Strategies for Viral Diagnostic Contamination Risk Reduction: From Prevention to Validation
This article provides a comprehensive framework for researchers, scientists, and drug development professionals to mitigate viral contamination risks in diagnostic and bioprocessing environments.
Strategies for Viral Diagnostic Contamination Risk Reduction: From Prevention to Validation
Abstract
This article provides a comprehensive framework for researchers, scientists, and drug development professionals to mitigate viral contamination risks in diagnostic and bioprocessing environments. It explores the foundational sources and impacts of contamination, details advanced methodological applications for detection and monitoring, offers troubleshooting and optimization strategies for existing protocols, and discusses rigorous validation and comparative analysis of emerging technologies. By synthesizing current best practices and novel approaches, this guide aims to enhance the reliability, safety, and integrity of viral diagnostics and biologics manufacturing.
Understanding the Sources and Impact of Viral Contamination
Defining Adventitious and Endogenous Viral Contaminants
FAQs on Viral Contaminants
1. What is the key difference between an adventitious and an endogenous viral agent?
- Adventitious Agents are microorganisms that are unintentionally introduced into the manufacturing process of a biological product. They are foreign contaminants that can be introduced via raw materials like cell substrates, bovine serum, or porcine trypsin [1]. Examples include viruses, bacteria, mycoplasma, and TSE agents.
- Endogenous Viral Agents are parts of viral genomes that have become integrated into the genome of the cell line itself. They are a inherent part of the cell substrate. A key example is the presence of retrovirus-like particles in Chinese Hamster Ovary (CHO) cells, which cause no visual change to the cells but can pose a potential risk [2].
2. Why are some viral contaminations, like endogenous retroviruses, difficult to detect?
Some viral contaminations do not cause a visible cytopathic effect (cell damage) [2]. Instead, the viral genome integrates into the host cell's DNA as a provirus, providing no visual evidence of contamination under a microscope. This "silent" contamination requires specific molecular techniques for detection [2].
3. What are the primary sources of adventitious virus introduction in bioproduction?
Cell cultures can become contaminated through three primary means [2]:
- Primary Contamination: The source of the cells was already infected (e.g., from an animal or human donor).
- Contaminated Raw Materials: The use of infected reagents like bovine serum or porcine trypsin.
- Cross-Contamination: From other infected cell cultures in the same lab or via animal passage.
4. What are the major historical incidents of viral contamination in vaccines?
Several notable events have shaped regulatory oversight [1]:
- Simian Virus 40 (SV40) in Polio Vaccine: Discovered in 1960, this monkey virus contaminated early batches of polio vaccine produced in rhesus monkey kidney cells [1].
- Porcine Circovirus (PCV1) in Rotavirus Vaccine: PCV1 viral DNA was detected in a licensed rotavirus vaccine, traced back to the use of porcine trypsin during manufacture [1].
5. What are "No Template Controls" and why are they critical in viral diagnostics?
A No Template Control (NTC) is a well in a qPCR plate that contains all the reaction components except for the DNA template [3]. It is a critical control to monitor for contamination. If amplification occurs in the NTC, it signals that one of the reagents or the laboratory environment is contaminated with the target DNA, which could lead to false-positive results in the actual samples [3].
Troubleshooting Guide for Contamination Prevention and Detection
| Problem | Possible Cause | Solution / Recommended Action |
|---|---|---|
| Amplification in No Template Control (NTC) [3] | Contaminated reagents or aerosolized amplicons in the lab environment. | Replace all suspected reagents. Establish separate pre- and post-amplification laboratory areas. Use uracil-N-glycosylase (UNG) in qPCR master mixes to degrade carryover contaminants [3]. |
| Unexplained, Inconsistent Test Results | Low-level, non-cytopathic viral contamination that doesn't cause cell death [2]. | Implement regular, sensitive molecular screening assays (e.g., PCR) for a broad panel of potential viral contaminants, even in the absence of visible cell damage. |
| Persistent Contamination After Cleaning | Ineffective surface decontamination. | Decontaminate work surfaces and equipment with a fresh 10-15% bleach solution (sodium hypochlorite), allowing 10-15 minutes of contact time before wiping. Follow with 70% ethanol cleaning for routine use [3]. |
| Suspected Raw Material Contamination | Adventitious viruses introduced via animal-derived reagents (e.g., serum, trypsin) [2] [1]. | Source raw materials from qualified suppliers with robust testing regimens. Implement and archive samples for retrospective testing. Incorporate viral clearance/inactivation steps in the production process where possible [1]. |
Experimental Protocols for Viral Detection and Risk Mitigation
Protocol 1: Establishing a Contamination-Free qPCR Workflow
This protocol outlines best practices to prevent DNA contamination in sensitive molecular assays like qPCR, which is crucial for accurate viral detection [3].
- Physical Separation of Work Areas: Establish dedicated, separate rooms for pre-amplification (reagent preparation, sample setup) and post-amplification (analysis of PCR products) activities. These areas should have independent equipment, lab coats, and consumables [3].
- Unidirectional Workflow: Personnel must not move from post-amplification areas back to pre-amplification areas on the same day without a complete change of personal protective equipment (PPE) [3].
- Use of Aerosol-Reduction Tips: Always use filtered, aerosol-resistant pipette tips to prevent cross-contamination between samples [3].
- UNG Treatment: Use a qPCR master mix containing uracil-N-glycosylase (UNG) and substitute dUTP for dTTP in the reaction. Incubate reactions at room temperature before thermocycling to allow UNG to enzymatically degrade any uracil-containing carryover DNA from previous amplifications [3].
- Rigorous Surface Decontamination: Regularly clean all work surfaces and equipment with 70% ethanol. In case of spills or suspected contamination, use a fresh 10% bleach solution [3].
Protocol 2: Archiving for Retrospective Adventitious Agent Testing
This methodology is critical for investigating contamination events and leveraging new technologies for risk reduction [1].
- Sample Identification: Identify and label samples from all critical stages of production, including cell bank seeds, bulk harvests, final product lots, and all biological raw materials (e.g., serum, trypsin) [1].
- Secure Storage: Archive samples in a dedicated, secure storage facility (e.g., -80°C freezer or vapor-phase liquid nitrogen) with controlled access and environmental monitoring.
- Documentation and Traceability: Maintain detailed records that provide full traceability, linking each archived sample to its source, production batch, and date. This is essential for a thorough root cause analysis if a contaminant is discovered post-market [1].
- Retrospective Analysis: In the event of a newly identified contaminant risk (e.g., a previously unknown virus), use archived samples to determine the origin, duration, and scope of the contamination. This allows for a precise risk assessment and targeted corrective actions [1].
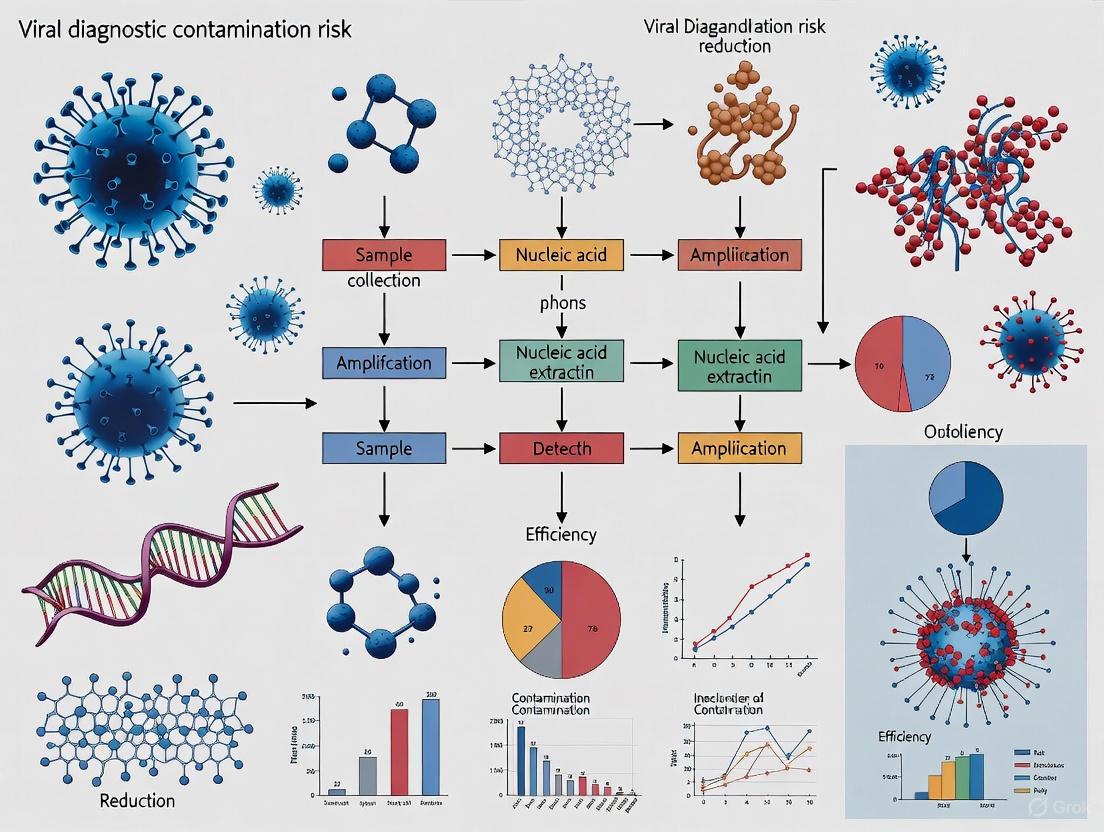
Visualizing Viral Contaminant Pathways and Detection Logic
The following diagram illustrates the logical workflow for defining, identifying, and managing different types of viral contaminants in bioprocessing.
Viral Contaminant Decision Pathway
The Scientist's Toolkit: Key Research Reagents & Materials
The following table details essential materials and their functions in the context of preventing and detecting viral contaminants.
| Reagent / Material | Function in Contamination Risk Reduction |
|---|---|
| Uracil-N-Glycosylase (UNG) [3] | An enzyme used in qPCR master mixes to prevent false positives by degrading carryover contamination from previous amplification products. |
| Aerosol-Resistant Filtered Pipette Tips [3] | Physical barriers that prevent aerosols and liquids from contaminating the pipette shaft, thereby reducing cross-contamination between samples. |
| Bovine Serum [2] [1] | A common growth medium supplement for cell cultures that is a potential source of adventitious viruses (e.g., bovine viral diarrhea virus) and requires rigorous testing. |
| Porcine Trypsin [2] [1] | A reagent used to passage adherent cell cultures that can be a source of viral contaminants like porcine parvovirus or porcine circovirus (PCV1). |
| Sodium Hypochlorite (Bleach) [3] | A potent chemical decontaminant used at 10-15% dilution to effectively destroy DNA and inactivate viruses on laboratory surfaces and equipment. |
| Mycoplasma Testing Kits | Essential for routine screening of cell cultures for mycoplasma contamination, which is another major class of adventitious agent [4]. |
Troubleshooting Guides
Troubleshooting Guide: Cell Bank Contamination
Q: Our cell bank has failed a critical sterility test. What are the immediate steps we should take to contain the issue and identify the root cause?
A: A failed sterility test requires immediate and systematic action. The following workflow outlines the critical response and investigation path.
Immediate Actions:
- Quarantine: Immediately quarantine the entire affected cell bank lot and any working cell banks (WCBs) derived from it to prevent use in production or experiments [5].
- Documentation: Freeze all related documentation and initiate a deviation report as per your quality management system [6].
Root Cause Analysis: Investigate potential failure points across the entire lifecycle:
- Testing Process: Verify the sterility testing procedure itself. Confirm that bacteriostasis and fungistasis testing was performed prior to sterility testing to rule out sample matrix inhibition, which can cause false negatives [7]. Review reagent quality and analyst training.
- Cell Line History & Raw Materials: Scrutinize the complete history of the cell line, focusing on exposure to animal-derived raw materials like fetal bovine serum (FBS) or trypsin. The absence of Certificates of Analysis (CoAs) for these materials is a major risk factor for introducing microbial and viral contaminants [8] [7].
- Manufacturing Environment & Equipment: Audit the aseptic processing environment. Check records for environmental monitoring (viable and non-viable particulates), equipment sterilization validation (e.g., autoclave, SIP cycles), and cleaning validation of stainless-steel equipment to rule out biofilm formation [9] [6].
- Personnel & Aseptic Technique: Review gowning qualification records and environmental monitoring data linked to operator activities. Human error is a prevalent source of contamination, often due to breaks in aseptic technique [9] [5].
Troubleshooting Guide: Raw Material Contamination
Q: We suspect our cell culture media is a source of low-level, persistent microbial contamination. How can we confirm this and prevent recurrence?
A: Suspect raw materials require a rigorous qualification process. The logical flow below details the confirmation and prevention strategy.
Confirmation Steps:
- In-house Testing: Do not rely solely on the supplier's Certificate of Analysis (CoA). Perform your own tests on the suspect material batch for bioburden, sterility, and mycoplasma using compendial methods [5] [10].
- Process Simulation: Use the suspect media in a small-scale culture run with a non-critical cell line and closely monitor for pH shifts, turbidity, and microbial growth.
Prevention Strategies:
- Supplier Qualification: Audit your supplier's quality management system. Ensure they provide comprehensive CoAs that include testing for sterility, endotoxins, and mycoplasma, and Certificates of Origin for materials of biological origin [10].
- Material Upgrade: Transition from research-grade to GMP-grade raw materials for clinical development and commercial manufacturing. GMP-grade materials have stricter controls and testing protocols [10].
- Media Adaptation: Where possible, adapt your cell lines to serum-free and chemically defined media. This eliminates the high-risk variable of animal sera, a common source of adventitious agents like viruses and mycoplasma [8] [7].
Troubleshooting Guide: Human Operator Contamination
Q: An audit identified inconsistent aseptic practices among our staff. What is the most effective way to retrain personnel and reduce this contamination risk?
A: Inconsistent aseptic technique is a critical finding that requires a holistic approach combining training, monitoring, and process design.
Corrective and Preventive Actions:
- Re-training and Qualification: Implement a mandatory, hands-on re-training program for all personnel entering the aseptic processing area. This must include practical demonstrations in a mock environment. Follow this with a formal gowning qualification and aseptic technique qualification, where personnel perform media fills (process simulations) to prove their competency. Their access should be contingent on passing these qualifications [9] [6].
- Enhanced Monitoring: Increase the frequency of environmental monitoring during operations, including surface and air sampling, and settle plates. Correlate this data with specific personnel and shifts to identify patterns and target further training [9] [6].
- Procedure and Design Review: Simplify complex manual procedures to reduce intervention points. Implement closed processing systems and single-use technologies (e.g., sterile tubing welders, pre-sterilized single-use bags) to minimize direct operator contact with the product and process fluids [11] [12].
Frequently Asked Questions (FAQs)
Q1: What are the most critical tests required for a GMP-compliant Master Cell Bank (MCB)?
A: A comprehensive testing panel is required to ensure the safety and purity of an MCB. The tests are designed to detect microbial, viral, and cellular contaminants. The following table summarizes the key testing categories and methods.
Table 1: Critical Characterization Tests for a GMP Master Cell Bank (MCB)
| Test Category | Specific Assays & Methods | Key Target Contaminants / Attributes |
|---|---|---|
| Sterility Testing | Compendial methods (e.g., direct inoculation, membrane filtration) [7]. | Bacteria, fungi, and mold. |
| Mycoplasma Testing | Compendial culture methods (28 days) or validated rapid methods (e.g., PCR, fluorescence) [5] [7]. | Mycoplasma and Acholeplasma species. |
| Viral Safety Testing | In vitro assay: Inoculation on indicator cell lines (e.g., Vero, MRC-5) observed for CPE, HAD, HA [7]. | Broad spectrum of unknown viral contaminants. |
| In vivo assay: Inoculation into suckling/adult mice, guinea pigs, embryonated eggs [7]. | Viruses not detectable by in vitro methods. | |
| Species-specific tests: e.g., Antibody Production Tests (MAP, RAP) for rodent cells [7]. | Specific viruses (e.g., LCMV, Hantaan). | |
| Retrovirus Testing: Reverse transcriptase (RT) assays, transmission electron microscopy (TEM) [7]. | Endogenous and adventitious retroviruses. | |
| Identity & Genetic Stability | Karyology, Isoenzyme analysis, DNA fingerprinting (STR), Sequencing [8] [7]. | Confirmation of cell line identity and genetic integrity. |
Q2: Beyond sterility, what are the key quality attributes to check in critical raw materials like cell culture media?
A: While sterility is paramount, other quality attributes are critical for consistent cell growth and product quality.
Table 2: Key Quality Attributes for Critical Raw Materials (e.g., Cell Culture Media)
| Quality Attribute | Importance & Impact | Typical Testing Method |
|---|---|---|
| Endotoxin Level | Pyrogenic; can elicit immune responses in cells and patients. | LAL (Limulus Amebocyte Lysate) test. |
| Performance | Directly impacts cell growth, viability, and productivity. | Small-scale cell culture growth study. |
| pH & Osmolality | Critical biochemical parameters for cell health. | pH meter, osmometer. |
| Chemical Composition | Consistency in components (e.g., glucose, amino acids) is key for process reproducibility. | HPLC, GC-MS. |
| Viral Safety | Ensures no adventitious viruses are introduced via raw materials. | Supplier's virus validation studies; use of viral-inactivated materials (e.g., gamma-irradiated FBS) [10]. |
Q3: Our viral diagnostic assays are highly sensitive to cross-contamination. What practical lab design and workflow solutions can we implement?
A: Implementing strict procedural and physical controls is essential to prevent amplicon or sample cross-contamination.
- Physical Separation: Establish physically separated, dedicated rooms or areas for pre-amplification (sample prep, PCR setup) and post-amplification (PCR product analysis) activities. Implement unidirectional workflow and dedicated equipment for each area [9].
- Environmental Controls: Use HEPA-filtered air, positive air pressure in cleanrooms, and UV lights in biosafety cabinets to reduce airborne contaminants [9].
- Use of Closed Systems: Employ closed-system processing technologies, such as single-use bioreactor bags and sterile tube welders/sterile connectors. This minimizes the need for open manipulations and reduces the risk of contamination from the environment and human operators [12].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Contamination Control
| Item | Function & Rationale |
|---|---|
| GMP-Master Cell Bank (MCB) | A fully characterized, GMP-compliant bank provides a consistent and secure starting material, ensuring the identity, purity, and safety of the cell line used in production or testing [8] [7]. |
| Chemically Defined Media | Media formulations with fully known components eliminate the variability and adventitious agent risk associated with animal-derived sera like FBS, enhancing process consistency and safety [8] [10]. |
| Viral-Inactivated Serum | When serum is necessary, using gamma-irradiated FBS mitigates the risk of introducing viral contaminants [7]. |
| Single-Use Systems (SUS) | Pre-sterilized, disposable bioreactor bags, tubing, and filters eliminate the risk of cross-contamination between batches and remove the need for cleaning validation, reducing operational complexity [12]. |
| Rapid Mycoplasma Detection Kits | PCR- or fluorescence-based kits allow for faster detection of mycoplasma contamination compared to the 28-day compendial culture method, enabling quicker decision-making [5] [7]. |
| Validated Disinfectants | Using disinfectants with validated efficacy (e.g., sporicidal, bactericidal) and following a rotating regimen prevents the development of resistant microbial strains on surfaces [11]. |
This technical support center provides targeted troubleshooting guides and FAQs to help researchers mitigate viral contamination risks in cell culture-based bioprocesses, supporting broader thesis research on viral diagnostic contamination risk reduction.
Viral Contamination Troubleshooting FAQ
Q: What are the most critical yet often overlooked viral contaminants in cell culture? A: Two critical contaminants are the Epstein-Barr virus (EBV) and ovine herpesvirus 2 (OvHV-2). EBV is highly ubiquitous (infecting ~98% of humans) but is often not a primary safety priority because its detection methods are well-established. In contrast, OvHV-2 represents a more critical and complex challenge due to its ability to infect a wide range of organs and over 33 animal species, making its detection crucial for cross-species cell culture safety [13] [14] [15].
Q: Why is OvHV-2 contamination particularly problematic for bioprocessing? A: OvHV-2 poses a significant challenge in research and bioprocessing settings because its broad species tropism increases the risk of contaminating cell cultures derived from various animals. Furthermore, comprehensive and robust detection methodologies specific to OvHV-2 are not as established as for other viruses, creating a gap in safety protocols [14] [15].
Q: What are the primary sources of viral contamination in a bioprocess? A: Viral infections can originate from three main sources, requiring vigilance throughout the entire workflow [13]:
- Contaminated Cell Lines: The initial cells used in the process may already harbor a latent or active virus.
- Contaminated Raw Materials: Reagents, media, or supplements introduced into the culture can be a source.
- Process Breakdowns: Failures in production or purification procedures can introduce contamination.
Q: How can we differentiate between active infection and incidental presence of EBV in cell cultures? A: Distinguishing causality is a common diagnostic challenge. Relying solely on qualitative DNA detection (e.g., positive PCR) is insufficient. It is essential to employ supporting parameters such as viral load quantification (where a high load suggests active infection), analysis of CSF/serum ratios, and detection of intrathecal antibody synthesis to confirm a virus's active role in contamination [16].
Detection Methodologies for Featured Viral Contaminants
The table below summarizes established and emerging detection methods for key viral contaminants, providing a protocol foundation for your research.
