Viral Diagnostic Test Verification and Validation: A Comprehensive Guide for Researchers and Developers
This article provides a detailed guide to the verification and validation procedures essential for developing and deploying reliable viral diagnostic tests.
Viral Diagnostic Test Verification and Validation: A Comprehensive Guide for Researchers and Developers
Abstract
This article provides a detailed guide to the verification and validation procedures essential for developing and deploying reliable viral diagnostic tests. Aimed at researchers, scientists, and drug development professionals, it covers foundational principles, from defining verification vs. validation to navigating regulatory landscapes. It explores methodological applications for established and novel techniques like metagenomic sequencing, addresses common troubleshooting and optimization challenges, and outlines robust validation frameworks like the VALCOR protocol. The content synthesizes lessons from recent outbreaks, including COVID-19, and highlights emerging trends such as AI and federated learning to prepare for future diagnostic needs.
Core Principles and Regulatory Landscape of Viral Diagnostic Validation
A guide for researchers and scientists navigating the critical stages of assay development.
Core Definitions: Verification vs. Validation
| Feature | Verification | Validation |
|---|---|---|
| Primary Question | "Did we build the assay right?" [1] | "Did we build the right assay?" [1] |
| Objective | Confirm the test is designed, developed, and manufactured correctly according to predefined specifications and protocols. | Confirm the test is fit for its intended purpose and meets the needs of the end-user in a real-world setting. |
| Focus | Internal accuracy and precision; the technical performance of the assay itself. | External utility and reliability; the clinical or research effectiveness of the test results. |
| Stage of Conduct | Typically performed during the initial development and optimization of the assay, often in a controlled laboratory setting. | Typically performed after successful verification, on a larger scale that mirrors the intended use environment. |
| Primary Audience | Laboratory managers, development scientists, and technical staff. | Regulatory bodies, end-users (e.g., clinicians, researchers), and stakeholders. |
Frequently Asked Questions for Researchers
Technical & Procedural FAQs
Q1: During verification, our assay shows high precision but poor accuracy. What could be the cause? This discrepancy often points to a systematic error (bias) in your method. Troubleshoot using this protocol:
- Step 1: Calibrate Equipment. Verify the calibration of all instruments, including pipettes, centrifuges, and plate readers, using traceable standards.
- Step 2: Analyze Reference Materials. Test a certified reference material (CRM) or a known positive control from an alternate source. If the result is consistently biased, it confirms a systematic issue.
- Step 3: Review Reagent Preparation. Meticuously check the preparation, pH, and storage conditions of all buffers, standards, and reagents. A small error in concentration can cause significant bias.
- Step 4: Investigate Operator Technique. If possible, have a second experienced scientist repeat the assay to rule out individual technique as a factor.
Q2: How do I determine the appropriate sample size for a validation study? Validation sample size is determined by statistical power requirements for key claims. Follow this methodology:
- Define Key Parameters: Focus on sensitivity, specificity, and precision.
- Use Statistical Formulae: For sensitivity and specificity, use the following formula for a desired Confidence Interval (CI) width:
n = (Z^2 * p * (1-p)) / d^2where:n= required sample sizeZ= Z-score (e.g., 1.96 for 95% CI)p= expected proportion (e.g., expected sensitivity)d= desired margin of error (half the CI width)
- Incorporate Prevalence: For clinical studies, ensure your sample panel reflects the real-world prevalence of the condition. A biostatistician should be consulted to finalize the sample size.
Q3: Our validation results are inconsistent across different sample matrices (e.g., serum vs. saliva). How should we proceed? Matrix effects are a common challenge. Implement this systematic investigation:
- Protocol 1: Spike-and-Recovery Experiment.
- Spike a known quantity of the viral analyte into each problematic matrix and a control matrix (e.g., buffer).
- Measure the recovered concentration in each.
- Calculate the percentage recovery:
(Measured Concentration in Matrix / Measured Concentration in Control) * 100. - Acceptable recovery is typically 80-120%. Significant deviations indicate matrix interference.
- Protocol 2: Sample Dilution Linearity.
- Create a series of dilutions for an affected sample.
- Analyze the dilutions. If the measured analyte concentration is not proportional to the dilution factor, it suggests the presence of interfering substances that are diluted out.
- Solution: Based on the results, you may need to modify the sample preparation protocol, introduce a purification or extraction step, or specify limitations on acceptable sample matrices in your assay's instructions for use (IFU).
Compliance & Documentation FAQs
Q4: What is the minimum documentation required for a verification study? Your verification report should be a standalone document that allows for the reconstruction of the study. Essential elements include:
- Signed Protocol: The pre-approved study protocol outlining objectives, methods, and acceptance criteria.
- Raw Data: All original data, including instrument printouts, lab notebook pages, and electronic records.
- Summary Tables & Calculations: Data summarized with clear calculations for precision, accuracy, LoD, etc.
- Analysis Against Criteria: A direct comparison of results against pre-defined acceptance criteria.
- Deviations Log: A log of any deviations from the protocol, with an impact assessment.
- Conclusion: A definitive statement on whether the assay passed verification.
Q5: How should we handle a deviation or out-of-specification (OOS) result during validation? Do not discard OOS results. Follow a strict investigation procedure:
- Phase I (Laboratory Investigation): The analyst and supervisor conduct an immediate assessment to identify obvious analytical errors (e.g., calculation error, equipment malfunction, improper technique). This investigation must be documented.
- Phase II (Full OOS Investigation): If no clear assignable cause is found in Phase I, a formal investigation is launched. This includes:
- Retesting by a second analyst if possible.
- Review of reagent and sample integrity.
- A comprehensive review of the process and training records.
- Documentation: The entire investigation, including hypotheses, tests performed, and final conclusions, must be documented in the validation report. The OOS result may stand, or it may be invalidated based on clear, documented evidence.
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Viral Assay Development |
|---|---|
| Certified Reference Materials (CRMs) | Provides a gold standard with a defined, traceable quantity of the viral target or antibody. Critical for establishing assay accuracy and calibration during verification [2]. |
| Clinical Isolates & Biobanked Samples | Characterized, real-world patient samples used to challenge the assay. Essential for determining clinical sensitivity and specificity during validation studies. |
| Monoclonal & Polyclonal Antibodies | Key binding reagents for immunoassays (ELISA, LFIA). Specificity and lot-to-lot consistency of these antibodies are fundamental to the assay's performance and must be rigorously qualified [3]. |
| Molecular Standards (gBlocks, RNA Transcripts) | Synthetic nucleic acid fragments used as positive controls and for generating standard curves in PCR-based assays (qPCR, RT-qPCR). Used to determine the Limit of Detection (LoD) [2]. |
| Interferent Substances | Purified substances (e.g., bilirubin, hemoglobin, lipids, common medications) added to samples to test for assay interference. Used to establish assay robustness and specificity [2]. |
Experimental Workflow: From Concept to Validated Assay
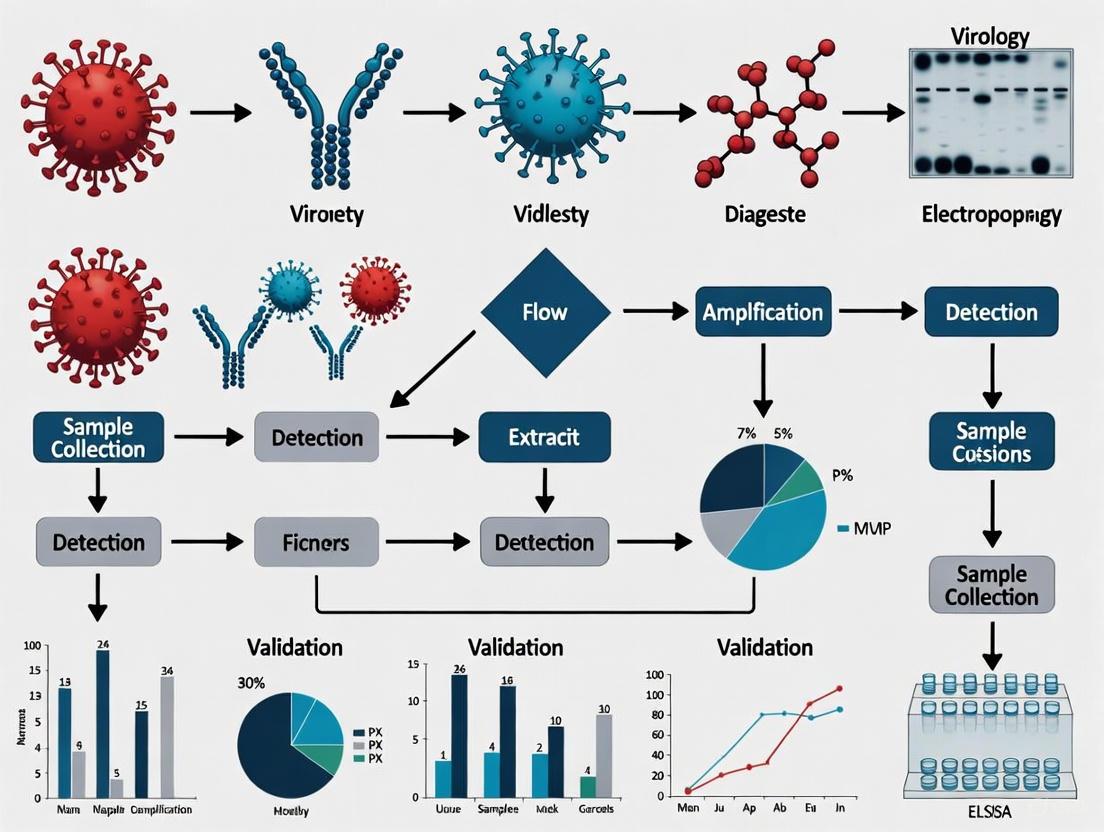
The following diagram illustrates the logical relationship and workflow between the key stages of assay verification and validation.
Regulatory Requirements and Quality Standards (CLIA, ISO, FDA/EUA)
Clinical laboratories operating in the United States navigate a complex regulatory landscape primarily governed by three key entities: the Clinical Laboratory Improvement Amendments (CLIA), the U.S. Food and Drug Administration (FDA), and the International Organization for Standardization (ISO). Understanding their distinct roles is fundamental to maintaining compliance while ensuring test quality and reliability [4].
Key Regulatory Bodies and Their Roles
| Regulatory Body | Authority & Scope | Primary Focus | Requirement Level |
|---|---|---|---|
| CLIA | U.S. federal regulations administered by CMS [5]. | Quality standards for all laboratory testing on human specimens [4]. | Mandatory for U.S. clinical labs [4]. |
| FDA | U.S. federal regulatory agency [4]. | Safety and effectiveness of medical devices, including in vitro diagnostic (IVD) tests [4]. | Mandatory for test manufacturers and market access [4]. |
| ISO 15189 | International voluntary organization [4]. | Quality and competence in medical laboratories; a quality management system framework [6]. | Voluntary, but demonstrates commitment to quality [4]. |
The Interplay of Regulations
- CLIA Compliance is Foundational: Any facility performing testing on human specimens for health assessment or diagnosis must hold an appropriate CLIA certificate [7]. CLIA regulations comprehensively cover the entire testing process, including personnel qualifications, quality control, proficiency testing, and quality assurance [4] [7].
- FDA's Evolving Role: While laboratories have traditionally been "users" of FDA-cleared tests, the FDA's final rule on Laboratory Developed Tests (LDTs) now subjects labs creating their own tests to additional FDA regulations as "manufacturers" [4]. The FDA also grants Emergency Use Authorizations (EUAs) for unapproved medical products during public health emergencies [8].
- ISO as the "Icing on the Cake": ISO 15189 certification is not a legal requirement but serves as a mark of excellence. It enhances a laboratory's quality management system and is often required for international work or specific contracts [4]. The standard must be updated to ISO 15189:2022 by December 2025, introducing enhanced requirements for risk management and point-of-care testing (POCT) [6].
Test Verification and Validation Protocols
Verification and validation are critical processes to ensure that a test method consistently produces accurate and reliable results for patient care.
CLIA Method Verification
For non-waived testing (moderate and high complexity), CLIA requires laboratories to establish or verify the performance specifications for each method prior to reporting patient results [7]. This process confirms that the test performs as expected in your laboratory environment.
Core Performance Specifications to Verify [7]:
| Specification | Definition | Common Verification Method |
|---|---|---|
| Accuracy | Closeness to the true value | Proficiency testing (PT) samples, comparison to a reference method. |
| Precision | Reproducibility of results (repeatability) | Testing replicates of the same sample. |
| Reportable Range | Span of reliable results between lowest and highest measurable values | Testing calibrators or patient samples across the claimed range. |
| Reference Range | Normal values for your patient population | Testing specimens from healthy individuals. |
Example Verification Experimental Protocol:
- Develop a Plan: The laboratory director or technical supervisor defines acceptance criteria for each performance specification based on manufacturer's claims, clinical needs, or published guidelines [7].
- Gather Materials: Collect a sufficient number of samples. A common approach is to use 20 specimens spanning the reportable range for quantitative tests, or 5 positive and 5 negative specimens for qualitative tests [7].
- Execute Testing: Run the samples according to the test's standard procedure over multiple days and by different technologists if possible to capture real-world variability.
- Analyze Data: Compare results against acceptance criteria. For example, calculate the coefficient of variation (CV%) for precision studies and assess bias for accuracy.
- Document and Approve: All procedures, raw data, and summary conclusions must be documented and approved by the laboratory director before the test is implemented for patient testing [7].
FDA Emergency Use Authorization (EUA)
During a declared public health emergency, the FDA may issue an EUA to allow the use of unapproved medical products or unapproved uses of approved products. This pathway was extensively used for COVID-19 and mpox diagnostics [8].
The EUA process involves a submission from the manufacturer or developer demonstrating that the product may be effective and that the known benefits outweigh the potential risks, given the emergency context [8]. The NIH's RADx initiative provided a model for third-party, independent test verification to accelerate this process during the COVID-19 pandemic [9].
Frequently Asked Questions (FAQs)
1. Our lab is already CLIA certified and we are developing a new LDT. Do we still need to follow CLIA rules, or just the new FDA LDT rules? You must follow both sets of regulations. The FDA's LDT regulations are in addition to, not instead of, CLIA requirements. Your laboratory must maintain its CLIA certification and comply with all applicable CLIA quality standards while also meeting the new FDA requirements for pre-market review, quality systems, and adverse event reporting for your LDT [4].
2. What is the most common area where labs struggle with quality and compliance? A significant challenge, especially for labs developing LDTs, is implementing the FDA's design control requirements. CLIA has no direct equivalent to these systematic processes for managing a test's design and development. Additionally, labs often face difficulties due to a lack of personnel with the expertise and time to fully grasp and implement the overlapping requirements from different regulatory bodies [4].
3. We are planning to get ISO 15189 accredited. What are the key changes in the 2022 version? The updated ISO 15189:2022 standard, which must be implemented by December 2025, introduces several key changes [6]:
- Integration of POCT requirements, previously in a separate standard (ISO 22870).
- Enhanced focus on risk management, requiring labs to implement more robust processes to identify and mitigate risks to quality.
- Updated structural and governance requirements with clearer roles and responsibilities.
4. Where do most laboratory errors occur? The majority of laboratory errors occur in the pre-analytical (test ordering, patient identification, specimen collection) and post-analytical (result reporting, data entry) phases. Less than 10% of errors happen during the actual testing or analytical phase. This highlights the importance of a robust quality assurance program that covers the entire testing process, not just the equipment in the lab [7].
5. What are the CLIA requirements for staff competency? CLIA requires laboratories to perform competency assessments for all testing personnel semiannually during the first year of employment and annually thereafter. This assessment must include six components [7]:
- Direct observation of routine test performance.
- Direct observation of instrument maintenance.
- Monitoring of test result reporting and recording.
- Review of test results, worksheets, QC, and PT records.
- Assessment of test performance through testing blind samples.
- Assessment of problem-solving skills.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and solutions essential for the development and verification of viral diagnostic tests.
| Item | Primary Function in Test R&D |
|---|---|
| Positive Control Material | Contains the target analyte (e.g., inactivated virus, synthetic RNA) to verify the test can detect a positive signal and monitor assay performance over time. |
| Negative Control Material | Confirms the test does not produce a false-positive signal due to contamination or non-specific reactions. |
| Calibrators | Standardized materials with known concentrations of the analyte used to create a calibration curve for quantitative tests, ensuring result accuracy across the measuring range. |
| Proficiency Testing (PT) Samples | External, third-party samples used to objectively compare a lab's testing performance against a reference method or peer labs, as required by CLIA [5] [7]. |
| Clinical Specimens | Residual patient samples (positive and negative) are the gold standard for clinical validation and verification studies, providing real-world matrix for evaluating accuracy [7]. |
| Third-Party Quality Control | Control materials not supplied by the test kit manufacturer, used to independently monitor the stability and reliability of the entire test system [10]. |
Experimental Workflow for Test Verification
The diagram below outlines the logical workflow for verifying a new diagnostic test or method in a clinical laboratory, integrating CLIA and quality management requirements.
The Critical Role of Independent Clinical Evaluation in Public Health
FAQs: Core Principles and Processes
Q1: What is the primary purpose of an independent clinical evaluation for a viral diagnostic test? The primary purpose is to provide an impartial, objective assessment of a test's analytical and clinical performance (e.g., sensitivity, specificity) and its safety. This independent verification is crucial for validating manufacturer claims, informing regulatory decisions, and ensuring that only reliable tests are deployed in public health programs, especially during outbreaks [9].
Q2: How does independent evaluation differ from a manufacturer's own internal studies? Independent evaluation is conducted by a third party with no commercial stake in the product's success. This eliminates potential conflicts of interest and provides regulatory agencies and the public with higher-confidence, unbiased data. Programs like the NIH's RADx initiative established academic hubs to perform this "apples to apples" comparison of different technologies under standardized conditions [9].
Q3: What are the key performance parameters evaluated for a rapid diagnostic test (RDT)? A comprehensive evaluation typically assesses a battery of parameters, including:
- Analytical Sensitivity (Limit of Detection): The lowest concentration of the virus the test can reliably detect [9].
- Clinical Sensitivity: The test's ability to correctly identify infected individuals (true positive rate) [9].
- Clinical Specificity: The test's ability to correctly identify uninfected individuals (true negative rate) [9].
- Cross-reactivity: Potential for false positives due to other similar pathogens [9].
- Repeatability: Consistency of results when the test is repeated under identical conditions [9].
- Usability: Ease of use by intended operators in real-world settings [9].
Q4: What is the regulatory significance of a Clinical Evaluation Report (CER) under the EU MDR? The Clinical Evaluation Report (CER) is a mandatory technical documentation that summarizes all clinical evidence related to a medical device, including diagnostic tests. It must demonstrate that the device is safe, performs as intended, and has a favorable benefit-risk profile. For legacy devices, a new CER under MDR requirements is often necessary due to stricter rules on demonstrating equivalence and requiring post-market clinical follow-up (PMCF) data [11] [12].
Troubleshooting Guides: Common Experimental Challenges
Challenge 1: Inconsistent Test Performance Across Sample Types
Problem: A test shows high sensitivity with nasopharyngeal (NP) swabs but inconsistent or reduced sensitivity with saliva samples.
Solution Strategy:
- Re-evaluate Sample Processing: Saliva may contain inhibitors or require specific processing steps (e.g., homogenization, heating) not needed for NP swabs. Optimize the sample preparation protocol to inactivate inhibitors and ensure the sample is compatible with the test's chemistry [13].
- Verify Viral Load Dynamics: Confirm that the sample type is appropriate for the disease stage. For some viruses, saliva may have a different viral load profile compared to NP swabs over the course of infection. Correlate test results with quantitative PCR (qPCR) data from the same sample type [13].
- Conduct a Method Comparison Study: Perform a head-to-head comparison using matched sample pairs (e.g., NP and saliva from the same patient at the same time) to statistically quantify the performance difference and establish sample-specific usage criteria [9].
Challenge 2: Demonstrating Equivalence for a Modified Test Under MDR
Problem: A manufacturer has modified a legacy test and needs to use data from the previous version to support the new one, but must prove equivalence under stricter MDR rules.
