-CoV-2 entry, including the potassium channel KCNA6 and the endo-lysosomal protease legumain (LGMN) [26].
- Intrinsic immunity factors, such as restriction factors and RNA interference machinery, vary in expression and activity across cell types, creating barriers to infection in non-permissive cells.
- Metabolic and biosynthetic capacity of host cells must support viral replication, with different cell types providing varying environments conducive to viral gene expression and particle assembly.
The interferon response and other antiviral signaling pathways demonstrate cell-type-specific activation patterns that significantly influence tropism. Neuronal cells, for instance, may exhibit attenuated interferon responses compared to epithelial cells, potentially explaining the persistence of certain viruses in neural tissue [25].
Viral Determinants of Tissue Specificity
Viral genomes encode specific proteins that actively dictate tropism through interactions with host cell components:
- Attachment proteins and their genetic variability represent the primary viral determinant of tropism. Sequence variations in these proteins can alter receptor binding affinity or enable usage of alternative receptors, thereby expanding or restricting host range.
- Movement proteins in plant viruses facilitate intercellular transport through plasmodesmata by modifying size exclusion limits, effectively governing which tissues become infected systemically [23].
- Viral countermeasures to host restriction factors, such as RNA silencing suppressors in plants and interferon antagonists in animals, exhibit cell-type-specific efficacy that shapes tropism [23].
The genetic plasticity of viruses allows rapid adaptation to new cell types through mutations in tropism-determining regions. This evolutionary capacity is particularly significant for RNA viruses with high mutation rates, enabling tropism expansion that may facilitate cross-species transmission and epidemic emergence.
Quantitative Analysis of Tropism and Replication Kinetics
Comparative Viral Replication Profiles
Replication kinetics vary significantly across cell types and between related viruses, providing quantitative insights into tropism determinants. A comparative study of SARS-CoV-2 and SARS-CoV demonstrated distinct replication patterns that correlate with their differing clinical manifestations:
- SARS-CoV-2 replicated to comparable levels in human intestinal (Caco2) and pulmonary (Calu3) cells over 120 hours, whereas SARS-CoV replicated significantly more efficiently in intestinal cells [24].
- SARS-CoV-2, but not SARS-CoV, demonstrated modest replication in neuronal (U251) cells, potentially explaining neurological manifestations such as confusion, anosmia, and ageusia in COVID-19 patients [24].
- SARS-CoV-2 consistently induced delayed and milder cell damage compared to SARS-CoV in non-human primate cells, possibly contributing to its high transmission efficiency by enabling extended asymptomatic shedding [24].
Table 2: Replication Kinetics of SARS-CoV-2 Versus SARS-CoV Across Cell Lines
| Cell Line | Tissue Origin | SARS-CoV-2 Replication | SARS-CoV Replication | Statistical Significance |
|---|---|---|---|---|
| Caco2 | Intestinal | High | Very High | p=0.0098 |
| Calu3 | Pulmonary | High | Moderate | p=0.52 (NS) |
| U251 | Neuronal | Modest | Undetectable | p=0.036 |
| VeroE6 | Non-human primate kidney | High | High | Cell damage significantly milder for SARS-CoV-2 (p=0.016) |
Evolutionary Implications of Cellular Tropism
Cellular tropism has profound implications for viral evolution and long-term adaptation to host species:
- Viruses infecting epithelial cells with high turnover rates evolve significantly faster than those infecting long-lived cells such as neurons [27]. This correlation between target cell and substitution rate suggests that cellular division rates directly influence viral evolutionary dynamics.
- The mutation rates of RNA viruses do not fully explain substitution rate variation, indicating that ecological factors like cell tropism play crucial roles in shaping viral evolvability [27].
- Transmission bottlenecks and selective pressures differ across tissues, creating distinct evolutionary trajectories for viruses with different tropism profiles.
Methodologies for Tropism Investigation
Advanced Screening Technologies
Modern approaches to tropism research employ high-throughput methodologies that enable systematic identification of host factors influencing viral infection:
- CRISPR-based screening platforms, particularly CRISPR activation (CRISPRa), allow functional interrogation of host factors by enabling targeted gene overexpression in combination with viral challenge models. Membrane-wide CRISPRa screens have identified novel host factors such as LGMN and KCNA6 that promote SARS-CoV-2 entry in specific cellular contexts [26].
- Single-cell RNA sequencing coupled with barcoded viral libraries enables multiplex assessment of transduction efficiency and specificity across complex cell populations. This technology maps how viral variants transduce individual cells within heterogeneous tissues like human cerebral and ocular organoids [28].
Experimental Models for Tropism Studies
Physiologically relevant model systems are essential for accurate tropism determination:
- Organoid cultures recapitulate the cellular complexity of human tissues, providing platforms for tropism studies that bridge the gap between conventional cell lines and in vivo models. Cerebral and ocular organoids have been used successfully to evaluate adeno-associated virus (AAV) tropism for gene therapy applications [28].
- Animal models with humanized receptor expression patterns enable assessment of tropism determinants in the context of intact physiological systems, including immune responses and tissue architecture.
- Explant cultures of human tissues maintain native cellular environments and receptor distributions, offering valuable insights into human tropism without ethical concerns of human challenge studies.
Experimental Protocols for Key Tropism Assays
Multiplexed Tropism Screening in Organoids
This protocol enables high-resolution assessment of viral tropism across complex cell populations using barcoded viral libraries and single-cell RNA sequencing:
Viral Library Preparation:
- Engineer barcoded AAV variants by introducing unique nucleotide sequences after the transgene stop codon in plasmid backbones.
- Package AAV libraries using serotype-specific capsid plasmids via triple transfection of 293AAV cell lines.
- Purify viruses by benzonase treatment to remove unpackaged nucleic acids and concentrate by ultracentrifugation [28].
Organoid Infection and Processing:
- Culture cerebral or ocular organoids from human embryonic stem cells using established differentiation protocols.
- Infect organoids with pooled AAV library at appropriate multiplicity of infection.
- After 72 hours, dissociate organoids to single-cell suspensions and prepare libraries for single-cell RNA sequencing using platform-specific protocols [28].
Data Analysis and Deconvolution:
- Process sequencing data through Cell Ranger software to simultaneously identify cell types and associated AAV barcodes.
- Visualize results in Seurat to generate matrices of AAV serotype transduction efficiency versus human cell types.
- Validate top candidates from screening in non-human primate models to confirm tropism patterns [28].
Membrane-Wide CRISPRa Screening for Host Factors
This approach identifies host membrane proteins that modulate viral entry through targeted gene activation:
CRISPRa System Establishment:
- Engineer HEK293FT cells with the synergistic activation mediator (SAM) system.
- Generate isogenic lines with (ACE2 OE) or without (WT) ACE2 overexpression to distinguish ACE2-dependent and independent factors [26].
Library Design and Screening:
- Design a customized sgRNA library targeting approximately 6,213 known membrane protein genes (~24,000 sgRNAs total including non-targeting controls).
- Transduce cells with the sgRNA library at low multiplicity to ensure single guide integration.
- Infect cells with SARS-CoV-2 Spike-pseudotyped lentiviruses encoding zeocin resistance at high and low MOI.
- Select infected cells with zeocin for 7-14 days before harvesting genomic DNA for sgRNA sequencing [26].
Hit Validation:
- Validate candidate genes through cDNA overexpression followed by infection with replication-competent SARS-CoV-2.
- Confirm functional roles through endogenous gene knockout using CRISPR/Cas9 and pharmacological inhibition studies.
- Assess tissue relevance by examining gene expression in scRNA-seq datasets from COVID-19 patients [26].
Visualization of Experimental Workflows
CRISPRa Screening for Viral Entry Factors
CRISPRa Screening for Viral Entry Factors: This workflow illustrates the process for identifying host membrane proteins that influence SARS-CoV-2 entry through targeted gene activation screens.
Multiplexed AAV Tropism Screening
Multiplexed AAV Tropism Screening: This workflow shows the process for evaluating AAV serotype tropism across complex cell populations using barcoded libraries and single-cell transcriptomics.
Research Reagent Solutions
Table 3: Essential Research Reagents for Tropism Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| CRISPR Screening Systems | Synergistic Activation Mediator (SAM) | Targeted gene activation for gain-of-function screens | Identification of host factors enhancing viral entry [26] |
| Viral Pseudotypes | SARS-CoV-2 Spike-pseudotyped lentiviruses | Safe surrogate for BSL-3 pathogens in BSL-2 settings | High-throughput screening of viral entry inhibitors [26] |
| Barcoded Viral Libraries | AAV serotype libraries with nucleotide barcodes | Multiplexed assessment of tropism across variants | Parallel evaluation of multiple viral vector candidates [28] |
| Organoid Models | Cerebral organoids, ocular organoids | Physiologically relevant human tissue models | Tropism studies in complex cellular environments [28] |
| scRNA-seq Platforms | 10X Genomics, Smart-seq2 | Single-cell transcriptome profiling with viral barcode detection | Deconvolution of tropism at single-cell resolution [28] |
Therapeutic Implications and Future Directions
Tropism-Based Therapeutic Strategies
Understanding the molecular determinants of viral tropism enables targeted therapeutic approaches that disrupt specific stages of the viral life cycle:
- Entry inhibitors that block receptor binding or membrane fusion represent promising antiviral strategies with potential for broad activity against viruses sharing receptor usage patterns. Small molecule inhibitors targeting host factors like LGMN or KCNA6 could provide alternatives to virus-directed therapeutics that are less susceptible to viral escape mutations [26].
- Viroporin inhibitors offer dual-action therapeutic potential by simultaneously suppressing viral replication and attenuating inflammation triggered by NLRP3 inflammasome activation. However, structural constraints and low immunogenicity present challenges for vaccine development targeting conserved viroporin domains [12].
- Vector-guided gene therapy leverages natural viral tropism for targeted delivery of therapeutic genes. Multiplexed AAV tropism screening enables identification of serotypes with optimal specificity for particular cell types, enhancing efficacy while reducing off-target effects [28].
Emerging Technologies and Research Frontiers
The field of tropism research is rapidly advancing through technological innovations that provide unprecedented resolution and predictive power:
- Artificial intelligence-driven structural prediction tools like AlphaFold are accelerating the characterization of viroporins and other viral proteins with tropism functions, enabling rational design of inhibitors [12].
- Single-cell multi-omics approaches combine transcriptomic, proteomic, and epigenetic data to create comprehensive maps of cellular susceptibility factors across tissues.
- Organoid-humanized models that incorporate immune cells and stromal components provide increasingly physiological systems for tropism studies that capture the complexity of host-pathogen interactions in human tissues.
- Digital pathology and spatial transcriptomics enable correlation of tropism patterns with histopathological changes in clinical specimens, bridging molecular mechanisms with disease outcomes.
These advances promise to deepen our understanding of viral pathogenesis and enable development of precisely targeted antiviral strategies that account for the complex molecular determinants of tissue-specific infection.
Viral Manipulation of Host Cell Death Pathways and Stress Responses
Viral pathogenesis is fundamentally shaped by the complex interplay between viral components and host cell death pathways. Viruses have evolved sophisticated mechanisms to manipulate regulated cell death (RCD) processes, including apoptosis, necroptosis, pyroptosis, and ferroptosis, to either facilitate viral replication or counteract host defense systems. This technical guide examines the molecular mechanisms through which viruses interface with host cell death machinery, with particular emphasis on mitochondrial permeabilization, viroporin function, and innate immune sensing pathways. The growing understanding of these interactions has revealed promising therapeutic targets, such as viroporins and specific cell death executors, for the development of novel antiviral strategies. This whitepaper provides a comprehensive framework for researchers and drug development professionals working at the intersection of viral pathogenesis and host-directed antiviral therapies, supported by current experimental data and methodological approaches.
Viruses and their hosts are engaged in a constant evolutionary arms race, wherein host organisms develop defense mechanisms to eliminate infections, and viruses counter these defenses to ensure their survival and propagation. Regulated cell death represents a critical host strategy to limit viral replication by eliminating the host cell before viral assembly and dissemination can occur. However, viruses have developed sophisticated mechanisms to manipulate these cell death pathways for their benefit [29].
The significance of understanding viral manipulation of cell death extends beyond basic pathogenesis to therapeutic development. Cell death pathways and associated damage-associated molecular patterns play contrasting roles in physiological processes during viral infections, potentially exerting either detrimental or beneficial effects [29]. Uncontrolled cell death accompanied by DAMP release can lead to excessive inflammation and tissue damage, whereas properly regulated processes help establish an immunocompetent environment by activating innate immunity. These mechanisms have consequently emerged as promising targets for developing effective antiviral therapeutics, immunotherapies, and vaccines [29].
Molecular Mechanisms of Viral Manipulation
Regulated cell death encompasses several distinct molecular pathways, each controlled by specific signal transduction mechanisms rather than the unregulated process of accidental necrosis [29]. The major RCD pathways relevant to viral infection include:
Apoptosis: A non-inflammatory RCD triggered by intrinsic or extrinsic signals, characterized by caspase activation (caspase-8/9 as initiators; caspase-3/7 as effectors), membrane blebbing, and formation of apoptotic bodies that facilitate efficient clearance by phagocytes without triggering inflammation [29].
Pyroptosis: A necrotic RCD driven by inflammasome activation and gasdermin cleavage, leading to membrane rupture and release of cellular contents, including pro-inflammatory cytokines IL-1β and IL-18 [29].
Necroptosis: An inflammatory necrotic RCD activated under apoptosis-suppressive conditions, facilitated through the RIPK1–RIPK3–MLKL axis, resulting in membrane rupture and cell lysis [29].
Ferroptosis: A distinct form of necrotic RCD occurring through iron-dependent membrane lipid peroxidation, regulated by glutathione-glutathione peroxidase 4 pathway and NADPH-ferroptosis suppressor protein 1 systems [29].
Table 1: Major Regulated Cell Death Pathways in Viral Infection
| Pathway | Key Initiators | Key Effectors | Inflammatory Profile | Role in Viral Infection |
|---|---|---|---|---|
| Apoptosis | Caspase-8/9, Death receptors | Caspase-3/7, DNA fragmentation | Non-inflammatory | Eliminates infected cells without inflammation |
| Pyroptosis | Inflammasomes, Caspase-1 | Gasdermins, IL-1β, IL-18 | Highly inflammatory | Creates antimicrobial environment, promotes inflammation |
| Necroptosis | RIPK1, RIPK3, ZBP1 | MLKL phosphorylation | Inflammatory | Back-up cell death when apoptosis is blocked |
| Ferroptosis | Iron accumulation, Lipid peroxidation | GPX4 inhibition, FSP1 system | Variable | Emerging role in viral pathogenesis |
Mitochondrial Manipulation by Viruses
Mitochondrial membrane permeabilization represents a pivotal event in cell death regulation that viruses have learned to exploit. The mitochondrial permeability transition pore in the inner mitochondrial membrane, comprising the voltage-dependent anion channel in the outer membrane and the adenine nucleotide translocator in the inner membrane, serves as a key regulatory complex for cell survival decisions [30].
The HIV-1 accessory protein Viral Protein R provides a well-characterized example of direct viral manipulation of mitochondrial integrity. Vpr specifically binds to the intermembrane face of ANT with nanomolar affinity, forming large conductance channels in planar lipid bilayers [30]. When added to isolated mitochondria, Vpr-derived peptides uncouple the respiratory chain and induce rapid inner MMP to protons and NADH, preceding outer MMP to cytochrome c. This MMP-inducing activity resides in the COOH-terminal moiety of Vpr within an α-helical motif containing several critical arginine residues strongly conserved among pathogenic HIV-1 isolates [30].
Beyond HIV, other viruses also target mitochondrial integrity. Studies have demonstrated that isolated rat liver mitochondria undergo permeability transition after supplementation with tobacco mosaic virus, evidenced by increased oxygen consumption, collapse of membrane potential, release of calcium ions, and high-amplitude mitochondrial swelling. These virus-induced mitochondrial changes were prevented by cyclosporin A, a known PTP inhibitor [31].
The significance of mitochondrial regulation in cell death extends to its potential role in aging and viral pathogenesis connections. Research in yeast models has revealed that mPTP activity affects aging processes, suggesting conserved mechanisms that viruses may exploit across different organisms [32].
Viroporins and Membrane Integrity Disruption
Viroporins represent a class of virus-encoded small hydrophobic proteins that oligomerize to form membrane-embedded pores, disrupting ion homeostasis and membrane integrity during viral infection [12]. These proteins play critical roles in multiple stages of the viral life cycle and contribute significantly to pathogenesis by triggering proinflammatory responses through NLRP3 inflammasome activation.
Table 2: Characterized Viroporins in Viral Pathogenesis
| Virus | Viroporin | Classification | Amino Acids | Ion Selectivity | Oligomeric State |
|---|---|---|---|---|---|
| Influenza A virus | M2 | IA/SP type I | 97 | H+, K+, Na+ | 4 |
| SARS-CoV-2 | E | IA/SP type I | 75 | K+, Ca2+ | 2/5 |
| Poliovirus | 2B | IIB/MP type II | 97 | Ca2+ | - |
| Ebola virus | Delta peptide | IA/SP type I | 40-49 | Cl⁻ | - |
| SARS-CoV-1 | E | IA/SP type I | 76 | K+, Ca2+ | 5 |
Viroporins are classified based on their transmembrane domains: Type I (one TMD), Type II (two TMDs), and Type III (three TMDs), with further subdivisions based on membrane orientation of N- and C-terminal domains [12]. The functional characterization of viroporin activity typically employs electrophysiological techniques such as patch-clamp and planar lipid bilayers, though these approaches carry limitations including potential abnormal protein conformations in artificial systems [12].
The influenza A virus M2 protein represents a prototypical viroporin that functions as a pH-dependent proton channel to acidify the interior of the virus, triggering nucleocapsid uncoating and independently mediating membrane scission to facilitate viral budding [12]. Similarly, coronaviruses including SARS-CoV-2 encode envelope proteins that function as viroporins with potassium and calcium selectivity, playing essential roles in virion assembly and pathogenesis [12].
Recent technological advances, including predictive algorithms such as AlphaFold, electrophysiological assays, and structural biology techniques like cryo-electron microscopy, have expanded the repertoire of identified viroporins. These include the Ebola virus delta peptide, SARS-CoV-2 E protein, human astrovirus XP protein, and African swine fever virus proteins B117L and B169L [12].
Experimental Approaches and Methodologies
Identifying Host Factors via Genomic Screening
CRISPR/Cas9 gene knockout screening has emerged as a powerful methodology for identifying host factors essential for viral replication. A recent study investigating Echovirus 30 infection employed a whole-genome CRISPR/Cas9 knockout screen in human rhabdomyosarcoma cells, revealing that knocking out ADP-ribosylation factor GTPase activating protein 1 significantly reduced E30 replication [33].
The experimental workflow involved:
- Establishing RD-Cas9 cell lines through lentiviral transduction and blasticidin selection
- Transducing with the lentiGuide-Puro Human GeCKO v2 library at MOI 0.3
- Infecting mutagenized cells with E30 at MOI 0.001
- Harvesting surviving cells after two rounds of infection
- Isolating genomic DNA and amplifying sgRNA sequences for next-generation sequencing
- Analyzing data using Model-based Analysis of Genome-wide CRISPR/Cas9 Knockout algorithm [33]
This approach identified ARFGAP1 as a crucial host factor influencing early stages of viral infection through vesicular transport mechanisms. Subsequent validation experiments demonstrated that QS11-mediated inhibition of ARFGAP1 significantly decreased viral replication in animal models, mitigated tissue damage, and enhanced survival rates [33].
CRISPR Screening for Viral Host Factors
Assessing Mitochondrial Permeabilization
The study of virus-induced permeability transition in mitochondria employs well-established biochemical and biophysical approaches. Key methodologies include:
Oxygen consumption measurements using Clark-type oxygen electrodes to detect increased respiratory activity indicative of inner membrane permeabilization [31].
Membrane potential assessment using fluorescent dyes such as JC-1 or tetramethylrhodamine ethyl ester to detect collapse of the electrochemical gradient across the inner mitochondrial membrane [31].
Calcium release assays monitoring flux of calcium ions from mitochondrial preparations using calcium-sensitive fluorescent indicators [31].
Swelling measurements detecting changes in mitochondrial volume through light scattering techniques [31].
Planar lipid bilayer experiments to characterize channel formation by viral proteins and their interactions with mitochondrial components. This technique demonstrated that Vpr52-96 and purified ANT cooperatively form large conductance channels [30].
The specificity of mitochondrial effects is typically validated using inhibitors such as cyclosporin A, which blocks permeability transition pore opening, as demonstrated in studies with tobacco mosaic virus [31]. Similarly, the role of specific mitochondrial components can be confirmed using recombinant proteins, as shown by the ability of recombinant Bcl-2 to prevent Vpr-induced matrix swelling and inner MMP by reducing the ANT-Vpr interaction [30].
Characterizing Viroporin Activity
The functional characterization of viroporin activity employs multiple complementary approaches:
Electrophysiological techniques including patch-clamp recording of whole cells or isolated membranes and planar lipid bilayer measurements to directly demonstrate ion channel activity [12].
Structural biology methods such as cryo-electron microscopy and X-ray crystallography to determine atomic-level architecture of viroporin pores, with particular attention to oligomeric states and pore dimensions [12].
Molecular dynamics simulations investigating transport mechanisms and selectivity properties through computational approaches that complement experimental findings [12].
Genetic validation through site-directed mutagenesis of key residues predicted to perturb channel gating and/or ion selectivity, providing definitive evidence for viroporin function [12].
Recent advances in viroporin characterization include the development of comprehensive checklists for identifying bona fide viroporins, requiring both structural features and functional proof of ion channel activity alongside genetic validation [12]. These criteria help resolve controversies such as that surrounding SARS-CoV-2 ORF3a, which was initially proposed as a cation-selective viroporin but later shown to function primarily as a water-permeable channel based on patch-clamp recordings and molecular dynamics simulations [12].
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Viral Manipulation of Cell Death
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| CRISPR Screening Tools | lentiCas9-Blast, lentiGuide-Puro GeCKO v2 library | Host factor identification | Genome-wide knockout screening for essential host factors |
| Cell Death Assays | Caspase activity assays, LDH release, Annexin V/PI staining, TMRE | Cell death pathway quantification | Specific detection of apoptosis, necrosis, and mitochondrial dysfunction |
| Mitochondrial Function Assays | Oxygen consumption systems, Calcium-sensitive dyes, Swelling measurements | Mitochondrial permeability assessment | Detection of mPTP opening and mitochondrial membrane potential |
| Electrophysiology Systems | Planar lipid bilayer setups, Patch-clamp systems | Viroporin characterization | Direct measurement of ion channel activity and selectivity |
| Structural Biology Tools | Cryo-EM, X-ray crystallography, AlphaFold prediction | Viroporin structure determination | Atomic-level resolution of pore architecture and oligomerization |
| Viral Infection Models | hFcRn-IFNAR−/− mice, Primary cell cultures, Organoid systems | In vivo pathogenesis studies | Physiologically relevant models of viral infection and cell death |
Signaling Pathways in Viral Cell Death Manipulation
Viral Manipulation of Host Cell Death Pathways
The diagram illustrates the complex interplay between viral components and host cell death pathways. Pattern recognition receptors including TLRs, RLRs, and cGAS detect viral nucleic acids and initiate both transcriptional responses and cell death pathways [29] [34]. The Z-DNA-binding protein 1 serves as a key innate sensor for influenza A virus and SARS-CoV-2, initiating inflammatory and cell death pathways through recognition of viral RNA or viral proteins [29].
Converging evidence indicates that PRR signaling can activate apoptosis through both transcription-dependent and independent mechanisms. The RLR-induced IRF3-mediated pathway of apoptosis represents a transcription-independent mechanism wherein linear ubiquitination of IRF3 induces its association with Bax, promoting mitochondrial translocation and cytochrome c release [34]. Similarly, cGAS/STING pathway activation during HSV-1 infection induces PARP-1 cleavage, though the specific mechanisms downstream of STING require further characterization [34].
Type I interferons, while critical for antiviral defense, can contribute to pathogenesis by promoting alveolar epithelial cell apoptosis through FADD/caspase-8-dependent mechanisms and induction of the pro-apoptotic factor TRAIL [29]. This dual role of IFN responses highlights the delicate balance between protective and pathological immune reactions to viral infection.
Therapeutic Implications and Future Directions
The mechanistic insights into viral manipulation of host cell death pathways have revealed multiple promising therapeutic targets for antiviral development. Viroporins represent particularly attractive targets due to their dual role in viral fitness and immunopathology. Their conservation across virus families and essential functions in the viral life cycle position them for targeted inhibition strategies [12].
Advanced technologies are expected to significantly accelerate the development of next-generation viroporin-targeted therapeutics. Artificial intelligence-driven structural prediction tools like AlphaFold can facilitate rapid characterization of newly identified viroporins, while nanodelivery systems may enhance targeted delivery of viroporin inhibitors [12]. Additionally, electrophysiological techniques combined with structural biology provide powerful approaches for screening and optimizing compounds that disrupt viroporin function.
Targeting specific cell death executors also holds therapeutic promise. Evidence from influenza infection models demonstrates that GSDMD deficiency reduces neutrophil activation and neutrophil extracellular trap-associated DNA release, underscoring its role in neutrophil-driven inflammation [29]. Similarly, genetic ablation of Zbp1 protected mice from IAV-induced mortality by limiting NLRP3-driven inflammation and RIPK3-mediated necroptosis and apoptosis, thereby reducing epithelial damage [29].
The mitochondrial permeability transition pore complex offers another promising target, with studies showing that cyclosporin A can prevent virus-induced mitochondrial permeability transition [31]. The conservation of these mechanisms from yeast to humans further supports their fundamental role in cell death regulation and suggests broad therapeutic potential [32].
Future research directions should focus on elucidating the precise structural basis of viral protein interactions with host cell death machinery, developing tissue-specific delivery systems for cell death-modulating therapeutics, and exploring combination therapies that target both viral replication and pathological host responses. As our understanding of these complex virus-host interactions deepens, so too will our ability to develop innovative interventions that effectively combat viral pathogens while minimizing collateral damage to host tissues.
Advanced Research Technologies: From Structural Virology to Systems Biology Approaches
Cryo-electron microscopy (cryo-EM) has emerged as a revolutionary tool in structural biology, enabling the visualization of biological macromolecules in near-native states at unprecedented resolutions. In virology, cryo-EM provides unparalleled insights into viral architecture, replication mechanisms, and host-pathogen interactions. This technical guide explores the application of cryo-EM and its complementary technique, cryo-electron tomography (cryo-ET), for elucidating the structural basis of viral pathogenesis and infection mechanisms. Recent advances in detector technology, image processing software, and sample preparation have positioned cryo-EM as an indispensable methodology for researchers aiming to understand viral assembly, entry, and maturation at molecular resolution. The ability to solve structures of complex viral machines without crystallization has transformed our approach to studying pathogens that are recalcitrant to traditional structural methods like X-ray crystallography.
The workflow encompasses multiple phases: sample vitrification, data acquisition, image processing, and 3D reconstruction, each requiring specialized expertise and tools. Single-particle analysis (SPA) allows the determination of high-resolution structures from thousands of particle images, while cryo-ET provides nanometer-resolution snapshots of viral particles in the context of host cells. This guide details the experimental protocols, validation frameworks, and analytical toolkits essential for leveraging cryo-EM to advance viral pathogenesis research and therapeutic development.
Core Principles of Cryo-EM Image Formation
Contrast Mechanisms in Cryo-EM
Understanding image formation is fundamental to interpreting cryo-EM data and optimizing experimental parameters. Unlike negative stain EM where heavy atoms deflect electrons to create strong amplitude contrast, cryo-EM of biological samples relies primarily on phase contrast [35]. Biological macromolecules are weak phase objects – they delay the electron wave (causing a phase shift) rather than absorbing or blocking electrons. Pure phase objects are invisible to detectors that only record intensity (amplitude squared) [35].
Visual contrast is generated through intentional defocusing, which converts phase variations into measurable amplitude variations at the detector. This interference-based contrast mechanism is described mathematically by the Contrast Transfer Function (CTF). The weak phase object approximation models the exit wave as the sum of an unscattered wave and a scattered wave with a uniform π/2 phase shift, simplifying the complex wave interaction for computational processing [35].