Table 1: Detection Methods for EBV and OvHV-2 in Cell Culture
| Virus | Applicable Cell Lines | Preferred Detection Methods | Protocol Details and Key Considerations |
|---|---|---|---|
| Epstein-Barr Virus (EBV) | B-lymphoblastoid cell lines (B-LCLs), 293 human embryonic kidney (293HEK) [14] | PCR: Detects EBV DNA with high sensitivity and specificity [14].In situ hybridization (ISH): Detects EBV-encoded small RNAs (EBERs) for localization [14].EBNA detection: Identifies EBNA proteins via ELISA or Western blot [14]. | PCR protocols are well-established and can distinguish between latent and lytic forms. ISH is ideal for confirming the presence and cellular location of the virus within a culture [13] [14]. |
| Ovine Herpesvirus 2 (OvHV-2) | Ovine peripheral blood lymphocytes [14] | PCR: The main tool for detection; however, methods are less universally established than for EBV [14].Advanced Sequencing: High-throughput sequencing (HTS) and single-cell analysis are emerging for revealing viral diversity [13]. | The primary challenge is the lack of a universally validated, robust detection method. Emerging technologies like HTS are recommended to close this gap [13] [14]. |
| Minute Virus of Mice (MVM) | Information on MVM was not available in the consulted sources. | Information on MVM was not available in the consulted sources. | Information on MVM was not available in the consulted sources. |
Advanced and Emerging Detection Technologies
The field of viral detection is rapidly evolving. The following workflow illustrates how traditional and modern methods can be integrated into a comprehensive contamination screening strategy.
Workflow Explanation:
- Traditional Methods provide an accessible first pass but may lack sensitivity [17].
- Molecular Methods (PCR) offer targeted, sensitive, and quantitative data crucial for determining active infection versus incidental presence [16] [14].
- Advanced Sequencing (HTS/mNGS) is powerful for uncovering unexpected contaminants and viral diversity, directly addressing gaps in understanding for viruses like OvHV-2 [13] [17].
- Emerging Technologies like CRISPR-based diagnostics and AI-assisted analysis represent the future of rapid, precise, and accessible testing, even in point-of-care settings [17].
The Scientist's Toolkit: Key Research Reagent Solutions
This table lists essential reagents and materials for implementing the detection protocols discussed.
Table 2: Essential Reagents for Viral Contamination Detection
| Research Reagent / Tool | Primary Function in Contamination Detection |
|---|---|
| PCR Assay Kits | Detect specific viral DNA with high sensitivity. Well-established for EBV; development is needed for robust OvHV-2 detection [13] [14]. |
| High-Throughput Sequencing (HTS) | Provides a comprehensive, unbiased screen for known and unknown viral contaminants, revealing viral diversity within cultures [13]. |
| In-situ Hybridization Probes | Locate viral RNA (e.g., EBERs in EBV) within cells, confirming infection and providing spatial context [14]. |
| Antibodies for Viral Antigens | Detect viral proteins (e.g., EBNA, VCA) via ELISA, Western Blot, or immunofluorescence to confirm active viral replication [14]. |
| Cell Line Authentication Kits | Perform STR profiling to ensure cell line identity and purity, a foundational quality control measure that mitigates risk [15]. |
Comparative Risk Analysis of Viral Contaminants
Understanding the relative risk profiles of different contaminants helps in allocating resources effectively. The following diagram summarizes the critical attributes of EBV and OvHV-2.
Risk Profile Explanation:
- EBV is managed effectively due to mature diagnostics, allowing it to be categorized as a lower-tier risk despite its ubiquity [13] [14].
- OvHV-2 presents a higher and more complex risk due to its broad host range and the lack of universally robust detection methods, labeling it a critical concern that requires more research and protocol development [13] [14] [15].
FAQ: Implementing a Viral Vigilance Strategy
Q: What is the single most important shift in mindset for preventing viral contamination? A: Move from a one-time check to a philosophy of continuous "viral vigilance." Monitoring is not a single step but an ongoing process integrated throughout the entire bioprocess ecosystem and workflow, from raw material qualification to final product purification [13].
Q: Are there new technologies that can help with the challenge of incidental viral detection? A: Yes. Metagenomic Next-Generation Sequencing (mNGS) is particularly valuable in complex diagnostic situations. However, when it detects a ubiquitous virus like EBV, it is critical to follow up with quantitative PCR (viral load) and other supporting clinical parameters to accurately determine if the virus is a causative agent or an incidental bystander [16].
The Economic and Clinical Consequences of Contamination Events
Contamination events in biomedical research and biopharmaceutical manufacturing pose severe risks, extending far beyond the laboratory bench. These incidents can derail diagnostic accuracy, compromise therapeutic safety, and inflict substantial economic losses. For researchers and drug development professionals, a proactive understanding of these consequences is fundamental to viral diagnostic contamination risk reduction. This technical support center provides a comprehensive resource to troubleshoot, prevent, and manage these risks, framing them within the critical context of their broader economic and clinical impact.
The table below summarizes the multifaceted consequences of contamination events, highlighting the direct and indirect costs across research and commercial production.
Table 1: Consequences of Contamination Events in Research and Biomanufacturing
| Impact Category | Economic Consequences | Clinical Consequences | |
|---|---|---|---|
| Research & Development | - Invalidated experimental data, leading to project delays and wasted funding [18].- Retraction of published studies, damaging scientific credibility.- Loss of precious or irreplaceable cell lines [18]. | - Preclinical findings based on contaminated systems can misdirect entire therapeutic development pipelines.- Incorrect diagnostic assay development due to compromised reagents. | |
| Biologics Manufacturing | - Production shutdowns; a single viral contamination can cost millions of dollars to resolve [19] [20].- Loss of entire product batches, leading to drug shortages and revenue loss [19].- Costs associated with root cause investigation, corrective actions, and facility decontamination [19]. | - Patients may not receive critical therapies (e.g., recombinant proteins, vaccines) [19] [20].- Risk of transmitting adventitious viruses to patients, a historic issue with blood and plasma products [19]. | |
| Broader Socioeconomic Effects | - Supply chain disruptions for medicines and vaccines [21] [22].- Reduced investor confidence and financing gaps, as seen during the Ebola outbreak where gaps exceeded \$600 million in affected countries [21].- Macroeconomic shocks, including decreased GDP growth and government tax revenues [21] [23]. | - Public health crises and loss of trust in health systems. | - Long-term health burdens from untreated conditions due to overwhelmed or disrupted healthcare services, as observed during the West Africa Ebola epidemic [21]. |
Troubleshooting FAQs: Contamination Identification and Control
Q1: My cell culture medium is turning yellow and I see moving particles under the microscope. What is this and what should I do?
- Identification: This is a classic sign of bacterial contamination. Under the microscope, you may observe large numbers of moving particles, often described as a "quicksand" effect [24].
- Action:
- For a mild contamination, wash the cells with PBS and treat with a high concentration of antibiotics (e.g., 10× penicillin/streptomycin). Note that this is often a temporary solution [24].
- For heavy contamination, the recommended course of action is to discard the culture immediately [24]. Thoroughly disinfect the incubator, water baths, and biosafety cabinet with appropriate disinfectants like 70% ethanol or sodium hypochlorite (bleach) to prevent spread [24] [18].
Q2: I suspect mycoplasma contamination in my cells. How can I confirm this, and how do I eradicate it?
- Identification: Mycoplasma does not cause medium turbidity or color change. Signs include slow cell growth, abnormal morphology, and under a microscope, tiny black dots may be visible. Staining with a DNA-specific dye (e.g., DAPI or Hoechst) and fluorescence microscopy can reveal filamentous patterns on the cell surface [18].
- Confirmation: Use a commercial mycoplasma detection kit. Common methods include PCR-based detection, DNA staining, or microbial culture [24] [18].
- Eradication: Treat cultures with a commercially available mycoplasma removal agent (e.g., 40607ES01/03/08 [24]). Be aware that treatments can be cytotoxic and may not always be 100% effective. Quarantine treated cells and reconfirm they are mycoplasma-free after several passages. The safest option for non-critical cultures is often to discard and start anew [24] [18].
Q3: What are the most common sources of viral contamination in biologic manufacturing, and how are they controlled?
- Sources: Common sources include the original cell bank, animal-derived reagents (e.g., fetal bovine serum), and during production via raw materials or operator error [19]. Prevalent viral contaminants include Murine Minute Virus (MMV), Vesivirus 2117, and Cache Valley virus [19].
- Risk Control: A multi-layered quality risk management approach is essential [25]. This includes:
- Thorough testing of cell banks and raw materials for viruses.
- Incorporating viral clearance steps into the production process, such as virus filtration (using filters with pores ≤ 20 nm), solvent/detergent treatment, and low-pH incubation [19].
- Defining and validating "functionally closed" systems in biomanufacturing to prevent adventitious agent ingress [25].
Experimental Protocols for Contamination Risk Reduction
Protocol 1: Routine Mycoplasma Detection by DNA Staining
Principle: This method uses a fluorescent dye to bind DNA. Mycoplasma, which adheres to the cell surface, will appear as particulate or filamentous fluorescence outside the host cell nuclei.
Materials:
- Mycoplasma Detection Kit (e.g., MycAway Plus, Cat. No. 40615ES25 [24])
- Cell culture of interest (grown on a sterile coverslip in a dish)
- Phosphate Buffered Saline (PBS)
- Fixative (e.g., Methanol or Acetic acid)
- DNA stain (e.g., DAPI or Hoechst stain)
- Antifade mounting medium
- Fluorescence microscope
Procedure:
- Grow test cells to 50-80% confluency on a sterile coverslip in a culture dish. Include a known positive control.
- Aspirate the medium and wash the cells gently with PBS.
- Fix the cells by adding fixative (e.g., cold methanol) for 15 minutes at room temperature.
- Aspirate the fixative and allow the coverslip to air dry completely.
- Prepare the DNA stain according to the kit instructions or manufacturer's recommendation.
- Add the stain to the fixed cells and incubate in the dark for 15-30 minutes.
- Gently rinse the coverslip with PBS to remove unbound stain.
- Mount the coverslip onto a microscope slide with antifade mounting medium.
- Visualize under a fluorescence microscope with the appropriate filter set. Examine the cytoplasm and areas between cells for punctate or filamentous staining.
Protocol 2: Viral Clearance Validation Study for Downstream Processing
Principle: This model experiment is used to validate that a manufacturing purification step (e.g., chromatography or virus filtration) can effectively remove and/or inactivate viral contaminants.
Materials:
- Scale-down model of the purification step (e.g., a small-scale chromatography column or filter)
- Process intermediate sample
- Model viruses (e.g., MMV for small, non-enveloped viruses; X-MuLV for large, enveloped viruses)
- Cell lines for viral titrations (e.g., Vero cells, A9 cells)
- Cell culture media and reagents
Procedure:
- Spiking: Spike a known quantity of the model virus (e.g., >10^6 virus particles/mL) into the process intermediate sample.
- Processing: Run the spiked sample through the scaled-down purification step under conditions that mimic the full-scale manufacturing process.
- Collection: Collect the product fraction (the output).
- Titration: Determine the viral titer in both the starting spiked material and the product fraction using a plaque assay or TCID50 assay on permissive cell lines.
- Calculation: Calculate the log reduction value (LRV) using the formula:
- LRV = Log10 (Virus titer in starting material) - Log10 (Virus titer in product)
- A high LRV (typically ≥ 4 logs) indicates a robust and effective viral clearance step [19].
The following diagram illustrates the core workflow for assessing and controlling viral contamination risk in a production or research setting.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Contamination Control and Detection
| Item Name | Function/Brief Explanation | Example Catalog Number |
|---|---|---|
| Mycoplasma Detection Kit | For routine monitoring of cell cultures for mycoplasma contamination via PCR, DNA staining, or enzymatic activity. Essential for validating cell line health. | 40615ES25 [24] |
| Mycoplasma Removal Reagent | A formulated reagent used to treat and eliminate mycoplasma from contaminated cell cultures without requiring cell passage through animals. | 40607ES01 [24] |
| Penicillin-Streptomycin (P/S) | A broad-spectrum antibiotic solution used in cell culture media to prevent bacterial contamination. Overuse can lead to antibiotic-resistant strains. | N/A in sources |
| Amphotericin B | An antifungal agent used to prevent and treat yeast and mold contamination. Can be toxic to cells at high concentrations. | N/A in sources |
| Virus Removal Filter | A filter with precisely sized pores (e.g., 20 nm or smaller) used in bioprocessing to physically remove viral particles from biological products [19]. | N/A in sources |
| Surface Disinfectant (e.g., Ethanol, Benzalkonium Chloride) | For decontaminating work surfaces, equipment, and incubators. 70% ethanol is common; stronger disinfectants are used for fungal outbreaks [24] [18]. | 40605ES02 [24] |
Implementing Robust Detection and Prevention Methodologies
The 'Prevent, Detect, Remove' Framework for Viral Safety
Troubleshooting Guide: Common Viral Safety Issues
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Upstream Prevention | Bioreactor contamination with adventitious viruses [26] | High-risk raw materials (e.g., plant-origin glucose, animal-derived sera) [26] | Implement high temperature short time (HTST) pasteurization for glucose solutions; Use virus-retentive filters on cell culture media [26]. |
| Contamination from raw materials [27] | Poorly characterized raw materials or sourcing from multiple vendors [27] | Use chemically defined, non-animal origin media and recombinant supplements; Rigorous supplier evaluation and raw material testing [26] [27]. | |
| Viral Detection | Inadequate detection sensitivity [27] | Limitations in assay methods or insensitivity of cell-based assays [27] | Employ multiple, orthogonal detection methods (e.g., in vitro assays, PCR); Test cell banks, raw materials, and process intermediates [28] [29] [26]. |
| Downstream Removal | Inconsistent viral clearance [27] | Over-reliance on a single clearance method; Process variability [27] | Implement robust, orthogonal downstream purification steps (inactivation + removal); Execute viral clearance validation studies [28] [29] [30]. |
| Cell Line Safety | Vulnerability to specific viruses (e.g., MVM) [26] | Use of standard, non-resistant cell lines [26] | Utilize genetically modified virus-resistant cell lines (e.g., MVM-resistant CHO cells) where available [26]. |
Frequently Asked Questions (FAQs)
Prevention Strategies
Q: What are the highest-risk raw materials for introducing viral contamination in mAb production? A: Raw materials of plant-origin (like glucose) and animal-derived components (like bovine serum or trypsin) are considered high-risk [26]. Glucose is particularly risky due to its source in sugarcane or beet fields, which can attract virus-carrying rodents. Mitigation strategies include HTST pasteurization and using virus-retentive filters designed for cell culture media [26].
Q: How can we prevent contamination from the supply chain? A: A robust risk mitigation strategy involves [26] [27]:
- Sourcing and Evaluation: Carefully select and vet raw material suppliers. Understand the complexities and risks throughout the entire supply chain.
- Material Substitution: Replace high-risk, animal-derived components with lower-risk alternatives, such as chemically defined cell culture media and non-animal origin recombinant supplements.
- Proactive Treatment: Apply viral inactivation or removal methods (e.g., UV-C, HTST, virus-reduction filtration) to culture media or its components before use.
Detection and Testing
Q: What are the key testing points for detecting viral contamination in a bioprocess? A: A comprehensive testing regimen covers [28] [29] [26]:
- Cell Banks: Master and working cell banks.
- Raw Materials: Critical culture components prior to use.
- Process Intermediates: Unprocessed bulk harvests. This layered approach ensures contamination is identified as early as possible.
Q: Why can't we guarantee a biologic is absolutely free of viral contamination? A: The current state of technology precludes claiming absolute absence of viruses due to [27]:
- Inherent Risk: All biopharmaceutical production using mammalian components carries an inherent risk.
- Detection Limitations: Assays have limited sensitivity, and adventitious viruses can sometimes escape detection. Therefore, regulatory safety relies on a holistic strategy that combines prevention, detection, and robust removal/inactivation processes to assure patient safety [27].
Removal and Inactivation
Q: What is the regulatory expectation for demonstrating viral clearance? A: Regulatory guidelines (ICH Q5A) require viral clearance studies to demonstrate the manufacturing process's capability to remove and inactivate viruses [27]. These studies validate that specific downstream purification steps (e.g., virus filtration, low pH incubation) can effectively reduce viral load, providing a safety margin in case a contaminant is introduced upstream [28] [29] [27].
Q: Why is it important to use orthogonal methods for viral clearance? A: Orthogonal methods use different mechanisms to inactivate or remove viruses. For example, a process might combine a chemical method (low pH inactivation) with a physical method (virus filtration). This approach is critical because viruses have diverse characteristics, and using multiple, independent methods ensures broad clearance capability and protects against process variability [27].
Experimental Protocols for Viral Safety
Protocol 1: Viral Clearance Validation for a Downstream Step
Objective: To determine the log10 reduction value (LRV) of a specific purification step for a model virus.
Materials:
- Scale-down model of the purification step (e.g., chromatography column, virus filter, incubation tank)
- Model virus (e.g., Murine Leukemia Virus (MuLV) or another relevant virus from regulatory guidelines)
- Appropriate cell-based assay for quantifying infectious virus (plaque assay or TCID50)
Methodology [27]:
- Spiking: Spike a known quantity of the model virus (e.g., >10^6 infectious units) into the process intermediate material that is the input for the step being studied.
- Processing: Run the spiked material through the scaled-down purification step under defined operating parameters (e.g., flow rate, pressure, buffer conditions).
- Collection: Collect the output (product) from the step.
- Titration: Determine the infectious virus titer in both the spiked starting material and the output material using the cell-based assay.
- Calculation: Calculate the LRV using the formula:
LRV = Log10 (Virus Titer in Input Material) - Log10 (Virus Titer in Output Material)
Interpretation: A high LRV (e.g., >4 log10) indicates robust clearance capability for that model virus by the manufacturing step.
Protocol 2: HTST Pasteurization for Raw Material Risk Mitigation
Objective: To validate the effectiveness of high-temperature short-time (HTST) treatment in inactivating viruses in a raw material solution.
Materials:
- HTST pasteurization system
- High-risk raw material solution (e.g., glucose)
- Model virus with high physico-chemical resistance (e.g., Parvovirus)
- Virus titration assay
Methodology [26]:
- Preparation: Spike the raw material solution with a high titer of the model virus.
- Treatment: Subject the spiked solution to HTST treatment under validated conditions (specific temperature and time, e.g., 100°C for seconds).
- Cooling: Rapidly cool the treated solution.
- Analysis: Measure the infectious virus titer in the solution before and after HTST treatment.
- Control: Run a non-heated control sample in parallel to account for any non-thermal virus loss.
Interpretation: Successful validation shows a significant reduction in viral titer (high LRV) in the treated sample with no impact on the raw material's performance in cell culture.
Framework and Workflow Visualization
Viral Safety Framework Flow
Viral Clearance Validation
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Solution | Function in Viral Safety | Key Consideration |
|---|---|---|
| Virus-Retentive Filters [26] | Remove both enveloped and non-enveloped viruses from cell culture media or process intermediates. | Use filters designed for specific fluid types (media vs. product) to balance throughput and viral retention. |
| Chemically Defined Media [26] | Eliminates risk from animal-derived components; provides consistent, defined composition. | Supports cell growth and productivity while reducing adventitious agent risk. |
| Non-Animal Origin Recombinant Supplements [26] | Replaces high-risk materials like bovine serum or trypsin. | Critical for mitigating contamination originating from raw materials. |
| Virus Panel for Clearance Studies [27] | Used to validate the capacity of downstream steps to inactivate/remove diverse viruses. | Must include relevant (e.g., retroviruses) and challenging (e.g., parvoviruses) model viruses. |
| Model Viruses (e.g., MuLV, MVM) [27] | Serve as surrogates in viral clearance studies to demonstrate reduction capability. | Chosen based on size, envelope, and resistance to represent potential contaminants. |
This technical support center provides troubleshooting guides and FAQs to help researchers address specific issues encountered while using advanced detection tools, with a focus on reducing contamination risks in viral diagnostics.
PCR Troubleshooting FAQs
1. No or Low PCR Product Yield
| Possible Cause | Solution |
|---|---|
| Suboptimal Reaction Components | Verify all components were added. Check reagent expiration dates and avoid multiple freeze-thaw cycles by aliquoting biological components [31] [32]. |
| Poor Template Quality/Quantity | Analyze DNA integrity via gel electrophoresis and check purity (A260/280 ratio ≥1.8). Use 1 pg–10 ng for plasmid DNA or 1 ng–1 µg for genomic DNA per 50 µL reaction [33] [31] [32]. Further purify template if contaminated with inhibitors [33] [34]. |
| Incorrect Annealing Temperature | Recalculate primer Tm and test an annealing temperature gradient starting 5°C below the lower Tm [33]. Lower the temperature in 2°C increments if too stringent [34]. |
| Insufficient Cycles or Extension Time | Increase cycle number (by 3-5 cycles, up to 40) for low-abundance targets [34]. Ensure extension time is sufficient for polymerase speed and amplicon length [31]. |
| Complex Template (e.g., GC-rich) | Use polymerases formulated for GC-rich templates and include GC enhancers or co-solvents like DMSO [33] [34] [35]. Increase denaturation temperature/time [35]. |
2. Multiple or Non-Specific Bands
| Possible Cause | Solution |
|---|---|
| Annealing Temperature Too Low | Increase annealing temperature incrementally (e.g., in 2°C increments) to improve specificity [33] [34] [32]. |
| Poor Primer Design | Verify primers are specific, have no self-complementarity, and avoid GC-rich 3' ends. Redesign if necessary, following standard design rules [33] [32] [35]. |
| Excess Primer or Template | Optimize primer concentration (typically 0.1–1 µM). Reduce the amount of template DNA if too much was used [33] [32] [35]. |
| Premature Replication | Use a hot-start polymerase. Set up reactions on ice and use a preheated thermocycler [33] [35]. |
| Contamination | Use filter pipette tips, establish separate pre- and post-PCR work areas, and include a no-template control [33] [34] [32]. |
3. Sequence Errors in PCR Product
| Possible Cause | Solution |
|---|---|
| Low-Fidelity Polymerase | Switch to a high-fidelity polymerase [33] [31] [35]. |
| Excessive Number of Cycles | Reduce the number of PCR cycles to minimize misincorporation errors [33] [31]. |
| Unbalanced dNTP Concentrations | Use fresh, equimolar dNTP mixes. Aliquot stocks to prevent degradation [33] [31] [35]. |
| High Mg²⁺ Concentration | Optimize and reduce Mg²⁺ concentration in the reaction [33] [35]. |
| Template DNA Damage | Limit UV light exposure when excising PCR products from gels. Start with a fresh, high-quality template [33] [31]. |
Next-Generation Sequencing (NGS) Troubleshooting FAQs
1. What are the key considerations when choosing an NGS method for low viral load samples?
The optimal NGS method depends on the required sensitivity, genome coverage, and need for non-targeted detection. A recent European multicentre study comparing methods for Hepatitis B Virus (HBV) genome characterization found significant performance differences [36].
