mRNA Vaccine Design and Development: From Platform Technology to Precision Medicine
This comprehensive review explores the rapidly evolving landscape of mRNA vaccine design and development, a field revolutionized by the success of COVID-19 vaccines and now expanding into oncology and other...
mRNA Vaccine Design and Development: From Platform Technology to Precision Medicine
Abstract
This comprehensive review explores the rapidly evolving landscape of mRNA vaccine design and development, a field revolutionized by the success of COVID-19 vaccines and now expanding into oncology and other infectious diseases. Tailored for researchers, scientists, and drug development professionals, the article synthesizes foundational principles, cutting-edge methodological advances, critical optimization strategies, and robust validation frameworks. It covers core topics including immunogenicity mechanisms, lipid nanoparticle (LNP) delivery systems, antigen design for conformational stability, and the integration of artificial intelligence for neoantigen selection. The review also examines the current clinical pipeline, with over 120 active trials and the first commercial mRNA cancer vaccine approvals anticipated by 2029, providing a strategic outlook on the future of this transformative platform technology in biomedical research and clinical application.
Core Principles and Immunological Mechanisms of mRNA Vaccines
The messenger RNA (mRNA) vaccine platform represents a transformative "plug-and-play" technology in vaccinology, fundamentally shifting away from traditional pathogen-dependent development toward an agile, antigen-agnostic framework. This paradigm utilizes a standardized, reusable backbone where the genetic sequence encoding a target antigen can be rapidly interchanged without re-engineering the core delivery system or manufacturing process [1]. The urgency demonstrated by emerging pathogens such as SARS-CoV-2, Zika virus, and novel influenza strains has underscored the critical limitation of traditional vaccine development, which often requires 15–20 years to bring a product to market [1]. In contrast, the plug-and-play nature of mRNA platforms slashes development timelines from years to months by reusing proven backbones, thereby reducing repetitive safety and production steps otherwise required for each new pathogen [1]. This modularity accelerates both regulatory approval and large-scale manufacturing, making it an indispensable technology for responsive public health intervention.
The foundational principle of this technology involves the in vitro transcription of synthetic mRNA that encodes a specific immunogenic protein from a pathogen. This mRNA is then formulated into lipid nanoparticles (LNPs) that protect the genetic material and facilitate its delivery into human cells [2]. Once inside the cytoplasm, the host cell's ribosomes translate the mRNA into the protein antigen, which is then presented to the immune system to elicit both humoral and cell-mediated immunity [1]. This direct host-cell expression of antigen mimics natural infection in a controlled manner, enabling the generation of robust, high-affinity antibodies and properly skewed T-helper responses, while memory B and T cells ensure rapid recall upon subsequent pathogen exposure [1]. The platform's flexibility allows researchers to simply "plug in" the mRNA sequence for a new antigen while using the same "play" components—the LNP delivery system and manufacturing workflow—across different vaccine targets.
Platform Advantages and Quantitative Comparisons
The plug-and-play mRNA platform offers distinct advantages across the vaccine development lifecycle, particularly when compared to traditional vaccine technologies. Table 1 provides a quantitative comparison of key development metrics across different vaccine platforms, highlighting the transformative potential of mRNA technology.
Table 1: Comparative Analysis of Vaccine Development Platforms
| Development Metric | Traditional Platforms (Live/Inactivated) | Viral Vector Platforms | mRNA Platform |
|---|---|---|---|
| Typical Development Timeline | 5–18 years [1] | 2–5 years (with existing vector) | Months to 2 years [1] [2] |
| Manufacturing Process | Pathogen-dependent, cell culture/egg-based | Cell culture-based | Cell-free in vitro transcription |
| Antigen Flexibility | Low; requires pathogen handling | Moderate; limited by pre-existing immunity | High; simple sequence exchange |
| Immune Profile | Strong, long-lasting immunity; risk of reversion (live) [1] | Efficient antigen presentation; pre-existing immunity can reduce efficacy [1] | Robust humoral and cellular response; tunable immunogenicity [1] |
| Production Scalability | Challenging; biological variability | Moderate | Highly scalable; synthetic process |
| Stability Profile | Often requires strict cold chain | Often requires frozen storage | Requires frozen or ultra-cold chain; stability improving |
This comparative analysis demonstrates that mRNA technology significantly accelerates research and production timelines while maintaining the capacity to elicit comprehensive immune responses [2]. The synthetic manufacturing process eliminates the need for biological substrates such as chicken eggs or cell cultures, avoiding potential issues like egg-adapted mutations that can diminish vaccine effectiveness against circulating strains [1]. The platform's agility was prominently demonstrated during the COVID-19 pandemic, where mRNA vaccines were among the first to receive authorization, with the plug-and-play nature of the platform enabling rapid updates to target emerging SARS-CoV-2 variants [3].
Beyond speed and flexibility, the mRNA platform offers substantial advantages in immune engineering. Researchers can strategically modify the mRNA sequence to enhance antigen expression or reduce unnecessary immunogenicity, and can co-deliver multiple mRNAs encoding different antigens within the same LNP formulation [1]. The LNP itself serves not only as a delivery vehicle but also as a built-in adjuvant, stimulating innate immune responses through pattern recognition receptors that ultimately shape adaptive immunity [4] [1]. This capacity for precise engineering enables the development of vaccines against pathogens that have previously eluded traditional approaches, including those with high mutation rates or complex life cycles, positioning the mRNA platform as a cornerstone of pandemic preparedness and emerging disease response.
Application Notes and Protocols
Protocol 1: Modular Antigen Design and mRNA Construct Assembly
This protocol describes the computational design and in vitro assembly of mRNA vaccine constructs, focusing on the SARS-CoV-2 spike protein as a model antigen. The process can be adapted to other pathogens through targeted sequence modifications.
Computational Design andIn SilicoOptimization
- Target Identification: Identify immunodominant antigens through reverse vaccinology, immunoproteomic screening, or literature mining. For SARS-CoV-2, the spike (S) glycoprotein serves as the primary target due to its role in host cell entry [4].
- Epitope Mapping: Use artificial intelligence (AI) and computational tools for accurate antigen and epitope identification, immune response modeling, and improved vaccine design [1].
- Sequence Optimization:
- Modify the native antigen coding sequence (CDS) to reflect human codon usage bias without altering the amino acid sequence.
- Incorporate stabilizing mutations (e.g., proline substitutions in SARS-CoV-2 S-2P) to maintain prefusion conformation.
- Ensure the inclusion of a leader sequence (e.g., tissue plasminogen activator signal peptide) for secretory protein trafficking.
- Add defined 5' and 3' untranslated regions (UTRs) that enhance mRNA stability and translational efficiency.
DNA Template Preparation andIn VitroTranscription (IVT)
- Template Construction:
- Synthesize the optimized CDS and clone into a plasmid vector containing a bacteriophage promoter (e.g., T7, SP6).
- Alternatively, generate linear DNA templates via PCR with integrated promoter sequences.
- Validate template fidelity through sequencing and analytical restriction digest [4].
- IVT Reaction Assembly:
- Set up the following reaction in a nuclease-free microcentrifuge tube:
- DNA template (1 µg)
- Transcription buffer (commercially available)
- Nucleotide triphosphates (NTPs, 6–8 mM each)
- Cap analog (e.g., CleanCap, 4–6 mM)
- RNA polymerase (e.g., T7, 0.5–1 U/µL)
- Pyrophosphatase (optional, to prevent pyrophosphate precipitation)
- RNase inhibitor (0.5–1 U/µL)
- Incubate at 37°C for 2–4 hours.
- Set up the following reaction in a nuclease-free microcentrifuge tube:
- mRNA Purification and Quality Control:
- Digest DNA template with DNase I (15 min, 37°C).
- Purify mRNA using silica membrane-based kits or liquid chromatography.
- Quantify yield via spectrophotometry (e.g., Nanodrop).
- Assess integrity by denaturing agarose gel electrophoresis or capillary electrophoresis.
Protocol 2: Lipid Nanoparticle (LNP) Formulation and Characterization
This protocol details the microfluidic formulation of LNPs for mRNA encapsulation, following the composition principles of clinically approved formulations.
LNP Preparation via Rapid Mixing
- Solution Preparation:
- Aqueous Phase: Dilute purified mRNA to 0.1–0.2 mg/mL in citrate buffer (pH 4.0).
- Lipid Phase: Prepare an ethanolic lipid mixture with the following molar composition:
- Ionizable cationic lipid (50 mol%)
- Phospholipid (10 mol%)
- Cholesterol (38.5 mol%)
- PEG-lipid (1.5 mol%)
- Microfluidic Mixing:
- Use a commercial microfluidic device or staggered herringbone mixer.
- Set the aqueous-to-organic flow rate ratio to 3:1.
- Maintain a total flow rate of 12–15 mL/min.
- Collect the resulting LNP suspension in a vessel containing a phosphate buffer (pH 7.4) for dialysi.
- Buffer Exchange and Sterile Filtration:
- Dialyze against phosphate-buffered saline (PBS) or Tris buffer (pH 7.4) for 18–24 hours at 4°C.
- Alternatively, use tangential flow filtration for larger volumes.
- Sterile-filter through a 0.22 µm polyethersulfone membrane.
- Store final formulated LNPs at 4°C or -80°C for long-term preservation.
LNP Characterization and Quality Control
- Physical Characterization:
- Determine particle size distribution and polydispersity index via dynamic light scattering.
- Measure zeta potential using electrophoretic light scattering.
- Visualize morphology using transmission electron microscopy.
- Encapsulation Efficiency and mRNA Integrity:
- Quantify encapsulated mRNA using a Ribogreen fluorescence assay.
- Validate encapsulation efficiency meets clinical specification range (typically >90%) [4].
- Confirm mRNA integrity post-encapsulation through gel electrophoresis.
Protocol 3: Preclinical Evaluation in Animal Models
This protocol outlines the in vivo assessment of mRNA-LNP vaccine candidates, including immunogenicity profiling and evaluation of anti-tumor effects in combination with immune checkpoint inhibitors (ICIs).
Immunization and Sample Collection
- Study Design:
- Use 6–8 week-old female C57BL/6 or BALB/c mice (n=6–8 per group).
- Include control groups (PBS, empty LNPs, relevant benchmark vaccines).
- Vaccination Regimen:
- Administer mRNA-LNP vaccine via intramuscular (IM) or subcutaneous (SC) injection.
- Use a prime-boost strategy with a 2–3 week interval between vaccinations.
- For anti-tumor studies, administer ICIs (e.g., anti-PD-1, anti-PD-L1, anti-CTLA-4) intraperitoneally concomitant with or following vaccination [4].
- Sample Collection Timeline:
- Collect serum pre-vaccination (Day 0) and at regular intervals post-vaccination (e.g., Days 14, 28, 42).
- Harvest spleens and lymph nodes for cellular immune analyses at study endpoint.
Humoral and Cellular Immune Response Analysis
- Antigen-Specific Antibody Titers:
- Determine endpoint titers or half-maximal effective concentration (EC50) via enzyme-linked immunosorbent assay (ELISA).
- Perform virus neutralization tests or surrogate assays if applicable.
- T Cell Responses:
- Isolate peripheral blood mononuclear cells (PBMCs) or splenocytes.
- Stimulate with antigen-specific peptide pools.
- Detect interferon-gamma (IFN-γ) production via enzyme-linked immunospot (ELISpot) or intracellular cytokine staining (ICS) followed by flow cytometry.
- Identify antigen-specific CD8⁺ and CD4⁺ T cell populations using major histocompatibility complex (MHC) multimers.
Evaluation of Tumor Sensitization to Immune Checkpoint Inhibition
- Tumor Model Establishment:
- Implant immunologically "cold" tumor cells (e.g., B16 melanoma, MC38 colon adenocarcinoma) subcutaneously in syngeneic mice.
- Monitor tumor volume 2–3 times weekly using caliper measurements.
- Treatment and Efficacy Assessment:
- Initiate treatment when tumors reach a palpable size (~50–100 mm³).
- Administer SARS-CoV-2 mRNA vaccines (e.g., BNT162b2 synthetic replica) alone or in combination with ICIs [4].
- Evaluate the substantial increase in type I interferon as a key mediator of RNA vaccine immunity [4].
- Monitor for epitope spreading against tumour-associated antigens as an indicator of sustained T cell responses [4].
- Immunological Analysis of Tumor Microenvironment (TME):
- Harvest tumors at endpoint and process to single-cell suspensions.
- Characterize tumor-infiltrating lymphocytes (TILs) via flow cytometry.
- Evaluate PD-L1 expression on tumor cells and immune cells following vaccination [4].
Experimental Workflow and Signaling Pathways
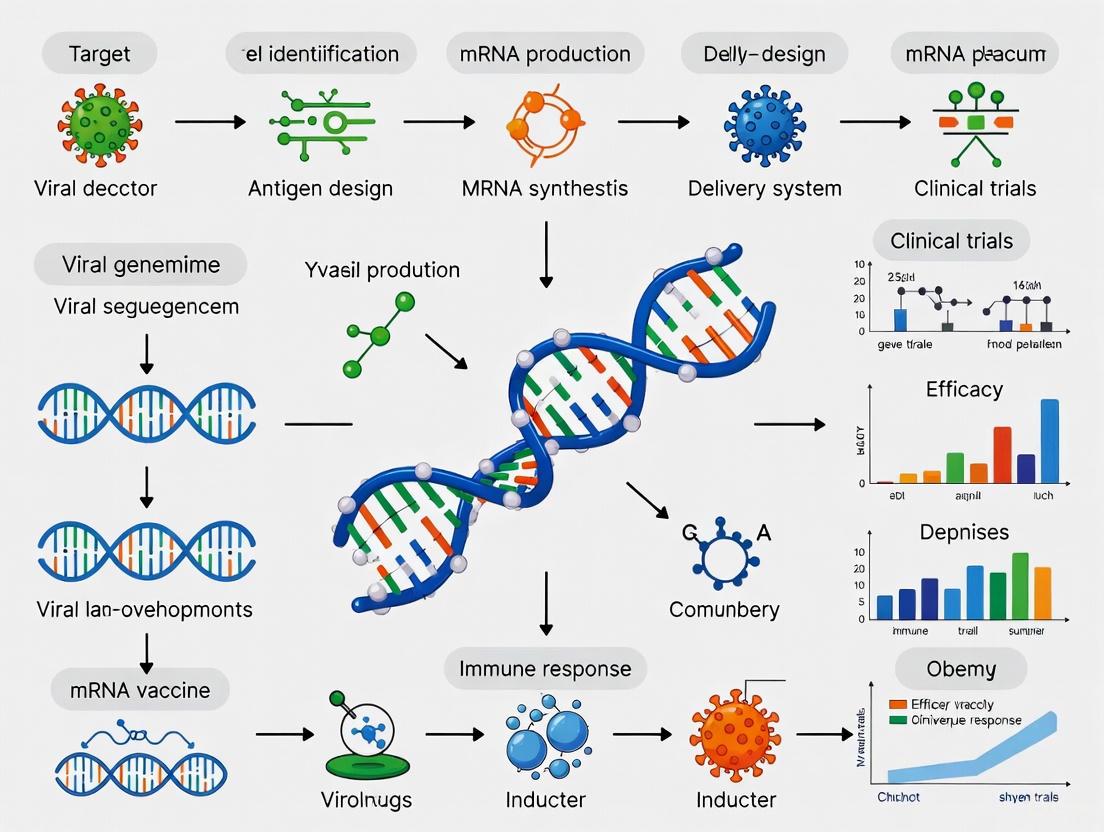
mRNA Vaccine Workflow: From Design to Immune Response
Diagram 1: End-to-end workflow for mRNA vaccine development and mechanism of action, highlighting the modular "plug-and-play" process from antigen design to immune activation.
Innate Immune Signaling Pathway Activated by mRNA-LNP Vaccines
Diagram 2: Innate and adaptive immune signaling cascade initiated by mRNA-LNP vaccines, depicting type I interferon-mediated sensitization to immune checkpoint inhibitors.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for mRNA Vaccine Development
| Research Reagent / Material | Function and Application | Technical Notes |
|---|---|---|
| Linearized DNA Template | Template for in vitro transcription of mRNA; contains promoter and antigen CDS. | Ensure high purity; verify sequence fidelity; use bacteriophage promoter (e.g., T7). |
| Nucleotide Triphosphates (NTPs) | Building blocks for mRNA synthesis; include modified nucleotides (e.g., pseudouridine). | Use modified nucleotides to reduce innate immunogenicity and enhance translation. |
| Cap Analog (e.g., CleanCap) | Synthetic 5' cap structure for mRNA; enhances translation and stability. | Co-transcriptional capping improves efficiency and yield compared to post-transcriptional methods. |
| Lipid Components for LNPs | Formulate nanoparticles for mRNA delivery and protection; typically ionizable lipid, phospholipid, cholesterol, PEG-lipid. | Optimize molar ratios for specific applications; ionizable lipid is crucial for endosomal escape. |
| Microfluidic Mixer | Device for rapid mixing of aqueous and organic phases to form uniform LNPs. | Enables reproducible, scalable LNP production; controlled parameters ensure batch-to-batch consistency. |
| Ribogreen Assay Kit | Fluorescence-based quantification of mRNA encapsulation efficiency in LNPs. | Compare fluorescence with/without detergent to distinguish encapsulated vs. free mRNA. |
| ELISpot Plates and Reagents | Detect antigen-specific T cell responses through cytokine (e.g., IFN-γ) secretion. | High sensitivity for low-frequency T cell responses; use peptide pools covering entire antigen. |
| MHC Multimers | Flow cytometry-based identification of antigen-specific T cells by T cell receptor binding. | Tetramers, pentamers, or dextramers; require knowledge of immunodominant epitopes and MHC restriction. |
| Anti-PD-1/PD-L1 Antibodies | Immune checkpoint inhibitors for combination studies in oncology models. | Use validated biological-grade antibodies for in vivo studies; optimize dosing schedule with vaccination. |
Concluding Remarks
The modular plug-and-play nature of the mRNA vaccine platform represents a paradigm shift in vaccinology, offering unprecedented speed and flexibility in addressing diverse public health threats. The standardized workflows, reagent systems, and analytical methods detailed in these Application Notes and Protocols provide researchers with a foundational framework for developing novel mRNA-based interventions. This technology's potential extends beyond infectious diseases into oncology, as evidenced by its capacity to sensitize tumors to immune checkpoint inhibitors through type I interferon-mediated immune activation [4]. As platform optimization continues—addressing challenges such as stability profiles and reactogenicity—the integration of artificial intelligence for antigen discovery and immune profiling will further enhance the precision and efficacy of next-generation mRNA vaccines [1]. This versatile platform establishes a new standard for rapid medical countermeasure development in an era of emerging biological threats.
Within the framework of mRNA vaccine design and development, understanding the precise immunogenicity profiles—the ability to provoke innate and adaptive immune responses—is paramount. The immunogenicity of mRNA vaccines is a double-edged sword: it is essential for establishing protective immunity but, if unregulated, can lead to adverse reactions or attenuated adaptive responses. This document details the core immune activation pathways, provides standardized protocols for their evaluation, and visualizes the complex cellular and molecular interactions involved, offering a practical resource for researchers and drug development professionals.
Fundamental Immune Activation Pathways
The immunogenicity of mRNA vaccines stems from two primary functions: the in situ production of antigenic proteins and the intrinsic immunostimulatory properties of the mRNA molecule itself. Figure 1 illustrates the complete sequence of these events, from vaccine administration to the generation of humoral and cellular immunity.
Innate Immune Recognition and Activation
The innate immune system provides the first line of defense and is critical for initiating adaptive immunity. mRNA vaccines are recognized as a "non-self" pattern by various Pattern Recognition Receptors (PRRs) [5].
- Endosomal Sensing: Single-stranded mRNA within endosomes is detected by Toll-like Receptors TLR7 and TLR8. This recognition triggers the downstream adapter protein Myeloid Differentiation Primary Response 88 (MyD88), leading to the production of pro-inflammatory cytokines and type I interferons (IFN-I) [5].
- Cytosolic Sensing: Double-stranded RNA (dsRNA) impurities, or certain mRNA structures, can be detected in the cytoplasm by receptors like Retinoic acid-inducible gene I (RIG-I) and Melanoma Differentiation-Associated protein 5 (MDA-5). These sensors signal through the mitochondrial antiviral signaling (MAVS) protein to induce IFN-I [5] [6].
- Type I Interferon Response: A cornerstone of the innate response to mRNA vaccines, IFN-I signaling through the interferon-α/β receptor (IFNAR) leads to the expression of hundreds of interferon-stimulated genes (ISGs). This response has a dual effect: it promotes dendritic cell maturation and activation, enhancing antigen presentation, but can also inhibit the translation of the mRNA-encoded antigen and attenuate the adaptive immune response [6] [5].
Recent studies emphasize that the mRNA component itself, rather than just the lipid nanoparticle (LNP) carrier, is essential for triggering a robust, IFNAR-dependent innate immune activation. This response is characterized by rapid dendritic cell activation, monocyte recruitment to draining lymph nodes, and a systemic cytokine profile [6].
Antigen Presentation and Adaptive Immune Priming
The adaptive immune response is characterized by its specificity and memory. mRNA vaccines elicit both humoral (antibody-mediated) and cellular (T-cell-mediated) immunity.
- MHC Class I Presentation (Cellular Immunity): The mRNA is translated into protein in the cytoplasm. This endogenously produced protein is processed by the proteasome into peptides, which are loaded onto MHC class I molecules and presented to CD8+ T cells. This pathway activates cytotoxic T lymphocytes (CTLs), which can directly identify and eliminate infected or malignant cells [7] [5].
- MHC Class II Presentation (Humoral Immunity): The vaccine-encoded protein can also be secreted or released from cells. As an exogenous antigen, it is taken up by professional Antigen-Presenting Cells (APCs), degraded in lysosomes, and the resulting peptides are presented on MHC class II molecules to CD4+ T helper cells. Activated CD4+ T cells are crucial for supporting B cell antibody production and amplifying CD8+ T cell responses [5].
- B Cell Activation: B cells can directly recognize the native, correctly folded antigen expressed by the mRNA vaccine through their B cell receptor (BCR). With help from CD4+ T cells, this triggers B cell proliferation, differentiation into plasma cells, and the generation of neutralizing antibodies [5].
Figure 1. Integrated Immune Activation Pathways of mRNA Vaccines. The diagram shows the journey of an LNP-mRNA vaccine from injection to the induction of adaptive immunity. Key components like the 5' Cap and UTRs facilitate cytosolic translation. The mRNA and potential dsRNA impurities are sensed by PRRs (TLR7/8, RIG-I, MDA5), triggering a type I interferon (IFN) response that shapes both innate and adaptive immunity. The translated antigen is presented via MHC-I to activate CD8+ T cells (cellular immunity) or via MHC-II to activate CD4+ T cells, which help B cells produce antibodies (humoral immunity).
Quantitative Data on Immune Responses
The following tables summarize key quantitative findings from recent preclinical and clinical studies, highlighting the immune correlates of different mRNA vaccine platforms and the impact of specific immune modulation strategies.
Table 1. Comparative Immunogenicity of Different mRNA Vaccine Platforms
| mRNA Platform | Dose | Antibody Titer (IgG) | Neutralizing Antibody Titer | T cell Response (IFN-γ+) | Key Findings | Reference |
|---|---|---|---|---|---|---|
| Self-Amplifying RNA (srRNA) - Influenza (H5N1) | 1 pg - 10 ng | High, dose-dependent (H5N1) | HI Titer >40 (protective) at 1 pg post-boost | Robust HA-specific CD8+ & CD4+ T cells down to 1 pg | 1,000,000-fold dose-sparing vs. conventional mRNA; superior durability | [8] |
| Circular RNA (Circ-RNA) - SARS-CoV-2 RBD | Not specified | Comparable to SAM | Comparable virus-neutralizing titer | Higher memory T cell response vs. SAM | High stability (4 weeks at 4°C); effective bivalent design | [9] [10] |
| Conventional mRNA - SARS-CoV-2 | Standard (e.g., 100 μg) | High | High (95% vaccine efficacy) | Strong CD4+ and CD8+ T cells | Potent IFNα response; can be attenuated by IFNAR blockade | [11] [6] |
Table 2. Impact of Innate Immune Modulation on Adaptive Immunity
| Experimental Intervention | Target | Effect on Innate Immunity | Impact on Adaptive Immunity | Key Outcome | Reference |
|---|---|---|---|---|---|
| IFNAR Blocking Antibodies | Type I IFN Receptor | Abrogates IFNAR signaling and downstream ISG expression | ↑ Frequencies of antigen-specific CD8+ T cells; ↑ Antigen-specific antibody titers | Transient inhibition enhances vaccine immunogenicity | [6] |
| Nucleoside Modification (e.g., m1Ψ) | RNA Sensors (e.g., TLRs, RIG-I) | Reduces innate sensor activation; "immuno-silent" | Enhances antigen expression, leading to a more robust adaptive response | Foundational technology for current mRNA vaccines | [6] [12] |
| SARS-CoV-2 mRNA Vaccine | N/A (Spike protein) | Substantial increase in type I IFN; innate immune cell activation | Primes de novo CD8+ T cells; synergizes with Immune Checkpoint Blockade | Associated with improved cancer survival in patients on immunotherapy | [13] |
Application Notes & Experimental Protocols
Protocol: Evaluating the Role of Type I Interferon Signaling in mRNA Vaccine Immunogenicity
This protocol utilizes IFNAR blockade to dissect the critical role of type I interferon signaling in shaping the immune response to LNP-mRNA vaccines, based on the methodology from [6].
4.1.1 Background The innate immune response, particularly signaling through the interferon-α/β receptor (IFNAR), can paradoxically attenuate the adaptive immune response to mRNA vaccines by inhibiting antigen translation. This protocol describes how to transiently block IFNAR in a murine model to enhance antigen-specific T cell and antibody responses.
4.1.2 Materials
- LNP-mRNA vaccine: Formulated with nucleoside-modified mRNA.
- Experimental Animals: Female C57BL/6J mice (6-8 weeks old) and IFNAR-/- mice as a control.
- Anti-IFNAR mAb: e.g., clone I-401-100 from Leinco Technologies.
- Flow Cytometry Antibodies: For characterizing immune cell populations (e.g., CD8, CD4, CD19, CD11c, CD11b).
- ELISA/ELISpot Kits: For quantifying antigen-specific antibodies and T cells.
4.1.3 Procedure
- Animal Grouping: Assign mice into groups (e.g., LNP-mRNA + Isotype control, LNP-mRNA + anti-IFNAR, LNP only, PBS).
- IFNAR Blockade: Administer 2.5 mg of anti-IFNAR monoclonal antibody intraperitoneally (IP) 24 hours before and 24 hours after immunization.
- Immunization: Administer the LNP-mRNA vaccine (e.g., 5 μg dose) via intramuscular (IM) injection into the hind leg.
- Sample Collection:
- Serum/Plasma: Collect blood at baseline, day 7, 14, and 28 post-immunization for antibody titer analysis by ELISA.
- Spleen and Lymph Nodes: Harvest tissues at day 7-10 for T cell analysis by intracellular cytokine staining (ICS) or ELISpot.
- Immune Cell Analysis by Flow Cytometry:
- Process lymphoid organs into single-cell suspensions.
- Stimulate cells with antigen-derived peptides and brefeldin A.
- Stain for surface markers (CD3, CD4, CD8) and intracellular cytokines (IFN-γ, TNF, IL-2).
- Analyze on a flow cytometer to identify polyfunctional T cell populations.
4.1.4 Data Analysis
- Compare the frequency and polyfunctionality of antigen-specific CD8+ and CD4+ T cells between anti-IFNAR and control groups.
- Quantify endpoint titers or area under the curve (AUC) for antigen-specific IgG antibodies.
- The expected result is a significant enhancement in both cellular and humoral immunity in the IFNAR-blocked group.
Protocol: Assessing Immunogenicity of Novel mRNA Platforms (srRNA/CircRNA)
This protocol outlines a comparative immunogenicity study for emerging mRNA platforms, such as self-amplifying RNA (srRNA) and circular RNA (CircRNA), against conventional mRNA [9] [8].
4.2.1 Background Next-generation mRNA platforms offer potential advantages like dose-sparing, improved stability, and enhanced T cell immunity. This head-to-head comparison in a relevant animal model is crucial for platform selection.
4.2.2 Materials
- mRNA Constructs: Conventional, srRNA, and CircRNA vaccines encoding the same antigen (e.g., SARS-CoV-2 RBD or Influenza HA).
- Animals: Appropriate models (e.g., mice, ferrets).
- Assays: ELISA for antigen-specific IgG, Virus Neutralization Assay (e.g., PRNT, FRNT), and T cell ELISpot/ICS kits.
4.2.3 Procedure
- Vaccine Formulation: Encapsulate all mRNA constructs in standardized LNP formulations.
- Immunization: Administer vaccines in a prime-boost regimen (e.g., days 0 and 21) across a range of doses (e.g., 0.1 μg to 10 μg) to establish a dose-response.
- Humoral Response Analysis:
- Measure antigen-specific IgG titers via ELISA at multiple time points (e.g., pre-prime, pre-boost, post-boost).
- Assess neutralizing antibody titers against live or pseudotyped virus.
- Cellular Response Analysis:
- Isolate splenocytes 1-2 weeks post-boost.
- Perform IFN-γ ELISpot or ICS using pools of overlapping peptides covering the target antigen.
- For memory T cell response, analyze tissues at a later time point (e.g., 4-8 weeks post-immunization).
4.2.4 Data Analysis
- Compare the magnitude and kinetics of antibody and T cell responses between platforms.
- Determine the relative dose-sparing potential (e.g., the lowest dose of srRNA that elicits a response equivalent to a standard dose of conventional mRNA).
- Evaluate stability by testing the immunogenicity of vaccines stored for different durations at 4°C.
The Scientist's Toolkit: Key Research Reagents
Table 3. Essential Reagents for Investigating mRNA Vaccine Immunogenicity
| Reagent / Material | Function / Application | Example Product / Specification |
|---|---|---|
| Nucleoside-Modified mRNA | Base material for vaccine; reduces innate immune activation and enhances translation. | N1-methylpseudouridine (m1Ψ) modified, cellulose purified to remove dsRNA impurities [6]. |
| Ionizable Lipid | Critical component of LNPs for encapsulating mRNA and enabling endosomal escape. | ALC-0315 (component of BNT162b2) [6]. |
| Anti-IFNAR Monoclonal Antibody | Tool for blocking type I interferon signaling to study its role in vaccine immunogenicity. | Clone I-401-100 (Leinco Technologies) [6]. |
| Deucravacitinib | TYK2 inhibitor; used to study downstream JAK-STAT signaling of IFNAR. | Formulated in PEG-300:Tween-80 vehicle for in vivo administration [6]. |
| Empty LNPs | Control for distinguishing the immunostimulatory effects of the LNP from the mRNA. | LNPs prepared with identical lipid composition but no mRNA payload [6]. |
| Codon-Optimized mRNA Construct | Enhances protein expression efficiency in the host, a key variable in immunogenicity. | Constructs with Kozak sequence, optimized GC content, and human-derived UTRs (e.g., beta-globin) [11] [7]. |
| CleanCap AG Cap 1 Analog | Co-transcriptional capping technology for producing mRNA with superior translation efficiency and reduced immunogenicity. | Yields >94% Cap 1 structure, crucial for evading innate immune sensors [11]. |
Visualizing Key Experimental Workflows
The following diagram outlines the core protocol for investigating the impact of innate immune modulation on mRNA vaccine efficacy, integrating the key reagents and procedures described above.
