Viral Load Quantification Methods: Correlation, Challenges, and Clinical Applications in Modern Biomedicine
This article provides a comprehensive analysis of viral load quantification methodologies, a cornerstone of clinical virology and therapeutic monitoring.
Viral Load Quantification Methods: Correlation, Challenges, and Clinical Applications in Modern Biomedicine
Abstract
This article provides a comprehensive analysis of viral load quantification methodologies, a cornerstone of clinical virology and therapeutic monitoring. We explore the foundational principles of molecular-based techniques, including RT-qPCR and ddPCR, and their critical applications in managing infections such as HIV, SARS-CoV-2, and transplant-related viruses. The content delves into persistent standardization challenges, interassay variability, and the impact of different sample matrices on result accuracy. By presenting comparative data and validation strategies, this review serves as a vital resource for researchers, scientists, and drug development professionals seeking to optimize viral load quantification for improved diagnostic reliability, treatment efficacy assessment, and public health surveillance.
The Bedrock of Viral Load Quantification: Principles, Significance, and Standardization Hurdles
Viral load (VL) refers to the quantity of a virus in a standardized volume of blood or other bodily fluid [1]. In clinical practice, it is a critical biomarker for monitoring the progression of viral infections and the effectiveness of antiviral therapies. For HIV, viral load "measures the quantity of HIV RNA in the blood," with results expressed as the number of copies per milliliter (copies/mL) of blood plasma [1]. The primary goal of antiretroviral therapy (ART) is suppression of the HIV viral load, making VL monitoring key to assessing treatment success [1].
The World Health Organization (WHO) has established three key categories for interpreting HIV viral load measurements [2]:
- Unsuppressed: >1000 copies/mL
- Suppressed: Detected but ≤1000 copies/mL
- Undetectable: Viral load not detected by the test used
Achieving an undetectable viral load is a critical public health goal, as people living with HIV who maintain this status have zero risk of transmitting HIV to their sexual partner(s) [2]. Those with a suppressed but detectable viral load have almost zero or negligible risk of transmission [2].
Clinical and Public Health Significance of Viral Load
Prognostic Value and Treatment Monitoring
Viral load serves as a crucial prognostic indicator across viral infections. In HIV management, monitoring a person's viral load is fundamental to assessing the success of ART [1]. Sicker patients generally have more virus than those with less advanced disease, making viral load a key marker of disease progression [1]. The global 95-95-95 targets emphasize achieving viral suppression in 95% of people receiving ART, recognizing its importance for both individual health and epidemic control [3].
Viral Load in Public Health Surveillance
Beyond individual patient care, population-level viral load data provides powerful insights for public health. The distribution of cycle threshold (Ct) values from reverse transcription quantitative polymerase chain reaction (RT-qPCR) testing can be used for epidemic nowcasting [4]. Ct values inversely correlate with viral load; lower Ct values indicate higher viral loads and typically suggest recent onset of infection [4]. During an epidemic, a population-level sample with predominantly low Ct values (high viral loads) indicates most sampled infections are recent, corresponding to a growing epidemic. Conversely, predominantly high Ct values (low viral loads) suggest a declining epidemic [4]. This approach complements traditional case count surveillance and has been successfully applied to track SARS-CoV-2 trends [4].
Table 1: Clinical and Public Health Applications of Viral Load Monitoring
| Application Area | Primary Use of Viral Load Data | Key Thresholds/Targets |
|---|---|---|
| HIV Treatment Monitoring | Assess effectiveness of antiretroviral therapy (ART) | Undetectable: Target for individual treatmentUnsuppressed (>1000 copies/mL): Indicates need for intervention [2] |
| Prevention of Transmission | Evaluate risk of HIV transmission | Undetectable = Zero sexual transmission risk [2] |
| Epidemic Surveillance | Nowcast epidemic growth rates using population Ct values | Lower average Ct (higher VL) = Growing epidemicHigher average Ct (lower VL) = Declining epidemic [4] |
| Therapeutic Efficacy | Monitor response to antiviral treatment (e.g., for HDV) | Precise quantification at low concentrations is critical [5] |
Quantitative Methods for Viral Load Measurement
Established and Emerging Methodologies
Accurate viral load quantification relies on sophisticated molecular techniques. The field is dominated by PCR-based methods, with ongoing innovations enhancing precision and accessibility.
Table 2: Comparison of Viral Load Quantification Technologies
| Method | Principle | Key Advantages | Key Limitations |
|---|---|---|---|
| Real-Time RT-PCR | Quantitative PCR using fluorescent probes and standard curves for quantification [6]. | Considered the gold standard; widely automated and established [6]. | Quantification depends on standard curves, introducing variability; susceptible to PCR inhibitors [6]. |
| Digital PCR (dPCR) | Partitions sample into thousands of nanoreactions for absolute target counting without standard curves [6]. | Superior accuracy and precision, especially for medium/high viral loads; less susceptible to inhibitors [6]. | Higher costs; reduced automation compared to Real-Time RT-PCR [6]. |
| Point-of-Care (POC) Tests | Simplified, rapid tests for use in decentralized settings [7]. | Increases monitoring coverage in resource-limited settings; uses alternative samples (e.g., dried blood spots) [7] [2]. | May have different performance characteristics compared to laboratory-based tests [2]. |
Performance Comparison: dPCR vs. Real-Time RT-PCR
A 2025 comparative study of respiratory virus diagnostics during the 2023-2024 "tripledemic" provided robust experimental data on the performance of dPCR versus Real-Time RT-PCR [6]. The study analyzed 123 respiratory samples positive for influenza A, influenza B, RSV, or SARS-CoV-2, stratified by Ct values into high (Ct ≤25), medium (Ct 25.1–30), and low (Ct >30) viral load categories [6].
Table 3: Experimental Performance Data: dPCR vs. Real-Time RT-PCR [6]
| Virus | Viral Load Category | Method with Superior Accuracy | Key Performance Findings |
|---|---|---|---|
| Influenza A | High | dPCR | dPCR demonstrated superior accuracy for high viral loads. |
| Influenza B | High | dPCR | dPCR demonstrated superior accuracy for high viral loads. |
| SARS-CoV-2 | High | dPCR | dPCR demonstrated superior accuracy for high viral loads. |
| RSV | Medium | dPCR | dPCR showed greater consistency and precision for quantifying intermediate viral levels. |
| All Viruses | - | dPCR | dPCR showed greater overall consistency and precision than Real-Time RT-PCR. |
The study concluded that dPCR offers absolute quantification without standard curves and demonstrates superior accuracy, particularly for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV [6]. However, the authors noted that the routine implementation of dPCR is currently limited by higher costs and reduced automation compared to Real-Time RT-PCR [6].
Experimental Protocols for Viral Load Quantification
Detailed dPCR Workflow for Respiratory Viruses
The following protocol is adapted from a 2025 study comparing dPCR and Real-Time RT-PCR for respiratory virus quantification [6].
1. Sample Collection and Storage
- Collect nasopharyngeal swabs or other respiratory samples (e.g., bronchoalveolar lavage) in appropriate viral transport media.
- Store samples at 4°C for processing within 72 hours or at -80°C for long-term storage.
2. Nucleic Acid Extraction
- Use an automated extraction system, such as the KingFisher Flex system.
- Employ a viral RNA/DNA extraction kit, such as the MagMax Viral/Pathogen kit.
- Elute nucleic acids in nuclease-free water or the elution buffer provided by the kit.
3. Digital PCR Assay Setup
- Platform: Use a nanowell-based dPCR system (e.g., QIAcuity from QIAGEN).
- Reaction Mix: Prepare a multiplex dPCR reaction containing:
- dPCR supermix
- Optimized primer-probe sets specific for each target (e.g., influenza A, influenza B, RSV, SARS-CoV-2)
- An internal control to monitor extraction and amplification efficiency
- The extracted nucleic acid template
- Partitioning: Load the reaction mix into a nanowell plate, which partitions the sample into approximately 26,000 individual reactions.
4. Endpoint PCR Amplification
- Run the partitioned plate on a thermal cycler using cycling conditions optimized for the primer-probe sets and dPCR instrument.
- Standard cycling conditions include: reverse transcription, polymerase activation, and 40-45 cycles of denaturation/annealing-extension.
5. Fluorescence Reading and Data Analysis
- After amplification, the dPCR instrument reads the fluorescence in each nanowell.
- Use instrument software (e.g., QIAcuity Suite Software) to analyze the fluorescence data and determine the absolute copy number (copies/μL) of each target in the original sample based on the ratio of positive to negative wells (Poisson statistics).
HDV RNA Quantification Assay Comparison Protocol
A 2025 quality control study highlights the critical protocol elements for reliable HDV RNA monitoring, which is paramount for assessing response to anti-HDV therapy [5].
Objective: To compare the diagnostic performance of different quantitative HDV-RNA assays used in clinical practice.
Methodology:
- Sample Panels: Two panels were distributed to 30 testing centers.
- Panel A: 8 serial dilutions of a WHO/HDV standard (range: 0.5–5.0 log10 IU/mL).
- Panel B: 20 clinical samples (range: 0.5–6.0 log10 IU/mL).
- Participating Assays: Multiple commercial assays (e.g., RoboGene, EurobioPlex, RealStar, AltoStar, Bosphore) and in-house assays.
- Performance Metrics:
- Sensitivity: Determined by the 95% Limit of Detection (LOD).
- Precision: Calculated as intra- and inter-run Coefficient of Variation (CV).
- Accuracy: Assessed by the difference between expected and observed HDV-RNA levels.
- Linearity: Evaluated by linear regression analysis (R²).
Key Findings:
- Sensitivity: The 95% LOD varied significantly across assays, from 3 IU/mL (AltoStar) to 100-316 IU/mL (EuroBioplex).
- Accuracy: Six assays showed minimal bias (<0.5 log10 IU/mL), while others had >1 log10 underestimations.
- Precision: RealStar, Bosphore-on-InGenius, and EurobioPlex showed the highest precision (mean intra-run CV <20%).
- Linearity: Most assays showed good linearity (R² >0.90) overall, but performance at low viral loads (<1000 IU/mL) varied.
This study underscores the heterogeneous sensitivities of different HDV-RNA assays, which can hamper proper quantification, particularly at low viral loads, and raises the need for improved assay performance [5].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents and Materials for Viral Load Research
| Reagent/Material | Function in Viral Load Assays | Exemplars / Notes |
|---|---|---|
| Automated Nucleic Acid Extraction Systems | Isolate viral RNA/DNA from clinical samples with high purity and consistency, minimizing cross-contamination. | STARlet Seegene platform [6], KingFisher Flex system [6]. |
| Extraction Kits | Contain optimized buffers and magnetic beads for specific binding and elution of nucleic acids. | MagMax Viral/Pathogen kit [6], STARMag Universal Cartridge Kit [6]. |
| dPCR Supermix | A ready-to-use master mix containing polymerase, dNTPs, and stabilizers optimized for partitioning and endpoint amplification. | QIAcuity PCR Master Mix [6]. |
| Primer-Probe Sets | Target-specific oligonucleotides for amplification and fluorescent detection of the viral genome. | Commercially validated, multiplexable sets for viruses (e.g., Influenza A/B, RSV, SARS-CoV-2) [6]. |
| dPCR Partitioning Plates/Cartridges | Microfluidic chips or plates that physically partition the PCR reaction into thousands of individual reactions. | QIAcuity nanoplates [6]. |
| WHO International Standards | Provide a universal reference for calibrating assays, enabling comparability of results across labs and methods. | WHO/HDV standard [5]. |
| Internal Controls | Non-target nucleic sequences added to the sample to monitor the efficiency of nucleic acid extraction and amplification. | Critical for identifying PCR inhibition and validating negative results [6]. |
Viral load quantification remains a cornerstone of modern virology, with critical applications spanning individual patient prognosis, therapeutic monitoring, and public health surveillance. While Real-Time RT-PCR continues to be the workhorse technology in clinical laboratories, Digital PCR is emerging as a more precise alternative for absolute quantification, particularly beneficial for research and resolving equivocal results [6]. The choice of methodology must balance accuracy, cost, and throughput requirements.
Future progress hinges on standardizing assays across platforms, as evidenced by the variability in HDV RNA testing [5], and on improving access to reliable viral load monitoring in decentralized settings through point-of-care technologies and alternative sample types [7] [2]. As viral load research continues to evolve, its integration into clinical and public health practice will be fundamental to managing existing epidemics and preparing for future viral threats.
The accurate quantification of viral load is a cornerstone of modern molecular diagnostics, profoundly impacting patient management, therapeutic monitoring, and public health surveillance [8]. For years, Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) has served as the gold standard for detecting RNA viruses. However, the evolving demands of clinical research, particularly the need for absolute quantification and enhanced sensitivity for low viral loads, have highlighted certain limitations of this technique [9]. Digital PCR (dPCR), and its droplet-based counterpart ddPCR, represent a paradigm shift in nucleic acid quantification, offering a fundamentally different approach that does not rely on external calibration curves [10]. This guide objectively compares the performance of RT-qPCR and ddPCR platforms, framing the analysis within the critical context of viral load quantification method correlation research for an audience of researchers, scientists, and drug development professionals.
Fundamental Principles and Workflows
RT-qPCR is a relative quantification method. It works by reverse transcribing RNA into complementary DNA (cDNA), which is then amplified in a real-time thermal cycler. The instrument monitors fluorescence during each PCR cycle, and the cycle threshold (Ct) at which the fluorescence crosses a predefined level is used to estimate the starting quantity of the target nucleic acid. This estimation requires a standard curve constructed from samples of known concentration [10] [9]. The entire process occurs in a single, bulk reaction, making its efficiency susceptible to inhibitors present in the sample and sequence variations affecting primer binding [8].
ddPCR, a variant of dPCR, achieves absolute quantification through sample partitioning. The reaction mixture is divided into thousands to millions of nanoliter-sized droplets, with each droplet functioning as an individual PCR reactor [11]. After end-point PCR amplification, the droplets are analyzed to count the number that contains the target sequence (positive) versus those that do not (negative). The absolute concentration of the target nucleic acid, in copies per microliter of input, is then calculated directly using Poisson statistics, eliminating the need for a standard curve [10] [12].
The workflow for nanoplate-based dPCR systems, such as the QIAcuity, integrates partitioning, thermocycling, and imaging into a single, fully automated instrument, enabling a streamlined process from sample to result in under two hours [12].
Side-by-Side Technical Comparison
Table 1: Core Technical Characteristics of RT-qPCR and ddPCR.
| Feature | RT-qPCR | ddPCR |
|---|---|---|
| Quantification Type | Relative (requires standard curve) [10] [9] | Absolute (no standard curve) [10] [12] |
| Measurement Basis | Cycle threshold (Ct) during exponential phase [12] | End-point counting of positive partitions [11] [12] |
| Dynamic Range | Broad [10] | Limited by number of partitions [8] |
| Sensitivity & Precision | High for most routine applications | Superior for rare targets and low-abundance sequences [10] [12] |
| Tolerance to Inhibitors | Susceptible to PCR inhibitors [10] | High tolerance due to sample partitioning [10] [8] |
| Tolerance to Amplification Efficiency Variations | Highly affected [12] | Largely unaffected [12] |
| Detection of Rare Mutations | Mutation rate >1% [12] | Mutation rate ≥0.1% [12] |
| Throughput & Speed | High throughput, established fast protocols [10] | Traditionally lower throughput; newer nanoplate systems offer higher speed and automation [6] [12] |
| Cost Considerations | Lower per-sample cost, well-established [10] | Higher cost per sample, though becoming more competitive [6] |
Experimental Data in Viral Load Quantification
Performance in Clinical and Environmental Surveillance
Recent studies directly comparing these platforms provide compelling evidence of their respective performances. A 2025 study on respiratory viruses (Influenza A/B, RSV, SARS-CoV-2) found that dPCR demonstrated superior accuracy and precision, particularly for samples with high viral loads and medium loads of RSV [6]. The technology showed greater consistency than RT-qPCR in quantifying intermediate viral levels, which is crucial for accurate disease progression monitoring [6].
In environmental applications, such as wastewater surveillance, ddPCR's superior sensitivity is vital for early outbreak detection. One study reported that for the trace detection of SARS-CoV-2 RNA in wastewater, the assay limit of detection (ALOD) for ddPCR was approximately 2–5 times lower than that for RT-qPCR [13]. In another study analyzing 50 wastewater samples with low viral load, an RT-ddPCR assay detected SARS-CoV-2 in all 50 samples, whereas RT-qPCR only concurrently detected the virus in 21 samples, with 4 samples testing negative [11]. This demonstrates ddPCR's power in low-prevalence and trace-level monitoring scenarios.
Impact on Clinical Trial Assessment
A pivotal 2025 study underscored how the choice of molecular platform can directly influence the assessment of antiviral drug efficacy [9]. In clinical trials for the drug Azvudine, the viral load quantified by RT-qPCR showed no significant difference between the antiviral-treated and placebo groups. However, when the same samples were analyzed using ddPCR, a significant reduction in viral load was observed in the treated group on days 3, 5, 7, and 9 post-treatment [9]. This critical finding indicates that ddPCR's enhanced sensitivity and absolute quantification can uncover treatment effects that may be obscured by the variability and logarithmic approximations inherent in RT-qPCR standard curve-based quantification.
Table 2: Summary of Key Comparative Study Findings.
| Study Context | Key Finding | Implication |
|---|---|---|
| Respiratory Virus Detection (2025) [6] | dPCR showed superior accuracy for high viral loads (Influenza A/B, SARS-CoV-2) and medium loads (RSV). | Enhanced diagnostic accuracy and better understanding of co-infection dynamics. |
| Wastewater Surveillance [11] [13] | RT-ddPCR ALOD 2-5x lower than RT-qPCR; higher detection rates in low-prevalence samples. | More effective early warning system for community-level outbreaks. |
| Antiviral Clinical Trial (2025) [9] | ddPCR revealed significant viral load reduction post-treatment; RT-qPCR showed no significant difference. | More sensitive and reliable measurement of therapeutic efficacy in drug development. |
| SARS-CoV-2 Variant Detection [11] | RT-ddPCR assay showed high repeatability (CV <10%) and low limits of detection (e.g., ~4 copies/reaction for N gene). | Robust tool for precise quantification and tracking of emerging variants. |
Experimental Protocols for Method Comparison
For researchers seeking to validate or compare these technologies, the following outlines a generalized experimental protocol based on cited studies.
Sample Collection and Nucleic Acid Extraction
- Sample Type: The choice of sample matrix (e.g., nasopharyngeal swabs, bronchoalveolar lavage, wastewater) should reflect the research question [6] [11]. For wastewater, a concentration step (e.g., ultrafiltration) is often required prior to extraction [11].
- RNA Extraction: Use commercial kits designed for viral RNA purification (e.g., RNeasy Mini Kit, QIAamp Viral RNA Mini Kit) from automated or manual platforms [6] [11] [13]. It is critical to include an internal control during extraction to monitor efficiency and potential inhibition [13].
- Sample Stratification: To ensure a comprehensive comparison, stratify samples based on RT-qPCR Ct values into categories such as high (Ct ≤ 25), medium (Ct 25.1–30), and low (Ct > 30) viral load [6].
Assay Design and Platform-Specific Workflows
- Primer/Probe Design: Design or select primer-probe sets targeting conserved viral genes (e.g., N and S genes for SARS-CoV-2) [11]. For multiplexing, use fluorophores with non-overlapping emission spectra.
- RT-qPCR Workflow:
- Reaction Setup: Prepare a master mix containing reverse transcriptase, DNA polymerase, dNTPs, primers, probes, and buffer. Aliquot into reaction wells and add template RNA.
- Thermocycling: Run on a real-time cycler with a program typically including reverse transcription, polymerase activation, and 40-45 cycles of denaturation, annealing, and extension.
- Data Analysis: Generate a standard curve from serial dilutions of a known standard. Determine the quantity of unknown samples by interpolation from the standard curve based on their Ct values [11] [9].
- ddPCR Workflow:
- Reaction Setup: Prepare a similar master mix, often optimized for the specific digital platform.
- Partitioning: On a droplet generator or nanoplate system, partition each sample reaction mixture into thousands of individual droplets or nanowells [6] [11].
- PCR Amplification: Perform end-point PCR on the partitioned sample.
- Droplet Reading and Analysis: Run the plate on a droplet reader that counts the positive and negative partitions for each sample. The software then applies Poisson statistics to calculate the absolute concentration of the target (copies/μL) [11] [12].
Data Analysis and Correlation
- Statistical Comparison: Use correlation analyses (e.g., Spearman's rank correlation) and measures of agreement (e.g., Cohen's kappa) to compare the quantitative results and detection rates between the two platforms [6] [11].
- Sensitivity and LOD Calculation: Determine the absolute limit of detection (LOD) for each platform by testing serial dilutions of the target nucleic acid. The LOD is typically defined as the lowest concentration at which ≥95% of replicates are positive [11].
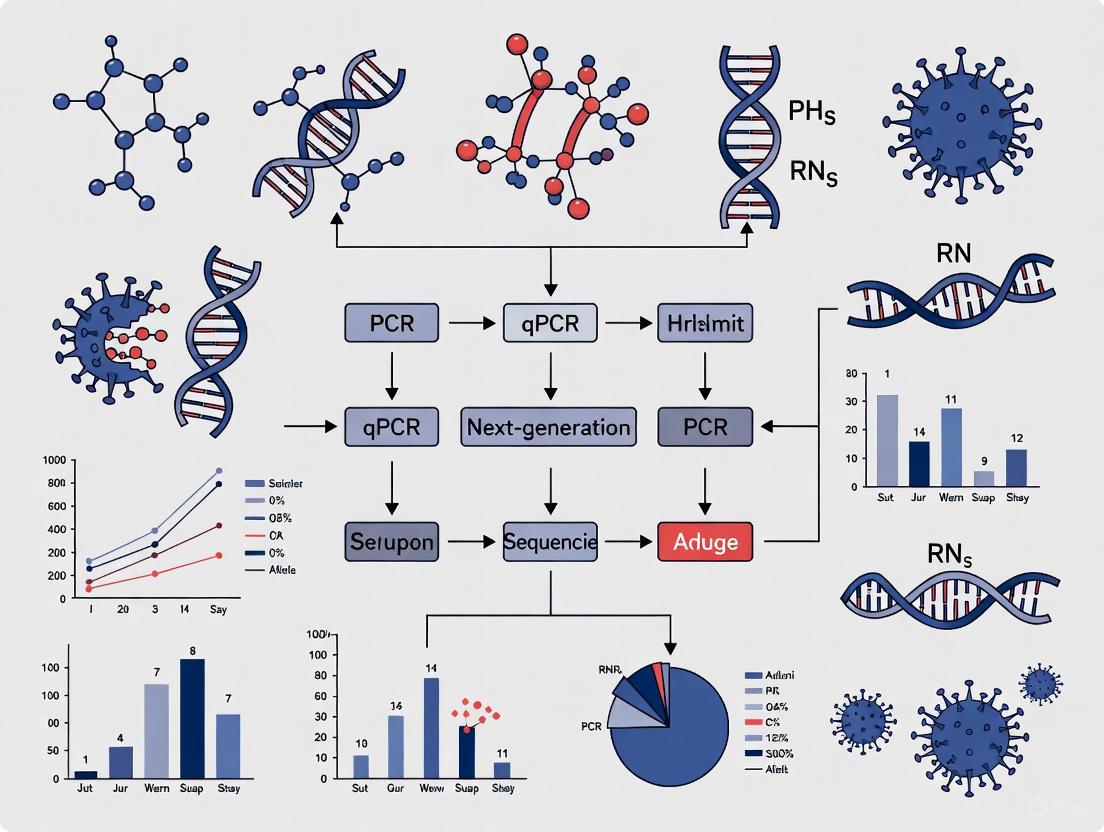
Diagram Title: Comparative Workflow of RT-qPCR and ddPCR for Viral Load Quantification
Essential Research Reagent Solutions
Successful implementation and comparison of these platforms depend on a suite of critical reagents and kits.