Table: NGS Method Performance for Viral Genome Detection at Low Loads
| NGS Method | Sensitivity (Viral Load) | Key Advantages | Key Limitations |
|---|---|---|---|
| Untargeted Metagenomics | >10 IU/ml for some viruses, but failed for HBV in study [36] | Detects unexpected/novel viruses; unbiased approach [36]. | Low sensitivity; high host background; complex data analysis [36]. |
| Probe-Capture + Illumina | >1000 IU/ml (for full HBV genome) [36] | Detects multiple pre-defined pathogens; accommodates incidental virus detection [36]. | Higher cost; longer turnaround time; limits genome characterization near ends [36]. |
| PCR + Illumina | >200 IU/ml (for full HBV genome) [36] | Good sensitivity; well-established; high accuracy [36]. | Risk of contamination; limited to targeted regions [36]. |
| PCR + Nanopore | >10 IU/ml (for full HBV genome) [36] | Lowest cost; rapid turnaround; high sensitivity [36]. | Highest risk of contamination; slightly lower read accuracy [36]. |
2. How can contamination be minimized in sensitive NGS workflows?
Contamination is a major concern, especially for highly sensitive PCR-based methods [36]. Key strategies include:
- Physical Separation: Establish distinct, dedicated areas for pre- and post-PCR/NGS work. Never bring reagents or equipment from the post-amplification area back to the clean setup area [34].
- Rigorous Controls: Always include negative controls (e.g., no-template) to detect carryover contamination [34] [36].
- Technical Vigilance: Use aerosol-filter pipette tips and wear gloves. Consider UV irradiation of workstations and pipettes to damage residual DNA [34].
In Vitro Assay Contamination Control FAQs
1. My cell cultures are contaminated. How can I identify the source and decontaminate?
Table: Common Cell Culture Contaminants and Identification
| Contaminant Type | Common Characteristics | Detection Methods |
|---|---|---|
| Bacteria | Media turbidity; rapid pH change (yellow); black sand-like particles under microscope [37]. | Direct microscopic observation; Gram staining; culture methods [37]. |
| Mycoplasma | Subtle changes; premature yellowing of medium; slowed cell growth; altered cell morphology [37]. | PCR; fluorescence staining (e.g., Hoechst); electron microscopy [37]. |
| Fungi | Visible filamentous structures (hyphae); white spots or yellow precipitates in media [37]. | Direct microscopic observation; culture on antifungal plates [37]. |
Decontamination Strategies:
- Antibiotic/Antimycotic Treatment: Apply high concentrations of appropriate agents (e.g., tetracyclines for mycoplasma; penicillin/streptomycin for bacteria; amphotericin B for fungi) for shock treatment, then maintain with regular doses [37].
- Physical Methods: For severe and persistent contamination, autoclave contaminated cultures and reagents. Mycoplasma can also be heat-inactivated at 41°C for 10 hours [37].
- Source Elimination: If contamination is recurrent, discard all potentially contaminated reagents and cell lines. Re-isolate or obtain new, clean cell stocks [37].
2. What is a structured response plan for a viral contamination event in a bioproduction facility?
A robust response plan is critical for patient safety and resuming operations [38]. A three-phase approach is recommended:
Key Elements:
- Phase 1: Confirmation & Containment: Immediately notify the core Virus Contamination Response Team (VCRT) upon an out-of-specification (OoS) result. Confirm the finding with a third-party specialist and initiate physical containment of affected areas and materials [38].
- Phase 2: Identification & Decontamination: Identify the contaminating virus and determine the full extent of the contamination. Execute a thorough decontamination of the facility using validated methods, and verify success using biological indicators [38].
- Phase 3: Resumption & Prevention: Conduct a thorough root cause investigation. Implement robust Corrective and Preventive Actions (CAPA) before systematically returning the facility to service [38].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Material | Function in Viral Diagnostics | Key Considerations |
|---|---|---|
| High-Fidelity DNA Polymerase | Amplifies target DNA sequences with minimal error rates, crucial for accurate sequencing and detection [33] [35]. | Essential for reducing sequence errors in PCR products intended for downstream cloning or NGS library prep. |
| Hot-Start Polymerase | Reduces non-specific amplification and primer-dimer formation by remaining inactive until a high-temperature activation step [33] [35]. | Critical for improving assay specificity and sensitivity, especially in multiplex PCR. |
| PCR Additives (e.g., GC Enhancer) | Aids in denaturing complex templates with high GC-content or secondary structures, ensuring efficient amplification [33] [34]. | Polymerase-specific formulations are most effective. |
| Nucleic Acid Probes (for Capture) | Enriches for target pathogen sequences from complex samples prior to NGS, increasing sensitivity for known viruses [36]. | Allows for parallel detection of multiple pre-defined pathogens in a single assay. |
| dNTP Mix | Provides the essential nucleotides (dATP, dCTP, dGTP, dTTP) for DNA polymerase to synthesize new DNA strands [33]. | Must be fresh and equimolar to prevent misincorporation errors. Aliquoting is recommended. |
| Mg²⁺ Solution | A critical co-factor for DNA polymerase activity; concentration directly influences enzyme fidelity, specificity, and yield [33] [35]. | Requires optimization for each primer-template system. Vortex thoroughly before use. |
Strategies for Raw Material Sourcing and Cell Bank Characterization
Frequently Asked Questions (FAQs)
FAQ 1: What are the key principles for sourcing raw materials to minimize viral contamination risk? A comprehensive, risk-based control strategy is essential for raw materials (RMs) to ensure the highest attainable safety concerning viruses and other adventitious agents [39]. Key principles include:
- Risk Assessment: Evaluate all RMs entering the process, focusing on their origin (synthetic, plant, animal, or microbiologically derived), nature, and quality oversight [39] [40].
- Supplier Qualification: Purchase RMs from approved suppliers who provide full traceability and data on their manufacturing process, handling, and packaging [40] [41].
- Robust Testing: Implement a testing program for bioburden and specific pathogens, commensurate with the RM's risk level and intended use [39] [40].
FAQ 2: My cell culture shows a sudden drop in pH and appears turbid. What is the likely cause? This is a classic sign of bacterial contamination [42]. Under a microscope, bacteria may appear as tiny, moving granules between your cells [42]. You should isolate the contaminated culture immediately and decontaminate the work area [42].
FAQ 3: What are the critical tests for characterizing a Master Cell Bank (MCB)? Characterization of an MCB confirms identity, genetic stability, and purity [43]. The battery of tests typically includes [43]:
- Identity: Species confirmation via methods like STR analysis or QPCR [43] [44].
- Purity (Sterility): Tests for microbial contaminants (sterility, mycoplasma) and adventitious viruses [43].
- Viral Safety: Specific tests for retroviruses and other viruses relevant to the cell species (e.g., bovine, porcine, or human viruses depending on the cell's history) [43].
FAQ 4: How can I prevent cross-contamination of my cell line with other fast-growing lines? Cross-contamination is a serious and established problem [42]. To prevent it:
- Source Carefully: Obtain cell lines from reputable cell banks [42].
- Authenticate Routinely: Periodically check cell line characteristics using DNA fingerprinting, karyotype, or isotype analysis [44] [42].
- Practice Aseptic Technique: Always maintain good aseptic technique in the lab [42].
Troubleshooting Guides
Problem: Recurring Microbial Contamination in Media Preparation
Scenario: A firm experiences multiple media fill failures. The contaminant was not recovered using conventional microbiological techniques but was later identified via 16S rRNA gene sequencing as Acholeplasma laidlawii, a mycoplasma species known to penetrate 0.2-micron filters [45].
Investigation and Resolution Protocol:
- Identify the Organism: Use specialized methods like PCR or gene sequencing to detect cell wall-deficient organisms like mycoplasma that do not grow on standard media [45] [42].
- Trace the Source: The investigation confirmed the contaminant was present in the non-sterile bulk powder of the tryptic soy broth (TSB) used [45].
- Implement Corrective Actions:
- Change Filtration Protocol: For media preparation, consider using a 0.1-micron filter to retain small microorganisms like Acholeplasma laidlawii [45].
- Source Sterile Materials: Where possible, use sterile, irradiated media powders from commercial suppliers to avoid the risk entirely [45].
- Validate Cleaning Procedures: Revalidate cleaning procedures to verify the removal of the contaminant [45].
Problem: Raw Material with High Contamination Risk
Scenario: A new raw material of animal origin is required for cell culture media. How do you mitigate the inherent viral contamination risk?
Risk Mitigation Protocol:
- Classify the Material: Classify the RM as high-risk due to its animal origin [39] [40].
- Assess Usage Point: Determine if the material is used upstream (higher risk due to potential virus amplification) or downstream [39].
- Select Mitigations:
- Prefer Animal-Component Free (ACF): Source an ACF version of the material if available [39].
- Supplier Qualification: Audit the supplier to ensure they use viral inactivation steps in their production process and provide a comprehensive Certificate of Analysis (C of A) [39] [41].
- Implement Testing: Perform in-house viral testing or specific pathogen testing on the RM lot prior to release for use [39] [40].
Experimental Protocols & Data Presentation
Protocol 1: Adventitious Virus Detection in Cell Banks
Method: In Vitro Assay for Adventitious Agents [43]
Objective: To detect a wide range of potential viral contaminants in cell bank samples.
Procedure:
- Cell Lines: Inoculate the test sample onto a panel of cell lines with proven susceptibility to various viruses. Common lines include Vero, MRC-5, HeLa, and CHO cells [43].
- Incubation: Maintain the cultures for at least 28 days, with periodic subculturing [43].
- Observation: Monitor the cells daily for cytopathic effects (CPE), such as changes in morphology, cell lysis, or granulation.
- Confirmation: Use hemadsorption or hemagglutination assays at the end of the observation period to detect the presence of non-cytopathic viruses [43].
Protocol 2: Bioburden Testing for Raw Materials
Method: Total Aerobic Microbial Count (TAMC) and Total Yeast and Mould Count (TYMC) [40]
Objective: To enumerate the number of viable microorganisms in a raw material sample.
Procedure:
- Sample Preparation: Prepare a 1:10 dilution of the sample (10g or 10mL in a suitable diluent). For solids, use a validated method to extract microorganisms [40].
- Method Suitability (Bacteriostasis/Fungistasis): Challenge the sample with a low-level inoculum (e.g., S. aureus, P. aeruginosa, C. albicans, B. subtilis, A. brasiliensis) to confirm the material itself does not inhibit microbial growth [40].
- Enumeration: Perform one of the following methods, chosen hierarchically [40]:
- a) Membrane Filtration: Filter the sample, place the membrane on Tryptone Soy Agar (TSA) for TAMC and Sabouraud Dextrose Agar (SDA) for TYMC.
- b) Pour Plate: Mix the sample with liquefied agar and pour into a Petri dish.
- c) Spread Plate: Spread the sample on the surface of solid agar.
- Incubation and Counting:
- Incubate TAMC plates at 30-35°C for 3-5 days.
- Incubate TYMC plates at 20-25°C for 5-7 days.
- Count all colonies and report as cfu per gram or milliliter [40].
Table 1: Microbial Limit Criteria for Non-Sterile Raw Materials
| Test | Acceptance Criteria (cfu/g or mL) | Pharmacopeia Reference |
|---|---|---|
| Total Aerobic Microbial Count (TAMC) | Not more than 10³ (Maximum acceptable count: 2000) | Ph. Eur. 5.1.4 [40] |
| Total Yeast and Mould Count (TYMC) | Not more than 10² (Maximum acceptable count: 200) | Ph. Eur. 5.1.4 [40] |
Table 2: Essential Characterization Tests for Cell Banks
| Test Category | Specific Assays | Applicability (MCB / WCB / EPCB) |
|---|---|---|
| Identity | STR Analysis, Cytochrome C Oxidase QPCR [43] [44] | MCB, (WCB), EPCB [43] |
| Purity - Sterility | Sterility Test (EP/USP/JP) [43] | MCB, WCB, EPCB [43] |
| Purity - Mycoplasma | Mycoplasma qPCR or Culture Method [43] | MCB, WCB, EPCB [43] |
| Purity - Adventitious Viruses | In Vitro Assay (28 days, 3 cell lines), In Vivo Assay [43] | MCB, (WCB), EPCB [43] |
| Viral Safety | Retrovirus Tests (TEM, XC plaque assay, PERT assay) [43] | MCB, WCB, EPCB [43] |
| Species-Specific Viruses | MAP, HAP, or qPCR for bovine/porcine/human viruses [43] | MCB, (WCB) [43] |
Visual Workflows and Strategies
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Contamination Control
| Item | Function/Application | Key Considerations |
|---|---|---|
| Cell Culture Media | Supports cell growth and maintenance. | Use sterile, endotoxin-tested media. Be aware that non-sterile powder is a contamination risk [45] [42]. |
| Tryptic Soy Broth (TSB) | Used in media fill simulations to test aseptic processes. | Can be a source of cryptic contaminants like Acholeplasma laidlawii; consider sterile, irradiated forms [45]. |
| Antibiotics & Antimycotics | Suppress bacterial and fungal growth. | Should not be used routinely to avoid masking low-level contamination and developing resistance [42]. |
| Sterilizing Grade Filters | Remove microorganisms from solutions and gases. | Standard 0.2-micron filters may not retain mycoplasma; 0.1-micron filters are required for these small organisms [45]. |
| Liquid Nitrogen | For cryopreservation and long-term storage of cell banks. | Must be stored in vapor-phase LN2 tanks with alarm-monitored backup supply for security [46]. |
| Characterization Assays | (qPCR, TEM, in vivo/in vitro virus tests) | Used to confirm identity and purity of cell banks and to test for specific adventitious agents [43]. |
Leveraging Alien Controls and Bioinformatic Tools like Cont-ID for Cross-Contamination Monitoring
Welcome to the Cross-Contamination Monitoring Support Center
This resource provides troubleshooting guides and FAQs for researchers implementing advanced cross-contamination monitoring protocols, specifically focusing on the use of Alien Controls and the bioinformatic tool Cont-ID. These materials support viral diagnostic workflows and are framed within a broader thesis on reducing contamination risks in high-throughput sequencing (HTS) for virus detection.
Frequently Asked Questions (FAQs)
Q1: What is an "Alien Control" and why is it mandatory for cross-contamination monitoring with HTS?
An Alien Control is defined as a matrix infected by a target (the "alien target") that belongs to the same group as the target organisms to be tested but cannot be present in the actual samples of interest [47]. It is processed alongside your samples as an external control.
- Function: It acts as a sentinel to monitor cross-contamination within a sequencing batch. The presence of reads from the alien virus in any test sample is a definitive indicator of contamination from the alien control to that sample [47].
- Why it's mandatory: HTS technologies have极高的分析灵敏度, where even a single viral read can be detected. The alien control provides an empirical, batch-specific measure of the contamination level, moving beyond arbitrary thresholds and enabling reliable bioinformatic filtering [47].
Q2: Our lab is new to Cont-ID. What are the basic requirements to run it?
To use Cont-ID effectively, you need to meet the following prerequisites [47]:
- Sequencing Technology: Cont-ID is designed for data generated by Illumina sequencing technology.
- Batch Processing: All samples in the sequencing batch must have been processed in parallel in the laboratory, following the same steps.
- Alien Control: At least one alien control must be included in the batch.
- Bioinformatic Input: Cont-ID relies on the output of standard bioinformatic analyses. You must provide a file containing the read counts for each virus species identified in every sample of the batch.
Q3: We detected a low number of viral reads in a sample. How can we determine if it's a true infection or cross-contamination?
This is a core challenge that the Alien Control/Cont-ID system is designed to address. The following workflow outlines the diagnostic process:
Q4: What are the most common sources of cross-contamination in HTS workflows, and how can we mitigate them?
Cross-contamination can occur at multiple stages. The table below summarizes common sources and preventive measures.
| Stage | Contamination Risk | Preventive Measure |
|---|---|---|
| Nucleic Acid Extraction | Aerosols or carryover between samples in a plate [47]. | Use of uracil-DNA glycosylase (UDG) to degrade carryover amplicons, physical separation of pre- and post-PCR areas [47]. |
| Library Preparation | Splashing, pipetting errors, or reagent contamination [47]. | Use of alternate dual indexes to identify index hopping, inter-run washing steps, and laboratory decontamination of surfaces and equipment [47]. |
| Sequencing | Index hopping or carryover from a previous sequencing run on the same machine [47]. | Use of unique dual indexes (UDIs), and following manufacturer decontamination protocols for the sequencer [47]. |
Troubleshooting Guides
Problem: Cont-ID is not classifying any detections, or the classification accuracy seems low.
| Possible Cause | Solution |
|---|---|
| Incorrect input file format | Ensure your read count file matches the expected format specified in the Cont-ID documentation. Validate the file with a simple test dataset. |
| Alien control not properly specified | Verify that the alien control is correctly labeled in your sample sheet and that the alien virus is abundant enough in the control to be detected. |
| Low-level contamination is below the detection threshold | Cont-ID's accuracy (91%) relies on a clear contamination signal. For very low-level cross-over, manual inspection and confirmation may still be necessary [47]. |
Problem: We are seeing a high rate of cross-contamination across many samples, as indicated by the alien control.
| Possible Cause | Solution |
|---|---|
| Contaminated shared reagents | Prepare fresh aliquots of critical reagents like water and buffers. Use filter tips for all pipetting steps. |
| Inadequate cleaning of equipment | Implement more rigorous decontamination protocols for laboratory equipment, such as robotic workstations and pipettes. Increase the frequency of cleaning. |
| Aerosol generation during sample handling | Review and refine techniques to minimize aerosol generation. Centrifuge tubes briefly before opening, and avoid vigorous vortexing of open tubes. |
Experimental Protocols
Protocol: Implementing Alien Controls in a Viral Metagenomics Study
- Alien Selection: Choose an alien virus that is phylogenetically similar to the viruses you are detecting but is impossible to find in your sample type (e.g., a plant virus in human clinical samples) [47].
- Sample Preparation: Grow the alien virus in its appropriate host system. Quantify the virus to achieve a high concentration, ideally close to the highest expected concentration in your test samples [47].
- Nucleic Acid Extraction: Process the alien control sample through the same nucleic acid extraction protocol as your test samples.
- Library Preparation and Sequencing: Include the alien control in the same library preparation batch and sequencing run as all your test samples.
- Data Analysis: Use the alien control's data as a reference point in your bioinformatic pipeline (e.g., Cont-ID) to assess cross-contamination levels.
Protocol: Validating Cont-ID Performance in Your Lab
To validate Cont-ID, you can create a mock sequencing batch with known positive and negative samples.
- Materials Needed:
- Known positive samples for specific viruses.
- Known negative samples.
- Your chosen alien control.
- Procedure:
- Spike known positive samples at various concentrations (high, medium, low).
- Process the entire mock batch (positives, negatives, alien control) together through extraction, library prep, and sequencing.
- Run the generated HTS data through your standard viral detection pipeline to get read counts.
- Execute Cont-ID using the read count file and the alien control designation.
- Compare Cont-ID's classifications against the expected results to calculate its accuracy and sensitivity in your specific lab context.
The Scientist's Toolkit: Key Research Reagents & Materials
The following table details essential materials for implementing this contamination monitoring framework.
| Item | Function |
|---|---|
| Alien Virus Isolate | The core of the control system. Provides a measurable signal for tracking the transfer of genetic material between samples during processing [47]. |
| Unique Dual Indexes (UDIs) | DNA barcodes used during library preparation. UDIs minimize the misassignment of reads to the wrong sample (index hopping), a common source of contamination in HTS [47]. |
| Nuclease-Free Water | A critical reagent for preparing solutions and dilutions. Using certified nuclease-free water prevents the introduction of external nucleic acids that can contaminate experiments. |
| Cont-ID Software | The bioinformatic tool that automates the detection of cross-contamination by analyzing read count patterns and the alien control signal across a batch of samples [47]. |
Environmental Monitoring and Rapid Mobile qPCR for Surface Contamination
This technical support center provides troubleshooting guides and FAQs to support researchers in reducing contamination risks in viral diagnostic and environmental monitoring workflows utilizing rapid mobile qPCR.