Figure 2. IFNAR Blockade Experimental Workflow. The diagram outlines the key steps and timeline for a study investigating the role of type I interferon signaling in mRNA vaccine immunogenicity. Mice are grouped and pre-treated with anti-IFNAR or control antibodies before and after immunization. Immune responses are analyzed at multiple time points to capture the peak of T cell (Day 7) and antibody (Day 14+) responses, with a final memory time point.
Application Note AN-2025-M001
Speed of Development and Manufacturing
The accelerated timeline from sequence identification to clinical-grade production represents a paradigm shift in vaccine development, particularly critical for pandemic response and rapidly mutating pathogens.
Table 1: Comparative Development Timelines: Traditional vs. mRNA Platforms
| Development Phase | Traditional Vaccines (Months) | mRNA Platform (Months) | Key Acceleration Factors |
|---|---|---|---|
| Antigen Identification & Design | 12-24 | 1-3 | In silico design; synthetic biology |
| Process & Formulation Development | 18-36 | 3-6 | Modular Lipid Nanoparticle (LNP) systems |
| Clinical Grade Manufacturing | 12-24 | 3-6 | Fully in vitro, cell-free transcription |
| Total Timeline | 42-84 | 7-15 | ~6-fold acceleration |
Experimental Protocol EP-101: Rapid Antigen Design and In Vitro Transcription (IVT)
- Objective: To generate a candidate mRNA vaccine construct encoding a target antigen from a novel pathogen within 72 hours of sequence availability.
- Materials:
- Pathogen genomic sequence data
- Codon optimization software (e.g., specialized algorithms)
- DNA synthesizer or gBlock gene fragments
- In Vitro Transcription Kit (includes T7 RNA polymerase, NTPs, cap analog)
- DNase I (RNase-free)
- mRNA purification kit (e.g., oligo-dT chromatography)
- Methodology:
- Sequence Optimization: Input the antigen's coding sequence into codon optimization software. Parameters include: maximizing GC content (~52%), optimizing untranslated regions (UTRs) for stability, and incorporating modified nucleosides (e.g., 1-methylpseudouridine) to reduce innate immune recognition [14].
- Template Preparation: Synthesize the linear DNA template via PCR, incorporating a T7 promoter sequence, the optimized coding sequence, and a poly-A tail sequence (typically 100-120 nucleotides).
- In Vitro Transcription: Assemble the IVT reaction per kit instructions. Incubate at 37°C for 2-4 hours.
- Template Digestion: Add DNase I to digest the DNA template, incubate for 15 minutes at 37°C.
- mRNA Purification: Purify the mRNA using an affinity-based purification kit to remove enzymes, truncated RNA, and unincorporated NTPs. Confirm integrity via capillary electrophoresis and quantify via spectrophotometry.
Diagram 1: mRNA Antigen Rapid Generation Workflow
Enhanced Safety Profile
The mRNA modality offers a fundamentally improved safety profile compared to traditional vaccine platforms, primarily due to its non-infectious, non-integrating, and transient mechanism of action.
Table 2: Safety Profile Comparison of Vaccine Platforms
| Safety Parameter | Live-Attenuated | Inactivated/Subunit | mRNA-LNP |
|---|---|---|---|
| Risk of Reversion to Virulence | Present (Low) | Absent | Absent |
| Risk of Integration into Host Genome | Not Applicable | Not Applicable | Absent [14] |
| Systemic Inflammatory Reactogenicity | Moderate-High | Low-Moderate | Low-Moderate (can be tuned via LNP design and nucleoside modification [14]) |
| Typical Side Effect Profile | Fever, myalgia common | Local pain, fatigue | Local pain, fatigue, transient fever (resolves in 24-48 hrs) |
| Established Rare Severe Events | Varies by pathogen (e.g., VAPP for OPV) | e.g., GBS for some influenza vaccines | Myopericarditis (rare, mostly in young males); anaphylaxis (extremely rare) [15] |
Experimental Protocol EP-201: Assessing mRNA Vaccine Safety and Innate Immune Activation
- Objective: To evaluate the innate immunogenicity and cytotoxicity of a novel mRNA-LNP formulation in vitro.
- Materials:
- Human peripheral blood mononuclear cells (PBMCs) or relevant cell line (e.g., THP-1)
- mRNA-LNP test article and control (e.g., buffer, non-coding mRNA-LNP)
- Cell culture media and reagents
- ELISA kits for human IFN-α, IFN-β, IL-6, TNF-α
- CellTiter-Glo Luminescent Cell Viability Assay
- Multi-mode microplate reader
- Methodology:
- Cell Seeding: Seed PBMCs or THP-1 cells in a 96-well plate at a density of 2 x 10^5 cells/well.
- Dosing: Treat cells with a concentration range of the mRNA-LNP test article and controls. Include a positive control (e.g., LPS for monocytes).
- Incubation: Incubate cells for 6 hours (for early cytokine measurement) and 24 hours (for viability and sustained response) at 37°C, 5% CO₂.
- Cytokine Analysis: Collect cell culture supernatant. Quantify levels of IFN-α, IFN-β, IL-6, and TNF-α via ELISA according to manufacturer protocols.
- Viability Assay: At 24 hours, add CellTiter-Glo reagent to respective wells, incubate, and measure luminescence. Calculate percent viability relative to untreated controls.
- Data Interpretation: Compare cytokine induction and viability profile of the test article against controls. Modern, nucleoside-modified mRNA should demonstrate minimal innate immune activation while maintaining high cell viability.
Diagram 2: mRNA Innate Immune Recognition Pathways
Unprecedented Scalability and Manufacturing Flexibility
mRNA vaccines transition biologics manufacturing from a cell-based, complex process to a precise, synthetic, and highly scalable biochemical process, enabling rapid response to global demand.
Experimental Protocol EP-301: Continuous-Flow Manufacturing of mRNA-LNP Vaccines
- Objective: To produce a research-scale batch of mRNA-LNP vaccine using a microfluidic-based continuous flow system, mimicking next-generation industrial processes [16].
- Materials:
- Purified mRNA antigen (from EP-101)
- Lipid components: Ionizable lipid, phospholipid, cholesterol, PEG-lipid
- Ethanol (absolute)
- Sodium Acetate buffer (pH 4.0)
- Tangential Flow Filtration (TFF) system
- PD-10 desalting columns
- Microfluidic mixer (e.g., staggered herringbone mixer, SHM)
- Syringe pumps
- Methodology:
- Lipid Solution Preparation: Dissolve the lipid mixture (ionizable lipid:phospholipid:cholesterol:PEG-lipid at predetermined molar ratios) in ethanol to a final concentration of 10-20 mg/mL.
- Aqueous Solution Preparation: Dilute the purified mRNA in sodium acetate buffer (pH 4.0) to a final concentration of 0.1-0.2 mg/mL.
- Microfluidic Mixing: Using syringe pumps, simultaneously introduce the aqueous mRNA phase and the ethanolic lipid phase into the two inlets of the microfluidic mixer at a controlled flow rate and specific volumetric ratio (e.g., 3:1 aqueous:organic). The rapid mixing in the device induces nanoprecipitation, forming LNPs.
- Buffer Exchange and Dilution: Collect the LNP formulation effluent and immediately dilute it with at least 5 volumes of PBS (pH 7.4) to quench the particle formation.
- Diafiltration and Concentration: Load the diluted LNP solution into a TFF system with a suitable molecular weight cutoff (e.g., 100 kDa). Diafilter against PBS (pH 7.4) to remove ethanol and exchange the buffer.
- Sterile Filtration: Pass the concentrated LNP formulation through a 0.22 µm sterile filter. Aliquot and store at -80°C. Characterize particles for size (DLS), polydispersity (PDI), encapsulation efficiency (RIBE), and concentration (HPLC).
Table 3: Scalability and Economic Advantages of mRNA Manufacturing
| Manufacturing Aspect | Traditional Egg-Based Influenza Vaccine | mRNA Vaccine (Continuous Flow System) |
|---|---|---|
| Initial Lead Time | ~6 months (for egg adaptation) | Near zero (sequence-based) |
| Production Cycle Time | ~6 months per batch | Potential for weeks; continuous operation [16] |
| Facility Footprint | Large, dedicated, BSL facilities | Modular, containerized (e.g., BioNTainer) [16] |
| Batch Consistency | Variable (biological system) | High (synthetic process) [16] |
| Dose Output / Facility Size | ~50M doses/year for a large facility | ~50M doses/year from 2 shipping containers [16] |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for mRNA Vaccine R&D
| Reagent Category | Specific Example | Critical Function in R&D | Technical Note |
|---|---|---|---|
| Nucleotide Triphosphates (NTPs) | CleanCap AG (3' OMe) Cap Analog | Co-transcriptional capping; enhances translation efficiency and reduces immunogenicity [14]. | Superior to post-transcriptional capping methods. |
| Ionizable Lipids | Proprietary SM-102, ALC-0315, or novel AI-designed lipids (e.g., AMG1541 [17]) | Critical for endosomal escape and mRNA delivery efficiency; key determinant of reactogenicity. | New lipids can dramatically reduce required dose (e.g., 100-fold improvement reported [17]). |
| Purification Resins | Oligo dT-cellulose / Magnetic Beads | Affinity purification of mRNA via poly-A tail; removes truncated transcripts and dsRNA impurities. | High purity is critical for reducing innate immune activation. |
| Enzymes | T7 RNA Polymerase, DNase I | Core enzyme for IVT; essential for template removal post-transcription. | High-yield, RNase-free formulations are mandatory. |
| Buffer & Salt Reagents | HEPES, Tris Buffer, Sodium Acetate | Maintain pH during IVT and LNP formation; critical for nanoparticle stability and efficacy. | Consistency is key for process transfer and scalability. |
Diagram 3: Core Components of the mRNA Vaccine Platform
The journey of messenger RNA (mRNA) vaccines from a theoretical concept to a clinical breakthrough represents one of the most significant advancements in modern medicine. This transformative technology, which demonstrated global impact during the COVID-19 pandemic, is the culmination of decades of persistent scientific investigation into mRNA biology, chemistry, and delivery systems. Framed within a broader thesis on mRNA vaccine design and development, this article delineates the critical experimental milestones and technical breakthroughs that have defined the field. For researchers and drug development professionals, understanding this evolutionary pathway is paramount for guiding future innovation, particularly in optimizing design principles and overcoming persistent translational challenges. The historical progression from proof-of-concept to clinical application underscores how fundamental discoveries in molecular biology, when combined with advances in nanomedicine, can yield a versatile therapeutic platform with applications spanning infectious diseases, oncology, and genetic disorders [7] [18].
Key Historical Milestones and Experimental Foundations
The development of mRNA vaccine technology spans several decades, marked by key discoveries that incrementally solved fundamental challenges related to mRNA stability, immunogenicity, and delivery. The following timeline and subsequent analysis capture the pivotal milestones that transformed mRNA from a biological concept into a validated clinical modality.
Table 1: Key Historical Milestones in mRNA Vaccine Development
| Year | Milestone | Key Researchers/Entities | Experimental Model | Significance |
|---|---|---|---|---|
| 1961 | Discovery of mRNA | Brenner, Jacob, Meselson | E. coli | Identification of messenger RNA as an information carrier [19]. |
| 1987 | Proof of Concept for Delivery | Malone et al. | Human cells & frog embryos | Demonstrated that mRNA mixed with fat droplets could be taken up by cells to produce proteins [20] [21]. |
| 1990 | First In Vivo Protein Expression | Wolff et al. | Mouse muscle | Showed that direct injection of naked mRNA into mouse muscle could lead to protein expression [19] [22]. |
| 1993 | First Proof-of-Concept mRNA Vaccine | Martinon et al. | Mice | First study showing an mRNA vaccine (against influenza) could elicit a specific immune response [11]. |
| 2005 | Nucleoside Modification to Reduce Immunogenicity | Karikó & Weissman | Human dendritic cells | Demonstrated that incorporating modified nucleosides (e.g., pseudouridine) suppressed innate immune activation and enhanced protein expression [19] [20]. |
| 2010s | Advancement of Lipid Nanoparticles (LNPs) | Multiple groups (e.g., Moderna, BioNTech) | Various animal models | Development of safe and effective ionizable LNPs for systemic mRNA delivery [22] [18]. |
| 2013-2017 | First Clinical Trials for Infectious Diseases | CureVac, Moderna | Human trials | Phase I trials of mRNA vaccines for rabies (CV7202), Zika (mRNA-1893), and others established initial safety and immunogenicity profiles in humans [19] [23]. |
| 2020 | First FDA Authorization of mRNA Vaccines | Pfizer/BioNTech, Moderna | Human populations | Global deployment of nucleoside-modified LNP-mRNA vaccines for COVID-19, demonstrating high efficacy and safety [7] [22]. |
Analysis of Critical Transitions
The timeline reveals two critical transitions that accelerated the field. The first, between 1987 and 1993, shifted the technology from an in vitro curiosity to a viable in vivo platform. Malone's experiment was pivotal as it established the core principle of using a synthetic delivery vector (fat droplets) to protect and deliver mRNA [21]. This was directly translated into the first vaccine proof-of-concept by Martinon et al., who encapsulated mRNA encoding an influenza antigen in liposomes and demonstrated the induction of virus-specific cytotoxic T-cells in mice [11].
The second critical transition occurred in the 2000s-2010s, moving the platform from promising preclinical data to human clinical applicability. The discovery by Karikó and Weissman was foundational, as it solved the major roadblock of excessive innate immune activation by synthetic mRNA. Their key experiment involved transecting human dendritic cells with in vitro-transcribed (IVT) mRNA containing unmodified nucleosides versus mRNA incorporating modified nucleosides like pseudouridine. They measured IFN-γ production and found that modified mRNA evaded immune recognition, leading to a marked increase in protein expression [19] [18]. This breakthrough, combined with parallel advances in LNP technology derived from siRNA therapeutics, created a robust, clinically viable formulation that protected the mRNA payload, facilitated cellular uptake, and provided inherent adjuvant activity [22] [18].
Detailed Experimental Protocols for Key Milestones
Understanding the precise methodologies behind these milestones provides a practical toolkit for researchers designing novel mRNA-based therapeutics. The following protocols detail the foundational experiments.
Protocol 1: Early Proof-of-Concept for mRNA Transfection and Protein Expression
This protocol is adapted from the landmark 1987-1990 experiments that first established the feasibility of using exogenous mRNA to produce proteins in vivo [20] [21].
- Objective: To demonstrate that synthetic mRNA delivered via a lipid carrier can be taken up by cells in vitro and in vivo and translated into a functional protein.
Materials:
- mRNA Template: In vitro-transcribed mRNA encoding a reporter protein (e.g., luciferase or β-galactosidase).
- Delivery Vehicle: Cationic lipid solution (e.g., DOTMA or a simple mixture of mRNA with fat droplets).
- Cells/Animals: Human cells in culture (e.g., HeLa) and/or mouse models.
- Assay Kits: Protein quantification assay (e.g., ELISA, Western blot, or luciferase activity assay).
Procedure:
- mRNA Synthesis: Transcribe the target mRNA in vitro using a bacteriophage RNA polymerase (e.g., T7 polymerase) and a DNA template containing the coding sequence. Include a 5' cap analogue and a 3' poly(A) tail in the reaction.
- Formulation:
- Mix the synthesized mRNA with the cationic lipid solution to form mRNA-lipid complexes.
- Incubate the mixture at room temperature for 15-30 minutes to allow for complex formation.
- In Vitro Transfection:
- Add the mRNA-lipid complexes to cultured human cells.
- Incubate for 24-48 hours.
- In Vivo Administration:
- In a mouse model, inject the formulated mRNA intramuscularly or intravenously.
- Analysis:
- After 24-48 hours, lyse the cells or tissue.
- Quantify the expression of the reporter protein using the appropriate assay (e.g., measure luminescence for luciferase).
- Confirm protein expression and localization via Western blot or immunohistochemistry.
Expected Outcomes: Successful experiments will yield a statistically significant increase in the target protein levels in treated cells or animal tissues compared to negative controls (e.g., treated with lipid only or scrambled mRNA). This confirms the core principle that delivered mRNA can instruct host cells to produce a protein of interest.
Protocol 2: Validating the Impact of Nucleoside Modifications on Immunogenicity and Expression
This protocol is based on the critical 2005 work by Karikó and Weissman that revolutionized mRNA stability and translatability [19] [18].
- Objective: To compare the innate immune activation and protein expression levels induced by unmodified mRNA versus nucleoside-modified mRNA.
Materials:
- mRNA Constructs:
- Test Group 1: IVT mRNA with unmodified uridine.
- Test Group 2: IVT mRNA with modified uridine (e.g., pseudouridine or N1-methylpseudouridine).
- Control: A non-coding RNA or transfection reagent alone.
- Cells: Human immune cells, such as dendritic cells or monocytes.
- Assays: ELISA kits for IFN-α, and a protein expression assay (e.g., flow cytometry for a specific antigen or SEAP assay).
- mRNA Constructs:
Procedure:
- Cell Preparation: Culture human dendritic cells in appropriate media.
- Transfection:
- Transfect the cells with equal masses of either unmodified or nucleoside-modified mRNA using a standard transfection reagent.
- Include the negative control.
- Incubation: Incubate the cells for 16-24 hours.
- Sample Collection:
- Collect cell culture supernatant.
- Harvest a portion of the cells.
- Analysis:
- Immunogenicity: Measure the concentration of type I interferons (e.g., IFN-α) in the supernatant using ELISA.
- Protein Expression: Analyze the harvested cells via flow cytometry to quantify the level of the protein encoded by the mRNA.
Expected Outcomes: Cells transfected with nucleoside-modified mRNA will show significantly lower levels of IFN-α secretion and concurrently higher levels of the encoded protein compared to cells transfected with unmodified mRNA. This result validates that nucleoside modification is a critical strategy for mitigating the innate immune response and maximizing therapeutic protein yield.
Visualization of Critical Workflows
The following diagrams illustrate the logical relationship between key challenges and their corresponding technical solutions, as well as the core mechanism of action of mRNA vaccines.
Diagram 1: Evolution of mRNA Vaccine Technology
This diagram maps the historical challenges in mRNA vaccine development to the breakthroughs that resolved them.
Diagram 2: Mechanism of Immunization by LNP-mRNA Vaccines
This diagram illustrates the cellular mechanism by which LNP-formulated mRNA vaccines induce an immune response.
The Scientist's Toolkit: Essential Research Reagents
The development and production of mRNA vaccines rely on a specific set of reagents and materials. The following table details key components and their functions critical for both research and Good Manufacturing Practice (GMP) production.
Table 2: Essential Research Reagent Solutions for mRNA Vaccine Development
| Category | Reagent/Material | Function | Key Consideration |
|---|---|---|---|
| mRNA Synthesis | DNA Template Plasmid | Provides the genetic template for in vitro transcription (IVT). | Must contain a promoter for T7/SP6 RNA polymerase, the antigen ORF, and a poly(A) tail sequence [11] [18]. |
| T7 RNA Polymerase | Enzyme that transcribes mRNA from the DNA template. | High yield and fidelity are critical for efficient production [19] [18]. | |
| Modified Nucleotides (e.g., N1-methylpseudouridine) | Building blocks for IVT mRNA. Replaces unmodified nucleotides to decrease immunogenicity and enhance stability [19] [18]. | The specific modification (e.g., pseudouridine vs. m1Ψ) can impact protein yield and immune profile. | |
| 5' Capping | CleanCap Technology | Co-transcriptional capping method that yields a high percentage of Cap 1 structure [11]. | Superior to enzymatic capping post-transcription, simplifying the process and increasing efficiency. |
| Purification | Chromatography Materials (FPLC/HPLC) | Removes reaction contaminants like double-stranded RNA (dsRNA), truncated transcripts, and residual enzymes [22]. | Purity is essential for reducing innate immune activation and ensuring consistent product quality. |
| Delivery System | Ionizable Cationic Lipids (e.g., DLin-MC3-DMA, ALC-0315) | Key component of LNPs; ionizable at acidic pH to encapsulate mRNA and facilitate endosomal escape in cells [22] [18]. | The chemical structure dictates efficacy and toxicity profiles. |
| PEGylated Lipid | Stabilizes LNP formulation, modulates pharmacokinetics, and reduces particle aggregation [18]. | Can influence reactogenicity and the protein corona formation. | |
| Helper Lipids (Cholesterol, DSPC) | Integrate into LNP bilayer to enhance structural integrity and fluidity [18]. | Critical for membrane fusion and stability during storage and transport. | |
| Analytical Assays | Cell-based Potency Assays (e.g., using BHK cells) | Measures the expression of the encoded antigen post-transfection to confirm biological activity of the mRNA product [23]. | A critical quality attribute for batch release. |
| dsRNA-Specific ELISA/Kits | Detects and quantifies dsRNA impurities, which are potent inducers of type I interferon [22]. | Essential for monitoring the purity and safety of the final mRNA product. |
Understanding the Self-Adjuvant Effect and Innate Immune Sensing
The lipid nanoparticle (LNP)-encapsulated, nucleoside-modified mRNA vaccine platform represents a transformative advancement in vaccinology, distinguished by its built-in adjuvanticity that does not require traditional adjuvants [24]. This "self-adjuvant" effect stems from the vaccine's fundamental components—both the mRNA molecule itself and the LNP delivery system—which are recognized by the host's innate immune system as non-self, thereby triggering a cascade of immune-activating events [25] [26]. The self-adjuvant effect is crucial for initiating the innate immune responses that subsequently shape potent and durable adaptive immunity [27]. Understanding the precise mechanisms of innate immune sensing of mRNA vaccines is therefore paramount for optimizing their design, improving their efficacy, and mitigating undesirable reactogenicity [24] [28]. This application note details the key mechanisms, experimental data, and methodologies central to investigating these processes, providing a resource for researchers in mRNA vaccine development.
Core Mechanisms of Innate Immune Sensing
The immunogenicity of mRNA-LNP vaccines is driven by the synergistic effect of two primary components: the mRNA molecule, which can be sensed as a foreign pathogen-associated molecular pattern (PAMP), and the LNP, which functions as both a delivery vehicle and an adjuvant [24] [26].
Sensing of the mRNA Component
The innate immune system detects exogenous mRNA through multiple pattern recognition receptors (PRRs) located in various cellular compartments [29] [26]. The specific receptors engaged and the resulting immune profile depend on the nature of the RNA and its impurities.
- Endosomal Sensing: Single-stranded mRNA is primarily sensed by Toll-like receptor 7 (TLR7) and TLR8 within endosomes, leading to the production of pro-inflammatory cytokines and type I interferons (IFN-I) via the MyD88 signaling pathway [25] [29]. Double-stranded RNA (dsRNA) impurities, which can form during in vitro transcription, are potent ligands for TLR3, signaling through the TRIF pathway to induce IFN-I [24] [29].
- Cytosolic Sensing: Once released into the cytoplasm, mRNA and dsRNA impurities can be detected by cytosolic sensors. RIG-I and MDA5 recognize dsRNA and signal through the mitochondrial antiviral-signaling protein (MAVS) to induce a robust IFN-I response [29] [26]. Additionally, dsRNA can activate PKR and OAS, which can inhibit mRNA translation and promote RNA degradation, respectively [24] [29].
Nucleoside modifications (e.g., N1-methylpseudouridine) and high purification to remove dsRNA contaminants are key strategies to modulate this immunogenicity, reducing excessive innate activation while still allowing for a beneficial level of IFN signaling [24].
Adjuvant Effect of the Lipid Nanoparticle (LNP)
The LNP carrier is not an inert delivery vehicle but a significant contributor to the vaccine's adjuvanticity [24]. "Empty" LNPs (formulated without mRNA) can induce local inflammatory responses, characterized by the production of cytokines such as IL-6, GM-CSF, and CCL2 [30] [24]. The ionizable lipid within the LNP is considered critical for this adjuvant activity, though its precise sensing mechanism is still under investigation [24]. The LNP promotes the recruitment and activation of innate immune cells at the injection site and in the draining lymph nodes, creating a pro-inflammatory environment that supports the initiation of adaptive immunity [30] [6].
Table 1: Innate Immune Sensors for mRNA Vaccine Components
| Vaccine Component | Sensing Receptors | Signaling Pathway | Key Cytokine Outputs |
|---|---|---|---|
| mRNA / dsRNA | TLR7/8 (endosomal) | MyD88 | Pro-inflammatory cytokines |
| TLR3 (endosomal) | TRIF | Type I Interferons (IFN-α/β) | |
| RIG-I, MDA5 (cytosolic) | MAVS | Type I Interferons | |
| PKR, OAS (cytosolic) | - | Translation inhibition, RNA degradation | |
| Lipid Nanoparticle (LNP) | Mechanism not fully defined | Inflammasome (?) / IL-6 dependent | IL-6, GM-CSF, CCL2, other chemokines |
Integrated Signaling Pathway
The following diagram summarizes the coordinated innate immune sensing of the mRNA and LNP components of the vaccine, leading to the induction of type I interferons and pro-inflammatory cytokines, which collectively shape the adaptive immune response.
Key Experimental Findings and Data
Recent single-cell transcriptomic studies have delineated the distinct and synergistic contributions of the mRNA and LNP components to the vaccine's innate immune profile and subsequent adaptive immunity.
Distinct Roles of mRNA and LNP
Comprehensive analysis of the vaccine injection site in mice revealed two major axes of transcriptional responses [30]:
- LNP-Driven Response (PC1 Axis): This response is characterized by the induction of pro-inflammatory cytokines and chemokines (e.g., IL-6, TNF, CCL2) and is primarily observed in stromal cells (fibroblasts, endothelial cells). This axis is triggered by both empty LNPs and full mRNA-LNP vaccines [30].
- mRNA-Driven Response (PC2 Axis): This response is highly specific to the mRNA component and is dominated by type I interferon-stimulated genes (ISGs; e.g., ISG15, OASL1). This signature is particularly strong in migratory dendritic cells (mDCs) at the injection site and draining lymph nodes and requires the presence of the mRNA payload within the LNP [30].
Cellular Targets and Fate of mRNA
A critical finding is the identification of injection-site fibroblasts as primary cells enriched with the delivered mRNA. These fibroblasts specifically express IFN-β in response to the mRNA component, establishing a local IFN-rich environment that contributes to the activation of surrounding immune cells [30].
Modulating the IFN Response for Enhanced Immunity
Evidence indicates that the potent IFN-I response triggered by the mRNA, while important for immune activation, can also attenuate the adaptive immune response, potentially by inhibiting antigen translation [6]. Studies in murine models demonstrate that transient blockade of the type I interferon receptor (IFNAR) following immunization significantly enhances both the cellular (antigen-specific CD8+ T cells) and humoral (antigen-specific antibodies) adaptive immune responses [6]. This suggests that fine-tuning the IFN-I signal is a promising strategy for improving mRNA vaccine efficacy.
Table 2: Key Quantitative Findings from Recent mRNA Vaccine Innate Immunity Studies
| Experimental Finding | Model System | Key Readout | Quantitative Outcome / Effect |
|---|---|---|---|
| Fibroblast mRNA Uptake [30] | Mouse single-cell RNA-seq | % of spike mRNA+ cells at injection site | Fibroblasts, endothelial cells, and pericytes highly enriched (2-46% of cells positive, decreasing over time) |
| IFN-β Enhancement of Immunity [30] | Mouse co-injection model (LNP-subunit vaccine + IFN-β) | Antigen-specific T cell responses | Co-injection substantially enhanced cellular immune responses |
| IFNAR Blockade [6] | Mouse IFNAR blocking model | Antigen-specific CD8+ T cells & antibodies | Significant increase in T cell frequencies and antibody titers |
| LNP-specific Cytokine Induction [24] | In vivo and in vitro models | Cytokine production (e.g., IL-6) | Empty LNPs induce IL-6, CCL2, GM-CSF, etc. |
Detailed Experimental Protocols
This section provides methodologies for key experiments used to dissect the self-adjuvant effect of mRNA-LNP vaccines.
Protocol: Single-Cell RNA Sequencing of the Vaccine Injection Site
This protocol is adapted from a study that generated a comprehensive atlas of early immune responses to mRNA vaccination [30].
Objective: To profile the cellular composition and transcriptomic changes at the mRNA vaccine injection site over time.
Materials and Reagents:
- Animals: Female BALB/c mice (age-matched)
- Vaccines: mRNA-LNP (e.g., encoding SARS-CoV-2 spike), empty LNP control, saline (PBS) control
- Dissociation Kit: Skeletal Muscle Dissociation Kit
- Single-Cell Library Prep Kit: 10x Genomics Chromium Single Cell 3' Reagent Kit
- Sequencing Platform: Illumina NovaSeq
Methodology:
- Immunization: Administer mRNA-LNP, empty LNP, or PBS via intramuscular injection into the anterior thigh muscle of mice. Perform both prime and boost injections (3-week interval).
- Tissue Harvest: Euthanize mice at multiple time points post-injection (e.g., 2, 16, 40 hours). Resect the entire injection site (anterior thigh muscle).
- Single-Cell Suspension: Mechanically and enzymatically digest the muscle tissue using the dissociation kit to create a single-cell suspension. Filter through a 70μm cell strainer.
- Library Preparation and Sequencing:
- Count viable cells and adjust concentration.
- Load cells onto the Chromium Controller to generate single-cell gel bead-in-emulsions (GEMs).
- Perform reverse transcription, cDNA amplification, and library construction according to the manufacturer's instructions.
- Sequence libraries to a sufficient depth (e.g., >50,000 reads per cell).
- Bioinformatic Analysis:
- Process raw sequencing data using Cell Ranger to align reads, generate feature-barcode matrices, and perform initial clustering.
- Use Seurat or Scanpy for downstream analysis: normalization, integration, clustering, and identification of differentially expressed genes (DEGs).
- Annotate cell types using canonical marker genes.
- Map vaccine-encoded mRNA reads to a custom reference (e.g., spike open reading frame) to identify and quantify mRNA+ cells.
Protocol: Assessing the Role of Type I Interferon SignalingIn Vivo
This protocol outlines the method for transiently blocking IFNAR to evaluate its impact on vaccine-induced immunity [6].
Objective: To determine the effect of transient IFNAR signaling blockade on the adaptive immune response to an LNP-mRNA vaccine.
Materials and Reagents:
- Animals: Wild-type C57BL/6J mice
- Vaccine: LNP-mRNA (e.g., 5μg dose)
- Anti-IFNAR mAb: Anti-mouse IFNAR1 monoclonal antibody
- Isotype Control: Matching isotype control antibody
- ELISpot Kit: IFN-γ ELISpot kit
- Flow Cytometry Reagents: Fluorochrome-conjugated antibodies against CD3, CD8, CD4, and MHC-I tetramers for relevant antigen
Methodology:
- IFNAR Blockade:
- Inject mice intraperitoneally with 2.5 mg of anti-IFNAR mAb or isotype control.
- Administer the first dose 24 hours before LNP-mRNA immunization and the second dose 24 hours after immunization.
- Immunization: Immunize mice intramuscularly with LNP-mRNA vaccine.
- Immune Response Analysis:
- Humoral Immunity: Collect serum 7-14 days post-boost. Measure antigen-specific antibody titers using ELISA.
- Cellular Immunity (ELISpot): Isolate splenocytes 1-2 weeks post-boost. Stimulate cells with antigen peptides. Perform IFN-γ ELISpot according to kit instructions to quantify antigen-specific T-cell responses.
- Cellular Immunity (Flow Cytometry): Stimulate splenocytes with antigen peptides in the presence of brefeldin A. Stain surface markers (CD3, CD8, CD4) and intracellular IFN-γ. Analyze by flow cytometry. Use MHC-I tetramers to directly identify antigen-specific CD8+ T cells.
