Optimizing Viral Cell Culture Cytopathic Effects: A Comprehensive Guide for Enhanced Detection and Yield
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on optimizing cytopathic effect (CPE) analysis in viral cell culture.
Optimizing Viral Cell Culture Cytopathic Effects: A Comprehensive Guide for Enhanced Detection and Yield
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on optimizing cytopathic effect (CPE) analysis in viral cell culture. It covers the foundational principles of CPE, including the structural changes in host cells induced by viral infection and its critical role as a diagnostic tool in virology. The scope extends to advanced methodological applications for improving CPE yield and clarity, systematic troubleshooting for common culture challenges, and the integration of novel validation technologies such as artificial intelligence and comparative assays. By synthesizing established protocols with emerging innovations, this resource aims to enhance the accuracy, efficiency, and reliability of viral culture workflows in both research and therapeutic development.
Understanding Cytopathic Effects: The Hallmark of Viral Infection in Cell Culture
Cytopathic effect (CPE) refers to the structural changes in host cells that are caused by viral invasion. When a virus induces these morphological changes, it is termed cytopathogenic. These changes are a visible manifestation of viral infection at the cellular level and are crucial for virologists in diagnosing and studying viral pathogens [1] [2].
CPEs occur when an infecting virus causes lysis (dissolution) of the host cell or when the cell dies without lysis because it can no longer reproduce [2]. For researchers, observing the type and rate of CPE appearance provides critical information for virus identification and assessing the efficacy of antiviral compounds [1] [3].
Frequently Asked Questions (FAQs) on CPE
Q1: What are the most common types of cytopathic effects observed in cell culture? Common CPE types include rounding of the infected cell, fusion with adjacent cells to form syncytia (large cytoplasmic masses containing many nuclei), and the appearance of nuclear or cytoplasmic inclusion bodies [1] [4]. Other types are total destruction of the cell monolayer, focal degeneration, swelling and clumping, and vacuolization (foamy degeneration) [1].
Q2: Why is assessing CPE important in antiviral drug development? CPE-based assays are vital for directly measuring a compound's ability to inhibit viral replication that leads to cell death. The reduction or prevention of CPE indicates effective antiviral activity. These assays measure viral infectivity directly, are highly reproducible, and are more cost-effective than many alternative methods like RT-qPCR or immunoassays [3].
Q3: Can the type of CPE help identify the virus? Yes, many viruses cause characteristic CPEs that serve as an important diagnostic tool. For example, paramyxoviruses often form syncytia, while adenoviruses cause swelling and clumping of cells. The rate of CPE appearance also helps identify the virus type, distinguishing between rapid and slow viruses [1] [5].
Troubleshooting Common CPE Assay Issues
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| No CPE Observed | Low multiplicity of infection (MOI) | Titrate virus stock to determine optimal MOI [3]. |
| Incorrect incubation temperature/time | Adhere to optimized parameters for specific virus (e.g., 33°C for HCoV-OC43, 37°C for HCoV-NL63) [3]. | |
| High Background/Non-specific Effects | Cell line contamination | Use pure, authenticated cell lines; CPE can test cell line purity [1]. |
| Cytotoxicity of test compound | Include compound-only controls to distinguish antiviral from general cytotoxic effects [3]. | |
| Poor Assay Reproducibility | Inconsistent cell seeding density | Follow standardized seeding protocols (e.g., 2.5x10^4 cells/mL for RD cells in HCoV-OC43 assay) [3]. |
| Variable reading of CPE between operators | Use standardized scoring criteria or automated methods like impedance-based assays [6]. | |
| Inconsistent Staining in CPE Assay | Suboptimal staining conditions | Optimize stain concentration and incubation time; neutral red is a sensitive, inexpensive option [3]. |
Standardized Experimental Protocols
Protocol 1: CPE Inhibition Assay for Human Coronaviruses
This protocol is used for the primary screening of antiviral compounds against common human coronaviruses in a 96-well format [3].
- Cell Seeding: Seed appropriate cell monolayers in a 96-well tissue culture plate. Use the optimized cell line and density for your virus (see Table 2).
- Compound Application: Incubate with serial dilutions of the test compound for a pre-treatment period (e.g., 1-2 hours).
- Virus Inoculation: Infect cells with the virus at a low, pre-optimized MOI. Include virus-only (no compound) and cell-only (no virus) controls on the same plate.
- Incubation: Incubate plates at the optimal temperature and for the duration required for the specific virus to develop CPE (e.g., 4.5 days for HCoV-OC43 at 33°C).
- Viability Staining: Add a viability stain like Neutral Red and incubate.
- Data Acquisition and Analysis: Measure absorbance. The level of CPE inhibition is calculated based on the signal in virus-only controls (100% CPE) and cell-only controls (0% CPE). The half-maximal effective concentration (EC50) of the compound is then determined.
Protocol 2: Plaque Assay for Coronavirus Titration
This protocol is used as a secondary assay to confirm antiviral activity and quantify infectious virus particles [3].
- Cell Seeding: Seed cells in 6-well plates to form confluent monolayers.
- Infection and Adsorption: Inoculate with virus dilutions, allow adsorption for a set time (e.g., 1 hour) with periodic rocking.
- Overlay Addition: Remove the inoculum and cover the cell monolayer with a semi-solid overlay medium (e.g., carboxymethylcellulose). This restricts viral spread to neighboring cells, leading to discrete plaque formation.
- Incubation: Incubate plates for the optimized number of days at the required temperature (see Table 2).
- Plaque Visualization: Remove the overlay, fix the cells, and stain with a crystal violet solution. Plaques appear as clear areas against a background of stained viable cells.
- Plaque Counting: Count the plaques to calculate the plaque-forming units per milliliter (PFU/mL) of the original virus stock.
Quantitative Data for CPE and Plaque Assays
The table below summarizes optimized parameters for CPE and plaque assays with common human coronaviruses, as used in recent research [3].
Table 1: Optimized Assay Conditions for Human Coronaviruses
| Virus | Assay Type | Cell Line | Seeding Density | Incubation Temperature (°C) | Incubation Time (Days) |
|---|---|---|---|---|---|
| HCoV-OC43 | CPE | RD | 2.5x10^4 cells/mL | 33 | 4.5 |
| Plaque | RD | 2.5x10^4 cells/mL | 33 | 4.5 | |
| HCoV-229E | CPE | MRC-5 | 5.0x10^4 cells/mL | 33 | 5.5 |
| Plaque | RD | 2.5x10^4 cells/mL | 33 | 5.5 | |
| HCoV-NL63 | CPE | Vero E6 | 2.0x10^4 cells/mL | 37 | 4 |
| Plaque | Vero E6 | 2.0x10^4 cells/mL | 37 | 4 |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CPE-Based Antiviral Research
| Reagent/Cell Line | Function in CPE Research | Example Use Case |
|---|---|---|
| Vero E6 Cells | Permissive cell line for many viruses, including HCoV-NL63 and SARS-CoV-2. | Used in plaque assays and for virus propagation [3] [6]. |
| RD Cells | Human rhabdomyosarcoma cell line susceptible to HCoV-OC43 and HCoV-229E. | Ideal for both CPE inhibition and plaque assays for certain coronaviruses [3]. |
| MRC-5 Cells | Human fibroblast cell line used for CPE assays with HCoV-229E. | A standard cell line for observing characteristic viral CPE [3]. |
| Neutral Red Stain | Viability dye used in CPE inhibition assays. | Accumulates in live cells; loss of signal indicates virus-induced cell death [3]. |
| Crystal Violet Stain | Histological stain used in plaque assays. | Stains the intact monolayer; plaques appear as clear, unstained zones [3]. |
| Remdesivir | Broad-spectrum antiviral nucleotide analogue; positive control. | Calibrates assays by demonstrating known inhibition of coronavirus CPE [3]. |
| GC-376 | Protease inhibitor active against coronaviruses; positive control. | Used to validate assay performance and as a benchmark for new antivirals [3]. |
Advanced and Emerging Methodologies
Impedance-Based Real-Time CPE Analysis
Modern tools like the xCELLigence Real-Time Cell Analysis (RTCA) system allow for label-free, high-throughput quantification of CPE. This method measures electrical impedance across a cell monolayer—reported as a Cell Index (CI). As healthy cells adhere and grow, the CI increases. When a virus infects the monolayer and induces CPE, cells detach and die, causing a rapid decrease in CI. The time taken for the CI to drop by 50% (tCI50) can be correlated with viral concentration, providing a highly reproducible and quantitative alternative to traditional TCID50 or plaque assays [6].
Digital Holographic Tomography
Emerging optical techniques like Digital Holographic Tomography (DHT) are being investigated for the rapid, label-free detection of virus-induced CPE. This technology enables non-destructive, quantitative phenotyping of cells, potentially reducing the time required to detect viral infection compared to conventional methods [7].
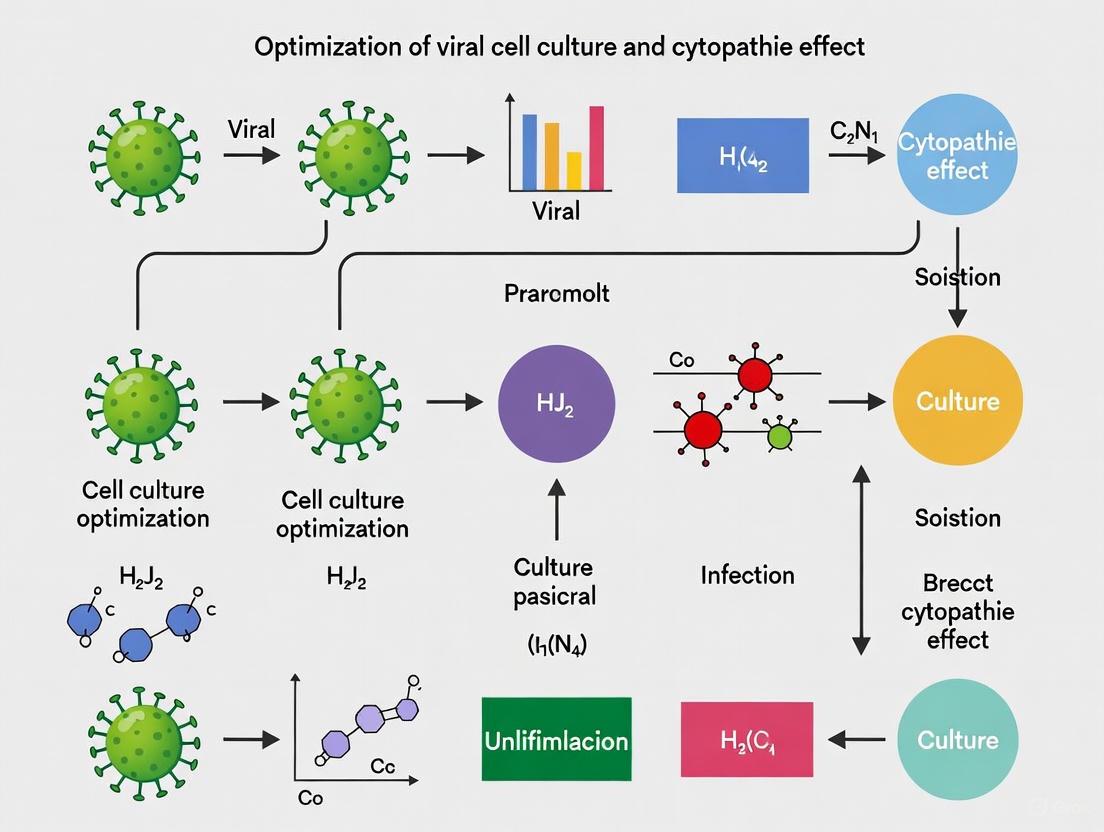
The following diagram illustrates the decision-making process for selecting the appropriate CPE-based assay based on research goals.
Diagram 1: A workflow for selecting the optimal CPE-based assay based on screening needs, throughput, and desired readout.
The Diagnostic Significance of CPE in Virology and Drug Discovery
FAQs: Understanding Cytopathic Effects (CPE) in Viral Research
1. What is a Cytopathic Effect (CPE) and why is it significant in virology? A cytopathic effect (CPE) refers to the structural changes in host cells caused by viral infection and replication. These morphological changes, which can include cell rounding, enlargement, granulation, syncytia formation, and cell lysis, are a primary indicator of viral presence and activity in cell culture [8] [9]. CPE serves as a fundamental diagnostic tool in virology labs for virus isolation, identification, and for assessing the efficacy of antiviral compounds during drug discovery campaigns [9] [10].
2. What are the common types of CPE and which viruses cause them? Different viruses induce characteristic CPE patterns that trained personnel can recognize:
- Cell rounding and detachment: Commonly caused by SARS-CoV-2 in Vero cells [9] and Herpes Simplex Virus (HSV-2) in A549 cells [8].
- Syncytia formation: Multinucleated cells resulting from cell fusion, induced by viruses like Respiratory Syncytial Virus (RSV) and some paramyxoviruses [9].
- Cytoplasmic inclusions: Often associated with Bovine Parainfluenza Virus Type 3 (BPIV3) [9].
- Vacuolation and nuclear alterations: Observed with adenovirus infections [9].
3. How can I troubleshoot unclear or ambiguous CPE in my experiments? Unclear CPE can result from several factors:
- Low viral titer: Ensure adequate multiplicity of infection (MOI) through proper virus titration.
- Cell line suitability: Verify that your cell line is permissive to the virus being studied. For example, MDBK cells are susceptible to bovine viruses while Vero cells support replication of various viruses including SARS-CoV-2 [9].
- Incubation time: Some viruses require extended incubation periods to manifest visible CPE.
- Cellular aging: Morphological changes due to poor cell health can mimic viral CPE [9].
- Confirmation testing: Always confirm viral replication with supplementary tests like PCR or immunoassays, as some CPEs can be ambiguous [9].
4. What advanced methods are available for CPE quantification? Beyond subjective microscopic evaluation, several quantitative approaches exist:
- AI-based image analysis: Systems like AIRVIC use convolutional neural networks to detect and classify CPE in label-free images with high accuracy [9].
- Cell viability staining: Crystal violet staining after viral challenge provides quantitative measurement of cell survival [10].
- High-content screening: Automated imaging systems in 96-well formats enable high-throughput CPE assessment for drug discovery [11].
Troubleshooting Guide: Common CPE Experimental Challenges
Problem: Absent or Minimal CPE Despite Confirmed Infection
Potential Causes and Solutions:
- Insufficient viral infectivity: Repropagate your viral stock and redetermine the TCID50 (50% tissue culture infectious dose) to ensure adequate infectivity [11] [9].
- Suboptimal multiplicity of infection (MOI): Perform an MOI time-course experiment to establish the ideal virus-to-cell ratio for your system [9].
- Incorrect cell confluence: Infect cells at the appropriate density (typically 70-90% confluent) as overcrowded monolayers resist infection [10].
- Cell line passage number: Use low-passage cells as extended passaging can reduce viral susceptibility.
- Inadequate incubation time: Extend the observation period as some viruses, like certain strains of BoGHV-4, require up to 150 hours to manifest CPE [9].
Problem: Excessive CPE Leading to Complete Cell Destruction Too Rapidly
Potential Causes and Solutions:
- Too high MOI: Titrate down the viral inoculum to achieve a more controlled infection progression [9].
- Harvest timing: Monitor CPE progression more frequently and harvest at earlier timepoints [9].
- Alternative cell lines: Test a less permissive cell line to slow CPE development while maintaining viral replication.
Problem: Inconsistent CPE Across Experimental Replicates
Potential Causes and Solutions:
- Cell passage divergence: Use cells within a strict passage range and maintain consistent culture conditions.
- Viral stock stability: Ensure proper aliquoting and storage of viral stocks to prevent titer degradation.
- Infection protocol variability: Standardize media volumes, incubation times, and washing steps across all replicates.
- Contamination check: Implement routine mycoplasma and viral contamination screening [8].
Essential Methodologies for CPE-Based Research
CPE Inhibition Assay for Antiviral Screening
The CPE inhibition assay is a widely used method to evaluate antiviral compound efficacy by measuring their ability to protect cells from virus-induced cytopathology [10].
Detailed Protocol:
- Cell preparation: Harvest A549 cells using trypsin/EDTA, dilute in growth media, and plate in 96-well plates at appropriate density [10].
- Compound treatment: Prepare serial two-fold dilutions of test compounds or interferon standards in a separate plate, then transfer to the cell plate. Include controls (cell-only and virus-only) [10].
- Pre-incubation: Incubate plates for 18-24 hours at 37°C/5% CO₂ to allow compound uptake [10].
- Viral challenge: Add a predetermined dilution of challenge virus (e.g., EMCV for A549 cells) that produces 100% CPE within the assay timeframe. Add media only to cell control wells [10].
- CPE development: Incubate until complete CPE develops in virus controls (typically 40-56 hours) [10].
- Quantification: Remove media, fix remaining cells with formaldehyde or methanol, and stain with crystal violet solution. Destain and measure absorbance at 570nm or perform microscopic examination [10].
- Data analysis: Calculate percentage protection compared to cell controls (100% survival) and virus controls (0% survival) to determine EC₅₀ values [10].
High-Throughput CPE Assay in Human Airway Epithelial (HAE) Models
Advanced 3D tissue models enable more physiologically relevant CPE assessment:
Automated Protocol:
- HAE model preparation: Use human-derived tracheal/bronchial epithelial cells cultured at air-liquid interface (ALI) in 96-well format [11].
- Virus titration: Pre-determine TCID₅₀ for each respiratory virus (Influenza, RSV, SARS-CoV-2) to establish optimal infection conditions [11].
- Automated infection: Implement liquid handling systems for consistent apical infection of HAE tissues [11].
- CPE quantification: Measure infectious virus in apical samples using CPE or virus titer reduction assays in appropriate cell lines [11].
- Quality control: Ensure Z' values >0.75 for robust assay performance in high-throughput screening [11].
Quantitative CPE Data and Analysis
CPE Manifestation Timelines Across Virus-Cell Systems
| Virus | Cell Line | Time to Initial CPE | Key CPE Features | Reference |
|---|---|---|---|---|
| SARS-CoV-2 | Vero | 48 hours | Cell rounding, detachment | [9] |
| BoGHV-4 (MOVAR 33/63) | MDBK | 8-150 hours | Variable by strain | [9] |
| BoAHV-1 | MDBK | 8-72 hours | Nuclear alterations | [9] |
| BAdV-1 | MDBK | 8-76 hours | Vacuolation, inclusions | [9] |
| BPIV3 | MDBK | 8-128 hours | Syncytia, cytoplasmic inclusions | [9] |
AI-Based CPE Detection Performance
| Virus Strain | Cell Line | Detection Accuracy | Notes | Reference |
|---|---|---|---|---|
| BoGHV-4 DN-599 | MDBK | 100% | Highest accuracy | [9] |
| BoGHV-4 MOVAR 33/63 | Vero | 87.99% | Lowest accuracy in study | [9] |
| Multiple bovine viruses | MDBK | 87.61% | Multi-class classification | [9] |
| Multiple bovine viruses | Multiple | 63.44% | Without cell line specification | [9] |
Research Reagent Solutions for CPE Studies
| Reagent/System | Function | Application Example | |
|---|---|---|---|
| A549 Cell Line | Human lung carcinoma cells for interferon and antiviral studies | CPE inhibition assays with EMCV challenge | [10] |
| Vero Cell Line | African green monkey kidney cells for viral isolation | SARS-CoV-2 propagation and CPE analysis | [9] |
| MDBK Cell Line | Bovine kidney cells for veterinary virology | Bovine herpesvirus (BoAHV-1, BoGHV-4) CPE studies | [9] [10] |
| Crystal Violet Staining | Cell viability dye for CPE quantification | Fixed-cell staining after viral challenge | [10] |
| EMCV | Encephalomyocarditis virus for interferon bioassays | CPE induction in A549 cells | [10] |
| VSV | Vesicular stomatitis virus for interferon assays | CPE induction in MDBK or L929 cells | [10] |
Experimental Workflows and Diagnostic Pathways
CPE-Based Antiviral Screening Workflow
CPE Diagnostic Decision Pathway
When a virus infects a permissive cell, it often induces structural changes known as cytopathic effects (CPE) [1] [4]. These morphological changes are a critical visual indicator of viral infection in cell culture and can be characteristic enough to aid in the provisional identification of the virus responsible [12]. Observing CPE involves examining unfixed, unstained cells under the low power of an optical microscope, though some types of CPE require fixation and staining for proper identification [1]. The rate at which CPE appears can also be a diagnostic clue, with "rapid" viruses causing effects in 1-2 days and "slow" viruses taking 4-5 days at a low multiplicity of infection [1].
A Guide to Common CPE Types
The table below summarizes the common visual manifestations of cytopathic effects that you may observe in your cell cultures.
| CPE Type | Key Morphological Changes | Example Viruses |
|---|---|---|
| Cell Rounding | Often the first sign of infection; cells detach and become rounded [1] [4]. | Enteroviruses [1]. |
| Syncytium Formation | Fusion of adjacent infected cells, forming large cytoplasmic masses with multiple nuclei (polykaryons) [1] [4]. | Herpesviruses, some paramyxoviruses [1]. |
| Inclusion Bodies | Abnormal structures within the nucleus or cytoplasm; areas where viral components are synthesized or assembled [1] [4]. | Various, including adenoviruses (intranuclear) and reoviruses (perinuclear) [4]. |
| Total Destruction | Rapid shrinkage, increased density (pyknosis), and complete detachment of the entire cell monolayer [1]. | Enteroviruses [1]. |
| Subtotal Destruction | Partial detachment of the cell monolayer; some cells remain attached [1]. | Some togaviruses, picornaviruses, and paramyxoviruses [1]. |
| Focal Degeneration | Localized areas of infection (foci) where cells become enlarged, rounded, and refractile; spreads via direct cell-to-cell contact [1]. | Herpesviruses, poxviruses [1]. |
| Swelling & Clumping | Significant cell swelling followed by clustering; cells eventually detach [1]. | Adenoviruses [1]. |
| Foamy Degeneration (Vacuolization) | Formation of large or numerous cytoplasmic vacuoles; requires fixation and staining to observe [1]. | Certain retroviruses, paramyxoviruses, and flaviviruses [1]. |
Troubleshooting Common CPE Research Challenges
FAQ: I suspect my cell culture has a viral contaminant, but I see no obvious CPE. What could be happening? Some viral infections are non-cytocidal or cause minimal morphological changes [4]. Furthermore, certain contaminants like non-cell病理 virus and mycoplasma may not cause clear CPE [13]. Mycoplasma, for instance, does not kill cells but can alter cell metabolism, cause chromosomal aberrations, and slow cell growth, potentially compromising your experimental results [13]. In such cases, the presence of virus must be detected using other methods, such as hemadsorption, interference assays, or direct detection of viral antigens or nucleic acids [12] [4].
FAQ: My CPE assay results are inconsistent and not reproducible. What factors should I check? Inconsistency can stem from several sources related to your cell culture health and experimental conditions:
- Cell Line Purity: Cross-contamination between cell lines is a widespread problem [14]. Regularly authenticate your cell lines to ensure you are working with the correct cells.
- Mycoplasma Contamination: As noted above, this common contaminant can affect cell health and metabolism without causing lysis, thereby skewing CPE results [13]. Implement routine mycoplasma testing using methods like DNA staining or PCR [13].
- Multiplicity of Infection (MOI) and Incubation Time: The rate and appearance of CPE are highly dependent on the MOI and the time post-infection [1] [3]. Adhere to optimized protocols specific to your virus and cell line. The table below provides examples of optimized conditions for different human coronaviruses [3].
| Virus | Assay | Cell Line | Incubation Temperature (°C) | Incubation Time (days) |
|---|---|---|---|---|
| HCoV-OC43 | CPE | RD | 33 | 4.5 |
| HCoV-229E | CPE | MRC-5 | 33 | 5.5 |
| HCoV-NL63 | CPE | Vero E6 | 37 | 4 |
FAQ: How can I objectively quantify CPE, especially when it is subtle? Traditional visual scoring of CPE can be subjective. To overcome this, you can use cell viability assays that link CPE to a quantifiable signal. For example, the Neutral red uptake assay is a cost-effective and sensitive method used to assess cell viability in CPE-based antiviral screens [3]. Neutral red is taken up by viable cells; the extent of CPE correlates with a reduction in dye uptake. Alternatively, AI-powered automated systems like AIRVIC are now being developed to detect and classify label-free CPE from microscopy images, providing unbiased infectivity scoring [15].
Essential Protocols for CPE-Based Research
Protocol: Cytopathic Effect (CPE) Inhibition Assay for Antiviral Screening
This protocol is used to evaluate the efficacy of antiviral compounds by measuring their ability to protect cells from virus-induced CPE [3].
Workflow:
- Cell Seeding: Seed an appropriate cell line (e.g., Vero E6, MRC-5) in a 96-well tissue culture plate to form a confluent monolayer [3].
- Compound Addition: Add serial dilutions of the test antiviral compound to the cells and incubate for a suitable period (e.g., 1 hour).
- Virus Infection: Inoculate the cells with a standardized titer of virus. The multiplicity of infection (MOI) must be optimized for the specific virus-cell pair (see troubleshooting table for examples). Include virus-only (no compound) and cell-only (no virus) controls [3].
- Incubation: Incubate the plates at the optimal temperature for the virus (e.g., 33°C or 37°C) until CPE is clearly evident in the virus-only control wells (typically 4-6 days) [3].
- Viability Staining: Remove the medium and add a viability stain like Neutral red (e.g., 0.034% for 2 hours). Alternatively, other tetrazolium-based dyes like MTT can be used.
- Measurement and Analysis: After staining, measure the absorbance. The percentage of CPE inhibition is calculated based on the signal from compound-treated, infected cells relative to the virus-only and cell-only controls [3].
Protocol: Plaque Assay for Virus Quantification
The plaque assay is a fundamental method for determining viral titer (plaque-forming units per mL, PFU/mL) based on the principle that a single infectious virus particle will initiate a infection, leading to a localized area of CPE (a plaque).
Workflow:
- Cell Seeding: Seed a permissive cell line in 6-well plates to form a confluent monolayer [3].
- Virus Infection and Adsorption: Inoculate the cells with serial dilutions of the viral sample. Allow the virus to adsorb for a defined period (e.g., 1 hour) with occasional rocking.
- Overlay Addition: Cover the cell monolayer with a semi-solid overlay medium (e.g., containing agarose or carboxymethylcellulose). This prevents the unrestricted spread of virus in the liquid medium, forcing newly produced virus to infect only adjacent cells, leading to the formation of discrete plaques [3].
- Incubation: Incubate the plates for the required time until plaques become visible (typically several days).
- Plaque Visualization: Often, a second overlay containing a vital dye like Neutral red is added. Live cells take up the dye and appear red, while plaques—areas of dead cells—remain clear and unstained [3].