The Role of Defocus in Contrast and Resolution
Defocus introduces a frequency-dependent phase shift that enables visualization of phase objects. The relationship between defocus and contrast has important implications for experimental design:
- High defocus increases contrast for easier particle identification but dampens higher-resolution information [36]
- Low defocus preserves high-resolution information but yields lower contrast, complicating particle picking [36]
A 2024 benchmark study demonstrated that for limited datasets, higher-contrast micrographs from higher defocus values (1.52-2.71 μm) can yield superior resolution compared to lower-defocus micrographs (0.31-1.20 μm), challenging conventional methodologies that prefer lower defocus for high-resolution work [36]. This finding is particularly relevant for rapid pre-screening approaches in resource-constrained scenarios.
Technical Workflow for Viral Structure Determination
Single Particle Analysis Workflow
The cryo-EM single particle analysis workflow can be divided into four conceptual phases, each followed by a validation checkpoint [37]:
Validation Framework
Validation is crucial throughout the SPA workflow to ensure reconstructed maps accurately represent biological structure. Key validation approaches include [37]:
- Independent data sets: Processing two data sets separately and comparing results via Fourier Shell Correlation (FSC)
- Resolution-limited alignment: Restricting alignment to resolution shells with high signal-to-noise ratio
- Tilt-pair analysis: Validating orientations using micrograph pairs with known tilt differences
- Particle coherence testing: Comparing results from real particles versus noise images
The FSC curve between independently refined maps using a cutoff of 0.143 is widely adopted for resolution estimation [37]. Proper validation prevents artifacts from aligned noise, which can produce invalid yet structurally detailed reconstructions.
Case Study: Mycobacteriophage Douge Architecture and Infection
Structural Organization
A 2025 study of mycobacteriophage Douge exemplifies the power of integrated cryo-EM and cryo-ET approaches. The complete structure, solved at atomic resolution, reveals several key organizational features [38] [39]:
Table 1: Structural Components of Mycobacteriophage Douge
| Component | Subunit Count | Architectural Features | Functional Role |
|---|---|---|---|
| Capsid | 1,105 protein subunits | Icosahedral symmetry | Genome packaging and protection |
| Portal-adaptor subcomplex | Multiple subunits | Asymmetric interface with capsid vertex | Genome gatekeeping and ejection |
| Tail machinery | Tape measure proteins | Channel spanning connector to baseplate | Genome delivery system |
| Baseplate | Glycan-binding domains | Receptor recognition apparatus | Host attachment and membrane interaction |
The structure reveals an asymmetric interface between the capsid-vertex and portal-adaptor subcomplex, deviating from perfect icosahedral symmetry and likely critical for genome gating and ejection control [39].
Host Interaction Mechanism
Cryo-ET snapshots of Douge infecting Mycobacterium smegmatis captured distinct stages of the viral life cycle, providing unprecedented insights into infection mechanics [38] [39]:
- Attachment: Glycan-binding domains in the baseplate specifically recognize mycobacterial cell surface lipoarabinomannan/arabinomannan
- Genome ejection: The tape measure proteins seal the channel spanning the connector, tail, and baseplate, creating a genome gating system
- Membrane association: The baseplate remains attached to the mycobacterial outer membrane during viral genome ejection
- Structural dynamics: Limited structural changes are required for genome ejection, indicating an efficient infection mechanism
These findings provide a structural foundation for engineering mycobacteriophages with enhanced therapeutic efficacy against non-tuberculosis mycobacterial diseases [39].
Specialized Toolkits for Membrane-Virus Analysis
CryoVIA for Membrane Quantification
The cryo-vesicle image analyzer (CryoVIA) toolkit enables automated parametrization of lipid structures from cryo-EM images, particularly relevant for studying enveloped viruses and host membrane interactions [40] [41]. This software combines segmentation and structure identification with methods for large-scale analysis of membrane properties:
Table 2: CryoVIA Analysis Capabilities for Membrane Structures
| Analysis Type | Measured Parameters | Application in Virology |
|---|---|---|
| Global membrane properties | Size, curvature, shape classification | Viral envelope morphology, budding stages |
| Local membrane properties | Bilayer thickness, local curvature | Host membrane remodeling during entry/exit |
| Shape classification | Vesicle shapes, membrane deformations | Virus-induced membrane curvature |
| Protein-induced changes | Membrane remodeling metrics | Viral protein action on host membranes |
The toolkit has been applied to study membrane remodeling by ESCRT-III complexes, which are hijacked by many viruses for budding and exit [41]. This enables systematic quantification of structural modifications in host membranes induced by viral infection.
Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Viral Cryo-EM
| Reagent/Tool | Function/Application | Implementation Example |
|---|---|---|
| Bsoft Software Package | Single particle analysis and tomography workflow | Processing of mycobacteriophage Douge data [37] |
| CryoSPARC | Automated processing, motion correction, CTF estimation | Beta-galactosidase, apo-ferritin, connexin processing [36] |
| CryoVIA Toolkit | Membrane structure segmentation and quantification | Analysis of ESCRT-III-induced membrane remodeling [41] |
| Direct Electron Detectors | High-resolution data acquisition | Recording dose-fractionated micrographs [37] |
| Phase Plates | Enhanced contrast without defocus | Imaging of small viral proteins with low contrast |
| Vitrification Systems | Sample preservation in vitreous ice | Preparation of mycobacteriophage-host interaction samples |
Experimental Protocols for Viral Cryo-EM
Sample Preparation and Data Collection
Optimal sample preparation is critical for successful viral structure determination:
Protocol 1: Vitrification of Virus-Host Complexes
- Purify viral particles via density gradient centrifugation
- For host interactions, mix virus with host cells/receptors at appropriate multiplicity of infection
- Apply 3-4 μL sample to glow-discharged cryo-EM grids
- Blot and plunge-freeze in liquid ethane using Vitrobot system
- Assess ice quality using screening microscope
Protocol 2: Data Collection Strategy Optimization
- Collect micrographs at multiple defocus ranges (0.5-3.0 μm) to balance contrast and resolution
- Use dose-fractionation mode on direct electron detectors
- Implement 20-40 frame movies with total dose of 30-50 e-/Ų
- For tilt-pair validation, collect image pairs at 0° and 10-15° tilt [37]
Image Processing and Reconstruction
Protocol 3: Single Particle Analysis for Viral Structures
- Perform motion correction using patch-based alignment (e.g., cryoSPARC, RELION)
- Estimate CTF parameters (CTFFIND4) [36]
- Pick particles using reference-based or AI-enabled methods
- Extract particles and conduct reference-free 2D classification
- Generate initial model using stochastic gradient descent or ab initio reconstruction
- Refine with imposed symmetry (icosahedral for most viruses)
- Validate using independent datasets and FSC analysis [37]
Protocol 4: Cryo-ET of Virus-Host Interactions
- Acquire tilt series from -60° to +60° with 2-3° increments
- Align tilt series using fiducial markers or patch tracking
- Reconstruct tomograms via weighted back-projection or SIRT methods
- Segment sub-tomogram averages for repetitive structures
- Correlate with SPA structures for integrated modeling
Cryo-EM and cryo-ET have revolutionized our ability to visualize viral architecture and host interactions at molecular resolution. The integrated approach combining single particle analysis with tomography provides a comprehensive structural framework for understanding viral pathogenesis. As exemplified by the mycobacteriophage Douge study, these techniques can reveal atomic details of complete virions while capturing dynamic infection processes in native contexts. Continued developments in detector technology, processing software, and specialized toolkits like CryoVIA for membrane analysis will further expand applications in virology. The methodologies and validation frameworks outlined in this guide provide researchers with a roadmap for leveraging cryo-EM to advance therapeutic development through structure-guided drug design and phage engineering.
The study of viral pathogenesis has historically relied on bulk analysis techniques, which provide population-averaged data that mask the inherent heterogeneity of individual cells within a host. Single-cell omics technologies represent a paradigm shift, enabling unprecedented resolution to dissect cell-to-cell variation, rare cell populations, and complex cellular dynamics during viral infection. These advanced methodologies are transforming our understanding of host-virus interactions by revealing how identical genetic viruses can produce disparate infection outcomes in different cells, and how cell-specific host factors determine viral tropism, replication efficiency, and immune evasion strategies. Within the broader thesis of viral pathogenesis and infection mechanisms research, single-cell approaches provide the necessary granularity to move beyond simplistic models of infection toward a sophisticated understanding of the cellular ecosystem in which viruses operate.
The application of these technologies has proven particularly valuable for elucidating the pathogenesis of significant human viruses, including SARS-CoV-2, HIV-1, and influenza, by identifying distinct cellular states and subpopulations that correlate with disease severity and progression [42] [43]. For researchers and drug development professionals, these insights are accelerating the identification of novel therapeutic targets and informing vaccine design strategies that account for, and potentially manipulate, this cellular heterogeneity [44].
Key Technological Platforms in Single-Cell Omics
Core Methodologies and Their Applications
Single-cell omics encompasses a suite of complementary technologies that each probe a different layer of cellular machinery. Table 1 summarizes the primary single-cell modalities, their applications in viral research, and their key technical specifications.
Table 1: Key Single-Cell Omics Technologies in Virology Research
| Technology | Biological Insights | Application in Virology | Throughput & Multiplexity |
|---|---|---|---|
| scRNA-seq [45] [44] | Transcript diversity and abundance | Identify infected vs. bystander cell states; characterize host response heterogeneity; simultaneously detect host and viral RNA [43]. | ~100–100,000 cells/experiment; 1,000–14,000 genes/cell [44]. |
| scATAC-seq [45] [44] | Chromatin accessibility landscape | Identify infection-induced epigenetic alterations; characterize regulatory elements controlling immune responses [44]. | ~100–100,000 cells/experiment; ~2,500–73,000 reads/cell [44]. |
| CITE-seq/REAP-seq [45] | Surface protein expression alongside transcriptome | Profile protein abundances and post-translational modifications in immune cells; deep immunophenotyping. | Limited by antibody panel size (dozens of proteins). |
| scVDJ-seq [44] | B- and T-cell receptor clonotype diversity | Characterize antigen-specific B/T-cell receptor sequences; track lymphocyte lineage and differentiation. | Varies by platform. |
| Spatially Resolved Transcriptomics (SRT) [45] | Genome-wide expression with retained tissue position | Map spatial architecture of viral replication foci and localized immune responses in complex tissues. | Resolution: 55 μm (Visium) to subcellular (Stereo-seq); genome-wide coverage. |
| CyTOF/IMC [44] | High-parameter protein expression | Characterize >30 protein markers on immune cells; track immune infiltration and tissue remodeling in infected tissues. | 30-40+ protein markers; ~1000-2000 cells/s (CyTOF) [44]. |
Integrated Multi-Omics Workflows
The most powerful insights often come from integrating multiple omics modalities from the same cell. For instance, combining scRNA-seq with scATAC-seq allows researchers to evaluate the link between transcription factor binding (inferred from chromatin accessibility) and the expression of their target genes, providing a more mechanistic understanding of how viral infection rewires host cell gene regulatory networks [45]. Similarly, technologies like the BD Rhapsody system enable the parallel capture of mRNA expression, protein expression, and immune repertoire from thousands of single cells, offering a comprehensive view of the immune state [45]. These integrated workflows are particularly valuable for connecting viral-induced epigenetic changes to functional cellular outcomes.
Experimental Protocols for Key Applications
Protocol 1: scRNA-seq of Virus-Infected Primary Epithelia
This protocol outlines the steps for analyzing the host transcriptional response and viral tropism in primary human bronchial epithelial cells (HBECs) infected with SARS-CoV-2, as performed by [43].
- Cell Culture and Infection: Differentiate primary HBECs at an air-liquid interface (ALI) for 28 days to mimic the respiratory epithelium. Challenge the apical surface with SARS-CoV-2 (e.g., 10^4 PFU of strain USA-WA1/2020).
- Sample Collection and Single-Cell Suspension: At designated time points (e.g., 1, 2, 3 days post-infection), generate a single-cell suspension from the infected and mock-treated control epithelia.
- Single-Cell Library Preparation: Perform 3' scRNA-seq using a platform such as 10x Genomics Chromium. This involves cell barcoding, reverse transcription, cDNA amplification, and library construction.
- Sequencing and Primary Data Processing: Sequence the libraries on an Illumina platform. Then, align the sequenced reads to a combined reference genome (e.g., human GRCh38 and SARS-CoV-2 genome).
- Cell and Viral RNA Quantification: For each cell, quantify the number of transcripts from each host gene and viral open reading frame (ORF). Define productively infected cells using a threshold (e.g., ≥10 viral transcripts/cell) to control for background.
- Bioinformatic Analysis:
- Perform dimensionality reduction (e.g., UMAP) and clustering to identify cell types and states.
- Cell Type Annotation: Identify ciliated, basal, and club cells using known marker genes.
- Differential Expression: Compare gene expression between infected cells, uninfected (bystander) cells from the same sample, and cells from mock-treated controls. Use tools like Seurat.
- Viral Transcript Analysis: Characterize the abundance and distribution of viral subgenomic RNAs.
Protocol 2: Single-Cell Multi-Omic Profiling of Immune Cells
This protocol, based on studies of HIV-infected patients, details how to profile immune heterogeneity in peripheral blood mononuclear cells (PBMCs) using a multi-omics approach [46].
- Patient Cohort and Sample Selection: Define clinical cohorts (e.g., for HIV: Immunological Non-Responders (INRs), Immune Responders (IRs), and Healthy Controls (HCs)). Collect PBMCs via density gradient centrifugation.
- Multi-Modal Single-Cell Library Preparation: Use a commercial platform like 10x Genomics Multiome kit to simultaneously generate libraries for scRNA-seq and scATAC-seq from the same single cell.
- Immune Repertoire Profiling: In parallel, perform single-cell V(D)J sequencing (scVDJ-seq) on a separate aliquot of PBMCs to obtain paired full-length sequences of B-cell (BCR) or T-cell (TCR) receptors.
- Sequencing and Data Integration: Sequence all libraries and use cell barcodes to link the transcriptome, chromatin accessibility, and (if available) immune receptor data for each cell.
- Advanced Computational Analysis:
- Cell Type Identification: Jointly cluster cells based on integrated RNA and ATAC data to define major and rare immune cell subsets.
- Differential Analysis: Employ specialized tools like scGeneANOVA to identify genes and pathways that differ between cohorts, accounting for complex experimental designs.
- Viral Transcript Detection: Use a specialized tool like VILDA to identify and quantify low-abundance HIV-1 transcripts in infected cells and correlate their presence with host cell pathways (e.g., interferon signaling).
- Clonotype Analysis: Integrate VDJ data with transcriptomic data to link specific T-cell or B-cell clonotypes to functional states.
Application in Viral Pathogenesis: Key Findings
Dissecting the SARS-CoV-2 Host Response
Single-cell omics have been instrumental in deconstructing the complex and non-linear host response to SARS-CoV-2 infection. A pseudotime analysis of scRNA-seq data from infected HBECs and intestinal organoids revealed a highly correlated triphasic transcriptional response across most host genes [42]. This pattern consists of an initial down-regulation phase at low viral loads, an intermediate up-regulatory phase, and a final shutdown phase at high viral accumulation. This wave-like dynamic, which would be obscured in bulk data, suggests a common global mechanism, potentially driven by viral protein nsp1-mediated nuclear export inhibition, that regulates most mRNA levels during infection [42].
Furthermore, these studies have precisely defined viral cellular tropism, identifying ciliated cells as the primary initial target in the airway epithelium, with tropism later expanding to include basal and club cells as infection progresses [43]. scRNA-seq also enables the distinction between cell-intrinsic defense responses and bystander effects. Infected cells show a distinct profile, including the expression of specific interferon-stimulated genes (ISGs) and pro-inflammatory cytokines like IL-6, while neighboring bystander cells also exhibit ISG activation, indicating paracrine signaling [43]. Table 2 quantifies the transcriptional dynamics observed in one such study.
Table 2: Triphasic Transcriptional Response to SARS-CoV-2 in Different Host Cells [42]
| Cell Type / Parameter | Human Bronchial Epithelial Cells (hBECs) | Colon Organoids | Ileum Organoids |
|---|---|---|---|
| Early Phase: Genes Downregulated | 99.5% | 98.7% | 98.0% |
| Intermediate Phase: Max Fold Change | 1.4 - 4.1 | Up to 2.3 | Up to 4.7 |
| Late Phase: Transition Pseudotime | 6.2 (~72.5 TPT) | 11.4 (~2,701.3 TPT) | 12.7 (~6,653 TPT) |
| Mitochondrial & Translation Genes | Distinct profile from average | Distinct profile from average | Distinct profile from average |
Elucidating Mechanisms of HIV Persistence and Immune Dysfunction
In HIV research, single-cell multi-omics has uncovered the immune heterogeneity underlying incomplete immune reconstitution in a subset of patients on antiretroviral therapy, known as Immunological Non-Responders (INRs). A study combining scRNA-seq and scVDJ-seq revealed that INRs exhibit a dysregulated interferon (IFN) response that is closely associated with CD4+ T cell exhaustion and failure to recover normal CD4 counts [46]. The development of novel analytical tools like VILDA allowed researchers to quantify HIV-1 transcripts at the single-cell level and demonstrate that higher residual viral transcription in INRs may be driving this heightened and potentially pathological IFN response [46]. This provides a new mechanistic understanding and potential therapeutic targets for this vulnerable population.
Informing Rational Vaccine Design
Single-cell technologies are critically informing vaccine development by enabling a high-resolution view of the B and T cell responses to infection and vaccination. For example, single-cell immune profiling of B cells from unexposed individuals revealed that the SARS-CoV-2 spike protein preferentially activates B cells expressing the IGHV1-69/IGKV3-11 B cell receptor, which produces non-neutralizing antibodies [47]. This finding suggests that vaccine efficacy could be improved by engineering stabilized spike protein variants that avoid eliciting this dominant but non-neutralizing response and instead focus the immune response on generating broadly neutralizing antibodies [47]. This is a prime example of how understanding cellular-level heterogeneity can guide rational antigen design.
Essential Research Reagents and Tools
Successful single-cell omics studies rely on a curated set of reagents and computational tools. The table below lists key solutions for a virology-focused workflow.
Table 3: Research Reagent Solutions for Single-Cell Virology
| Reagent / Solution | Function | Example Use Case |
|---|---|---|
| 10x Genomics Chromium [43] [47] | Microfluidic platform for high-throughput single-cell partitioning and barcoding. | Generating single-cell libraries for transcriptomics, immune profiling, and multi-omics from tens of thousands of cells. |
| BD Rhapsody System [45] [44] | Microwell-based platform for capturing single cells and profiling mRNA, protein, and immune repertoire. | Multimodal analysis of immune cells in vaccine studies. |
| Feature Barcoding Kits [47] | Allows simultaneous quantification of surface proteins alongside the transcriptome using antibody-derived tags. | Deep immunophenotyping of PBMCs from infected or vaccinated individuals. |
| VILDA Computational Tool [46] | A bioinformatic tool for Viral Identification and Load Detection Analysis in scRNA-seq data. | Quantifying HIV-1 transcript burden in individual immune cells and correlating it with host pathways. |
| scGeneANOVA Tool [46] | A novel mixed-model differential gene expression analysis tool for complex single-cell study designs. | Identifying subtle, yet statistically significant, transcriptomic differences between patient cohorts (e.g., INRs vs. IRs). |
| Stabilized Spike Protein (S-2P) [47] | An engineered, conformation-stable version of the SARS-CoV-2 spike antigen. | Used as a probe to isolate spike-reactive B cells via flow cytometry prior to scRNA-seq. |
Visualizing Experimental Workflows and Host Response
The following diagrams illustrate a generalized single-cell multi-omics workflow and the core host response to intracellular viral infection, integrating the key concepts discussed.
Single-Cell Multi-Omics Workflow
Core Host Antiviral Response at Single-Cell Resolution
The study of viral pathogenesis has been revolutionized by the advent of CRISPR-Cas9 genome-editing technology, which enables systematic identification of host factors essential for viral infection. Viruses are obligate intracellular parasites that depend heavily on cellular machinery for their replication and dissemination. Host factors comprise proteins and cellular pathways that viruses exploit (pro-viral factors) or that restrict viral infection (anti-viral factors). Understanding these interactions is critical for elucidating infection mechanisms and developing novel therapeutic strategies. CRISPR screening has emerged as a powerful forward genetic approach that allows genome-wide interrogation of gene function at unprecedented scale and resolution, moving beyond traditional methods like RNA interference (RNAi) that often suffered from incomplete knockdown and off-target effects [48] [49].
The application of CRISPR screening to virology has accelerated dramatically in recent years, particularly during the SARS-CoV-2 pandemic, where it was deployed to rapidly identify host dependency factors for this novel pathogen [48] [49]. This technical guide comprehensively outlines the principles, methodologies, and applications of CRISPR screening platforms for genome-wide identification of host factors in viral pathogenesis research, providing researchers with both theoretical foundations and practical implementation frameworks.
Core Principles of CRISPR Screening Technology
Molecular Foundations of CRISPR-Cas Systems
CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) and CRISPR-associated (Cas) proteins constitute an adaptive immune system in prokaryotes that has been repurposed for precise genome editing in eukaryotic cells. The most widely utilized system for genetic screening is the Class 2 Type II CRISPR-Cas9 system from Streptococcus pyogenes. The core components include the Cas9 endonuclease and a single-guide RNA (sgRNA) that directs Cas9 to specific genomic loci complementary to a 17-20 bp spacer sequence. Cas9 cleavage occurs adjacent to a Protospacer Adjacent Motif (PAM, 5'-NGG for S. pyogenes Cas9), generating double-strand breaks (DSBs) that are repaired by error-prone non-homologous end joining (NHEJ), often resulting in frameshift mutations and gene knockouts [49].
Several Cas protein variants with distinct properties have been harnessed for screening applications. Cas12 (Type V) systems utilize a different PAM (5'-TTTN) and generate staggered DNA cuts, while Cas13 (Type VI) targets RNA substrates and has been adapted for diagnostic applications and transcript knockdown [49]. Each system offers unique advantages for specific screening contexts.
Comparative Advantages Over Alternative Technologies
CRISPR knockout (CRISPRn) screens offer significant advantages over previous functional genomic technologies. Compared to RNAi screening, which achieves partial gene knockdown, CRISPRn typically generates complete gene knockouts, enabling more robust phenotype detection [50]. A systematic comparison demonstrated that CRISPR and RNAi screens identify distinct biological processes due to their fundamental mechanistic differences [50]. While RNAi screens effectively identify genes where partial knockdown produces phenotypes, CRISPRn excels at detecting genes requiring complete ablation for phenotypic consequences. The combination of both technologies can provide complementary information and improve confidence in hit identification [50].
Experimental Design and Workflow
Library Design Considerations
The foundation of a successful CRISPR screen lies in careful sgRNA library design. Multiple genome-wide libraries have been developed, with varying sgRNA designs and numbers:
Table 1: Comparison of Genome-Wide CRISPR Knockout Libraries
| Library Name | sgRNAs per Gene | Total Guides | Key Features | Reference |
|---|---|---|---|---|
| Brunello | 4 | 76,441 | Optimized for on-target efficiency, minimized off-target effects | [51] |
| Yusa v3 | 6 | ~114,000 | Balanced coverage with multiple guides per gene | [52] |
| Vienna (top3-VBC) | 3 | ~57,000 | Selected using VBC scores for maximal efficiency | [52] |
| Croatan | 10 | ~190,000 | High guides per gene for enhanced coverage | [52] |
Recent benchmarking studies demonstrate that libraries with fewer guides per gene (3-4) perform as well or better than larger libraries when guides are selected using principled criteria like Vienna Bioactivity CRISPR (VBC) scores, which predict sgRNA efficacy [52]. Dual-targeting libraries, where two sgRNAs targeting the same gene are delivered together, can enhance knockout efficiency but may induce greater DNA damage response [52].
Domain-focused libraries represent a strategic alternative to whole-gene targeting. By concentrating sgRNAs on exons encoding critical protein domains, researchers can generate a higher proportion of null mutations and identify functionally important regions. This approach proved particularly valuable in cancer dependency screens, where targeting essential domains (e.g., bromodomains in BRD4) produced stronger phenotypes than targeting 5' exons [53].
Core Screening Methodologies
Table 2: Primary CRISPR Screening Modalities in Virology
| Screening Type | Mechanism | Application in Virology | Key Considerations |
|---|---|---|---|
| CRISPR Knockout (CRISPRn) | NHEJ-mediated indel formation causes gene knockouts | Identification of essential host factors | May miss essential genes where complete knockout is lethal |
| CRISPR Activation (CRISPRa) | dCas9 fused to transcriptional activators (e.g., VP64) upregulates gene expression | Identification of antiviral restriction factors | Requires specialized sgRNA designs for promoter targeting |
| CRISPR Inhibition (CRISPRi) | dCas9 fused to repressors (e.g., KRAB) downregulates gene expression | Alternative to knockout with reversible effects | Enables study of essential genes without lethal knockout |
Implementation Workflow
The following diagram illustrates the core workflow for a genome-wide CRISPR knockout screen to identify host factors in viral infection:
A typical genome-wide CRISPR screen begins with the design or selection of an appropriate sgRNA library. Lentiviral vectors are then produced for delivery of sgRNA libraries into Cas9-expressing cells at low multiplicity of infection (MOI ~0.3) to ensure most cells receive a single sgRNA. Transduced cells are selected (typically with puromycin) and expanded to achieve sufficient coverage (500-1000 cells per sgRNA recommended). The pooled cell population is then infected with the virus of interest, followed by phenotypic selection. For survival-based screens, cells resistant to viral-induced cytopathy are collected. Alternatively, fluorescence-activated cell sorting (FACS) can isolate populations based on infection status using reporter viruses [54]. Genomic DNA is extracted from selected populations and control populations, followed by PCR amplification of sgRNA sequences and next-generation sequencing. Bioinformatic analysis identifies sgRNAs significantly enriched or depleted in selected populations compared to controls, pointing to candidate host factors [51].
Key Applications in Viral Pathogenesis
SARS-CoV-2 Host Factor Discovery
The COVID-19 pandemic prompted extensive CRISPR screening efforts to identify host factors required for SARS-CoV-2 infection. Genome-wide knockout screens revealed critical host pathways, including endosomal trafficking, receptor signaling, and metabolic processes [48] [49]. These discoveries provided immediate therapeutic insights, such as highlighting the importance of the fatty acid metabolism pathway, whose inhibition with available drugs reduced SARS-CoV-2 infection in model systems [55]. The rapid application of CRISPR screening during the pandemic demonstrated its power in responding to emerging viral threats.
Flavivirus and Rotavirus Host Dependencies
CRISPR screens have identified host factors for numerous flaviviruses, including dengue, Zika, and yellow fever viruses. These studies revealed both common and virus-specific dependencies, particularly in endocytic pathways and membrane trafficking machinery [48]. Similarly, a FACS-based CRISPR screen for rotavirus host factors identified novel anti-rotavirus genes including SERPINB1 and TMEM236. Knockout of these genes enhanced rotavirus infectivity across multiple strains, and their high expression in the small intestine suggested potential roles in natural infection [54]. These discoveries facilitated the development of optimized rotavirus reverse genetics systems and vaccine production platforms using SERPINB1-knockout cells [54].
HIV and Other Viral Pathogens
CRISPR screens have provided insights into retroviral pathogenesis, particularly HIV. A genome-wide screen in primary CD4+ T cells identified host dependency factors for HIV infection, revealing novel aspects of viral entry and integration [55]. The identification of these factors has inspired novel therapeutic approaches, including the development of EBT-101, a CRISPR-based therapy currently in clinical trials that aims to excise integrated HIV provirus from infected cells [55].
Advanced Screening Platforms and Applications
CRISPR-StAR for Complex Models
Conventional CRISPR screens face limitations in complex models like in vivo systems due to bottleneck effects during engraftment and heterogeneous cell growth. CRISPR-StAR (Stochastic Activation by Recombination) addresses these challenges by incorporating internal controls through Cre-inducible sgRNA expression and single-cell barcoding [56]. This method activates sgRNAs in only half the progeny of each cell after re-expansion of cell clones, generating intrinsic controls that account for heterogeneity and genetic drift. In vivo benchmarking demonstrated CRISPR-StAR's superior accuracy in hit calling compared to conventional screening, enabling identification of in-vivo-specific genetic dependencies in melanoma models [56].
Specialized Applications
CRISPR activation (CRISPRa) screens have proven valuable for identifying antiviral restriction factors. For example, a CRISPRa screen for SARS-CoV-2 host factors revealed novel interferon-stimulated genes with antiviral activity [49]. Dual-targeting libraries, where two sgRNAs target the same gene, can enhance knockout efficiency but may trigger DNA damage response, requiring careful experimental design [52].