Table 3: Key Research Reagents for Viral Load Quantification Studies.
| Reagent / Kit | Function | Example Use Case |
|---|---|---|
| Viral RNA Extraction Kits (e.g., QIAamp Viral RNA Mini, RNeasy Mini, MagMax Viral/Pathogen) | Purification and isolation of viral RNA from complex sample matrices like swabs or wastewater. | Essential first step for all downstream molecular analysis; ensures high-quality, inhibitor-free RNA [11] [13]. |
| One-Step RT-qPCR Master Mix | Contains reverse transcriptase and hot-start DNA polymerase in an optimized buffer for direct amplification of RNA targets. | Streamlines the RT-qPCR workflow, reducing pipetting steps and potential contamination [13]. |
| ddPCR Supermix (for Probes) | Optimized reaction mix for digital PCR applications, ensuring stable droplet formation and efficient amplification. | Critical for generating robust and reproducible data on droplet-based systems [11]. |
| Primer/Probe Sets | Sequence-specific oligonucleotides for target detection. Probes are typically labeled with fluorophores (FAM, VIC/HEX). | Fundamental for assay specificity; dual-labeled probe sets allow for multiplex detection of different viral targets [11]. |
| Quantified RNA Standards | Synthetic or biologically derived RNA of known concentration for generating standard curves. | Required for absolute quantification and determining the assay's limit of detection (LOD) in RT-qPCR [9]. |
| Inhibition Control (e.g., Murine Hepatitis Virus - MHV) | Exogenous control added to the sample to monitor for the presence of PCR inhibitors. | Added to samples prior to extraction to assess RNA extraction efficiency and identify inhibition in downstream assays [13]. |
Both RT-qPCR and ddPCR are powerful molecular techniques with distinct strengths that recommend them for different applications within viral load quantification research. RT-qPCR remains the workhorse for high-throughput, routine diagnostics due to its broad dynamic range, established protocols, and lower cost [10]. In contrast, ddPCR excels in scenarios demanding high precision, absolute quantification without standards, superior sensitivity for low viral loads, and resilience to inhibitors or sequence variations [6] [11] [9].
The choice between platforms should be guided by the specific research objectives. For drug development professionals, the ability of ddPCR to reveal subtle changes in viral load during antiviral therapy trials makes it an invaluable tool for assessing treatment efficacy [9]. For public health researchers, its enhanced sensitivity is crucial for wastewater-based epidemiology and early outbreak detection [11] [13]. As the field advances, the trend is not necessarily toward replacement but toward the complementary use of both technologies, leveraging their respective advantages to paint a more complete and accurate picture of viral dynamics.
Viral load quantification represents a critical pillar in the management and treatment of viral infections, serving as a cornerstone for clinical decision-making, treatment efficacy monitoring, and drug development. For both Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV), precise viral load measurement is indispensable for guiding treatment initiation, assessing therapeutic success, and preventing drug resistance [14]. Despite technological advancements, the diagnostic landscape remains fragmented with multiple platforms, reagents, and methodologies, creating substantial challenges in result interpretation, clinical trial data comparison, and patient management across different sites and studies.
This variability is particularly problematic for global health initiatives and multi-center clinical trials, where standardized outcomes are essential for valid data comparison. The World Health Organization's 2030 goals of reaching 95% HIV diagnosis/treatment coverage and reducing HCV incidence by 90% face significant obstacles due to insufficient diagnostic tools and lack of harmonization across testing platforms [14]. This article provides a comprehensive comparison of current viral load quantification technologies for HIV and HCV, analyzes their performance characteristics, and underscores the imperative for standardized approaches in viral load monitoring to advance both clinical management and drug development pipelines.
Performance Comparison of Viral Load Assays
HCV RNA Quantification Assays
The performance characteristics of four commercially available HCV RNA quantification reagents were evaluated using multiple serum panels to assess analytical sensitivity, specificity, precision, and genotype inclusivity. These reagents employed real-time PCR technology with the PCR-fluorescence probing method commonly used in diagnostic laboratories [15].
Table 1: Performance Characteristics of HCV RNA Quantification Assays
| Reagent | Analytical Sensitivity | Analytical Specificity | Limit of Detection (LOD) | Intra-assay CV | Inter-assay CV |
|---|---|---|---|---|---|
| A | 100% | 100% | 25 IU/mL | 1.48-4.37% | 1.74-4.84% |
| B | 100% | 100% | 50 IU/mL | 1.48-4.37% | 1.74-4.84% |
| C | 100% | 100% | 50 IU/mL | 1.48-4.37% | 1.74-4.84% |
| D | 100% | 100% | 50 IU/mL | 1.48-4.37% | 1.74-4.84% |
All four reagents demonstrated 100% analytical sensitivity and specificity (95% CI: 79.95-100), with no cross-reactivity to common interfering substances or viruses such as HBV and HIV. The reagents showed strong linear correlations (R² > 0.95) between measured and expected HCV RNA levels across their respective quantitative ranges [15]. The evaluation utilized seven distinct serum panels: basic, analytical specificity, seroconversion, analytical sensitivity, precision, genotype qualification, and linearity panels to ensure comprehensive assessment.
For genotype detection, all assays successfully detected and quantified HCV genotypes 1-6, which is crucial given the geographical distribution of HCV genotypes. In China, for instance, GT1b and GT2a are the most common subtypes, though emerging subtypes (GT3 and GT6) in southern regions necessitate genotype-inclusive diagnostic assays to prevent detection failures [15]. The robust performance across diverse genotypes ensures utility in global contexts and multi-center trials.
HIV-1 Viral Load Assays
HIV-1 viral load monitoring has evolved significantly, with current research focusing on both improved laboratory methods and alternative sampling approaches to increase testing accessibility.
Table 2: HIV-1 Viral Load Assay Performance and Method Comparisons
| Method/Assay | Sample Type | Correlation with Reference | Mean Difference | Clinical Utility |
|---|---|---|---|---|
| Dried Blood Spot (DBS) | Whole blood on filter paper | r = 0.796 (p < 0.001) | 0.66 ± 0.70 log copies/mL | Resource-limited settings |
| Plasma vs Serum | Plasma/Serum pairs | Strong correlation | Minimal bias | Serum alternative for specific settings |
| Novel Rapid Test | Finger-prick blood | R² = 0.97-0.99 with reference | Not specified | Point-of-care settings |
A study comparing dried blood spot (DBS) and plasma HIV-1 viral load measurements using the Roche COBAS AmpliPrep/COBAS TaqMan assay demonstrated a strong correlation (r = 0.796, p < 0.001) between these methods [16]. The mean difference between DBS and plasma measurements was 0.66 ± 0.70 log copies/mL, suggesting that DBS samples could be a suitable alternative for periodic monitoring of HIV-1 viral loads, particularly in resource-limited settings due to minimal invasive blood collection, higher stability at room temperature, and ease of transportation [16].
Similarly, a comparative evaluation of plasma and serum HIV-1 viral load measurements found strong correlation between these sample types, indicating that serum might be a suitable alternative sample for periodic monitoring of HIV viral load, especially in specific clinical circumstances such as when patients are undergoing antenatal care services where serum is the most commonly available test sample [17].
Emerging technologies are further revolutionizing viral load monitoring. A recent development in rapid simultaneous self-testing for HIV and HCV viral loads integrates RNA extraction and multiplex RT-PCR in a single portable device [14]. This system uses only 100 μL of finger-prick blood and provides results in under one hour, achieving a limit of detection (LOD) of 5 copies/reaction and demonstrating strong correlation (R² = 0.97-0.99) with standard Bio-Rad benchtop systems [14].
Impact of Viral Load Thresholds on Clinical Outcomes
HIV Viral Load Thresholds and Diagnostic Challenges
The establishment of appropriate viral load thresholds has significant implications for diagnosis and monitoring. China's diagnostic guidelines recently lowered the viral load threshold from 5,000 to 1,000 copies/mL for HIV diagnosis [18]. This change demonstrated a significant improvement in detection rates - when using 5,000 copies/mL as the threshold, the HIV positivity rate was 89.87%, which increased to 97.46% when the threshold was lowered to 1,000 copies/mL (P = 0.009) [18].
Despite this improvement, challenges remain in acute HIV infection (AHI) diagnosis. A study analyzing the Beijing PRIMO cohort found that 4 cases (1.15%) had viral loads < 1,000 copies/mL prior to confirmed positive antibody results, with the longest interval between a viral load < 1,000 copies/mL and a subsequent positive Western blot result being 42 days [18]. This highlights the diagnostic significance of low-level viremia during the serological window period and supports the prioritization of nucleic acid testing (NAT) for individuals with high-risk profiles and negative or indeterminate antibodies to shorten the diagnostic window.
Viral Suppression Metrics in HIV Care
The definition of viral suppression also varies across guidelines and programs, impacting reported outcomes. A study examining differences between the Centers for Disease Control and Prevention (CDC) definition of viral suppression used by the Ryan White HIV/AIDS Program (RWHAP) - last viral load measurement <200 copies/mL - and more robust definitions of durable viral suppression found significant variations [3].
While 94-95% of individuals met the CDC definition of viral suppression, when alternative metrics requiring all viral loads under 200 copies/mL with either (1) one viral load required; (2) two viral loads required; or (3) two viral loads more than 90 days apart required, annual rates of viral suppression dropped to 87-92% [3]. These findings demonstrate that current metrics may overestimate sustained viral suppression, with implications for both clinical management and public health reporting.
Experimental Protocols for Viral Load Assay Evaluation
Standardized Evaluation Framework for HCV Assays
The performance evaluation of HCV RNA quantification reagents followed a rigorous protocol based on the "Protocol for the laboratory evaluation of HCV molecular assays" and "Guidance on test method validation for in vitro diagnostic medical devices" issued by WHO [15]. The evaluation incorporated multiple serum panels:
- HCV RNA Basic Serum Panel: Comprised 40 serum samples (20 HCV RNA-positive and 20 HCV RNA-negative) to evaluate initial analytical sensitivity and specificity.
- Analytical Specificity Panel: Contained 40 serum samples negative for HCV antibodies and HCV RNA but positive for HBV or HIV, plus samples exhibiting hemolysis, lipemia, or other interference factors.
- Seroconversion Panel: Utilized the PHV928 panel (SeraCare Life Sciences) consisting of 9 vials of serum samples to evaluate early detection sensitivity.
- Analytical Sensitivity Panel: Employed samples prepared by diluting the WHO International Standard for HCV RNA to determine the limit of detection.
- Precision Panel: Assessed both intra-assay and inter-assay variability across multiple runs.
- Genotype Qualification Panel: Evaluated detection capability across HCV genotypes 1-6.
- Linearity Panel: Assessed the quantitative linear range of each assay.
All stock specimens from HCV RNA serum panels were tested in parallel with the four reagents following manufacturers' instructions, with operations and data analysis conducted under blinded or double-blinded conditions to minimize bias [15].
HIV Viral Load Comparison Methodology
The comparative evaluation of DBS versus plasma HIV-1 viral load measurements followed a standardized protocol [16]. Participants provided 4 mL of venous blood collected in EDTA anticoagulant tubes. For DBS preparation, approximately 50 μL of blood was dispensed onto Whatman 903 filter paper cards with five spots per card. The blood spots were air-dried at room temperature for 4-6 hours and stored in zip-lock plastic bags with silica gel desiccant pouches. Plasma was harvested from whole blood samples via centrifugation at 2500 RPM for 10 minutes.
HIV-1 RNA extraction from DBS samples utilized two half-spots (6mm in diameter) trimmed from each filter paper card, while plasma samples used 1100 μL aliquots. The COBAS AmpliPrep instrument performed automated specimen processing based on silica-based capture principles. The quantification was performed using the COBAS TaqMan version 2.0 Analyzer, with detection utilizing HIV-1-specific oligonucleotide probes labeled with fluorescent dye [16].
Statistical analysis included Pearson's correlation to assess the relationship between plasma and DBS measurements and Bland-Altman plots to evaluate the level of agreement and identify potential proportional bias between the two methods.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Viral Load Quantification Studies
| Reagent/Material | Manufacturer/Example | Function | Key Characteristics |
|---|---|---|---|
| HCV RNA Quantification Reagents | Wantai BioPharm, Daan Gene, Beijing NaGene, Kehua Bio-Engineering | HCV RNA detection and quantification | Real-time PCR with fluorescence probing, LOD: 25-50 IU/mL |
| HIV-1 Viral Load Assay | Roche COBAS AmpliPrep/COBAS TaqMan v2.0 | HIV-1 RNA extraction and quantification | Automated system, LOD: <20 copies/mL |
| DBS Filter Paper | Whatman 903 | Sample collection and storage | Standardized cellulose matrix for blood collection |
| RNA Extraction Kit | QIAGEN QIAamp Viral RNA Mini Kit | Nucleic acid purification | Silica-based membrane technology |
| International Standards | WHO International Standard for HCV RNA | Assay calibration and standardization | Traceable reference materials |
| Multiplex RT-PCR Reagents | Custom formulations | Simultaneous detection of multiple targets | Enables HIV/HCV co-testing |
| Quality Control Panels | SeraCare Life Sciences | Assay validation and QC | Characterized performance panels |
The selection of appropriate reagents and materials is critical for robust viral load quantification. International standards, such as the WHO International Standard for HCV RNA, play a vital role in assay calibration and harmonization across different platforms and laboratories [15]. Quality control panels with characterized performance metrics are essential for both initial validation and ongoing quality assurance.
For emerging technologies, such as the rapid multiplex HIV/HCV testing platform, specialized reagents enabling rapid RNA extraction and accelerated thermal cycling are necessary. The system developed by Liu and colleagues achieves complete RNA extraction and multiplex RT-PCR in under 60 minutes through optimized reagent formulations and accelerated thermal cycling protocols with 1-second denaturation and extension steps [14].
The comparative analysis of viral load quantification technologies for HIV and HCV reveals both significant advancements and critical challenges in standardization. While current assays demonstrate excellent performance characteristics - with high sensitivity, specificity, and precision - variability in platforms, methodologies, and definitions of key thresholds creates substantial obstacles for both clinical management and drug development.
The emergence of novel technologies, such as rapid multiplex testing platforms and alternative sampling methods like DBS, offers promising opportunities to expand testing accessibility and efficiency. However, these innovations must be accompanied by robust standardization efforts to ensure result comparability across different settings and platforms.
For researchers and drug development professionals, the imperative for standardization extends beyond technical performance to encompass clinical endpoints and reporting metrics. Harmonized definitions of virologic suppression, standardized evaluation protocols, and traceable reference materials are essential components of a cohesive viral load quantification ecosystem. As we strive toward global elimination targets for both HIV and HCV, a renewed focus on standardization will be crucial for accurate disease monitoring, effective treatment evaluation, and successful drug development.
Interassay variability represents a fundamental challenge in biomedical research and clinical diagnostics, particularly in the field of viral load quantification. This variability refers to the differences in measurement results that occur when the same sample is tested using different assays, instruments, or reagent systems. The lack of universal standards across testing platforms creates significant obstacles for comparing data across studies, establishing consistent clinical thresholds, and ensuring reproducible research outcomes. In viral load quantification, where precise measurements directly influence clinical decisions and research conclusions, this variability can undermine the validity and translational potential of scientific findings.
The core of this challenge lies in the absence of standardized reference materials and harmonized protocols. Different manufacturers utilize unique calibration standards, reagent formulations, and measurement technologies, leading to systematic differences in reported values. Even when assays target the same analyte, these methodological differences can produce substantially divergent results. The establishment of universal standards is therefore critical not only for improving the reliability of individual assays but also for enabling meaningful correlations across different viral load quantification methods.
Experimental Evidence of Interassay Variability
Variability in TROP2 Immunohistochemistry Assays
A 2025 study investigating TROP2 expression in triple-negative breast cancer provides compelling evidence of significant interassay variability. Researchers analyzed 26 tumor samples using three different immunohistochemistry assays on a Dako Omnis platform according to manufacturer protocols [19].
The experimental protocol involved:
- Sample Preparation: Twenty-six triple-negative breast cancer samples were processed for analysis.
- Assay Systems: Three different immunohistochemistry assays were employed: ENZO-ABS380-0100 (Assay A, used in ASCENT trial), Abcam SP295 (Assay B, used in TROPiCS-02 trial), and Santa Cruz B9-sc-376746 (Assay C, used in cross-sectional studies).
- Quantification Method: TROP2 expression on tumor cell membranes was quantified using the H-score system, with categories defined as low (H-score ≤ 100), intermediate (> 101 to ≤ 200), and high (> 200).
- Statistical Analysis: Assay agreement was evaluated using Cohen's κ and Gwet's AC2 statistics.
The results demonstrated striking disparities in TROP2 expression classification across the three assays [19]:
Table 1: TROP2 Expression Classification Across Different Assays
| Assay | Low Expressors | Intermediate Expressors | High Expressors |
|---|---|---|---|
| Assay A | 57.7% (n=15) | 34.6% (n=9) | 7.7% (n=2) |
| Assay B | 19.2% (n=5) | 42.3% (n=11) | 38.4% (n=10) |
| Assay C | 15.4% (n=4) | 46.2% (n=12) | 38.4% (n=10) |
The overall concordance between all three assays was only fair to moderate (AC2 = 0.35, p = 0.0067), while assays B and C showed substantial agreement (80.8% concordance, κ = 0.81; p < 0.0001). These findings highlight how assay selection can dramatically influence biomarker classification, potentially affecting patient stratification for targeted therapies like sacituzumab govitecan [19].
Variability in Direct Oral Anticoagulant (DOAC) Monitoring
A study investigating interassay variability between direct oral anticoagulant (DOAC) calibrated anti-factor Xa assays further demonstrates this challenge in clinical measurement [20]. The experimental protocol included:
- Sample Collection: 70 apixaban and 59 rivaroxaban samples from participants in the Perioperative Anticoagulation Use for Surgery Evaluation trial.
- Testing Platforms: Simultaneous testing using Biophen reagents on BCS XP analyzer (Siemens), HemosIL reagents on ACL TOP analyzer (Werfen), and Stago reagents on STA CompactMAX analyzer (Diagnostica Stago).
- Analysis Method: Interassay correlations were analyzed at the predetermined clinical cutoff of 30 ng/mL and compared with median anti-FXa levels.
The results showed moderate-to-very strong correlations for both apixaban (r = 0.7271-0.9467) and rivaroxaban (r = 0.6531-0.9702). Despite these correlations, anti-FXa levels were significantly different between all instrument-reagent combinations in samples below 30 ng/mL. Importantly, 7.8% (10/129) of samples were discrepantly classified across the 30 ng/mL clinical threshold, potentially affecting clinical decision-making regarding urgent procedures [20].
Establishing Universal Standards for Viral Detection
Development of a Universal SARS-CoV-2 Standard
To address the critical need for standardization in viral detection, researchers have developed a universal national standard for both SARS-CoV-2 antigen and nucleic acid detection [21] [22]. The experimental methodology for this development included:
- Viral Preparation: A SARS-CoV-2 Omicron BA.1 strain (hCoV-19/Hong Kong/HKU-691/2021) was cultured with Vero cells and inactivated using β-propiolactone (BPL).
- Inactivation Comparison: The impact of heat inactivation and BPL inactivation on detection was compared using digital PCR (dPCR), qPCR, and sequencing.
- Value Assignment: The concentration was assigned via multi-laboratory digital PCR involving three different dPCR systems.
- Standard Preparation: Bulk preparations were lyophilized into 3 mL vials with 0.5 mL per vial and stored at -20°C.
- Validation Testing: The standard was used to evaluate the limits of detection (LoDs) of commercial antigen rapid detection tests (Ag-RDTs) and nucleic acid amplification tests (NAATs) using a common unitage.
The research demonstrated that BPL inactivation maintained comparable nucleic acid titers to heat inactivation while preserving better antigen activity. The national standard concentration was assigned as 1.04 × 10^8 Unit/mL (standard uncertainty: 3.48 × 10^6 Unit/mL) [21]. Utilizing this universal standard enabled direct comparison of LoDs between Ag-RDTs and NAATs, revealing that while NAATs generally exhibited lower LoDs, some Ag-RDT sensitivity approached NAAT levels [22].
This universal standard represents a significant advancement as it overcomes the historical challenge of quantifying viral antigens without a standardized unit of measurement, which previously hindered precise analytical evaluation of Ag-RDTs and comparison with NAATs [21].
Regulatory Frameworks for Standardization
The United States Pharmacopeia (USP) plays a critical role in establishing public quality standards that support the design, manufacture, testing, and regulation of drug substances and products [23]. Regulatory agencies recognize that USP standards strengthen quality, streamline development, support regulatory compliance, and increase regulatory predictability for drugs. The development of these standards involves a collaborative process with industry stakeholders, regulatory decision-makers, and scientific experts [23].
The establishment of universal standards for prescription container labeling demonstrates the importance of standardization in improving patient outcomes. Wide variability in prescription labels across individual prescriptions, pharmacies, and states can contribute to medication errors. The USP standards address this by providing specific direction on organizing labels in a patient-centered manner that improves readability and gives explicit instructions [24].