The Scientist's Toolkit: Key Research Reagents
The following table lists essential reagents and their applications for studying the innate immune sensing of mRNA vaccines.
Table 3: Essential Research Reagents for Investigating mRNA Vaccine Innate Immunity
| Research Reagent / Tool | Primary Function/Application | Key Utility in mRNA Vaccine Research |
|---|---|---|
| N1-methylpseudouridine (m1Ψ) mRNA [24] | Nucleoside-modified mRNA with reduced immunogenicity | Standard component to enhance translation and modulate innate sensing; baseline for comparing unmodified mRNA effects. |
| Ionizable Lipids (e.g., ALC-0315, SM-102) [24] | Key component of LNPs for endosomal escape and adjuvant effect | Used in LNP formulation to study the specific adjuvant contribution of the lipid component. |
| Empty LNPs [30] [6] | LNP formulation without an mRNA payload | Critical control for dissecting the immune contribution of the LNP carrier vs. the mRNA payload. |
| Anti-IFNAR Blocking Antibody [6] | In vivo blockade of type I interferon signaling | Tool to investigate the functional role of IFN-I responses in shaping vaccine immunogenicity and efficacy. |
| IFN-γ ELISpot Kit | Ex vivo quantification of antigen-specific T cell responses | Standard assay for evaluating the cellular immune response induced by vaccination. |
| PRR Agonists/Antagonists | Activate or inhibit specific innate sensing pathways | Used to delineate the contribution of specific receptors (e.g., TLR7, RIG-I, MDA5) to the overall immune response. |
Visualization of Experimental Workflow
The following diagram outlines a consolidated experimental workflow for deconvoluting the self-adjuvant effect of mRNA-LNP vaccines, integrating the protocols and concepts described above.
Advanced Antigen Design, Delivery Systems, and Expanding Applications
Within the broader thesis of advancing mRNA vaccine design, the strategic engineering of antigen structure is a cornerstone for developing potent and durable immunogens. The native, prefusion conformation of many viral glycoproteins often presents the most vulnerable targets for neutralizing antibodies. However, these proteins are frequently metastable, undergoing conformational changes to facilitate host cell entry. Through precision antigen engineering, scientists can stabilize these antigens in their prefusion state, thereby eliciting a more potent and protective immune response. This document provides detailed application notes and protocols for two principal structure-based stabilization strategies: proline substitution and disulfide bond engineering, framing them within the context of modern mRNA vaccine development for researchers and drug development professionals.
Principles of Structure-Based Antigen Design
Structure-based vaccine design begins with a detailed examination of the target antigen's architecture. The goal is to stabilize a specific conformational state—typically the prefusion form of a viral fusion protein—by increasing its thermodynamic and kinetic stability. This is achieved by manipulating the fundamental forces that govern protein folding, including hydrophobic interactions, hydrogen bonding, and electrostatic forces [31]. The choice of stabilization strategy is guided by high-resolution structural data from techniques such as X-ray crystallography and cryo-electron microscopy (cryo-EM), often complemented by computational modeling [32] [33].
The workflow below outlines the logical progression from structural analysis to the selection and validation of a stabilization strategy.
Proline Stabilization Strategies
Mechanism and Application Notes
Introducing proline mutations is a widely validated strategy for stabilizing the prefusion conformation of class I viral fusion proteins. Proline's unique cyclic structure acts as a helix breaker due to its restricted phi-angle and lack of an amide hydrogen for helical hydrogen bonding. When introduced at the N-terminal end of a helix in a helix-turn-helix motif that refolds during fusion, proline substitution kinetically traps the protein in its prefusion state by disfavoring the formation of the extended postfusion coiled-coil [31] [32].
This approach has been successfully applied to the spike (S) proteins of coronaviruses. The seminal S-2P mutation (K986P/V987P in SARS-CoV-2) stabilizes the prefusion conformation and was a cornerstone of the first-generation COVID-19 mRNA vaccines (BNT162b2 and mRNA-1273) [32] [31]. Second-generation designs, such as the S-6P variant (incorporating F817P, A892P, A899P, A942P, K986P, V987P), have demonstrated even greater stability and immunogenicity, including broader cross-neutralizing activity against variants of concern like Delta and Omicron [32].
Protocol: Design and In Vitro Validation of Proline-Stabilized Antigens
Objective: To design a proline-stabilized antigen and validate its conformational stability and antigenicity in vitro.
Materials:
- Expression vector (e.g., pcDNA3.1) containing the gene for the target viral glycoprotein.
- Site-directed mutagenesis kit.
- Mammalian cell line for protein expression (e.g., Expi293F cells).
- Conformation-specific monoclonal antibodies.
- Equipment for Differential Scanning Fluorimetry (nanoDSF) and Size Exclusion Chromatography (SEC).
Procedure:
- Structural Analysis and Design:
- Identify helix-turn-helix motifs in the target protein that undergo conformational rearrangement during membrane fusion using structural data (PDB files) and literature.
- Select target residues at the N-terminal end of these helices for substitution with proline.
- Use software like PyMol or Rosetta for in silico modeling to assess the structural impact of the proposed mutations.
Gene Construct Generation:
- Introduce the selected proline mutations into the antigen gene using a site-directed mutagenesis protocol per the manufacturer's instructions.
- Sequence the entire gene to confirm the presence of the desired mutations and the absence of errors.
Recombinant Protein Expression and Purification:
- Transfect Expi293F cells with the wild-type and proline-mutant plasmids using a standard transfection reagent.
- Culture cells for 3-7 days and harvest the supernatant.
- Purify the secreted antigen using affinity chromatography (e.g., Ni-NTA for his-tagged proteins) followed by buffer exchange.
Conformational Stability Assessment:
- Differential Scanning Fluorimetry (nanoDSF): Determine the melting temperature (Tm) of the wild-type and stabilized antigens. A higher Tm indicates improved thermodynamic stability. Use a protein concentration of 0.5-1 mg/mL and a temperature ramp of 1°C/min.
- Size Exclusion Chromatography (SEC): Analyze the oligomeric state and homogeneity of the proteins. A single, symmetric peak at the expected molecular weight for the trimer (or other native oligomer) confirms proper folding and assembly.
Antigenicity Validation:
- Perform an enzyme-linked immunosorbent assay (ELISA) to test binding of conformation-specific antibodies. Coat plates with 1 µg/mL of wild-type or stabilized antigen. Incubate with a dilution series of known prefusion-specific and postfusion-specific antibodies. A stabilized prefusion antigen will show strong binding to prefusion-specific antibodies and weak binding to postfusion-specific antibodies.
Quantitative Outcomes of Proline Stabilization
Table 1: Efficacy of Proline Stabilization in Vaccine Antigens
| Antigen / Vaccine | Stabilization Strategy | Key Mutations | Immunogenicity Outcome | Reference / Trial |
|---|---|---|---|---|
| SARS-CoV-2 (1st Gen) | S-2P | K986P, V987P | Foundation of BNT162b2 & mRNA-1273; high efficacy (94-95%) | [32] [34] |
| SARS-CoV-2 (2nd Gen) | S-6P | F817P, A892P, A899P, A942P, K986P, V987P | 28.3- to 50.3-fold ↑ in nAb titers vs S-2P; cross-neutralization | BNT162b5 (Phase 2, NCT05472038) [32] |
| MERS-CoV Spike | S-2P | K983P, V984P | Stabilized prefusion conformation, enhanced immunogenicity | [32] [31] |
Disulfide Bond Engineering Strategies
Mechanism and Application Notes
Disulfide bond engineering involves introducing paired cysteine mutations at strategic positions within the antigen. The covalent bond formed between the sulfur atoms of the two cysteines conformationally "locks" the protein, drastically reducing its flexibility and increasing its kinetic stability by disfavoring transition to alternative states [31] [35].
This method has been pivotal for pathogens like Respiratory Syncytial Virus (RSV). The DS-Cav1 construct, which incorporates disulfide bonds and cavity-filling mutations, stabilized the prefusion F protein and paved the way for effective RSV vaccines, including the mRNA-1345 (mRESVIA) vaccine, which demonstrated 83.7% efficacy in a Phase III trial [32] [33]. Beyond enveloped viruses, disulfide engineering has also been successfully applied to stabilize virus-like particles (VLPs) for non-enveloped viruses like norovirus. Introducing a single disulfide bond (N112C/N189C) in the GII.3 norovirus VLP significantly increased yield, thermal stability, and ultimately elicited superior humoral immune responses in mice compared to the wild-type VLP [35].
Protocol: Rational Design and Testing of Disulfide-Stabilized Antigens
Objective: To design a disulfide-stabilized antigen and biochemically confirm the formation of the disulfide bond and its stabilizing effect.
Materials:
- All materials listed in Section 3.2.
- Non-reducing and reducing Laemmli sample buffers.
- Materials for Negative-Stain Electron Microscopy (nsEM).
Procedure:
- Rational Design of Cysteine Pairs:
- Analyze the antigen structure to identify two backbone positions that are spatially proximal (Cβ–Cβ distance < 4-6 Å) in the desired prefusion state but become separated in the postfusion state.
- Select residues in flexible loops, hinges, or at subunit interfaces. Avoid positions that are part of known neutralizing epitopes.
- Use computational tools (e.g., Disulfide by Design, PyRosetta) to model the cysteine substitutions and predict the feasibility of disulfide bond formation.
Generation, Expression, and Purification:
- Follow the same steps as in Section 3.2, Steps 2-3, to generate and purify the disulfide mutant antigen.
Disulfide Bond Formation Analysis:
- Non-Reducing vs. Reducing SDS-PAGE: Prepare two samples of the purified antigen: one with standard reducing buffer (containing β-mercaptoethanol or DTT) and one with non-reducing buffer. A disulfide-stabilized protein will migrate faster on non-reducing gels due to its more compact structure, while the reduced protein will migrate at its expected monomeric weight.
Stability and Functional Assays:
- Perform nanoDSF and SEC as described in Section 3.2 to assess thermal stability and oligomeric state.
- For VLPs or complex antigens, use nsEM to visualize particle homogeneity and integrity. Compare wild-type and stabilized samples stained with uranyl acetate.
- Conduct functional assays such as HBGA blocking assays (for norovirus) or receptor binding assays (for coronaviruses) to ensure the engineered disulfide does not disrupt key functional domains [35].
Quantitative Outcomes of Disulfide Bond Engineering
Table 2: Efficacy of Disulfide Bond Engineering in Vaccine Antigens
| Antigen / Vaccine | Stabilization Strategy | Key Mutations / Bond | Immunogenicity & Stability Outcome | Reference / Trial |
|---|---|---|---|---|
| RSV F Protein | DS-Cav1 (Disulfide + Cavity-fill) | Multiple (S155C, S290C, S190F, V207L) | Foundation for mRNA-1345; 83.7% efficacy against LRTD | Phase III [32] [33] |
| Norovirus GII.3 VLP | Single Disulfide (DS1) | N112C / N189C | ↑ Yield, ↑ thermal stability, superior HBGA blocking Ab in mice | [35] |
| SARS-CoV-2 Spike | Disulfide "Lock" | RBD-directed disulfide bonds | Controlled RBD "up"/"down" states; balanced immune response | [32] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Precision Antigen Engineering
| Reagent / Material | Function / Application | Example Product / Specification |
|---|---|---|
| Expi293F Cell Line | Mammalian protein expression system for producing properly folded and glycosylated antigens. | Thermo Fisher Scientific, Cat # A14527 |
| Site-Directed Mutagenesis Kit | Introduction of point mutations (proline or cysteine) into plasmid DNA. | Q5 Site-Directed Mutagenesis Kit (NEB) |
| nanoDSF Instrument | Label-free measurement of protein thermal stability (Tm). | Prometheus Panta (NanoTemper) |
| AKTA Pure System | Fast Protein Liquid Chromatography (FPLC) for Size Exclusion Chromatography (SEC). | Cytiva |
| Conformation-Specific mAbs | Critical reagents for validating the native prefusion structure via ELISA and other binding assays. | e.g., Prefusion-specific anti-RSV F mAb |
| Negative-Stain EM Reagents | Visualizing the structure and homogeneity of VLPs and protein complexes. | Uranyl Acetate, 400-mesh Carbon-coated grids |
The integration of proline stabilization and disulfide bond engineering into the mRNA vaccine development pipeline represents a paradigm shift in antigen design. These structure-guided strategies enable the production of robust, conformationally defined immunogens that are directly encoded by the mRNA platform. As demonstrated by their critical role in successful vaccines against COVID-19 and RSV, and their promising application in developing candidates for pathogens like norovirus, these precision engineering techniques are indispensable for creating the next generation of vaccines against existing and emerging pathogenic threats. The provided protocols offer a foundational roadmap for researchers to apply these powerful techniques in their own vaccine development efforts.
Lipid Nanoparticles (LNPs) have emerged as the cornerstone delivery system for messenger RNA (mRNA) therapeutics, decisively enabling the clinical success of mRNA vaccines and expanding into broader therapeutic areas. As non-viral vectors, LNPs effectively address the fundamental challenges of mRNA delivery—including enzymatic degradation, cellular uptake, and endosomal escape—through a multicomponent architecture that stabilizes the nucleic acid payload and facilitates its intracellular release. The unparalleled efficacy of LNP-formulated COVID-19 vaccines, with efficacy rates of approximately 95%, has validated this platform and accelerated its adoption for infectious diseases, cancer immunotherapy, and rare genetic disorders [36] [37]. This document details the core components, advanced formulations, and standardized protocols that define LNPs as the gold standard in mRNA delivery, providing researchers with actionable methodologies for therapeutic development.
LNP Architecture and Next-Generation Components
A deep understanding of LNP composition is essential for rational design. The core structure consists of four key components, each fulfilling a distinct functional role, with recent research focusing on novel ionizable lipids and strategic PEG-lipid optimization to enhance efficacy and safety.
Table 1: Core Components of mRNA-LNPs
| Component | Function | Examples | Recent Advances |
|---|---|---|---|
| Ionizable Lipid | Encapsulates mRNA, mediates endosomal escape via protonation | SM-102, ALC-0315 | AMG1541: Cyclic structures, ester tails for biodegradability [17]. Lipid 7: Tail length modulation reduces liver accumulation [38]. |
| Helper Phospholipid | Stabilizes LNP structure, promotes membrane fusion | DSPC, DOPE | DOPE often preferred for enhanced fusogenicity [36]. |
| Cholesterol | Enhances membrane integrity and stability, promotes fusion | Cholesterol | Integral to LNP morphology and fluidity [36]. |
| PEGylated Lipid | Shields LNP surface, controls particle size, modulates PK | DMG-PEG2000, ALC-0159 | Optimal content is application-dependent (1.5-5.0 mol%), balancing stability vs. cellular uptake [39]. |
Innovations in Ionizable Lipids
Ionizable lipids are the central functional component of LNPs. Novel designs focus on improving biodegradability and reducing organ-specific toxicity. The lipid AMG1541, featuring cyclic structures and ester-containing tails, demonstrated a hundred-fold increase in delivery efficiency in murine models compared to SM-102, enabling a proportional reduction in vaccine dose [17]. Concurrently, strategies to mitigate liver accumulation and associated hepatotoxicity have led to lipids like Lipid 7, which is engineered with specific tail lengths to enhance expression at the injection site while reducing off-target accumulation [38].
Optimizing PEGylated Lipids
The PEG-lipid component presents a formulation dilemma, requiring a balance between nanoparticle stability and cellular uptake. Systematic investigation reveals a bell-shaped relationship between PEG-lipid content and transfection efficiency. An in vitro study found that 1.5% DMG-PEG2000 yielded optimal mRNA transfection, whereas 5% DMG-PEG2000 was superior for in vivo performance, attributed to improved nanoparticle stability and prolonged systemic circulation [39]. This underscores the necessity of context-specific formulation optimization.
Advanced Formulation Strategies and Quantitative Performance
The field is advancing beyond standard formulations to address challenges in loading capacity, targeting, and stability. The following table summarizes the performance of next-generation LNP systems.
Table 2: Performance of Advanced LNP Formulation Strategies
| Formulation Strategy | Key Mechanism | Reported Efficacy/Improvement | Primary Application |
|---|---|---|---|
| Metal-Ion Enrichment (L@Mn-mRNA) | Mn2+ pre-condenses mRNA into high-density core | ≈2x mRNA loading capacity; ≈2x cellular uptake [40] | Platform for dose-sparing vaccines |
| Ionizable Lipid AMG1541 | Enhanced endosomal escape; biodegradable ester tails | 100x higher potency vs. SM-102 (in mice) [17] | Intramuscular vaccines (e.g., Influenza) |
| Low-Liver-Accumulation (Lipid 7) | Tail-length engineering to alter biodistribution | 3x higher mRNA expression at injection site; reduced hepatotoxicity [38] | Therapeutic tumor vaccines (e.g., HPV) |
| Buffer Optimization | Histidine buffer mitigates lipid oxidation & RNA adducts | Enables room-temperature stability for 6 months vs. 2 weeks in PBS [41] | Improving shelf-life and storage |
Experimental Protocols for LNP Development
This section provides detailed methodologies for key procedures in LNP research and development.
Protocol: Microfluidic Formulation of mRNA-LNPs
This is the standard method for producing monodisperse, stable LNPs [39] [38].
- Objective: To prepare mRNA-LNPs with high encapsulation efficiency and a narrow particle size distribution.
- Materials:
- Lipid Stock Solution: Ionizable lipid, DSPC, Cholesterol, and DMG-PEG2000 dissolved in anhydrous ethanol (e.g., total lipid concentration of 12.5 mM).
- Aqueous Phase: mRNA dissolved in citrate or acetate buffer (e.g., 25-50 mM, pH 5.0).
- Microfluidic mixer (e.g., NanoAssemblr, microfluidic chip with T-junction).
- Syringe pumps or pressure-controlled pump.
- Tris-HCl buffer (pH 7.8) for dialysis or diafiltration.
- Procedure:
- Prepare Phases: Mix the lipid components at the desired molar ratio (e.g., 50:10:38.5:1.5 for ionizable lipid:DSPC:Chol:DMG-PEG) in ethanol. Dilute mRNA in acid buffer to a concentration suitable for mixing.
- Microfluidic Mixing: Load the organic and aqueous phases into separate syringes. Pump the solutions through a microfluidic mixer at a defined flow rate ratio (typically 3:1, aqueous:organic) and a controlled total flow rate (e.g., 12 mL/min).
- Initial Processing: Collect the resulting LNP suspension and dilute it with Tris-HCl buffer (pH 7.8).
- Buffer Exchange & Purification: Remove ethanol and exchange the buffer into the final storage buffer (e.g., sucrose, histidine) using tangential flow filtration (TFF) or dialysis.
- Sterile Filtration: Filter the final LNP solution through a 0.22 µm sterile filter.
Protocol: Characterization of mRNA-LNPs
Comprehensive characterization is critical for quality control and correlating structure with function [39] [38].
- Objective: To determine the critical quality attributes (CQAs) of formulated mRNA-LNPs.
- Procedures:
- Particle Size and PDI: Measure hydrodynamic diameter and polydispersity index (PDI) via Dynamic Light Scattering (DLS). Acceptable PDI is typically ≤0.2.
- Zeta Potential: Measure surface charge using Laser Doppler Micro-electrophoresis.
- mRNA Encapsulation Efficiency (EE%):
- Prepare two samples: (A) intact LNPs diluted in buffer, and (B) LNPs lysed with 1-2% Triton X-100.
- Add RiboGreen reagent to both samples.
- Measure fluorescence (Ex/Em: 480/520 nm). The fluorescence of sample A represents free mRNA, while sample B represents total mRNA.
- Calculate EE%:
EE% = [1 - (Fluorescence A / Fluorescence B)] * 100.
- Morphology: Visualize LNPs using Transmission Electron Microscopy (TEM) with negative staining (e.g., 1% uranyl acetate).
Protocol: In Vitro Screening of Transfection Efficiency
This protocol provides a medium-throughput method for screening LNP libraries [38].
- Objective: To evaluate the functionality of LNPs in delivering mRNA to cultured cells.
- Materials:
- Relevant cell lines (e.g., HeLa, DC2.4, 293T).
- LNP formulation encapsulating reporter mRNA (e.g., eGFP, Luciferase).
- Flow cytometer (for eGFP) or microplate reader (for Luciferase).
- Procedure:
- Seed cells in a 24-well plate at a density of 2x10^5 cells/well and culture overnight.
- Transfert cells with LNPs containing a standardized amount of mRNA (e.g., 200 ng).
- Incubate for 24-48 hours.
- For eGFP mRNA: Harvest cells, and analyze the percentage of eGFP-positive cells and mean fluorescence intensity using a flow cytometer.
- For Luciferase mRNA: Lyse cells and measure luminescent signal using a microplate reader according to the luciferase assay kit instructions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for LNP Research
| Reagent / Material | Function / Role | Example Specifications |
|---|---|---|
| Ionizable Lipids | Functional core of the LNP; enables mRNA encapsulation and endosomal escape | SM-102, ALC-0315 (patented); AMG1541, Lipid 7 (novel designs) [17] [38] |
| PEGylated Lipids | Controls nanoparticle size, stability, and pharmacokinetics | DMG-PEG2000 (C14 tail), DSPE-PEG2000 (C18 tail) [39] |
| Helper Phospholipids | Supports LNP bilayer structure and membrane fusion | DSPC, DOPE [36] |
| Microfluidic Mixer | Enables reproducible, scalable production of monodisperse LNPs | NanoAssemblr, custom PDMS chips [37] |
| RiboGreen Assay Kit | Critical for quantifying mRNA encapsulation efficiency | Quant-iT RiboGreen RNA Assay Kit [39] [38] |
| Histidine Buffer | Formulation buffer that enhances LNP stability at room temperature | 10-50 mM, pH ~6.0-6.5, mitigates lipid oxidation [41] |
Visualizing the LNP Development Workflow
The following diagram illustrates the integrated workflow for the rational design, formulation, and testing of novel Lipid Nanoparticles.
The design and development of effective mRNA vaccines hinge on the precise optimization of the mRNA molecule itself. The remarkable success of mRNA vaccines against SARS-CoV-2 has underscored the critical importance of sequence engineering to enhance translational efficiency, stability, and immunogenicity while minimizing undesirable immune activation. This document provides detailed application notes and protocols for the three pillars of mRNA sequence optimization: nucleoside modification, untranslated region (UTR) engineering, and poly(A) tail design. Framed within the broader context of mRNA vaccine design, these guidelines are intended to equip researchers and drug development professionals with the foundational and advanced techniques required to develop next-generation mRNA therapeutics.
Nucleoside Modification
Chemical modification of nucleosides is a foundational strategy to improve the performance of mRNA vaccines. These modifications are crucial for reducing the innate immunogenicity of in vitro transcribed (IVT) mRNA and can significantly enhance both the stability and translational efficiency of the transcript.
Rationale and Key Modifications
Native mRNA is recognized by pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) and RIG-I, triggering type I interferon responses that can inhibit translation. Replacing natural nucleosides with modified analogues is an effective method to dampen this recognition. The most prominent modification involves replacing uridine (U) with pseudouridine (Ψ) or its methylated derivative, N1-methylpseudouridine (m1Ψ), which has been a key feature of clinically approved COVID-19 mRNA vaccines [42] [43]. These modifications not only reduce immunogenicity but also improve translation efficiency. However, recent studies indicate that m1Ψ can cause ribosomal frameshifting, potentially leading to the production of off-target proteins, a factor that must be considered in vaccine design [42].
Other common modifications include 5-methylcytidine (m5C), 5-methyluridine (m5U), and N1-methyladenosine (m1A), which can also lower immunogenicity [42]. Beyond immunogenicity, recent innovations explore ribose modifications, such as the introduction of a 2´-fluoro (2´-F) group at specific positions within the open reading frame (ORF). Notably, modifying the first nucleoside of a codon (1st NC) with 2´-F can significantly bolster mRNA stability without substantially compromising translation, whereas similar modifications at the second or third nucleoside are more detrimental to protein production [44].
Table 1: Common Nucleoside Modifications and Their Effects
| Modification | Base | Key Effects | Considerations |
|---|---|---|---|
| N1-methylpseudouridine (m1Ψ) | Uridine | Significantly reduces innate immune activation; enhances translation efficiency [43] [42]. | Can induce ribosomal frameshifting, potentially leading to aberrant protein products [42]. |
| Pseudouridine (Ψ) | Uridine | Reduces immunogenicity; improves translation efficiency [42]. | Effect may be less pronounced than m1Ψ. |
| 2´-fluoro (2´-F) | Ribose (any base) | Increases nuclease resistance and mRNA stability. Position-dependent effect: best tolerated at the first nucleoside of a codon [44]. | Modification at the second or third codon nucleoside can suppress translation by 30-50% [44]. |
| 5-methylcytidine (m5C) | Cytidine | Reduces immunogenicity [42]. | Often used in combination with uridine modifications. |
| 5-methyluridine (m5U) | Uridine | Reduces immunogenicity [42]. | An alternative to pseudouridine modifications. |
Protocol: Evaluating Nucleoside-Modified mRNA
Objective: To produce and test the functionality of mRNA incorporating modified nucleosides. Application: Screening modified nucleotides for enhanced translation and reduced immunogenicity in vaccine candidates.
Materials and Reagents:
- DNA Template: A linearized plasmid containing T7 promoter, target ORF (e.g., SARS-CoV-2 spike protein), and a poly(A) tail sequence.
- Nucleoside Triphosphates (NTPs): Standard NTPs or modified NTPs (e.g., m1Ψ-UTP, m5C-CTP).
- IVT Kit: T7 RNA polymerase, reaction buffer, RNase inhibitor.
- Capping Reagent: CleanCap AG (for co-transcriptional capping) [11].
- DNase I (RNase-free): To digest the DNA template post-transcription.
- mRNA Purification Kit: e.g., silica membrane-based kits or LiCl precipitation.
- Cell Culture: Relevant cell lines (e.g., HEK-293, HeLa, or primary human cells).
- Transfection Reagent: Lipid nanoparticles (LNPs) or commercial transfection reagents.
- Analysis Tools: ELISA kits for antigen quantification, flow cytometry antibodies, or luciferase assay systems.
Procedure:
- In Vitro Transcription (IVT):
- Set up a reaction mixture containing 1 µg of linearized DNA template, T7 RNA polymerase buffer, 7.5 mM of each NTP (including modified NTPs as required), and T7 RNA polymerase.
- For co-transcriptional capping, include CleanCap AG reagent. This yields a high proportion (~94%) of the desired Cap 1 structure, which is superior to Cap 0 for translation and immune evasion [11].
- Incubate at 37°C for 2-4 hours.
- DNase I Treatment and Purification:
- Add DNase I to the IVT reaction and incubate for 15-30 minutes at 37°C to remove the DNA template.
- Purify the mRNA using a commercial purification kit, following the manufacturer's instructions. Determine concentration and purity by spectrophotometry (A260/A280 ratio).
- Quality Control:
- Analyze mRNA integrity by denaturing agarose gel electrophoresis. A single, sharp band should be visible.
- Use LC-MS to confirm the sequence and modification incorporation for critical applications [44].
- Cell Transfection and Expression Analysis:
- Culture appropriate cells (e.g., HEK-293) in a 24-well plate until 70-90% confluent.
- Formulate the purified mRNA into LNPs or complex with a transfection reagent.
- Transfert cells with a dose range of mRNA (e.g., 10-500 ng/well). Include an unmodified mRNA control and a mock transfection control.
- Harvest cells 24-48 hours post-transfection.
- Quantify Protein Expression:
- ELISA: Use antigen-specific ELISA to quantify protein production in cell lysates or supernatants [44].
- Flow Cytometry: If the encoded protein is surface-expressed, use specific antibodies for detection and analysis [43].
- Luciferase Assay: If the ORF encodes luciferase, measure luminescence activity in cell lysates [45].
UTR Engineering
The 5' and 3' untranslated regions (UTRs) are critical regulatory elements that control mRNA stability, localization, and translational efficiency. Optimizing UTRs is essential for maximizing therapeutic protein expression.
Protocol: Screening UTR Combinations
Objective: To empirically determine the optimal 5' and 3' UTR combination for a given mRNA construct. Application: Optimizing UTRs for vaccine antigens or therapeutic proteins to achieve maximal and sustained expression.
Materials and Reagents:
- DNA Templates: A library of linearized plasmids with identical ORFs (e.g., firefly luciferase or the antigen of interest) but varying combinations of 5' and 3' UTRs.
- IVT and Transfection Reagents: As listed in Section 2.2.
- In Vivo Model: Mice for intramuscular or intravenous administration of formulated mRNA.
Procedure:
- Construct Design and mRNA Synthesis:
- Clone selected 5' and 3' UTR combinations upstream and downstream of the reporter ORF in an IVT plasmid vector.
- Generate mRNA from each construct using the IVT and purification protocol described in Section 2.2, ensuring consistent capping and tailing.
- In Vitro Screening:
- Transfect each mRNA construct into relevant cell lines (e.g., HeLa, A549) in triplicate.
- Measure reporter gene expression (e.g., luminescence) at multiple time points (e.g., 6, 24, 48 hours) to assess both the peak and duration of expression.
- Identify the top-performing UTR combinations for further validation.
- In Vivo Validation:
- Formulate the lead mRNA candidates into LNPs.
- Administer the mRNA-LNPs to mice (e.g., 5 µg via intramuscular injection) [45].
- Monitor protein expression over time using non-invasive imaging (for luciferase) or serum analysis (for secreted proteins like hEPO) [45].
- For vaccine contexts, immunize mice and measure antigen-specific T-cell and antibody responses to confirm the enhanced immunogenicity of the optimized construct [46].
Poly(A) Tail Engineering
The 3' poly(A) tail is a key determinant of mRNA stability and translation, primarily through its interaction with poly(A)-binding protein (PABP), which promotes ribosome recycling and protects the mRNA from decay.
Tail Length, Structure, and Modification
While longer poly(A) tails (e.g., 100-120 nucleotides) generally enhance translation and stability by recruiting more PABP, recent research highlights that tail structure is equally important. Introducing structural elements into the tail can profoundly impact mRNA function.
A pivotal innovation is the design of a loop structure within the poly(A) tail. For example, a tail designed as "A50-Linker-A50-complementary linker sequence" (A50L50LO) allows the linker to base-pair with its complementary sequence, forming a stable loop. This structure has been shown to significantly enhance translation efficiency and prolong protein expression both in vitro and in vivo compared to standard linear poly(A) tails [45].
Furthermore, chemical modifications can be applied to the poly(A) tail. Incorporating 2'-F or 2'-O-MOE modifications every few nucleotides, particularly in the terminal region, can further increase stability by protecting the tail from nucleases. Combining these modifications with a phosphorothioate backbone linkage in the terminal nucleotides can offer additional stability benefits [44].
Table 2: Poly(A) Tail Designs and Their Performance
| Tail Design | Description | Performance & Effect |
|---|---|---|
| A120 | Linear sequence of 120 adenosines. | Standard long tail; good translation efficiency [45]. |
| A50L50LX | A50-Linker-A50 with non-complementary linker. | Linear control; performance similar to A120 [45]. |
| A50L50LO | A50-Linker-A50 with a complementary linker sequence that forms a loop. | Highest protein expression in vitro and in vivo; improved mRNA stability and duration [45]. |
| Modified A-tail | e.g., 2'-F modification every 2 nt, with terminal 2'-O-MOE and phosphorothioate. | Increases nuclease resistance; enhances translational activity compared to unmodified poly(A) [44]. |
Protocol: Engineering and Testing a Looped Poly(A) Tail
Objective: To construct an mRNA with a loop-stabilized poly(A) tail and evaluate its efficacy. Application: Enhancing the stability and translational capacity of mRNA vaccines, particularly for applications requiring durable protein expression.