Solution Strategy: The MDR requires demonstration of equivalence in technical, biological, and clinical characteristics [11].
- Technical: Provide evidence that the devices have similar design, specifications, properties, and are used under similar conditions of use (including software algorithms) [11].
- Biological: For tests involving substances introduced into the body, demonstrate identical substances and similar biocompatibility [11].
- Clinical: Show the devices have the same clinical condition, intended purpose, same kind of user, and similar critical performance and safety data [11].
- Documentation: Complete a detailed "Equivalence Table" as guided by MDCG, providing scientific justifications for any differences and arguing why they are not clinically significant [11].
Challenge 3: Poor Clinical Sensitivity in a Point-of-Care Rapid Antigen Test
Problem: A lateral flow antigen test for a respiratory virus fails to detect infections in patients with moderate viral loads, leading to false negatives.
Solution Strategy:
- Determine the Limit of Detection (LoD): Precisely establish the test's analytical sensitivity using cultured virus or synthetic antigens in a clinically relevant matrix. Compare this LoD to the typical viral load range observed in patient populations. A test with an LoD higher than the infectious threshold will have poor clinical sensitivity [9] [14].
- Evaluate Sample Collection Kit Compatibility: Some sample collection buffers or transport media can interfere with the test's immunoassay. Test the device with samples collected in different approved media to identify potential incompatibilities [13].
- Investigate Reader-Based Detection: If the test is visually interpreted, consider transitioning to a digital reader. Fluorescent or electrochemical-based readers can objectively detect weaker signals, improving sensitivity and reducing user interpretation errors [13] [15].
Experimental Protocols for Key Evaluations
Protocol 1: Analytical Sensitivity and Limit of Detection (LoD) Study
Objective: To determine the lowest concentration of the target virus (e.g., SARS-CoV-2) that the test can detect ≥95% of the time.
Materials:
- Cultured infectious virus or synthetic target (e.g., inactivated whole virus, recombinant antigen, RNA transcript).
- Appropriate negative matrix (e.g., synthetic saliva, universal transport medium).
- Test device and required reagents.
- Standard reference method (e.g., RT-qPCR).
Methodology:
- Sample Preparation: Serially dilute the virus or target in the negative matrix to cover a range from an expected detectable concentration down to below the expected LoD.
- Testing: Test each dilution level a minimum of 20 times (or as per regulatory guidance) with the device.
- Data Analysis: Calculate the proportion of positive results at each dilution level. The LoD is the lowest concentration at which ≥19/20 (95%) replicates test positive. Confirm this concentration in at least three independent experiments [9].
Protocol 2: Clinical Performance Evaluation (Sensitivity/Specificity)
Objective: To assess the test's ability to correctly identify infected and non-infected individuals compared to a reference standard.
Materials:
- Clinically characterized patient samples (e.g., remnant de-identified samples from clinical laboratories).
- A validated reference method (e.g., FDA-authorized PCR test for a viral target).
- Test devices.
Methodology:
- Sample Selection: Select a panel of samples that represent the test's intended use population, including positive samples with a range of viral loads and negative samples. Include samples with potential cross-reactive organisms to assess specificity.
- Blinded Testing: Test all samples with the investigational device under evaluation in a blinded manner.
- Data Analysis:
- Calculate Clinical Sensitivity: (Number of True Positives / (Number of True Positives + Number of False Negatives)) × 100.
- Calculate Clinical Specificity: (Number of True Negatives / (Number of True Negatives + Number of False Positives)) × 100.
- Report results with 95% confidence intervals [9] [16].
Research Reagent Solutions
This table details essential materials and their functions in the development and evaluation of viral diagnostic tests.
| Research Reagent / Material | Function in Test Development & Evaluation |
|---|---|
| Recombinant Antigens & Monoclonal Antibodies | Key components for developing immunoassays (e.g., lateral flow tests); used to capture and detect viral proteins. Critical for defining test specificity [13] [15]. |
| * Synthetic RNA Transcripts & DNA Oligonucleotides* | Non-infectious controls for developing and calibrating nucleic acid amplification tests (NAAT). Essential for determining analytical sensitivity (LoD) and verifying assay performance [9]. |
| Inactivated Whole Virus | Provides a more authentic target for evaluating test performance compared to recombinant components, as it presents antigens in a native conformation [13]. |
| Clinical Sample Panels | Well-characterized, remnant patient samples used as the gold standard for establishing clinical sensitivity and specificity during validation studies [9] [16]. |
| Microfluidic Chips & Cartridges | The physical platform for many modern "lab-on-a-chip" and molecular POC tests. They integrate sample preparation, amplification, and detection into a single, automated system [13]. |
Workflow Diagrams
Independent Test Evaluation Pathway
Clinical Evaluation Report (CER) Lifecycle
The COVID-19 pandemic created an unprecedented global demand for reliable diagnostic testing, placing immense pressure on regulatory systems and laboratory networks. The emergency use authorization (EUA) pathway enabled rapid deployment of tests but revealed significant challenges in maintaining validation standards during a crisis [17]. The experience demonstrated that sustainable validation resources—including standardized protocols, reusable reagent kits, and clear regulatory guidance—are critical for ensuring diagnostic accuracy during future outbreaks. The core lesson is that validation infrastructure must be built during peacetime to be effective during emergencies.
Regulatory Frameworks and Validation Priorities
Evolving Regulatory Pathways
The U.S. Food and Drug Administration (FDA) implemented a prioritized review process for SARS-CoV-2 tests as the pandemic evolved. The agency's experience led to important policy shifts that can inform future outbreak response strategies [17]. The table below summarizes key regulatory priorities established during the pandemic:
Table 1: FDA Review Priorities for Diagnostic Tests During the COVID-19 Pandemic
| Priority Category | Description | Intended Impact |
|---|---|---|
| Innovative Technology | Tests employing novel technological approaches | Address complex diagnostic challenges with new solutions |
| Unmet Public Health Need | Tests diagnosing infection with new variants or subvariants | Fill critical gaps in testing capabilities |
| Government Partnership | Tests supported by U.S. government stakeholders (BARDA, NIH RADx) | Leverage coordinated resource investment |
| Supplemental EUA Requests | Submissions fulfilling a condition of an existing EUA | Streamline authorization for test modifications |
The FDA now strongly encourages developers to pursue traditional premarket pathways (de novo classification or 510(k) clearance) rather than relying on EUA mechanisms, reflecting a maturation of the regulatory landscape for molecular diagnostics [17].
Laboratory Modification Policies
A critical flexibility emerged for high-complexity CLIA-certified laboratories modifying EUA-authorized tests. The FDA specified conditions under which laboratories could implement modifications without new EUA submissions, provided that [17]:
- Modifications do not change the indication for use
- Changes do not alter analyte specific reagents (e.g., PCR primers/probes)
- Laboratories validate the modification and confirm equivalent performance
- Use remains limited to the implementing laboratory
This policy balance between flexibility and oversight offers a model for future outbreaks, enabling rapid adaptation while maintaining quality standards.
Diagnostic Test Validation: Protocols and Procedures
Verification of EUA COVID-19 Diagnostic Tests
The American Society for Microbiology (ASM) developed step-by-step verification procedures to help laboratories implement EUA molecular tests efficiently while ensuring accuracy [18]. These guidelines address the unique characteristics and limitations of different assay formats, including direct sample-to-answer systems, point-of-care devices, and high-complexity batched-based testing.
Table 2: Essential Components of Test Verification Protocols
| Component | Description | Application in COVID-19 Testing |
|---|---|---|
| Necessary Supplies | Reagents, controls, consumables | Identification of critical supply chain dependencies |
| Quality Control Standards | Positive, negative, internal controls | Establishing baseline performance metrics |
| Safety Requirements | Personal protective equipment, biosafety protocols | Protecting laboratory personnel during specimen handling |
| Assay Limitations | Known cross-reactivities, interference | Understanding diagnostic test boundaries |
Analytical and Clinical Validation
Comprehensive test validation requires both analytical studies (establishing test performance characteristics) and clinical studies (demonstrating real-world accuracy). The FDA provides tailored recommendations through EUA templates that reflect current thinking on validation requirements for different test types [17].
Test Validation Workflow
Research Continuity During Public Health Emergencies
Challenges in Clinical Research
The COVID-19 pandemic significantly disrupted clinical research across multiple domains. A comprehensive narrative review identified four major categories of challenges [19]:
- Researcher/Investigator Issues: Travel restrictions, reduced funding allocation to non-COVID research, and safety concerns for research staff.
- Participant and Ethical Concerns: Volunteer unwillingness, difficulties with informed consent processes, and ethical challenges in following up vulnerable patients.
- Administrative Issues: Institutional review board operational disruptions and contractual delays.
- Research Implementation Problems: Inability to conduct in-person assessments and interventions.
Remote Research Solutions
In response to these challenges, researchers developed innovative remote methodologies that can be incorporated into future validation resource planning [19]:
- Remote monitoring through phone or video visits
- Electronic data capture systems minimizing in-person contact
- Virtual platforms for participant interaction and questionnaire completion
- Modified consent processes using digital signatures and telehealth platforms
These solutions enable research continuity while maintaining ethical standards and data integrity during public health emergencies.
Diagnostic Performance and Error Mitigation
Test Performance Characteristics
Understanding the limitations of different testing methodologies is crucial for appropriate implementation and interpretation. The performance characteristics of SARS-CoV-2 tests varied significantly by methodology and timing [20].
Table 3: Performance Characteristics of SARS-CoV-2 Diagnostic Tests
| Test Type | Average Sensitivity | Average Specificity | Optimal Use Conditions |
|---|---|---|---|
| Laboratory-based RT-PCR | 58-96% [20] | ~100% [20] | Symptomatic individuals, reference testing |
| Point-of-Care Molecular | 96.9% [20] | 100% [20] | Settings requiring rapid turnaround |
| Rapid Antigen (Symptomatic) | 72.0% [20] | 99.6% [20] | Early symptom onset (first week) |
| Rapid Antigen (Asymptomatic) | 58.1% [20] | 99.6% [20] | Serial testing strategies |
Cognitive Biases in Diagnostic Decision-Making
The pandemic highlighted how cognitive biases can affect diagnostic accuracy. Key biases identified included [20]:
- Availability bias: Overdiagnosing conditions that are prominent in recent experience while missing less common conditions
- Anchoring bias: Resisting alteration of initial diagnostic impressions despite contradictory evidence
- Implicit biases: Potentially contributing to disparities in testing and diagnosis across demographic groups
Mitigation strategies include diagnostic time-outs, deliberate consideration of alternative diagnoses, and using clinical decision support systems to estimate probabilities of alternative diagnoses [20].
Instrumentation and Research Reagent Solutions
Establishing standardized, reusable reagent kits and equipment protocols is essential for sustainable validation resources. The table below outlines key research reagent solutions and their functions based on methodologies used in COVID-19 research:
Table 4: Essential Research Reagent Solutions for Diagnostic Validation
| Reagent/Equipment Category | Function in Validation | Application Examples |
|---|---|---|
| Positive Control Materials | Verify test sensitivity and reproducibility | Inactivated virus, synthetic RNA controls, armored RNA |
| Negative Control Materials | Establish test specificity and identify contamination | Human specimen matrix without virus, transport media |
| Cross-Reactivity Panels | Assess assay specificity against related pathogens | Other coronaviruses, respiratory pathogens |
| Interference Substances | Identify potential assay interferents | Mucin, blood, common medications |
| Reference Standard Materials | Calibrate assays and establish quantitative ranges | WHO International Standards, FDA reference panels |
| Quality Control Reagents | Monitor assay performance over time | Low-positive, negative, internal controls |
Point-of-Care Testing Implementation
Regulatory Requirements for Point-of-Care Settings
Point-of-care testing presented unique implementation challenges during the pandemic. The CDC established specific guidance for SARS-CoV-2 rapid testing in these settings, emphasizing that [21]:
- Any site performing or interpreting tests for someone other than the individual being tested needs a CLIA certificate
- A CLIA Certificate of Waiver is appropriate if SARS-CoV-2 point-of-care testing is the only testing performed
- Sites must use FDA-authorized tests and follow manufacturer instructions precisely
Quality Assurance in Point-of-Care Testing
Implementing sustainable validation resources for point-of-care settings requires robust quality management systems. Key components include [21]:
- Pre-test processes: Proper reagent storage, specimen collection technique, and patient identification
- Testing processes: Adherence to manufacturer timing, quality control performance, and prevention of cross-contamination
- Post-test processes: Accurate result interpretation, timely reporting, and proper instrument decontamination
Point-of-Care Testing Quality Management
The COVID-19 pandemic revealed critical gaps in diagnostic validation infrastructure while simultaneously generating innovative solutions. Building sustainable resources for future outbreaks requires [17] [19] [18]:
- Standardized verification protocols that can be rapidly adapted to new pathogens
- Flexible regulatory pathways that balance speed with rigorous review
- Remote research methodologies that maintain study continuity during disruptions
- Reusable reagent platforms that minimize development timelines
- Cognitive debiasing strategies that improve diagnostic accuracy
By institutionalizing these lessons into peacetime operations, the global research community can establish the validation resources needed to respond more effectively to future public health emergencies.
Methodologies in Practice: From Standard PCR to Metagenomic Sequencing and AI
Nucleic Acid Amplification Tests (NAATs) are foundational tools in modern molecular diagnostics, detecting viral pathogens by amplifying and identifying their genetic material. These tests were crucial during the COVID-19 pandemic for diagnosing SARS-CoV-2 infection, exemplifying their critical role in infectious disease management [22]. The verification and validation of these tests are essential components of diagnostic development, ensuring they meet rigorous performance standards for clinical use. Within this framework, NAATs primarily fall into two methodological categories: thermocycling-dependent methods like Reverse Transcription Polymerase Chain Reaction (RT-PCR) and isothermal amplification methods that operate at a constant temperature [23]. The validation process must critically address analytical factors such as the limit of detection (LOD) and false-positive rates, which are vital for establishing test reliability and informing clinical decision-making [22]. This guide provides a structured technical resource for researchers and developers navigating the experimental and troubleshooting phases of NAAT development and application.
Core Principles and Techniques
NAATs encompass a range of techniques designed to amplify specific nucleic acid sequences from pathogens. The two main approaches are defined by their temperature requirements during amplification.
- RT-PCR and PCR-Based Methods: These tests require thermal cycling between different temperatures for denaturation, annealing, and extension. They are typically performed in a laboratory setting and are considered the gold standard for sensitivity [23].
- Isothermal Amplification Methods: These tests amplify nucleic acids at a single, constant temperature, simplifying instrumentation and potentially enabling point-of-care use. Common isothermal techniques include [24] [25] [23]:
- Loop-mediated isothermal amplification (LAMP)
- Nickin endonuclease amplification reaction (NEAR)
- Transcription-mediated amplification (TMA)
- Helicase-dependent amplification (HDA)
- Recombinase polymerase amplification (RPA)
- Strand displacement amplification (SDA)
Comparative Analysis of Key NAAT Platforms
The table below summarizes the fundamental operational differences between a classic PCR method and a representative isothermal method, LAMP, which is increasingly prominent in molecular diagnostics [25].
Table 1: Comparison of Standard PCR and LAMP Characteristics
| Property | PCR | LAMP |
|---|---|---|
| Amplification Process | Cycles through three temperature steps (e.g., 95°C, ~60°C, 72°C) | Occurs at a constant temperature (60–65°C) |
| Denaturation | Achieved via high heat | Performed by strand-displacing polymerase |
| Equipment | Requires a thermocycler | Does not require a thermocycler; can use a water bath or heat block |
| Typical Reaction Time | At least 90 minutes to results | Often less than 30 minutes to results |
| Sensitivity | Can detect targets at nanogram levels | Can detect targets at femtogram levels |
| Result Visualization | Typically requires gel electrophoresis | Can be visualized via colorimetric change or turbidity |
Troubleshooting Guides and FAQs
This section addresses common experimental challenges encountered during NAAT development and validation, providing evidence-based solutions.
No or Weak Amplification
Table 2: Troubleshooting No or Weak Amplification
| Possible Cause | Recommended Solution |
|---|---|
| Insufficient Template | - Verify template quantity and quality; consider increasing input amount within the assay's validated range [26].- For low-abundance targets, increase PCR cycles up to 40 [27]. |
| PCR Inhibitors | - Dilute the template to reduce inhibitor concentration [27].- Purify the template using a dedicated clean-up kit [27].- Use polymerases known for high inhibitor tolerance, such as Bst for LAMP or Terra PCR Direct for PCR [25] [27]. |
| Suboptimal Reaction Conditions | - For PCR: Lower the annealing temperature in 2°C increments, increase extension time, or optimize Mg2+ concentration [26] [27].- Ensure all reaction components are thoroughly mixed [26]. |
| Enzyme or Reagent Issues | - Include a positive control to confirm reagent functionality [27].- Ensure the DNA polymerase is appropriate for the application (e.g., proofreading for high fidelity, strand-displacing for LAMP) [26] [25]. |
Nonspecific Amplification or High Background
- Problematic Primer Design: Use BLAST alignment to check for off-target complementarity, especially at the 3' ends. Redesign primers if necessary, ensuring they lack complementary sequences or consecutive G/C nucleotides at the 3' end to prevent primer-dimer formation [27].
- Non-Stringent Reaction Conditions:
- For PCR: Increase the annealing temperature stepwise, use a "touchdown PCR" protocol, or reduce the number of cycles [26] [27].
- For all NAATs: Reduce the amount of template or primer concentration if they are in excess [26] [27].
- Use Hot-Start Enzymes: Employ hot-start DNA polymerases that remain inactive until a high-temperature activation step, which suppresses nonspecific amplification initiated during reaction setup [26].
- SYBR Green Artifacts in qPCR: If using SYBR Green, check the melt curve for multiple peaks, which can indicate primer-dimers or nonspecific products. Optimize primer design and reaction conditions to ensure specificity [28].
False Positives and Contamination Control
Contamination is a critical concern in high-sensitivity NAATs, especially in a validation laboratory setting.
- Sources of Contamination: The most common sources are amplicons from previous reactions (carryover contamination), cloned DNA, sample-to-sample cross-contamination, and exogenous DNA in the laboratory environment or reagents [27].
- Prevention Strategies:
- Physical Separation: Establish physically separated "pre-PCR" and "post-PCR" areas. Equipment, pipettes, lab coats, and reagents dedicated to the pre-PCR area should never enter the post-PCR area [27].
- Workflow and Reagents: Use aerosol-filter pipette tips. Aliquot reagents into small portions for single-use and store them separately from DNA samples and amplicons [27].
- No-Template Controls: Always run a control reaction that omits template DNA to monitor for contamination [27].
- Decontamination Protocols: If contamination occurs, decontaminate workstations and pipettes with 10% bleach and/or UV irradiation. UV light can cross-link and damage residual DNA, but exposure time should be limited for reagents or equipment that may be sensitive to UV degradation [27].
Experimental Protocols for Validation
Protocol: Real-Time LAMP Assay for Tuberculosis Detection
A 2025 validation study detailed a real-time LAMP (rt-LAMP) assay for pulmonary tuberculosis, providing a model protocol for isothermal test development [29].
- Primer Design: Primers were designed targeting the mpt64 gene using LAMP designer software. The final primer set included Forward and Backward Inner Primers (FIP, BIP), Outer Primers (F3, B3), and Loop Primers (LF, LB) [29].
- Reaction Setup:
- Master Mix (per reaction): 1.6 µM FIP/BIP, 0.4 µM F3/B3, 0.2 µM LF/LB, 1X WarmStart LAMP Master Mix, 2 µM SYTO 16 fluorescent dye, nuclease-free water to volume.
- Procedure: 20 µL of master mix was aliquoted, and 5 µL of extracted DNA template was added. The reaction was run at 65°C for 40 minutes in a real-time PCR machine configured for isothermal fluorescence reading [29].
- Limit of Detection (LOD) Determination:
- A recombinant plasmid containing the mpt64 target was created and serially diluted.
- The DNA copy number per µL was calculated using the formula:
Number of copies/µl = (M x 6.022x10^23 x 10^-9) / (n x 660)where M is the DNA concentration in ng/µl and n is the plasmid length in base pairs. - The LOD was determined to be 10 copies/µl by testing each dilution in triplicate [29].