Methodological Approaches to Mitigate Variability
Matched Pairs Analysis
Research published in the Journal of Cheminformatics demonstrates that analyzing potency differences between matched compound pairs can reduce the impact of interassay variability [25] [26]. The methodology for this approach involves:
- Data Curation: Implementing minimal and maximal curation procedures for Ki and IC50 data from the ChEMBL32 database.
- Pair Identification: Using the rdRascalMCES algorithm to identify structural analogs between compatible assays based on Maximum Common Edge Subgraphs (MCES).
- Analysis Method: Calculating the difference in pChEMBL values for matched pairs within the same assay, then comparing these differences across assays (ΔΔpChEMBL).
- Statistical Evaluation: Assessing data quality using Median Absolute Error (MAE) and fractions of values exceeding 0.3 (F > 0.3) and 1.0 (F > 1.0) pChEMBL units.
This study revealed that potency differences between matched pairs exhibit less variability than individual compound measurements, suggesting that systematic assay differences may partially cancel out in paired data. The data showed that with minimal curation, agreement within 0.3 pChEMBL units was 44-46% for Ki and IC50 values, improving to 66-79% with extensive curation. Similarly, the percentage of pairs with differences exceeding 1 pChEMBL unit dropped from 12-15% to 6-8% with maximal curation [25].
Statistical Quantification of Variability
Proper quantification of interassay variability is essential for assessing methodological reliability. The coefficient of variability (CV) provides a standardized approach for this quantification [27]:
- Inter-Assay CV: Measures plate-to-plate consistency, calculated from the mean values for high and low controls on each plate. Acceptable inter-assay CVs are generally less than 15%.
- Intra-Assay CV: Measures the variability between duplicate measurements within the same assay plate. Acceptable intra-assay CVs should be less than 10%.
The calculation involves determining the standard deviation of measurements divided by the mean of the measurements, expressed as a percentage. Poor intra-assay CVs (>10%) often reflect technical issues such as pipetting errors, sample handling problems, or equipment calibration issues [27].
Visualization of Experimental Approaches
The following workflow diagrams illustrate key experimental methodologies discussed in this review for assessing and mitigating interassay variability.
Diagram 1: TROP2 IHC variability assessment. This workflow illustrates the experimental approach used to evaluate interassay variability in TROP2 immunohistochemistry staining, from sample processing through statistical analysis of concordance [19].
Diagram 2: Universal standard development process. This workflow outlines the key steps in establishing a universal standard for SARS-CoV-2 detection, enabling direct comparison between antigen and nucleic acid tests [21] [22].
Research Reagent Solutions for Standardization
The following table details essential research reagents and materials critical for conducting standardized viral load quantification and addressing interassay variability.
Table 2: Essential Research Reagents for Standardization Studies
| Reagent/Material | Function and Application | Experimental Context |
|---|---|---|
| β-Propiolactone (BPL) | Virus inactivation while preserving antigen integrity | Universal standard preparation for SARS-CoV-2 [21] |
| Digital PCR Systems | Absolute nucleic acid quantification without calibration curves | Value assignment for universal standards [21] |
| Reference Standards | Calibrator materials with assigned unitage | Harmonizing measurements across different platforms [21] |
| Matched Molecular Pairs | Structural analogs for comparing potency differences | Assessing interassay variability in chemical datasets [25] |
| Quality Controls | High and low concentration controls for precision monitoring | Calculating inter-assay and intra-assay coefficients of variation [27] |
| Standardized Buffers | Consistent sample dilution and matrix conditions | Universal buffer (10 mM PBS, 1% HSA, 0.1% trehalose) for standard preparation [21] |
The persistent challenges of interassay variability and the lack of universal standards remain significant obstacles in viral load quantification and biomarker assessment. The experimental evidence demonstrates substantial variability across different assay systems, which can impact clinical interpretations and research conclusions. However, methodological approaches such as matched pairs analysis, statistical quantification of variability, and the development of universal standards offer promising pathways toward improved harmonization.
The establishment of universal standards for SARS-CoV-2 detection represents a significant advancement in the field, providing a model for standard development for other viral targets. Similarly, regulatory frameworks and quality standards play an essential role in promoting consistency across testing platforms. As research continues to address these challenges, the implementation of standardized reagents, rigorous validation protocols, and transparent reporting of variability metrics will be crucial for enhancing the reliability and correlation of viral load quantification methods across different platforms and laboratories.
From Bench to Bedside: Applied Viral Load Quantification Across Pathogens and Sample Types
Viral infections remain a major cause of morbidity and mortality in transplant recipients, necessitating precise viral load monitoring to guide preemptive therapy and prevent allograft loss. Quantitative nucleic acid testing (QNAT) has become the cornerstone for managing post-transplant viral infections, allowing clinicians to distinguish between latent infection and active disease. This guide objectively compares the quantification methodologies, clinical thresholds, and performance characteristics for four herpesviruses with significant post-transplant implications: cytomegalovirus (CMV), BK polyomavirus (BKV), Epstein-Barr virus (EBV), and human herpesvirus 6 (HHV-6). Understanding the correlation between viral load kinetics and clinical outcomes is essential for optimizing patient management in transplant virology.
Viral Load Thresholds and Clinical Correlations
Comparative Analysis of Viral Load Thresholds
Table 1: Clinically Significant Viral Load Thresholds in Transplant Virology
| Virus | Specimen Type | Clinical Threshold | Clinical Correlation | Performance Characteristics |
|---|---|---|---|---|
| CMV | Plasma | 1,700 IU/mL (SOT) [28] | Distinguishes CMV disease from asymptomatic infection [28] | Sensitivity 80%, Specificity 74% (SOT) [28] |
| Plasma | 1,350 IU/mL (HSCT) [28] | Distinguishes CMV disease from asymptomatic infection [28] | Sensitivity 87%, Specificity 87% (HSCT) [28] | |
| Plasma | 830 IU/mL [29] | Treatment initiation threshold | Program-wide standardized threshold [29] | |
| BKV | Plasma | Qualitative NAT+ [30] | Rules out BKVAN | Sensitivity 97.7%, Specificity 90.7%, NPV 99.9% [30] |
| Plasma | >1.0E+04 copies/mL [30] | Predicts BKVAN in viremic patients | Sensitivity 56.3%, PPV 54.6% [30] | |
| EBV | Plasma | Varies by assay [31] [32] | PTLD risk stratification | Qualitative monitoring essential [31] |
| HHV-6 | CSF | Detection alone insufficient [33] | Clinical relevance uncertain | No VL correlation with disease likelihood [33] |
Kinetic Parameters and Clinical Outcomes
Table 2: Viral Load Kinetic Parameters Predicting Adverse Outcomes
| Kinetic Parameter | Clinical Impact | Timeframe | Risk Magnitude |
|---|---|---|---|
| First CMV episode >15 days [29] | Predicts transplant failure | First viremic episode | 3-fold increased risk [29] |
| Maximum CMV VL ≥4.0 log10 IU/mL [29] | Predicts transplant failure | First viremic episode | 3-fold increased risk [29] |
| Recurrent CMV infection [29] | Graft failure and death | Multiple episodes | Progressive risk increase [29] |
| Cumulative viremia duration [29] | Graft failure and death | Entire post-transplant period | Survival declines to 30% [29] |
| Total viral load AUC [29] | Graft failure and death | Entire post-transplant period | Survival declines to 7% [29] |
Experimental Protocols and Methodologies
Standardized CMV Viral Load Testing Protocol
The COBAS AmpliPrep/COBAS TaqMan CMV Test (CAP/CTM CMV) represents the FDA-approved standardized approach for CMV quantification [28]. The assay demonstrates a lower limit of detection (LoD) of 91 IU/mL in plasma, with lower limit of quantification (LLoQ) at 137 IU/mL and upper limit of quantification (ULoQ) at 9,100,000 IU/mL [28].
Sample Processing Protocol:
- Collection: Whole blood collected in EDTA tubes followed by centrifugation at 4000 rpm for 10 minutes to separate plasma [34]
- Extraction Methods Comparison:
- Automatic magnetic bead-based extraction (EZ1 DSP Virus kit/Virus mini kit): Higher throughput with minimal contamination risk [34]
- Manual silica membrane extraction (QIAamp DSP Virus kit): Labor-intensive but effective [34]
- Heating protocol: 90 μL plasma incubated with protease Q at 56°C for 15 min, followed by inactivation at 90°C for 10 min [34]
- Modifications for Whole Blood: Required 1:6 dilution in Specimen Pre-Extraction Reagent, incubation at 56°C for 10 min with shaking at 1000 rpm [28]
- Quantification Correction: Applied -0.43 log10 IU/mL calibration correction factor to log-transformed results [28]
BKV Nucleic Acid Testing Protocol
BKV monitoring employs real-time PCR methodologies with evolving platform technologies [30]. The diagnostic approach differs significantly based on clinical context.
Analytical Performance Characteristics:
- Abbott Alinity m BKV AMPL kit: Demonstrates 96.6% sensitivity in plasma, 95.8% sensitivity in urine, with correlation coefficients of 0.965 (plasma) and 0.971 (urine) compared to reference methods [35]
- Random-access testing: Enables reduced turnaround time between sampling and result availability [35]
Clinical Application Protocol:
- Surveillance context: Negative qualitative NAT during protocol surveillance provides 99.9% negative predictive value for excluding BKVAN at 2.6% prevalence [30]
- Viremic patient context: QNAT exceeding 1.0E+04 BKPyV-DNA copies/mL shows limited predictive value (PPV 54.6%) [30]
EBV and HHV-6 Detection Methodologies
EBV Quantification Advances:
- NeuMoDx EBV Quant Assay 2.0: Automated system demonstrating 95.3% positive percent agreement and 95.1% negative percent agreement with cobas EBV test [32]
- Assay limitations: Increased variability observed at upper and lower limits of dynamic range [32]
HHV-6 Clinical Significance Assessment:
- Retrospective analysis protocol: Review of 8,778 samples from 8,222 individuals between 2010-2021 [33]
- Clinical categorization: HHV-6 detection classified as unlikely (83%), possible (14%), or likely (3%) clinically relevant [33]
- Critical finding: No significant difference in HHV-6 DNA levels between clinical significance categories [33]
Diagnostic Workflow and Clinical Decision Pathways
Post-Transplant Viral Monitoring Algorithm
Diagram 1: Viral monitoring algorithm for CMV management in transplantation. D: Donor, R: Recipient serostatus.
BKV Associated Nephropathy Diagnostic Pathway
Diagram 2: BKV diagnostic pathway highlighting high NPV of qualitative testing.
Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Transplant Virology
| Reagent/Platform | Virus Target | Function/Application | Performance Characteristics |
|---|---|---|---|
| CAP/CTM CMV Test (Roche) | CMV | FDA-approved CMV quantification in plasma [28] | LoD: 91 IU/mL (plasma), LoD: 240 IU/mL (whole blood) [28] |
| Artus CMV QS-RGQ kit (Qiagen) | CMV | Real-time PCR quantification [34] | Compatible with multiple extraction methods [34] |
| Abbott Alinity m BKV AMPL kit | BKV | Random-access BKV quantification [35] | Sensitivity: 96.6% (plasma), 95.8% (urine) [35] |
| Argene BKV R-gene kit (BioMerieux) | BKV | BKV DNA quantification [30] | Used with Roche LightCycler platforms [30] |
| NeuMoDx EBV Quant Assay 2.0 | EBV | Automated EBV DNA quantification [32] | PPA: 95.3%, NPA: 95.1% [32] |
| EZ1 Advanced XL (Qiagen) | Multiple | Automated nucleic acid extraction [34] | Magnetic bead technology, minimal cross-contamination [34] |
| QIAamp DNA Mini Kit (Qiagen) | Multiple | Manual nucleic acid extraction [36] | Silica membrane technology [36] |
| FilmArray ME Panel | HHV-6 | Syndromic testing for CNS infections [33] | Detects HHV-6 but clinical utility questionable [33] |
Discussion and Future Directions
The correlation between viral load kinetics and clinical outcomes in transplant recipients continues to evolve with standardization of quantification methodologies. CMV viral load thresholds have been successfully established for distinguishing disease from infection, with kinetic parameters providing prognostic information about allograft survival [28] [29]. In contrast, BKV monitoring demonstrates exceptional utility for ruling out nephropathy but limited positive predictive value, highlighting the complex relationship between viremia and tissue-invasive disease [30].
The clinical significance of EBV and HHV-6 detection remains more challenging to interpret. While EBV quantification assays continue to improve in performance characteristics [32], the inclusion of HHV-6 in routine diagnostic panels for CNS infections requires reconsideration given the limited clinical relevance in most detection scenarios [33].
Future directions in transplant virology include the investigation of novel biomarkers such as Torque Teno virus (TTV) for immunologic risk stratification [37], the development of standardized extraction methodologies across platforms [34] [35], and the implementation of viral load kinetics as predictive tools for individualizing immunosuppression regimens. The successful integration of viral quantification data into clinical decision-making requires ongoing correlation between laboratory values and patient outcomes, particularly for viruses where therapeutic thresholds remain ill-defined.
The accurate detection and quantification of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remains a critical component of public health responses and clinical management of COVID-19. While reverse transcription quantitative polymerase chain reaction (RT-qPCR) has established itself as the gold standard for diagnostic testing, reverse transcription droplet digital PCR (RT-ddPCR) has emerged as a powerful alternative with potential advantages in specific scenarios. This comparison guide objectively evaluates the performance characteristics of both platforms in the context of respiratory sample testing, providing researchers and clinicians with evidence-based insights to inform methodological selection for viral load quantification and monitoring.
Fundamental Technological Differences
RT-qPCR is a relative quantification method that measures the amplification of target nucleic acids during PCR cycles in real-time, requiring standard curves for quantification. It has been widely implemented for SARS-CoV-2 detection in clinical and public health laboratories worldwide [11] [38].
RT-ddPCR utilizes a limiting dilution approach where the reaction mixture is partitioned into thousands of nanoliter-sized droplets, with each droplet functioning as an individual PCR reactor. Following end-point amplification, positive and negative droplets are counted, and the target concentration is absolutely quantified using Poisson statistics without the need for standard curves [11] [38].
Comprehensive Performance Metrics
Table 1: Direct performance comparison between RT-qPCR and RT-ddPCR for SARS-CoV-2 detection
| Performance Parameter | RT-qPCR | RT-ddPCR | Experimental Support |
|---|---|---|---|
| Limit of Detection (LOD) | 12.0 copies/μL [39] | 0.066 copies/μL [39] | Wastewater analysis [39] |
| Quantification Approach | Relative (requires standard curve) | Absolute (Poisson statistics) | Multiple studies [11] [38] |
| Precision | Subject to amplification efficiency variations | Coefficient of variation <10% [11] | Serial dilution studies [11] |
| Tolerance to Inhibitors | Moderate | High [38] [40] | Complex matrices comparison [39] [40] |
| Detection in Low Viral Load Samples | 21/50 positive in wastewater [11] | 50/50 positive in wastewater [11] | Wastewater sample analysis [11] |
| Multiplexing Capability | Established [41] [42] | Developing | Clinical validation [41] [42] |
Table 2: Clinical performance comparison in respiratory samples
| Clinical Performance | RT-qPCR | RT-ddPCR | Study Details |
|---|---|---|---|
| Positive Detection Rate | 89/130 [43] | 93/130 [43] | 130 clinical samples [43] |
| Suspected Cases | 9/130 [43] | 21/130 [43] | Hospitalized patients [43] |
| Negative Results | 32/130 [43] | 16/130 [43] | Oropharyngeal swabs [43] |
| Coincidence Rate | 98.65% [11] | 98.65% [11] | 148 pharyngeal swabs [11] |
| Kappa Value | 0.94 [11] | 0.94 [11] | Method agreement [11] |
Experimental Protocols and Methodologies
Representative RT-ddPCR Protocol for SARS-CoV-2 Detection
The following protocol was adapted from established methodologies with proven sensitivity and specificity for SARS-CoV-2 variants [11] [44]:
Sample Preparation and RNA Extraction:
- Collect respiratory samples (nasopharyngeal or oropharyngeal swabs) in universal viral transport medium
- Extract RNA using commercial kits (e.g., RNeasy Mini Kit, Qiagen)
- Elute RNA in 50 μL nuclease-free water
- Store extracts at -80°C if not used immediately
Reaction Setup:
- Prepare 20 μL reaction mixture containing:
- 5 μL One-Step RT-ddPCR Supermix
- 2 μL primer-probe mix (final concentration: 900 nM primers, 250 nM probe)
- 2 μL reverse transcriptase
- 1 μL 300 mM DTT
- 8 μL nuclease-free water
- 2 μL RNA template
- Primers and probes target SARS-CoV-2 N and S genes [11]
Droplet Generation and Thermal Cycling:
- Generate droplets using automated droplet generator
- Transfer droplets to 96-well PCR plate
- Seal plate and run with following thermal protocol:
- Reverse transcription: 45°C for 60 minutes
- Enzyme activation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing/extension: 53.5°C for 60 seconds
- Enzyme deactivation: 98°C for 10 minutes
- Hold at 4°C
Droplet Reading and Analysis:
- Transfer plate to droplet reader
- Analyze using Poisson statistics to determine absolute copy numbers
- Set fluorescence thresholds based on negative controls
- Report copies/μL of reaction mixture
Representative RT-qPCR Protocol for SARS-CoV-2 Detection
Reaction Setup:
- Prepare 20-25 μL reaction mixture containing:
- One-Step RT-qPCR master mix
- Primers and probes targeting SARS-CoV-2 genes (N1, N2, E, or ORF1ab)
- 5-10 μL RNA template
- Include appropriate positive and negative controls
Thermal Cycling:
- Reverse transcription: 50°C for 10-30 minutes
- Initial denaturation: 95°C for 1-10 minutes
- 40-45 cycles of:
- Denaturation: 95°C for 10-15 seconds
- Annealing/extension: 55-60°C for 30-60 seconds
- Data collection during annealing/extension phase
Analysis:
- Determine cycle threshold (Ct) values
- Compare to standard curve for quantification
- Interpret results based on established cutoffs (typically Ct <37-40)
Figure 1: Comparative workflow of RT-qPCR and RT-ddPCR for SARS-CoV-2 detection
Research Reagent Solutions
Table 3: Essential research reagents and materials for SARS-CoV-2 detection assays
| Reagent/Material | Function | Example Products/References |
|---|---|---|
| RNA Extraction Kits | Nucleic acid purification from clinical samples | RNeasy Mini Kit (Qiagen) [11], AllPrep PowerViral DNA/RNA Kit [39] |
| One-Step RT-PCR Master Mixes | Combined reverse transcription and PCR amplification | One-Step RT-ddPCR Advanced Kit for Probes (Bio-Rad) [11], QuantiNova Pathogen Mastermix [40] |
| Primer/Probe Sets | Target-specific amplification and detection | N1, N2, E gene assays [41] [11], ORF1ab gene assays [43] |
| Digital PCR Reagents | Droplet generation and stabilization | Droplet Generation Oil, Droplet Reader Oil [45] |
| Positive Controls | Assay validation and quality control | SARS-CoV-2 RNA standards [40], quantified viral RNA [11] |
| Internal Controls | Monitoring extraction and amplification efficiency | MS2 bacteriophage [41] [40], human RNase P [43] |
Applications and Method Selection Guidelines
Optimal Use Cases for RT-ddPCR
RT-ddPCR demonstrates superior performance in specific scenarios that are particularly relevant to research and advanced clinical applications:
Low Viral Load Detection: Multiple studies have confirmed the advantage of RT-ddPCR in detecting SARS-CoV-2 in samples with low viral loads. In wastewater surveillance, RT-ddPCR detected SARS-CoV-2 in 50/50 samples compared to only 21/50 by RT-qPCR [11]. This enhanced sensitivity makes it invaluable for early infection detection, monitoring treatment response, and discharge testing where residual viral RNA persists at minimal levels.
Absolute Quantification Requirements: When precise viral load quantification is necessary without reliance on standard curves, RT-ddPCR provides absolute quantification that enables more accurate longitudinal monitoring and inter-laboratory comparisons [38]. This is particularly valuable in clinical trials and pathogenesis studies where precise viral kinetics measurement is required.
Complex Matrices: The partitioning technology of ddPCR enhances tolerance to PCR inhibitors commonly found in complex sample types, including wastewater, saliva, and certain respiratory specimens [39] [38]. This reduces false-negative results and improves reliability in environmental surveillance and alternative sample testing.
Optimal Use Cases for RT-qPCR
RT-qPCR remains the preferred method for many routine applications due to its established infrastructure and practical advantages:
High-Throughput Diagnostic Testing: For large-scale screening and routine diagnostic applications where rapid turnaround time is essential, RT-qPCR offers established workflows, higher throughput capacity, and lower per-sample costs [41]. The extensive validation and standardization of RT-qPCR protocols support its continued use in clinical diagnostics.
Multiplex Assays: RT-qPCR has well-established capabilities for multiplex detection of multiple pathogens in a single reaction [41] [42]. Recently developed multiplex assays simultaneously detect SARS-CoV-2, influenza A/B, and other respiratory pathogens with high sensitivity and specificity [42] [46], providing comprehensive respiratory pathogen testing.
Resource-Limited Settings: The wider availability of instrumentation, lower reagent costs, and established regulatory frameworks make RT-qPCR more accessible for routine clinical use and resource-limited settings [42].
Both RT-qPCR and RT-ddPCR offer distinct advantages for SARS-CoV-2 detection in respiratory samples. RT-qPCR remains the workhorse for high-throughput diagnostic testing due to its established infrastructure, rapid turnaround times, and cost-effectiveness. In contrast, RT-ddPCR provides enhanced sensitivity and absolute quantification benefits that are particularly valuable for research applications, low viral load detection, and precise viral load monitoring. The selection between these platforms should be guided by specific application requirements, with RT-ddPCR offering complementary capabilities that address specific limitations of conventional RT-qPCR, particularly in surveillance and research contexts where maximum sensitivity and precise quantification are paramount.
The accurate quantification of HIV-1 viral load is a cornerstone for monitoring antiretroviral therapy efficacy and achieving global treatment targets. While plasma-based viral load testing remains the gold standard, dried blood spot (DBS) sampling has emerged as a pivotal alternative for expanding access to virological monitoring, particularly in resource-limited settings. This guide provides a comprehensive, data-driven comparison of the performance characteristics of DBS versus plasma for HIV-1 RNA quantification. We synthesize recent evidence on correlation strength, quantitative bias, and diagnostic concordance from field evaluations across multiple countries and assay platforms. Furthermore, we detail standardized experimental protocols for sample processing and analysis, visualize methodological workflows, and catalog essential research reagents. This objective analysis aims to inform researchers, scientists, and program implementers on the appropriate applications and limitations of DBS within viral load quantification method correlation research.