Materials and Reagents:
- DNA Template: Plasmid containing the ORF of interest followed by the "A50-Linker-Complementary Linker-A50" sequence.
- IVT and Formulation Reagents: As previously described.
- In Vivo Imaging System (IVIS): For longitudinal tracking of luciferase expression in live animals.
Procedure:
- Template Construction and mRNA Synthesis:
- Synthesize a DNA fragment encoding the desired looped tail structure (e.g., A50L50LO) and clone it downstream of the ORF stop codon in your IVT vector.
- Generate mRNA from this construct and a linear tail control (e.g., A120) using the standard IVT protocol.
- In Vitro Characterization:
- Transfert cells with equimolar amounts of the looped-tail and control mRNAs.
- Measure protein output at 6, 24, and 48 hours post-transfection. The A50L50LO construct is expected to show superior, sustained expression, especially at later time points [45].
- In Vivo Efficacy Assessment:
- Formulate the mRNAs into LNPs and administer to mice intramuscularly.
- Image luciferase activity at 6 and 24 hours post-injection. The looped-tail mRNA should maintain a significantly higher signal at the 24-hour mark [45].
- For vaccine studies, immunize mice with mRNAs encoding a viral antigen (e.g., influenza HA) and compare the magnitude of the resulting humoral and cellular immune responses.
Integrated Workflow and Signaling Pathways
The optimization of nucleosides, UTRs, and the poly(A) tail is an interconnected process. The following diagram and workflow summarize the key decision points and their functional impacts on mRNA vaccine design.
Diagram 1: The interrelationship between mRNA optimization strategies and their primary functional outcomes. The three core engineering approaches (green) each target a specific key performance attribute (blue) to collectively produce an optimized mRNA vaccine candidate (red).
Integrated Experimental Workflow
- Design: Create a library of mRNA constructs that systematically vary one parameter at a time (e.g., UTR combination, nucleoside mix, tail structure).
- Synthesis: Produce mRNA using high-fidelity IVT with co-transcriptional capping (e.g., CleanCap) to ensure consistency.
- In Vitro Screening: Transfert constructs into biologically relevant cell lines. Use high-throughput methods (e.g., luciferase, flow cytometry) to quantify protein expression and ELISA/qPCR to assess immunogenicity and mRNA half-life.
- Lead Formulation: Formulate top-performing candidates into LNPs. Different ionizable lipids (e.g., SM-102, cKK-E10) can synergistically impact translation and immune activation and should be tested [43].
- In Vivo Validation: Evaluate lead formulations in animal models for protein expression kinetics, immunogenicity (antibody and T-cell responses), and efficacy against pathogen challenge.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for mRNA Sequence Optimization and Analysis
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| Modified NTPs | Reduces immunogenicity and can enhance translation of IVT mRNA. | N1-methylpseudouridine-5'-triphosphate (m1Ψ TP) [42]. |
| Co-transcriptional Capping Reagent | Adds a 5' cap during IVT, improving translation efficiency and mRNA stability. | CleanCap AG [11]. Yields a high percentage of Cap 1 structure. |
| Ionizable Lipids for LNPs | Critical component of delivery vehicles; affects mRNA delivery, translation, and reactogenicity. | SM-102, cKK-E10, OF-02. Choice of lipid can synergize with nucleoside modifications [43]. |
| Linearized DNA Template | Template for IVT mRNA synthesis. | Plasmid with strong promoter (e.g., T7), optimized UTRs, ORF, and defined poly(A) tail. |
| T7 RNA Polymerase | Enzyme for synthesizing mRNA from a DNA template in vitro. | High-yield, mutant versions can reduce dsRNA byproducts [42]. |
| Luciferase Assay Kit | Quantitative measurement of translation efficiency for screening. | Firefly or NanoLuc luciferase systems for in vitro and in vivo tracking [45]. |
| RNA Purification Kits | Purification of IVT mRNA from reaction components. | Silica-membrane spin columns or LiCl precipitation. |
The success of mRNA vaccines during the COVID-19 pandemic has validated a versatile platform technology with transformative potential across medicine. Unlike conventional vaccine approaches, mRNA technology offers a rapid, cell-free manufacturing process and exceptional flexibility in antigen design, enabling swift responses to evolving pathogens [18] [47]. The core principle involves in vitro transcribed (IVT) mRNA encoding target antigens being delivered to host cells, where it is translated to produce proteins that elicit robust adaptive immune responses, including both humoral and cellular immunity [32]. This "plug-and-play" platform allows researchers to substitute mRNA sequences encoding different target antigens while using the same established production process, saving time and reducing costs compared to other vaccine platforms [18]. As the field matures, applications have expanded dramatically beyond SARS-CoV-2 to include respiratory syncytial virus (RSV), oncology, and veterinary medicine, demonstrating the technology's remarkable adaptability for diverse therapeutic needs.
mRNA Vaccine Technology: Core Principles and Workflows
mRNA Design and Synthesis
The developmental workflow for mRNA vaccines begins with careful design of the antigen sequence and mRNA structural elements. Synthetic mRNA for therapeutic applications is designed to mimic mature eukaryotic mRNA structure, containing five critical sections from 5' to 3': a 5' cap, 5' untranslated region (UTR), an open reading frame encoding the antigen, 3' UTR, and a poly(A) tail [18]. Each component plays a crucial role in mRNA stability, translational efficiency, and immunogenicity.
Table 1: Essential Components of Synthetic mRNA
| Component | Function | Optimization Strategies |
|---|---|---|
| 5' Cap | Facilitates ribosomal binding, protects from exonuclease degradation, reduces immune recognition | Use of Anti-Reverse Cap Analogs (ARCAs), enzymatic 2'-O-methylation [48] [18] |
| 5' and 3' UTRs | Regulate mRNA translation, half-life, and subcellular localization | Incorporation of naturally occurring UTRs from highly expressed genes (e.g., α- and β-globin); elimination of destabilizing elements [18] |
| Open Reading Frame | Encodes the antigen of interest | Codon optimization; nucleoside modifications (e.g., pseudouridine); stabilization of antigen in prefusion conformation [18] [32] |
| Poly(A) Tail | Enhances translational efficiency and mRNA stability | Optimal length of 100-150 nucleotides; incorporation of regulatory elements to prevent plasmid instability [48] [18] |
Innovative algorithms like LinearDesign have revolutionized mRNA sequence optimization by simultaneously addressing mRNA stability and codon usage. This algorithm treats mRNA design as a lattice parsing problem in computational linguistics, efficiently navigating the vast sequence space to identify optimal designs that improve mRNA half-life and protein expression [49]. In vivo studies demonstrate that vaccines designed with this approach can increase antibody titers by up to 128-fold compared to conventional codon-optimized benchmarks [49].
Delivery Systems and Immune Activation
The delivery of mRNA into cells represents a critical technological challenge, overcome primarily by lipid nanoparticles (LNPs). LNPs typically consist of four components: an ionizable lipid, cholesterol, a helper phospholipid, and a PEGylated lipid, which together encapsulate and protect the fragile mRNA core [18]. These nanoparticles facilitate cellular uptake through endocytosis and subsequent endosomal escape, releasing mRNA into the cytoplasm for translation.
The subsequent immune response involves a carefully orchestrated series of events. Antigen-presenting cells (APCs) uptake and translate the mRNA, presenting the resulting antigens on MHC molecules to activate T cells. B cells recognizing the antigen receive T cell help, leading to their differentiation into antibody-producing plasma cells and memory B cells [50]. This process generates both neutralizing antibodies and cytotoxic T cells, providing comprehensive immune protection.
Diagram 1: mRNA Vaccine Mechanism of Action
Application Note: mRNA Vaccines for Respiratory Syncytial Virus (RSV)
Antigen Design and Preclinical Validation
Respiratory syncytial virus (RSV) represents a significant target for mRNA vaccine development, particularly for pediatric and elderly populations. A key advancement has been the stabilization of the RSV fusion (F) protein in its prefusion conformation (preF), which exposes important neutralizing epitopes that become masked in the postfusion state [51] [32]. Engineering approaches include introducing proline mutations and disulfide bonds to lock the protein in the prefusion state, dramatically improving immunogenicity [32].
Recent research has demonstrated the efficacy of bivalent mRNA vaccines targeting both RSV A and B serotypes. In a rodent model study, mRNA vaccines expressing stabilized preF proteins elicited robust antigen-specific binding antibodies, neutralizing antibodies, and Th1-biased T-cell responses [51]. The vaccine candidates significantly reduced lung viral loads and pathology upon challenge with live RSV A2 virus, with no evidence of vaccine-enhanced respiratory disease (VERD) - a critical safety consideration for RSV vaccines [51].
Table 2: Preclinical Efficacy Data for RSV mRNA Vaccines in Rodent Models
| Parameter | Results | Experimental Details |
|---|---|---|
| Neutralizing Antibody Response | Robust responses against both RSV A and B subtypes | Measured by plaque reduction neutralization test (PRNT) in serum [51] |
| Cellular Immune Response | Th1-biased T-cell responses with antigen-specific IFN-γ production | ELISpot assay performed on splenocytes; cytokine profiling [51] |
| Viral Load Reduction | Significant reduction in lung infectious viral loads post-challenge | Cotton rats challenged with live RSV A2 virus; viral titers measured by plaque assay [51] |
| Lung Pathology | Marked reduction in pulmonary inflammation and tissue damage | Histopathological examination of lung tissues post-challenge [51] |
| Safety Profile | No evidence of vaccine-enhanced respiratory disease (VERD) | Comprehensive clinical observation and histological analysis [51] |
Protocol: Evaluation of RSV mRNA Vaccine Efficacy in Rodent Models
Objective: To assess the immunogenicity and protective efficacy of bivalent RSV preF mRNA vaccines in mouse and cotton rat models.
Materials and Methods:
- mRNA Vaccine Preparation: Prepare nucleoside-modified mRNA encoding stabilized prefusion F proteins from RSV A2 and RSV B strains using T7 RNA polymerase-mediated in vitro transcription. Incorporate 5' cap structure (CleanCap) and poly(A) tail. Encapsulate mRNA in lipid nanoparticles (LNPs) composed of ionizable lipid, DSPC, cholesterol, and PEG-lipid at precise molar ratios [51].
- Animal Immunization: Use 6-8 week-old female BALB/c mice and 7-10 week-old female cotton rats. Immunize animals intramuscularly with 1-10 μg mRNA vaccine doses at 0 and 3 weeks. Include control groups receiving saline or DS-Cav1 preF protein with Adju-phos adjuvant [51].
- Serological Analysis: Collect serum samples 2-3 weeks post-second immunization. Measure RSV-specific IgG antibodies by ELISA. Perform plaque reduction neutralization tests (PRNT) against RSV A2 and RSV B strains using HEp-2 cells [51].
- Cellular Immune Response Assessment: Isolate splenocytes 3 weeks post-boost. Perform IFN-γ ELISpot assays using peptides covering RSV F protein. Stimulate cells with RSV F peptides for 48-72 hours and quantify cytokine production by ELISA [51].
- Virus Challenge and Protection: Challenge cotton rats intranasally with 10^6 PFU RSV A2 virus 4 weeks post-final immunization. Sacrifice animals 4-5 days post-challenge. Collect lung tissues for viral plaque assay and histopathological examination [51].
Application Note: mRNA Technology in Veterinary Medicine
Current Landscape and Advantages
The application of mRNA technology in veterinary medicine represents a rapidly expanding field with distinct advantages over traditional vaccine approaches. mRNA vaccines induce both antibody and T-cell responses, providing comprehensive immune protection against infectious diseases [52]. Their rapid development timeline is particularly valuable for addressing emerging veterinary pathogens, as the platform enables quick antigen discovery and vaccine formulation without the need for viral culture [52].
Current veterinary mRNA vaccine development targets multiple significant pathogens, including:
- Rabies virus
- Influenza virus
- Zoonotic mosquito-borne flaviviruses
- Coronaviruses
- Foot-and-mouth disease virus
- Porcine reproductive and respiratory syndrome virus (PRRSV) [52]
- African swine fever virus (ASFV) [32]
- Porcine epidemic diarrhea virus (PEDV) [32]
The technology also shows promise for cancer immunotherapy in animals, with investigations underway for mammary tumors in dogs [52]. Alternative delivery methods such as spray and oral administration are being explored for wildlife and livestock populations, potentially enabling mass vaccination approaches that would be impractical with traditional injectable vaccines [52].
Antigen Design Considerations for Veterinary Applications
Antigen design for veterinary mRNA vaccines follows similar principles to human vaccines but must account for species-specific factors. For coronaviruses affecting livestock, such as porcine epidemic diarrhea virus (PEDV), stabilization of the spike protein in prefusion conformation has been explored, though the specific molecular mechanisms differ from those of beta-coronaviruses like SARS-CoV-2 [32]. The PEDV spike protein contains a region called the Dϕ domain that can induce protective antibodies in pigs, suggesting it as a promising target for vaccine design [32].
Future directions include leveraging cryo-electron microscopy and artificial intelligence prediction models to elucidate conformational rearrangement mechanisms of pathogen surface proteins, providing critical foundations for rational immunogen design tailored to veterinary applications [32].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for mRNA Vaccine Development
| Reagent/Category | Function | Examples/Specifications |
|---|---|---|
| In Vitro Transcription Kit | mRNA synthesis from DNA templates | T7, T3, or SP6 RNA polymerase; ribonucleotide triphosphates; cap analogs (e.g., CleanCap) [18] |
| Nucleoside Modifications | Reduce immunogenicity, enhance translation | Pseudouridine, N1-methylpseudouridine [18] |
| Lipid Nanoparticle Components | mRNA encapsulation and delivery | Ionizable lipids, DSPC, cholesterol, PEG-lipid [18] [51] |
| Purification Systems | Remove contaminants from IVT mRNA | Oligo-dT affinity chromatography, HPLC, tangential flow filtration [51] [48] |
| Cell Lines for Immunoassays | Antigen expression and neutralization assays | HEK293 (antigen expression), HEp-2 (RSV neutralization) [51] |
| Animal Models | Preclinical efficacy and safety testing | BALB/c mice, cotton rats (for RSV) [51] |
The applications of mRNA technology extend far beyond COVID-19, encompassing diverse fields from RSV prophylaxis to veterinary medicine. The core advantages of the platform - rapid development, flexible antigen design, and ability to induce balanced immune responses - position it as a transformative technology for addressing unmet medical and veterinary needs. Continued optimization of mRNA design algorithms, delivery systems, and manufacturing processes will further enhance the efficacy, stability, and accessibility of these vaccines. As research progresses, mRNA technology holds exceptional promise for addressing emerging infectious diseases, cancer, and other challenging therapeutic areas across human and veterinary medicine.
The rapid deployment of messenger RNA (mRNA) vaccines during the COVID-19 pandemic demonstrated the transformative potential of RNA-based technologies in modern medicine [53]. While conventional mRNA platforms continue to play a crucial role, several next-generation RNA technologies have emerged to address limitations in durability, potency, manufacturing, and dosing requirements. Circular RNA (circRNA), self-amplifying RNA (saRNA), and trans-amplifying RNA (taRNA) represent three distinct evolutionary paths in the development of advanced nucleic acid therapeutics [54] [55] [56]. These platforms are positioned to overcome key challenges associated with first-generation mRNA vaccines, including the need for ultra-cold storage, relatively short-lived immune responses for some targets, and the high doses required for efficacy [57] [53].
The fundamental distinction between these platforms lies in their structural and functional mechanisms. CircRNA possesses a covalently closed continuous loop structure that confers exceptional stability and resistance to exonuclease degradation [55]. saRNA incorporates viral replication machinery that enables intracellular amplification of the encoded antigen, resulting in prolonged and enhanced protein expression [56]. taRNA represents a modular advancement of the saRNA concept, separating the replicase and antigen-encoding sequences into distinct RNA strands to improve manufacturing flexibility and efficiency [58] [59]. Together, these platforms are expanding the therapeutic landscape for infectious diseases, cancer immunotherapy, and potentially genetic disorders, offering researchers a diverse toolkit for addressing previously intractable medical challenges [60] [61].
Table 1: Core Characteristics of Next-Generation RNA Platforms
| Platform | Structural Features | Key Advantages | Primary Applications |
|---|---|---|---|
| Circular RNA (circRNA) | Covalently closed loop structure, no free ends | Exceptional stability, prolonged antigen expression, reduced storage requirements | Cancer immunotherapy, infectious disease vaccines, protein replacement therapies |
| Self-Amplifying RNA (saRNA) | Single RNA strand encoding both replicase and antigen | Dose-sparing (lower doses needed), prolonged antigen expression, potent immune responses | Infectious disease vaccines, particularly where durable immunity is required |
| Trans-Amplifying RNA (taRNA) | Two separate RNA strands: replicase + antigen | Manufacturing flexibility, component pre-production, dose-sparing, modification flexibility | Pandemic preparedness, rapid response vaccines, personalized cancer vaccines |
Circular RNA (circRNA) Platforms
Molecular Design and Mechanisms
Circular RNAs constitute a novel class of RNA molecules characterized by their covalently closed continuous loop structure, which confers remarkable stability and resistance to exonuclease degradation [55]. This structural integrity arises from the absence of free 5' and 3' ends, effectively eliminating the primary substrates for RNA-degrading enzymes. The biogenesis of circRNAs occurs naturally in eukaryotic cells through a "back-splicing" mechanism where a downstream 5' splice site joins with an upstream 3' splice site [55]. For therapeutic applications, circRNAs are engineered synthetically to incorporate essential elements including an internal ribosome entry site (IRES) that facilitates cap-independent translation, optimized open reading frames encoding the antigen of interest, and structural motifs that ensure circularization efficiency and translational fidelity [55] [61].
The translational potential of circRNA vaccines was convincingly demonstrated in recent preclinical studies focusing on cancer immunotherapy. Researchers developed minimal circRNA vectors (typically under 300 nucleotides) encoding tumor-specific antigens and observed significantly improved lymphatic trafficking and accumulation in antigen-presenting cells compared to conventional mRNA platforms [61]. These circRNA vaccines, when administered in combination with immune checkpoint blockade therapy, generated approximately ten times more antigen-specific T-cells than state-of-the-art linear mRNA vaccines while maintaining a superior safety profile [61]. The enhanced stability of circRNA enables sustained antigen expression that promotes the development of robust, long-lasting immune responses critical for both oncological applications and protective vaccination against challenging pathogens.
Experimental Protocol: circRNA Vaccine Production and Evaluation
circRNA Synthesis:
- Template Design: Construct a DNA template containing, in sequence: a 5' homology arm, reverse complementary intronic sequences flanking the antigen-encoding region, optimized IRES element, antigen open reading frame, and a 3' homology arm.
- In Vitro Transcription: Perform RNA synthesis using T7 RNA polymerase in a reaction containing modified nucleotides (e.g., N1-methylpseudourine) to reduce innate immune recognition.
- Circularization: Catalyze RNA circularization using purified group I intron-derived ribozymes or RNA ligases, followed by high-performance liquid chromatography purification to isolate closed circular molecules.
- Quality Control: Validate circRNA integrity via RNase R treatment (circRNA should be resistant) and gel electrophoresis to confirm circular conformation.
Nanoparticle Formulation:
- Prepare ionizable lipid, phospholipid, cholesterol, and PEG-lipid in ethanol at molar ratios optimized for circRNA delivery.
- Combine circRNA in aqueous buffer (pH 4.5) with the lipid mixture using microfluidic mixing at a flow rate ratio of 3:1 (aqueous:ethanol).
- Dialyze the resulting lipid nanoparticles (LNPs) against phosphate-buffered saline (pH 7.4) for 24 hours to remove ethanol and establish neutral pH.
- Filter-sterilize LNPs through 0.22μm membranes and characterize particle size (typically 70-100nm), polydispersity index (<0.2), encapsulation efficiency (>90%), and circRNA integrity.
In Vivo Efficacy Assessment:
- Immunize C57BL/6 mice (n=8 per group) subcutaneously with 5μg circRNA-LNPs at days 0 and 14.
- Collect serum samples weekly to monitor antigen-specific antibody titers via ELISA.
- Isolate splenocytes at day 28 for intracellular cytokine staining to quantify antigen-specific CD8+ and CD4+ T-cell responses.
- For tumor challenge models, inoculate mice with syngeneic cancer cells expressing the target antigen one week after booster immunization and monitor tumor growth twice weekly.
Research Reagent Solutions for circRNA Development
Table 2: Essential Reagents for circRNA Research
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Circularization Enzymes | Group I intron ribozymes, T4 RNA ligase | Catalyze backbone ligation for loop formation |
| Purification Systems | HPLC with anion-exchange columns, RNase R treatment | Isify functional circRNA from linear contaminants |
| Delivery Vehicles | Ionizable LNPs (DLin-MC3-DMA), PEG-lipids | Protect circRNA and facilitate cellular uptake |
| Quality Control Assays | RNase R resistance test, Northern blot, nanopore sequencing | Verify structural integrity and sequence accuracy |
| In Vitro Translation Systems | Rabbit reticulocyte lysate, HEK-293 cell transfection | Assess protein expression potential |
Self-Amplifying RNA (saRNA) Platforms
Platform Architecture and Immunological Advantages
Self-amplifying RNA platforms represent a significant advancement in RNA vaccine technology through the incorporation of viral replication machinery that enables intracellular amplification of the encoded antigen [56]. These vectors are derived from the genomes of positive-sense RNA viruses such as alphaviruses and flaviviruses, preserving the non-structural proteins (nsP1-4) that constitute the RNA-dependent RNA polymerase complex while replacing the structural viral genes with the antigen of interest [57] [56]. This strategic design creates a replication-competent RNA molecule capable of amplifying itself within the host cell cytoplasm, resulting in substantially higher and more prolonged antigen expression compared to conventional mRNA platforms [57].
The key advantage of saRNA technology is its exceptional dose-sparing capability, which has been demonstrated across multiple disease targets. Clinical evidence for this platform continues to mature, with recent Phase 1 trial data for RBI-4000—an saRNA rabies vaccine—showing that de novo immunogenicity could be achieved at doses as low as 0.1 micrograms while maintaining durable immune responses [57]. This represents a potential 10- to 100-fold reduction in required RNA dose compared to conventional mRNA vaccines. Importantly, the extended antigen expression profile of saRNA vaccines appears to translate to enhanced durability of immune responses. Head-to-head comparisons have demonstrated that saRNA vaccines against both SARS-CoV-2 and rabies elicit antibody responses with similar or improved durability compared to traditional vaccine technologies [57]. This attribute positions saRNA as a particularly promising platform for pathogens where long-lasting immunity is essential for effective protection.
Experimental Protocol: saRNA Vaccine Potency and Durability Assessment
saRNA Construct Design:
- Backbone Selection: Utilize alphavirus-derived sequences (e.g., Venezuelan equine encephalitis virus) containing nsP1-4 genes encoding the RNA replication machinery.
- Antigen Cloning: Subclone the antigen gene of interest (e.g., rabies glycoprotein G, SARS-CoV-2 spike) into the saRNA backbone downstream of the subgenomic promoter, replacing native structural genes.
- Sequence Optimization: Implement codon optimization and GC content adjustment for enhanced translational efficiency in human cells while preserving secondary structure elements critical for replicase recognition.
In Vitro Potency Assay:
- Seed BHK-21 cells in 24-well plates at 2×10^5 cells/well and incubate for 24 hours to reach 80% confluency.
- Transfect cells with saRNA (100ng/well) using a cationic lipid transfection reagent according to manufacturer specifications.
- Harvest cell supernatants and lysates at 6, 24, 48, 72, and 96 hours post-transfection.
- Quantify antigen expression via ELISA and assess RNA amplification kinetics using quantitative RT-PCR with primers specific for antigen-encoding sequences.
- Normalize data to conventional mRNA transfection controls to calculate fold-increase in antigen expression duration and magnitude.
Durability Assessment in Murine Models:
- Immunize BALB/c mice (n=10 per group) intramuscularly with saRNA-LNPs at doses of 0.1μg, 1μg, and 10μg, including a conventional mRNA control group (30μg).
- Collect serum samples at weeks 2, 4, 8, 12, 16, 24, and 32 post-immunization.
- Quantify antigen-specific IgG titers via ELISA and perform virus neutralization assays where applicable.
- At week 32, isolate splenocytes for memory T-cell phenotyping via flow cytometry using surface markers (CD44, CD62L) and intracellular cytokine staining following antigen recall.
Research Reagent Solutions for saRNA Development
Table 3: Essential Reagents for saRNA Research
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Viral Backbones | VEEV nsP1-4 genes, Sindbis virus replicon | Provide RNA amplification machinery |
| Cell Lines | BHK-21, Vero76 (high transferability) | Support saRNA replication and protein expression |
| Detection Assays | Antigen-specific ELISA, plaque reduction neutralization | Quantify expression potency and functional antibodies |
| Formulation Components | Ionizable lipids (SM-102), cholesterol | Protect large RNA constructs and facilitate delivery |
| Animal Models | BALB/c mice, Syrian hamsters | Evaluate immunogenicity and durability |
Trans-Amplifying RNA (taRNA) Platforms
Modular System Design and Manufacturing Advantages
Trans-amplifying RNA technology represents an innovative approach that builds upon the saRNA concept by physically separating the replicase and antigen-encoding components into two distinct RNA molecules [58] [59]. This modular architecture consists of a replicase mRNA that encodes the viral RNA-dependent RNA polymerase and a separate antigen-encoding transcript that contains the necessary recognition elements for amplification [58]. The system leverages the fundamental principle that the replicase enzyme, once translated, can act in trans to recognize and amplify the antigen-encoding RNA strand, leading to substantial intracellular amplification of the target antigen [58] [59]. This bifurcated design addresses several limitations associated with conventional saRNA platforms while preserving their dose-sparing advantages.
The taRNA system offers substantial improvements in manufacturing flexibility and efficiency. By separating the replicase and antigen components, the platform enables pre-production and stockpiling of the replicase mRNA, which can be universally employed across multiple vaccine targets [59]. When a new pathogen emerges, only the antigen-encoding component needs to be developed and validated, potentially compressing vaccine development timelines [59]. Recent preclinical studies of a taRNA vaccine encoding a consensus SARS-CoV-2 spike protein demonstrated neutralizing antibody levels comparable to conventional mRNA vaccines while using approximately 40 times less antigen-encoding mRNA [58]. This dose-sparing effect, combined with the platform's enhanced manufacturability, positions taRNA as a particularly promising technology for rapid pandemic response and personalized cancer vaccines where manufacturing agility is paramount.
Experimental Protocol: taRNA Vaccine Assembly and Potency Validation
Two-Component System Assembly:
- Replicase mRNA Production: In vitro transcribe and cap the replicase mRNA (encoding VEEV nsP1-4) using CleanCap co-transcriptional capping with complete nucleoside modification (e.g., N1-methylpseudouridine) to reduce innate immune activation.
- Antigen mRNA Production: In vitro transcribe the antigen-encoding mRNA containing the gene of interest flanked by the required replicase recognition sequences (5' and 3' UTRs from VEEV), using minimal nucleotide modifications to ensure compatibility with the replicase.
- LNP Co-formulation: Co-encapsulate replicase and antigen mRNAs at optimized ratios (typically 1:4 w/w) in LNPs using microfluidic mixing technology. Alternative approaches include separate LNP formulations mixed before administration.
In Vitro Validation of Replication Efficiency:
- Seed HEK-293T cells in 12-well plates and transfect with either (a) antigen mRNA alone (250ng), (b) replicase mRNA alone (250ng), or (c) both mRNAs (250ng each) using lipofectamine 3000.
- Harvest cell lysates at 6, 12, 24, 48, and 72 hours post-transfection.
- Quantify antigen expression via Western blot and/or ELISA, normalizing to total protein concentration.
- Extract total RNA and perform quantitative RT-PCR to measure antigen mRNA amplification using primers specific for the antigen-encoding sequence.
- Calculate fold-increase in both antigen protein and mRNA levels in the taRNA system compared to antigen mRNA alone.
In Vivo Dose-Sparing Evaluation:
- Immunize hACE2 transgenic mice (n=8 per group) with taRNA formulations containing decreasing amounts of antigen mRNA (0.1μg, 0.5μg, 1μg) while maintaining constant replicase mRNA (1μg).
- Include control groups receiving conventional mRNA vaccine (10μg) and saRNA vaccine (1μg).
- Collect serum at weeks 2, 4, and 8 post-immunization for neutralizing antibody assessment via PRNT assay.
- Challenge mice with live virus (e.g., SARS-CoV-2 Omicron BA.1 variant) at week 10 and monitor viral load in lungs 3 days post-infection via qRT-PCR.
- Assess T-cell responses in splenocytes via ELISpot for interferon-γ production following stimulation with antigen-specific peptides.
Research Reagent Solutions for taRNA Development
Table 4: Essential Reagents for taRNA Research
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Modular RNA Systems | VEEV split systems, SINV replicase | Provide validated two-component platforms |
| Co-formulation Systems | Microfluidic mixers, charge-based encapsulation | Enable efficient packaging of multiple RNA strands |
| Amplification Detectors | Stem-loop qPCR primers, Northern blot assays | Quantify RNA amplification in trans |
| Cell-free Expression | Rabbit reticulocyte lysate, HEK-293 extracts | Test component compatibility and function |
| Animal Disease Models | hACE2 transgenic mice, ferret models | Evaluate protection against pathogen challenge |
Comparative Analysis and Future Perspectives
Technical and Commercial Positioning
The three next-generation RNA platforms present distinct technical profiles that position them for different therapeutic applications and commercialization pathways. CircRNA technology offers exceptional stability and prolonged antigen expression, making it particularly suitable for cancer immunotherapy and situations where cold-chain independence is critical [55] [61]. saRNA platforms excel in their dose-sparing capabilities and ability to generate durable immune responses, positioning them as ideal candidates for prophylactic vaccines against infectious diseases where long-lasting immunity is essential [57] [56]. taRNA systems combine the dose-sparing advantages of saRNA with enhanced manufacturing flexibility, creating a platform particularly well-suited for rapid pandemic response and personalized cancer vaccines where manufacturing agility is paramount [58] [59].
Table 5: Quantitative Comparison of Next-Generation RNA Platforms
| Performance Metric | circRNA | saRNA | taRNA |
|---|---|---|---|
| Dose Requirement | Comparable to mRNA | 10-100x lower than mRNA | 40-100x lower than mRNA |
| Antigen Expression Kinetics | Prolonged (>7 days) | Extended (>14 days) | Extended (>14 days) |
| Manufacturing Complexity | Moderate (challenging circularization) | High (large construct size) | Moderate (two-component system) |
| Stability at 4°C | High (weeks to months) | Moderate (weeks) | Moderate (weeks) |
| Clinical Stage | Preclinical | Phase 3 (rabies, COVID-19) | Preclinical |
| Therapeutic Index | High (efficacy vs. reactogenicity) | Moderate | Moderate to High |
From a commercial perspective, each platform addresses different segments of the pharmaceutical market. circRNA vaccines, with their superior stability profile, may eventually offer significant advantages in global distribution, particularly in resource-limited settings where ultra-cold storage infrastructure is unavailable [55] [61]. saRNA vaccines, with their demonstrated durability in clinical trials, present opportunities for vaccines requiring less frequent boosting [57]. The modular nature of taRNA technology makes it particularly attractive for both pandemic preparedness—where the replicase component can be stockpiled in advance—and personalized cancer vaccines, where rapid manufacturing turnaround is essential [59]. As these platforms mature, they are likely to coexist rather than compete directly, with each occupying specific therapeutic niches based on their unique technical and manufacturing characteristics.