- Clinical Performance:
- The assay was validated on 350 patient samples against a microbiological reference standard (MGIT culture).
- Sensitivity: 89.36% (95% CI: 76.9–96.45%)
- Specificity: 94.06% (95% CI: 90.77–96.44%) [29]
Workflow Diagram: NAAT Experimental and Validation Pathway
The following diagram illustrates a generalized workflow for the development and validation of a NAAT, from sample processing to result interpretation, incorporating key quality control steps.
The Scientist's Toolkit: Key Research Reagents
Successful development and troubleshooting of NAATs depend on the selection of appropriate reagents. The table below lists essential materials and their functions.
Table 3: Essential Reagents for NAAT Development
| Reagent / Material | Function / Explanation |
|---|---|
| Bst DNA Polymerase | The primary enzyme for LAMP. Derived from Bacillus stearothermophilus, it has strong strand-displacement activity for isothermal amplification [25]. |
| Hot-Start DNA Polymerase | A modified enzyme for PCR that is inactive at room temperature, preventing nonspecific amplification and primer-dimer formation during reaction setup [26]. |
| dNTPs | Deoxynucleotide triphosphates (dATP, dCTP, dGTP, dTTP) are the building blocks for DNA synthesis. They must be provided in balanced, equimolar concentrations to prevent misincorporation [26]. |
| Magnesium Ions (Mg²⁺) | A critical cofactor for DNA polymerases. Its concentration must be optimized, as it influences enzyme activity, primer annealing, and amplicon specificity [26]. |
| Primers | Short, single-stranded DNA sequences designed to be complementary to the target pathogen's genome. Careful design is paramount for specificity and efficiency [26]. |
| Fluorescent Dyes (e.g., SYTO 16, SYBR Green) | Intercalating dyes that bind double-stranded DNA, allowing for real-time monitoring of amplification in platforms like qPCR and rt-LAMP [28] [29]. |
| Nuclease-Free Water | A pure, contaminant-free solvent used to prepare reaction mixes, ensuring no enzymatic degradation of nucleic acids or primers occurs. |
| Positive Control | A well-characterized sample containing the target sequence, used to verify that the entire testing process is functioning correctly [27]. |
Sample Preparation and Enrichment Protocols for Metagenomic Sequencing
Metagenomic next-generation sequencing (mNGS) offers a comprehensive, unbiased method for detecting nearly all potential pathogens—viruses, bacteria, fungi, and parasites—in a single assay, making it particularly valuable for diagnosing infections with non-specific clinical presentations such as meningitis, encephalitis, and respiratory syndromes [30]. The reliability of these results is fundamentally dependent on robust sample preparation and enrichment protocols, which are crucial for enhancing pathogen nucleic acid recovery and minimizing background host and non-target material [31] [32] [33].
The following sections detail the foundational and advanced methodologies, provide a visual workflow, and address common troubleshooting challenges encountered during library preparation.
Core Sample Preparation & Enrichment Methodologies
Foundational mNGS Workflow for CSF
This protocol, validated in a CLIA-certified laboratory for diagnosing neurological infections, outlines the core steps for cerebrospinal fluid (CSF) processing [30].
Experimental Protocol [30]:
- Microbial Enrichment: Begin with sample processing to enrich for microbial content.
- Nucleic Acid Extraction: Extract total nucleic acids from the sample.
- Library Construction:
- Use the Nextera library construction method.
- Perform two rounds of PCR amplification.
- Library Pooling: Pool libraries in equimolar concentrations.
- Sequencing: Sequence on an Illumina instrument, targeting 5 to 20 million sequences per library.
- Bioinformatics Analysis: Analyze raw sequence data using the SURPI+ pipeline, which includes:
- Filtering algorithms to confirm pathogen hits.
- Taxonomic classification for species-level identification.
- A graphical user interface (SURPIviz) for result review and reporting.
Performance Metrics: This assay demonstrated a 92% sensitivity and 96% specificity in identifying causative pathogens from CSF samples when compared to conventional microbiological testing [30].
Advanced Enrichment via Probe Capture for Respiratory Pathogens
Probe-based enrichment significantly improves sensitivity, especially for viruses, by selectively isolating pathogen-derived nucleic acids. The following protocol was benchmarked using 40 clinical nasopharyngeal swabs [31].
Experimental Protocol [31]:
- Sample Lysis: Use chaotropic salt-based buffer combined with bead beating.
- Nucleic Acid Extraction: Perform a magnetic bead-based semi-automatic extraction of total nucleic acids (TNA).
- Library Preparation: Generate Illumina sequencing libraries from DNA or RNA.
- Probe Capture Enrichment: Subject libraries to in-solution capture enrichment using a panel of biotinylated tiling RNA probes (120nt) targeting 76 respiratory pathogens.
- Sequencing: Sequence enriched libraries on Illumina or Nanopore platforms.
Performance Metrics [31]:
- The overall detection rate increased from 73% to 85% after probe capture with Illumina sequencing.
- Probe capture boosted unique pathogen reads by 34.6-fold for DNA sequencing and 37.8-fold for cDNA sequencing.
- This method significantly improved genome coverage, particularly for viruses.
Optimized Viral Metagenomics Protocol for Clinical Samples
This protocol was optimized for various clinical samples (plasma, urine, throat swabs) and uses a combination of physical and enzymatic methods to enrich for viral particles [32] [33].
Experimental Protocol [33]:
- Sample Pre-processing: Centrifuge samples at 2,000 RPM for 10 minutes.
- Filtration: Pass the supernatant through a 0.45-μm PES filter to remove cells and larger debris.
- Nuclease Treatment (Crucial Step):
- Treat the filtrate with a nuclease mix (DNase and RNase A) for 1 hour at 37°C.
- This step degrades free-floating host and bacterial nucleic acids, while capsid-protected viral nucleic acids remain intact.
- Remove nuclease activity by protease treatment.
- Nucleic Acid Extraction: Use commercial kits (e.g., QIAamp Viral RNA Mini Kit) with high starting volumes (500-1000 μl) eluted into a small volume (25 μl) to maximize concentration.
- Unbiased Amplification: Perform reverse transcription and random amplification of RNA and DNA in separate reactions to ensure complete genome coverage.
Workflow Visualization
The following diagram synthesizes the key steps from the cited protocols into a generalized, optimized workflow for metagenomic sequencing of clinical samples, highlighting critical enrichment and preparation stages.
Troubleshooting Common Library Preparation Issues
Common problems during NGS library preparation can derail an entire metagenomic sequencing run. The table below outlines frequent issues, their root causes, and proven corrective actions [34].
| Problem Category | Typical Failure Signals | Common Root Causes | Corrective Actions |
|---|---|---|---|
| Sample Input / Quality | Low yield; smear on electropherogram; low complexity [34]. | Degraded DNA/RNA; contaminants (phenol, salts); inaccurate quantification [34]. | Re-purify input; use fluorometric quantification (Qubit); check purity ratios (260/280 ~1.8) [34]. |
| Fragmentation & Ligation | Unexpected fragment size; sharp ~70-90 bp peak (adapter dimers) [34]. | Over-/under-shearing; improper adapter-to-insert molar ratio; poor ligase performance [34]. | Optimize fragmentation parameters; titrate adapter ratios; ensure fresh enzymes and buffers [34]. |
| Amplification & PCR | Overamplification artifacts; high duplicate rate; bias [34]. | Too many PCR cycles; carryover enzyme inhibitors; primer exhaustion [34]. | Reduce PCR cycles; re-purify sample to remove inhibitors; optimize primer and polymerase conditions [34]. |
| Purification & Cleanup | High adapter-dimer signal; sample loss; carryover of salts [34]. | Incorrect bead-to-sample ratio; over-dried beads; pipetting errors [34]. | Precisely follow cleanup protocols; avoid over-drying beads; implement technician checklists [34]. |
Research Reagent Solutions
This table lists key reagents and kits used in the validated protocols, providing researchers with essential materials for establishing these methods.
| Reagent / Kit Name | Function / Application | Key Characteristics / Targets |
|---|---|---|
| Nextera / Illumina DNA Prep [30] [35] | Library construction for NGS. | Tagmentation-based library prep; widely considered a "gold-standard" for metagenomics [35]. |
| Biotinylated RNA Probe Panels [31] | Targeted enrichment of pathogen sequences. | Tiling probes (120nt) targeting 76 respiratory pathogens; boosts sensitivity and read depth [31]. |
| QIAamp Viral RNA Mini Kit [33] | Nucleic acid extraction from clinical samples. | Optimized for viral nucleic acid recovery from plasma, swabs, and urine [33]. |
| SURPI+ Software Pipeline [30] | Bioinformatic analysis of mNGS data. | Rapid pathogen identification and taxonomic classification; includes graphical interface for clinical review [30]. |
Frequently Asked Questions (FAQs)
Q1: How can I improve the detection of viruses with low abundance in respiratory samples? A1: Probe-based enrichment is highly effective. Using a panel targeting 76 respiratory pathogens has been shown to increase the detection rate from 73% to 85% and boost unique viral reads by nearly 40-fold, significantly improving sensitivity for pathogens like Influenza B and Rhinovirus [31].
Q2: What is the critical step in preparing plasma samples for viral metagenomics? A2: Nuclease treatment is crucial. After filtration, treating the sample with DNase and RNase degrades unprotected host and bacterial nucleic acids. This enriches for capsid-protected viral genomes, dramatically improving the signal-to-noise ratio in subsequent sequencing [33].
Q3: My NGS libraries have a very low yield. What are the most likely causes? A3: Low yield most commonly stems from (1) poor input quality/degradation, (2) contaminants inhibiting enzymes, or (3) inaccurate quantification leading to suboptimal reaction conditions. Always use fluorometric quantification (e.g., Qubit) over UV absorbance and re-purify samples if contaminants are suspected [34].
Q4: How do I set thresholds for reporting a pathogen in a clinical mNGS assay to avoid false positives? A4: Establishing rigorous thresholds is key. For bacteria, fungi, and parasites, using a normalized metric like RPM-r (Reads per Million in sample / RPM in no-template control) can minimize false positives from background contamination. An RPM-r threshold of 10 was validated to maximize accuracy. For viruses, requiring reads from ≥3 distinct genomic regions adds stringency [30].
Validation Frameworks for Antigen-Detection Rapid Diagnostic Tests (RDTs)
Core Validation Concepts for Laboratory Professionals
The reliability of Antigen-Detection Rapid Diagnostic Tests (RDTs) hinges on a rigorous validation framework, which distinguishes between verification (confirming a commercial test's stated performance) and validation (establishing performance for laboratory-developed tests or novel applications) [36] [37]. For CE/IVD-labeled tests, laboratories must perform verification to confirm precision under local conditions [36]. In contrast, "home-brewed" or extensively modified tests require full validation to establish their sensitivity, specificity, precision, and linearity [36]. This process is foundational for integrating RDTs into clinical virology and public health practice, ensuring that tests perform as expected in their intended operational context.
A unified framework for diagnostic test evaluation during emerging outbreaks emphasizes the critical feedback loop between test accuracy evaluation, public health modeling, and intervention impact [38]. This approach is essential for responding to epidemics, where test deployment is urgent and pathogen characteristics may evolve rapidly.
Key Differences: Verification vs. Validation
Table: Comparison of Verification and Validation Requirements
| Aspect | Verification (CE/IVD-labeled Tests) | Validation (Home-brewed Tests) |
|---|---|---|
| Primary Goal | Confirm manufacturer's stated performance claims [36] | Establish complete performance characteristics [36] |
| Sensitivity Assessment | Typically not required if manufacturer's claims are verified [36] | Required using 10 positive and 10 low-positive specimens [36] |
| Specificity Assessment | Typically not required if manufacturer's claims are verified [36] | Required using 20 negative but potentially cross-reactive specimens [36] |
| Precision Evaluation | Required (intra-assay precision with 3 replicates of 1 positive and 1 low-positive sample) [36] | Required [36] |
| Linearity Evaluation | Required for quantitative NAT systems [36] | Required for quantitative systems [36] |
Diagram: Diagnostic Test Implementation Decision Pathway
Troubleshooting Guides & FAQs
Common Technical Issues and Resolutions
Q1: Our laboratory is encountering inconsistent results between different lots of the same RDT brand. What is the systematic approach to identify the root cause?
A: Inconsistent inter-lot performance suggests potential issues with manufacturing quality control or component stability. Implement this investigative protocol:
- Documentation Review: Verify that all lots were stored under identical conditions (temperature, humidity) and are within their expiration dates [39].
- Controlled Re-testing: Select a panel of well-characterized specimens (positive, negative, and low-positive). Test these specimens across the different lots in parallel, using the same operator, equipment, and reagents to control for variables [36].
- Component Analysis: Systematically assess all test components, not just the cassette. Critical findings from malaria RDT evaluations highlight that defects in accessories are a common source of error [40]. Specifically check:
- Buffer Vials: Visually inspect for uniformity and measure the volume in multiple vials from each lot. Variations in buffer volume or concentration can dramatically alter test performance [40].
- Blood Transfer Devices (BTDs): Evaluate the mean blood volume transferred by BTDs from each lot. Substandard BTDs can deliver non-uniform blood volumes, leading to false negatives (insufficient blood) or illegible results (excess blood) [40].
- Escalation: Report findings to the manufacturer. If defects are confirmed, request replacement of defective lots. The World Health Organization (WHO) has issued notices regarding variable buffer volumes, recommending against procurement until defects are resolved [40].
Q2: We observe faint test lines at low antigen concentrations that are difficult for personnel to interpret consistently. How can we objectively define the limit of detection (LoD) and reduce subjectivity?
A: Subjective interpretation of faint lines is a major source of inter-operator variability. Implement a quantitative, laboratory-anchored framework to define the LoD objectively [41].
- Digital Signal Capture: Use a standardized method (e.g., cell phone camera with fixed settings) to capture test strip images [41].
- Signal Intensity Quantification: Process images using software to calculate the normalized signal intensity of the test line against the background. This converts visual band intensity into a continuous, objective variable [41].
- Modeling Dose-Response: Fit the normalized intensity data against antigen concentration using a model (e.g., Langmuir-Freundlich adsorption model:
I = kC^b / (1 + kC^b), whereIis intensity andCis concentration) to characterize the test's signal response [41]. - Establish Probabilistic LoD: Incorporate the statistical distribution of your user population's visual acuity. The LoD should be defined as the antigen concentration at which a predefined percentage of trained users can reliably detect the test line, bridging laboratory data with real-world use [41].
Q3: What are the primary causes of false-negative results in antigen RDTs, and how can our validation protocol address them?
A: False negatives primarily stem from antigen levels falling below the test's detection threshold. A robust validation protocol must account for this.
- Low Parasitemia/Viral Load: Sensitivity decreases significantly when pathogen concentration is low [42]. This is a fundamental limitation of RDTs.
- Target Genetic Variability: For tests targeting specific proteins (e.g., HRP2 for malaria), deletions in the corresponding gene can lead to false negatives [42]. This is a well-documented issue with Plasmodium falciparum in certain regions.
- Prozone Effect: Very high antigen concentrations can sometimes saturate the antibodies, leading to a false negative or a faint line [42]. This is less common but should be considered.
- Inadequate Sample Collection: Insufficient sample material is a frequent user error [39].
- Validation Solution: During validation, ensure your positive sample panel includes specimens with low antigen concentrations (e.g., high qRT-PCR cycle thresholds for SARS-CoV-2) to empirically determine the test's clinical sensitivity curve and its lower limit of reliable detection [36] [41].
Q4: Our point-of-care antigen test for SARS-CoV-2 shows good sensitivity in lab evaluations but poorer performance in real-world deployment. What factors should we re-examine in our validation framework?
A: This discrepancy highlights the difference between ideal laboratory conditions and real-world application. Expand your validation framework to include:
- User Usability Studies: Evaluate performance with intended users (e.g., healthcare workers, self-testing public) rather than only trained laboratory personnel. The "naked-eye limit of detection" varies across the user population and must be characterized [41].
- Environmental Robustness Testing: Validate test performance under various environmental conditions (temperature, humidity) that mimic storage and use settings in homes, clinics, or community centers [40] [39].
- Specimen Type and Quality: Test performance using specimens collected in real-world settings, which may differ in quality from those collected by highly trained phlebotomists or clinicians [36].
- Modeling Real-World Performance: Use a Bayesian predictive model to compose the laboratory-derived signal-to-concentration model, the user LoD distribution, and a viral-load calibration (e.g., from qRT-PCR Ct values). This generates a predicted Positive Percent Agreement (PPA) curve as a function of viral load, which can be compared against real-world outcomes [41].
Advanced Technical Troubleshooting
Table: Advanced Troubleshooting for Research & Development
| Problem | Investigation Methodology | Potential Resolution |
|---|---|---|
| High Background Noise | Inspect test strip for red cell adherence; review conjugate pad composition and sample buffer lytic agents [42]. | Optimize buffer formulations; include surfactants to reduce non-specific binding. |
| Poor Line Intensity | Characterize kinetic curve of signal development; test antibody pair affinity and concentration [41]. | Source higher-affinity antibody pairs; increase test line antibody concentration. |
| Low Specificity/Cross-Reactivity | Test against a panel of potentially cross-reactive organisms or antigens [36]. | Identify and replace non-specific antibodies; add blocking agents to the buffer. |
Experimental Protocols for Key Validation Experiments
Protocol for Determining Limit of Detection (LoD)
Objective: To empirically determine the lowest concentration of target antigen that the RDT can reliably detect.
Materials:
- Recombinant target protein or inactivated virus with known concentration.
- Negative clinical matrix (e.g., nasal swab medium, blood).
- Pipettes and serial dilution equipment.
- Timers.
Methodology:
- Prepare Dilution Series: Perform a log-scale serial dilution of the antigen in the negative clinical matrix, covering a range from above the expected LoD to below it.
- Testing: Test each dilution level multiple times (e.g., n=20 replicates) as per the RDT's Instructions for Use (IFU) [36].
- Data Analysis: Calculate the proportion of positive results at each concentration. The LoD is defined as the lowest concentration at which ≥95% of replicates test positive [36] [41].
- Advanced Quantification (Recommended): For a more rigorous analysis, use digital imaging to measure normalized test line intensity. Model the dose-response relationship using the Langmuir-Freundlich isotherm to understand the dynamic range and precisely interpolate the LoD [41].
Protocol for Assessing Precision (Repeatability)
Objective: To measure the variation in results when the same sample is tested multiple times under identical, within-run conditions.
Materials:
- One positive sample with a high antigen concentration.
- One low-positive sample near the LoD.
- Multiple test kits from the same lot.
Methodology:
- Sample Preparation: Aliquot the two characterized samples.
- Intra-assay Precision: Test each sample (high positive and low positive) at least three times within a single run [36].
- Analysis: For qualitative tests, all results must be concordant (e.g., all positive). For quantitative tests (if signal is measured), calculate the coefficient of variation (CV) for the signal intensities. A CV of <10-15% is generally acceptable, though manufacturer claims should be verified.
Protocol for Specificity and Cross-Reactivity Testing
Objective: To confirm the test does not generate false-positive results with samples containing potentially cross-reacting organisms or interfering substances.
Materials:
- A panel of 20 negative clinical specimens [36].
- Cultured isolates or recombinant proteins of related pathogens (e.g., other coronaviruses for SARS-CoV-2 tests, or other Plasmodium species for malaria tests) [42].
Methodology:
- Panel Testing: Test the panel of negative specimens. The test should demonstrate ≥99% specificity with this panel [36].
- Cross-Reactivity Challenge: Test the RDT with high concentrations of the related pathogens. A true-specific test should yield a negative result.
- Genetic Diversity: For viruses with high mutation rates, check primer and probe sequences against genomic databases to ensure they target conserved regions, minimizing the risk of false negatives due to genetic drift [36].
Diagram: Quantitative RDT Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
A standardized set of reagents and materials is critical for reproducible RDT validation and development.