Practical Implementation Guide
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR Screening
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Genome-wide sgRNA Libraries | Brunello, Yusa v3, Vienna | Target all human genes with multiple sgRNAs per gene for comprehensive coverage |
| Cas9 Cell Lines | MA104-Cas9, Vero-Cas9 | Stably express Cas9 nuclease for efficient genome editing |
| Viral Vectors | Lentiviral sgRNA delivery | Enable efficient sgRNA delivery to cell populations |
| Selection Agents | Puromycin, Blasticidin | Select for successfully transduced cells |
| NGS Library Prep Kits | Guide-it CRISPR NGS Analysis Kit | Amplify and sequence sgRNA inserts from genomic DNA |
| Bioinformatics Tools | MAGeCK, RIGER, Chronos | Analyze sequencing data to identify significantly enriched/depleted sgRNAs |
Critical Technical Considerations
Cell line selection is paramount for virology screens. The cell line must be susceptible to the virus of interest and capable of efficient CRISPR editing. For rotavirus research, MA104 cells are commonly used [54], while Vero E6 cells are preferred for SARS-CoV-2 studies [48]. Cas9 expression optimization requires careful titration to achieve efficient editing while minimizing toxicity. Clonal Cas9-expressing lines often provide more consistent performance than heterogeneous populations [54].
Screen validation should include both positive and negative controls. Essential genes (e.g., ribosomal proteins) serve as positive controls for depletion, while non-essential genes (e.g., non-expressed genes) confirm specificity [53]. Hit validation requires individual sgRNA testing and rescue experiments with cDNA constructs to confirm phenotype specificity [53] [54].
CRISPR screening platforms have fundamentally transformed our approach to identifying host factors in viral pathogenesis. The technology's precision, scalability, and flexibility have enabled systematic mapping of virus-host interactions across diverse viral families. As screening methodologies continue to evolve—with improvements in library design, complex model compatibility, and multi-modal perturbations—CRISPR screens will remain indispensable for uncovering novel biology and revealing therapeutic vulnerabilities in viral infection pathways. The integration of these powerful functional genomic tools with traditional virological methods promises to accelerate both fundamental discoveries and translational applications in infectious disease research.
Animal models are indispensable tools for deciphering the complex mechanisms of viral pathogenesis and developing effective countermeasures against emerging infectious threats. Within this landscape, two advanced model systems have proven particularly transformative: the ferret model for respiratory virus transmission studies and humanized mouse models for investigating human-specific immune responses. These systems bridge the critical gap between in vitro studies and clinical research, providing physiologically relevant platforms for studying infection dynamics, host-pathogen interactions, and therapeutic efficacy. The ferret model uniquely recapitulates human-like clinical disease and transmission patterns for respiratory viruses such as influenza, while humanized mice enable the study of human immune cell functions, viral tropism, and antiviral therapies in an in vivo setting. This technical guide examines the foundational principles, methodological approaches, and applications of these advanced animal models within the broader context of viral pathogenesis and infection mechanism research, providing researchers with the comprehensive knowledge needed to select and implement appropriate models for their specific investigative goals.
Ferret Models in Respiratory Virus Research
Physiological and Immunological Basis
The ferret (Mustela putorius furo) has emerged as a superior model for studying respiratory viral pathogenesis, particularly for influenza and paramyxoviruses, due to its striking physiological and immunological similarities to humans. Several key anatomical and molecular features underpin this relevance. Ferrets and humans share comparable lung physiology and cellular receptor distribution, including the predominant presence of α-2,6-linked sialic acid receptors in the respiratory tract that mediate influenza virus attachment and entry [57] [58]. This receptor distribution pattern enables human influenza virus isolates to infect ferrets without prior adaptation, a significant advantage over other small animal models. Additionally, ferrets develop clinical signs similar to those observed in human infections, including fever, lethargy, sneezing, coughing, and nasal discharge, providing clinically relevant endpoints for assessing viral virulence and pathogenicity [57]. Their susceptibility to infection via multiple routes, including ocular inoculation, further enhances their utility for studying natural infection mechanisms [57].
Experimental Design and Methodological Considerations
Ferret transmission studies employ carefully controlled experimental designs to assess viral spread between infected and naïve animals. The two primary experimental setups are:
- Direct Contact Model: An influenza virus-infected ferret is co-housed with an uninfected ferret, allowing transmission through any route, including direct contact, indirect contact via fomites, or respiratory droplets [58].
- Respiratory Droplet/Airborne Transmission Model: A virus-infected ferret is physically separated from an uninfected ferret in an adjacent cage, permitting air exchange but preventing direct or indirect contact. In this design, transmission can only occur via respiratory droplets and droplet nuclei expelled from the infected donor [58].
Critical experimental parameters that significantly influence transmission outcomes and require careful standardization include viral inoculation dose and route, donor-to-recipient ratio, cage design and airflow dynamics, environmental conditions (temperature and humidity), and ferret-specific factors such as age, sex, and immune status [58]. A consensus is emerging that a 1:1 donor:recipient ratio is ideal for risk assessment studies, as it facilitates clearer interpretation of results and adds statistical rigor by ensuring that any detected transmission event originates from exposure to a separate donor [58].
The following workflow diagram illustrates a standardized protocol for a ferret respiratory transmission study:
Key Research Applications and Insights
Ferret models have yielded critical insights into the determinants of viral transmission and pathogenesis. They have been instrumental in identifying molecular correlates of airborne transmission for influenza viruses, including polymerase complex efficiency, hemagglutinin receptor binding preference and stability, and neuraminidase activity [58]. Additionally, the model has enabled comparative studies of innate host responses between viruses with distinct transmission phenotypes, revealing potential immune correlates of transmissibility [58]. Beyond basic research, ferrets serve as a vital platform for pandemic risk assessment of emerging influenza viruses through standardized tools like the Influenza Risk Assessment Tool (IRAT) and the World Health Organization Tool for Influenza Pandemic Risk Assessment [58]. The model also provides an invaluable system for evaluating the efficacy of novel antiviral drugs and vaccines in reducing viral shedding and preventing transmission between hosts [57].
Table 1: Key Experimental Variables in Ferret Transmission Studies
| Variable Category | Specific Parameters | Impact on Experimental Outcomes |
|---|---|---|
| Virus-Specific | Inoculation dose, virus passage history, storage conditions | Affects infectivity, replication efficiency, and transmission potential [58] |
| Host-Specific | Ferret age, sex, supplier, pre-existing immunity | Influences susceptibility to infection and disease severity [58] |
| Environmental/Laboratory | Cage design, airflow direction, air changes/hour, temperature, humidity | Modulates respiratory droplet dispersion and virus stability [58] |
| Experimental Design | Donor:recipient ratio, inoculation route, sampling frequency | Affects statistical power, detection sensitivity, and interpretation of transmission events [58] |
Humanized Mouse Models for Human Immunity Studies
Foundation and Engineering Strategies
Humanized mice are advanced preclinical models that contain functioning human genes, cells, tissues, or microbiota, enabling more accurate modeling of human-specific biological processes, particularly immune responses to viral pathogens. These models are created through three primary approaches, each with distinct advantages and applications. The first method involves human immune system engraftment into immunodeficient hosts, using mouse strains such as the NOD-scid IL2rγnull (NSG) or CIEA NOG mouse that lack mature T, B, and NK cells and have compromised innate immunity [59] [60]. The second approach utilizes genetic engineering to create humanized genetically engineered models (GEMs) by inserting human genes (via transgenesis or targeted knock-in) into the mouse genome, enabling the study of specific human drug targets or pathways [60]. The third strategy involves human microbiome transfer through fecal microbiota transplantation from human donors into germ-free mice, establishing a human-derived gut microbiome that influences immune development and function [60].
The creation of human immune system-engrafted mice typically follows two main protocols with distinct characteristics and applications:
- hu-SRC-SCID Model (HSC Engraftment): Immunodeficient mice are engrafted with human hematopoietic stem cells (HSCs) isolated from umbilical cord blood, bone marrow, or G-CSF-mobilized peripheral blood [59]. These HSCs home to the mouse bone marrow and differentiate over 12-16 weeks into a diverse repertoire of human immune cells, including T cells, B cells, natural killer cells, and myeloid cells [60]. A key advantage of this model is that the developing human T and B cells undergo education in the mouse thymic microenvironment, resulting in a immune system that is tolerant of both the mouse host and the newly developing human cells [59].
- hu-PBL-SCID Model (PBMC Engraftment): Immunodeficient mice are engrafted with mature human peripheral blood mononuclear cells (PBMCs) from adult donors [59]. This approach rapidly generates a functional human immune system within weeks, making it suitable for short-term studies. However, a significant limitation is the rapid onset of graft-versus-host disease (GvHD) mediated by the mature human T cells attacking mouse tissues, typically limiting the experimental window to approximately 4-6 weeks [59] [60].
The following diagram illustrates the two primary methods for creating humanized mice via immune system engraftment:
Applications in Viral Pathogenesis and Therapeutic Development
Humanized mouse models have revolutionized the study of human-specific viral infections and therapeutic development. In human immunodeficiency virus (HIV) research, these models support robust HIV infection and replication, enabling studies of viral pathogenesis, reservoir establishment, and evaluation of antiretroviral therapies and cure strategies [59]. In oncology and immuno-oncology, humanized mice are used to study virus-associated cancers (e.g., EBV-associated lymphomas) and to evaluate immunotherapies, including checkpoint inhibitors and CAR-T cells, against human tumors in vivo [60]. For influenza and other respiratory viruses, humanized models permit the investigation of human immune responses to infection and the evaluation of vaccine candidates that elicit human antibody responses [57]. These models also facilitate preclinical drug testing by expressing human drug targets (e.g., PD-1, CTLA-4) or metabolic enzymes, providing more predictive platforms for assessing drug efficacy, toxicity, and pharmacokinetics [60].
Table 2: Comparison of Humanized Mouse Model Generation Methods
| Parameter | hu-SRC-SCID Model (HSC Engraftment) | hu-PBL-SCID Model (PBMC Engraftment) |
|---|---|---|
| Cell Source | CD34+ hematopoietic stem cells from umbilical cord blood, fetal liver, or mobilized peripheral blood [59] | Peripheral blood mononuclear cells (PBMCs) from adult donors [59] |
| Time to Engraftment | 12-16 weeks for full immune system development [60] | 1-2 weeks for functional immune cells [59] |
| Key Advantages | Develops multilineage human immune system; T cells undergo negative selection and are host-tolerant; suitable for long-term studies [59] [60] | Rapid establishment of functional human immunity; enables studies of mature human immune cell function; suitable for short-term experiments [59] |
| Major Limitations | Lengthy engraftment period; variable human cell reconstitution levels between mice; some innate immune cell populations may be underdeveloped [59] | Rapid onset of Graft-versus-Host Disease (GvHD) limits experimental window to ~4 weeks; primarily engrafts T cells; lacks developing immune system [59] [60] |
| Ideal Applications | Studies of human hematopoietic development, immune responses to pathogens/vaccines, and long-term infection models [59] | Analysis of pre-existing human immune responses, allograft rejection, and short-term drug efficacy studies [59] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of advanced animal models requires specific reagents and materials carefully selected for their intended applications. The following table details key solutions used in ferret transmission studies and humanized mouse generation.
Table 3: Essential Research Reagents for Advanced Animal Models
| Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Immunodeficient Mouse Strains | Serve as hosts for human immune system engraftment | NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ (NSG), BALB/c-Rag2nullIL2rγnull, CIEA NOG mouse [59] [60] |
| Human Hematopoietic Stem Cells (HSCs) | Reconstitute human immune system in immunodeficient mice | CD34+ cells isolated from umbilical cord blood, fetal liver, or G-CSF-mobilized peripheral blood [59] |
| Human Peripheral Blood Mononuclear Cells (PBMCs) | Rapid engraftment of mature human lymphocytes | Isolated from peripheral whole blood or spleen of adult donors via Ficoll density gradient centrifugation [59] |
| Virus Inoculation Stocks | Infection of donor animals in transmission studies | Characterized for titer (TCID50, PFU), passage history, and genetic sequence [58] |
| Specific Path-Free (SPF) Ferrets | Subjects for respiratory virus transmission studies | Sourced from reputable commercial suppliers; typically 4-6 months old; seronegative for target virus [58] |
| Cytokine-Expressing NOG Mice | Enhanced human immune cell development | NOG mice transgenic for human cytokines (IL-3, GM-CSF, etc.) to support myeloid cell differentiation [60] |
Ferret transmission models and humanized mouse systems represent complementary, powerful tools for elucidating viral pathogenesis mechanisms and developing effective countermeasures. The ferret model provides an unparalleled system for studying respiratory virus transmission, pathogenesis, and intervention strategies in a naturally susceptible host that closely mirrors human disease. Meanwhile, humanized mice enable detailed investigation of human immune responses to viral infection, evaluation of human-specific therapeutics, and modeling of human-specific aspects of viral pathogenesis that cannot be recapitulated in standard laboratory mice. As these models continue to be refined through standardization of experimental parameters (ferrets) and incorporation of human cytokines and tissue grafts (humanized mice), their predictive value for human disease outcomes will further increase. The strategic integration of both systems in coordinated research programs offers a comprehensive approach to understanding and combating current and emerging viral threats, ultimately accelerating the translation of basic research findings into clinical applications.
Viral pathogenesis is the process by which a viral infection leads to disease, encompassing the sequence of events from virus entry and replication within the host to the manifestation of clinical symptoms [2] [16]. A critical challenge in virology has been moving from static, post-infection observations to dynamically visualizing these processes as they occur within living systems. Live-cell imaging represents a transformative approach in this field, allowing researchers to directly observe the spatiotemporal dynamics of viral spread in real time [61]. This capability is vital for understanding the mechanistic nature of virus-host interactions, which informs the development of targeted antiviral strategies and reveals fundamental concepts in cellular biology [61].
The traditional methods of studying viral pathogenesis—such as electron microscopy or analysis of fixed tissues—provide only snapshots of infection [61]. In contrast, live-cell imaging enables researchers to track the entire viral life cycle as it unfolds, offering unprecedented insights into the sequential events of infection and the underlying molecular mechanisms that cause tissue damage and disease [2] [16]. For pathogenic viruses like human immunodeficiency virus type 1 (HIV-1), which has been extensively studied using these techniques, this approach has illuminated previously unobservable processes including viral entry, intracellular trafficking, assembly, and cell-to-cell transmission [61]. The integration of biosensor technology with advanced microscopy has further enhanced this capability, enabling the detection of specific viral activities without requiring genetic modification of the virus itself [61] [62]. This technical guide explores the current methodologies, applications, and experimental protocols that constitute the state-of-the-art in tracking viral spread in real time, framed within the broader context of viral pathogenesis research.
Fundamental Concepts and Imaging Strategies
The Need for Visualization in Viral Pathogenesis
The fundamental stages of viral pathogenesis include implantation at the portal of entry, local replication, systemic dissemination to target organs, and subsequent shedding of virus into the environment [2]. Whether these processes result in subclinical infection or overt disease depends on a complex interplay between viral virulence factors and host defenses [2] [16]. A key determinant is viral tissue tropism—the affinity for specific body tissues—which is influenced by factors such as cell surface receptors, host transcription factors, and physical barriers [2]. Understanding precisely how and when viruses navigate these cellular and anatomical landscapes is crucial for deciphering pathogenesis mechanisms.
While powerful genomics-based approaches can identify host factors involved in viral replication, they rarely provide information about the dynamics of these interactions—where and when they occur within the living cell [61]. Live-cell imaging addresses this limitation by enabling direct visualization of these processes as they happen, with sufficient spatiotemporal resolution to track individual virions or viral components [61]. This "seeing is believing" philosophy has revealed that viral pathogenesis involves not just the direct cytopathic effects of viral replication, but also complex immunopathological events where host immune responses contribute to tissue damage and disease symptoms [16].
Engineering Visible Viruses
The first major strategy for live-cell imaging involves creating engineered "visible" viruses where specific viral components are labeled with fluorescent markers [61]. This direct labeling approach allows researchers to track defined elements of the viral life cycle in real time. The most common method utilizes fluorescent proteins (FPs) like GFP and its variants, which can be genetically encoded within the viral genome [61]. Despite the challenge of working with compact viral genomes that often optimize coding efficiency, researchers have successfully generated functional FP-tagged viruses for various applications.
Table: Strategies for Engineering Visible Retroviruses
| Viral Component | Labeling Strategy | Key Applications | Considerations |
|---|---|---|---|
| Gag/Gag-Pol Proteins | FP inserts within viral genome | Study virion assembly, subcellular trafficking, cell-to-cell transmission [61] | May impact protein function and replication efficiency; requires functional validation |
| Viral Envelope (Env) | FP-tagged Env proteins or antibody-quantum dot conjugates [61] | Visualization of envelope dynamics and incorporation into virions | Challenging for some viruses like HIV-1; proxy labeling often preferred |
| Viral RNA Genomes | RNA stem-loop scaffolds (MS2, Bgl, PP7) with cognate FP-fused binding proteins [61] | Tracking viral genome trafficking and packaging | Allows dual-labeling with Gag-FP to study genome-protein interactions |
| Proxy Labeling | FP-tagged viral (Vpr) or host (CypA) proteins incorporated into virions [61] | Study post-entry events and virion dynamics | Enables tracking of non-modified viruses; may not represent fully native interactions |
Viral Biosensor Systems
The second major approach utilizes biosensor cells engineered to detect and report specific viral activities, providing an indirect method for tracking infection [61] [62]. These systems are particularly valuable because they enable researchers to study native, non-modified viruses without potentially altering replication efficiency through genetic manipulation [61]. Biosensor platforms detect successful viral infection by responding to specific viral activities that either activate or downregulate expression of fluorescent marker proteins [61].
For HIV-1, widely used biosensors employ the HIV-1 Long Terminal Repeat (LTR) promoter to drive FP expression in a Tat-dependent manner [61]. In these systems, fluorescence activation serves as a direct indicator of successful viral infection and gene expression. Alternative biosensor designs utilize stably expressed FP-tagged host proteins, such as APOBEC3G, that are downregulated by specific viral proteins, thereby reporting on viral activity through decreased fluorescence [61]. Beyond these engineered systems, native cellular responses to infection—including cytoskeletal remodeling, induction of antiviral gene expression, and activation of apoptotic pathways—can also serve as biosensors for detecting and monitoring viral replication dynamics [61].
A visual summary of the two primary approaches for tracking viral spread in real time, showing both direct viral labeling strategies and indirect biosensor systems that converge on the common goal of visualizing viral dynamics.
Technical Implementation and Methodologies
The Viral Live-Cell Imaging Toolkit
Successful implementation of live-cell imaging for tracking viral spread requires appropriate selection of microscopy platforms and imaging modalities, each with distinct advantages for specific applications [61]. Widefield microscopes coupled with bright light sources and broad filter sets represent the most common and versatile setups due to their ease of use and relatively low cost [61]. However, their limited axial resolution and issues with out-of-focus light present challenges for single particle tracking, often necessitating computational deconvolution strategies [61].
For higher resolution applications, particularly those requiring single virion tracking, laser-based systems offer superior performance. Confocal microscopes provide enhanced optical sectioning capabilities, while Total Internal Reflection Fluorescence (TIRF) microscopy exploits evanescent wave excitation to selectively illuminate a thin region (typically <200 nm) immediately adjacent to the coverslip [61] [62]. This makes TIRF ideal for studying processes occurring at the plasma membrane, such as viral attachment, fusion, and assembly. When implementing any live-cell imaging modality, maintaining stable incubation conditions (temperature, CO₂, humidity) is essential for preserving cell viability throughout extended time-lapse experiments.
Table: Imaging Modalities for Viral Live-Cell Imaging
| Imaging Modality | Light Source | Best Resolution & Applications | Limitations |
|---|---|---|---|
| Widefield | Broad spectrum (mercury or LED) | Lateral: ~200-300 nm; ideal for overview imaging and high-throughput screening [61] | Limited axial resolution; out-of-focus light requires deconvolution |
| Laser Scanning Confocal | Laser | Lateral: ~180-250 nm; Axial: ~500-800 nm; superior optical sectioning for 3D reconstruction [61] | Slower acquisition speeds; potential photobleaching and phototoxicity |
| TIRF | Laser | Axial: ~100 nm; ideal for single particle tracking at cell membrane [61] [62] | Restricted to events near coverslip; limited penetration depth |
Experimental Protocol: Norovirus Detection via TIRF-Based Biosensor
The following detailed protocol exemplifies the application of TIRF microscopy combined with a sandwich-type biosensor assay for detecting individual Norovirus particles, demonstrating the principles of high-sensitivity viral detection [62].
Principle: This assay detects whole virus particles with single-virus sensitivity using a sandwich configuration where virus-like particles (VLPs) are first captured onto a supported lipid bilayer containing specific glycosphingolipid (GSL) ligands, then visualized using fluorescently-labeled phospholipid vesicles containing the same ligand [62].
Materials:
- Norovirus VLPs (Ast/6139/01 strain or similar)
- Supported lipid bilayer formation components (e.g., SiO₂ substrates)
- Glycosphingolipid ligands (H type I GSL)
- Rhodamine-labeled phospholipid vesicles
- TIRF microscope system with temperature control
- iXon EMCCD camera or equivalent high-sensitivity detector
- MatLab-based analysis software or equivalent
Procedure:
- Prepare sensing interface: Create a non-fouling supported lipid bilayer incorporating 10% H type I GSL to specifically capture Norovirus VLPs [62].
- Incubate with virus: Introduce Norovirus VLP sample (12.5 pM concentration used in development) and incubate to allow specific binding to GSL ligands in the lipid bilayer [62].
- Apply detection vesicles: Introduce rhodamine-labeled phospholipid vesicles containing 5% H type I GSL, which bind to captured VLPs in a sandwich configuration [62].
- TIRF imaging: Using TIRF illumination, acquire time-lapse movies (typically 1000 frames at 5 fps) to distinguish surface-bound vesicles from those in solution [62].
- Multi-position imaging: Image all wells of interest in at least 7 different positions to ensure reproducible statistics [62].
- Automated detection: Analyze images using MatLab-based software, counting a fluorescent vesicle only if present on a predefined number of successive frames with intensity exceeding a set threshold [62].
- Kinetic analysis: Record the number of new vesicles over time to produce association plots and determine vesicle residence times to differentiate specific from non-specific binding [62].
Validation and Optimization: This assay achieves a limit of detection (LOD) of approximately 10⁶ particles/mL, representing a significant improvement over previous biosensors for Norovirus detection [62]. The entire assay can be completed within two hours, substantially faster than PCR-based methods [62]. Key to the assay's performance is the non-fouling nature of the sensing interface, which minimizes non-specific binding, and the ability to discriminate specific interactions through analysis of vesicle residence times [62].
Protocol: Live-Cell Imaging of HIV-1 Assembly and Trafficking
This protocol details the methodology for visualizing HIV-1 assembly and cell-to-cell transmission using FP-tagged Gag proteins, a foundational approach in retroviral live-cell imaging [61].
Principle: HIV-1 Gag and Gag-Pol proteins drive virion assembly and can be engineered to carry FP inserts while retaining infectivity, enabling direct visualization of assembly sites, intracellular trafficking, and cell-to-cell transmission events [61].
Materials:
- FP-tagged HIV-1 Gag constructs (Gag-GFP, Gag-mCherry, etc.)
- Permissive cell line (e.g., HEK293T, T-cell lines)
- Live-cell imaging chamber with environmental control (37°C, 5% CO₂)
- High-resolution confocal or TIRF microscope system
- Image analysis software (e.g., ImageJ, Volocity, Imaris)
Procedure:
- Molecular construction: Engineer HIV-1 molecular clones to express Gag fused to FPs, typically inserted between the MA and CA domains, though various positions have been successfully utilized [61].
- Virus production: Transfect permissive cells (e.g., HEK293T) with FP-tagged Gag constructs alongside other necessary viral components to produce replication-competent particles.
- Cell preparation: Plate target cells (e.g., susceptible T-cell lines) on imaging-optimized dishes or coverslips at appropriate density for single-cell resolution.
- Infection and imaging: Infect target cells with FP-tagged virus and begin time-lapse imaging, typically 24-48 hours post-infection when Gag expression is robust.
- Multi-color imaging: For studies of viral genome trafficking, co-express FP-tagged Gag with viral RNA labeled via MS2-GFP or similar RNA stem-loop systems [61].
- Image acquisition: Acquire time-lapse series with appropriate temporal resolution (seconds to minutes depending on process studied) while maintaining physiological conditions.
- Quantitative analysis: Track individual particles or assembly sites over time to quantify parameters such as movement velocities, assembly kinetics, and transfer efficiency between cells.
Technical Considerations: Functional FP-tagged Gag constructs must be validated for proper particle assembly and infectivity compared to wild-type virus [61]. For studies of viral spread, co-culture systems with both producer and target cells enable visualization of cell-to-cell transmission events, which occur more efficiently than cell-free infection for many viruses [61]. Phototoxicity must be carefully managed through optimization of exposure times, light intensity, and imaging frequency to preserve normal cellular function throughout extended observations.
Workflow for implementing live-cell imaging to study viral pathogenesis, showing the key decision points from experimental design through data interpretation.
Advanced Applications and Research Applications
The Scientist's Toolkit: Essential Research Reagents
Implementing live-cell imaging for viral tracking requires specific reagents and tools carefully selected based on research objectives. The following table summarizes key solutions for studying viral pathogenesis through real-time imaging approaches.
Table: Research Reagent Solutions for Viral Live-Cell Imaging
| Research Reagent | Function/Application | Key Features & Considerations |
|---|---|---|
| FP-tagged Viral Constructs | Direct labeling of viral proteins (Gag, Env) for visualization of assembly and trafficking [61] | Requires validation of functionality; position of FP insertion critical for preserving protein function |
| RNA Stem-Loop Systems (MS2, PP7) | Specific labeling of viral genomes for tracking replication and packaging [61] | Enables dual-color imaging with viral proteins; scaffold size may impact genome function |
| Virus Biosensor Cells (e.g., GHOST cells) | Detection of native, non-modified viruses through reporter gene activation [61] | Enables study of clinical isolates without genetic manipulation; specificity depends on promoter elements |
| High-Sensitivity EMCCD Cameras | Detection of low-light fluorescence signals with minimal noise for single particle tracking [62] | Essential for TIRF applications; cooling to -100°C reduces dark noise; high quantum efficiency critical |
| TIRF Microscopy Systems | Selective illumination of cell surface for high-resolution imaging of attachment and fusion events [61] [62] | Ideal for studying viral entry and assembly at plasma membrane; requires specialized optics |
| Supported Lipid Bilayers | Biomimetic membrane systems for studying virus-receptor interactions [62] | Enable control of receptor density and composition; minimal non-specific binding |
Applications in Understanding Viral Pathogenesis
Live-cell imaging has provided transformative insights into multiple aspects of viral pathogenesis by revealing the dynamic behaviors of viruses within living systems. In understanding viral entry mechanisms, TIRF microscopy has enabled researchers to visualize the initial attachment of individual virions to cell surfaces, their lateral movement along membranes, and the precise moments of fusion and internalization [61] [62]. For viruses like Norovirus, this approach has revealed the kinetics of receptor binding and the multivalent interactions that facilitate efficient entry [62].
In studying intracellular trafficking, the combination of FP-tagged viral components and confocal microscopy has illuminated how viruses hijack cellular transport systems to reach their replication sites. For HIV-1, real-time tracking of FP-tagged Gag proteins has revealed previously unappreciated aspects of assembly dynamics, including the formation of higher-order oligomers at the plasma membrane and the complex process of viral genome packaging [61]. Similarly, the use of MS2-GFP labeled genomes has enabled researchers to follow the fate of individual viral RNA molecules from nuclear export through incorporation into nascent particles [61].
Perhaps most significantly, live-cell imaging has revolutionized our understanding of cell-to-cell transmission, demonstrating that many viruses, including HIV-1, can spread directly between adjacent cells through specialized structures like virological synapses [61]. This mode of transmission provides a more efficient dissemination pathway than cell-free infection and offers partial protection from neutralizing antibodies, with important implications for pathogenesis and therapeutic design [61]. By visualizing these events in real time, researchers have identified the cellular structures and molecular interactions that facilitate viral spread within tissues.
Future Perspectives and Concluding Remarks
The field of live-cell imaging for tracking viral spread continues to evolve with emerging technologies that promise even deeper insights into viral pathogenesis. Current challenges include the need for better labeling strategies that minimally perturb viral function, improved spatial and temporal resolution to capture rapid viral dynamics, and the development of multivariate imaging systems that can simultaneously track multiple viral and cellular components throughout complete replication cycles [61]. The integration of super-resolution techniques with live-cell imaging represents a particularly promising direction, potentially enabling researchers to bridge the gap between molecular-scale interactions and cellular-scale pathogenesis.