Quantitative Performance Comparison: DBS vs. Plasma
Extensive research has demonstrated that DBS samples produce quantitatively comparable results to plasma, albeit with a consistent, measurable bias. The following tables summarize key performance metrics from recent studies.
Table 1: Summary of Quantitative Correlation from Recent Studies
| Study Location & Citation | Sample Size (n) | Assay Platform | Mean Log Difference (DBS - Plasma) | Correlation Coefficient (r) |
|---|---|---|---|---|
| Northwest Ethiopia [16] [47] | 48 | Roche COBAS AmpliPrep/COBAS TaqMan v2.0 | +0.66 ± 0.70 log copies/mL | 0.796 (p < 0.001) |
| India (South) [48] | 62 | Abbott RealTime HIV-1 PCR | -0.41 log copies/mL | 0.982 (p < 0.0001) |
The data indicates a strong positive correlation between DBS and plasma viral load measurements, though the direction and magnitude of the mean log difference can vary. The Ethiopian study reported DBS viral loads were, on average, 0.66 log copies/mL higher than paired plasma measurements [16]. In contrast, the study from India found DBS measurements to be slightly lower [48]. This underscores the importance of platform-specific and context-specific validation.
Table 2: Operational and Diagnostic Characteristics
| Characteristic | Plasma (Gold Standard) | Dried Blood Spot (DBS) |
|---|---|---|
| Sample Volume | Larger volumes required (e.g., 1 mL for plasma harvest from 4 mL whole blood) [16] | Minimal volume (e.g., ~50 µL spotted onto filter paper) [16] |
| Stability & Transport | Requires cold chain (freezing at -20°C) for storage and transport [16] | Stable at room temperature for extended periods; ease of transport via mail [16] [49] |
| Concordance for Recent Infection (Zimbabwe) [50] [51] | 10.1% (47/464) classified recent | 12.3% (57/464) classified recent |
| Overall Categorical Agreement (Zimbabwe) [50] | - | 97.4% (452/464) with plasma |
For classifying recent infections, DBS and plasma show high categorical agreement, though slight differences in classification rates exist. In a large study in Zimbabwe, DBS assigned a slightly higher proportion of samples as recent compared to plasma (12.3% vs. 10.1%), with an overall concordance of 97.4% for recent/long-standing classification [50] [51].
Experimental Protocols for Method Comparison
To ensure valid and reproducible comparisons between DBS and plasma viral load measurements, adherence to standardized experimental protocols is critical. The following section details the key methodologies cited in recent literature.
Sample Collection and Processing
The foundational step involves the paired collection of venous blood for both sample types from study participants.
- Whole Blood Collection: A total of 4 mL of venous blood is collected into a vacutainer tube containing EDTA anticoagulant [16].
- Plasma Harvesting: Plasma is separated from whole blood via centrifugation, typically at 2500 RPM for 10 minutes. The harvested plasma is then aliquoted into cryovials [16].
- DBS Preparation: Approximately 50 µL of whole blood is dispensed onto each of five circles on a Whatman 903 filter paper card. The spots are air-dried at room temperature for 4-6 hours [16].
- Storage: Plasma aliquots are stored frozen at -20°C until testing. DBS cards are placed in zip-lock plastic bags with silica gel desiccant pouches and can be stored at -20°C or, for shorter periods, at room temperature [16].
HIV-1 RNA Extraction and Quantification
The Roche COBAS AmpliPrep/COBAS TaqMan system provides an automated platform for processing both sample types, as described in the Ethiopian study [16].
RNA Extraction:
- Plasma: A 1100 µL aliquot of plasma is loaded into the COBAS AmpliPrep instrument for automated RNA extraction, which is based on the silica-based capture principle [16].
- DBS: Two half-spots (6 mm in diameter) are punched out from the DBS card using a clean forceps and transferred to a lysis solution. The same automated extraction process on the COBAS AmpliPrep is then followed [16].
- A known concentration of HIV-1 Quantitation Standard (QS) RNA is added to both sample types to monitor extraction efficiency and act as an internal control [16].
Amplification and Detection: The extracted RNA (both target HIV-1 RNA and the QS) is eluted and added to an amplification mixture. The COBAS TaqMan analyzer performs real-time PCR amplification and quantification. The results are reported in log copies/mL [16].
Data Analysis for Method Comparison
Robust statistical analysis is essential for evaluating the agreement between the two methods.
- Correlation Analysis: Pearson’s correlation is used to assess the strength of the linear relationship between log-transformed DBS and plasma viral load values [16] [47].
- Bland-Altman Plot: This analysis is used to visualize the agreement between the two methods by plotting the difference between DBS and plasma values against their average. It helps identify any systematic bias and the limits of agreement [16] [47].
- Categorical Agreement: For studies involving recent infection testing (RITA), the concordance in classifying infections as "recent" or "long-standing" between DBS and plasma is calculated [50] [51].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of DBS or plasma-based viral load testing relies on a suite of specialized reagents and materials. The table below catalogs key solutions and their functions as derived from the experimental protocols.
Table 3: Key Research Reagent Solutions for HIV-1 Viral Load Testing
| Reagent / Material | Function / Application | Example from Search Results |
|---|---|---|
| EDTA Vacutainer Tubes | Anticoagulant for venous blood collection, prevents clotting for plasma and DBS preparation. | Used for collecting 4 mL of venous blood [16]. |
| Whatman 903 Filter Paper | Standardized cellulose paper for depositing and drying fixed volumes of blood for DBS. | ~50 µL of blood dispensed on each of five spots [16]. |
| Silica Gel Desiccant | Hygroscopic agent packaged with DBS cards to absorb moisture and maintain sample stability during storage and transport. | Placed in zip-lock bags with DBS cards [16]. |
| Roche COBAS AmpliPrep Reagents | Automated, silica-based system for the extraction and purification of HIV-1 RNA from both plasma and DBS samples. | Used for RNA extraction from 1100 µL plasma or two 6mm DBS punches [16]. |
| Roche COBAS TaqMan HIV-1 Test v2.0 | Real-time PCR assay for the amplification and quantitative detection of extracted HIV-1 RNA. | Used for quantification on the COBAS TaqMan analyzer [16]. |
| HIV-1 Quantitation Standard (QS) | Internal control with a known concentration of non-human RNA; added to each sample to monitor extraction efficiency and quantify the target. | Processed alongside patient samples during RNA extraction [16]. |
| Simoa Dry Blood Extraction Kit | Standardized solution for extracting proteins/analytes from DBS samples, compatible with ultrasensitive biomarker detection platforms. | Mentioned for streamlining DBS workflow for neurological biomarkers [52]. |
Discussion and Research Implications
The body of evidence confirms that DBS is a highly reliable alternative to plasma for HIV-1 viral load monitoring, particularly for determining treatment failure at the clinical threshold of 1000 copies/mL. The strong correlations and high categorical agreement underscore its validity [16] [50] [48]. The primary advantage of DBS lies in its logistical simplicity: minimal invasive blood collection, elimination of the cold chain, and ease of transportation from remote collection sites to centralized laboratories [16]. This directly addresses a critical barrier to achieving the UNAIDS 95-95-95 targets in resource-limited settings.
However, researchers must account for the consistent quantitative bias observed between the two methods. The slightly higher viral loads typically seen with DBS are likely attributable to the presence of cell-associated viral DNA in addition to RNA in whole blood, and potential hematocrit effects influencing elution volume from filter paper [16]. Consequently, while DBS is excellent for clinical monitoring and surveillance, plasma remains the preferred matrix for precise viral load quantification in clinical trials or pathogenesis studies requiring the highest accuracy.
Future research should focus on standardizing DBS protocols across different assay platforms and developing adjusted clinical cut-offs where necessary. Furthermore, the application of DBS for other diagnostic purposes, such as HIV drug resistance genotyping and the measurement of other biomarkers using ultrasensitive technologies like Simoa, represents a promising frontier for decentralized healthcare and large-scale research studies [52].
Wastewater-Based Surveillance (WBS) has emerged as a powerful public health tool, providing an unbiased, population-level snapshot of infectious disease dynamics. This guide compares its performance against traditional clinical surveillance and details the experimental protocols that underpin this novel methodology.
Performance Comparison: WBS vs. Clinical Surveillance
The table below summarizes quantitative findings from key studies, directly comparing the performance of WBS against clinical surveillance systems.
Table 1: Performance Metrics of Wastewater-Based Surveillance (WBS)
| Study Context & Scale | Correlation with Clinical Cases | Lead Time of WBS Signal | Key Findings & Advantages |
|---|---|---|---|
| National (Switzerland): 118 WWTPs, 23,025 samples [53] | Correlation with hospitalizations improved from 0.55 (raw data) to 0.77 after statistical adjustment for lab and demographic bias [53]. | Information not specified | Adjusted WBS data revealed distinct, evolving geographic clusters of SARS-CoV-2. WBS is less susceptible to biases from variable individual testing behaviors [53]. |
| Regional (Alberta, Canada): 12 WWTPs over 17 months [54] | Strong correlation during the third wave (r = 0.97); overall correlations ranged from r = 0.51 to 0.86 across communities of various sizes [54]. | Information not specified | The strength of correlation was not affected by the size of the population in the sewershed. WBS provides an unbiased, non-discriminate estimation of prevalence [54]. |
| City (Fuzhou, China): One WWTP serving 1.5 million people [55] | Positive correlation with sentinel hospital positivity rates and outpatient visits [55]. | 0 to 17 days lead time, with peaks in wastewater viral concentration preceding clinical reports [55]. | Wastewater surveillance effectively predicted COVID-19 infection trends, offering an early warning tool for public health [55]. |
| Near-Source (Schools): Four public schools [56] | SARS-CoV-2 RNA in school wastewater was associated with, and often preceded, clinically confirmed cases among students [56]. | Acted as a leading indicator of clinical disease within the school [56]. | Technically challenging with lower success rates in sample collection (64/79 vs. 66/66 for WWTPs) and lower viral concentrations compared to municipal WWTPs [56]. |
| Multi-System (China): Integrated surveillance (Wastewater, Hospital, Digital) [57] | Moderate correlation (N gene concentration: ρ = 0.698; N gene positivity: ρ = 0.776) [57]. | Same-day associations (lag 0) were identified for wastewater signals [57]. | An integrated, multichannel surveillance strategy leveraging multiple data streams can strengthen early warning and situational awareness [57]. |
Detailed Experimental Protocols for WBS
The validity of WBS hinges on standardized, yet adaptable, experimental protocols. The following methodologies are compiled from the cited studies.
Wastewater Sample Collection and Handling
The foundational step involves collecting representative samples of raw influent wastewater.
- Sampling Type: Most studies use 24-hour composite samples, which pool small volumes of wastewater collected at regular intervals over a day to account for diurnal variations [54] [55].
- Sampling Frequency: Ranges from multiple times per week (e.g., 2-3 days/week) [54] to once every three days [55].
- Sample Transport and Storage: After collection, samples are immediately transported under refrigeration and typically processed within 24 hours of collection. Early in the pandemic, freezing (-20°C) was common, but storage at 4°C has also been effectively used [54].
Virus Concentration and Nucleic Acid Extraction
Due to the highly dilute nature of wastewater, concentrating the virus is a critical step.
- Concentration by Centrifugation and Filtration: A common method involves a preliminary centrifugation step (e.g., 4,500g for 10 min) to remove large solids, followed by ultrafiltration of the supernatant using centrifugal filter units (e.g., 30-kDa molecular weight cut-off) to concentrate viral particles [54].
- Nucleic Acid Extraction: The concentrated sample undergoes nucleic acid extraction using commercial kits designed for soil, stool, or viral samples to co-purify RNA and DNA and overcome PCR inhibitors common in wastewater [54] [58]. The extracted nucleic acid is eluted in a small volume (e.g., 100 μL) [54].
Target Detection and Quantification
This step identifies and quantifies the pathogen of interest, typically via PCR-based methods.
- Reverse Transcription Quantitative PCR (RT-qPCR): This is the most widely used method. It involves a one-step RT-qPCR assay targeting specific genes of the virus (e.g., the N1 and N2 regions of the SARS-CoV-2 nucleocapsid gene) [54] [55].
- Absolute Quantification: The CT values from RT-qPCR are converted to absolute concentrations (e.g., genome copies per mL of wastewater) using a standard curve generated from samples with known concentrations of the target gene [55].
- Metagenomic Sequencing: For broader pathogen detection or variant tracking, shotgun metagenomic sequencing is used. This involves sequencing all nucleic acid in a sample, followed by computational assembly and alignment to reference databases to identify pathogens and their genomes [58].
Data Normalization and Analysis
To enable comparisons across time and space, measured viral concentrations are normalized.
- Normalization by Flow Rate and Population: Viral concentration (gc/mL) is multiplied by the daily wastewater flow rate (L/day) to calculate the total daily viral load, which is then normalized by the population served by the WWTP to report population-normalized viral load (e.g., gc/day/person) [53].
- Normalization by Fecal Biomarkers: To account for variations in human fecal input, viral concentrations are often normalized using biomarkers of human feces that are consistently shed at high levels, such as Pepper Mild Mottle Virus (PMMoV) or crAssphage [54] [56].
- Statistical Modeling: Advanced statistical models, including Bayesian frameworks, are employed to adjust for sources of bias and variability, such as differences between laboratory protocols and local population demographics [53].
Workflow of a Wastewater-Based Surveillance Program
The diagram below visualizes the step-by-step process of a typical WBS program, integrating the experimental protocols described above.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and materials essential for implementing WBS, based on the methodologies cited in the studies.
Table 2: Key Research Reagents and Materials for WBS
| Reagent / Material | Function in WBS Protocol |
|---|---|
| Centrifugal Filter Units (e.g., 30-kDa MWCO) | To concentrate viral particles from large volumes (e.g., 100 mL) of wastewater supernatant by ultrafiltration [54]. |
| Nucleic Acid Extraction Kits | To extract and purify total nucleic acid (RNA/DNA) from concentrated wastewater samples, often with protocols optimized for complex environmental samples [54]. |
| PCR Primers/Probes (e.g., for SARS-CoV-2 N1/N2) | For the specific detection and quantification of the target pathogen using RT-qPCR assays [54] [55]. |
| Standard Curves (Quantification Standards) | Comprised of known concentrations of the target gene, essential for converting RT-qPCR cycle threshold (Ct) values into absolute concentrations (e.g., gene copies/mL) [55]. |
| Process Controls (e.g., Cultured hCoV-229E) | A non-target virus added to each sample to measure the efficiency of the virus concentration and extraction steps, ensuring data quality [54]. |
| Inhibition Controls (e.g., Salmon DNA) | An exogenous DNA spike added to the sample to assess the degree of PCR inhibition from co-extracted wastewater contaminants, ensuring quantification accuracy [54]. |
| Fecal Biomarkers (e.g., PMMoV, CrAssphage) | Used as internal standards to normalize target pathogen signal for variations in human fecal input, improving data comparability [54] [56]. |
Navigating Technical Pitfalls and Enhancing Assay Precision in Viral Load Testing
In viral load quantification research, the reliability of experimental data hinges critically on controlling pre-analytical variables. Evidence indicates that approximately 70% of errors in diagnostic measurements originate in the pre-analytical phase, encompassing sample collection, storage, and processing [59]. For researchers and drug development professionals, systematic management of these variables is not merely a procedural concern but a fundamental determinant of data integrity, particularly in method correlation studies where consistency across platforms is paramount.
The transition of a sample from its in vivo state to laboratory analysis introduces multiple potential sources of variability. These include collection method appropriateness, time-to-processing intervals, storage conditions, and lysis efficiency [59]. In the specific context of viral load quantification, each variable can significantly impact nucleic acid yield, quality, and ultimate quantification accuracy. This guide objectively compares key parameters and methodologies to establish evidence-based practices for optimizing pre-analytical workflows, thereby enhancing the correlation and reproducibility of viral quantification methods.
Comparative Analysis of Pre-Analytical Conditions and Reagents
Sample Storage and Stability Conditions
The stability of biological analytes under various storage conditions is a foundational pre-analytical consideration. The following table synthesizes stability data for diverse sample types and analytes relevant to virological research.
Table 1: Stability of Analytes Under Various Storage Conditions
| Sample Type / Analyte | Room Temperature (RT) | Refrigerated (2-8°C) | Frozen (-20°C) | Frozen (-70°C or below) |
|---|---|---|---|---|
| Whole Blood (Coagulation Factors) | PT/aPTT stable ≤24h; FV unstable (↓60% in 24h) [60] | FII, FVII, FX stable ≤24h; FV stable ≤8h [60] | PT/aPTT stable ≤3 mo; not recommended for FVIII [60] | Most factors stable ≥18 months [60] |
| Centrifuged Plasma (Coagulation) | aPTT stable ≤8h; PT stable ≤24h [60] | Varies by factor (e.g., FVIII ≤2h) [60] | Short-term storage (≤2 weeks) acceptable [60] | Long-term storage preferred [60] |
| Flow Cytometry Samples | Storage ≤24h acceptable but increases debris/doublets [61] | Varies by cell type and marker [61] | Not typically used for cell surface immunophenotyping | Not typically used for cell surface immunophenotyping |
| DNA/RNA | Degrades rapidly without stabilizer | Short-term holding (with stabilizer) | Acceptable for long-term storage [59] | Gold standard for long-term storage [59] |
| Buccal Swab Lysates (for direct PCR) | Buffer chemistry and pH are critical; STR GO! buffer's high pH can inhibit MPS [62] | Buffer chemistry and pH are critical | Not applicable for direct PCR workflows | Not applicable for direct PCR workflows |
Lysis Buffer Performance and Compatibility
The efficiency of viral lysis and nucleic acid release is highly dependent on buffer composition and compatibility with downstream applications. The following table compares the performance of different lysis approaches in various experimental contexts.
Table 2: Comparison of Lysis Methods and Buffer Performance
| Lysis Buffer / Method | Compatible Downstream Analysis | Key Advantages | Key Limitations / Required Optimizations |
|---|---|---|---|
| SwabSolution (Promega) | Capillary Electrophoresis (CE), MPS (with optimization) [62] | Validated for direct PCR with ForenSeq; reduces hands-on time [62] | Can cause PCR inhibition in MPS; requires additive (5X AmpSolution) [62] |
| STR GO! Lysis Buffer (QIAGEN) | CE (with Investigator kit) [62] | Designed for compatibility with specific CE kits | High pH can inhibit MPS; requires spin-column purification for MPS [62] |
| Trizol / RNAlater | RNA sequencing, qRT-PCR [59] | Preserves RNA integrity immediately upon collection | Requires testing for specific sample types; incompatible with direct PCR |
| Fix & Perm (Life Technologies) | Cell surface + intracytoplasmic (SM+CY) staining for Flow Cytometry [61] | Allows combined surface and intracellular marker analysis | Can cause slight differences in cell population percentages vs. SM-only [61] |
| Generic Lysis Buffer (for E. coli) | Culture, filtration, OD measurement [63] | Can be characterized and optimized for specific applications | Requires validation for each novel application and sample type |
Detailed Experimental Protocols
Protocol: Evaluating Anticoagulant and Sample Age Impact on Cell Phenotyping
This protocol, derived from EuroFlow consortium experiments, assesses how anticoagulant choice and storage duration affect flow cytometry results in immunophenotyping [61].
- Sample Collection: Collect peripheral blood or bone marrow from healthy donors or patients in parallel using K3 EDTA and sodium heparin tubes.
- Sample Storage: Process samples immediately (0 h) or after storage for 24 hours at room temperature (RT).
- Staining Procedure:
- Follow EuroFlow standard operating procedures (SOPs) for staining.
- For Surface Membrane (SM)-only staining: Incubate with antibodies for 30 minutes, then lyse red cells with FACS Lysing Solution (1:10 dilution) [61].
- For SM + Cytoplasmic (SM+CY) staining: After surface staining, fix and permeabilize cells using Fix & Perm reagent for 15 minutes before intracellular staining [61].
- Flow Cytometry Acquisition: Acquire data on a calibrated flow cytometer (e.g., FACS Canto II) using standardized settings.
- Data Analysis:
- Analyze using software such as Infinicyt.
- Record the Median Fluorescence Intensity (MFI) for each marker on target cell populations.
- Calculate the percentage of identifiable cell populations, debris, and doublets.
- Calculate MFI differences between conditions (e.g., EDTA vs. heparin, 0h vs. 24h) using the formula:
[(MFI_ConditionA - MFI_ConditionB) / MFI_ConditionA] * 100%. - Consider MFI differences outside the ±30% range as biologically significant [61].
Protocol: Optimization of Crude Buccal Swab Lysates for MPS
This protocol addresses the optimization of direct PCR from buccal swabs for sensitive Massive Parallel Sequencing (MPS) workflows, a common challenge in generating viral sequence data [62].
- Sample Collection and Lysis:
- Collect buccal cells using cotton swabs.
- Lyse cells in SwabSolution or STR GO! Lysis Buffer according to the manufacturer's guidelines.
- Overcoming PCR Inhibition:
- For SwabSolution Lysates: Add 5X AmpSolution reagent directly to the PCR reaction to neutralize inhibitors [62].
- For STR GO! Lysates: Purify the lysate using a spin-column kit (e.g., QIAamp DNA Investigator Kit) to remove inhibitors and adjust buffer chemistry. Do not use these lysates directly in MPS.
- MPS Library Preparation and Sequencing:
- Use the optimized lysate with the ForenSeq DNA Signature Prep Kit (Primer Mix A or B).
- Purify, normalize, and denature libraries as per the manufacturer's protocol.
- Sequence on a platform such as the MiSeq FGx.
- Quality Assessment:
- Analyze data with the ForenSeq UAS software.
- Calculate the call rate for each sample:
(Number of successfully called genotypes / Total number of markers) * 100[62]. - A successful run should show a significant reduction in profile failure rates compared to unoptimized lysates.
Workflow Visualization: Pre-Analytical Phase
The following diagram maps the decision points and pathways within the pre-analytical phase, highlighting critical variables that require stringent control to ensure sample quality for viral load quantification.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful management of pre-analytical variables requires the use of specific, high-quality reagents. The following table details key materials and their functions in sample collection, storage, and lysis.