- Plaque Counting and Titer Calculation: Count the distinct plaques at an appropriate dilution and calculate the viral titer in PFU/mL.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key materials used in CPE-based virology research.
| Reagent / Material | Function in CPE Research |
|---|---|
| Permissive Cell Lines (e.g., Vero, MRC-5, RD) | Host cells that support viral replication and display characteristic CPE [3] [16]. |
| Viral Growth Medium | Often a low-serum maintenance medium optimized for viral replication and CPE development [16]. |
| Neutral Red Dye | A vital stain used in CPE inhibition and plaque assays to quantify cell viability and plaque formation [3]. |
| Agarose / Carboxymethylcellulose | Used to prepare a semi-solid overlay in plaque assays to confine viral spread and allow plaque formation [3]. |
| Positive Control Antivirals (e.g., Remdesivir, GC-376) | Used to calibrate and validate CPE-based antiviral assays, ensuring they are functioning correctly [3]. |
| Optical Microscope | Essential for the daily observation and documentation of morphological changes in cell cultures [1] [13]. |
For researchers in virology and drug development, the cytopathic effect (CPE) is a critical visual indicator of viral infection in cell culture. It refers to the structural changes in host cells caused by viral invasion [1]. Accurately identifying and quantifying these morphological changes is fundamental to research on viral replication cycles, antiviral drug efficacy, and vaccine development. This technical support guide provides troubleshooting and methodologies to optimize your CPE-based research.
FAQs: Troubleshooting Cytopathic Effect Analysis
1. My cell monolayer is showing non-specific detachment, making it hard to distinguish from early CPE. How can I confirm viral infection?
Non-specific detachment can occur due to factors like cell culture age, contamination, or rough handling. To confirm viral infection:
- Run appropriate controls: Always include a mock-infected control culture from the same passage, processed identically to your infected samples. Any detachment in the control indicates a non-viral issue [17].
- Look for characteristic CPE patterns: Non-specific detachment is often random. True CPE typically begins in foci and spreads. Use the table below to identify virus-specific morphological changes.
- Employ secondary confirmation assays: Even with characteristic CPE, confirm infection with a different method, such as:
- Immunostaining: Use a virus-specific antibody to detect viral proteins inside fixed cells [18].
- Molecular methods: Perform RT-PCR or qPCR to detect viral genetic material in the culture supernatant.
- Plaque Assay: Titrate the supernatant on a fresh cell monolayer to quantify infectious viral particles [18].
2. I need to quantify viral infection precisely, but plaque assays are low-throughput and variable. What are my alternatives?
Plaque assays, while a gold standard, can indeed be time-consuming and subject to variability. Consider these high-throughput, quantitative approaches:
- Quantitative Flow Cytometry (qFCM): This method uses fluorescently tagged antibodies against viral proteins (e.g., against IPNV VP2 protein) to quantify the percentage of infected cells and the amount of viral protein per cell. It is repeatable, reproducible, and can be standardized using Molecules of Equivalent Soluble Fluorochrome (MESF) units [18].
- Flow Virometry (FVM): This technique allows for the direct detection and quantification of individual viral particles. It requires a flow cytometer optimized for small particles and proper staining protocols, such as using SYBR Green I or SYBR Gold for nucleic acid staining [19] [20].
3. My flow virometry data has a high background, masking the viral particle signal. How can I improve the signal-to-noise ratio?
A high background is a common challenge in FVM due to the small size of viruses. Here are key optimization steps:
- Optimize staining protocol: A fractional factorial design has shown that adding glutaraldehyde (0.2-0.5% final concentration) during sample fixation can significantly increase the target event count and mean fluorescence intensity while reducing background [19].
- Ultra-filtration: Filter all buffers through a 0.1-µm filter and virus samples through a 0.45-µm filter to remove impurities, crystals, and cellular debris that contribute to background noise [20].
- Instrument tuning: Decrease the flow rate and increase the laser and detector power to enhance the detection of small particles. Use commercially available synthetic micro-beads of various sizes to calibrate your machine [20].
- Automated data analysis: Instead of manual gating, use algorithmic clustering methods like OPTICS (Ordering Points to Identify Cluster Structure), which can work as well as or better than manual gating and identify features difficult to detect manually [19].
Quantitative Data: CPE and Viral Detection Methods
The table below summarizes key characteristics of different methods used to analyze viral infections in cell culture.
Table 1: Comparison of Viral Detection and Quantification Methods
| Method | What It Measures | Key Advantages | Key Limitations | Typical Time to Result |
|---|---|---|---|---|
| CPE Observation | Structural damage to cell monolayer [1] | Simple, inexpensive, provides visual confirmation | Subjective, semi-quantitative, does not differentiate infectious from non-infectious virus | 1-7 days [1] |
| Plaque Assay | Number of infectious viral particles (PFU/mL) | Gold standard for measuring infectivity | Low-throughput, slow, variable, requires susceptible cell line | 3-7 days [18] |
| Flow Virometry (FVM) | Count of individual viral particles [19] [20] | High-throughput, rapid, analyzes native particles | Cannot differentiate infectivity, requires specialized protocol optimization | Minutes to hours |
| Quantitative Flow Cytometry (qFCM) | Percentage of infected cells and viral protein load [18] | High-throughput, quantitative, can study viral protein heterogeneity | Requires specific antibodies, only measures cell-associated infection | A few hours |
Essential Experimental Protocols
Protocol 1: Flow Virometry for Viral Detection in Water Samples
This optimized protocol for detecting T4 bacteriophage can be adapted for other viral surrogates in complex matrices [19].
- Sample Fixation: Fix the sample with glutaraldehyde at a final concentration of 0.2-0.5%.
- Staining: Dilute the sample in Tris-EDTA (TE) buffer. Stain with SYBR Gold at a final dilution of 1 × 10⁻⁴ of the commercial stock.
- Incubation: Incubate the stained sample for 15 minutes in the dark at room temperature.
- Data Acquisition: Analyze the sample on a flow cytometer calibrated for small particles using reduced wide-angle detection for forward scatter and increased laser power.
- Data Analysis: Analyze the data using density-based clustering algorithms like OPTICS for robust particle identification and enumeration.
Protocol 2: Quantitative Flow Cytometry for Viral Protein Measurement
This protocol for quantifying IPNV VP2 protein in infected BF-2 cells is a model for intracellular viral protein detection [18].
- Infection and Harvest: Infect a cell monolayer at a low MOI (e.g., 0.01-0.1). After appropriate incubation, disperse and harvest the cells using PBS and vigorous pipetting.
- Fixation and Permeabilization: Centrifuge cells and fix/permeabilize for 30 min at 4°C with 4% paraformaldehyde and 0.1% saponin in PBS with an RNase inhibitor.
- Staining:
- Centrifuge and wash cells twice with a washing buffer (PBS, 0.2% BSA, 0.1% saponin, RNase inhibitor).
- Incubate with a primary monoclonal antibody against your target viral protein (e.g., anti-IPNV VP2) for 60 min at room temperature.
- Wash twice.
- Incubate with a fluorochrome-conjugated secondary antibody (e.g., FITC-goat anti-mouse) for 45 min at room temperature.
- Data Acquisition and Quantification:
- Wash cells twice and resuspend in sort buffer.
- Acquire data on a flow cytometer.
- Standardize fluorescence data using a MESF (Molecules of Equivalent Soluble Fluorochrome) kit to convert arbitrary fluorescence units into absolute molecular counts.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Viral CPE and Quantification Experiments
| Reagent | Function/Application | Example & Notes |
|---|---|---|
| Cell Lines | Susceptible host for viral propagation and CPE observation. | BF-2 cells for IPNV [18]; specific cell lines are required for different viruses. |
| Virus-Specific Antibodies | Detection and quantification of viral proteins via immunofluorescence (e.g., qFCM) [18]. | Anti-IPNV VP2 monoclonal antibody; critical for specific detection. |
| Nucleic Acid Stains | Staining viral genomes for direct particle counting via Flow Virometry [19] [20]. | SYBR Gold, SYBR Green I; used for protocols like T4 bacteriophage detection. |
| Fixatives/Permeabilizers | Preserve cell structure and allow antibody entry for intracellular staining. | Paraformaldehyde (fixative) and Saponin (permeabilizer) used in qFCM protocols [18]. |
| Fluorochrome Conjugates | Tag antibodies for detection in flow-based assays. | FITC-conjugated secondary antibodies; other fluorophores can be used depending on instrument lasers [18]. |
| Quantitative Standards | Calibrate fluorescence intensity for absolute quantification in qFCM. | MESF (Molecules of Equivalent Soluble Fluorochrome) beads [18]. |
| Glutaraldehyde | Fixative that enhances fluorescence signal and reduces background in Flow Virometry [19]. | Used at 0.2-0.5% final concentration in FVM protocols. |
Frequently Asked Questions (FAQs)
FAQ 1: What is Multiplicity of Infection (MOI) and how do I calculate it for my experiment?
The Multiplicity of Infection (MOI) is the ratio of infectious viral particles to the number of target cells present in a defined space, such as a cell culture well [21] [22]. It is a critical parameter for ensuring efficient infection. The basic formula is:
MOI = (Number of Viral Particles) / (Number of Target Cells) [21].
To calculate the volume of virus stock needed, you can use the formula:
Virus Volume (ml) = (MOI × Total Cell Number) / Virus Titer (IU/ml) [21].
Example Calculation: If you want to achieve an MOI of 10, your virus titer is 1 x 10⁶ IU/ml, and you have 1 x 10⁵ cells, you would need (10 × 1 × 10⁵) / (1 × 10⁶) = 1.0 ml of virus [21].
FAQ 2: Why does my experiment show low CPE despite using a theoretically sufficient MOI?
Low CPE at a sufficient calculated MOI can stem from several factors:
- Viral Tropism: The virus may not efficiently enter your specific host cell type. Viral tropism is largely determined by the interaction between the viral attachment proteins (e.g., coronavirus Spike protein) and specific host cell receptors (e.g., ACE2 for SARS-CoV-2) [23] [24]. If the receptor is absent or expressed at low levels, infection will be inefficient.
- Host Cell Permissivity: The cell must not only allow virus entry but also support intracellular viral replication. This depends on the cell's metabolic state (dividing vs. non-dividing), the presence of essential host factors (e.g., cellular proteases like TMPRSS2 for priming coronavirus Spike protein), and intact innate immune pathways [21] [23] [25].
- Inaccurate Virus Titer: The plaque-forming unit (PFU) or infectious unit (IU) titer of your virus stock may be inaccurate, leading to the use of an effectively lower MOI [22].
- Suboptimal Infection Conditions: Factors like incubation temperature, media composition, and the presence of transduction enhancers (e.g., polybrene) can significantly impact infection efficiency [21] [3].
FAQ 3: How can I determine the optimal MOI for a new virus and cell line combination?
The most reliable method is to perform a pilot infection experiment [21].
- Design MOI Conditions: Infect your target cells with a range of MOIs (e.g., 1, 2, 5, 10, 15, 30) using a reporter virus (e.g., GFP-expressing) if possible [21].
- Infect and Incubate: Allow sufficient time for the viral life cycle and transgene expression (e.g., 48-72 hours for lentiviruses) [21].
- Evaluate Infection Efficiency: Quantify the percentage of infected cells (via fluorescence, immunohistochemistry, or CPE scoring) at each MOI.
- Select Optimal MOI: Choose the minimum MOI that results in 100% infection or the desired level of CPE with minimal cytotoxicity [21].
FAQ 4: What are the different types of Cytopathic Effects (CPE) and what do they indicate?
CPE refers to virus-induced structural changes in host cells [26] [27]. Common types include:
- Cell Rounding and Lysis: Cells detach and lyse, often seen with picornaviruses and influenza viruses [25] [26].
- Syncytia Formation: Fusion of infected cells to form multinucleated giant cells, a hallmark of paramyxoviruses and some coronaviruses like SARS-CoV-2 [24] [26].
- Vacuolation and Membrane Rearrangements: Formation of cytoplasmic vacuoles or membrane structures that serve as viral replication factories [26].
- Inclusion Bodies: Discrete areas within the nucleus or cytoplasm where viral components accumulate [26].
- Apoptosis vs. Necrosis: Programmed cell death (apoptosis) or uncontrolled cell death (necrosis) can be triggered as a host defense mechanism or as a direct result of viral replication [25].
Troubleshooting Guides
Problem: High Cytotoxicity at High MOI
- Potential Cause: Excessive viral load can overwhelm cellular machinery, trigger strong innate immune responses, or induce apoptosis [21] [25].
- Solution:
- Titrate the MOI downwards to find the lowest effective dose.
- Harvest viral supernatant or cells earlier in the infection cycle before CPE becomes too advanced.
- Consider using inducible or low-expression vector systems to reduce the metabolic burden on the host cell.
Problem: Inconsistent CPE Across Replicate Wells
- Potential Cause: Inconsistent cell seeding density, uneven distribution of virus in the culture well, or clumping of cells or viral particles [27].
- Solution:
- Ensure a uniform, near-confluent monolayer of healthy cells at the time of infection [27].
- Mix the virus inoculum thoroughly before adding to cells.
- Gently rock the plate after adding the virus to ensure even distribution.
- Use a consistent and accurate method for counting cells and determining virus titer.
Problem: No CPE Observed in a Normally Susceptible Cell Line
- Potential Cause: Loss of viral infectivity due to improper storage or handling, outdated or incorrect virus stock, or use of the wrong cell line [24].
- Solution:
- Re-titer your virus stock to confirm its infectivity.
- Check the identity and passage number of your cell line.
- Ensure that infection conditions (temperature, media, serum) are optimal for your specific virus.
- Include a positive control (e.g., a known permissive cell line) in your experiment.
Quantitative Data Reference
Table 1: Probability of Cell Infection at Different MOI Values
The percentage of cells infected at least once can be calculated using the Poisson distribution [22]. P(n>0) = 1 - e^(-MOI)
| MOI | Percentage of Cells Infected (≥1 virus particle) |
|---|---|
| 0.1 | 9.5% |
| 0.5 | 39.3% |
| 1 | 63.2% |
| 2 | 86.5% |
| 3 | 95.0% |
| 5 | 99.3% |
Table 2: Suggested Lentivirus MOI for Selected Human Cell Lines
This table provides a starting point for MOI optimization with common cell lines [21].
| Cell Line | Description | Suggested MOI |
|---|---|---|
| HeLa | Human Cervical Carcinoma | 3 |
| A549 | Human Lung Carcinoma | 5 |
| HCT116 | Human Colon Carcinoma | 5 |
| MCF7 | Human Breast Adenocarcinoma | 2 |
| Jurkat | Human Acute T Cell Leukemia | 10 |
| U2-OS | Human Bone Osteosarcoma | 5 |
Key Experimental Protocols
Protocol: Cytopathic Effect (CPE) Assay for Antiviral Screening (96-well format) [3]
Purpose: To quantify viral infection and evaluate the efficacy of antiviral compounds by measuring virus-induced cell death.
Materials:
- Cell Line: Permissive for the virus of interest (e.g., Vero E6 for HCoV-NL63).
- Virus: Aliquoted stock with known titer.
- Compounds: Antiviral agents (e.g., Remdesivir as a positive control).
- Neutral Red Stain or other cell viability dyes.
- 96-well tissue culture plates.
- Plate reader or image cytometer.
Method:
- Cell Seeding: Seed cells in 96-well plates at an optimized density to form a confluent monolayer by the next day (e.g., 2.5 x 10⁴ cells/well for RD cells). Incubate overnight [3] [27].
- Compound Treatment: Add serial dilutions of the test and control compounds to the wells.
- Virus Inoculation: Infect cells at a predetermined MOI (e.g., MOI of 0.01-1). Include virus-only (no compound) and cell-only (no virus) controls [3].
- Incubation: Incubate plates at the optimal temperature for the virus (e.g., 33°C or 37°C) for the required time (e.g., 4-6 days) [3].
- Staining and Quantification:
- Add Neutral Red solution to the culture medium and incubate.
- Wash plates to remove unincorporated dye.
- Elute the incorporated dye from viable cells and measure the absorbance at 540 nm.
- Alternatively, use an image cytometer to automatically quantify the loss of cell monolayer confluence, reduction in cell count, or changes in cell morphology [27].
- Data Analysis: Calculate the percentage of CPE inhibition or the 50% effective concentration (EC₅₀) for the test compound.
Signaling Pathways and Workflows
Diagram Title: Viral Tropism and CPE Development Pathway
Diagram Title: CPE Assay Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CPE-based Virology Research
| Item | Function/Benefit |
|---|---|
| Suspension Cell Lines (e.g., MDCK.SUS2) | Allow high-density culture in bioreactors for large-scale virus production [28]. |
| Chemically Defined Media (e.g., Smif8) | Provides consistent, serum-free growth conditions, reducing variability and downstream processing complexity [28]. |
| Transduction Enhancers (e.g., Polybrene, ViralMax) | Increase viral infection efficiency by neutralizing charge repulsions between virions and the cell membrane [21]. |
| Sulfated Cellulose Membrane Adsorbers (SCMA) | Chromatography matrices used for efficient purification of viral particles (e.g., influenza) based on heparin-mimicry pseudo-affinity [28]. |
| Neutral Red Stain | A viability dye incorporated by live cells, used to quantitatively measure virus-induced CPE in assay formats [3]. |
| Image Cytometry Systems (e.g., Celigo) | Automates the imaging and analysis of CPE in microplates, enabling high-throughput, quantitative assessment of cell monolayer destruction, cell count, and morphology [27]. |
| Clarification Filters (e.g., Sartopure PP3) | Used for primary clarification of cell culture broth to remove cell debris before virus purification [28]. |
| Trypsin (TPCK-treated) | Essential for the propagation of influenza and other viruses by cleaving the viral hemagglutinin, enabling multiple cycles of infection [28]. |
Advanced Protocols for Maximizing CPE Yield and Clarity in the Lab
In viral cell culture research, the Multiplicity of Infection (MOI), which defines the ratio of viral particles to target cells, is a critical parameter that directly determines the success of experiments ranging from viral stock production to antiviral drug screening. Optimizing MOI is essential for achieving high infection rates while maintaining cell viability, as an excessively high MOI can trigger rapid cytopathic effects (CPE) and cell death, compromising experimental results. This technical support resource provides comprehensive guidelines and troubleshooting strategies for researchers navigating the complexities of MOI optimization within the broader context of cytopathic effect research.
Core Concepts and Key Definitions
Multiplicity of Infection (MOI) is a quantitative measure expressing the average number of viral particles present per target cell at the time of infection. It is a foundational parameter in virology that predicts the proportion of cells receiving at least one viral particle.
Cytopathic Effect (CPE) refers to the structural changes in host cells resulting from viral infection. These morphological alterations, which include cell rounding, enlargement, granulation, syncytia formation, and eventual cell lysis or detachment, are visual indicators of viral replication and pathogenicity.
Critical Quality Attributes (CQAs) in virally transduced cell cultures include transduction efficiency, cell viability and function, and Vector Copy Number (VCN). These measurable characteristics must be rigorously monitored to ensure product quality, with clinical programs generally maintaining VCN below 5 copies per cell for optimal safety and efficacy [29].
MOI Optimization Guidelines and Data
MOI Selection Based on Research Application
The optimal MOI varies significantly depending on the specific research goals and experimental system. The table below summarizes recommended MOI ranges for different applications:
| Research Application | Recommended MOI Range | Key Considerations | Supporting Data |
|---|---|---|---|
| Antiviral Drug Screening | 0.1 [30] | Balances measurable infection with minimal rapid CPE; allows observation of drug effects | Z' factor > 0.5, indicating excellent assay discrimination [30] |
| Viral Replication Studies | 0.5 [31] | Prevents excessive cell lysis that could obscure compound protective effects | Used for evaluating Rosmarinic acid against EV-A71 [31] |
| CAR-T Cell Manufacturing | Varies (efficiency typically 30-70%) [29] | Requires careful titration to balance efficiency and safety | Lower MOI ranges reduce incidence of high VCN cells [29] |
| Virus Production/Propagation | Higher ranges often used | Aims to infect most cells for maximum viral yield | TCID50 assays used for titer determination [30] |
Cell Type-Specific Susceptibility
Different cell types exhibit varying susceptibility to viral transduction, necessitating MOI adjustments:
- T cells demonstrate high proliferative capacity and become highly amenable to viral transduction upon activation, typically transduced with gamma-retroviral and lentiviral vectors [29].
- Natural Killer (NK) cells present low baseline transduction efficiency due to innate immune properties, often requiring higher viral titers or tropism-engineered vectors [29].
- Macrophages are relatively refractory to standard lentiviral vectors due to the restriction factor SAMHD1, though strategies incorporating the HIV-2 accessory protein Vpx can significantly enhance infection efficiency [32].
- Vero cells (African green monkey kidney cells) are widely used in virology due to deficiency in interferon production, allowing efficient viral replication without this innate immune response [30].
Troubleshooting Common MOI Problems
Low Transduction Efficiency
Problem: Insufficient percentage of cells successfully expressing the transgene.
Potential Causes and Solutions:
- Suboptimal viral titer: Concentrate viral stocks using ultracentrifugation, filter-based ion exchange chromatography, or size exclusion chromatography [33].
- Inadequate virus-cell contact: Use transduction enhancers such as polybrene or commercial alternatives (e.g., ViralEntry). These cationic polymers reduce electrostatic repulsion between negatively charged cell and viral membranes [33].
- Incorrect cell confluency: Target 25-50% confluency for transduction, as over-confluent cells lack sufficient nutrients while under-confluent cells may not survive transduction stress [33].
- Vector-cell mismatch: Select viral vectors with appropriate tropism for your target cells. For AAV vectors, utilize serotype screening kits to identify optimal variants for specific tissue types [33].
Low Target Cell Viability
Problem: Excessive cell death following transduction.
Potential Causes and Solutions:
- Cytotoxicity from high MOI: Decrease the amount of virus added by using smaller volumes or diluting your viral stock [33].
- Unhealthy cells pre-transduction: Ensure cells are contaminant-free (e.g., test for Mycoplasma) and maintain at least 90% viability before transduction. Avoid using over-passaged cells [33].
- Toxic transgene or enhancers: Reduce exposure time by changing growth media 4-24 hours after transduction or use an inducible expression system. Optimize enhancer concentration (e.g., polybrene typically 1-8μg/ml) [33].
- Prolonged viral exposure: Reduce transduction duration to minimize cell stress while maintaining efficiency [29].
Essential Experimental Protocols
Determining Optimal MOI: A Step-by-Step Protocol
This foundational protocol enables empirical determination of optimal MOI for any cell-virus combination.
Materials Required:
- Target cells in culture
- Viral stock with known titer
- Multi-well plates (e.g., 24-well or 96-well format)
- Appropriate cell culture medium
- Transduction enhancer (if applicable)
- Assessment reagents (e.g., fluorescence microscope, flow cytometry, viability assays)
Procedure:
- Cell Seeding: Seed target cells at appropriate density (e.g., 10,000 cells/well for Vero cells in 96-well plates) and culture overnight to reach optimal confluency (typically 25-50%) [30].
- Virus Dilution: Prepare serial dilutions of viral stock to cover a range of MOI values (e.g., 0.1, 0.5, 1, 5, 10).
- Transduction: Replace medium with viral dilutions. Include appropriate controls (untreated cells, vehicle control).
- Incubation: Incubate for determined period (typically 4-24 hours), then replace with fresh medium if needed.
- Assessment: After appropriate expression period (e.g., 48-72 hours), assess transduction efficiency and cell viability.
- Analysis: Calculate optimal MOI as the point that maximizes transduction while maintaining >80% cell viability.
Comprehensive Post-Transduction Analysis
Transduction Efficiency Assessment:
- Flow Cytometry: For fluorescent reporters, quantify percentage of positive cells.
- qPCR/ddPCR: Measure Vector Copy Number (VCN) with droplet digital PCR (ddPCR) as the gold standard for superior precision [29].
- Functional Assays: Measure cytokine secretion upon antigen stimulation or specific functional outputs.
Cell Viability and Function Assessment:
- Viability Staining: Use trypan blue exclusion or more sensitive Annexin V/7-AAD staining analyzed by flow cytometry [29].
- Metabolic Assays: Employ CCK-8 assays to measure metabolic activity [31].
- Membrane Integrity Tests: Quantify lactate dehydrogenase (LDH) release as a marker of cell damage [31].
- Functional Assays: Implement IFN-γ ELISpot assays, cytotoxicity assays measuring target cell lysis, or real-time cytotoxicity measurements using platforms like xCELLigence [29].
Advanced Research Applications
AI-Assisted CPE Detection
Emerging technologies are transforming CPE analysis through artificial intelligence:
- AIRVIC System: An AI-powered platform utilizing convolutional neural networks (ResNet50) trained on 40,369 microscopy images to detect and classify label-free cytopathic effects induced by various viruses [9].
- Performance Metrics: Demonstrated 100% accuracy for BoGHV-4 DN-599 strain in MDBK cells, with multi-class accuracy of 87.61% for bovine viruses in MDBK cells [9].
- Application Potential: Enables unbiased infectivity scoring and facilitates viral isolation and antiviral efficacy testing, representing a significant advancement over subjective visual CPE assessment [9].
High-Throughput Screening Assays
Advanced screening methodologies enable efficient MOI optimization and antiviral testing:
- Dual-Color Fluorescent Assays: Permit simultaneous evaluation of antiviral efficacy and cytotoxicity within a single workflow, streamlining high-throughput compound screening [30].
- Validation Approach: Uses known inhibitors (e.g., cycloheximide) as positive controls and virus-specific antivirals (e.g., acyclovir for HSV) as negative controls to validate assay performance [30].
- Z' Factor Analysis: Statistical measure of assay quality (Z' > 0.5 indicates excellent separation between infected and uninfected controls) [30].
The Scientist's Toolkit: Essential Research Reagents
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Viral Vectors | Lentivirus, AAV, Adenovirus, Retrovirus [33] | Delivery of genetic material into target cells | Varying tropism, immunogenicity, and payload capacity [29] |
| Transduction Enhancers | Polybrene, ViralEntry [33] | Improve viral infectivity by reducing electrostatic repulsion | Cell-type specific toxicity; concentration optimization needed [33] |
| Cell Viability Assays | CCK-8, LDH release, ATP assays [31] | Quantify metabolic activity, membrane integrity, and energy status | Different mechanisms (metabolic vs. membrane damage) [31] |
| Viral Titer Assays | TCID50, Plaque assays [30] | Determine infectious viral particles per volume | Plaque assays more labor-intensive but provide direct quantification [30] |
| Cytokines/Supplements | IL-2, IL-7, IL-15 [29] | Support expansion, survival and function post-transduction | Essential for primary immune cells like T and NK cells [29] |
Pathway: MOI Optimization and CPE Cascade
The following diagram illustrates the relationship between MOI parameters and their downstream effects on cellular outcomes, highlighting key decision points and monitoring parameters in the optimization process.
Frequently Asked Questions (FAQs)
Q1: How do I calculate MOI for my experiment? MOI is calculated using the formula: MOI = (Number of viral particles) / (Number of target cells). This requires accurate determination of viral titer (e.g., by TCID50 or plaque assay) and precise counting of target cells at the time of transduction. For initial experiments, conduct a pilot study with a range of MOI values to determine the optimal ratio for your specific cell-virus system.
Q2: Why does the same MOI give different results across cell types? Different cell types express varying levels of viral receptors and possess intrinsic antiviral defenses. For example, macrophages express SAMHD1 that restricts lentiviral infection, while NK cells have low baseline transduction efficiency due to innate immune properties [29]. Always optimize MOI for each specific cell type rather than assuming cross-system consistency.