Table: Key Research Reagent Solutions for RDT Development
| Reagent/Material | Function & Importance in Validation/Development |
|---|---|
| Recombinant Antigen Proteins | Used for calibration curves, LoD determination, and linearity studies. Provides a standardized, safe material for initial assay characterization [41]. |
| Inactivated Virus or Cultured Parasites | Essential for assessing test performance with intact pathogen structures, which may better mimic clinical samples than recombinant proteins alone [41]. |
| Clinical Specimen Panels | Well-characterized, banked clinical samples (positive, negative, low-positive) are the gold standard for determining clinical sensitivity and specificity [36]. |
| Monoclonal/Polyclonal Antibodies | The core capture and detection reagents. Affinity and specificity of antibody pairs directly determine the sensitivity and specificity of the RDT [42]. |
| Lateral Flow Strip Components (Nitrocellulose membrane, conjugate pad, sample pad, absorbent pad) | The physical platform for the assay. Membrane pore size, flow rate, and pad compositions must be optimized for consistent performance and minimal background [42]. |
| Specimen Collection Swabs & Buffer | The initial sample collection and preservation. Swab material and buffer composition can impact antigen stability and release, critically influencing test accuracy [40] [39]. |
Leveraging AI and Federated Learning for Enhanced Diagnostic Accuracy and Data Privacy
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center is designed for researchers and scientists developing AI-driven diagnostic tools for viral diseases. The guidance below addresses common technical challenges within a federated learning framework, contextualized by the requirements of rigorous diagnostic test verification and validation procedures [9].
Frequently Asked Questions (FAQs)
FAQ 1: How can we ensure our federated learning model generalizes well across different hospitals with varied data types?
A primary challenge in federated learning is data heterogeneity. To ensure robust generalization:
- Utilize Synthetic Data: Employ Generative Adversarial Networks (GANs) to create synthetic, high-quality medical datasets. This supplements limited or imbalanced real-world data from individual sites, bolstering model resilience and reducing overfitting [43].
- Implement Advanced Architectures: Leverage modern model architectures like Vision Transformers for image-based diagnosis, which can capture complex patterns more effectively than conventional CNNs, or MLP-Mixer for processing image patches [43] [44].
- Standardize Preprocessing: While data remains decentralized, agree on common pre-processing steps (e.g., image normalization, sequence alignment standards) with all participating sites to minimize technical variation.
FAQ 2: Our model performs well locally but the global federated model is inaccurate. What could be the cause?
This is a classic sign of client drift, often due to non-IID (Independently and Identically Distributed) data across clients [45]. Solutions include:
- Algorithm Selection: Use aggregation algorithms designed for heterogeneity. While Federated Averaging (FedAvg) is common, consider alternatives like FedProx (addresses system and statistical heterogeneity) or SCAFFOLD (uses control variates to correct client drift) [46].
- Check Data Distribution: Use tools to analyze the data distribution across participating sites without sharing raw data. This can help diagnose severe imbalances.
- Stratified Sampling: If possible, implement stratified sampling on the client side before local training to ensure each local dataset better represents the overall population distribution.
FAQ 3: How can we make the predictions of our "black-box" AI model trustworthy for clinicians?
For clinical adoption, model interpretability is crucial. Integrate Explainable AI (XAI) techniques:
- Post-hoc Explanations: Apply methods like LIME (Local Interpretable Model-agnostic Explanations) or SHAP (SHapley Additive exPlanations) to generate feature importance maps (e.g., highlighting regions in a chest X-ray that contributed most to a COVID-19 diagnosis) [43].
- Incorporate Transparency: Choose model architectures that offer a degree of inherent interpretability where possible. The use of XAI fosters transparency, making AI decisions clear and reliable for healthcare practitioners [43].
FAQ 4: We need to incorporate new, incrementally arriving data from ongoing surveillance. How can we do this without retraining from scratch?
This challenge requires combining federated learning with continual learning.
- Cross-Paradigm Fusion: Implement a framework that integrates both methodologies. Federated learning preserves privacy across institutions, while continual learning allows the model to learn from new data (new viral strains, new imaging protocols) without catastrophically forgetting previously acquired knowledge [44].
- Techniques like LwF: Algorithms such as Learning without Forgetting (LwF) can be integrated into the federated learning process. This approach uses knowledge distillation to retain performance on old tasks while learning new ones [44].
Troubleshooting Guides
Problem: Model Convergence is Slow or Unstable During Federated Training
- Check 1: Local Learning Rates. Excessively high local learning rates can cause divergence. Reduce the local learning rate and observe the global model's stability across communication rounds [46].
- Check 2: Client Participation. If only a small fraction of clients participates in each round, convergence can be slow and noisy. Increase the number of clients selected per round, if computationally feasible.
- Check 3: Data Quality on Clients. Internally validate data labels and quality on local clients. Inconsistent labeling between sites is a major source of instability. The use of a third-party test verification hub, like the ACME POCT in the RADx program, can provide a benchmark for model performance [9].
Problem: Data Privacy Concerns Remain Despite Using Federated Learning
- Check 1: Secure Aggregation. Ensure that the model update aggregation process on the central server uses a secure multi-party computation protocol. This prevents the server from identifying the source of any individual update.
- Check 2: Differential Privacy. Add calibrated noise to the model updates (gradients) before they are sent from the local client to the server. This provides a mathematical guarantee of privacy, protecting against certain types of inference attacks [46].
- Check 3: Encrypted Communication. Verify that all communication channels between clients and the central server are encrypted using standard protocols like TLS/SSL.
Problem: Performance Degradation When Identifying New or Emerging Pathogens
- Check 1: Feature Selection. For genomic pathogen identification, ensure your model uses an automatic, effective feature selection mechanism tailored to recognize novel patterns in genome sequences, rather than relying solely on known markers [46].
- Check 2: Model Architecture for Genomics. Use a dedicated deep federated learning model for genome sequences. For example, a DFL-based LeNet model has shown 99.12% accuracy in identifying new infections from genomic data while preserving privacy [46].
- Check 3: Out-of-Distribution Detection. Implement modules that can detect when an input sample (e.g., a genome sequence or medical image) is too different from the training data, allowing the model to return "uncertain" as a safety feature, similar to the InfEHR system [47].
The table below summarizes key performance metrics from recent studies applying AI and FL to infectious disease diagnostics.
Table 1: Performance Metrics of AI/Federated Learning Models in Infectious Disease Diagnostics
| Application / Model | Accuracy | Sensitivity/Recall | Specificity/Precision | Key Metric | Citation |
|---|---|---|---|---|---|
| DFL-LeNet for New Infection ID (Genomes) | 99.12% | Recall: 98.04% | Precision: 98.23% | F1-Score: 96.24% | [46] |
| Federated COVID-19 Screening (CXR Images) | Up to 99.6% | N/A | N/A | Global Accuracy | [48] |
| MLP-Mixer + LwF (Multi-class Thoracic Infection) | 54.34% | N/A | N/A | Average Accuracy | [44] |
| InfEHR for Neonatal Sepsis Prediction (EHR) | N/A | N/A | N/A | 12-16x better ID than current methods | [47] |
| Federated Model (FedCNNAvg) for Malaria | 98.92% | N/A | N/A | Accuracy | [44] |
Detailed Experimental Protocols
Protocol 1: Developing a Federated Learning Model for Medical Image Analysis
This protocol outlines the steps for training a model to classify chest X-rays for viral pneumonia (e.g., COVID-19) using a federated setup [43] [48].
System Initialization & Client Selection:
- The central server initializes a global model (e.g., a Vision Transformer or pre-trained CNN).
- Define learning parameters: number of communication rounds (e.g., 100), batch size, loss function (e.g., cross-entropy), and learning rate.
- Select a subset of available clinical institutions (clients) to participate in each training round.
Local Model Distribution:
- The central server sends the current global model weights to each participating client.
Local Model Training:
- On each client's server (e.g., a hospital's secure server), the model is trained on the local private dataset of chest X-rays.
- Data Augmentation: To prevent overfitting on limited local data, apply a pipeline of transformations (rotation, scaling, flipping) to artificially expand the dataset [43].
- Perform several epochs of stochastic gradient descent to minimize the loss function, resulting in updated local model weights.
Model Update Transmission:
- Each client sends its updated model weights (or gradients) back to the central server. Crucially, the raw image data never leaves the local server.
Secure Model Aggregation:
- The central server aggregates the local updates. The most common algorithm is Federated Averaging (FedAvg), which computes a weighted average of the model updates based on the size of each client's dataset [46].
w_global = Σ (n_k / n) * w_kwheren_kis the number of samples on clientk,nis the total samples, andw_kis the model from clientk.
Model Evaluation & Iteration:
- The updated global model is evaluated on a held-out validation set.
- Steps 2-5 are repeated for multiple communication rounds until the model converges.
Protocol 2: Identifying New Infections from Genome Sequences Using DFL
This protocol describes a privacy-preserving method for identifying novel pathogens from genomic data [46].
Data Preprocessing & Feature Selection:
- Collect genome sequences (GSs) from known viruses and any emerging strains.
- Convert raw DNA/RNA sequences into a numerical representation suitable for deep learning (e.g., k-mer frequency vectors, one-hot encoding).
- Implement an automatic feature selection process to extract features most relevant for distinguishing new infections.
Model Architecture Definition:
- Design a Deep Federated Learning (DFL) model. The referenced study uses a LeNet-based architecture adapted for sequence data [46].
Federated Training Loop:
- IID Assessment: Assess if the genomic data is Independently and Identically Distributed (IID) across clients. Performance can be evaluated under both IID and non-IID distributions [46].
- Follow the core FL steps from Protocol 1: distribute the DFL-LeNet model, train locally on genomic data, and aggregate updates (e.g., via FedAvg) on a central server.
Model Evaluation & Dependability Analysis:
- Evaluate the final global model on a test set of known and novel sequences.
- Report standard metrics: accuracy, precision, recall, F1-score, and AUC-ROC.
- Perform a computational complexity and dependability analysis to ensure the model is robust and suitable for deployment [46].
Workflow and System Diagrams
Federated Learning Architecture
Integrated AI Diagnostic Framework
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for AI-Driven Infectious Disease Research
| Resource / Tool | Type | Primary Function in Research | Example/Reference |
|---|---|---|---|
| Public Genomic & Imaging Datasets | Data | Training and validation of AI models; foundational for robust and generalizable model development. | COVID-XRAY, COVID-CT datasets [44]; NIH Chest X-Ray dataset [44] |
| High-Throughput Sequencing (HTS) Data | Data | Enables AI-driven pathogen identification, variant monitoring, and transmission tracing. | SARS-CoV-2 genomic sequences [49] |
| Federated Learning (FL) Framework | Software | Enables collaborative model training across institutions without sharing raw data, ensuring privacy. | Frameworks using FedAvg, FedProx [46] |
| Generative Adversarial Network (GAN) | Algorithm/Model | Generates synthetic medical data to augment limited datasets, reducing overfitting and improving model robustness [43]. | Used in integrated frameworks for data augmentation [43] |
| Explainable AI (XAI) Tools | Software | Provides interpretability for AI decisions, crucial for clinical trust and validation (e.g., generates saliency maps). | LIME, SHAP [43] |
| Deep Learning Model Architectures | Model | Core engines for pattern recognition in complex data like images and sequences. | Vision Transformers, MLP-Mixer [43] [44], DFL-LeNet [46] |
Overcoming Common Challenges in Test Validation and Implementation
Frequently Asked Questions
Q1: What are the most critical pre-analytical factors that can invalidate viral diagnostic test results? The most critical factors are sample quality, proper collection technique, and correct handling immediately after collection. Specifically, hemolysis, improper sample volume (under-filling tubes), and the use of wrong collection containers account for a majority of pre-analytical errors [50]. For molecular diagnostics, delays in processing that lead to nucleic acid degradation are particularly detrimental [51].
Q2: How does tube under-filling specifically affect coagulation tests like PT/APTT? Under-filling a citrate tube disrupts the critical blood-to-anticoagulant ratio (typically 9:1). An excess of anticoagulant causes over-citration, leading to only partial re-calcification during testing and resulting in artificially prolonged clotting times. This can be misinterpreted as a coagulation disorder [52].
Q3: Our study involves patients with high hematocrits. How do we adjust for this in coagulation testing?
When a patient's hematocrit is elevated (e.g., >0.55 or 55%), the plasma volume in the sample is reduced. To maintain the correct anticoagulant-to-plasma ratio, the volume of trisodium citrate anticoagulant must be decreased. You can calculate the required volume using the following formula [52]:
C (ml) = 1.85 x 10-3 x (100 - Hct (%)) x V (ml)
Where C is the volume of 3.2% Trisodium citrate, Hct is the patient's hematocrit percentage, and V is the volume of whole blood in the tube.
Q4: What is the maximum recommended delay for processing samples before viral load testing? While stability is analyte-dependent, delays of over 4 hours between collection and processing can significantly affect the results of many laboratory tests [52]. For viral load testing, which relies on intact nucleic acids, it is crucial to follow manufacturer-specific instructions. Best practice is to process samples as soon as possible, and to separate plasma from cells promptly if any delay is anticipated to prevent analyte degradation [53] [51].
Q5: Why is a serum potassium result sometimes drastically different from a whole blood potassium result? This discrepancy is a classic pre-analytical issue. Serum is obtained after blood has clotted. During clotting, platelets can rupture and release their intracellular potassium. If a patient has a high platelet count (thrombocythemia), this release can cause pseudohyperkalemia (falsely high potassium) in the serum, while the whole blood potassium value reflects the true, in-vivo level [54].
Troubleshooting Common Pre-Analytical Problems
| Problem | Potential Causes | Corrective & Preventive Actions |
|---|---|---|
| Hemolyzed Sample [54] [50] | Difficult venipuncture, forced transport through narrow-gauge needles, improper handling or vigorous mixing [53]. | Ensure clean venipuncture technique. Avoid forceful expulsion. Mix tubes by gentle inversion. |
| Lipemic Sample [50] | Non-fasting patient, recent heavy meal, or underlying metabolic disorder. | Ensure patient fasting for 8-12 hours as required [50]. |
| Clotted Sample in Anticoagulant Tube [50] | Inadequate mixing after collection, delayed mixing, or under-filling of tube. | Invert tubes gently 5-10 times immediately after collection to ensure proper mixing with anticoagulant. |
| Insufficient Sample Volume [54] | Under-filling of tube, difficult venipuncture, or patient-related factors. | Draw the correct volume to maintain blood-to-anticoagulant ratio. Use pediatric tubes for volume-restricted patients. |
| Delayed Sample Processing [52] [51] | Logistical delays, improper scheduling, or long transport times. | Implement strict protocols for transport and processing. Centrifuge and separate plasma/serum promptly upon receipt. |
| Improper Sample Storage Temperature [51] | Lack of clear protocols or malfunctioning equipment. | Define and validate storage conditions for each analyte. Use calibrated freezers/fridges with continuous temperature monitoring. |
Pre-Analytical Variables and Their Impact
The table below summarizes key variables and their potential effects on test results, which is vital for test validation procedures [54] [52] [50].
| Variable Category | Specific Variable | Potential Effect on Diagnostic Results |
|---|---|---|
| Physiological | Recent Food Ingestion (Non-fasting) | ↑ Glucose, Triglycerides; Lipemia can cause optical interference [50] [53]. |
| Exercise | ↑ Muscle enzymes (CK, AST, LDH), Potassium [53]. | |
| Stress | ↑ Cortisol, White Blood Cell count [53]. | |
| Drugs/Biotin Supplements | Physiological or analytical interference with immunoassays (e.g., biotin) [50]. | |
| Sample Collection | Tourniquet Time & Fist Clenching | ↑ Potassium, Lactate; Hemoconcentration increases proteins and protein-bound analytes [54]. |
| Order of Draw | Contamination from anticoagulant (e.g., EDTA K₂-EDTA K₃) carryover [54]. | |
| Tube Under-filling (Citrate) | Artificially prolonged coagulation times [52]. | |
| Sample Handling & Transport | Delay in Processing | ↓ Glucose; ↑ Potassium, LDH; Degradation of labile analytes [53]. |
| Incomplete Mixing | Clotting in anticoagulant tubes; Inhomogeneous samples [50]. | |
| Improper Temperature | Degradation of proteins, nucleic acids, and labile hormones [51]. | |
| Repeated Freeze-Thaw Cycles | Degradation of analytes, loss of antibody activity in serological tests [51]. |
Experimental Protocols for Pre-Analytical Validation
A core part of diagnostic test verification is validating that your pre-analytical procedures do not compromise the sample. Below are key methodologies.
Protocol 1: Validating Sample Stability Over Time Objective: To determine the maximum allowable time between sample collection and analysis for key analytes without significant result alteration [51]. Methodology:
- Sample Collection: Collect a sufficient volume of blood from a minimum of 5 healthy volunteers into appropriate tubes.
- Aliquoting: Process (centrifuge and separate) the samples within 1 hour of collection. Create multiple identical aliquots of plasma/serum for each donor.
- Storage Conditions: Store the aliquots at the intended pre-analytical storage temperature (e.g., room temperature (20-25°C), refrigerated (4°C)).
- Time-Point Analysis: Analyze the aliquots in a single batch to avoid inter-assay variation. Use time points such as:
- Baseline (0 hours)
- 2 hours
- 4 hours
- 8 hours
- 24 hours
- Data Analysis: Calculate the mean and standard deviation for each analyte at each time point. A change of more than the defined allowable total error (based on biological variation goals) is considered significant.
Protocol 2: Investigating the Effect of Hematocrit on Coagulation Tests Objective: To confirm the need for anticoagulant volume adjustment in samples from subjects with high hematocrit [52]. Methodology:
- Sample Preparation: Obtain whole blood from donors. For in-vitro testing, the hematocrit can be artificially adjusted by adding or removing plasma.
- Tube Filling: Fill citrate tubes with blood at varying hematocrit levels (e.g., 0.40, 0.50, 0.60, 0.65). Ensure the tubes are filled to the correct nominal volume.
- Testing: Perform PT and APTT testing on all samples in duplicate.
- Data Analysis: Plot the PT/APTT results against the hematocrit value. A significant positive correlation (prolonging times with increasing Hct) indicates a strong interference, validating the need for the anticoagulant volume calculation provided in the FAQs.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Pre-Analytical Work |
|---|---|
| K₂-EDTA Tubes | Prevents coagulation by chelating calcium; the preferred sample for hematology and molecular diagnostics (e.g., viral load testing from whole blood). |
| Sodium Citrate Tubes | Gently chelates calcium, used for coagulation studies. The 3.2% concentration is the standard for PT/APTT tests. |
| Serum Separator Tubes (SST) | Contains a gel that forms a physical barrier between serum and clot during centrifugation, simplifying processing. |
| Cell-Free DNA BCT Tubes | Specialized blood collection tubes that stabilize nucleated blood cells to prevent the release of genomic DNA, preserving the integrity of circulating tumor DNA (ctDNA) or viral DNA. |
| Paxgene RNA Tubes | Contains additives that immediately stabilize RNA for gene expression profiling, critical for host-response research in viral infections. |
| DNA/RNA Shield | A reagent that immediately inactivates nucleases and protects nucleic acids from degradation at room temperature, useful for swab samples. |
Pre-Analytical Phase Workflow
The following diagram maps the logical workflow of the pre-analytical phase, highlighting critical control points where errors can occur.
Mitigating False Positives/Negatives and Cross-Reactivity Issues
In viral diagnostic test verification and validation, false results and cross-reactivity are not merely operational nuisances; they represent critical failures that can compromise clinical decisions, patient outcomes, and public health initiatives. A false positive occurs when a test incorrectly detects a condition that is not present, while a false negative fails to detect an existing infection [55]. Cross-reactivity, a common cause of false positives, happens when a test reacts to non-target molecules or organisms that share structural similarities with the target pathogen, such as antibodies or genetic sequences from a harmless virus triggering a positive signal for a serious infection [55] [56]. Addressing these issues is fundamental to developing reliable, clinically valuable diagnostic tests.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary technical causes of false positives in viral diagnostics? False positives primarily stem from assay cross-reactivity, where test components (e.g., antibodies or primers) bind to non-target analytes from related viruses or host cells [56]. Other major causes include cross-contamination of samples during processing, degradation of samples or reagents, and over-amplification in Nucleic Acid Amplification Tests (NAATs) like PCR, which can amplify even minute, non-significant contaminants [55].