Table 3: Essential Reagents for Pre-Analytical Sample Management
| Reagent / Material | Primary Function | Application Notes |
|---|---|---|
| K3 EDTA Tubes | Anticoagulant (chelates Ca²⁺); preferred for lymphocyte immunophenotyping [61] | Provides longer marker expression stability for lymphocytes compared to heparin [61]. |
| Sodium Heparin Tubes | Anticoagulant (enhances antithrombin); can better preserve granulocyte antigens [61] | Not suitable for morphological assessment; can artefactually increase CD11b on monocytes [61]. |
| SwabSolution (Promega) | Lysis buffer for crude lysate preparation from buccal swabs [62] | Enables direct PCR but may require optimization (e.g., AmpSolution) for sensitive MPS applications [62]. |
| STR GO! Lysis Buffer (QIAGEN) | Lysis buffer designed for direct PCR with specific CE kits [62] | High pH can be incompatible with MPS kits; spin-column purification is recommended for MPS workflows [62]. |
| RNAlater / Trizol | RNA stabilizer; inhibits RNases immediately upon sample collection [59] | Critical for preserving accurate viral RNA quantification; choice between them should be validated for the specific sample type. |
| FACS Lysing Solution | Lyses non-nucleated red blood cells while preserving white blood cells for flow cytometry [61] | Typically used at a 1:10 (v/v) dilution in distilled water for SM-only staining protocols [61]. |
| Fix & Perm Reagent | Permeabilization buffer for intracellular (cytoplasmic) staining in flow cytometry [61] | Allows for combined surface and intracellular marker analysis (SM+CY); requires a fixation step first [61]. |
| 5X AmpSolution | PCR additive to neutralize inhibitors in crude lysates [62] | Effective for overcoming PCR inhibition in SwabSolution lysates for MPS, maintaining a direct PCR workflow [62]. |
The correlation and reliability of viral load quantification methods are fundamentally constrained by the least controlled pre-analytical variable. As demonstrated, variables ranging from anticoagulant selection and storage duration to lysis buffer chemistry exert measurable and often dramatic effects on downstream analytical results. A rigorous, standardized approach to sample collection, storage, and processing is not ancillary but central to robust assay performance. By adopting the evidence-based comparisons and optimized protocols outlined herein, researchers can significantly reduce pre-analytical noise, thereby enhancing the accuracy, reproducibility, and translational value of viral load data in both basic research and drug development contexts.
The Role of International Standards and Secondary Calibrators
In the field of virology and infectious disease management, particularly in transplant medicine and drug development, the accurate quantification of viral load is a critical parameter for diagnosing active infection, monitoring patient response to therapy, and assessing the efficacy of antiviral treatments [64] [65]. Quantitative real-time PCR (qPCR) has served as the cornerstone technique for this purpose. However, this method has been historically plagued by significant inter-laboratory variability, making the comparison of results across different clinical and research sites challenging [64]. This variability stems from differences in nucleic acid extraction methods, amplification platforms, primers, probes, and, most importantly, the calibrators used to generate quantitative standards [64].
The introduction of World Health Organization (WHO) International Standards was a landmark step toward mitigating this problem. These standards provide a universal reference with a defined potency in International Units (IU), intended to harmonize results across different measurement procedures [64] [65]. Secondary calibrators, or certified reference materials (CRMs), are then calibrated against these primary WHO standards and are used by diagnostic manufacturers and clinical laboratories in their routine test calibration hierarchies [66] [67]. The property that allows a reference material to show the same numerical relationship as clinical samples across different measurement procedures is known as commutability [67]. The availability of commutable secondary CRMs is crucial for ensuring the long-term equivalence of laboratory results for patient samples [66]. This guide objectively compares the performance of viral load quantification with and without the use of international standards and evaluates the accuracy of modern secondary calibrators.
Comparative Analysis of Viral Load Assay Performance
Impact of WHO International Standards on Inter-laboratory Variability
The variability of viral load results has been extensively documented through proficiency testing surveys. Data from 554 laboratories revealed a high degree of interlaboratory variability for several viruses, with interquartile ranges as high as 1.46 log10 copies/mL and the overall range for a given sample spanning up to 5.66 log10 copies/mL [65]. The adoption of WHO International Standards, which allow results to be reported in IU/mL, has led to some improvement in result variability. This improvement is more pronounced for certain viruses, with Epstein-Barr virus (EBV) viral load data showing notable improvement, while challenges remain for others [65].
A pivotal multicenter study compared CMV and EBV viral load testing at four major transplant centers. The findings highlighted a critical disparity: CMV viral load testing was accurate and within acceptable variation, whereas EBV viral load data were more variable and less accurate despite the use of international standards [64]. This suggests that for certain viruses, the mere existence of an international standard does not automatically guarantee harmonization, and other factors, such as the choice of extraction method or amplification target, may still contribute significant variability.
Table 1: Comparison of CMV and EBV Viral Load Assay Performance Across Multiple Centers
| Virus | Accuracy vs. WHO Standards | Inter-laboratory Variability | Key Findings |
|---|---|---|---|
| Cytomegalovirus (CMV) | Accurate [64] | Acceptable variation [64] | Comparison of viral load measurements across sites is possible using current assays and controls [64]. |
| Epstein-Barr Virus (EBV) | Less accurate [64] | More variable [64] | Despite WHO standards, data variability makes inter-laboratory comparison difficult [64]. |
| BK Virus (BKV) & Adenovirus (ADV) | Not specified in study | High variability (pre-standardization) [65] | Viral loads showed a high degree of interlaboratory variability across all tested viruses [65]. |
Accuracy of Secondary Calibrators
Secondary calibrators are essential for the day-to-day operation of clinical laboratories. Their accuracy is paramount for reliable patient results. A recent 2024 study re-evaluated the accuracy of commercially produced secondary standards for BK virus (BKV) and CMV using digital PCR (dPCR), a method known for its absolute quantification capabilities without the need for a standard curve [68].
The study found that modern secondary standards show markedly improved agreement with their nominal values compared to earlier assessments. The bias from manufacturer-assigned values ranged from 0.0 to 0.9 log10 units (either copies or IU)/mL [68]. Two key factors were identified that contributed to better accuracy:
- Normalization to International Units (IU): Standards calibrated to IU showed superior performance.
- Value Assignment by dPCR: Standards whose values were assigned using digital PCR demonstrated better agreement with nominal values compared to those assigned by real-time PCR (qPCR) [68].
This indicates a substantial improvement in the production of secondary viral standards, while also supporting the broader adoption of IU as a reporting unit and dPCR for value assignment in reference materials.
Table 2: Comparison of Quantitative Viral Load Technologies
| Technology | Quantification Method | Key Advantages | Key Limitations |
|---|---|---|---|
| Real-time PCR (qPCR) | Relative quantification using a standard curve [9]. | Widely available, accessible, and well-established [9]. | Sensitivity and quantification are limited by the standard curve; potential for high inter-laboratory variability [64] [9]. |
| Droplet Digital PCR (ddPCR) | Absolute quantification by partitioning samples into thousands of droplets [68] [9]. | Does not require a standard curve; higher sensitivity and precision; better for low viral loads [68] [9]. | More expensive and technically complex [9]. |
Experimental Protocols and Methodologies
Multicenter Comparison of Viral Load Testing
A study designed to compare CMV and EBV viral load testing across four clinical laboratories provides a robust experimental model for assessing standardization [64].
- Study Design: Viral load testing was performed at four independent clinical laboratories affiliated with major academic transplant centers. Each laboratory processed samples according to its own center-specific standard operating procedures (SOPs), and all samples were tested blindly [64].
- Quantitation Panels: Two types of panels were tested for each virus:
- Commercial Panel: The OptiQuant CMVtc and EBV Plasma Panels (Acrometrix) with manufacturer-specified copy numbers.
- WHO International Standard Panel: Comprising triplicate ten-fold serial dilutions of the 1st WHO International Standard for CMV (strain Merlin) and EBV (strain B95-8), reconstituted and diluted in dialyzed, defibrinated human plasma [64]. All panel components were anonymized, frozen at -80°C, and shipped on dry ice to each site.
- Viral Load Assays: Methodologies varied across sites, as detailed in Table 3. Key variations included:
- Nucleic Acid Extraction: Different automated systems (QiaCube, QiaSymphony, MagNA Pure) and kits with varying sample input volumes (200-1000 µL) and elution volumes (50-100 µL) [64].
- Amplification & Detection: Most sites used the Qiagen artus TM EBV/CMV kits targeting EBNA1 and Major IE genes, respectively, but on different platforms (Applied Biosystems 7500, QuantStudio 12K Flex, RotorGene Q). One site used a lab-developed assay targeting UL54 for CMV, and another used the Primera Dx ViraQuant kit on an ICEPlex system [64].
Table 3: Procedural Characteristics of Viral Load Assays at Participating Centers
| Site | Nucleic Acid Extraction | Amplification & Detection | Target Gene | Reportable Range |
|---|---|---|---|---|
| 1 | QiAmp Virus on BioRobot MDX | Qiagen artus on ABI 7500 | EBV: EBNA1CMV: Major IE | EBV: 500–5,000,000 cp/mLCMV: 313–3,130,000 cp/mL |
| 2 | QiAmp DNA Blood Mini Kit on QiaCube | Qiagen artus on QuantStudio 12K | EBV: EBNA1CMV: Major IE | EBV: >25 cp/mLCMV: >50 cp/mL |
| 3 | Virus/Bacteria kit on QiaSymphony | Qiagen artus on RotorGene Q | EBV: EBNA1CMV: Major IE | EBV: 300–1,500,000 cp/mLCMV: 1000–5,000,000 cp/mL |
| 4 | MinElute kit on QiaCube | Primera Dx ViraQuant on ICEPlex | EBV: EBNA-LPCMV: US28 | EBV: 750–15,000,000 cp/mLCMV: 750–15,000,000 cp/mL |
| 5 | MagNA Pure Compact | Lab-developed assays on ABI 7500/7300 | EBV: EBNA1CMV: UL54 | EBV: 4,000–40,000,000 cp/mLCMV: 2,000–1,250,000 cp/mL |
Digital PCR for Value Assignment of Secondary Standards
The 2024 study that re-examined the accuracy of secondary standards employed a rigorous methodology centered on digital PCR [68].
- Materials: Commercially produced secondary standards for both BKV and CMV were obtained from three different manufacturers.
- Digital PCR (dPCR) Analysis: The study used dPCR to provide an absolute count of viral copies without relying on a standard curve. This technique partitions a sample into thousands of nanoreactions, and a positive or negative amplification in each partition is counted to determine the absolute quantity of the target nucleic acid [68] [9].
- Comparison: The measured values from the dPCR analysis were compared against the nominal values (the manufacturer's assigned values) provided for each secondary standard. The bias was calculated as the difference between the measured log10 value and the nominal log10 value, reported in either copies/mL or IU/mL [68].
Visualizing the Standardization and Commutability Workflow
The following diagram illustrates the hierarchical pathway from international standards to patient results and the critical role of commutability assessments for secondary calibrators.
Diagram Title: Pathway to Standardized Viral Load Results
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in viral load quantification and standardization experiments, as derived from the cited methodologies.
Table 4: Essential Research Reagents for Viral Load Quantification
| Reagent / Material | Function in Viral Load Testing | Examples from Experimental Protocols |
|---|---|---|
| WHO International Standard | Primary reference material with defined International Units (IU) used to harmonize results globally. | 1st WHO International Standard for CMV (NIBSC 09/162); for EBV (NIBSC 09/260) [64]. |
| Secondary Calibrators (CRMs) | Commercially produced calibrators traceable to WHO Standards, used in routine lab test calibration. | OptiQuant CMVtc & EBV Plasma Panels (Acrometrix) [64]; Commercial BKV & CMV standards from various manufacturers [68]. |
| Nucleic Acid Extraction Kits | To isolate and purify viral DNA/RNA from clinical samples (e.g., plasma) for downstream PCR. | QiAmp DNA Blood Mini Kit, MagNA Pure Compact Nucleic Acid Isolation Kit [64]. |
| qPCR Master Mixes & Kits | Reagents containing enzymes, buffers, and probes for the amplification and detection of specific viral targets. | Qiagen artus TM EBV/CMV kits, Lab-developed master mixes [64]. |
| Digital PCR Reagents | Specialized master mixes and consumables for absolute quantification of viral load without a standard curve. | Reagents for partitioning samples (e.g., droplet generation oil) and PCR amplification [68] [9]. |
The adoption of WHO International Standards has undeniably improved the comparability of viral load data across different laboratories, particularly for viruses like CMV [64] [65]. However, challenges with inter-laboratory variability persist, especially for EBV, indicating that the standard alone cannot overcome all sources of methodological variation. The performance of secondary calibrators has seen significant improvements in recent years, with biases narrowing substantially [68]. The move towards value assignment of these calibrators using digital PCR and reporting in International Units is a positive step that promises even greater accuracy and harmonization in the future. For researchers and drug development professionals, these advancements are critical. They enable more reliable cross-comparison of data from multicenter clinical trials, enhance the assessment of antiviral drug efficacy by providing more precise viral load measurements, and ultimately contribute to better patient management strategies [64] [9]. The continued focus on commutability and the integration of advanced technologies like dPCR into the calibration hierarchy will be paramount for the next generation of viral load testing.
Quantitative viral load measurement is a cornerstone of modern virology, essential for diagnostics, vaccine development, and therapeutic monitoring [69] [70]. However, the persistence of PCR inhibitors in complex biological samples and the inherent inefficiencies of nucleic acid extraction from limited samples pose significant challenges to assay robustness, particularly for rare targets or low-frequency viral reservoirs [71] [72]. Quantitative real-time PCR (qPCR), while widely implemented, relies on calibration curves and is sensitive to efficiency variations caused by inhibitors [73] [70] [74]. This article objectively compares the performance of droplet digital PCR (ddPCR) with qPCR, focusing on the former's enhanced tolerance to inhibitors and its compatibility with simplified sample preparation methods like crude lysate, which circumvent the need for nucleic acid purification.
Performance Comparison: ddPCR vs. qPCR
The table below summarizes key performance characteristics of ddPCR and qPCR based on comparative studies.
Table 1: Quantitative Comparison of ddPCR and qPCR Performance Characteristics
| Performance Characteristic | ddPCR | qPCR | Experimental Context |
|---|---|---|---|
| Quantification Method | Absolute, without standard curve [74] | Relative, requires standard curve [70] [74] | Fundamental assay design [71] [74] |
| Precision (at higher concentrations) | Superior (Less variability) [73] | Lower (Higher variability) [73] | WHO and AcroMetrix CMV standards [73] |
| Sensitivity (LOD in clinical samples) | ( 4 \log_{10} ) copies/mL [73] | ( 3 \log_{10} ) copies/mL [73] | CMV in plasma samples [73] |
| Tolerance to Inhibitor (SDS) | Higher (IC(_{50}) log difference: 0.554 - 0.628) [72] | Lower (Reference) [72] | Inhibitors spiked into CMV PCR reactions [72] |
| Tolerance to Inhibitor (Heparin) | Higher (IC(_{50}) log difference: 0.655 - 0.855) [72] | Lower (Reference) [72] | Inhibitors spiked into CMV PCR reactions [72] |
| Tolerance to Inhibitor (EDTA) | Comparable (IC(_{50}) log difference: ~0.02 - 0.12) [72] | Comparable (Reference) [72] | Inhibitors spiked into CMV PCR reactions [72] |
| Performance with Crude Lysate | Accurate quantification demonstrated [71] | Not evaluated for crude lysate in sources | TREC quantification from 200 cells [71] |
| Dynamic Range | Wide, but may be narrower than qPCR [73] [74] | Very wide [74] | CMV standard dilution series [73] |
The Crude Lysate Method: A Protocol for Limited Samples
The preparation of crude lysate for ddPCR involves cell lysis without subsequent nucleic acid purification, preserving template material that might otherwise be lost. This protocol is adapted from a 2025 study that quantified rare T-Cell Receptor Excision Circles (TRECs) from limited cell samples [71].
The following diagram illustrates the streamlined workflow for preparing and analyzing samples via crude lysate ddPCR.
Detailed Experimental Protocol
- Cell Lysis: Resuspend the cell pellet (200–16,000 cells) in 20 µL of lysis buffer. The cited study found that Buffer 2 from the SuperScript IV CellsDirect cDNA Synthesis Kit yielded superior accuracy and linearity compared to other lysis buffers [71].
- Viscosity Breakdown (Critical Step): Treat the lysate with a DNase I-based viscosity breakdown protocol. This step digests genomic DNA and other nucleic acids that increase sample viscosity, which can otherwise impede droplet generation and lead to inaccurate quantification. This step was shown to significantly improve assay reliability and accuracy [71].
- Droplet Digital PCR Setup:
- Prepare the ddPCR reaction mix containing ddPCR master mix, primers, and probes.
- Combine the processed crude lysate with the reaction mix.
- Generate droplets using a droplet generator.
- Perform endpoint PCR amplification on a thermal cycler using the following profile [71]:
- Hold: 95°C for 10 minutes
- 40 cycles of:
- 94°C for 30 seconds
- 60°C for 60 seconds
- Final Hold: 12°C
- Droplet Reading and Analysis: Load the post-amplification droplets into a droplet reader. Use analysis software (e.g., QuantaSoft) to count positive and negative droplets and apply Poisson statistics to determine the absolute concentration of the target in the original lysate [71].
Mechanisms of Inhibition Tolerance in ddPCR
The fundamental principle of ddPCR—partitioning a sample into thousands of nanoliter-sized droplets—confers a higher tolerance to common PCR inhibitors compared to qPCR. The mechanism for this enhanced robustness is illustrated below.
In qPCR, inhibitors are distributed homogenously throughout the single reaction volume, negatively impacting the amplification efficiency of the entire sample. This leads to a higher Cycle threshold (Ct) and consequently, an underestimation of the target concentration [70]. In contrast, in ddPCR, the inhibitor is also partitioned. While droplets containing both a target molecule and a high local concentration of inhibitor may show delayed amplification or reduced fluorescence, they are still identifiable as positive at endpoint analysis. Quantification relies on the binary count of positive droplets, making the assay less susceptible to efficiency variations [72]. This mechanism allows ddPCR to maintain accuracy in the presence of inhibitors like SDS and heparin, against which it demonstrates significantly higher tolerance than qPCR [72].
Essential Research Reagent Solutions
The following table lists key reagents and their critical functions in setting up robust crude lysate ddPCR assays, based on the methodologies cited.
Table 2: Key Research Reagent Solutions for Crude Lysate ddPCR
| Reagent / Kit | Function in Crude Lysate ddPCR |
|---|---|
| SuperScript IV CellsDirect cDNA Synthesis Kit (Lysis Buffer) | Provides an optimized buffer for effective cell lysis that maintains target integrity and supports subsequent amplification [71]. |
| DNase I Enzyme | Critical for viscosity breakdown; digests genomic DNA to reduce sample viscosity, enabling consistent droplet generation and accurate quantification [71]. |
| ddPCR Master Mix | A specialized PCR mix containing DNA polymerase, dNTPs, and buffers formulated for the water-oil emulsion system of ddPCR [71]. |
| Droplet Generation Oil | Creates the water-oil emulsion necessary to partition the sample into tens of thousands of nanoliter-sized droplets [73]. |
| Primer/Probe Sets | Target-specific oligonucleotides for amplification and detection; must be highly specific and efficient. Pan-genotypic coverage should be verified for viral targets [75]. |
| PCR Enhancers (e.g., KAPA Enhancer) | Can be added to mitigate potential PCR inhibition from components in the cell lysate, improving the signal-to-noise ratio [75]. |
The body of evidence demonstrates that ddPCR offers a robust analytical platform, particularly in scenarios where assay robustness is challenged by PCR inhibitors or limited starting material. Its digital quantification principle inherently confers greater tolerance to inhibitors like SDS and heparin compared to qPCR. Furthermore, the successful adaptation of ddPCR for use with crude lysate protocols [71] simplifies workflows, minimizes template loss, and enables the quantification of rare targets from small cell populations. For researchers and drug development professionals working with complex samples, such as in viral reservoir studies or rare cell analysis, ddPCR provides a precise and reliable tool for absolute viral load quantification where traditional qPCR may struggle.
Statistical Approaches for Data Normalization and Bias Adjustment
In viral load quantification, the precision of research and diagnostic outcomes is fundamentally dependent on robust statistical methods for data normalization and bias adjustment. These techniques are crucial for ensuring that experimental results are accurate, comparable, and reproducible, particularly when correlating findings across different methodologies such as RT-qPCR and ddPCR. This guide objectively compares prevalent normalization and bias correction approaches, evaluates their impact on assay performance, and provides supporting experimental data. Framed within viral load quantification research, this analysis equips scientists and drug development professionals with the knowledge to select appropriate statistical tools for enhancing data integrity in molecular diagnostics and therapeutic development.
Data normalization and bias adjustment are foundational statistical processes used to remove non-biological, systematic variations from datasets, thereby allowing for meaningful comparisons across different experiments, platforms, or conditions. In the context of viral load quantification, such technical variations can arise from differences in sample collection, nucleic acid extraction efficiency, reagent batch effects, and instrument calibration.
Normalization typically refers to the process of scaling individual data points to a common baseline or standard. In viral load studies, this is essential for comparing results from different analytical runs or laboratories. The primary goal is to minimize the impact of confounding variables, making the data more reliable for assessing true biological differences, such as changes in viral titer in response to an antiviral treatment [76].
Bias Adjustment, on the other hand, often involves correcting for systematic errors that can skew results in a particular direction. A critical application in biomedical research is addressing class imbalance in datasets, where one outcome (e.g., infected samples) is vastly outnumbered by another (e.g., non-infected controls). Left uncorrected, models trained on such data can become biased toward predicting the majority class, leading to poor diagnostic performance for the minority class. Techniques like bias adjustment directly modify the model's parameters, such as the intercept term in a logistic regression, to counteract this imbalance and improve predictive accuracy for all classes [77].
Understanding and applying these techniques is not merely a statistical exercise; it is a critical component of ensuring that research conclusions and subsequent public health decisions are based on accurate and unbiased data.
Comparative Analysis of Normalization Techniques
Common Normalization Methods
Various normalization techniques are employed in quantitative data analysis, each with distinct mathematical foundations and optimal use cases. The table below summarizes the core features of several prevalent methods.