Emerging Applications and Future Directions
The application landscape for next-generation RNA platforms continues to expand beyond infectious disease vaccines. In oncology, circRNA vaccines have demonstrated remarkable potential, generating ten times more antigen-specific T-cells compared to state-of-the-art linear mRNA vaccines in preclinical models [61]. The exceptional stability of circRNA enables sustained presentation of tumor neoantigens, critical for breaking immune tolerance against self-antigens. Similarly, saRNA and taRNA platforms are being explored for cancer immunotherapy, leveraging their prolonged antigen expression to maintain persistent immune activation against tumor cells [60]. Clinical trials investigating RNA vaccines for pancreatic cancer and melanoma have shown promising results, with vaccine-induced immune responses persisting for nearly four years in some pancreatic cancer patients [60].
Future development of these platforms will focus on addressing remaining challenges, particularly in delivery optimization and manufacturing scalability. Next-generation lipid nanoparticles with tissue-specific targeting ligands are already showing improved delivery efficiency to lymphoid tissues and reduced off-target effects [54] [60]. Manufacturing innovations continue to reduce production timelines for personalized cancer vaccines from nine weeks to under four weeks, though costs remain challenging at over $100,000 per patient for fully personalized approaches [60]. The integration of artificial intelligence is revolutionizing neoantigen selection through advanced algorithms, while CRISPR-enhanced platforms enable real-time optimization of RNA constructs [60]. As these technologies mature, the first commercial RNA cancer vaccines are anticipated by 2029, potentially establishing a new paradigm in personalized oncology [60].
Addressing Stability, Efficacy, and Safety Challenges in mRNA Vaccine Development
Overcoming Immunogenicity and Reactogenicity Hurdles
The success of mRNA vaccine technology, as demonstrated during the COVID-19 pandemic, represents a transformative advance in vaccinology. However, a significant challenge persists in balancing effective immunogenicity—the ability to provoke a protective immune response—against reactogenicity—the tendency to cause adverse reactions such as fatigue, fever, and injection site pain [26] [62]. These undesirable side effects at protective dose levels can impact vaccine tolerability and acceptance [62]. This document outlines detailed application notes and experimental protocols for researchers aiming to overcome these hurdles through innovative platform optimization, focusing on lipid nanoparticle (LNP) engineering and innate immune modulation.
The following tables consolidate key quantitative findings from recent research on modulating mRNA vaccine properties.
Table 1: Impact of RNAx on Gene of Interest (GOI) Expression and Cytokine Response
| Experimental Model | Condition | GOI Expression Fold-Change | Cytokines Suppressed (Count) | Key Findings |
|---|---|---|---|---|
| BJ Fibroblast Cell Line | saRNA + RNAx (in cis) | 8 to 62-fold increase [62] | Not Specified | Enhancement varies by reporter construct (HA-nLuc, sec-nLuc, fLuc) [62] |
| BJ Fibroblast Cell Line | saRNA + RNAx (in trans) | Up to 11-fold increase [62] | Not Specified | Dose-dependent enhancement of sec-nLuc expression [62] |
| C57BL/6 Mice (in vivo) | saRNA-LNP + RNAx (in trans) | 170-fold increase (Day 1) [62] | Not Specified | RNAx in trans significantly enhanced nLuc expression vs. saRNA alone [62] |
| Human PBMCs | saRNA-LNP + RNAx (in trans) | Not Measured | 14 out of 15 [62] | RNAx in trans potently suppressed saRNA-induced proinflammatory cytokines (e.g., IFN-α, IFN-γ, IP-10) [62] |
Table 2: Impact of LNP Component Modification on Vaccine Profile
| LNP Component | Modification | Effect on Immunogenicity | Effect on Reactogenicity |
|---|---|---|---|
| PEG-lipid | Reduced PEG chain length and molar ratio | Increased antigen-specific antibody and CD8+ T cell responses [63] | Data not specified in source |
| Cholesterol | Substitution with plant sterols (e.g., stigmasterol) | Induced antibody and CD8+ T cell responses comparable to control [63] | Significantly reduced inflammatory cytokine production and adverse reactions (e.g., fever) [63] |
| Phospholipids | Replaced with phospholipids of different head/tail groups | Induced antibody and CD8+ T cell responses comparable to control [63] | Significantly reduced inflammatory cytokine production and adverse reactions [63] |
Experimental Protocols
Protocol: Evaluating the RNAx Platform with saRNA Vaccines
This protocol describes a method to assess the co-delivery of an mRNA encoding the Cardiovirus leader protein (RNAx) as a means to reduce reactogenicity while preserving the immunogenicity of self-amplifying RNA (saRNA) vaccines [62].
3.1.1. Background and Principle The replication of saRNA generates double-stranded RNA (dsRNA) intermediates, which are potent inducers of innate immunity (e.g., type I interferons). While this provides adjuvant effects, overactivation can lead to high reactogenicity and may also suppress antigen expression and adaptive immune responses [62]. The RNAx platform encodes a protein that modulates nucleocytoplasmic transport (NCT), broadly dampening excessive innate immune signaling and rescuing protein translation, thereby improving the vaccine's therapeutic window [62].
3.1.2. Materials
- saRNA-LNP Formulation: saRNA encoding the antigen of interest (e.g., Influenza hemagglutinin-nanoLuciferase fusion) encapsulated in lipid nanoparticles [62].
- RNAx Construct: A discrete, nucleoside-modified mRNA encoding the optimized Cardiovirus leader protein [62].
- Cells: BJ human diploid fibroblast cells, 293T cells, and primary human Peripheral Blood Mononuclear Cells (PBMCs) [62].
- Animals: C57BL/6 mice (6-8 weeks old) [62].
- Key Reagents: Cell culture media, transfection reagent, luciferase assay kit, multiplex cytokine assay (e.g., for IFN-α, IFN-γ, IP-10), ELISA kits for antigen-specific antibodies, and reagents for T-cell analysis (e.g., intracellular cytokine staining) [62].
3.1.3. Procedure
Part A: In Vitro Transfection and Analysis
- Cell Seeding: Seed appropriate cell types (BJ, 293T, PBMCs) in multi-well plates.
- Transfection Complex Formation:
- Experimental Group: Co-transfect cells with a constant amount of saRNA-LNP (e.g., 100 ng) and increasing doses of RNAx (in trans). A typical mass ratio to test is 36% RNAx (w/w of saRNA) [62].
- Control Groups: Include wells transfected with saRNA-LNP alone and mock-transfected wells.
- Incubation: Incubate cells for 24-48 hours under standard conditions.
- Harvest and Analysis:
Part B: In Vivo Immunization and Evaluation
- Formulation Preparation: Prepare LNP formulations containing saRNA alone or saRNA co-encapsulated/comixed with RNAx (e.g., at 10-50% w/w ratio) [62].
- Animal Immunization:
- Randomly group mice (n=5-10 per group).
- Administer formulations via intramuscular injection (e.g., 2 µg total RNA per mouse) [62].
- Prime and boost at a 3-4 week interval.
- Longitudinal Monitoring:
- Reactogenicity: Post-injection, monitor mice for systemic reactogenicity biomarkers (e.g., serum levels of inflammatory cytokines). Non-invasive in vivo bioluminescence imaging can be performed at days 1, 6, and 13 to track antigen expression kinetics [62].
- Terminal Immunogenicity Assessment:
- Humoral Immunity: Collect serum pre- and post-immunization. Measure antigen-specific IgG antibody titers using ELISA. Perform virus neutralization assays if applicable.
- Cellular Immunity: Isolate splenocytes. Stimulate with antigen-derived peptides and measure antigen-specific T-cell responses via intracellular cytokine staining (e.g., for IFNγ) or ELISpot [62].
3.1.4. Data Analysis
- Compare GOI expression and cytokine levels between experimental and control groups in vitro using paired t-tests.
- For in vivo data, compare antibody titers, T-cell responses, and cytokine levels between groups using appropriate statistical tests (e.g., Kruskal-Wallis with Dunn's multiple comparisons). A successful outcome is characterized by significantly suppressed inflammatory cytokines and maintained or enhanced antibody and T-cell responses in the RNAx group [62].
Protocol: Systematic Optimization of LNP Components
This protocol provides a methodology for screening and optimizing the non-ionizable lipid components of mRNA-LNPs to modulate immunogenicity and reactogenicity [63].
3.2.1. Background and Principle While ionizable lipids are often the focus of LNP development, other structural lipids (PEG-lipids, cholesterol, phospholipids) significantly impact protein expression, immune activation, and adverse reactions. Targeted modification of these components presents a viable strategy to decouple strong immunogenicity from high reactogenicity [63].
3.2.2. Materials
- mRNA: Nucleoside-modified mRNA encoding a target antigen.
- Lipids: A library of ionizable lipids, PEG-lipids with varying chain lengths (e.g., DMG-PEG, DSG-PEG), cholesterol, and plant sterols (e.g., stigmasterol, sitosterol), and diverse phospholipids (e.g., DSPC, DOPE, DPPC) [63].
- Microfluidic Device: For reproducible LNP formulation.
- Animals: Appropriate murine models.
- Key Reagents: Equipment for Dynamic Light Scattering (DLS) for particle characterization, ELISA kits, flow cytometry reagents, and cytokine assay kits.
3.2.3. Procedure
- LNP Library Formulation:
- Use a standard microfluidic mixing technique to prepare a series of mRNA-LNPs.
- Keep the ionizable lipid and mRNA constant. Systematically vary the structure or molar ratio of one component at a time (PEG-lipid, cholesterol/sterol, phospholipid) [63].
- Purify formulated LNPs via dialysis or tangential flow filtration.
- LNP Characterization:
- Measure the particle size, polydispersity index (PDI), and zeta potential of each LNP formulation using DLS.
- Determine mRNA encapsulation efficiency using a dye-binding assay (e.g., RiboGreen).
- In Vivo Screening:
- Immunize groups of mice with each LNP formulation from the library via intramuscular injection.
- Monitor and record local and systemic adverse reactions.
- Collect serum post-injection to quantify inflammatory cytokines (e.g., IL-6, TNF-α) as reactogenicity markers.
- At a predetermined timepoint (e.g., Day 7 or 21), collect serum to assess antigen-specific antibody titers by ELISA. Analyze T-cell responses from splenocytes to assess immunogenicity [63].
3.2.4. Data Analysis
- Perform correlation analysis between LNP physicochemical properties, in vivo protein expression, immunogenicity (antibody/CD8+ T-cell levels), and reactogenicity (cytokine levels, adverse events) [63].
- Identify lead formulations that demonstrate a favorable profile: high immunogenicity with low reactogenicity.
Signaling Pathways and Workflows
Mechanism of RNAx-mediated Innate Immune Modulation
The following diagram illustrates how the RNAx platform balances innate immune signaling to improve the saRNA vaccine profile.
LNP Optimization Workflow for Enhanced Vaccine Profile
This workflow outlines the systematic process for optimizing LNP components to improve mRNA vaccine properties.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for mRNA Vaccine Optimization Research
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| RNAx Construct | mRNA encoding the Cardiovirus leader protein; co-delivered to dampen innate immune signaling and reduce reactogenicity. | A discrete, nucleoside-modified mRNA. Optimal effects observed when delivered in trans at 36% w/w ratio to saRNA [62]. |
| Self-Amplifying RNA (saRNA) | Vaccine platform enabling longer-lasting antigen expression at lower doses, enhancing immunogenicity. | Often based on viral vectors like Venezuelan Equine Encephalitis Virus (VEEV). Requires careful modulation to control dsRNA-induced reactogenicity [62]. |
| Ionizable Lipids | Key component of LNPs for encapsulating and delivering mRNA; crucial for endosomal escape and efficiency. | ALC-0315 (Comirnaty), SM-102 (Spikevax). Often held constant while optimizing other LNP components [63]. |
| PEG-lipids | Stabilize LNP formation and control particle size. Modifying structure/ratio can enhance immunogenicity. | DMG-PEG2000, DSG-PEG2000. Reducing PEG chain length and molar ratio can increase antibody and CD8+ T cell responses [63]. |
| Sterols | Regulate LNP membrane fluidity and integrity. Substitution can lower reactogenicity. | Cholesterol or plant sterols (e.g., Stigmasterol). Plant sterol substitution can reduce inflammatory cytokines and fever [63]. |
| Phospholipids | Provide structural support to the LNP bilayer. Structural changes can mitigate adverse reactions. | DSPC, DOPE, DPPC. Replacing standard phospholipids can maintain immunogenicity while reducing reactogenicity [63]. |
| Pattern Recognition Receptor (PRR) Assays | In vitro tools to quantify innate immune activation by RNA sensors, guiding design of less reactogenic constructs. | Assays for TLR3, TLR7/8, RIG-I, MDA5. Used to validate that design changes (e.g., nucleoside modifications) reduce PRR activation [26]. |
Enhancing Thermostability and Cold-Chain Logistics
The efficacy of messenger RNA (mRNA) vaccines is critically dependent on maintaining the integrity of the labile mRNA molecule from production to administration. The unprecedented success of mRNA vaccines during the COVID-19 pandemic highlighted their transformative potential but also exposed a key limitation: their dependency on stringent cold-chain logistics for stability [64]. Conventional mRNA vaccines require ultra-cold storage, typically between -80°C and -60°C, posing significant financial and operational challenges for global distribution, particularly in low- and middle-income countries (LMICs) with limited cold-chain infrastructure [65] [66]. Enhancing the thermostability of mRNA vaccines is therefore not merely a technical goal but a public health imperative to enable equitable global access and improve preparedness for future pandemics.
This application note details the latest scientific advances and provides standardized protocols for the development and evaluation of thermostable mRNA vaccine platforms. Framed within the broader context of mRNA vaccine design and development, the content is structured to provide researchers, scientists, and drug development professionals with practical tools to overcome stability bottlenecks.
Current Landscape and Stability Challenges
The instability of mRNA vaccines stems primarily from the inherent susceptibility of the RNA molecule to degradation by hydrolysis and nucleases. This chemical instability necessitates encapsulation in lipid nanoparticles (LNPs) and storage at ultra-low temperatures, which complicates last-mile delivery [66]. Temperature excursions outside the specified range can lead to irreversible damage, including mRNA degradation and a reduction in the vaccine's potency and immunogenicity [67] [68]. Studies estimate that up to 35% of vaccines can be compromised by temperature mishandling, resulting in significant financial waste and public health risks [68].
Table 1: Stability Profiles of Different COVID-19 mRNA Vaccine Formats
| Vaccine Platform | Long-Term Storage | Thawed/Ready-to-Use Stability | Key Stability Characteristics & Challenges |
|---|---|---|---|
| Comirnaty (nucleoside-modified) | -90°C to -60°C (18 months) [66] | 1 month at 2°C to 8°C (unopened); 6 hours at 2°C to 30°C (after dilution) [66] | Different LNP composition and molar lipid ratios than Spikevax; stability is deeply related to temperature [66]. |
| Spikevax (nucleoside-modified) | -50°C to -15°C (9 months) [66] | 30 days at 2°C to 8°C (unopened); 19 hours at 2°C to 25°C (after puncture) [66] | Characterized by very different particle size profiles and behaviors against handling/stress vs. Comirnaty [66]. |
| ARCoV (experimental) | Room temperature for at least 1 week [69] | N/S (Liquid formulation) | Thermostable LNP-encapsulated mRNA vaccine encoding the RBD of SARS-CoV-2; demonstrated protection in animal models [69]. |
| Circular RNA (experimental) | 4 weeks at 4°C [10] | N/S | Unmodified Circ-RNA vaccine is more stable at 4°C than a self-amplifying RNA (SAM) vaccine; induced a higher memory T cell response [10]. |
Key Strategies for Enhancing Thermostability
Improving the thermostability of mRNA vaccines requires a multi-faceted approach, integrating innovations in mRNA sequence design, delivery vehicle engineering, and formulation.
Optimized mRNA Sequence Design
The stability and translational efficiency of mRNA are heavily influenced by its primary and secondary structures. The LinearDesign algorithm represents a breakthrough in this domain. It formulates mRNA design as a lattice parsing problem in computational linguistics, efficiently searching the vast sequence space to find an mRNA sequence that simultaneously optimizes both thermodynamic stability (via minimum free energy) and codon usage (via the Codon Adaptation Index) [49]. This principled design has been shown to substantially improve mRNA half-life, protein expression, and increase antibody titers by up to 128 times in mice compared to conventional codon-optimization benchmarks [49].
Advanced Vaccine Platforms and Delivery Systems
Novel platforms that circumvent the instability of linear mRNA are under active investigation. Circular RNA (Circ-RNA) vaccines have demonstrated superior stability, maintaining integrity for at least 4 weeks at 4°C while eliciting robust neutralizing antibodies and T-cell responses [10]. Similarly, innovative delivery vehicles like the ACM Tunable Platform (ATP) are being engineered specifically for thermostability, allowing for mRNA storage at standard refrigerator temperatures of 2°C to 8°C, thereby removing the need for frozen storage [70].
Improved Lipid Nanoparticle (LNP) Formulations
The composition of LNPs is a critical determinant of stability. Research indicates that Comirnaty and Spikevax, despite using the same mRNA-LNP technology, have different thermal stability profiles, which is likely attributable to differences in their LNP components and molar lipid ratios [66]. Optimizing the ionizable lipid, phospholipid, cholesterol, and PEG-lipid components can improve the robustness of the LNP, enhancing its resistance to temperature-induced aggregation and degradation.
Experimental Protocols for Stability Assessment
Rigorous in-use stability testing is essential for characterizing novel vaccine candidates. The following protocol, adapted from published research, provides a methodology for analyzing the physical stability of mRNA-LNP vaccines [66].
Protocol 1: In-Use Stability Testing of mRNA-LNP Vaccines by Dynamic Light Scattering (DLS) and Transmission Electron Microscopy (TEM)
1.0 Principle This protocol assesses the stability of mRNA-LNP formulations by subjecting them to stress conditions that mimic handling and evaluates critical quality attributes like particle size and morphology. Changes in LNP size are indicative of aggregation and potential loss of potency [66].
2.0 Materials and Equipment
- mRNA-LNP vaccine samples (e.g., Comirnaty, Spikevax, or novel candidates)
- Medical-grade sodium chloride injection (0.9%)
- Sterile syringes and needles (e.g., BD Microlance 18G, 1 mL BD Plastipak syringes)
- Amber glass vials (2 mL, to protect from light)
- Clear glass vials (2 mL, for light exposure studies)
- Dynamic Light Scattering (DLS) instrument
- Transmission Electron Microscope (TEM)
- Vortex mixer
- Temperature-controlled incubator or water bath
3.0 Methodology
3.1 Sample Preparation
- Comirnaty: Dilute the 0.45 mL concentrate with 1.8 mL of 0.9% sodium chloride solution to achieve a total volume of 2.25 mL, as per the SmPC [66].
- Spikevax: Use the ready-to-administer dispersion directly from the multidose vial; no dilution is required [66].
3.2 Stress Testing Conditions
- Thermal Stress: Expose samples to room temperature (e.g., ~25°C) for defined periods (e.g., 2, 6, 24 hours).
- Light Stress:
- Natural Light: Expose samples in clear vials to ambient laboratory light.
- Accelerated Light: Use a photostability chamber with controlled light irradiation.
- Mechanical Stress:
- Vortexing: Subject samples to vortex vibration for 1-5 minutes.
- Manual Shaking: Agitate samples vigorously by hand for a set duration.
- Simulated Use: Pass samples through syringes via multiple injection cycles (e.g., 10 cycles).
- Long-Term Storage Simulation: Store diluted samples in syringes at 2-8°C or room temperature for up to 24 hours.
3.3 Analysis
- Dynamic Light Scattering (DLS): Qualitatively analyze the particle size distribution of control and stressed samples. A significant increase in mean particle size or polydispersity indicates physical instability and aggregation [66].
- Transmission Electron Microscopy (TEM): To support DLS findings, analyze the morphology of the LNPs. Visual confirmation of particle fusion or irregular shapes provides further evidence of degradation [66].
4.0 Interpretation Compare the size profiles and morphology of stressed samples against the unstressed control. A stable formulation will show minimal changes in size distribution and maintain a uniform, spherical morphology under TEM after stress testing.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Thermostability Studies
| Item | Function / Application in Research |
|---|---|
| In Vitro Transcription (IVT) Kit | Produces mRNA transcripts with high yield for initial vaccine construction and testing [64]. |
| CleanCap AG Reagent | Enables co-transcriptional capping during mRNA synthesis, resulting in a high proportion of the Cap 1 structure, which is critical for enhanced stability and translational efficiency [64]. |
| Lipid Nanoparticle (LNP) Components | Ionizable lipid, phospholipid, cholesterol, and PEG-lipid for formulating and optimizing the delivery vehicle that protects the mRNA [64] [70]. |
| Phase-change Materials | Used in portable vaccine carriers for passive temperature maintenance during transport in resource-limited settings [67] [65]. |
| Digital Data Loggers | Provide real-time temperature monitoring and documentation throughout the storage and transport process, critical for identifying temperature excursions [67] [68]. |
| Medical-Grade Refrigerators/Freezers | Ensure precise and uniform temperature control (e.g., +2°C to +8°C, -25°C to -15°C, -90°C to -60°C) for vaccine storage, as domestic units are unsuitable [67] [68]. |
Workflow and Strategic Framework
The following diagram illustrates the logical relationship and workflow between the key strategies for developing thermostable mRNA vaccines, from initial design to final evaluation.
Diagram 1: Strategic Workflow for Enhancing mRNA Vaccine Thermostability. This diagram outlines the multi-pronged approach and evaluation pipeline for developing thermostable mRNA vaccines, from addressing core challenges to final candidate selection.
Tissue-Specific Targeting and LNP Surface Functionalization
Lipid nanoparticles (LNPs) have emerged as the foremost non-viral delivery platform for RNA therapeutics, demonstrating remarkable success in vaccine applications and genetic medicine [71] [72]. Conventional LNPs predominantly accumulate in the liver following systemic administration, limiting their application for therapies targeting other tissues [73] [74]. Tissue-specific targeting through surface functionalization represents a pivotal strategy to overcome this limitation, enhancing therapeutic efficacy while minimizing off-target effects and systemic toxicity. These engineering approaches modify LNP surfaces with various targeting ligands that direct encapsulated nucleic acids to specific cell types or organs, enabling precise therapeutic interventions beyond hepatic applications [73].
The fundamental structure of LNPs comprises four key lipid components: ionizable lipids, helper phospholipids, cholesterol, and PEGylated lipids [71] [74]. Ionizable lipids are crucial for mRNA encapsulation and endosomal escape, while PEG-lipids enhance particle stability and prevent aggregation [73]. Surface engineering leverages this modular architecture by incorporating targeting ligands without compromising core LNP functions. Recent advances have demonstrated that strategic modifications to LNP surfaces can dramatically alter biodistribution patterns and cellular tropism, opening new possibilities for treating genetic disorders, cancers, and infectious diseases with unprecedented precision [75] [76].
Core Principles of LNP Surface Engineering
Surface Engineering Strategies and Ligand Incorporation
The surface functionalization of LNPs employs three primary strategies: substitution of conventional PEG-lipids with functionalized alternatives, alteration of surface charge, and modification with targeting ligands [73]. These approaches can be achieved through direct incorporation of pre-synthesized ligand-lipid conjugates or post-formulation conjugation techniques. The selection of appropriate ligands depends on the target cell type, receptor expression patterns, and intended therapeutic application.
Table 1: Major Surface Engineering Strategies for LNPs
| Strategy | Mechanism | Common Ligands | Applications |
|---|---|---|---|
| PEG-lipid Substitution | Replacing conventional PEG-lipids with functionally modified variants | Amine-, carboxyl-, or carboxy-ester-modified PEG-lipids [76] | Altering cellular tropism, enhancing tissue penetration |
| Charge Modification | Adjusting surface potential through cationic or anionic lipids | Ionizable lipids with tertiary amines, carboxylic acid groups [76] | Improving cellular uptake, altering protein corona formation |
| Ligand Conjugation | Attaching targeting moieties to LNP surface | Antibodies, peptides, aptamers, small molecules (e.g., GalNAc) [73] [75] | Cell-specific targeting, receptor-mediated uptake |
The "in-lipid mixing" method represents the most straightforward approach for incorporating targeting ligands, where pre-synthesized ligand-lipid conjugates are directly included in the lipid mixture during LNP formulation [73]. This method bypasses additional conjugation steps and purification requirements, simplifying the formulation process. Alternatively, post-insertion techniques allow ligands to be incorporated after LNP formation, preserving their functional integrity, particularly for sensitive biological ligands like antibodies and proteins [75].
Ligand Types and Their Applications
Various ligand classes have been successfully employed for LNP targeting, each offering distinct advantages for specific applications:
Antibodies and Antibody Fragments: Provide high specificity and affinity for cell surface receptors. Recent innovations include nanobody-based capture systems that orient antibodies optimally on LNP surfaces [75]. For instance, the TP1107 nanobody system captures antibodies via their Fc domain, ensuring proper orientation and enhancing binding efficiency by eightfold compared to conventional methods [75].
Peptide Ligands: Short peptide sequences targeting specific receptors offer advantages in stability and manufacturing. Peptides targeting immune cells, such as T cells, have been utilized for cancer immunotherapy applications [73].
Small Molecules: Low molecular weight compounds like GalNAc (N-acetylgalactosamine) enable efficient hepatocyte targeting through the asialoglycoprotein receptor (ASGPR) [73] [74]. This approach has proven highly successful for siRNA delivery to the liver.
Carbohydrate Ligands: Sugar moieties such as mannose target antigen-presenting cells through lectin receptors, making them valuable for vaccine development [73].
Advanced Functionalization Protocols
Nanobody-Mediated Antibody Capture System
A breakthrough in antibody-directed targeting involves a versatile capture system that immobilizes antibodies on LNP surfaces without chemical modification [75]. This protocol details the methodology for implementing this innovative approach.
Experimental Protocol: Nanobody-Mediated Antibody Functionalization
Materials Required:
- TP1107 nanobody with site-specific azido-phenylalanine incorporation [75]
- DBCO-PEG2000-DSPE lipid conjugate
- LNP formulation (standard composition: ionizable lipid, DSPC, cholesterol, PEG-lipid)
- Target antibody (e.g., anti-CD5 for T cells, anti-CD117 for hematopoietic stem cells)
- Dialysis equipment or tangential flow filtration system
Procedure:
- Nanobody-Lipid Conjugation:
LNP Formulation:
- Prepare LNPs using standard microfluidic mixing with composition: ionizable lipid (50%), cholesterol (38.5%), DSPC (10%), and PEG-lipid (1.5%) [75].
- Characterize initial LNP size (typically 80-90 nm) and polydispersity index (<0.2) using dynamic light scattering.
Nanobody Incorporation:
Antibody Capture:
- Add target antibody to nanobody-functionalized LNPs at appropriate concentration (typically 10-50 μg/mL).
- Incubate for 30 minutes at room temperature without purification [75].
Quality Control:
- Assess final particle size and distribution.
- Evaluate targeting efficiency using cell-binding assays.
- Measure mRNA encapsulation efficiency (>90% expected).
This methodology enables highly specific targeting, demonstrated by T cell transfection efficiencies more than 1,000 times higher than non-targeted LNPs and eightfold improvements over conventional antibody conjugation techniques [75].
PEG-Variant Surface Modification for Altered Tropism
Surface charge modification through functionalized PEG-lipids represents a powerful strategy to redirect LNP biodistribution without complex ligand conjugation [76]. This protocol describes the formulation of LNP variants with distinct surface charges and their application in retinal gene delivery.
Experimental Protocol: PEG-Variant LNP Formulation
Materials Required:
- Ionizable lipid (e.g., DLin-MC3-DMA or SM102)
- Helper lipids (DSPC, DOPE)
- Cholesterol
- Conventional PEG-lipid (DMG-PEG2000)
- Functionalized PEG-lipids: DSPE-PEG2000-Amine, DSPE-PEG2000-Carboxy-NHS, DSPE-PEG2000-Carboxylic acid
- Microfluidic mixer (e.g., NanoAssemblr)
- mRNA (e.g., Cre recombinase, Cas9)
Procedure:
- Lipid Solution Preparation:
- Prepare ethanolic lipid mixture with standard molar ratios: ionizable lipid (50%), cholesterol (38.5%), DSPC (10%), total PEG-lipids (1.5%) [76].
- For functionalized variants: reduce DMG-PEG2000 to 1.2% and include 0.3% of functionalized PEG-lipid [76].
- LNPa: contains DSPE-PEG2000-Amine
- LNPx: contains DSPE-PEG2000-Carboxy-NHS
- LNPz: contains DSPE-PEG2000-Carboxylic acid
LNP Formulation:
- Utilize microfluidic mixing with aqueous phase (mRNA in citrate buffer, pH 4.0) to ethanol phase ratio 3:1.
- Maintain total flow rate of 12 mL/min [76].
Buffer Exchange and Characterization:
Functional Validation:
- Evaluate cellular uptake in target cells (e.g., 661w photoreceptor cells).
- Assess endosomal escape using Galectin 8-GFP reporter system [76].
- Validate protein expression in target tissues (e.g., retinal photoreceptors for LNPx and LNPz).
This approach demonstrates that surface charge modifications alone can dramatically alter cellular tropism, with negatively charged LNPx and LNPz variants transfecting photoreceptors (27% and 16% respectively) while conventional LNPs primarily target retinal pigmented epithelium [76].
Quantitative Analysis of Targeting Efficiency
Table 2: Performance Metrics of Advanced Targeting Strategies
| Targeting Strategy | Target Cell/Tissue | Transfection Efficiency | Specificity Enhancement | Key Applications |
|---|---|---|---|---|
| Nanobody-Antibody Capture [75] | T cells | >1,000x vs non-targeted LNPs | 8x vs conventional antibody conjugation | Cancer immunotherapy, autoimmune diseases |
| GalNAc conjugation [73] [74] | Hepatocytes | >50% protein expression | >90% hepatic delivery | siRNA therapeutics, metabolic diseases |
| PEG-variant (LNPx) [76] | Photoreceptors | 27% transfection rate | Pan-retinal distribution | Retinal gene editing, inherited retinal diseases |
| Peptide-modified LNPs [73] | Immune cells | 4-26x vs serum-starved methods | Cell-specific expression | Vaccines, immune oncology |
| Charge-modified LNPs [76] | Various cell types | Varies by surface potential | Altered biodistribution | Tissue-specific delivery beyond liver |
The quantitative data demonstrate substantial improvements in targeting efficiency achieved through advanced surface functionalization strategies. The nanobody-mediated antibody capture system stands out with remarkable specificity enhancements, making it particularly valuable for applications requiring precise cell-type targeting, such as engineered immune cell therapies [75]. Similarly, chemical modifications like GalNAc conjugation achieve exceptional hepatic specificity, which has proven instrumental in developing RNAi therapeutics for liver diseases [73] [74].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for LNP Surface Functionalization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Ionizable Lipids | SM-102, DLin-MC3-DMA [77] [75] | mRNA encapsulation, endosomal escape | Critical for formulation efficacy; structure affects tropism |
| PEG-Lipids | DMG-PEG2000, DSPE-PEG2000 [73] [76] | Particle stability, circulation time | Chain length affects dissociation rate; can be functionalized |
| Targeting Ligands | GalNAc, mannose, A5G33 peptide [73] | Cell-specific binding | Direct biodistribution; receptor density impacts efficiency |
| Antibody Capture | TP1107 nanobody [75] | Optimal antibody orientation | Enhances binding affinity 8x vs conventional methods |
| Functionalized PEG | DSPE-PEG-Amine, DSPE-PEG-Carboxyl [76] | Surface charge modulation | Alters cellular tropism without additional ligands |
| Characterization Tools | Capillary western, NTA, TEM [75] | Quality assessment | Essential for verifying surface modification success |
Schematic Workflows for LNP Functionalization
Nanobody-Mediated Antibody Capture Workflow
Diagram Title: Nanobody-Mediated Antibody Capture Workflow
PEG-Variant LNP Formulation Process
Diagram Title: PEG-Variant LNP Formulation Process
Surface functionalization strategies have transformed LNPs from broadly distributed delivery vehicles into precision tools for RNA therapeutics. The protocols and data presented herein demonstrate that both ligand-based targeting and surface charge modifications can dramatically enhance tissue specificity and therapeutic efficacy. As the field advances, key challenges remain in optimizing ligand density, ensuring manufacturing reproducibility, and validating targeting efficiency in clinical settings.