Troubleshooting Guide for Contamination and Assay Performance
The following table outlines common qPCR issues encountered during environmental monitoring, their potential causes, and recommended corrective actions.
| Issue Observed | Potential Causes | Troubleshooting Steps & Solutions |
|---|---|---|
| Amplification in No Template Control (NTC) [3] [48] [49] | Contaminated reagents (primers, master mix, water) [48]; Carryover amplicon contamination from previous runs [3]; Aerosol contamination during pipetting [3]. | Replace reagents systematically [3]; Implement physical separation of pre- and post-PCR areas [3]; Use aerosol-resistant filter tips [3]; Decontaminate surfaces with 10-15% fresh bleach solution [3]; Employ UNG (uracil-N-glycosylase) enzyme treatment to degrade carryover contaminants [3] [48]. |
| High Ct (Cycle Threshold) Values/Late Amplification [50] | Low template concentration/quality [50]; Presence of PCR inhibitors [50] [49]; Degraded primers/probes [50]; Suboptimal reaction efficiency [50]. | Confirm template quality and concentration [50]; Check primer/probe integrity and freeze-thaw cycles [50]; Use additives like BSA or DMSO to counteract inhibitors [49]; Verify pipetting accuracy and reagent mixing [50]. |
| Non-Specific Amplification (e.g., Multiple Peaks in Melt Curve) [50] | Primers binding to non-target sequences; Annealing temperature too low [50]; Contaminated reagents or environment [50]. | Optimize annealing temperature [50]; Check primer design for specificity; Review assay conditions for contamination [50]. |
| No Amplification [50] [49] | Template omission [49]; Presence of strong PCR inhibitors [49]; Incorrect thermal cycler settings [50]; Failed reagent (e.g., degraded probe, enzyme inactivity) [49]. | Verify template was added [49]; Check thermal cycler program [50]; Include a positive control to confirm reagent/assay functionality [50]; Use an internal positive control (IPC) to check for inhibition [49]. |
| Inconsistent Replicates [50] | Inconsistent pipetting [50]; Inadequate mixing of reagents [50]; Uneven sealing of reaction plates causing evaporation [50]. | Calibrate pipettes and ensure proper technique [50]; Mix reagents thoroughly before aliquoting [50]; Ensure plates are properly sealed [50]. |
Frequently Asked Questions (FAQs)
Q1: What is the most critical control for monitoring contamination in every qPCR run? The No Template Control (NTC) is essential. It contains all reaction components except the nucleic acid template. Amplification in the NTC indicates contamination of one or more reagents or the environment with the target sequence, necessitating a review of procedures and reagents [3] [48].
Q2: How can laboratory layout minimize contamination risks? Implementing a unidirectional workflow with physically separated areas is fundamental [3] [51].
- Pre-PCR Area (Pre-amplification): Dedicated to reagent preparation, sample handling, and reaction setup. This area should have dedicated equipment, lab coats, and consumables [3].
- Post-PCR Area (Post-amplification): Dedicated to the qPCR instrument and analysis of amplified products. Nothing from the post-PCR area should return to the pre-PCR area without rigorous decontamination [3] [51].
Q3: Our research involves mobile qPCR for onsite water testing. How reliable are the results from portable systems? Validation studies demonstrate that onsite qPCR with portable equipment can yield highly reliable results. One study showed that marker genes quantified with a portable Q qPCR instrument agreed within ±0.3 log10 units with results from conventional laboratory equipment, supporting its use for rapid, onsite decision-making [52].
Q4: Besides laboratory surfaces, what unexpected items can be sources of contamination? Personal items such as mobile phones, jewelry, and even hair can transmit contamination. One study found virus RNA on 38.5% of healthcare workers' mobile phones [53]. Adherence to strict personal protective equipment (PPE) protocols and avoiding introducing personal items into pre-PCR areas is critical [3] [53].
Experimental Protocol: Onsite qPCR for Fecal Pollution Tracking in Surface Waters
This detailed methodology, adapted from a field deployment study, enables rapid, onsite quantification of microbial source-tracking markers in water samples using portable equipment [52].
Principle
This protocol uses a portable qPCR system to quantitatively detect host-associated genetic markers (e.g., HF183 for human-specific Bacteroides) directly at the sampling site. This allows for near real-time assessment of fecal contamination in surface waters, reducing the risk of sample alteration during transport and storage [52].
Equipment & Reagents
- Portable Q qPCR Instrument (e.g., Quantabio) [52]
- Portable vacuum pump and filtration units [52]
- Portable centrifuge and vortex mixer [52]
- Portable fluorometer (e.g., Qubit) for DNA quantification [52]
- DNeasy PowerWater Kit (Qiagen) or equivalent for DNA extraction [52]
- qPCR master mix and validated primer/probe sets for target genes (e.g., HF183, 16S rRNA, E. coli rodA) [52]
- Aerosol-resistant filtered pipette tips [3]
- Personal protective equipment (dedicated lab coats, gloves) [3]
- Surface decontamination supplies (fresh 10% bleach, 70% ethanol) [3]
Step-by-Step Procedure
Workflow for Onsite qPCR Analysis
- Onsite Sample Collection: Collect water samples (e.g., 100-300 mL from river, storm drain) in sterile bottles. Simultaneously measure physicochemical parameters (temperature, pH, turbidity) using portable meters [52].
- Sample Concentration: Filter the water sample through a 0.22 µm membrane filter using a portable vacuum pump to concentrate microbial biomass [52].
- Onsite DNA Extraction:
- Transfer the filter membrane to the lysis tubes provided in the DNA extraction kit.
- Perform the extraction protocol (including bead-beating via vortex) strictly within the designated "pre-PCR" area of the mobile laboratory, using dedicated portable equipment (centrifuge, vortex) [52].
- Elute the purified DNA in the provided elution buffer.
- DNA Quality Control: Use a portable fluorometer to quantify the extracted DNA yield. This step is optional but helps assess extraction success [52].
- qPCR Reaction Setup:
- Prepare the qPCR master mix on a clean, decontaminated surface in the pre-PCR area.
- Include essential controls: No Template Control (NTC), positive control (with known template), and if applicable, a negative control for extraction [48].
- Use aerosol-resistant pipette tips throughout.
- Aliquot the master mix and add the extracted DNA sample.
- Portable qPCR Run: Transfer the sealed reaction plate to the portable qPCR instrument located in the "post-PCR" area of the mobile lab. Initiate the optimized cycling protocol for the target markers [52].
- Onsite Data Analysis: Analyze the qPCR data (Ct values, standard curves) using the software connected to the portable instrument. Results for key markers like HF183 can be generated within 3 hours of sampling, enabling rapid risk assessment [52].
Research Reagent Solutions for Environmental qPCR
The following table lists key reagents and materials critical for successful and contamination-free environmental qPCR.
| Reagent / Material | Function / Purpose | Key Considerations for Use |
|---|---|---|
| Aerosol-Resistant Filtered Pipette Tips [3] [51] | Prevents aerosol-borne contaminants from entering pipette shafts and cross-contaminating samples and reagents. | Essential for all liquid handling steps, especially in master mix preparation and sample addition [3]. |
| Master Mix with UNG (Uracil-N-Glycosylase) [3] [48] | Enzymatically degrades any PCR products (amplicons) from previous reactions that contain uracil, preventing "carryover contamination." | Requires the use of dUTP in the nucleotide mix during the initial PCR to create uracil-containing amplicons [3]. |
| DNeasy PowerWater Kit [52] | DNA extraction kit optimized for efficient lysis of diverse microorganisms (including Gram-positive bacteria) in water samples and efficient removal of PCR inhibitors (e.g., humic acids). | Validated for use with portable equipment (vortex) for onsite applications; effective for samples with high suspended solids [52]. |
| Validated Primer/Probe Sets (e.g., HF183, 16S rRNA) [54] [52] | Targets specific genetic markers for microbial source tracking (human, animal) or general fecal indicators. | Ensures assay specificity and sensitivity. Aliquot primers and probes to minimize freeze-thaw cycles and prevent degradation [50] [51]. |
| Surface Decontamination Solution (10% fresh bleach) [3] [51] | Inactivates contaminating nucleic acids on work surfaces, equipment, and touchpoints. | Must be prepared fresh weekly for maximum efficacy. Allow 10-15 minutes of contact time before wiping with deionized water [3]. |
Troubleshooting Common Pitfalls and Optimizing Protocols
Overcoming Limitations in Assay Sensitivity and Specificity
Frequently Asked Questions
What are the most common factors that reduce sensitivity in point-of-care viral diagnostics? Common factors include inefficient nucleic acid extraction from complex samples, enzymatic inhibition during amplification, suboptimal primer/probe design, and low target abundance. Furthermore, in integrated "one-pot" assays, competition between target amplification and reporter cleavage can significantly reduce sensitivity [55].
How can I improve the specificity of my CRISPR-based diagnostic assay to avoid false positives? Specificity can be enhanced by using multiple guide RNAs (gRNAs) targeting unique pathogen sequences, carefully designing gRNAs with stable secondary structures to minimize off-target binding, and employing chemical or physical methods to compartmentalize amplification and detection steps, thereby reducing amplicon contamination [55].
My one-pot RPA-CRISPR assay shows delayed and attenuated signal. What could be the cause? This is frequently caused by excessive cis-cleavage activity, where the Cas enzyme degrades the amplicon product before it can be detected. To resolve this, use gRNAs with asymmetric cleavage activity that favor trans-cleavage (reporter cleavage) over cis-cleavage (amplicon degradation). Optimizing the ratios of multiple gRNAs can also improve kinetics and signal strength [55].
What are the best practices to minimize contamination risk in molecular point-of-care tests? Key practices include using closed-tube systems like lateral flow assays for end-point detection, implementing single-use, disposable cartridges, and incorporating uracil-DNA glycosylase (UDG) systems to degrade carryover amplicons in subsequent tests. Physical separation of pre- and post-amplification areas is also critical, even in point-of-care settings [56] [55].
Experimental Protocols for Enhanced Assay Performance
Protocol 1: Developing a High-Sensitivity, One-Pot RPA-CRISPR Assay
This protocol is adapted from a sensitive tuberculosis detection assay (ActCRISPR-TB) and can be modified for other viral targets [55].
gRNA Design and Screening:
- Tile the target genetic sequence (e.g., a conserved viral region) to identify potential gRNA binding sites, including those with non-canonical Protospacer Adjacent Motifs (PAMs) [55].
- Screen candidate gRNAs for stable secondary structures and low cis-cleavage activity relative to their trans-cleavage activity. Normalized activity comparisons can identify gRNAs that favor trans-cleavage, which is crucial for signal accumulation in a one-pot system [55].
Reaction Setup and Optimization:
- Set up a one-pot reaction in a single tube containing:
- Sample: Extracted nucleic acid.
- Primers: 500 nM each of forward and reverse RPA primers.
- Magnesium: 16.8 nM Mg²⁺ (optimized concentration).
- RNP Complex: 40 nM Cas12a protein pre-complexed with a combination of gRNAs (e.g., 30 nM gRNA-5 and 10 nM gRNA-2, as used in the study) [55].
- ssDNA Reporter: 600 nM fluorescent or lateral-flow compatible reporter.
- Incubate the reaction at a constant temperature of 36–40 °C for 45–60 minutes [55].
- Set up a one-pot reaction in a single tube containing:
Signal Detection:
- Monitor fluorescence in real-time or use a lateral flow dipstick at the endpoint. A positive sample with 5 copies/μL sensitivity should be detectable within 15-60 minutes [55].
Protocol 2: Utilizing Multiple gRNAs to Boost Signal and Specificity
- Identify Complementary gRNAs: Select 2-3 gRNAs that target distinct, non-overlapping sites on the same amplicon and have been individually validated for target specificity [55].
- Optimize gRNA Ratios: At a constant total gRNA concentration, test different molar ratios of the gRNAs. A slight shift in ratio can markedly affect assay kinetics. For example, a 30:10 ratio of a high-trans-cleavage gRNA to a supporting gRNA may enhance signal, while a 10:30 ratio may attenuate it due to increased cis-cleavage activity [55].
- Validate Performance: Determine the new limit of detection (LoD) and specificity of the multi-gRNA assay. The cited study achieved a LoD of 5 copies/μL using a combination of three gRNAs, a 20-fold improvement over a single canonical gRNA [55].
Quantitative Data on Diagnostic Performance
The table below summarizes the performance of advanced molecular assays as reported in recent studies.
Table 1: Performance Metrics of Advanced Diagnostic Assays
| Assay Technology | Pathogen Target | Limit of Detection (LoD) | Clinical Sensitivity | Clinical Specificity | Time to Result |
|---|---|---|---|---|---|
| ActCRISPR-TB (One-pot) [55] | Mycobacterium tuberculosis | 5 copies/μL | 93% (respiratory samples) | 100% | 15-45 minutes |
| Multi-guide RNA Cas12a Assay [55] | Tuberculosis (various samples) | 5 copies/μL | 74% (prospective tongue swabs) | 100% | 60 minutes |
| CRISPR-based Systems (General) [57] | Various VPVIs* | Varies by target and design | High (Technology-dependent) | High (Technology-dependent) | Rapid (minutes to hours) |
| Biosensor-based POC assays [57] | Various VPVIs* | High (with signal amplification) | Good to High | Good to High | Minutes |
*VPVIs: Vaccine-Preventable Viral Infections (e.g., mpox, hepatitis, influenza, dengue, COVID-19) [57].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Developing Advanced Viral Diagnostics
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Cas12a Protein | CRISPR-associated nuclease; binds gRNA to cleave target DNA and a reporter molecule upon recognition. | Preferred for its robust trans-cleavage activity. Requires compatibility with isothermal amplification buffers [55]. |
| Guide RNAs (gRNAs) | Directs the Cas protein to the specific target nucleic acid sequence. | Using multiple gRNAs targeting distinct sites can enhance both sensitivity and signal intensity [55]. |
| RPA Primers | Amplifies the target nucleic acid sequence at a constant temperature (isothermal amplification). | Primer design is critical for efficiency and specificity. Asymmetric primer ratios can be used to favor the production of single-stranded DNA for certain Cas enzymes [55]. |
| ssDNA Reporter | Produces a detectable signal (fluorescent or colorimetric) when cleaved by the Cas-gRNA complex. | A quenched fluorescent probe (e.g., FAM/ZEN/Iowa Black FQ) or biotin/FAM-labeled probe for lateral flow detection is standard [55]. |
| Lateral Flow Dipstick | Provides a simple, visual, endpoint readout for point-of-care use. | Detracts labeled reporters, often used with biotin- and FAM-labeled complexes in a sandwich format [55]. |
| Biosensors | Transducers that convert a biological interaction (e.g., antigen-antibody binding) into a measurable signal. | Incorporate nanomaterials for signal amplification. Ideal for compact, portable POC devices [57]. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow and key mechanisms in a high-sensitivity, one-pot CRISPR assay.
Diagram 1: One-pot asymmetric CRISPR assay workflow.
This diagram details the signaling pathway that dictates assay sensitivity.
Diagram 2: CRISPR Cas12a cis vs. trans cleavage pathways.
Addressing Cross-Contamination in High-Throughput Sequencing Workflows
Cross-contamination presents a significant challenge in high-throughput sequencing (HTS), particularly in viral diagnostics and metagenomic studies where it can lead to erroneous variant calls and false-positive results. This technical support guide addresses common contamination sources and provides actionable solutions to maintain data integrity within viral diagnostic workflows. Implementing robust contamination control measures is essential for reliable results in research and drug development applications.
FAQs: Understanding Sequencing Contamination
Contamination in HTS originates from two major sources:
External contamination: Introduced from outside the sample during collection and processing. This includes contaminants from skin, laboratory equipment, collection tubes, laboratory surfaces, extraction kits, PCR reagents, and even molecular biology-grade water [58]. Commercial extraction kits often contain microbial DNA contaminants (often called "kitome") that vary between batches and manufacturers [58].
Internal/cross-contamination: Occurs between samples during library preparation, particularly during liquid handling procedures. This is especially problematic in amplicon-based HTS methods where pipetting and transferring amplified products between PCRs creates significant contamination risk [59].
How does contamination specifically affect viral metagenomic studies?
Viral metagenomics is particularly vulnerable to contamination effects because:
- Low biomass samples have minimal viral nucleic acids, making them susceptible to being overwhelmed by contaminating sequences [58]
- Reagent contamination with viral sequences (e.g., equine infectious anemia virus or murine leukemia virus found in reverse transcriptase enzymes) can generate false positives [58]
- Cross-contamination between samples during library preparation can lead to erroneous variant calling and false minority variants [59]
- Control sequences and spike-ins (such as PhiX in Illumina or DCS in Nanopore) can persist in public databases if not properly removed [60]
What controls can I implement to detect contamination?
Effective contamination monitoring requires strategic controls:
- Negative System Controls (NSCs): Include non-target amplicons (e.g., MS2 bacteriophage RNA replicase gene) in separate reaction wells to capture cross-contaminating reads during library preparation [59]
- Reagent blanks: Process blank samples alongside experimental samples to identify kit-derived contaminants [58]
- Statistical thresholds: Establish cut-off values based on prediction intervals (e.g., 99.99% prediction intervals) from control data to filter contamination reads [59]
Are some sequencing protocols more prone to contamination?
Yes, certain methodologies present higher contamination risks:
- Amplicon-based approaches utilizing two sequential PCRs have heightened contamination risk during amplified product transfer [59]
- RNA sequencing is more susceptible than DNA sequencing due to the additional reverse transcription step [58]
- Protocols requiring whole-genome amplification introduce more contamination opportunities through additional processing steps [58]
- Manual library preparation methods show higher contamination rates compared to automated systems due to increased manual transfer steps [58]
Troubleshooting Guides
Problem: Suspected Sample-to-Sample Cross-Contamination
Observable Symptoms:
- Detection of unexpected viral sequences in negative controls
- Similar minority variants appearing across multiple samples
- Inconsistent replication of low-frequency variants between technical replicates
Diagnostic Steps:
- Review Laboratory Protocols: Identify steps with high contamination potential, particularly during amplicon transfer in targeted sequencing [59]
- Analyze Negative Controls: Map all NSC reads against target reference sequences to quantify contamination levels [59]
- Check Batch Effects: Determine if contamination correlates with specific processing dates, technicians, or reagent lots [58]
Solutions:
- Implement automated liquid handling systems to reduce manual transfer errors [59] [58]
- Include NSCs in multiple well positions to identify spatial contamination patterns within plates [59]
- Redesign workflow to minimize amplicon manipulation and tube openings
- Use unique dual indices to identify and filter cross-contaminated samples bioinformatically
Problem: Reagent-Derived Contamination ("Kitome")
Observable Symptoms:
- Consistent background contaminants across all samples processed together
- Detection of unexpected microbial or viral taxa with low read counts
- Higher background noise in low-biomass samples
Diagnostic Steps:
- Process Reagent Blanks: Extract and sequence blank samples using the same reagents [58]
- Compare Reagent Lots: Process the same control sample with different reagent batches to identify batch-specific contaminants [58]
- Analyze Contaminant Patterns: Identify consistent "kitome" signatures specific to extraction kits and reagents [58]
Solutions:
- Use the same reagent batches throughout a project to maintain consistent background [58]
- Implement enzymatic treatments (e.g., DNase) to reduce nucleic acid contaminants in reagents [58]
- Include extraction blanks in every sequencing run to establish background subtraction thresholds
- Select reagents with minimal contaminant profiles based on manufacturer testing data
Problem: In Silico Contamination in Data Analysis
Observable Symptoms:
- Persistent spike-in sequences (PhiX, DCS) in assembled genomes [60]
- Misclassification of control sequences as biological contaminants [60]
- Host sequences dominating metagenomic samples
Diagnostic Steps:
- Screen for Control Sequences: Map reads to databases of known spike-ins and control sequences [60]
- Check Sequence Classification: Verify taxonomic assignments against expected species
- Analyze Assembly Anomalies: Identify regions with unexpected homology to common contaminants
Solutions:
- Implement bioinformatic decontamination pipelines like CLEAN that remove unwanted sequences from both long and short reads [60]
- Use "keep" parameters to preserve sequences from closely related species while removing contaminants [60]
- Apply strict filtering thresholds based on negative control read counts [59]
- Verify findings using multiple classification approaches
Experimental Protocols for Contamination Control
Protocol 1: Contamination-Monitored Library Preparation for Viral Sequencing
This protocol adapts methods from [59] for influenza A virus sequencing with enhanced contamination controls:
Materials:
- Sentosa SX101 liquid handling platform or equivalent automated system
- Nextera XT DNA Library Preparation Kit (Illumina)
- MS2 bacteriophage amplicons (1130 bp RNA replicase gene) for NSC
- Modified primers with complete Nextera transposon sequences
Procedure:
- Primer Design: Add complete Nextera transposon sequences as overhanging regions adjacent to 5'-end of target-specific sequences (Tuni-12 and Tuni-13 for influenza) [59]
- Primer Titration: Perform initial optimization to achieve even coverage across all gene segments [59]
- Library Preparation Setup:
- Distribute samples across plate with NSCs in strategic well positions
- Use automated liquid handling to minimize cross-contamination
- Process negative extraction controls alongside samples
- Indexing PCR: Utilize dual indexing strategies to track cross-contamination
- Quality Control: Assess library quality and confirm NSC purity
Protocol 2: Bioinformatic Decontamination with CLEAN Pipeline
The CLEAN pipeline [60] provides comprehensive decontamination for various sequencing data types:
Input Requirements:
- FASTQ files (short-read, long-read, or FASTA-formatted sequences)
- Contamination reference FASTA file (optional)
- Platform specification (Illumina, Nanopore, or PacBio)
Procedure:
- Setup: Install CLEAN from https://github.com/rki-mf1/clean using Nextflow [60]
- Mapping: Reads are mapped against contamination reference using minimap2 (default) or BWA MEM for short reads [60]
- Classification: Separate mapped (contaminant) from unmapped (clean) reads using SAMtools [60]
- Optional k-mer Filtering: For Illumina data, use bbduk for direct k-mer-based filtering [60]
- Quality Reporting: Generate quality reports for input, clean, and contamination files using FastQC, NanoPlot, or QUAST [60]
- Report Generation: MultiQC summarizes all quality reports and mapping statistics in HTML format [60]
Special Parameters:
dcs_strict: For ONT DCS control, exclusively considers reads aligning to DCS and covering artificial ends [60]min_clip: Filter mapped reads by total length of soft-clipped positions [60]keep: Specify reference sequences to preserve if falsely classified as contaminants [60]
Data Analysis and Interpretation
Quantitative Contamination Assessment
Table: Contamination Read Thresholds from Influenza A Sequencing Study [59]
| Gene Segment | Maximum Contamination Reads in NSC | Recommended Cut-off Method |
|---|---|---|
| Segment 1 | 159 reads | 99.99% prediction interval |
| Segment 2 | 76 reads | 99.99% prediction interval |
| Segment 3 | 188 reads | 99.99% prediction interval |
| Segment 4 | 88 reads | 99.99% prediction interval |
| Segment 5 | 139 reads | 99.99% prediction interval |
| Segment 6 | 74 reads | 99.99% prediction interval |
| Segment 7 | 706 reads | 99.99% prediction interval |
| Segment 8 | 178 reads | 99.99% prediction interval |
Contamination Source Identification
Table: Common Contamination Sources and Mitigation Strategies [58]
| Contamination Source | Examples | Mitigation Strategies |
|---|---|---|
| Extraction kits | Microbial DNA in commercial kits | Use same batches throughout project; include extraction blanks |
| Polymerases | Bacterial DNA in Taq polymerase | Use high-fidelity enzymes with minimal contaminants |
| Laboratory environment | Airborne contaminants; surface bacteria | Implement UV irradiation; regular cleaning protocols |
| Human sources | Skin flora; mishandling | Use gloves; minimize sample exposure |
| Cross-contamination | Amplified product carryover | Physical separation of pre- and post-PCR areas |
Research Reagent Solutions
Table: Essential Materials for Contamination-Controlled Viral Sequencing
| Reagent/Kit | Function | Contamination Control Features |
|---|---|---|
| Nextera XT DNA Library Prep Kit | Library preparation for Illumina platforms | Enzymatic fragmentation reduces contamination risk vs mechanical shearing |
| CLEAN Bioinformatics Pipeline | Computational decontamination | Removes spike-ins, host sequences, and user-specified contaminants |
| MS2 Bacteriophage Amplicons | Negative System Control (NSC) | Non-target control for detecting cross-contamination |
| Automated Liquid Handling Systems | Library preparation automation | Reduces manual transfer errors and cross-contamination |
| High-Fidelity Polymerases | Amplification for low-biomass samples | Minimal microbial DNA contaminants compared to standard Taq |
Workflow Diagrams
Contamination Control Workflow: This diagram illustrates the complete sequencing workflow with key contamination risks (red) and corresponding control measures (blue) at each stage.