FAQ 2: Beyond test chemistry, what operational and patient factors can lead to false negatives? False negatives are often linked to biological and operational timing. Testing too early or too late in the infection cycle can result in viral loads below the test's detection limit or after the pathogen has been cleared [57]. Furthermore, certain patient conditions, such as individuals undergoing specific chemotherapeutic treatments, can suppress the host's immune response, leading to reduced expression of viral biomarkers and potentially causing false negatives in tests that rely on the host response, like nasal biomarkers [58].
FAQ 3: How can cross-reactivity be systematically evaluated during test development? A robust validation requires testing the assay against a panel of closely related pathogens and common commensal organisms. For example, when developing an alphavirus serological test, it must be challenged with sera from infections with other alphaviruses (e.g., Chikungunya, Mayaro) to quantify cross-reactive binding [56]. Similarly, molecular tests should be checked for in-silico and wet-lab specificity against genetic sequences of non-target viruses likely to be present in the same patient population [15].
FAQ 4: In outbreak settings, is it ever acceptable to use a test with lower specificity? Mathematical modeling for diseases like Ebola demonstrates that trade-offs can be considered. A rapid diagnostic test (RDT) with lower specificity (e.g., 95% vs. 99% for PCR) can still reduce the overall epidemic size if it enables a drastically shorter time-to-isolation and a much higher testing rate. The benefit stems from isolating truly infected individuals faster, which outweighs the cost of temporarily isolating some false positives [59]. This is a strategic public health decision, not a clinical one.
Troubleshooting Guides
Guide 1: Investigating a High Rate of False Positives
Problem: Your in-house PCR or antigen test is showing an unacceptably high rate of false positives upon clinical validation.
Step-by-Step Investigation:
- Verify with a Gold Standard: Re-test the discrepant samples (those that are test-positive but culture-negative or positive via a different, validated NAAT) using a confirmatory method, such as a PCR targeting a different gene region or sequencing.
- Check for Cross-Reactivity:
- Action: Run the test against a panel of known cross-reactive organisms. If you are testing for SARS-CoV-2, include samples containing other human coronaviruses (e.g., HKU1, OC43), influenza, and RSV.
- Tool: Use BLAST to check the specificity of your primers and probes against genetic databases.
- Review Laboratory Workflow:
- Action: Audit your lab for potential contamination sources. Introduce negative controls at multiple stages: during nucleic acid extraction, master mix preparation, and post-amplification.
- Tool: Implement strict unidirectional workflow (from pre- to post-amplification areas) and use UV irradiation or enzymatic degradation methods to eliminate carryover contamination.
- Assess Reagent and Sample Quality:
- Action: Check the lot numbers and expiration dates of all reagents. Test a set of known negative samples to see if the problem is batch-specific.
- Tool: Use automated nucleic acid extraction systems and lyophilized, room-temperature-stable master mixes to reduce variability and contamination risk [9] [60].
Guide 2: Addressing Poor Sensitivity and False Negatives
Problem: Your diagnostic test is failing to detect true positive samples, resulting in low sensitivity.
Step-by-Step Investigation:
- Confirm Target Presence:
- Action: Ensure the target pathogen is present and viable in the sample. For culture-based methods, check viability; for NAATs, use a different primer/probe set to confirm.
- Optimize Sample Collection and Storage:
- Action: Poor collection technique or sample degradation is a major cause of false negatives. Validate swab types, transport media, and storage conditions (time and temperature).
- Tool: Use universal transport media validated for your target and ensure samples are frozen at -80°C if not tested immediately [58].
- Determine Limit of Detection (LoD):
- Action: Perform a serial dilution of a standard with known concentration (e.g., genome copies/mL) to establish the LoD. Compare your test's LoD to that of commercially available tests.
- Tool: Use synthetic controls or quantified viral stocks for precise LoD determination.
- Check for Inhibitors:
- Action: Re-test the false-negative sample after dilution, purification, or spiking with a known positive control to identify the presence of PCR inhibitors.
- Tool: Incorporate an internal control (e.g., a human housekeeping gene) into the reaction to detect inhibition.
Data and Protocols
Experimental Protocol for Cross-Reactivity Testing
Objective: To empirically determine the specificity of a viral diagnostic assay and its potential for cross-reactivity.
Materials:
- Test device/assay kit
- Positive control (target virus)
- Negative control (matrix-only)
- Cross-reactivity panel (closely related viruses, common co-circulating viruses, and human cell lines)
- Standard laboratory equipment (pipettes, timers, etc.)
Methodology:
- Panel Preparation: Prepare dilutions of each organism in the cross-reactivity panel to a high titer (e.g., 10^6 PFU/mL or copies/mL) in the appropriate sample matrix (e.g., universal transport media, serum).
- Testing: Run each member of the panel in replicates (n≥3) according to the test's standard operating procedure.
- Data Collection: Record the results (positive/negative) and any signal strength (e.g., Ct value for PCR, band intensity for lateral flow).
- Analysis: Any positive signal generated by a non-target organism is considered evidence of cross-reactivity. The degree of cross-reactivity can be semi-quantified by comparing the signal strength to that of the true positive control.
Quantitative Data on Test Performance and Impact
Table 1: Comparative Analytical Sensitivity of Diagnostic Technologies from RADx Initiative Evaluation This data, from the NIH's independent test verification hub, shows how different technologies from various companies detected the same patient sample at serial dilutions, enabling a direct performance comparison [9].
| Company Size (Employees) | Test Technology | Intended Use Setting | Result at Stated Sample Dilution (Viral Load) | ||||
|---|---|---|---|---|---|---|---|
| >1,000 | Antigen | Point-of-Care | Positive (Undiluted) | Negative (1:10) | Nt | Nt | Nt |
| 10-200 | RNA | Point-of-Care | Positive | Positive | Positive | Positive | Nt |
| 10-200 | Antigen | Central Lab | Nt | Positive | Positive | Positive | Positive |
| <10 | Antigen | Point-of-Care | Positive | Negative | Nt | Nt | Nt |
| Sample Viral Load (GE ml⁻¹) | 2x10⁶ | 2x10⁵ | 2x10⁴ | 2x10³ | 2x10² |
Table 2: Impact of Diagnostic Test Trade-Offs on Ebola Outbreak Size This mathematical modeling study for Ebola demonstrates how trading test accuracy for speed and accessibility can significantly reduce the total number of cases in an outbreak scenario [59].
| Test Scenario | Change in Mean Total Cases | Key Parameters |
|---|---|---|
| High-Accuracy PCR (Baseline) | Baseline (9,150 cases) | Sensitivity: 99%, Specificity: >99%, Time-to-isolation: 1.5 days |
| Reduced Sensitivity Only | Increase of 223% | Sensitivity: 85%, Other parameters unchanged |
| Reduced Specificity Only | Increase of 14.1% | Specificity: 99%, Other parameters unchanged |
| Faster Time-to-Isolation Only | Decrease of 47.7% - 87.7% | Time-to-isolation: 30 min, Accuracy unchanged |
| Combined RDT-like Scenario | Net Reduction of 71.6% - 92.3% | Lower accuracy, but faster results and higher testing rate |
Visualized Workflows
Diagnostic Cross-Reactivity Investigation Workflow
This diagram outlines the systematic process for identifying and addressing the root causes of cross-reactivity in assay development.
Test Utility Trade-Off Decision Model
This diagram illustrates the strategic decision-making process for selecting a diagnostic test in an outbreak context, where accuracy is balanced against speed and accessibility.
The Scientist's Toolkit: Essential Reagent Solutions
Table 3: Key Research Reagents for Mitigating Diagnostic Errors This table lists critical reagents and materials used in developing and validating robust viral diagnostics, along with their specific functions in minimizing false results.
| Reagent / Material | Function & Role in Mitigation |
|---|---|
| Barcoded Magnetic Beads | Used in multiplex syndromic panels (e.g., BioCode GPP) to simultaneously detect multiple pathogens with high specificity, reducing the risk of cross-reactivity and false positives by spatially separating detection events [55]. |
| Lyophilized Master Mixes | Room-temperature-stable PCR/LAMP mixes simplify storage, reduce preparation steps, and minimize reagent degradation and operator-induced variability, which are potential sources of false positives and negatives [60]. |
| Monoclonal Antibody Pairs | High-specificity paired antibodies for immunoassays are selected to bind to unique epitopes on the target antigen, minimizing non-specific binding and cross-reactivity with related viruses [60]. |
| Synthetic Controls & Standards | Quantified synthetic genes or viral particles serve as positive controls for LoD studies and inhibitor testing, and as negative controls for contamination checks, essential for validating test accuracy [60]. |
| Universal Transport Media | Preserves viral nucleic acid and antigen integrity during sample transport and storage, preventing degradation that leads to false negatives [58]. |
Strategies for Managing Resource Constraints and Supply Chain Disruptions
For researchers, scientists, and drug development professionals, the processes of test verification and validation are the bedrock of reliable viral diagnostics. These procedures ensure that diagnostic tests consistently achieve their stated performance claims, from analytical sensitivity and specificity to precision and linearity [36]. However, this critical scientific work does not occur in a vacuum; it is entirely dependent on a stable and resilient supply chain for essential reagents, equipment, and materials.
Supply chain disruptions represent a direct and immediate threat to diagnostic research and development. Resource constraints can delay vital validation studies, while shortages of key components can force protocol modifications, potentially invalidating previously established performance characteristics. The recent COVID-19 pandemic highlighted how disruptions—whether from material shortages, logistics delays, or geopolitical events—can severely impact the availability of essential tests [61] [9]. Therefore, managing these supply chain challenges is not merely an operational task but a fundamental scientific necessity to ensure that diagnostic tests for viruses are both valid and available when needed most. This guide provides troubleshooting strategies to help research professionals navigate these complex interdependencies.
FAQs and Troubleshooting Guides
This section addresses common supply chain challenges encountered in a research and development setting and provides actionable strategies for mitigation.
FAQ 1: How can we maintain verification timelines when a key raw material faces a global shortage?
Issue: A shortage of a critical raw material (e.g., a specific enzyme or nitrocellulose membrane) is threatening to halt your test verification pipeline.
Troubleshooting Guide:
- Step 1: Activate a Cross-Functional Crisis Team. Immediately assemble a team with representatives from R&D, procurement, quality assurance, and supply chain management. This ensures coordinated efforts and rapid decision-making [62].
- Step 2: Assess and Prioritize. Use a risk assessment matrix to identify which validation projects are most critical. Prioritize the allocation of remaining materials to projects with the highest public health impact or most imminent deadlines [63].
- Step 3: Leverage Supplier Relationships. Go beyond your primary supplier. Contact alternative suppliers, even if their materials are not yet qualified. Explore the possibility of "research-use-only" materials to keep development work moving while initiating expedited qualification processes for new sources [61] [64].
- Step 4: Investigate Formulation Flexibility. Work with your R&D team to determine if the assay formulation can be adapted to use an alternative, more readily available material without compromising the test's fundamental performance. This may require a partial re-validation, but it is preferable to a complete stall [65].
FAQ 2: What is the first thing to do when a shipment of critical components is delayed, jeopardizing a validation study?
Issue: A shipment of a key component, such as specialized microparticles or conjugated antibodies, is stuck in a logistics bottleneck, putting a scheduled validation study at risk.
Troubleshooting Guide:
- Step 1: Communicate Transparently. Immediately inform all stakeholders, including senior management and collaborating labs, about the potential delay. Proactive communication manages expectations and allows for collaborative problem-solving [62].
- Step 2: Explore All Logistics Options. Contact the shipping carrier to understand the exact nature of the delay. Investigate the feasibility and cost of expedited shipping for the remaining route or for rerouting the shipment entirely [61].
- Step 3: Implement Resource Rerouting. Assess your internal and partner network for any available stock. Could another project's allocation be temporarily borrowed with a guaranteed replacement? This strategy of reroute flexibility—sourcing from existing network connections—can effectively mitigate short-term shortages [65].
- Step 4: Adapt the Validation Timeline. If the delay is inevitable, formally revise the project timeline. Use the gained time to advance other preparatory work, such as finalizing protocol documents or preparing data analysis templates, to minimize the overall impact on the project's critical path [66].
FAQ 3: How do we qualify a new supplier for a critical reagent under time-sensitive conditions?
Issue: You need to rapidly qualify a new supplier for a critical reagent due to a supply disruption, but the standard qualification process is too lengthy.
Troubleshooting Guide:
- Step 1: Perform an Expedited Audit. Instead of a full on-site audit, conduct a rigorous desktop audit and virtual meeting with the new supplier. Focus on their Quality Management System (e.g., ISO 13485 certification), their sourcing of raw materials, and their production consistency data [64] [36].
- Step 2: Execute a Focused Verification Protocol. Design a condensed but high-priority verification study. This should, at a minimum, confirm:
- Analytical Sensitivity (LoD): Does the reagent perform equivalently in detecting the target at the established limit of detection?
- Specificity: Does it show the same cross-reactivity profile?
- Precision: Does it provide reproducible results in your assay system? [36]
- Step 3: Use a Bridging Study. If you have existing data and retained samples from the previous reagent lot, perform a direct comparison (bridging study) between the old and new reagent to demonstrate equivalence quickly [36].
- Step 4: Implement Enhanced Incoming QC. Until a track record is established, institute 100% testing of incoming lots from the new supplier against a well-characterized reference standard to catch any potential deviations early [64].
Data Presentation: Quantitative Impact of Resource Constraints
Understanding the landscape of common constraints and the effectiveness of various mitigation strategies is crucial for strategic planning. The tables below summarize survey data and mitigation effectiveness.
Table 1: Top Current Resource Constraints Affecting Business Viability (Survey of 143 Supply Chain Leaders) [63]
| Resource Constraint | Percentage of Leaders Reporting |
|---|---|
| Skilled Labor / Talent | 39% |
| Semiconductor Chips / Electronic Components | 26% |
| Raw Materials | 26% |
| Manufacturing Capacity | 23% |
| Energy | 22% |
| Logistics Capacity | 21% |
Table 2: Effectiveness of Key Mitigation Strategies for Supply Chain Disruptions
| Mitigation Strategy | Key Metric/Outcome | Application in Diagnostic Research |
|---|---|---|
| Reroute Flexibility [65] | Reduces final-buyer supply deficit by up to 50% under 70% supply shock. | Sourcing substitute reagents or materials from existing alternative distributors within the network. |
| Supplier Diversification [62] | Mitigates risk of complete stoppage from single point of failure. | Pre-qualifying multiple suppliers for critical raw materials (e.g., antibodies, polymers, membranes). |
| Inventory Buffering [61] [62] | Increases time-to-survive before shortage impacts operations. | Maintaining strategic stockpiles of long-lead-time or high-risk critical components. |
| Digital Visibility Tools [64] | Enables real-time monitoring and proactive issue identification. | Using supply chain management software to track reagent orders, inventory levels, and supplier lead times. |
Experimental Protocols for Key Analyses
Protocol 1: Expedited Verification of a Critical Raw Material from a New Supplier
1.0 Objective: To rapidly verify the performance equivalence of a critical raw material (e.g., an antigen for a lateral flow test) from a new supplier, in response to a supply disruption of the primary material.
2.0 Principle: A focused set of experiments will compare the new material against the currently qualified material (or a well-characterized retained sample) using key performance parameters to ensure no significant degradation in assay performance.
3.0 Materials:
- New supplier's raw material (test article)
- Qualified reference material (control article)
- All other standardized reagents and equipment for the diagnostic assay
- Pre-characterized clinical or spiked samples (positive, low-positive, and negative)
4.0 Procedure:
- 4.1 Preparation: Reconstitute or prepare both test and control articles according to their respective specifications.
- 4.2 Limit of Detection (LoD) Comparison:
- Prepare a dilution series of the target analyte in a relevant matrix.
- Test each dilution with both the test and control articles (n=3 replicates per dilution).
- Determine the lowest concentration at which all replicates are detected for each material. The LoD should not differ by more than one dilution step.
- 4.3 Precision Assessment:
- Test a low-positive sample (2-3x the expected LoD) with both materials across three different runs, with two operators and on different days (intermediate precision).
- The coefficient of variation (%CV) between results obtained with the test and control articles should not exceed a pre-defined threshold (e.g., 15%).
- 4.4 Specificity Check:
- Test a panel of potentially cross-reacting analytes or interfering substances.
- The results (positive/negative) and signal intensities should be concordant between the test and control articles.
5.0 Acceptance Criteria: The new material is considered verified for emergency use if all defined acceptance criteria for LoD, precision, and specificity are met relative to the control article [36].
Protocol 2: Stress Testing a Supply Route for a Critical Research Reagent
1.0 Objective: To model and understand the vulnerability of a supply route for a critical reagent and to evaluate the effectiveness of contingency plans.
2.0 Principle: Using a data-driven model, simulate a sudden stop in supply from a primary vendor and observe the time until a "shortage" impacts research activities, with and without mitigation strategies like reroute flexibility.
3.0 Materials:
- Supply chain mapping data (primary vendor, secondary vendors, lead times, inventory levels)
- Consumption data for the reagent (average weekly usage)
- Simulation software or a structured spreadsheet model
4.0 Procedure:
- 4.1 Model Baseline Operation: Input your current inventory level, weekly usage rate, and lead time from the primary vendor. Establish a "shortage threshold" (e.g., a 2-week supply).
- 4.2 Simulate a Disruption: Model a scenario where supply from the primary vendor is halted for a defined period (e.g., 60 days).
- 4.3 Measure Time-to-Shortage: Calculate the number of days until your inventory falls below the shortage threshold.
- 4.4 Introduce Mitigation Strategies: Re-run the simulation incorporating strategies such as:
- Inventory Buffering: Increasing the starting safety stock level.
- Reroute Flexibility: Switching to a pre-identified secondary vendor with a different lead time once the primary vendor fails [65].
- 4.5 Analyze Results: Compare the "time-to-shortage" and "shortage severity" between the baseline scenario and the scenarios with mitigation strategies.
5.0 Data Analysis: The strategy that most effectively delays the onset and reduces the severity of the shortage should be formalized as a contingency plan for that reagent.
Workflow and Relationship Diagrams
The following diagram illustrates the logical decision workflow for managing a supply disruption of a critical reagent in a research setting, from identification to resolution.
Diagram 1: Supply Disruption Response Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagent Solutions for Diagnostic Test Verification
| Research Reagent / Material | Critical Function in Verification/Validation | Key Considerations for Supply Resilience |
|---|---|---|
| Monoclonal/Polyclonal Antibodies | Core component for target capture and detection in immunoassays. Defines test specificity and sensitivity. | Diversify: Identify multiple clone sources. Buffer: Stockpile based on stability. Characterize: Keep detailed characterization data to ease supplier switching [9] [36]. |
| Enzymes (e.g., PCR Polymerases) | Essential for nucleic acid amplification in molecular assays. Impacts sensitivity, robustness, and reproducibility. | Quality: Ensure thermal stability and fidelity. Dual-Source: Maintain two validated enzyme suppliers. Buffer: High-value, stable critical reagent [61] [64]. |
| Synthetic Nucleic Acids | Used as positive controls, calibrators, and for determining Limit of Detection (LoD). | Generic Sequences: Use where possible to avoid single-source dependency. Long Shelf-Life: Can be stockpiled. Multiple Vendors: Source from several oligo synthesis companies [36]. |
| Nitrocellulose Membranes | The matrix for capillary flow and reaction in lateral flow immunoassays. Impacts test line clarity and flow time. | Specification-Driven: Source based on precise technical specs (pore size, flow rate) not just brand. Pre-Qualify: Rigorously test membranes from 2-3 suppliers during R&D phase [64]. |
| Clinical Sample Panels | Used for clinical sensitivity/specificity studies. Must be well-characterized (positive, negative, cross-reactive). | Collaborate: Partner with biobanks and other institutions. Bank: Create internal sample repositories. Ethical Sourcing: Ensure proper informed consent for future use [9] [36]. |
Within viral diagnostic test verification and validation, the accuracy of a result is fundamentally dependent on the quality of the original sample. Complex biological samples such as plasma, urine, and throat swabs each present unique matrices and pre-analytical challenges that can interfere with assay performance. This technical support center provides targeted troubleshooting guides and frequently asked questions to assist researchers and scientists in optimizing their sample processing protocols, ensuring the reliability and reproducibility of data in drug and diagnostic development.