Table 1: Comparison of Common Data Normalization Techniques
| Technique | Formula | Key Feature | Best Use Case | Limitations |
|---|---|---|---|---|
| Z-Score (Standardization) | ( \frac{x - \mu}{\sigma} ) | Centers data around a mean (μ) of 0 and a standard deviation (σ) of 1. | Algorithms assuming a Gaussian distribution (e.g., linear regression, PCA) [76]. | Sensitive to extreme outliers. |
| Min-Max Scaling | ( \frac{x - min}{max - min} ) | Rescales data to a fixed range, typically [0, 1]. | Neural networks and algorithms requiring data on a bounded scale [76]. | Highly sensitive to outliers; compressed range if outliers present. |
| Quantile Normalization | Non-parametric; forces identical distributions across samples. | Makes distributions across different samples statistically identical. | Microarray data, high-throughput sequencing for cross-sample comparison [78]. | Assumes most features are not differentially expressed. |
| Linear Regression Normalization | Models and removes a linear trend from the data. | Corrects for systematic bias dependent on the magnitude of the measured parameter. | Liquid chromatography-mass spectrometry (LC-MS) data [78]. | Assumes a linear relationship underlying the bias. |
Methodological Workflow for Normalization
The application of normalization methods follows a general experimental protocol. The following diagram illustrates the key decision points and steps in a standard normalization workflow for quantitative data like viral load measurements.
Diagram 1: A workflow for selecting a data normalization technique.
Protocol for Application:
- Data Assessment: Begin by visually inspecting the raw data using histograms or box plots to understand its distribution and identify the potential presence of extreme outliers [79].
- Goal Definition: Determine the primary objective. Is it to make different samples comparable (e.g., multiple RT-qPCR runs), to standardize features for a machine learning model, or to prepare data for a specific statistical test that requires normally distributed data? [76]
- Technique Selection: Follow the logic in Diagram 1. For instance, if outliers are a major concern and the goal is feature standardization, Robust Scaling (which uses median and interquartile range) is preferable to Z-score or Min-Max [76]. If the data is roughly Gaussian and no outliers are present, Z-score is often a suitable default.
- Implementation and Validation: Apply the chosen normalization. Validate its effectiveness by ensuring that technical replicates show no statistically significant differences after processing, as demonstrated in proteomics studies [78].
Experimental Comparison of Viral Load Quantification Methods
Experimental Design and Correlation Analysis
The correlation between different viral load quantification methods was exemplified in a 2025 study comparing Reverse Transcription Quantitative PCR (RT-qPCR) and Droplet Digital PCR (ddPCR) for SARS-CoV-2 detection [9]. This study utilized data from randomized, double-blind, placebo-controlled clinical trials (NCT04668235, NCT05033145) conducted between 2021 and 2022.
Experimental Protocol:
- Sample Population: 453 patients with mild or moderate COVID-19.
- Sample Type: Nasal swabs.
- Comparison Method: Samples from each patient were tested in parallel using both RT-qPCR and ddPCR techniques.
- Data Collection: Viral load was tracked over multiple days (D1, D3, D5, etc.) in both placebo and antiviral-treated (Azvudine) groups.
- Quantification Basis: RT-qPCR estimated viral load via a standard curve, while ddPCR provided absolute quantification by counting nucleic acid molecules in partitioned droplets [9].
The results demonstrated a strong positive correlation between the two techniques during the initial phase of infection, validating RT-qPCR as a useful tool for tracking infection trends.
Table 2: Correlation of Viral Load Quantification by RT-qPCR and ddPCR over Time (Adapted from [9])
| Study Day | Correlation Coefficient (RHO) | P-value |
|---|---|---|
| Day 1 | 0.88 | < 0.001 |
| Day 3 | 0.84 | < 0.001 |
| Day 5 | 0.81 | < 0.001 |
| Day 7 | 0.79 | < 0.001 |
| Day 9 | 0.65 | < 0.001 |
| Day 11 | Not Significant | - |
| Day 13 | Not Significant | - |
Performance Divergence and Sensitivity Analysis
Despite a strong initial correlation, a key performance divergence was observed, particularly in the context of therapeutic monitoring. While the antiviral-treated group showed no significant difference in viral load compared to the placebo group when measured by RT-qPCR, ddPCR revealed a significant reduction in viral load on days 3, 5, 7, 9, and 11 (p < 0.002 to p < 0.001) [9].
This discrepancy underscores a critical bias in the RT-qPCR method when used for absolute quantification. The reliance on a standard curve constrains the estimated viral load, preventing it from exceeding the curve's upper limit. In contrast, ddPCR's absolute counting provides a more sensitive and reliable measure of the true viral load, especially at lower concentrations or when precise quantification is needed to assess treatment efficacy [9]. The relationship between these methodologies and their connection to bias is illustrated below.
Diagram 2: Method comparison and bias source in viral load quantification.
Advanced Application: Bias Adjustment for Imbalanced Data
Conceptual Framework and Algorithm
In machine learning applications for virology—such as classifying infected versus non-infected hosts from complex data—a common challenge is class imbalance. This occurs when the number of instances in one class significantly outweighs the other, causing a model to become biased toward the majority class.
Bias Adjustment is a direct algorithmic technique to mitigate this problem. The core idea is to recalibrate the bias term (or intercept) in a classification model during training to account for the uneven distribution of classes [77].
Algorithm for Binary Classification:
- For each epoch during model training, calculate the average output of the model's function,
f(x), for each class. - Represent this average for a class as
δ. - Adjust the model's bias term by subtracting
δfrom its current value. This adjustment ensures that the expected value off(x) - δbecomes zero, making the model predict each class as equally likely in the absence of other features [77]. - For final prediction, use the last calculated
δvalue from training to adjust the bias term in the activation function (e.g., sigmoid).
Theoretical Equivalence and Simulation
Bias adjustment is not an isolated technique but is theoretically linked to other common strategies for handling class imbalance. A 2025 simulation study demonstrated that oversampling (duplicating minority class instances) and adjusting class weights (increasing the cost of misclassifying minority instances) primarily affect the model's bias term, leaving its core functional relationships with features largely unchanged [77].
This finding unifies these approaches: oversampling, adjusting class weights, and explicit bias adjustment are, in essence, different means of achieving the same statistical adjustment. The choice between them can be based on computational efficiency and implementation convenience rather than a fundamental difference in outcome [77].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting viral load quantification experiments, particularly those involving PCR-based methods.
Table 3: Key Research Reagent Solutions for Viral Load Quantification
| Reagent / Material | Function | Application Note |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolate and purify viral RNA/DNA from complex sample matrices like wastewater or clinical swabs. | Critical for removing PCR inhibitors; efficiency impacts final viral load [80]. |
| Reverse Transcriptase Enzyme | Converts RNA into complementary DNA (cDNA) for PCR amplification. | Essential for RNA viruses (e.g., SARS-CoV-2, Dengue); fidelity and activity affect quantification accuracy [9]. |
| Taq Polymerase & Master Mix | Enzymatic amplification of target DNA sequences. Includes dNTPs and optimized buffer. | The core of PCR; batch-to-batch consistency is vital for reproducible Cq/Ct values in RT-qPCR [9]. |
| Sequence-Specific Primers & Probes | Bind to target viral sequences for specific amplification and detection. | Design is critical for specificity and sensitivity; must be validated for different viral serotypes [80]. |
| Quantification Standards | Known concentrations of synthetic nucleic acid used to generate a standard curve. | Required for absolute quantification in RT-qPCR; source of potential bias if not accurately calibrated [9]. |
| Wastewater Concentration Agents | (e.g., PEG) Concentrate viral particles from large-volume wastewater samples. | Key for Wastewater-Based Surveillance (WBS); allows detection of viruses in low-prevalence populations [80]. |
| RNase/DNase Inhibitors | Protect target nucleic acids from degradation during sample processing and storage. | Preserves sample integrity from collection to analysis, preventing underestimation of viral load. |
Head-to-Head: A Critical Comparative Analysis of Viral Load Quantification Assays
Within viral load quantification method correlation research, selecting the appropriate molecular technique is paramount for generating reliable, publication-quality data. Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) has long been the established gold standard for detecting and quantifying RNA viruses [81]. However, the more recent development of Droplet Digital PCR (ddPCR) offers a complementary approach based on different principles [82]. This guide provides an objective, data-driven comparison of these two technologies, focusing on their performance in sensitivity, dynamic range, and quantification methodology, which is critical for researchers and drug development professionals working in areas such as infectious disease monitoring, vaccine efficacy studies, and biomarker validation. The fundamental distinction lies in their core methodology: RT-qPCR is a relative quantification method that relies on external standard curves and measures amplification in real-time during the exponential phase, while ddPCR provides absolute quantification by partitioning a sample into thousands of nanodroplets, performing end-point PCR, and counting positive reactions using Poisson statistics [12] [83]. This difference in mechanism underlies the varied performance characteristics explored in this article.
Key Technological Differences and Principles of Operation
The operational workflows of RT-qPCR and ddPCR are fundamentally distinct, leading to their unique performance characteristics. Understanding these core principles is essential for selecting the appropriate method for a given application.
The diagram above illustrates the core procedural differences between the two technologies. RT-qPCR operates as a bulk reaction, where the entire sample mixture is amplified in a single tube or well. Fluorescence is monitored in real-time during the exponential phase of amplification, and the cycle at which the fluorescence crosses a predefined threshold (the quantification cycle or Cq) is recorded [12] [84]. The target concentration is determined by comparing the Cq value to a standard curve of known concentrations, resulting in a relative quantification [83].
In contrast, ddPCR begins with partitioning the sample into thousands of nanoliter-sized droplets, with each droplet functioning as an individual PCR reactor. This partitioning step is critical. After end-point PCR amplification, each droplet is analyzed for fluorescence to be counted as positive or negative for the target [12] [82]. The absolute concentration of the target, in copies per microliter, is then directly calculated based on the proportion of positive droplets using Poisson distribution statistics, eliminating the need for a standard curve [81] [83].
Comparative Performance Data from Clinical and Environmental Studies
Direct comparisons of RT-qPCR and ddPCR across various studies reveal distinct performance profiles, particularly regarding sensitivity, precision, and robustness.
Table 1: Quantitative Performance Comparison of RT-qPCR and ddPCR
| Performance Metric | RT-qPCR | ddPCR | Supporting Data |
|---|---|---|---|
| Quantification Approach | Relative (via Standard Curve) | Absolute (Direct Counting) | [12] [83] |
| Limit of Detection (LOD) | Varies with assay; less sensitive for low targets | Excellent; can detect ≤ 1 copy/μL [81] | LOD for SARS-CoV-2 N1: 1.99 copies/μL (ddPCR) [81] |
| Limit of Quantification (LOQ) | Broader dynamic range | Narrower dynamic range, can saturate at high concentrations [83] | LOQ for a nanoplate dPCR system: 54 copies/reaction [85] |
| Precision & Reproducibility | Good for mid-to-high abundance targets | Superior for low-abundance targets and small fold-changes (<2-fold) [84] [82] | ddPCR demonstrated superior accuracy for high viral loads of influenza A/B and SARS-CoV-2 [6] |
| Tolerance to PCR Inhibitors | Sensitive; inhibitors affect amplification efficiency and Cq values | Highly tolerant; partitioning dilutes inhibitors [83] [10] | dPCR showed greater consistency, particularly in complex respiratory matrices [6] |
Table 2: Application-Based Suitability and Cost Analysis
| Factor | RT-qPCR | ddPCR |
|---|---|---|
| Best Suited Applications | Routine gene expression, high-throughput pathogen screening, moderate-to-high abundance targets [82] | Detection of rare mutations, viral load monitoring (low copy), copy number variation, liquid biopsy [83] [82] |
| Sample Throughput | High (96- or 384-well formats) | Lower throughput due to partitioning step [83] |
| Cost Per Reaction | Lower | Higher (instrument and consumables) [83] |
| Assay Development & Validation | Well-established, requires standard curve and efficiency optimization | Simplified multiplexing, no standard curves needed [82] |
A 2025 study on respiratory viruses during the 2023-2024 "tripledemic" found that dPCR demonstrated "superior accuracy, particularly for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV," showing greater consistency and precision than RT-qPCR [6]. For trace-level detection, such as in wastewater surveillance, ddPCR's superior sensitivity is a key advantage. One study on SARS-CoV-2 reported that the assay limit of detection (ALOD) using RT-dPCR was "approximately 2–5 times lower than those using RT-qPCR" [13]. However, some studies, particularly those involving environmental samples like wastewater, have found the sensitivity gain to be more marginal, suggesting that the choice may depend on the specific sample matrix [86].
Detailed Experimental Protocols for Method Comparison
To ensure a fair and accurate comparison between RT-qPCR and ddPCR, the experimental design must minimize all variables except for the detection platform itself. The following protocols are synthesized from cited studies to serve as a template for a rigorous head-to-head performance evaluation.
Sample Preparation and Nucleic Acid Extraction
- Sample Collection: Use clinically relevant samples, such as nasopharyngeal swabs or wastewater samples, confirmed to be positive for the target pathogen (e.g., SARS-CoV-2, influenza) [6] [81]. Include samples stratified by expected viral load (high, medium, low) based on prior RT-qPCR Ct values.
- RNA Extraction: Perform nucleic acid extraction using standardized, automated systems (e.g., KingFisher Flex, STARlet Seegene) with validated kits [6] [81]. It is critical to split each extracted RNA sample into two aliquots for parallel testing on both platforms to eliminate extraction bias.
- Inhibition Testing: For wastewater or other complex matrices, consider using an inhibition removal kit (e.g., OneStep PCR Inhibitor Removal Kit) to assess the impact of inhibitors [86].
RT-qPCR Workflow and Protocol
- Reaction Setup: Use a one-step RT-qPCR approach. A typical 20 μL reaction contains: 10 μL of 2X One-Step Reaction Mix, 400 nM of each forward and reverse primer, 250 nM of probe, and 4 μL of template RNA [86].
- Thermocycling Conditions:
- Data Analysis: Generate a standard curve using a serially diluted standard of known concentration (e.g., synthetic RNA). The concentration of unknown samples is determined by interpolating their Cq values against this curve [13].
ddPCR Workflow and Protocol
- Reaction Setup: Use a one-step RT-ddPCR kit. A typical 20-22 μL reaction contains: 5 μL of One-Step RT-ddPCR Supermix, 2 μL of reverse transcriptase, 1 μL of DTT (300 mM), 900 nM of each primer, 250 nM of probe, and 4 μL of template RNA [86].
- Droplet Generation: Load the reaction mixture into a droplet generator (e.g., QX200 from Bio-Rad) to create thousands of nanoliter-sized droplets [81] [84].
- Thermocycling Conditions:
- Reverse Transcription: 50°C for 60 min.
- Enzyme Activation: 95°C for 10 min.
- Amplification (40-45 cycles): 94°C for 30 s (denaturation) and 61°C for 60 s (annealing/extension). A ramp rate of 2°C/s is recommended [86]. Note: Data is collected at the endpoint, not during cycling.
- Enzyme Deactivation: 98°C for 10 min.
- Droplet Reading and Analysis: Transfer the PCR-amplified droplets to a droplet reader (e.g., QX200). The software (e.g., QuantaSoft) counts the positive and negative droplets for each sample and uses Poisson statistics to calculate the absolute concentration in copies/μL [81] [86].
Visualization of Comparative Performance Logic
The following diagram synthesizes the decision-making process for selecting between RT-qPCR and ddPCR based on key experimental parameters and desired outcomes.
Essential Research Reagent Solutions
The following table details key reagents and materials required for performing the comparative experiments described in this guide, based on the methodologies from the cited literature.
Table 3: Essential Research Reagents for RT-qPCR and ddPCR Comparison
| Item | Function | Example Products & Kits |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolate high-quality RNA from complex clinical or environmental samples. | QIAamp Viral RNA Mini Kit [13], RNeasy PowerMicrobiome Kit [13], MagMax Viral/Pathogen Kit [6] |
| One-Step RT-qPCR Master Mix | Contains reverse transcriptase and DNA polymerase for direct amplification from RNA in a single tube. | TaqMan Fast Virus 1-Step Master Mix [13], Luna Universal Probe One-Step Reaction Mix [86] |
| One-Step RT-ddPCR Master Mix | Specialized supermix for digital PCR, containing reagents for reverse transcription, PCR, and droplet stabilization. | One-Step RT-ddPCR Advanced Kit for Probes [86] |
| Primer/Probe Assays | Target-specific oligonucleotides for amplification and detection. | Commercially validated assays (e.g., CDC N1, N2 for SARS-CoV-2) [81] [13] |
| Quantification Standards | Known-concentration reference materials for constructing standard curves in RT-qPCR. | AccuPlex SARS-CoV-2 Reference Material [81], synthetic RNA controls [86] |
| Droplet Generation Oil/Consumables | Essential for creating the water-in-oil emulsion droplets in ddPCR. | DG8 Cartridges and Gaskets (Bio-Rad) [84] |
| PCR Plates & Seals | Hardware for housing reactions during thermal cycling. | 96-well PCR plates, foil seals [86] |
Both RT-qPCR and ddPCR are powerful techniques for viral load quantification, yet they serve complementary roles in the researcher's toolkit. RT-qPCR remains the most suitable technology for high-throughput, routine quantification where target abundance is moderate to high, cost-effectiveness is critical, and a wide dynamic range is needed. Its established protocols and lower per-reaction cost make it ideal for large-scale screening [83] [82].
Conversely, ddPCR excels in applications demanding high precision, absolute quantification, and superior sensitivity. It is the preferred method for detecting low-abundance targets, quantifying subtle fold-changes (less than 2-fold), analyzing rare mutations, and working with challenging samples that may contain PCR inhibitors [6] [84] [82]. Its ability to provide absolute quantification without standard curves also simplifies assay development and validation.
The choice between these platforms should be guided by the specific experimental questions, sample types, and resource constraints. For comprehensive research programs, a hybrid strategy—using RT-qPCR for initial screening and ddPCR for confirmatory analysis of critical or low-level targets—can be highly effective in leveraging the distinct strengths of both technologies [83].
In the field of virology, accurately quantifying viral load is a cornerstone for clinical management, therapeutic development, and understanding disease pathogenesis. The emergence of SARS-CoV-2 and the subsequent COVID-19 pandemic have starkly highlighted the critical importance of reliable and comparable viral quantification methods. For researchers, scientists, and drug development professionals, selecting an appropriate methodology is not merely a technical choice but a fundamental decision that can shape experimental outcomes and clinical interpretations. This guide provides a objective comparison of the performance of major viral load quantification platforms, focusing on their correlation and concordance. Framed within the broader thesis that methodological agreement is vital for advancing viral load research, this analysis synthesizes experimental data to illustrate the strengths, limitations, and optimal applications of each technique, thereby offering a evidence-based resource for methodological selection in research and development.
Key Viral Load Quantification Platforms
The most commonly employed molecular methods for viral load quantification include reverse transcription quantitative PCR (RT-qPCR) and digital droplet PCR (ddPCR). While both are nucleic acid amplification tests, their underlying principles and quantification approaches differ significantly, leading to variations in their performance characteristics.
RT-qPCR is a widely established technique that estimates viral load by measuring the amplification of viral RNA in real-time. The quantity is determined by comparing the cycle threshold (Ct)—the number of amplification cycles required for the signal to cross a detection threshold—to a standard curve of known concentrations. The Ct value is inversely proportional to the viral load; a lower Ct indicates a higher amount of starting viral RNA [87] [88]. Although it is the workhorse of molecular diagnostics, its reliance on a standard curve and sensitivity to amplification efficiency can introduce variability [9].
ddPCR represents an advancement in quantification technology. This method partitions a sample into thousands of nanoliter-sized droplets, effectively creating individual reaction chambers. PCR amplification occurs within each droplet, and after the run, the droplets are analyzed to count the number that contains the target nucleic acid. This allows for absolute quantification of the viral load without the need for a standard curve, as the copy number is directly calculated using Poisson statistics [9]. This principle often grants ddPCR higher sensitivity and precision, particularly for samples with low viral loads [9].
Other methods also play crucial roles in viral load assessment. Viral Titration (VT), often performed via assays that detect cytopathic effect (CPE) in cell culture, quantifies infectious viral particles (e.g., TCID50/ml) rather than viral RNA [89] [90]. Immunohistochemistry (IHC) is a qualitative or semi-quantitative technique that uses antibodies to detect the presence and distribution of viral antigens within tissues, providing spatial context that molecular methods cannot [90].
Table 1: Comparison of Major Viral Load Quantification Platforms
| Method | Quantification Principle | Key Output | Primary Application |
|---|---|---|---|
| RT-qPCR | Relative quantification against a standard curve | Cycle Threshold (Ct) | Gold standard for diagnosis; widespread clinical use |
| ddPCR | Absolute quantification by partitioning and counting | Copies per mL | Detecting low viral loads; absolute quantification without standards |
| Viral Titration | Quantification of infectious virus in cell culture | TCID50/mL | Determining infectivity and culturable virus |
| Immunohistochemistry | Antibody-based detection of viral antigens | Semi-quantitative score (e.g., 0-3) | Evaluating viral distribution and association with tissue lesions |
Comparative Performance Data
Analytical Sensitivity and Concordance
A direct comparison of RT-qPCR and ddPCR for monitoring SARS-CoV-2 in patient samples reveals important differences in analytical performance. A 2025 study with 453 patients found that while both methods showed a strong positive correlation (RHO values 0.65-0.88) in viral load trends from days 1 to 9, ddPCR consistently detected higher absolute viral copy numbers. This discrepancy is attributed to the nature of RT-qPCR providing a logarithmic approximation constrained by its standard curve, whereas ddPCR provides an actual count of viral copies. The heightened sensitivity of ddPCR was particularly evident in assessing the efficacy of an antiviral treatment (Azvudine), where it showed a statistically significant reduction in viral load on days 3, 5, 7, 9, and 11, a dynamic that RT-qPCR failed to capture [9].
Studies in animal models further illuminate the agreement between different methods. Research on 342 SARS-CoV-2-infected rodents demonstrated that the agreement between techniques is highly dependent on the sample type and the infection phase. There was moderate agreement between methods detecting active viral replication (e.g., RT-qPCR and viral titration on tissue homogenates). However, the percentage of agreement between all methods decreased over time, and there was poor agreement specifically between RT-qPCR results and viral titration from oropharyngeal swabs. This underscores that RT-qPCR and viral titration on tissues are most reliable during the early and peak phases of infection [89] [90].
Correlation with Clinical and Transmission Outcomes
The relationship between quantified viral load and clinical or transmission outcomes is a critical area of investigation. A 2021 clinical study on 365 COVID-19 patients categorized into three groups based on RT-qPCR Ct values found that disease severity (mild, moderate, severe) did not show a statistically significant correlation with the Ct value groups. However, several biochemical parameters—including ALT, AST, CRP, and bilirubin—were significantly deranged across the different viral load groups, suggesting that viral load may have a more direct correlation with certain pathological processes than with the overall clinical severity classification [88].