Future developments will likely focus on combinatorial approaches that integrate multiple targeting strategies, develop novel ligand-receptor systems for currently inaccessible tissues, and refine conjugation chemistry to maintain ligand functionality while maximizing LNP stability. The continued innovation in LNP surface engineering promises to expand the therapeutic landscape for mRNA medicines, enabling treatments for genetic disorders, cancers, and infectious diseases with unprecedented precision and efficacy.
The development of personalized vaccines, particularly in the oncology sector, represents a paradigm shift in therapeutic medicine. These bespoke biologics are designed to target the unique mutational profile of an individual's tumor, offering unprecedented precision in cancer treatment [78] [60]. However, the manufacturing of these vaccines presents formidable challenges in scalability, timeline compression, and cost reduction. Each vaccine is a singular pharmaceutical product, requiring dedicated production lines and rigorous quality control specific to a single patient [79]. This application note details the cutting-edge innovations that are addressing these bottlenecks, enabling the transition of personalized cancer vaccines from research concepts to viable clinical therapeutics. By integrating advances in synthetic biology, automation, and artificial intelligence, the field is achieving remarkable reductions in both production timelines and associated costs, paving the way for broader clinical application [60] [80].
Current Landscape: Timelines and Costs
The production of a personalized mRNA cancer vaccine is a complex, multi-stage process. As of 2025, the landscape is characterized by rapid evolution, with significant disparities between conventional approaches and those enhanced by recent innovations.
Table 1: Key Manufacturing Milestones and Durations for Personalized mRNA Cancer Vaccines
| Manufacturing Stage | Conventional Timeline | Innovative Timeline | Key Innovations Enabling Reduction |
|---|---|---|---|
| Tumor Sample to Sequencing Data | 2-3 weeks | 1-2 weeks | Automated nucleic acid extraction, streamlined NGS protocols |
| Neoantigen Identification & Vaccine Design | 1-2 weeks | < 1 week | AI-powered bioinformatics platforms, cloud computing |
| DNA Template Production | 3-4 weeks | 1-3 days | Enzymatic DNA synthesis (e.g., DNA Script's SYNTAX system) [80] |
| mRNA Synthesis & Formulation | 1-2 weeks | ~1 week | Optimized in vitro transcription, scalable LNP formulation |
| Quality Control & Release | 1-2 weeks | 3-7 days | Rapid analytics, parallelized assays, Real-time release testing (RTRT) |
| Total Production Timeline | 8-12 weeks | ~4 weeks [60] | Holistic process integration and automation |
Table 2: Cost Analysis and Key Cost Drivers in Personalized Vaccine Manufacturing
| Cost Factor | Estimated Cost (USD) | Notes and Mitigation Strategies |
|---|---|---|
| Total Current Cost per Patient | > $100,000 [60] | Highly variable; depends on cancer type and platform. |
| Genomic Sequencing & Bioinformatic Analysis | $5,000 - $10,000 | Costs are decreasing with higher-throughput, cheaper sequencing. |
| GMP Manufacturing (Materials & Labor) | $50,000 - $80,000 | Largest cost driver; mitigated by closed-loop automated systems [60]. |
| Quality Control/Quality Assurance | $15,000 - $25,000 | Simplified QC paradigms for personalized products are under regulatory discussion. |
| Cold Chain & Logistics | $5,000 - $10,000 | Lyophilization (freeze-drying) of mRNA vaccines can eliminate ultra-cold chain requirements [60] [81]. |
Detailed Protocols for Key Manufacturing Innovations
Protocol: Rapid DNA Template Production via Enzymatic Synthesis
Background: The production of DNA templates has historically been a critical path bottleneck, relying on weeks-long bacterial fermentation (plasmid DNA) and purification [80]. Enzymatic DNA synthesis (EDS) offers a cell-free, rapid alternative.
Objective: To synthesize a high-quality, linear DNA template encoding patient-specific neoantigens within 72 hours.
Materials:
- DNA Synthesizer: SYNTAX system (DNA Script) or equivalent [80].
- Reagents: EDS nucleotide mix (dATP, dTTP, dCTP, dGTP, and proprietary modified nucleotides), primer-bound solid support, synthesis buffers.
- Purification Kits: Solid-phase extraction kits for oligonucleotide purification.
- QC Equipment: Capillary electrophoresis (e.g., Fragment Analyzer), Sanger sequencing apparatus.
Procedure:
- Sequence Input: Upload the final DNA sequence (typically 500-1500 base pairs) for the neoantigen minigene to the synthesizer software.
- Primer Immobilization: The system initializes with a primer covalently bound to a solid support.
- Cycle of Synthesis: The instrument executes repeated cycles of:
- Deprotection: Flows a deblocking solution to activate the growing chain's end.
- Coupling: Flows a single nucleotide, coupled with a modified terminator, to the chain via enzymatic addition using terminal deoxynucleotidyl transferase (TdT).
- Capping: Flows a capping solution to terminate any failed chains, ensuring synthesis fidelity.
- Post-Synthesis Processing:
- Cleavage & Deprotection: The full-length DNA product is cleaved from the solid support, and final deprotection removes any remaining protecting groups.
- Purification: Purify the product using a solid-phase extraction kit to remove short failure sequences and reagents.
- Quality Control:
- Purity & Length: Analyze 100 ng of the product via capillary electrophoresis. The sample must show a single dominant peak at the expected molecular weight.
- Sequence Verification: Perform Sanger sequencing on the final template. The sequence must have >99.9% identity to the input sequence.
- Output: The verified DNA template is now ready for the in vitro transcription (IVT) reaction to produce mRNA. The entire process, from sequence to template, is completed within 3 days [80].
Protocol: Automated, Closed-System Manufacturing Workflow
Background: Traditional biomanufacturing requires extensive open-handling steps, increasing contamination risk, manual labor, and timeline. Integrated closed systems automate this process.
Objective: To integrate the steps from DNA template to filled mRNA-LNP drug product with minimal human intervention, reducing total hands-on time and contamination risk.
Materials:
- Equipment: Integrated bioreactor system (e.g., for IVT), tangential flow filtration (TFF) skid, automated LNP formulator (e.g., using microfluidic mixing), and vial filling machine.
- Reagents: IVT enzyme mix, NTPs, CleanCap AG co-transcriptional capping agent, lipid mixture (ionizable lipid, DSPC, cholesterol, PEG-lipid), aqueous and alcohol buffers.
- Software: Manufacturing Execution System (MES) for recipe control and data tracking.
Procedure:
- System Setup and Sanitization: The closed-system modules are connected, and flow paths are sanitized according to GMP standards.
- In Vitro Transcription (IVT):
- The DNA template is automatically transferred to the IVT bioreactor.
- Pre-mixed IVT reagents are added. The reaction proceeds at 37°C for 2-4 hours.
- The reaction is halted by adding DNase to digest the DNA template.
- mRNA Purification:
- The IVT mixture is transferred through a TFF system for buffer exchange and concentration.
- An optional affinity chromatography step can be integrated for high-purity mRNA capture.
- Lipid Nanoparticle (LNP) Formulation:
- The purified mRNA is mixed with an aqueous buffer in one reservoir.
- A lipid mixture in ethanol is held in a second reservoir.
- The two solutions are pumped at a controlled ratio (typically 3:1 aqueous:ethanol) into a microfluidic mixer, resulting in instantaneous LNP formation.
- Buffer Exchange and Final Filtration:
- The formulated LNPs are diafiltered into the final formulation buffer (e.g., sucrose-containing buffer for cryoprotection) using a TFF system to remove residual ethanol.
- The bulk drug substance is passed through a sterile 0.22 µm filter.
- Fill-Finish: The filtered mRNA-LNP solution is automatically dispensed into vials, which are stoppered and capped.
- Real-Time Quality Control: In-line sensors monitor critical process parameters (pH, particle size, RNA concentration). Samples for critical quality attributes (identity, potency, purity) are taken automatically at key steps. This automated workflow has been demonstrated to reduce the mRNA production and formulation timeline from several weeks to under one week [60].
Visualizing the Optimized Workflow
The following diagram illustrates the integrated and accelerated workflow for manufacturing personalized mRNA vaccines, contrasting the traditional and innovative paths.
The Scientist's Toolkit: Essential Research Reagent Solutions
The implementation of these advanced protocols requires a suite of specialized reagents and tools. The following table details key solutions for developing and manufacturing personalized mRNA vaccines.
Table 3: Research Reagent Solutions for Personalized mRNA Vaccine Development
| Reagent/Material | Function | Key Characteristics & Examples |
|---|---|---|
| Enzymatic DNA Synthesis Kits | Rapid, template-free synthesis of linear DNA constructs for IVT. | DNA Script's SYNTAX system; enables production of DNA templates in days versus weeks [80]. |
| In Vitro Transcription (IVT) Kits | Synthesis of mRNA from a DNA template. | GMP-grade kits with co-transcriptional capping (e.g., CleanCap); ensure high-yield production of capped, polyadenylated mRNA. |
| Lipid Nanoparticle (LNP) Components | Formulation of mRNA into stable, delivery-competent nanoparticles. | Pre-mixed GMP-grade lipid blends (ionizable lipid, DSPC, Cholesterol, PEG-lipid); critical for efficient intracellular delivery. |
| AI-Powered Neoantigen Prediction Software | In silico identification of immunogenic tumor neoantigens from sequencing data. | Proprietary algorithms (e.g., from Neomatrix, Gritstone); filters for HLA binding affinity, TCR recognition, and dissimilarity from self to minimize autoimmunity risk [60] [81]. |
| Lyophilization (Freeze-Drying) Protectors | Stabilization of mRNA-LNP formulations for room-temperature storage. | Lyoprotectants like sucrose and trehalose; form a stable glassy matrix, potentially obviating the need for a cold chain [60]. |
The field of personalized vaccine manufacturing is undergoing a revolutionary transformation, driven by technological convergence. Innovations in enzymatic DNA synthesis, automated closed-system production, AI-driven design, and advanced analytics are collectively compressing development timelines from 3 months to approximately 4 weeks, while actively addressing prohibitive costs [60] [80]. These advancements are not merely incremental; they are fundamentally enhancing the feasibility of delivering truly personalized immunotherapy to cancer patients. As these protocols and systems continue to mature and gain regulatory acceptance, they promise to establish a new standard in precision medicine, turning the visionary goal of accessible, individualized cancer treatment into a clinical reality.
Addressing Theoretical Safety Concerns and DNA Impurity Debates
The rapid development and deployment of mRNA vaccines against SARS-CoV-2 have fundamentally transformed the landscape of vaccinology. Despite their demonstrated success in curbing the COVID-19 pandemic, these vaccines have been subject to theoretical safety concerns and ongoing scientific debates, particularly regarding DNA impurities. These discussions have gained prominence in scientific forums and regulatory meetings, highlighting the need for clear methodological standards and transparent data interpretation [82]. Within the broader context of mRNA vaccine design and development research, this document addresses these debates by providing evidence-based analysis, standardized protocols for impurity quantification, and an overview of emerging platform technologies that may address current limitations.
Recent presentations at regulatory advisory committee meetings have brought forth various alleged "safety uncertainties" concerning mRNA COVID-19 vaccines, including claims about cancer risks and immune system alterations. However, scientific evaluation indicates that many of these concerns are based on misinterpretations of studies or flawed science presented without proper context [82]. This application note aims to equip researchers and drug development professionals with the methodological rigor necessary to navigate these complex debates while advancing the mRNA vaccine platform.
DNA Impurity Debates: Methodological Considerations
The Core of the Controversy
The debate surrounding DNA impurities in mRNA vaccines primarily concerns the accuracy of quantification methods and the biological relevance of findings. All mRNA vaccines undergo a manufacturing process that utilizes DNA templates for in vitro transcription, necessitating rigorous purification to remove residual DNA fragments. Regulatory agencies worldwide, including the FDA and EMA, have established a limit of 10 ng of residual DNA per vaccine dose [83]. While some studies have reported DNA contamination exceeding regulatory limits by several hundred-fold, these findings have been contested on methodological grounds [82] [83].
A pivotal consideration in this debate is the fundamental difference in chemical properties between DNA and mRNA. Despite both being nucleic acids, DNA exhibits greater stability under typical storage conditions, potentially persisting for decades in the absence of degrading enzymes, while mRNA is comparatively labile. This disparity complicates both the removal of DNA during manufacturing and its accurate quantification in the final product [83].
Methodological Discrepancies in DNA Quantification
The controversy largely stems from divergent methodological approaches to DNA quantification, each with distinct limitations and applications:
- qPCR-Based Methods: Manufacturers typically use quantitative polymerase chain reaction (qPCR) targeting a specific 69-base-pair sequence within the 7824-base-pair DNA template. This method measures only approximately 1% of the total template sequence and relies on mathematical extrapolation to estimate total DNA content. Critics argue this approach assumes proportional degradation across all template sequences during DNase digestion, an assumption that may not hold in practice [83].
- Fluorescence Spectroscopic Methods: Alternative protocols utilize fluorescent dyes like Qubit fluorometry to measure total DNA content directly. This method requires prior dissolution of lipid nanoparticles (LNPs) with detergents to release encapsulated DNA. While providing a direct measurement of total DNA, this approach may be susceptible to interference from vaccine components [83].
The scientific community has expressed concerns about studies reporting high DNA contamination levels. As noted in [82], "all these studies have used methods that do not allow for correct measurement of DNA." Specifically, methods using fluorescent dyes may overestimate DNA content due to interference from high mRNA and lipid concentrations in the vaccine samples if not properly calibrated [82].
Regulatory and Analytical Context
Regulatory perspectives emphasize that concerns about DNA contamination remain largely theoretical. Multiple layers of cellular protection prevent foreign DNA fragments from integrating into human genomes or otherwise causing harm [82]. Independent verification efforts, including an unpublished study under review at npj Vaccines, have found residual DNA levels "below approved limits, in very low quantities relative to mRNA, and degraded into small fragments" [82].
The journal Methods and Protocols issued an Expression of Concern in June 2025 regarding a paper that advocated for fluorescence-based DNA quantification, noting ongoing investigation into the appropriateness of its methodology and validity of its data [84]. This highlights the evolving nature of this scientific discussion and the importance of methodological rigor.
Quantitative Data Comparison
Table 1: Comparison of DNA Quantification Methods for mRNA Vaccines
| Method | Principle | Target Sequence | Reported DNA Levels | Advantages | Limitations |
|---|---|---|---|---|---|
| qPCR | Amplification of specific DNA sequence | 69 bp of 7824 bp plasmid (<1% of total) | Within regulatory limits (manufacturer data) | High specificity for template DNA; sensitive | Extrapolates from <1% of sequence; may not detect fragmented DNA |
| Fluorescence Spectroscopy | Fluorescent dye binding to DNA | Total DNA | 36-627x above limits (contested studies) [82] | Direct total DNA measurement | Potential interference from mRNA/lipids; requires LNP dissolution |
| Independent Verification | Multiple methods | Total DNA | Below regulatory limits [82] | Multi-method validation | Limited publicly available data |
Table 2: Key Considerations in DNA Impurity Risk Assessment
| Factor | Considerations | Regulatory Status |
|---|---|---|
| DNA Fragment Size | Large fragments vs. small degraded fragments; potential for biological activity | Fragmentation expected during manufacturing |
| Cellular Uptake Mechanisms | DNA encapsulated in LNPs may have different uptake profiles than free DNA | Not fully characterized |
| Integration Risk | Multiple cellular barriers prevent genomic integration; theoretical risk only | No evidence of integration in vivo |
| Immunogenicity | Potential for innate immune activation by bacterial DNA sequences | Considered in risk-benefit assessment |
Experimental Protocols
Protocol 1: DNA Quantification via Fluorescence Spectroscopy
This protocol details the procedure for direct DNA quantification in mRNA vaccine samples using fluorescence spectroscopy, adapted from methodologies described in the literature [83].
Reagents and Equipment
- mRNA vaccine samples
- Triton X-100 detergent (1% solution in TE buffer)
- TE buffer (10 mM Tris-HCl, 1 mM EDTA, pH 8.0)
- Quant-iT PicoGreen dsDNA reagent (or similar DNA-binding fluorescent dye)
- DNase-free water
- Standard DNA for calibration curves
- Fluorometer with appropriate excitation/emission filters (∼480 nm/520 nm for PicoGreen)
- Microcentrifuge tubes
- Vortex mixer
- Heating block or water bath
Procedure
Sample Preparation:
- Allow vaccine vials to reach room temperature before analysis.
- Transfer 100 µL of vaccine to a clean microcentrifuge tube.
- Add 10 µL of 1% Triton X-100 solution to dissolve LNPs.
- Vortex thoroughly for 30 seconds and incubate at room temperature for 10 minutes.
Standard Curve Preparation:
- Prepare DNA standards in the range of 0-500 pg/µL in TE buffer with 0.1% Triton X-100 to match sample matrix.
Dye Addition and Incubation:
- Prepare working dye solution according to manufacturer instructions.
- Add 100 µL of each standard and sample to separate tubes containing 100 µL of dye solution.
- Mix thoroughly and incubate at room temperature for 5 minutes, protected from light.
Fluorescence Measurement:
- Measure fluorescence using appropriate instrument settings.
- Generate standard curve and calculate DNA concentration in samples by interpolation.
Validation Controls:
- Include samples spiked with known DNA quantities for recovery assessment.
- Perform measurements in triplicate to ensure reproducibility.
Protocol 2: qPCR-Based DNA Quantification
This protocol outlines the standard qPCR method used by manufacturers for residual DNA quantification, with attention to potential methodological limitations [83].
Reagents and Equipment
- mRNA vaccine active substance (pre-LNP formulation)
- qPCR master mix with DNA polymerase
- Sequence-specific primers and probes for target sequence (e.g., T7 promoter region)
- DNA standards from linearized plasmid template
- DNase-free water
- Real-time PCR instrument
- PCR plates or tubes
- Microcentrifuge
Procedure
Standard Curve Preparation:
- Prepare dilution series of linearized plasmid DNA in the expected concentration range.
- Use the same matrix as the sample when possible to account for potential inhibition.
Sample Preparation:
- Use active substance (mRNA before LNP encapsulation) according to manufacturer protocols.
- Dilute samples to fall within the quantitative range of the standard curve.
qPCR Reaction Setup:
- Prepare reaction mix according to manufacturer instructions.
- Add standards and samples to designated wells in triplicate.
- Seal plate and centrifuge briefly to remove bubbles.
Amplification Parameters:
- Use manufacturer-recommended cycling conditions.
- Include appropriate controls (no-template, negative extraction, positive).
Data Analysis:
- Generate standard curve from dilution series.
- Calculate DNA concentration in samples by comparison to standard curve.
- Apply correction factors as validated in method development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for DNA Impurity Analysis
| Reagent/Equipment | Application | Function | Considerations |
|---|---|---|---|
| Quant-iT PicoGreen dsDNA Assay | Fluorescence-based DNA quantification | Binds dsDNA with high sensitivity; >1000x selective over RNA | Potential interference from LNPs; requires controls |
| Triton X-100 Detergent | LNP dissolution | Disrupts lipid nanoparticles to release encapsulated nucleic acids | Optimization required for complete LNP dissolution |
| T7 Promoter-specific Primers/Probes | qPCR quantification | Amplifies specific 69 bp target sequence in residual DNA template | Only detects specific sequence; extrapolation required |
| Linearized Plasmid DNA Standard | Standard curve generation | Provides reference for quantitative analysis | Should mimic manufacturing process fragments |
| DNase I Enzyme | DNA removal during manufacturing | Degrades DNA templates after mRNA transcription | Limited digestion to preserve mRNA integrity |
Addressing Theoretical Safety Concerns
IgG4 Antibody Class Switching
Among the theoretical safety concerns raised is the observation that repeated mRNA vaccination can lead to an increased proportion of spike-specific IgG4 antibodies, a phenomenon noted in several studies including a 2023 Science Immunology paper [82]. IgG4 antibodies are generally associated with tolerance and may have reduced effector functions compared to other antibody subclasses.
However, the clinical significance of this observation remains uncertain. Dr. Kilian Schober, a co-senior author of the Science Immunology paper, stated that these findings "do not raise any safety concerns" and represent "primarily an 'interesting immunological observation'" [82]. Current evidence indicates that repeated COVID-19 vaccination continues to protect against severe disease despite this immunological phenomenon.
Next-Generation mRNA Vaccine Platforms
Emerging mRNA technologies aim to address both real and theoretical concerns associated with current LNP-based mRNA vaccines:
Lipid-Free mRNA Formulations: Researchers have developed alumina-coated, lipid-free mRNA vaccines using atomic layer deposition techniques. These formulations demonstrate equivalent or enhanced immunogenicity compared to LNP-based vaccines while offering improved thermostability - addressing both cold-chain limitations and lipid-associated reactogenicity concerns [85].
Metal Ion-Mediated mRNA Enrichment: A manganese ion (Mn²⁺)-mediated mRNA enrichment strategy achieves nearly twice the mRNA loading capacity compared to conventional LNP formulations. This L@Mn-mRNA platform enhances cellular uptake while reducing the lipid dose required, potentially mitigating lipid-related toxicity concerns [40].
Enhanced Manufacturing Controls: Advances in manufacturing include improved template DNA removal, enhanced purification processes, and more sensitive analytical methods to detect and quantify process-related impurities [86].
The debates surrounding DNA impurities and theoretical safety concerns in mRNA vaccines highlight the critical importance of methodological rigor, appropriate data interpretation, and contextual understanding in vaccine science. While legitimate scientific discussion continues, current evidence indicates that DNA impurity levels in approved mRNA vaccines fall within regulatory limits when measured using validated methods. Theoretical concerns regarding immune alterations remain just that - theoretical - without compelling clinical evidence of harm.
The ongoing evolution of mRNA platform technologies promises to address current limitations while enhancing the safety profile of this transformative vaccine modality. As the field advances, researchers should maintain rigorous standards for impurity quantification, transparent reporting of methodological limitations, and balanced interpretation of findings within the broader context of vaccine benefit-risk assessment.
The future of mRNA vaccine technology lies not only in addressing current debates but in proactively designing next-generation platforms that preemptively mitigate theoretical concerns while expanding the utility of this versatile platform against diverse infectious diseases, cancers, and genetic disorders [54] [11].
Clinical Trial Outcomes, Regulatory Landscapes, and Comparative Effectiveness
The field of mRNA therapeutics has expanded dramatically beyond its initial success in coronavirus disease 2019 (COVID-19) vaccination, emerging as a versatile platform for oncology, infectious diseases, and other therapeutic areas. Current clinical development encompasses over 120 RNA cancer vaccine trials across various malignancies, including lung, breast, prostate, melanoma, pancreatic, and brain tumors, representing a significant expansion from previous years [60]. This robust pipeline demonstrates the broad applicability of RNA vaccine platforms, with over 60 candidates in clinical development and the first commercial approvals anticipated by 2029 [60]. The diversity of cancer types under investigation validates the transformative potential of this therapeutic approach, particularly for historically challenging targets like pancreatic ductal adenocarcinoma and glioblastoma [60].
The unprecedented clinical advances observed from 2024 to 2025 have established mRNA vaccines as a viable treatment option across multiple cancer types, catalyzing global expansion of phase 3 trial programs [60]. This growth has been facilitated by decades of meticulous research into mRNA biology, particularly rapid progress over the past 20 years that enabled the successful development of COVID-19 mRNA vaccines [87]. These vaccines demonstrated that mRNA technology is safe, reliable, and cost-efficient, setting the stage for its application across diverse therapeutic areas [87]. The clinical pipeline continues to evolve with innovations in trial design, endpoint selection, and regulatory frameworks specifically adapted for cancer vaccine development [60].
Quantitative Analysis of Active Clinical Trials
Table 1: mRNA Vaccine Clinical Trials by Therapeutic Area and Development Phase
| Therapeutic Area | Phase I | Phase I/II | Phase II | Phase II/III | Phase III | Total Trials |
|---|---|---|---|---|---|---|
| Oncology | 35 | 28 | 42 | 8 | 12 | ~125 |
| Infectious Diseases | 15 | 10 | 12 | 5 | 8 | ~50 |
| Other Indications | 5 | 3 | 4 | 1 | 2 | ~15 |
Table 2: Promising mRNA Vaccine Candidates in Advanced-Stage Clinical Development
| Candidate | Target | Developer | Phase | Key Characteristics |
|---|---|---|---|---|
| mRNA-4157 (V940) | Melanoma | Moderna-Merck | Phase 3 | Personalized cancer vaccine; 44% reduction in recurrence risk with pembrolizumab [60] |
| BNT113 | HPV+ Head & Neck Cancer | BioNTech | Phase 2 | Targets HPV16 antigens; combined with pembrolizumab [87] |
| CVGBM | Glioblastoma | Phase 1 | Newly diagnosed, surgically resected MGMT-unmethylated GBM [87] | |
| BNT116 | NSCLC | BioNTech | Phase 2 | Combined with cemiplimab in advanced NSCLC with PD-L1 ≥50% [87] |
| mRNA-1010 | Influenza | Moderna | Phase 2/3 | Tetravalent seasonal influenza vaccine [7] |
The oncology sector dominates the mRNA clinical trial landscape, with investigations expanding across numerous cancer types. The sustained clinical benefit of mRNA-4157 in combination with pembrolizumab has been reinforced by extended follow-up data, showing 3-year recurrence-free survival rates maintaining superiority over pembrolizumab monotherapy [60]. This success has catalyzed global expansion of the phase 3 trial program, with regulatory submissions anticipated in 2026 [60]. Beyond personalized cancer vaccines, off-the-shelf approaches targeting shared tumor-associated antigens continue to advance through clinical development, offering alternative strategies for faster patient access [87].
In infectious diseases, numerous mRNA vaccine candidates are progressing through clinical trials for pathogens beyond SARS-CoV-2. Moderna's mRNA-1010 tetravalent influenza vaccine represents one of the most advanced programs, currently in phase II/III clinical trials [7]. Additional candidates targeting respiratory syncytial virus (RSV), human immunodeficiency virus (HIV), mpox, and Zika virus demonstrate the platform's flexibility for addressing diverse viral threats [87]. The rapid sequence adaptation capability of mRNA platforms makes them particularly valuable for addressing mutating pathogens like influenza and emerging viral variants [7].
Key Methodologies and Experimental Protocols
Personalized mRNA Cancer Vaccine Design and Manufacturing
The production of personalized mRNA cancer vaccines involves a complex, multi-step process that begins with tumor sample acquisition and culminates in formulated vaccine product. The following protocol outlines key steps for neoantigen-targeted vaccine manufacturing:
Step 1: Tumor Sequencing and Neoantigen Identification
- Obtain tumor tissue sample via biopsy or surgical resection, along with matched normal tissue (typically blood)
- Perform whole-exome sequencing and RNA sequencing to identify somatic mutations
- Utilize artificial intelligence-driven platforms incorporating multi-omics data analysis to identify optimal tumor-specific targets while predicting immunogenicity and potential immune escape mechanisms [60]
- Prioritize mutations based on HLA binding affinity, tumor clonality, and gene expression levels
- Select 10-20 validated neoantigens for vaccine inclusion
Step 2: DNA Template Preparation and mRNA Synthesis
- Design and synthesize DNA plasmids encoding selected neoantigens with optimized codon usage
- Linearize plasmid DNA using restriction enzymes for run-off transcription
- Perform in vitro transcription (IVT) using bacteriophage RNA polymerase (T7, T3, or SP6) with nucleotide triphosphates, including modified nucleosides (e.g., pseudouridine, N1-methylpseudouridine) to reduce immunogenicity [18]
- Co-transcriptionally cap mRNA using CleanCap technology to achieve >90% cap 1 structure incorporation [11]
- Incorporate poly(A) tail of approximately 100 nucleotides, either encoded in DNA template or added enzymatically
Step 3: mRNA Purification and Quality Control
- Digest DNA template using DNase treatment
- Remove contaminants including truncated RNA transcripts, residual nucleotides, and enzymes using chromatographic purification methods (e.g., HPLC, FPLC)
- Specifically remove double-stranded RNA contaminants that activate innate immune sensors and reduce protein expression [48]
- Confirm mRNA identity, purity, and integrity using analytical methods including capillary electrophoresis, UV spectroscopy, and sequencing
- Verify sterility, endotoxin levels, and absence of residual process contaminants
Step 4: Lipid Nanoparticle Formulation
- Prepare lipid mixture containing ionizable cationic lipid, phospholipid, cholesterol, and PEG-lipid in ethanol phase
- Combine mRNA in aqueous buffer (pH 4-5) with lipid ethanol solution using microfluidic mixing device
- Formulate nanoparticles through rapid mixing, enabling spontaneous self-assembly
- Dialyze against neutral pH buffer to remove ethanol and establish stable lipid bilayer structure
- Filter sterilize final LNP product and package in vials for storage at -80°C to -20°C
Step 5: Final Product Release Testing
- Characterize LNP particle size (typically 70-100 nm), polydispersity index, mRNA encapsulation efficiency, and identity
- Confirm potency through in vitro expression of encoded antigens
- Validate sterility, endotoxin levels, and absence of visible particulates
- Establish stability profile under recommended storage conditions
The manufacturing process for personalized pancreatic cancer vaccines has been optimized to an average of 9 weeks from surgery to the first vaccine dose, with successful vaccine creation achieved for 18 of 19 study participants, representing a substantial improvement in production efficiency [60]. However, manufacturing costs for personalized approaches continue to exceed $100,000 per patient, necessitating continued innovation in automated production systems [60].
Diagram 1: Personalized mRNA Cancer Vaccine Workflow. This diagram illustrates the multi-step process from tumor sampling to vaccine administration, highlighting key stages in neoantigen identification, vaccine manufacturing, and clinical implementation.