From the perspective of viral pathogenesis research, these technical advances will facilitate more comprehensive understanding of how viral spread within hosts translates to disease manifestations. The ability to track viral population dynamics in real time, while simultaneously monitoring host cell responses, will help elucidate the balance between direct cytopathic effects and immunopathological damage that underlies many viral diseases [16]. Furthermore, the application of these technologies to animal models of infection, though technically challenging, promises to connect cellular-level events with tissue- and organism-level pathogenesis.
For researchers and drug development professionals, the methodologies described in this technical guide provide powerful tools for identifying and validating novel therapeutic targets. By revealing previously unobservable aspects of the viral life cycle, live-cell imaging and biosensor technologies enable the development of interventions that target specific stages of viral spread [61]. Additionally, these approaches facilitate the assessment of antiviral efficacy in physiologically relevant contexts, including the critical process of cell-to-cell transmission that often represents the primary mode of viral dissemination within hosts. As these technologies continue to mature, they will undoubtedly play an increasingly central role in both basic virology research and the development of next-generation antiviral strategies.
Overcoming Research Challenges: Technical Hurdles and Experimental Optimization Strategies
In the field of viral pathogenesis and infection mechanisms research, a significant translational challenge exists: extrapolating findings from controlled in vitro environments to predict outcomes in complex living systems (in vivo). While in vitro models offer invaluable insights into cellular and molecular interactions, they often fail to fully recapitulate the physiological complexity of an entire organism, leading to limitations in predicting therapeutic efficacy and safety. This whitepaper provides a technical guide for researchers and drug development professionals on advanced methodologies and strategic frameworks designed to bridge this critical gap, with a specific focus on applications in virology and infectious disease research.
Methodological Frameworks for Translation
Transcriptomic Benchmarking and Points of Departure (PODs)
A powerful strategy for validating in vitro models involves comparing transcriptomic responses to specific stimuli or insults across different systems. A 2025 study on inhalation toxicity provides a robust template for this approach, directly comparing gene expression changes in both in vitro and in vivo models exposed to volatile organic compounds (VOCs) [63] [64].
- Core Methodology: Researchers assessed physiological responses and respiratory tract gene changes in adult mice after a single acute nose-only inhalation exposure to selected compounds (acrolein, dichloromethane, trichloroethylene, 1,3-butadiene). These in vivo findings were then compared with gene expression responses from differentiated primary human bronchial epithelial cells (pHBECs) and immortalized BEAS-2B cells exposed to the same VOCs at the air-liquid interface (ALI) [63] [64].
- Data Analysis: Whole transcriptome analyses of mouse nasal septum and lung samples and human in vitro cell lysates were performed. To enable cross-system comparisons, researchers calculated VOC cellular uptake and applied a generic physiologically based toxicokinetic (PBTK) model to estimate internal lung concentrations, a process known as in vitro to in vivo extrapolation (IVIVE) [63].
- Key Finding: Although distinct gene expression patterns were observed between human and mouse tissues, the transcriptomic points of departure (PODs) derived from benchmark dose modeling using predicted internal concentrations were largely comparable (within 2-fold for most compounds). This highlights that while specific pathways may differ, overall sensitivity can be consistent when internal dose is accounted for [63].
Advanced Biomimetic Culture Platforms
Moving beyond traditional 2D cell cultures is critical for meaningful translation in viral research. Next-generation biomimetic platforms strive to replicate key aspects of the in vivo environment [65].
- 3D Organoid Cultures: These self-organizing, three-dimensional structures derived from stem cells model the complex architectures and cellular heterogeneity of native tissues, providing a more realistic environment for studying host-pathogen interactions.
- Organs-on-Chips (OOCs): Microfluidic devices that line living human cells on channels to simulate the activities, mechanics, and physiological responses of entire organs or organ structures. They can incorporate fluid flow, mechanical stretching (e.g., for lung models), and co-culture of multiple cell types [65].
- 3D Bioprinting: This technology allows for the precise spatial patterning of cells and biomaterials to create complex, patient-specific tissue constructs for studying infection and testing antiviral agents [65].
These platforms incorporate critical biophysical cues such as suspension flow, air interface, mechanical stimulation, and a stiffened extracellular matrix (ECM), which significantly influence cell maturation, proliferation, and responses to pharmacological agents or viral challenge [65].
Quantitative Comparison of Model Systems
The table below summarizes a quantitative comparison of transcriptomic responses from a bridging study, illustrating how data can be systematically evaluated across different model systems [63] [64].
Table 1: Comparison of Transcriptomic Points of Departure (PODs) Across Model Systems
| Chemical Exposure | In Vitro POD (Human Airway Cells) | In Vivo POD (Mouse Lung) | Fold Difference | Key Conserved Pathway/Biomarker |
|---|---|---|---|---|
| Acrolein | [Value from study] | [Value from study] | < 2-fold | Oxidative Stress (e.g., HMOX1) |
| 1,3-Butadiene | [Value from study] | [Value from study] | < 2-fold | Inflammatory Response |
| Trichloroethylene | [Value from study] | [Value from study] | < 2-fold | Cellular Stress Response |
| Dichloromethane | [Value from study] | [Value from study] | > 2-fold* | Species-specific Metabolism |
Note: The larger fold difference for Dichloromethane is attributed to known species-specific differences in metabolic activation, underscoring the importance of considering comparative metabolism in translational models [63].
The table below categorizes and describes the primary advanced culture platforms used to bridge the in vitro-in vivo gap.
Table 2: Advanced Biomimetic Culture Platforms for Viral Pathogenesis Research
| Platform Type | Key Feature | Primary Application in Virology | Considerations |
|---|---|---|---|
| Air-Liquid Interface (ALI) Cultures | Differentiates cells to create in vivo-like epithelial barriers | Modeling respiratory virus infection (e.g., influenza, SARS-CoV-2) | Excellent for epithelial response; lacks full immune component [64] |
| Organ-on-a-Chip | Incorporates fluid flow and mechanical forces | Studying viral entry, replication, and cytopathicity under physiological flow | Technically complex; can be low-throughput [65] |
| 3D Organoids | Self-organizing 3D structures with multiple cell types | Host-pathogen interactions, viral tropism, and tissue-specific damage | Can lack vasculature and immune cells; variable reproducibility [65] |
| Biomimetic Hydrogels | Tunable extracellular matrix (ECM) stiffness and composition | Investigating impact of tissue mechanics on viral replication and spread | Requires characterization of matrix properties [65] |
Experimental Protocols for Bridging Studies
Protocol: DirectIn VitrotoIn VivoTranscriptomic Comparison
This protocol is adapted from a study bridging human cell-based assays and mouse models [63] [64].
In Vitro Exposure System:
- Culture relevant cells (e.g., primary human bronchial epithelial cells, pHBECs) at an air-liquid interface (ALI) until fully differentiated.
- Use an ALI Cell Culture Exposure System (CCES) to expose cells to a log range of sub-cytotoxic concentrations of the challenge agent (e.g., viral particles, chemical stimulant) for a defined period (e.g., 2 hours).
- Maintain cells in a 37°C incubator for a post-exposure recovery period (e.g., 4 hours) before collecting lysates for transcriptomic analysis.
In Vivo Exposure:
- Subject adult mice (e.g., C57BL/6) to a single, acute exposure matching the in vitro conditions (e.g., nose-only inhalation for 4 hours for volatile agents).
- Monitor real-time physiological responses (e.g., respiratory function via plethysmography).
- Post-exposure, humanely euthanize animals and collect relevant tissues (e.g., lung, nasal septum).
Transcriptomic Analysis & Benchmark Dose (BMD) Modeling:
- Extract total RNA from both in vitro lysates and in vivo tissues.
- Perform whole transcriptome RNA sequencing.
- Conduct differential gene expression analysis for each exposure group versus controls.
- Perform benchmark dose (BMD) modeling on the most sensitive biological pathways identified to calculate a transcriptomic point of departure (POD) for each system.
IVIVE and Data Integration:
- Calculate cellular uptake of the challenge agent in vitro.
- Apply a physiologically based toxicokinetic (PBTK) model to estimate internal tissue and cell concentrations.
- Compare PODs across systems using both administered and internal doses to assess concordance.
Protocol: Establishing a Biomimetic Organoid Platform for Viral Studies
This protocol outlines the key steps for creating a more physiologically relevant in vitro system [65].
- Stem Cell Sourcing and Expansion: Obtain human primary cells or induced pluripotent stem cells (iPSCs). Expand and maintain these cells in self-renewing media under defined conditions.
- 3D Differentiation: Embed stem cells in a defined, tunable extracellular matrix (ECM) scaffold (e.g., Matrigel, synthetic hydrogels). Induce differentiation towards the target tissue lineage (e.g., lung, intestine) using a specific cocktail of growth factors and small molecules over 2-4 weeks.
- Platform Maturation and Characterization: Culture the developing organoids under conditions that promote maturation, potentially incorporating mechanical stimulation (e.g., cyclic stretching for lung) or flow. Characterize the resulting organoids via immunohistochemistry (for marker expression), qPCR, and functional assays to validate their physiological relevance.
- Viral Challenge and Analysis: Infect mature organoids with the virus of interest. Monitor viral replication kinetics (e.g., via plaque assay, qRT-PCR), cytopathic effects (histology), and host responses (e.g., transcriptomics, cytokine secretion) over time.
Visualization of Conceptual and Experimental Workflows
Conceptual Framework for Bridging Data
The following diagram illustrates the strategic integration of data from various model systems to enhance predictive power for human outcomes.
Advanced Platform Workflow
This workflow details the operational process for utilizing advanced biomimetic platforms in a virology research context.
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below lists key reagents and materials crucial for implementing the advanced methodologies described in this guide.
Table 3: Research Reagent Solutions for Bridging Studies
| Reagent/Material | Function | Specific Application Example |
|---|---|---|
| Primary Human Cells (e.g., pHBECs) | Provides a biologically relevant, human-derived model system for study. | Differentiating at ALI to model the human airway for respiratory virus infection studies [64]. |
| Tunable Hydrogels/ECM Matrices | Provides a biomimetic 3D scaffold with controllable mechanical and biochemical properties. | Supporting 3D organoid growth to mimic tissue-specific stiffness and composition for viral pathogenesis studies [65]. |
| ALI Culture Inserts | Enables polarization and differentiation of epithelial cells by exposing the apical surface to air. | Creating a physiologically relevant model of the respiratory epithelium for aerosolized viral challenge [64]. |
| PBTK Modeling Software | Predicts the absorption, distribution, metabolism, and excretion (ADME) of compounds in a biological system. | Performing IVIVE to translate in vitro effective concentrations to in vivo equivalent human doses [63]. |
| Whole Transcriptome Kits | Allows for comprehensive analysis of gene expression changes across the entire genome. | Identifying conserved and divergent pathway responses between in vitro and in vivo systems post-challenge [63] [64]. |
| Microfluidic Chips | Creates miniature systems that can simulate organ-level functions and incorporate fluid flow. | Housing Organ-on-a-Chip models to study viral infection under physiological flow conditions [65]. |
Accurate viral detection is a cornerstone of effective viral pathogenesis research, directly influencing the development of diagnostics, therapeutics, and public health interventions. The persistence of global viral threats, from the recent COVID-19 pandemic to seasonal tripledemics of influenza, RSV, and SARS-CoV-2, underscores an urgent and continuous need for detection technologies that are not only highly sensitive and specific but also deployable in complex, real-world sample matrices [66] [67]. The core challenge lies in the intricate nature of clinical and environmental samples, which often contain PCR inhibitors, variable mucus content, and cellular debris that can interfere with molecular assays, leading to reduced sensitivity and false-negative results [67]. Furthermore, the high mutation rates of viruses and the emergence of novel pathogens complicate the design of robust detection systems, as assays must evolve to maintain specificity against shifting viral genomes [66] [68]. This technical guide delves into the advances and methodologies at the forefront of overcoming these hurdles, with a specific focus on Surface-Enhanced Raman Scattering (SERS) and Digital PCR (dPCR), framing them within the broader context of understanding viral infection mechanisms and host-pathogen interactions.
Advanced Detection Technologies: Principles and Comparative Performance
Surface-Enhanced Raman Scattering (SERS) Technology
SERS technology has emerged as a powerful tool for virus detection, leveraging the enhancement of Raman signals through the local surface plasmon resonance effect generated by metal nanostructures. Its exceptional sensitivity, high resolution, and rapid data acquisition make it particularly suitable for detecting low viral loads in complex samples [66]. The core of SERS technology lies in the "hotspot" effect created by metal nanoparticles (e.g., gold, silver), which significantly amplifies the Raman scattering signal by locally enhancing the electromagnetic field, achieving enhancement factors of 10^6 to 10^8 times [66].
Two primary SERS detection strategies are employed:
- Label-free SERS Detection: This method directly captures the intrinsic Raman scattering signals generated by the virus itself. It avoids complex sample pretreatment and labeling steps, enabling rapid detection and real-time monitoring. However, the inherently weak Raman signals from viruses can pose a challenge for obtaining highly reproducible spectral data [66].
- Label-based SERS Detection: This indirect method uses SERS tags functionalized with Raman reporter molecules and specific recognition elements (e.g., antibodies, aptamers) that bind to the virus. The binding event generates a robust and highly sensitive signal from the reporter molecule, not the virus itself. This approach offers high sensitivity and reproducibility but involves more complex operational procedures [66].
SERS demonstrates significant potential for on-site, rapid virus detection, holding promise for applications in clinical diagnostics, environmental monitoring, and public health surveillance [66].
Digital PCR (dPCR) for Absolute Quantification
Digital PCR (dPCR) represents a paradigm shift in nucleic acid detection by enabling absolute quantification of viral RNA without the need for a standard curve. The method works by partitioning a PCR mixture into thousands of individual reactions (nanowells or droplets), with each partition functioning as a separate PCR vessel. Following endpoint amplification, the platform counts the positive and negative reactions to provide an absolute copy number of the target molecule [67].
A 2025 comparative study of respiratory virus diagnostics during the 2023–2024 tripledemic highlighted the superior performance of dPCR, particularly the nanowell-based QIAcuity system, compared to the traditional gold standard, Real-Time RT-PCR [67]. The study analyzed 123 respiratory samples stratified by viral load and found that dPCR offered greater accuracy and precision, especially for intermediate viral levels.
Table 1: Comparative Performance of dPCR vs. Real-Time RT-PCR in Respiratory Virus Detection (2025 Study)
| Virus Target | Superior Method (by Viral Load Category) | Key Performance Advantage |
|---|---|---|
| Influenza A | dPCR (High viral load) | Superior accuracy |
| Influenza B | dPCR (High viral load) | Superior accuracy |
| SARS-CoV-2 | dPCR (High viral load) | Superior accuracy |
| RSV | dPCR (Medium viral load) | Greater consistency and precision |
| All Targets | dPCR | Less susceptible to sample matrix effects and PCR inhibitors |
While dPCR demonstrates enhanced technical performance, its routine implementation in clinical labs is currently tempered by higher costs and reduced automation compared to the well-established Real-Time RT-PCR workflows [67].
Experimental Protocols for Advanced Viral Detection
Detailed Protocol: SERS-Based Virus Detection (Label-Based Approach)
The following protocol outlines a standard sandwich-style, label-based SERS detection method for viruses, which can be adapted for various targets.
1. SERS Substrate Preparation:
- Synthesis of Metal Nanoparticles: Synthesize gold or silver nanoparticles (e.g., ~60nm spherical nanoparticles) via the citrate reduction method. Characterize the nanoparticles using UV-Vis spectroscopy (to confirm plasmon resonance peak) and dynamic light scattering (for size distribution).
- Functionalization of Nanoparticles: Incubate the nanoparticles with a Raman reporter molecule (e.g., 4-aminothiophenol, 5,5'-dithiobis(2-nitrobenzoic acid)) at a defined molar ratio (e.g., 1:1000) for 1-2 hours. The reporter molecule must adsorb onto the metal surface and exhibit a strong, unique Raman fingerprint.
- Addition of Recognition Element and Protection Layer: Conjugate specific antibodies or aptamers to the reporter-coated nanoparticles via EDC-NHS chemistry or thiol-gold interactions. Finally, passivate the surface with a protective layer, such as polyethylene glycol (PEG), to prevent non-specific binding and stabilize the SERS tag.
2. Sample Preparation and Capture:
- Virus Enrichment (if needed): Pre-treat complex samples (e.g., nasopharyngeal swabs in transport media) with centrifugation or filtration to concentrate viral particles and remove large debris.
- Immobilization of Capture Probe: Coat a solid substrate (e.g., a silicon wafer, glass slide, or magnetic bead) with a capture antibody that is specific to the target virus but different from the detection antibody on the SERS tag.
3. Assay Procedure:
- Incubation and Binding: Incubate the prepared sample with the capture substrate for 30-60 minutes to allow the virus to bind to the capture probe.
- Washing: Gently wash the substrate with a suitable buffer (e.g., phosphate-buffered saline with Tween 20, PBS-T) to remove unbound material and reduce background signal.
- SERS Tag Addition: Introduce the functionalized SERS tags to the substrate and incubate for another 30-60 minutes, forming a "capture-virus-detection" sandwich complex.
- Final Washing and Signal Acquisition: Perform a final stringent wash to remove any unbound SERS tags. The substrate is then air-dried and placed under a Raman spectrometer for signal acquisition. The intensity of the reporter molecule's characteristic peak is quantified and correlated with viral concentration [66].
Detailed Protocol: Digital PCR (dPCR) for Viral RNA Quantification
This protocol uses a nanowell-based dPCR system (e.g., QIAcuity, Qiagen) for absolute quantification of viral RNA from respiratory samples.
1. Nucleic Acid Extraction:
- Extract total nucleic acids from clinical samples (e.g., nasopharyngeal swabs, bronchoalveolar lavage) using an automated system (e.g., KingFisher Flex) with a viral/pathogen nucleic acid kit (e.g., MagMax Viral/Pathogen kit). Include an internal control during extraction to monitor extraction efficiency.
2. dPCR Reaction Setup:
- Prepare the dPCR reaction mix according to the manufacturer's instructions for the chosen platform. A typical 20-40 µL reaction volume will contain:
- dPCR Master Mix (including reverse transcriptase for RNA viruses and DNA polymerase).
- Optimized primer-probe sets specific for the target virus (e.g., Influenza A, SARS-CoV-2). Multiplex assays targeting up to five targets are possible.
- The extracted RNA template.
- Gently mix and briefly centrifuge the reaction mixture.
3. Partitioning and Amplification:
- Load the reaction mixture into the designated nanowell plate or cartridge. The instrument automatically partitions the sample into approximately 26,000 nanowells.
- Transfer the plate to the thermocycler module and run the optimized PCR cycling conditions. A standard protocol may include: reverse transcription (50°C for 30 min), initial denaturation (95°C for 2 min), followed by 40-45 cycles of denaturation (95°C for 15 sec) and annealing/extension (60°C for 60 sec).
4. Data Analysis:
- After amplification, the instrument scans each nanowell for fluorescence signals.
- Using the instrument's software (e.g., QIAcuity Suite Software), apply a fluorescence amplitude threshold to distinguish positive wells (containing the target molecule) from negative wells.
- The software calculates the absolute concentration of the target in copies per microliter of the input reaction volume using Poisson statistics: Concentration = -ln(1 - p) / V, where 'p' is the fraction of positive partitions and 'V' is the volume of each partition [67].
Visualization of Methodologies and Viral Mechanisms
SERS Detection Workflow Diagram
dPCR Partitioning and Quantification Diagram
Viroporin Role in Viral Pathogenesis Diagram
Understanding viral pathogenesis is critical for developing detection strategies. Viroporins, virus-encoded ion channels, are key players in the virus life cycle and are emerging as promising therapeutic and diagnostic targets.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Advanced Viral Detection
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| SERS Substrates | Provides signal enhancement via plasmonic "hotspots". | Gold or silver nanoparticles (spherical, rods), functionalized with Raman reporters (e.g., 4-aminothiophenol). Critical for achieving 10^6-10^8 signal enhancement [66]. |
| Specific Recognition Elements | Binds target virus with high specificity for capture and detection. | Monoclonal antibodies, aptamers, or molecularly imprinted polymers. Used in both SERS tags and dPCR sample preparation workflows [66] [67]. |
| dPCR Reagents & Plates | Enables absolute quantification via sample partitioning and amplification. | dPCR master mix (with reverse transcriptase), target-specific primer-probe sets, and nanowell plates (e.g., QIAcuity plates) or droplet generators [67]. |
| Nucleic Acid Extraction Kits | Isolates viral RNA/DNA from complex sample matrices. | Automated kit-based systems (e.g., KingFisher with MagMax Viral/Pathogen kit). Includes internal controls to monitor extraction efficiency and presence of inhibitors [67]. |
| Viroporin-Targeting Compounds | Research tools for studying viral pathogenesis and as potential antivirals. | Compounds like Amantadine (targets Influenza A M2 protein). Used to investigate the role of viroporins in the virus life cycle, informing diagnostic strategies [12]. |
The optimization of viral detection in complex samples remains a dynamic and critical field of research. Technologies like SERS and dPCR are pushing the boundaries of sensitivity and specificity, offering solutions that are progressively overcoming the challenges posed by sample complexity and low viral loads. The integration of these advanced detection methods with a deeper understanding of viral pathogenesis, such as the function of viroporins and other molecular mechanisms, will be pivotal for the next generation of diagnostic tools [66] [12] [68]. Future progress hinges on standardizing detection protocols, developing more robust and cost-effective platforms, and leveraging artificial intelligence for data analysis and target prediction. By bridging cutting-edge detection technology with fundamental virology research, the scientific community can better prepare for and respond to the persistent and evolving threat of viral diseases.
Standardizing Assays for Drug Screening and Vaccine Evaluation
Assay standardization forms the cornerstone of reproducible and reliable research in viral pathogenesis and drug development. Within the context of viral infection mechanisms, standardized quantitative methods are indispensable for deciphering the complex dynamics between viruses and their hosts. These assays provide the critical data needed to understand viral replication cycles, quantify host immune responses, and evaluate the efficacy of antiviral therapeutics and prophylactic vaccines. The fundamental challenge in virology research lies in distinguishing between mere viral presence and actual infectious capability, a distinction that requires meticulously calibrated assays capable of generating comparable results across laboratories and over time. As quantitative molecular analyses have demonstrated, measuring viral load and understanding its dynamics are essential correlates for disease progression and treatment efficacy assessment [69]. This technical guide establishes a framework for standardizing the most critical assays used in modern virology research, with particular emphasis on their application in screening antiviral compounds and evaluating vaccine candidates.
Core Quantitative Assays in Virology
Virology research employs a suite of complementary assays that provide distinct but interconnected data about viral behavior. The selection of appropriate assays depends on the specific research question, whether it involves quantifying infectious viral particles, measuring total viral components, or modeling viral dynamics within host systems.
Infectivity Assays: Measuring Functional Virus
Infectivity assays remain the gold standard for quantifying functional, replication-competent viral particles, providing critical information for vaccine development and antiviral screening.
Plaque Assay
The plaque assay represents one of the most established and reliable methods for quantifying infectious virus particles [70]. This method relies on the principle that a single infectious virus particle can initiate a focus of infection that spreads locally to neighboring cells, ultimately leading to detectable zones of cell death (plaques) under appropriate overlay conditions.
Experimental Protocol:
- Cell Preparation: Seed permissive cells (e.g., MRC-5 cells for varicella virus) in 6-well plates at a density of 2.4-3 × 10⁵ cells/well and incubate for 2 days until a confluent monolayer forms [71].
- Virus Inoculation: Prepare serial 10-fold dilutions of the virus sample. Remove culture medium from cells and inoculate with diluted virus samples, typically in duplicate or triplicate for each dilution.
- Virus Absorption: Incubate plates for 90 minutes at 37°C to allow virus attachment and entry.
- Overlay Application: Replace inoculum with a semi-solid overlay medium (e.g., 0.8% agarose in MEM with serum and antibiotics) to restrict viral spread to adjacent cells [71].
- Incubation and Staining: Incubate plates for 4-10 days until plaques develop. For visualization, add a second overlay containing neutral red stain (which stains viable cells but leaves plaques clear) or fix cells and stain with Coomassie blue after 7 days of incubation [70] [71].
- Plaque Counting and Titer Calculation: Count distinct plaques and calculate titer using the formula: PFU/mL = (number of plaques) / (dilution factor × volume of inoculum in mL). Report as plaque-forming units per mL (PFU/mL).
The plaque assay's major strength lies in its direct measurement of infectious virus, though it requires several days to complete and depends on the virus causing visible cytopathic effects [70].
Focus Forming Assay
For viruses that do not induce clear cytopathic effects or cell death, the focus forming assay provides a valuable alternative by immunodetection of viral antigens.
Experimental Protocol:
- Follow initial steps similar to plaque assay through incubation period.
- Fix cells and permeabilize using appropriate methods (e.g., methanol or formaldehyde fixation).
- Incubate with primary antibody specific for the virus of interest.
- Detect bound antibody using enzyme-conjugated secondary antibodies (e.g., horseradish peroxidase) with colorimetric substrates or fluorescently tagged antibodies.
- Count foci of infection and calculate titer as focus-forming units per mL (FFU/mL).
This method enables earlier detection than traditional plaque assays (as foci can be detected before visible plaques form) but requires specific, well-characterized antibodies and adds significant cost to virus quantitation [70].
TCID₅₀ Assay
The Tissue Culture Infectious Dose 50 (TCID₅₀) assay represents an endpoint dilution method that determines the dilution at which 50% of inoculated cultures show infectivity.
Experimental Protocol:
- Prepare serial dilutions of virus sample.
- Inoculate multiple culture wells (typically 8-12) per dilution with a standardized volume.
- Incubate for a predetermined period and score each well as positive or negative for infection based on cytopathic effect or other markers.
- Calculate the TCID₅₀ using statistical methods such as the Karber or Reed-Muench methods.
While less precise than plaque assays and requiring more replicates, TCID₅₀ assays are particularly useful for viruses that do not form distinct plaques and enable higher throughput screening [70].
Molecular and Biochemical Assays
Molecular techniques provide complementary information to infectivity assays by measuring total viral components rather than just functional particles.
Quantitative PCR (qPCR)
Quantitative PCR represents a highly sensitive method for quantifying viral nucleic acids, with applications in tracking viral load in both research and clinical settings.
Experimental Protocol:
- RNA/DNA Extraction: Isolate viral nucleic acids from samples using appropriate extraction methods.
- Reverse Transcription: For RNA viruses, perform reverse transcription to generate cDNA.
- Amplification and Detection: Set up reactions with sequence-specific primers, fluorescent probes (e.g., TaqMan), and PCR reagents. Run in real-time PCR instrument with appropriate standards of known concentration.
- Data Analysis: Generate standard curve from known standards and interpolate sample concentrations [69].
The fluorogenic probe-based methodology (TaqMan) allows direct quantitation during the exponential phase of amplification, providing a simple, fast technique for quantifying both RNA and DNA viruses [69]. However, it cannot distinguish between infectious and non-infectious viral particles.
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA provides a method for quantifying viral proteins or antiviral antibodies, with applications in vaccine evaluation and diagnostic development.
Experimental Protocol:
- Coat microplate wells with capture antibody (for antigen detection) or antigen (for antibody detection).
- Block nonspecific binding sites with protein-based blocking buffer.
- Add samples and standards, incubate to allow binding.
- Add detection antibody conjugated to enzyme (e.g., horseradish peroxidase).
- Add enzyme substrate and measure color development spectrophotometrically.
- Generate standard curve and calculate sample concentrations.
Standardization Approaches and Method Validation
Assay standardization requires careful attention to reference materials, procedural consistency, and statistical validation to ensure comparable results across laboratories and over time.
Reference Materials and Controls
The implementation of standardized reference materials, such as the Korean Reference Material for Varicella Vaccine (KRMVV), enables harmonization of results across different laboratories [71]. This specific material, with an assigned titer of 4.26 log₁₀ PFU/dose when measured by the agar overlay method (AOM), serves as a positive control to normalize measurements between different methodologies and laboratories [71]. Similar reference materials should be established for other viral pathogens to improve reliability and objectivity in lot release testing and research applications.
Method Comparison and Selection
Comparative studies demonstrate that methodological choices significantly impact results and their interpretation. In a collaborative study comparing the agar overlay method (AOM) and plaque staining method (PSM) for varicella vaccine testing, the PSM demonstrated advantages for quality control analysis, leading to its adoption as a standardized method [71]. Such systematic comparisons are essential for establishing optimal protocols for specific applications.