The link between viral load and infectiousness has been quantitatively established. A sophisticated modeling study, which reconstructed the viral load of index cases at the time of contact, inferred that the probability of transmission is strongly dependent on viral load. The model predicted that for household contacts, the transmission probability increased from a baseline of 5% for viral loads below 10^6 copies/mL to as high as 48% for viral loads exceeding 10^10 copies/mL. The probability of transmission peaked around the time of symptom onset, with large inter-individual variations. This relationship was less pronounced in non-household contacts, highlighting the role of both viral load and contact context in transmission dynamics [91].
Table 2: Summary of Key Comparative Findings from Experimental Studies
| Study Focus | Key Finding on Correlation/Concordance | Experimental Data |
|---|---|---|
| RT-qPCR vs. ddPCR (Clinical) | Strong positive correlation in trend (D1-D9), but ddPCR shows higher absolute values and better tracks antiviral efficacy. | Correlation coefficient (RHO): 0.65-0.88 (p<0.001); Significantly higher sensitivity for ddPCR (p<0.002 to p<0.001) [9]. |
| Method Agreement (Animal Model) | Moderate overall agreement; agreement decreases over time; poor agreement between RT-qPCR and viral titration from swabs. | Agreement assessed by Cohen’s kappa; best performance of RT-qPCR and VT on tissue homogenates in early/peak infection [89] [90]. |
| Viral Load vs. Clinical Severity | No statistically significant correlation found between Ct value groups and disease severity. | p-value >0.05 for severity vs. Ct group; significant p-value (<0.05) for ALT, AST, CRP, bilirubin [88]. |
| Viral Load vs. Infectiousness | A strong, quantifiable relationship exists, with transmission probability rising sharply with viral load. | ~5% transmission probability at <10^6 copies/mL vs. ~48% at ≥10^10 copies/mL in households [91]. |
Experimental Protocols for Method Comparison
To ensure the validity and reproducibility of viral load method comparisons, standardized experimental protocols are essential. The following sections detail common methodologies derived from the cited literature.
Protocol for Parallel RT-qPCR and ddPCR Analysis
This protocol is adapted from a clinical study comparing SARS-CoV-2 viral load monitoring using both techniques [9].
- Sample Collection and Preparation: Nasopharyngeal or oropharyngeal swabs are collected from patients and placed in viral transport medium (VTM). Nucleic acids are extracted from the VTM using a commercial viral RNA kit (e.g., from Qiagen) on an automated extraction system (e.g., EZ1 Advanced XL), following the manufacturer's instructions. The final elution volume is typically 60 μL.
- Reverse Transcription Quantitative PCR (RT-qPCR):
- The RT-qPCR is performed using a one-step master mix and primers/probes targeting conserved viral genes (e.g., E, N, or ORF1ab).
- A standard curve is mandatory for quantification. It is generated using serial dilutions (e.g., 10-fold) of a positive control of known concentration, such as SARS-CoV-2 viral RNA at 1 × 10^4 copies/μL.
- The thermocycling conditions are as follows: Reverse transcription at 50°C for 15 minutes; initial denaturation at 95°C for 1 minute; followed by 45 cycles of denaturation at 95°C for 15 seconds and annealing/extension at 60°C for 30 seconds (with fluorescence collection).
- The viral load is estimated based on the Ct value and the standard curve.
- Droplet Digital PCR (ddPCR):
- The ddPCR reaction mix is prepared using a one-step RT-ddPCR master mix and the same primers/probes as used in the RT-qPCR assay for direct comparison.
- The reaction mix and sample extract are loaded into a droplet generator, which partitions the sample into approximately 20,000 nanoliter-sized droplets.
- The droplets are transferred to a PCR plate and amplified on a thermal cycler with a similar profile to the RT-qPCR protocol.
- After amplification, the plate is loaded into a droplet reader, which counts the positive and negative droplets for the target. The absolute concentration (copies/μL) is calculated by the instrument's software using Poisson statistics.
- Data Analysis: Viral loads from both methods are log-transformed for analysis. Correlation is assessed using statistical methods like Spearman's rank correlation coefficient (RHO). Statistical tests (e.g., t-tests or ANOVA) are used to compare viral load reductions between treatment groups over time.
Protocol for Multi-Method Agreement in Animal Models
This protocol is derived from studies assessing SARS-CoV-2 in experimentally infected rodents [90].
- Animal Infection and Sampling: Golden Syrian hamsters or K18-hACE2 transgenic mice are intranasally inoculated with a defined dose of the virus (e.g., 10^3 to 10^5.8 TCID50). At predetermined time points post-inoculation (e.g., 2, 4, and 7 days), animals are euthanized, and samples are collected. These typically include oropharyngeal swabs in VTM and tissues such as nasal turbinate, lungs, and brain, which are divided for molecular, virological, and histological analysis.
- RNA Extraction and RT-qPCR: Homogenates are created from tissue samples. RNA is extracted from swab media and tissue homogenates. RT-qPCR is performed to detect both viral genomic RNA (gRNA) and subgenomic RNA (sgRNA, an indicator of active replication) using specific primers/probes (e.g., targeting the E gene). Samples with a Ct value > 36.8 are considered negative.
- Viral Titration (Infectivity Assay): Homogenates of tissue samples or swab media are used to infect permissive cell lines (e.g., Vero-E6 cells). The cultures are observed for several days for the development of a virus-induced cytopathic effect (CPE). The infectious titer is calculated using the Reed-Muench method to determine the median Tissue Culture Infectious Dose (TCID50/mL). Samples below the limit of quantification (e.g., <10^1.8 TCID50/mL) are considered negative.
- Immunohistochemistry (IHC): Tissue samples are fixed in formalin, embedded in paraffin, and sectioned. Slides are stained using a primary antibody specific for a viral antigen (e.g., Nucleoprotein). The staining is evaluated by a pathologist in a blinded manner and assigned a semi-quantitative score (e.g., 0 = absent, 1 = low/multifocal, 2 = moderate/multifocal, 3 = high/diffuse).
- Agreement Analysis: Results from each method are first dichotomized (positive/negative) based on their predefined thresholds. Pairwise agreement between methods (e.g., RT-qPCR vs. VT, VT vs. IHC) is assessed using Cohen's kappa coefficient to correct for chance agreement. The correlation between positive results on a continuous scale (e.g., Ct value vs. IHC score) can be evaluated using Spearman's correlation.
Essential Research Reagent Solutions
The successful implementation of the protocols above relies on a suite of specific reagents and materials. The following table details key solutions for viral load quantification research.
Table 3: Essential Research Reagents for Viral Load Quantification
| Reagent/Material | Function/Description | Example Use Case |
|---|---|---|
| Viral Transport Medium (VTM) | Preserves viral integrity in swab samples during transport and storage. | Collection of nasopharyngeal/oropharyngeal swabs from patients or animals [90] [92]. |
| Nucleic Acid Extraction Kits | Isolate pure viral RNA from complex clinical samples (VTM, tissue homogenates). | Preparation of template RNA for downstream RT-qPCR and ddPCR assays [9] [92]. |
| One-Step RT-qPCR/RT-ddPCR Master Mix | Contains enzymes and reagents for reverse transcription and PCR amplification in a single tube. | Detection and quantification of SARS-CoV-2 RNA in extracted samples [9] [92]. |
| Primers & Probes | Sequence-specific oligonucleotides that bind and detect target viral genes (e.g., E, N, S, ORF1ab). | Amplifying and detecting SARS-CoV-2 RNA; using multiple targets increases assay robustness [90] [92]. |
| Quantified RNA Standards | Synthetic RNA of known concentration used to generate a standard curve for RT-qPCR. | Enabling absolute quantification and ensuring assay performance across different runs [9] [92]. |
| Cell Lines (e.g., Vero-E6) | Permissive cells used to culture and quantify infectious virus particles. | Viral titration assays to determine TCID50/mL and confirm active, replicating virus [89] [90]. |
| Specific Antibodies | Used in IHC to detect viral antigen proteins within fixed tissue sections. | Localizing and semi-quantifying virus distribution and load in tissues (e.g., lung) [90]. |
| gBlock Gene Fragments | Synthetic double-stranded DNA fragments containing target viral sequences. | Generating in-vitro transcribed RNA for use as a quantitative standard when none is commercially available [92]. |
The comparative analysis of viral load quantification methodologies reveals a landscape defined by correlation but also by critical differences in performance. RT-qPCR remains the accessible and reliable workhorse for clinical diagnosis, while ddPCR offers superior sensitivity and absolute quantification, particularly valuable for monitoring low viral loads and assessing antiviral drug efficacy in research settings. Methods that detect infectious virus, like viral titration, provide a different dimension of information that does not always perfectly align with nucleic acid detection, a discrepancy that researchers must account for.
The choice of methodology should be dictated by the specific research question. For pure detection and large-scale screening, RT-qPCR is sufficient. For studies requiring the utmost precision, absolute quantification, or detection of low-abundance targets, ddPCR is the preferred tool. Meanwhile, techniques like viral titration and IHC remain indispensable for answering questions about infectivity and tissue pathology, respectively. A multi-faceted approach, leveraging the strengths of each platform, will provide the most comprehensive understanding of viral dynamics and continue to drive forward both basic virology and applied drug development.
Viral load quantification serves as a critical biomarker for managing viral infections, guiding treatment decisions, and evaluating therapeutic efficacy in both clinical and research settings. The precision and accuracy of these quantification methods directly impact patient outcomes and drug development processes. This guide provides a comparative analysis of viral load measurement technologies within the broader context of viral load quantification method correlation research, focusing on case studies in COVID-19 and HIV management. For researchers and drug development professionals, understanding the technical nuances, performance characteristics, and clinical applicability of these methods is paramount for advancing therapeutic strategies and optimizing patient care. The continuous evolution of viral pathogens, including the emergence of new variants and recombinants, further underscores the necessity for reliable and adaptable quantification platforms that can accommodate genetic diversity while maintaining analytical sensitivity [93] [94].
Comparative Analysis of Viral Load Quantification Methods
Viral load quantification methodologies differ fundamentally in their technical principles, analytical performance, and suitability for specific clinical or research applications. The two primary categories of nucleic acid amplification tests (NAATs) are signal amplification and target amplification techniques, each with distinct advantages and limitations.
Method Classifications and Principles
Reverse Transcription Quantitative PCR (RT-qPCR) represents the most widely adopted target amplification technique for RNA virus quantification. This method relies on the reverse transcription of viral RNA into complementary DNA (cDNA), followed by quantitative PCR amplification with fluorescence-based detection in real-time. Quantification is achieved through comparison to a standard curve of known concentrations, making it a relative quantification method [95] [9]. While RT-qPCR offers high throughput and widespread accessibility, its accuracy is dependent on the quality and reliability of the standard curve, and it may be affected by amplification inhibitors and sequence variations.
Digital Droplet PCR (ddPCR) is an emerging target amplification technology that provides absolute quantification without requiring a standard curve. The technique partitions the sample into thousands of nanoliter-sized droplets, each functioning as an individual PCR reaction. After amplification, the fraction of positive droplets is counted, and the original target concentration is calculated using Poisson statistics. This partitioning approach enhances resistance to inhibitors and improves precision for low-abundance targets [95] [9].
Branched DNA (bDNA) assays utilize signal amplification rather than target amplification. This method involves capturing target RNA onto a solid phase followed by hybridization with multiple sets of oligonucleotide probes that ultimately amplify the signal through branching structures. Since bDNA does not involve nucleic acid amplification, it is less susceptible to contamination and PCR inhibitors, but may have lower overall sensitivity compared to amplification-based methods [94].
Performance Comparison in Clinical Applications
The performance characteristics of viral load assays become particularly evident when applied to diverse clinical scenarios and genetically variable viruses. The following comparative data illustrates key performance differences across platforms and their implications for clinical management.
Table 1: Comparative Performance of Viral Load Assays Across Pathogens
| Pathogen | Assay Method | Sensitivity (LLoQ) | Dynamic Range | Key Advantages | Identified Limitations |
|---|---|---|---|---|---|
| SARS-CoV-2 | RT-qPCR | Varies by assay | Varies by assay | Widely available, standardized | Limited sensitivity at low viral loads; relative quantification only [95] |
| SARS-CoV-2 | ddPCR | <10 copies/mL | Up to 10^6 copies/mL | Absolute quantification; superior for low viral loads; higher sensitivity [95] [9] | Higher cost; technical complexity; lower throughput [9] |
| HIV-1 Group M | LCx HIV RNA Quantitative | 50 copies/mL | 50-1,000,000 copies/mL | Reliable quantification across diverse subtypes [94] | Platform-specific limitations |
| HIV-1 Group M | AMPLICOR HIV-1 MONITOR v1.5 | 50 copies/mL | 50-75,000 copies/mL | Established clinical utility | Failed to detect Group O viruses [94] |
| HIV-1 Group O | LCx HIV RNA Quantitative | 50 copies/mL | 50-1,000,000 copies/mL | Effectively quantifies genetically diverse strains [94] | Limited comparative data for newer platforms |
| HIV-1 Group O | bDNA v3.0 | 50 copies/mL | 50-500,000 copies/mL | Detects Group O viruses | Consistently underquantified group O strains [94] |
Table 2: Correlation Between RT-qPCR and ddPCR for SARS-CoV-2 Viral Load Monitoring
| Study Population | Day of Testing | Correlation Coefficient (RHO) | Statistical Significance (p-value) | Key Finding |
|---|---|---|---|---|
| Moderate COVID-19 (IGZ-1) | D1-D9 | 0.65-0.88 | <0.001 | Strong positive correlation during early disease phase [9] |
| Mild COVID-19 (IGZ-2) | D1-D9 | 0.65-0.88 | <0.001 | Consistent correlation across disease severity [9] |
| Both populations | D11-D13 | No significant correlation | NS | Divergence in late disease phase [9] |
The data from comparative studies demonstrate that method selection significantly influences viral load interpretation and, consequently, clinical decision-making. For SARS-CoV-2, ddPCR exhibits enhanced sensitivity for detecting low viral loads, which is particularly valuable for assessing treatment response and disease progression in immunocompromised patients or those receiving antiviral therapies [95] [9]. In HIV management, the genetic diversity of the virus presents unique challenges, as evidenced by the variable performance of different assays against non-subtype B viruses and group O strains [94]. This highlights the importance of selecting assays with proven efficacy against the specific viral populations relevant to the patient demographic or research focus.
Experimental Protocols for Method Comparison
Robust experimental design is essential for meaningful comparison of viral load quantification methods. The following protocols outline standardized approaches for evaluating assay performance across different viral pathogens and sample types.
Sample Preparation and Processing
Sample Collection and Storage:
- For SARS-CoV-2 testing, collect nasopharyngeal swabs, nasal swabs, or lower respiratory tract samples using appropriate collection kits. Store samples at 4°C for processing within 72 hours or at -70°C for long-term storage [95] [9].
- For HIV-1 testing, collect plasma samples in EDTA-containing tubes via venipuncture. Process within 6 hours of collection by centrifugation at 800-1600 × g for 20-30 minutes at room temperature. Aliquot plasma into sterile tubes and store at -70°C until analysis [94] [96].
- For method comparison studies, parallel sampling is recommended, where sufficient sample volume is divided for simultaneous testing by different platforms.
Nucleic Acid Extraction:
- Use automated extraction systems (e.g., QIAamp, MagNA Pure) with appropriate chemistry for viral RNA isolation.
- Input volumes should be standardized across methods (typically 200-1000 μL) to enable direct comparison.
- Include extraction controls (negative and positive) to monitor extraction efficiency and potential contamination.
- Elute nucleic acids in nuclease-free water or TE buffer and store at -70°C if not used immediately.
Parallel Testing Methodology
SARS-CoV-2 Protocol (Based on IGZ-1/IGZ-2 Studies):
- Sample Panel Preparation: Create a panel of clinical samples representing a range of viral loads (low, medium, high) as determined by reference methods. Include serial samples collected over time from treated patients to monitor viral dynamics [9].
- RT-qPCR Analysis: Perform RT-qPCR using approved primer/probe sets targeting conserved regions (e.g., N, E, ORF1ab genes). Use a standard curve generated from serial dilutions of quantified SARS-CoV-2 RNA (e.g., 1 × 10^4 copies/μL) for absolute quantification [9].
- ddPCR Analysis: Partition extracted RNA into approximately 20,000 droplets using a droplet generator. Perform reverse transcription and PCR amplification with the same primer/probe sets used for RT-qPCR. Read plates on a droplet reader to determine copies/μL based on Poisson statistics [9].
- Data Analysis: Calculate correlation coefficients (e.g., RHO values) between methods across different time points and disease severities. Perform statistical testing (e.g., t-tests) to evaluate significant differences in viral load reduction between treatment groups [9].
HIV-1 Subtype Diversity Protocol:
- Virus Panel Preparation: Assemble a panel of well-characterized viral isolates representing predominant group M subtypes (A-G) and recombinants, as well as group O viruses. Include the WRAIR clade panel or similar reference materials [94].
- Serial Dilution Series: Prepare fivefold serial dilutions of each virus isolate in HIV-1-negative human plasma to assess quantification linearity across the dynamic range [94].
- Parallel Testing: Test all samples using multiple commercial platforms (e.g., LCx HIV, AMPLICOR MONITOR v1.5, bDNA v3.0) according to manufacturers' specifications [94].
- Sequence Analysis: Perform sequence analysis of primer and probe binding regions (gag p24, pol integrase, env gp41) to identify mismatches that may impact quantification accuracy [94].
- Statistical Comparison: Calculate mean differences, coefficients of variation, and regression parameters to evaluate agreement between methods across different subtypes.
Research Reagent Solutions for Viral Load Quantification
Selecting appropriate reagents and reference materials is fundamental to establishing robust viral load quantification assays. The following table outlines essential research reagents and their applications in method development and validation.
Table 3: Essential Research Reagents for Viral Load Assay Development
| Reagent Category | Specific Examples | Function & Application | Performance Considerations |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp Viral RNA Mini Kit, MagNA Pure Compact RNA Isolation Kit | Isolation of viral nucleic acids from clinical samples; removal of PCR inhibitors | Input volume compatibility; yield efficiency; processing time; automation capability |
| Reverse Transcriptase Enzymes | SuperScript IV Reverse Transcriptase, PrimeScript RTase | cDNA synthesis from viral RNA templates; first step in RT-PCR and ddPCR | Processivity; fidelity; tolerance to inhibitors; temperature optimum |
| PCR Master Mixes | TaqMan Fast Virus 1-Step Master Mix, ddPCR Supermix for Probes | Provides optimized buffer, enzymes, and dNTPs for amplification | Compatibility with probe chemistry; inhibitor resistance; amplification efficiency |
| Quantified RNA Standards | AccuPlex SARS-CoV-2 Reference Material, HIV-1 Subtype Panels | Standard curve generation for RT-qPCR; assay calibration and quality control | Commutability with clinical samples; stability; concentration accuracy; subtype representation |
| Primer/Probe Sets | CDC SARS-CoV-2 N1/N2 assays, HIV-1 gag/pol targets | Sequence-specific detection of viral targets; determines assay specificity | Conservation across variants; minimal self-complementarity; GC content; specificity testing |
| Droplet Generation Oil | DG8 Cartridges for Droplet Digital PCR | Formation of nanoliter-sized droplets for ddPCR partitioning | Low fluorescence background; stable droplet formation; chemical compatibility |
| Positive Controls | Whole virus preparations, in vitro transcribed RNA | Monitoring of extraction efficiency; inhibition detection; process control | Similar extraction characteristics to target; stability; concentration consistency |
| Negative Controls | Nuclease-free water, human plasma/serum negative for target viruses | Contamination monitoring; background signal assessment | Confirmed absence of target; matrix matching to clinical samples |
The selection and quality control of these reagent solutions directly impact the reliability, reproducibility, and diagnostic accuracy of viral load quantification assays. Researchers should prioritize reagents that have been validated for their specific application and sample matrix, with particular attention to lot-to-lot consistency and stability under anticipated storage conditions.
Clinical Implications and Therapeutic Monitoring
The choice of viral load quantification method has direct consequences for clinical decision-making and therapeutic monitoring in both COVID-19 and HIV management.
Impact on COVID-19 Management
In COVID-19, viral load dynamics serve as an important indicator of disease progression and treatment response. The enhanced sensitivity of ddPCR has demonstrated particular utility in several clinical scenarios:
Therapeutic Monitoring:
- Clinical trials of antivirals such as AZVUDINE (FNC) revealed that ddPCR could detect significant viral load reductions between treated and placebo groups as early as day 3 (p < 0.002), while RT-qPCR showed no significant differences [9].
- This heightened sensitivity enables more precise assessment of antiviral efficacy, particularly for evaluating early treatment response and determining optimal treatment duration.
Resolution of Discordant Results:
- ddPCR has proven valuable in detecting persistent infection in immunocompromised patients who test negative by RT-qPCR but continue to experience symptoms, enabling appropriate extension of antiviral therapy [95].
- The absolute quantification capability of ddPCR eliminates variability associated with standard curve generation in RT-qPCR, providing more reliable measurements for tracking viral clearance [9].
Impact on HIV Clinical Management and Drug Development
In HIV care, accurate viral load monitoring is essential for guiding antiretroviral therapy decisions and assessing treatment efficacy:
Management of Diverse HIV Strains:
- Studies have demonstrated significant variability in assay performance across different HIV-1 subtypes. For example, the AMPLICOR HIV-1 MONITOR v1.5 test failed to detect group O viruses entirely, while the LCx HIV assay reliably quantified both group M and group O viruses [94].
- This highlights the critical importance of selecting appropriate quantification methods in regions with diverse HIV strains or when managing infections acquired in different geographical locations.
Clinical Trial Considerations:
- The high genetic diversity of HIV necessitates viral load assays capable of accurately quantifying non-subtype B viruses in clinical trials to ensure reliable assessment of investigational antiretrovirals across global populations [94].
- Comparative studies have shown that treatment outcomes between clinical trial participants and routine care patients were similar when using consistent viral load monitoring approaches, supporting the generalizability of trial results to real-world settings [97].
The selection of viral load quantification methods represents a critical decision point with far-reaching implications for clinical management and therapeutic development in viral diseases. Based on comparative studies across COVID-19 and HIV, ddPCR technology offers distinct advantages for applications requiring high sensitivity and absolute quantification, particularly in therapeutic monitoring and resolution of discordant clinical findings. However, RT-qPCR remains the workhorse for routine diagnostic applications due to its established infrastructure, lower cost, and high throughput capacity. For HIV management, method selection must account for viral genetic diversity, with platform choice guided by the subtypes prevalent in the target population. As viral pathogens continue to evolve and new therapeutics emerge, the ongoing evaluation and refinement of viral load quantification methods will remain essential for optimizing patient outcomes and advancing drug development. Researchers and clinicians should consider these performance characteristics, along with their specific application requirements and resource constraints, when selecting the most appropriate viral load quantification platform.