Immune Monitoring and Biomarker Analysis
Assessment of immunogenicity and treatment response represents a critical component of mRNA vaccine clinical trials. The following protocols outline standard methodologies for evaluating cellular and humoral immune responses:
Protocol 1: T-cell Response Evaluation by ELISpot
- Isolate peripheral blood mononuclear cells (PBMCs) from patient blood samples collected pre-vaccination and at multiple timepoints post-vaccination
- Plate PBMCs in duplicate or triplicate in IFN-γ antibody-coated plates
- Stimulate with pools of peptides corresponding to vaccine antigens or individual epitopes
- Include positive controls (mitogens) and negative controls (DMSO or irrelevant peptides)
- Develop plates using enzyme-conjugated detection antibodies and substrate solution
- Quantify spot-forming units (SFUs) using automated ELISpot reader
- Calculate antigen-specific T-cell frequency as SFUs per million PBMCs after subtracting background
Protocol 2: Multiparametric Flow Cytometry for T-cell Phenotyping
- Stain PBMCs with fluorescently-labeled antibody panels targeting surface markers (CD3, CD4, CD8, CD45RA, CCR7) and intracellular cytokines (IFN-γ, TNF-α, IL-2)
- Stimulate cells with antigenic peptides for 6-16 hours in the presence of protein transport inhibitors
- Include viability dye to exclude dead cells from analysis
- Acquire data on flow cytometer with minimum 12-color configuration
- Analyze data using computational approaches to identify antigen-specific T-cell populations and characterize memory differentiation (naïve, central memory, effector memory, terminally differentiated)
- Assess polyfunctionality based on production of multiple cytokines
Protocol 3: Humoral Response Assessment
- Quantify antigen-specific antibody titers using ELISA with recombinant protein coating
- Evaluate neutralizing antibody capacity using pseudovirus or live virus neutralization assays when applicable
- Measure antibody subclass distribution (IgG1, IgG2, IgG3, IgG4) and antibody-dependent cellular cytotoxicity (ADCC) activity for relevant targets
Recent studies have incorporated additional cutting-edge methodologies including T-cell receptor sequencing to track clonal expansion, mass cytometry (CyTOF) for deep immune phenotyping, and spatial transcriptomics to evaluate immune cell infiltration in tumor microenvironments [88] [60]. These comprehensive immune monitoring approaches enable correlation of vaccine-induced immune responses with clinical outcomes, facilitating identification of predictive biomarkers.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for mRNA Vaccine Development
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| mRNA Synthesis | CleanCap AG cap analog, N1-methylpseudouridine, T7 RNA polymerase | Co-transcriptional capping, reduced immunogenicity, in vitro transcription [11] |
| Purification | DNase I, HPLC/FPLC systems, oligo-dT cellulose | Template removal, dsRNA elimination, mRNA purification [48] |
| Lipid Nanoparticles | Ionizable lipids (DLin-MC3-DMA), DSPC, cholesterol, PEG-lipids | mRNA encapsulation, cellular delivery, endosomal escape [18] |
| Immune Monitoring | ELISpot kits, multiplex cytokine panels, MHC multimers | T-cell response quantification, cytokine profiling, antigen-specific T-cell detection |
| Cell Culture | Dendritic cells, antigen-presenting cell lines, autologous T-cells | In vitro potency assays, antigen presentation assessment |
The expansive clinical pipeline of over 120 active trials across multiple indications demonstrates the remarkable transition of mRNA vaccine technology from theoretical concept to clinical reality. The promising results observed in oncology, particularly with personalized neoantigen vaccines, suggest this platform may fundamentally transform cancer treatment paradigms when combined with complementary immunotherapies [88] [60]. The documented improvement in overall survival for cancer patients who received mRNA COVID-19 vaccines alongside immunotherapy provides compelling evidence for the immune-potentiating effects of mRNA platforms beyond their specific antigenic targets [88].
Future developments in the mRNA clinical trial landscape will likely focus on several key areas: enhancing manufacturing efficiency to reduce costs and production timelines, improving delivery systems for better tissue targeting and reduced reactogenicity, developing more sophisticated neoantigen prediction algorithms through artificial intelligence integration, and establishing standardized immune monitoring frameworks to identify correlates of protection [60] [87]. Additionally, combination strategies with other therapeutic modalities including cell therapies, cytokine therapies, and targeted agents will expand the clinical utility of mRNA vaccines across diverse patient populations [7] [87].
As the field continues to mature, the ongoing clinical trials will provide critical insights into optimal vaccine design, dosing schedules, and patient selection criteria. With first commercial approvals anticipated by 2029, mRNA vaccines are positioned to become cornerstone therapeutics in personalized oncology and infectious disease prevention, ultimately realizing their potential to transform treatment across a broad spectrum of human diseases [60].
mRNA-based cancer vaccines have emerged as transformative immunotherapeutic platforms, demonstrating unprecedented clinical efficacy across multiple challenging malignancies. The period from 2024 to 2025 has marked a pivotal turning point in oncology, with breakthrough results in melanoma, pancreatic cancer, and glioblastoma establishing this technology as a viable treatment modality. These advances leverage the unique capability of mRNA vaccines to train the immune system to recognize and eliminate specific cancer cells, representing a significant advancement in personalized cancer care [60]. The convergence of artificial intelligence, novel delivery systems, and optimized mRNA architectures has accelerated clinical development, with over 120 active clinical trials currently underway across various cancer types [60]. This document provides a comprehensive technical summary of the most significant recent breakthroughs, detailed experimental methodologies, and specialized reagent solutions to support research and development in this rapidly evolving field.
Clinical Breakthroughs: Efficacy Data Across Cancer Types
Recent clinical trials have demonstrated remarkable efficacy of mRNA cancer vaccines in malignancies traditionally resistant to immunotherapy. The table below summarizes quantitative efficacy data from key studies reported in 2024-2025.
Table 1: Clinical Efficacy of mRNA Cancer Vaccines Across Indications
| Cancer Type | Vaccine Platform | Combination Therapy | Key Efficacy Metrics | Trial Phase |
|---|---|---|---|---|
| Melanoma | mRNA-4157 (Personalized) | Pembrolizumab (anti-PD-1) | 44% reduction in recurrence risk; Superior 3-year recurrence-free survival vs. pembrolizumab monotherapy [60] | Phase 3 |
| Pancreatic Ductal Adenocarcinoma | Personalized mRNA Vaccine | Adjuvant chemotherapy | Vaccine-induced immune responses persisting nearly 4 years; Reduced recurrence risk at 3-year follow-up vs. non-responders [60] | Phase 2 |
| Glioblastoma | Layered mRNA Nanoparticle | Not specified | Rapid immune system reprogramming within 48 hours; Conversion of "cold" to "hot" tumors; Preclinical models: Treated pet dogs lived nearly 4x longer than historical expectations [60] | Preclinical/Human trials |
| Advanced NSCLC | SARS-CoV-2 mRNA Vaccine | Immune Checkpoint Inhibitors | Median survival: 37.33 months (vaccinated + ICI) vs. 20.6 months (ICI alone); 3-year OS: 55.7% vs. 30.8% (HRadj = 0.51) [88] [13] | Retrospective |
| Metastatic Melanoma | SARS-CoV-2 mRNA Vaccine | Immune Checkpoint Inhibitors | Median OS: Not reached (vaccinated) vs. 26.67 months (unvaccinated); 36-month OS: 67.6% vs. 44.1% (HRadj = 0.37) [88] [13] | Retrospective |
The mechanistic basis for these clinical improvements involves significant immune system reprogramming. mRNA vaccines function as potent immune activators that create a favorable environment for combination therapies, particularly immune checkpoint inhibitors [88]. In preclinical models, SARS-CoV-2 mRNA vaccines induced a substantial increase in type I interferon, enabling innate immune cells to prime CD8+ T cells that target tumour-associated antigens [13]. This effect was most pronounced in patients with immunologically "cold" tumors, who experienced a nearly five-fold improvement in three-year overall survival when receiving mRNA vaccines in conjunction with immunotherapy [88].
Table 2: Immune Correlates of Vaccine Response Across Studies
| Immune Parameter | Preclinical Findings | Human Correlates | Functional Significance |
|---|---|---|---|
| Type I Interferon | Substantial increase post-vaccination | Increases in IFNα detected in healthy volunteers | Enhances APC priming of T cells in lymphoid organs [13] |
| PD-L1 Expression | Upregulated on tumor cells following vaccination | Increased PD-L1 expression on tumors in vaccinated patients | Tumor defense mechanism blocked by concomitant ICI therapy [88] [13] |
| T-cell Priming | Enhanced antigen-presenting cell priming of CD8+ T cells | Myeloid-lymphoid activation observed | Enables epitope spreading against tumor-associated antigens [13] |
| Tumor Microenvironment | Conversion from "cold" to "hot" status | Vigorous immune cell infiltration in treated tumors | Creates permissive environment for immune-mediated tumor killing [60] |
Experimental Protocols: Key Methodologies
Layered Nanoparticle Delivery System for Brain Tumors
Background: This protocol describes the development of layered lipid nanoparticles capable of crossing the blood-brain barrier and reprogramming the immune system to attack glioblastoma within 48 hours of administration.
Materials:
- Biocompatible ionizable lipids (proprietary formulations)
- Cholesterol and phospholipid components
- PEG-lipids for stability
- mRNA constructs encoding tumor-associated antigens
- Microfluidic mixing device
Procedure:
- Nanoparticle Formulation:
- Prepare lipid mixture in ethanol at 1:1:0.5:0.03 molar ratio (ionizable lipid:cholesterol:phospholipid:PEG-lipid)
- Dilute mRNA in citrate buffer (pH 4.0) at 0.2 mg/mL concentration
- Combine solutions using microfluidic mixer at 1:3 aqueous-to-ethanol flow rate ratio
- Dialyze against PBS (pH 7.4) for 24 hours to remove ethanol
Characterization:
- Measure particle size and polydispersity via dynamic light scattering (Target: 80-100 nm, PDI <0.2)
- Determine encapsulation efficiency using Ribogreen assay (>90% target)
- Verify mRNA integrity by gel electrophoresis
In Vivo Evaluation:
- Administer particles intravenously to glioblastoma-bearing mouse models at 0.5 mg/kg mRNA dose
- Monitor tumor infiltration by immune cells via flow cytometry at 24, 48, and 72 hours
- Assess survival benefit compared to control formulations [60]
Macroporous Hydrogel-Based Dendritic Cell Recruitment
Background: This methodology addresses the challenge of inefficient mRNA uptake by dendritic cells through active recruitment using a chemokine-loaded hydrogel platform.
Materials:
- Methacrylated hyaluronic acid (MeHA)
- Photoinitiator (Irgacure 2959)
- CCL20 chemokine (dendritic cell attractant)
- mRNA-loaded lipid nanoparticles
- UV light source for crosslinking
Procedure:
- Hydrogel Fabrication:
- Prepare 2% (w/v) MeHA solution in PBS
- Add 0.05% (w/v) photoinitiator and mix with mRNA-LNPs (100 μg/mL final concentration)
- Incorporate CCL20 chemokine at 100 ng/mL concentration
- Inject subcutaneously into mouse model and crosslink with UV light (365 nm, 5 mW/cm², 5 minutes)
Dendritic Cell Recruitment Assessment:
- Excise hydrogel implants at days 3, 7, and 14 post-implantation
- Digest hydrogel with hyaluronidase and analyze infiltrating cells by flow cytometry
- Quantify CD11c+ MHC II+ dendritic cells as percentage of total cells
T-cell Activation Analysis:
- Isolate T cells from draining lymph nodes
- Co-culture with bone marrow-derived dendritic cells pulsed with tumor antigens
- Measure IFN-γ production by ELISA and tumor-specific cytotoxicity [89]
SARS-CoV-2 mRNA Vaccine Synergy with Immune Checkpoint Blockade
Background: This protocol leverages commercially available SARS-CoV-2 mRNA vaccines to sensitize tumors to immune checkpoint inhibition, based on findings from MD Anderson Cancer Center.
Materials:
- Commercial SARS-CoV-2 mRNA vaccines (BNT162b2 or mRNA-1273)
- Anti-PD-1/PD-L1 antibodies (clinical grade)
- Tumor-bearing mouse models (syngeneic or humanized)
- Flow cytometry panel for immune profiling
Procedure:
- Vaccination Schedule:
- Administer SARS-CoV-2 mRNA vaccine (10 μg mRNA equivalent) intramuscularly
- Prime and boost regimen (days 0 and 21)
- Initiate anti-PD-1 therapy (200 μg intraperitoneally) beginning day 7 after first vaccination
Immune Monitoring:
- Collect blood and tumor tissue at multiple timepoints
- Measure type I interferon levels in serum via multiplex ELISA
- Quantify PD-L1 expression on tumor cells by flow cytometry
- Analyze tumor-infiltrating lymphocytes (CD8+, CD4+, Treg populations)
Efficacy Assessment:
Signaling Pathways and Experimental Workflows
Diagram 1: Mechanism of SARS-CoV-2 mRNA Vaccine Synergy with Immunotherapy
Diagram 2: Hydrogel-Based Dendritic Cell Recruitment and Activation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for mRNA Cancer Vaccine Development
| Reagent Category | Specific Product/Technology | Research Function | Key Applications |
|---|---|---|---|
| mRNA Synthesis | CleanCap AG co-transcriptional capping | Enables single-step production of cap 1 mRNA | All mRNA vaccine platforms; enhances translation efficiency [60] |
| Lipid Nanoparticles | Ionizable lipids (e.g., DLin-MC3-DMA, SM-102) | Forms core structure for mRNA encapsulation | Systemic delivery; tissue-specific targeting [90] [60] |
| Dendritic Cell Markers | Anti-CD11c, Anti-MHC II antibodies | Identification and quantification of dendritic cells | Immune monitoring; vaccine efficacy assessment [89] |
| Cryo-EM Reagents | Graphene oxide grids, Vitrobot systems | High-resolution imaging of LNP structure | Quality control; formulation optimization [90] |
| Chemokine Reagents | Recombinant CCL20/MIP-3α | Dendritic cell recruitment to vaccination site | Hydrogel-based vaccine platforms [89] |
| IFNα ELISA Kits | High-sensitivity multiplex assays | Quantification of type I interferon response | Immune activation monitoring; mechanism studies [13] |
| Flow Cytometry Panels | T-cell exhaustion markers (PD-1, TIM-3, LAG-3) | Assessment of T-cell differentiation状态 | Tumor microenvironment analysis [88] |
| 3D Bioprinting Systems | Extrusion-based printers with temperature control | Fabrication of macroporous hydrogel scaffolds | Tissue engineering approaches to vaccine delivery [89] |
The breakthrough results in melanoma, pancreatic cancer, and brain tumors underscore the transformative potential of mRNA vaccine technology in oncology. The documented 44% reduction in recurrence risk for melanoma patients receiving mRNA-4157 combined with pembrolizumab, along with unprecedented responses in traditionally immunotherapy-resistant pancreatic cancer, represents a paradigm shift in cancer treatment [60]. The unexpected synergy between SARS-CoV-2 mRNA vaccines and immune checkpoint inhibitors further expands the potential applications of this platform, suggesting that non-tumor-targeting mRNA vaccines can function as potent immune modulators to sensitize resistant tumors to existing immunotherapies [88] [13].
Future development will focus on optimizing delivery systems for enhanced tissue targeting, reducing manufacturing timelines and costs for personalized vaccines, and identifying predictive biomarkers for patient selection. With over 60 candidates in clinical development and the first commercial approvals anticipated by 2029, mRNA cancer vaccines are positioned to become cornerstone therapeutics in personalized oncology, offering transformative hope for cancer patients worldwide [60]. The integration of artificial intelligence for neoantigen selection, CRISPR for construct optimization, and continued innovation in nanoparticle design will further accelerate this progress, potentially enabling rapid development of effective cancer vaccines for a broad spectrum of malignancies.
The Infectious Diseases Society of America (IDSA) released comprehensive guidelines in October 2025 for the use of vaccines against respiratory tract infections (RTIs) in immunocompromised patients during the 2025-2026 season [91]. These evidence-based recommendations address a critical challenge in clinical practice: optimizing protection for over 40 million Americans with impaired immunity who remain vulnerable to severe outcomes from COVID-19, influenza, and respiratory syncytial virus (RSV) despite vaccination [92]. The guidelines were developed through systematic literature reviews and GRADE methodology assessments, focusing on patient-important outcomes including hospitalization, mortality, and progression to severe disease [91].
For mRNA vaccine researchers and developers, these guidelines highlight both the significant advances and persistent limitations of current mRNA platforms in immunocompromised populations. While mRNA vaccines demonstrate measurable effectiveness, their attenuated and short-lived protection in immunocompromised hosts underscores the need for next-generation designs that can overcome the specific immunological barriers present in these patients [91] [92]. This creates an imperative for innovative approaches that enhance immunogenicity and durability in the context of compromised immune function.
Quantitative Effectiveness Data
The IDSA guidelines provide specific vaccine effectiveness (VE) metrics for COVID-19 vaccination in immunocompromised populations, derived from cohort studies and test-negative case-control designs [91] [93]. The following table summarizes the key effectiveness outcomes:
Table 1: COVID-19 Vaccine Effectiveness in Immunocompromised Patients
| Outcome Measure | Vaccine Effectiveness | Certainty of Evidence |
|---|---|---|
| Hospitalization | 33% - 56% (VE 46%, 95% CI 39-52% in cohort study; VE 37%, 95% CI 29-44% in case-control studies) | Moderate |
| Critical Illness | 40% (95% CI 26-51%) | Moderate |
| Mortality | 61% (95% CI 36-77%) | Low |
| ED/Urgent Care Visits | 34% (95% CI 22-45%) | Moderate |
| Outpatient Visits | 40% (95% CI 19-55%) | Moderate |
These data reveal crucial patterns for vaccine developers. First, the moderate level of protection against hospitalization (33-56%) contrasts with the higher effectiveness generally observed in immunocompetent populations, highlighting the need for improved formulations. Second, the marked reduction in critical illness and mortality (40-61%) confirms the biological value of vaccination even in compromised hosts, supporting continued optimization rather than abandonment of the platform. Third, the relatively short follow-up time in these studies (median <2 months) indicates rapidly waning immunity, suggesting that durability represents a key limitation in this population [91].
For influenza and RSV vaccines, the IDSA guidelines strongly recommend age-appropriate vaccination for immunocompromised individuals but note that high-dose or adjuvanted influenza vaccines may provide more robust immune responses [91] [94]. Specifically for influenza, live-attenuated vaccines (e.g., FluMist) are contraindicated in immunocompromised patients and should be avoided in their close contacts [91] [94].
Recommended Vaccination Protocols
Patient Population Definition
The IDSA guidelines specifically define immunocompromised patients as those with impaired immune systems due to either underlying disease or immunosuppressive medications [91]. This includes:
- Hematologic malignancies and solid tumors receiving chemotherapy
- Primary immunodeficiencies
- Autoimmune diseases treated with immunosuppressants or biologics
- HIV with severe immunosuppression (CD4 <15% or <200/mm³)
- Solid organ transplant (SOT) recipients
- Hematopoietic cell transplantation (HCT) recipients
- CAR-T cell therapy recipients
Notably, patients with chronic organ dysfunction (e.g., end-stage renal disease requiring dialysis, cirrhosis, or end-stage heart disease) were not included in this specific guideline [91]. This precise definition enables researchers to appropriately target enrollment for clinical trials of novel vaccine candidates.
Vaccination Timing and Dosing Protocols
The guidelines emphasize that shared clinical decision-making is essential for optimizing vaccination timing in relation to immunosuppressive therapy schedules, travel, and individual risk factors [93]. The following experimental protocol can guide clinical trials evaluating novel vaccine candidates:
Table 2: Vaccination Protocol for Immunocompromised Populations
| Parameter | Protocol Specification |
|---|---|
| Vaccine Formulation | Use age-appropriate 2025-2026 FDA-approved COVID-19, influenza, and RSV vaccines [91] |
| Administration | Intramuscular injection; coadministration of COVID-19, influenza, and RSV vaccines is appropriate [91] [93] |
| Timing | Administer as soon as possible during respiratory virus season; consider treatment cycles for patients undergoing immunosuppressive therapy [91] |
| Dosing Strategy | Strong recommendation for initial dose; second dose likely extends protection [91] |
| Special Populations | For immunocompromised patients <18 years, RSV administration should be guided by shared decision making [91] |
| Household Contacts | Recommend vaccination of household members and close contacts [91] [93] |
Alternative Vaccine Platforms in Development
Beyond current mRNA vaccines, researchers are investigating alternative platforms to address the limitations in immunocompromised populations. GeoVax's GEO-CM04S1 represents one such approach - a multi-antigen, Modified Vaccinia Ankara (MVA)-based COVID-19 vaccine designed to stimulate both humoral (antibody) and cellular (T-cell) immunity [92]. This broader immune activation may be particularly important for patients who fail to mount adequate antibody responses from current mRNA vaccines [92].
Phase 2 trials of GEO-CM04S1 in immunocompromised patients with chronic lymphocytic leukemia (CLL) and hematopoietic stem cell transplant recipients have demonstrated durable T-cell responses and sustained neutralizing activity across variants [92]. Notably, in the CLL study, the mRNA vaccine arm was halted for not meeting pre-determined continuation criteria, while GEO-CM04S1 exceeded continuation endpoints [92].
Experimental Methodology for Vaccine Assessment
Immune Monitoring Workflow
The following diagram illustrates the comprehensive immune monitoring workflow for assessing vaccine responses in immunocompromised populations:
Research Reagent Solutions
The following reagents and materials are essential for conducting comprehensive vaccine immune response studies in immunocompromised populations:
Table 3: Essential Research Reagents for Vaccine Immunogenicity Studies
| Reagent/Material | Application | Specific Considerations |
|---|---|---|
| ELISA/Electrochemiluminescence | Quantification of antigen-specific antibodies | Focus on anti-spike IgG, neutralizing antibodies; establish seroconversion thresholds [91] |
| Interferon-gamma ELISpot | Detection of antigen-specific T-cell responses | Critical for assessing cellular immunity in patients with B-cell deficiencies [92] |
| Flow Cytometry Panels | Immune phenotyping of lymphocyte populations | Include CD4+, CD8+, Tfh, memory subsets; activation/exhaustion markers [88] |
| MHC Multimers | Antigen-specific T-cell detection | Require HLA typing; identify responses to specific epitopes [7] |
| Neutralization Assays | Functional antibody assessment | Use pseudovirus or live virus systems; test against variants [91] |
| RNA Extraction/Kits | Viral load quantification | Assess vaccine impact on infection severity [91] |
| Cytokine Detection Assays | Inflammatory response profiling | Multiplex panels to characterize innate and adaptive immune activation [88] |
mRNA Vaccine Synergy with Immunotherapy
Emerging evidence suggests mRNA vaccines may enhance responses to cancer immunotherapy, creating important implications for vaccine design. A recent study from MD Anderson Cancer Center demonstrated that cancer patients who received mRNA COVID vaccines within 100 days of starting immunotherapy were twice as likely to be alive three years after treatment compared to unvaccinated patients [88].
The mechanistic pathway for this synergistic effect involves:
This mechanism was validated in multiple cancer cohorts. In advanced non-small cell lung cancer, vaccinated patients (n=180) demonstrated a median survival of 37.33 months compared to 20.6 months in unvaccinated patients (n=704) [88]. Most remarkably, patients with immunologically "cold" tumors (low PD-L1 expression) experienced a nearly five-fold improvement in three-year overall survival following mRNA vaccination [88].
These findings have prompted a randomized Phase III trial to determine if mRNA COVID vaccines should become part of the standard of care for patients receiving immune checkpoint inhibition [88]. For vaccine developers, this represents a paradigm-shifting application of mRNA technology beyond infectious disease prevention into adjuvant cancer therapy.
Future Research Directions
The IDSA guidelines identify critical knowledge gaps that should inform future research priorities for mRNA vaccine development targeting immunocompromised populations:
Correlates of Protection: Establishing immunogenicity thresholds and correlates of protection across diverse immunocompromised subgroups remains a fundamental challenge [93]. Different underlying conditions and treatments create distinct immunological environments that may require customized correlates.
Platform Optimization: Current mRNA vaccines provide incomplete protection, highlighting the need for platform improvements including enhanced delivery systems, improved antigen design, and adjuvant strategies specifically evaluated in immunocompromised hosts [91] [92].
Durability and Waning Immunity: The relatively short duration of protection in immunocompromised patients necessitates research into extended-release formulations, prime-boost strategies, and schedule optimization tailored to specific immunodeficiency types [91].
Combination Immunotherapies: The synergistic effect between mRNA vaccines and checkpoint inhibitors in oncology suggests potential for rational combination approaches that leverage innate immune activation by mRNA platforms to enhance broader immune responses [88].
Personalized Approaches: The demonstrated success of personalized mRNA cancer vaccines targeting individual tumor neoantigens suggests potential application for infectious diseases in immunocompromised hosts, particularly those with suboptimal responses to standard vaccines [78].
These research priorities align with the broader trajectory of mRNA vaccine science, which is expanding from infectious diseases into cancer therapy, autoimmune conditions, and personalized medicine [7] [95]. However, recent funding cuts to mRNA research totaling $500 million through BARDA threaten to slow progress in addressing these critical questions [96] [97]. The scientific community must advocate for sustained investment in mRNA platform optimization to fully realize its potential for protecting vulnerable immunocompromised populations.
Emerging Data on Enhanced Immunotherapy Responses with mRNA Vaccines
Recent groundbreaking research has revealed that mRNA vaccines, initially developed for infectious diseases like COVID-19, demonstrate significant potential to enhance antitumor immunity when combined with cancer immunotherapies. These findings represent a paradigm shift in mRNA vaccine applications, suggesting that their immunostimulatory properties can be leveraged to overcome resistance to immune checkpoint inhibitors (ICIs) in oncology [13] [98]. This application note examines the emerging evidence, underlying mechanisms, and practical methodologies for investigating the synergistic effects of mRNA vaccines and immunotherapy, providing researchers with a framework for exploring this promising therapeutic combination.
Key Clinical Evidence and Quantitative Outcomes
Survival Benefits in Advanced Cancers
Table 1: Overall Survival Improvement with mRNA Vaccination and Immune Checkpoint Inhibition
| Cancer Type | Patient Cohort | Median Survival (No Vaccine) | Median Survival (With Vaccine) | 3-Year Overall Survival (No Vaccine) | 3-Year Overall Survival (With Vaccine) | Hazard Ratio (Adj) |
|---|---|---|---|---|---|---|
| Non-small cell lung cancer (Stage III/IV) | 180 vaccinated vs. 704 unvaccinated | 20.6 months | 37.3 months | 30.8% | 55.7% | 0.51 (95% CI: 0.37-0.71) |
| Metastatic melanoma | 43 vaccinated vs. 167 unvaccinated | 26.67 months | Not reached | 44.1% | 67.6% | 0.37 (95% CI: 0.18-0.74) |
Data compiled from retrospective analysis of patients treated at The University of Texas MD Anderson Cancer Center, showing significant improvement in overall survival when mRNA COVID-19 vaccines were administered within 100 days of initiating immune checkpoint inhibitor therapy [13] [88].
The survival benefit was particularly pronounced in patients with immunologically "cold" tumors characterized by low PD-L1 expression, who typically respond poorly to ICIs alone. These patients experienced a nearly five-fold improvement in three-year overall survival with mRNA vaccine receipt [88]. Importantly, this effect was specific to mRNA vaccines, as patients who received non-mRNA pneumonia or influenza vaccines within the same timeframe showed no detectable survival benefit [13].
Comparative Vaccine Platform Immunogenicity
Table 2: Platform-Specific Immune Profiles and Clinical Implications
| Vaccine Platform | Antigen Kinetics | Innate Immune Activation | T-cell Immunogenicity | Impact of Pre-existing Immunity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| mRNA-LNP | Rapid expression, peaks at 6-24 hours, then declines | Potent type I IFN response, robust antigen presentation and costimulation | Strong CD8+ T-cell activation | Minimal impact from repeated use | Rapid development, flexibility for boosting, potent IFN activation | Transient antigen expression, reactogenicity concerns |
| Adenovirus (Ad5) | Slower onset, sustained expression over days | Moderate innate activation | Strong single-dose T-cell responses | Significantly reduced by pre-existing vector immunity | Single-dose efficacy, durable antigen expression | Limited by seroprevalence, challenging re-administration |
| Protein Subunit | Immediate availability, rapid clearance | Weaker innate immune activation | Primarily antibody responses, weaker T-cell activation | Minimal impact from repeated use | Established safety profile, thermostability | Requires adjuvants, weaker cellular immunity |
Data from comparative studies of vaccine platforms demonstrating the unique immunostimulatory profile of mRNA vaccines that may contribute to enhanced immunotherapy responses [99] [100].
Mechanism of Action: mRNA Vaccine-Mediated Immune Sensitization
Preclinical and clinical investigations have elucidated a multistep mechanism through which mRNA vaccines enhance sensitivity to immune checkpoint blockade:
Figure 1: Mechanism of mRNA Vaccine-Mediated Sensitization to Immunotherapy
Detailed Signaling Pathway
The synergistic effect begins with mRNA vaccine administration via lipid nanoparticles (LNPs), which induces a substantial type I interferon (IFN) surge [13]. This IFN response enables innate immune cells, particularly dendritic cells, to prime CD8+ T cells against tumor-associated antigens through enhanced antigen presentation and costimulation [13] [100]. The activated T cells then infiltrate tumors, prompting an adaptive resistance mechanism wherein tumor cells increase PD-L1 expression as a defense strategy. This PD-L1 upregulation creates an ideal environment for ICIs, which block this inhibitory pathway and unleash the primed T cells to effectively eliminate cancer cells [13] [88] [98].
Experimental Protocols and Methodologies
Preclinical Model Development Protocol
Protocol Title: Evaluating mRNA Vaccine and ICI Synergy in Murine Tumor Models
Materials Required:
- Syngeneic mouse tumor models (e.g., MC38, B16)
- mRNA vaccine (commercial COVID-19 mRNA vaccines or tumor antigen-encoding mRNA)
- Immune checkpoint inhibitors (anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies)
- Flow cytometry reagents for immune profiling
- Equipment for in vivo imaging (if using luciferase-expressing tumors)
Procedure:
- Tumor Implantation: Implant 5×10^5 to 1×10^6 syngeneic tumor cells subcutaneously into the flanks of 6-8 week old mice.
- Vaccination Schedule: Administer mRNA vaccine (1-10μg mRNA content) via intramuscular injection when tumors reach 50-100mm³.
- Checkpoint Inhibition: Administer ICIs (100-200μg per dose) intraperitoneally 1-3 days post-vaccination.
- Immune Monitoring:
- Harvest tumors and lymphoid organs at designated endpoints
- Process tissues for flow cytometry analysis of T cell populations (CD8+, CD4+), activation markers (CD69, CD44), and exhaustion markers (PD-1, TIM-3)
- Analyze myeloid populations (dendritic cells, macrophages) and PD-L1 expression
- Tumor Measurement: Monitor tumor dimensions 2-3 times weekly using calipers.
- Statistical Analysis: Compare tumor growth curves and survival using appropriate statistical tests (log-rank test for survival, repeated measures ANOVA for tumor growth) [13].
Technical Notes: mRNA vaccines can be reconstituted from commercial COVID-19 vaccines or synthesized in-house. For in-house preparation, verify mRNA size, encapsulation efficiency (target >90%), nanoparticle size distribution (target 70-100nm), polydispersity (<0.2), and charge before in vivo administration [13].
Clinical Correlation Study Protocol
Protocol Title: Retrospective Analysis of mRNA Vaccine and ICI Outcomes in Cancer Patients
Data Collection:
- Cohort Identification: Identify patients receiving ICIs for advanced cancers (NSCLC, melanoma) within specified timeframe.
- Exposure Definition: Document mRNA vaccine administration (BNT162b2 or mRNA-1273) within 100 days of ICI initiation.
- Covariable Assessment: Collect data on clinical stage, histology, steroid use, performance status, mutation status, comorbidities, and treatment year.
- Outcome Measures:
- Overall survival (OS) from ICI initiation
- Progression-free survival (PFS)
- Objective response rates
Statistical Analysis:
- Multivariate Analysis: Use Cox proportional hazards regression to control for identified covariables.
- Propensity Score Matching: Address potential confounding factors through matched cohort analysis.