FAQs and Troubleshooting Guides
General Pre-Analytical Considerations
Q: What are the universal pre-analytical factors to control for these sample types? A: Key factors include consistent collection timing, proper sample containment, and stringent temperature control during storage and transport. Variations in these factors can significantly alter analyte stability. For instance, samples for viral RNA detection are optimally stored at +4°C in an appropriate preservation buffer, with freezing at -70°C or below recommended for longer-term storage to prevent nucleic acid degradation [67] [68].
Q: How can I quickly verify if a sample processing error has occurred? A: Implement a sample quality control step. For nucleic acid-based tests, this can include quantifying RNA/DNA yield and purity (A260/A280 ratio) or amplifying a ubiquitous human gene (e.g., RNase P) to confirm that the sample is amplifiable and was collected properly [69].
Throat Swab-Specific Protocol
Q: My throat swab samples are yielding low viral RNA, leading to false negatives. How can I improve detection? A: Low RNA recovery can stem from several points in the protocol:
- Collection Technique: Ensure the swab vigorously contacts the tonsillar pillars and posterior oropharynx. Inadequate sampling surface contact is a common cause of low yield.
- Swab Type: Use synthetic-tipped (e.g., flocked) swabs over cotton-tipped ones, as they release cellular material more efficiently.
- Storage Buffer: Immediately post-collection, place the swab in a recommended viral transport medium (VTM). Avoid swabs with guanidinium-based media if subsequent antigen testing is planned [68].
- Storage Temperature: Process swabs promptly. If a delay is unavoidable, store at +4°C for up to 48-72 hours. For longer storage, freeze at -70°C or below [68].
Q: What is the optimal workflow for processing throat swabs for rRT-PCR? The diagram below outlines a standardized workflow to maximize reliability.
Plasma/Serum-Specific Protocol
Q: How does the choice between plasma and serum impact viral diagnostic results? A: The choice is analyte-dependent. Plasma is generally preferred for molecular tests because it provides a higher yield of cell-free viral nucleic acids and avoids the potential loss of analytes during the clot formation process required for serum separation [67] [69]. Serum is traditionally used for serological assays to detect immunoglobulins (IgG, IgM).
Q: Hemolysis is a common issue in our plasma samples. Could this affect our viral rRT-PCR results? A: Yes, significantly. Hemolyzed samples contain hemoglobin, lactoferrin, and other PCR inhibitors that can reduce the efficiency of the amplification reaction, leading to decreased sensitivity or false-negative results [67]. It is crucial to visually inspect samples post-centrifugation and use nucleic acid extraction methods that include robust wash steps to remove these inhibitors.
Urine-Specific Protocol
Q: We are detecting viral RNA in urine. The results are inconsistent. What could be the cause? A: Urine is a complex matrix with variable pH, high ionic strength, and the presence of metabolites that can be potent inhibitors of enzymatic reactions like PCR [70]. To improve consistency:
- Sample Preparation: Incorporate dilution, filtration, or solid-phase extraction steps to remove inhibitors [70].
- Centrifugation: For some viruses, a pre-centrifugation step can concentrate viral particles from a larger volume of urine, improving the limit of detection.
- Sample Timing: The time of day and the patient's hydration status can greatly affect analyte concentration. Standardize collection protocols (e.g., first-morning void) where possible.
Q: Can urine be used for purposes other than direct pathogen detection? A: Absolutely. Urine is a valuable matrix for disease surveillance and antibody detection. Saliva-based immunoassays, which are similar in principle to urine tests, show great promise for large-scale disease surveillance due to their non-invasive nature [68]. Furthermore, urine can be screened for specific host biomarkers that indicate disease states or metabolic responses to infection [70].
Comparative Analysis of Sample Types
The table below summarizes key performance characteristics of different sample types based on clinical studies for viral detection, using SARS-CoV-2 as a model pathogen.
Table 1: Comparative Analysis of Clinical Specimens for Viral Detection (e.g., SARS-CoV-2) via rRT-PCR
| Sample Type | Reported Positivity Rate (%) | Key Advantages | Key Limitations & Challenges |
|---|---|---|---|
| Bronchoalveolar Lavage (BAL) | Highest (~95%) [69] | Direct sampling of lower respiratory tract; very high viral load. | Highly invasive; generates aerosols; requires specialized personnel; not suitable for screening. |
| Sputum | High (~88%) [69] | High viral load; useful in symptomatic patients. | Can be difficult to obtain from patients with dry cough; requires homogenization. |
| Nasopharyngeal Swab (NPS) | Moderate-High (Varies) [69] | Standardized, widely accepted method. | Uncomfortable for patient; technique-sensitive; risk to healthcare workers. |
| Saliva | Moderate (Can be comparable to NPS) [67] [71] | Non-invasive; self-collection possible; reduces healthcare worker risk. | Viscosity can complicate pipetting; potential for food/drink contamination; may require sample pre-treatment. |
| Plasma/Serum | Low (<50%) [69] | Useful for serology and viremic phase detection. | Lower viral load for direct pathogen detection; presence of PCR inhibitors (e.g., hemoglobin). |
| Urine | Low (Rare) [69] | Non-invasive; easy to collect in large volumes. | Very low viral load for many pathogens; complex matrix with potent PCR inhibitors [70]. |
| Feces/Rectal Swab | Moderate (Can persist after respiratory clearance) [68] | Useful for monitoring prolonged shedding and gastrointestinal involvement. | Complex matrix requiring specialized extraction protocols. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials critical for working with complex samples in a viral diagnostic context.
Table 2: Key Research Reagent Solutions for Complex Sample Processing
| Item | Function & Application | Critical Considerations for Use |
|---|---|---|
| Flocked Swabs | Sample collection from throat and nasopharynx. Superior release of cellular material compared to cotton swabs. | Ensure compatibility with downstream extraction kits and transport media. |
| Viral Transport Medium (VTM) | Preserves viral integrity and nucleic acids during swab transport and storage. | Do not use guanidinium-based VTM if antigen testing is required. Maintain cold chain. |
| Magnetic Bead-Based NA Extraction Kits | Purification of nucleic acids (RNA/DNA) from plasma, urine, swab eluates, and other complex samples. | Effective for removing PCR inhibitors (e.g., from urine or hemolyzed plasma). Optimize binding and wash steps for sample type. |
| Lyophilized Colorimetric LAMP Assays | Isothermal nucleic acid amplification for point-of-care or resource-limited settings. | Enables visual, equipment-free readout. Stable at room temperature, eliminating cold chain [72]. |
| Nucleic Acid Preservation Buffers | Chemical stabilization of RNA/DNA at room temperature for extended periods. | Crucial for stabilizing samples during shipping or when freezing is not immediately possible. |
| PCR Inhibitor Removal Additives | Added to master mixes or sample lysis buffers to neutralize common inhibitors. | Enhances assay robustness and sensitivity, particularly for challenging matrices like urine and stool. |
Advanced Experimental Protocol: Integrated Sample-to-Result Workflow
This protocol outlines a modern, portable molecular diagnostic workflow suitable for processing various sample types, integrating power-free nucleic acid extraction and lyophilised isothermal amplification, as validated in recent studies [72].
1. Sample Inactivation and Lysis:
- For swabs: Elute the swab in 1 mL of an inactivating medium (e.g., COPAN eNAT).
- For plasma/urine: Mix 200 µL of sample with an equal volume of lysis/binding buffer containing guanidine thiocyanate and magnetic silica beads.
- Incubate at room temperature for 2 minutes to ensure complete lysis and binding of nucleic acids to the magnetic beads.
2. Power-Free Nucleic Acid Extraction (Using SmartLid or similar magnetic technology):
- Lysis-Binding: Transfer the lysate to the first (red) tube. Use a magnetic lid to capture the bead-bound NA complex.
- Washing: Transfer the magnetic lid with captured beads sequentially through two wash buffers (yellow tubes) to remove proteins, inhibitors, and other contaminants.
- Elution: Transfer the beads into the final (green) tube containing nuclease-free water or a low-salt elution buffer. Resuspend by pipetting to release the purified NA.
3. Lyophilised Colorimetric LAMP Amplification:
- Resuspend a lyophilised LAMP pellet (containing primers, polymerase, dNTPs, and pH-sensitive dye) with the purified eluate.
- Incubate the reaction at a constant temperature of 60–65 °C for 20–35 minutes in a low-cost, portable heat block.
- Result Interpretation: A color change from pink (negative) to yellow (positive) indicates target amplification, visualized by the naked eye.
4. Validation and Quality Control:
- Benchmark the entire workflow against a gold-standard extracted qPCR method using a panel of known positive and negative clinical samples.
- Report performance metrics including analytical sensitivity (LoD), clinical sensitivity, and specificity [72]. For example, a validated mpox assay using this platform demonstrated 94.1% sensitivity and 100% specificity [72].
Establishing Robust Validation Frameworks and Comparative Assay Performance
Frequently Asked Questions (FAQs)
Q1: When is validation required for a diagnostic test? Validation is required when a system or test is used in a Good Practice (GxP) process, to make decisions about product quality, or to generate data for submissions to regulatory bodies like the FDA. For viral diagnostics, this is a legal requirement to ensure the test is safe and effective for its intended use [73] [74].
Q2: What is the difference between clinical performance verification and clinical validation? These terms are often used in a specific regulatory context. Verification is the evaluation of a diagnostic technology to determine its preliminary analytical and clinical performance (e.g., limits of detection, sensitivity, specificity) in a controlled setting [9]. Validation is the broader process of confirming that the test satisfies its intended purpose and is clinically useful in a real-world setting, often through a prospective clinical study [74] [75].
Q3: Why is a multi-site, blinded clinical validation study important? A multi-site, blinded validation study is a robust method to assess how a test performs across different clinical settings and patient populations. This approach reduces bias and provides high-quality evidence of real-world performance, which is crucial for regulatory approval and building clinical trust [76].
Q4: What are the consequences of inadequate validation? Inadequate validation can have serious consequences, including regulatory citations from bodies like the FDA, failure to obtain necessary certifications, and most critically, a direct impact on patient safety due to inaccurate test results [77] [74].
Q5: How can synthetic data be used in validation, and how is its quality assured? Synthetic or artificial specimens, such as those generated by AI models like Generative Adversarial Networks (GANs), can augment limited real datasets. However, their use requires a systematic validation protocol combining quantitative metrics and qualitative expert assessments to evaluate realism, fidelity, diversity, and, ultimately, their usefulness in the clinical validation process [78].
Troubleshooting Common Experimental Issues
Poor Documentation and Planning
- Problem: Unclear requirements and poor documentation at the start of validation, leading to a lack of clarity on what to test and how.
- Solution: Before testing, define and document all software and process requirements. Use these documents to drive your verification and validation (V&V) activities. From a regulatory perspective, "if you don't document what you did, you didn't do it" [77].
Inadequate Test Tool Validation
- Problem: Data from V&V tests is unreliable because the test tools and methods themselves have not been properly validated.
- Solution: Before formal testing, verify that all V&V tools (e.g., modeling software, data analysis tools) are working correctly and that the test methods are well-defined and managed [77].
Failure to Test the Final Product
- Problem: The product design changes during development, but the V&V testing is not repeated, meaning the tested version is not the final version.
- Solution: Any change in design or requirements should trigger an update to the documentation and a repeat of the relevant V&V tests to ensure the final product has been fully evaluated [77].
Lack of Independence in Evaluation
- Problem: Bias is introduced because the team that developed the test is also solely responsible for its evaluation.
- Solution: A level of independence from the development team is recommended for V&V activities. This ensures unbiased, reliable, and secure conduct, adding significant value to the development process [77].
Key Experimental Protocols & Data
Protocol: External Clinical Validation of an AI-Based Diagnostic Tool
This protocol, adapted from a study on an AI tool for echocardiography, provides a robust framework for validating a viral diagnostic test [75].
- Study Design: A prospective cohort study conducted in multiple phases, involving multiple readers and multiple cases.
- Participants: Recruit participants referred for testing as part of routine clinical practice. Define clear inclusion/exclusion criteria (e.g., based on symptoms, known infection status, comorbidities).
- Comparator Groups: Involve professionals of different experience levels (e.g., low, medium, high) to compare the test's performance against human judgment.
- Reference Panel: Establish a panel of highly experienced experts to provide reference measurements or diagnoses against which the new test is judged.
- Primary Outcomes: Typically, the non-inferiority of the new test's accuracy (sensitivity, specificity) compared to the standard method or human expert.
- Secondary Outcomes: Can include the time required for diagnosis and usability feedback from the professionals using the tool [75].
Protocol: Systematic Validation of Synthetic Specimens
This protocol outlines a holistic approach to validating artificially generated specimens, such as synthetic dermoscopic images, which can be adapted for viral diagnostic specimens [78].
- Generation: Use a model like a StyleGAN2 to generate synthetic positive and negative specimens.
- Matching: Match synthetic specimens with real ones.
- Expert Panel: Engage a panel of domain experts (e.g., virologists, pathologists).
- Qualitative Assessment: Experts assess the images across multiple attributes (e.g., realism, texture, confidence in classification) using a Likert scale.
- Quantitative Analysis: Calculate accuracy, sensitivity, specificity, and inter-rater agreement (e.g., Fleiss' Kappa) to objectively analyze the expert evaluations.
Performance Data from Diagnostic Test Validation
The table below summarizes quantitative performance data from real-world test verification studies, providing benchmarks for validation targets [76] [9].
Table 1: Performance Metrics from Diagnostic Test Validation Studies
| Test Type / Target | Sensitivity | Specificity | Area Under the Curve (AUC) | Citation |
|---|---|---|---|---|
| AI for Invasive Breast Carcinoma | 95.51% | 93.57% | 0.99 | [76] |
| AI for Ductal Carcinoma In Situ (DCIS) | 93.20% | 93.79% | 0.98 | [76] |
| High-Performance RADx COVID-19 Tests* | Varies by dilution/limit of detection | Varies by dilution/limit of detection | Not Reported | [9] |
*The RADx initiative evaluated tests using serial dilutions of a positive patient pool. The best-performing tests could detect SARS-CoV-2 RNA at dilutions of 1:1,000 to 1:10,000, indicating a very low limit of detection [9].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Validation Panel Sourcing
| Reagent / Material | Function in Validation |
|---|---|
| Clinical Specimens | Sourced from patient cohorts; serve as the gold standard for assessing real-world clinical performance and accuracy [75]. |
| Synthetic Specimens | Artificially generated samples (e.g., via GANs) used to augment datasets, test edge cases, and ensure robustness when real samples are scarce [78]. |
| Reference Panel Measurements | Definitive diagnoses or measurements provided by a panel of expert consensus; the benchmark against which the new test is validated [75]. |
| Blinded Sample Sets | A curated set of clinical and synthetic specimens where the testing personnel are unaware of the reference results; crucial for eliminating bias during validation [76]. |
Validation Workflow and Specimen Sourcing Diagrams
Diagnostic Test Validation Workflow
Specimen Sourcing Strategy
This technical support center provides troubleshooting and guidance for researchers and scientists engaged in the verification and validation of viral diagnostic tests. The following FAQs and guides address common challenges encountered during experimental procedures, framed within the context of rigorous test validation as required for regulatory compliance and high-quality research outcomes.
Frequently Asked Questions (FAQs)
FAQ 1: What is the relationship between sensitivity and specificity, and why is their inverse relationship important for my viral diagnostic test?
Sensitivity and specificity are inversely related test characteristics intrinsic to the diagnostic assay itself [79]. As sensitivity increases, specificity tends to decrease, and vice versa [79].
- Sensitivity is the proportion of true positives the test correctly identifies out of all individuals who actually have the disease. A test with 100% sensitivity will identify all patients with the condition [79] [80].
- Specificity is the proportion of true negatives the test correctly identifies out of all individuals who do not have the disease. A test with 100% specificity will correctly identify all healthy patients [79] [80].
This inverse relationship is crucial because it means you cannot maximize both simultaneously. The choice involves a trade-off based on the clinical or research context. A highly sensitive test is critical for "ruling out" disease when the consequence of missing a case is severe. A highly specific test is vital for "ruling in" a disease when a false positive could lead to unnecessary treatments, anxiety, or expense [79] [80].
FAQ 2: How do I investigate the cause of a high false-positive rate in my diagnostic assay?
A high false-positive rate indicates a problem with the test's specificity. The following troubleshooting guide can help identify the root cause.
| Potential Cause | Investigation | Corrective Action |
|---|---|---|
| Cross-reactivity | Review the test's known cross-reactivities. Test the assay against a panel of samples known to contain related viruses or other potential interfering substances. | Redesign probe/target sequences or change antibody clones to improve specificity. Increase the stringency of wash buffers. |
| Sample Contamination | Audit laboratory procedures for amplicon contamination, especially in nucleic acid amplification tests (NAATs). Use dedicated equipment and workspaces for pre- and post-amplification steps. | Implement rigorous cleaning protocols using EPA-registered disinfectants [81]. Use dUTP and Uracil-DNA Glycosylase (UDG) to degrade carryover amplicons. |
| Reagent Degradation | Check the lot numbers and expiration dates of all critical reagents, particularly detection antibodies or enzymes. | Repeat the test with a new, in-date batch of reagents. Optimize reagent storage conditions. |
| Inadequate Sample Quality | Review sample collection, transport, and storage procedures. Hemolyzed, lipemic, or improperly stored samples can interfere. | Re-train staff on proper sample handling protocols. Re-run the test with a freshly collected sample, if possible. |
FAQ 3: My test's Limit of Detection (LOD) appears inconsistent between experiments. What factors should I review in my protocol?
An inconsistent LOD suggests variability in the experimental conditions or reagents. Key factors to review are summarized in the table below.
| Factor | Impact on LOD | Protocol Checklist |
|---|---|---|
| Sample Matrix | Different sample types (e.g., nasopharyngeal swab vs. saliva) can contain different inhibitors that affect amplification efficiency. | Validate the LOD using the exact same sample matrix intended for clinical use. Use a universal transport medium that has been validated for your assay. |
| Nucleic Acid/Antigen Extraction | Inefficient or variable extraction yields directly cause inconsistent detection of low viral loads. | Standardize the extraction method and kit across all validation runs. Ensure automated extraction instruments are properly calibrated. |
| Reaction Efficiency | Minor variations in master mix composition, pipetting accuracy, or thermal cycler calibration can significantly impact sensitivity. | Use a single, validated master mix lot for LOD studies. Perform precise pipette calibration. Validate thermal cycler block uniformity. |
| Reference Material | Using different sources or dilutions of the positive control can introduce variability. | Use a standardized, quantified reference material (e.g., from NIBSC or ATCC) for all LOD determinations. Prepare a large, single batch of dilutions to use across experiments. |
FAQ 4: How do predictive values differ from sensitivity and specificity, and what is the role of disease prevalence?
Predictive values, unlike sensitivity and specificity, are highly dependent on disease prevalence in the population being tested [79].
- Positive Predictive Value (PPV): The probability that a subject with a positive test result truly has the disease.
- Negative Predictive Value (NPV): The probability that a subject with a negative test result truly does not have the disease.
Sensitivity and specificity are considered stable test characteristics, while PPV and NPV change with prevalence [79]. When a disease is highly prevalent, the PPV increases, and the test is better at 'ruling in' the disease. Conversely, in a low-prevalence setting, the NPV is higher, and the test is better at 'ruling out' the disease [79]. Therefore, a test validated in a high-prevalence population may perform with a lower PPV when deployed for widespread screening in a general, low-prevalence population.
Experimental Protocols & Methodologies
Protocol 1: Determining Sensitivity and Specificity Using a 2x2 Table
This methodology allows for the calculation of essential accuracy metrics by comparing the new test results to a gold standard.
- Objective: To calculate the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of a new viral diagnostic test.
- Materials:
- Clinical specimens (e.g., nasopharyngeal swabs, serum) from patients with and without the target viral infection.
- The new in-house or commercial diagnostic test kit.