Statistical Considerations for Validation
Robust statistical analysis forms the foundation of assay validation. The collaborative study on varicella vaccine testing employed several key approaches:
- Z-score analysis confirmed technical proficiency across participating laboratories, with scores within ±1 considered acceptable [71].
- Geometric mean titer (GMT) calculation provided a composite measure of viral potency.
- Geometric coefficient of variation (GCV) quantified inter-laboratory variability, with lower values indicating better reproducibility [71].
For reliable titers in plaque assays, researchers should plate each sample dilution in at least duplicate (preferably triplicate) and incorporate results from multiple countable dilutions in final calculations using appropriate statistical formulas [70].
Quantitative Models of Viral Dynamics
Mathematical modeling of viral dynamics provides powerful insights into pathogenesis and treatment effects, transforming raw assay data into biological understanding.
Within-Host Viral Dynamics Modeling
Mathematical models fit to longitudinal viral load data enable comparison of viral dynamics across different pathogens. For example, such models have revealed that the within-host reproduction number at symptom onset (RS0) of SARS-CoV-2 is significantly larger than that of MERS-CoV and similar to SARS-CoV, suggesting greater difficulty in controlling SARS-CoV-2 infection with antivirals [72]. These models further demonstrated that SARS-CoV-2 reaches its viral load peak just 2.0 days after symptom onset, considerably faster than MERS-CoV (12.2 days) or SARS-CoV (7.2 days) [72]. This accelerated timeline has critical implications for the window of therapeutic intervention.
Modeling Antiv Treatment Effects
Viral dynamic models can predict the efficacy of antiviral drugs with different mechanisms of action:
- Blocking de novo infection: Most effective when initiated before the viral load peak.
- Inhibiting virus production: Similarly time-sensitive, with maximal effect when started early.
- Promoting cytotoxicity of infected cells: Less sensitive to timing of initiation, maintaining effectiveness even after peak viremia [72].
Combination therapies that pair cytotoxicity-promoting agents with drugs that block de novo infection or virus production act synergistically, particularly when initiated early in infection [72].
Emerging Technologies: Artificial Intelligence in Vaccine Research
Artificial intelligence (AI) and machine learning are revolutionizing vaccine development by accelerating and enhancing multiple stages of the research pipeline.
AI Applications Across the Vaccine Development Workflow
Traditional machine learning approaches (random forests, support vector machines, gradient boosting, and logistic regression) dominate tasks ranging from antigen discovery to epitope prediction and supply-chain optimization [73]. Deep learning architectures, including convolutional and recurrent neural networks, generative adversarial networks, and variational autoencoders, have proven instrumental in multiepitope vaccine design and adaptive clinical trial simulations [73]. AI-driven integration of multi-omic data has significantly accelerated epitope mapping, reducing discovery timelines by months compared to conventional methods [73].
AI-Enhanced Public Engagement and Sentiment Analysis
Beyond core research applications, AI tools provide capabilities for monitoring public attitudes toward vaccines through sentiment analysis and enabling tailored communication strategies to address vaccine hesitancy [73]. These applications demonstrate the expanding role of computational approaches throughout the entire vaccine development and implementation ecosystem.
The Scientist's Toolkit: Essential Research Reagents
Table 1: Key Research Reagents for Standardized Virology Assays
| Reagent/Cell Line | Function and Application | Specification Guidelines |
|---|---|---|
| MRC-5 Cells | Human diploid lung fibroblast cell line used for propagating various human viruses including varicella | Use within 30 population doubling levels (PDLs); maintain in MEM with HEPES, L-glutamine, and 10% FBS [71] |
| Agarose Overlay | Semisolid medium to restrict viral spread in plaque assays | Prepare 0.8% (w/v) in MEM with serum; heat sterilize and cool to 40°C before use [71] |
| Neutral Red Stain | Vital stain for visualizing viable cells in plaque assays | Use in third overlay at 0.33% (w/v) to distinguish clear plaques against stained cell monolayer [71] |
| Coomassie Blue Stain | Protein stain for plaque visualization in liquid overlay methods | Stain fixed cells for 30 min to 3 hours; plaques appear as unstained areas on blue background [71] |
| Reference Materials | Standardized viral preparations for assay calibration | Use consistent reference materials (e.g., KRMVV for varicella) to normalize inter-laboratory results [71] |
| Virus-Specific Antibodies | Immunodetection for focus-forming assays and ELISA | Validate specificity and titer for each virus; optimize concentration through checkerboard titration |
Experimental Workflows and Signaling Pathways
The following diagrams illustrate key experimental workflows and conceptual frameworks in standardized virology research.
Plaque Assay Workflow
Viral Dynamics Modeling Approach
Assay Standardization Framework
Comparative Analysis of Virology Assays
Table 2: Comparison of Major Virus Quantification Methods
| Assay Type | Measured Parameter | Detection Range | Time Required | Key Applications | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Plaque Assay | Infectious virus (PFU/mL) | 10¹-10⁸ PFU/mL [70] | 4-10 days [70] | Vaccine potency, antiviral screening | Measures functional virus, quantitative | Labor-intensive, slow, requires cytopathic effect |
| Focus Forming Assay | Infectious virus (FFU/mL) | Similar to plaque assay | 2-7 days [70] | Viruses without cytopathic effect | Earlier detection, works for non-lytic viruses | Requires specific antibodies, added cost |
| TCID₅₀ | Infectious dose (TCID₅₀/mL) | 10¹-10⁸ TCID₅₀/mL | Similar to plaque assay | Viruses that don't form plaques | Works for non-plaque forming viruses | Less precise, requires more replicates |
| qPCR | Viral genome copies | 10²-10¹¹ copies/mL [69] | 4-8 hours | Viral load monitoring, diagnosis | Highly sensitive, rapid, quantitative | Does not measure infectivity |
| ELISA | Viral antigen or antibodies | Varies by target | 4-24 hours | Serology, antigen detection | High throughput, equipment access | May cross-react, limited sensitivity |
Standardized assays provide the essential foundation for advancing our understanding of viral pathogenesis and developing effective countermeasures against viral threats. The integration of classical virology methods with modern computational approaches, including artificial intelligence and mathematical modeling, creates a powerful framework for accelerating drug discovery and vaccine development. As the field continues to evolve, maintaining rigor in assay validation and implementation remains paramount for generating reproducible, clinically relevant data. The continued refinement of these standardized approaches will enhance our capacity to respond to emerging viral threats and improve global pandemic preparedness.
Navigating Viral Sequence Diversity and Evolution in Experimental Design
Viral sequence diversity, generated by high mutation rates and recombination events, is a fundamental driver of pathogenesis, immune evasion, and therapeutic resistance. Understanding and navigating this diversity is therefore not merely a technical challenge but a cornerstone of effective virology research and countermeasure development. This guide provides a structured framework for integrating evolutionary principles into the experimental design of viral pathogenesis studies. Framing research within the context of viral pathogenesis and infection mechanisms necessitates a forward-looking approach that anticipates viral evolution [74]. Recent research underscores that evolutionary selection pressures act decisively on viral genomes to shape and preserve distinct genomic signatures, which are patterns of oligonucleotide frequencies and biases within the genetic code [75]. These signatures are not random; they are often highly specific at the species level and reflect a complex interplay of viral and host factors. Consequently, experimental design must account for this dynamic landscape to ensure that findings are robust, reproducible, and relevant to the evolving nature of viral threats. This document outlines key concepts, data interpretation strategies, experimental protocols, and visualization tools to equip researchers with the methodologies needed to dissect viral sequence diversity within the broader framework of molecular pathogenesis.
Quantitative Landscape of Viral Genomic Diversity
The genomic signature of a virus encapsulates its unique patterns of oligonucleotide frequencies, GC content, and codon usage. A large-scale analysis of 2,768 eukaryotic viral species revealed that most possess highly specific genomic signatures, a trait strongly correlated with genome size [75]. The table below summarizes the prevalence of species-specific genomic signatures across different viral genome size categories, illustrating that viruses with larger genomes are more likely to possess a distinguishable signature.
Table 1: Prevalence of Species-Specific Genomic Signatures by Viral Genome Size
| Genome Size (Nucleotides) | Percentage with Species-Specific Genomic Signatures |
|---|---|
| ≥ 50,000 | 78% |
| 20,000 - 49,999 | 45% |
| 10,000 - 19,999 | 22% |
| 5,000 - 9,999 | 16% |
| ≤ 5,000 | 9% |
Furthermore, genomic signatures vary significantly in their specificity across different viral types and families. While some families show strong conservation of signatures among members, others exhibit vast distinctness between species. The degree to which a virus's genomic signature resembles or diverges from that of its host provides critical insights into the selective pressures acting upon it, which can inform the design of attenuated vaccines and antiviral strategies [75].
Table 2: Genomic Signature Specificity and Host Interaction by Virus Type
| Virus Type | Typical Genomic Signature Specificity | Common Dissimilarity to Host Signature | Implications for Experimental Design |
|---|---|---|---|
| dsDNA Viruses | High (often species-specific) | Consistent dissimilarity | Signature stability supports phylogenetic and tracking studies. |
| Large Genome Viruses | High | Consistent dissimilarity | Focus on viral-encoded replication and repair machinery. |
| ssRNA Viruses | Variable (low to moderate) | Slight similarities in some cases (e.g., Flaviviridae) | Assess host adaptation pressures; consider codon and codon-pair bias. |
| Viruses with Small Genomes | Low | Often no match to any family profile | Requires high-depth sequencing to overcome low signature prevalence. |
Core Experimental Protocols for Analyzing Viral Diversity
Protocol: Identification and Functional Characterization of Viroporins
Viroporins are virus-encoded transmembrane proteins that form pores, modulating ion homeostasis and playing critical roles in the viral life cycle, from entry to release. Their disruption of host cell integrity and role in triggering pro-inflammatory responses like NLRP3 inflammasome activation make them key targets for antiviral strategies [12].
1. In Silico Identification:
- Objective: To predict potential viroporin candidates from viral genomic sequences.
- Methodology:
- Sequence Analysis: Scan the viral proteome for small (often <120 amino acids), hydrophobic proteins containing predicted transmembrane domains (TMDs). Tools like TMHMM or Phobius are commonly used.
- AlphaFold Prediction: Utilize AI-driven structural prediction algorithms (e.g., AlphaFold) to model the tertiary structure of candidate proteins and predict potential pore-forming oligomeric states [12].
- Checklist Application: Apply a structured checklist for viroporin identification, which requires evidence of structural features (TMDs, oligomeric architecture), functional ion channel activity, and genetic validation [12].
2. Electrophysiological Functional Confirmation:
- Objective: To empirically confirm ion channel activity of the candidate viroporin.
- Methodology:
- Heterologous Expression: Express the candidate protein in a system such as Xenopus laevis oocytes or HEK-293 cells.
- Patch-Clamp Recording: Perform whole-cell or single-channel patch-clamp recordings to detect transmembrane currents in response to voltage or chemical gradients.
- Planar Lipid Bilayer Measurement: Reconstitute the purified candidate protein into an artificial lipid bilayer and measure ion conductance under controlled conditions. This confirms pore-forming capability in a minimal system [12].
- Critical Validation: Mutate key amino acid residues (e.g., His37 and Trp41 in influenza A M2) predicted to be involved in gating or ion selectivity. A significant perturbation or abolition of channel activity upon mutation provides definitive genetic validation [12].
3. Cellular Assay for Pathogenic Function:
- Objective: To assess the viroporin's impact on cellular homeostasis and inflammation.
- Methodology:
- Membrane Permeability Assay: Transfert cells with the viroporin gene and assay for increased uptake of small, membrane-impermeable molecules.
- Ion Imaging: Use fluorescent dyes (e.g., Fluo-4 for Ca²⁺) to detect changes in intracellular ion concentrations.
- Inflammasome Activation Assay: Co-transfect the viroporin gene with an NLRP3 reporter construct and measure caspase-1 activation or IL-1β release to evaluate its role in pro-inflammatory responses [12].
Protocol: Tracking Viral Evolution via Genomic Signature Analysis
This protocol uses k-mer frequency analysis with Variable-Length Markov Chains (VLMCs) to track and compare viral sequences, useful for studies on transmission, evolution, and emergence.
1. Sequence Pre-processing:
- Objective: To prepare high-quality viral genome sequences for analysis.
- Methodology:
- Data Retrieval: Download complete viral genome sequences from databases like NCBI GenBank.
- Masking: Use tools like DustMasker to remove low-complexity and repeat regions, preventing bias in k-mer frequency calculations [75].
- Segmentation: For viruses with segmented genomes, analyze each segment separately.
2. Genomic Signature Modeling:
- Objective: To build a model that captures the unique oligonucleotide pattern of a viral genome.
- Methodology:
- Data Partitioning: Divide each viral sequence into two parts: the first 30% (the query sequence) and the last 70% (the profile sequence).
- VLMC Training: Train a VLMC model on the profile sequence. This model generalizes the frequencies of fixed-length k-mers, adapting the depth of the Markov chain based on the genome's statistics to balance power and robustness [75].
- Signature Extraction: The trained VLMC represents the genomic signature of that specific viral sequence.
3. Signature Comparison and Specificity Classification:
- Objective: To determine the specificity of a viral genomic signature and its relationship to other viruses.
- Methodology:
- Comparison: Compare the signature of the query sequence against the profile signatures of all viruses in the dataset.
- Classification:
- Species-Specific: The query signature is most similar to its own profile signature.
- Genus/Family-Specific: The query signature matches the profile of a different species within the same genus or family.
- Non-Specific: The query does not match any profile within the same family, which is common in viruses with small genomes [75].
- Statistical Testing: Use simulation approaches with random query-profile pairing and Bonferroni-corrected t-tests to validate the statistical significance of matches.
Visualization of Concepts and Workflows
Viral Pathogenesis and Viroporin Function
The following diagram illustrates the central role of viroporins in the viral life cycle and the subsequent mechanisms that lead to cellular damage and neurological sequelae, integrating concepts from viral pathogenesis [12] [25].
Diagram 1: Viroporin role in pathogenesis and sequelae.
Genomic Signature Analysis Workflow
This workflow outlines the computational process for analyzing viral genomic signatures to track evolution and diversity, as derived from current methodologies [75].
Diagram 2: Genomic signature analysis workflow.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their applications for studying viral sequence diversity, pathogenesis, and viroporin function.
Table 3: Research Reagent Solutions for Viral Diversity and Pathogenesis Studies
| Research Reagent / Material | Function / Application in Experimental Design |
|---|---|
| Heterologous Expression Systems (Xenopus oocytes, HEK-293 cells) | Provides a controlled cellular environment for the electrophysiological characterization of putative viroporins and their mutant variants [12]. |
| Planar Lipid Bilayer Setup | A minimalistic, artificial membrane system used to reconstitute and directly measure the ion channel activity and selectivity of purified viroporin proteins [12]. |
| Patch-Clamp Electrophysiology Rig | The gold-standard equipment for detecting and quantifying ion currents across cell membranes resulting from viroporin channel activity [12]. |
| Codon-Optimized Viral Gene Constructs | Synthetic genes designed with host-specific codon usage to ensure efficient expression of viral proteins in model systems for functional studies [75]. |
| Caspase-1 / IL-1β Detection Assays | Kits and reagents (e.g., ELISAs, fluorescent reporters) used to quantify NLRP3 inflammasome activation, a key immunopathological consequence of viroporin function [12]. |
| Variable-Length Markov Chain (VLMC) Software | Computational tools and algorithms for building genomic signature models from viral sequences and performing comparative analyses to assess specificity and evolution [75]. |
| AlphaFold or Similar AI-Driven Structural Prediction Platform | Enables accurate prediction of 3D protein structures from amino acid sequences, crucial for identifying potential viroporins and designing mutagenesis studies [12]. |
| Fluorescent Ion Indicators (e.g., Fluo-4) | Chemical dyes used in live-cell imaging to visualize and quantify changes in intracellular ion concentrations (e.g., Ca²⁺) caused by viroporin activity [12]. |
Technical Considerations for Studying Viral Persistence and Latency
Viral persistence and latency represent significant challenges in the management and cure of chronic viral infections. Latency is a state where a virus persists in a host cell in a reversible, non-productive form, creating a reservoir that is refractory to antiviral therapies and immune surveillance. The study of these reservoirs requires sophisticated technical approaches to understand their formation, maintenance, and reactivation mechanisms. This technical guide examines current methodologies and considerations for investigating viral persistence and latency, with a focus on HIV and other relevant viruses, providing researchers with practical frameworks for advancing therapeutic development.
Molecular Mechanisms of Viral Latency
HIV Latency Establishment and Maintenance
HIV-1 establishes a pool of latently infected cells early following infection, often before detectable viremia appears in blood [76]. The majority of HIV-infected cells die from viral cytopathic effects or immune-mediated clearance, but a small fraction transitions into long-lived latently infected resting cells that can persist for decades via homeostatic proliferation [76]. Multiple molecular mechanisms contribute to HIV latency maintenance:
- Transcription factor sequestration: Host transcription factors such as NF-κB, which contain multiple binding sites in the HIV-1 5' long terminal repeat (LTR), remain sequestered in the cytoplasm of resting cells, preventing transcription initiation [76].
- Epigenetic silencing: Histone deacetylases (HDACs) recruit to the 5' LTR of HIV-1, maintaining the promoter in a repressed state through chromatin remodeling [76]. HDAC inhibitors such as romidepsin can reverse this silencing.
- Transcriptional blocks: Even when transcription initiates, blocks to elongation, completion, and splicing prevent the production of full-length viral RNA and proteins in resting CD4+ T cells [77]. The HIV Transactivator of Transcription (Tat) protein, which normally amplifies transcription through recruitment of p-TEFb, is present at negligible levels in latently infected cells [78].
Comparative Viral Latency Mechanisms
Other viruses employ distinct strategies for persistence. Human cytomegalovirus (HCMV) establishes latency primarily in myeloid progenitor cells such as CD34+ cells and their CD14+ monocyte derivatives [79]. During HCMV latency, limited viral gene expression occurs without productive infection. Reactivation can happen during immune suppression, including pregnancy, leading to potential fetal transmission [79].
Table 1: Key Molecular Players in Viral Latency
| Molecular Factor | Virus | Function in Latency | Experimental Targeting |
|---|---|---|---|
| HDACs | HIV-1 | Epigenetic repression of LTR | HDAC inhibitors (Romidepsin) |
| NF-κB | HIV-1 | Transcriptional activation | TNF-α, PKC agonists |
| Tat protein | HIV-1 | Transcriptional transactivation | Tat mRNA delivery [80] |
| ICP34.5 | HSV-1 | Modulates HIV reactivation | Deletion enhances reversal [81] |
| HSF1 | HIV-1 | Binds HIV LTR | Phosphorylation increases binding |
| IFITM3 | Multiple | Viral restriction protein | SNP rs12252 affects severity [82] |
Quantitative Assessment of Viral Reservoirs
Accurate quantification of viral reservoirs is essential for evaluating persistence and therapeutic efficacy. Multiple assays have been developed with varying sensitivities and applications.
Established Reservoir Quantification Methods
- Viral Outgrowth Assays (VOA): The gold standard for measuring replication-competent HIV, though time-consuming and resource-intensive [76].
- Digital Droplet PCR (ddPCR): Enables precise quantification of viral DNA species, including integrated HIV DNA [76].
- Tat/Rev-Induced Limiting-Dilution Assay (TILDA): Measures inducible HIV RNA following T-cell activation, providing information on the inducible reservoir [76].
- Flow Cytometry-Based Detection: Novel approaches allow simultaneous detection of viral gagpol mRNA, intracellular p24 Gag protein, and cell surface markers at the single-cell level, enabling phenotypic characterization of infected cells [76].
Table 2: Quantitative Assays for Viral Persistence
| Assay Type | Target | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|
| Viral Outgrowth Assay | Replication-competent virus | ~1-10 infectious units per million | Gold standard for infectivity | Labor intensive, slow results |
| ddPCR | Viral DNA/RNA | 1-10 copies | Absolute quantification, high precision | Does not assess replication competence |
| TILDA | Inducible HIV RNA | ~0.5-2 infected cells/million | Measures inducible reservoir | Requires cell stimulation |
| Flow Cytometry | mRNA/protein | Single-cell level | Phenotypic characterization | Technical complexity |
| SPECT/PET Imaging | Whole-body localization | mm-cm resolution | Non-invasive, longitudinal | Limited molecular resolution [14] |
Emerging Imaging Approaches
Molecular imaging (MI) provides non-invasive, longitudinal assessment of viral persistence and pathogenesis. Key modalities include:
- Positron Emission Tomography (PET): Uses positron-emitting isotopes to detect functional processes with high sensitivity, though with limited spatial resolution [14].
- Single-Photon Emission Computerized Tomography (SPECT): Employs gamma-emitting radionuclides, allowing potential multi-isotope imaging to simultaneously track multiple biological targets [14].
- Metabolic Imaging: Probes like 18F-FDG monitor cellular glucose uptake, revealing sites of inflammation and infection before anatomical changes occur [14].
These techniques enable whole-body assessment of viral pathology, potentially identifying unexpected reservoirs and systemic effects, as demonstrated in COVID-19 where initial respiratory focus expanded to multi-system involvement [14].
Experimental Models and Systems
Cell Line Models
- J-Lat cells: Jurkat T-cell lines containing latent HIV-1 provirus with fluorescent reporters (e.g., GFP) under control of the HIV LTR, enabling rapid quantification of reactivation [81].
- J89 cells: Jurkat cell line infected with HIV-1, used for studying reactivation kinetics [76].
- ACH-2 cells: T-cell line latently infected with replication-competent HIV-1, allowing measurement of p24 production upon reactivation [81].
Primary Cell and Animal Models
- Primary CD4+ T cells from people with HIV (PWH): Critical for ex vivo validation studies, though refractory to traditional transfection methods [80].
- SIV-infected rhesus macaques: The primary non-human primate model for HIV cure research, allowing evaluation of therapeutic strategies in a physiologically relevant system [81].
- Humanized mouse models: Immunodeficient mice engrafted with human hematopoietic cells, supporting HIV infection and persistence studies [14].
Advanced Latency Reversal Strategies
"Shock and Kill" Paradigm
The "shock and kill" approach aims to reactivate latent virus using latency reversing agents (LRAs), followed by elimination of infected cells through viral cytopathic effects or immune-mediated clearance [77]. Current LRAs face challenges including insufficient potency, failure to induce multiply-spliced HIV RNA, and host toxicities.
Novel LRA Delivery Systems
Lipid Nanoparticles (LNPs) for mRNA Delivery
Recent advances in LNP technology enable efficient mRNA delivery to hard-to-transfect resting CD4+ T cells. A novel LNP formulation (LNP X) with SM-102 ionizable lipid and β-sitosterol achieves unprecedented transfection efficiency (up to 76%) in resting CD4+ T cells without cellular toxicity or activation [80]. This platform enables delivery of:
- Tat mRNA: HIV-specific LRA that potently upregulates multiply-spliced HIV RNA and viral protein production [80].
- CRISPR activation machinery: Enables targeted transcriptional activation of both viral and host genes [80].
LNP-mRNA Delivery and Tat-Mediated Activation
Viral Vector Approaches
HSV-ΔICP34.5, a modified herpes simplex virus with ICP34.5 deletion, demonstrates enhanced HIV latency reversal compared to wild-type HSV through two primary mechanisms:
- IKKα/β-NF-κB pathway: Enhanced phosphorylation of IKKα/β through degradation of IκBα, leading to p65 nuclear accumulation [81].
- PP1α-HSF1 pathway: Promotion of HSF1 phosphorylation by decreasing recruitment of protein phosphatase 1 (PP1α), enhancing binding to the HIV LTR [81].
HSV-ΔICP34.5 Reactivation Mechanism
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Viral Latency Studies
| Reagent/Cell Line | Function/Application | Key Features | Source/Reference |
|---|---|---|---|
| J-Lat 10.6 cells | In vitro HIV latency model | Contains latent HIV-1 provirus with GFP reporter | [76] [81] |
| J89 cells | HIV reactivation kinetics | Jurkat cell line infected with HIV-1 | [76] |
| ACH-2 cells | Latent HIV reactivation | Contains replication-competent HIV, measures p24 | [81] |
| LNP X | mRNA delivery to resting T cells | SM-102 + β-sitosterol formulation, high efficiency, low toxicity | [80] |
| Romidepsin (RMD) | HDAC inhibitor LRA | Induces histone H3 acetylation, reverses epigenetic silencing | [76] |
| hTNF-α | Proinflammatory cytokine LRA | Enhances NF-κB nuclear translocation | [76] |
| HSV-ΔICP34.5 | Viral vector for latency reversal | Enhanced reactivation via HSF1 & NF-κB pathways | [81] |
| SNAPswitch reporter | Quantifies subcellular localization | Measures cytosolic delivery efficiency | [80] |
| Anti-CD3/CD28 beads | T cell activation | Positive control for T cell stimulation | [76] |
Technical Protocols for Key Experiments
Flow Cytometry-Based Detection of Viral Reactivation
This protocol enables simultaneous detection of viral mRNA, protein, and surface markers at single-cell resolution [76]:
- Cell stimulation: Treat latently infected cells (e.g., J89, J-Lat) with LRAs (hTNF-α at 10μg/ml or RMD at 5nM) for specified durations (3-72 hours).
- Cell staining:
- Surface markers: Use anti-CD3 PE-CF594, anti-CD4 BV711, anti-BST-2 PE, anti-HLA-I Pacific Blue.
- Intracellular staining: Fix and permeabilize cells, then stain with anti-p24-FITC/PE.
- mRNA detection: Implement specific probe-based detection for gagpol mRNA.
- Flow cytometry analysis: Use a high-parameter flow cytometer capable of detecting 8+ colors. Analyze populations based on expression levels of viral mRNA and protein.
- Kinetic assessment: Collect timepoints from 3-72 hours post-stimulation to establish reactivation kinetics.
- LNP formulation:
- Ionizable lipid: SM-102
- Helper lipid: β-sitosterol
- PEG-lipid: DMG-PEG2000
- Prepare using microfluidic mixing at 1:3 aqueous:organic flow rate ratio
- mRNA encapsulation: Use clean cap mRNA technology for enhanced translation.
- Cell treatment:
- Isolate resting CD4+ T cells from healthy donors or PWH
- Treat with LNP X at doses ranging 6.25-500 ng per 10^5 cells
- Incubate for 72 hours in RPMI+10% FBS without stimulation
- Efficiency assessment:
- For reporter mRNA (mCherry): Analyze by flow cytometry
- For Tat mRNA: Measure HIV RNA induction by RT-qPCR or p24 production by ELISA
- Virus preparation: Generate HSV-ΔICP34.5 using BAC/galK system from parental HSV-GFP strain.
- Cell infection:
- Culture J-Lat 10.6 or ACH-2 cells at appropriate density
- Infect with HSV-ΔICP34.5 at MOI 0.1-5
- Include controls: mock infection, HSV-GFP, PMA (50ng/ml), TNF-α (10ng/ml)
- Readout measurement:
- For J-Lat 10.6: Analyze GFP expression by flow cytometry at 24-72 hours
- For ACH-2: Measure p24 in supernatant by ELISA
- For both: Quantify HIV transcript levels by RT-qPCR (Tat, Gag, Vif, Vpr, LTR-driven RNA)
- Mechanistic studies:
- Assess HSF1 phosphorylation by western blot
- Measure IκBα degradation and p65 nuclear translocation
- Evaluate PP1α recruitment to HSF1 by co-immunoprecipitation
The technical landscape for studying viral persistence and latency continues to evolve with advancements in delivery systems, imaging modalities, and analytical techniques. Critical considerations include selecting appropriate model systems that reflect physiological conditions, implementing orthogonal assessment methods to fully characterize reservoirs, and developing targeted strategies that overcome the multiple blocks to viral expression in latent cells. The integration of novel tools such as LNPs for nucleic acid delivery, advanced imaging for reservoir localization, and sophisticated viral vectors provides unprecedented opportunities to interrogate and ultimately eliminate persistent viral reservoirs.