- Sensitivity Analyses:
- Vary vaccination window (50 vs. 100 days)
- Restrict to patients treated during pandemic period
- Account for immortal time bias
- Subgroup Analyses: Evaluate effects in patients with "cold" vs. "hot" tumor microenvironments based on PD-L1 expression [13] [88].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Investigating mRNA Vaccine-Immunotherapy Synergy
| Category | Specific Reagents | Function/Application | Technical Considerations |
|---|---|---|---|
| mRNA Vaccine Platforms | BNT162b2 (Pfizer-BioNTech), mRNA-1273 (Moderna), custom tumor antigen mRNA | Antigen-specific immune activation, innate immune stimulation | Commercial COVID-19 vaccines can be repurposed for proof-of-concept studies; custom mRNA requires LNP encapsulation |
| Lipid Nanoparticles | ALC-0315, ALC-0159, SM-102, DMG-PEG2000 | mRNA delivery and cellular uptake | Size (70-100nm), PDI (<0.2), encapsulation efficiency (>90%) critical for efficacy |
| Immune Checkpoint Inhibitors | Anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies | Blockade of inhibitory immune signals | Multiple dosing schedules should be tested relative to vaccination timing |
| Immune Monitoring Tools | Flow cytometry panels (CD3, CD4, CD8, CD69, PD-1, PD-L1), IFN-α/β ELISpot, cytokine multiplex assays | Characterization of immune responses | Focus on T cell activation markers and myeloid populations in tumor microenvironment |
| Animal Models | Syngeneic tumor models (MC38, B16-F10), genetically engineered models, humanized mouse models | In vivo efficacy evaluation | Select models with appropriate "cold" tumor microenvironment for maximum translational relevance |
Computational and AI Approaches for mRNA Vaccine Optimization
Emerging computational frameworks are accelerating the development of optimized mRNA vaccine formulations for immunotherapy applications. These approaches integrate synthetic transcriptomics with artificial intelligence-driven optimization to guide lipid nanoparticle design and predict immune activation [90]. Key computational strategies include:
AI-Guided Sequence Optimization: Machine learning algorithms predict optimal mRNA sequences for enhanced stability and translation efficiency while minimizing unwanted immunostimulation [86].
In Silico Immune Simulation: Tools like the Universal Immune System Simulator model immune responses to mRNA vaccines, enabling prediction of immunogenicity prior to in vivo testing [90].
LNPs Formulation Optimization: Random Forest regression models trained on simulated LNP parameters can predict immune activation values and identify optimal design parameters (size, charge, PEG content) [90].
These computational methods enable rapid, data-driven optimization of mRNA vaccine delivery systems, significantly shortening development timelines and reducing costs while supporting the creation of more personalized and adaptable cancer immunotherapy strategies [90] [86].
The convergence of evidence from retrospective clinical analyses, preclinical models, and mechanistic studies strongly supports the role of mRNA vaccines as potent immune modulators that can sensitize tumors to checkpoint inhibition. The documented survival benefits across multiple cancer types, particularly in traditionally immunotherapy-resistant "cold" tumors, highlight the transformative potential of this combination approach.
Future research directions should focus on optimizing mRNA vaccine design specifically for immunotherapy applications, identifying ideal timing and sequencing relative to ICI administration, and developing next-generation mRNA constructs that maximize antitumor immunity while minimizing systemic reactogenicity. A multicenter, randomized Phase III trial is currently being designed to validate these findings and determine whether mRNA vaccines should be incorporated into standard care for patients receiving immune checkpoint inhibition [88] [98].
The implications of these findings extend beyond COVID-19 mRNA vaccines, suggesting that strategically designed mRNA platforms could be developed as universal immune-sensitizing agents to expand the population of cancer patients who benefit from immunotherapy.
The regulatory landscape for RNA-based cancer vaccines is undergoing a significant transformation, driven by unprecedented clinical advances and the need to accommodate highly personalized therapeutic platforms. The period from 2024–2025 has marked a pivotal moment in RNA cancer vaccine development, establishing this therapeutic modality as a viable treatment option across multiple cancer types [60]. This evolution in regulatory science is characterized by the development of specialized guidance documents, adaptation of approval pathways for personalized biologics, and strategic planning for anticipated first commercial approvals by 2029 [60]. The foundational knowledge gained from the rigorous evaluation of COVID-19 mRNA vaccines has informed regulatory approaches for cancer applications, with agencies implementing frameworks that address the unique challenges of therapeutic cancer vaccines while maintaining rigorous safety and efficacy standards [60]. This document examines the current regulatory evolution, provides detailed experimental protocols for vaccine characterization, and outlines the critical pathway toward the anticipated first commercial approvals of RNA cancer vaccines.
Current Regulatory Landscape and FDA Guidance
Recent Regulatory Developments and Guidance Documents
The U.S. Food and Drug Administration (FDA) has established specialized regulatory pathways and guidance documents specifically addressing the unique challenges of therapeutic cancer vaccines. In 2024, the FDA released comprehensive guidance titled "Clinical Considerations for Therapeutic Cancer Vaccines," which provides sponsors with detailed recommendations for Investigational New Drug (IND) applications [60]. This guidance addresses critical considerations for both early-phase and late-phase clinical trials specific to cancer vaccine development, establishing standardized frameworks for clinical trial design, endpoint selection, and regulatory submission requirements. The FDA's Center for Biologics Evaluation and Research (CBER) has demonstrated increased readiness for advanced therapy approvals, with eight novel cell and gene therapy approvals in 2024 representing an increase from prior years and signaling the agency's projection of approving 10–20 cell and gene therapies annually by 2025 [60].
The regulatory pathway for RNA cancer vaccines has been accelerated through special designations, including FDA Breakthrough Therapy status and EMA PRIME (PRIority MEdicines) scheme recognition for leading candidates [60]. These designations facilitate more intensive regulatory guidance, rolling review of data, and potential accelerated assessment timelines. The FDA's approach has evolved to address the personalized nature of RNA cancer vaccines, which present unique manufacturing, quality control, and clinical development challenges compared to traditional pharmaceutical products.
International Harmonization Efforts
Global regulatory harmonization efforts have intensified with World Health Organization (WHO) initiatives to standardize mRNA vaccine manufacturing protocols and regulatory requirements internationally [60]. The WHO's mRNA Technology Transfer Programme continues to expand, supporting the development of manufacturing capabilities in low- and middle-income countries while establishing regulatory harmonization frameworks to facilitate global access to approved RNA cancer vaccines. The European Medicines Agency (EMA) has maintained general alignment with FDA approaches while developing EU-specific considerations for RNA therapeutics through its Advanced Therapy Medicinal Products (ATMP) Committee, which provides specialized expertise for novel RNA cancer vaccine evaluations [60].
Table 1: Key Regulatory Guidance Documents and Initiatives for RNA Cancer Vaccines
| Regulatory Body | Guidance/Initiative | Key Focus Areas | Status/Impact |
|---|---|---|---|
| U.S. FDA | "Clinical Considerations for Therapeutic Cancer Vaccines" (2024) | IND requirements, clinical trial design, endpoint selection | Active guidance for sponsors |
| European Medicines Agency | PRIME (PRIority MEdicines) scheme | Accelerated assessment for promising therapies | Multiple RNA vaccines designated |
| World Health Organization | mRNA Technology Transfer Programme | Standardization of manufacturing protocols | Global capacity building |
| FDA CBER | Advanced Therapy Approvals Pathway | Cell and gene therapy regulatory framework | 8 approvals in 2024, increasing capacity |
Anticipated Approval Timeline and Clinical Progress
Projected Regulatory Milestones and First Commercial Approvals
Expert analyses and clinical development trajectories indicate that the first commercial mRNA cancer vaccine could receive regulatory approval by 2029, marking a significant milestone in oncology therapeutics [60]. This projection is supported by the robust clinical development pipeline, with over 60 mRNA cancer vaccine candidates currently undergoing clinical trials and two advanced candidates in Phase III trials as of 2025 [101]. The sustained clinical benefit demonstrated by leading candidates has catalyzed global expansion of Phase III trial programs, with regulatory submissions anticipated starting in 2026 [60].
The regulatory momentum for advanced therapy approvals creates favorable conditions for RNA cancer vaccine approvals as these products advance through Phase III trials. The FDA's demonstrated capacity to evaluate and approve complex biologics, evidenced by the accelerated development and authorization cycles for updated COVID-19 vaccines, provides a regulatory precedent for efficient review of updated vaccine formulations targeting evolving cancer antigens [102] [103]. This established regulatory agility will be crucial as RNA cancer vaccines evolve toward targeting multiple neoantigens and combination regimens with established immunotherapies.
Breakthrough Clinical Evidence Supporting Approval
Unprecedented clinical breakthroughs in 2024–2025 have demonstrated the transformative potential of RNA cancer vaccines across multiple challenging malignancies. The success of mRNA-4157 (V940) in combination with pembrolizumab in melanoma patients has demonstrated significant improvements in efficacy, with a 44% reduction in recurrence risk compared to checkpoint inhibitor monotherapy [60]. Extended follow-up data have shown sustained clinical benefit, with 3-year recurrence-free survival rates maintaining superiority over pembrolizumab monotherapy, reinforcing the long-term therapeutic potential of this approach [60].
Revolutionary advances in pancreatic cancer vaccines represent a particularly significant achievement, addressing one of the most challenging malignancies where only 12% of patients survive five years [60]. The personalized mRNA vaccine developed by Memorial Sloan Kettering Cancer Center in collaboration with BioNTech demonstrated remarkable efficacy in pancreatic ductal adenocarcinoma patients, with vaccine-induced immune responses persisting for nearly four years after treatment and showing a reduced risk of cancer recurrence at three-year follow-up compared to non-responders [60]. Similarly, the development of novel layered nanoparticle delivery systems has achieved unprecedented rapid immune system activation against brain tumors, with University of Florida researchers reporting that their mRNA cancer vaccine successfully reprogrammed the immune system to attack glioblastoma within 48 hours of administration [60].
Table 2: Clinical Trial Progress of Leading RNA Cancer Vaccine Candidates
| Vaccine Platform | Cancer Indication | Trial Phase | Key Efficacy Findings | Estimated Approval Timeline |
|---|---|---|---|---|
| mRNA-4157 (V940) + pembrolizumab | Melanoma | Phase III | 44% reduction in recurrence risk; sustained 3-year RFS benefit | 2026 (regulatory submission) |
| Personalized mRNA vaccine (BioNTech) | Pancreatic ductal adenocarcinoma | Phase II | Immune responses persisting ~4 years; reduced recurrence risk at 3-year follow-up | 2028-2029 |
| Layered nanoparticle mRNA vaccine | Glioblastoma | Phase I/II | Rapid immune activation within 48 hours; conversion of "cold" to "hot" tumors | 2029-2030 |
| saRNA vaccine platform | Multiple solid tumors | Phase I/II | Enhanced potency with lower dosing requirements | 2030+ |
Experimental Protocols for RNA Cancer Vaccine Characterization
Protocol 1: Neoantigen Selection and Vaccine Design
Purpose: To identify and prioritize neoantigens for incorporation into personalized RNA cancer vaccines using artificial intelligence-driven platforms.
Materials and Reagents:
- Tumor tissue samples (fresh frozen or FFPE)
- matched normal DNA sample
- RNA sequencing library preparation kit
- Whole exome sequencing kit
- AI-based neoantigen prediction platform (commercial or in-house)
- HLA typing kit
- In vitro transcription system
- Lipid nanoparticles (LNPs) for formulation
Procedure:
- Tumor and Normal Sequencing: Perform whole-exome sequencing (WES) of tumor and matched normal DNA to identify somatic mutations. Concurrently, conduct RNA sequencing to determine gene expression levels.
- HLA Typing: Determine patient's HLA class I and II alleles using high-resolution HLA typing methods.
- Neoantigen Prediction: Process sequencing data through AI-driven neoantigen prediction platforms that incorporate multi-omics data analysis to identify optimal tumor-specific targets [60]. The algorithm should analyze:
- Somatic mutations (single nucleotide variants, insertions/deletions)
- HLA binding affinity using neural network-based prediction tools
- Tumor-specific gene expression levels
- Clonality of mutations within the tumor
- Likelihood of T-cell receptor recognition
- Neoantigen Prioritization: Generate a ranked list of candidate neoantigens using machine learning algorithms that process whole-exome sequencing data within hours [60]. Prioritize mutations based on:
- Combined HLA binding affinity score (<50nM preferred)
- High tumor expression (FPKM >1)
- Clonal mutation status (high cancer cell fraction)
- Absence in normal tissues
- Vaccine Construct Design: Design mRNA sequences encoding selected neoantigens, incorporating optimized untranslated regions (UTRs) for enhanced ribosome loading and translation efficiency, codon optimization for improved translation efficiency, and adjusted local RNA structures to increase stability and expression fidelity [104].
- Vaccine Manufacturing: Synthesize mRNA vaccine using in vitro transcription and formulate with optimized lipid nanoparticles for delivery.
Protocol 2: Immune Response Monitoring and Vaccine Efficacy Assessment
Purpose: To evaluate the immunogenicity and functional efficacy of RNA cancer vaccines through comprehensive immune monitoring.
Materials and Reagents:
- Peripheral blood mononuclear cells (PBMCs) from vaccinated patients
- ELISpot kits (IFN-γ, Granzyme B)
- Flow cytometry panel antibodies (CD3, CD4, CD8, CD45, activation markers)
- MHC multimers for vaccine-targeted neoantigens
- Cytokine detection multiplex assays
- Target cancer cell lines
- Autologous dendritic cells
Procedure:
- Sample Collection: Collect peripheral blood at baseline and at multiple timepoints post-vaccination (e.g., weeks 2, 4, 8, 12, and 24).
- PBMC Isolation: Isolate PBMCs using density gradient centrifugation and cryopreserve for batch analysis.
- T-cell Response Quantification: a. ELISpot Analysis: Perform IFN-γ and Granzyme B ELISpot assays using pools of neoantigen peptides to quantify antigen-specific T-cell responses. b. Flow Cytometry: Use multiparameter flow cytometry to characterize T-cell phenotypes, activation markers, and memory differentiation. c. MHC Multimer Staining: Employ peptide-MHC multimer staining to precisely quantify neoantigen-specific T-cell populations.
- Functional Assays: a. Cytokine Production: Measure cytokine production (IFN-γ, TNF-α, IL-2) by intracellular staining after neoantigen stimulation. b. Cytolytic Activity: Evaluate cytotoxic potential of vaccine-induced T-cells against autologous dendritic cells loaded with neoantigen peptides or HLA-matched tumor cells.
- Tumor Infiltration Assessment: For accessible tumors, perform immunohistochemistry or genomic analysis of tumor-infiltrating lymphocytes pre- and post-vaccination to evaluate vaccine-induced changes in the tumor microenvironment.
- Clinical Correlation: Correlate immunologic findings with clinical outcomes including recurrence-free survival, overall survival, and radiographic tumor responses.
Visualization of RNA Cancer Vaccine Development Pathway
Diagram 1: RNA Cancer Vaccine Development Pathway from Discovery to Approval
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for RNA Cancer Vaccine Development
| Reagent/Material | Function/Purpose | Key Characteristics | Application Notes |
|---|---|---|---|
| Lipid Nanoparticles (LNPs) | mRNA delivery vehicle | Biocompatible with internal fat layers enabling high mRNA loading; tissue-specific targeting capabilities | Next-generation LNPs achieve rapid immune system reprogramming within 48 hours [60] |
| In Vitro Transcription System | mRNA synthesis | High-yield production of modified nucleoside-containing mRNA | Enables incorporation of pseudouridine to reduce immunogenicity |
| AI-Based Neoantigen Prediction Platforms | Target identification | Multi-omics data analysis; HLA binding prediction; TCR recognition modeling | Processes whole-exome sequencing data within hours to generate ranked neoantigen lists [60] |
| HLA Typing Kits | Patient-specific HLA allele identification | High-resolution typing for class I and II alleles | Essential for personalized vaccine design to match neoantigens to patient HLA |
| Flow Cytometry Panels | Immune monitoring | Multiparameter panels for T-cell phenotyping (activation, memory, exhaustion) | Critical for evaluating vaccine-induced immune responses in clinical trials |
| MHC Multimers | Antigen-specific T-cell detection | Tetramers/dextramers loaded with neoantigen peptides | Enables precise quantification of vaccine-induced T-cell populations |
| Automated Manufacturing Systems | Personalized vaccine production | Closed-system platforms with real-time quality monitoring | Reduces production timelines from 9 weeks to under 4 weeks [60] |
The regulatory evolution for RNA cancer vaccines represents a paradigm shift in oncology drug development, characterized by adaptable frameworks that accommodate highly personalized approaches while maintaining rigorous safety and efficacy standards. With the FDA's development of specialized guidance for therapeutic cancer vaccines and the anticipated first commercial approvals by 2029, the field is poised for transformative growth. The integration of artificial intelligence for neoantigen selection, advances in nanoparticle delivery systems, and innovations in personalized manufacturing are converging to create a robust pipeline of promising candidates. Researchers and developers should align their programs with the evolving regulatory considerations outlined in this document, particularly the emphasis on clinical trial design, manufacturing quality, and comprehensive immune monitoring strategies. As the regulatory pathway becomes increasingly defined, RNA cancer vaccines are positioned to become cornerstone therapeutics in personalized oncology, offering new treatment avenues for cancer patients worldwide.
Conclusion
The field of mRNA vaccine design and development has transitioned from a promising technological platform to a cornerstone of modern immunology and precision medicine. The integration of sophisticated antigen design, advanced LNP delivery systems, and AI-driven optimization has created a powerful, adaptable framework for addressing diverse medical challenges from evolving pathogens to complex cancers. Current clinical successes, particularly in oncology where mRNA vaccines have demonstrated unprecedented survival benefits when combined with immunotherapy, underscore the transformative potential of this technology. Future directions will focus on developing universal vaccines for influenza and COVID-19, enhancing manufacturing efficiency for personalized cancer vaccines, and achieving broader tissue targeting through next-generation delivery systems. As regulatory frameworks evolve to accommodate these advances, mRNA technology is poised to redefine therapeutic strategies across biomedical research and clinical practice, offering new hope for treating some of medicine's most intractable conditions.
References
- 1. Accelerating vaccine development: Plug-and-play ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12266562/]
- 2. Health Technology Assessment of mRNA Vaccines [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568131/]
- 3. Interim Estimates of 2024–2025 COVID-19 Vaccine ... [https://www.cdc.gov/mmwr/volumes/74/wr/mm7406a1.htm]
- 4. SARS-CoV-2 mRNA vaccines sensitize tumours to immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611756/]
- 5. Technological Breakthroughs and Advancements in the ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1524317/abstract]
- 6. The mRNA component of LNP-mRNA vaccines triggers ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1670350/full]
- 7. mRNA Vaccines: Current Applications and Future Directions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572956/]
- 8. Safety and immunogenicity of an optimized self-replicating ... [https://www.nature.com/articles/s41467-025-55843-9]
- 9. Comparison of immunogenicity and protection efficacy of ... [https://pubmed.ncbi.nlm.nih.gov/41031374/]
- 10. Comparison of immunogenicity and protection efficacy of ... [https://www.sciencedirect.com/science/article/pii/S2589004225017596]
- 11. a comprehensive review of mRNA vaccine technology and ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02645-6]
- 12. Advancing mRNA vaccines: A comprehensive review of ... [https://pubmed.ncbi.nlm.nih.gov/40571008/]
- 13. SARS-CoV-2 mRNA vaccines sensitize tumours to immune ... [https://www.nature.com/articles/s41586-025-09655-y]
- 14. Advancing mRNA vaccines: A comprehensive review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025060568]
- 15. CIDRAP Op-Ed: Vaccine effectiveness and safety: What the numbers truly mean in 2025 | CIDRAP [https://www.cidrap.umn.edu/covid-19/cidrap-op-ed-vaccine-effectiveness-and-safety-what-numbers-truly-mean-2025]
- 16. Advancements and challenges in next-generation mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599430/]
- 17. Particles that enhance mRNA delivery could reduce vaccine dosage and costs | MIT News | Massachusetts Institute of Technology [https://news.mit.edu/2025/particles-enhance-mrna-delivery-could-reduce-vaccine-dosage-costs-1107]
- 18. mRNA vaccines for infectious diseases: principles, delivery ... [https://www.nature.com/articles/s41573-021-00283-5]
- 19. Progress and prospects of mRNA-based drugs in pre- ... [https://www.nature.com/articles/s41392-024-02002-z]
- 20. History of COVID-19: Outbreaks and vaccine timeline [https://www.mayoclinic.org/diseases-conditions/history-disease-outbreaks-vaccine-timeline/covid-19]
- 21. The tangled history of mRNA vaccines [https://www.nature.com/articles/d41586-021-02483-w]
- 22. COVID-19 mRNA vaccines: Platforms and current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8856755/]
- 23. mRNA-Based Vaccines and Therapeutics for COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9785933/]
- 24. Innate immune mechanisms of mRNA vaccines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9641982/]
- 25. Vaccine adjuvants: mechanisms and platforms [https://www.nature.com/articles/s41392-023-01557-7]
- 26. Decrypting the Immune Symphony for RNA Vaccines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390541/]
- 27. Vaccine Adjuvants: Putting Innate Immunity to Work - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3420356/]
- 28. Vaccine adjuvants: Tailoring innate recognition to send the ... [https://www.sciencedirect.com/science/article/pii/S1074761324001365]
- 29. Technological breakthroughs and advancements in the ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1524317/full]
- 30. Innate immune responses against mRNA vaccine promote ... [https://www.nature.com/articles/s41467-024-51411-9]
- 31. Principles and practical applications of structure-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9611442/]
- 32. Precision-engineered mRNA vaccines: antigen design ... [https://animaldiseases.biomedcentral.com/articles/10.1186/s44149-025-00186-7]
- 33. Novel Strategies for Developing Next-Generation Vaccines to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474351/]
- 34. The Future of mRNA Platforms: Strategic Pause or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12557348/]
- 35. Stabilization of norovirus GII.3 virus-like particles by ... [https://www.nature.com/articles/s41541-025-01254-2]
- 36. Design Strategies for Novel Lipid Nanoparticle for mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497691/]
- 37. Lipid nanoparticles driving mRNA vaccine innovations [https://www.sciencedirect.com/science/article/abs/pii/S2352940725002057]
- 38. Low-liver-accumulation lipid nanoparticles enhance the ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06924-2]
- 39. Formulation-Driven Optimization of PEG-Lipid Content in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388858/]
- 40. Engineering of mRNA vaccine platform with reduced lipids ... [https://www.nature.com/articles/s41467-025-63965-3]
- 41. Buffer optimization of siRNA-lipid nanoparticles mitigates ... [https://www.nature.com/articles/s41467-025-63651-4]
- 42. mRNA medicine: Recent progresses in chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311907/]
- 43. Synergistic effect of nucleoside modification and ionizable ... [https://www.nature.com/articles/s41541-025-01263-1]
- 44. Position-specific ORF nucleoside-ribose modifications ... [https://www.nature.com/articles/s41467-025-65788-8]
- 45. Loop structure in poly(A) tail of mRNA vaccine enhances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623927/]
- 46. Evaluation of synthetic mRNA with selected UTR ... [https://www.sciencedirect.com/science/article/pii/S2162253125002021]
- 47. The Application of mRNA Technology for Vaccine Production ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031289/]
- 48. Developing mRNA-vaccine technologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3597572/]
- 49. Algorithm for optimized mRNA design improves stability ... [https://www.nature.com/articles/s41586-023-06127-z]
- 50. A quantitative systems pharmacology approach to support ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8674002/]
- 51. Frontiers | A bivalent mRNA against vaccine infection in rodent... RSV [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1542592/full]
- 52. Understanding mRNA and DNA vaccines in veterinary medicine [https://www.dvm360.com/view/understanding-mrna-and-dna-vaccines-in-veterinary-medicine]
- 53. Research progress of mRNA vaccines for infectious diseases [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03060-x]
- 54. The current and future landscape of RNA-based therapies ... [https://www.nature.com/articles/s43856-025-01166-1]
- 55. CircRNA: Unlocking new frontiers in therapeutic and ... [https://pubmed.ncbi.nlm.nih.gov/41109952/]
- 56. Review The advent of clinical self-amplifying RNA vaccines [https://www.sciencedirect.com/science/article/pii/S1525001625002692]
- 57. Durability of next-generation self-replicating RNA vaccine ... [https://www.nature.com/articles/s43856-025-01147-4]
- 58. Trans amplifying mRNA vaccine expressing consensus ... [https://www.nature.com/articles/s41541-025-01166-1]
- 59. New research to investigate next generation 'trans- ... [https://cepi.net/new-research-investigate-next-generation-trans-amplifying-mrna-vaccines]
- 60. Current Progress and Future Perspectives of RNA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12153701/]
- 61. Circular RNA: An Emerging Class of RNA in the Fight Against ... [https://pharmacy.umich.edu/news/circular-rna-an-emerging-class-of-rna-in-the-fight-against-cancer-and-infectious-and-genetic-diseases/]
- 62. Controlling reactogenicity while preserving immunogenicity ... [https://www.nature.com/articles/s41541-025-01135-8]
- 63. Modulating Immunogenicity and Reactogenicity in mRNA- ... [https://pubmed.ncbi.nlm.nih.gov/40700637/]
- 64. Revolutionizing immunization: a comprehensive review of mRNA vaccine technology and applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11900334/]
- 65. Supporting use of thermostable vaccines during public health emergencies: Considerations and recommendations for the future - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8575557/]
- 66. Analysing the In-Use Stability of mRNA-LNP COVID-19 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10675537/]
- 67. Best Practices for Cold Chain Vaccine Storage | solution [https://www.phchd.com/apac/biomedical/service-downloads/evolving-science-for-the-future/cold-chain-vaccine-storage]
- 68. Essential Guide to Safe Vaccine Storage in 2025 [https://praxas.com/en/vaccine-storage-2025/]
- 69. A Thermostable mRNA Vaccine against COVID-19 - PubMed [https://pubmed.ncbi.nlm.nih.gov/32795413/]
- 70. Boosting access to mRNA vaccines through innovative mRNA delivery platform | CEPI [https://cepi.net/boosting-access-mrna-vaccines-through-innovative-mrna-delivery-platform]
- 71. The optimization strategies of LNP-mRNA formulations [https://www.sciencedirect.com/science/article/abs/pii/S1773224724002156]
- 72. Current landscape of mRNA technologies and delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389359/]
- 73. Surface engineering of lipid nanoparticles: targeted nucleic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10951480/]
- 74. Navigating the intricate in-vivo journey of lipid nanoparticles tailored for the targeted delivery of RNA therapeutics: a quality-by-design approach | Journal of Nanobiotechnology | Full Text [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-024-02972-w]
- 75. A versatile antibody capture system drives specific in vivo delivery of mRNA-loaded lipid nanoparticles | Nature Nanotechnology [https://www.nature.com/articles/s41565-025-01954-9]
- 76. Lipid nanoparticles with PEG-variant surface modifications ... [https://www.nature.com/articles/s41467-023-42189-3]
- 77. Protocol for in vitro transfection of mRNA-encapsulated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597280/]
- 78. Personalized mRNA Vaccines Will Revolutionize Cancer ... [https://www.scientificamerican.com/article/personalized-mrna-vaccines-will-revolutionize-cancer-treatment-if-federal/]
- 79. Personalized Cancer Vaccine Market Size to Exceed USD ... [https://www.biospace.com/press-releases/personalized-cancer-vaccine-market-size-to-exceed-usd-8-501-14-million-by-2034]
- 80. Pushing mRNA vaccine development timelines to new ... [https://cepi.net/pushing-mrna-vaccine-development-timelines-new-speeds]
- 81. The Dawn of Personalized DNA Vaccines [https://www.insideprecisionmedicine.com/topics/precision-medicine/the-dawn-of-personalized-dna-vaccines/]
- 82. CDC Vaccine Panel Presentation Distorts Research on Safety of mRNA COVID-19 Vaccines - FactCheck.org [https://www.factcheck.org/2025/11/cdc-vaccine-panel-presentation-distorts-research-on-safety-of-mrna-covid-19-vaccines/]
- 83. Methodological Considerations Regarding the Quantification of DNA Impurities in the COVID-19 mRNA Vaccine Comirnaty® - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11130870/]
- 84. Expression of Concern: König, B.; Kirchner, J.O. Methodological Considerations Regarding the Quantification of DNA Impurities in the COVID-19 mRNA Vaccine Comirnaty®. Methods Protoc. 2024, 7, 41 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12285950/]
- 85. Lipid-free, thermostable mRNA vaccines prepared using ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925005209]
- 86. Considerations for mRNA Product Development, Regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116195/]
- 87. Clinical development of therapeutic mRNA applications [https://www.sciencedirect.com/science/article/pii/S1525001625002084]
- 88. ESMO 2025: mRNA-based COVID vaccines generate ... [https://www.mdanderson.org/newsroom/research-newsroom/-esmo-2025--mrna-based-covid-vaccines-generate-improved-response.h00-159780390.html]
- 89. Research lab publishes breakthrough on mRNA cancer ... [https://ecancer.org/en/news/27124-research-lab-publishes-breakthrough-on-mrna-cancer-vaccines]
- 90. A Computational Framework for Optimizing mRNA Vaccine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1628583/full]
- 91. Seasonal RTI Vaccinations in Immunocompromised Patients [https://www.idsociety.org/Seasonal-RTI-Vaccinations-in-Immunocompromised-Patients/]
- 92. Press Releases [https://www.geovax.com/investors/press-releases/geovax-welcomes-new-idsa-guidance-highlighting-need-for-tailored-covid-19-vaccines-for-immunocompromised-patients]
- 93. IDSA releases COVID vaccine guidance for people with ... [https://www.cidrap.umn.edu/covid-19/idsa-releases-covid-vaccine-guidance-people-weakened-immune-systems]
- 94. IDSA releases RSV and flu vaccine guidelines for people ... [https://www.idsociety.org/news--publications-new/articles/2025/idsa-releases-rsv-and-flu-vaccine-guidelines-for-people-who-are-immunocompromised/]
- 95. World-changing mRNA vaccines [https://www.pennmedicine.org/about/pioneering-the-future-of-medicine/mrna]
- 96. Risks of Cuts to mRNA Vaccine Development | Johns Hopkins [https://publichealth.jhu.edu/2025/risks-of-cuts-to-mrna-vaccine-development]
- 97. HHS Winds Down mRNA Vaccine Development Under ... [https://www.hhs.gov/press-room/hhs-winds-down-mrna-development-under-barda.html]
- 98. Study finds COVID-19 mRNA vaccine sparks immune ... [https://ufhealth.org/news/2025/study-finds-covid-19-mrna-vaccine-sparks-immune-response-to-fight-cancer]
- 99. Comparative analysis of adenovirus, mRNA, and protein ... [https://pubmed.ncbi.nlm.nih.gov/41212056/]
- 100. Comparative analysis of adenovirus, mRNA, and protein ... [https://insight.jci.org/articles/view/198069]
- 101. The Future Of mRNA Cancer Vaccines Looks ... [https://www.biospace.com/press-releases/the-future-of-mrna-cancer-vaccines-looks-commercially-viable]
- 102. COVID-19 Vaccines (2025-2026 Formula) for Use in the ... [https://www.fda.gov/vaccines-blood-biologics/industry-biologics/covid-19-vaccines-2025-2026-formula-use-united-states-beginning-fall-2025]
- 103. FDA Approves and Authorizes Updated mRNA COVID-19 ... [https://www.fda.gov/news-events/press-announcements/fda-approves-and-authorizes-updated-mrna-covid-19-vaccines-better-protect-against-currently]
- 104. mRNA vaccine sequence and structure design and optimization [https://pubmed.ncbi.nlm.nih.gov/39608721/]