Effective contamination control in high-throughput sequencing requires integrated strategies spanning wet laboratory procedures and bioinformatic analysis. By implementing systematic monitoring through negative controls, standardizing reagent use, automating liquid handling, and applying computational decontamination tools like CLEAN, researchers can significantly reduce contamination risks in viral diagnostic workflows. These practices are essential for maintaining data integrity and ensuring reliable results in both research and clinical applications.
Troubleshooting Guides
Vaporized Hydrogen Peroxide (VHP) Troubleshooting
Problem: Inconsistent Biological Indicator (BI) Kill in Validation Studies
- Potential Cause 1: Inadequate VHP distribution leading to shadowed or low-concentration zones.
- Solution: Verify secondary distribution system (e.g., HVAC, strategically placed fans). Perform detailed chamber mapping using multiple chemical and biological indicators to identify weak spots. Ensure all room penetrations are sealed during the cycle [61].
- Potential Cause 2: Improper environmental conditions (Temperature and Humidity).
- Potential Cause 3: Residual organic material or moisture on surfaces.
Problem: Long Cycle Times Impacting Laboratory Workflow
- Potential Cause: Use of portable, non-piped VHP generators that remain in the room during aeration.
UV-C Technology Troubleshooting
Problem: Failure to Achieve Expected Log Reduction on Surfaces
- Potential Cause 1: "Line-of-Sight" limitation and shadowing.
- Potential Cause 2: Incorrect UV Dose Calculation.
- Solution: The germicidal effect is a function of intensity and exposure time (Dose = Intensity × Time). Measure UV-C intensity at the target surface with a radiometer and increase exposure time accordingly to achieve the required dose [65].
- Potential Cause 3: Lamp output degradation over time.
- Solution: Implement a preventive maintenance schedule that includes regular cleaning of lamp sleeves and periodic replacement of UV-C lamps according to the manufacturer's specifications, even if they haven't burned out [65].
Problem: Integrating Far-UVC in Occupied Spaces
- Potential Cause: Concerns about human exposure to 254 nm UV-C radiation.
- Solution: Consider Far-UVC (222 nm) technology. Evidence suggests 222 nm light effectively inactivates pathogens while having reduced penetration into human skin and eyes, making it promising for continuous disinfection in occupied spaces like laboratories [65] [67]. Ensure all safety protocols and regulatory guidance for occupied spaces are followed.
Manual Cleaning Troubleshooting
Problem: High Bioburden Recovery After Manual Disinfection
- Potential Cause 1: Human error and inconsistent application.
- Potential Cause 2: Incorrect contact time for the disinfectant.
- Solution: Review the disinfectant's manufacturer instructions. Ensure the solution remains wet on the surface for the entire recommended, validated contact time to achieve microbial kill [68].
- Potential Cause 3: Incompatibility of disinfectant with the surface material or soil load.
- Solution: Validate the cleaning agent for the specific surfaces and soils in your lab. Neutral detergents may be needed to remove residue before sporicidal disinfectant application [63].
Frequently Asked Questions (FAQs)
Q1: Can VHP or UV-C replace manual cleaning entirely in a viral diagnostics lab? A: No. Manual cleaning is an essential first step to remove visible soil, dust, and organic matter that can shield microorganisms from VHP vapor or UV-C light [67] [64]. Both VHP and UV-C are disinfection or biodecontamination technologies, not cleaning processes. A robust strategy uses manual cleaning followed by an automated technology for a higher assurance level [67].
Q2: For a high-throughput lab, which is more suitable: VHP or UV-C? A: UV-C is typically faster for daily decontamination of flat, line-of-sight surfaces, with cycles lasting minutes [66]. VHP cycles are longer (hours) but provide more comprehensive coverage, including hard-to-reach and shadowed areas [66] [63]. The choice depends on your risk assessment: speed (UV-C) vs. comprehensiveness (VHP). For rapid turnover of equipment like biosafety cabinets, UV-C may be ideal. For terminal decontamination of a room post-maintenance, VHP is superior [66] [63].
Q3: How do I validate that my decontamination method is effective? A: Validation requires a documented protocol using defined acceptance criteria.
- For VHP: Use biological indicators (e.g., Geobacillus stearothermophilus spores) and chemical indicators placed at worst-case locations to verify a defined log reduction (e.g., a 6-log reduction) and vapor distribution [62] [63].
- For UV-C: Validate using microbiological methods (e.g., inoculated carriers with target viruses or bacteria) and radiometry to measure the delivered UV dose, correlating it to log reduction [65].
- For Manual Cleaning: Common methods include swab or rinse sampling for chemical residues (e.g., total organic carbon) or bioburden after cleaning [68].
Q4: What are the key safety considerations for VHP and UV-C? A:
- VHP: Requires a sealed environment. Operators must not be present during the cycle. Room air must be verified as safe (using sensors) before re-entry due to potential irritant effects of residual H₂O₂ [66] [61].
- UV-C (254 nm): Presents an exposure hazard to skin and eyes. Rooms must be unoccupied during operation, and safety interlocks are recommended to prevent accidental exposure [65]. Far-UVC (222 nm) has different safety profiles and may be used in occupied spaces, but following all applicable safety guidelines is critical [65] [67].
Quantitative Data Comparison
The table below summarizes key performance metrics for the decontamination strategies, crucial for risk assessment and protocol design.
Table 1: Quantitative Comparison of Decontamination Methods
| Parameter | Manual Disinfection | Vaporized Hydrogen Peroxide (VHP) | UV-C Technology |
|---|---|---|---|
| Typical Log Reduction | Varies by agent and technique; sporicides can achieve >6-log [63] | Capable of a >6-log reduction of bacterial spores [63] [64] | Varies by dose and organism; 1-4 log for spores in practice [65] |
| Cycle Time | 30 mins - 2 hrs (labor-intensive) | 1.5 - 5 hours (including aeration) [66] [63] | Minutes to 1.5 hours [66] |
| Coverage | All physical surfaces (dependent on operator) | Comprehensive, including complex and hidden areas [66] [63] | Line-of-sight only; shadowed areas are not treated [66] |
| Automation Level | Fully manual | Fully automated cycles [61] | Can be automated with timers/sensors |
| Key Operational Limitation | Human error, contact time, chemical residues | Room sealing, environmental control (T, RH) [63] | Shadowing, distance from source, lamp aging [65] |
Experimental Protocols
Protocol: Validating a VHP Decontamination Cycle
Objective: To demonstrate that the VHP cycle consistently achieves a ≥6-log reduction of Geobacillus stearothermophilus spores within a specified enclosure.
Materials:
- VHP Generator (Integrated or Portable)
- Biological Indicators (BIs) containing ≥10⁶ G. stearothermophilus spores
- Chemical Indicators
- Biological Indicator Reader or Culture Media
- Data Loggers for Temperature and Humidity
Methodology:
- Preparation: Perform a validated manual cleaning of the room. Seal all penetrations. Place BIs and chemical indicators at predetermined worst-case locations (e.g., farthest from injection point, inside cabinets, under tables) [63].
- Cycle Development & Execution: Condition the room to the required temperature and humidity. Execute the VHP cycle (injection, dwell, aeration) as per the developed protocol [62] [61].
- Post-Cycle Analysis: Retrieve the BIs after cycle completion and aeration. Aseptically transfer each BI to sterile culture media and incubate according to the manufacturer's specifications.
- Interpretation: The cycle is considered validated if all test BIs show no growth (sterile) and the quality control BIs (non-exposed) show growth, confirming a ≥6-log reduction [63].
Protocol: Determining the UV-C Dose for Viral Inactivation
Objective: To establish the UV-C dose (J/m²) required to achieve a target log reduction (e.g., 3-log) of a model virus on a non-porous surface.
Materials:
- UV-C Device with known intensity at 254 nm
- UV-C Radiometer
- Model Virus Suspension (e.g., Murine Norovirus, Phi6)
| Research Reagent Solutions | Function |
|---|---|
| Geobacillus stearothermophilus Biological Indicators | Gold-standard for validating sterility assurance and sporicidal efficacy of VHP processes [63]. |
| Hydrogen Peroxide Solution (e.g., 35% w/v) | The consumable active agent for VHP systems, vaporized to create the microbiocidal vapor [63] [61]. |
| Chemical Indicators (VHP) | Provide an immediate, visual confirmation of VHP vapor exposure and distribution throughout the decontaminated space [63]. |
| UV-C Radiometer | Critical instrument for measuring the intensity (μW/cm²) of UV-C light at 254 nm, used to calculate the delivered dose [65]. |
| Low-Pressure Mercury Amalgam Lamps | A type of UVC lamp known for stable output and high efficiency at 254 nm, ideal for demanding applications [65]. |
| Far-UVC Excimer Lamps (222 nm) | Produce 222 nm wavelength, shown to inactivate pathogens while presenting a lower risk for human exposure, enabling use in occupied spaces [65] [67]. |
| Cell Culture Media & Reagents | Essential for propagating and titrating viral stocks used in UV-C and disinfectant efficacy testing. |
- Cell Culture Line for Virus Propagation and Plaque Assay
- Coupons (e.g., stainless steel, plastic)
Methodology:
- Surface Inoculation: Apply a small, controlled volume of the virus suspension onto coupons and allow it to dry.
- UV-C Exposure: Place the inoculated coupons at a fixed distance from the UV-C source. Expose coupons for varying time periods (e.g., 0, 30, 60, 120 seconds). Measure the UV-C intensity at the coupon surface with a radiometer for each time point. Dose (J/m²) = Intensity (W/m²) × Time (s) [65].
- Virus Recovery and Titration: After exposure, immediately recover the virus from the coupon using a neutralizer solution. Determine the viable virus titer for each coupon using a plaque assay or TCID₅₀ method.
- Data Analysis: Plot the log₁₀ of the surviving virus fraction against the UV-C dose. The dose required for a 3-log (99.9%) reduction can be calculated from the curve's slope (D-value) [65].
Strategy Selection and Experimental Workflow
The following diagram illustrates the logical decision-making process for selecting and validating a decontamination strategy.
Research Reagent Solutions
The table below lists key materials and reagents essential for developing and validating decontamination processes.
Table 2: Essential Research Reagents for Decontamination Studies
STR Profiling Troubleshooting Guide
Q1: What are common causes of incomplete or weak STR profiles, and how can they be resolved?
Incomplete or weak STR profiles often stem from issues during the DNA extraction or amplification steps. The following table outlines common problems and their solutions.
| Problem | Cause | Solution |
|---|---|---|
| PCR Inhibition [69] | Presence of hematin (from blood) or humic acid (from soil) inhibiting DNA polymerase. | Use extraction kits with additional washing steps designed to remove inhibitors [69]. |
| Ethanol Carryover [69] | Incomplete drying of DNA samples after purification. | Ensure DNA samples are completely dried post-extraction; do not shorten drying steps [69]. |
| Imbalanced STR Profiles [69] | Inaccurate pipetting during amplification setup. | Use calibrated pipettes and thoroughly vortex primer mixes before use [69]. |
| Allelic Dropout [69] | Too much or too little template DNA, or insufficient master mix concentration. | Use accurate DNA quantification to determine the optimal template amount for amplification [69]. |
Q2: How can issues during the separation and detection phase of STR analysis be fixed?
Problems in the final detection phase can affect profile clarity. Key issues relate to the reagents and dye sets used.
- Imbalanced Dye Channels or Artifacts: This is frequently caused by using incorrect or non-recommended dye sets for the specific STR chemistry. Always adhere to the manufacturer-recommended dye sets to ensure balanced fluorescence signals and minimize artifacts [69].
- Peak Broadening or Reduced Signal Intensity: This is often due to the use of degraded formamide. Formamide quality is critical for proper DNA separation. Use high-quality, deionized formamide and minimize its exposure to air to prevent degradation. Avoid re-freezing aliquots to maintain reagent integrity [69].
Q3: What is the best approach for interpreting low-template DNA (LT-DNA) STR profiles?
For low-template DNA samples, a single analysis can be unreliable due to stochastic effects like allele dropout. The preferred method is to perform replicate amplifications and apply a consensus approach [70]. This involves analyzing the sample multiple times and only considering alleles that appear consistently across replicates. This method provides a more objective and reliable interpretation, as it helps distinguish true alleles from artifacts, even though it may yield fewer peaks in the final profile [70].
Mycoplasma Testing Troubleshooting Guide
Q4: What are the consequences of mycoplasma contamination in cell cultures, and how can it be prevented?
Mycoplasma contamination is a serious and common issue, affecting 15-35% of continuous cell cultures [71]. It can significantly alter cell physiology, leading to:
- Chromosomal aberrations and changes in gene expression [71]
- Disruption of cell metabolism and inhibition of cell proliferation [72] [71]
- Changes in membrane antigenicity and reduced virus production [71]
Prevention is the best strategy and involves several key practices [71]:
- Aseptic Technique: Use proper personal protective equipment (PPE) and work in a certified laminar flow hood.
- Quarantine New Cell Lines: Isolate new cell lines until they are confirmed to be mycoplasma-free.
- Routine Testing: Implement a schedule for routine mycoplasma testing on all cell cultures.
- Avoid Antibiotic Reliance: Standard antibiotics like penicillin and streptomycin are largely ineffective against mycoplasma. Do not rely on them for prevention [71].
Q5: What methods are available for detecting mycoplasma contamination, and how do they compare?
The primary regulatory-accepted methods are culture-based and molecular tests. The table below summarizes common detection methods.
| Method | Principle | Time to Result | Key Advantage | Key Disadvantage |
|---|---|---|---|---|
| Direct Culture [72] [71] | Growth on agar plates to form "fried egg" colonies. | 28 days [72] | Considered a gold standard. | Very long turnaround; only detects cultivable species [72]. |
| Indirect Culture (DAPI/Hoechst) [72] [71] | Stains DNA in indicator cells; mycoplasmas appear as filamentous fluorescence. | ~10 days [72] | Detects some non-cultivable species. | Low signal intensity; requires expert interpretation [72]. |
| PCR/qPCR [73] | Detects mycoplasma DNA using specific primers and probes. | ~5 hours [73] | Fast, sensitive, and specific. | Detects DNA, not necessarily viable organisms. |
Q6: Our lab wants faster mycoplasma testing for lot-release of bioproducts. What are our options?
Rapid, sensitive PCR-based methods are now available and are a strong alternative to traditional culture. For example, the MycoSEQ Mycoplasma Detection Kit is a qPCR-based assay that provides results in approximately five hours and meets regulatory sensitivity requirements [73]. These kits include crucial controls:
- Discriminatory Positive Control (DPC): Confirms the detection assay is working and distinguishes accidental control contamination from a true positive [73].
- Internal Positive Control (IPC): Identifies the presence of inhibitors in the sample that could cause a false-negative result [73].
Research Reagent Solutions
Essential materials and reagents for implementing these quality control assays.
| Item | Function | Example |
|---|---|---|
| Glycan-Coated Magnetic Nanoparticles [74] | Isolate and concentrate microbial contaminants from large sample volumes (e.g., 1L water) for faster detection. | Technology for rapid water pathogen testing [74]. |
| DNA Polymerase I & Modified Nucleotides [72] | Enzymatically label nicks in mycoplasmal DNA for highly sensitive immunofluorescence detection, superior to DAPI staining. | Key component in a novel, sensitive mycoplasma detection assay [72]. |
| TaqMan qPCR Assays [73] | Provide highly specific and quantitative detection of mycoplasma DNA for fast, reliable lot-release testing. | MycoSEQ Plus Mycoplasma Detection Kit [73]. |
| High-Quality, Deionized Formamide [69] | Ensures proper denaturation and separation of DNA fragments during capillary electrophoresis in STR analysis. | Critical reagent for STR analysis [69]. |
| Adventitious Virus Detection Test [75] | Uses nanopore sequencing for broad-spectrum detection of viral contaminants in biopharmaceutical manufacturing. | ViruSure's GLP-validated test [75]. |
Experimental Workflow Diagrams
STR Analysis Workflow
Mycoplasma Detection Methods
Cost-Benefit Analysis of Risk Mitigation Investments
Frequently Asked Questions (FAQs)
Q1: What is the primary financial challenge when justifying advanced risk-mitigation investments, such as a new biosensor system? The core challenge is balancing the significant upfront and ongoing costs against benefits that can be difficult to quantify. Reducing equity exposure or investing in costly risk-mitigation strategies comes with an opportunity cost. An optimized portfolio of risk mitigation strategies, rather than a single approach, can improve financial outcomes by minimizing this opportunity cost while achieving the desired risk reduction [76].
Q2: How can I quantify intangible benefits like "reduced operational disruption" or "enhanced research integrity" in my analysis? While challenging, you should assign a monetary value to these intangibles. For reduced disruption, estimate the cost of delayed projects or lost researcher hours during a contamination-related shutdown. For enhanced research integrity, consider the value of preventing a study invalidation that could require costly repetition or harm grant funding prospects. Use estimation techniques or proxy measures, document all assumptions, and perform a sensitivity analysis to show how these values impact your results [77] [78].
Q3: My cost-benefit analysis (CBA) yields a negative Net Present Value (NPV) for a proposed containment equipment upgrade. Does this mean I should automatically reject the investment? Not necessarily. A negative NPV based on direct financials alone suggests the project may not be financially optimal. However, you must re-examine your analysis for critical unquantified factors. In a viral diagnostic context, this could include the catastrophic cost of a complete research shutdown, reputational damage affecting future funding, or the value of complying with anticipated stricter safety regulations. A sensitivity analysis can help evaluate how changes in key assumptions affect the outcome [77] [78].
Q4: What is a reasonable discount rate to use for a long-term investment in laboratory safety infrastructure? The discount rate should reflect the cost of capital and the risk profile of the investment. For stable, long-term infrastructure projects, organizations often use a rate between 5% and 10%. A higher rate is used for riskier projects. It is crucial to use a rate that aligns with your institution's financial policy and to perform a sensitivity analysis on this variable, as it significantly impacts the present value of future costs and benefits [78].
Q5: Our facility is considering a new HVAC system with MERV-13 filtration and UVGI. How do we calculate the "Equivalent Air Changes per Hour (eACH)" to meet CDC guidelines? The eACH combines ventilation from outdoor air, filtration, and air treatment into a single metric. CDC recommends aiming for 5 eACH in public indoor spaces to help reduce viral particles [79]. The calculation is based on the volume of filtered, treated, or outside air supplied per unit time, divided by the volume of the room. You will need to:
- Calculate the outdoor air change rate from your HVAC system.
- Add the equivalent clean air delivery rate from your portable air cleaners and upper-room UVGI systems. Consult an HVAC professional or use specialized tools to perform this calculation accurately for your specific space and equipment [79].
Troubleshooting Guides
Issue 1: Inconsistent Results in Pathogen Detection Experiments
Problem: Yielding variable results when detecting target viruses (e.g., SARS-CoV-2, Influenza) using qPCR following a new biosensor protocol.
Solution:
- Step 1: Verify Primer/Probe Integrity: Confirm that primers and probes for conserved genes (like the matrix (M) or nucleocapsid protein (NP) for initial identification) are specific, have not degraded, and are optimized for the viral clades in circulation. An optimized dual-target qPCR method can help maintain sensitivity across diverse virus clades [80].
- Step 2: Check Sample Integrity: Ensure environmental samples are collected, transported, and stored correctly to prevent RNA degradation. Use appropriate viral transport media and maintain cold chain.
- Step 3: Re-calibrate Equipment: Confirm that pipettes, qPCR machines, and biosensors are properly calibrated. Run a standard curve with known template concentrations to assess amplification efficiency.