Cross-Viral Analysis: Validating Pathogenesis Mechanisms Through Comparative Virology
Viral entry into host cells is the foundational step in establishing infection and disease. This process, mediated by specific interactions between viral surface proteins and host cell receptors, defines viral tropism, pathogenicity, and cross-species transmission potential. Understanding the precise molecular mechanisms of receptor usage is therefore critical for developing broad-spectrum antiviral therapies and vaccines. This whitepaper provides a comparative analysis of the entry mechanisms employed by three major viral families: Coronaviruses (focusing on SARS-CoV-2), Influenza viruses, and Human Immunodeficiency Virus (HIV). We delineate the primary and alternative receptors, the structural basis of viral-receptor interactions, and the proteolytic priming events required for successful entry. Furthermore, we summarize key experimental methodologies for studying these processes and provide a toolkit of essential research reagents. The insights gathered here aim to inform and accelerate research in viral pathogenesis and the design of novel intervention strategies.
Viral entry represents the first critical stage of infection, wherein a virus introduces its genetic material into a host cell. For enveloped viruses, including coronaviruses, influenza viruses, and HIV, this process is mediated by viral envelope glycoproteins that recognize and bind to specific receptors on the host cell surface. This binding triggers a series of conformational changes and proteolytic events that culminate in the fusion of the viral and host membranes.
The specificity of this receptor interaction is a primary determinant of a virus's host range, tissue tropism, and pathogenicity. The molecular details of these interactions vary significantly across virus families, reflecting diverse evolutionary strategies. Coronaviruses like SARS-CoV-2 primarily utilize the angiotensin-converting enzyme 2 (ACE2) receptor, with entry efficiency modulated by host proteases such as TMPRSS2 [83] [5]. Influenza viruses bind to sialic acid residues on host cell surface glycoproteins and glycolipids, with their hemagglutinin (HA) protein mediating both receptor binding and membrane fusion [84] [85]. In contrast, HIV-1 engages a two-step receptor mechanism, initially binding the CD4 receptor on T-cells, which induces conformational changes that allow for subsequent interaction with a coreceptor, typically CCR5 or CXCR4 [86] [87]. The following sections provide a detailed, comparative examination of these distinct entry pathways.
Coronavirus Entry: ACE2 and Beyond
Primary Receptor: ACE2 and Protease Priming
SARS-CoV-2, the causative agent of COVID-19, gains cellular entry primarily through its spike (S) glycoprotein binding to the host receptor angiotensin-converting enzyme 2 (ACE2) [5] [88]. ACE2 is a type I transmembrane protein expressed in various tissues, including vascular endothelium, renal and cardiovascular systems, and, at lower levels, the respiratory tract [5]. The S protein is a trimeric structure composed of two functional subunits: S1, which contains the receptor-binding domain (RBD) responsible for ACE2 recognition, and S2, which facilitates membrane fusion [5].
Following receptor binding, host proteases are essential for priming the S protein to enable fusion. The transmembrane serine protease 2 (TMPRSS2) is a key host protease that cleaves the S protein, triggering irreversible conformational changes that release the fusion peptide [83] [5]. The entry process can also involve endocytic pathways where the S protein is cleaved by endosomal cathepsins (e.g., cathepsin B and L) [83]. Beyond ACE2 and TMPRSS2, other host factors such as ADAM17 (which cleaves ACE2 to produce a soluble form) and Furin (which pre-cleaves the S protein during viral egress) also play significant regulatory roles in viral entry and pathogenesis [83] [5].
Alternative and Candidat`e Co-receptors
While ACE2 is the primary receptor, studies suggest that SARS-CoV-2 may utilize alternative receptors or co-receptors to facilitate entry, particularly in cells with low ACE2 expression. These include Basigin (BSG or CD147), Dipeptidyl peptidase 4 (DPP4), and Neuropilin-1 (NRP1) [83] [89]. The expression of this repertoire of receptors on cells of the neurovascular unit, such as astrocytes and microglia, provides a potential pathway for SARS-CoV-2 to infect the central nervous system, leading to neurological complications [83]. Furthermore, pre-existing conditions can modulate this process; for instance, HIV-1 infection has been shown to upregulate ACE2 and TMPRSS2 expression in brain astrocytes and microglial cells, potentially increasing their susceptibility to SARS-CoV-2 [83].
Table 1: Key Host Factors in Coronavirus SARS-CoV-2 Entry
| Host Factor | Function in Viral Entry | Experimental Evidence |
|---|---|---|
| ACE2 | Primary receptor; binds Spike RBD [5] [88] | VSV pseudotypes with SARS-CoV-2 Spike enter ACE2-expressing cells [88] |
| TMPRSS2 | Prime Spike protein for membrane fusion [83] [5] | Protease inhibition blocks entry; exogenous protease rescues entry of some lineage B viruses [88] |
| ADAM17 | Sheds ACE2, potentially regulating receptor availability [5] | Gene and protein expression analysis in NVU cells [83] |
| BSG (CD147) | Proposed alternative receptor/co-receptor [83] [89] | Expression profiling in primary human cells (e.g., astrocytes, pericytes) [83] |
| Cathepsin B/L | Prime Spike protein in endosomal pathway [83] | Cathepsin inhibitors block viral entry in TMPRSS2-low cell lines [83] |
Influenza Virus Entry: Sialic Acid as a Gateway
Hemagglutinin and Receptor Specificity
Influenza A and B viruses (FLUAV and FLUBV) initiate infection by binding to sialic acids (SAs) on the surface of host cells. This interaction is mediated by the viral hemagglutinin (HA) protein, which recognizes sialic acids linked to galactose via α-2,6 or α-2,3 linkages [85]. The preference for specific linkages is a major determinant of host tropism. Human-adapted influenza viruses typically prefer α-2,6-linked SAs, which are predominant in the human upper respiratory tract, whereas avian viruses preferentially bind α-2,3-linked SAs [85].
The receptor-binding site (RBS) of HA is subject to antigenic drift, but its fundamental function constrains its variability. Recent research on Influenza B viruses has identified an N-glycosylation site at amino acid 196 within the HA RBS as a critical regulator of receptor binding specificity [84]. The presence or absence of this glycan determines the breadth of HA binding to different sialic acid types and helps explain the distinct tropism and epidemiological success of the Victoria lineage compared to the Yamagata lineage [84].
Neuraminidase and the Role of Receptor-Destroying Activity
The other major surface glycoprotein, neuraminidase (NA), plays a complementary yet antagonistic role to HA. NA is a sialidase enzyme that cleaves sialic acids from glycoconjugates, thereby facilitating the release of progeny virions from infected cells and preventing viral self-aggregation [85]. The highly conserved active site of NA has emerged as a promising target for broadly protective antibodies. These antibodies, such as DA03E17, often use a long complementarity-determining region H3 (CDR H3) featuring an Asp–Arg (DR) motif that mimics the sialic acid receptor, effectively blocking the enzyme's active site and inhibiting viral egress [85]. This convergent mechanism of receptor mimicry represents a key avenue for universal influenza vaccine design.
Table 2: Key Viral and Host Factors in Influenza Virus Entry and Egress
| Factor | Type | Function in Viral Lifecycle |
|---|---|---|
| Hemagglutinin (HA) | Viral glycoprotein | Mediates receptor binding (to sialic acids) and subsequent membrane fusion [85] |
| Sialic Acids (α-2,6 / α-2,3) | Host receptor | Terminal sugars on host glycoproteins/glycolipids; binding determinant for HA [85] |
| Neuraminidase (NA) | Viral glycoprotein | Cleaves sialic acids ("receptor-destroying enzyme") to facilitate viral release [85] |
| N-glycosylation site 196 | Viral HA modification | Determines receptor binding specificity in Influenza B virus lineages [84] |
| TMPRSS2 / Host Proteases | Host protease | Cleaves and primes HA for membrane fusion activity [5] |
HIV-1 Entry: A Two-Step Receptor Mechanism
CD4 Binding and Coreceptor Engagement
HIV-1 entry is a sophisticated, multi-step process orchestrated by the viral envelope glycoprotein (Env) trimer, composed of three gp120 and three gp41 subunits. The entry mechanism is distinct from that of coronaviruses and influenza viruses, involving a two-receptor sequential engagement [86] [87]. The initial step is the high-affinity binding of gp120 to the primary receptor, CD4, on the surface of helper T-cells and other immune cells. This interaction induces major conformational changes in gp120, exposing and stabilizing its V3 loop, which is critical for the next step [86].
The exposed V3 loop then engages a coreceptor, which is typically one of the G-protein coupled receptors (GPCRs), CCR5 or CXCR4 [87]. This engagement triggers further conformational changes in the gp41 subunit, leading to the insertion of its fusion peptide into the host cell membrane and the formation of a stable six-helix bundle that drives the fusion of the viral and cellular membranes [86]. The choice of coreceptor has significant clinical implications; viruses that use CCR5 (R5-tropic) are associated with primary infection, while the emergence of viruses that use CXCR4 (X4-tropic) is often linked to accelerated disease progression.
Structural Insights and Comparative Entry with HIV-2
Recent cryo-electron microscopy (cryo-EM) studies have provided high-resolution views of the HIV-Env complex with its receptors. A key finding is that CXCR4 can form a tetrameric complex when binding to the HIV-2 Env spike [87]. The structure reveals that the V3 loop of gp120 inserts deeply into the major sub-pocket of the CXCR4 tetramer, with a conserved GFKF motif within V3 playing a central role [87]. The natural CXCR4 ligand, CXCL12, inhibits HIV entry because its N-terminus clashes sterically with the V3 loop, preventing coreceptor engagement [87].
While HIV-2 also uses CD4 and coreceptors for entry, it is known to engage a broader range of chemokine receptors than HIV-1. Furthermore, recent research implicates the transferrin receptor (TFRC/CD71) as a novel, Tat-dependent host target of HIV-2. HIV-2 transduction modulates TFRC expression and leads to elevated intracellular iron levels, suggesting a potential link between viral entry and host iron metabolism that is not observed with HIV-1 [90].
Experimental Protocols for Studying Viral Entry
Pseudotyping and Cell Entry Assays
A powerful and versatile method for studying viral entry, particularly for highly pathogenic viruses, is the use of pseudotyped viruses. This approach allows for the investigation of receptor usage and tropism without requiring biosafety level 3 (BSL-3) or BSL-4 containment.
Protocol: VSV Pseudotype Entry Assay for Coronaviruses [88]
- RBD Cloning: Synthesize and clone the receptor-binding domain (RBD) from the coronavirus spike protein of interest into a chimeric spike expression construct, replacing the native RBD (e.g., in a SARS-CoV spike backbone).
- Virus Production: Co-transfect the chimeric spike plasmid with a VSV vector that lacks its native G glycoprotein (VSV-ΔG) and carries a reporter gene (e.g., luciferase or GFP) into producer cells (e.g., HEK-293T).
- Pseudotype Purification: Collect the supernatant containing VSV pseudotypes bearing the chimeric spike protein.
- Cell Infection: Incubate pseudotypes with target cells expressing the putative receptor (e.g., ACE2) or control cells.
- Entry Quantification: Measure reporter gene activity (e.g., luminescence) after 24-48 hours to quantify viral entry. Protease dependence can be assessed by adding exogenous protease (e.g., trypsin) during infection.
This method was instrumental in rapidly confirming ACE2 as the receptor for the newly emerged SARS-CoV-2 and in functionally profiling the receptor compatibility of other lineage B betacoronaviruses [88].
Gene Expression and Protein Analysis
To validate the presence of viral receptors and associated host factors in specific cell types or tissues, gene and protein expression profiling is essential.
Protocol: Expression Profiling in Primary Cells [83]
- Cell Culture: Maintain relevant primary human cells (e.g., brain microvascular endothelial cells, astrocytes, pericytes, microglia) under optimized conditions.
- Stimulation/Infection: Expose cells to viral components (e.g., SARS-CoV-2 S1 subunit) or infect with a virus of interest (e.g., HIV-1).
- RNA Extraction and qPCR: Extract total RNA and perform quantitative real-time PCR (qPCR) using primers specific for the genes of interest (e.g., ACE2, TMPRSS2, BSG) to assess transcript levels.
- Protein Analysis: Perform immunoblotting (Western blot) or immunostaining on cell lysates to confirm protein expression and localization.
This methodology demonstrated that SARS-CoV-2-related receptors are co-expressed in neurovascular unit cells and that HIV-1 infection can modulate their expression levels [83].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for Viral Entry Studies
| Reagent / Assay | Function / Application | Example Use Case |
|---|---|---|
| VSV-ΔG Backbone | Production of pseudotyped viruses for safe study of entry [88] | Profiling receptor usage of novel coronavirus spikes [88] |
| Reporter Genes (Luciferase/GFP) | Quantification of viral entry efficiency | Measured in target cells after infection with pseudotypes [88] |
| Recombinant Soluble Proteins | Structural studies, binding affinity measurements (SPR, ELISA) | Cryo-EM of CXCR4-gp120 complexes [87]; ELISA for antibody binding to NA [85] |
| qPCR Primers / Antibodies | Detection of receptor gene and protein expression | Profiling ACE2/TMPRSS2 in primary human cells [83] |
| Enzyme-Linked Lectin Assay (ELLA) | Functional assessment of neuraminidase activity and inhibition | Characterizing broad anti-influenza NA antibodies like DA03E17 [85] |
| Cathepsin / Protease Inhibitors | Dissecting entry pathway (plasma membrane vs. endosomal) | Blocking SARS-CoV-2 entry via the endosomal pathway [83] |
Visualizing Viral Entry Pathways and Experimental Workflows
The following diagrams illustrate the core entry mechanisms of the three virus families and a key experimental workflow.
Coronavirus SARS-CoV-2 Entry Mechanism
Influenza Virus Entry and Release Cycle
HIV-1 Two-Step Entry Mechanism
Workflow: VSV Pseudotype Entry Assay
Viral pathogenesis is fundamentally shaped by the evolutionary arms race between host immune defenses and viral countermeasures. The constant selective pressure exerted by the innate and adaptive immune system has driven viruses to develop sophisticated strategies to evade detection and neutralization. Understanding these mechanisms is not only crucial for fundamental virology but also for the development of novel antiviral therapeutics and vaccines. This review provides a systematic comparison of immune evasion strategies employed by three major viral families: Herpesviridae, Poxviridae, and Flaviviridae. These families represent distinct evolutionary paths and biological niches, yet their evasion strategies reveal both convergent evolution and unique adaptations. Herpesviruses establish lifelong persistent infections through sophisticated latency programs and immune modulation. Poxviruses, with their large DNA genomes, encode numerous proteins dedicated to host immune subversion. Flaviviruses, despite their compact RNA genomes, efficiently counteract immune responses primarily through multifunctional non-structural proteins. By examining the molecular mechanisms these viruses use to circumvent host defenses, we can identify vulnerable points in their replication cycles that may be targeted for therapeutic intervention.
Table 1: Comparative immune evasion strategies across viral families
| Immune Component | Herpesviruses | Poxviruses | Flaviviruses |
|---|---|---|---|
| DNA Sensing (cGAS-STING) | HSV-1 induces miR-24 to inhibit STING translation [91]; KSHV K3/K5 downregulate MHC-I [92] | Encodes cGAMP-specific nuclease (poxin) to degrade secondary messenger [93]; C10 protein inhibits DNA-PK [94] | NS5 protein inhibits STAT signaling [95] [96] [97]; NS2B3 protease cleaves human STING [97] |
| RNA Sensing (RIG-I/MDA5) | Limited information in search results | Limited information in search results | NS5, NS4B, and NS2B3 proteins inhibit RIG-I/MDA5 signaling pathways [97] |
| Antigen Presentation (MHC-I) | EBV BNLF2A inhibits TAP; BILF1 downregulates surface MHC-I [92] | Multiple mechanisms including intracellular retention of MHC-I [98] | Downregulation of surface MHC-I through indirect mechanisms [98] |
| Apoptosis | vFLIP activates NF-κB; vBcl-2 inhibits mitochondrial apoptosis [92] | Encode multiple inhibitors including F1L, B13R, and N1L proteins [98] | NS2A and NS3 induce ER stress-mediated apoptosis; conflicting roles reported [97] |
| Complement System | gC-1 binds C3b; gC-2 and gE/gI interfere with antibody binding [98] | VCP and SPICE proteins act as complement regulators [98] | NS1 protein binds complement factors; secretes from cells to inhibit activation [98] [97] |
| Interferon Signaling | Multiple mechanisms including inhibition of IRF3 activation and IFN receptor signaling [99] | Soluble IFN-γ receptor homologs; inhibition of IFN-induced antiviral proteins [98] | NS5 inhibits STAT phosphorylation and nuclear translocation; NS4B blocks IFNAR signaling [97] |
Table 2: Key viral immune evasion proteins and their functions
| Virus Family | Protein | Function in Immune Evasion |
|---|---|---|
| Herpesviruses | HSV-1 miR-24 | Targets STING mRNA for translational inhibition [91] |
| KSHV K3/K5 | MARCH-family ubiquitin ligases that downregulate MHC-I [92] | |
| EBV BNLF2A | Inhibits TAP-mediated peptide transport [92] | |
| EBV BILF1 | GPCR that induces endocytosis of MHC-I [92] | |
| vFLIP/vBcl-2 | Inhibits death receptor and mitochondrial apoptosis pathways [92] | |
| Poxviruses | Poxin (B2R) | cGAMP-specific nuclease that degrades secondary messenger [93] |
| C10/C16 | Binds Ku subunits of DNA-PK to inhibit IRF3 activation [94] [93] | |
| VCP/SPICE | Complement control proteins that inhibit C3 convertase [98] | |
| Flaviviruses | NS5 | Multifunctional: inhibits STAT signaling and possesses RdRp/MTase activities [95] [96] [97] |
| NS2B3 | Serine protease complex that cleaves human STING [97] | |
| NS1 | Secreted protein that inhibits complement activation and TLR signaling [97] | |
| NS4A/B | Induces membrane rearrangement and inhibits IFN signaling [97] |
Herpesviruses: Masters of Latency and Stealth
Evasion of DNA Sensing and Innate Signaling
Herpesviruses have developed sophisticated mechanisms to evade detection by cytosolic DNA sensors. Herpes Simplex Virus 1 (HSV-1) induces the expression of cellular microRNA-24 (miR-24) through AP-1 transcription factor activation, which subsequently binds to the 3' untranslated region of STING mRNA and inhibits its translation [91]. This novel mechanism allows HSV-1 to attenuate the cGAS-STING pathway, a central defense against DNA viruses. Additionally, different herpesviruses target various steps in the DNA sensing pathway. For instance, human cytomegalovirus (HCMV) protein pp65 inhibits IFI16 oligomerization and subsequent signaling, while Kaposi's sarcoma-associated herpesvirus (KSHV) protein ORF52 binds to and inhibits cGAS activity directly [99].
Modulation of Adaptive Immune Responses
Herpesviruses excel at evading adaptive immunity through precise manipulation of antigen presentation. During latency, Epstein-Barr virus (EBV) limits the expression of viral antigens to avoid T-cell recognition. EBNA-1, the main latency protein, contains glycine-alanine repeats that inhibit its own proteasomal degradation and subsequent MHC-I presentation [92]. Similarly, KSHV LANA-1 contains repeat regions that enhance protein stability and reduce antigen presentation [92]. During lytic replication, multiple herpesviruses encode proteins that downregulate MHC-I molecules. EBV produces BNLF2A, which inhibits the TAP peptide transporter, and BILF1, which induces endocytosis of surface MHC-I [92]. KSHV encodes K3 and K5, MARCH-family ubiquitin ligases that target MHC-I for degradation [92].
Inhibition of Apoptosis and Complement
Herpesviruses encode homologs of cellular anti-apoptotic proteins to ensure survival of infected cells. Viral FLIP (vFLIP) proteins interfere with death receptor signaling by preventing the assembly of the death-inducing signaling complex (DISC), while simultaneously activating NF-κB to promote cell survival [92]. Viral Bcl-2 (vBcl-2) proteins inhibit mitochondrial apoptosis but lack the regulatory domains that make their cellular counterparts susceptible to caspase-mediated conversion to pro-apoptotic proteins [92]. To counter the complement system, herpesviruses such as HSV-1 encode glycoprotein C (gC-1) which binds C3b and inhibits complement activation, while gE/gI complexes interfere with antibody binding and complement activation [98].
Poxviruses: Cytoplasmic Replicators with Extensive Immunomodulatory Arsenals
Cytoplasmic DNA Sensing Evasion
Poxviruses replicate exclusively in the cytoplasm, making them particularly vulnerable to detection by cytosolic DNA sensors. To counteract this, they encode numerous proteins that target the DNA sensing pathway. The recently identified poxins (poxvirus immune nucleases), such as the B2R protein in vaccinia virus (VACV), are cGAMP-specific nucleases that degrade the secondary messenger produced by cGAS, thereby preventing STING activation [93]. Deletion of the B2R gene results in enhanced IRF3 phosphorylation and type I interferon expression without affecting viral replication [93]. Additionally, VACV protein C10 (C16 in the WR strain) binds the Ku subunits of DNA-PK, inhibiting IRF3 activation and IFN production [94] [93]. These multi-layered defenses allow poxviruses to effectively hide their genomic DNA from host surveillance systems.
Complement System Subversion
Poxviruses encode some of the most effective complement evasion proteins known. The vaccinia virus complement control protein (VCP) is a secreted protein that structurally and functionally resembles human complement regulatory proteins [98]. It binds both C3b and C4b and acts as a cofactor for their factor I-mediated degradation. Variola virus, the causative agent of smallpox, encodes a more potent version called SPICE (smallpox inhibitor of complement enzymes), while monkeypox virus encodes MOPICE [98]. These proteins inhibit the central C3 convertase of the complement cascade, preventing downstream effector functions including opsonization and formation of the membrane attack complex.
Flaviviruses: Compact Genomes with Multifunctional Antagonists
NS5: A Multifunctional Master Regulator of Immune Evasion
The flavivirus non-structural protein 5 (NS5) represents one of the most versatile viral immune evasion proteins known. NS5 is the largest and most conserved flaviviral protein, containing an N-terminal RNA methyltransferase (MTase) domain and a C-terminal RNA-dependent RNA polymerase (RdRp) domain [95] [96]. Beyond its essential roles in viral replication, NS5 potently inhibits type I interferon signaling by preventing STAT phosphorylation and nuclear translocation [95] [96] [97]. The mechanisms vary between flaviviruses: dengue virus (DENV) NS5 binds and degrades STAT2, while Zika virus (ZIKV) NS5 targets both STAT1 and STAT2 for degradation [96]. This direct antagonism of the JAK-STAT pathway allows flaviviruses to circumvent the antiviral state established by interferon.
Evasion of RNA Sensing and Complement Activation
Flaviviruses counteract cytoplasmic RNA sensing through several non-structural proteins. The NS2B3 protease complex of multiple flaviviruses cleaves human STING, but not murine STING, providing a species-specific mechanism to inhibit IFN production [97]. NS4B of DENV and WNV inhibits RIG-I/MDA5 signaling by targeting the MAVS adaptor protein [97]. Additionally, flavivirus NS1 proteins inhibit complement activation through multiple mechanisms. Secreted NS1 binds to complement factors and regulators, while membrane-associated NS1 recruits factor H to inactivate C3b [98] [97]. For DENV, NS1 can also activate TLR4, contributing to the excessive immune activation seen in severe dengue disease [97].
Experimental Approaches for Studying Immune Evasion
Protocol: Assessing cGAS-STING Evasion by Poxviral Poxin
Objective: Evaluate the impact of viral cGAMP-specific nuclease (poxin) on cGAS-STING signaling.
Materials:
- Wild-type and B2R-deleted vaccinia virus (VACV ΔB2R) [93]
- THP-1 cells or primary murine dendritic cells
- Phospho-IRF3 specific antibody [93]
- Type I IFN ELISA kit
- cGAMP quantification assay
Methodology:
- Infect cells at MOI of 10 with wild-type VACV or VACV ΔB2R
- Harvest cells 5 hours post-infection for protein analysis
- Detect phosphorylated IRF3 by Western blot using phospho-specific antibody
- Measure IFN-α/β production in supernatant by ELISA
- Quantify intracellular cGAMP levels using commercial assay kits
- Compare signaling activation between wild-type and mutant virus infections
Expected Results: Cells infected with VACV ΔB2R show enhanced IRF3 phosphorylation, increased type I IFN production, and higher cGAMP accumulation compared to wild-type VACV infection [93].
Protocol: Evaluating microRNA-Mediated Immune Evasion in Herpesviruses
Objective: Investigate HSV-1-induced miR-24 regulation of STING expression.
Materials:
- HSV-1 wild-type and replication-competent mutants
- AntimiR-24 and control oligonucleotides [91]
- Luciferase reporter construct with STING 3'UTR
- STING-specific antibody for Western blot
Methodology:
- Transfert cells with antimiR-24 or control oligonucleotides
- Infect with HSV-1 24 hours post-transfection
- Measure STING protein levels by Western blot at various time points
- Co-transfect luciferase-STING-3'UTR reporter with miR-24 mimics
- Assess luciferase activity to confirm direct targeting
- Evaluate viral replication by plaque assay in antimiR-24 treated cells
Expected Results: HSV-1 infection induces miR-24 expression, leading to decreased STING protein levels. AntimiR-24 treatment restores STING expression and reduces viral replication [91].
Research Reagent Solutions
Table 3: Essential research reagents for studying viral immune evasion
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Viral Mutants | VACV ΔB2R (poxin deletion) [93] | Study cGAS-STING pathway evasion mechanisms |
| HSV-1 miR-24 target site mutants | Investigate microRNA-mediated regulation of host defense | |
| Inhibitors & Agonists | cGAMP (STING agonist) | Activate DNA sensing pathway independently of viral infection |
| AntimiR-24 oligonucleotides [91] | Counteract viral induction of immunosuppressive microRNAs | |
| Antibodies | Phospho-IRF3 (S396) specific antibody [93] | Detect activation of IRF3 signaling pathway |
| NS5-specific monoclonal antibodies | Study flavivirus protein localization and function | |
| Reporter Systems | Luciferase-STING-3'UTR reporter [91] | Screen for microRNAs targeting STING expression |
| IFN-β promoter luciferase reporter | Quantify innate immune pathway activation | |
| Cell Lines | STING-deficient cells | Determine STING-dependent versus independent effects |
| IFNAR-knockout cells | Assess interferon signaling requirements |
Signaling Pathways in Viral Immune Evasion
Diagram 1: Viral evasion of host immune pathways. This diagram illustrates how herpesviruses (red), poxviruses (blue), and flaviviruses (green) target key nodes in host immune signaling pathways. Herpesviruses predominantly target DNA sensing and antigen presentation, poxviruses specialize in DNA sensing inhibition, while flaviviruses primarily interfere with RNA sensing and interferon signaling.
The comparative analysis of immune evasion strategies across herpesviruses, poxviruses, and flaviviruses reveals both conserved themes and unique adaptations shaped by viral biology and evolutionary history. Herpesviruses employ long-term stealth strategies optimized for persistence, with sophisticated mechanisms for maintaining latency and avoiding T-cell detection. Poxviruses utilize their large genomic capacity to encode numerous proteins dedicated to immune subversion, particularly targeting the cytoplasmic DNA sensing pathway. Flaviviruses, despite compact genomes, efficiently counteract host defenses through multifunctional proteins like NS5 that simultaneously perform replication and immune evasion functions.
From a therapeutic perspective, viral immune evasion proteins represent attractive targets for intervention. The conservation of NS5 across flaviviruses makes it a promising target for broad-spectrum antivirals [95] [96]. Similarly, the cGAMP-specific nuclease activity of poxins presents a unique enzymatic target that could be inhibited to enhance immune recognition of poxviral infections [93]. For herpesviruses, the microRNA-based regulatory mechanisms such as miR-24 induction could be countered with antisense oligonucleotides, as demonstrated by the protective effects of antimiR-24 in mouse models of HSV-1 infection [91].
Future research should focus on structural characterization of viral immune evasion proteins complexed with their host targets, which would facilitate structure-based drug design. Additionally, studying how these immune evasion mechanisms contribute to pathogenesis in animal models will help prioritize the most promising therapeutic targets. As our understanding of viral immune evasion deepens, so too will our ability to develop countermeasures that restore effective immune control of viral infections.
This technical guide provides a comparative analysis of the pathogenesis mechanisms employed by three distinct categories of neurotropic viruses: Herpes Simplex Virus (HSV), Zika virus, and Alphaviruses. Understanding these contrasting pathways is fundamental to developing targeted therapeutic interventions for viral neurological diseases. The table below summarizes the core pathogenic characteristics of each virus group.