Q3: What is an acceptable Vector Copy Number (VCN) for transduced cells? Clinical programs generally maintain VCN below 5 copies per cell for optimal safety and efficacy [29]. Lower MOI ranges typically reduce the incidence of high VCN cells. Monitor VCN using ddPCR for superior precision compared to standard qPCR methods [29].
Q4: How can I improve transduction efficiency in difficult-to-transduce cells? Strategies include: using viral vectors with cell-specific pseudotypes, incorporating transduction enhancers like polybrene, utilizing spinoculation to enhance cell-vector contact, pre-activating cells to upregulate viral receptor expression, and employing engineered vectors (e.g., Vpx-containing lentiviruses for macrophages) [29] [32] [33].
Q5: What are the signs of excessive MOI in my culture? Indicators include rapid decline in cell viability, significant changes in cell morphology, high LDH release indicating membrane damage, reduced metabolic activity (CCK-8 assay), and decreased ATP levels. These signs typically manifest within 24-48 hours post-transduction and necessitate MOI reduction in subsequent experiments [31].
Frequently Asked Questions (FAQs)
Q1: What are the most common reasons my host cells are not achieving optimal confluency?
Several factors related to technique, environment, and culture components can prevent cells from reaching the desired confluency.
- Handling Technique: Insufficient or uneven mixing of the cell inoculum can lead to foam or bubbles, which hinder uniform cell attachment and growth. Static electricity on plastic vessels can also disrupt attachment, especially in low-humidity environments [34].
- Incubation Conditions: Repeatedly opening the incubator causes temperature fluctuations, and how vessels are stacked can create hot or cold spots. Evaporation from media, often due to low humidity in the incubator's water reservoir, can negatively impact growth rates and patterns [34].
- Culture Media and Supplements: Using the wrong media formulation, or media with insufficient quality or incorrect supplementation (e.g., with fetal bovine serum), can fail to support healthy cell proliferation [35] [34].
Q2: How can I quickly troubleshoot a sudden change in cell health or growth rate?
A systematic approach is key to isolating the variable causing the problem.
- Hypothesize: Based on the symptoms (e.g., cell death, slow growth, detachment), list potential causes like contamination, technique error, or media issue.
- Test: Compare your current media with a fresh batch from a different lot or supplier. Simultaneously, check for microbial contamination (e.g., bacteria, fungi, mycoplasma) via microscopy or dedicated detection kits [35] [8].
- Analyze: If the problem persists with new media and contamination is ruled out, closely review your recent techniques and the incubator's environment (e.g., temperature, CO₂ levels, humidity) [34].
Q3: Beyond basic culture, what are advanced methods for optimizing host cells for specific virology applications like CPE research?
Advanced methods move beyond standard maintenance to actively engineer and optimize the cellular environment.
- Media Optimization: Frameworks like Bayesian Optimization can be used to efficiently design custom cell culture media blends. This data-driven approach finds media compositions that maximize specific objectives, such as supporting the viability of primary cells (e.g., PBMCs) or enhancing recombinant protein production, often with far fewer experiments than traditional methods [36].
- Cell Line Engineering: Technologies like multiplexed CRISPR editing allow for simultaneous modifications across multiple genes to optimize cellular performance. This can enhance productivity, stability, and robustness by targeting pathways that improve nutrient uptake or reduce metabolic waste [37].
- Real-Time Monitoring: Integrating Process Analytical Technology (PAT) allows for real-time tracking of key parameters like metabolite levels (glucose, lactate), viable cell density, and dissolved oxygen. This enables dynamic control of the culture environment, maintaining optimal cell health and ensuring process consistency [37].
Troubleshooting Guides
Problem: Poor Cell Attachment and Uneven Growth
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| Spotty, uneven cell attachment | Static electricity on culture vessel | Wipe the outside of the vessel or use an antistatic device; avoid rubbing the vessel against its package [34]. |
| Heavy growth on vessel sides | Insufficient cell inoculum or too little media during feeding | Ensure adequate cell seeding density and use the correct volume of medium for the vessel size [34]. |
| Concentric rings of cell growth | Vibration from incubator fan, foot traffic, or nearby equipment | Place the incubator on a sturdy, level surface away from vibration sources [34]. |
| Overall poor attachment across all vessels | Incorrect or degraded extracellular matrix (ECM) coating | Ensure ECM proteins like laminin, collagen, or fibronectin are used correctly as cell attachment substrates [35]. |
Problem: Slow Growth Rate or Low Viability
| Symptom | Possible Cause | Recommended Action |
|---|---|---|
| Gradual decline in growth rate | Suboptimal culture medium | Test a new batch of media or a different formulation optimized for your specific cell type [34]. |
| Unexplained cell death | Microbial contamination (e.g., mycoplasma) | Perform regular contamination checks using PCR-based detection kits [35]. |
| Cells appear healthy but won't expand | Inaccurate cell counting during passaging or cryopreservation | Calibrate counting methods and ensure cryopreservation is performed at high viability with suitable freeze media [35]. |
| Low viability post-thaw | Incorrect freeze/thaw conditions | Review cryopreservation protocols, including the use of cryoprotectants like DMSO and controlled-rate freezing [35]. |
Quantitative Assessment of Cell Health in CPE Assays
Accurately quantifying cell viability and cytotoxicity is fundamental to measuring viral cytopathic effects. The table below summarizes common assay methods.
| Assay Type | Principle | Readout | Application in CPE Research |
|---|---|---|---|
| Cell Viability (e.g., CellTiter-Glo) | Quantifies ATP from metabolically active cells [38] | Luminescence (higher signal = more viable cells) | Measures the reduction in host cell viability due to viral infection. Antiviral compounds increase the signal [39] [38]. |
| Cytotoxicity (e.g., CellTox Green) | Fluorescent dye binds DNA of dead cells with compromised membranes [38] | Fluorescence (higher signal = more dead cells) | Directly measures virus-induced cell death. Antiviral compounds decrease the fluorescent signal [38]. |
| CPE Inhibition Assay | Visual assessment of cells protected from CPE by antiviral compounds [10] | Microscopy / Crystal Violet Staining | A classic method to confirm antiviral activity by observing the preservation of a cell monolayer after viral challenge [10]. |
Experimental Protocol: Cytopathic Effect (CPE) Inhibition Assay
This protocol outlines a standard method for assessing antiviral compound efficacy by measuring the inhibition of virus-induced cell death, adapted from established screening methods [39] [10].
1. Materials
- Host cells (e.g., Vero E6, A549) [39] [10]
- Virus stock (e.g., SARS-CoV-2, RSV, EMCV) of known titer [38] [10]
- Test compounds and controls
- Cell culture medium and plates (e.g., 96-well or 384-well)
- Fixative (e.g., ethanol) and stain (e.g., crystal violet) or a homogeneous viability/cytotoxicity assay kit (e.g., CellTiter-Glo or CellTox Green) [38] [10]
2. Cell Seeding and Compound Treatment
- Detach and count host cells. Seed them into a multi-well plate at an optimal density (e.g., 3,000-4,000 cells per well for a 384-well plate) [39] [38].
- Prepare serial dilutions of the test compounds in a separate plate.
- Transfer compound dilutions to the cell plate. Include controls: cell control (cells only, no virus, no compound) and virus control (cells + virus, no compound).
- Incubate the plate for a pre-defined period (e.g., 24 hours) at 37°C/5% CO₂ to allow cells to adhere and compounds to take effect [10].
3. Viral Infection
- After incubation, inoculate the cells with a pre-titered volume of virus. The Multiplicity of Infection (MOI) should be optimized; for screening, an MOI of 0.002 to 0.1 is often used [39] [38].
- Return the plate to the incubator for the duration of the assay (typically 48-72 hours) [39] [38].
4. Endpoint Analysis
- Viability/Cytotoxicity Assay: Following the manufacturer's instructions, add reagents like CellTiter-Glo or CellTox Green to the plate. Measure luminescence or fluorescence with a microplate reader [38].
- Visual Staining Method: Aspirate media, fix cells with ethanol, and stain with crystal violet. Visually inspect or quantify the stained monolayer under a microscope [10].
5. Data Analysis
- Normalize data to the controls: 100% protection is defined by the cell control (no virus), and 0% protection is defined by the virus control (virus only).
- Calculate the percentage of CPE inhibition for each compound using the formula:
% CPE Inhibition = [(Sample - Virus Control) / (Cell Control - Virus Control)] * 100 - Compounds showing significant inhibition of CPE (e.g., >50% at a given concentration) are considered hits for further validation [38].
Workflow Visualization
Host Cell Preparation for CPE Research
CPE Inhibition Assay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Host Cell Preparation and CPE Assays |
|---|---|
| Vero E6 Cells | A commonly used mammalian cell line (e.g., from monkey kidney) that is highly permissive to a wide range of viruses, including SARS-CoV-2, making it a standard host for CPE assays [39] [38]. |
| A549 Cells | A human lung carcinoma cell line sensitive to human interferons and used in CPE inhibition assays, often challenged with viruses like EMCV [10]. |
| Cell Culture Media (DMEM, RPMI-1640) | Basal nutrient formulations providing essential components for cell growth and maintenance. Specific blends can be optimized for different cell types and applications [36] [35]. |
| Fetal Bovine Serum (FBS) | A rich source of growth factors, hormones, and lipids that is supplemented into basal media to support robust cell growth and proliferation [35]. |
| Trypsin/EDTA | A protease (trypsin) and chelating agent (EDTA) solution used to dissociate adherent cells from the culture vessel surface for passaging or harvesting [35]. |
| CellTiter-Glo Luminescent Assay | A homogeneous method to determine the number of viable cells in culture based on quantitation of ATP, which signals metabolically active cells [39] [38]. |
| CellTox Green Cytotoxicity Assay | A fluorescent dye that enters cells with compromised membranes and binds to DNA, providing a direct measure of dead cells in a population [38]. |
| Antibiotics (e.g., Penicillin/Streptomycin) | Added to culture media to prevent bacterial contamination, which is critical for maintaining the integrity of long-term CPE experiments [35]. |
Viral transduction is a fundamental technique for introducing foreign DNA into cells using viral vectors, a process essential in gene therapy and advanced biotherapeutic development [40]. The efficiency of this process is often hampered by the electrostatic repulsion between negatively charged viral particles and the target cell membrane [41] [42]. Viral transduction enhancers are specialized reagents designed to overcome this barrier, thereby significantly improving the rate of successful gene delivery [41]. Their strategic use is critical for the optimization of viral cell culture in cytopathic effect research, enabling more reliable and reproducible experimental outcomes. This technical support center provides a comprehensive guide to troubleshooting common issues and optimizing the use of enhancers such as Polybrene and ViralEntry.
FAQs: Resolving Common Experimental Challenges
Q1: Why is my viral transduction efficiency low even when using Polybrene?
Low transduction efficiency with Polybrene can stem from several factors:
- Incorrect Polybrene Concentration: The optimal working concentration for Polybrene typically falls between 3-10 µg/ml, but this is cell-type dependent [40]. Excessive concentrations can be cytotoxic, while insufficient amounts fail to neutralize charge repulsion effectively [41].
- Cell Line Sensitivity: Some cell types, particularly primary cells, stem cells, and immune cells like T lymphocytes, are highly sensitive to Polybrene's toxicity [41] [43]. This cytotoxicity can reduce cell viability and thus lower observable efficiency.
- Suboptimal Viral Titer: The potency of your viral stock is a primary factor. Ensure you are using an appropriate Multiplicity of Infection (MOI) and confirm the functional titer of your virus [44].
- Serum Interference: The type and source of serum in your culture medium can significantly affect transduction efficiency. It is recommended to test different sera during protocol optimization [42].
Q2: What can I use instead of Polybrene for sensitive cell types?
For cell types sensitive to Polybrene, several effective alternatives are available:
- DEAE-Dextran: Scientific studies have shown that DEAE-Dextran can provide superior transduction enhancement for many cell lines and primary cell cultures compared to Polybrene [42].
- Protamine Sulfate: This is a commonly used, less toxic substitute for Polybrene, especially recommended for sensitive cell lines [45].
- Next-Generation Enhancers: Commercial reagents like ViralEntry are specifically formulated to be highly effective and less toxic, capable of boosting transduction by over 10-fold in difficult-to-transduce cells like primary T lymphocytes [43].
- Methodological Changes: Techniques such as spinoculation (centrifugation of virus onto cells) can enhance virus-cell contact and improve efficiency without relying solely on chemical enhancers [41] [40].
Q3: How should I handle and store transduction enhancers to maintain their efficacy?
Proper handling is crucial for reagent performance:
- Polybrene: This reagent is highly sensitive to freeze-thaw cycles. For best results, store stock solutions at -20°C in single-use aliquots and avoid refreezing thawed aliquots [44].
- ViralEntry: The manufacturer recommends storage at 4°C. Storage at -80°C can lead to a slight reduction in infection efficiency, though it will still perform better than no enhancer or Polybrene alone [43].
Troubleshooting Guide: Enhancing Viral Transduction
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Transduction Efficiency | Incorrect enhancer concentration [41]; Low viral titer [44]; Cell type not susceptible [29] | Titrate enhancer concentration [40]; Re-titer virus [44]; Use a tropism-engineered vector [29] |
| High Cell Death Post-Transduction | Cytotoxicity from enhancer [41]; Excessive viral load [29]; Prolonged incubation [29] | Switch to a less toxic enhancer (e.g., ViralEntry, protamine sulfate) [43] [45]; Lower the MOI [29]; Reduce incubation time [29] |
| Inconsistent Results Between Experiments | Improper reagent storage [44]; Variations in serum batch [42]; Virus degradation from freeze-thaw [44] | Use fresh, single-use aliquots [44]; Standardize serum type and batch [42]; Avoid repeated freezing/thawing of virus [44] |
| Poor Transduction in Immune Cells | Innate immune defenses [29]; Low receptor expression [29] | Use high-efficacy enhancers like ViralEntry [43]; Pre-activate cells [29]; Employ spinoculation [40] |
Quantitative Data and Protocol Selection
Comparative Performance of Transduction Enhancers
Table 1: Comparison of Common Viral Transduction Enhancers. This table synthesizes data from product sheets and peer-reviewed studies.
| Enhancer | Typical Working Concentration | Key Advantages | Key Limitations | Ideal Use Case |
|---|---|---|---|---|
| Polybrene | 3 - 10 µg/ml [40] [45] | Widely used, well-understood mechanism [41] | Can be cytotoxic to sensitive cells [41]; Sensitive to freeze-thaw [44] | Robust, established cell lines (e.g., HEK293, HeLa) [40] |
| DEAE-Dextran | ~6 µg/ml [42] | Superior performance to Polybrene in some cell lines [42] | Performance is serum-type dependent [42] | Cell lines and primary cultures where it has been tested [42] |
| Protamine Sulfate | ~10 µg/ml [42] [45] | Less toxic alternative to Polybrene [45] | May be less effective than newer polymers [42] | Polybrene-sensitive cell lines [45] |
| ViralEntry | 1X (from 100X stock) [43] | High efficacy (>10x boost); low toxicity; works on difficult cells [43] | Higher cost than traditional options | Primary cells, T cells, B cells, and other hard-to-transduce cells [43] |
Optimized Experimental Protocols
Standard Protocol for Transducing Adherent Cells with Polybrene
This protocol is adapted from BPS Bioscience for transducing cells like HEK293, CHO, or HeLa [40].
- Day 1: Seed cells at a density of ~150,000 cells per well in a 6-well plate in 2 ml of complete medium. Add the lentivirus and Lenti-Fuse Polybrene Viral Transduction Enhancer to a final concentration of 5 µg/ml. Swirl gently to mix and incubate at 37°C with 5% CO₂ overnight.
- Day 2: Remove the medium containing the virus and replace it with 2 ml of fresh medium. Note: If the virus and polybrene do not adversely affect the cells, the medium change is optional, and the incubation with the virus can be extended to 48-72 hours.
- Day 3-4: 48-72 hours post-transduction, the transduced cells are ready for analysis (e.g., flow cytometry, Western Blot) [40].
Spinoculation Protocol for Suspension Cells
This method, recommended for cells like Jurkat, THP-1, and primary T cells, enhances infection through centrifugation [40].
- Day 1: Harvest cells by centrifugation. Resuspend and count the cells, then dilute them to 5 x 10⁵ cells/ml in fresh medium.
- In a 1.5 ml tube, mix 750 µl of cell suspension with the virus and Polybrene (to a final concentration of 8 µg/ml).
- Incubate the mixture for 20 minutes at room temperature.
- Centrifuge the virus/cells mixture for 30 minutes at 800 x g at 32°C.
- Remove the supernatant and resuspend the cell pellet in 3 ml of fresh medium. Transfer the cells to a 6-well plate.
- Incubate at 37°C with 5% CO₂ for 48-72 hours before analysis [40].
Visualizing the Workflow: From Problem to Solution
The following diagram outlines a logical decision-making process for troubleshooting and optimizing your viral transduction experiments.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key research reagents and materials for viral transduction experiments.
| Item | Function/Description | Example Use Case |
|---|---|---|
| Polybrene | A cationic polymer that neutralizes charge repulsion between cells and viral particles [41] [40]. | General transduction of robust, adherent cell lines [40]. |
| ViralEntry | A next-generation, high-efficiency transduction enhancer with low cytotoxicity [43]. | Transduction of difficult primary cells (T cells, B cells) [43]. |
| Protamine Sulfate | A cationic agent used as a less toxic alternative to Polybrene [45]. | Transduction of cell lines sensitive to Polybrene [45]. |
| DEAE-Dextran | A polycation that can provide superior transduction enhancement for some systems [42]. | An alternative to Polybrene for specific cell lines and primary cultures [42]. |
| Puromycin | A selection antibiotic for cells transduced with vectors containing a puromycin resistance gene [45]. | Selecting stably transduced cell populations post-transduction [45]. |
| Fibronectin | A recombinant protein that can enhance transduction, often used with sensitive hematopoietic cells [44]. | Improving transduction in cells highly sensitive to chemical enhancers [44]. |
In the field of viral cell culture and gene therapy, selecting the appropriate viral vector is a fundamental decision that directly impacts the success and validity of research outcomes. The optimization of studies, particularly those investigating cytopathic effects, hinges on a deep understanding of vector characteristics. This technical support center provides a comparative guide and troubleshooting resource for researchers navigating the complexities of Lentivirus (LV), Adeno-Associated Virus (AAV), and Adenovirus (AdV). By addressing frequently asked questions and common experimental challenges, this guide aims to equip scientists with the knowledge to select the optimal vector for their specific application, ensuring experimental rigor and reproducibility.
Viral Vector Comparison Tables
The following tables summarize the core characteristics, advantages, and disadvantages of each viral vector to inform your selection process.
Table 1: Key Characteristics of Lentivirus, AAV, and Adenovirus
| Feature | Lentivirus (LV) | Adeno-Associated Virus (AAV) | Adenovirus (AdV) |
|---|---|---|---|
| Virus Type | Enveloped, single-stranded RNA [46] [47] | Non-enveloped, single-stranded DNA [48] [47] | Non-enveloped, double-stranded DNA [49] [47] |
| Packaging Capacity | 8-12 kb [46] [47] | ~4.7 kb [48] [46] | Up to ~7-8 kb [49] [47] |
| Integration Profile | Integrates into host genome [46] [50] | Primarily remains episomal [46] [47] | Non-integrating [49] [47] |
| Expression Onset | Slow (requires integration) | Slow | Rapid (1-3 days) [49] |
| Expression Duration | Long-term (stable) [46] [49] | Long-term (stable in non-dividing cells) [47] [50] | Transient [49] [47] |
| Immunogenicity | Moderate | Low [48] [47] | High [49] [47] |
| Tropism | Broad (dividing & non-dividing cells) [49] [47] | Varies by serotype; broad [49] [50] | Very broad [49] |
Table 2: Advantages and Disadvantages at a Glance
| Vector | Primary Advantages | Primary Disadvantages and Risks |
|---|---|---|
| Lentivirus (LV) | Stable, long-term expression; broad tropism; large cargo capacity [46] [49] [47] | Risk of insertional mutagenesis [46] [50]; lower titer than AdV [49] |
| AAV | Low immunogenicity; high safety profile; long-term expression; diverse serotypes for specific targeting [48] [49] [47] | Limited packaging capacity [48] [46]; potential for pre-existing immunity [46] |
| Adenovirus (AdV) | High transduction efficiency; very rapid expression; high titer; infects dividing and non-dividing cells [49] [47] | High immunogenicity [49] [47]; transient expression [49] [47] |
Troubleshooting Guides and FAQs
Low Transduction Efficiency
Problem: The target cells are not being effectively transduced, leading to poor transgene expression.
Solutions:
- Confirm Viral Titer: Low functional titer is a common issue. Concentrate your viral stock via ultracentrifugation to increase the number of infectious particles per volume [44].
- Use Transduction Enhancers: Add cationic reagents like Polybrene (at ~8 µg/mL) to reduce electrostatic repulsion between the viral particle and the cell membrane, which can increase transduction efficiency by up to 10-fold. For primary or sensitive cells, use Fibronectin as a less toxic alternative [44].
- Freeze-Thaw Host Cells: For AAV, a single freeze-thaw cycle of the target cells immediately before transduction has been shown to increase efficiency by approximately 15-fold [44].
- Verify Vector Integrity: Viral vectors can undergo genomic rearrangements during production. Perform a diagnostic restriction enzyme digest on your viral prep and compare it to a known control to ensure the genome is intact [44].
- Check Transgene Size: For AAV, ensure your transgene and regulatory elements do not exceed the ~4.7 kb packaging limit, as this drastically reduces efficiency [48] [46].
Suboptimal Gene Expression
Problem: Transduction is successful, but transgene expression is weak, unstable, or absent.
Solutions:
- Check Expression Timeline: Confirm you are harvesting cells at the correct time post-transduction. Adenovirus expression peaks rapidly (1-3 days), while AAV and Lentivirus require more time for nuclear processing and/or integration, leading to slower expression onset [49] [47].
- Validate Promoter and Elements: Ensure your construct uses a promoter that is active in your specific cell type. The limited capacity of AAV may require the use of smaller, cell-specific promoters.
- Assess Genome Status: For Lentivirus, confirm successful integration into the host genome if long-term expression in dividing cells is required. For AAV, remember that it exists primarily as an episome, which can be diluted in rapidly dividing cells [46] [47].
Managing Immunogenicity and Safety
Problem: Vector-induced immune responses are confounding experimental results, particularly in vivo.
Solutions:
- Vector Selection: For in vivo studies where low immunogenicity is critical, AAV is the preferred choice due to its low pathogenicity and non-integrating nature [48] [47] [50].
- Use Purified Vectors: Impurities like host cell proteins can trigger immune responses. Purify viral stocks using methods like ultracentrifugation or affinity chromatography to remove empty capsids and cellular debris [51] [52].
- Employ Safety-Modified Vectors: Use third-generation lentiviral packaging systems, which split the viral genome across multiple plasmids, to reduce the risk of generating replication-competent viruses and improve safety [46] [47].
Experimental Selection and Workflow
The following diagram outlines a logical workflow for selecting the most appropriate viral vector based on key experimental parameters, framing the decision-making process within the context of research optimization.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Viral Vector Production and Transduction
| Reagent | Function | Key Considerations |
|---|---|---|
| Polybrene | Cationic polymer that neutralizes charge repulsion between viral particles and cell membranes, enhancing transduction efficiency [44]. | Can be toxic to sensitive or primary cells. Store in single-use aliquots to avoid freeze-thaw degradation [44]. |
| Fibronectin | Recombinant protein used as a less toxic alternative to Polybrene for enhancing transduction, particularly in hematopoietic and primary cells [44]. | Can increase transduction efficiency by about 1.5-fold [44]. |
| VSV-G Envelope | Glycoprotein from the Vesicular Stomatitis Virus used to pseudotype Lentivirus, granting it a very broad tropism [47] [50]. | A standard choice for enabling Lentivirus to infect a wide range of cell types. |
| HEK293 Cell Line | A standard producer cell line used in the clinical manufacture of AAV, Adenovirus, and Lentivirus [52]. | Ensure the cell line history is known and it has been properly tested for purity and viral safety for cGMP compliance [52]. |
| Ultracentrifugation | A key method for concentrating viral stocks and purifying viral particles from impurities and empty capsids [44] [51] [52]. | Critical for achieving high-titer stocks. Remove packaging cell debris by filtration (0.45 µm) before centrifugation [44]. |
| LentiBOOST / AdenoBOOST | Proprietary transduction enhancer solutions designed to improve the efficiency of lentiviral and adenoviral transduction in various cell types [47]. | A commercial solution for overcoming low efficiency in hard-to-transduce cells. |
Troubleshooting Guides
My cells are not growing or are growing slowly.
| Possible Cause | Recommended Solution |
|---|---|
| Incorrect growth medium | Use the pre-warmed growth medium recommended by the cell supplier for your specific cell type [53] [54]. |
| Poor quality serum | Test serum from a different lot to ensure it supports growth [53]. |
| High passage number | Use healthy, low-passage number cells [53]. |
| Culture overconfluence | Passage cells when they are in the log-phase growth stage, before they reach confluency [53]. |
| Mycoplasma contamination | Discard contaminated cultures and obtain new cell stocks. Use fresh media and reagents [53] [54]. |
| Incorrect osmotic pressure | Check the osmolality of the complete medium. Most mammalian cells tolerate 260 to 350 mOsm/kg [53]. |
| Exhausted medium supplements | Replace medium or supplement with growth-promoting components like GlutaMAX to prevent glutamine exhaustion [53]. |
| Incorrect cell seeding density | Plate thawed cells at the highest density recommended by the supplier to optimize recovery. In assays, ensure cells remain in the growth phase and do not become over-confluent [53] [55]. |
My cell culture media changes color rapidly, indicating a pH shift.
| Possible Cause | Recommended Solution |
|---|---|
| Incorrect CO₂ tension | Adjust the percentage of CO₂ in the incubator based on the sodium bicarbonate concentration in your medium [53] [56]. |
| Overly tight flask caps | Loosen tissue culture flask caps by a quarter-turn to allow for gas exchange [53]. |
| Insufficient buffering | Add HEPES buffer to a final concentration of 10–25 mM for additional pH stabilization [53]. |
| Incorrect salt base | Use an Earle's salts-based medium in a CO₂ environment and a Hanks' salts-based medium in atmospheric conditions [53]. |
| Bacterial, yeast, or fungal contamination | Discard the culture and medium. Attempt to decontaminate if the culture is irreplaceable [53]. |
My adherent cells are not attaching to the culture vessel.
| Possible Cause | Recommended Solution |
|---|---|
| Unsuitable cultureware | Check that you are not using dishes designed for suspension culture, which have hydrophobic surfaces [54]. |
| Lack of required coating | Coat dishes with poly-L-lysine, collagen, or fibronectin to improve adherence for certain cell lines [54]. |
| Over-trypsinization | Reduce trypsinization time or use less trypsin. Mycoplasma contamination can also cause detachment issues [53]. |
| Presence of attachment inhibitors | Check the medium for necessary attachment factors [53]. |
I suspect my culture is contaminated with mycoplasma or virus.
| Possible Cause | Recommended Solution |
|---|---|
| Suboptimal aseptic technique | Examine and optimize sterile procedures. Always work in a dedicated cell culture hood with appropriate PPE [54]. |
| Infected cell stock | Perform microbiological testing on working and master stocks to validate they are contamination-free [54]. |
| Reliance on antibiotics | Limit routine antibiotic use, as they can mask low-level infections. Consider maintaining one antibiotic-free culture for monitoring [54]. |
| Contaminated reagents | Use sterile tips, pipettes, and autoclaved tools. Regularly clean and decontaminate the working area [54]. |
FAQs
How do I match my CO₂ incubator setting to my culture medium?