Assessing the Influence of Laboratory Protocols on Wastewater Surveillance Data
Wastewater surveillance has emerged as a crucial public health tool, providing an unbiased community-level snapshot of pathogen circulation. The reliability of this data, however, is fundamentally dependent on the laboratory protocols employed for sample processing and analysis. Substantial methodological variability across laboratories can introduce significant quantification biases, challenging the comparability of surveillance data across different locations and timepoints [98]. This guide objectively compares the performance of leading laboratory protocols in wastewater surveillance, providing researchers and public health professionals with experimental data to inform method selection and standardization efforts. Within the broader context of viral load quantification method correlation research, understanding these influences is paramount for developing robust, transferable interpretation models that can enhance public health decision-making.
Key Laboratory Workflows in Wastewater Surveillance
The journey from wastewater sample to quantifiable viral data involves several critical steps, each introducing potential variability. The workflow begins with sample collection and preparation, proceeds through viral concentration and RNA extraction, and culminates in molecular detection and data normalization. A generalized workflow is depicted in the diagram below.
Sample Concentration Methods
Virus concentration is a critical first step to detect low viral abundances in wastewater. Multiple methods are employed, with significant performance differences.
Polyethylene Glycol (PEG) Precipitation: This method uses PEG and salts to precipitate viruses out of solution via centrifugation. A 2024 study demonstrated that PEG-based concentration yielded higher detection sensitivity and viral loads for SARS-CoV-2 compared to skimmed milk flocculation (SMF) when processing samples from a wastewater treatment plant in Greece [99]. The protocol involves stirring wastewater with glycine, followed by centrifugation and precipitation with PEG 8000 and NaCl [99].
Skimmed Milk Flocculation (SMF): This technique relies on the adsorption of viruses onto skimmed milk flocs in an acidified solution. The flakes settle by gravity, and the pellet is collected via centrifugation. While cost-effective, the aforementioned study found it to be less sensitive than PEG precipitation for SARS-CoV-2 [99].
Ultrafiltration & Ultracentrifugation: These methods use physical forces—either filtration through specialized membranes or high-speed centrifugation—to concentrate viral particles. The CDC notes these as viable approaches, particularly highlighting ultracentrifugation for primary sludge samples [100].
RNA Extraction and Detection
Following concentration, viral RNA must be efficiently extracted and purified from the complex wastewater matrix to avoid inhibition in downstream molecular assays.
RNA Extraction: Commercial kits designed for environmental samples are recommended, with protocols that include RNase denaturants to preserve RNA integrity. To prevent degradation, extracted RNA should be aliquoted and stored at -70°C or below to avoid multiple freeze-thaw cycles [100] [101].
Molecular Detection:
- RT-qPCR (Reverse Transcription Quantitative PCR): The most common method for detecting and quantifying viral RNA in wastewater. It performs reverse transcription and DNA amplification in real-time, with results quantified against a standard curve [100] [101].
- RT-ddPCR (Reverse Transcription Droplet Digital PCR): This method partitions the sample into thousands of nanoliter-sized droplets for individual PCR reactions. A key advantage is that it reduces the effects of inhibition common in wastewater samples, as reverse transcription occurs within separate droplets rather than in a bulk solution [100] [101].
Comparative Performance of Key Protocols
The selection of laboratory protocols directly influences the sensitivity, accuracy, and inter-laboratory comparability of wastewater surveillance data. The table below summarizes quantitative performance data from comparative studies.
Table 1: Quantitative Comparison of Wastewater Surveillance Method Performance
| Method Category | Specific Method/Assay | Key Performance Finding | Reported Quantitative Data | Study Context |
|---|---|---|---|---|
| Virus Concentration | Polyethylene Glycol (PEG) Precipitation | Higher detection sensitivity and viral loads vs. SMF | Consistent higher viral loads than SMF from identical samples [99] | SARS-CoV-2 in WWTP influent [99] |
| Virus Concentration | Skimmed Milk Flocculation (SMF) | Lower detection sensitivity vs. PEG | Lower viral loads than PEG from identical samples [99] | SARS-CoV-2 in WWTP influent [99] |
| Data Normalization | PMMoV Normalization | High inter-lab variability | ICC = 0.22 (poor concordance) [102] | Inter-lab study across 15 methods [102] |
| Inter-lab Comparability | SARS-CoV-2 RT-qPCR | Moderate concordance across labs | ICC ≈ 0.70 (moderate concordance) [102] | Inter-lab study across 15 methods [102] |
| Rapid Detection | RPA with Nanodiamonds | High sensitivity & specificity for raw wastewater | 100% Sensitivity, 100% Specificity; LOD: 7 copies/assay [103] | Pilot with Welsh National WBE samples [103] |
| Rapid Detection | RPA with Carbon Black | Lower sensitivity vs. nanodiamond platform | 80% Sensitivity, 100% Specificity [103] | Pilot with Welsh National WBE samples [103] |
Impact on Data Comparability and Public Health Action
The influence of laboratory protocols extends beyond technical performance to directly impact the utility of data for public health decision-making.
Inter-Laboratory Variability: A 2025 inter-laboratory study analyzing split samples across 15 different laboratory methods found that SARS-CoV-2 measurements showed moderate concordance even without standardized protocols [102]. However, assays targeting Pepper Mild Mottle Virus (PMMoV), a common fecal normalization target, displayed significant method-specific variability, complicating data comparison when normalized results are used [102].
Link to Public Health Action: The design and consistency of laboratory protocols influence whether surveillance data can trigger public health actions. A comprehensive review found that only 84 of 974 wastewater studies described public health actions, with a mere 28 incorporating strategies to facilitate action within their study designs [104]. Studies conducted by public health institutes, which often have more standardized protocols, were more likely to result in action [104].
Standardization and Quality Control Frameworks
To mitigate the confounding effects of methodological variability, leading health agencies and researchers have developed quality control frameworks and data standardization approaches.
Laboratory Controls for Quality Assurance
The CDC recommends several essential laboratory controls to ensure data quality and comparability [100].
Table 2: Essential Research Reagent Solutions for Quality Control
| Reagent / Control | Example Substances | Primary Function | Importance for Data Quality |
|---|---|---|---|
| Matrix Recovery Control | Murine coronavirus, Bovine coronavirus | Quantify virus loss during sample processing | Corrects for variable recovery efficiency; vital for cross-method comparison [100] |
| Human Fecal Normalization | Pepper Mild Mottle Virus (PMMoV), crAssphage | Estimate human fecal content in sample | Accounts for wastewater dilution and population changes [100] [101] |
| Inhibition Assessment | Synthetic SARS-CoV-2 RNA, Purified non-human coronavirus RNA | Detect substances inhibiting RT or PCR | Identifies need for extract dilution or protocol optimization [100] |
| Quantitative Measurement Controls | RNA standards of known concentration | Calibrate quantification instruments | Ensures accuracy of reported viral concentrations for RT-qPCR/ddPCR [100] |
Data Standardization Approaches
Given the practical difficulty of standardizing all laboratory methods, innovative approaches for data standardization have been proposed.
The Data Standardization Test: This approach involves distributing non-spiked, field-collected wastewater samples to different labs for analysis. The relative quantification results are used to identify and correct for systematic biases between methods, enabling data comparison without requiring method standardization [98]. This approach accurately reflects biases in routine surveillance without relying on spiked surrogates, which may not perfectly mimic native viral behavior [98].
Wastewater Viral Activity Level (WVAL): The CDC employs this metric to standardize data across different sites and laboratories. The WVAL compares current virus levels to a site-specific baseline, creating a standardized unit that facilitates comparison across geography and time. The calculation involves data validation, log-transformation, and outlier removal to enhance robustness [105].
Emerging Protocols and Technologies
The field of wastewater surveillance is rapidly evolving, with new technologies aiming to address limitations of traditional protocols.
Rapid Near-Source Testing: To overcome the 24-72 hour delays associated with traditional PCR-based testing, researchers are developing rapid, near-source tests. A 2025 study demonstrated a novel platform using Recombinase Polymerase Amplification (RPA) with fluorescent nanodiamond dipsticks, achieving a limit of detection of 7 copies per assay with 100% sensitivity and specificity in a pilot study [103]. This "lab-in-a-suitcase" solution can provide results within 2 hours, enabling rapid public health interventions [103].
Challenges in Granular Surveillance: Applying wastewater surveillance to specific buildings like schools presents unique challenges. A 2025 study found that school wastewater had markedly lower levels of both SARS-CoV-2 RNA and fecal biomarkers compared to municipal wastewater treatment plants, suggesting lower fecal input and making detection more technically challenging [56]. This highlights how surveillance scale must inform method selection, with more sensitive protocols required for near-source applications.
Laboratory protocols exert a profound influence on the quality, comparability, and public health utility of wastewater surveillance data. The evidence indicates that while method diversity presents challenges for data harmonization, strategic implementation of quality controls and data standardization approaches can effectively mitigate these issues. For researchers and public health officials, the key recommendations are: 1) Transparently document all methodological parameters, 2) Systematically implement recommended laboratory controls to quantify recovery and inhibition, and 3) Adopt data standardization practices like the Data Standardization Test or WVAL metric when integrating data from multiple sources. As the science evolves, emerging technologies like near-source rapid testing promise to expand the applications of wastewater surveillance, though they will require their own rigorous performance validation against established gold-standard methods.
Conclusion
The accurate quantification of viral load remains indispensable for clinical management and public health, yet the field is marked by significant methodological diversity and standardization challenges. The comparative analysis confirms that while RT-qPCR is a widely accessible workhorse, ddPCR offers distinct advantages in sensitivity, precision, and resistance to inhibitors, enabling absolute quantification without standard curves. The persistent interassay variability, particularly for non-HIV viruses, underscores an urgent need for widespread adoption of international standards and FDA-cleared assays. Future directions must focus on harmonizing laboratory protocols, developing novel normalization strategies for complex sample types like wastewater, and integrating advanced methods like ddPCR more broadly into clinical and research pipelines to fully realize the potential of viral load data in guiding therapeutic decisions and surveillance efforts.
References
- 1. Glossary of HIV/AIDS Terms - HIV [https://www.hiv.va.gov/provider/glossary/uv.asp]
- 2. The role of HIV viral suppression in improving individual ... [https://www.who.int/publications/i/item/9789240055179]
- 3. CROI 2025: The Challenges of Sustaining Viral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12324711/]
- 4. Nowcasting epidemic trends using hospital [https://www.nature.com/articles/s41467-025-65237-6]
- 5. Comparison of diagnostic performances of HDV-RNA ... [https://www.sciencedirect.com/science/article/pii/S1386653225000927]
- 6. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 7. Viral load monitoring for people living with HIV in the era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9202111/]
- 8. Present and Future Applications of Digital PCR in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11083499/]
- 9. Comparative Analysis of Viral Load Quantification Using ... [https://www.mdpi.com/1422-0067/26/2/725]
- 10. When to Choose Digital PCR vs. Real-Time PCR? [https://www.thermofisher.com/blog/behindthebench/when-to-choose-digital-pcr-vs-real-time-pcr/]
- 11. Droplet digital RT-PCR method for SARS-CoV-2 variants ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267190/]
- 12. dPCR vs qPCR [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-vs-qpcr]
- 13. Comparison of RT-qPCR and RT-dPCR Platforms for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8848507/]
- 14. Rapid simultaneous self-testing of HIV and HCV viral loads ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325007195]
- 15. Analytical performance and standardization of four HCV ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1594410/full]
- 16. Comparison of dried blood spot (DBS) and plasma HIV-1 viral ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02762-2]
- 17. Comparative evaluation of plasma and serum HIV-1 viral load ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0315717]
- 18. The performance of low HIV viral load values for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512948/]
- 19. Inter-Assay Variability of TROP2 Immunohistochemistry in ... [https://pubmed.ncbi.nlm.nih.gov/40914741/]
- 20. Investigating interassay variability between direct oral ... [https://www.sciencedirect.com/science/article/pii/S2475037925002237?dgcid=rss_sd_all]
- 21. The establishment of a universal standard for both viral ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02954-w]
- 22. The establishment of a universal standard for both viral ... [https://pubmed.ncbi.nlm.nih.gov/41094578/]
- 23. Quality and Regulatory Predictability: Shaping USP ... [https://www.fda.gov/drugs/news-events-human-drugs/quality-and-regulatory-predictability-shaping-usp-standards-12112025]
- 24. USP Releases First Universal Standards for Content and ... [https://nabp.pharmacy/news/news-releases/usp-releases-first-universal-standards-for-content-and-appearance-of-prescription-labels-to-promote-patient-understanding/]
- 25. Matched pairs demonstrate robustness against inter-assay ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-00956-y]
- 26. Matched pairs demonstrate robustness against inter-assay ... [https://pubmed.ncbi.nlm.nih.gov/39833966/]
- 27. Calculating Inter- and Intra-Assay Coefficients of Variability [https://salimetrics.com/calculating-inter-and-intra-assay-coefficients-of-variability/]
- 28. Comparison of Standardized Cytomegalovirus (CMV) Viral Load Thresholds in Whole Blood and Plasma of Solid Organ and Hematopoietic Stem Cell Transplant Recipients with CMV Infection and Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5570102/]
- 29. Impact of viral load kinetics and recurrent cytomegalovirus ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1600289/full]
- 30. The Accuracy of Blood Nucleic Acid Testing to Predict BK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448171/]
- 31. Advances in Epstein–Barr Virus Detection - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390056/]
- 32. Performance evaluation of the NeuMoDx™ EBV Quant ... [https://www.sciencedirect.com/science/article/pii/S0732889325002792]
- 33. Detection of human herpesvirus type 6 DNA in ... [https://www.sciencedirect.com/science/article/pii/S138665322500126X]
- 34. Comparability of CMV DNA Extraction Methods and Validation of Viral Load - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8788495/]
- 35. Comparison of the Abbott Alinity m and Qiagen Artus ... [https://www.sciencedirect.com/science/article/pii/S2772707624001735]
- 36. Detection of Herpesviruses (Predominantly HHV-6) in Patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025303/]
- 37. Immune Monitoring Goes Viral – Torque Teno Virus for ... [https://www.frontierspartnerships.org/journals/transplant-international/articles/10.3389/ti.2025.15074/full]
- 38. The potential application of digital PCR in detecting ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093425000448]
- 39. Assessing sensitivity and reproducibility of RT-ddPCR and RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8267102/]
- 40. Droplet Digital PCR or Real-Time PCR as a Method for ... [https://www.mdpi.com/1999-4915/17/6/772]
- 41. A sensitive multiplex RT-qPCR assay to detect SARS-CoV ... [https://www.medrxiv.org/content/10.1101/2025.03.31.25323652v1]
- 42. Development and clinical validation of a novel multiplex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368015/]
- 43. of reverse-transcription Comparison and droplet digital qPCR for... PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC8933867/]
- 44. Frontiers | Droplet digital RT - PCR method for SARS - CoV - 2 variants... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1635733/full]
- 45. Development of two step reverse transcription droplet ... [https://www.sciencedirect.com/science/article/abs/pii/S1344622324001469]
- 46. Development and validation of a multiplex RT-qPCR ... [https://www.sciencedirect.com/science/article/pii/S2590093525000013]
- 47. Comparison of dried blood spot (DBS) and plasma HIV-1 ... [https://pubmed.ncbi.nlm.nih.gov/40375258/]
- 48. Comparison of HIV-1 RNA level estimated with plasma and ... [https://www.sciencedirect.com/science/article/pii/S0255085721008471]
- 49. Therapeutic drug monitoring of levetiracetam – Is dried ... [https://www.sciencedirect.com/science/article/pii/S0009912025000426]
- 50. Comparing the test performance of dried-blood-spot and ... [https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0003791]
- 51. Comparing the test performance of dried-blood-spot and ... [https://pubmed.ncbi.nlm.nih.gov/41191565/]
- 52. Dried Plasma Spots (DPS) Coupled with Ultra-sensitive ... [https://www.quanterix.com/blog-dried-plasma-spots-dps-coupled-with-ultra-sensitive-biomarker-detection-advancing-alzheimers-biomarker-testing/]
- 53. Key insights for future surveillance efforts | PLOS Water [https://journals.plos.org/water/article?id=10.1371/journal.pwat.0000453]
- 54. Wastewater-Based Surveillance Is an Effective Tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9514327/]
- 55. Wastewater-Based Surveillance of SARS-CoV-2 and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474395/]
- 56. Performance and suitability of wastewater based- ... [https://www.nature.com/articles/s41598-025-16995-2]
- 57. Comparative Performance of Wastewater, Clinical, and ... [https://www.jmir.org/2025/1/e70232]
- 58. Time-series sewage metagenomics distinguishes seasonal ... [https://www.nature.com/articles/s41467-024-51957-8]
- 59. Pre-Analytical Sample Handling: What Can You Do Better? [https://bitesizebio.com/31073/pre-analytical-sample-handling/]
- 60. May 2025: Sample Stability [https://www.aniara.com/blog/may-2025-sample-stability.html]
- 61. Impact of Pre-Analytical and Analytical Variables Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8833630/]
- 62. Systematic optimisation of crude buccal swab lysate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003550/]
- 63. Characterization and Optimization of Lysis Buffer Activity [https://bio-protocol.org/exchange/minidetail?id=10784058&type=30]
- 64. Multicenter Comparison of Laboratory Performance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4481866/]
- 65. Progress in Quantitative Viral Load Testing: Variability and ... [https://pubmed.ncbi.nlm.nih.gov/27852673/]
- 66. Recommendations for assessing commutability of a ... [https://www.sciencedirect.com/science/article/pii/S0009898124023507]
- 67. Recommendations for Setting a Criterion for Assessing ... [https://www.nist.gov/publications/recommendations-setting-criterion-assessing-commutability-secondary-calibrator]
- 68. Accuracy of quantitative viral secondary standards - PubMed [https://pubmed.ncbi.nlm.nih.gov/38380932/]
- 69. A robust approach for the quantitation of viral concentration ... [https://pubmed.ncbi.nlm.nih.gov/16839272/]
- 70. The mathematics of qRT-PCR in virology [https://virologyresearchservices.com/2025/01/13/the-mathematics-of-qrt-pcr-in-virology/]
- 71. Absolute quantification of rare gene targets in limited ... [https://www.nature.com/articles/s41598-025-94115-w]
- 72. Tolerance of droplet-digital PCR versus real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4247175/]
- 73. Comparison of Droplet Digital PCR to Real-Time PCR for Quantitative Detection of Cytomegalovirus - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3553899/]
- 74. What Are the Advantages of ddPCR Over Other PCR ... [https://mogene.com/what-are-the-advantages-of-ddpcr-over-other-pcr-variants/]
- 75. A single-cell digital PCR method tailored for quantification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512710/]
- 76. Data Normalization Demystified: A Guide to Cleaner Data [https://www.flagright.com/post/data-normalization-demystified-a-guide-to-cleaner-data]
- 77. Unveiling the Power of Bias Adjustment: Enhancing ... [https://towardsdatascience.com/unveiling-the-power-of-bias-adjustment-enhancing-predictive-precision-in-imbalanced-datasets-ecad1836fc58/]
- 78. Normalization Approaches for Removing Systematic Biases ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1992440/]
- 79. Presenting Quantitative Data Graphically [https://courses.lumenlearning.com/waymakermath4libarts/chapter/presenting-quantitative-data-graphically/]
- 80. Methodological Approach for Dengue Viral Load ... [https://www.researchprotocols.org/2025/1/e71635]
- 81. Analytical and Clinical Performance of Droplet Digital PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8316104/]
- 82. qPCR vs. ddPCR: Which Is Best for You? [https://www.bioradiations.com/qpcr-vs-ddpcr-assays-select-the-best-gene-expression-analysis-method-for-your-application1125/]
- 83. Digital PCR vs. Real-Time PCR: Understanding the Key ... [https://www.labmanager.com/digital-pcr-vs-real-time-pcr-understanding-the-key-differences-33665]
- 84. Droplet Digital PCR versus qPCR for gene expression ... [https://www.nature.com/articles/s41598-017-02217-x]
- 85. Comparing the precision of two digital PCR applications for ... [https://www.nature.com/articles/s41598-025-13143-8]
- 86. Evaluating the sensitivity of droplet digital PCR for the ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1271594/full]
- 87. Clinical Significance of Quantitative Viral Load in Patients ... [https://www.sciencedirect.com/science/article/pii/S2667036423000201]
- 88. Correlation of Viral Load With the Clinical and Biochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8388060/]
- 89. Agreement and differential use of laboratory methods for ... [https://pubmed.ncbi.nlm.nih.gov/36458182/]
- 90. Agreement and differential use of laboratory methods for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1016201/full]
- 91. Quantifying the relationship between SARS-CoV-2 viral ... [https://elifesciences.org/articles/69302]
- 92. Development and validation of viral load assays to quantitate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7883709/]
- 93. Therapeutic Approaches for COVID-19: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182464/]
- 94. Comparative Performance of Three Viral Load Assays on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC87842/]
- 95. Comparative Analysis of Viral Load Quantification Using ... [https://pubmed.ncbi.nlm.nih.gov/39859446/]
- 96. Comparison of serum and plasma viral load measurements ... [https://www.sciencedirect.com/science/article/pii/S2667038022000667]
- 97. Comparative efficacy versus effectiveness of initial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2848720/]
- 98. Enabling quantitative comparison of wastewater ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969724062296]
- 99. Wastewater Surveillance of SARS-CoV-2 - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11436116/]
- 100. Wastewater Surveillance Testing Methods [https://archive.cdc.gov/www_cdc_gov/nwss/testing.html]
- 101. Analysis Methods [https://nywastewatcher.io/analysis-methods]
- 102. Harmonizing SARS-CoV-2 wastewater surveillance results ... [https://pubmed.ncbi.nlm.nih.gov/40857943/]
- 103. Towards ultra-sensitive and rapid near-source wastewater- ... [https://www.nature.com/articles/s41467-025-63192-w]
- 104. Review Wastewater surveillance studies on pathogens and ... [https://www.sciencedirect.com/science/article/pii/S0048969725016225]
- 105. CDC's Wastewater Surveillance Data Methodology [https://www.cdc.gov/nwss/data-methods.html]