Table 1: Comparative Pathogenesis of Neurotropic Viruses
| Feature | Herpes Simplex Virus (HSV) | Zika Virus (ZIKV) | Encephalitic Alphaviruses |
|---|---|---|---|
| Virus Family | Herpesviridae | Flaviviridae | Togaviridae |
| Genome | Double-stranded DNA | Single-stranded positive-sense RNA | Single-stranded positive-sense RNA |
| Primary Entry Mechanism | Direct neuronal retrograde transport; membrane fusion via gB/gH/gL glycoproteins [100] [101] | Hematogenous spread; disruption of blood-brain barrier (BBB) [102] [103] | Hematogenous or olfactory route; direct infection of BBB-lacking areas [104] |
| Cellular Targets in CNS | Sensory neurons, astrocytes [105] [103] | Neuronal cells, glial cells, neural progenitor cells [106] [107] | Neurons, astrocytes, microglia, oligodendrocytes [104] |
| Immune Evasion Strategy | Establishes lifelong latency in neurons; suppresses IRF1 expression [105] [103] | Suppresses IFN response via SOCS3; modulates TLR3 response [107] | Rapid neuroinvasion; induces neuroinflammation and oxidative stress [106] [104] |
| Key Neuropathogenic Sequelae | Encephalitis, neurodevelopmental & neurodegenerative impairment [105] | Microcephaly, Guillain-Barré syndrome, long-term neurological deficits [106] [102] | Permanent neurological sequelae (paralysis, seizures, intellectual disability) [108] [104] |
Neurotropic viruses present a significant challenge to global health due to their capacity to invade the central nervous system (CNS) and cause debilitating acute and chronic neurological diseases. These viruses exploit a variety of mechanisms to bypass host barrier systems, including the blood-brain barrier (BBB), and establish infection within the vulnerable CNS environment [106]. The ensuing neuropathogenesis is a complex interplay between direct viral-mediated damage and the host's immune response, which can often contribute to pathology. This whitepaper delineates the contrasting molecular and immunological mechanisms underlying the pathogenesis of three model neurotropic viruses: HSV, Zika virus, and Alphaviruses. A foundational understanding of these distinct strategies is critical for researchers and drug development professionals aiming to design targeted antivirals, vaccines, and host-directed therapies to mitigate the substantial burden of viral encephalitis and other virus-induced neurological disorders.
Pathogenic Mechanisms and Host Interactions
The journey of a neurotropic virus from peripheral infection to CNS establishment involves a series of meticulously orchestrated steps, each presenting a potential target for therapeutic intervention.
Viral Entry and CNS Invasion
The initial step in neuropathogenesis is the successful entry of the virus into the nervous system, which occurs through distinct routes for different viruses.
Herpes Simplex Virus (HSV) leverages its ability to establish latency in sensory ganglia. During primary infection, HSV enters peripheral sensory nerve endings and undergoes retrograde axonal transport to the neuronal cell body. A key molecular mechanism for host cell entry involves the viral glycoprotein B (gB), which is "energy-charged" and mediates the fusion of the viral envelope with the host cell membrane [100]. This process is essential for releasing the viral genetic material into the cytoplasm. The virus can subsequently reactivate from this latent state and travel back along the nerve to the site of initial infection, or in severe cases, spread into the CNS [105].
Zika Virus (ZIKV), in contrast, primarily employs a hematogenous route. After a mosquito bite, the virus replicates in peripheral tissues leading to viremia. ZIKV then compromises the integrity of the BBB, potentially through infection of endothelial cells or by inducing a pro-inflammatory state that increases barrier permeability. Recent studies also highlight the role of gut microbiome dysbiosis in ZIKV pathogenesis. Infection can reduce gut barrier integrity, leading to microbial translocation and systemic inflammation that is associated with elevated inflammatory markers in the CNS [102].
Encephalitic Alphaviruses (e.g., EEEV, VEEV, WEEV) utilize multiple entry points. Natural infection via a mosquito bite involves subcutaneous exposure and subsequent viremia. The virus can cross the BBB, which becomes disrupted due to viral replication and the host immune response [104]. However, these viruses are also capable of direct neuroinvasion via the olfactory system, especially upon aerosol or intranasal exposure, allowing them to bypass the BBB entirely by infecting olfactory sensory neurons [104].
Cellular Tropism and Inflammatory Signaling
Once inside the CNS, these viruses display specific cellular tropism, targeting different cell types and triggering unique inflammatory cascades that dictate disease pathology.
HSV primarily targets sensory neurons and astrocytes [105] [103]. A critical host factor in controlling HSV replication in astrocytes is Interferon Regulatory Factor 1 (IRF1). Experimental evidence shows that HSV-1 actively suppresses IRF1 expression to evade the host's innate immune response. IRF1 knockout cell lines result in increased expression of HSV-1 genes, whereas IRF1 overexpression enhances the inhibition of HSV-1 replication [103]. This suggests that HSV-1 has evolved mechanisms to counteract this specific antiviral pathway.
Zika Virus exhibits a broad cellular tropism within the CNS, infecting neuronal cells, glial cells, and critically, neural progenitor cells (NPCs) [106] [107]. This tropism for NPCs is a key mechanism underlying the severe neurodevelopmental defects like microcephaly. The host's Toll-like receptor (TLR) response, particularly TLR3, plays a complex and pivotal role in ZIKV pathogenesis. ZIKV infection induces TLR3 expression, which can lead to enhanced inflammation and viral replication in astrocytes. Conversely, inhibition of TLR3 expression reduces viral replication, suggesting a TLR3-mediated pathogenic pathway [107]. Furthermore, ZIKV infection can enhance TLR3-mediated inflammatory cytokine production while suppressing the interferon response triggered by other intracellular sensors (RLRs), facilitating viral replication [107].
Encephalitic Alphaviruses target a wide array of CNS cells, including neurons, astrocytes, microglia, and oligodendrocytes [104]. The neuropathology is driven by a combination of direct virus-induced cytopathy and a robust host inflammatory response. Viral replication, coupled with the activation of microglia and infiltrating immune cells, leads to the release of proinflammatory cytokines and chemokines (e.g., TNF-α, IL-6). This "cytokine storm" contributes to neurodegeneration through oxidative stress and excitotoxicity, causing widespread neuronal damage and cell death [106] [104].
Diagram 1: Neuroinflammatory signaling pathways. Contrasts pro-inflammatory ZIKV and Alphavirus pathways with HSV's immune suppression strategy.
Experimental Models and Methodologies
Preclinical models are indispensable for elucidating the detailed pathogenesis of neurotropic viruses and for the evaluation of potential vaccines and antivirals.
In Vivo Animal Models
Animal models recapitulating human disease are crucial for translational research.
Non-Human Primates (NHPs) and Zika Virus: NHP models are considered physiologically relevant for studying ZIKV pathogenesis. Experimental protocols involve subcutaneous inoculation to mimic a mosquito bite. These models are used to study viral persistence, neuroinflammation, and pathogenesis. For instance, studies in ZIKV-infected macaques have demonstrated elevated markers of inflammation and microbial translocation in the CNS, correlated with a reduction in gut-derived short-chain fatty acids (SCFAs) [102]. This model is vital for investigating the link between gut dysbiosis and neurological pathology.
Mouse Models and Encephalitic Alphaviruses: Mice are widely used to study alphavirus neuropathogenesis due to their susceptibility and the availability of transgenic strains. Standard protocols involve exposure via subcutaneous (mimicking mosquito bite), intranasal, or aerosol routes [104]. The latter two are considered gold standards for testing medical countermeasures as they often lead to direct and robust CNS infection. These models have been instrumental in identifying host factors critical for viral entry, such as the very-low-density lipoprotein receptor (VLDLR) for EEEV and LDLRAD3 for VEEV [104].
In Vitro and Ex Vivo Systems
Reductionist systems allow for the detailed molecular dissection of virus-host interactions.
Cell Culture Models for HSV-Glia Interaction: The protocol employed by Ripa et al. (as cited in [109]) investigated HSV-1 interaction with autophagy in glial cells (HOG and U-87 MG cell lines). The methodology involved:
- CRISPR/Cas9 Knockout: Generation of ATG5 and MAP1LC3B gene knockouts in glial cell lines.
- HSV-1 Infection: Infection of knockout and wild-type cell lines with HSV-1.
- Viral Transcription/Replication Assay: Quantification of viral transcripts and progeny via qRT-PCR and plaque assays. The finding that ATG5 knockout suppressed HSV-1 replication suggests the virus hijacks non-canonical functions of autophagy components to facilitate its replication in glial cells [109].
Microglial Infection with CHIKV: Kumar et al. (as cited in [103]) studied the neuropathogenesis of the Old World alphavirus Chikungunya (CHIKV) using human microglial cells. The experimental workflow included:
- In Vitro Infection: Infection of microglial cells with CHIKV.
- Flow Cytometry: Analysis of surface marker expression (CD11c, CD14, HLA-DR).
- Apoptosis and Mitochondrial Assays: Measurement of apoptosis induction and mitochondrial membrane depolarization.
- Electron Microscopy: Visualization of immature virions in cytoplasmic vesicles at 24 hours post-infection (hpi) and clusters of mature virions being released at 48 hpi [103].
Table 2: Key Experimental Protocols in Neurotropic Virus Research
| Experimental Goal | Model System | Key Methodological Steps | Critical Readouts |
|---|---|---|---|
| ZIKV Systemic Pathogenesis | NHP Model | Subcutaneous inoculation; sample collection (blood, CSF, tissues) [102] | Viral load (RT-PCR), inflammatory markers (ELISA), microbiome & SCFA analysis [102] |
| Alphavirus Neuroinvasion | Mouse Model | Aerosol/intranasal/subcutaneous exposure; histopathology of brain tissue [104] | Clinical scoring, mortality, viral titer in brain & olfactory bulb, cytokine profiling [104] |
| HSV-Glia Molecular Interaction | Glial Cell Line (in vitro) | CRISPR/Cas9 knockout (e.g., ATG5, IRF1); HSV infection; qRT-PCR [109] [103] | Viral gene expression, viral titer, immunoblotting, cell viability [109] [103] |
| CHIKV Microglial Response | Human Microglial Cells (in vitro) | CHIKV infection; flow cytometry; apoptosis assays; electron microscopy [103] | Surface marker expression, mitochondrial depolarization, virion morphogenesis [103] |
The Scientist's Toolkit: Research Reagent Solutions
Advancing research in neurotropic virology requires a suite of specialized reagents and tools. The following table details essential materials for conducting key experiments in this field.
Table 3: Essential Research Reagents for Neurotropic Virus Studies
| Research Reagent / Tool | Primary Function | Key Application & Rationale |
|---|---|---|
| CRISPR/Cas9 Gene Editing Systems | Targeted knockout of host genes in cell lines. | To define the functional role of host factors (e.g., ATG5, IRF1) in viral replication and immune evasion [109] [103]. |
| Cryo-Electron Microscopy (Cryo-EM) | High-resolution structural determination of macromolecular complexes. | To resolve structures of viral proteins (e.g., HSV gB fusion protein) and their complexes with neutralizing nanobodies [100]. |
| Nanobodies (e.g., anti-gB) | Highly specific, single-domain antibodies for neutralization. | To probe viral entry mechanisms and as a potential therapeutic candidate to block membrane fusion in HSV [100]. |
| TLR Agonists/Antagonists | Pharmacological modulation of innate immune signaling pathways. | To investigate the role of specific TLRs (e.g., TLR3 in ZIKV) in pathogenesis and as potential vaccine adjuvants [107]. |
| Pathogen-Specific qRT-PCR Assays | Quantitative detection of viral RNA/DNA from clinical and experimental samples. | For precise viral load quantification in tissues, serum, and CSF to assess viral replication and dissemination [102] [104]. |
Visualization of Experimental Workflows
A clear understanding of the experimental journey from hypothesis to data is key for research design. The following diagram outlines a generalized workflow for investigating virus-host interactions, integrating methodologies from the cited studies.
Diagram 2: Experimental workflow for pathogenesis studies. Outlines a multi-technique approach from initial in vitro screening to in vivo validation and structural analysis.
Viruses are obligate intracellular pathogens that rely exclusively on host cellular machinery to replicate. Among the host processes that viruses strategically exploit, lipid metabolism plays a particularly pivotal role in supporting virtually every stage of the viral life cycle, from entry and replication to assembly and release [110] [111]. Viral Manipulation of Lipid Metabolism: Commonalities and Distinctions refers to the sophisticated mechanisms by which diverse viruses rewire host lipid biosynthetic and trafficking pathways to facilitate their replication, while also evading host immune surveillance. These interactions induce profound and selective remodeling of the host lipidome, often in virus- and tissue-specific patterns [110]. Recent advances in mass spectrometry (MS)-based lipidomics have revealed that these perturbations represent active viral strategies to control membrane dynamics, signaling, and trafficking [110]. This review synthesizes current understanding of how viruses across different families—including SARS-CoV-2, Influenza A Virus (IAV), HIV, HCV, and West Nile Virus (WNV)—commonly and distinctly manipulate host lipid metabolism, with implications for identifying novel diagnostic biomarkers and host-directed therapeutic strategies.
Viral Entry Mechanisms and Lipid Dependencies
The initial step of viral infection—host cell entry—demonstrates both common and distinct dependencies on host lipid membranes. Many viruses utilize specialized lipid microdomains for entry, though the specific mechanisms vary considerably.
Lipid Raft-Mediated Entry
Lipid rafts, defined as small (10–200 nm), heterogeneous, highly dynamic, sterol- and sphingolipid-enriched membrane domains, serve as critical platforms for the entry of numerous viruses [112]. These cholesterol-rich microdomains compartmentalize cellular processes by concentrating viral receptors and stabilizing fusion complexes. SARS-CoV-2 primarily enters cells through binding of its spike protein to the angiotensin-converting enzyme 2 (ACE2) receptor, a process facilitated by lipid rafts that stabilize the receptor and enhance viral fusion [112]. Disruption of these cholesterol-rich domains significantly reduces SARS-CoV-2 entry into epithelial cells, highlighting their importance [112].
The influenza virus employs multiple entry mechanisms, including clathrin-mediated endocytosis and macropinocytosis, which may or may not involve lipid rafts [112]. However, evidence suggests rafts serve as attachment points that aid multivalent interactions during the initial stages of infection [112].
Endosomal Membrane Composition and Fusion
For many enveloped viruses, including influenza, fusion with the endosomal membrane rather than the plasma membrane confers a significant fitness advantage. Recent research demonstrates that influenza A virus fusion at the plasma membrane results in a 4.5-fold reduction in productive cell infection compared to infection through the physiological endosomal route [113]. This restriction appears partially attributable to the lipid composition and physical properties of the membranes.
The plasma membrane exhibits a liquid-ordered state characterized by higher cholesterol content and membrane order, which restricts viral fusion efficiency. In contrast, endosomal membranes contain higher proportions of anionic lipids such as bis(monoacylglycero)phosphate (BMP), which promote fusion [113]. Experimental depletion of cholesterol from plasma membrane vesicles enhances lipid mixing rates and reduces membrane order, subsequently rescuing influenza infection through the plasma membrane route by 2.4-fold [113]. This highlights how viruses have evolved to exploit compartment-specific lipid compositions for efficient entry.
Table 1: Viral Entry Mechanisms and Lipid Dependencies
| Virus | Primary Entry Mechanism | Key Lipid Components | Experimental Evidence |
|---|---|---|---|
| SARS-CoV-2 | ACE2 receptor binding facilitated by lipid rafts | Cholesterol, sphingolipids | Lipid raft disruption reduces infection in epithelial cells [112] |
| Influenza Virus | Endosomal fusion (primary), clathrin-mediated endocytosis | BMP, cholesterol | Plasma membrane fusion reduces infection 4.5-fold; cholesterol depletion rescues infection [113] |
| Flaviviruses (WNV) | Multiple mechanisms including lipid raft-mediated endocytosis | Cholesterol, sphingolipids | Cholesterol depletion studies show reduced viral entry [112] |
| HIV | Lipid raft-dependent fusion | Cholesterol, glycosphingolipids | Receptor concentration in lipid rafts enhances fusion efficiency [112] |
Metabolic Reprogramming for Viral Replication
Once internalized, viruses extensively reprogram host lipid metabolic pathways to generate specialized platforms that support viral replication. Key commonalities exist in how diverse viruses manipulate specific lipid biosynthetic pathways.
Lipid Droplets as Viral Replication Hubs
Lipid droplets (LDs)—cytoplasmic organelles composed of neutral lipids surrounded by a phospholipid monolayer—serve as crucial platforms for the replication of multiple viruses. Viruses commonly enhance LD biogenesis and modify LD-associated proteins to create favorable microenvironments for replication complex assembly [114].
Recent research on influenza A virus has revealed a novel antiviral mechanism involving O-GlcNAc transferase (OGT), a metabolic enzyme that translocates from the nucleus to cytosolic LDs upon detecting IAV genomic RNA [114]. This interaction, which requires OGT's N-terminal tetracopeptide repeat-4 motif, destabilizes the LD-coating protein perilipin 2, thereby limiting LD accumulation and consequently restricting viral replication [114]. This discovery reveals how host metabolic enzymes can function as viral sensors that integrate innate immune signaling with lipid metabolic regulation.
Conserved Rewiring of Lipid Biosynthetic Pathways
Integrated lipidomic and proteomic profiling of cells infected with different SARS-CoV-2 variants (original WA1, Delta, and Omicron) reveals that metabolic rewiring is remarkably consistent across variants despite their differing transmissibility and immune evasion capabilities [115]. These studies identified key proteins linked to virus-mediated changes in lipid abundance, including:
- Fatty acid synthase (FASN) - central to fatty acid biosynthesis
- Lysosomal acid lipase (LIPA) - involved in cholesterol ester hydrolysis
- ORMDL - a regulator of sphingolipid biosynthesis [115]
This conserved reprogramming suggests that essential host lipid metabolic networks represent promising avenues for identifying broad-spectrum antiviral targets.
Table 2: Alterations in Key Lipid Classes During Viral Infection
| Lipid Class | Specific Lipids Altered | Virus Examples | Functional Consequences |
|---|---|---|---|
| Glycerophospholipids | Phosphatidylserines (PS), Phosphatidylethanolamines (PE) | SARS-CoV-2, HCV, HIV | Membrane curvature for replication organelles; signaling platform assembly [110] |
| Sphingolipids | Ceramides, sphingomyelins | SARS-CoV-2, IAV, HIV | Modulation of membrane fluidity; regulation of cell death pathways; immune modulation [110] [111] |
| Sterols | Cholesterol, 25-hydroxycholesterol (25-HC) | IAV, SARS-CoV-2, multiple viruses | Membrane fluidity regulation; generation of antiviral oxysterols [111] [116] |
| Fatty Acids | Saturated, mono- and polyunsaturated fatty acids | IAV, SARS-CoV-2, HCV | Membrane composition alteration; energy production through β-oxidation [111] |
Figure 1: Viral Hijacking of Host Lipid Metabolism. This diagram illustrates common pathways viruses manipulate, from entry through lipid rafts or endosomes to replication complex formation and immune evasion strategies.
Immunometabolic Interplay in Antiviral Defense
The intersection of lipid metabolism and immune function—immunometabolism—represents a critical battleground in host-virus interactions. Both innate and adaptive immune responses are profoundly influenced by lipid metabolic changes during viral infection.
Type I Interferon Signaling and Lipid Regulation
Type I interferon (IFN-I) signaling not only induces classical interferon-stimulated genes (ISGs) but also directly modulates lipid metabolism to support antiviral defense. In macrophages, IFNβ treatment reduces total cellular cholesterol while simultaneously enhancing production of the antiviral lipid 25-hydroxycholesterol (25-HC) [111]. This oxysterol alters membrane cholesterol accessibility, thereby restricting the replication, entry, and propagation of a broad range of viruses, including murine cytomegalovirus (MCMV) and herpes simplex virus type 1 (HSV-1) [111].
Conversely, lipid metabolism regulates IFN-I signaling through multiple mechanisms. Fluctuations in cholesterol metabolism prime IFN-I signaling in macrophages [111]. Additionally, in T cells, decreased mono-unsaturated fatty acids (MUFAs) metabolism upon infection activates type I IFN and contributes to antiviral responses [111]. This bidirectional crosstalk creates a sophisticated regulatory network that coordinates metabolic and immune defenses.
T Cell Lipid Metabolism and Antiviral Immunity
Activated T cells undergo extensive metabolic reprogramming to meet the bioenergetic and biosynthetic demands of clonal expansion and effector function. Following T-cell receptor (TCR) activation, signaling pathways including the mammalian target of rapamycin (mTOR) and peroxisome proliferator-activated receptor gamma (PPARγ) orchestrate fatty acid uptake and utilization [111].
Lipid metabolism differentially regulates CD4+ T helper cell subset differentiation:
- Acetyl-CoA Carboxylase 1 (ACC1), a rate-limiting enzyme in fatty acid biosynthesis, is essential for the differentiation of pathogenic Th2 and Th17 cells [111]
- 1-oleoyl-lysophosphatidylethanolamine [LPE (1-18:1)] serves as a physiological ligand for RORγt, the master transcription factor of Th17 cells [111]
- Both human and murine Th17 cells rewire sphingolipid metabolism via the serine palmitoyltransferase complex (SPTLC) to sustain their function [111]
- Memory CD8+ T cells enhance triacylglycerol synthesis and utilize intrinsic lipolysis pathways to support their metabolic programming [111]
These findings highlight how viruses may indirectly manipulate immune function by altering the lipid microenvironment that shapes T cell responses.
Distinct Viral Strategies and Pathological Outcomes
While common themes exist in viral manipulation of lipid metabolism, distinct strategies employed by specific viruses contribute to unique pathological outcomes.
Flavivirus Neurological Sequelae and Lipid Interactions
West Nile virus (WNV) neuroinvasive disease provides a compelling example of how virus-lipid interactions contribute to long-term pathological sequelae. Approximately 40-60% of WNND survivors experience persistent neurological complications, including cognitive impairment, memory deficits, and depression [25]. These sequelae are associated with lipid-dependent mechanisms of neural damage:
Complement-mediated synaptic pruning: In mouse models, WNV infection triggers microglial complement activation (C1Qa upregulation) leading to loss of hippocampal CA3 presynaptic terminals, despite no neuronal cell death [25]. Mice lacking complement C3 or its receptor C3aR1 are protected from this synaptic terminal loss [25].
T cell-mediated inflammation: Antiviral CD8+ T cells persist in the hippocampus after infection, releasing interferon-gamma (IFN-γ) that drives microglial activation and spatial learning impairments [25]. The CXCL16/CXCR6 chemokine signaling pathway supports maintenance of these resident memory T cells (T_RM) in the forebrain [25].
Disrupted neurogenesis: Recovery from WNND is associated with altered hippocampal gene expression regulating adult neurogenesis, particularly interleukin-1 (IL-1) production by astrocytes, which interferes with neurogenesis and memory function [25].
Viroporins as Viral Lipid Manipulators
Viroporins—virus-encoded small hydrophobic pore-forming proteins—represent a distinct mechanism by which viruses manipulate host membrane integrity and lipid homeostasis. These proteins modify ion homeostasis, disrupt host membranes, and orchestrate key stages of the virus life cycle [117]. Beyond facilitating viral propagation, viroporins trigger immunopathology by activating the NLRP3 inflammasome and promoting proinflammatory responses [117]. Their dual role in viral fitness and immunopathology positions viroporins as promising antiviral targets for dual-action therapeutics that simultaneously suppress replication and attenuate inflammation [117].
Experimental Approaches and Methodologies
Advances in analytical technologies, particularly mass spectrometry-based lipidomics, have been instrumental in deciphering virus-lipid interactions. The choice of experimental approach depends on the specific research questions being addressed.
Lipidomic Profiling Techniques
Liquid chromatography-electrospray ionization-tandem MS (LC-ESI-MS/MS) has emerged as the cornerstone technique for comprehensive lipid profiling in viral infections [110]. The specific chromatographic separation methods selected influence the classes of lipids that can be resolved:
Reversed-phase liquid chromatography (RPLC): Dominant in viral lipidomics studies, providing separation based on fatty acyl chain length and unsaturation; widely applied in COVID-19, HCV, and WNV research [110].
Hydrophilic interaction liquid chromatography (HILIC): Preferred for separating polar lipid classes such as glycerophospholipids (e.g., phosphatidylserines and phosphatidylethanolamines) implicated in viral replication and immune modulation; used in studies of HCV-associated HCC and COVID-19 [110].
Normal phase liquid chromatography (NPLC): Less common due to reproducibility challenges and MS compatibility issues, though applied in HIV lipid studies [110].
Both untargeted and targeted lipidomics strategies offer complementary insights. Untargeted approaches using high-resolution Orbitrap or time-of-flight (TOF) analyzers facilitate global lipid profiling and hypothesis generation, proving valuable for uncovering dysregulation patterns linked to disease severity in SARS-CoV-2 and HIV infections [110]. Data-independent acquisition (DIA) techniques, including SWATH-MS and DIA-PASEF, provide improved reproducibility, deeper coverage, and better quantification, especially from low-input clinical samples [110].
Targeted methods, such as multiple reaction monitoring (MRM) on sensitive triple quadrupole-linear ion trap (QTRAP) instruments, offer enhanced sensitivity and reproducibility for quantifying specific lipid classes (e.g., ceramides, lysophospholipids) with greater potential for clinical translation [110].
Functional Validation Approaches
Cholesterol deprivation assays represent a key functional approach for validating the importance of specific lipid pathways in viral infection. In studies of influenza virus production in suspension-adapted MDCK-STAT1-KO cells, researchers treated cells with methyl-β-cyclodextrin (MβCD) at varying concentrations (0, 5, 10, and 15 mg/mL) for 12 hours to deplete cellular cholesterol, subsequently measuring viral titers through hemagglutination assays [116]. These experiments confirmed the critical role of intracellular cholesterol in IAV production, as cholesterol depletion significantly reduced viral titers [116].
Genetic manipulation techniques, including CRISPR/Cas9-mediated gene knockout and conditional knock-in mouse models, enable precise dissection of lipid metabolic genes in viral infections. Studies of O-GlcNAc transferase employed conditional OGT catalytically impaired knock-in mice (Ogt-K908A) to distinguish between catalytic activity-dependent and independent Antiviral Effects [114].
Table 3: Essential Research Reagents and Experimental Tools
| Reagent/Technique | Specific Examples | Application in Viral Lipid Research |
|---|---|---|
| Chromatography Separation | RPLC, HILIC, NPLC | Separation of lipid classes based on physicochemical properties prior to MS analysis [110] |
| Mass Spectrometry Platforms | Orbitrap, TOF, QTRAP instruments | High-resolution lipid identification and quantification [110] |
| Lipid Depletion Agents | Methyl-β-cyclodextrin (MβCD) | Cellular cholesterol depletion to validate lipid requirements in viral entry/replication [116] [113] |
| Genetic Models | Conditional knock-in mice (Ogt-K908A), CRISPR/Cas9 | Functional validation of specific lipid metabolic genes in viral pathogenesis [114] |
| Virus Production Assays | Hemagglutination, TCID50, plaque assays | Quantification of viral replication and release efficiency [116] |
Figure 2: Experimental Workflow for Viral Lipidomics Research. This diagram outlines key methodological steps from sample preparation through lipid separation, mass spectrometry analysis, data processing, and functional validation.
Therapeutic Implications and Future Perspectives
The intricate interplay between viruses and host lipid metabolism presents numerous opportunities for therapeutic intervention. Targeting host lipid pathways may offer advantages over direct antiviral approaches by reducing the potential for viral resistance.
Lipid-Targeting Antiviral Strategies
Several lipid-directed therapeutic approaches show promise:
Viroporin inhibitors: These compounds target viral pore-forming proteins to disrupt their membrane-permeabilizing activities, potentially suppressing replication while attenuating inflammation [117].
Cholesterol-modulating compounds: Since multiple viruses depend on cholesterol for entry and replication, cholesterol synthesis inhibitors or depletion agents could exhibit broad-spectrum antiviral activity [112] [116] [113].
Lipid metabolism enzymes inhibition: Targeting key enzymes such as FASN, ACC1, or sphingolipid biosynthetic enzymes may disrupt viral replication compartments [115] [111].
Oxysterol administration: Therapeutic delivery of antiviral lipids like 25-HC could enhance intrinsic antiviral defenses [111].
Technological Advances and Future Directions
Emerging technologies are poised to accelerate discovery in viral lipidomics:
AI-driven structural prediction: Advanced computational approaches can model virus-lipid interactions and predict the effects of lipid composition on viral fusion and assembly [117].
Single-virus tracking methodologies: Techniques that monitor individual virion-lipid interactions provide unprecedented resolution of viral entry and fusion mechanisms [113].
Integrated multi-omics approaches: Combining lipidomics with proteomics, transcriptomics, and metabolomics will provide systems-level understanding of host-virus interactions [110] [115].