The required CO₂ concentration is determined by the sodium bicarbonate (NaHCO₃) concentration in your medium to maintain a physiological pH of 7.2–7.4 [56]. The table below provides general guidance.
| Sodium Bicarbonate (NaHCO₃) Concentration | Recommended CO₂ Setting |
|---|---|
| < 1.5 g/L | 4% CO₂ |
| 1.5 – 2.2 g/L (e.g., EMEM + Earle's Salts) | 5% CO₂ [53] [56] |
| 2.2 – 3.4 g/L | 7% CO₂ |
| > 3.5 g/L (e.g., DMEM) | 10% CO₂ [56] |
Note: While DMEM (with 3.7 g/L NaHCO₃) is often used in 5% CO₂, this results in a slightly alkaline pH (≈7.5). Actively growing cells often correct this through metabolic activity, but low-density or slow-growing cultures may require a higher CO₂ setting (e.g., 7.5–10%) to maintain optimal pH [56].
Why is experimental reproducibility a problem in viral cytopathic effect (CPE) and drug testing assays?
A major cause is uncontrolled changes in the cellular metabolic environment during the assay [55]. Key factors include:
- Nutrient Depletion: Glucose and glutamine can be rapidly consumed, leading to metabolite scarcity [55].
- Waste Accumulation: Lactate and ammonia can build up to inhibitory or toxic levels, altering cell physiology and pH [55].
- Variable Cell Density: Differences in seeding density can lead to inconsistent nutrient consumption, waste production, and contact inhibition [55] [8].
- Viral Contamination: Unidentified viral contaminants like Epstein-Barr virus (EBV) or ovine herpesvirus 2 (OvHV-2) can compromise cell health and introduce unpredictable variables, undermining research integrity and bioprocess safety [8].
What is a metabolically rationalized approach to culture optimization?
This involves designing assay conditions that maintain a stable metabolic environment to ensure robust and reproducible results [55]. The workflow below outlines the optimization process.
How do I adapt cells to serum-free medium (SFM) for viral vector production?
Serum-free media reduce contamination risk, variability, and facilitate downstream purification [57] [58]. Adaptation should be a gradual process:
- Initiate Adaptation: Subculture cells into a 50:50 mixture of original serum-supplemented medium and the target SFM [57].
- Increase SFM Proportion: Once cells exceed a density of 2 × 10⁶ cells/mL with >90% viability, subculture them into a 75:25 mixture of SFM to serum-supplemented medium [57].
- Complete Transition: When cells are growing robustly again, subculture them into 100% SFM [57].
Experimental Protocols
Protocol 1: Enzymatic Dissociation of Adherent Cells
This is a general procedure for subculturing adherent cells using trypsin or similar enzymes [59].
- Aspirate and Discard the spent cell culture media.
- Wash the cell layer with a balanced salt solution without calcium and magnesium (e.g., DPBS) to remove all traces of serum, which contains trypsin inhibitors. Rinse by rocking the flask for 1–2 minutes and discard the solution [59] [57].
- Add Dissociation Solution (e.g., 0.25% Trypsin-EDTA or TrypLE) at 2–3 mL per 25 cm² of surface area. Ensure the solution covers the cell sheet.
- Incubate the flask at 37°C. Rock gently and monitor under a microscope. Cells typically detach in 5–15 minutes. Tap the flask if necessary to expedite removal [59] [57].
- Neutralize Enzymatic Activity: Once cells are detached, add complete growth medium (containing serum) to the flask. Serum inactivates trypsin.
- Collect Cells: Pipette the suspension repeatedly to disperse clumps. Transfer to a conical tube and centrifuge at 100 × g for 5–10 minutes.
- Resuspend and Count: Discard the supernatant. Resuspend the cell pellet in fresh, pre-warmed complete medium. Determine viable cell density and percent viability using an automated cell counter or hemocytometer [59] [57].
- Seed cells into new culture vessels according to your standard protocol.
Protocol 2: Decontamination of Mycoplasma-Infected Cultures
Decontamination is difficult, and discarding cultures is often the best recourse. For irreplaceable cultures, the following procedure using antibiotics can be attempted [53].
- Confirm and Isolate: Determine the contaminant is mycoplasma and immediately isolate the culture from all other cell lines.
- Clean Environment: Thoroughly clean incubators and laminar flow hoods with a laboratory disinfectant.
- Dose-Response Test:
- Dissociate, count, and dilute the contaminated cells in antibiotic-free media.
- Dispense the cell suspension into a multiwell plate.
- Add a range of antibiotic concentrations (e.g., Ciprofloxacin or Plasmocin) to the wells.
- Observe cells daily for signs of toxicity (sloughing, vacuoles, rounding). Determine the lowest concentration that is toxic.
- Treat Culture: Culture the cells for 2–3 passages using the antibiotic at a concentration one- to two-fold lower than the toxic level.
- Test for Eradication: Culture the cells in antibiotic-free medium for 4–6 passages and re-test for mycoplasma to determine if the contamination has been eliminated. Keep the culture quarantined throughout this process [53].
The Scientist's Toolkit: Research Reagent Solutions
| Reagent | Function & Application |
|---|---|
| Trypsin-EDTA | Protease solution for dissociating adherent cells from the culture surface [59] [57]. |
| TrypLE Express Enzyme | Animal-origin-free recombinant enzyme for cell dissociation; a direct substitute for trypsin [59]. |
| Cell Dissociation Buffer | Non-enzymatic, gentle method for dissociating lightly adherent cells or when cell surface proteins must remain intact [59]. |
| Dispase | Protease effective for detaching cells as intact sheets, useful for primary tissue dissociation, often used with collagenase [59]. |
| Collagenase | Enzyme for digesting collagenous components in primary tissues to obtain single-cell suspensions [59]. |
| HEPES Buffer | Chemical buffer added to culture medium (10-25 mM) to maintain stable pH outside a CO₂ incubator or with frequent gas exchange [53]. |
| GlutaMAX Supplement | Dipeptide substitute for L-glutamine; more stable in solution and reduces the formation of toxic ammonia [53]. |
| Poly-L-Lysine | Coating agent applied to culture surfaces to enhance attachment for difficult-to-adhere cell lines [54]. |
| Insulin, Transferrin, Selenium (ITS) | Key components of serum-free media formulations that support cell growth and proliferation in the absence of serum [57]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the typical timeframe for achieving optimal transduction efficiency, and what factors influence it? Optimal transduction efficiency is highly dependent on the specific cell type and viral vector used. In clinical CAR-T cell manufacturing, transduction efficiencies typically range between 30–70% [29]. Achieving this requires careful optimization of several factors:
- Cell Quality: The activation state of the cell is critical. Pre-activating cells, such as T cells via CD3/CD28 stimulation, upregulates viral receptor expression and significantly enhances transduction [29].
- Multiplicity of Infection (MOI): This is the ratio of viral particles to target cells. Careful titration of the MOI is necessary to balance high efficiency with safety, as excessively high MOI can lead to toxicity and increased vector copy number (VCN) [29].
- Incubation Time: The duration of cell-vector contact must be sufficient for transduction to occur. Shorter times may yield low efficiency, while excessively long times can compromise cell viability [29].
- Enhancement Techniques: Methods like spinoculation (centrifugation during transduction) enhance cell-vector contact and can improve outcomes [29]. Some streamlined protocols are now eliminating lengthy spinoculation steps by optimizing other parameters simultaneously [60].
FAQ 2: How does the choice of viral vector determine the expression window of the transgene? The transgene expression window is fundamentally dictated by the viral vector's genome design and its life cycle.
- Lentiviruses (LVs) and Gamma-Retroviruses (γRVs): These vectors provide stable, long-term transgene expression because they integrate into the host cell's genome. This is essential for persistent therapeutic cell populations, such as CAR-T cells [29].
- Adenoviruses (AVs) and Adeno-Associated Viruses (AAVs): These are non-integrating viral platforms, resulting in transient transgene expression. They are suitable for applications requiring short-term genetic modification, such as certain vaccines or transient immunomodulation [29].
FAQ 3: What are the key phases of viral infection in cell culture, and how do they relate to transgene expression and cytopathic effect (CPE)? Adenovirus infection studies provide a clear model of the phased progression, which offers insights for transduction timing. The infection can be divided into distinct periods [61]:
- Early Phase (e.g., 1-24 hours post-infection): This period covers viral attachment, entry, and early gene expression. Host cell gene expression changes are triggered, particularly in immune pathways. Transgene expression begins.
- Late Phase (e.g., after 24 hours post-infection): Commencing with viral DNA replication, this phase involves a dramatic shift to viral late gene expression and a concurrent sharp down-regulation of most host cell genes. Robust transgene expression occurs.
- CPE Onset (e.g., after 36 hours post-infection): Visible CPE, including cell rounding, detachment, and lysis, becomes apparent. The number of down-regulated host genes increases dramatically, leading to cell death and the release of progeny virus. Monitoring is crucial to harvest transduced cells before widespread CPE compromises cell viability and product yield [61].
FAQ 4: How can I monitor transduction success and the onset of CPE without specialized equipment? While quantitative PCR (for VCN) and flow cytometry (for transduction efficiency) are standard, CPE offers a visual indicator.
- Microscopic Observation: CPE encompasses visible morphological changes in the host cells, such as cell rounding, syncytia formation (cell fusion), granulation, and eventual detachment from the culture surface [8] [9].
- AI-Based Tools: Emerging technologies like AIRVIC (AI Recognition of Viral CPE) use convolutional neural networks to automatically detect and classify label-free CPE in cell cultures, providing an unbiased and potentially more sensitive method for monitoring infection progression and health of the culture [9].
Troubleshooting Guides
Problem: Low Transduction Efficiency
- Potential Cause 1: Incorrect cell health or activation state.
- Solution: Ensure cells are healthy and actively proliferating. For primary T cells, use pre-activation with CD3/CD28 beads or similar agonists. Supplement culture with appropriate cytokines (e.g., IL-2 for T cells) [29].
- Potential Cause 2: Suboptimal multiplicity of infection (MOI).
- Solution: Titrate the viral vector to determine the ideal MOI for your specific cell type. Start with a range from low (e.g., 1-5) to high (e.g., 20-50) [29].
- Potential Cause 3: Insufficient cell-vector contact.
Problem: Poor Cell Viability Post-Transduction
- Potential Cause 1: Viral toxicity from an excessively high MOI.
- Solution: Reduce the MOI. High viral loads can stress and kill cells. Re-titrate to find a balance between efficiency and viability [29].
- Potential Cause 2: Overly long transduction duration.
- Solution: Reduce the incubation time with the viral vector. Shorter, optimized periods can minimize stress while still allowing for efficient gene delivery [29].
- Potential Cause 3: Inadequate culture conditions.
- Solution: Supplement the culture medium with survival cytokines like IL-2, IL-7, or IL-15, which are critical for maintaining the health of immune cells like T cells and NK cells post-transduction [29].
Problem: Early or Excessive Cytopathic Effect (CPE)
- Potential Cause 1: Harvesting cells too late in the infection cycle.
- Solution: For vectors that cause CPE (e.g., Adenovirus), establish a detailed time-course experiment. Determine the peak of transgene expression and harvest cells before widespread CPE and cell lysis occur. The late phase of infection, just before significant CPE, is often optimal [61].
- Potential Cause 2: High viral load.
- Solution: If using a high MOI is necessary, closely monitor cells and harvest at an earlier time point. The progression of CPE is dose- and time-dependent [9].
Data Presentation
Table 1: Critical Process Parameters and Their Impact on Transduction Timing
This table summarizes key parameters to optimize for controlling the transduction period and expression window.
| Parameter | Definition | Impact on Timing & Expression | Optimal Range / Consideration |
|---|---|---|---|
| Multiplicity of Infection (MOI) | Ratio of infectious viral particles to target cells. | Higher MOI can accelerate transduction and increase efficiency but may cause toxicity and high VCN [29]. | Must be titrated for each cell type; clinical programs often aim for a VCN below 5 [29]. |
| Transduction Duration | Time cells are exposed to the viral vector. | Insufficient time reduces efficiency; excessive time can lower cell viability [29]. | Varies by vector and cell type; often 8-24 hours. |
| Cell Activation State | The pre-stimulation of target cells before transduction. | Activated cells (e.g., T cells) upregulate viral receptors, drastically improving the rate and efficiency of transduction [29]. | Critical for primary cells; activate 24-48 hours pre-transduction. |
| Vector Selection | Choice of viral vector (e.g., LV, γRV, AV, AAV). | Determines the expression window: integrating vectors (LV, γRV) offer long-term expression; non-integrating (AV, AAV) offer transient expression [29]. | LV for stable expression in dividing/non-dividing cells; AV for high efficiency & transient expression. |
Table 2: Quantitative Data from Viral Infection Time-Course Studies
This table provides example quantitative data from transcriptomic and proteomic studies, illustrating the dynamic changes during viral infection.
| Virus / Cell Line | Phase / Time Post-Infection | Key Observations | Data Type |
|---|---|---|---|
| Adenovirus Type 2 (Ad2) / Human Lung Fibroblasts (IMR-90) | Early Phase (1-12 hpi) | Cellular gene expression changes triggered; genes involved in immune response are highly up-regulated [61]. | Transcriptomics |
| Adenovirus Type 2 (Ad2) / Human Lung Fibroblasts (IMR-90) | Late Phase (after 24 hpi) | Commencement of viral DNA replication; dramatic down-regulation of cellular gene expression; viral late genes expressed [61]. | Transcriptomics |
| Adenovirus Type 2 (Ad2) / Human Lung Fibroblasts (IMR-90) | CPE Onset (after 36 hpi) | Number of down-regulated genes increases dramatically; cell lysis and detachment [61]. | Transcriptomics / Visual |
| SARS-CoV-2 / Vero Cells | 48 hours post-infection | CPE (cell rounding, detachment, lysis) can be observed [9]. | Visual (CPE) |
Experimental Protocols
Protocol 1: Time-Course Experiment for Monitoring Transgene Expression and CPE Onset This protocol helps determine the optimal harvest time by tracking key events over the course of transduction and infection.
- Infect Cells: Seed target cells and infect with your viral vector at a predetermined MOI. Include an uninfected control.
- Time-Point Sampling: At regular intervals post-transduction (e.g., 6h, 12h, 24h, 48h, 72h), harvest samples for analysis.
- Analyze Samples:
- Transduction Efficiency: Use flow cytometry to measure the percentage of cells expressing the transgene (e.g., CAR or GFP reporter) at each time point [29].
- Cell Viability: Perform trypan blue exclusion assays or flow cytometry with Annexin V/7-AAD staining to assess viability [29].
- CPE Monitoring: Visually inspect cultures under a microscope for morphological changes indicative of CPE (cell rounding, syncytia, detachment) [8] [9]. Document with images.
- Data Correlation: Plot transduction efficiency and viability against time. The optimal harvest window is typically when efficiency plateaus at a high level and before viability drops significantly due to CPE.
Protocol 2: Droplet Digital PCR (ddPCR) for Vector Copy Number (VCN) Analysis Controlling VCN is critical for safety and consistent transgene expression. ddPCR is the gold standard for precise VCN quantification [29].
- Genomic DNA (gDNA) Extraction: Harvest transduced cells and isolate high-quality gDNA using a standard kit. Ensure accurate quantification.
- Assay Design: Design and validate specific primer/probe sets for your transgene and a single-copy reference gene within the host genome.
- Droplet Generation and PCR: Mix the gDNA with the assay mix and oil to generate thousands of nanoliter-sized droplets. Perform PCR amplification on the droplet emulsion.
- Droplet Reading and Analysis: Run the amplified droplets in a droplet reader to count the positive and negative droplets for each target.
- VCN Calculation: The VCN is calculated based on the ratio of the transgene concentration to the reference gene concentration. Clinical programs generally maintain VCN below 5 copies per cell [29].
Pathway and Workflow Visualizations
Diagram 1: Strategic Timing in Viral Transduction Workflow
This diagram outlines the key decision points and considerations for timing in a typical transduction experiment.
Diagram 2: Host Cell Response to Viral Transduction
This diagram illustrates the dynamic and often opposing responses of host cell transcription and translation during viral infection, based on 'omics' studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Viral Transduction and CPE Research
| Reagent / Material | Function in Experiment | Example & Notes |
|---|---|---|
| Lentiviral Vectors | Delivery of transgenes for stable, long-term expression. | Often pseudotyped with VSV-G envelope for broad tropism. Use self-inactivating (SIN) designs for enhanced safety [29]. |
| Cell Activation Reagents | Pre-stimulation of target cells to enhance transduction. | Anti-CD3/CD28 beads or antibodies for T cell activation. Critical for upregulating viral receptors [29] [60]. |
| Cytokines | Support cell survival, expansion, and function post-transduction. | IL-2 for T cells; IL-15 for NK cells. Essential for maintaining viability of primary immune cells [29]. |
| Transduction Enhancers | Chemicals or polymers that increase transduction efficiency. | Compounds like Polybrene or protamine sulfate can reduce charge repulsion between viral particles and cell membrane [29]. |
| AI-Based CPE Detection Tool | Automated, label-free classification and detection of cytopathic effects. | Web-based platforms like AIRVIC (AI Recognition of Viral CPE) use convolutional neural networks (e.g., ResNet50) to analyze microscopy images [9]. |
Troubleshooting Low CPE: Solving Common Challenges in Viral Culture
Addressing Low Transgene Expression and Transduction Efficiency
Within the context of viral cell culture and cytopathic effect (CPE) research, achieving high transgene expression and efficient cell transduction is paramount. Low efficiency can obscure experimental results, lead to misinterpretation of viral pathogenicity, and ultimately hinder drug development. This guide provides targeted troubleshooting strategies to overcome these common bottlenecks, ensuring reliable and robust experimental outcomes for researchers and scientists.
Troubleshooting Guide: FAQs and Solutions
FAQ 1: My transgene expression levels are low despite successful transduction. What vector design elements should I check?
Low expression after successful transduction often originates in the vector design itself. Key elements to optimize include:
- Codon Optimization: This process tailors the transgene's genetic code to match the codon usage preferences of the host organism, which can dramatically enhance translation efficiency. One study directly compared codon optimization to other vector modifications and found it generated a more significant improvement in expression levels than even switching to a self-complementary AAV vector design [62].
- Polyadenylation (Poly A) Signal: The poly A signal is critical for mRNA stability and nuclear export. Research in CHO cells has demonstrated that the choice of poly A signal significantly influences stable transgene expression levels. For instance, synthetic (Synt) and SV40 poly A elements were shown to maintain higher long-term expression compared to other common signals like BGH [63].
- Promoter Strength and Specificity: The promoter drives transgene transcription and must be chosen carefully. Testing different promoters (e.g., strong constitutive vs. cell-specific) is essential to find the one that provides adequate expression in your target cells without causing off-target effects [64]. A time-course experiment is recommended to determine the optimal post-transduction time for peak expression.
FAQ 2: My transduction efficiency is poor in hard-to-transduce primary immune cells. How can I improve this?
Difficult-to-transduce cells, such as primary T cells and NK cells, require optimized physical and chemical parameters.
- Spinoculation Optimization: This centrifugation technique enhances virus-to-cell contact. Data shows that increasing the relative centrifugal force (RCF) and duration directly improves transduction efficiency in T cells and NK cells without damaging cell viability [65]. Optimal parameters identified in one study included forces up to 2000 x g for 60-90 minutes [65].
- Critical Reagent Titration: The concentration of polycationic reagents like Polybrene is a double-edged sword. While it neutralizes charge repulsion, excessive amounts can reduce cell viability without improving transduction. Furthermore, both the number and the concentration of viral particles are independently important; higher concentrations in a smaller volume lead to superior gene transduction [65].
- Envelope and Vector Choice: The viral envelope protein determines cell entry. For instance, in T cells, RDF-pseudotyped retroviruses can yield much higher expression than VSV-G-pseudotyped retroviruses. The choice between lentiviral and retroviral vectors should also be considered based on whether the target cells are dividing or non-dividing [65].
FAQ 3: I am observing off-target expression with my recombinase-dependent AAV vectors (e.g., DIO/FLEx). What is the cause and how can I minimize it?
Off-target or "leaky" expression is a known issue with DIO/FLEx vectors and is primarily caused by spontaneous recombination of the homologous lox or frt sites during plasmid amplification in bacteria, even in recombinase-deficient strains [64].
- Know Your Recombination Rate: The first step is to contact your vector supplier (e.g., Addgene) to obtain the quantified recombination rate for your specific vector lot, which typically ranges from 0.1% to 3% [64].
- Optimize Viral Titer: The most effective way to minimize leaky expression is to systematically titrate down your viral preparation. Using the lowest possible titer that still provides robust expression in your target Cre-positive cells will dramatically reduce off-target expression in Cre-negative cells. One study successfully prevented off-target expression by diluting the virus 200-300 fold [64].
- Test Serotype and Promoter: A serotype with high tropism for your specific cell type of interest allows you to use a lower overall titer, reducing off-target delivery. Similarly, a cell-type-specific promoter can provide an additional layer of specificity, though its activity must be validated in your specific system [64].
FAQ 4: How can I accurately determine if my viral transduction was successful and quantify its efficiency?
Accurate assessment is crucial and should move beyond just observing CPE.
- Go Beyond CPE: Many viruses are non-cytopathic or cause CPE too slowly for practical efficiency checks. Relying solely on visible cell destruction can lead to false negatives [66] [12].
- Reporter Genes: The use of genes encoding fluorescent proteins (e.g., GFP, mCherry) or enzymes (e.g., luciferase) allows for precise quantification of transduction efficiency via flow cytometry or luminescence assays, providing a direct and quantitative readout [66] [67] [65].
- qPCR/PCR-Based Titration: Be cautious when using PCR-based methods to determine physical viral titer. These methods cannot differentiate between infectious and non-infectious viral particles, potentially leading to an overestimation of functional titer [65].
The following tables consolidate key quantitative findings from the literature to guide your experimental planning.
Table 1: Impact of Vector Design and Transduction Parameters on Efficiency
| Parameter | Effect on Expression/Transduction | Key Quantitative Findings | Context |
|---|---|---|---|
| Codon Optimization [62] | Increases protein synthesis | Generated a more significant improvement than self-complementarity in AAV vectors [62]. | AAV8, liver gene transfer |
| Self-Complementary (sc) vs. Single-Stranded (ss) AAV [62] | Bypasses rate-limiting second-strand synthesis; dose-dependent effect | 7-fold increase with sc at low dose (3x10^9 GC); no significant difference at high dose (1x10^10 GC) [62]. | AAV8, liver gene transfer |
| Poly A Signal [63] | Affects long-term mRNA stability & expression | SV40 and Synthetic Poly A maintained higher long-term eGFP expression in stable CHO cell pools vs. BGH and others [63]. | CHO cells, stable transfection |
| Spinoculation g-force [65] | Enhances virus-cell contact | ~6-fold increase in luciferase signal in T cells at 2000 x g vs. no spinoculation [65]. | Primary human T cells, lentivirus |
| Spinoculation Duration [65] | Enhances virus-cell contact | Longer spin times (90 min for T cells, 60 min for NK cells) yielded best transduction [65]. | Primary T & NK cells |
| Viral Particle Concentration [65] | Critical for infection success | Higher concentration of the same number of viral particles led to superior transduction in 293T and T cells [65]. | 293T & primary T cells |
Table 2: Optimized Spinoculation Protocol for Primary Immune Cells
| Parameter | Recommended Optimal Condition | Note / Alternative |
|---|---|---|
| Speed (RCF) | 2000 x g | No negative impact on T or NK cell growth was observed [65]. |
| Duration | 90 min (T cells), 60 min (NK cells) | Efficiency is proportional to spin time within tested limits [65]. |
| Polybrene Concentration | 1x (Standard Concentration) | Higher concentrations (e.g., 3x, 5x, 10x) reduced cell viability without improving transduction [65]. |
| Number of Rounds | Multiple rounds (e.g., 2x) | Multiple spinoculations enhanced gene transduction without impairing T cell growth [65]. |
Essential Experimental Protocols
Protocol 1: Optimized Lentiviral Production and Spinoculation
This protocol, adapted from current methods, is designed to maximize transduction efficiency, particularly in hard-to-transduce cells [67] [65].
Part A: High-Titer Lentivirus Production (Using HEK-293T Cells)
- Seed Producer Cells: Plate HEK-293T cells at a density of 0.6 × 10^5 cells/cm² and culture for 24 hours to reach ~80% confluency [67].
- Prepare DNA-Lipid Complex: For a 150 mm culture dish, mix:
- 17 µg lentiviral transfer plasmid (e.g., sgLenti-mCherry)
- 17 µg packaging plasmid (psPAX2)
- 5.7 µg envelope plasmid (pMD2.G)
- Add Opti-MEM reduced serum medium to a final volume of 2.1 mL.
- Add 140 µl P3000 reagent.
- In a separate tube, mix 160 µl Lipofectamine LTX and 40 µl Lipofectamine 3000 with 2.1 ml Opti-MEM.
- Combine the DNA and Lipofectamine mixtures, incubate for 30 minutes at room temperature [67].
- Transfect: Add the complex dropwise to the HEK-293T cells. Gently shake the dish to distribute evenly.
- Collect Viral Supernatant: At 24 hours post-transfection, replace the medium with fresh growth medium. Collect the virus-containing supernatant 72 hours post-transfection, filter through a 0.45 µm filter, and concentrate ~10-fold using centrifugal concentration columns (e.g., Vivaspin) [67].
Part B: Spinoculation of Target Cells
- Prepare Target Cells: Seed 25,000 primary immune cells (e.g., pre-activated T cells) per well in a 96-well U-bottom plate. Pellet cells by centrifugation at 500 x g for 3 min and remove supernatant [65].
- Apply Virus: Add 12.5 µl of concentrated viral solution to the cell pellet. Adjust the total volume to 50 µl with fresh medium without resuspending the cells.
- Add Polybrene: Add polybrene to a final concentration of 10 µg/ml [67].
- Centrifuge: Centrifuge the plate at 2000 x g for 90 minutes (for T cells) at 37°C [65].
- Recover and Culture: After spinoculation, transfer cells to a larger culture vessel (e.g., 48-well plate) with fresh medium. Analyze transduction efficiency (e.g., via flow cytometry for a reporter gene) 4 days post-infection [67].
Protocol 2: Systematic Titration of AAV DIO/FLEx Vectors to Minimize Off-Target Expression
This protocol is critical for experiments requiring strict cell-type-specific expression, such as in neuroscience [64].
- Determine Physical Titer and Recombination Rate: Obtain the genomic titer (GC/mL) and the specific recombination rate (e.g., 0.1% - 0.8%) for your AAV-DIO/FLEx vector lot from the supplier [64].
- Prepare a Dilution Series: Based on the physical titer, prepare a wide range of dilutions. For example, if your stock is 1x10^13 GC/mL, prepare dilutions at 10^-1, 10^-2, 10^-3, and 10^-4, which correspond to 1x10^12, 1x10^11, 1x10^10, and 1x10^9 GC/mL, respectively [64].