- Step 4: Include Appropriate Controls: Always include a negative control (no template) and a positive control (known quantity of target RNA) to identify contamination or reaction failure.
Issue 2: High False-Negative Rate in Rapid Antigen Testing
Problem: A new lateral flow antigen-capture test is failing to detect low viral loads, leading to false negatives.
Solution:
- Step 1: Evaluate Limit of Detection (LoD): Compare the LoD of your test with the expected viral load in samples. Traditional colloidal gold-based tests may have low sensitivity [80].
- Step 2: Consider Advanced Materials: Investigate using label-free quantum dot (QD) probes, which can lower the detection limit significantly (e.g., to 0.09 ng/mL). A QD-linked fluorescence immunoassay (QD-LFIA) can provide objective, rapid results with higher sensitivity, suitable for field applications [80].
- Step 3: Optimize Sample Preparation: Concentrate the viral material from the sample if possible. Review the sample application and buffer composition to ensure optimal binding conditions.
Quantitative Data and Financial Analysis
Table 1: Categorization of Costs and Benefits for Risk Mitigation Investments
| Category | Type | Examples in Viral Diagnostic Research |
|---|---|---|
| Costs | Direct Costs | - Biosensor hardware (e.g., $500,000 for manufacturing equipment [78])- High-efficiency MERV-13 HVAC filters [79]- Reagents for qPCR (primers, probes, enzymes) [80] |
| Indirect Costs | - Laboratory space utilities (rent, electricity) [78]- Administrative overhead for project management [77] | |
| Intangible Costs | - Temporary reduction in lab productivity during system implementation [77] | |
| Opportunity Costs | - Benefits lost from other research projects not funded due to this investment [77] [78] | |
| Benefits | Direct Benefits | - Reduced costs from canceled/repeated experiments due to contamination- Increased revenue from faster, more reliable diagnostic throughput |
| Indirect Benefits | - Improved brand reputation leading to more grant funding [78]- Increased overall research productivity [81] | |
| Intangible Benefits | - Enhanced researcher safety and morale [78]- Averting future pandemics by creating a prevention mechanism [81] |
Table 2: Cost-Benefit Analysis Framework and Financial Formulas
| Analysis Step | Description | Application Example |
|---|---|---|
| Define Scope & Objectives | Outline project objectives, timeline, and success metrics. Example goal: "Reduce respiratory illnesses in the research facility by 25%." [81] [77] | A project aims to install a clean-air system ($500,000 cost) with a 5-year life to protect research integrity [81] [78]. |
| Assign Monetary Values | Quantify all costs and benefits. For intangibles, use proxies (e.g., value of a researcher's saved time). | Annual net benefit from preventing disruptions: $180,000. Annual maintenance cost: $20,000 [78]. |
| Calculate Present Value (PV) | Convert future cash flows to today's value using a discount rate. Formula: PV = FV / (1 + r)^n [78] |
With a 10% discount rate, the PV of $180,000 in Year 1 is $163,636 [78]. |
| Calculate Net Present Value (NPV) | Sum of PV of all benefits minus PV of all costs. Formula: NPV = Σ(PV of Benefits) - Σ(PV of Costs) [78] |
If total PV of benefits = $680,670 and total PV of costs = $575,000, then NPV = $105,670. A positive NPV suggests financial viability. |
| Calculate CBA Ratio | Ratio of PV of Benefits to PV of Costs. Formula: CBA Ratio = Σ(PV of Benefits) / Σ(PV of Costs) [78] |
A ratio greater than 1.0 indicates benefits outweigh costs. Example: $680,670 / $575,000 = 1.18 [78]. |
Experimental Protocols for Validation
Protocol 1: Validation of Biosensor Pathogen Detection Sensitivity
Objective: To determine the Limit of Detection (LoD) and specificity of a biosensor for target respiratory viruses (e.g., SARS-CoV-2, Influenza) in an aerosolized environment [81] [80].
Materials:
- Biosensor system prototype with computational modeling software [81]
- Aerosolization chamber
- Viral transport media
- Serial dilutions of inactivated target viruses (SARS-CoV-2, Influenza) and non-target viruses (e.g., RSV) as negative controls
- RNA extraction kit
- qPCR system and validated primer-probe sets for target viruses [80]
Methodology:
- Sample Aerosolization: In a controlled BSL-2 lab, aerosolize serial dilutions of inactivated virus solutions into the chamber to simulate a range of environmental loads.
- Biosensor Operation: Activate the biosensor system to sample air from the chamber and run its detection protocol in real-time [81].
- Reference Sampling: Concurrently, collect air samples using a reference method (e.g., impingement into viral transport media) for parallel qPCR analysis [80].
- qPCR Analysis: Extract RNA from reference samples and run qPCR using protocols recommended by the WHO/WOAH [80].
- Data Analysis: Compare biosensor output (positive/negative, signal strength) with qPCR results (genome copies per cubic meter of air). The LoD is the lowest virus concentration at which the biosensor achieves ≥95% detection rate.
Protocol 2: Evaluating Intervention Efficacy for Contamination Risk Reduction
Objective: To assess the effectiveness of engineering interventions (increased ventilation, filtration, UVGI) in reducing aerosolized pathogen concentration [81] [79].
Materials:
- Test room (e.g., a mock laboratory or day care center setting [81])
- HVAC system capable of modulating airflow and filtration (up to MERV-13) [79]
- Upper-room Ultraviolet Germicidal Irradiation (UVGI) system [79]
- Aerosol generator
- Particle counter or qPCR air sampler
- Inactivated virus or safe viral surrogate (e.g., MS2 bacteriophage)
Methodology:
- Baseline Measurement: Aerosolize the viral surrogate into the test room with standard ventilation. Measure the airborne concentration over time using the particle counter/qPCR sampler.
- Intervention Testing: Repeat the aerosolization under different intervention conditions:
- Data Analysis: For each condition, calculate the decay rate of the aerosolized surrogate and the equivalent air changes per hour (eACH). Compare the results to the baseline and to the target of 5 eACH recommended by the CDC [79].
Visualized Workflows and Pathways
Cost-Benefit Analysis Workflow
Integrated Biosensor Risk Mitigation System
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Viral Diagnostic & Contamination Control Research
| Item | Function & Application |
|---|---|
| qPCR Primers/Probes | Target conserved viral genes (e.g., M, NP) for initial pathogen detection and subtype-specific genes (HA) for further characterization. Essential for validating biosensor sensitivity and conducting environmental sampling [80]. |
| Quantum Dot (QD) Conjugates | Used to develop high-sensitivity lateral flow immunoassays (QD-LFIA). They lower the detection limit for viral antigens compared to traditional colloidal gold, reducing false negatives in point-of-care tests [80]. |
| MERV-13 Air Filters | High-efficiency particulate air filters installed in HVAC systems. They are a core engineering control to remove aerosolized virus particles from recirculated air, directly reducing indoor contamination risk [79]. |
| Ultraviolet Germicidal Irradiation (UVGI) | A well-established air treatment technology. Upper-room UVGI inactivates microorganisms, including respiratory viruses, by damaging their genetic code. Used as a supplemental intervention to reduce disease transmission [79]. |
| Viral Transport Media | A solution used to store and transport clinical specimens containing viruses. It preserves viral viability and nucleic acid integrity for subsequent analysis by virus isolation, qPCR, or sequencing [80]. |
| Next-Generation Sequencing (NGS) | A technology used for comprehensive viral genomic characterization after a positive detection. It identifies mutations, tracks viral evolution, and guides evidence-based mitigation strategies [80]. |
Validating Methods and Comparing Emerging Technologies
FAQs: ICH Q5A(R2) Viral Safety Evaluation
1. What is the scope of the updated ICH Q5A(R2) guideline? ICH Q5A(R2) provides risk-based principles and mitigation strategies to assure the viral safety of biotechnology products derived from characterized cell lines of human or animal origin [82] [83]. The January 2024 update incorporates advances in scientific knowledge and regulatory expectations, expanding its scope to include new product types like viral-vector-derived products and addressing modern manufacturing approaches such as continuous manufacturing [84] [85].
2. What new product types are covered in the revised guideline? The revision explicitly considers products that have emerged since the original guideline, including genetically engineered viral vectors (e.g., adeno-associated virus - AAV), virus-like particles (VLPs), protein subunits made using baculovirus, herpes-simplex virus, or adenovirus production systems, and nanoparticle-based vaccines [84]. A new Annex 7 is dedicated to these products [84].
3. How does the guideline address viral safety for continuous manufacturing? For continuous manufacturing (CM), the guideline acknowledges that viral safety controls must account for system dynamics, monitoring frequency, and start-up/shutdown phases [84]. It discusses using prior knowledge from batch processes for modular validation, treating some continuous processes as a series of "minibatch" pulses, and establishing scaled-down batch models for viral-clearance studies of unit operations like chromatography and viral filtration [84].
4. What advanced virus detection methods are recommended? The guideline encourages using New Generation Sequencing (NGS) and other nucleic-acid amplification techniques (NATs) like PCR [84]. NGS is recommended as a replacement for certain in vivo tests (e.g., HAP, MAP, RAP tests) due to its broad virus-detection capabilities and alignment with the 3R principle to reduce animal use [84]. These methods require proper validation for their intended use [84].
5. What is a risk-based approach for viral vector products? For viral vector products, a risk-based approach addresses contamination risks from raw materials, testing for adventitious viruses, helper viruses, and replication-competent viruses at appropriate manufacturing steps, and demonstrating clearance of these viruses during downstream processing [84]. The approach must consider the specific viral vector and production system used [84].
Troubleshooting Common Viral Safety Issues
| Problem Area | Common Challenge | Proposed Solution | Regulatory Reference / Justification |
|---|---|---|---|
| Viral Clearance Studies for New Modalities | Viral vectors are themselves the product, making standard viral clearance/inactivation steps challenging. | Implement a risk-based control strategy. Use model viruses representing most likely adventitious/endogenous/helper viruses. Justify virus choice and consider virus-specific filters and detergents [84]. | ICH Q5A(R2) Annex 7 for viral-vector-derived products [84]. |
| Testing with New Analytical Methods | Method validation for NGS for broad virus detection. | Provide a complete validation package. Use available reference-virus reagents. Control critical steps: sampling, nucleic acid extraction, library prep, sequencing platform selection, and bioinformatics analysis [84]. | ICH Q5A(R2) encourages NGS to replace in vivo tests with broad detection capabilities [84]. |
| Adapter: Continuous Manufacturing | Designing a viral clearance study for a connected, continuous downstream process. | Use prior knowledge and scaled-down batch models for unit operations (e.g., chromatography, low-pH inactivation). Justify that relevant dynamic parameters (pH, pressure, concentration) are controlled within validated ranges [84]. | ICH Q5A(R2) acknowledges feasibility of using batch-process PrK for CM unit operations [84]. |
| Cell Substrate Characterization | Limited characterization knowledge for novel cell substrates (e.g., insect cell lines). | Perform extensive testing for adventitious and endogenous viruses on Master Cell Banks (MCBs), Working Cell Banks (WCBs), and cells at the limit of in vitro cell age (LIVCA). For insect cells, include testing for specific intracellular contaminants like insect rhabdovirus [84]. | ICH Q5A(R2) outlines data for marketing application, including cell line qualification [82] [84]. |
Experimental Protocol: Viral Clearance Validation for a Downstream Unit Operation
This protocol outlines a laboratory-scale viral clearance study for a chromatography step, demonstrating the capacity of the manufacturing process to remove and/or inactivate potential viral contaminations [84].
1. Principle A scaled-down model of the manufacturing chromatography column is challenged with a preparation of a relevant model virus. The infectious virus titer is measured in the load material and the collected product fraction to calculate the log reduction factor (LRF).
2. Materials and Equipment
- Relevant model virus (e.g., MuLV for retroviruses, Parvovirus for small, non-enveloped viruses)
- Scaled-down chromatography column (validated to represent the manufacturing process)
- Cell-based infectivity assay (or NAT method, if qualified) for virus titration
- Appropriate cell line for the infectivity assay
- Buffer solutions matching the manufacturing process
3. Procedure
- Step 1: Model Virus Preparation. Prepare a high-titer stock of the chosen model virus.
- Step 2: Spiking. Spike a known volume of the virus preparation into the process intermediate (product load) for the column. Mix thoroughly to ensure homogeneity. Take a sample from the spiked load for virus titration (
Load Titer). - Step 3: Down-Scale Chromatography. Process the spiked load material over the scaled-down chromatography column using validated operational parameters (flow rate, buffer composition, pH, conductivity, temperature, etc.) that mimic the manufacturing scale.
- Step 4: Collection. Collect the product fraction (eluate) from the column run.
- Step 5: Post-Run Titration. Titrate the collected product fraction for infectious virus (
Product Titer). Assay the load and product samples in parallel for an accurate LRF calculation.
4. Calculation and Interpretation
Calculate the Log Reduction Factor (LRF) using the formula:
LRF = Log10 (V1 × T1) - Log10 (V2 × T2)
Where:
V1= Volume of the spiked load materialT1= Infectious virus titer in the spiked load materialV2= Volume of the product fraction (eluate)T2= Infectious virus titer in the product fraction
A high LRF indicates robust viral clearance capacity for that unit operation. The overall process LRF is the sum of LRFs from individual dedicated viral clearance steps.
Essential Research Reagent Solutions
| Item | Function in Viral Safety Evaluation |
|---|---|
| Characterized Cell Banks (MCB/WCB) | Provide a consistent and qualified source of production cells. Testing these banks for viral contaminants is the first critical step in the viral safety strategy [84]. |
| Model Viruses | Used in viral clearance studies to validate the removal/inactivation capacity of the manufacturing process. They should represent potential contaminating viruses (adventitious, endogenous, or helper viruses) relevant to the cell line and product [84]. |
| Reference-Virus Reagents | Crucial for qualifying and validating new molecular analytical methods like NGS. They provide a standard with distinct physical, chemical, and genomic characteristics for assay performance assessment [84]. |
| Nucleic Acid Amplification Test (NAT) Kits | (e.g., PCR-based tests). Used for specific virus detection or to measure model virus levels in clearance studies. They can supplement or replace cell-based assays, especially when interference is an issue [84]. |
| Indicator Cell Lines | Used in co-culture assays (e.g., for detecting endogenous retroviruses) or for amplifying and detecting a wide range of adventitious viruses present in a test sample. |
Process Flow for Viral Safety Assurance
Testing Strategy for Viral Vector Products
Validation of Viral Clearance Studies in Downstream Processing
Frequently Asked Questions (FAQs)
Q1: What is the primary goal of a viral clearance validation study? The primary goal is to demonstrate, through robust data, that the downstream purification process for a biologic drug can effectively remove or inactivate potential viral contaminants to safe levels, thereby ensuring product safety for patients. These studies are a regulatory mandate for filings such as Investigational New Drug (IND) applications and Biological License Applications (BLA) [86].
Q2: How do the updated ICH Q5A(R2) guidelines impact study design? The revised ICH Q5A(R2) guideline, finalized in 2024, introduces more flexible validation requirements [87]. Key impacts include:
- Reduced Log Reduction Target: The target level for virus removal has been lowered from 6 logs to 4 logs for certain steps, which can reduce the number of required process steps [87].
- Acceptance of Prior Knowledge: The guidelines encourage the use of prior knowledge and platform data to support submissions, potentially reducing the scope of product-specific testing [87] [88].
- New Modalities: The scope now explicitly includes cell and gene therapy products, acknowledging that viral clearance for these can be very limited [87].
Q3: What are the most common technical challenges encountered during viral clearance studies? Researchers often face several technical hurdles:
- Poor Model Performance: A scale-down model that does not accurately mimic the manufacturing-scale process can invalidate results [89].
- Matrix Effects & Product Interference: Complex product solutions with proteins and excipients can shield viruses or interfere with assays, leading to inaccurate clearance measurements [86].
- Filter Clogging: The use of low-purity, high-titer virus stocks can cause abnormal phenomena like filter clogging and flux decay during filtration steps, making the study unrepresentative [89].
- Protein Aggregation: Aggregation, especially with high-concentration products or after thawing frozen materials, can impact both product quality and accurate viral clearance determination [87].
Q4: For a CHO-cell derived product, what model virus is used to demonstrate retrovirus clearance? The Xenotropic Murine Leukemia Virus (XMuLV) is a standard model retrovirus used. With the updated ICH Q5A(R2), Retrovirus-Like Particles (RVLPs) derived directly from CHO cells can also be used to validate the clearance of this endogenous particle of concern [86] [88].
Q5: What is a major consideration when validating viral clearance for a continuous manufacturing process? A significant challenge is the lack of a universally established platform and clearly defined study strategies. Key uncertainties include the definition of a "batch," and the appropriate duration and frequency of virus spiking for these prolonged processes [87].
Troubleshooting Guides
Low Log Reduction Value (LRV) in Virus Filtration
- Problem: Observed LRV is lower than expected for a virus retention filter step.
- Investigation & Resolution:
Potential Cause Investigation Action Corrective & Preventive Actions Filter Fouling or Clogging Analyze feed stream for high levels of aggregates or impurities. Check pressure profiles during the run. Pre-filter the load material. Optimize feed stream conditions (pH, conductivity). Use ultra-pure virus stocks to keep spiking percentage low (<1%) [89]. Inappropriate Filter Selection Review vendor data on filter compatibility with your molecule type (e.g., mAb vs. bispecific antibody). Screen different filter membranes (e.g., second-generation parvovirus filters) optimized for challenging molecules [89]. Pressure Fluctuations Review process data for pressure pauses or deviations from the validated pressure profile. Implement stricter process controls. Consider filters known to be robust against pressure interruptions [87].
Inconsistent Viral Inactivation Kinetics
- Problem: Low-pH or Solvent/Detergent (S/D) inactivation fails to achieve consistent, rapid viral kill.
- Investigation & Resolution:
Potential Cause Investigation Action Corrective & Preventive Actions Incorrect pH or Hold Time Calibrate pH probes and verify the actual hold time in the tank. Re-validate the hold time from the point of pH adjustment. Ensure proper mixing after acid addition. Product/Matrix Interference Test the impact of product concentration and solution composition (e.g., buffers, proteins) on inactivation efficacy. Define and control critical process parameters (CPPs) like protein concentration. Consider evaluating newer, milder detergents that are less harsh on sensitive molecules [89]. Outdated S/D Reagents Verify the concentration and shelf-life of detergent stocks (e.g., Triton X-100, which is being phased out in Europe) [90]. Qualify alternative detergents. Establish robust reagent qualification procedures [90].
Inadequate Viral Clearance in Continuous Processing
- Problem: Designing a viral clearance study for a continuous downstream process.
- Investigation & Resolution:
Potential Cause Investigation Action Corrective & Preventive Actions Undefined Study Parameters Map the entire continuous process to identify all unit operations and potential integration points. Engage regulators early. Define the "batch" for reporting. Plan for prolonged virus spiking to cover the dynamic state of the process [87]. Lack of Scale-Down Model Develop a representative model for the continuous unit operation (e.g., multi-column chromatography). Design the scale-down model to mimic residence times, flow rates, and cycling frequencies of the full-scale process. Use prior knowledge and platform data where possible [87].
Experimental Protocols
Protocol for a Virus Spiking Study on a Chromatography Step
This protocol outlines the methodology for validating viral clearance for a chromatography step in a downstream process [86] [89].
1. Principle: A scale-down model of the chromatography column is challenged with a high-titer virus spike. The amount of infectious virus in the load material and the product fraction is quantified, and the log reduction value (LRV) is calculated.
2. Key Materials and Reagents:
- Model Viruses: Select based on risk assessment. Common choices include:
- Scale-Down Model: A chromatographic column that accurately represents the manufacturing-scale process in bed height, resin lot, flow rate, buffer composition, and temperature.
- In-Process Material: The product stream from the previous manufacturing step, stored under validated conditions.
- Cell Culture & Media: For the infectivity assay (e.g., TCID50).
3. Procedure:
- Model Qualification: Demonstrate that the scale-down model mirrors the manufacturing process in terms of key performance indicators (e.g., chromatogram profile, step yield, product quality).
- Virus Spiking: Thaw the virus stock and mix it gently with the in-process material. Keep the spike ratio low (typically ≤1% v/v) to avoid altering the product stream's properties [89].
- Run the Column: Load the spiked material onto the equilibrated scale-down column. Execute the entire chromatography cycle (load, wash, elution) as per the manufacturing process.
- Sample Collection: Collect samples from the following:
- The spiked load material (pre-column)
- The product pool (e.g., elution fraction)
- Potentially from wash and strip fractions
- Virus Quantification: Determine the infectious virus titer in the pre-column and post-column product samples using a validated assay, most commonly the 50% Tissue Culture Infective Dose (TCID50) assay.
- Calculation:
- Calculate the total infectious virus load in the pre-column sample (Vpre).
- Calculate the total infectious virus load in the post-column product sample (Vpost).
- LRV = Log10 (Vpre) - Log10 (Vpost)
Protocol for a Low-pH Viral Inactivation Study
1. Principle: The product stream is adjusted to a specific low-pH condition (e.g., pH 3.5-3.9) and held for a defined time. Samples are taken at various time points to determine the kinetics of viral inactivation [86].
2. Key Materials and Reagents:
- Model Virus: Typically an enveloped virus like XMuLV or Pseudorabies Virus (PRV).
- In-Process Material: The product pool from the preceding chromatography step.
- Acidification Solution: (e.g., Citric or Acetic Acid).
- Neutralization Solution: (e.g., Tris base).
3. Procedure:
- Setup: Perform the study in a temperature-controlled environment. Pre-chill the in-process material if required.
- Time Zero Sample: Take a sample of the in-process material before acidification.
- Acidification: Rapidly add the acidification solution to the material with constant mixing to achieve the target pH.
- Hold & Sampling: Start the timer. Take samples at predetermined time points (e.g., 0, 5, 15, 30, 60 minutes). Immediately neutralize each sample upon collection.