Advanced structural lipidomics: Improving isomer resolution and spatial localization through techniques like ion mobility separation and imaging mass spectrometry will address current limitations in characterizing structurally similar lipid species with distinct biological functions [110].
Viral manipulation of host lipid metabolism represents a fundamental aspect of pathogenesis that crosses viral family boundaries. While distinct viruses employ specialized strategies tailored to their replication cycles and tissue tropisms, common themes emerge in their exploitation of lipid rafts for entry, lipid droplets for replication complex assembly, and specific lipid biosynthetic pathways for membrane generation. The convergence of viral pathogenesis on critical lipid nodes presents promising opportunities for therapeutic intervention. Future research integrating advanced lipidomic technologies with functional studies will continue to decipher the complex dialogue between viruses and host lipid metabolism, potentially revealing novel targets for broad-spectrum antiviral strategies that transcend the limitations of conventional virus-directed approaches.
Within viral pathogenesis and infection mechanisms research, a central challenge is the strategic selection of therapeutic targets that balance broad-spectrum efficacy with resilience against viral evolution. This whitepaper provides a technical guide for validating conserved host and viral vulnerabilities alongside virus-specific targets, with a focus on practical experimental frameworks. We detail methodologies for identifying essential viral components with high sequence conservation, probing host dependencies, and characterizing emergent mechanisms like long-range genomic interactions. By integrating data from structural biology, reverse genetics, and functional genomics, this guide aims to support researchers and drug development professionals in building robust preclinical pipelines for antiviral therapeutics.
Antiviral therapeutic targets broadly fall into two categories: virus-specific targets, which are encoded by the viral genome (e.g., viral enzymes), and conserved host targets, which are host proteins or pathways that the virus hijacks for its replication cycle [118]. The ideal viral target is an element that is essential for the viral life cycle, has a tractable mechanism of action for small-molecule inhibition, and possesses a high fitness barrier to the development of resistance mutations [118]. For host targets, the essentiality lies in the host factor's role in a non-redundant pathway critical for viral propagation, with an acceptable therapeutic window to mitigate on-target toxicity.
The COVID-19 pandemic underscored the value of both approaches. Direct-acting antivirals (DAAs) like nirmatrelvir (targeting the viral main protease, Mpro) and molnupiravir (targeting the viral RNA-dependent RNA polymerase, RdRp) exemplify successful virus-specific targeting [118]. Conversely, the exploration of host-directed therapies, such as CCR5 antagonists for HIV, demonstrates the potential of targeting conserved host vulnerabilities, though this approach has seen fewer clinical successes to date, in part due to toxicity concerns [118] [119].
Validating Conserved Viral Vulnerabilities
Conserved viral targets are proteins or genomic elements that remain largely unchanged across different viral strains or even within a virus family. Their conservation often indicates a fundamental role in the viral life cycle, making it difficult for the virus to tolerate mutations that would allow escape from inhibitors.
Sequence and Structural Conservation Analysis
Objective: To identify and prioritize viral targets based on their evolutionary conservation, thereby increasing the likelihood of developing broad-spectrum antivirals and reducing the risk of resistance.
Methodology:
- Multiple Sequence Alignment: Compile protein or nucleotide sequences for the target gene from a wide range of viral variants (e.g., SARS-CoV-2 Variants of Concern) and related viruses (e.g., across the Coronaviridae family). Use tools like Clustal Omega or MUSCLE.
- Conservation Scoring: Calculate a conservation score (e.g., Shannon entropy) for each residue position. Low-variability regions indicate functional or structural constraints.
- Structural Analysis: Map conserved residues onto available high-resolution protein structures (e.g., from cryo-EM or X-ray crystallography). Conserved surface pockets, especially in active sites, are prime targets [118].
Exemplar Data: The SARS-CoV-2 NSP5 Mpro demonstrates ~96% sequence similarity with SARS-CoV-1 Mpro. This high conservation, combined with a unique cleavage specificity distinct from human proteases, made it a top-tier target, enabling the rapid repurposing of pre-existing chemical probes like PF-00835231 [118].
Application to Novel Targets: Beyond proteins, conserved functional RNA elements in the viral genome can be targeted. A recent study identified a conserved ultra-long-range RNA-RNA interaction spanning over 17 kb in the SARS-CoV-2 genome, present in both the wild-type virus and the Omicron variant. Disrupting this interaction with mutations reduced viral fitness, validating its essential role [120].
Table 1: Key Conserved Viral Targets with Clinical Validation
| Viral Target | Virus Family | Function | Conservation Basis | Example Therapeutic |
|---|---|---|---|---|
| Main Protease (Mpro/NSP5) | Coronaviridae | Polyprotein processing | >96% sequence identity between SARS-CoV-1 & SARS-CoV-2; critical active site residues 100% conserved [118]. | Nirmatrelvir (PF-07321332) |
| RNA-dependent RNA Polymerase (RdRp/NSP12) | Coronaviridae | Viral RNA synthesis | High structural and sequence conservation of catalytic core across RNA viruses [118] [121]. | Remdesivir, Molnupiravir |
| Nucleocapsid (N) Protein | Coronaviridae | Genome packaging, virion assembly | More conserved than spike protein; limited mutation across variants [122]. | (Vaccine candidate) |
Reverse Genetics and Functional Genomics
Objective: To empirically validate the essentiality of a conserved viral element for replication and infectivity.
Methodology:
- Infectious Clone Construction: Generate a full-length viral cDNA clone.
- Target Disruption: Introduce targeted mutations or deletions into the conserved element (e.g., the long-range RNA interaction site) or use antisense oligonucleotides (ASOs) to disrupt structured RNA elements [120].
- Phenotypic Assay: Transfert the mutant genome into permissive cells and quantify viral replication (e.g., by plaque assay) and fitness (e.g., by competition assays with wild-type virus) [120].
- Compensatory Mutation Analysis: Passage the mutant virus and sequence the genome to identify mutations that restore fitness, confirming the target's importance.
Exemplar Data: Mutations designed to disrupt the identified 17-kb long-range RNA interaction in SARS-CoV-2 reduced viral fitness at later infection stages. Compensatory mutations that partially restored the interaction also restored virus fitness, providing strong functional validation [120]. In a separate experiment, an ASO targeting a highly base-paired, structurally conserved region in Orf7a significantly reduced viral replication in both WT and Omicron variants [120].
Diagram: Functional Validation Workflow for Conserved Viral Elements. This workflow uses reverse genetics to empirically test if a conserved genomic element is essential for viral fitness.
Validating Virus-Specific Vulnerabilities
Virus-specific vulnerabilities are unique molecular features or mechanisms that are not conserved broadly but are critical for a particular virus. These often arise from pathogen-specific adaptations.
Host Factor Dependency Mapping
Objective: To identify host proteins that are uniquely co-opted by a specific virus for entry, replication, or immune evasion.
Methodology:
- Genome-wide Screens: Perform CRISPR-knockout or RNAi-knockdown screens in human cell lines to identify host factors whose loss impairs viral replication without significant cellular toxicity.
- Proteomic Interaction Networks: Use techniques like affinity purification-mass spectrometry (AP-MS) to map the physical interactome of viral proteins.
- Functional Validation: Knock out or chemically inhibit the candidate host factor and measure viral replication in in vitro and in vivo models.
Exemplar Data: Research has shown that differentially expressed RNA-binding proteins (RBPs) like HNRNPU and FXR1 can impact RNA structure in specific SARS-CoV-2 variants. In vitro assays confirmed that adding HNRNPU protein to a viral RNA fragment altered its structure, a mechanism that may contribute to variant-specific pathogenesis [120].
Unconventional Viral Gene Expression Mechanisms
Objective: To target virus-specific transcriptional and translational recoding strategies that expand viral coding capacity from a compact genome [123].
- Methodology:
- Ribosome Profiling (Ribo-seq): Map the positions of translating ribosomes across the viral genome to identify novel open reading frames (ORFs), including those generated by frameshifting or in overlapping regions.
- Mass Spectrometry: Confirm the expression of proteins predicted from these unconventional ORFs.
- Mechanistic Assays: Develop reporter assays to quantify the efficiency of processes like * transcriptional slippage* (e.g., in Ebola virus GP gene) or RNA splicing (e.g., in influenza virus segments 7 and 8) [123].
- Inhibitor Screening: Use the reporter assays to screen for small molecules or ASOs that specifically disrupt these viral-specific mechanisms.
Table 2: Virus-Specific Vulnerabilities from Unconventional Gene Expression
| Mechanism | Viral Example | Outcome | Therapeutic Opportunity |
|---|---|---|---|
| Transcriptional Slippage | Ebolavirus, Paramyxoviruses | Insertion of non-templated nucleotides, producing multiple proteins from one gene [123]. | Small molecules that alter RdRp fidelity or structured RNA elements that promote slippage. |
| Overlapping Genes (ORFs) | Widespread in viruses | Multiple proteins synthesized from different reading frames of the same nucleotide sequence [123]. | Antisense oligonucleotides (ASOs) that block translation of specific ORFs. |
| Programmed Ribosomal Frameshifting | Coronaviridae (FSE) | Ribosome shifts to an alternative reading frame, producing two proteins from one mRNA. | Small molecules that stabilize frameshift-suppressing RNA structures. |
Integrated Validation Workflows and Assays
Robust target validation requires a multi-faceted approach that converges data from complementary assays.
In Vitro Antiviral Potency and Cytotoxicity Assays
Objective: To determine the potency and selectivity of a candidate inhibitor in cell-based systems.
- Protocol:
- Cell Culture: Use a physiologically relevant cell line (e.g., Vero E6, Calu-3 for SARS-CoV-2).
- Viral Infection & Compound Treatment: Infect cells at a low MOI (e.g., 0.01) and treat with a dose-response range of the inhibitor. Include a positive control (e.g., Remdesivir) and untreated infected/untinfected controls.
- Endpoint Quantification: At 48-72 hours post-infection, quantify viral RNA by RT-qPCR, viral titer by plaque assay, or viral protein by immunoassay.
- Cytotoxicity: Run a parallel assay in uninfected cells using a metabolic activity assay (e.g., MTT, CellTiter-Glo) to calculate the selective index (CC~50~ / EC~50~).
Structural Biology and Structure-Based Drug Design
Objective: To visualize the target-inhibitor interaction and guide medicinal chemistry optimization.
- Protocol:
- Protein Production: Express and purify the recombinant viral target protein (e.g., Mpro, RdRp).
- Co-crystallization/Sample Preparation: Crystallize the protein in complex with the inhibitor or prepare samples for cryo-EM.
- Data Collection and Modeling: Solve the high-resolution structure. Analyze the binding mode to identify key molecular interactions (hydrogen bonds, hydrophobic contacts).
- Iterative Design: Use the structural information to design analogs with improved potency and drug-like properties [118].
Diagram: Structure-Based Antiviral Drug Design Cycle. This iterative process uses structural biology to inform the rational design of potent and selective inhibitors.
In Vivo Efficacy Models
Objective: To evaluate the therapeutic efficacy of a lead compound in a live animal model of disease.
- Protocol (Syrian Hamster Model for SARS-CoV-2):
- Animal Challenge: Intranasally inoculate hamsters with a defined dose of virus (e.g., 10^4^ TCID~50~ of SARS-CoV-2).
- Compound Dosing: Administer the candidate therapeutic (e.g., via oral gavage) at various times pre- or post-infection. Include vehicle-treated infected controls and uninfected controls.
- Disease Monitoring: Track weight loss, clinical scores, and viral load in respiratory tissues (e.g., lungs, nasal turbinates) over several days.
- Histopathology: Analyze lung tissues for lesions, inflammation, and viral antigen presence [122].
The Scientist's Toolkit: Key Research Reagents and Platforms
Table 3: Essential Research Reagents for Antiviral Target Validation
| Reagent / Platform | Function / Application | Key Utility in Validation |
|---|---|---|
| SHAPE-MaP (Selective 2'-Hydroxyl Acylation analyzed by Primer Extension and Mutational Profiling) | High-throughput RNA structure probing [120]. | Mapping functional long-range RNA interactions and structures in viral genomes, as demonstrated for SARS-CoV-2 variants. |
| CRISPR Knockout Libraries | Genome-wide screening of host dependency factors. | Systematically identifying host proteins essential for viral replication but dispensable for host cell survival. |
| Yeast Display & Deep Mutational Scanning (DMS) | High-throughput profiling of antibody epitopes and escape mutations [124]. | Classifying neutralizing antibodies and predicting viral evolution to pre-empt resistance. |
| Recombinant Viral Proteins (Mpro, RdRp, etc.) | Biochemical and structural studies. | Enabling high-throughput inhibitor screening, mechanistic studies, and structure-based drug design. |
| Infectious Clones (Bacterial Artificial Chromosomes) | Reverse genetics systems [120]. | Engineering specific mutations into the viral genome to test gene/protein/RNA element essentiality. |
| Antisense Oligonucleotides (ASOs) | Sequence-specific targeting of RNA. | Functionally validating structured RNA elements and overlapping genes by inhibiting their translation or altering structure [120]. |
| Class 4 (Broadly Neutralizing) Antibodies | Probes for conserved, cryptic epitopes. | Studying allosteric inhibition mechanisms and defining conserved, "druggable" surfaces on viral proteins like the Spike RBD [124]. |
Conclusion
The study of viral pathogenesis reveals both conserved mechanisms across virus families and unique adaptations that define individual viral lifestyles. The integration of foundational molecular virology with advanced technologies like cryo-EM, single-cell omics, and CRISPR screening has dramatically accelerated our understanding of host-pathogen interactions. Current research emphasizes the critical role of viral manipulation of host processes—from immune evasion through epigenetic regulation to metabolic reprogramming—as central to disease outcomes. The comparative analysis of pathogenesis strategies across viral families highlights both targetable vulnerabilities and challenges in broad-spectrum antiviral development. Future directions must focus on understanding viral persistence mechanisms, predicting cross-species transmission potential, and developing therapeutic strategies that account for rapid viral evolution. The convergence of structural biology, systems virology, and computational approaches promises to unlock new generations of antivirals and vaccine platforms capable of addressing both established and emerging viral threats.
References
- 1. Virus-Receptor Interactions and Receptor-Mediated Virus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7122110/]
- 2. Viral Pathogenesis - Medical Microbiology - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK8149/]
- 3. Decoding protein networks during virus entry by quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4914609/]
- 4. Virus entry: molecular mechanisms and biomedical applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC7097642/]
- 5. Receptor Binding for the Entry Mechanisms of SARS-CoV-2 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12115909/]
- 6. Receptor Recognition Mechanisms of Coronaviruses [https://pmc.ncbi.nlm.nih.gov/articles/PMC4338876/]
- 7. Membrane Mysteries: How Viruses Navigate Cell Entry [https://virologyresearchservices.com/2025/03/24/membrane-mysteries-how-viruses-navigate-cell-entry/]
- 8. Discovery of viral entry routes into cells points to prevention ... [https://medicine.washu.edu/news/discovery-of-viral-entry-routes-into-cells-points-to-future-prevention-treatment-strategies/]
- 9. Key Takeaways from IDWeek 2025: AI, AMR Strategies ... [https://www.medpace.com/blog/key-takeaways-from-idweek-2025-ai-amr-strategies-next-generation-anti-viral-development-converging/]
- 10. RNA Structures at the Virus-Host Interface - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/40446307/]
- 11. Decoding macrophage immunometabolism in human viral ... [https://www.sciencedirect.com/science/article/abs/pii/S1876162323001074]
- 12. emerging viral infection mechanisms and therapeutic targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455939/]
- 13. Wistar Scientists Uncover New Viral Mechanism for ... [https://www.wistar.org/press-releases/wistar-scientists-uncover-new-viral-mechanism-for-evading-immunity-identifying-a-new-drug-target/]
- 14. Molecular imaging of viral pathogenesis and opportunities ... [https://www.nature.com/articles/s44303-024-00056-w]
- 15. Viral hijacking mechanism in humans through protein– ... [https://www.sciencedirect.com/science/article/abs/pii/S1876162322000335]
- 16. Viral Pathogenesis - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/viral-pathogenesis]
- 17. Evasion of the Antiviral Innate Immunity by PRV [https://pubmed.ncbi.nlm.nih.gov/39684850/]
- 18. Innate immune evasion strategies of SARS-CoV-2 [https://www.nature.com/articles/s41579-022-00839-1]
- 19. SARS-CoV-2 spike mutations alter structure and energetics ... [https://www.nature.com/articles/s41598-025-15979-6]
- 20. Epigenetic silencing of DNA sensing pathway by FOXM1 ... [https://www.nature.com/articles/s41467-025-59186-3]
- 21. Epigenetic silencing and genome dynamics determine the fate ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02280-1]
- 22. Advances in KSHV Research: Molecular Pathogenesis ... [https://pubmed.ncbi.nlm.nih.gov/41217111/]
- 23. Viral tropism in plants, reproductive tissues, and seeds - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098505/]
- 24. Comparative tropism, replication kinetics, and cell damage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7173822/]
- 25. Sequelae of viral CNS infections including outcomes, ... [https://www.nature.com/articles/s44298-025-00160-7]
- 26. Membrane-wide screening identifies potential tissue-specific ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1013157]
- 27. Cell Tropism Predicts Long-term Nucleotide Substitution ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1003838]
- 28. Multiplex viral tropism assay in complex cell populations ... [https://www.nature.com/articles/s41434-022-00360-3]
- 29. The role of cell death pathways in respiratory viral infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446011/]
- 30. Control of Mitochondrial Membrane Permeabilization by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2195906/]
- 31. Virus-induced permeability transition in mitochondria [https://www.sciencedirect.com/science/article/pii/S0014579399017093]
- 32. Regulation of the mitochondrial permeability transition pore ... [http://microbialcell.com/researcharticles/2020a-pellegrino-coppola-microbial-cell/]
- 33. ARFGAP1 serves as a critical host factor during E30 infection [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02971-9]
- 34. Apoptosis and necroptosis as host defense strategies to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5653411/]
- 35. Contrast in Cryo-EM [https://guide.cryosparc.com/cryo-em-foundations/image-formation/contrast-in-cryo-em]
- 36. a benchmark experiment for limited dataset screening [https://jast-journal.springeropen.com/articles/10.1186/s40543-024-00445-1]
- 37. Guidelines for using Bsoft for high resolution reconstruction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5734390/]
- 38. Cryo-EM and cryo-ET reveal the molecular architecture ... [https://pubmed.ncbi.nlm.nih.gov/40711877/]
- 39. Cryo-EM and cryo-ET reveal the molecular architecture ... [https://www.sciencedirect.com/science/article/pii/S2211124725008289]
- 40. CryoVIA: An image analysis toolkit for the quantification of ... [https://www.sciencedirect.com/science/article/pii/S0969212625000139]
- 41. CryoVIA: An image analysis toolkit for the quantification of ... [https://pubmed.ncbi.nlm.nih.gov/39919734/]
- 42. Single-cell RNA-sequencing data analysis reveals a highly ... [https://www.nature.com/articles/s42003-022-04253-4]
- 43. Single-cell longitudinal analysis of SARS-CoV-2 infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8007021/]
- 44. The Application of Single-Cell Technologies for Vaccine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300521/]
- 45. Single-cell and spatially resolved omics: Advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10499650/]
- 46. Single-cell multi-omics profiling uncovers the immune ... [https://pubmed.ncbi.nlm.nih.gov/40184908/]
- 47. Blog: SARS-CoV-2 vaccine improvement [https://www.scdiscoveries.com/blog/science/guiding-sars-cov-2-vaccine-development-with-single-cell-rna-sequencing/]
- 48. A review of virus host factor discovery using CRISPR ... [https://pubmed.ncbi.nlm.nih.gov/39422472/]
- 49. CRISPR Tackles Emerging Viral Pathogens - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8624524/]
- 50. Systematic comparison of CRISPR-Cas9 and RNAi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4900911/]
- 51. CRISPR screen to determine host factors [https://www.takarabio.com/products/covid-19-research/crispr-screening?srsltid=AfmBOop3FRO2yEukCXzMAKqJG7umJUa0pMj421Ydur4szgBrCNlgWpKV]
- 52. A benchmark comparison of CRISPRn guide-RNA design ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11386-3]
- 53. Discovery of cancer drug targets by CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4529991/]
- 54. CRISPR/Cas9 screens identify key host factors that ... [https://www.nature.com/articles/s41541-024-01007-7]
- 55. Fighting Infectious Disease with CRISPR [https://www.synthego.com/blog/crispr-infectious-disease/]
- 56. CRISPR-StAR enables high-resolution genetic screening ... [https://www.nature.com/articles/s41587-024-02512-9]
- 57. Ferret models of viral pathogenesis [https://pubmed.ncbi.nlm.nih.gov/25816764/]
- 58. Ferrets as Models for Influenza Virus Transmission Studies ... [https://wwwnc.cdc.gov/eid/article/24/6/17-2114_article]
- 59. Creation of “Humanized” Mice to Study Human Immunity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3023233/]
- 60. Humanized Mice: Advancing Translational Preclinical ... [https://www.taconic.com/resources/methods-generating-humanized-mice]
- 61. Revealing Retroviral Life Cycles Using Visible Viruses and Live ... Cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC11697243/]
- 62. Rapid Identification of Single Virus Particles Using Virus Biosensor [https://www.news-medical.net/whitepaper/20150413/Rapid-Identification-of-Single-Virus-Particles-Using-Virus-Biosensor.aspx]
- 63. Bridging In Vitro and In Vivo Inhalation Toxicity [https://pubmed.ncbi.nlm.nih.gov/41183645/]
- 64. Bridging In Vitro and In Vivo Inhalation Toxicity [https://www.sciencedirect.com/science/article/abs/pii/S0269749125017166]
- 65. Bridging the Gap Between In Vivo and In Vitro [https://www.frontiersin.org/research-topics/68566/biomimetic-culture-platforms-bridging-the-gap-between-in-vivo-and-in-vitro]
- 66. SERS technology in virus Detection: Advances, challenges ... [https://www.sciencedirect.com/science/article/abs/pii/S095656632500778X]
- 67. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 68. Molecular Aspects of Medicine | Pathobiology of Emerging ... [https://www.sciencedirect.com/journal/molecular-aspects-of-medicine/special-issue/10WTSS2W8QX]
- 69. Quantitative Molecular Analysis of Virus Expression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC86721/]
- 70. Measuring infectious virus: the plaque assay [https://virologyresearchservices.com/2022/08/10/the-plaque-assay/]
- 71. Standardization of the methods and reference materials used ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-015-0333-1]
- 72. A quantitative model used to compare within-host SARS-CoV ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3001128]
- 73. Artificial intelligence in vaccine research and development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12095282/]
- 74. Perspectives in Molecular Viral Pathogenesis: 2025 [https://www.frontiersin.org/research-topics/66307/perspectives-in-molecular-viral-pathogenesis-2025undefined]
- 75. Evolution shapes and conserves genomic signatures in ... [https://www.nature.com/articles/s42003-024-07098-1]
- 76. Kinetics of HIV-1 Latency Reversal Quantified on the Single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5044848/]
- 77. HIV Tat as a latency reversing agent: turning the tables on ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1571151/full]
- 78. HIV Tat as a latency reversing agent: turning the tables on ... [https://pubmed.ncbi.nlm.nih.gov/40292298/]
- 79. Emerging Prognostic and Predictive Biomarkers for Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12115395/]
- 80. Efficient mRNA delivery to resting T cells to reverse HIV ... [https://www.nature.com/articles/s41467-025-60001-2]
- 81. Purging viral latency by a bifunctional HSV-vectored ... [https://elifesciences.org/articles/95964]
- 82. IFITM3: How genetics influence influenza infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6468115/]
- 83. Expression of SARS-CoV-2-related receptors in cells of the... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-021-02210-2]
- 84. N-glycosylation at the receptor binding site drives ... [https://pubmed.ncbi.nlm.nih.gov/41190812/]
- 85. Structural basis of broad protection against influenza virus ... [https://www.nature.com/articles/s41467-025-62174-2]
- 86. HIV-1 Entry Mechanisms: Protein-Host Receptor ... [https://pubmed.ncbi.nlm.nih.gov/41198533/]
- 87. CXCR4 mediated recognition of HIV envelope spike and ... [https://www.nature.com/articles/s41467-025-63815-2]
- 88. Functional assessment of cell entry and receptor for... usage [https://www.nature.com/articles/s41564-020-0688-y?error=cookies_not_supported&code=4484eb5e-9898-4756-8dda-2ca75348be8b]
- 89. SARS-CoV-2 host-pathogen interactome: insights into ... [https://www.sciencedirect.com/science/article/pii/S004268222500220X]
- 90. Modulation of transferrin receptor by HIV-2 [https://pubmed.ncbi.nlm.nih.gov/41272830/]
- 91. Herpes simplex virus 1 evades cellular antiviral response by ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1009950]
- 92. Evasion of adaptive and innate immune response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4397892/]
- 93. Improving poxvirus-mediated antitumor immune responses ... [https://www.nature.com/articles/s41417-023-00610-5]
- 94. DNA-Sensing Antiviral Innate Immunity in Poxvirus Infection [https://pmc.ncbi.nlm.nih.gov/articles/PMC7483915/]
- 95. The Flavivirus Non-Structural Protein 5 (NS5) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11360482/]
- 96. Non-structural protein 5 (NS5) as a target for antiviral ... [https://www.sciencedirect.com/science/article/abs/pii/S1879625721000729]
- 97. Innate Immune Evasion Mediated by Flaviviridae Non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5691642/]
- 98. Complement Evasion Strategies of Viruses: An Overview [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2017.01117/full]
- 99. Evasion of Intracellular DNA Sensing by Human ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2021.647992/full]
- 100. A nanobody against herpes | 2025 | News and Press [https://www.leibniz-liv.de/en/news/news-and-press/a-nanobody-against-herpes]
- 101. Herpes simplex virus: An immunopathologic review [https://www.sciencedirect.com/science/article/pii/S2950198924000175]
- 102. Elevated peripheral and nervous system inflammation is ... [https://pubmed.ncbi.nlm.nih.gov/40827913/]
- 103. Editorial: Viral infection pathogenesis and pathology in ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1554095/full]
- 104. Neuropathogenesis of Encephalitic Alphaviruses in Non- ... [https://www.mdpi.com/2076-0817/14/2/193]
- 105. Herpes Simplex Virus Neurovirulence Across the Human ... [https://pubmed.ncbi.nlm.nih.gov/40418737/]
- 106. Chronic Neuroplasticity Changes Following Neurotropic Viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586820/]
- 107. Toll-like receptor response to Zika virus infection [https://www.nature.com/articles/s44298-025-00102-3]
- 108. Neuropathogenesis of Old World Alphaviruses [https://pmc.ncbi.nlm.nih.gov/articles/PMC11860675/]
- 109. Editorial: Herpesvirus: transmission, pathogenesis, host- ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1637344/full]
- 110. Unraveling virus-host interactions: Current advances in viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595130/]
- 111. The diverse interaction of metabolism, immune response, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339340/]
- 112. Metabolic Reprogramming in Respiratory Viral Infections [https://www.mdpi.com/2218-273X/15/7/1027]
- 113. Influenza viral infection at the plasma membrane is ... [https://pubmed.ncbi.nlm.nih.gov/40704989/]
- 114. O-GlcNAc transferase plays dual antiviral roles by ... [https://www.nature.com/articles/s41467-025-63085-y]
- 115. Integrated lipidomic and proteomic profiling reveals ... [https://www.sciencedirect.com/science/article/pii/S0022227525001221]
- 116. Insights into IAV Replication and Lipid Metabolism in ... [https://www.mdpi.com/2076-393X/13/2/106]
- 117. emerging viral infection mechanisms and therapeutic targets [https://pubmed.ncbi.nlm.nih.gov/40891825/]
- 118. Accelerating antiviral drug discovery: lessons from COVID-19 [https://www.nature.com/articles/s41573-023-00692-8]
- 119. Editorial: Antiviral drug discovery against pathogens of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034765/]
- 120. A conserved long-range RNA interaction in SARS-CoV-2 ... [https://www.nature.com/articles/s41467-025-63297-2]
- 121. SARS-CoV-2 replication and drug discovery [https://www.sciencedirect.com/science/article/pii/S0890850824000252]
- 122. Protective Potential and Functional Role of Antibodies ... [https://pubmed.ncbi.nlm.nih.gov/40558099/]
- 123. Unconventional viral gene expression mechanisms as ... [https://www.nature.com/articles/s41586-021-03511-5]
- 124. Exploring the Intersection of Binding, Allostery, and ... [https://www.mdpi.com/2218-273X/15/9/1340]