- Inject into Animal Model: Administer each dilution to your animal model (e.g., stereotactic injection into the brain), ensuring all other parameters (volume, injection speed, site) are kept constant.
- Analyze Expression: After a standardized expression period (e.g., 3-4 weeks), analyze the tissue for:
- ON-Target Expression: Check for robust expression in your Cre-positive target cells.
- OFF-Target Expression: Carefully examine Cre-negative areas or cell types for any leaky expression.
- Identify Optimal Titer: The correct working titer is the highest dilution that still provides strong ON-target expression while eliminating detectable OFF-target expression. One successful study used a 200-300 fold dilution of a high-titer stock to achieve this balance [64].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Optimizing Transduction and Expression
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Polybrene [67] [65] | A polycation that neutralizes charge repulsion between viral particles and cell membranes, enhancing viral entry. | High concentrations are toxic to primary cells (e.g., T cells, NK cells). A final concentration of 10 µg/ml is often used [65]. |
| VSV-G Envelope Plasmid (pMD2.G) [67] | Provides the Vesicular Stomatitis Virus G glycoprotein for pseudotyping, conferring broad tropism to lentiviral particles. | A standard for producing lentiviruses with wide host range. |
| Alternative Envelopes (e.g., RDF) [65] | Different envelope proteins can target specific cell types with higher efficiency (e.g., RDF for T cells). | Critical for hard-to-transduce cells; requires empirical testing for your specific cell type [65]. |
| Codon-Optimized Transgene [62] | A synthetic gene sequence engineered to use optimal codons for the host organism, maximizing translation efficiency. | Can have a more powerful effect on expression levels than other vector modifications like self-complementarity [62]. |
| Optimized Poly A Signal (SV40, Synthetic) [63] | Ensures proper mRNA processing, stability, and nuclear export, leading to higher and more stable protein yields. | SV40 and Synthetic Poly A showed superior performance in maintaining long-term expression in CHO cells [63]. |
| Fluorescent Reporter Genes (eGFP, mCherry) [67] [65] | Enable rapid, quantitative assessment of transduction efficiency and transgene expression via flow cytometry or microscopy. | Allows for tracking of successfully transduced cells over time without the need for cell lysis [65]. |
This guide provides a structured, evidence-based approach to diagnosing and resolving the common yet critical issue of low viral titer in a research setting. Within the broader context of optimizing viral cell culture for cytopathic effect research, achieving and maintaining high-titer viral stocks is fundamental. Low titers can compromise experimental reproducibility, hinder the assessment of virus-host interactions, and delay drug development pipelines. This resource consolidates troubleshooting methodologies and technical protocols, focusing on three primary levers under a researcher's control: storage and handling practices, the structural constraints of the viral vector—specifically insert size—and culture optimization techniques.
Troubleshooting Guide: Key Questions and Solutions
FAQ 1: My viral titers are consistently low after production. What are the first parameters I should check?
Begin by systematically investigating the variables with the most significant and immediate impact on titer.
A: Optimize Storage and Handling: Improper storage is a major cause of titer loss.
- Temperature Stability: Maintain a consistent, ultra-low storage temperature. Viruses are typically stored at -80°C or colder to preserve viability [68]. Fluctuations in temperature can be devastating.
- Avoid Freeze-Thaw Cycles: Each freeze-thaw cycle can degrade viral particles. Data from one source indicates a 25% loss of viral titer with each freeze-thaw cycle [33]. Aliquot your viral stocks into single-use volumes to avoid repeated thawing.
- Use Cryoprotectants: Adding stabilizing agents like PEG6000 to a final concentration of 5% before freezing can help protect viral integrity during storage [33].
B: Review Transfection and Production Conditions: The production process itself is often the source of low yield.
- Transfection Reagent: Use a transfection reagent specifically designed for high-titer virus production. Specialized reagents can significantly outperform standard reagents, with some systems generating up to 10-fold higher titers and improved percentages of full capsids for AAV vectors [69].
- Cell Density and Health: Infect or transfert cells when they are at optimal density and high viability (>90%). Over-confluent or unhealthy cells will not produce high titers [33] [69].
- Multiplicity of Infection (MOI): Using an excessively high MOI during stock production can lead to cytotoxicity and the accumulation of defective interfering particles, thereby reducing the quality of the stock [33].
FAQ 2: I am cloning a large gene insert. How might this be affecting my viral titer?
The size of the genetic insert is a critical and frequently overlooked factor that directly impacts viral titer and stability.
A: Respect Packaging Constraints: Every viral vector has a strict upper limit on the amount of genetic material it can package. Exceeding this limit drastically reduces titer.
Packaging Limits Table:
Viral Vector Approximate Insert Size Limit Key Considerations Adeno-associated Virus (AAV) < 5 kb [70] Titers decrease as insert size approaches the packaging limit [33]. Lentivirus ~8 kb [70] [71] Beyond this size, the viral titer begins to drop drastically [70]. Adenovirus Up to ~15 kb [70] [71] Known for its relatively large packaging capacity. Retrovirus < 8 kb [33] Similar constraints to lentivirus but only infects dividing cells. Impact on Stability: Beyond just initial titer, larger inserts are inherently more unstable. Engineered viruses with inserted sequences are often unstable over time, and the inserted sequences can be rapidly lost upon passaging, a phenomenon strongly influenced by viral genome organization [71].
B: Mitigate Insert-Driven Instability:
- Consider cDNA vs. Genomic DNA: For expression studies, cDNA is typically sufficient and more compact than a full genomic sequence [70].
- Split Large Genes: For very large genes, one innovative strategy involves splitting the gene into two fragments and cloning each into separate AAV vectors. Upon co-infection, the full protein can be reconstituted [70].
FAQ 3: Beyond basic culture, how can I optimize my bioprocess to maximize titer?
Moving from standard batch culture to optimized fed-batch or perfusion processes can overcome the "cell density effect," where specific productivity drops at high cell densities.
A: Implement Fed-Batch Strategies: Supplementing cultures with concentrated nutrients can sustain cell growth and viral production at high densities.
- Evidence: One study cultivating HEK 293 cells demonstrated that a customized fed-batch process enabled infection at high cell densities (5 x 10^6 cells/mL) while maintaining cell-specific productivity, resulting in a six-fold improvement in volumetric titer for an Adenovirus type 5 vector, reaching 3.0 x 10^10 total viral particles/mL [72].
- Method: This involves selecting supportive basal media and adding concentrated feeds (commercial or developed in-house) at strategic time points to replenish nutrients [72].
B: Ensure Proper Viral Activation: For some viruses, proteolytic cleavage is essential for infectivity.
- Example - Rotavirus: The rotavirus attachment protein requires activation by trypsin. Protocols specify adding trypsin to a final concentration of 10 µg/mL to the virus inoculum before adsorption, and then maintaining a lower concentration (0.5 µg/mL) in the culture medium post-infection for efficient propagation [73].
- Serum-Free Conditions: Fetal bovine serum (FBS) inhibits the activation of some viruses like rotavirus and must be thoroughly washed out before infection [73].
The following table consolidates key quantitative findings from the literature to serve as a reference for your optimization efforts.
Table 1: Summary of Key Experimental Data from Literature
| Parameter | Virus/System | Quantitative Finding | Context |
|---|---|---|---|
| Freeze-Thaw Impact | Viral Vectors (General) | ~25% titer loss/cycle [33] | Handling & Storage |
| Fed-Batch Productivity | Adenovirus Type 5 (Ad5) | 6-fold increase; 3.0 x 10^10 TVP/mL [72] | Process Optimization |
| Detection Limit | RSV Biosensor | 0.88 PFU/mL [74] | Analytics & QC |
| Trypsin Concentration | Rotavirus | Activation: 10 µg/mL; Maintenance: 0.5 µg/mL [73] | Culture Protocol |
| Diagnostic Concordance | geneLEAD/VIASURE vs. Manual RT-qPCR | Pearson’s R²: 0.90 (SARS-CoV-2) - 0.95 (RSV) [75] | Analytics & QC |
Essential Experimental Protocols
This protocol exemplifies a standardized method for propagating viruses in cell culture, highlighting critical steps like serum removal and viral activation.
Materials:
- Virus stock
- Confluent MA104 cells in a 150 cm² flask
- Porcine pancreatic trypsin (2 mg/mL stock)
- Serum-free Medium 199
- Serum-free Medium 199 with 0.5 µg/mL trypsin
Method:
- Prepare Cells: Remove growth medium from a confluent monolayer of MA104 cells. Wash the monolayer three times with 10 mL of pre-warmed, serum-free Medium 199 to inhibit serum proteins.
- Activate Virus: Thaw the virus stock. In a sterile tube, combine a volume of virus stock equivalent to an MOI of ≤0.1 with trypsin to a final concentration of 10 µg/mL. Mix and incubate for 1 hour in a 37°C water bath.
- Dilute Inoculum: Add serum-free Medium 199 to the activated virus to bring the final trypsin concentration to < 2 µg/mL. The total volume for a 150 cm² flask should be at least 3 mL.
- Adsorb Virus: Remove the final wash from the cell monolayer. Add the inoculum and incubate the flask for 1 hour at 37°C, rocking every 10-15 minutes to ensure even coverage.
- Maintain Infection: After adsorption, remove the inoculum and wash the monolayer once with serum-free medium. Add 20 mL of serum-free Medium 199 containing 0.5 µg/mL trypsin.
- Harvest Virus: Incubate cells at 37°C for 3-7 days until advanced cytopathic effect (CPE) is observed (full monolayer disruption). Freeze the flask at -80°C.
- Clarify Lysate: Perform three freeze-thaw cycles to release cell-associated virus. Clarify the lysate by centrifugation to remove large debris. Aliquot and store the supernatant (viral stock) at -80°C.
This protocol outlines a strategic approach to optimizing transfection conditions to maximize titer.
Materials:
- High-productivity cell line (e.g., HEK 293 variant)
- Supportive cell culture media (e.g., LV-MAX, FreeStyle 293)
- Specialized transfection reagent (e.g., TransIT-VirusGEN)
- Plasmid DNA (transfer and packaging plasmids)
Method:
- Baseline Assessment: Start with the manufacturer's recommended protocol for your transfection reagent and cell line.
- Systematically Vary Parameters: Test the following parameters one at a time, using a reporter virus (e.g., GFP) to measure functional titer:
- Cell Density: Test a range of densities at transfection (e.g., 2-5 x 10^6 cells/mL for suspension HEK 293).
- DNA Mass: Titrate the total amount of DNA per volume of culture.
- Reagent:DNA Ratio: Test different ratios (e.g., 3:1, 4:1 vol:wt).
- Complexation Time: Vary the incubation time of the DNA-transfection reagent complex.
- Enhancers: Evaluate the addition of "Enhancer" solutions 18-24 hours post-transfection.
- Harvest and Titer: Harvest the virus-containing supernatant at 48-72 hours post-transfection. Quantify the viral titer using an appropriate method (e.g., plaque assay, flow cytometry for functional titer, or qPCR for physical titer).
- Analyze and Iterate: Identify the conditions that yield the highest functional titer. Use these optimized conditions for large-scale production.
Workflow Visualization
The following diagram outlines a logical decision-making workflow for diagnosing and resolving low viral titer issues.
The Scientist's Toolkit: Key Research Reagent Solutions
This table lists essential materials and reagents cited in the literature for improving viral titer and process efficiency.
Table 2: Essential Research Reagents for Viral Titer Optimization
| Reagent / Material | Function / Application | Key Finding / Rationale |
|---|---|---|
| Specialized Transfection Reagents (e.g., TransIT-VirusGEN [69]) | Form DNA complexes for efficient entry into production cells. | Outperformed PEI-based reagents, generating significantly more full AAV capsids and higher functional titers for lentivirus [69]. |
| High-Producivity Cell Lines (e.g., adapted HEK 293SF [72] [69]) | Cell substrate for viral vector production. | Specialized lines grown in supportive media are geared toward maximizing viral vector productivity [69]. |
| Fed-Batch Media & Feeds (Commercial or in-house [72]) | Replenishes nutrients to sustain high-density cultures. | Enabled infection at high cell density (5 x 10^6 cells/mL) with a 6-fold improvement in Ad5 volumetric titer [72]. |
| Trypsin (Porcine pancreatic type IX [73]) | Proteolytic activation of viral attachment proteins (e.g., for Rotavirus). | Essential cleavage step for infectivity; used at 10 µg/mL for activation and 0.5 µg/mL for maintenance in culture [73]. |
| Cryoprotectants (e.g., PEG6000 [33]) | Stabilizes viral particles during freezing. | Adding to a final concentration of 5% before freezing helps stabilize viral stocks against degradation [33]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary signs that my cell culture is experiencing cytotoxicity from a viral infection?
A1: Cytotoxicity from viral infection, known as cytopathic effect (CPE), manifests through specific morphological changes in the cell monolayer. Common signs include:
- Cell Rounding and Detachment: The infected cells lose their typical shape, become rounded, and eventually detach from the culture surface [12] [4].
- Syncytia Formation: Fusion of infected cells with adjacent cells to form large, multi-nucleated cytoplasmic masses (polykaryocytes) [4].
- Inclusion Bodies: Appearance of abnormal structures in the nucleus or cytoplasm, which can represent accumulations of viral components or altered host cell structures [4].
- Vacuolization and Lysis: The cytoplasm develops vacuoles, and ultimately, the cell membrane ruptures (lysis), leading to the destruction of the monolayer [12].
Q2: How can I distinguish between cell death caused by a high Multiplicity of Infection (MOI) and death from an underlying unhealthy culture?
A2: Distinguishing between these causes requires careful observation and control experiments.
- High MOI Cytotoxicity: This typically causes rapid, synchronized, and extensive cell death that correlates directly with the amount of virus used. The CPE is often uniform across the monolayer. You can confirm this by testing a range of MOIs; a lower MOI should result in reduced and slower CPE progression [12].
- Unhealthy Culture: Cell death in an unhealthy culture often precedes viral infection or occurs inconsistently. Signs include excessive granularity, slow growth, and abnormal pH shifts in the medium without viral infection. This can be caused by factors like microbial contamination (e.g., mycoplasma), nutrient exhaustion, or suboptimal culture conditions. Running controls with mock-infected cells from the same passage is crucial to identify this issue [8].
Q3: What are the best methods to detect latent or persistent viral contaminants in my cell lines that could be affecting cell health?
A3: Some viruses can establish persistent infections without causing obvious CPE, making them difficult to detect visually [12] [4]. Robust detection methods are essential:
- PCR-Based Assays: Standard and digital PCR (ddPCR) are highly sensitive for detecting viral nucleic acids, even for viruses like Epstein-Barr Virus (EBV) that exist in both active and latent forms [8] [76].
- High-Throughput Sequencing (HTS): This advanced technology can detect a wide range of known and novel adventitious viruses without prior sequence knowledge, making it ideal for comprehensive bioprocess safety testing [77].
- Other Methods: Techniques like hemadsorption or interference assays can also be used to detect the presence of viruses that do not cause CPE [12].
Troubleshooting Guides
Problem: Rapid and Widespread Cell Death Post-Infection
Potential Cause: Cytotoxicity from an excessively high Multiplicity of Infection (MOI).
Investigation and Solutions:
| Investigation Step | Action & Solution |
|---|---|
| Confirm the Cause | Titrate your virus stock to determine the exact titer. Perform an infection time-course using a range of MOIs (e.g., 0.1, 1, 10) and include a mock-infected control. |
| Optimize Infection | Reduce the MOI. Use the lowest MOI that achieves your experimental goal (e.g., transgene expression, virus production). For highly cytopathic viruses, even an MOI of 1 can lead to rapid oncolysis [78]. |
| Monitor Closely | Observe the cells frequently under a microscope post-infection. A lower MOI will result in a slower progression of CPE, allowing you to harvest virus or analyze data at the optimal time point [12]. |
Problem: Unexpected or Inconsistent Cell Death in Both Infected and Control Cultures
Potential Cause: Underlying unhealthy cell culture or covert viral contamination.
Investigation and Solutions:
| Investigation Step | Action & Solution |
|---|---|
| Check Culture Health | Review your cell culture practices: passage cells at the correct confluence, use fresh medium, and check for signs of contamination (e.g., color change, cloudiness). Always use healthy, low-passage cells for infections [8]. |
| Test for Contaminants | Implement a routine quality control program. This should include mycoplasma testing and screening for common viral contaminants like Epstein-Barr Virus (EBV) or Ovine Herpesvirus 2 (OvHV-2) using PCR or other validated methods [8]. |
| Authenticate Cell Lines | Use short tandem repeat (STR) profiling to ensure your cell line has not been cross-contaminated or misidentified [8]. |
| Use Robust Detection | For comprehensive safety, consider adopting High-Throughput Sequencing (HTS) to broadly detect adventitious viruses in biological products and cell banks [77]. |
Experimental Protocol: Assessing Virus-Induced Cytotoxicity
Aim: To quantitatively assess the cytopathic effect (CPE) of a virus on a permissive cell line and determine the optimal MOI for experiments.
Materials:
- Permissive cell line (e.g., A549 for respiratory viruses [78])
- Virus stock of known titer
- Complete cell culture medium and maintenance medium
- Tissue culture-treated multi-well plates
- Inverted microscope
- Cell viability assay kit (e.g., MTT, PrestoBlue)
Method:
- Seed Cells: Plate cells in a multi-well plate at a standard density (e.g., 1x10^5 cells/well for a 24-well plate) to achieve 80-90% confluence at the time of infection.
- Inoculate Virus: The next day, prepare serial dilutions of your virus stock. Aspirate the medium from the wells and inoculate with virus at a range of MOIs (e.g., 0.01, 0.1, 1, 10). Include mock-infected controls (maintenance medium only).
- Adsorb and Maintain: Allow the virus to adsorb for 1-2 hours at 37°C with periodic rocking. After adsorption, remove the inoculum, wash the monolayer with PBS, and add fresh maintenance medium.
- Monitor and Score CPE: Observe the cells daily under an inverted microscope. Use a standardized CPE scoring system (e.g., 0: no CPE, 1: 25% CPE, 2: 50% CPE, 3: 75% CPE, 4: 100% cell destruction [12]).
- Quantify Viability: At predetermined time points (e.g., 24, 48, 72 hours post-infection), perform a cell viability assay according to the manufacturer's instructions to generate quantitative data.
Signaling Pathways in Virus-Induced Cell Death
Viral infection can activate multiple, overlapping cell death pathways. The specific pathway engaged can depend on the virus and the host cell line. Research on oncolytic viruses, for example, has shown that they can dynamically engage both apoptosis and necroptosis to mediate cell lysis [78]. Genetic deletion of key regulators in one pathway can lead the virus to switch to an alternative death pathway.
Research Reagent Solutions
Essential materials and reagents for troubleshooting cytotoxicity in viral cell culture research.
| Reagent / Material | Function / Application |
|---|---|
| Cell Line Authentication (STR Profiling) | Confirms the genetic identity of the cell line, preventing misidentification and cross-contamination, which can cause unpredictable responses to infection [8]. |
| Mycoplasma Detection Kit | Routinely screens for mycoplasma contamination, a common cause of poor cell health and unreliable experimental results [8]. |
| PCR Assays for Viral Contaminants | Detects specific latent or persistent viruses (e.g., EBV, OvHV-2) in cell banks that may compromise cell viability without showing clear CPE [8]. |
| Droplet Digital PCR (ddPCR) | Provides absolute quantification of viral load with high sensitivity and tolerance to inhibitors; useful for precise virus titration and contaminant detection [76]. |
| High-Throughput Sequencing (HTS) | Offers a broad, unbiased method for detecting known and novel adventitious viruses in biological samples and cell substrates [77]. |
| Cell Viability Assays (e.g., MTT) | Provides quantitative data on cell health and virus-induced cytotoxicity, complementing qualitative CPE scoring [78]. |
This technical support center provides troubleshooting guides and FAQs to help researchers address the critical challenge of adventitious viral contamination in cell culture systems. This content is framed within the broader thesis of optimizing viral cell culture for cytopathic effect (CPE) research, ensuring that foundational studies on viral mechanisms and antiviral efficacy are built upon pure, uncontaminated biological systems.
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common sources of viral contamination in a cell culture lab? Viral contamination can arise from several sources, including the original cell lines or animal-derived reagents (such as bovine serum), through cross-contamination from other infected cultures in the lab, or via exposure from manufacturing operators [79] [80]. Ensuring that all cell lines are obtained from reputable cell banks and that all animal-derived reagents are properly tested and sourced can significantly mitigate this risk [81].
FAQ 2: My cell culture medium appears clear, and the cells look fine under my regular microscope. Can I assume it is free from viral contamination? No. Many viral contaminants do not cause visible changes in the culture medium, and some viruses do not produce obvious CPE in all cell types [9]. Contaminants like mycoplasma can be extremely difficult to detect without specific testing [81]. Routine monitoring using specialized methods like PCR, ELISA, or electron microscopy is essential to confirm the absence of viral agents [81] [80].
FAQ 3: I suspect my irreplaceable cell line is contaminated. Can I decontaminate it? It is sometimes possible to decontaminate a valuable culture, but the process is complex and not always successful. The first step is to isolate the contaminated culture and identify the contaminant (e.g., bacteria, fungus, mycoplasma) [81]. For biological contaminants, you may attempt a procedure using high concentrations of antibiotics or antimycotics, but their toxicity to your cell line must first be empirically determined. The culture is then passaged several times at a concentration just below the toxic level, followed by culture in antibiotic-free medium to verify if the contamination has been eliminated [81].
FAQ 4: How can Artificial Intelligence (AI) help in detecting viral contamination? AI systems, particularly deep learning convolutional neural networks (CNNs), can be trained to automatically detect virus-induced CPEs in label-free microscopy images [9]. These systems can identify subtle, virus-specific morphological changes in cells (like rounding, syncytia formation, or detachment) that might be missed by the human eye, providing an unbiased, high-throughput method for early contamination detection and virus classification [9].
Troubleshooting Common Problems
Problem 1: Unexplained Changes in Cell Morphology or Culture Death
- Potential Cause: Adventitious viral infection or contamination with mycoplasma.
- Solution:
- Isolate the Culture: Immediately move the suspect culture away from other cell lines to prevent spread [81].
- Perform Diagnostic Tests: Use PCR-based assays to test for specific viruses or mycoplasma. For a broad screening approach, electron microscopy can visually identify unknown viral particles [80].
- Check Control Cells: Compare with a frozen stock of the same cell line that has not been in continuous culture to rule out genetic drift or other non-contamination factors.
Problem 2: Low Transduction Efficiency in Viral Vector Experiments
- Potential Cause: Low viral titer or suboptimal infection conditions.
- Solution:
- Concentrate Your Viral Stock: Use methods like ultracentrifugation to increase the viral titer [33].
- Optimize the Multiplicity of Infection (MOI): Perform a pilot experiment using a reporter virus (e.g., GFP-expressing) on your target cells to determine the ideal number of viral particles per cell. Too few particles result in low efficiency, while too many can cause cytotoxicity [33].
- Use a Transduction Enhancer: Reagents like polybrene can reduce electrostatic repulsion between the viral particle and the cell membrane, improving infection rates [33].
Problem 3: Inconsistent or Atypical Cytopathic Effects (CPE)
- Potential Cause: Co-contamination with multiple adventitious agents or misidentification of the CPE.
- Solution:
- Implement AI-Based CPE Classification: Tools like AIRVIC (AI Recognition of Viral CPE) can objectively classify CPEs from microscopy images, reducing subjective interpretation errors [9].
- Confirm with Orthogonal Methods: Use immunofluorescence or PCR to confirm the identity of the virus causing the CPE [81].
- Authenticate Your Cell Line: Perform DNA fingerprinting or karyotype analysis to rule out cross-contamination with another cell line, which can alter the apparent CPE [81].
Quantitative Data on AI-Assisted CPE Detection
The following data, derived from a recent study, demonstrates the performance of an AI system (AIRVIC) in detecting and classifying viral CPEs from microscopy images, showcasing its potential as a powerful tool for contamination monitoring [9].
Table 1: Performance of AI (AIRVIC) in Detecting Virus-Induced CPEs
| Virus | Cell Line | AI Detection Accuracy |
|---|---|---|
| BoGHV-4 (DN-599 strain) | MDBK | 100.00% |
| Bovine Parainfluenza Virus 3 (BPIV3) | MDBK | 97.30% |
| SARS-CoV-2 | Vero | 94.41% |
| Bovine Adenovirus-1 (BAdV-1) | MDBK | 93.67% |
| BoGHV-4 (MOVAR 33/63 strain) | Vero | 87.99% |
Table 2: AI Performance in Multi-Virus Classification
| Classification Scenario | AI Classification Accuracy |
|---|---|
| Multi-class accuracy for bovine viruses in MDBK cells | 87.61% |
| Multi-class accuracy for viruses across different cell lines | 63.44% |
Experimental Protocols for Prevention and Detection
Protocol 1: Routine Screening for Adventitious Agents Using PCR This is a standard method for sensitive detection of specific contaminants [80].
- Sample Collection: Collect supernatant from your cell culture.
- Nucleic Acid Extraction: Isolate total DNA and/or RNA from the sample.
- PCR Amplification: Use GMP-compliant, pre-validated qPCR assays targeting common adventitious agents (e.g., Sf Rhabdovirus, Mycoplasma species). Master mixes specifically ultra-purified to remove background DNA are recommended for the lowest limits of detection [80].
- Data Analysis: Analyze amplification curves. The use of digital PCR systems can provide absolute quantification of low-level targets [80].
Protocol 2: Establishing a High-Throughput Antiviral Screening System Using a Surrogate Virus This protocol is useful for labs studying antivirals while minimizing risks associated with human pathogens [82].
- Select a Surrogate Virus: Use a safer, engineered virus that shares key replication features with pathogenic viruses. Example: Recombinant Viral Hemorrhagic Septicemia Virus (rVHSV) expressing eGFP as a surrogate for RNA viruses [82].
- Prepare Host Cells: Seed Epithelioma Papulosum Cyprini (EPC) cells in a 96-well plate.
- Inoculate and Screen: Mix rVHSV with the cells in the presence of the compounds or extracts to be screened. Optimize the MOI, serum concentration (e.g., 2% FBS for VHSV replication), and temperature (e.g., 15°C for VHSV) [82].
- Measure Outcome: After incubation, measure the intensity of eGFP fluorescence or observe the CPE. A reduction in fluorescence or CPE compared to controls indicates antiviral activity [82].
- Calculate Selectivity Index (SI): Determine the compound's cytotoxic concentration (CC50) and its virus inhibition concentration (IC50). The SI is CC50/IC50; a high SI indicates a strong and safe antiviral candidate [82].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for Adventitious Agent Testing
| Product Name / Type | Function | Example Application |
|---|---|---|
| MycoSEQ Detection System | Sensitive PCR-based detection of >90 mycoplasma species. | Routine screening of cell banks and production cultures for mycoplasma contamination [80]. |
| ViralSEQ Detection System | GMP-compliant qPCR kits for specific adventitious viruses. | Targeted testing for common viral contaminants like Sf Rhabdovirus and Vesivirus in biomanufacturing [80]. |
| TaqPath BactoPure Master Mix | Ultra-purified qPCR master mix for microbial detection. | Highly sensitive, multiplex detection of bacterial, viral, and fungal DNA targets in quality control testing [80]. |
| ViralEntry Transduction Enhancer | Cationic polymer that improves viral infectivity. | Increasing transduction efficiency of viral vectors (e.g., lentivirus, AAV) in difficult-to-transduce cells [33]. |
| AAV Serotype Kits | Kit to determine the optimal adeno-associated virus (AAV) serotype. | Identifying the best AAV capsid serotype for efficient gene delivery to specific target tissues in research [33]. |
Workflow Diagrams for Contamination Management
The following diagram illustrates the key decision points and actions for handling suspected contamination.