- Virus Quantification: Determine the infectious virus titer for each time-point sample and the time-zero sample using the TCID50 assay.
- Analysis: Plot the remaining virus titer (log10) over time. The study is considered successful if the validation target (e.g., a ≥4 LRV) is achieved and sustained by the end of the hold time.
Visualized Workflows and Pathways
Viral Clearance Study Workflow
Decision Pathway for Study Design
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and materials used in viral clearance studies [86] [89] [88].
| Reagent/Material | Function & Rationale in Viral Clearance Studies |
|---|---|
| Model Virus Stocks (e.g., XMuLV, MVM) | Serve as surrogates for potential contaminants. They represent different virus families, sizes, and physical structures (enveloped vs. non-enveloped) to challenge the clearance mechanism [86]. |
| Ultra-Pure Virus Stocks | High-purity, high-titer virus preparations that enable a low spiking ratio (≤1%). This minimizes alterations to the product stream, prevents filter clogging, and leads to more accurate and reliable LRVs [89]. |
| BSL-1 Compatible Surrogates (e.g., MockV Kits) | Non-infectious virus-like particles (e.g., for MVM or RVLP) that allow for viral clearance prediction in a BSL-1 lab. They de-risk process development by enabling early, in-house assessment of clearance efficacy [88]. |
| Retrovirus-Like Particles (RVLPs) | Non-infectious particles derived directly from CHO cells. With ICH Q5A(R2), they can be used to validate the clearance of this endogenous retroviral particle of concern, providing a more relevant assessment than model viruses alone [88]. |
| Scale-Down Chromatography Columns | Miniaturized versions of manufacturing-scale columns that are qualified to accurately mimic the performance of the full-scale step, allowing for representative and cost-effective validation studies [86] [89]. |
| Validated Detergents (e.g., Triton X-100 replacements) | Chemicals used in solvent/detergent (S/D) viral inactivation. Newer, milder, and more environmentally friendly detergents are being qualified as legacy materials like Triton X-100 are phased out [90] [89]. |
Viral diagnostics are a critical component of modern public health and clinical medicine, with the ongoing emergence of viral pathogens underscoring the need for rapid, accurate detection methods. The selection of an appropriate diagnostic platform involves careful consideration of factors including sensitivity, specificity, throughput, cost, and technical requirements. This technical support center provides a comparative analysis of three cornerstone technologies—Polymerase Chain Reaction (PCR), Next-Generation Sequencing (NGS), and Mass Spectrometry (MS)—with a specific focus on troubleshooting common experimental challenges and reducing contamination risks within viral diagnostic workflows.
Technology Comparison: Core Principles and Applications
The following table summarizes the key characteristics, advantages, and limitations of PCR, NGS, and Mass Spectrometry for virus detection.
Table 1: Comparative analysis of PCR, NGS, and mass spectrometry for virus detection
| Feature | PCR (and qPCR) | Next-Generation Sequencing (NGS) | Mass Spectrometry (MS) |
|---|---|---|---|
| Detection Target | Specific nucleic acid sequences [91] [92] | Broad-spectrum nucleic acids (untargeted) or targeted sequences [93] [94] | Viral proteins and peptides [95] |
| Primary Application | Targeted detection of known pathogens [93] [92] | Pathogen discovery, outbreak surveillance, whole-genome sequencing [93] [94] | Untargeted and targeted pathogen identification [95] |
| Sensitivity | High (can detect low copy numbers) [91] [92] | Variable; can be lower than PCR, improved with enrichment [93] | Moderate (comparable to CT ≤27 for SARS-CoV-2) [95] |
| Specificity | High (primer/probe dependent) [92] | High (sequence-based identification) [93] | High (peptide-based identification) [95] |
| Throughput | High (especially for qPCR) [92] | Moderate to High (batch processing) [93] [94] | Very High (up to 60 samples/day) [95] |
| Multiplexing Capability | Limited (multiplex PCR exists but is constrained) [95] | High (can detect thousands of pathogens simultaneously) [93] | High (can identify multiple viruses from one sample) [95] |
| Key Advantage | Speed, cost-effectiveness, high sensitivity for known targets [91] [96] | Untargeted discovery, comprehensive genomic data [93] [94] | Rapid, untargeted protein-based identification, high throughput [95] |
| Key Limitation | Limited to known targets; prone to contamination [91] [97] | High cost, complex data analysis, infrastructure demands [93] [94] | Lower sensitivity than PCR, limited to proteome database coverage [95] |
Troubleshooting Guides and FAQs
PCR Troubleshooting Guide
PCR is a foundational technique, but its sensitivity makes it vulnerable to contamination and amplification issues. The following FAQs address common problems.
FAQ: What should I do if I obtain no amplification products?
- Check your controls: Always include a positive control to verify all reaction components are functional [97].
- Optimize cycling parameters: Increase the number of PCR cycles (e.g., by 3-5 cycles, up to 40) for low-abundance targets. If that fails, lower the annealing temperature in 2°C increments or increase the extension time [97].
- Investigate template quality: The template may contain PCR inhibitors (e.g., phenol, heparin, salts) or have high GC content. Dilute the template, re-purify it, or use a polymerase resistant to inhibitors [97] [35].
- Verify primers: Check primer design for specificity and optimal melting temperature (Tm). Consider using nested PCR for difficult targets [97] [35].
FAQ: How can I resolve nonspecific amplification or smeared bands on a gel?
- Increase specificity: Raise the annealing temperature, use a hot-start polymerase, or employ touchdown PCR [97] [35].
- Adjust reaction components: Reduce the amount of template DNA or primer concentration to minimize primer-dimer formation and mis-priming [97] [35].
- Shorten annealing time: For some polymerases, using a short annealing time (5-15 seconds) is essential for specific amplification [97].
FAQ: What are the best practices to prevent and eliminate PCR contamination?
Contamination is a major risk for false-positive results. Adherence to strict laboratory practices is the most effective countermeasure.
- Physically separate workspaces: Establish distinct, dedicated "pre-PCR" and "post-PCR" areas. Equipment (pipettes, centrifuges, lab coats) and consumables must never move from the post-PCR to the pre-PCR area [97].
- Use dedicated supplies: Use pipette tips with aerosol filters exclusively for setting up PCR reactions [97].
- Include negative controls: Always run a negative control (no-template control) to monitor for contamination [97].
- Decontaminate: Clean workstations and equipment with 10% bleach. Expose pipettes to UV light in a laminar flow hood to cross-link contaminating DNA [97].
NGS Troubleshooting Guide
Next-Generation Sequencing, particularly viral metagenomics (vmNGS), offers powerful, untargeted detection but involves complex workflows prone to specific failure points.
FAQ: Why is my NGS library yield low, and how can I fix it?
Low yield is a common issue in library preparation. The following table outlines primary causes and corrective actions.
Table 2: Troubleshooting low yield in NGS library preparation
| Root Cause | Mechanism of Failure | Corrective Action |
|---|---|---|
| Poor Input Quality | Degraded DNA/RNA or contaminants (phenol, salts) inhibit enzymes [98]. | Re-purify input sample; check purity via 260/280 and 260/230 ratios; use fluorometric quantification (e.g., Qubit) over UV absorbance [98]. |
| Fragmentation Issues | Over- or under-shearing produces fragments outside the optimal size range for adapter ligation [98]. | Optimize fragmentation parameters (time, energy); analyze fragment size distribution post-shearing [98]. |
| Inefficient Ligation | Suboptimal adapter-to-insert ratio or poor ligase performance reduces library complexity [98]. | Titrate adapter concentration; ensure fresh ligase and buffer; optimize ligation temperature and time [98]. |
| Overly Aggressive Cleanup | Desired fragments are excluded during bead-based size selection [98]. | Precisely follow bead-to-sample volume ratios; avoid over-drying beads during cleanup [98]. |
FAQ: My sequencing data shows high adapter dimer content or other artifacts. What went wrong?
- Review ligation efficiency: A sharp peak at ~70-90 bp on an electropherogram indicates adapter dimers, often due to an excess of adapters or inefficient ligation. Titrate the adapter-to-insert molar ratio [98].
- Avoid over-amplification: Using too many PCR cycles during library amplification can lead to increased duplicates and amplification artifacts. It is better to re-amplify from leftover ligation product than to over-cycle a weak product [98].
- Optimize purification: Ensure proper size selection to remove short fragments and adapter dimers before sequencing [98].
Mass Spectrometry Troubleshooting
Viral proteomics, such as the vPro-MS workflow, is an emerging untargeted method for virus identification.
FAQ: What are the critical steps for successful untargeted virus detection using mass spectrometry?
- Comprehensive peptide library: The vPro-MS workflow relies on a curated in-silico peptide library covering the entire human virome to enable confident identification [95].
- Efficient sample preparation: Use a lysis buffer that effectively inactivates viruses. The S-Trap protocol for digestion is recommended for robustness [95].
- Advanced data acquisition: Employ Data-Independent Acquisition (DIA) methods like diaPASEF on timsTOF instruments for deep, untargeted peptide sampling and high throughput [95].
- Rigorous data analysis: Use a dedicated scoring algorithm (e.g., vProID score) to assess the confidence of virus identification from the proteomics data [95].
Essential Research Reagent Solutions
The following table details key reagents and their functions critical for successful viral detection experiments across the three platforms.
Table 3: Key research reagents and materials for viral detection methodologies
| Reagent / Material | Function | Application |
|---|---|---|
| Hot-Start DNA Polymerase | Reduces non-specific amplification by inhibiting polymerase activity until high temperatures are reached [97] [35]. | PCR |
| PCR Additives (e.g., GC Enhancer, DMSO) | Aids in denaturing GC-rich templates and resolving secondary structures to improve amplification efficiency [97] [35]. | PCR |
| Universal Primers (e.g., 16S rRNA, ITS) | Amplifies conserved genomic regions for broad identification of bacteria or fungi prior to sequencing [93]. | Targeted NGS (tNGS) |
| Nucleic Acid Enrichment Kits | Increases the proportion of viral nucleic acids relative to host background, improving sequencing sensitivity [93] [94]. | Metagenomic NGS (mNGS) |
| vPro Peptide Spectral Library | A curated library of tryptic peptides from all human-pathogenic viruses; enables untargeted identification from MS data [95]. | Mass Spectrometry |
| Structural Viral Proteins | The most abundant viral proteins (core, envelope); the primary targets for optimal detection sensitivity in proteomics [95]. | Mass Spectrometry |
Experimental Workflow Visualization
The diagrams below illustrate the generalized workflows for the primary viral detection methods discussed, highlighting key steps for contamination control and optimal performance.
PCR Workflow and Contamination Control
NGS Library Preparation Workflow
vPro-MS Proteomics Workflow
Evaluating Point-of-Care and Rapid Diagnostic Technologies
Troubleshooting Guides & FAQs for Viral Diagnostic Contamination Risk Reduction
This technical support resource addresses common experimental challenges in point-of-care (POC) and rapid diagnostic development, with a specific focus on mitigating contamination risks that can compromise assay accuracy in viral detection.
Troubleshooting Guide: Common Experimental Issues
Table 1: Troubleshooting Common Point-of-Care Diagnostic Experimental Issues
| Problem | Potential Causes | Recommended Solutions | Supporting Context |
|---|---|---|---|
| Low detection rates for respiratory viruses | Low viral load in sample; suboptimal specimen collection; assay lacks sensitivity [99]. | Use tests with high analytical sensitivity; ensure proper specimen collection training; employ multiplex panels for co-infections [99] [100]. | During peak flu seasons, positivity rates can be as low as 20-30% in symptomatic adults, highlighting need for highly sensitive tests [99]. |
| Low sensitivity/specificity in field settings | Variable biological samples (e.g., whole blood); matrix interference; pre-analytical errors [101] [102] [57]. | Implement robust internal controls; use sample purification steps; integrate ML algorithms for improved signal interpretation [57] [100]. | Hemolysis in whole blood samples accounts for up to 70% of pre-analytical errors, critically impacting potassium and other analyte results [102]. |
| Contamination leading to false positives | Amplified nucleic acid carryover; contaminated reagents or surfaces; inadequate workflow separation [57]. | Implement closed-system, microfluidic cartridges; use uracil-DNA glycosylase (UDG) protocols; physically separate pre- and post-amplification areas [57]. | Nucleic Acid Amplification Tests (NAATs) are highly susceptible to contamination, requiring specialized containment strategies to avoid false positives [57]. |
| Inconsistent results between operators | Subjective visual interpretation of results (e.g., faint test lines); complex, multi-step protocols; insufficient training [99] [100]. | Use automated readers with built-in algorithms; develop simplified, user-friendly protocols; implement comprehensive and recurrent training [99] [100]. | Machine learning models, particularly convolutional neural networks (CNNs), can standardize result interpretation and reduce user-dependent variability [100]. |
Frequently Asked Questions (FAQs)
Q1: What is the single most critical step to reduce pre-analytical errors in whole blood point-of-care testing?
A1: Preventing hemolysis is paramount. Hemolysis is the leading cause of pre-analytical errors, accounting for up to 70% of such issues in POC testing with whole blood, and significantly skews potassium results [102]. Mitigation strategies include:
- Training: Comprehensive training for staff on proper sample collection and handling techniques.
- Technology: Adoption of POC devices with integrated hemolysis detection capabilities to flag compromised samples before analysis [102].
Q2: How can we improve the accuracy of rapid tests when used by untrained individuals in decentralized settings?
A2: Integrate Machine Learning (ML) for result interpretation. The main challenge is the subjective reading of results, like faint lines on lateral flow assays [100].
- Solution: Use smartphone-based applications or portable readers with integrated ML algorithms. These tools use supervised learning models to analyze test lines objectively, reducing false positives and negatives caused by human error [100]. This digital tool is a core innovation for reducing user-dependent contamination of results.
Q3: Our molecular POC tests are highly accurate but suffer from amplicon contamination. What containment strategies are most effective?
A3: Adopt closed-system designs and enzymatic controls. Contamination from amplified nucleic acids (amplicons) is a major risk for NAATs [57].
- Closed Systems: Utilize microfluidic cartridges that encapsulate the entire amplification and detection process, preventing amplicon release into the environment [57].
- UDG Protocol: Incorporate uracil-DNA glycosylase (UDG) into the reaction mix. This enzyme selectively degrades uracil-containing prior amplicons before the new amplification reaction begins, preventing carryover contamination without affecting the new thymine-containing template [57].
Q4: What are the key regulatory considerations when validating a new rapid diagnostic to ensure reliability?
A4: Follow standardized validation frameworks focusing on accuracy and reproducibility. Key guidance documents, such as the ICMR's 2025 Guidance, outline critical requirements [103]:
- Performance Metrics: Rigorously evaluate analytical and clinical performance, including sensitivity, specificity, and limit of detection (LoD).
- Reproducibility: Assess the test's precision across different operators, lots, and instruments.
- Regulatory Compliance: Ensure the test conforms to relevant standards (e.g., ISO 20916:2019, ISO 15189:2022) and regional medical device rules for in-vitro diagnostics (IVD) [103].
Experimental Protocols for Contamination Risk Evaluation
Protocol 1: Benchtop Evaluation for Pre-analytical Error and Contamination
This protocol is designed to stress-test a diagnostic device under realistic, error-prone conditions.
1. Objective: To determine the robustness of a POC diagnostic device against common pre-analytical errors and user mishandling. 2. Materials:
- POC device and test kits
- Clinical samples (e.g., whole blood, buccal swabs) or simulated specimens
- Equipment for sample "spiking" (e.g., pipettes) 3. Methodology:
- Inclusivity/Exclusivity Testing: Spike samples with known quantities of target and non-target organisms to verify the test accurately identifies the correct target [104].
- Error Simulation: Deliberately introduce common errors during testing:
- Hemolysis: Test with deliberately hemolyzed whole blood samples [102].
- User Error: Simulate incorrect swab insertion, power interruptions, or failure to add all required reagents [104].
- Environmental Stress: Expose test components to non-ideal temperatures or physical impact to assess durability [99].
- Data Analysis: Compare results from error-simulated tests with controls performed under ideal conditions. Calculate the rate of false positives/negatives and signal deviation.
Protocol 2: Validating a Closed-System NAAT against Amplicon Contamination
This protocol assesses the effectiveness of a contained system at preventing false positives from amplicon contamination.
1. Objective: To validate that a closed-system, cartridge-based NAAT platform prevents environmental contamination from amplicons. 2. Materials:
- Closed-system NAAT platform and cartridges
- High-concentration amplicon solution
- Surface swabs for environmental sampling 3. Methodology:
- Contamination Challenge: In a controlled environment, open cartridges containing negative samples on a benchtop previously exposed to a high-concentration amplicon aerosol.
- Environmental Monitoring: Use surface swabs to collect samples from the work area and the exterior of the test cartridges after the simulation. Test these swabs for the presence of amplicons.
- Result Analysis: Run the challenged negative samples on the platform. A robust system will show zero false positives in the negative samples, demonstrating its resistance to external contamination.
Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Contamination Control
| Reagent/Material | Function in Research & Development | Application in Contamination Risk Reduction |
|---|---|---|
| Uracil-DNA Glycosylase (UDG) | Enzyme used in NAAT master mixes [57]. | Selectively degrades carryover amplicons from previous reactions, preventing false positives [57]. |
| Closed-System Microfluidic Cartridges | Single-use devices that integrate sample preparation, amplification, and detection [57]. | Physically contain the entire reaction, isolating amplicons from the laboratory environment and user [57]. |
| Hemolysis Detection Reagents | Indicators or integrated sensors in POC devices [102]. | Flags pre-analytically compromised whole blood samples before analysis, preventing erroneous results [102]. |
| Machine Learning Algorithms (e.g., CNNs) | Computational tools for image and data analysis [100]. | Automate and standardize the interpretation of test results (e.g., reading faint lines), removing subjective user error and reducing misclassification [100]. |
| Multiplex PCR Assays | Molecular tests that detect multiple targets (e.g., virus and resistance markers) in one reaction [102] [57]. | Reduces the number of separate tests needed, minimizing overall sample handling and potential for cross-contamination while providing more data from a single sample [102]. |
Experimental Workflow for Contamination Control
The diagram below outlines a logical workflow for integrating contamination control measures into the development of a point-of-care diagnostic test.
Benchmarking Traditional Cell Culture Against Modern Molecular Assays
Frequently Asked Questions
1. What are the main types of cell culture used in viral diagnostics? Cell culture methods have evolved significantly. Traditional cell culture often uses screw-cap tubes where cells grow in a monolayer and are examined for virus-induced morphological changes, a process that can take days to weeks [105]. Modern formats include:
- Shell Vials & Cluster Plates: Smaller containers that allow for easy centrifugation, enhancing the speed of virus adsorption into the host cells [105] [106].
- Cryopreserved Cell Cultures: Monolayer cells are grown in shell vials and stored in liquid nitrogen for ready use, maintaining sensitivity to various pathogens [105].
- Co-cultured Cells: Different cell types are grown together in a single vial to detect a broader range of viruses simultaneously [105] [106].
- Transgenic Cell Lines: Genetically engineered cells contain reporter genes that activate in the presence of a specific virus, allowing for rapid and specific identification [105] [106].
2. My cell culture medium has become cloudy and the pH has dropped suddenly. What does this indicate? This is a classic sign of bacterial contamination [42]. Under a microscope, bacteria may appear as tiny, moving granules between your cells. Such contamination is typically introduced through a break in aseptic technique. You should isolate the contaminated culture immediately and decontaminate your work area and incubators [42].
3. How can I detect viral contamination that doesn't cause obvious cell death? Not all viruses cause a clear cytopathic effect (CPE). For these, or for faster results, pre-CPE (or "pre-CPE") molecular methods are used [106]. After inoculating a shell vial culture and using centrifugation to enhance infection, the cells are stained with virus-specific, fluorescently-labeled antibodies after a short incubation (e.g., 24-48 hours). The presence of the virus is confirmed by detecting the fluorescent signal before any CPE is visible [105] [106].
4. What are the key advantages of molecular assays like PCR over traditional culture? Molecular diagnostics offer several key advantages, particularly for rapid outbreak investigation and highly sensitive detection [107] [108].
- Speed: Results can be obtained in hours, compared to days or weeks for some cultures [107] [108].
- Sensitivity & Specificity: They can detect minute amounts of viral genetic material with high precision, reducing false negatives and false positives [107] [109] [108].
- Scope: They can identify viruses that do not grow well in culture or detect specific genetic markers for drug resistance [107] [108].
5. When might traditional cell culture still be the preferred method? Despite being slower, traditional cell culture is still considered a gold standard for virus isolation because it [105] [108]:
- Allows for the propagation of novel or unexpected viruses that might not be targeted by a specific molecular assay.
- Provides a live virus isolate for further characterization, vaccine development, or phenotypic antiviral susceptibility testing [108].