- Gold standard test for comparison (e.g., FDA-approved EUA test, PCR, or viral culture).
- Experimental Workflow:
Procedure:
- Collect a sufficient number of patient samples (e.g., n=1000) to ensure statistical power.
- Run all samples using both the new test (the "index" test) and the established gold standard test. The tests should be performed blinded, meaning the operator does not know the result of the other test.
- Tabulate the results in a 2x2 contingency table, as shown below.
- Use the values in the table to calculate the key performance metrics using the formulas provided.
Example Data and Calculations:
| Gold Standard Positive | Gold Standard Negative | Total | |
|---|---|---|---|
| Index Test Positive | 369 (True Positive, A) | 58 (False Positive, B) | 427 |
| Index Test Negative | 15 (False Negative, C) | 558 (True Negative, D) | 573 |
| Total | 384 | 616 | 1000 |
- Formulas:
- Sensitivity = A / (A + C) = 369 / 384 = 96.1%
- Specificity = D / (B + D) = 558 / 616 = 90.6%
- Positive Predictive Value (PPV) = A / (A + B) = 369 / 427 = 86.4%
- Negative Predictive Value (NPV) = D / (C + D) = 558 / 573 = 97.4% [79]
Protocol 2: Establishing the Limit of Detection (LOD) via Probit Analysis
The LOD is the lowest concentration of the analyte that can be reliably detected by the assay.
- Objective: To determine the lowest viral concentration at which the test achieves a detection rate of ≥95%.
- Materials:
- Serial dilutions of the target virus (or its nucleic acid/synthetic transcript) in a relevant negative sample matrix.
- Full test kit reagents.
- Procedure:
- Prepare a dilution series of the virus spanning the expected low end of the detectable range (e.g., from 1000 copies/mL to 10 copies/mL).
- Test each dilution level multiple times (a minimum of 20 replicates is recommended for robust statistical analysis).
- Record the proportion of positive results at each concentration level.
- Use probit regression analysis (available in most statistical software packages) to model the relationship between the log10 concentration and the probability of detection.
- The LOD is defined as the concentration at which 95% of the test replicates are positive.
Protocol 3: Evaluating Precision (Repeatability and Reproducibility)
Precision measures the random variation and agreement between repeated measurements under specified conditions.
- Objective: To assess the test's variability within-run (repeatability) and between-run, between-operator, between-day, and between-lot (reproducibility).
- Materials:
- Clinical samples or contrived specimens with viral concentrations near the medical decision point(s) (e.g., low positive, high positive).
- Procedure:
- Select at least two levels of controls (low and high positive).
- For repeatability (within-run precision): Analyze the same sample multiple times (e.g., 20 replicates) in a single run by the same operator using the same equipment and reagents.
- For reproducibility (intermediate precision): Analyze the same samples over multiple days (e.g., 5 days), with two runs per day, by different operators, and using different reagent lots, if possible.
- Calculate the mean, standard deviation (SD), and coefficient of variation (%CV) for the quantitative output (e.g., Ct value, signal intensity) for each level.
- Acceptance Criterion: The %CV should be within pre-defined limits based on the assay's performance claims and regulatory guidance (e.g., ≤ 10-15% for molecular tests).
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Viral Diagnostic Testing |
|---|---|
| Barcoded Magnetic Beads (BMB) | Technology that integrates digital barcodes with molecular and immunochemistry for high-throughput, multiplexed detection of pathogens from a single sample [82]. |
| Gold Standard Test | An established, validated reference method (e.g., an FDA-authorized test, viral culture, or PCR with sequencing) used as a comparator to evaluate the new index test's performance [79] [80]. |
| Synthetic Oligonucleotides | Chemically synthesized nucleic acid fragments used as positive controls, for assay development, and for standard curve generation in nucleic acid amplification tests (NAATs) [83]. |
| Enzyme-Linked Antibodies | Antibodies conjugated to enzymes (e.g., Horseradish Peroxidase) used in ELISA and Western Blot to detect the presence of a specific viral antigen or antibody, producing a measurable colorimetric signal [83]. |
| Field-Effect Transistor (FET) | A type of electrochemical biosensor where a bioreceptor (e.g., an antibody) is immobilized on a graphene sheet. Binding of a viral antigen (e.g., SARS-CoV-2 spike protein) alters the electrical current, enabling highly sensitive detection [83]. |
| Surface Imprinted Polymers (SIPs) | Synthetic polymers with tailor-made cavities that act as artificial antibodies, selectively capturing and concentrating target viral particles for enhanced detection in complex samples like serum [83]. |
The VALCOR protocol (VALidation of severe acute respiratory CORona virus-2 assays) establishes a harmonized and standardized framework for the validation of SARS-CoV-2 diagnostic assays. Developed in response to the COVID-19 pandemic, this protocol addresses the critical need for comprehensive test validation after many assays received only provisional authorization for emergency use without thorough validation. The primary objective of VALCOR is to define common criteria that SARS-CoV-2 assays must fulfill, thereby limiting false negative and false positive results through systematic performance evaluation, specifically for nucleic acid amplification tests (NAATs) used to detect SARS-CoV-2 viral RNA in respiratory specimens [84].
Inspired by the successful VALGENT (VALidation of HPV GENotyping Tests) framework for human papillomavirus tests, VALCOR creates a structured, open-source approach to address the unprecedented need for diagnostic testing during the pandemic. The protocol is designed to benchmark the performance of rapidly evolving SARS-CoV-2 assays, filling a significant gap in comprehensive validation processes that emerged due to the urgent need for testing capacity. By generating robust validation data for assays used in SARS-CoV-2 diagnosis, VALCOR may also serve as a basis for validation protocols for other infectious diseases [84].
Core Components of the VALCOR Framework
Study Design and Methodology
VALCOR employs a multi-centre cross-sectional diagnostic test accuracy study design to assess the diagnostic parameters of SARS-CoV-2 assays. The consortium entails a collaboration between coordinating institutions and virology laboratories (provider laboratories), preferentially those serving as national reference centres for SARS-CoV-2 control. The protocol involves provider laboratories compiling a VALCOR panel composed of clinical and artificial samples that are first tested with an established reference SARS-CoV-2 test. Well-defined aliquots prepared from these VALCOR samples are then sent to client laboratories for testing with an index SARS-CoV-2 test requiring evaluation [84].
The primary outcomes measured are virological sensitivity and specificity of index tests to detect the presence of SARS-CoV-2 as defined by the reference test. Additionally, the limit of detection is assessed on a series of dilutions of both clinical and artificial specimens. This rigorous methodology ensures standardized evaluation across different testing platforms and laboratories [84].
VALCOR Sample Panel Composition
The VALCOR panel is carefully designed to comprehensively evaluate assay performance across various conditions and sample types. The standardized panel includes 220 clinical specimens (180 non-diluted and 40 diluted) plus additional dilutions of artificial standard reference viral RNA material [84].
Table: Composition of the VALCOR Clinical Sample Panel
| Sample Type | Description | Quantity |
|---|---|---|
| Hospitalized Cases | Samples from hospitalized, SARS-CoV-2 confirmed cases | 40 samples |
| Non-hospitalized Cases | Samples from non-hospitalized, SARS-CoV-2 confirmed cases | 50 samples |
| Negative Cases | Samples from SARS-CoV-2 negative cases | 90 samples |
| Diluted Samples | Four dilutions (1:2, 1:10, 1:20, 1:50) of 10 samples from non-hospitalized patients | 40 samples |
The panel includes two primary types of specimens:
Artificial specimens containing specified SARS-CoV-2 RNA sequences prepared by institutions specialized in producing standard reference materials for microbiological agents, such as the Joint Research Centre of the European Commission (JRC), National Institute of Standards and Technology (NIST), American Type Culture Collection (ATCC), and BEI Resources. A series of dilutions are prepared from these materials to assess the limits of detection and ranges of detectability [84].
Clinical specimens consisting of residual original rough material or extracted RNA after SARS-CoV-2 testing stored in biobanks of VALCOR provider laboratories. These include nasopharyngeal, oropharyngeal, or other respiratory tract specimens from COVID-19 patients, healthy carriers of SARS-CoV-2, and subjects not carrying SARS-CoV-2 [84].
To ensure sample integrity, each fresh sample of the VALCOR panel is divided into aliquots of the original material and stored at -80°C until shipment to client laboratories. Comprehensive data on the pre-analytical phase of testing, including sample retrieval process, transport and storage conditions, and storage media type, are recorded in detail, as these factors can significantly impact test performance [84].
Diagram Title: VALCOR Protocol Workflow and Sample Panel Composition
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What types of SARS-CoV-2 assays does the VALCOR protocol validate? The VALCOR protocol is specifically designed for the validation of nucleic acid amplification tests (NAATs) used to detect SARS-CoV-2 viral RNA. This includes reverse transcription-polymerase chain reaction (RT-PCR) assays, which are considered the gold standard for SARS-CoV-2 detection, as well as other amplification methods such as isothermal amplification including transcription-mediated amplification (TMA) and loop-mediated isothermal amplification (LAMP) [84].
Q2: How does VALCOR address the impact of SARS-CoV-2 variants on assay performance? While the core VALCOR protocol focuses on general assay validation, the framework can be adapted to evaluate assay performance against specific variants. The inclusion of artificial specimens with calibrated amounts of viral RNA representing different sequences allows for assessing detection capabilities across variants. Additionally, the protocol's comprehensive approach to evaluating sensitivity and specificity using diverse clinical samples enhances the likelihood of identifying variant-related performance issues [84] [85].
Q3: What are the specific requirements for sample collection and storage in VALCOR studies? VALCOR panels include samples suspended in various transport media, including Universal Transport Medium (UTM), Phosphate Buffered Saline (PBS), and eNAT medium. Detailed information on the pre-analytical phase, including sample retrieval processes, transport conditions, storage media, and storage temperatures, is systematically recorded as these factors significantly impact test performance. Samples are typically stored at -80°C and shipped to participating laboratories under controlled conditions [84].
Q4: How does VALCOR handle the validation of assays for different specimen types? The protocol primarily focuses on nasopharyngeal and oropharyngeal specimens, which are the standard for SARS-CoV-2 detection. However, it also accommodates other specimens from the respiratory tract. The inclusion of diverse clinical samples from both hospitalized and non-hospitalized patients enhances the evaluation of assay performance across different specimen qualities and viral loads [84].
Q5: What performance metrics does VALCOR generate for evaluated assays? VALCOR generates comprehensive performance metrics including:
- Sensitivity and specificity compared to reference methods
- Limit of detection (LoD) determined through dilution series
- Analytical sensitivity across different viral concentrations
- Reproducibility and reliability data [84]
Troubleshooting Common Experimental Issues
Issue 1: Inconsistent Results Across Sample Dilutions
Problem: Unexpected variations in detection when testing the dilution series of clinical samples or artificial reference materials.
Solution:
- Verify the dilution technique and ensure consistent buffer composition across all dilutions.
- Confirm the homogeneity of the original sample before aliquoting and dilution.
- Check for potential inhibitors in the dilution buffer that might affect amplification.
- Validate dilution series with independent methods to confirm expected concentration relationships.
Root Cause Analysis: Inconsistent dilution practices or variations in sample matrix effects can lead to non-linear detection patterns, compromising LoD determination [84].
Issue 2: Discrepancies Between Reference and Index Assay Results
Problem: Systematic discrepancies occurring between results from the established reference assay and the index assay being validated.
Solution:
- Review the target genes and regions for each assay, as differences in sensitivity to specific genomic regions can cause discrepancies.
- Verify primer and probe sequences against current circulating strains to identify potential mismatches.
- Check for differences in amplification efficiency due to reagent formulations or instrument platforms.
- Confirm RNA extraction efficiency and potential degradation in sample aliquots.
Root Cause Analysis: Differences in assay design, target selection, or amplification conditions can lead to varying sensitivity, particularly with sequence variations or different viral loads [84] [85].
Issue 3: Poor Reproducibility in Low Viral Load Samples
Problem: Inconsistent detection of samples with low viral loads, leading to variable sensitivity estimates.
Solution:
- Implement stringent quality control measures for reagents, particularly enzymes used in amplification.
- Standardize sample processing protocols across different operators and equipment.
- Increase replicate testing for low positive samples to establish statistical confidence.
- Verify proper calibration of equipment and consistent thermal cycling conditions.
Root Cause Analysis: The stochastic nature of low-copy number RNA targets combined with minor technical variations can significantly impact reproducibility near the assay's limit of detection [84] [68].
Experimental Protocols and Methodologies
VALCOR Implementation Methodology
The implementation of VALCOR follows a standardized procedure to ensure consistent validation across participating laboratories:
Panel Compilation: Provider laboratories compile the VALCOR panel according to the specified composition of 220 clinical specimens and artificial reference materials. Clinical specimens are obtained from COVID-19 patients, healthy carriers of SARS-CoV-2, and negative controls, with appropriate ethical approvals [84].
Reference Testing: All samples in the panel are first tested with an established reference SARS-CoV-2 test at the provider laboratory. The reference test typically follows standard RT-PCR protocols targeting conserved regions of the SARS-CoV-2 genome, such as the E, N, or S genes [84] [68].
Aliquot Preparation: Well-defined aliquots are prepared from the VALCOR samples under controlled conditions to maintain sample integrity. Aliquots are stored at -80°C until shipment [84].
Sample Distribution: Aliquots are shipped to client laboratories using standardized shipping conditions with appropriate cold chain maintenance. Documentation includes detailed information on pre-analytical conditions [84].
Index Assay Testing: Client laboratories test the received panel with the index SARS-CoV-2 assay according to the manufacturer's instructions or established laboratory protocols. Testing must be performed within specified stability windows [84].
Data Analysis: Results from index testing are compared against reference results to calculate sensitivity, specificity, and other performance metrics. Limit of detection is determined based on the dilution series results [84].
Reporting: Comprehensive validation reports are generated, including all performance metrics and any observed limitations or special considerations for the evaluated assay [84].
Molecular Detection Methods for SARS-CoV-2
Within the broader VALCOR framework, various molecular detection methods can be validated. The RT-PCR process typically involves:
RNA Extraction: Viral RNA is extracted from clinical samples using automated or manual extraction methods. Proper extraction is critical for assay performance and must be standardized [68].
Reverse Transcription: Extracted RNA is reverse transcribed into complementary DNA (cDNA) using reverse transcriptase enzymes and specific primers [68].
PCR Amplification: cDNA is amplified using thermal cycling with specific primers and probes targeting SARS-CoV-2 genes. Common targets include:
Detection: Fluorescent probes enable real-time detection of amplification, with cycle threshold (Ct) values indicating viral load [68].
For variant detection, advanced methods like the multiplex RT-PCR assay with allele-specific primer-probe sets can differentiate between variants such as Delta and Omicron by targeting specific mutations in the spike protein's receptor-binding domain (RBD) [85].
Diagram Title: SARS-CoV-2 Molecular Detection Workflow
Research Reagent Solutions and Essential Materials
Key Research Reagents for SARS-CoV-2 Assay Validation
Table: Essential Research Reagents for SARS-CoV-2 Assay Validation
| Reagent Category | Specific Examples | Function in Validation |
|---|---|---|
| Reference Materials | JRC, NIST, ATCC, BEI Resources SARS-CoV-2 RNA reference materials | Provide standardized viral RNA with calibrated concentrations for limit of detection studies and analytical sensitivity assessment [84] |
| Transport Media | Universal Transport Medium (UTM), Phosphate Buffered Saline (PBS), eNAT | Maintain sample integrity during storage and transport; different media may impact assay performance [84] |
| Enzymes for Amplification | Reverse transcriptase, DNA polymerase, hot-start enzymes | Catalyze RNA conversion to cDNA and DNA amplification; critical for sensitivity and specificity [68] |
| Primers and Probes | Oligonucleotides targeting E, N, S, M, ORF1ab genes | Specific binding to SARS-CoV-2 sequences; determine assay specificity and variant detection capability [85] [68] |
| Extraction Reagents | Lysis buffers, wash buffers, elution buffers, magnetic beads | Isolate and purify viral RNA from clinical samples; efficiency impacts overall assay sensitivity [68] |
| Positive Controls | Inactivated SARS-CoV-2 virus, synthetic RNA controls | Verify proper assay function in each run; ensure consistent performance [84] |
| Negative Controls | Nuclease-free water, human genomic DNA, other coronavirus RNA | Identify contamination and assess specificity; critical for false positive determination [84] |
Sample Collection Materials
Proper sample collection is fundamental to reliable SARS-CoV-2 detection. The VALCOR protocol emphasizes standardized collection procedures:
- Swab Types: Nasopharyngeal swabs with long, flexible shafts made of plastic or metal are recommended for proper collection from the nasopharyngeal region [86].
- Personal Protective Equipment (PPE): Guidelines require appropriate PPE including gowns, non-sterile gloves, protective masks, and face shields for healthcare workers performing collections [86].
- Collection Technique: Proper technique involves flexing the patient's head to follow the anatomical trajectory of the nasal passages, lifting the tip of the nose for better visibility, inserting the swab to the level of the posterior wall of the nasopharynx, holding for a few seconds to absorb secretions, and gently withdrawing [86].
Training healthcare personnel in proper collection techniques is essential, as studies show that even with training, average compliance scores for proper procedure are approximately 7.6 out of 10, with over 70% of participants correctly following fundamental steps [86].
The VALCOR protocol represents a significant advancement in the standardization of SARS-CoV-2 assay validation, providing a much-needed framework for comprehensive evaluation of diagnostic tests. By establishing harmonized criteria and methodologies, VALCOR addresses the critical quality gaps that emerged during the rapid deployment of SARS-CoV-2 tests during the pandemic emergency phase.
This systematic approach to validation, incorporating diverse clinical samples and standardized reference materials, generates robust performance data that enables informed decisions about test selection and utilization. The troubleshooting guides and FAQs provided in this technical support resource address common implementation challenges, facilitating proper adoption of the protocol across different laboratory settings.
As SARS-CoV-2 continues to circulate and evolve, and as new emerging pathogens inevitably arise, the principles and methodologies established by VALCOR will serve as an important model for future diagnostic test validation frameworks. The commitment to standardized, evidence-based test evaluation remains essential for effective pandemic preparedness and response, ensuring that diagnostic tests perform reliably in real-world conditions to support clinical and public health decision-making.
Comparative Analysis of Test Performance Across Different Platforms and Settings
| Assay Name | Manufacturer | Target Antibody | Target Antigen | Method | Pooled Diagnostic Odds Ratio (DOR) |
|---|---|---|---|---|---|
| Elecsys Anti-SARS-CoV-2 | Roche | Total Antibody | Not Specified | ECLIA | 1701.56 |
| Elecsys Anti-SARS-CoV-2 N | Roche | Not Specified | Nucleocapsid (N) | ECLIA | 1022.34 |
| Abbott SARS-CoV-2 IgG | Abbott | IgG | Not Specified | CMIA | 542.81 |
| Euroimmun Anti-SARS-CoV-2 S1-IgG | EUROIMMUN | IgG | Spike Subunit 1 (S1) | ELISA | 190.45 |
| LIAISON SARS-CoV-2 S1/S2 IgG | DiaSorin | IgG | Spike Subunits 1 & 2 (S1/S2) | CLIA | 178.73 |
| Euroimmun Anti-SARS-CoV-2 N-IgG | EUROIMMUN | IgG | Nucleocapsid (N) | ELISA | 82.63 |
| Euroimmun Anti-SARS-CoV-2 IgA | EUROIMMUN | IgA | Not Specified | ELISA | 45.91 |
| Test Category | Example Platforms/Methods | Typical Sensitivity | Typical Specificity | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Molecular (PCR) | Cobas 6800/8800, Cobas Liat, RT-PCR | 92.8% - 98.8% [87] [88] | High (Near 100%) | High sensitivity, gold standard, quantitative, multi-target variants more resilient to mutations [89] | Longer turnaround time, requires lab infrastructure, higher cost |
| Rapid Antigen (Ag-RDTs) | Flowflex, Onsite, Hotgen, Covios, SureStatus | ~59% (overall); <30% at low viral loads [87] [90] | ~99% [90] | Speed (minutes), ease of use, low cost, point-of-care | Sensitivity highly dependent on viral load; performance varies by brand and variant [91] [90] |
| Serological (Antibody) | ECLIA (e.g., Roche), CMIA (e.g., Abbott) | Varies by immunoglobulin and antigen (see Table 1) | High | Detects past infection, useful for seroprevalence studies | Not for acute diagnosis; accuracy varies by antibody type [92] |
| Ag-RDT Brand | Omicron BA.1 (PFU/mL) | Omicron BA.5 (PFU/mL) | Delta (PFU/mL) | Alpha (PFU/mL) |
|---|---|---|---|---|
| AllTest, Flowflex, Fortress, etc. | ≤ 2.5 x 10² | ≤ 5.0 x 10² | ≤ 5.0 x 10² | ≤ 5.0 x 10² |
| Core Test, Covios, etc. | > 2.5 x 10² | ≤ 5.0 x 10² | ≤ 5.0 x 10² | ≤ 5.0 x 10² |
| RespiStrip | 5.0 x 10⁴ | 1.0 x 10² | 5.0 x 10² | > 5.0 x 10² |
Troubleshooting Guides and FAQs
FAQ 1: Performance and Variants
Q1: Why does the sensitivity of our rapid antigen test seem to be dropping over time?