Adventitious Agent Response Workflow
This workflow outlines the steps for a high-throughput screening system using a surrogate virus, which is key for safe and efficient antiviral discovery.
Surrogate Virus Screening Workflow
Technical Support Center
Troubleshooting Guides
Guide 1: Addressing Poor or No Viral Cytopathic Effect (CPE)
| Problem Phenomenon | Possible Cause | Recommended Solution |
|---|---|---|
| No observable CPE in infected culture [8] | Incorrect host cell line selected | Confirm cell line is susceptible to the specific virus; consult literature for known permissive cell lines [8]. |
| Low viral infectivity (titer) | Re-titer your viral stock to ensure adequate Multiplicity of Infection (MOI) is used for inoculation. | |
| CPE appears inconsistent or weak | Suboptimal culture conditions | Verify that temperature, CO₂, and medium pH are correctly maintained for the specific cell line [83]. |
| Cell health issues pre-infection | Ensure cells are in log-phase growth and are sub-cultured well before reaching 100% confluence [84]. | |
| Rapid cell death post-infection (non-specific) | Microbial contamination (e.g., Mycoplasma) | Test cultures for Mycoplasma and other contaminants prior to infection [83]. |
| Toxicity from inoculation buffer | Include a mock-infected control (virus diluent only) to rule out toxicity from the inoculum itself. |
Guide 2: Managing Cell Culture Contamination
| Problem Phenomenon | Possible Cause | Recommended Solution |
|---|---|---|
| Cloudy culture media; pH shifts [83] | Bacterial contamination | Discard culture and reagents. Decontaminate incubators and hoods. Use antibiotics and practice strict aseptic technique [83]. |
| Floating fungal masses or hyphae under microscope [83] | Fungal contamination | Discard culture and reagents. Decontaminate work areas. Use antimycotics like Amphotericin B [83]. |
| Culture degradation without obvious cause [83] | Mycoplasma contamination | Use a dedicated Mycoplasma detection test (e.g., PCR, ELISA). Quarantine affected cultures and treat if possible [83]. |
| Altered cell growth or morphology [8] | Viral contamination (e.g., EBV, OvHV-2) | Use specific detection methods like PCR to identify the virus. Quarantine or discard the affected cell line [8]. |
| Cell line misidentification [83] | Cross-contamination | Authenticate cell lines regularly using STR profiling [83]. |
Frequently Asked Questions (FAQs)
Q1: My cells are not adhering properly after thawing. What should I check? A1: First, confirm you are using the recommended extracellular matrix (e.g., PriCoat T25 Flasks or Applied Cell Extracellular Matrix) [84]. Ensure the culture vessel was properly coated before plating. Verify that the thawing protocol was followed precisely, including the centrifugation step to remove residual cryoprotectant like DMSO [84].
Q2: How can I confirm that a cytopathic effect (CPE) I'm observing is due to my virus and not general cell death? A2: Always include proper controls. An uninfected control culture (same cell line, same passage, cultured in parallel) is essential. Compare the morphology of infected cells to the healthy, dividing cells in the control. Specific CPE (cell rounding, syncytia formation) that progresses in a dose-dependent manner with the viral inoculum strongly indicates viral activity [8].
Q3: What are the critical steps for cryopreserving my cells to ensure good recovery later? A3: Use the recommended cryopreservation medium (e.g., complete growth media with 10% DMSO) [84]. Freeze cells at a high viability and optimal density. Use a controlled-rate freezer or an isopropanol freezing container to achieve a slow cooling rate of approximately -1°C per minute. Finally, store cells in the vapor phase of liquid nitrogen or below -130°C [84].
Q4: Why is STR profiling important, and how often should it be done? A4: STR profiling is a DNA fingerprinting technique that authenticates your cell line, ensuring you are working with the correct cells and that they have not been cross-contaminated [83]. This is critical for research reproducibility. It should be performed upon receiving a new cell line, before starting a new series of experiments, and at regular intervals (e.g., every 3 months) for continuously cultured lines [83].
Q5: How do I detect latent viral contaminants like Epstein-Barr Virus (EBV) in my cell culture? A5: Polymerase Chain Reaction (PCR) is a highly sensitive and established method for detecting both active and latent forms of viruses like EBV [8]. You can use specific primers to amplify viral DNA sequences from cell lysates.
Experimental Protocols for Viral CPE Research
Protocol 1: Standard Method for Initiating a Viral CPE Assay
Principle: To successfully infect a susceptible cell monolayer with a virus and observe the subsequent development of cytopathic effect.
Materials:
- Susceptible adherent cell line (e.g., A549 [8])
- Complete growth medium
- Viral inoculum
- Sterile PBS
- Tissue culture flasks or multi-well plates
Methodology:
- Cell Seeding: Seed an appropriate number of cells into a culture vessel to achieve 70-80% confluence at the time of infection. Incubate overnight at 37°C and 5% CO₂ [84].
- Virus Inoculation:
- Aspirate the growth medium from the cells.
- Wash the cell monolayer gently with pre-warmed sterile PBS to remove serum and debris.
- Add the viral inoculum, diluted in serum-free medium or the recommended infection medium, to the cells.
- Incubate for 1-2 hours to allow for viral adsorption, gently rocking the plate every 15 minutes.
- Post-Inoculation:
- After the adsorption period, aspirate the inoculum.
- Add fresh complete growth medium to support both cell and potential viral growth.
- Return the culture to the incubator.
- CPE Observation:
- Observe cultures daily under a light microscope for morphological changes indicative of CPE [8].
- Compare the infected cultures to mock-infected controls.
Protocol 2: Differentiating Apoptosis from Virus-Induced Necrosis
Principle: To distinguish the mode of cell death during CPE, which can provide insights into the viral mechanism of action.
Materials:
- Infected and control cell cultures
- Assay kits for apoptosis/necrosis (e.g., detecting caspase activation for apoptosis, or membrane integrity dyes for necrosis)
Methodology:
- Sample Preparation: At various time points post-infection, harvest the culture supernatant and trypsinize the adherent cells. Combine the supernatant and cells to capture both detached and adherent cells [84].
- Staining: Following the manufacturer's instructions, stain the cell samples with specific fluorescent dyes that distinguish apoptotic cells (e.g., Annexin V) from necrotic cells (e.g., propidium iodide).
- Analysis: Analyze the stained cells using flow cytometry or fluorescence microscopy. Apoptotic cells will be positive for Annexin V, while necrotic cells will be positive for both Annexin V and propidium iodide.
Signaling Pathways and Workflows for Viral CPE
Viral CPE Research Workflow
Cell Death Pathway Analysis
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Application |
|---|---|
| PriCoat T25 Flasks (G299) [84] | A specially coated surface that provides the optimal extracellular matrix for adherence and growth of sensitive cell lines like skeletal myoblasts. |
| Applied Cell Extracellular Matrix (G422) [84] | A type I collagen-based coating solution used to prepare culture surfaces for optimal cell attachment and growth. |
| STR Profiling Service [83] | A service that performs Short Tandem Repeat analysis to authenticate cell lines, confirming their identity and detecting cross-contamination. |
| Mycoplasma Detection Kit [83] | A test kit (often based on PCR) used to detect the presence of Mycoplasma contamination, an invisible threat that can sabotage cell cultures. |
| Cryopreservation Medium (TM024) [84] | A ready-to-use medium containing cryoprotectants like DMSO, formulated for the long-term storage of cells in liquid nitrogen while preserving viability. |
| FGF2 (Z101455) [84] | Fibroblast Growth Factor 2, a supplement used in growth media to promote cell proliferation and maintain the undifferentiated state of certain cell types. |
| Trypsin-EDTA (0.25%) [84] | A solution of the enzyme trypsin and EDTA used to dissociate adherent cells from the culture vessel surface for subculturing or passaging. |
Validating and Quantifying CPE: From Traditional Assays to AI-Powered Analysis
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My viral infection is not producing a clear cytopathic effect (CPE) in cell culture. What could be the issue? Several factors can affect CPE development. First, verify the multiplicity of infection (MOI) and incubation parameters are optimized for your specific virus and cell line. For instance, HCoV-OC43 requires 4.5 days at 33°C in RD cells, while HCoV-NL63 shows CPE in 4 days at 37°C in Vero E6 cells [3]. Second, confirm cell line susceptibility; some viruses exhibit distinct CPE in different lines [3]. Third, consider using a more sensitive detection method like a luminescent ATP-based viability assay (e.g., Viral ToxGlo) if visual CPE is subtle [85].
Q2: How can I distinguish virus-induced CPE from non-specific cellular aging or toxicity? Uninfected control wells are essential. True viral CPE typically progresses over time and exhibits characteristic patterns [1]. Artificial intelligence systems like AIRVIC can be trained to differentiate virus-specific CPE from other morphological changes using label-free microscopy images, reducing subjectivity [9]. Additionally, staining techniques can help visualize specific features like inclusion bodies or syncytia that are hallmarks of viral infection [1].
Q3: I need a quantitative, high-throughput alternative to manual microscopy for CPE assessment. What are my options? Viability and cytotoxicity assays adapted to microplate readers are excellent for high-throughput screening (HTS) [38] [85].
- Luminescent Viability Assays: Measure cellular ATP levels (e.g., CellTiter-Glo). Viable cells maintain ATP, so antiviral compounds increase the signal [38] [85].
- Fluorescent Cytotoxicity Assays: Use dyes that enter dead/damaged cells (e.g., CellTox Green). Viral CPE increases fluorescence, which inhibitors reduce [38]. These methods provide robust, quantitative data with Z´ factors suitable for HTS, allowing you to screen thousands of compounds rapidly [38] [85].
Q4: What are the specific staining techniques to confirm different types of CPE? While some CPEs (like cell rounding or syncytia) can be seen in live cultures, others require staining [1]. Neutral red staining is a cost-effective method used in CPE assays to visualize viable cells [3]. For inclusion bodies, cells must be fixed and stained (e.g., with histological dyes) to observe these abnormal nuclear or cytoplasmic structures under light microscopy [1]. The specific stain used depends on the inclusion body's composition and location.
Table 1: Optimized CPE and Plaque Assay Conditions for Human Coronaviruses
| Virus | Assay Type | Cell Line | Seeding Density | Incubation Temperature (°C) | Incubation Time (Days) |
|---|---|---|---|---|---|
| HCoV-OC43 | CPE | RD | 2.5x10⁴ cells/mL | 33 | 4.5 |
| HCoV-OC43 | Plaque | RD | 2.5x10⁴ cells/mL | 33 | 4.5 |
| HCoV-229E | CPE | MRC-5 | 5x10⁴ cells/mL | 33 | 5.5 |
| HCoV-229E | Plaque | RD | 2.5x10⁴ cells/mL | 33 | 5.5 |
| HCoV-NL63 | CPE | Vero E6 | 2x10⁴ cells/mL | 37 | 4 |
| HCoV-NL63 | Plaque | Vero E6 | 2x10⁴ cells/mL | 37 | 4 |
Table 2: Common CPE Types and Associated Viruses
| CPE Type | Key Morphological Characteristics | Example Viruses |
|---|---|---|
| Total Destruction | Rapid shrinking, pyknosis, and detachment of the entire cell monolayer [1]. | Enteroviruses [1] |
| Subtotal Destruction | Partial detachment of the cell monolayer [1]. | Some Togaviruses, Picornaviruses [1] |
| Focal Degeneration | Localized areas (foci) of enlarged, rounded, refractile cells; spreads concentrically [1]. | Herpesviruses, Poxviruses [1] |
| Swelling and Clumping | Cells swell significantly and clump together before detaching [1]. | Adenoviruses [1] |
| Syncytium Formation | Fusion of plasma membranes, creating large cells with multiple nuclei (polykaryons) [1]. | Some Herpesviruses, Paramyxoviruses [1] |
| Inclusion Bodies | Abnormal structures in nucleus/cytoplasm; visible after staining [1]. | Various (e.g., Rabies, Cytomegalovirus) |
Experimental Protocols
Protocol 1: CPE Inhibition Assay for Antiviral Screening (96-well format)
This protocol is adapted for high-throughput screening of compounds against human coronaviruses in a BSL-2 facility [3].
- Cell Seeding: Seed susceptible cells (e.g., RD for HCoV-OC43, Vero E6 for HCoV-NL63) in flat-bottomed 96-well plates at densities specified in Table 1. Grow to confluence.
- Compound Application: Add serial dilutions of test and control compounds (e.g., remdesivir, GC-376) to the cells. Include virus-only and cell-only controls.
- Virus Infection: Infect cells with virus at a predetermined MOI (e.g., low MOI to avoid rapid CPE). Include mock-infected controls.
- Incubation: Incubate plates at the optimal temperature and time for the virus (see Table 1).
- Viability Staining and Quantification:
- Data Analysis: Calculate % CPE inhibition or % viability relative to controls. Determine EC₅₀ values for active compounds.
Protocol 2: Plaque Assay for Viral Titration and Confirmation of Antiviral Activity
This labor-intensive method is ideal as a secondary confirmatory assay [3].
- Cell Seeding: Seed appropriate cells in 6-well plates at the specified density (Table 1) and grow to confluence.
- Virus Infection and Inoculation: Serially dilute the virus sample. Aspirate media from cells and inoculate with virus dilutions. Adsorb for a specified time with periodic agitation.
- Overlay and Incubation: Remove the inoculum and cover the cell monolayer with a semi-solid overlay medium (e.g., carboxymethylcellulose). This restricts viral spread to neighboring cells, enabling plaque formation. Incubate for the time specified in Table 1.
- Plaque Visualization:
- Remove overlay, fix cells, and stain with a visible dye like crystal violet. Plaques appear as clear areas against a stained background of viable cells [3].
- Plaque Counting and Analysis: Count plaques to calculate the viral titer (PFU/mL). For antiviral testing, a reduction in plaque number or size indicates compound activity.
Workflow and Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Assays for CPE Research
| Item | Function/Application | Example Use |
|---|---|---|
| Neutral Red | A cost-effective and sensitive dye used to stain viable cells in CPE inhibition assays [3]. | Quantifying the number of living cells remaining after viral infection in a 96-well plate format [3]. |
| CellTiter-Glo Luminescent Assay | Measures cellular ATP levels as a biomarker for metabolically active, viable cells. Homogeneous "add-mix-measure" protocol [38] [85]. | High-throughput screening of compound libraries for antiviral activity; cell viability is reported by luminescence signal [38] [85]. |
| CellTox Green Fluorescent Assay | A fluorescent dye that binds to DNA in dead cells with compromised membranes. Measures cytotoxicity [38]. | Quantifying virus-induced cell death in real-time or endpoint assays; fluorescence increases with CPE [38]. |
| Check-Direct CPE Assay | A multiplex PCR for direct detection of carbapenemase-producing Enterobacteriaceae (CPE) from rectal swabs. Note: This is for bacterial CPE, not viral cytopathic effect [86]. | Rapid screening for antimicrobial resistance in clinical microbiology settings [86]. |
| Vero E6 & MRC-5 Cell Lines | Permissive cell lines commonly used for virus isolation and CPE assays [3]. | Propagating human coronaviruses (e.g., HCoV-NL63 in Vero E6) and observing virus-specific CPE [3]. |
Core Principles and Assay Selection
Cell viability and metabolic assays are fundamental tools in viral cytopathic effect (CPE) research, enabling the quantification of virus-induced cell damage and the assessment of antiviral compound efficacy. These assays function by measuring specific markers of cellular metabolic activity or health. The choice of assay is critical, as each has distinct mechanisms, advantages, and limitations that make it suitable for particular applications within a viral CPE research workflow.
The diagram above outlines the fundamental principles and primary applications of the three core assays in viral CPE research. The table below provides a detailed comparison of their key detection parameters to guide appropriate assay selection.
Table 1: Key Detection Parameters for Cell Viability Assays
| Parameter | MTT Assay | XTT Assay | ATP-based Luminescence |
|---|---|---|---|
| Detection Method | Colorimetric | Colorimetric | Bioluminescent |
| What is Measured | Metabolic activity (dehydrogenase enzymes) | Metabolic activity (dehydrogenase enzymes) | Cellular ATP content |
| Signal Type | Formazan crystals (insoluble) | Formazan dye (soluble) | Luminescent light |
| Readout Wavelength | 570 nm (reference: 630 nm) [87] [88] | 450-500 nm [89] | N/A (light intensity measured) [90] |
| Key Viability Indicator | Mitochondrial and cellular reductase activity [87] [91] | Mitochondrial dehydrogenase activity [89] | Presence of intracellular ATP [90] |
Troubleshooting Common Assay Problems
Even with a well-chosen assay, researchers often encounter technical challenges that can compromise data quality. This section addresses frequent issues across all platforms and provides targeted solutions for each assay type.
General Microplate Assay Issues
Many problems originate from the microplate format itself, affecting multiple assay types simultaneously.
Table 2: Troubleshooting General Microplate and Cell Culture Issues
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| High Background Noise | Autofluorescence from media components (e.g., phenol red, Fetal Bovine Serum) [92]. | Use phenol red-free media or alternative buffers like PBS+ for measurements. Measure from below the microplate if possible [92]. |
| Edge Effect (Evaporation in perimeter wells) | Uneven evaporation from outer wells during incubation [93]. | Use microplates designed to minimize evaporation. Pre-warm media to 37°C before adding. Use a humidified incubator. Consider a perimeter barrier or only using inner wells for critical assays [93]. |
| Meniscus Formation (Affects absorbance path length) | Hydrophilic plate surfaces; use of reagents like TRIS, acetate, or detergents [92]. | Use hydrophobic microplates (not tissue-culture treated for absorbance). Avoid detergents like Triton X. Fill wells to near capacity. Use a path length correction tool if available on your reader [92]. |
| High Inter-well Variability | Inconsistent cell seeding; low number of measurement flashes [92]. | Ensure homogeneous cell suspension when seeding. Use an orbital shaker during incubation if needed. Increase the number of flashes on your microplate reader (e.g., 10-50 flashes) to average out signal noise [92]. |
| Unexpected Cell Death | DMSO cytotoxicity; viral contamination [8] [93]. | Use the lowest possible DMSO concentration (typically <0.5-1.0%) and include matched vehicle controls for every drug dose [93]. Implement robust cell culture QC, including STR profiling and mycoplasma/viral testing (e.g., PCR for EBV, OvHV-2) [8]. |
Assay-Specific Troubleshooting
Each assay technology has its own unique set of potential pitfalls.
MTT Assay Specific Issues
Problem: Precipitate does not dissolve properly.
- Cause: Inefficient solubilization of formazan crystals [88].
- Solution: After removing MTT solution, add an appropriate solubilization solvent (e.g., DMSO, acidified isopropanol, or SDS solution) and ensure thorough mixing using an orbital shaker or pipetting. Gently pipette stubborn crystals to achieve a homogeneous solution [88].
Problem: Low or No Signal.
- Cause: Incorrect cell seeding density; insufficient MTT incubation time; degraded MTT reagent [91] [88].
- Solution: Optimize cell number for your specific cell line and experimental duration. Ensure cells are in logarithmic growth phase. Incubate typically for 2-4 hours (do not exceed 6 hours to avoid cell stress). Prepare fresh MTT stock solution and store protected from light and moisture [88].
XTT Assay Specific Issues
Problem: High background in blank wells.
Problem: Weak signal development.
- Cause: Insufficient number of metabolically active cells; incorrect concentration of the electron-coupling reagent (PMS) [89].
- Solution: Ensure the cell density is optimized so that the population is in the log phase of growth during the assay. Confirm that the XTT/PMS mixture is prepared in the correct ratio as specified in the protocol [89].
ATP-based Luminescence Assay Specific Issues
Problem: Rapid signal decay.
Problem: Inconsistent replication.
- Cause: Inadequate reagent mixing or uneven cell lysis [90].
- Solution: Ensure thorough mixing of the cell lysate and reagent, either by orbital shaking or pipetting, to create a homogeneous solution before reading. For 3D cultures, use an ATP assay specifically optimized for such models (e.g., CellTiter-Glo 3D) with stronger lytic capacity [90].
Experimental Protocols for Viral CPE Research
Standardized protocols are essential for generating reliable and reproducible data in viral infection models. The following workflows are optimized for a 96-well plate format.
MTT Assay Protocol for Assessing Viral CPE
This protocol measures the reduction in metabolic activity of cells due to viral infection [87] [88].
Workflow Overview:
Detailed Steps:
- Cell Seeding: Seed cells in a 96-well tissue culture-treated microplate at an optimized density (e.g., 7.5 x 10³ cells/well for many lines) in growth medium and culture until 70-90% confluent [93] [88].
- Viral Infection: Infect cells with the virus at various multiplicities of infection (MOI). Include controls: uninfected cells (cell control) and virus-only background (virus control). Incubate for the desired period to allow CPE development.
- MTT Addition: Prepare MTT stock solution (5 mg/mL in sterile PBS) [88]. Add 50 μL of this solution directly to each well containing 100 μL of culture medium (final concentration ~0.2-0.5 mg/mL) [87].
- Incubation: Incubate the plate for 2 to 4 hours at 37°C in a CO₂ incubator. Monitor for the appearance of purple formazan crystals under a microscope [88].
- Solubilization: Carefully aspirate the spent medium and MTT solution without disturbing the crystals. Add 100-150 μL of solubilization solvent (e.g., DMSO, acidified isopropanol, or 10% SDS in 0.01 M HCl) to each well [87] [88].
- Signal Measurement: Wrap the plate in foil and shake gently on an orbital shaker for 10-15 minutes to fully dissolve the crystals. Measure the absorbance at 570 nm with a reference wavelength of 630 nm using a microplate reader [88].
XTT Assay Protocol for Viral Cytotoxicity
The XTT assay is ideal for high-throughput screening of antiviral compounds as it does not require a solubilization step [89].
Workflow Overview:
Detailed Steps:
- Cell Preparation: Seed cells (e.g., 5 x 10⁴ cells/well) in a 96-well plate and culture overnight [89].
- Infection/Treatment: Infect cells with the virus and/or treat with the antiviral compound of interest.
- Incubation: Incubate cell cultures for the required time to observe CPE or drug effect (e.g., 24 hours for rapid cytotoxicity) [89].
- XTT Labeling Mixture Preparation: Thaw the XTT reagent and the electron-coupling reagent (PMS). For one 96-well plate, mix 5 mL of XTT labeling reagent with 0.1 mL of PMS reagent. Prepare this mixture immediately before use [89].
- Reagent Addition and Incubation: Add 50 μL of the XTT labeling mixture to each well. Incubate the plate for 4 hours (for proliferation) or up to 18 hours (for cytotoxicity) at 37°C in a CO₂ incubator [89].
- Absorbance Measurement: Measure the absorbance of the formazan product using a microplate reader. The optimal wavelength is between 450-500 nm, with a reference wavelength above 650 nm [89].
ATP-based Luminescence Assay Protocol for Viral CPE
This protocol offers high sensitivity for quantifying cell viability in viral infection studies and is amenable to high-throughput screening [90].
Detailed Steps:
- Cell Culture and Infection: Seed and infect cells in a white-walled 96-well plate (optimal for luminescence signal reflection) using the same principles as the MTT protocol.
- Equilibration: Remove the plate from the incubator and allow it to equilibrate to room temperature for approximately 30 minutes. This ensures consistent luminescent signal generation.
- Reagent Preparation: Thaw the CellTiter-Glo reagent according to the manufacturer's instructions.
- Reagent Addition: Add a volume of CellTiter-Glo Reagent equal to the volume of cell culture medium present in each well (e.g., add 100 μL of reagent to 100 μL of medium containing cells).
- Mixing and Lysis: Mix the contents thoroughly for 2 minutes on an orbital shaker to induce cell lysis and ensure homogeneous distribution of the luminescent signal.
- Signal Stabilization: Incubate the plate at room temperature for 10 minutes to stabilize the luminescence signal.
- Luminescence Measurement: Record the luminescence using a plate-reading luminometer or a microplate reader with luminescence detection capabilities. The signal is stable for several hours [90].
The Scientist's Toolkit: Research Reagent Solutions
Selecting the right reagents and materials is fundamental to assay success. The following table catalogs essential solutions for performing these assays in the context of viral research.
Table 3: Essential Research Reagents and Materials
| Item | Function / Description | Example Products / Notes |
|---|---|---|
| XTT Assay Kit | A complete kit containing XTT salt and an electron-coupling reagent (PMS) for ready-to-use solution preparation. | Cell Proliferation Kit II (XTT) [89]. |
| MTT Reagent | The yellow tetrazolium salt substrate. Can be purchased as a powder or as part of a kit with solubilization solution. | MTT powder (e.g., Thiazolyl Blue Tetrazolium Bromide) or MTT-based kits (e.g., CellTiter 96) [87]. |
| ATP Assay Kits | A single, ready-to-use reagent for high-throughput viability testing based on ATP quantification. | CellTiter-Glo Luminescent Cell Viability Assay [90]. |
| Solubilization Solvents | Used to dissolve the water-insoluble formazan crystals produced in the MTT assay. | DMSO, Acidified Isopropanol (0.04N HCl), or 10% SDS solution [87] [88]. |
| Serum-Free Medium | Used to dilute and add MTT to cells, preventing interference from serum components that can skew results [88]. | DMEM, RPMI 1640, or other basal media without serum. |
| 96-well Microplates | The standard platform for cell-based assays. Choice of plate color matters: clear for absorbance, white for luminescence, black for fluorescence. | Tissue culture-treated, flat-bottom plates [92] [88]. |
| Microplate Reader | Instrument for detecting assay signals. Requires absorbance capability for MTT/XTT and luminescence capability for ATP assays. | Readers with temperature control and automatic gain adjustment are advantageous [92]. |
Frequently Asked Questions (FAQs)
Q1: My MTT assay shows high variability between replicates. What steps can I take to improve consistency?
- A: High variability often stems from technical inconsistencies. To improve replicability:
- Ensure a homogeneous cell suspension when seeding by pipetting or gentle vortexing immediately before dispensing.
- Use multi-channel pipettes for reagent addition.
- Optimize cell seeding density to avoid over-confluence, which can lead to nutrient depletion and increased variability [93].
- Increase the number of flashes on your microplate reader (e.g., 10-50 flashes) to average out signal noise [92].
- Include matched DMSO vehicle controls for every drug concentration to account for solvent effects [93].
Q2: Can I use the MTT assay for real-time monitoring of viral CPE?
- A: No, the MTT assay is an endpoint assay. The process of MTT reduction is cytotoxic to cells, and the formazan crystals must be solubilized before reading, which terminates the experiment [87] [91]. For real-time monitoring of cell health during viral infection, consider kinetic assays like the RealTime-Glo MT Cell Viability Assay or continuous ATP monitoring assays [90].
Q3: Why is my ATP assay signal low even when many cells appear viable under the microscope?