Troubleshooting Common Contamination Issues
| Issue & Signs | Likely Contaminant | Immediate Action | Prevention & Long-Term Solution |
|---|---|---|---|
| Cloudy medium, sudden pH drop, tiny moving granules under microscope. | Bacteria [42] | Isolate culture. Discard media and culture. Decontaminate incubator and hood. [42] | Strict aseptic technique. Avoid routine antibiotics to prevent resistant strains. [42] |
| Stable pH then rapid increase, ovoid particles that bud (yeast), or wispy filaments (mold). | Fungi (Yeast or Mold) [42] | Isolate culture. Discard media and culture. Thoroughly clean equipment. [42] | Regular cleaning of incubators and water baths. Use antimycotics sparingly and only for short-term applications. [42] |
| No visible signs, but cells exhibit slow growth, abnormal morphology, or other unexplained experimental artifacts. | Mycoplasma [42] | Test all cultures regularly using PCR, ELISA, or specific staining. Isolate positive cultures. [42] | Obtain cells from reputable banks. Test new cell lines upon arrival and maintain a master stock. Quarantine new cultures. [42] |
| Unexpected or anomalous results during genetic or protein analysis. | Cross-Contamination (e.g., with a fast-growing cell line like HeLa) [42] | Authenticate the cell line using DNA fingerprinting, karyotyping, or isoenzyme analysis. [42] | Practice good aseptic technique. Handle only one cell line at a time. Obtain cell lines from reputable bioresource centers (e.g., ATCC). [42] |
Quantitative Comparison: Traditional vs. Modern Methods
The table below summarizes key performance metrics for different diagnostic approaches, highlighting how modern methods address the limitations of traditional techniques.
| Method | Typical Turnaround Time | Key Advantage | Primary Limitation | Relative Cost |
|---|---|---|---|---|
| Traditional Cell Culture | 2 days - several weeks [105] | Gold standard for virus isolation; can detect novel pathogens [105] [108] | Slow; requires expertise; cannot detect non-cytopathic viruses [105] [106] | Low (media & tubes) [105] |
| Shell Vial Culture (pre-CPE) | 1 - 2 days [106] [108] | Faster than traditional culture; allows for specific immunostaining [105] [106] | Still requires cell culture infrastructure and skills [106] | Moderate [105] |
| Immunoassays (e.g., ELISA) | Hours [109] | Rapid; well-established; robust [107] [109] | Lower sensitivity; potential for cross-reactivity (false positives) [107] [109] | Low - Moderate [107] |
| Molecular Assays (e.g., PCR) | Hours [107] [108] | Extremely high sensitivity and specificity; rapid development for new viruses [107] [108] | Requires specialized equipment; risk of amplicon contamination; may detect non-viable virus [109] [108] | Higher initial investment [107] |
Experimental Protocol: Shell Vial Culture with Pre-CPE Immunofluorescence
This protocol is a modernized cell culture method designed to reduce time-to-result and allow for specific virus identification.
Objective: To rapidly detect a viral pathogen in a clinical sample using centrifugation-enhanced inoculation and immunofluorescence staining.
Materials:
- Shell vials containing a monolayer of appropriate cell lines (e.g., MRC-5, A549) [105]
- Clinical sample (e.g., respiratory secretion, tissue homogenate)
- Cell culture medium and reagents
- Phosphate-buffered saline (PBS)
- Fixative (e.g., cold acetone or methanol)
- Virus-specific primary antibody
- Fluorescently-labeled secondary antibody
- Centrifuge with shell vial rotors
- Humidified incubator at 35–37°C with 5% CO₂
- Fluorescence microscope
Method:
- Sample Preparation: Vortex the sample medium and centrifuge. Use the supernatant for inoculation [105].
- Inoculation: Add 0.2–0.3 mL of the sample supernatant to the shell vial [105].
- Centrifugation: Centrifuge the vials at a low speed (e.g., 700 x g) for 30-60 minutes at room temperature. This step enhances viral adsorption into the cells [106].
- Incubation: Remove the inoculum, add fresh maintenance medium, and incubate the vials at 35–37°C with 5% CO₂ for 24-48 hours [105] [106].
- Fixation: After incubation, remove the medium, wash the monolayer with PBS, and add fixative for 5-10 minutes.
- Staining:
- Apply the virus-specific primary antibody to the fixed monolayer and incubate as required.
- Wash to remove unbound antibody.
- Apply the fluorescently-labeled secondary antibody and incubate in the dark.
- Perform a final wash [106].
- Detection: Examine the monolayer under a fluorescence microscope. The presence of specific fluorescence indicates a positive result for the target virus [106].
Decision Pathway for Viral Diagnostic Method Selection
The following diagram illustrates a logical workflow for choosing the most appropriate diagnostic method based on the experimental context and requirements.
The Scientist's Toolkit: Essential Research Reagents
This table details key materials and reagents used in the viral diagnostic methods discussed.
| Item | Function in Experiment | Key Consideration |
|---|---|---|
| Cell Lines (RhMK, MRC-5, A549) | Act as host systems for viral replication and isolation [105]. | Selection of the correct cell line is critical, as different viruses grow preferentially in specific cell types [105]. |
| Shell Vials / Cluster Plates | Provide a sterile, compact container with a growth surface for cells, optimized for centrifugation [105] [106]. | Enables rapid infection via centrifugation, significantly reducing incubation time [106]. |
| Virus-Specific Antibodies | Used for immunofluorescence staining in pre-CPE detection to identify a specific virus [105] [106]. | The specificity of the antibody is paramount to avoid cross-reactivity and false positives [109]. |
| Nucleic Acid Extraction Kits | Isolate and purify viral DNA or RNA from a sample for molecular assays [107]. | The quality and purity of the extracted nucleic acid directly impact the sensitivity and accuracy of downstream PCR [107] [110]. |
| PCR Master Mix | Contains enzymes, nucleotides, and buffers necessary to amplify target viral genetic sequences [107] [108]. | Requires precise thermal cycling equipment. Isothermal master mixes (e.g., for LAMP) can simplify the process for point-of-care use [110]. |
| Transport & Storage Media | Preserve sample integrity from collection to processing [105]. | Must maintain pathogen viability for culture and prevent degradation of nucleic acids for molecular testing [105]. |
Conclusion
Effective viral diagnostic contamination risk reduction requires a multi-layered strategy that integrates foundational knowledge, robust methodological application, continuous troubleshooting, and rigorous validation. The convergence of advanced molecular tools like NGS, sophisticated bioinformatics, and automated decontamination technologies is setting a new standard for safety and accuracy. Future directions will likely involve the greater adoption of real-time, in-process monitoring systems and the development of even more sensitive and inclusive detection panels. For researchers and drug developers, embracing this comprehensive and proactive approach is paramount to ensuring the integrity of scientific data and the safety of biological products for patients worldwide.
References
- 1. Adventitious Agents and Live Viral Vectored Vaccines [https://pmc.ncbi.nlm.nih.gov/articles/PMC5130882/]
- 2. Virus contaminations of cell cultures – A biotechnological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3463984/]
- 3. Avoiding Contamination | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/good-laboratory-practice-avoid-contamination-qpcr-experiments.html]
- 4. A history of adventitious agent contamination and the ... [https://www.sciencedirect.com/science/article/pii/S1045105622000690]
- 5. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 6. Strategies for Contamination Control [https://www.biopharminternational.com/view/strategies-for-contamination-control]
- 7. Mastering Cell Bank Production | BioPharm International [https://www.biopharminternational.com/view/mastering-cell-bank-production]
- 8. Cell Bank Preparation and Characterization - BioProcess International [https://www.bioprocessintl.com/cell-line-development/cell-banking-in-the-spotlight-advising-biologics-developers-about-cell-bank-preparation-and-characterization]
- 9. Contamination in pharmaceutical industry: types, causes ... [https://lindstromgroup.com/pharmaceutical-contamination-types-causes-and-prevention/]
- 10. Ensuring Quality in Cell and Gene Therapy: Overcoming Raw Material Challenges in CMC and GMP Compliance [https://www.atlantisbioscience.com/blog/ensuring-quality-in-cell-and-gene-therapy-overcoming-raw-material-challenges-in-cmc-and-gmp-compliance/]
- 11. Contamination-Control Processes [https://www.bioprocessintl.com/risk-management/what-unseen-trouble-lies-within-your-processes-]
- 12. Contamination Prevention: How Single-Use Systems Can ... [https://www.pharmtech.com/view/contamination-prevention-how-single-use-systems-can-ensure-safe-clean-and-efficient-bioprocess-envir]
- 13. Practicing Viral Vigilance Over Cell Culture-Based Processes [https://www.genengnews.com/topics/bioprocessing/viral-vigilance/]
- 14. Viral contamination in cell culture: analyzing the impact of Epstein Barr virus and Ovine Herpesvirus 2 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893573/]
- 15. Frontiers | Viral contamination in cell culture: analyzing the impact of Epstein Barr virus and Ovine Herpesvirus 2 [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1442321/full]
- 16. Diagnostic criteria for Epstein-barr virus-associated encephalitis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243388/]
- 17. Advances in Epstein-Barr Virus Detection: From Traditional ... [https://pubmed.ncbi.nlm.nih.gov/40872741/]
- 18. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOooMMSKk5qHVsyRjHXE3_XFm4qrNjjbSlqwslzLzHY9U2FZxPypg]
- 19. Viral contamination in biologic manufacture and ... [https://www.nature.com/articles/s41587-020-0507-2]
- 20. Viral contamination in biologic manufacture and ... [https://pubmed.ncbi.nlm.nih.gov/32341561/]
- 21. Infectious disease and economics: The case for considering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6330263/]
- 22. Socioeconomic impacts of airborne and droplet-borne ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-08993-y]
- 23. The Economic Risks and Impacts of Epidemics [https://www.imf.org/en/publications/fandd/issues/2018/06/economic-risks-and-impacts-of-epidemics-bloom]
- 24. Troubleshooting Cell Culture Contamination: A Practical ... [https://www.yeasenbio.com/blogs/cell/troubleshooting-cell-culture-contamination-a-practical-solution-guide]
- 25. Risk Assessment and Risk Control of Virus Contaminations [https://cbi.mit.edu/about-cbi/collaboration/caacb/caacb-projects/risk-assessment-and-risk-control-of-virus-contaminations/]
- 26. Preventing Contamination in mAb Process [https://www.merckmillipore.com/IL/en/applications/pharmaceutical-and-biopharmaceutical-manufacturing/monoclonal-antibody-manufacturing/preventing-adventitious-agent-contamination]
- 27. Fundamental Strategies for Viral Clearance - Part 1 [https://www.bioprocessintl.com/viral-clearance/fundamental-strategies-for-viral-clearance-part-1-exploring-the-regulatory-implications]
- 28. Viral Safety Strategy for mABs: Prevent, Detect, Remove | Merck [https://www.merckmillipore.com/DE/de/ps-learning-centers/Viral-Safety-Assurance/M9Wb.qB.YYQAAAFeJ1ISRXbG,nav]
- 29. Viral Safety Strategy for mABs: Prevent, Detect, Remove [https://www.merckmillipore.com/INTL/en/ps-learning-centers/Viral-Safety-Assurance/M9Wb.qB.YYQAAAFeJ1ISRXbG,nav]
- 30. Viral Clearance [https://www.merckmillipore.com/PG/en/products/pharma-and-biopharma-manufacturing/viral-clearance]
- 31. PCR Basic Troubleshooting Guide [https://www.creative-biogene.com/blog/pcr-basic-troubleshooting-guide]
- 32. PCR Troubleshooting Guide [https://www.genscript.com/pcr-troubleshooting-guide.html]
- 33. PCR Troubleshooting Guide [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide?srsltid=AfmBOoo6GBZQujD3rQNNxK8tEMkHiIkLgbsxs4aNtzjRc-q6_gkepFZ4]
- 34. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting?srsltid=AfmBOoqKiG_9aorNTlMi6RHpsem1Y07Fuwazl4SKWIYhemjVYdHqjvPc]
- 35. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 36. Next-Generation Sequencing Methods for Sensitive ... [https://www.medrxiv.org/content/10.1101/2025.06.17.25329745v1.full-text]
- 37. Troubleshooting Cell Culture Contamination [https://www.creative-bioarray.com/support/troubleshooting-cell-culture-contamination-a-comprehensive-guide.htm]
- 38. Viral Contamination in Bioproduction Facilities [https://www.bioprocessintl.com/viral-clearance/a-response-plan-for-viral-contamination-in-bioproduction-facilities]
- 39. Viral Risk Evaluation of Raw Materials Used in ... [https://www.bioprocessintl.com/qa-qc/viral-risk-evaluation-of-raw-materials-used-in-biopharmaceutical-production]
- 40. Understanding contamination: Raw materials [https://www.rssl.com/insights/life-science-pharmaceuticals/understanding-contamination-raw-materials/]
- 41. A Quick Guide for Sourcing Biopharmaceutical Raw Materials [https://www.bioprocessintl.com/biochemicals-raw-materials/a-quick-guide-for-sourcing-biopharmaceutical-raw-materials]
- 42. Culture Cell | Thermo Fisher Scientific - US Contamination [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 43. GMP Cell & Virus Bank Characterization [https://virusure.com/services/gmp-cell-virus-bank-characterization/]
- 44. How to maintain a cell ? – Single Use Support bank [https://www.susupport.com/blogs/knowledge/how-to-maintain-a-cell-bank]
- 45. Questions and Answers on Current Good Manufacturing ... [https://www.fda.gov/drugs/guidances-drugs/questions-and-answers-current-good-manufacturing-practice-regulations-production-and-process]
- 46. Cell bank system, establishment, and application in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409320/]
- 47. Cont-ID: detection of sample cross-contamination in viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10576407/]
- 48. Controlling for contamination in qPCR testing - LGC [https://blog.biosearchtech.com/how-to-control-for-contamination-in-qpcr-testing]
- 49. Real-Time PCR Troubleshooting [https://www.generi-biotech.com/real-time-pcr-troubleshooting/]
- 50. PCR/qPCR Troubleshooting Quick Reference [https://biopathogenix.com/pcr-qpcr-troubleshooting-quick-reference/]
- 51. How to Avoid Contamination in Your qPCR Experiments [https://rheniumbio.co.il/how-to-avoid-contamination-in-your-qpcr-experiments/]
- 52. A Mobile Laboratory Enables Fecal Pollution Source ... [https://www.mdpi.com/2073-4441/14/8/1224]
- 53. Contamination of healthcare workers' mobile phones by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7129817/]
- 54. Rapid detection method of bacterial pathogens in surface ... [https://www.nature.com/articles/s41598-023-49774-y]
- 55. Sensitive pathogen DNA detection by a multi-guide RNA ... [https://www.nature.com/articles/s41467-025-63094-x]
- 56. Molecular point-of-care testing technologies: Current status ... [https://www.sciencedirect.com/science/article/pii/S2950160125000063]
- 57. Impact of Point-of-Care Testing on Diagnosis, Treatment, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763637/]
- 58. Contamination Issue in Viral Metagenomics [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.745076/full]
- 59. Contamination-controlled high-throughput whole genome sequencing for influenza A viruses using the MiSeq sequencer | Scientific Reports [https://www.nature.com/articles/srep33318]
- 60. Targeted decontamination of sequencing data with CLEAN [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288876/]
- 61. Guide to implementing a VHP system for facility ... [https://www.sterislifesciences.com/Resources/Technical-Learning-Library/Technical-Learning-Library-Folder/Articles/Guide-to-Implementing-a-VHP-System-for-Facility-Biodecontamination]
- 62. VHP Sterilization Validation: 2025 Protocols - QUALIA [https://qualia-bio.com/blog/vhp-sterilization-validation-2025-protocols/]
- 63. VHP Decontamination Following Maintenance Activities [https://www.bioprocessintl.com/facility-design-engineering/cleanroom-decontamination-application-of-hydrogen-peroxide-vapor-following-maintenance-activities]
- 64. Vaporized Hydrogen Peroxide - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/vaporized-hydrogen-peroxide]
- 65. Understanding UVC Technology: How Germicidal UV ... [https://www.light-sources.com/blog/understanding-uvc-technology-how-germicidal-uv-systems-target-pathogens-in-air-water-and-surfaces/]
- 66. Choosing UV-C or VHP for Cleanroom Decontamination [https://www.ipu.dk/blog/surface-decontamination/]
- 67. Manual Cleaning vs. Far-UVC [https://uvmedico.com/news/manual-cleaning-vs.-far-uvc]
- 68. Validation of Cleaning Processes (7/93) [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/validation-cleaning-processes-793]
- 69. A Troubleshooting Guide for Common Issues in STR Analysis [https://www.forensicmag.com/Forensic-Tips/613460-A-Troubleshooting-Guide-for-Common-Issues-in-STR-Analysis/]
- 70. Response to Grisedale and Van Daal: comparison of STR ... profiling [https://pmc.ncbi.nlm.nih.gov/articles/PMC3544642/]
- 71. Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 72. A New Sensitive Method for the Detection of Mycoplasmas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6952905/]
- 73. Accelerate your Mycoplasma Testing - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/bioprocessing-accelerate-your-mycoplasma-testing/]
- 74. Faster methods for detecting viruses in food, water | MSUToday [https://msutoday.msu.edu/news/2025/08/detecting-water-contamination-earlier]
- 75. ViruSure launches pioneering viral contamination test for ... [https://nanoporetech.com/news/virusure-launches-pioneering-first-in-class-viral-contamination-test-for-biopharmaceuticals-using-oxford-nanopore-technology]
- 76. A Framework for Constructing Equity-Risk-Mitigation ... [https://rpc.cfainstitute.org/research/financial-analysts-journal/2020/framework-constructing-equity-risk-mitigation-portfolios]
- 77. What Is Cost-Benefit Analysis? 4 Step Process - HBS Online [https://online.hbs.edu/blog/post/cost-benefit-analysis]
- 78. Cost-Benefit Analysis: Step-by-Step Guide & Examples [https://www.rippling.com/blog/cost-benefit-analysis-example]
- 79. Preventing the Spread of Respiratory Viruses in Public ... [https://www.epa.gov/indoor-air-quality-iaq/preventing-spread-respiratory-viruses-public-indoor-spaces]
- 80. Prevention and control of avian influenza virus [https://www.nature.com/articles/s41467-025-58882-4]
- 81. Disrupting infectious diseases - The Source - WashU [https://source.washu.edu/2025/10/disrupting-infectious-diseasesas/]
- 82. ICH Q5A(R2) Guideline on viral safety evaluation of ... [https://www.ema.europa.eu/en/ich-q5ar2-guideline-viral-safety-evaluation-biotechnology-products-derived-cell-lines-human-or-animal-origin-scientific-guideline]
- 83. Q5A(R2) Viral Safety Evaluation of Biotechnology Products ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q5ar2-viral-safety-evaluation-biotechnology-products-derived-cell-lines-human-or-animal-origin]
- 84. Viral Safety With ICH Q5A Revision 2 [https://www.bioprocessintl.com/viral-clearance/viral-safety-for-biotechnology-products-including-viral-vectors-ich-q5a-revision-2-brings-updated-and-more-comprehensive-guidance]
- 85. Q5A(R2) Viral Safety Evaluation of Biotechnology Products ... [https://www.federalregister.gov/documents/2024/01/11/2024-00407/q5ar2-viral-safety-evaluation-of-biotechnology-products-derived-from-cell-lines-of-human-or-animal]
- 86. Viral Clearance Testing: Qualifying Downstream Processes [https://ritaibioreactor.com/viral-clearance-testing/]
- 87. New Technologies for Viral Clearance [https://www.biopharminternational.com/view/new-technologies-for-viral-clearance]
- 88. Viral Clearance Validation [https://www.cygnustechnologies.com/viral-clearance?srsltid=AfmBOoqtbWhWaiguqbwqPy8xLwgvkdcwQ-9frYux-11EpEHracA2EVNk]
- 89. Overcoming Viral Clearance Challenges [https://www.biopharminternational.com/view/overcoming-viral-clearance-challenges]
- 90. Downstream Processing: Viral Clearance and Inactivation [https://www.bioprocessintl.com/viral-clearance/introduction-viral-clearance-and-inactivation-in-downstream-processing]
- 91. Virus Detection: A Review of the Current and Emerging ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8093571/]
- 92. From Tradition to Innovation: Diverse Molecular ... [https://www.mdpi.com/2075-4418/14/24/2876]
- 93. Next-Generation Sequencing for Infectious Diseases ... [https://myadlm.org/cln/articles/2021/september/next-generation-sequencing-for-infectious-diseases-diagnostics-is-it-worth-the-hype]
- 94. Viral Metagenomic Next-Generation Sequencing for One ... [https://www.mdpi.com/1422-0067/26/19/9831]
- 95. vPro-MS enables identification of human-pathogenic ... [https://www.nature.com/articles/s41467-025-62469-4]
- 96. Next-Generation Nucleic Acid-Based Diagnostics for Viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388196/]
- 97. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting?srsltid=AfmBOorHCE7VjMoa5VrgVLZSNhNSFU_BI4ZD9a8mgltjeLuXtQDG_Ti9]
- 98. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 99. Advancing point of care testing for respiratory viruses [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/poc-respiratory-virus-testing.html]
- 100. Machine learning in point-of-care testing: innovations, ... [https://www.nature.com/articles/s41467-025-58527-6]
- 101. Exploring innovations in point-of-care diagnostics for the ... [https://www.sciencedirect.com/science/article/pii/S2543106425000018]
- 102. What are the 2025 Trends in Diagnostics? [https://www.hartmannyoung.com/resources/blog/what-are-the-2025-trends-in-diagnostics-/]
- 103. ICMR's 2025 Guidance on Rapid Diagnostic Validation & ... [https://cliniexperts.com/regulatory-update/guidance-document-on-validation-of-rapid-diagnostics-for-pathogen-identification-and-antimicrobial-susceptibility-testing-ast-2025/]
- 104. Developing Rapid Diagnostic Tests for Infectious Diseases [https://www.hopkinsmedicine.org/news/articles/2025/02/developing-rapid-diagnostic-tests-for-infectious-diseases]
- 105. Traditional and Modern Cell Culture in Virus Diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4850366/]
- 106. Virus Detection: A Review of the Current and Emerging ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.637559/full]
- 107. Molecular Diagnostics or Traditional ... [https://www.celnovte.com/solution/molecular-diagnostics-vs-traditional-diagnostics-a-complete-comparison/]
- 108. Molecular Diagnostic Assays for Detection of Viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7099217/]
- 109. Pathogen Testing: Immunoassay vs. Molecular Methods [https://www.eurofinsus.com/food-testing/resources/pathogen-testing-immunoassay-vs-molecular-methods/]
- 110. Advances in point-of-care and molecular techniques to ... [https://www.nature.com/articles/s41545-024-00368-9]