A: This could be due to the emergence of new SARS-CoV-2 variants. Viral mutations, particularly in the nucleocapsid (N) protein targeted by most Ag-RDTs, can affect test performance [91]. For instance, evaluations of 34 Ag-RDTs showed that analytical sensitivity varied significantly across variants, with some tests demonstrating reduced performance against specific lineages like Omicron BA.1 [91]. It is critical to use tests that have been clinically validated against circulating variants and to participate in external quality assessment programs to monitor real-world performance.
Q2: What is the primary factor causing false-negative results in rapid antigen tests?
A: The primary factor is low viral load. Studies consistently show that sensitivity is highest in patients with high viral loads (low Cq values on PCR) and drops significantly as viral load decreases. One real-world study reported sensitivity dropped to as low as 5.59% for samples with a Cq ≥ 33 (indicating low viral load), compared to over 90% for samples with a Cq < 20 (high viral load) [90]. This often occurs in the very early or late stages of infection [87].
FAQ 2: Protocols and Procedures
Q3: Our point-of-care molecular test is producing invalid results. What are the first steps in troubleshooting?
A: Follow this systematic troubleshooting guide:
- Reagent Storage and Handling: Confirm all reagents and test components are within their expiration dates and have been stored according to the manufacturer's instructions. Do not use components showing signs of damage or discoloration [21].
- Sample Collection and Volume: Verify that the correct specimen type (e.g., nasopharyngeal swab) was used and that the collection was performed correctly. Ensure the recommended sample volume was applied [21] [88].
- Instrument Calibration: Perform regular quality control and instrument calibration as specified by the manufacturer. If quality control fails, identify and correct issues before proceeding with patient testing [21].
- Cross-Contamination: When processing multiple specimens in batches, change gloves between each specimen to avoid cross-contamination [21].
Q4: How can we verify the performance of a new test in our laboratory, especially against a new variant?
A: A robust verification pipeline should include both analytical and clinical assessments [91] [9].
- Analytical Sensitivity (LoD): Determine the limit of detection using cultured SARS-CoV-2 virus of the relevant variant, quantified by plaque assays (PFU/mL) and RT-qPCR (RNA copies/mL). Compare the LoD to established criteria (e.g., from WHO or MHRA) [91].
- Clinical Sensitivity: Use characterized clinical specimens (e.g., nasopharyngeal swabs in viral transport medium) from patients infected with the variant. The viral load should be determined by RT-qPCR, and test sensitivity should be calculated across a range of viral loads [91] [90].
- Third-Party Verification: Programs like the NIH's Rapid Acceleration of Diagnostics (RADx) provide models for impartial, third-party test verification, which can be particularly valuable for validating performance claims [9].
Experimental Protocols for Test Verification
Objective: To establish the lowest concentration of SARS-CoV-2 virus that an Ag-RDT can reliably detect, using different Variants of Concern (VOCs).
Materials:
- Cultured SARS-CoV-2 virus (e.g., Ancestral/WT, Alpha, Delta, Omicron sub-lineages)
- Cell culture medium (e.g., Dulbecco's Modified Eagle Medium)
- Plaque assay kit for quantification in PFU/mL
- RT-qPCR kit for quantification in RNA copies/mL
- The Ag-RDT(s) to be evaluated
Methodology:
- Virus Culture and Quantification: Propagate each SARS-CoV-2 VOC in a suitable cell line. Quantify the viral stock using a plaque assay to determine the titer in Plaque-Forming Units per mL (PFU/mL). In parallel, extract RNA and use RT-qPCR to determine the concentration in RNA copies/mL.
- Sample Serial Dilution: Serially dilute the viral stock in viral transport medium or a suitable buffer to create a range of concentrations (e.g., 10-fold dilutions).
- Test Execution: Apply each dilution to the Ag-RDT according to the manufacturer's instructions. Include a negative control (diluent only) for each test.
- Data Analysis: The Limit of Detection (LoD) is defined as the lowest viral concentration at which the test returns a positive result. This should be confirmed with multiple replicates (e.g., 5 out of 5 positive results). Compare the LoD in PFU/mL and RNA copies/mL for each VOC against regulatory criteria (e.g., WHO's target of ≤ 1.0 x 10⁶ RNA copies/mL) [91].
Objective: To assess the clinical sensitivity and specificity of an Ag-RDT in a real-world or simulated clinical setting.
Materials:
- Paired nasopharyngeal swabs from symptomatic and/or asymptomatic individuals
- Viral Transport Medium (VTM)
- Ag-RDT kit(s)
- RNA extraction kit
- RT-qPCR system and reagents (e.g., CDC 2019-nCoV RT-PCR Diagnostic Panel)
Methodology:
- Sample Collection: Collect two nasopharyngeal swabs simultaneously from each study participant. One swab is for the Ag-RDT, and the other is placed in VTM for RT-qPCR testing.
- Rapid Testing: Perform the Ag-RDT immediately on the first swab, following the manufacturer's instructions. Record the result.
- RT-qPCR Testing: Store the VTM sample at -80°C if not processed immediately. Extract RNA and run RT-qPCR to detect SARS-CoV-2. Record the Cq (quantification cycle) value as a measure of viral load.
- Data Analysis: Create a 2x2 contingency table to calculate sensitivity, specificity, Positive Predictive Value (PPV), and Negative Predictive Value (NPV). Stratify the results based on the viral load (Cq values) to demonstrate performance across different infection phases [90]. A prospective study design, as used in the Cobas Liat evaluation, ensures real-world relevance [88].
Experimental Workflow and Signalling Pathway Diagrams
Test Verification Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Viral Diagnostic Test Verification
| Item | Function/Benefit | Example Use Case |
|---|---|---|
| Cultured SARS-CoV-2 VOCs | Provides characterized viral material for determining analytical sensitivity (LoD) against specific variants. | Evaluating the impact of N-protein mutations in Omicron on Ag-RDT performance [91]. |
| Plaque Assay Kit | Quantifies infectious virus titer in Plaque-Forming Units per mL (PFU/mL), a critical measure for LoD studies. | Standardizing viral concentrations before testing serial dilutions on Ag-RDTs [91]. |
| RT-qPCR Assay | The gold standard for detecting viral RNA; provides quantitative Cq values to correlate with antigen test results. | Confirming SARS-CoV-2 positivity in clinical samples and stratifying results by viral load [90] [88]. |
| Clinical Specimens in VTM | Archived or fresh patient samples (nasopharyngeal swabs) for real-world clinical sensitivity/specificity studies. | Assessing test performance across a spectrum of viral loads from actual patient infections [90]. |
| Proficiency Testing Panels | External quality control samples used to ensure a laboratory's testing process is accurate and reliable. | Participating in CAP's SARS-CoV-2 Molecular (COV2) or Antigen (COVAG) programs [93]. |
Conclusion
The rigorous verification and validation of viral diagnostic tests are foundational to effective clinical decision-making and public health response. A robust framework, as outlined, must integrate clear regulatory standards, advanced methodological applications, proactive troubleshooting, and comparative performance data. The lessons from the COVID-19 pandemic underscore the urgent need for pre-established networks, harmonized protocols, and adaptable resources to enable rapid evaluation during future outbreaks. Looking ahead, the integration of innovative technologies like AI and decentralized data analysis, coupled with ongoing refinement of validation protocols for novel platforms, will be crucial for advancing diagnostic accuracy, security, and global accessibility.
References
- 1. What is COBIT Framework ? A Detailed Guide [https://sprinto.com/blog/cobit-framework/]
- 2. 7 Phases of COBIT Implementation: A Comprehensive Guide [https://www.theknowledgeacademy.com/blog/cobit-implementation/]
- 3. COBIT 5 Principles: Fully Explained [https://www.theknowledgeacademy.com/blog/cobit-5-principles/]
- 4. FDA, CLIA, and ISO—Which Regulations Apply to Your Clinical Lab? | Today's Clinical Lab [https://www.clinicallab.com/fda-clia-and-iso-which-regulations-apply-to-your-clinical-lab-28044]
- 5. Clinical Laboratory Improvement Amendments (CLIA) | FDA [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/clinical-laboratory-improvement-amendments-clia]
- 6. ISO 15189 Quality Requirements by December 2025 [https://theproficientlab.com/navigating-the-transition-iso-15189-quality-requirements-by-december-2025/]
- 7. Clinical Laboratory Improvement Amendments (CLIA) [https://www.aafp.org/family-physician/practice-and-career/managing-your-practice/clia.html]
- 8. Emergency Use Authorization [https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization]
- 9. The need for new test verification and regulatory support for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9007716/]
- 10. 2025 IFCC Recommendations for IQC [https://www.westgard.com/essays/quality-requirements-and-standards/ifcc-iqc-2025.html]
- 11. MDCG Guidance Documents Overview on Clinical ... [https://www.greenlight.guru/blog/mdcg-documents-overview-clinical-investigations-evaluations]
- 12. Medical Device Clinical Evaluation | MDR Compliance Guide [https://mantrasystems.com/eu-mdr-compliance/clinical-evaluation]
- 13. Advances in the Rapid Diagnostic of Viral Respiratory Tract ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8895598/]
- 14. Rapid diagnostic test: a critical need for outbreak ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11085978/]
- 15. Recent Progress on Rapid Diagnostic Methods for Viral ... [https://www.sciencedirect.com/science/article/pii/S2950248925000811]
- 16. Clinical validation of an AI-based blood testing device for ... [https://www.nature.com/articles/s41591-025-03933-y]
- 17. COVID-19 Test Development and Review [https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/covid-19-test-development-and-review-faqs-testing-sars-cov-2]
- 18. Verify Emergency Use Authorization (EUA) COVID-19 ... [https://asm.org/protocols/eua-covid-19-testing-protocol]
- 19. Challenges and solutions in clinical research during the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10404843/]
- 20. Coronavirus Disease 2019 (COVID-19) and Diagnostic Error [https://psnet.ahrq.gov/primer/coronavirus-disease-2019-covid-19-and-diagnostic-error]
- 21. Guidance for SARS-CoV-2 Rapid Testing in Point-of-Care ... [https://www.cdc.gov/covid/php/lab/point-of-care-testing.html]
- 22. Ensuring accuracy in the development and application of ... [https://www.sciencedirect.com/science/article/pii/S0098299724000347]
- 23. Nucleic Acid Amplification Tests (NAATs) | CDC [https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/lab/naats.html]
- 24. Critical Review of Methods for Isothermal Amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7726081/]
- 25. Isothermal Nucleic Acid Amplification Techniques (INAAT) [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/isothermal-nucleic-acid-amplification.html]
- 26. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 27. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting?srsltid=AfmBOooCTqxZpO9voQy4fxcSu9-gFBGabdShIbT7Txwv-LuBVby9TUAr]
- 28. Real-Time PCR Basics Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/real-time-pcr-basics-support/real-time-pcr-basics-support-troubleshooting.html]
- 29. Validation study of a novel, rapid, open platform real-time ... [https://www.nature.com/articles/s41598-025-93565-6]
- 30. Laboratory validation of a clinical metagenomic sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6499319/]
- 31. Empirical assessment of the enrichment-based ... [https://www.nature.com/articles/s41598-024-75120-x]
- 32. Optimization and validation of sample preparation for ... [https://pubmed.ncbi.nlm.nih.gov/28789678/]
- 33. Optimization and validation of sample preparation for ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-017-0317-z]
- 34. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 35. Evaluation of the Effects of Library Preparation Procedure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8510527/]
- 36. Verification and validation of diagnostic laboratory tests in ... [https://www.sciencedirect.com/science/article/pii/S1386653207002582]
- 37. Verification and validation of diagnostic laboratory tests in ... [https://pubmed.ncbi.nlm.nih.gov/17766174/]
- 38. A unified framework for diagnostic test development and ... [https://www.nature.com/articles/s43856-024-00691-9]
- 39. Troubleshooting Common Antigen Self-Test Kit Problems: [https://cetrixstore.com/blogs/news/troubleshooting-common-antigen-self-test-kit-problems-a-comprehensive-guide?srsltid=AfmBOorX_4XgjeYAEUIZ4tV08ukB7Cqe9or4LzY5SXB2As7T6OwJDvUR]
- 40. Quality issues with malaria rapid diagnostic test accessories ... [https://malariajournal.biomedcentral.com/articles/10.1186/s12936-017-1820-1]
- 41. Real-World Performance of COVID-19 Antigen Tests [https://xmed.jmir.org/2025/1/e68376]
- 42. Malaria Rapid Diagnostic Tests: Literary Review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8145891/]
- 43. Overcoming diagnostic and data privacy challenges in viral ... [https://www.frontiersin.org/journals/virology/articles/10.3389/fviro.2025.1625855/full]
- 44. Cross paradigm fusion of federated and continual learning ... [https://www.nature.com/articles/s41598-025-06077-8]
- 45. Open problems in medical federated learning [https://www.sciencedirect.com/org/science/article/pii/S1744008422000167]
- 46. A privacy-preserving dependable deep federated learning ... [https://www.nature.com/articles/s41598-025-89612-x]
- 47. AI System Finds Crucial Clues for Diagnoses in Electronic ... [https://www.mountsinai.org/about/newsroom/2025/ai-system-finds-crucial-clues-for-diagnoses-in-electronic-health-records]
- 48. Federated learning as a smart tool for research on infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11580691/]
- 49. Artificial Intelligence in Infectious Disease Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562594/]
- 50. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 51. Expert Pre-Analytical Work Processing - Sampled [https://sampled.com/the-critical-role-of-pre-analytical-work/]
- 52. Pre-Analytical Variables [https://www.practical-haemostasis.com/Quality%20Assurance/pre_analytical_variables.html]
- 53. Non-disease variables [https://eclinpath.com/test-basics/non-disease-variables/]
- 54. Preanalytical Variables and Their Influence on the Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6238383/]
- 55. The Implications of False Positives in Diagnostic Testing [https://www.apbiocode.com/false-positives/]
- 56. Antibody cross-reactivity among alphaviruses clinical practice [https://pubmed.ncbi.nlm.nih.gov/40866148/]
- 57. Interpreting Diagnostic Tests for COVID-19 in 2025 [https://carelife.md/interpreting-diagnostic-tests-for-covid-19-in-2025-what-you-need-to-know/]
- 58. Nasal biomarker testing to rule out viral respiratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216728/]
- 59. Evaluating the impact of trade-offs in diagnostic test accuracy ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11273-y]
- 60. 2025 Outlook: Emerging Viruses & Next-Gen Respiratory DX [https://meridianbioscience.com/lifescience-blog/emerging-viruses-next-generation-of-respiratory-diagnostics-2025-outlook/]
- 61. 5 Strategies for Managing Supply Chain Disruptions [https://www.netsuite.com/portal/resource/articles/erp/handle-supply-chain-disruptions.shtml]
- 62. Supply chain disruption and how to manage it [https://www.thecorporategovernanceinstitute.com/insights/guides/supply-chain-disruption-and-how-to-manage-it/?srsltid=AfmBOor5_Ib1OFOIHGqc-s6k9xfE3oxPgc0Y4Ztns4xuAEh6KCGUJRNc]
- 63. Gartner Identifies Three Actions for Supply Chain Leaders ... [https://www.gartner.com/en/newsroom/press-releases/2024-06-11-gartner-identifies-three-actions-for-supply-chain-leaders-to-mitigate-long-term-resource-constraints]
- 64. Supply Chain Disruptions: 10 Tips to Improve Resilience [https://www.sap.com/resources/supply-chain-disruption-10-tips]
- 65. Adapting to disruptions: Managing supply chain resilience ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10793953/]
- 66. Disruptions in Supply Chain: How to Manage and Avoid [https://www.pelico.ai/resources/our-articles/disruptions-in-supply-chain-how-to-manage-and-avoid]
- 67. Find the right sample: A study on the versatility of saliva and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6311079/]
- 68. Advances and Challenges in SARS-CoV-2 Detection [https://www.mdpi.com/2075-4418/14/5/519]
- 69. Comparative analysis of various clinical specimens in ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0249408]
- 70. Current trends and challenges in point-of-care urinalysis ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993622002692]
- 71. Next-Generation Nucleic Acid-Based Diagnostics for Viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388196/]
- 72. Portable molecular diagnostic platform for rapid point-of- ... [https://www.nature.com/articles/s41467-025-57647-3]
- 73. Validation FAQ (Frequently Asked Questions about ... [https://www.ofnisystems.com/services/validation/validation-faq/]
- 74. 7 Common Validation Questions, Answered [https://dicksondata.com/common-validation-questions?srsltid=AfmBOooxccphAj3fVtW-QpMLME406xXvzmlPHR8mX1cY425OlaOOKED0]
- 75. Clinical Validation of an Artificial Intelligence–Based Tool ... [https://www.researchprotocols.org/2023/1/e44650]
- 76. Validation and real-world clinical application of an artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9723672/]
- 77. The Most Common Pitfalls in Verification and Validation [https://criticalsoftware.com/en/news/common-pitfalls-in-verification-validation]
- 78. Design and development of a systematic validation ... [https://www.sciencedirect.com/science/article/pii/S020852162500066X]
- 79. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive Values and Likelihood Ratios - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 80. Sensitivity and specificity - Wikipedia [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 81. Guidance on Performing Routine Diagnostic Testing for ... [https://www.cdc.gov/viral-hemorrhagic-fevers/php/laboratories/guidance-on-performing-routine-diagnostic-testing-for-patients-with-suspected-vhfs-or-other.html]
- 82. Validating a New Test in Your Laboratory [https://www.apbiocode.com/diagnostic-test-validation/]
- 83. Medical viruses: diagnostic techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10334571/]
- 84. VALCOR: a protocol for the validation of SARS-corona virus-2 ... [https://archpublichealth.biomedcentral.com/articles/10.1186/s13690-022-00869-4]
- 85. Development and validation of novel RT-PCR assay for ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000933]
- 86. Practical Challenges in the Diagnosis of SARS-CoV-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12196300/]
- 87. Antigen testing vs PCR: less haste, more speed please [https://www.cepheid.com/en-US/insights/insight-hub/respiratory-health/2025/09/antigen-testing-vs-pcr-less-haste-more-speed-please.html]
- 88. Detection of SARS-CoV-2 in Settings Including Point-of-Care [https://link.springer.com/article/10.1007/s40121-025-01186-3]
- 89. Molecular Diagnostic Tests for SARS-CoV-2 [https://www.fda.gov/medical-devices/covid-19-emergency-use-authorizations-medical-devices/in-vitro-diagnostics-euas-molecular-diagnostic-tests-sars-cov-2]
- 90. Real-world accuracy of SARS-CoV-2 antigen detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12036026/]
- 91. Comparison of the analytical and clinical sensitivities of 34 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502672/]
- 92. An Indirect Comparison of Diagnostic Accuracy for Seven ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418076/]
- 93. SARS-CoV-2 Proficiency Testing/External Quality ... [https://www.cap.org/laboratory-improvement/proficiency-testing/sars-cov-2-proficiency-testing-programs]