- A: A discrepancy between visual inspection and ATP signal can occur due to several factors:
- Metabolic Quiescence: The cells may be alive but in a metabolically quiescent state (e.g., contact-inhibited), leading to low ATP pools.
- Incomplete Lysis: Ensure the lysis reagent is thoroughly mixed, especially with 3D culture models. Consider using an ATP assay specifically formulated for 3D cultures, which has stronger detergents [90].
- Reagent Degradation: Check the integrity and storage conditions of the ATP assay reagent.
Q4: How does viral contamination specifically impact these viability assays?
- A: Viral contamination, such as from Epstein Barr virus (EBV) or Ovine Herpesvirus 2 (OvHV-2), can severely compromise assay results and research integrity [8]. These contaminants can:
- Alter cellular metabolism, directly affecting the signal in MTT and XTT assays.
- Cause cytopathic effects (CPE), leading to cell death and reduced signal in all viability assays, which can be misinterpreted as a treatment effect.
- It is crucial to implement robust authentication and quality control measures, including STR profiling and routine testing for mycoplasma and common viral contaminants, to ensure the validity of your experimental models [8].
Troubleshooting Guide: Common AI-CPE Classification Issues
This guide addresses specific problems you might encounter when implementing deep learning models for label-free Cytopathic Effect (CPE) classification in viral cell culture research.
FAQ 1: My AI model trains but fails to classify CPE in new images. What should I check?
This common issue often stems from problems with training data or model configuration.
- Confirm Recipe/Model Is Active: Navigate to your model management interface and ensure your classification recipe is marked as active. Only one recipe can be active at a time [94].
- Verify Classifier Setup: Open your model's configuration and confirm that at least one Region of Interest (ROI) is defined and that a classifier block has been added to it. Check for any errors or warnings in the ROI configuration [94].
- Check Training Data Quality: Go to the classifier tab and verify that sufficient images have been uploaded and accurately labeled for at least two classes (e.g., "CPE" and "No CPE"). Ensure the "Train" button was clicked and completed successfully, and the status reads "Trained," not "Needs Training" or "Not Ready" [94]. If trained in a "Fast Mode" for testing, accuracy may be too low for production; retrain in "Accurate Mode" [94].
- Restart the System: If everything seems configured correctly but the classifier still doesn't respond, a simple restart can help. Power cycle the camera or analysis system, wait 20–30 seconds for a complete reboot, and test again with a new trigger. This reloads the model and classifier runtime from scratch [94].
FAQ 2: My viral stocks are producing inconsistent or weak CPE, leading to poor AI classification. How can I stabilize infectivity?
The consistency and reliability of CPE-based assays depend heavily on the stability of the virus's infectious properties [95].
- Avoid Freeze-Thaw Cycles: Viral stocks can be sensitive to freeze-thaw cycles, with reports of titer losses from 5% to 50% per cycle [44]. To preserve infectivity and ensure reproducible CPE, prepare single-use aliquots of the virus in suspension that are appropriately sized for your experiment. Virus stocks should not be refrozen once thawed [95].
- Check for Packaging Cell Debris: If you are producing your own viral vectors, remove packaging cell debris before concentration or use. This can be done by filtering the virus solution (through a 0.45 µm or 0.22 µm filter) or a low-speed centrifugation step (5 minutes at 300-500 g) to avoid contaminating your transduction [44].
- Concentrate Low-Titer Stocks: If you have low titers, you can concentrate your virus by ultracentrifugation of the viral stock, followed by resuspension of the collected particles in a smaller volume of cold, sterile PBS [44].
- Enhance Virus-Cell Contact: Use reagents like Polybrene (a cationic reagent) to increase transduction efficiency by reducing repulsive electrostatic forces between the virus and cell membrane. It can increase efficiency by 10-fold, but it is highly sensitive to freeze-thaw cycles and should be stored in single-use aliquots. For cells sensitive to Polybrene toxicity (e.g., hematopoietic or primary cells), fibronectin is an alternative [44].
FAQ 3: I've followed the protocol, but my transductions are inefficient and no CPE is observed. What are my "Hail Mary" options?
When standard optimization fails, consider these steps to diagnose the problem.
- Check for Viral Vector Rearrangements: Depending on the composition of your viral vector, it may undergo genomic rearrangements during replication. To avoid this, try amplifying the viral vector with bacteria designed to minimize rearrangements, such as NEB Stable, or use a standard strain like DH5α grown at 30°C instead of 37°C. Perform a diagnostic restriction enzyme digest and compare it to reliable controls to check the integrity of your viral genome [44].
- Verify Viral Production in Packaging Cells: Check if the virus is being generated by your transfected packaging cells. If the packaging cells have been successfully transfected and produced infectious virus, they may themselves become infected. Approximately 72 hours after transfection, you can attempt to select them with the antibiotic whose resistance gene is encoded in the viral vector. A surviving population of about 20–50% of the cells after 1–3 days suggests successful viral production [44].
- Optimize Cell Line and Assay Conditions: The sensitivity of CPE detection can vary greatly depending on the virus-host system [95]. For instance, in plaque assays, the use of Vero cells—particularly low-passage Vero E6 cells—is critical as they influence plaque morphology, size, and clarity [95]. Extensively optimize parameters like cell seeding density, growth medium, and the timing of virus inoculation relative to cell seeding [95].
Experimental Protocol: Implementing the AIRVIC Deep Learning Framework
The following methodology is adapted from the AIRVIC (AI Recognition of Viral CPE) system, which utilizes Convolutional Neural Networks (CNNs) for label-free virus classification [9].
Dataset Generation and CPE Imaging
- Cell Culture and Virus Infection: Propagate your target viruses in permissive cell lines (e.g., Vero or MDBK cells). Calculate the multiplicities of infection (MOIs) using assays like TCID₅₀. Infect cells at various MOIs (e.g., from 0.0001 to 1.0) to capture a range of CPE progression [9].
- Image Acquisition: Collect time-lapse microscopy images at various magnifications (e.g., 20X) across multiple post-infection time points (e.g., from 8 hours to 150 hours). The goal is to capture the full dynamic range of CPE, from early subtle changes to complete cell destruction. The AIRVIC study collected 40,369 images across various conditions, highlighting the need for a large and diverse dataset for robust model training [9].
- Example CPE Manifestations: Be prepared to capture diverse CPE phenotypes, which can include [9]:
- Cell rounding and enlargement
- Syncytia (cell fusion) formation
- Vacuolation
- Cell lysis and detachment
- Cytoplasmic inclusions and nuclear alterations
AI Model Architecture and Training (ResNet50)
- Model Selection: The AIRVIC system employed ResNet50 as its primary convolutional neural network architecture, comparing it against other architectures like ResNet18, MobileNetV2, and YGNet to balance complexity and predictive capability [9].
- Handling Data Imbalance: In initial training phases, you may encounter high accuracy but low F1 scores (e.g., 0.8439 accuracy vs. 0.4576 F1), emphasizing the effect of dataset imbalance. Mitigate this by employing strategies like oversampling minority classes or using weighted loss functions during training [9].
- Training and Validation: Split your image dataset into training, validation, and test sets. Use the training set to teach the model to associate image features with specific CPE patterns or virus classes. Use the validation set to tune hyperparameters and avoid overfitting.
Performance Evaluation and Validation
- Quantitative Metrics: Evaluate your model using standard metrics such as Accuracy, F1-score, and Area Under the Receiver Operating Characteristic Curve (AUROC) [9] [96].
- Benchmarking: Compare the performance of your AI-based CPE classification against traditional methods like plaque assays or TCID₅₀ in terms of speed, accuracy, and reproducibility [95].
- Hierarchical Classification: For complex tasks, consider a hierarchical model structure. AIRVIC demonstrated that classification accuracy for bovine viruses in MDBK cells was 87.61%, but dropped to 63.44% when the cell line was not specified, highlighting the importance of context in model design [9].
Performance Data for AI-Based CPE Detection
The table below summarizes quantitative performance data from relevant studies to set realistic expectations for model deployment.
| Virus / System | Cell Line | Task | Performance Metric | Result | Note |
|---|---|---|---|---|---|
| BoGHV-4 (DN-599 strain) [9] | MDBK | CPE Detection | Accuracy | 100% | Highest accuracy among tested models |
| BoGHV-4 (MOVAR 33/63 strain) [9] | Vero | CPE Detection | Accuracy | 87.99% | Lowest accuracy among tested models |
| Bovine Viruses [9] | MDBK | Virus Classification | Multi-class Accuracy | 87.61% | Cell line specified |
| Bovine Viruses [9] | Not Specified | Virus Classification | Multi-class Accuracy | 63.44% | Cell line not specified |
| DeepVirusClassifier [96] | in silico | SARS-CoV-2 Sequence Classification | Sensitivity | >99% | For sequences with <2000 mutations |
The Scientist's Toolkit: Essential Research Reagent Solutions
This table details key materials and reagents critical for successful viral CPE research and AI model development.
| Item Name | Function / Application | Key Consideration |
|---|---|---|
| Vero / Vero E6 Cells [9] [95] | Permissive cell line for virus replication and CPE formation (e.g., SARS-CoV-2, bovine viruses). | Low-passage Vero E6 cells are critical for consistent plaque morphology in assays [95]. |
| Polybrene [44] | Cationic reagent that enhances viral transduction efficiency by promoting virus adsorption to the cell membrane. | Highly sensitive to freeze-thaw; store in single-use aliquots. Can be toxic to sensitive cells. |
| Fibronectin [44] | Membrane-interacting protein that enhances transduction efficiency, especially for primary or sensitive cells. | An alternative to Polybrene for cells susceptible to cytotoxicity. |
| Serum-Free Media (SFM) [97] | Supports cell growth and virus production while reducing lot-to-lot variability and risk of adventitious agents. | Requires adaptation of cells. Media choice (e.g., DMEM, OptiPRO) strongly impacts viral titers. |
| Fixed-Bed Bioreactor (e.g., iCELLis) [97] | Scalable production system for viruses using adherent cells, offering a large surface area in a small footprint. | Facilitates manufacturing with reduced cost and footprint compared to roller bottles. |
| Agilent xCELLigence RTCA [95] | Instrument system for label-free, real-time monitoring of CPE via cellular impedance. | Provides continuous, quantitative kinetic data, overcoming the subjectivity of endpoint assays. |
| Agilent BioTek Cytation [95] | Automated cell imaging multimode reader for objective visualization and quantification of plaques or CPE. | Reduces time and subjectivity associated with manual counting in plaque assays. |
Experimental Workflow for AI-Powered CPE Classification
The diagram below outlines the core workflow for developing and deploying a deep learning model for label-free CPE classification.
AI-Powered CPE Classification Workflow
Troubleshooting Algorithm for Classification Failure
Follow this logical decision tree to systematically diagnose issues when your AI classifier fails to run or produce results.
Classifier Troubleshooting Algorithm
The AI Recognition of Viral CPE (AIRVIC) system represents a transformative advancement in virological diagnostics, leveraging artificial intelligence to automate the detection and classification of virus-induced cytopathic effects (CPEs). CPEs refer to the structural changes in host cells resulting from viral infection, including cell rounding, swelling, shrinkage, lysis, and syncytia formation [27] [5]. Traditional CPE identification relies on labor-intensive manual observation by trained personnel, introducing subjectivity and requiring additional confirmatory tests [98] [9]. AIRVIC addresses these limitations through a web-based, label-free platform that provides unbiased infectivity scoring, facilitates viral isolation, and enables high-throughput antiviral efficacy testing [98] [9].
Developed to support the optimization of viral cell culture research, AIRVIC utilizes convolutional neural networks (CNNs) with ResNet50 as its primary architecture [98] [9]. The system was trained on an extensive dataset of 40,369 microscopy images at various magnifications, encompassing CPEs induced by SARS-CoV-2, BAdV-1, BPIV3, BoAHV-1, and two strains of BoGHV-4 in Vero and MDBK cell lines [9]. This comprehensive training enables AIRVIC to distinguish viral CPEs from morphological changes due to non-viral factors like cellular aging, significantly reducing the need for supplementary post-isolation procedures and accelerating research workflows in virology and drug development [9].
Experimental Protocols & Performance Data
Core Methodology and Training
The AIRVIC system was developed using a rigorous experimental protocol to ensure robust performance across diverse viral pathogens and cell lines. The foundational methodology involved:
- Virus Propagation and Cell Culture: Bovine viruses were propagated in MDBK cells, while SARS-CoV-2 was cultured in Vero cells. Virus stocks were titrated using TCID₅₀ assays to determine the multiplicities of infection (MOIs) for subsequent infections [9].
- Comprehensive Image Acquisition: Data collection spanned various MOIs (ranging from 0.0001 to 1.0) and multiple time points (from 8 to 150 hours post-infection). This approach captured the temporal progression of CPEs across different viral strains and cell lines, resulting in a dataset of 40,369 microscopy images [9].
- Architecture Selection and Training: After comparative analysis of architectures including ResNet18, ResNet50, MobileNetV2, and YGNet, ResNet50 was selected as the primary CNN architecture. The models were trained to perform both binary classification (CPE detection) and multi-class classification (virus identification) [9].
Key Performance Metrics
AIRVIC demonstrated variable but generally high accuracy in detecting and classifying virus-specific CPEs, with performance metrics summarized in the table below.
Table 1: AIRVIC Performance in Virus-specific CPE Detection
| Virus Strain | Host Cell Line | Task | Performance Metric | Value |
|---|---|---|---|---|
| BoGHV-4 DN-599 | MDBK | CPE Detection | Accuracy | 100% [98] [9] |
| BoGHV-4 MOVAR 33/63 | Vero | CPE Detection | Accuracy | 87.99% [98] [9] |
| Multiple Bovine Viruses | MDBK | Virus Classification | Multi-class Accuracy | 87.61% [9] |
| Multiple Bovine Viruses | Not Specified | Virus Classification | Multi-class Accuracy | 63.44% [9] |
The data reveals several critical insights. AIRVIC achieved perfect accuracy for the BoGHV-4 DN-599 strain in MDBK cells, demonstrating the potential for expert-level diagnostic performance under optimal conditions [98] [9]. Performance variation across virus strains and cell lines highlights the biological complexity of CPE manifestation; the system struggled more with the BoGHV-4 MOVAR 33/63 strain in Vero cells [98]. Furthermore, the significant drop in classification accuracy when the cell line was not specified underscores the critical importance of cell context in virological analysis and the hierarchical design of the AIRVIC system, which optimally functions with known cell line parameters [9].
Experimental Workflow
The following diagram illustrates the end-to-end experimental workflow for utilizing the AIRVIC system in a virology research setting.
Technical Support Center
Troubleshooting Guides
Issue 1: Low CPE Detection Accuracy in Specific Cell-Virus Combinations
- Problem: AIRVIC model performance is suboptimal (e.g., lower accuracy similar to the 87.99% observed for BoGHV-4 MOVAR 33/63 in Vero cells) [9].
- Investigation Steps:
- Verify the health and confluence of the host cell monolayer prior to infection. Inadequate confluence (near 100% is ideal) can obscure CPE visualization and analysis [27].
- Confirm the viral titer (TCID₅₀) and MOI used. Deviation from the optimal range used in AIRVIC's training data (MOI of 0.0001 to 1.0) can lead to atypical CPE progression [9].
- Check image quality. Ensure microscopy images are captured at the magnifications used for training and are free of significant artifacts or contamination [9].
- Resolution:
- Adhere strictly to the protocol for host cell seeding density to ensure a uniform monolayer [27].
- Titrate the virus stock to determine the correct MOI for your specific experimental setup before running AIRVIC analysis.
- If the issue persists, note that AIRVIC's hierarchical structure is most accurate when the cell line is specified. Retraining or fine-tuning the model with additional, domain-specific data may be necessary for novel cell-virus combinations [98] [9].
Issue 2: Inconsistent Model Performance Across Time Points
- Problem: CPE detection results vary significantly when images from different post-infection time points are analyzed.
- Investigation Steps:
- Review the time points used. AIRVIC was trained on images captured from 8 to 150 hours post-infection. Using time points outside this range may yield unpredictable results [9].
- Analyze the CPE progression. Early time points may exhibit subtle, non-diagnostic morphological changes, while late time points might show complete cell destruction that is less specific.
- Resolution:
- Follow a multi-point time-course imaging protocol, as used in AIRVIC's development, to capture the full spectrum of CPE development [9].
- For quantitative analyses, standardize the post-infection time for image capture across all experiments to ensure consistency.
Issue 3: Poor Virus Classification Results
- Problem: The system detects CPE but fails to correctly classify the virus, especially in a multi-class setting.
- Investigation Steps:
- Confirm the cell line is correctly specified. Virus classification accuracy drops significantly (e.g., from 87.61% to 63.44%) when the cell line is not provided, as CPE morphology is cell-context dependent [9].
- Verify the virus strains in use are among those the model was trained on (SARS-CoV-2, BAdV-1, BPIV3, BoAHV-1, BoGHV-4). The model cannot reliably classify untrained viruses.
- Resolution:
- Always provide the cell line information when using the AIRVIC platform.
- For virus strains not in the original training set, leverage AIRVIC's CPE detection capability and use traditional methods for confirmatory virus identification.
Frequently Asked Questions (FAQs)
Q1: What are the specific CPE features that AIRVIC detects? AIRVIC is trained to identify a range of virus-induced morphological changes, including cell rounding, swelling, shrinkage, lysis, detachment, and syncytia formation (multinucleated giant cells) [27] [5]. The precise features vary by virus; for example, SARS-CoV-2 in Vero cells causes rounding, swelling, and loss of monolayer, while paramyxoviruses like BPIV3 often induce syncytia [9] [5].
Q2: What is the throughput of the AIRVIC system compared to manual methods? AIRVIC automates a process that is traditionally manual and subjective. While a direct time comparison is not provided in the results, automated image cytometry systems like the Celigo (which shares conceptual similarities with AIRVIC's analysis step) can image and analyze a full 96-well plate in under 10 minutes [27]. This represents a substantial increase over the manual observation of each well under a microscope.
Q3: Can AIRVIC be used with cell lines or viruses not listed in the original study? The current AIRVIC models are optimized for the specific virus-cell combinations used in its training. Using it with untrained viruses or cell lines will likely result in reduced accuracy. However, the study highlights AIRVIC's adaptable hierarchical structure, suggesting it can be retrained or fine-tuned with new datasets to expand its capabilities [98] [9].
Q4: What are the minimum technical requirements for generating images compatible with AIRVIC? The system was trained on microscopy images at various magnifications [98]. For optimal performance, users should ensure their imaging conditions (e.g., magnification, contrast method) are consistent with those used during model development. The use of brightfield imaging without labeling is sufficient [9] [27].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and reagents essential for conducting CPE analysis experiments compatible with the AIRVIC system.
Table 2: Essential Research Reagents for Viral CPE Analysis
| Item | Function/Description | Example in AIRVIC Context |
|---|---|---|
| Vero Cells | A cell line derived from African green monkey kidney epithelial cells; highly permissive to a wide range of viruses. | Used for propagation of SARS-CoV-2 and various bovine viruses (BoGHV-4, BAdV-1, etc.) to study virus-specific CPEs [9]. |
| MDBK Cells | (Madin-Darby Bovine Kidney) A bovine-specific cell line critical for isolating and growing bovine respiratory viruses. | Used for propagation of bovine viruses (BoAHV-1, BPIV3, BAdV-1, BoGHV-4) to study relevant CPEs for veterinary virology [9]. |
| Virus Stocks | Characterized stocks of viruses for infection studies, with titers determined by assays like TCID₅₀. | AIRVIC was validated using SARS-CoV-2, BAdV-1, BPIV3, BoAHV-1, and two strains of BoGHV-4 [98] [9]. |
| Cell Culture Media & Reagents | Provides nutrients and the appropriate environment for host cell growth and virus replication. | Essential for maintaining Vero and MDBK cell monolayers before and during viral infection [9]. |
| Image Cytometer / Microscope | Instrument for capturing digital images of cell monolayers for quantitative analysis of CPE. | AIRVIC analyzes microscopy images. Automated image cytometers (e.g., Celigo) enable high-throughput, quantitative CPE analysis in brightfield [27]. |
System Architecture and Data Flow
The logical flow of data within the AIRVIC system, from image input to diagnostic output, is visualized in the following diagram.
The accurate detection of viruses is a cornerstone of virology research, clinical diagnostics, and drug development. The selection of an appropriate detection method directly impacts the reliability, efficiency, and translational value of experimental outcomes. This technical support center focuses on four principal methodologies: Cytopathic Effect (CPE)-based assays, Polymerase Chain Reaction (PCR)-based methods, Immunoassays, and Reporter Cell Lines. Each technique operates on distinct principles, offering unique advantages and facing specific limitations. CPE-based methods rely on the visual observation of virus-induced morphological changes in cell cultures, representing one of the oldest and most direct forms of viral detection [66]. In contrast, PCR-based techniques amplify and detect specific viral nucleic acid sequences with exceptional sensitivity, while immunoassays utilize antigen-antibody interactions to identify viral proteins or host immune responses [66] [99]. Reporter cell lines, a more recent advancement, employ genetically engineered cells that produce a measurable signal, such as luminescence or fluorescence, upon viral infection [66] [100].
Understanding the comparative performance characteristics of these methods is crucial for optimizing viral cell culture research. This guide provides a structured framework for method selection, detailed protocols, and targeted troubleshooting to address common experimental challenges. The content is specifically designed to support researchers, scientists, and drug development professionals in enhancing the accuracy, reproducibility, and efficiency of their virological studies. By framing this information within the context of CPE research optimization, we aim to provide a practical resource that bridges foundational techniques with modern technological advancements.
Method Comparison & Selection Guide
The choice of a viral detection method should be guided by the specific research question, considering factors such as the need to detect infectious versus non-infectious virus, required throughput, turnaround time, and available resources. The following table provides a quantitative comparison of the four core methods to aid in this decision-making process.
Table 1: Comparative Performance of Viral Detection Methods
| Method | Detection Target | Key Advantage | Key Limitation | Typical Workflow Duration | Sensitivity (Limit of Detection) |
|---|---|---|---|---|---|
| CPE-Based Assays | Live, infectious virus via cell death [101] | Confirms infectious virus; no specialized equipment needed [66] | Time-consuming; subjective; cannot detect non-cytopathic viruses [66] | 2 to 6 days [66] [101] | Varies by virus (e.g., ~100 TCID₅₀ for Tulane virus) [101] |
| PCR-Based Methods | Viral nucleic acids (DNA or RNA) [66] | High sensitivity and speed; can be quantitative [102] [103] | Cannot differentiate between infectious and non-infectious virus [66] [101] | Several hours to 1 day [102] | Very high (e.g., 1-10 PFU/mL for RSV via RT-PCR) [103] |
| Immunoassays | Viral proteins or host antibodies [66] [99] | High specificity; can indicate immune response or recent infection [66] [104] | Requires specific, high-quality antibodies; potential for cross-reactivity [66] | Several hours to 1 day [99] | Moderate to High (e.g., ~10⁻⁹ M for ELISA) [100] |
| Reporter Cell Lines | Live virus via induced signal (e.g., luminescence) [66] [100] | Objective, quantitative readout; high-throughput compatible [100] | Complex and costly cell line development [66] [100] | 1 to 3 days | Very High (e.g., ~10⁻¹² M for RGA) [100] |
Selection Guidance
- For Determining Infectious Viral Titers: If the research question requires confirmation of live, replicating virus, CPE-based assays (Plaque or TCID₅₀) are the traditional standard. Reporter cell lines offer a more quantitative and often faster alternative for this purpose [66] [101].
- For Maximum Sensitivity and Speed: When the priority is to detect minimal amounts of viral material quickly, such as in early infection or for viruses that are difficult to culture, PCR-based methods are superior [102] [103].
- For High-Throughput Drug Screening: Reporter gene assays are ideal for screening large compound libraries due to their objective, luminescence or fluorescence-based readouts and compatibility with automated systems [100].
- For Diagnosing Immune Response: To detect past exposure or characterize the host's immune response to a virus, immunoassays that detect IgM and IgG antibodies are the most appropriate tools [66] [104].
Method-Specific Troubleshooting Guides
CPE-Based Assays
Table 2: Troubleshooting for CPE-Based Assays
| Problem | Possible Cause | Solution |
|---|---|---|
| No CPE Observed | Virus does not replicate in cell line used [66]. | Use a more susceptible or permissive cell line (e.g., Vero, HEK293, MDCK) [66]. |
| Low multiplicity of infection (MOI). | Increase the virus inoculum or concentration. | |
| Incorrect incubation conditions. | Verify and optimize temperature, CO₂ levels, and culture medium. | |
| High Background Cell Death | Bacterial or fungal contamination [66]. | Use antibiotic-antimycotic solutions in media; practice sterile technique. |
| Toxic substances in clinical specimen [66]. | Dilute the sample or use purification methods (e.g., filtration). | |
| Poor cell health. | Use low-passage, actively dividing cells; optimize seeding density. | |
| Variable or Inconsistent CPE | Inconsistent cell seeding. | Standardize cell counting and seeding protocols. |
| Uneven infection. | Ensure proper rocking/swirling of plate during virus adsorption. | |
| Subjective CPE scoring. | Train multiple observers; use standardized scoring criteria; employ staining (e.g., crystal violet) to visualize plaques more clearly. |
PCR-Based Methods
Table 3: Troubleshooting for PCR-Based Methods
| Problem | Possible Cause | Solution |
|---|---|---|
| No Amplification | Poor DNA/RNA template quality or quantity [105]. | Check template purity and concentration (A260/A280); make new primer solutions [105]. |
| Inhibitors present in sample. | Re-purify nucleic acids; use a dilution of the template. | |
| Incorrect annealing temperature. | Perform a temperature gradient PCR to optimize Tm [105]. | |
| Non-Specific Bands/Peaks | Primer-dimer formation or mis-priming [105]. | Increase annealing temperature; use hot-start Taq polymerase; follow primer design rules (avoid repeats, self-complementarity) [105]. |
| Excessive primer or template concentration. | Lower primer concentration; decrease the number of cycles [105]. | |
| False Positives (Contamination) | Carryover of amplicons or plasmid DNA [105]. | Use separate pre- and post-PCR workstations; use uracil-DNA glycosylase (UNG) in qPCR mix [103]; use sterile tips. |
| High Variability Between Replicates | Pipetting inaccuracies [105]. | Calibrate pipettes; use master mixes for reaction consistency [105]. |
| Improper mixing of reagents. | Vortex and centrifuge all reagents before use. |
Immunoassays (e.g., ELISA)
Table 4: Troubleshooting for Immunoassays
| Problem | Possible Cause | Solution |
|---|---|---|
| High Background Signal | Non-specific binding [99] [104]. | Optimize blocking buffer (e.g., BSA, non-fat milk); increase wash stringency (e.g., add Tween-20 to PBS) [99]. |
| Cross-reactivity of secondary antibody [99]. | Use an adsorption-verified secondary antibody. | |
| Weak or No Signal | Insufficient antigen or antibody [106]. | Check reagent concentrations; increase incubation times. |
| Inactive enzyme conjugate [106]. | Prepare fresh substrate working solution; ensure proper storage of conjugates. | |
| Incorrect wash buffer. | Verify wash buffer composition and pH. | |
| High Well-to-Well Variation | Inconsistent washing [104]. | Use an automated plate washer or standardize manual washing technique. |
| Bubbles in wells during reading. | Centrifuge plate briefly before reading; remove bubbles with a needle. |
Reporter Cell Lines
Table 5: Troubleshooting for Reporter Cell Lines
| Problem | Possible Cause | Solution |
|---|---|---|
| Low Signal-to-Noise Ratio | Low transfection efficiency (for transient assays) [106]. | Optimize transfection conditions using a fluorescent protein control; use high-quality plasmid DNA [106]. |
| Low promoter activity [106]. | Use stronger or different inducible promoters; incubate cells longer after treatment [106]. | |
| Substrate auto-oxidation or degradation [106]. | Protect substrate from light and air; prepare fresh working solution; avoid repeated freeze-thaw cycles [106]. | |
| High Signal in Uninfected Controls | Contamination of control sample [106]. | Use new sample aliquots; change pipette tips after each well [106]. |
| Leaky promoter expression. | Use a tighter inducible promoter system; include transcriptional repressors in the construct design. | |
| High Assay Variability | Unstable cell line [100]. | Use low-passage, cryopreserved stocks; generate clonal cell lines using CRISPR/Cas9 for targeted gene integration to ensure consistency [100]. |
| Inconsistent cell plating. | Standardize cell counting and seeding density. |
Frequently Asked Questions (FAQs)
Q1: Can PCR be used to measure infectious viral titer? No, standard PCR detects viral nucleic acids but cannot distinguish between genomes from infectious virions and those from degraded virus or free nucleic acids [66] [101]. To approximate infectivity with molecular methods, pre-treatment steps like RNase exposure (for RNA viruses) can be used to digest unprotected RNA, ensuring that only encapsidated genomes are amplified [101]. However, for a definitive measure of infectious units, cell-based methods (CPE or reporter assays) remain the gold standard [101] [103].
Q2: My reporter assay has high background. What are the first steps to fix this? First, ensure you are using the appropriate microplate. Black plates are recommended over white plates for luminescence assays to reduce cross-talk and background, despite yielding lower raw RLU values [106]. Second, check the serum in your culture media, as certain types (e.g., donor adult bovine serum) can inhibit some luciferases and increase background [106]. Finally, prepare fresh substrate working solution immediately before use, as auto-oxidation over time is a common cause of high background [106].
Q3: When should I choose a TCID₅₀ assay over a plaque assay? The TCID₅₀ assay is often preferred for viruses that do not form clear, distinct plaques [101]. It is also less labor-intensive and can be more easily adapted to higher-throughput formats. However, the plaque assay provides a direct count of plaque-forming units (PFU) and is generally considered less variable. A study on Tulane virus found a strong but not 1:1 correlation between the two, with 1 PFU being equivalent to approximately 6.69 TCID₅₀ units, highlighting that the units are not directly interchangeable [101].
Q4: What is the key advantage of reporter cell lines over traditional CPE reading? The primary advantage is the replacement of a subjective, qualitative measurement (visual inspection of cell death) with an objective, quantitative data point (luminescence or fluorescence) [66] [100]. This eliminates observer bias, increases assay precision, enables high-throughput screening, and can significantly reduce the time to obtain results, as signal production often occurs before visible CPE develops [100].
Q5: Why is my ELISA standard curve non-linear or erratic? This is most commonly due to improper pipetting technique or miscalibrated pipettes, leading to inaccurate serial dilutions of the standard [104]. Ensure your pipettes are regularly serviced and calibrated. Other causes include bubbles in the wells during the reading step, uneven coating of the plate, or degradation of the standard or enzyme conjugate. Always use fresh, high-quality reagents and ensure the stop solution has been thoroughly mixed into all wells [104].
Research Reagent Solutions
The following table lists essential materials and reagents critical for successfully implementing the viral detection methods discussed in this guide.
Table 6: Essential Research Reagents and Their Functions
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Susceptible Cell Lines (e.g., Vero, HEK293, MDCK) [66] | Host system for virus propagation and CPE/Reporter assays. | Select based on viral tropism and permissivity; use low-passage stocks for consistency [66]. |
| Transfection-Grade Plasmid DNA | For creating transient or stable reporter cell lines. | High purity (supercoiled) is critical for good transfection efficiency and reproducible results [106]. |
| Luciferase Assay Kits | Provide optimized lysis buffers and stabilized substrates for reporter assays. | Follow storage and stability guidelines meticulously (e.g., some working solutions are stable for only 2-4 hours) [106]. |
| PCR Master Mix | Pre-mixed solution containing Taq polymerase, dNTPs, and buffer for PCR. | Reduces setup time and contamination risk; choose mixes with UNG for carryover prevention [105]. |
| High-Affinity Antibody Pairs | Critical for sandwich ELISA development and specificity. | Verify minimal cross-reactivity; optimize matched pair concentrations [99] [104]. |
| Cell Culture Sera (e.g., FBS) | Provides essential nutrients and growth factors for cell maintenance. | Batch testing is recommended; some serum types can inhibit specific assays like secreted luciferase activity [106]. |
Experimental Workflows & Signaling Pathways
PCR-Based Viral Detection Workflow
Reporter Cell Line Signaling Pathway
Viral Detection Method Selection Algorithm
Technical Support Center: Troubleshooting Guides and FAQs
This technical support resource addresses common challenges in integrating real-time impedance monitoring with high-throughput screening (HTS) for viral cytopathic effect (CPE) research. The guidance is specifically framed within the context of optimizing viral cell culture studies.
Frequently Asked Questions
Q1: Our impedance data for detecting viral CPE shows high well-to-well variability. What could be causing this? Inconsistent cell seeding is the most common cause. Ensure uniform cell distribution by optimizing seeding protocols using automated liquid handlers. Validate seeding consistency by running a 24-hour impedance baseline check before infection; a Z'-factor above 0.5 indicates a robust assay [107]. Second, verify that your nanopatterned substrates, if used to mimic physiological conditions, have uniform pattern fidelity, as inconsistencies can create artificial gene regulation and variable cellular responses [108].
Q2: How can I distinguish virus-induced CPE from general cytotoxicity in real-time impedance readings? Implement orthogonal assays to confirm specificity. While impedance can track morphology changes like cell rounding and detachment, complement this with a cellular fitness screen such as the CellTiter-Glo viability assay post-impedance measurement [109]. Furthermore, establish distinct impedance signatures: a gradual decline may indicate general toxicity, whereas a rapid, specific drop could correlate with viral CPE confirmed by platforms like AIRVIC, which uses AI to classify virus-specific effects [9].
Q3: What are the key considerations for adapting a real-time impedance protocol to a 96-well or 384-well HTS format? Throughput and data management are critical. Utilize platforms specifically designed for HTS, such as semiconductor 96-microplate platforms with integrated electrode arrays [110]. For data processing, ensure your system can handle the throughput. Techniques like Fast-Fourier Transform (FFT) applied to square wave measurements can reconstruct impedance spectra rapidly without external analyzers, making them suitable for multi-well formats [111]. Miniaturized data interfaces are essential for parallel operation of multiple plates within incubators [110].
Q4: Can real-time impedance monitoring be used for viruses that do not cause clear or rapid CPE? Yes, but it requires a more sensitive setup. Impedance is highly effective for monitoring subtle morphological and functional changes in real-time, even without visible CPE [110]. For viruses with delayed or subtle effects, enhance detection sensitivity by using multi-frequency impedance analysis. Measuring at several frequencies (e.g., 250 Hz to 16 kHz) simultaneously can capture a wider range of cellular parameters, providing a more nuanced profile of infection progression [110].
Troubleshooting Common Experimental Issues
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Poor Signal-to-Noise Ratio | Electrode inconsistency; environmental fluctuations; cell debris. | Use CMOS plates with high electrode density (e.g., 4096 electrodes/well) [110]. | Implement daily calibration with standardized solutions; use integrated systems designed for incubator environments [110]. |
| Irreproducible Dose-Response | Compound solubility issues; uneven viral infection; assay interference. | Include counter-screens (e.g., detergent-based) to identify assay-interfering compounds [109]. | Use DMSO controls; include BSA or detergents in buffers to prevent aggregation; standardize viral inoculation protocols (e.g., consistent MOI, adsorption time) [109]. |
| Inability to Resolve Single-Cell Effects | Low spatial resolution of electrodes; population-averaged readouts. | Adopt platforms with a 25 µm electrode pitch for near single-cell resolution [110]. | Use high-content impedance imaging to extract >20 parameter images, enabling single-cell analysis within a population [110]. |
Experimental Protocols for Viral CPE and Impedance Monitoring
Protocol 1: Real-Time Impedance-Based Profiling of Viral CPE in a 96-Well Format
This protocol uses a semiconductor microplate platform to monitor viral infection in real time.
Key Materials:
- Platform: Semiconductor 96-microplate with 4,096 electrodes per well (25 µm pitch) and compatible data acquisition system [110].
- Software: Custom software for electric field impedance measurements and data analysis.
- Cells: Adherent cell lines relevant to your virus (e.g., Vero, MDBK).
- Virus: Viral stock of interest, titered to determine Multiplicity of Infection (MOI).
Methodology:
- Cell Seeding: Seed cells uniformly into the wells of the CMOS microplate. Use a working volume of 120 µL per well and allow cells to adhere for 24 hours in a standard incubator [110].
- Baseline Measurement: Initiate continuous impedance monitoring post-seeding. Use field-based configurations (Vertical Field, Lateral Field) at multiple frequencies (e.g., 250 Hz, 1 kHz, 4 kHz, 16 kHz) to establish a stable, baseline cellular profile. A full plate scan can be completed in approximately 2 minutes [110].
- Viral Infection: Inoculate cells with the virus at a predetermined MOI. Include control wells with inoculum only (mock infection).
- Real-Time Monitoring: Continue impedance scanning every 15 minutes for the experiment's duration (e.g., 72 hours). The system will generate over 20 impedance parameter images per time point, quantifying cell barrier integrity, attachment, and morphology [110].
- Data Analysis: Normalize impedance data to the pre-infection baseline. Use parameters like cell index or specific morphological maps to quantify the timing and magnitude of CPE. Correlate impedance trends with orthogonal endpoint assays (e.g., plaque assay, PCR) [9].
Protocol 2: orthogonal Validation Using AI-Based CPE Classification
This protocol validates impedance findings using a label-free AI imaging system.
Key Materials:
- Platform: Web-based AI system (e.g., AIRVIC) trained on label-free microscopy images of virus-infected cells [9].
- Imager: High-throughput microscope compatible with microplates.
- Cells and Virus: Same as used in Protocol 1.
Methodology:
- Parallel Experiment Setup: In a separate standard 96-well plate, replicate the infection conditions from the impedance experiment.
- Image Acquisition: At key time points identified by the impedance data (e.g., onset of impedance drop, peak effect), automatically acquire phase-contrast images using the high-throughput microscope.
- AI Analysis: Upload images to the AI platform (e.g., AIRVIC). The system, typically based on a convolutional neural network like ResNet50, will detect and classify the CPE, providing an unbiased infectivity score [9].
- Data Integration: Correlate the AI-based CPE scores with the real-time impedance parameters. This confirms that the impedance changes are specifically due to viral CPE and not general cytotoxicity.
Signaling Pathways, Workflows, and Logical Diagrams
Diagram 1: Integrated HTS Workflow for Viral CPE Research
Diagram 2: Real-Time Impedance Data Processing Logic
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and technologies for implementing HTS with real-time impedance monitoring in viral CPE research.
| Item Name | Function/Application | Key Features |
|---|---|---|
| Semiconductor 96-Microplate | High-resolution, real-time impedance imaging of cell sheets in a standard HTS format. | 4,096 electrodes/well; 25 µm spatial resolution; >20 parameter images; compatible with automated fluid handlers [110]. |
| Nanogroove-Enhanced Impedance Biosensor | Enhanced precision in cellular behavior analysis for drug screening on physiological-mimicking substrates. | Self-assembled monolayers (SAMs) for uniform nanopatterning; integrated within 96-well electrode arrays; reveals gene expression differences vs. flat surfaces [108]. |
| Web-Based AI Platform (e.g., AIRVIC) | Label-free detection and classification of viral cytopathic effects from microscopy images. | ResNet50 CNN architecture; trained on tens of thousands of images; provides unbiased infectivity scoring; accessible web interface [9]. |
| Orthogonal Assay Kits | Counter-screens and cellular fitness assays to validate hits and exclude false positives. | Cell viability (CellTiter-Glo), cytotoxicity (LDH assay), and high-content staining (Cell Painting) kits [109]. |
| High-Precision Impedance Analyzer | Validation and optimization of electrode-tissue interfaces and general bioimpedance research. | Broad frequency range (e.g., 100 µHz - 100 MHz); high accuracy (down to 0.01%); scalable channel options for multiplexing [112]. |
| Versatile High-Voltage Generator | Research on electroporation as a tool for viral delivery or tissue ablation, with real-time monitoring. | Capable of delivering both high-voltage IRE pulses and low-voltage sensing pulses for real-time impedance tracking without additional equipment [111]. |
Conclusion
The optimization of viral cell culture cytopathic effects is a multi-faceted process that integrates foundational knowledge of virology with precise methodological execution, proactive troubleshooting, and cutting-edge validation technologies. Mastering these elements—from fine-tuning MOI and culture conditions to leveraging AI for unbiased CPE detection—is paramount for advancing virology research, antiviral drug screening, and the development of gene therapies. The future of CPE analysis lies in the increased adoption of automation, sophisticated computational models, and high-throughput systems that will provide deeper, more quantitative insights into viral pathogenesis and therapeutic efficacy, ultimately accelerating discoveries in biomedical and clinical research.
References
- 1. Cytopathic effect [https://en.wikipedia.org/wiki/Cytopathic_effect]
- 2. Cytopathic effect (CPE) [https://www.britannica.com/science/cytopathic-effect]
- 3. Cytopathic Effect Assay and Plaque Assay to Evaluate in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8855088/]
- 4. Effects on Cells - Medical Microbiology - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK7979/]
- 5. Cytopathic Effect - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/cytopathic-effect]
- 6. Impedance-based method for the quantification of ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093425000035]
- 7. Digital Holographic Tomography for Rapid, Label-Free ... [https://opg.optica.org/abstract.cfm?uri=ECBO-2025-Th3A.5]
- 8. Viral contamination in cell culture: analyzing the impact of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1442321/full]
- 9. A web-based artificial intelligence system for label-free ... [https://www.nature.com/articles/s41598-025-89639-0]
- 10. Cytopathic Effect Inhibition Assay [https://antiviral.creative-diagnostics.com/cytopathic-effect-inhibition-assay.html]
- 11. A high-throughput human tissue model for respiratory viruses [https://pubmed.ncbi.nlm.nih.gov/40581228/]
- 12. Protocols Cytopathic Effects of Viruses [https://asm.org/protocols/cytopathic-effects-of-viruses-protocols]
- 13. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOop8U6NmkHdrTmir5LciTsN3ni64ScRjWDFqCJ4PauTO1_gG0p3T]
- 14. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 15. A web-based artificial intelligence system for label-free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11836352/]
- 16. Virology Culture Guide [https://www.atcc.org/resources/culture-guides/virology-culture-guide]
- 17. Cytopathic Effect: Types, Mechanisms & Examples Explained [https://www.vedantu.com/biology/cytopathic-effect]
- 18. Quantitative Flow Cytometry to Measure Viral Production ... [https://www.mdpi.com/2076-3417/8/10/1734]
- 19. Flow virometry for water-quality assessment: protocol ... [https://www.nature.com/articles/s41545-023-00224-2]
- 20. Flow Virometry: An Easy Introduction for Biologists [https://bitesizebio.com/58688/flow-virometry/]
- 21. What is Multiplicity of Infection (MOI)? | abm Inc. [https://info.abmgood.com/multiplicity-of-infection-moi]
- 22. Multiplicity of infection - Wikipedia [https://en.wikipedia.org/wiki/Multiplicity_of_infection]
- 23. In Vitro Models for Studying Entry, Tissue Tropism, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8221881/]
- 24. Virus Entry Is a Major Determinant of Cell Tropism ... - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC111928/]
- 25. Cytopathic effects: virus-modulated manifestations of innate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7126625/]
- 26. Cytopathogenic Effect - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/cytopathogenic-effect]
- 27. Cytopathic Effects Analysis [https://www.revvity.com/ask/cytopathic-effects]
- 28. Optimization of cell culture‐derived influenza A virus particles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6999594/]
- 29. Optimizing viral transduction in immune cell therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046913/]
- 30. Development, validation, and application of a dual-color ... [https://www.nature.com/articles/s41598-025-16087-1]
- 31. Combined Antiviral and Cytoprotective Action of ... [https://www.mdpi.com/2076-0817/14/7/622]
- 32. Enhanced infection efficiency and cytotoxicity mediated by ... [https://www.sciencedirect.com/science/article/pii/S2405844023090941]
- 33. Cell Culture – How to Optimize your Viral Transduction [https://info.abmgood.com/cell-culture-optimizing-viral-transduction]
- 34. What's Killing My Cell Cultures? Troubleshooting ... [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/what-is-killing-my-cell-cultures-troubleshooting-cell-growth-issues.html]
- 35. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOorxFGI62YVPa2ONmYzZBn3H-H6FF_J8eF1JIvldCR7408XuDtV9]
- 36. Accelerating cell culture media development using ... [https://www.nature.com/articles/s41467-025-61113-5]
- 37. Cell Culture Trends To Watch In 2025 [https://www.bioprocessonline.com/doc/cell-culture-trends-to-watch-in-0001]
- 38. Viral cytopathic effects measured in a drug discovery screen [https://www.bmglabtech.com/en/application-notes/viral-cytopathic-effects-measured-in-a-drug-discovery-screen/]
- 39. SARS-CoV-2 cytopathic effect (CPE) - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK579896/]
- 40. Polybrene-based Viral Transduction Protocol [https://bpsbioscience.com/polybrene-based-viral-transduction-protocol]
- 41. Polybrene Lentivirus Resources [https://bioinnovatise.com/articles/polybrene-lentivirus/]
- 42. Optimization of the transductional efficiency of lentiviral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3456965/]
- 43. ViralEntry™ Transduction Enhancer (100X) [https://www.abmgood.com/viralentry-transduction-enhancer.html]
- 44. 5 Tips for Troubleshooting Viral Transductions [https://blog.addgene.org/5-tips-for-troubleshooting-viral-transductions]
- 45. Protocol 3 - Lentivirus Transduction into Target Cell Lines [https://hollingscancercenter.musc.edu/research/shared-resources/shrna/lentivirus-transduction]
- 46. AAV vs Lentivirus – Which Viral Vector Is Right For My ... [https://bioinnovatise.com/articles/aav-vs-lentivirus-which-viral-vector-is-right-for-my-research/]
- 47. A complete guide to viral vectors [https://www.revvity.com/blog/a-complete-guide-to-viral-vector]
- 48. Adeno-Associated Virus Vectors in Retinal Gene Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292589/]
- 49. The Differences Between AAV, Adenovirus, and Lentivirus [https://www.hanbiology.com/blog/the-differences-between-aav-adenovirus-and-lentivirus.html]
- 50. AAV Vs. Lentiviral Vectors - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/aav-vs-lv/]
- 51. What is Viral Purification? Uses, How It Works & Top... Vector [https://www.linkedin.com/pulse/what-viral-vector-purification-uses-how-works-top-r8cqe]
- 52. Guide To Viral Vector Production & Development [https://bataviabiosciences.com/guide-to-viral-vector-production-from-bench-to-bedside-faster/]
- 53. Mammalian Cell Culture Basics Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-culture-support-center/mammalian-cell-culture-basics-support/mammalian-cell-culture-basics-support-troubleshooting.html]
- 54. Cell culture troubleshooting [https://www.ptglab.com/support/cell-culture-protocol/cell-culture-troubleshooting/?srsltid=AfmBOopSjkrpC60Zb5my0De7ASZvGz0STBRePQ4ta5atdMpmj7P0ziq5]
- 55. Rational cell culture optimization enhances experimental ... [https://www.nature.com/articles/s41598-018-21050-4]
- 56. CO2 concentration and pH control in the cell ... [https://www.culturecollections.org.uk/culture-collection-news/co2-concentration-and-ph-control-in-the-cell-culture-laboratory/]
- 57. Optimization of Key Factors in Serum Free Medium for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7393043/]
- 58. Enabling cell culture technologies for the intensification & scale-up of viral vector manufacturing [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3036/enabling-cell-culture-technologies-for-the-intensification-scaleup-of-viral-vector-manufacturing]
- 59. Cell Culture Troubleshooting Guide [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-troubleshooting/cell-culture-troubleshooting-guide]
- 60. Protocol for the simultaneous activation and lentiviral ... [https://www.sciencedirect.com/science/article/pii/S2666166725000917]
- 61. Transcriptomic and proteomic analyses reveal new insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6332865/]
- 62. Effects of Self-Complementarity, Codon Optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6445178/]
- 63. Enhanced Transgene Expression by Optimization of Poly A ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.722722/full]
- 64. A Practical Guide to Optimizing AAV DIO and FLEx Vector ... [https://blog.addgene.org/a-practical-guide-to-optimizing-aav-dio-and-flex-vector-expression]
- 65. Optimized conditions for gene transduction into primary ... [https://www.nature.com/articles/s41598-023-39597-2]
- 66. Cell Cultures for Virology: Usability, Advantages, and Prospects [https://pmc.ncbi.nlm.nih.gov/articles/PMC7662242/]
- 67. Process for an efficient lentiviral cell transduction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7200879/]
- 68. Safe and Efficient Storage of Chemical and Virus Samples [https://www.scisure.com/blog/safe-efficient-storage-of-chemical-virus-samples]
- 69. How can I increase my viral titers and improve ... [https://www.mirusbio.com/increase-aav-titer-percent-full/?srsltid=AfmBOoqhVqZEmmZdXiFmKIlwtapZDmiRvy33o0w8IsB2GncgQ-k9-T-k]
- 70. What is the biggest insert for a viral vector? - (Feb/06/2009 ) [https://www.protocol-online.org/biology-forums-2/posts/6204.html]
- 71. On the stability of sequences inserted into viral genomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6855363/]
- 72. Optimization of Culture Media and Feeding Strategy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11125598/]
- 73. Culturing, Storage, and Quantification of Rotaviruses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3403738/]
- 74. Plasmonic optical fiber biosensors for ultra-low detection of ... [https://www.nature.com/articles/s41598-025-04239-2]
- 75. Performance Evaluation of a Fully Automated Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294030/]
- 76. One Assay, Nine Targets: Advancing Viral Surveillance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529474/]
- 77. Virus detection by short read high throughput sequencing ... [https://www.nature.com/articles/s41541-025-01104-1]
- 78. Syncytial death mediated by oncolytic rVSV-NDV ... [https://www.sciencedirect.com/science/article/pii/S2950329925000967]
- 79. A history of adventitious agent contamination and the ... [https://www.sciencedirect.com/science/article/pii/S1045105622000690]
- 80. Improving Adventitious Agent Testing in Biologics ... [https://www.thermofisher.com/blog/behindthebench/improving-adventitious-agent-testing-in-biologics-manufacturing/]
- 81. Cell Culture Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 82. Development of a Mass Antiviral Screening System Using ... [https://www.mdpi.com/1999-4915/17/11/1522]
- 83. Product Technical Support [https://www.atcc.org/support/product-technical-support]
- 84. Immortalized Human Skeletal Myoblasts (LHCN-M2) [https://www.abmgood.com/immortalized-human-skeletal-myoblasts-lhcn-m2.html]
- 85. Determine Viral-Induced Cytopathic Effect Using a ... [https://www.promega.com/resources/pubhub/determine-viral-induced-cytopathic-effect-using-a-luminescent-assay/]
- 86. Multicentre evaluation of the Check-Direct CPE® assay for ... [https://pubmed.ncbi.nlm.nih.gov/25637518/]
- 87. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 88. MTT assay and its use in cell viability and proliferation ... [https://www.abcam.com/en-us/knowledge-center/cell-biology/mtt-assay]
- 89. Protocol Guide: XTT Assay for Cell Viability and Proliferation [https://www.merckmillipore.com/TR/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/cell-counting-and-health-analysis/cell-proliferation-kit-xtt-assay]
- 90. ATP Assays | What is an ATP Assay? [https://www.promega.com/resources/guides/cell-biology/atp-assays/]
- 91. The MTT Assay: Utility, Limitations, Pitfalls, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8657538/]
- 92. The Ultimate Guide to Troubleshooting Microplate Assays [https://bitesizebio.com/81249/troubleshooting-microplate-assays/]
- 93. Optimization of cell viability assays to improve replicability ... [https://www.nature.com/articles/s41598-020-62848-5]
- 94. Classifier Not Running [https://docs.overview.ai/docs/New%20ov20%20doc/Overview%20ai%20Product%20Documentation%2021124ca12582803bb843cda6b4d4e5c6/Classifier%20Not%20Running%2021524ca1258280738c77f1f43e5d9f0f]
- 95. Viral Infectivity Assays [https://www.agilent.com/about/tektalk/en/viral-infectivity-assays.html?srsltid=AfmBOorL0_p7vHsmYqApkcUxJXuJ3SeqMdO4oP8O9tE-z8FSTlaGN6vm]
- 96. a deep learning tool for classifying SARS-CoV-2 based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11225326/]
- 97. Serum‐Free Japanese Encephalitis Virus Production in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541546/]
- 98. A web-based artificial intelligence system for label-free virus... [https://pubmed.ncbi.nlm.nih.gov/39966536/]
- 99. Types Of Immunoassay - And When To Use Them [https://www.quanterix.com/immunoassay-technologies-past-present-and-future/]
- 100. Advancements in the application of reporter gene cell lines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460214/]
- 101. Comparison of cell-based and PCR-based assays as methods for measuring infectivity of Tulane virus - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0166093415300161]
- 102. Development of real-time PCR methods for quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058689/]
- 103. Comparison of Quantitative Reverse Transcription-PCR to Viral Culture for Assessment of Respiratory Syncytial Virus Shedding - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC193781/]
- 104. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 105. PCR Troubleshooting Guide & Solutions [https://www.bosterbio.com/protocol-and-troubleshooting/pcr-troubleshooting?srsltid=AfmBOor9ZvQkHmppCjMHP9AAMQtrJmzqOd3mWwgOClEEQPy0AXyvZ6z4]
- 106. Reporter Gene Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/protein-assays-analysis-support-center/reporter-gene-assays-support/reporter-gene-assays-support-troubleshooting.html]
- 107. High-Throughput Screening (HTS): A Simple Guide ... [https://www.chemcopilot.com/blog/hts-material-discovery]
- 108. High-Throughput 96-Well Nanogroove-Enhanced Electrical ... [https://pubmed.ncbi.nlm.nih.gov/40534247/]
- 109. Brief Guide: Experimental Strategies for High-Quality Hit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293735/]
- 110. A semiconductor 96-microplate platform for electrical- ... [https://www.nature.com/articles/s41467-023-43333-9]
- 111. Real-Time Impedance Monitoring During Electroporation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7309040/]
- 112. How Ingestible Devices and Impedance Analysis Work ... [https://sciospec.com/portfolio/advancing-gastrointestinal-electrophysiology-how-ingestible-devices-and-impedance-analysis-work-together/]